User login
Antidepressant-induced cardioprotection after event reverses with a vengeance
SAN FRANCISCO – If ever a study drove home the point that depression – including post–acute coronary syndrome depression – is a chronic relapsing disorder requiring long-term maintenance therapy, it’s the COPES trial.
COPES (Collaborative Psychosocial Evaluation Studies) was a randomized, prospective, single-blind trial in which patients with persistent depressive symptoms after an ACS event received 6 months of enhanced, centralized antidepressant therapy or usual care. Six months post randomization, the intervention group showed significantly lower depression scores than controls did, together with an accompanying impressive reduction in the combined endpoint of death, myocardial infarction (MI), or unstable angina.
That’s the good news. The COPES message that effective antidepressant therapy appears to reduce the risk of recurrent cardiac events has met with a warm reception.
Now the bad news: A just-completed 2-year follow-up of COPES participants showed that the cardioprotective benefit didn’t persist. Between 6 months and 2 years, a catch-up phenomenon occurred, such that at the 2-year mark the cumulative cardiac event rate in the intervention and usual-care arms was essentially the same, Dr. Siqin Ye reported at the annual meeting of the American College of Cardiology.
"Depression is a relapsing, remitting chronic illness, and the effect of brief enhanced depression therapy after ACS may diminish over time. In future studies we’re going to need to examine how the benefits of short-term depression therapy can be sustained long-term in post-ACS patients with depression," said Dr. Ye, a cardiologist at the Center for Behavioral Cardiovascular Health of Columbia University Medical Center, New York.
That should not be difficult to accomplish, he explained in an interview. The main form of antidepressant therapy utilized in COPES, known as problem-solving therapy, can be delivered over the phone or on the Internet, making it amenable to ongoing, periodic, low-cost maintenance therapy sessions.
COPES included 157 patients with persistent depressive symptoms after an ACS event as defined by a Beck Depression Inventory score of 10 or more both during their initial hospitalization and 3 months later. They were randomized to enhanced depression therapy involving their choice of problem-solving therapy and/or antidepressant medication using a stepped-care approach with reevaluation and adjustments every 8 weeks, or to usual care. The primary care physicians and cardiologists of patients in the usual-care group received a letter from the investigators informing them that their patient had elevated depressive symptoms.
Three-quarters of patients in the intervention group opted for problem-solving therapy, 20% chose medication, and the rest picked dual therapy. Once the 6-month intervention ended, there were no more problem-solving therapy sessions, and continuation of antidepressant medications was left up to the patient’s own physicians.
Problem-solving therapy is a brief, protocol-driven therapy in which patients are taught how to evaluate and address their psychosocial problems. It was originally developed for use in the IMPACT (Improving Mood-Promoting Access to Collaborative Treatment) trial (JAMA 2002;288:2836-45). In COPES, patients had weekly individual sessions with a psychiatrist or other mental health professional trained in problem-solving therapy that lasted 30-45 minutes.
During the 6-month intervention, 3 major cardiac events occurred in the intervention group, compared with 11 in the usual-care arm. However, between 6 months and 2 years, there were 2 deaths and 9 hospitalizations for acute MI or unstable angina in the original intervention group, compared with 1 death and 2 hospitalizations among controls. Thus, the 2-year total was 14 events in each group.
Stated another way, the risk of a major cardiac event in the enhanced depression therapy group was 77% lower than in the usual-care group during the 6 months of the intervention, but afterward it was 3.4-fold higher than in the usual-care group, according to Dr. Ye.
The COPES trial was funded by the National Heart, Lung, and Blood Institute. Dr. Ye reported having no financial conflicts.
SAN FRANCISCO – If ever a study drove home the point that depression – including post–acute coronary syndrome depression – is a chronic relapsing disorder requiring long-term maintenance therapy, it’s the COPES trial.
COPES (Collaborative Psychosocial Evaluation Studies) was a randomized, prospective, single-blind trial in which patients with persistent depressive symptoms after an ACS event received 6 months of enhanced, centralized antidepressant therapy or usual care. Six months post randomization, the intervention group showed significantly lower depression scores than controls did, together with an accompanying impressive reduction in the combined endpoint of death, myocardial infarction (MI), or unstable angina.
That’s the good news. The COPES message that effective antidepressant therapy appears to reduce the risk of recurrent cardiac events has met with a warm reception.
Now the bad news: A just-completed 2-year follow-up of COPES participants showed that the cardioprotective benefit didn’t persist. Between 6 months and 2 years, a catch-up phenomenon occurred, such that at the 2-year mark the cumulative cardiac event rate in the intervention and usual-care arms was essentially the same, Dr. Siqin Ye reported at the annual meeting of the American College of Cardiology.
"Depression is a relapsing, remitting chronic illness, and the effect of brief enhanced depression therapy after ACS may diminish over time. In future studies we’re going to need to examine how the benefits of short-term depression therapy can be sustained long-term in post-ACS patients with depression," said Dr. Ye, a cardiologist at the Center for Behavioral Cardiovascular Health of Columbia University Medical Center, New York.
That should not be difficult to accomplish, he explained in an interview. The main form of antidepressant therapy utilized in COPES, known as problem-solving therapy, can be delivered over the phone or on the Internet, making it amenable to ongoing, periodic, low-cost maintenance therapy sessions.
COPES included 157 patients with persistent depressive symptoms after an ACS event as defined by a Beck Depression Inventory score of 10 or more both during their initial hospitalization and 3 months later. They were randomized to enhanced depression therapy involving their choice of problem-solving therapy and/or antidepressant medication using a stepped-care approach with reevaluation and adjustments every 8 weeks, or to usual care. The primary care physicians and cardiologists of patients in the usual-care group received a letter from the investigators informing them that their patient had elevated depressive symptoms.
Three-quarters of patients in the intervention group opted for problem-solving therapy, 20% chose medication, and the rest picked dual therapy. Once the 6-month intervention ended, there were no more problem-solving therapy sessions, and continuation of antidepressant medications was left up to the patient’s own physicians.
Problem-solving therapy is a brief, protocol-driven therapy in which patients are taught how to evaluate and address their psychosocial problems. It was originally developed for use in the IMPACT (Improving Mood-Promoting Access to Collaborative Treatment) trial (JAMA 2002;288:2836-45). In COPES, patients had weekly individual sessions with a psychiatrist or other mental health professional trained in problem-solving therapy that lasted 30-45 minutes.
During the 6-month intervention, 3 major cardiac events occurred in the intervention group, compared with 11 in the usual-care arm. However, between 6 months and 2 years, there were 2 deaths and 9 hospitalizations for acute MI or unstable angina in the original intervention group, compared with 1 death and 2 hospitalizations among controls. Thus, the 2-year total was 14 events in each group.
Stated another way, the risk of a major cardiac event in the enhanced depression therapy group was 77% lower than in the usual-care group during the 6 months of the intervention, but afterward it was 3.4-fold higher than in the usual-care group, according to Dr. Ye.
The COPES trial was funded by the National Heart, Lung, and Blood Institute. Dr. Ye reported having no financial conflicts.
SAN FRANCISCO – If ever a study drove home the point that depression – including post–acute coronary syndrome depression – is a chronic relapsing disorder requiring long-term maintenance therapy, it’s the COPES trial.
COPES (Collaborative Psychosocial Evaluation Studies) was a randomized, prospective, single-blind trial in which patients with persistent depressive symptoms after an ACS event received 6 months of enhanced, centralized antidepressant therapy or usual care. Six months post randomization, the intervention group showed significantly lower depression scores than controls did, together with an accompanying impressive reduction in the combined endpoint of death, myocardial infarction (MI), or unstable angina.
That’s the good news. The COPES message that effective antidepressant therapy appears to reduce the risk of recurrent cardiac events has met with a warm reception.
Now the bad news: A just-completed 2-year follow-up of COPES participants showed that the cardioprotective benefit didn’t persist. Between 6 months and 2 years, a catch-up phenomenon occurred, such that at the 2-year mark the cumulative cardiac event rate in the intervention and usual-care arms was essentially the same, Dr. Siqin Ye reported at the annual meeting of the American College of Cardiology.
"Depression is a relapsing, remitting chronic illness, and the effect of brief enhanced depression therapy after ACS may diminish over time. In future studies we’re going to need to examine how the benefits of short-term depression therapy can be sustained long-term in post-ACS patients with depression," said Dr. Ye, a cardiologist at the Center for Behavioral Cardiovascular Health of Columbia University Medical Center, New York.
That should not be difficult to accomplish, he explained in an interview. The main form of antidepressant therapy utilized in COPES, known as problem-solving therapy, can be delivered over the phone or on the Internet, making it amenable to ongoing, periodic, low-cost maintenance therapy sessions.
