User login
American Association for the Surgery of Trauma (AAST): Annual Meeting
Trauma surgeons placed intracranial pressure monitors safely
SAN FRANCISCO – Complications developed with 3% of 298 intracranial pressure monitors inserted by trauma surgeons and with 0.8% of 112 monitors placed by neurosurgeons in patients with traumatic brain injury, a statistically insignificant difference.
Mortality rates were 37% for patients in the trauma surgeon group and 30% for patients in the neurosurgeon group, a difference that also was not significant, Dr. Sadia Ilyas and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They retrospectively studied data for patients with traumatic brain injury (TBI) who received intracranial pressure monitors in 2006 through 2011 at one Level I trauma center. The trauma surgeons there had undergone training and credentialing in 2005 by neurosurgeons at the same facility for insertion of the monitors because neurosurgery coverage is not always available, explained Dr. Ilyas of Wright State University, Dayton, Ohio.
Complications in this series consisted of device malfunction or dislodgement, with no major or life-threatening complications.
Trauma surgeons in the training program each viewed two 10-minute instructional videos, were proctored by a neurosurgeon in a cadaver lab, and placed three monitors in patients under proctoring by a neurosurgeon. General surgery residents received similar training but were not credentialed to place intracranial pressure monitors without direct supervision.
Guidelines from the Brain Trauma Foundation recommend intracranial pressure monitoring in patients with severe TBI who have a Glasgow Coma Scale score of 8 or lower and an abnormal CT scan. Monitoring typically involves placement of a ventriculostomy or an intracranial pressure intraparenchymal monitor (bolt monitor).
In the study, 97% of all monitors placed were parenchymal monitors. Among those placed by neurosurgeons, 12% were ventriculostomies, which have the added advantage of therapeutic use but are more challenging to insert. "It is our view that placement of ICP parenchymal monitors is a more reasonable alternative for non-neurosurgeons," she said.
Six previous studies of 904 intracranial pressure monitors inserted by non-neurosurgeons found complication rates of 0%-8% with parenchymal monitors and 15% with ventriculostomy.
Each year in the United States approximately 200,000 people are hospitalized for TBI and 50,000 die from TBI. In 2010, an estimated 4,400 neurosurgeons were actively practicing in the United States (1.4 for every 100,000 residents), not all practiced trauma care, and a third were older than 55 years, she said.
Dr. Ilyas reported having no financial disclosures.
On Twitter @sherryboschert
These results have essentially been published before in other studies, and this paper doesn’t break any new ground.
I want to drive home the point that it is important, at least in my practice, to try to use ventriculostomy as the first line of monitoring because you can use it as a therapeutic tool to drain cerebrospinal fluid as well as just monitor. I do use parenchymal monitors but I can’t cannulate the ventricle.
A bigger issue is what to do with the information that you get from these monitors. Regardless of who puts these things in, someone needs to know how to treat the patients. Personally, I’ve been dismayed by the trend in recent years for so-called neuro critical care doctors to focus on things like temperature and serum sodium. It seems like very few intensivists who care for TBI patients really understand cerebral metabolism, cerebral blood flow, cerebral pathophysiology, and related processes.
As Dr. Ilyas and her colleagues have shown, the technical insertion of these devices is really not that difficult, but knowing the indications for when to put them in and when not to put them in, knowing how to interpret the data, and integrating the care of these patients into the neuro service are much more difficult things to do.
One problem with this paper is that it describes only short-term periprocedural complications. The real standard for measuring efficacy of interventions in TBI patients is long-term follow-up, which historically has been 6 months from injury and now more recent trials are using 12 months or even longer.
Dr. Alex B. Valadka is a neurosurgeon at the Seton Brain and Spine Institute, Austin, Tex. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
These results have essentially been published before in other studies, and this paper doesn’t break any new ground.
I want to drive home the point that it is important, at least in my practice, to try to use ventriculostomy as the first line of monitoring because you can use it as a therapeutic tool to drain cerebrospinal fluid as well as just monitor. I do use parenchymal monitors but I can’t cannulate the ventricle.
A bigger issue is what to do with the information that you get from these monitors. Regardless of who puts these things in, someone needs to know how to treat the patients. Personally, I’ve been dismayed by the trend in recent years for so-called neuro critical care doctors to focus on things like temperature and serum sodium. It seems like very few intensivists who care for TBI patients really understand cerebral metabolism, cerebral blood flow, cerebral pathophysiology, and related processes.
As Dr. Ilyas and her colleagues have shown, the technical insertion of these devices is really not that difficult, but knowing the indications for when to put them in and when not to put them in, knowing how to interpret the data, and integrating the care of these patients into the neuro service are much more difficult things to do.
One problem with this paper is that it describes only short-term periprocedural complications. The real standard for measuring efficacy of interventions in TBI patients is long-term follow-up, which historically has been 6 months from injury and now more recent trials are using 12 months or even longer.
Dr. Alex B. Valadka is a neurosurgeon at the Seton Brain and Spine Institute, Austin, Tex. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
These results have essentially been published before in other studies, and this paper doesn’t break any new ground.
I want to drive home the point that it is important, at least in my practice, to try to use ventriculostomy as the first line of monitoring because you can use it as a therapeutic tool to drain cerebrospinal fluid as well as just monitor. I do use parenchymal monitors but I can’t cannulate the ventricle.
A bigger issue is what to do with the information that you get from these monitors. Regardless of who puts these things in, someone needs to know how to treat the patients. Personally, I’ve been dismayed by the trend in recent years for so-called neuro critical care doctors to focus on things like temperature and serum sodium. It seems like very few intensivists who care for TBI patients really understand cerebral metabolism, cerebral blood flow, cerebral pathophysiology, and related processes.
As Dr. Ilyas and her colleagues have shown, the technical insertion of these devices is really not that difficult, but knowing the indications for when to put them in and when not to put them in, knowing how to interpret the data, and integrating the care of these patients into the neuro service are much more difficult things to do.
One problem with this paper is that it describes only short-term periprocedural complications. The real standard for measuring efficacy of interventions in TBI patients is long-term follow-up, which historically has been 6 months from injury and now more recent trials are using 12 months or even longer.
Dr. Alex B. Valadka is a neurosurgeon at the Seton Brain and Spine Institute, Austin, Tex. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Complications developed with 3% of 298 intracranial pressure monitors inserted by trauma surgeons and with 0.8% of 112 monitors placed by neurosurgeons in patients with traumatic brain injury, a statistically insignificant difference.
Mortality rates were 37% for patients in the trauma surgeon group and 30% for patients in the neurosurgeon group, a difference that also was not significant, Dr. Sadia Ilyas and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They retrospectively studied data for patients with traumatic brain injury (TBI) who received intracranial pressure monitors in 2006 through 2011 at one Level I trauma center. The trauma surgeons there had undergone training and credentialing in 2005 by neurosurgeons at the same facility for insertion of the monitors because neurosurgery coverage is not always available, explained Dr. Ilyas of Wright State University, Dayton, Ohio.
Complications in this series consisted of device malfunction or dislodgement, with no major or life-threatening complications.
Trauma surgeons in the training program each viewed two 10-minute instructional videos, were proctored by a neurosurgeon in a cadaver lab, and placed three monitors in patients under proctoring by a neurosurgeon. General surgery residents received similar training but were not credentialed to place intracranial pressure monitors without direct supervision.
Guidelines from the Brain Trauma Foundation recommend intracranial pressure monitoring in patients with severe TBI who have a Glasgow Coma Scale score of 8 or lower and an abnormal CT scan. Monitoring typically involves placement of a ventriculostomy or an intracranial pressure intraparenchymal monitor (bolt monitor).
In the study, 97% of all monitors placed were parenchymal monitors. Among those placed by neurosurgeons, 12% were ventriculostomies, which have the added advantage of therapeutic use but are more challenging to insert. "It is our view that placement of ICP parenchymal monitors is a more reasonable alternative for non-neurosurgeons," she said.
Six previous studies of 904 intracranial pressure monitors inserted by non-neurosurgeons found complication rates of 0%-8% with parenchymal monitors and 15% with ventriculostomy.
Each year in the United States approximately 200,000 people are hospitalized for TBI and 50,000 die from TBI. In 2010, an estimated 4,400 neurosurgeons were actively practicing in the United States (1.4 for every 100,000 residents), not all practiced trauma care, and a third were older than 55 years, she said.
Dr. Ilyas reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Complications developed with 3% of 298 intracranial pressure monitors inserted by trauma surgeons and with 0.8% of 112 monitors placed by neurosurgeons in patients with traumatic brain injury, a statistically insignificant difference.
Mortality rates were 37% for patients in the trauma surgeon group and 30% for patients in the neurosurgeon group, a difference that also was not significant, Dr. Sadia Ilyas and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They retrospectively studied data for patients with traumatic brain injury (TBI) who received intracranial pressure monitors in 2006 through 2011 at one Level I trauma center. The trauma surgeons there had undergone training and credentialing in 2005 by neurosurgeons at the same facility for insertion of the monitors because neurosurgery coverage is not always available, explained Dr. Ilyas of Wright State University, Dayton, Ohio.
Complications in this series consisted of device malfunction or dislodgement, with no major or life-threatening complications.
Trauma surgeons in the training program each viewed two 10-minute instructional videos, were proctored by a neurosurgeon in a cadaver lab, and placed three monitors in patients under proctoring by a neurosurgeon. General surgery residents received similar training but were not credentialed to place intracranial pressure monitors without direct supervision.
Guidelines from the Brain Trauma Foundation recommend intracranial pressure monitoring in patients with severe TBI who have a Glasgow Coma Scale score of 8 or lower and an abnormal CT scan. Monitoring typically involves placement of a ventriculostomy or an intracranial pressure intraparenchymal monitor (bolt monitor).
In the study, 97% of all monitors placed were parenchymal monitors. Among those placed by neurosurgeons, 12% were ventriculostomies, which have the added advantage of therapeutic use but are more challenging to insert. "It is our view that placement of ICP parenchymal monitors is a more reasonable alternative for non-neurosurgeons," she said.
Six previous studies of 904 intracranial pressure monitors inserted by non-neurosurgeons found complication rates of 0%-8% with parenchymal monitors and 15% with ventriculostomy.
Each year in the United States approximately 200,000 people are hospitalized for TBI and 50,000 die from TBI. In 2010, an estimated 4,400 neurosurgeons were actively practicing in the United States (1.4 for every 100,000 residents), not all practiced trauma care, and a third were older than 55 years, she said.
Dr. Ilyas reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: Complications developed with 3% of monitors placed by trauma surgeons and 0.8% placed by neurosurgeons.
Data source: Retrospective review of 410 patients with TBI who received intracranial pressure monitors in 2006-2011.
Disclosures: Dr. Ilyas reported having no financial disclosures.
Trauma center rankings differ by mortality, morbidity
SAN FRANCISCO – Trauma centers are ranked on the basis of in-hospital mortality rates, but pay-for-performance programs will benchmark them based on in-hospital complications – and there’s not good concordance between the two measures, a study of data from 248 trauma centers suggests.
Investigators used data on 449,743 patients aged 16 years or older who had blunt/penetrating injuries and an Injury Severity Score of 9 or higher to generate risk-adjusted, observed-to-expected mortality rates for each trauma center They ranked each facility based on mortality rate as a high-performing, average, or low-performing center and used complication rates to rank them again based on observed-to-expected morbidity ratios.
Only 40% of centers received the same benchmark using these two measures, Dr. Zain G. Hashmi and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Dividing each performance ranking into quintiles, the two rankings diverged by at least one quintile for 79% of trauma centers. Only 21% were assigned the same quintile rank in the mortality benchmarking as in the morbidity benchmarking. A two-quintile divergence in rankings was noted in 21%, and a three-quintile difference in 23%, said Dr. Hashmi, a research fellow at Johns Hopkins University, Baltimore.
Overall, the unadjusted mortality rate was 7% and the morbidity rate was 10%. The most frequent complications were pneumonia in 4%, acute respiratory distress syndrome in 2%, and deep venous thrombosis in 2%.
The complications used for the morbidity benchmarking included pneumonia, deep venous thrombosis, acute respiratory distress syndrome, acute renal failure, sepsis, pulmonary embolism, decubitus ulcer, surgical site infection, myocardial infarction, cardiac arrest, unplanned intubation, and stroke.
The Centers for Medicare and Medicaid Services is implementing pay-for-performance programs in the public health sector nationwide under the Affordable Care Act to incentivize high quality of care and penalize low quality of care. The programs may soon be extended to trauma care, which could incorrectly penalize centers that are the best performers based on mortality benchmarks, he said.
"We need to develop more appropriate measures of trauma quality before pay-for-performance" programs come to trauma centers, perhaps using multiple quality indicators such as mortality, length of stay, complications, and failure to rescue, he said.
Data for the study came from the National Trauma Data Bank for 2007-2010.
Dr. Hashmi reported having no financial disclosures.
On Twitter @sherryboschert
The authors reached the very predictable conclusion that the two benchmarking approaches have no correlation whatsoever. They did not come quite as close to embracing the other obvious conclusion that, in fact, neither benchmark encompasses, or perhaps even approximates, the quality of care given at an individual center. And they don’t really offer us an alternative.
We’ve been seeking the best way to measure the quality of care for the injured patient for decades, long before the concepts "pay for performance" or "value-based purchasing" became something of our daily lives. One thing we certainly learned is that quality is a complex, nuanced, and maybe even an elusive concept, sort of like one of Plato’s forms – we can’t see it directly, and we have to figure out what it is by the shadows it casts.
 |
|
Unfortunately, before you can really measure something, you do have to know a little bit about what it is you’re trying to measure. Otherwise, you’re likely to pick the wrong tool. For reasons of obvious practicality, the approach that is most commonly taken, just like the approach in this paper, is to measure the things we can, perhaps in very, very sophisticated ways, and then try somehow to take that result and connect it in some way to that elusive concept, quality.
If nothing else, this paper illustrates the weakness inherent in that approach. Without going into the potential methodological flaws, I would submit that the hypothesis is poorly focused. There was no observed concordance between mortality and morbidity because there is no reason to expect that there should be. They measure entirely different things, and neither one of those things is necessarily very much connected to quality, which is really what we’d like to get a handle on.
The better approach, I’d suggest, is to postulate, a priori, a definition of what quality might be or at least a set of characteristics that might represent quality, and then set about to measure against that model.
Dr. Robert Winchell is a surgeon at Maine Medical Center in Portland. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
The authors reached the very predictable conclusion that the two benchmarking approaches have no correlation whatsoever. They did not come quite as close to embracing the other obvious conclusion that, in fact, neither benchmark encompasses, or perhaps even approximates, the quality of care given at an individual center. And they don’t really offer us an alternative.
We’ve been seeking the best way to measure the quality of care for the injured patient for decades, long before the concepts "pay for performance" or "value-based purchasing" became something of our daily lives. One thing we certainly learned is that quality is a complex, nuanced, and maybe even an elusive concept, sort of like one of Plato’s forms – we can’t see it directly, and we have to figure out what it is by the shadows it casts.
 |
|
Unfortunately, before you can really measure something, you do have to know a little bit about what it is you’re trying to measure. Otherwise, you’re likely to pick the wrong tool. For reasons of obvious practicality, the approach that is most commonly taken, just like the approach in this paper, is to measure the things we can, perhaps in very, very sophisticated ways, and then try somehow to take that result and connect it in some way to that elusive concept, quality.
If nothing else, this paper illustrates the weakness inherent in that approach. Without going into the potential methodological flaws, I would submit that the hypothesis is poorly focused. There was no observed concordance between mortality and morbidity because there is no reason to expect that there should be. They measure entirely different things, and neither one of those things is necessarily very much connected to quality, which is really what we’d like to get a handle on.
The better approach, I’d suggest, is to postulate, a priori, a definition of what quality might be or at least a set of characteristics that might represent quality, and then set about to measure against that model.
Dr. Robert Winchell is a surgeon at Maine Medical Center in Portland. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
The authors reached the very predictable conclusion that the two benchmarking approaches have no correlation whatsoever. They did not come quite as close to embracing the other obvious conclusion that, in fact, neither benchmark encompasses, or perhaps even approximates, the quality of care given at an individual center. And they don’t really offer us an alternative.
We’ve been seeking the best way to measure the quality of care for the injured patient for decades, long before the concepts "pay for performance" or "value-based purchasing" became something of our daily lives. One thing we certainly learned is that quality is a complex, nuanced, and maybe even an elusive concept, sort of like one of Plato’s forms – we can’t see it directly, and we have to figure out what it is by the shadows it casts.
 |
|
Unfortunately, before you can really measure something, you do have to know a little bit about what it is you’re trying to measure. Otherwise, you’re likely to pick the wrong tool. For reasons of obvious practicality, the approach that is most commonly taken, just like the approach in this paper, is to measure the things we can, perhaps in very, very sophisticated ways, and then try somehow to take that result and connect it in some way to that elusive concept, quality.
If nothing else, this paper illustrates the weakness inherent in that approach. Without going into the potential methodological flaws, I would submit that the hypothesis is poorly focused. There was no observed concordance between mortality and morbidity because there is no reason to expect that there should be. They measure entirely different things, and neither one of those things is necessarily very much connected to quality, which is really what we’d like to get a handle on.
The better approach, I’d suggest, is to postulate, a priori, a definition of what quality might be or at least a set of characteristics that might represent quality, and then set about to measure against that model.
Dr. Robert Winchell is a surgeon at Maine Medical Center in Portland. These are excerpts of his remarks as discussant of the study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Trauma centers are ranked on the basis of in-hospital mortality rates, but pay-for-performance programs will benchmark them based on in-hospital complications – and there’s not good concordance between the two measures, a study of data from 248 trauma centers suggests.
Investigators used data on 449,743 patients aged 16 years or older who had blunt/penetrating injuries and an Injury Severity Score of 9 or higher to generate risk-adjusted, observed-to-expected mortality rates for each trauma center They ranked each facility based on mortality rate as a high-performing, average, or low-performing center and used complication rates to rank them again based on observed-to-expected morbidity ratios.
Only 40% of centers received the same benchmark using these two measures, Dr. Zain G. Hashmi and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Dividing each performance ranking into quintiles, the two rankings diverged by at least one quintile for 79% of trauma centers. Only 21% were assigned the same quintile rank in the mortality benchmarking as in the morbidity benchmarking. A two-quintile divergence in rankings was noted in 21%, and a three-quintile difference in 23%, said Dr. Hashmi, a research fellow at Johns Hopkins University, Baltimore.
Overall, the unadjusted mortality rate was 7% and the morbidity rate was 10%. The most frequent complications were pneumonia in 4%, acute respiratory distress syndrome in 2%, and deep venous thrombosis in 2%.
The complications used for the morbidity benchmarking included pneumonia, deep venous thrombosis, acute respiratory distress syndrome, acute renal failure, sepsis, pulmonary embolism, decubitus ulcer, surgical site infection, myocardial infarction, cardiac arrest, unplanned intubation, and stroke.
The Centers for Medicare and Medicaid Services is implementing pay-for-performance programs in the public health sector nationwide under the Affordable Care Act to incentivize high quality of care and penalize low quality of care. The programs may soon be extended to trauma care, which could incorrectly penalize centers that are the best performers based on mortality benchmarks, he said.
"We need to develop more appropriate measures of trauma quality before pay-for-performance" programs come to trauma centers, perhaps using multiple quality indicators such as mortality, length of stay, complications, and failure to rescue, he said.
Data for the study came from the National Trauma Data Bank for 2007-2010.
Dr. Hashmi reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Trauma centers are ranked on the basis of in-hospital mortality rates, but pay-for-performance programs will benchmark them based on in-hospital complications – and there’s not good concordance between the two measures, a study of data from 248 trauma centers suggests.
Investigators used data on 449,743 patients aged 16 years or older who had blunt/penetrating injuries and an Injury Severity Score of 9 or higher to generate risk-adjusted, observed-to-expected mortality rates for each trauma center They ranked each facility based on mortality rate as a high-performing, average, or low-performing center and used complication rates to rank them again based on observed-to-expected morbidity ratios.
Only 40% of centers received the same benchmark using these two measures, Dr. Zain G. Hashmi and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Dividing each performance ranking into quintiles, the two rankings diverged by at least one quintile for 79% of trauma centers. Only 21% were assigned the same quintile rank in the mortality benchmarking as in the morbidity benchmarking. A two-quintile divergence in rankings was noted in 21%, and a three-quintile difference in 23%, said Dr. Hashmi, a research fellow at Johns Hopkins University, Baltimore.
Overall, the unadjusted mortality rate was 7% and the morbidity rate was 10%. The most frequent complications were pneumonia in 4%, acute respiratory distress syndrome in 2%, and deep venous thrombosis in 2%.
The complications used for the morbidity benchmarking included pneumonia, deep venous thrombosis, acute respiratory distress syndrome, acute renal failure, sepsis, pulmonary embolism, decubitus ulcer, surgical site infection, myocardial infarction, cardiac arrest, unplanned intubation, and stroke.
The Centers for Medicare and Medicaid Services is implementing pay-for-performance programs in the public health sector nationwide under the Affordable Care Act to incentivize high quality of care and penalize low quality of care. The programs may soon be extended to trauma care, which could incorrectly penalize centers that are the best performers based on mortality benchmarks, he said.
"We need to develop more appropriate measures of trauma quality before pay-for-performance" programs come to trauma centers, perhaps using multiple quality indicators such as mortality, length of stay, complications, and failure to rescue, he said.
Data for the study came from the National Trauma Data Bank for 2007-2010.
Dr. Hashmi reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: Only 40% of trauma centers received the same ranking when judged by mortality or morbidity rates.
Data source: Retrospective analysis that ranked 238 centers as high, average, or low performing, based on data on 449,743 patients with blunt/penetrating injuries and an Injury Severity Score of 9 or higher.
Disclosures: Dr. Hashmi reported having no financial disclosures.
Blunt trauma outcomes improved by early transfusion
SAN FRANCISCO – Giving patients severely injured by blunt trauma a blood transfusion before they arrived at a trauma center was associated with a 95% reduction in deaths within 24 hours and a 64% reduction in deaths within 30 days, a retrospective study of 1,415 patients found.
Transfusion before arrival at the trauma center also was associated with an 88% reduction in the incidence of trauma-induced coagulopathy, Dr. Joshua B. Brown and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They analyzed data from the prospective Inflammation and Host Response to Injury cohort study for patients with blunt injury in hemorrhagic shock who arrived at a trauma center within 2 hours of injury, 50 of whom received a blood transfusion before arrival. The investigators found that prearrival blood transfusion was associated with better outcomes after controlling for the effects of demographics, time to the trauma center, the severity of injury and shock, early resuscitation, and other confounders.
These preliminary data are compelling but require prospective validation, said Dr. Brown of the University of Pittsburgh.
Prehospital resuscitation of patients severely injured by blunt trauma has focused on use of crystalloids, and the next logical step is to bring blood-based resuscitation to prehospital settings, he said. Hemorrhage and coagulopathy have been major causes of death in blunt trauma patients.
In the study, patients who got a transfusion before arrival at the trauma center received a median of 1.3 units of blood prearrival. They were more likely to be hypotensive and to have a lower base deficit compared with patients who were not transfused before arrival, suggesting a higher severity of injury and shock in the transfusion group, he said. The groups did not differ significantly in age, gender, or Injury Severity Score.
Patients who received a transfusion before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
In a subsequent matched cohort analysis of 113 patients from the study, those receiving a pre–trauma center transfusion (35 patients) had a 98% reduction in mortality at 24 hours, an 88% reduction in 30-day mortality, and a 99% reduction in the risk of trauma-induced coagulopathy, Dr. Brown reported.
Dr. Brown reported having no financial disclosures.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
The role of blood-based resuscitation in salvaging the severely injured patient remains an area of intense scrutiny. We spend a lot of time at meetings talking about this very subject.
The authors note that there are multiple studies that have looked at blood-based resuscitation, including things like blood to plasma and platelet ratios, the timing of blood product transfusion, and the use of institutional transfusion protocols. Sometimes they give completely different answers.
Despite these variabilities, I think what we are seeing is that early use of blood products in the correct patient population does result in better survival. It’s a logical question for the trauma researcher to then ask, how early should blood be given? How early can blood be given?
The authors identified over 1,400 patients who met inclusion criteria. Ultimately, they demonstrated a statistically significant benefit to prehospital transfusion in terms of both 24-hour and 30-day mortality as well as trauma-induced coagulopathy. These are very intriguing results.
They state that the median volume of blood transfused prior to reaching the trauma center was 1.3 units, ranging from 1-2.3 units. I wonder how they can explain the fact that 1 unit of prehospital blood resulted in such a significant difference in mortality and coagulopathy. That is a lot of bang for your buck.
The low numbers in the prehospital transfusion group raise some questions, but I do agree that this is interesting research and it is worthy of prospective study.
Dr. Stephanie Savage is a surgeon at the University of Tennessee, Memphis. These are excerpts of her remarks as discussant of the study at the meeting. She reported having no financial disclosures.
The role of blood-based resuscitation in salvaging the severely injured patient remains an area of intense scrutiny. We spend a lot of time at meetings talking about this very subject.
The authors note that there are multiple studies that have looked at blood-based resuscitation, including things like blood to plasma and platelet ratios, the timing of blood product transfusion, and the use of institutional transfusion protocols. Sometimes they give completely different answers.
Despite these variabilities, I think what we are seeing is that early use of blood products in the correct patient population does result in better survival. It’s a logical question for the trauma researcher to then ask, how early should blood be given? How early can blood be given?
The authors identified over 1,400 patients who met inclusion criteria. Ultimately, they demonstrated a statistically significant benefit to prehospital transfusion in terms of both 24-hour and 30-day mortality as well as trauma-induced coagulopathy. These are very intriguing results.
They state that the median volume of blood transfused prior to reaching the trauma center was 1.3 units, ranging from 1-2.3 units. I wonder how they can explain the fact that 1 unit of prehospital blood resulted in such a significant difference in mortality and coagulopathy. That is a lot of bang for your buck.
The low numbers in the prehospital transfusion group raise some questions, but I do agree that this is interesting research and it is worthy of prospective study.
Dr. Stephanie Savage is a surgeon at the University of Tennessee, Memphis. These are excerpts of her remarks as discussant of the study at the meeting. She reported having no financial disclosures.
The role of blood-based resuscitation in salvaging the severely injured patient remains an area of intense scrutiny. We spend a lot of time at meetings talking about this very subject.
The authors note that there are multiple studies that have looked at blood-based resuscitation, including things like blood to plasma and platelet ratios, the timing of blood product transfusion, and the use of institutional transfusion protocols. Sometimes they give completely different answers.
Despite these variabilities, I think what we are seeing is that early use of blood products in the correct patient population does result in better survival. It’s a logical question for the trauma researcher to then ask, how early should blood be given? How early can blood be given?
The authors identified over 1,400 patients who met inclusion criteria. Ultimately, they demonstrated a statistically significant benefit to prehospital transfusion in terms of both 24-hour and 30-day mortality as well as trauma-induced coagulopathy. These are very intriguing results.
They state that the median volume of blood transfused prior to reaching the trauma center was 1.3 units, ranging from 1-2.3 units. I wonder how they can explain the fact that 1 unit of prehospital blood resulted in such a significant difference in mortality and coagulopathy. That is a lot of bang for your buck.
The low numbers in the prehospital transfusion group raise some questions, but I do agree that this is interesting research and it is worthy of prospective study.
Dr. Stephanie Savage is a surgeon at the University of Tennessee, Memphis. These are excerpts of her remarks as discussant of the study at the meeting. She reported having no financial disclosures.
SAN FRANCISCO – Giving patients severely injured by blunt trauma a blood transfusion before they arrived at a trauma center was associated with a 95% reduction in deaths within 24 hours and a 64% reduction in deaths within 30 days, a retrospective study of 1,415 patients found.