COPES included 157 patients with persistent depressive symptoms after an ACS event as defined by a Beck Depression Inventory score of 10 or more both during their initial hospitalization and 3 months later. They were randomized to enhanced depression therapy involving their choice of problem-solving therapy and/or antidepressant medication using a stepped-care approach with reevaluation and adjustments every 8 weeks, or to usual care. The primary care physicians and cardiologists of patients in the usual-care group received a letter from the investigators informing them that their patient had elevated depressive symptoms.
Three-quarters of patients in the intervention group opted for problem-solving therapy, 20% chose medication, and the rest picked dual therapy. Once the 6-month intervention ended, there were no more problem-solving therapy sessions, and continuation of antidepressant medications was left up to the patient’s own physicians.
Problem-solving therapy is a brief, protocol-driven therapy in which patients are taught how to evaluate and address their psychosocial problems. It was originally developed for use in the IMPACT (Improving Mood-Promoting Access to Collaborative Treatment) trial (JAMA 2002;288:2836-45). In COPES, patients had weekly individual sessions with a psychiatrist or other mental health professional trained in problem-solving therapy that lasted 30-45 minutes.
During the 6-month intervention, 3 major cardiac events occurred in the intervention group, compared with 11 in the usual-care arm. However, between 6 months and 2 years, there were 2 deaths and 9 hospitalizations for acute MI or unstable angina in the original intervention group, compared with 1 death and 2 hospitalizations among controls. Thus, the 2-year total was 14 events in each group.
Stated another way, the risk of a major cardiac event in the enhanced depression therapy group was 77% lower than in the usual-care group during the 6 months of the intervention, but afterward it was 3.4-fold higher than in the usual-care group, according to Dr. Ye.
The COPES trial was funded by the National Heart, Lung, and Blood Institute. Dr. Ye reported having no financial conflicts.
AT ACC 13
Major finding: Patients with persistent depression post acute coronary syndrome had a 77% reduction in death, MI, or unstable angina during the 6 months they were on enhanced antidepressant therapy, compared with similar patients on usual care. However, a rebound effect was seen such that their risk of a major cardiac event during the next 18 months was 3.4-fold greater than in controls.
Data source: The COPES trial was a randomized, prospective, multicenter, single-blind trial involving 157 patients with persistent depression after ACS.
Disclosures: The COPES trial was funded by the National Heart, Lung, and Blood Institute. The presenter reported having no financial conflicts.
Atrial fib symptoms milder but mortality higher in men
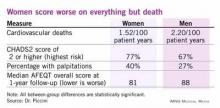
SAN FRANCISCO – Women with atrial fibrillation have significantly more debilitation than men with the disorder, but men with atrial fibrillation have double the cardiovascular death rate than their female counterparts, based on data collected from more than 10,000 U.S. patients.
During follow-up of the 5,842 men and 4,290 women with atrial fibrillation who were enrolled in the registry, women’s cumulative rate of cardiovascular death lagged 54% behind men’s, a statistically significant difference, Dr. Jonathan P. Piccini reported at the annual meeting of the American College of Cardiology.
The rate of all-cause death ran a relative 31% lower in women compared with men, but this difference seemed mostly due to the cardiovascular-death disparity because rates of noncardiovascular deaths in women and men with atrial fibrillation were virtually identical, said Dr. Piccini, an electrophysiology cardiologist at Duke University in Durham, N.C.
Despite this survival advantage, women with atrial fibrillation fare worse than men by several other measures. Women report worse symptoms, more functional impairment, and worse quality of life; they also spend significantly less time in their target anticoagulant range and they have a higher stroke risk than men, he reported.
"When we see women with atrial fibrillation, we should be aware that they are more likely to have worse symptoms and quality of life. Symptoms need to be treated; when a patient persists in having symptoms, treatment to control the symptoms is very important," he said in an interview. "We need to investigate the registry data to see why women have more symptoms and worse quality of life. This is the largest quality of life study ever done in atrial fibrillation."
Among the 10,132 patients enrolled in the registry, 1,339 participated in a substudy that serially measured quality of life using the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire (Circ. Arrhythm. Electrophysiol. 2011;4:15-25). "We have the power to look at the effects of different treatments so we can assess how changing treatment affects quality of life," Dr. Piccini said.
The Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT AF) enrolled both prevalent and new-onset atrial fibrillation patients at 184 diverse practice settings, including primary care, cardiology, and electrophysiology offices, between June 2010 and August 2011. The enrolled men were an average of 73 years old, while the women averaged 77 years of age.
Coronary disease was present in 39% of men and 23% of the women, but 17% of the women had a history of stroke or transient ischemic attack, compared with 14% of the men. Both sexes had a similar distribution of atrial fibrillation type, but women had clearly higher CHADS2 scores, a measure of stroke risk. The percentage of patients with a score of 0 or 1, the lowest-risk patients, was 33% among men and 23% among women.
Every symptom assessed was more common among women, led by the most frequent symptom, palpitations, which affected 40% of women and 27% of men. The next most common symptoms – exertional dyspnea, fatigue, and lightheadedness – were each several percentage points more common in women than men, all statistically significant differences.
Reassuringly, use of rate and rhythm-control treatments and oral anticoagulation were very similar among men and women, but women more frequently had a prolonged gap between their anticoagulation checkups, and their time spent within the target international normalized ratio of 2.0-3.0 was 65%, significantly below the 68% rate in men.
The rate of new heart failure during follow-up was the same in the men and women. Women had higher stroke risk based on their CHADS2 scores, but their stroke rate, while numerically greater than in men, was not significantly higher.
AFEQT results from the registry subset showed that women had significantly worse (lower) scores than men overall and for each of four AFEQT component scores tallied at both baseline and 1-year follow-up: symptoms, daily activity, treatment concern, and treatment satisfaction.
The ORBIT AF registry is sponsored by Janssen. Dr. Piccini said that he has financial relationships with Boston Scientific, GE Healthcare, Janssen, Johnson & Johnson, Medtronic, and Pfizer Bristol-Myers Squibb.
On Twitter @mitchelzoler
SAN FRANCISCO – Women with atrial fibrillation have significantly more debilitation than men with the disorder, but men with atrial fibrillation have double the cardiovascular death rate than their female counterparts, based on data collected from more than 10,000 U.S. patients.
During follow-up of the 5,842 men and 4,290 women with atrial fibrillation who were enrolled in the registry, women’s cumulative rate of cardiovascular death lagged 54% behind men’s, a statistically significant difference, Dr. Jonathan P. Piccini reported at the annual meeting of the American College of Cardiology.
The rate of all-cause death ran a relative 31% lower in women compared with men, but this difference seemed mostly due to the cardiovascular-death disparity because rates of noncardiovascular deaths in women and men with atrial fibrillation were virtually identical, said Dr. Piccini, an electrophysiology cardiologist at Duke University in Durham, N.C.
Despite this survival advantage, women with atrial fibrillation fare worse than men by several other measures. Women report worse symptoms, more functional impairment, and worse quality of life; they also spend significantly less time in their target anticoagulant range and they have a higher stroke risk than men, he reported.
"When we see women with atrial fibrillation, we should be aware that they are more likely to have worse symptoms and quality of life. Symptoms need to be treated; when a patient persists in having symptoms, treatment to control the symptoms is very important," he said in an interview. "We need to investigate the registry data to see why women have more symptoms and worse quality of life. This is the largest quality of life study ever done in atrial fibrillation."
Among the 10,132 patients enrolled in the registry, 1,339 participated in a substudy that serially measured quality of life using the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire (Circ. Arrhythm. Electrophysiol. 2011;4:15-25). "We have the power to look at the effects of different treatments so we can assess how changing treatment affects quality of life," Dr. Piccini said.
The Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT AF) enrolled both prevalent and new-onset atrial fibrillation patients at 184 diverse practice settings, including primary care, cardiology, and electrophysiology offices, between June 2010 and August 2011. The enrolled men were an average of 73 years old, while the women averaged 77 years of age.
Coronary disease was present in 39% of men and 23% of the women, but 17% of the women had a history of stroke or transient ischemic attack, compared with 14% of the men. Both sexes had a similar distribution of atrial fibrillation type, but women had clearly higher CHADS2 scores, a measure of stroke risk. The percentage of patients with a score of 0 or 1, the lowest-risk patients, was 33% among men and 23% among women.
Every symptom assessed was more common among women, led by the most frequent symptom, palpitations, which affected 40% of women and 27% of men. The next most common symptoms – exertional dyspnea, fatigue, and lightheadedness – were each several percentage points more common in women than men, all statistically significant differences.
Reassuringly, use of rate and rhythm-control treatments and oral anticoagulation were very similar among men and women, but women more frequently had a prolonged gap between their anticoagulation checkups, and their time spent within the target international normalized ratio of 2.0-3.0 was 65%, significantly below the 68% rate in men.
The rate of new heart failure during follow-up was the same in the men and women. Women had higher stroke risk based on their CHADS2 scores, but their stroke rate, while numerically greater than in men, was not significantly higher.