Transfusion before arrival at the trauma center also was associated with an 88% reduction in the incidence of trauma-induced coagulopathy, Dr. Joshua B. Brown and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They analyzed data from the prospective Inflammation and Host Response to Injury cohort study for patients with blunt injury in hemorrhagic shock who arrived at a trauma center within 2 hours of injury, 50 of whom received a blood transfusion before arrival. The investigators found that prearrival blood transfusion was associated with better outcomes after controlling for the effects of demographics, time to the trauma center, the severity of injury and shock, early resuscitation, and other confounders.
These preliminary data are compelling but require prospective validation, said Dr. Brown of the University of Pittsburgh.
Prehospital resuscitation of patients severely injured by blunt trauma has focused on use of crystalloids, and the next logical step is to bring blood-based resuscitation to prehospital settings, he said. Hemorrhage and coagulopathy have been major causes of death in blunt trauma patients.
In the study, patients who got a transfusion before arrival at the trauma center received a median of 1.3 units of blood prearrival. They were more likely to be hypotensive and to have a lower base deficit compared with patients who were not transfused before arrival, suggesting a higher severity of injury and shock in the transfusion group, he said. The groups did not differ significantly in age, gender, or Injury Severity Score.
Patients who received a transfusion before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
In a subsequent matched cohort analysis of 113 patients from the study, those receiving a pre–trauma center transfusion (35 patients) had a 98% reduction in mortality at 24 hours, an 88% reduction in 30-day mortality, and a 99% reduction in the risk of trauma-induced coagulopathy, Dr. Brown reported.
Dr. Brown reported having no financial disclosures.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
SAN FRANCISCO – Giving patients severely injured by blunt trauma a blood transfusion before they arrived at a trauma center was associated with a 95% reduction in deaths within 24 hours and a 64% reduction in deaths within 30 days, a retrospective study of 1,415 patients found.
Transfusion before arrival at the trauma center also was associated with an 88% reduction in the incidence of trauma-induced coagulopathy, Dr. Joshua B. Brown and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
They analyzed data from the prospective Inflammation and Host Response to Injury cohort study for patients with blunt injury in hemorrhagic shock who arrived at a trauma center within 2 hours of injury, 50 of whom received a blood transfusion before arrival. The investigators found that prearrival blood transfusion was associated with better outcomes after controlling for the effects of demographics, time to the trauma center, the severity of injury and shock, early resuscitation, and other confounders.
These preliminary data are compelling but require prospective validation, said Dr. Brown of the University of Pittsburgh.
Prehospital resuscitation of patients severely injured by blunt trauma has focused on use of crystalloids, and the next logical step is to bring blood-based resuscitation to prehospital settings, he said. Hemorrhage and coagulopathy have been major causes of death in blunt trauma patients.
In the study, patients who got a transfusion before arrival at the trauma center received a median of 1.3 units of blood prearrival. They were more likely to be hypotensive and to have a lower base deficit compared with patients who were not transfused before arrival, suggesting a higher severity of injury and shock in the transfusion group, he said. The groups did not differ significantly in age, gender, or Injury Severity Score.
Patients who received a transfusion before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
In a subsequent matched cohort analysis of 113 patients from the study, those receiving a pre–trauma center transfusion (35 patients) had a 98% reduction in mortality at 24 hours, an 88% reduction in 30-day mortality, and a 99% reduction in the risk of trauma-induced coagulopathy, Dr. Brown reported.
Dr. Brown reported having no financial disclosures.
sboschert@frontlinemedcom.com
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: Patients transfused before arrival at a trauma center showed a 95% lower 24-hour mortality rate, a 64% lower 30-day mortality rate, and an 88% lower risk of trauma-induced coagulopathy.
Data source: Secondary retrospective analysis of data from a prospective cohort study on 1,415 patients with blunt injury and hemorrhagic shock who arrived at a trauma center within 2 hours of injury.
Disclosures: Dr. Brown reported having no financial disclosures.
Mixed results with angiography for splenic injuries
SAN FRANCISCO – Trauma centers that nonselectively performed angiography on patients with high-grade blunt splenic injury did not significantly reduce the likelihood of delayed splenectomy in a retrospective analysis of data on 6,870 patients treated at 267 hospitals.
On an individual patient level, however, use of angiography was associated with a reduced risk of delayed splenectomy (more than 6 hours after admission) after researchers controlled for the influence of multiple other factors, Dr. Ben L. Zarzaur and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
These somewhat conflicting findings suggest that "nonselective protocol-driven use of angiography at the hospital in the setting of high-grade blunt splenic injury does not benefit in terms of splenic salvage. Angiography use should be tailored to the individual patient," said Dr. Zarzaur of the University of Tennessee, Memphis.
"Attention should be paid to overall injury severity and splenic injury severity" because more severe injuries were associated with delayed splenectomy in the study, he said, adding, "Particular attention should be considered for screening for splenic vascular abnormalities."
The investigators used data from the National Trauma Data Bank (NTDB) on adults treated for high-grade blunt splenic injury at Level I or II trauma centers that admitted at least 10 such patients in 2007-2010, with high-grade injury defined as Abbreviated Injury Scale grade 3 or higher. They stratified hospital angiography use as none, low (in less than 20% of patients with high-grade blunt splenic injury), or high (in 20% or more of these patients).
Approximately 30% of patients at high-angiography centers underwent urgent splenectomy, compared with 33%-36% at hospitals with no or low-angiography use, a difference that was statistically significant. While the likelihood of a delayed splenectomy was 33% higher at low-angiography hospitals and 49% higher at hospitals without angiography, compared with high-angiography hospitals, these differences were not significant, Dr. Zarzaur reported.
The investigators used the classification of hospitals – no-, low-, or high-angiography use – to represent the three schools of thought that have developed over the past few decades regarding angiography for patients with blunt splenic injury who do not undergo immediate urgent splenectomy. The minimalist school of thought recommends using observation, not angiography for blunt splenic injury. The maximalist school of thought favors protocol-driven use of angiography for patients with certain grades of spleen injury. In between, physicians who favor a selective strategy use CT or clinical criteria or both to try and identify patients at high risk for delayed splenectomy, and reserve the risks of angiography for those patients, he said.
They chose a cutoff of 20% angiography use in patients with high-grade blunt splenic injury to discriminate between low- and high-angiography use because that represented the 90th percentile for all trauma centers in the study.
Nine percent of patients were treated at hospitals that did not use angiography for blunt splenic injury, 66% at low-angiography hospitals, and 25% at high-angiography hospitals.
Patients with grade 5 blunt splenic injury were more than twice as likely to need delayed splenectomy, compared with patients with grade 3 or 4 injury. Higher overall Injury Severity Scores (10 or higher) also doubled the risk for delayed splenectomy.
Patients with grades 4 or 5 blunt splenic injury were significantly more likely to undergo angiography at high-angiography centers than at low-angiography centers. High-angiography centers were more likely than were low-angiography centers to remove spleens with grade 5 injury after angiography, though this difference did not reach statistical significance.
Continuing controversy around the use of angiography for blunt splenic injury is illustrated by a 2011 survey of members of the American Association for the Surgery of Trauma. Members favored observation, not angiography, for grades 1 and 2 spleen injuries but showed no consensus on higher-grade injuries (J. Trauma 2011;70:1026-31).
A recent study of 1,275 patients treated for blunt splenic injury at four trauma centers that showed a significantly better chance of saving the spleen at hospitals with higher use of splenic artery embolization, especially in patients with higher-grade splenic injury (J. Trauma Acute Care Surg. 2013;75:69-74).
The current study excluded patients who died on arrival at the hospital, patients who were admitted more than 24 hours after injury, and patients who underwent splenectomy within 6 hours of admission (early splenectomy).
Dr. Zarzaur reported having no financial disclosures.
On Twitter @sherryboschert
Almost 20 years after the initial description and 30 years after we began using splenic angiography in the management of blunt splenic injury, why is it that we simply can’t settle this question? When is splenic angiography and/or catheter therapy useful in high-grade injuries?
In this study, the authors have reviewed the National Trauma Data Bank (NTDB) and have demonstrated that, at hospitals that use angiography more frequently than other hospitals, the rate of delayed splenectomy in high-grade splenic injury (defined as grades 3-5) is not different. They suggest that angiography should be selective, with particular attention to screening for vascular abnormalities.
 |
|
The authors collected information on both angiography and angiography with embolization. However, in the manuscript and the talk, they only refer to high-angiography centers. This seems to me to be a fundamental problem. This is particularly true because recent data from Jacksonville suggest that embolization of truly high-grade injury such as grade 4 injuries (even in the absence of blush) improves the salvage rate of nonoperative management.
In addition, the authors selected 20% as their cutoff for high- and low-angiography centers because 20% represented the 90th percentile of centers with regard to angiography use. I think that’s French for "it made the data analyzable." However, 20% is relatively low. If the authors wish to look at nonselective angiography they should look at us. We’re maximalists. We do angiography on 100% of patients with grades 3, 4 and 5 injuries. That’s nonselective use of angiography.
The intelligent use of this technique requires interpretation of CT and then the details of the patient presentation. For instance, a grade 4 splenic injury with or without blush but no hemoperitoneum and a totally stable patient is, in my mind, amenable to catheter therapy. Another patient with a grade 4 injury and reactive extravasation outside of the spleen and a huge peritoneum is probably best served by operative exploration. Both are grade 4 injuries, but the patients are fundamentally different.
The authors’ conclusions suggest that there is a relationship between splenic vascular injury identified on CT and success or failure of nonoperative management. This is clearly the authors’ prejudice, as they have published these findings a number of times. We’ve known for years, thanks to work from the authors’ institution, that expectant management of a patient with blush on CT fails 70% of the time and a significant number of the blushes are seen on day 3 but not day 1. Since the authors have absolutely no information on the presence or absence of blush in this data set, I fail to see how that can be one of their conclusions.
How, then, can we make sense of this? I believe the answer is in the manuscript’s last paragraph, which begins, "Another limitation of this study stems from the limitations of the NTDB." There’s little doubt that the NTDB can record an accurate snapshot of practice in the United States, but in my mind, it lacks the specificity to really answer the question, when is splenic angiography useful in high-grade injuries?
The authors have no information on presence of absence of blush, hemodynamic status other than at admission, blood transfusion rate, or technique of embolization, and they recognize that some of the data may not be accurate. I just don’t believe that the NTDB can actually answer this question.
In the end, rules are rarely helpful in the care of patients. Intelligent application of innovative techniques cannot solely be governed by rules. Perhaps the take-home message here is that the use of angiography and embolization to treat higher-grade splenic injuries is perhaps not something that everybody should be using. It may be that this technique is best preserved for high-volume centers with a real interest and a real expertise in this subject.
Dr. Thomas M. Scalea is a professor of surgery at the University of Maryland, Baltimore. These are excerpts of his remarks as a discussant of the study at the meeting. He reported having no financial disclosures.
Almost 20 years after the initial description and 30 years after we began using splenic angiography in the management of blunt splenic injury, why is it that we simply can’t settle this question? When is splenic angiography and/or catheter therapy useful in high-grade injuries?
In this study, the authors have reviewed the National Trauma Data Bank (NTDB) and have demonstrated that, at hospitals that use angiography more frequently than other hospitals, the rate of delayed splenectomy in high-grade splenic injury (defined as grades 3-5) is not different. They suggest that angiography should be selective, with particular attention to screening for vascular abnormalities.
 |
|
The authors collected information on both angiography and angiography with embolization. However, in the manuscript and the talk, they only refer to high-angiography centers. This seems to me to be a fundamental problem. This is particularly true because recent data from Jacksonville suggest that embolization of truly high-grade injury such as grade 4 injuries (even in the absence of blush) improves the salvage rate of nonoperative management.
In addition, the authors selected 20% as their cutoff for high- and low-angiography centers because 20% represented the 90th percentile of centers with regard to angiography use. I think that’s French for "it made the data analyzable." However, 20% is relatively low. If the authors wish to look at nonselective angiography they should look at us. We’re maximalists. We do angiography on 100% of patients with grades 3, 4 and 5 injuries. That’s nonselective use of angiography.
The intelligent use of this technique requires interpretation of CT and then the details of the patient presentation. For instance, a grade 4 splenic injury with or without blush but no hemoperitoneum and a totally stable patient is, in my mind, amenable to catheter therapy. Another patient with a grade 4 injury and reactive extravasation outside of the spleen and a huge peritoneum is probably best served by operative exploration. Both are grade 4 injuries, but the patients are fundamentally different.
The authors’ conclusions suggest that there is a relationship between splenic vascular injury identified on CT and success or failure of nonoperative management. This is clearly the authors’ prejudice, as they have published these findings a number of times. We’ve known for years, thanks to work from the authors’ institution, that expectant management of a patient with blush on CT fails 70% of the time and a significant number of the blushes are seen on day 3 but not day 1. Since the authors have absolutely no information on the presence or absence of blush in this data set, I fail to see how that can be one of their conclusions.
How, then, can we make sense of this? I believe the answer is in the manuscript’s last paragraph, which begins, "Another limitation of this study stems from the limitations of the NTDB." There’s little doubt that the NTDB can record an accurate snapshot of practice in the United States, but in my mind, it lacks the specificity to really answer the question, when is splenic angiography useful in high-grade injuries?
The authors have no information on presence of absence of blush, hemodynamic status other than at admission, blood transfusion rate, or technique of embolization, and they recognize that some of the data may not be accurate. I just don’t believe that the NTDB can actually answer this question.
In the end, rules are rarely helpful in the care of patients. Intelligent application of innovative techniques cannot solely be governed by rules. Perhaps the take-home message here is that the use of angiography and embolization to treat higher-grade splenic injuries is perhaps not something that everybody should be using. It may be that this technique is best preserved for high-volume centers with a real interest and a real expertise in this subject.
Dr. Thomas M. Scalea is a professor of surgery at the University of Maryland, Baltimore. These are excerpts of his remarks as a discussant of the study at the meeting. He reported having no financial disclosures.
Almost 20 years after the initial description and 30 years after we began using splenic angiography in the management of blunt splenic injury, why is it that we simply can’t settle this question? When is splenic angiography and/or catheter therapy useful in high-grade injuries?
In this study, the authors have reviewed the National Trauma Data Bank (NTDB) and have demonstrated that, at hospitals that use angiography more frequently than other hospitals, the rate of delayed splenectomy in high-grade splenic injury (defined as grades 3-5) is not different. They suggest that angiography should be selective, with particular attention to screening for vascular abnormalities.
 |
|
The authors collected information on both angiography and angiography with embolization. However, in the manuscript and the talk, they only refer to high-angiography centers. This seems to me to be a fundamental problem. This is particularly true because recent data from Jacksonville suggest that embolization of truly high-grade injury such as grade 4 injuries (even in the absence of blush) improves the salvage rate of nonoperative management.
In addition, the authors selected 20% as their cutoff for high- and low-angiography centers because 20% represented the 90th percentile of centers with regard to angiography use. I think that’s French for "it made the data analyzable." However, 20% is relatively low. If the authors wish to look at nonselective angiography they should look at us. We’re maximalists. We do angiography on 100% of patients with grades 3, 4 and 5 injuries. That’s nonselective use of angiography.
The intelligent use of this technique requires interpretation of CT and then the details of the patient presentation. For instance, a grade 4 splenic injury with or without blush but no hemoperitoneum and a totally stable patient is, in my mind, amenable to catheter therapy. Another patient with a grade 4 injury and reactive extravasation outside of the spleen and a huge peritoneum is probably best served by operative exploration. Both are grade 4 injuries, but the patients are fundamentally different.
The authors’ conclusions suggest that there is a relationship between splenic vascular injury identified on CT and success or failure of nonoperative management. This is clearly the authors’ prejudice, as they have published these findings a number of times. We’ve known for years, thanks to work from the authors’ institution, that expectant management of a patient with blush on CT fails 70% of the time and a significant number of the blushes are seen on day 3 but not day 1. Since the authors have absolutely no information on the presence or absence of blush in this data set, I fail to see how that can be one of their conclusions.
How, then, can we make sense of this? I believe the answer is in the manuscript’s last paragraph, which begins, "Another limitation of this study stems from the limitations of the NTDB." There’s little doubt that the NTDB can record an accurate snapshot of practice in the United States, but in my mind, it lacks the specificity to really answer the question, when is splenic angiography useful in high-grade injuries?
The authors have no information on presence of absence of blush, hemodynamic status other than at admission, blood transfusion rate, or technique of embolization, and they recognize that some of the data may not be accurate. I just don’t believe that the NTDB can actually answer this question.
In the end, rules are rarely helpful in the care of patients. Intelligent application of innovative techniques cannot solely be governed by rules. Perhaps the take-home message here is that the use of angiography and embolization to treat higher-grade splenic injuries is perhaps not something that everybody should be using. It may be that this technique is best preserved for high-volume centers with a real interest and a real expertise in this subject.
Dr. Thomas M. Scalea is a professor of surgery at the University of Maryland, Baltimore. These are excerpts of his remarks as a discussant of the study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Trauma centers that nonselectively performed angiography on patients with high-grade blunt splenic injury did not significantly reduce the likelihood of delayed splenectomy in a retrospective analysis of data on 6,870 patients treated at 267 hospitals.
On an individual patient level, however, use of angiography was associated with a reduced risk of delayed splenectomy (more than 6 hours after admission) after researchers controlled for the influence of multiple other factors, Dr. Ben L. Zarzaur and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
These somewhat conflicting findings suggest that "nonselective protocol-driven use of angiography at the hospital in the setting of high-grade blunt splenic injury does not benefit in terms of splenic salvage. Angiography use should be tailored to the individual patient," said Dr. Zarzaur of the University of Tennessee, Memphis.
"Attention should be paid to overall injury severity and splenic injury severity" because more severe injuries were associated with delayed splenectomy in the study, he said, adding, "Particular attention should be considered for screening for splenic vascular abnormalities."
The investigators used data from the National Trauma Data Bank (NTDB) on adults treated for high-grade blunt splenic injury at Level I or II trauma centers that admitted at least 10 such patients in 2007-2010, with high-grade injury defined as Abbreviated Injury Scale grade 3 or higher. They stratified hospital angiography use as none, low (in less than 20% of patients with high-grade blunt splenic injury), or high (in 20% or more of these patients).
Approximately 30% of patients at high-angiography centers underwent urgent splenectomy, compared with 33%-36% at hospitals with no or low-angiography use, a difference that was statistically significant. While the likelihood of a delayed splenectomy was 33% higher at low-angiography hospitals and 49% higher at hospitals without angiography, compared with high-angiography hospitals, these differences were not significant, Dr. Zarzaur reported.
The investigators used the classification of hospitals – no-, low-, or high-angiography use – to represent the three schools of thought that have developed over the past few decades regarding angiography for patients with blunt splenic injury who do not undergo immediate urgent splenectomy. The minimalist school of thought recommends using observation, not angiography for blunt splenic injury. The maximalist school of thought favors protocol-driven use of angiography for patients with certain grades of spleen injury. In between, physicians who favor a selective strategy use CT or clinical criteria or both to try and identify patients at high risk for delayed splenectomy, and reserve the risks of angiography for those patients, he said.
They chose a cutoff of 20% angiography use in patients with high-grade blunt splenic injury to discriminate between low- and high-angiography use because that represented the 90th percentile for all trauma centers in the study.
Nine percent of patients were treated at hospitals that did not use angiography for blunt splenic injury, 66% at low-angiography hospitals, and 25% at high-angiography hospitals.
Patients with grade 5 blunt splenic injury were more than twice as likely to need delayed splenectomy, compared with patients with grade 3 or 4 injury. Higher overall Injury Severity Scores (10 or higher) also doubled the risk for delayed splenectomy.
Patients with grades 4 or 5 blunt splenic injury were significantly more likely to undergo angiography at high-angiography centers than at low-angiography centers. High-angiography centers were more likely than were low-angiography centers to remove spleens with grade 5 injury after angiography, though this difference did not reach statistical significance.
Continuing controversy around the use of angiography for blunt splenic injury is illustrated by a 2011 survey of members of the American Association for the Surgery of Trauma. Members favored observation, not angiography, for grades 1 and 2 spleen injuries but showed no consensus on higher-grade injuries (J. Trauma 2011;70:1026-31).
A recent study of 1,275 patients treated for blunt splenic injury at four trauma centers that showed a significantly better chance of saving the spleen at hospitals with higher use of splenic artery embolization, especially in patients with higher-grade splenic injury (J. Trauma Acute Care Surg. 2013;75:69-74).
The current study excluded patients who died on arrival at the hospital, patients who were admitted more than 24 hours after injury, and patients who underwent splenectomy within 6 hours of admission (early splenectomy).
Dr. Zarzaur reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Trauma centers that nonselectively performed angiography on patients with high-grade blunt splenic injury did not significantly reduce the likelihood of delayed splenectomy in a retrospective analysis of data on 6,870 patients treated at 267 hospitals.
On an individual patient level, however, use of angiography was associated with a reduced risk of delayed splenectomy (more than 6 hours after admission) after researchers controlled for the influence of multiple other factors, Dr. Ben L. Zarzaur and his associates reported at the annual meeting of the American Association for the Surgery of Trauma.
These somewhat conflicting findings suggest that "nonselective protocol-driven use of angiography at the hospital in the setting of high-grade blunt splenic injury does not benefit in terms of splenic salvage. Angiography use should be tailored to the individual patient," said Dr. Zarzaur of the University of Tennessee, Memphis.
"Attention should be paid to overall injury severity and splenic injury severity" because more severe injuries were associated with delayed splenectomy in the study, he said, adding, "Particular attention should be considered for screening for splenic vascular abnormalities."
The investigators used data from the National Trauma Data Bank (NTDB) on adults treated for high-grade blunt splenic injury at Level I or II trauma centers that admitted at least 10 such patients in 2007-2010, with high-grade injury defined as Abbreviated Injury Scale grade 3 or higher. They stratified hospital angiography use as none, low (in less than 20% of patients with high-grade blunt splenic injury), or high (in 20% or more of these patients).
Approximately 30% of patients at high-angiography centers underwent urgent splenectomy, compared with 33%-36% at hospitals with no or low-angiography use, a difference that was statistically significant. While the likelihood of a delayed splenectomy was 33% higher at low-angiography hospitals and 49% higher at hospitals without angiography, compared with high-angiography hospitals, these differences were not significant, Dr. Zarzaur reported.
The investigators used the classification of hospitals – no-, low-, or high-angiography use – to represent the three schools of thought that have developed over the past few decades regarding angiography for patients with blunt splenic injury who do not undergo immediate urgent splenectomy. The minimalist school of thought recommends using observation, not angiography for blunt splenic injury. The maximalist school of thought favors protocol-driven use of angiography for patients with certain grades of spleen injury. In between, physicians who favor a selective strategy use CT or clinical criteria or both to try and identify patients at high risk for delayed splenectomy, and reserve the risks of angiography for those patients, he said.
They chose a cutoff of 20% angiography use in patients with high-grade blunt splenic injury to discriminate between low- and high-angiography use because that represented the 90th percentile for all trauma centers in the study.
Nine percent of patients were treated at hospitals that did not use angiography for blunt splenic injury, 66% at low-angiography hospitals, and 25% at high-angiography hospitals.
Patients with grade 5 blunt splenic injury were more than twice as likely to need delayed splenectomy, compared with patients with grade 3 or 4 injury. Higher overall Injury Severity Scores (10 or higher) also doubled the risk for delayed splenectomy.
Patients with grades 4 or 5 blunt splenic injury were significantly more likely to undergo angiography at high-angiography centers than at low-angiography centers. High-angiography centers were more likely than were low-angiography centers to remove spleens with grade 5 injury after angiography, though this difference did not reach statistical significance.
Continuing controversy around the use of angiography for blunt splenic injury is illustrated by a 2011 survey of members of the American Association for the Surgery of Trauma. Members favored observation, not angiography, for grades 1 and 2 spleen injuries but showed no consensus on higher-grade injuries (J. Trauma 2011;70:1026-31).
A recent study of 1,275 patients treated for blunt splenic injury at four trauma centers that showed a significantly better chance of saving the spleen at hospitals with higher use of splenic artery embolization, especially in patients with higher-grade splenic injury (J. Trauma Acute Care Surg. 2013;75:69-74).
The current study excluded patients who died on arrival at the hospital, patients who were admitted more than 24 hours after injury, and patients who underwent splenectomy within 6 hours of admission (early splenectomy).
Dr. Zarzaur reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: The likelihood of delayed splenectomy was 33% higher at centers without angiography and 49% higher at low-angiography centers, compared with high-angiography centers, but the differences were not statistically significant.
Data source: Retrospective analysis of data from the National Trauma Data Bank on 6,870 patients treated for blunt splenic injury at 267 hospitals.
Disclosures: Dr. Zarzaur reported having no financial disclosures.
Inpatient intervention changed patients’ attitudes about violence
SAN FRANCISCO – An inpatient intervention that used gunshot or stab wounds as "teachable moments" significantly improved some attitudes about violence in a randomized study of 40 hospitalized trauma patients.
The prospective pilot study administered the Attitudes Toward Guns and Violence Questionnaire (AGVQ) before and after the intervention or usual care for patients treated at Temple University Hospital, Philadelphia, from January to June 2012. Their general proclivity toward violence (the overall AGVQ score) decreased by 20% in the intervention group (from a mean score of 15 to 12.1) and held steady in the control group (scores of 11.5 and 11.3).
Two subscales of the AGVQ also produced significant attitudinal changes after the intervention, a four-part program called Turning Point, Dr. Catherine E. Loveland-Jones and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Patients’ comfort with aggression (or acceptance of violence as a part of everyday life) decreased from a mean score of 4.2 to 2.8 after the intervention (a 33% reduction) compared with scores of 2.9 and 2.8, respectively, in the control group.
The greatest change was seen in scores for aggressive response to shame. Patients in the intervention group showed a 44% reduction in their sensitivity to disrespect from others and the belief that violence is the best means for preserving one’s damaged self-esteem, said Dr. Loveland-Jones of Temple University. Their mean scores decreased from 3.6 to 2 after the intervention, compared with scores of 3.1 and 2.6 in the control group.
"We believe that attitude change is fundamental and really the first step to behavior change," she said. The ongoing study is nearing its goal of enrolling 80 patients.
A separate program at her institution to prevent violence in youth also had its greatest impact on attitudes about shame and violence. The findings are encouraging because reaction to shame is thought to be a driver of violence in the study’s population, she said.
All patients in the study received the usual social services care offered at the urban Level 1 trauma center to victims of gunshot and stab wounds, consisting of team care from a trauma outreach coordinator, a case manager, and a social worker. The 21 patients in the Turning Point group also watched a video of their resuscitation in the trauma bay and a reality-based movie about violence. They met with a gunshot wound survivor, were introduced to an outpatient case manager, and received a psychiatric evaluation if the patient or a clinician requested one.
"I think the most important part of our program is our referral to outpatient services," Dr. Loveland-Jones said. Previous data suggest that "meeting mental health needs and finding employment for patients are the most important," and that moderate- to high-intensity case management in the first 3 months after the trauma helps achieve that.
The study enrolled English-speaking adults with gunshot or stab wounds who had a Glasgow Coma Score of 15. The cohort "overwhelmingly" consisted of black males in their 20s, she said. In general, more than half of gunshot victims in Philadelphia are young, she added.
The Turning Point program costs $50,000 per year and subcontracts with an established community group for the outpatient case management.
Two subscales of the AGVQ did not change significantly in either group. Scores were lowest for reported levels of gun-related excitement, "suggesting that guns are viewed as necessary and commonplace rather than exciting," she said. The AGVQ scores before and after the intervention were 0.1 and 0.5 in the control group, respectively, and remained at 0.3 in the Turning Point group.