AFEQT results from the registry subset showed that women had significantly worse (lower) scores than men overall and for each of four AFEQT component scores tallied at both baseline and 1-year follow-up: symptoms, daily activity, treatment concern, and treatment satisfaction.
The ORBIT AF registry is sponsored by Janssen. Dr. Piccini said that he has financial relationships with Boston Scientific, GE Healthcare, Janssen, Johnson & Johnson, Medtronic, and Pfizer Bristol-Myers Squibb.
On Twitter @mitchelzoler
SAN FRANCISCO – Women with atrial fibrillation have significantly more debilitation than men with the disorder, but men with atrial fibrillation have double the cardiovascular death rate than their female counterparts, based on data collected from more than 10,000 U.S. patients.
During follow-up of the 5,842 men and 4,290 women with atrial fibrillation who were enrolled in the registry, women’s cumulative rate of cardiovascular death lagged 54% behind men’s, a statistically significant difference, Dr. Jonathan P. Piccini reported at the annual meeting of the American College of Cardiology.
The rate of all-cause death ran a relative 31% lower in women compared with men, but this difference seemed mostly due to the cardiovascular-death disparity because rates of noncardiovascular deaths in women and men with atrial fibrillation were virtually identical, said Dr. Piccini, an electrophysiology cardiologist at Duke University in Durham, N.C.
Despite this survival advantage, women with atrial fibrillation fare worse than men by several other measures. Women report worse symptoms, more functional impairment, and worse quality of life; they also spend significantly less time in their target anticoagulant range and they have a higher stroke risk than men, he reported.
"When we see women with atrial fibrillation, we should be aware that they are more likely to have worse symptoms and quality of life. Symptoms need to be treated; when a patient persists in having symptoms, treatment to control the symptoms is very important," he said in an interview. "We need to investigate the registry data to see why women have more symptoms and worse quality of life. This is the largest quality of life study ever done in atrial fibrillation."
Among the 10,132 patients enrolled in the registry, 1,339 participated in a substudy that serially measured quality of life using the Atrial Fibrillation Effect on Quality of Life (AFEQT) questionnaire (Circ. Arrhythm. Electrophysiol. 2011;4:15-25). "We have the power to look at the effects of different treatments so we can assess how changing treatment affects quality of life," Dr. Piccini said.
The Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT AF) enrolled both prevalent and new-onset atrial fibrillation patients at 184 diverse practice settings, including primary care, cardiology, and electrophysiology offices, between June 2010 and August 2011. The enrolled men were an average of 73 years old, while the women averaged 77 years of age.
Coronary disease was present in 39% of men and 23% of the women, but 17% of the women had a history of stroke or transient ischemic attack, compared with 14% of the men. Both sexes had a similar distribution of atrial fibrillation type, but women had clearly higher CHADS2 scores, a measure of stroke risk. The percentage of patients with a score of 0 or 1, the lowest-risk patients, was 33% among men and 23% among women.
Every symptom assessed was more common among women, led by the most frequent symptom, palpitations, which affected 40% of women and 27% of men. The next most common symptoms – exertional dyspnea, fatigue, and lightheadedness – were each several percentage points more common in women than men, all statistically significant differences.
Reassuringly, use of rate and rhythm-control treatments and oral anticoagulation were very similar among men and women, but women more frequently had a prolonged gap between their anticoagulation checkups, and their time spent within the target international normalized ratio of 2.0-3.0 was 65%, significantly below the 68% rate in men.
The rate of new heart failure during follow-up was the same in the men and women. Women had higher stroke risk based on their CHADS2 scores, but their stroke rate, while numerically greater than in men, was not significantly higher.
AFEQT results from the registry subset showed that women had significantly worse (lower) scores than men overall and for each of four AFEQT component scores tallied at both baseline and 1-year follow-up: symptoms, daily activity, treatment concern, and treatment satisfaction.
The ORBIT AF registry is sponsored by Janssen. Dr. Piccini said that he has financial relationships with Boston Scientific, GE Healthcare, Janssen, Johnson & Johnson, Medtronic, and Pfizer Bristol-Myers Squibb.
On Twitter @mitchelzoler
AT ACC 13
Major finding: Cardiovascular death in women with atrial fibrillation was 54% lower than affected men after adjustment for clinical differences.
Data source: ORBIT AF registry, which included 10,132 adults enrolled at 184 U.S. sites.
Disclosures: The ORBIT AF registry is sponsored by Janssen. Dr. Piccini said that he has financial relationships with Boston Scientific, GE Healthcare, Janssen, Johnson & Johnson, Medtronic, and Pfizer Bristol-Myers Squibb.
Can digoxin get another chance for heart failure?
One of the late-breaker reports at the American College of Cardiology’s annual meeting in March had results from a post hoc analysis of 16-year-old data from the DIG trial, by far the largest study to ever assess digoxin for heart failure, a treatment that precipitously dropped out of favor during the decade following the initial DIG report in 1997. Not your typical back story for a late breaker.
The researchers who ran the new analysis of the old DIG data also took what seem like two sizable leaps by framing their new look as a way to get a sense whether digoxin treatment could cut the large number of Medicare patients with heart failure who need rehospitalization within a month after a hospital discharge.
Dr. Ali Ahmed, a cardiologist from the University of Alabama, Birmingham, who presented this ACC late breaker, noted how clinicians and hospital officials are eager to find safe and effective treatments for cutting heart failure readmissions, especially since last Oct. 1 when the Centers for Medicare and Medicaid Services began penalizing hospitals that accumulate high heart failure readmission numbers.
One leap was that the patients in the 1990s enrolled in the Digitalis Investigation Group (DIG) trial all had chronic, stable heart failure, without recent hospitalization. Although the post hoc analysis that Dr. Ahmed presented showed that the half of the DIG patients who were aged 65 or older had their heart failure hospitalization rate cut by a third while on digoxin, compared with patients on placebo, a statistically significant difference for the analysis’ primary endpoint, Dr. Ahmed admitted in his talk that the relevance of his findings to the new Medicare penalties was doubly limited. First, because the DIG population comprised ambulatory patients rather than ones just out of the hospital, and second because the endpoint examined in DIG was index hospital admission rather than readmission. Two pretty important differences.
On top of that, many heart failure experts who heard the results were quick to question the meaning in 2013 of data collected from heart failure patients back in the mid-1990s whose background regimens completely lacked beta-blockers, aldosterone receptor antagonists (spironolactone and eplerenone), and implanted cardiac devices, treatments that have since become cornerstones of heart failure management.
Digoxin "is not a therapy we should embrace wholeheartedly until there is a new trial with contemporary management," commented Dr. Mariell L. Jessup, a heart failure specialist at the University of Pennsylvania, Philadelphia, who cochaired the late-breaker session in which Dr. Ahmed spoke.
But if it was so questionable to use 16-year old, clearly outdated data to address in a post hoc way an issue – 30-day hospital readmissions for heart failure – with at best tangential relevance to what was examined in the DIG trial, what else might be behind this curious report from a large group of prominent heart-failure specialists? (You can see all their names in the article published online simultaneous to Dr. Ahmed’s ACC report [Am. J. Med. 2013;126 (doi:10.1016/j.amjmed.2013.02.001)]).
The answer seems to be their desire to promote digoxin, keep it current in cardiology chatter, and build pressure for a new, prospective study that reexamines the incremental benefit of digoxin on top everything else that heart failure patients receive today. They see current heart failure management, especially efforts to cut hospitalizations for acute decompensation and also cut the rate at which decompensated patients wind up back in the hospital a second time, as woefully inadequate and stand discouraged after many new agents have failed to make a dent in this problem.
"Dismissing digoxin, which was approved by the FDA only 10 years ago and has been used for 2,000 years, in the face of a high event rate [among heart failure patients] when we cannot find any new drugs, is not a wise clinical decision," said Dr. Mihai Gheorghiade, a cardiologist with Northwestern University, Evanston, Ill., who coauthored the new analysis and is a leader of the movement to resurrect digoxin. Using digoxin "isn’t controversial if you see benefit from it and if we are desperate to find something for these patients," he said during a press conference at the meeting.
Efforts to rehabilitate and reevaluate digoxin in heart failure have been going on since the mid-2000s. Dr. Ahmed, Dr. Gheorghiade, and their associates published their first reanalysis of the DIG data in 2005 (Eur. Heart J. 2006;27:178-86), which was recognized by an editorialist at the time as a call to "rehabilitate" digoxin (Eur. Heart J. 2006;27:127-9). In 2006, Dr. Gheorghiade lamented digoxin’s neglect and fall from standard heart failure management, having been muscled out by treatments with big-pocket backers – beta-blockers, ACE inhibitors, and cardiac resynchronization devices; concerns over digoxin’s safety (which he says is obviated by using low dosages), and most of all the absence of any company with enough of a financial interest in digoxin to promote it and fund more studies (Circulation 2006;113:2556-64).