Scores were highest for feelings of gun-related power and safety, "suggesting that there is a very strong view in our community that guns are a necessary means for preserving personal safety," she said. The AGVQ scores before and after the intervention were 5 and 5.2 in the control group and 6 and 6.4 in the Turning Point group, respectively.
The study excluded 119 (75%) of 159 potential participants, primarily patients who stayed in the hospital less than 48 hours (69%). A total of 9% of patients refused to participate. Other reasons for exclusion were police custody (7%), devastating neurologic injury (4%), severe psychiatric disorder (2%), and unknown reasons (2%). Investigators also excluded 3% who were non-English speakers, 2% who left the hospital against medical advice, and 2% who planned to relocate after discharge.
Patients in the Turning Point group were significantly more likely to be alcohol abusers (26%), compared with the control group (14%), and were significantly younger – an average of 22 years vs. 31 years in the control group.
The investigators designed the Turning Point program components based on a prior survey that asked similar patients what would be useful. Unlike tactics in some programs such as Scared Straight that "don’t work," Turning Point’s videos are not meant to scare patients but to provide a platform for discussing the gravity of their injuries and how much they value their lives, she said.
"I applaud the compassion and insight of those individuals who conducted and participated in Turning Point, which is much needed and long overdue. It just goes to show that you can use almost any situation as a teachable moment; and when an individual is faced with his own mortality, he is likely to be all ears," remarked Dr. A. Maria Hester, a hospitalist with Baltimore-Washington Medical Center. Dr. Hester writes the "Teachable Moments" blog for Hospitalist News.
Dr. Loveland-Jones reported having no financial disclosures.
On Twitter @sherryboschert
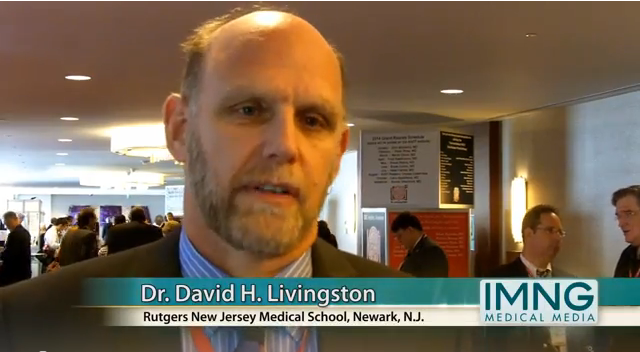
It was 13 years ago now that Surgeon General C. Everett Koop recognized violent injury as a public health issue. His statement, and the concept of violence prevention implicit in his statement, has served as a foundation for the development of hospital-based violence prevention programs nationwide.
Fast-forward to 2013 and the violence prevention programs that have been recognized as an integral part of many of our trauma centers, championed by surgeons, emergency medicine physicians, trauma nurse coordinators, community leaders, and hospital foundations and even administrations. Today, the National Network of Hospital-Based Violence Intervention Programs boasts 22 full members and 12 emerging programs (with more on the horizon and other groups such as Turning Points) to be admired.
The mission of the National Network has been to establish best practices for violence prevention programs and to provide some technical support to fledgling programs so that groups wanting to establish programs don’t have to start from scratch or reinvent the wheel. Integral to the development of best practices is quantitative scientific studies demonstrating feasibility, utility, interim and long-term efficacy, and perhaps fidelity.
As the authors of this paper recognized, several quantitative studies have demonstrated positive results, with ultimate reduction in injury recidivism. Just as vital, however, to best understand the components of success or failure are programmatic analyses. The authors provide us with one such study, and I applaud them for their efforts. Dr. Loveland-Jones and her colleagues representing Temple’s violence prevention program Turning Point did a very nice job in providing us with appropriate context.
I also applaud them for conducting a randomized controlled trial in this field, as many of us know it’s quite difficult given the characteristic lack of equipoise, especially in our communities that are particularly affected by violence. I would just caution the authors but also encourage them to continue with the psychiatric evaluation. That is so important in our patient population.
It is only by these programmatic studies and the multi-institutional documentation that we’re engaged in now that the successes and failures can be identified so we can move to best practices for violence prevention as standard of care in many of our trauma centers.
Dr. Rochelle Dicker is director of the San Francisco Injury Center at San Francisco General Hospital. These are excerpts of her remarks as the discussant of the study at the meeting.
It was 13 years ago now that Surgeon General C. Everett Koop recognized violent injury as a public health issue. His statement, and the concept of violence prevention implicit in his statement, has served as a foundation for the development of hospital-based violence prevention programs nationwide.
Fast-forward to 2013 and the violence prevention programs that have been recognized as an integral part of many of our trauma centers, championed by surgeons, emergency medicine physicians, trauma nurse coordinators, community leaders, and hospital foundations and even administrations. Today, the National Network of Hospital-Based Violence Intervention Programs boasts 22 full members and 12 emerging programs (with more on the horizon and other groups such as Turning Points) to be admired.
The mission of the National Network has been to establish best practices for violence prevention programs and to provide some technical support to fledgling programs so that groups wanting to establish programs don’t have to start from scratch or reinvent the wheel. Integral to the development of best practices is quantitative scientific studies demonstrating feasibility, utility, interim and long-term efficacy, and perhaps fidelity.
As the authors of this paper recognized, several quantitative studies have demonstrated positive results, with ultimate reduction in injury recidivism. Just as vital, however, to best understand the components of success or failure are programmatic analyses. The authors provide us with one such study, and I applaud them for their efforts. Dr. Loveland-Jones and her colleagues representing Temple’s violence prevention program Turning Point did a very nice job in providing us with appropriate context.
I also applaud them for conducting a randomized controlled trial in this field, as many of us know it’s quite difficult given the characteristic lack of equipoise, especially in our communities that are particularly affected by violence. I would just caution the authors but also encourage them to continue with the psychiatric evaluation. That is so important in our patient population.
It is only by these programmatic studies and the multi-institutional documentation that we’re engaged in now that the successes and failures can be identified so we can move to best practices for violence prevention as standard of care in many of our trauma centers.
Dr. Rochelle Dicker is director of the San Francisco Injury Center at San Francisco General Hospital. These are excerpts of her remarks as the discussant of the study at the meeting.
It was 13 years ago now that Surgeon General C. Everett Koop recognized violent injury as a public health issue. His statement, and the concept of violence prevention implicit in his statement, has served as a foundation for the development of hospital-based violence prevention programs nationwide.
Fast-forward to 2013 and the violence prevention programs that have been recognized as an integral part of many of our trauma centers, championed by surgeons, emergency medicine physicians, trauma nurse coordinators, community leaders, and hospital foundations and even administrations. Today, the National Network of Hospital-Based Violence Intervention Programs boasts 22 full members and 12 emerging programs (with more on the horizon and other groups such as Turning Points) to be admired.
The mission of the National Network has been to establish best practices for violence prevention programs and to provide some technical support to fledgling programs so that groups wanting to establish programs don’t have to start from scratch or reinvent the wheel. Integral to the development of best practices is quantitative scientific studies demonstrating feasibility, utility, interim and long-term efficacy, and perhaps fidelity.
As the authors of this paper recognized, several quantitative studies have demonstrated positive results, with ultimate reduction in injury recidivism. Just as vital, however, to best understand the components of success or failure are programmatic analyses. The authors provide us with one such study, and I applaud them for their efforts. Dr. Loveland-Jones and her colleagues representing Temple’s violence prevention program Turning Point did a very nice job in providing us with appropriate context.
I also applaud them for conducting a randomized controlled trial in this field, as many of us know it’s quite difficult given the characteristic lack of equipoise, especially in our communities that are particularly affected by violence. I would just caution the authors but also encourage them to continue with the psychiatric evaluation. That is so important in our patient population.
It is only by these programmatic studies and the multi-institutional documentation that we’re engaged in now that the successes and failures can be identified so we can move to best practices for violence prevention as standard of care in many of our trauma centers.
Dr. Rochelle Dicker is director of the San Francisco Injury Center at San Francisco General Hospital. These are excerpts of her remarks as the discussant of the study at the meeting.
SAN FRANCISCO – An inpatient intervention that used gunshot or stab wounds as "teachable moments" significantly improved some attitudes about violence in a randomized study of 40 hospitalized trauma patients.
The prospective pilot study administered the Attitudes Toward Guns and Violence Questionnaire (AGVQ) before and after the intervention or usual care for patients treated at Temple University Hospital, Philadelphia, from January to June 2012. Their general proclivity toward violence (the overall AGVQ score) decreased by 20% in the intervention group (from a mean score of 15 to 12.1) and held steady in the control group (scores of 11.5 and 11.3).
Two subscales of the AGVQ also produced significant attitudinal changes after the intervention, a four-part program called Turning Point, Dr. Catherine E. Loveland-Jones and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Patients’ comfort with aggression (or acceptance of violence as a part of everyday life) decreased from a mean score of 4.2 to 2.8 after the intervention (a 33% reduction) compared with scores of 2.9 and 2.8, respectively, in the control group.
The greatest change was seen in scores for aggressive response to shame. Patients in the intervention group showed a 44% reduction in their sensitivity to disrespect from others and the belief that violence is the best means for preserving one’s damaged self-esteem, said Dr. Loveland-Jones of Temple University. Their mean scores decreased from 3.6 to 2 after the intervention, compared with scores of 3.1 and 2.6 in the control group.
"We believe that attitude change is fundamental and really the first step to behavior change," she said. The ongoing study is nearing its goal of enrolling 80 patients.
A separate program at her institution to prevent violence in youth also had its greatest impact on attitudes about shame and violence. The findings are encouraging because reaction to shame is thought to be a driver of violence in the study’s population, she said.
All patients in the study received the usual social services care offered at the urban Level 1 trauma center to victims of gunshot and stab wounds, consisting of team care from a trauma outreach coordinator, a case manager, and a social worker. The 21 patients in the Turning Point group also watched a video of their resuscitation in the trauma bay and a reality-based movie about violence. They met with a gunshot wound survivor, were introduced to an outpatient case manager, and received a psychiatric evaluation if the patient or a clinician requested one.
"I think the most important part of our program is our referral to outpatient services," Dr. Loveland-Jones said. Previous data suggest that "meeting mental health needs and finding employment for patients are the most important," and that moderate- to high-intensity case management in the first 3 months after the trauma helps achieve that.
The study enrolled English-speaking adults with gunshot or stab wounds who had a Glasgow Coma Score of 15. The cohort "overwhelmingly" consisted of black males in their 20s, she said. In general, more than half of gunshot victims in Philadelphia are young, she added.
The Turning Point program costs $50,000 per year and subcontracts with an established community group for the outpatient case management.
Two subscales of the AGVQ did not change significantly in either group. Scores were lowest for reported levels of gun-related excitement, "suggesting that guns are viewed as necessary and commonplace rather than exciting," she said. The AGVQ scores before and after the intervention were 0.1 and 0.5 in the control group, respectively, and remained at 0.3 in the Turning Point group.
Scores were highest for feelings of gun-related power and safety, "suggesting that there is a very strong view in our community that guns are a necessary means for preserving personal safety," she said. The AGVQ scores before and after the intervention were 5 and 5.2 in the control group and 6 and 6.4 in the Turning Point group, respectively.
The study excluded 119 (75%) of 159 potential participants, primarily patients who stayed in the hospital less than 48 hours (69%). A total of 9% of patients refused to participate. Other reasons for exclusion were police custody (7%), devastating neurologic injury (4%), severe psychiatric disorder (2%), and unknown reasons (2%). Investigators also excluded 3% who were non-English speakers, 2% who left the hospital against medical advice, and 2% who planned to relocate after discharge.
Patients in the Turning Point group were significantly more likely to be alcohol abusers (26%), compared with the control group (14%), and were significantly younger – an average of 22 years vs. 31 years in the control group.
The investigators designed the Turning Point program components based on a prior survey that asked similar patients what would be useful. Unlike tactics in some programs such as Scared Straight that "don’t work," Turning Point’s videos are not meant to scare patients but to provide a platform for discussing the gravity of their injuries and how much they value their lives, she said.
"I applaud the compassion and insight of those individuals who conducted and participated in Turning Point, which is much needed and long overdue. It just goes to show that you can use almost any situation as a teachable moment; and when an individual is faced with his own mortality, he is likely to be all ears," remarked Dr. A. Maria Hester, a hospitalist with Baltimore-Washington Medical Center. Dr. Hester writes the "Teachable Moments" blog for Hospitalist News.
Dr. Loveland-Jones reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – An inpatient intervention that used gunshot or stab wounds as "teachable moments" significantly improved some attitudes about violence in a randomized study of 40 hospitalized trauma patients.
The prospective pilot study administered the Attitudes Toward Guns and Violence Questionnaire (AGVQ) before and after the intervention or usual care for patients treated at Temple University Hospital, Philadelphia, from January to June 2012. Their general proclivity toward violence (the overall AGVQ score) decreased by 20% in the intervention group (from a mean score of 15 to 12.1) and held steady in the control group (scores of 11.5 and 11.3).
Two subscales of the AGVQ also produced significant attitudinal changes after the intervention, a four-part program called Turning Point, Dr. Catherine E. Loveland-Jones and her associates reported at the annual meeting of the American Association for the Surgery of Trauma.
Patients’ comfort with aggression (or acceptance of violence as a part of everyday life) decreased from a mean score of 4.2 to 2.8 after the intervention (a 33% reduction) compared with scores of 2.9 and 2.8, respectively, in the control group.
The greatest change was seen in scores for aggressive response to shame. Patients in the intervention group showed a 44% reduction in their sensitivity to disrespect from others and the belief that violence is the best means for preserving one’s damaged self-esteem, said Dr. Loveland-Jones of Temple University. Their mean scores decreased from 3.6 to 2 after the intervention, compared with scores of 3.1 and 2.6 in the control group.
"We believe that attitude change is fundamental and really the first step to behavior change," she said. The ongoing study is nearing its goal of enrolling 80 patients.
A separate program at her institution to prevent violence in youth also had its greatest impact on attitudes about shame and violence. The findings are encouraging because reaction to shame is thought to be a driver of violence in the study’s population, she said.
All patients in the study received the usual social services care offered at the urban Level 1 trauma center to victims of gunshot and stab wounds, consisting of team care from a trauma outreach coordinator, a case manager, and a social worker. The 21 patients in the Turning Point group also watched a video of their resuscitation in the trauma bay and a reality-based movie about violence. They met with a gunshot wound survivor, were introduced to an outpatient case manager, and received a psychiatric evaluation if the patient or a clinician requested one.
"I think the most important part of our program is our referral to outpatient services," Dr. Loveland-Jones said. Previous data suggest that "meeting mental health needs and finding employment for patients are the most important," and that moderate- to high-intensity case management in the first 3 months after the trauma helps achieve that.
The study enrolled English-speaking adults with gunshot or stab wounds who had a Glasgow Coma Score of 15. The cohort "overwhelmingly" consisted of black males in their 20s, she said. In general, more than half of gunshot victims in Philadelphia are young, she added.
The Turning Point program costs $50,000 per year and subcontracts with an established community group for the outpatient case management.
Two subscales of the AGVQ did not change significantly in either group. Scores were lowest for reported levels of gun-related excitement, "suggesting that guns are viewed as necessary and commonplace rather than exciting," she said. The AGVQ scores before and after the intervention were 0.1 and 0.5 in the control group, respectively, and remained at 0.3 in the Turning Point group.
Scores were highest for feelings of gun-related power and safety, "suggesting that there is a very strong view in our community that guns are a necessary means for preserving personal safety," she said. The AGVQ scores before and after the intervention were 5 and 5.2 in the control group and 6 and 6.4 in the Turning Point group, respectively.
The study excluded 119 (75%) of 159 potential participants, primarily patients who stayed in the hospital less than 48 hours (69%). A total of 9% of patients refused to participate. Other reasons for exclusion were police custody (7%), devastating neurologic injury (4%), severe psychiatric disorder (2%), and unknown reasons (2%). Investigators also excluded 3% who were non-English speakers, 2% who left the hospital against medical advice, and 2% who planned to relocate after discharge.
Patients in the Turning Point group were significantly more likely to be alcohol abusers (26%), compared with the control group (14%), and were significantly younger – an average of 22 years vs. 31 years in the control group.
The investigators designed the Turning Point program components based on a prior survey that asked similar patients what would be useful. Unlike tactics in some programs such as Scared Straight that "don’t work," Turning Point’s videos are not meant to scare patients but to provide a platform for discussing the gravity of their injuries and how much they value their lives, she said.
"I applaud the compassion and insight of those individuals who conducted and participated in Turning Point, which is much needed and long overdue. It just goes to show that you can use almost any situation as a teachable moment; and when an individual is faced with his own mortality, he is likely to be all ears," remarked Dr. A. Maria Hester, a hospitalist with Baltimore-Washington Medical Center. Dr. Hester writes the "Teachable Moments" blog for Hospitalist News.
Dr. Loveland-Jones reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: General proclivity toward violence decreased 20%, comfort with aggression decreased 33%, and the inclination to respond aggressively to shame decreased 44% in the intervention group, with no significant changes in the control group.
Data source: A pilot randomized, controlled trial of 40 hospitalized victims of gunshot or stab wounds at one trauma center.
Disclosures: Dr. Loveland-Jones reported having no financial disclosures.
Outpatient laparoscopic appendectomy found safe, cost saving
SAN FRANCISCO – Implementing an outpatient laparoscopic appendectomy protocol for uncomplicated appendicitis allowed 88% of 345 cases at one institution to be performed without hospitalizing the patient overnight.
The outpatients went home an average of 171 minutes after completion of the surgery.
Forty patients were admitted (12%) because of pre-existing comorbidities in 15 patients, postoperative morbidity in 6, and a lack of transportation or assistance for 19, Dr. Richard C. Frazee and his associates reported.
Only 4 of the 305 patients who underwent the procedure as outpatients were admitted after going home, for an overall outpatient success rate of 87%, he said at the annual meeting of the American Association for the Surgery of Trauma. Reasons for readmission included fever, nausea and vomiting, partial small bowel obstruction, or deep vein thrombosis.
Morbidity affected 7% of patients in the form of urinary retention, wound infection, operative enterotomy, cecal serosal injury, deep vein thrombosis, or exacerbation of chronic obstructive pulmonary disease. One laparoscopic appendectomy was converted to open surgery; none of the patients died.
This is not the first time Dr. Frazee has presented his institution’s experience with the outpatient laparoscopic appendectomy protocol; he shared similar findings from an earlier series at the same meeting a few years ago. In an interview, he expressed some frustration that more hospitals haven’t adopted similar protocols.
By his rough calculation, 20% of all laparoscopic uncomplicated appendectomies performed in the United States each year cause perforations requiring hospitalization and 80% of the rest are successful outpatient procedures. That means 242,760 patients each year would not be hospitalized overnight for this surgery. Separate data show that the average U.S. length of hospitalization for laparoscopic appendectomy is 2 days, at an average cost of $1,900 per day. Nationwide adoption of an outpatient protocol potentially could avoid over $921 million in annual costs.
"It is time for us to create a change in the standard of care for uncomplicated appendicitis," said Dr. Frazee, chief of acute care surgery at Scott & White Healthcare in Temple, Tex.
His interest in the subject started when his son, an otherwise healthy young adult, complained about having to stay in the hospital after a laparoscopic appendectomy. Dr. Frazee conducted a review of 119 laparoscopic appendectomies at his institution and found that 35% of patients went home the same day, 61% were admitted for a day, and the few others were hospitalized longer. Morbidity was seen in 8%.
He and his colleagues developed an outpatient protocol in July 2010, under which patients undergoing uncomplicated laparoscopic appendectomies would not be admitted unless they were pregnant or younger than 17 years, or if a perforated or gangrenous appendicitis was discovered during the surgery. To qualify for same-day discharge, outpatients had to be able to tolerate intake of liquids, ambulate, urinate, and have adequate respiratory effort. They also had to be hemodynamically stable, have pain controlled with oral analgesics, have nausea and vomiting controlled, show no alteration in mental status from baseline, have the approval of their physician, and have appropriate supervision and assistance at home.
An initial review compared 116 patients treated under the protocol in 2010-2011 with historical controls and found a significant reduction in length of stay without increased morbidity. Under the protocol, 85% of patients were outpatients, compared with 35% in the control group. Postoperative morbidity affected 5% in the protocol group and 8% in the control group, and no patients were readmitted (Am. Surg. 2012;215:101-5).
Since then, the outpatient protocol has been the standard of care at his institution. The current report covers 166 men and 179 women treated under the protocol from July 2010 through December 2012. They had a mean age of 35 years and a mean body mass index of 31 kg/m2. Thirty-two percent had a history of prior abdominal surgery. Comorbidities at baseline included hypertension in 29%, diabetes in 11%, coronary artery disease in 4%, and chronic obstructive pulmonary disease in 1%.
Outpatients were sent home from the day surgery unit or the post–anesthetic care unit. Thirty percent were dismissed between 6 a.m. and noon, 15% went home between noon and 6 p.m., 25% were dismissed between 6 p.m. and midnight, and 30% went home between midnight and 6 a.m.
The investigators now are conducting a follow-up study to assess patient satisfaction with the protocol. "Our impression is that they like going home the same day," but a study will confirm whether this is true or not, he said.
Dr. Frazee reported having no financial disclosures.
This is a well-written paper that continues a series of contributions from the authors addressing management of acute appendicitis. A 1994 paper from the authors prospectively compared laparoscopic with open appendectomy. In 2012, the authors reported and described their protocol for outpatient management of laparoscopic appendectomy, comparing 116 patients with a matched historical cohort group. This paper is an update of the 2012 paper and now includes 345 patients.
They assume that their patients are at home, happy, and doing well after discharge. They may not be. The conclusions would be more valid if patients had completed a questionnaire that stated that they were home and doing well, as other authors have done in studying this disease.
The report provides mean times from the emergency department to the operating room and from completion of surgery to discharge. Median times would be helpful to know.
I congratulate them on a well-presented and well-written paper.
Dr. Andrew Peitzman is professor of surgery and chief of general surgery and of trauma/surgical critical care at the University of Pittsburgh. He gave these comments as the discussant of Dr. Frazee’s study at the meeting.
This is a well-written paper that continues a series of contributions from the authors addressing management of acute appendicitis. A 1994 paper from the authors prospectively compared laparoscopic with open appendectomy. In 2012, the authors reported and described their protocol for outpatient management of laparoscopic appendectomy, comparing 116 patients with a matched historical cohort group. This paper is an update of the 2012 paper and now includes 345 patients.
They assume that their patients are at home, happy, and doing well after discharge. They may not be. The conclusions would be more valid if patients had completed a questionnaire that stated that they were home and doing well, as other authors have done in studying this disease.
The report provides mean times from the emergency department to the operating room and from completion of surgery to discharge. Median times would be helpful to know.
I congratulate them on a well-presented and well-written paper.
Dr. Andrew Peitzman is professor of surgery and chief of general surgery and of trauma/surgical critical care at the University of Pittsburgh. He gave these comments as the discussant of Dr. Frazee’s study at the meeting.
This is a well-written paper that continues a series of contributions from the authors addressing management of acute appendicitis. A 1994 paper from the authors prospectively compared laparoscopic with open appendectomy. In 2012, the authors reported and described their protocol for outpatient management of laparoscopic appendectomy, comparing 116 patients with a matched historical cohort group. This paper is an update of the 2012 paper and now includes 345 patients.
They assume that their patients are at home, happy, and doing well after discharge. They may not be. The conclusions would be more valid if patients had completed a questionnaire that stated that they were home and doing well, as other authors have done in studying this disease.
The report provides mean times from the emergency department to the operating room and from completion of surgery to discharge. Median times would be helpful to know.
I congratulate them on a well-presented and well-written paper.
Dr. Andrew Peitzman is professor of surgery and chief of general surgery and of trauma/surgical critical care at the University of Pittsburgh. He gave these comments as the discussant of Dr. Frazee’s study at the meeting.
SAN FRANCISCO – Implementing an outpatient laparoscopic appendectomy protocol for uncomplicated appendicitis allowed 88% of 345 cases at one institution to be performed without hospitalizing the patient overnight.
The outpatients went home an average of 171 minutes after completion of the surgery.
Forty patients were admitted (12%) because of pre-existing comorbidities in 15 patients, postoperative morbidity in 6, and a lack of transportation or assistance for 19, Dr. Richard C. Frazee and his associates reported.
Only 4 of the 305 patients who underwent the procedure as outpatients were admitted after going home, for an overall outpatient success rate of 87%, he said at the annual meeting of the American Association for the Surgery of Trauma. Reasons for readmission included fever, nausea and vomiting, partial small bowel obstruction, or deep vein thrombosis.
Morbidity affected 7% of patients in the form of urinary retention, wound infection, operative enterotomy, cecal serosal injury, deep vein thrombosis, or exacerbation of chronic obstructive pulmonary disease. One laparoscopic appendectomy was converted to open surgery; none of the patients died.
This is not the first time Dr. Frazee has presented his institution’s experience with the outpatient laparoscopic appendectomy protocol; he shared similar findings from an earlier series at the same meeting a few years ago. In an interview, he expressed some frustration that more hospitals haven’t adopted similar protocols.
By his rough calculation, 20% of all laparoscopic uncomplicated appendectomies performed in the United States each year cause perforations requiring hospitalization and 80% of the rest are successful outpatient procedures. That means 242,760 patients each year would not be hospitalized overnight for this surgery. Separate data show that the average U.S. length of hospitalization for laparoscopic appendectomy is 2 days, at an average cost of $1,900 per day. Nationwide adoption of an outpatient protocol potentially could avoid over $921 million in annual costs.
"It is time for us to create a change in the standard of care for uncomplicated appendicitis," said Dr. Frazee, chief of acute care surgery at Scott & White Healthcare in Temple, Tex.
His interest in the subject started when his son, an otherwise healthy young adult, complained about having to stay in the hospital after a laparoscopic appendectomy. Dr. Frazee conducted a review of 119 laparoscopic appendectomies at his institution and found that 35% of patients went home the same day, 61% were admitted for a day, and the few others were hospitalized longer. Morbidity was seen in 8%.
He and his colleagues developed an outpatient protocol in July 2010, under which patients undergoing uncomplicated laparoscopic appendectomies would not be admitted unless they were pregnant or younger than 17 years, or if a perforated or gangrenous appendicitis was discovered during the surgery. To qualify for same-day discharge, outpatients had to be able to tolerate intake of liquids, ambulate, urinate, and have adequate respiratory effort. They also had to be hemodynamically stable, have pain controlled with oral analgesics, have nausea and vomiting controlled, show no alteration in mental status from baseline, have the approval of their physician, and have appropriate supervision and assistance at home.
An initial review compared 116 patients treated under the protocol in 2010-2011 with historical controls and found a significant reduction in length of stay without increased morbidity. Under the protocol, 85% of patients were outpatients, compared with 35% in the control group. Postoperative morbidity affected 5% in the protocol group and 8% in the control group, and no patients were readmitted (Am. Surg. 2012;215:101-5).
Since then, the outpatient protocol has been the standard of care at his institution. The current report covers 166 men and 179 women treated under the protocol from July 2010 through December 2012. They had a mean age of 35 years and a mean body mass index of 31 kg/m2. Thirty-two percent had a history of prior abdominal surgery. Comorbidities at baseline included hypertension in 29%, diabetes in 11%, coronary artery disease in 4%, and chronic obstructive pulmonary disease in 1%.
Outpatients were sent home from the day surgery unit or the post–anesthetic care unit. Thirty percent were dismissed between 6 a.m. and noon, 15% went home between noon and 6 p.m., 25% were dismissed between 6 p.m. and midnight, and 30% went home between midnight and 6 a.m.