Houston heart failure expert Dr. Biykem Bozkurt saw the new DIG analysis as part of this decade-long rehabilitation effort. The new analysis "is a call for the reexamination of digoxin in acute heart failure," she said as an ACC panelist who discussed the study.
Digoxin’s proponents seem to recognize their big challenge: A large, new study of dioxin on top of today’s standard treatments is the key to convincing skeptical colleagues, but who will pay for it? "The problem with digoxin is that no company sponsors it," Dr. Gheorghiade said.
Twitter @mitchelzoler
One of the late-breaker reports at the American College of Cardiology’s annual meeting in March had results from a post hoc analysis of 16-year-old data from the DIG trial, by far the largest study to ever assess digoxin for heart failure, a treatment that precipitously dropped out of favor during the decade following the initial DIG report in 1997. Not your typical back story for a late breaker.
The researchers who ran the new analysis of the old DIG data also took what seem like two sizable leaps by framing their new look as a way to get a sense whether digoxin treatment could cut the large number of Medicare patients with heart failure who need rehospitalization within a month after a hospital discharge.
Dr. Ali Ahmed, a cardiologist from the University of Alabama, Birmingham, who presented this ACC late breaker, noted how clinicians and hospital officials are eager to find safe and effective treatments for cutting heart failure readmissions, especially since last Oct. 1 when the Centers for Medicare and Medicaid Services began penalizing hospitals that accumulate high heart failure readmission numbers.
One leap was that the patients in the 1990s enrolled in the Digitalis Investigation Group (DIG) trial all had chronic, stable heart failure, without recent hospitalization. Although the post hoc analysis that Dr. Ahmed presented showed that the half of the DIG patients who were aged 65 or older had their heart failure hospitalization rate cut by a third while on digoxin, compared with patients on placebo, a statistically significant difference for the analysis’ primary endpoint, Dr. Ahmed admitted in his talk that the relevance of his findings to the new Medicare penalties was doubly limited. First, because the DIG population comprised ambulatory patients rather than ones just out of the hospital, and second because the endpoint examined in DIG was index hospital admission rather than readmission. Two pretty important differences.
On top of that, many heart failure experts who heard the results were quick to question the meaning in 2013 of data collected from heart failure patients back in the mid-1990s whose background regimens completely lacked beta-blockers, aldosterone receptor antagonists (spironolactone and eplerenone), and implanted cardiac devices, treatments that have since become cornerstones of heart failure management.
Digoxin "is not a therapy we should embrace wholeheartedly until there is a new trial with contemporary management," commented Dr. Mariell L. Jessup, a heart failure specialist at the University of Pennsylvania, Philadelphia, who cochaired the late-breaker session in which Dr. Ahmed spoke.
But if it was so questionable to use 16-year old, clearly outdated data to address in a post hoc way an issue – 30-day hospital readmissions for heart failure – with at best tangential relevance to what was examined in the DIG trial, what else might be behind this curious report from a large group of prominent heart-failure specialists? (You can see all their names in the article published online simultaneous to Dr. Ahmed’s ACC report [Am. J. Med. 2013;126 (doi:10.1016/j.amjmed.2013.02.001)]).
The answer seems to be their desire to promote digoxin, keep it current in cardiology chatter, and build pressure for a new, prospective study that reexamines the incremental benefit of digoxin on top everything else that heart failure patients receive today. They see current heart failure management, especially efforts to cut hospitalizations for acute decompensation and also cut the rate at which decompensated patients wind up back in the hospital a second time, as woefully inadequate and stand discouraged after many new agents have failed to make a dent in this problem.
"Dismissing digoxin, which was approved by the FDA only 10 years ago and has been used for 2,000 years, in the face of a high event rate [among heart failure patients] when we cannot find any new drugs, is not a wise clinical decision," said Dr. Mihai Gheorghiade, a cardiologist with Northwestern University, Evanston, Ill., who coauthored the new analysis and is a leader of the movement to resurrect digoxin. Using digoxin "isn’t controversial if you see benefit from it and if we are desperate to find something for these patients," he said during a press conference at the meeting.
Efforts to rehabilitate and reevaluate digoxin in heart failure have been going on since the mid-2000s. Dr. Ahmed, Dr. Gheorghiade, and their associates published their first reanalysis of the DIG data in 2005 (Eur. Heart J. 2006;27:178-86), which was recognized by an editorialist at the time as a call to "rehabilitate" digoxin (Eur. Heart J. 2006;27:127-9). In 2006, Dr. Gheorghiade lamented digoxin’s neglect and fall from standard heart failure management, having been muscled out by treatments with big-pocket backers – beta-blockers, ACE inhibitors, and cardiac resynchronization devices; concerns over digoxin’s safety (which he says is obviated by using low dosages), and most of all the absence of any company with enough of a financial interest in digoxin to promote it and fund more studies (Circulation 2006;113:2556-64).
Houston heart failure expert Dr. Biykem Bozkurt saw the new DIG analysis as part of this decade-long rehabilitation effort. The new analysis "is a call for the reexamination of digoxin in acute heart failure," she said as an ACC panelist who discussed the study.
Digoxin’s proponents seem to recognize their big challenge: A large, new study of dioxin on top of today’s standard treatments is the key to convincing skeptical colleagues, but who will pay for it? "The problem with digoxin is that no company sponsors it," Dr. Gheorghiade said.
Twitter @mitchelzoler
One of the late-breaker reports at the American College of Cardiology’s annual meeting in March had results from a post hoc analysis of 16-year-old data from the DIG trial, by far the largest study to ever assess digoxin for heart failure, a treatment that precipitously dropped out of favor during the decade following the initial DIG report in 1997. Not your typical back story for a late breaker.
The researchers who ran the new analysis of the old DIG data also took what seem like two sizable leaps by framing their new look as a way to get a sense whether digoxin treatment could cut the large number of Medicare patients with heart failure who need rehospitalization within a month after a hospital discharge.
Dr. Ali Ahmed, a cardiologist from the University of Alabama, Birmingham, who presented this ACC late breaker, noted how clinicians and hospital officials are eager to find safe and effective treatments for cutting heart failure readmissions, especially since last Oct. 1 when the Centers for Medicare and Medicaid Services began penalizing hospitals that accumulate high heart failure readmission numbers.
One leap was that the patients in the 1990s enrolled in the Digitalis Investigation Group (DIG) trial all had chronic, stable heart failure, without recent hospitalization. Although the post hoc analysis that Dr. Ahmed presented showed that the half of the DIG patients who were aged 65 or older had their heart failure hospitalization rate cut by a third while on digoxin, compared with patients on placebo, a statistically significant difference for the analysis’ primary endpoint, Dr. Ahmed admitted in his talk that the relevance of his findings to the new Medicare penalties was doubly limited. First, because the DIG population comprised ambulatory patients rather than ones just out of the hospital, and second because the endpoint examined in DIG was index hospital admission rather than readmission. Two pretty important differences.
On top of that, many heart failure experts who heard the results were quick to question the meaning in 2013 of data collected from heart failure patients back in the mid-1990s whose background regimens completely lacked beta-blockers, aldosterone receptor antagonists (spironolactone and eplerenone), and implanted cardiac devices, treatments that have since become cornerstones of heart failure management.
Digoxin "is not a therapy we should embrace wholeheartedly until there is a new trial with contemporary management," commented Dr. Mariell L. Jessup, a heart failure specialist at the University of Pennsylvania, Philadelphia, who cochaired the late-breaker session in which Dr. Ahmed spoke.
But if it was so questionable to use 16-year old, clearly outdated data to address in a post hoc way an issue – 30-day hospital readmissions for heart failure – with at best tangential relevance to what was examined in the DIG trial, what else might be behind this curious report from a large group of prominent heart-failure specialists? (You can see all their names in the article published online simultaneous to Dr. Ahmed’s ACC report [Am. J. Med. 2013;126 (doi:10.1016/j.amjmed.2013.02.001)]).
The answer seems to be their desire to promote digoxin, keep it current in cardiology chatter, and build pressure for a new, prospective study that reexamines the incremental benefit of digoxin on top everything else that heart failure patients receive today. They see current heart failure management, especially efforts to cut hospitalizations for acute decompensation and also cut the rate at which decompensated patients wind up back in the hospital a second time, as woefully inadequate and stand discouraged after many new agents have failed to make a dent in this problem.
"Dismissing digoxin, which was approved by the FDA only 10 years ago and has been used for 2,000 years, in the face of a high event rate [among heart failure patients] when we cannot find any new drugs, is not a wise clinical decision," said Dr. Mihai Gheorghiade, a cardiologist with Northwestern University, Evanston, Ill., who coauthored the new analysis and is a leader of the movement to resurrect digoxin. Using digoxin "isn’t controversial if you see benefit from it and if we are desperate to find something for these patients," he said during a press conference at the meeting.
Efforts to rehabilitate and reevaluate digoxin in heart failure have been going on since the mid-2000s. Dr. Ahmed, Dr. Gheorghiade, and their associates published their first reanalysis of the DIG data in 2005 (Eur. Heart J. 2006;27:178-86), which was recognized by an editorialist at the time as a call to "rehabilitate" digoxin (Eur. Heart J. 2006;27:127-9). In 2006, Dr. Gheorghiade lamented digoxin’s neglect and fall from standard heart failure management, having been muscled out by treatments with big-pocket backers – beta-blockers, ACE inhibitors, and cardiac resynchronization devices; concerns over digoxin’s safety (which he says is obviated by using low dosages), and most of all the absence of any company with enough of a financial interest in digoxin to promote it and fund more studies (Circulation 2006;113:2556-64).
Houston heart failure expert Dr. Biykem Bozkurt saw the new DIG analysis as part of this decade-long rehabilitation effort. The new analysis "is a call for the reexamination of digoxin in acute heart failure," she said as an ACC panelist who discussed the study.
Digoxin’s proponents seem to recognize their big challenge: A large, new study of dioxin on top of today’s standard treatments is the key to convincing skeptical colleagues, but who will pay for it? "The problem with digoxin is that no company sponsors it," Dr. Gheorghiade said.
Twitter @mitchelzoler
Skin capillary density drop reliably predicts preeclampsia
SAN FRANCISCO – A reduction in skin capillary density during pregnancy constitutes a novel independent and reliable noninvasive predictor of preeclampsia, according to Dr. Tarek Antonios of the University of London.
"Capillary density rarefaction is the most sensitive and specific predictor of preeclampsia to date. Combining capillary density rarefaction and the uterine artery Doppler pulsatility index increases the sensitivity of prediction to 86% and the specificity to 80%, figures that are by far more significant than any other published evidence about the clinical prediction of preeclampsia," he declared at the annual meeting of the American College of Cardiology.
Measurement of skin capillary density changes in pregnancy is inexpensive once the essential equipment – an intravital video microscope suitable for capillaroscopy – has been acquired, he added.
Cardiovascular risk factors known to predispose to preeclampsia include essential hypertension, diabetes, and obesity. Dr. Antonios and coworkers have surmised that the mechanism by which these disorders boost the risk of preeclampsia involves microcirculatory abnormalities and impaired tissue perfusion.
The investigators have developed a reproducible method of measuring skin capillary density on the dorsum of the hand. Further, they have demonstrated that reduced capillary density – which they term "structural capillary rarefaction" – beginning at about 20 weeks of gestation is a harbinger of subsequent onset of preeclampsia.
Dr. Antonios reported on 322 consecutive white women with singleton pregnancies, of whom 13 had a history of preeclampsia, 11 had a history of untreated stage 1 essential hypertension, and the rest were normotensive. They underwent five structured capillaroscopy assessments at 11-16 weeks’ of gestation, 20-24 weeks, 27-32 weeks, 34-38 weeks, and finally at 5-15 weeks post partum. The capillary density measurements were done in a temperature-controlled laboratory with a standardized technique.
Among the 305 women who completed the study, 16 (5%) developed preeclampsia. Four of the 16 (25%) had a history of preeclampsia, compared with just 3% of the 289 (1%) subjects with a normal pregnancy.
The women who became preeclamptic were also set apart by their mean 6.1 capillary/mm2 reduction in density between the weeks 20-24 measurement and the weeks 11-16 baseline. In contrast, the women with normal pregnancies averaged a 1.0 capillary/mm2 decrease during that time frame. Capillary rarefaction further increased over time in women who later developed preeclampsia: their mean reduction in density at the weeks 27-32 measurement was 11.4/mm2, compared with the weeks 11-16 baseline, while the controls averaged a 2.1 capillary/mm2 decrease.
In a multivariate regression analysis, the single strongest predictor of preeclampsia was a history of previous preeclampsia or essential hypertension, which was associated with a 35-fold increase in risk. Each 1 capillary/mm2 reduction in density at 20-24 weeks was associated with a 3% increase in risk, while at 27-32 weeks every 1 capillary/mm2 reduction in density conferred a 26% increase in the risk of preeclampsia.
Significant structural capillary rarefaction at weeks 27-32 had a 77% sensitivity and 77% specificity for subsequent preeclampsia. Combining an increased uterine artery Doppler pulsatility index with a finding of significant capillary density reduction at weeks 27-32 boosted the sensitivity to 86% and the specificity to 80%.
Given that only 16 participants in this study developed preeclampsia, the next step in this research is to conduct a large clinical trial to validate capillaroscopy as a clinical risk prediction tool with an eye toward its eventual integration into routine clinical practice, according to Dr. Antonios.
This study was funded by the British Heart Foundation. Dr. Antonios reported having no financial conflicts.
SAN FRANCISCO – A reduction in skin capillary density during pregnancy constitutes a novel independent and reliable noninvasive predictor of preeclampsia, according to Dr. Tarek Antonios of the University of London.
"Capillary density rarefaction is the most sensitive and specific predictor of preeclampsia to date. Combining capillary density rarefaction and the uterine artery Doppler pulsatility index increases the sensitivity of prediction to 86% and the specificity to 80%, figures that are by far more significant than any other published evidence about the clinical prediction of preeclampsia," he declared at the annual meeting of the American College of Cardiology.
Measurement of skin capillary density changes in pregnancy is inexpensive once the essential equipment – an intravital video microscope suitable for capillaroscopy – has been acquired, he added.
Cardiovascular risk factors known to predispose to preeclampsia include essential hypertension, diabetes, and obesity. Dr. Antonios and coworkers have surmised that the mechanism by which these disorders boost the risk of preeclampsia involves microcirculatory abnormalities and impaired tissue perfusion.
The investigators have developed a reproducible method of measuring skin capillary density on the dorsum of the hand. Further, they have demonstrated that reduced capillary density – which they term "structural capillary rarefaction" – beginning at about 20 weeks of gestation is a harbinger of subsequent onset of preeclampsia.
Dr. Antonios reported on 322 consecutive white women with singleton pregnancies, of whom 13 had a history of preeclampsia, 11 had a history of untreated stage 1 essential hypertension, and the rest were normotensive. They underwent five structured capillaroscopy assessments at 11-16 weeks’ of gestation, 20-24 weeks, 27-32 weeks, 34-38 weeks, and finally at 5-15 weeks post partum. The capillary density measurements were done in a temperature-controlled laboratory with a standardized technique.
Among the 305 women who completed the study, 16 (5%) developed preeclampsia. Four of the 16 (25%) had a history of preeclampsia, compared with just 3% of the 289 (1%) subjects with a normal pregnancy.
The women who became preeclamptic were also set apart by their mean 6.1 capillary/mm2 reduction in density between the weeks 20-24 measurement and the weeks 11-16 baseline. In contrast, the women with normal pregnancies averaged a 1.0 capillary/mm2 decrease during that time frame. Capillary rarefaction further increased over time in women who later developed preeclampsia: their mean reduction in density at the weeks 27-32 measurement was 11.4/mm2, compared with the weeks 11-16 baseline, while the controls averaged a 2.1 capillary/mm2 decrease.
In a multivariate regression analysis, the single strongest predictor of preeclampsia was a history of previous preeclampsia or essential hypertension, which was associated with a 35-fold increase in risk. Each 1 capillary/mm2 reduction in density at 20-24 weeks was associated with a 3% increase in risk, while at 27-32 weeks every 1 capillary/mm2 reduction in density conferred a 26% increase in the risk of preeclampsia.
Significant structural capillary rarefaction at weeks 27-32 had a 77% sensitivity and 77% specificity for subsequent preeclampsia. Combining an increased uterine artery Doppler pulsatility index with a finding of significant capillary density reduction at weeks 27-32 boosted the sensitivity to 86% and the specificity to 80%.
Given that only 16 participants in this study developed preeclampsia, the next step in this research is to conduct a large clinical trial to validate capillaroscopy as a clinical risk prediction tool with an eye toward its eventual integration into routine clinical practice, according to Dr. Antonios.
This study was funded by the British Heart Foundation. Dr. Antonios reported having no financial conflicts.
SAN FRANCISCO – A reduction in skin capillary density during pregnancy constitutes a novel independent and reliable noninvasive predictor of preeclampsia, according to Dr. Tarek Antonios of the University of London.
"Capillary density rarefaction is the most sensitive and specific predictor of preeclampsia to date. Combining capillary density rarefaction and the uterine artery Doppler pulsatility index increases the sensitivity of prediction to 86% and the specificity to 80%, figures that are by far more significant than any other published evidence about the clinical prediction of preeclampsia," he declared at the annual meeting of the American College of Cardiology.
Measurement of skin capillary density changes in pregnancy is inexpensive once the essential equipment – an intravital video microscope suitable for capillaroscopy – has been acquired, he added.
Cardiovascular risk factors known to predispose to preeclampsia include essential hypertension, diabetes, and obesity. Dr. Antonios and coworkers have surmised that the mechanism by which these disorders boost the risk of preeclampsia involves microcirculatory abnormalities and impaired tissue perfusion.