The investigators now are conducting a follow-up study to assess patient satisfaction with the protocol. "Our impression is that they like going home the same day," but a study will confirm whether this is true or not, he said.
Dr. Frazee reported having no financial disclosures.
SAN FRANCISCO – Implementing an outpatient laparoscopic appendectomy protocol for uncomplicated appendicitis allowed 88% of 345 cases at one institution to be performed without hospitalizing the patient overnight.
The outpatients went home an average of 171 minutes after completion of the surgery.
Forty patients were admitted (12%) because of pre-existing comorbidities in 15 patients, postoperative morbidity in 6, and a lack of transportation or assistance for 19, Dr. Richard C. Frazee and his associates reported.
Only 4 of the 305 patients who underwent the procedure as outpatients were admitted after going home, for an overall outpatient success rate of 87%, he said at the annual meeting of the American Association for the Surgery of Trauma. Reasons for readmission included fever, nausea and vomiting, partial small bowel obstruction, or deep vein thrombosis.
Morbidity affected 7% of patients in the form of urinary retention, wound infection, operative enterotomy, cecal serosal injury, deep vein thrombosis, or exacerbation of chronic obstructive pulmonary disease. One laparoscopic appendectomy was converted to open surgery; none of the patients died.
This is not the first time Dr. Frazee has presented his institution’s experience with the outpatient laparoscopic appendectomy protocol; he shared similar findings from an earlier series at the same meeting a few years ago. In an interview, he expressed some frustration that more hospitals haven’t adopted similar protocols.
By his rough calculation, 20% of all laparoscopic uncomplicated appendectomies performed in the United States each year cause perforations requiring hospitalization and 80% of the rest are successful outpatient procedures. That means 242,760 patients each year would not be hospitalized overnight for this surgery. Separate data show that the average U.S. length of hospitalization for laparoscopic appendectomy is 2 days, at an average cost of $1,900 per day. Nationwide adoption of an outpatient protocol potentially could avoid over $921 million in annual costs.
"It is time for us to create a change in the standard of care for uncomplicated appendicitis," said Dr. Frazee, chief of acute care surgery at Scott & White Healthcare in Temple, Tex.
His interest in the subject started when his son, an otherwise healthy young adult, complained about having to stay in the hospital after a laparoscopic appendectomy. Dr. Frazee conducted a review of 119 laparoscopic appendectomies at his institution and found that 35% of patients went home the same day, 61% were admitted for a day, and the few others were hospitalized longer. Morbidity was seen in 8%.
He and his colleagues developed an outpatient protocol in July 2010, under which patients undergoing uncomplicated laparoscopic appendectomies would not be admitted unless they were pregnant or younger than 17 years, or if a perforated or gangrenous appendicitis was discovered during the surgery. To qualify for same-day discharge, outpatients had to be able to tolerate intake of liquids, ambulate, urinate, and have adequate respiratory effort. They also had to be hemodynamically stable, have pain controlled with oral analgesics, have nausea and vomiting controlled, show no alteration in mental status from baseline, have the approval of their physician, and have appropriate supervision and assistance at home.
An initial review compared 116 patients treated under the protocol in 2010-2011 with historical controls and found a significant reduction in length of stay without increased morbidity. Under the protocol, 85% of patients were outpatients, compared with 35% in the control group. Postoperative morbidity affected 5% in the protocol group and 8% in the control group, and no patients were readmitted (Am. Surg. 2012;215:101-5).
Since then, the outpatient protocol has been the standard of care at his institution. The current report covers 166 men and 179 women treated under the protocol from July 2010 through December 2012. They had a mean age of 35 years and a mean body mass index of 31 kg/m2. Thirty-two percent had a history of prior abdominal surgery. Comorbidities at baseline included hypertension in 29%, diabetes in 11%, coronary artery disease in 4%, and chronic obstructive pulmonary disease in 1%.
Outpatients were sent home from the day surgery unit or the post–anesthetic care unit. Thirty percent were dismissed between 6 a.m. and noon, 15% went home between noon and 6 p.m., 25% were dismissed between 6 p.m. and midnight, and 30% went home between midnight and 6 a.m.
The investigators now are conducting a follow-up study to assess patient satisfaction with the protocol. "Our impression is that they like going home the same day," but a study will confirm whether this is true or not, he said.
Dr. Frazee reported having no financial disclosures.
AT THE AAST ANNUAL MEETING
Major finding: Outpatient laparoscopic uncomplicated appendectomies increased from 35% to 88% of the procedures under the outpatient protocol.
Data source: Review of 345 outpatient procedures at one institution from July 2010 through December 2012, compared with historical controls.
Disclosures: Dr. Frazee reported having no financial disclosures.
Two studies document a rise in gun wounds, homicides
SAN FRANCISCO – Deaths from gunshot wounds doubled between 2000 and 2012 in the region served by one New Jersey trauma center and gun-related homicides as a proportion of violent crimes increased by 27% in southern Arizona after the state stopped requiring permits for concealed weapons, separate studies found.
In 2000, 8% of patients treated for gunshot wounds died. That rate increased to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds seen at the New Jersey Trauma Center, a Level I trauma center in Newark. The proportion of 15-minute time increments in which the hospital was treating two or more patients for gunshot wounds increased from approximately 10% in 2000 to nearly 30% by the end of 2011, and the proportion of 15-minute increments in which three or more gunshot wounds were being treated increased from 1% to 16%, reported Dr. David H. Livingston and his associates.
Surgery on 71% of these patients plus other services incurred $115 million in costs, 75% of it unreimbursed. The mean cost per patient increased by 282% during the study period, reported Dr. Livingston of University Hospital, Newark, N.J., and a professor of surgery at Rutgers University, also in Newark.
"I think nationally this could be billions of dollars," perhaps double that, if these conservative estimates are extrapolated, he said at the annual meeting of the American Association for the Surgery of Trauma.
The drain on trauma center resources is enormous, he said. Half of the patients in his study needed ICU care, a third needed a ventilator, and just less than a third needed blood transfusions. All of these parameters increased by 50% to 180% during the study period.
The search for data produced a surprise relying solely on trauma registries for data on gunshot wounds and deaths would have missed one out of every five cases because 19% of patients were treated in the emergency department (ED) and sometimes admitted to services other than the trauma unit, he said. The study tapped not only the trauma registry but also ED billing records and the hospital’s financial records.
Further, there was a doubling of both the proportion of cases with three or more gunshot wounds (from 10% to 20%) and the proportion of cases with three or more body areas that had been shot (from 5% to 10%).
Data suggest that gun violence in New Jersey is geographically restricted and not random, he said. Five cities in the state accounted for 85% of gunshot wounds (Newark, Irvington, East Orange, Orange, and Elizabeth); 75% of patients were shot in the city in which they lived, 55% within a mile of home, 25% within a block of home, and 15% in their homes. Half of gunshot wounds occurred in 15% of the region by Census tract.
The New Jersey study included only interpersonal gunshot injuries, not self-inflicted wounds or shots from police. Patients in that study were predominantly young, black men who had been shot with a handgun. The mean age was 27 years, and 98% of cases involved a handgun. The cohort was 86% black, 9% Hispanic, 4% white, and 1% Asian. "This demographic is different than the demographic of our catchment area," Dr. Livingston noted.
A separate study compared gun-related injury and deaths in the 2 years before and the 2 years after July 2010, when Arizona made it legal in that state to carry a concealed weapon without a permit or training. The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that law was passed and deaths by firearms increased by 24% among victims of violent crimes and accidents, Dr. Rashna F. Ginwalla and her associates reported in a separate presentation.
The number of violent crimes and accidents stayed relatively stable, but the risk of any gun-related injury or death increased significantly by 11% after concealed-weapons regulations were eliminated, said Dr. Ginwalla, who led the study while at the University of Arizona, Tucson. Dr. Ginwalla now works in Rwanda for the University of Virginia, Charlottesville.
During the study period, Arizonans were more likely than was the general U.S. population to undergo a background check during a gun purchase, which the researchers used as a proxy for gun ownership. The study used data from the National Instant Criminal Background Check system, the trauma registry of the University of Arizona Medical Center (the only Level I trauma center for southern Arizona), the Pima County Medical Examiner’s Office, and the Tucson Police Department.
"While causality has not been established by this observational study, we have demonstrated an association between an increase in gun availability and gun-related homicides in the state," she said.
Dr. Ginwalla cited news reports that the United States has the highest per-capita gun ownership in the world – 89 gun owners/100,000 people, compared with the next-highest rates of 55/100,000 in Yemen, 46/100,000 in Switzerland, 45/100,000 in Finland, and 38/100,000 in Serbia.
Data on gun violence have been scarce since the U.S. Congress stopped funding federal research on gun violence in 1996. President Obama rescinded the ban in January 2013. The speakers said more research data could better inform debates about gun violence that invariably flare up after a mass shooting grabs headlines, such as the September 2013 shooting at the Washington Navy Yard and the December 2012 massacre at a Newtown, Conn. elementary school.
Perceptions of gun violence tend to be driven by these individual sensational events rather than "routine" gunshot wounds that happen much more frequently and in greater numbers, Dr. Livingston said. While the combined number of people killed and injured in the Navy Yard and Newtown shootings total in the dozens, an average of 527 people per year were treated for gunshot wounds just in the New Jersey study region. Of the 30,000 annual gunshot wounds, approximately half are self-inflicted and slightly less than half are the "routine" gunshot wounds happening every day, he said.
"Firearm violence continues to be a major public health problem in the United States," he said. "Unfortunately, it’s also a political football. Potential solutions are obfuscated and entwined with the controversy over gun control, turning a public health problem into a political debate."
Nonfatal gunshot wounds accounted for 85% of wounds in the study. "These are the ones that no one knows a lot about" because of the dearth of research, he added.
Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.
On Twitter @sherryboschert
Probably the most important message of the New Jersey study is that we need a reliable national database of firearm injuries. Most of the existing studies used trauma registries as their source of data. However, trauma registries, as was pointed out, do not include the victims who are treated and released from the emergency department. Further, victims can die at the scene and never reach hospital care; and not all victims are treated at trauma centers.
This major limitation of the registries causes a lot of confusion. For example, a recent front-page article in the Wall Street Journal reported a study that concluded that, over the last 6 years, the number of gunshot wounds has been increasing but the mortality rates have fallen, presumably because of better care. Another recent study reportedly found that over the same time period, the incidence of gunshot injuries has been going down while mortality has remained unchanged. It is obvious that we need a reliable national database to resolve these contradictions.
Dr. Demetrios Demetriades is a professor of surgery and director of acute care surgery at the University of Southern California, Los Angeles. He gave these remarks as the discussant of Dr. Livingston’s study at the meeting and reported having no financial disclosures.
Methodology, conclusions not firm
The issue of concealed-carry laws and their impact on violent crime has been a controversial political and public health issue in the United States. Currently, there are four types of concealed weapon laws. Five states now are unrestricted, like Arizona, where anyone can carry a concealed weapon without a state license. In 38 states, a permit is issued as long as the applicant meets certain requirements. Eight states "may" issue a permit and authorities may deny an applicant if a reasonable need to carry a concealed weapon in not met. The District of Columbia does not issue concealed weapons permits.
Proponents on both sides of this issue have used concealed-carry laws as a platform to espouse their viewpoints. However, today the general consensus of the public health community is that concealed weapons laws have minimal if any impact on violent crime in our nation relative to other legal political and societal factors.
Dr. Ginwalla and her colleagues sought to assess the impact of the state of Arizona’s repeal of its concealed-carry laws on gun-related injuries and deaths in the southern Arizona region. They concluded that after the repeal, gun-related homicides associated with violent crime increased significantly, presumably because of the increased presence of concealed weapons.
Although it seems intuitively reasonable that the increased access to concealed weapons would be related to the increase in gun-related fatalities in violent crimes, I have concerns regarding the study’s methodology and conclusions.
The entire "at-risk" population of violent crime decreased post repeal. Couldn’t we conclude that since there was less criminal activity after the repeal, concealed weapons were actually a deterrent?
Dr. Glen H. Tinkoff of Christiana Care Health System, Newark, Del., gave these comments as the discussant of Dr. Ginwall’s study at the meeting. He reported having no financial disclosures.
Probably the most important message of the New Jersey study is that we need a reliable national database of firearm injuries. Most of the existing studies used trauma registries as their source of data. However, trauma registries, as was pointed out, do not include the victims who are treated and released from the emergency department. Further, victims can die at the scene and never reach hospital care; and not all victims are treated at trauma centers.
This major limitation of the registries causes a lot of confusion. For example, a recent front-page article in the Wall Street Journal reported a study that concluded that, over the last 6 years, the number of gunshot wounds has been increasing but the mortality rates have fallen, presumably because of better care. Another recent study reportedly found that over the same time period, the incidence of gunshot injuries has been going down while mortality has remained unchanged. It is obvious that we need a reliable national database to resolve these contradictions.
Dr. Demetrios Demetriades is a professor of surgery and director of acute care surgery at the University of Southern California, Los Angeles. He gave these remarks as the discussant of Dr. Livingston’s study at the meeting and reported having no financial disclosures.
Methodology, conclusions not firm
The issue of concealed-carry laws and their impact on violent crime has been a controversial political and public health issue in the United States. Currently, there are four types of concealed weapon laws. Five states now are unrestricted, like Arizona, where anyone can carry a concealed weapon without a state license. In 38 states, a permit is issued as long as the applicant meets certain requirements. Eight states "may" issue a permit and authorities may deny an applicant if a reasonable need to carry a concealed weapon in not met. The District of Columbia does not issue concealed weapons permits.
Proponents on both sides of this issue have used concealed-carry laws as a platform to espouse their viewpoints. However, today the general consensus of the public health community is that concealed weapons laws have minimal if any impact on violent crime in our nation relative to other legal political and societal factors.
Dr. Ginwalla and her colleagues sought to assess the impact of the state of Arizona’s repeal of its concealed-carry laws on gun-related injuries and deaths in the southern Arizona region. They concluded that after the repeal, gun-related homicides associated with violent crime increased significantly, presumably because of the increased presence of concealed weapons.
Although it seems intuitively reasonable that the increased access to concealed weapons would be related to the increase in gun-related fatalities in violent crimes, I have concerns regarding the study’s methodology and conclusions.
The entire "at-risk" population of violent crime decreased post repeal. Couldn’t we conclude that since there was less criminal activity after the repeal, concealed weapons were actually a deterrent?
Dr. Glen H. Tinkoff of Christiana Care Health System, Newark, Del., gave these comments as the discussant of Dr. Ginwall’s study at the meeting. He reported having no financial disclosures.
Probably the most important message of the New Jersey study is that we need a reliable national database of firearm injuries. Most of the existing studies used trauma registries as their source of data. However, trauma registries, as was pointed out, do not include the victims who are treated and released from the emergency department. Further, victims can die at the scene and never reach hospital care; and not all victims are treated at trauma centers.
This major limitation of the registries causes a lot of confusion. For example, a recent front-page article in the Wall Street Journal reported a study that concluded that, over the last 6 years, the number of gunshot wounds has been increasing but the mortality rates have fallen, presumably because of better care. Another recent study reportedly found that over the same time period, the incidence of gunshot injuries has been going down while mortality has remained unchanged. It is obvious that we need a reliable national database to resolve these contradictions.
Dr. Demetrios Demetriades is a professor of surgery and director of acute care surgery at the University of Southern California, Los Angeles. He gave these remarks as the discussant of Dr. Livingston’s study at the meeting and reported having no financial disclosures.
Methodology, conclusions not firm
The issue of concealed-carry laws and their impact on violent crime has been a controversial political and public health issue in the United States. Currently, there are four types of concealed weapon laws. Five states now are unrestricted, like Arizona, where anyone can carry a concealed weapon without a state license. In 38 states, a permit is issued as long as the applicant meets certain requirements. Eight states "may" issue a permit and authorities may deny an applicant if a reasonable need to carry a concealed weapon in not met. The District of Columbia does not issue concealed weapons permits.
Proponents on both sides of this issue have used concealed-carry laws as a platform to espouse their viewpoints. However, today the general consensus of the public health community is that concealed weapons laws have minimal if any impact on violent crime in our nation relative to other legal political and societal factors.
Dr. Ginwalla and her colleagues sought to assess the impact of the state of Arizona’s repeal of its concealed-carry laws on gun-related injuries and deaths in the southern Arizona region. They concluded that after the repeal, gun-related homicides associated with violent crime increased significantly, presumably because of the increased presence of concealed weapons.
Although it seems intuitively reasonable that the increased access to concealed weapons would be related to the increase in gun-related fatalities in violent crimes, I have concerns regarding the study’s methodology and conclusions.
The entire "at-risk" population of violent crime decreased post repeal. Couldn’t we conclude that since there was less criminal activity after the repeal, concealed weapons were actually a deterrent?
Dr. Glen H. Tinkoff of Christiana Care Health System, Newark, Del., gave these comments as the discussant of Dr. Ginwall’s study at the meeting. He reported having no financial disclosures.
SAN FRANCISCO – Deaths from gunshot wounds doubled between 2000 and 2012 in the region served by one New Jersey trauma center and gun-related homicides as a proportion of violent crimes increased by 27% in southern Arizona after the state stopped requiring permits for concealed weapons, separate studies found.
In 2000, 8% of patients treated for gunshot wounds died. That rate increased to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds seen at the New Jersey Trauma Center, a Level I trauma center in Newark. The proportion of 15-minute time increments in which the hospital was treating two or more patients for gunshot wounds increased from approximately 10% in 2000 to nearly 30% by the end of 2011, and the proportion of 15-minute increments in which three or more gunshot wounds were being treated increased from 1% to 16%, reported Dr. David H. Livingston and his associates.
Surgery on 71% of these patients plus other services incurred $115 million in costs, 75% of it unreimbursed. The mean cost per patient increased by 282% during the study period, reported Dr. Livingston of University Hospital, Newark, N.J., and a professor of surgery at Rutgers University, also in Newark.
"I think nationally this could be billions of dollars," perhaps double that, if these conservative estimates are extrapolated, he said at the annual meeting of the American Association for the Surgery of Trauma.
The drain on trauma center resources is enormous, he said. Half of the patients in his study needed ICU care, a third needed a ventilator, and just less than a third needed blood transfusions. All of these parameters increased by 50% to 180% during the study period.
The search for data produced a surprise relying solely on trauma registries for data on gunshot wounds and deaths would have missed one out of every five cases because 19% of patients were treated in the emergency department (ED) and sometimes admitted to services other than the trauma unit, he said. The study tapped not only the trauma registry but also ED billing records and the hospital’s financial records.
Further, there was a doubling of both the proportion of cases with three or more gunshot wounds (from 10% to 20%) and the proportion of cases with three or more body areas that had been shot (from 5% to 10%).
Data suggest that gun violence in New Jersey is geographically restricted and not random, he said. Five cities in the state accounted for 85% of gunshot wounds (Newark, Irvington, East Orange, Orange, and Elizabeth); 75% of patients were shot in the city in which they lived, 55% within a mile of home, 25% within a block of home, and 15% in their homes. Half of gunshot wounds occurred in 15% of the region by Census tract.
The New Jersey study included only interpersonal gunshot injuries, not self-inflicted wounds or shots from police. Patients in that study were predominantly young, black men who had been shot with a handgun. The mean age was 27 years, and 98% of cases involved a handgun. The cohort was 86% black, 9% Hispanic, 4% white, and 1% Asian. "This demographic is different than the demographic of our catchment area," Dr. Livingston noted.
A separate study compared gun-related injury and deaths in the 2 years before and the 2 years after July 2010, when Arizona made it legal in that state to carry a concealed weapon without a permit or training. The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that law was passed and deaths by firearms increased by 24% among victims of violent crimes and accidents, Dr. Rashna F. Ginwalla and her associates reported in a separate presentation.
The number of violent crimes and accidents stayed relatively stable, but the risk of any gun-related injury or death increased significantly by 11% after concealed-weapons regulations were eliminated, said Dr. Ginwalla, who led the study while at the University of Arizona, Tucson. Dr. Ginwalla now works in Rwanda for the University of Virginia, Charlottesville.
During the study period, Arizonans were more likely than was the general U.S. population to undergo a background check during a gun purchase, which the researchers used as a proxy for gun ownership. The study used data from the National Instant Criminal Background Check system, the trauma registry of the University of Arizona Medical Center (the only Level I trauma center for southern Arizona), the Pima County Medical Examiner’s Office, and the Tucson Police Department.
"While causality has not been established by this observational study, we have demonstrated an association between an increase in gun availability and gun-related homicides in the state," she said.
Dr. Ginwalla cited news reports that the United States has the highest per-capita gun ownership in the world – 89 gun owners/100,000 people, compared with the next-highest rates of 55/100,000 in Yemen, 46/100,000 in Switzerland, 45/100,000 in Finland, and 38/100,000 in Serbia.
Data on gun violence have been scarce since the U.S. Congress stopped funding federal research on gun violence in 1996. President Obama rescinded the ban in January 2013. The speakers said more research data could better inform debates about gun violence that invariably flare up after a mass shooting grabs headlines, such as the September 2013 shooting at the Washington Navy Yard and the December 2012 massacre at a Newtown, Conn. elementary school.
Perceptions of gun violence tend to be driven by these individual sensational events rather than "routine" gunshot wounds that happen much more frequently and in greater numbers, Dr. Livingston said. While the combined number of people killed and injured in the Navy Yard and Newtown shootings total in the dozens, an average of 527 people per year were treated for gunshot wounds just in the New Jersey study region. Of the 30,000 annual gunshot wounds, approximately half are self-inflicted and slightly less than half are the "routine" gunshot wounds happening every day, he said.
"Firearm violence continues to be a major public health problem in the United States," he said. "Unfortunately, it’s also a political football. Potential solutions are obfuscated and entwined with the controversy over gun control, turning a public health problem into a political debate."
Nonfatal gunshot wounds accounted for 85% of wounds in the study. "These are the ones that no one knows a lot about" because of the dearth of research, he added.
Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Deaths from gunshot wounds doubled between 2000 and 2012 in the region served by one New Jersey trauma center and gun-related homicides as a proportion of violent crimes increased by 27% in southern Arizona after the state stopped requiring permits for concealed weapons, separate studies found.
In 2000, 8% of patients treated for gunshot wounds died. That rate increased to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds seen at the New Jersey Trauma Center, a Level I trauma center in Newark. The proportion of 15-minute time increments in which the hospital was treating two or more patients for gunshot wounds increased from approximately 10% in 2000 to nearly 30% by the end of 2011, and the proportion of 15-minute increments in which three or more gunshot wounds were being treated increased from 1% to 16%, reported Dr. David H. Livingston and his associates.
Surgery on 71% of these patients plus other services incurred $115 million in costs, 75% of it unreimbursed. The mean cost per patient increased by 282% during the study period, reported Dr. Livingston of University Hospital, Newark, N.J., and a professor of surgery at Rutgers University, also in Newark.
"I think nationally this could be billions of dollars," perhaps double that, if these conservative estimates are extrapolated, he said at the annual meeting of the American Association for the Surgery of Trauma.
The drain on trauma center resources is enormous, he said. Half of the patients in his study needed ICU care, a third needed a ventilator, and just less than a third needed blood transfusions. All of these parameters increased by 50% to 180% during the study period.
The search for data produced a surprise relying solely on trauma registries for data on gunshot wounds and deaths would have missed one out of every five cases because 19% of patients were treated in the emergency department (ED) and sometimes admitted to services other than the trauma unit, he said. The study tapped not only the trauma registry but also ED billing records and the hospital’s financial records.
Further, there was a doubling of both the proportion of cases with three or more gunshot wounds (from 10% to 20%) and the proportion of cases with three or more body areas that had been shot (from 5% to 10%).
Data suggest that gun violence in New Jersey is geographically restricted and not random, he said. Five cities in the state accounted for 85% of gunshot wounds (Newark, Irvington, East Orange, Orange, and Elizabeth); 75% of patients were shot in the city in which they lived, 55% within a mile of home, 25% within a block of home, and 15% in their homes. Half of gunshot wounds occurred in 15% of the region by Census tract.
The New Jersey study included only interpersonal gunshot injuries, not self-inflicted wounds or shots from police. Patients in that study were predominantly young, black men who had been shot with a handgun. The mean age was 27 years, and 98% of cases involved a handgun. The cohort was 86% black, 9% Hispanic, 4% white, and 1% Asian. "This demographic is different than the demographic of our catchment area," Dr. Livingston noted.
A separate study compared gun-related injury and deaths in the 2 years before and the 2 years after July 2010, when Arizona made it legal in that state to carry a concealed weapon without a permit or training. The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that law was passed and deaths by firearms increased by 24% among victims of violent crimes and accidents, Dr. Rashna F. Ginwalla and her associates reported in a separate presentation.
The number of violent crimes and accidents stayed relatively stable, but the risk of any gun-related injury or death increased significantly by 11% after concealed-weapons regulations were eliminated, said Dr. Ginwalla, who led the study while at the University of Arizona, Tucson. Dr. Ginwalla now works in Rwanda for the University of Virginia, Charlottesville.
During the study period, Arizonans were more likely than was the general U.S. population to undergo a background check during a gun purchase, which the researchers used as a proxy for gun ownership. The study used data from the National Instant Criminal Background Check system, the trauma registry of the University of Arizona Medical Center (the only Level I trauma center for southern Arizona), the Pima County Medical Examiner’s Office, and the Tucson Police Department.
"While causality has not been established by this observational study, we have demonstrated an association between an increase in gun availability and gun-related homicides in the state," she said.
Dr. Ginwalla cited news reports that the United States has the highest per-capita gun ownership in the world – 89 gun owners/100,000 people, compared with the next-highest rates of 55/100,000 in Yemen, 46/100,000 in Switzerland, 45/100,000 in Finland, and 38/100,000 in Serbia.
Data on gun violence have been scarce since the U.S. Congress stopped funding federal research on gun violence in 1996. President Obama rescinded the ban in January 2013. The speakers said more research data could better inform debates about gun violence that invariably flare up after a mass shooting grabs headlines, such as the September 2013 shooting at the Washington Navy Yard and the December 2012 massacre at a Newtown, Conn. elementary school.
Perceptions of gun violence tend to be driven by these individual sensational events rather than "routine" gunshot wounds that happen much more frequently and in greater numbers, Dr. Livingston said. While the combined number of people killed and injured in the Navy Yard and Newtown shootings total in the dozens, an average of 527 people per year were treated for gunshot wounds just in the New Jersey study region. Of the 30,000 annual gunshot wounds, approximately half are self-inflicted and slightly less than half are the "routine" gunshot wounds happening every day, he said.
"Firearm violence continues to be a major public health problem in the United States," he said. "Unfortunately, it’s also a political football. Potential solutions are obfuscated and entwined with the controversy over gun control, turning a public health problem into a political debate."
Nonfatal gunshot wounds accounted for 85% of wounds in the study. "These are the ones that no one knows a lot about" because of the dearth of research, he added.
Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.
On Twitter @sherryboschert
AT THE AAST ANNUAL MEETING
Major finding: The proportion of homicides related to guns in southern Arizona increased significantly from 1.97% to 2.45% after that state passed a law making it legal to carry a concealed weapon without a permit or training. In one New Jersey trauma center, the rate of deaths among gunshot wound victims rose from 8% in 2000 to 15% in 2011, according to a retrospective study of 6,323 gunshot wounds
Data source: A retrospective review of 6,323 gunshot wounds treated at one New Jersey trauma center from 2000-2011, and a retrospective review of data in southern Arizona 2 years before and after a 2010 law repealed concealed-carry limits.
Disclosures: Dr. Livingston and Dr. Ginwalla reported having no financial disclosures.