The investigators have developed a reproducible method of measuring skin capillary density on the dorsum of the hand. Further, they have demonstrated that reduced capillary density – which they term "structural capillary rarefaction" – beginning at about 20 weeks of gestation is a harbinger of subsequent onset of preeclampsia.
Dr. Antonios reported on 322 consecutive white women with singleton pregnancies, of whom 13 had a history of preeclampsia, 11 had a history of untreated stage 1 essential hypertension, and the rest were normotensive. They underwent five structured capillaroscopy assessments at 11-16 weeks’ of gestation, 20-24 weeks, 27-32 weeks, 34-38 weeks, and finally at 5-15 weeks post partum. The capillary density measurements were done in a temperature-controlled laboratory with a standardized technique.
Among the 305 women who completed the study, 16 (5%) developed preeclampsia. Four of the 16 (25%) had a history of preeclampsia, compared with just 3% of the 289 (1%) subjects with a normal pregnancy.
The women who became preeclamptic were also set apart by their mean 6.1 capillary/mm2 reduction in density between the weeks 20-24 measurement and the weeks 11-16 baseline. In contrast, the women with normal pregnancies averaged a 1.0 capillary/mm2 decrease during that time frame. Capillary rarefaction further increased over time in women who later developed preeclampsia: their mean reduction in density at the weeks 27-32 measurement was 11.4/mm2, compared with the weeks 11-16 baseline, while the controls averaged a 2.1 capillary/mm2 decrease.
In a multivariate regression analysis, the single strongest predictor of preeclampsia was a history of previous preeclampsia or essential hypertension, which was associated with a 35-fold increase in risk. Each 1 capillary/mm2 reduction in density at 20-24 weeks was associated with a 3% increase in risk, while at 27-32 weeks every 1 capillary/mm2 reduction in density conferred a 26% increase in the risk of preeclampsia.
Significant structural capillary rarefaction at weeks 27-32 had a 77% sensitivity and 77% specificity for subsequent preeclampsia. Combining an increased uterine artery Doppler pulsatility index with a finding of significant capillary density reduction at weeks 27-32 boosted the sensitivity to 86% and the specificity to 80%.
Given that only 16 participants in this study developed preeclampsia, the next step in this research is to conduct a large clinical trial to validate capillaroscopy as a clinical risk prediction tool with an eye toward its eventual integration into routine clinical practice, according to Dr. Antonios.
This study was funded by the British Heart Foundation. Dr. Antonios reported having no financial conflicts.
AT ACC 13
Major finding: A marked reduction in capillary density in the skin on the dorsum of the hand between gestational weeks 11-16 and 27-32 was associated with 77% sensitivity and 77% specificity for subsequent preeclampsia.
Data source: This was a prospective study involving 322 consecutive white women with singleton pregnancies who underwent structured measurement of skin capillary density on four designated occasions during pregnancy and once post partum.
Disclosures: The study was funded by the British Heart Foundation. Dr. Antonios reported having no financial conflicts.
CORE320: CT angiography bests SPECT for CAD diagnosis
SAN FRANCISCO – Coronary CT angiography outperformed myocardial perfusion single-photon emission CT for the diagnosis of obstructive coronary artery disease in a prospective multicenter head-to-head comparative study.
The CORE320 (Coronary Artery Evaluation Using 320-Row Multidetector Computed Tomography Angiography and Myocardial Perfusion) study included 381 patients with suspected or known coronary artery disease (CAD) who were scheduled for invasive quantitative coronary angiography. But first they all underwent coronary CT angiography (CTA) and single-photon emission CT (SPECT), with images analyzed in blinded independent core laboratories. The time interval between the two imaging studies was a mean of 9.4 days. Invasive coronary angiography served as the diagnostic reference standard in the 16-center, 8-country study, Dr. Marcelo F. Di Carli explained at the annual meeting of the American College of Cardiology.
The primary study endpoint was test accuracy as defined by the area under the receiver operating characteristic curve for identifying the 59% of subjects with at least a 50% stenosis by invasive coronary angiography. The rate was significantly better for CTA than SPECT: 89% vs. 69%.
CTA’s superior performance was driven by its greater sensitivity in detecting stenoses of 50% or more: 91% vs. 62% for SPECT. The two imaging modalities displayed similar specificity: 74% for CTA and 67% for SPECT.
CTA had a positive predictive value of 83% and a negative predictive value of 85%, compared with 73% and 55%, respectively, for SPECT, according to Dr. Di Carli of Brigham and Women’s Hospital, Boston.
The same pattern of results was seen with regard to diagnostic accuracy in detecting patients with at least a 70% stenosis, a prespecified secondary endpoint. CTA had 94% sensitivity, 60% specificity, a positive predictive value of 66%, and a negative predictive value of 92%. SPECT showed 72% sensitivity, 67% specificity, a 64% positive predictive value, and a 73% negative predictive value.
The average radiation dose was markedly lower with CTA: 3.54 mSv compared with 10.48 mSv for SPECT.
The study was funded by Toshiba. Dr. Di Carli reported having no relevant financial conflicts.
SAN FRANCISCO – Coronary CT angiography outperformed myocardial perfusion single-photon emission CT for the diagnosis of obstructive coronary artery disease in a prospective multicenter head-to-head comparative study.
The CORE320 (Coronary Artery Evaluation Using 320-Row Multidetector Computed Tomography Angiography and Myocardial Perfusion) study included 381 patients with suspected or known coronary artery disease (CAD) who were scheduled for invasive quantitative coronary angiography. But first they all underwent coronary CT angiography (CTA) and single-photon emission CT (SPECT), with images analyzed in blinded independent core laboratories. The time interval between the two imaging studies was a mean of 9.4 days. Invasive coronary angiography served as the diagnostic reference standard in the 16-center, 8-country study, Dr. Marcelo F. Di Carli explained at the annual meeting of the American College of Cardiology.
The primary study endpoint was test accuracy as defined by the area under the receiver operating characteristic curve for identifying the 59% of subjects with at least a 50% stenosis by invasive coronary angiography. The rate was significantly better for CTA than SPECT: 89% vs. 69%.
CTA’s superior performance was driven by its greater sensitivity in detecting stenoses of 50% or more: 91% vs. 62% for SPECT. The two imaging modalities displayed similar specificity: 74% for CTA and 67% for SPECT.
CTA had a positive predictive value of 83% and a negative predictive value of 85%, compared with 73% and 55%, respectively, for SPECT, according to Dr. Di Carli of Brigham and Women’s Hospital, Boston.
The same pattern of results was seen with regard to diagnostic accuracy in detecting patients with at least a 70% stenosis, a prespecified secondary endpoint. CTA had 94% sensitivity, 60% specificity, a positive predictive value of 66%, and a negative predictive value of 92%. SPECT showed 72% sensitivity, 67% specificity, a 64% positive predictive value, and a 73% negative predictive value.
The average radiation dose was markedly lower with CTA: 3.54 mSv compared with 10.48 mSv for SPECT.
The study was funded by Toshiba. Dr. Di Carli reported having no relevant financial conflicts.
SAN FRANCISCO – Coronary CT angiography outperformed myocardial perfusion single-photon emission CT for the diagnosis of obstructive coronary artery disease in a prospective multicenter head-to-head comparative study.
The CORE320 (Coronary Artery Evaluation Using 320-Row Multidetector Computed Tomography Angiography and Myocardial Perfusion) study included 381 patients with suspected or known coronary artery disease (CAD) who were scheduled for invasive quantitative coronary angiography. But first they all underwent coronary CT angiography (CTA) and single-photon emission CT (SPECT), with images analyzed in blinded independent core laboratories. The time interval between the two imaging studies was a mean of 9.4 days. Invasive coronary angiography served as the diagnostic reference standard in the 16-center, 8-country study, Dr. Marcelo F. Di Carli explained at the annual meeting of the American College of Cardiology.
The primary study endpoint was test accuracy as defined by the area under the receiver operating characteristic curve for identifying the 59% of subjects with at least a 50% stenosis by invasive coronary angiography. The rate was significantly better for CTA than SPECT: 89% vs. 69%.
CTA’s superior performance was driven by its greater sensitivity in detecting stenoses of 50% or more: 91% vs. 62% for SPECT. The two imaging modalities displayed similar specificity: 74% for CTA and 67% for SPECT.
CTA had a positive predictive value of 83% and a negative predictive value of 85%, compared with 73% and 55%, respectively, for SPECT, according to Dr. Di Carli of Brigham and Women’s Hospital, Boston.
The same pattern of results was seen with regard to diagnostic accuracy in detecting patients with at least a 70% stenosis, a prespecified secondary endpoint. CTA had 94% sensitivity, 60% specificity, a positive predictive value of 66%, and a negative predictive value of 92%. SPECT showed 72% sensitivity, 67% specificity, a 64% positive predictive value, and a 73% negative predictive value.
The average radiation dose was markedly lower with CTA: 3.54 mSv compared with 10.48 mSv for SPECT.
The study was funded by Toshiba. Dr. Di Carli reported having no relevant financial conflicts.
AT ACC 13
Major Finding: Coronary CT angiography had a 91% sensitivity and a 74% specificity for the detection of at least 50% stenosis in 381 patients with known or suspected CAD, superior to the 62% sensitivity and 67% specificity for myocardial perfusion single-photon emission CT in the same patients.
Data Source: CORE320, an ongoing prospective 16-center study comparing the diagnostic accuracy of two widely utilized noninvasive imaging methods in detecting obstructive CAD, with invasive quantitative coronary angiography serving as the reference standard.
Disclosures: The study is funded by Toshiba. The presenter reported having no relevant financial conflicts.
U.S. post-PCI cardiac rehabilitation referrals lag
SAN FRANCISCO – U.S. patients are not getting referred to cardiac rehabilitation programs following percutaneous coronary interventions, despite clear guidelines calling for it.
A review of more than 1.4 million Americans who underwent percutaneous coronary intervention at more than 1,300 U.S. hospitals during 2009-2011 showed that 59% received cardiac rehabilitation referral, a rate that lagged far behind several other post-PCI interventions, Dr. Krishna G. Aragam and his associates reported in a poster at the annual meeting of the American College of Cardiology.
"Rates of cardiac rehabilitation referral are well below those of other acute myocardial infarction quality-of-care measures with little change over the past 3 years," said Dr. Aragam, a cardiologist at the University of Pennsylvania, Philadelphia, and his associates.
Analysis of data collected in the CathPCI Registry of the National Cardiovascular Data Registry of the ACC also showed "considerable" interhospital variation in the rates of rehabilitation referral, with a majority of hospitals having rates that either ran greater than 80% or less than 20%.
A relatively low rate of rehabilitation referral reflects inferior patient care based on the endorsements that rehabilitation programs have received for post-PCI patients. The most recent PCI guidelines of the ACC and other professional societies rate cardiac rehabilitation following PCI a class 1A recommendation, saying that cardiac rehabilitation "should be recommended to patients after PCI." (Circulation 2011:124:2574-609). And last year the Centers for Medicare and Medicaid Services announced that starting in 2014 it would make referral to cardiac rehabilitation for patients following PCI or a myocardial infarction a hospital-performance measure.
If the numbers collected following PCIs as recently as 2011 are a guide, many hospitals will need to act quickly to make rehabilitation referral routine.
Data from 1,432,399 PCIs done at 1,310 U.S. hospitals during the 3 years starting in 2009 showed that discharge referrals to a cardiac rehabilitation program occurred for about 57% of PCI patients in 2009, which upticked to 61% in 2011. The analysis excluded patients who died while hospitalized, and those discharged to a nursing home, acute-care hospital, or hospice.
In contrast, data reported by Dr. Aragam and his associates showed that the next-lowest level of compliance with post-PCI recommendations was discharge prescription of an ACE inhibitor or angiotensin-receptor blocker in patients with a left-ventricular ejection fraction of less than 40%, which happened for about 80% of patients. At discharge, 95% of patients received an aspirin prescription, 90% received a statin prescription, and 85% were prescribed a beta-blocker.
The analysis also identified several factors that significantly linked with either an increased or decreased likelihood of referral to cardiac rehabilitation. Factors linked with rehab being less likely included older age, diabetes, peripheral artery disease, or prior revascularization. Factors that boosted the likelihood that patients received a rehabilitation referral included having an ST elevation MI, which boosted the referral rate by 66% compared with other PCI patients, and having a non-ST elevation MI, which raised the referral rate by 38%.
Dr. Aragam said that he had no disclosures.
SAN FRANCISCO – U.S. patients are not getting referred to cardiac rehabilitation programs following percutaneous coronary interventions, despite clear guidelines calling for it.
A review of more than 1.4 million Americans who underwent percutaneous coronary intervention at more than 1,300 U.S. hospitals during 2009-2011 showed that 59% received cardiac rehabilitation referral, a rate that lagged far behind several other post-PCI interventions, Dr. Krishna G. Aragam and his associates reported in a poster at the annual meeting of the American College of Cardiology.
"Rates of cardiac rehabilitation referral are well below those of other acute myocardial infarction quality-of-care measures with little change over the past 3 years," said Dr. Aragam, a cardiologist at the University of Pennsylvania, Philadelphia, and his associates.
Analysis of data collected in the CathPCI Registry of the National Cardiovascular Data Registry of the ACC also showed "considerable" interhospital variation in the rates of rehabilitation referral, with a majority of hospitals having rates that either ran greater than 80% or less than 20%.
A relatively low rate of rehabilitation referral reflects inferior patient care based on the endorsements that rehabilitation programs have received for post-PCI patients. The most recent PCI guidelines of the ACC and other professional societies rate cardiac rehabilitation following PCI a class 1A recommendation, saying that cardiac rehabilitation "should be recommended to patients after PCI." (Circulation 2011:124:2574-609). And last year the Centers for Medicare and Medicaid Services announced that starting in 2014 it would make referral to cardiac rehabilitation for patients following PCI or a myocardial infarction a hospital-performance measure.
If the numbers collected following PCIs as recently as 2011 are a guide, many hospitals will need to act quickly to make rehabilitation referral routine.
Data from 1,432,399 PCIs done at 1,310 U.S. hospitals during the 3 years starting in 2009 showed that discharge referrals to a cardiac rehabilitation program occurred for about 57% of PCI patients in 2009, which upticked to 61% in 2011. The analysis excluded patients who died while hospitalized, and those discharged to a nursing home, acute-care hospital, or hospice.
In contrast, data reported by Dr. Aragam and his associates showed that the next-lowest level of compliance with post-PCI recommendations was discharge prescription of an ACE inhibitor or angiotensin-receptor blocker in patients with a left-ventricular ejection fraction of less than 40%, which happened for about 80% of patients. At discharge, 95% of patients received an aspirin prescription, 90% received a statin prescription, and 85% were prescribed a beta-blocker.
The analysis also identified several factors that significantly linked with either an increased or decreased likelihood of referral to cardiac rehabilitation. Factors linked with rehab being less likely included older age, diabetes, peripheral artery disease, or prior revascularization. Factors that boosted the likelihood that patients received a rehabilitation referral included having an ST elevation MI, which boosted the referral rate by 66% compared with other PCI patients, and having a non-ST elevation MI, which raised the referral rate by 38%.
Dr. Aragam said that he had no disclosures.
SAN FRANCISCO – U.S. patients are not getting referred to cardiac rehabilitation programs following percutaneous coronary interventions, despite clear guidelines calling for it.
A review of more than 1.4 million Americans who underwent percutaneous coronary intervention at more than 1,300 U.S. hospitals during 2009-2011 showed that 59% received cardiac rehabilitation referral, a rate that lagged far behind several other post-PCI interventions, Dr. Krishna G. Aragam and his associates reported in a poster at the annual meeting of the American College of Cardiology.
"Rates of cardiac rehabilitation referral are well below those of other acute myocardial infarction quality-of-care measures with little change over the past 3 years," said Dr. Aragam, a cardiologist at the University of Pennsylvania, Philadelphia, and his associates.
Analysis of data collected in the CathPCI Registry of the National Cardiovascular Data Registry of the ACC also showed "considerable" interhospital variation in the rates of rehabilitation referral, with a majority of hospitals having rates that either ran greater than 80% or less than 20%.
A relatively low rate of rehabilitation referral reflects inferior patient care based on the endorsements that rehabilitation programs have received for post-PCI patients. The most recent PCI guidelines of the ACC and other professional societies rate cardiac rehabilitation following PCI a class 1A recommendation, saying that cardiac rehabilitation "should be recommended to patients after PCI." (Circulation 2011:124:2574-609). And last year the Centers for Medicare and Medicaid Services announced that starting in 2014 it would make referral to cardiac rehabilitation for patients following PCI or a myocardial infarction a hospital-performance measure.
If the numbers collected following PCIs as recently as 2011 are a guide, many hospitals will need to act quickly to make rehabilitation referral routine.
Data from 1,432,399 PCIs done at 1,310 U.S. hospitals during the 3 years starting in 2009 showed that discharge referrals to a cardiac rehabilitation program occurred for about 57% of PCI patients in 2009, which upticked to 61% in 2011. The analysis excluded patients who died while hospitalized, and those discharged to a nursing home, acute-care hospital, or hospice.
In contrast, data reported by Dr. Aragam and his associates showed that the next-lowest level of compliance with post-PCI recommendations was discharge prescription of an ACE inhibitor or angiotensin-receptor blocker in patients with a left-ventricular ejection fraction of less than 40%, which happened for about 80% of patients. At discharge, 95% of patients received an aspirin prescription, 90% received a statin prescription, and 85% were prescribed a beta-blocker.
The analysis also identified several factors that significantly linked with either an increased or decreased likelihood of referral to cardiac rehabilitation. Factors linked with rehab being less likely included older age, diabetes, peripheral artery disease, or prior revascularization. Factors that boosted the likelihood that patients received a rehabilitation referral included having an ST elevation MI, which boosted the referral rate by 66% compared with other PCI patients, and having a non-ST elevation MI, which raised the referral rate by 38%.
Dr. Aragam said that he had no disclosures.
AT ACC 13
Major finding: During 2009-2011, 59% of all U.S. PCI patients received a discharge referral to cardiac rehabilitation.
Data source: More than 1.4 million U.S. PCI patients during 2009-2011 enrolled in the CathPCI Registry of the National Cardiovascular data Registry of the American College of Cardiology.
Disclosures: Dr. Aragam said that he had no disclosures.
BNP screening effectively targets heart failure prevention
SAN FRANCISCO – Targeting a comprehensive cardiac-risk reduction program to adults with elevated natriuretic peptide significantly cut the rate of new left ventricular dysfunction, heart failure, and other cardiovascular events in a randomized trial with more than 1,300 patients.
"I think it was the structure of the intervention, the cohesion of care, rather than a specific intervention" that improved clinical outcomes, Dr. Kenneth M. McDonald said at the annual meeting of the American College of Cardiology. "Undoubtedly, a patient’s knowledge [of a high B-type natriuretic peptide level] improved their adherence to therapy." He and his associates ran the study at 39 primary care practices around Dublin that worked in collaboration with the cardiology department at St. Vincent’s University Hospital in Dublin.
The primary care physicians looked for patients at least 40 years old with at least one identified cardiovascular risk factor whose B-type natriuretic peptide (BNP) level rose above 50 pg/mL on an annual screening test. They referred these patients to St. Vincent’s for an intensified testing and management program similar to "the disease management structure we’ve used for several years for patients with heart failure," said Dr. McDonald, a professor of cardiology at St. Vincent’s and director of the heart failure unit. The program included a cardiology review and regular follow-up, echocardiography with Doppler and other cardiovascular investigations as needed, and nurse coaching.
"Routine BNP screening is not recommended in current guidelines. Perhaps this finding is the first step to get guidelines committees to address the use of BNP for screening," commented Dr. Sanjay Kaul, director of the vascular physiology and thrombosis research laboratory at the Burns and Allen Research Institute at Cedars Sinai Medical Center in Los Angeles.
Among the 1,374 patients enrolled in the STOP-HF (Screening to Prevent Heart Failure) trial, annual BNP measurement found 498 (36%) with a BNP level that rose above 50 pg/mL in at least one annual test. This included 235 patients randomized to the control arm and 263 randomized to the intervention group. The overall age of patients in the study averaged 65 years, but the age of those with elevated BNP averaged closer to 70 years.
During average follow-up of just over 4 years, patients referred to the cardiology program had 25 cases (10%) of heart failure or asymptomatic left ventricular dysfunction, compared with 44 cases (19%) in the control arm, a 54% odds ratio reduction that was statistically significant for the study’s primary endpoint. For the entire study group of 1,374 randomized patients, participation in the group eligible for referred care cut the primary endpoint by a relative 41%, compared with the controls, a statistically significant difference.
A secondary efficacy analysis that tallied the combined rate of incident heart failure, arrhythmia, myocardial infarction, unstable angina, cerebrovascular events, peripheral thrombosis, or pulmonary embolism found 51 events (7%) in the entire intervention group compared with 71 events (10%) in the control group, a 46% odds rate reduction that was statistically significant.
A study limitation was the large percentage of patients in both arms either lost to follow-up, 10%; or who withdrew their consent to participate, another 16%. "It challenges interpretation of the results," commented Dr. Kaul.
But Dr. McDonald and his associates were convinced by their findings.
"We believe the results are conclusive enough to roll this out as a clinical program," he said in an interview. "We are now extending this to another region of Ireland, and we will try to get this disseminated nationally."
He also foresees additional refinements to the program, possibly identifying other risk markers that can compliment BNP and further focus intervention.
"We have shown benefit, but a question is the cost of getting that benefit. BNP is clearly a step up from where we were, but that doesn’t mean we are as good as we could make it."
Dr. McDonald said that he had no disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – Targeting a comprehensive cardiac-risk reduction program to adults with elevated natriuretic peptide significantly cut the rate of new left ventricular dysfunction, heart failure, and other cardiovascular events in a randomized trial with more than 1,300 patients.
"I think it was the structure of the intervention, the cohesion of care, rather than a specific intervention" that improved clinical outcomes, Dr. Kenneth M. McDonald said at the annual meeting of the American College of Cardiology. "Undoubtedly, a patient’s knowledge [of a high B-type natriuretic peptide level] improved their adherence to therapy." He and his associates ran the study at 39 primary care practices around Dublin that worked in collaboration with the cardiology department at St. Vincent’s University Hospital in Dublin.
The primary care physicians looked for patients at least 40 years old with at least one identified cardiovascular risk factor whose B-type natriuretic peptide (BNP) level rose above 50 pg/mL on an annual screening test. They referred these patients to St. Vincent’s for an intensified testing and management program similar to "the disease management structure we’ve used for several years for patients with heart failure," said Dr. McDonald, a professor of cardiology at St. Vincent’s and director of the heart failure unit. The program included a cardiology review and regular follow-up, echocardiography with Doppler and other cardiovascular investigations as needed, and nurse coaching.
"Routine BNP screening is not recommended in current guidelines. Perhaps this finding is the first step to get guidelines committees to address the use of BNP for screening," commented Dr. Sanjay Kaul, director of the vascular physiology and thrombosis research laboratory at the Burns and Allen Research Institute at Cedars Sinai Medical Center in Los Angeles.
Among the 1,374 patients enrolled in the STOP-HF (Screening to Prevent Heart Failure) trial, annual BNP measurement found 498 (36%) with a BNP level that rose above 50 pg/mL in at least one annual test. This included 235 patients randomized to the control arm and 263 randomized to the intervention group. The overall age of patients in the study averaged 65 years, but the age of those with elevated BNP averaged closer to 70 years.
During average follow-up of just over 4 years, patients referred to the cardiology program had 25 cases (10%) of heart failure or asymptomatic left ventricular dysfunction, compared with 44 cases (19%) in the control arm, a 54% odds ratio reduction that was statistically significant for the study’s primary endpoint. For the entire study group of 1,374 randomized patients, participation in the group eligible for referred care cut the primary endpoint by a relative 41%, compared with the controls, a statistically significant difference.
A secondary efficacy analysis that tallied the combined rate of incident heart failure, arrhythmia, myocardial infarction, unstable angina, cerebrovascular events, peripheral thrombosis, or pulmonary embolism found 51 events (7%) in the entire intervention group compared with 71 events (10%) in the control group, a 46% odds rate reduction that was statistically significant.
A study limitation was the large percentage of patients in both arms either lost to follow-up, 10%; or who withdrew their consent to participate, another 16%. "It challenges interpretation of the results," commented Dr. Kaul.
But Dr. McDonald and his associates were convinced by their findings.
"We believe the results are conclusive enough to roll this out as a clinical program," he said in an interview. "We are now extending this to another region of Ireland, and we will try to get this disseminated nationally."
He also foresees additional refinements to the program, possibly identifying other risk markers that can compliment BNP and further focus intervention.
"We have shown benefit, but a question is the cost of getting that benefit. BNP is clearly a step up from where we were, but that doesn’t mean we are as good as we could make it."
Dr. McDonald said that he had no disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – Targeting a comprehensive cardiac-risk reduction program to adults with elevated natriuretic peptide significantly cut the rate of new left ventricular dysfunction, heart failure, and other cardiovascular events in a randomized trial with more than 1,300 patients.
"I think it was the structure of the intervention, the cohesion of care, rather than a specific intervention" that improved clinical outcomes, Dr. Kenneth M. McDonald said at the annual meeting of the American College of Cardiology. "Undoubtedly, a patient’s knowledge [of a high B-type natriuretic peptide level] improved their adherence to therapy." He and his associates ran the study at 39 primary care practices around Dublin that worked in collaboration with the cardiology department at St. Vincent’s University Hospital in Dublin.
The primary care physicians looked for patients at least 40 years old with at least one identified cardiovascular risk factor whose B-type natriuretic peptide (BNP) level rose above 50 pg/mL on an annual screening test. They referred these patients to St. Vincent’s for an intensified testing and management program similar to "the disease management structure we’ve used for several years for patients with heart failure," said Dr. McDonald, a professor of cardiology at St. Vincent’s and director of the heart failure unit. The program included a cardiology review and regular follow-up, echocardiography with Doppler and other cardiovascular investigations as needed, and nurse coaching.
"Routine BNP screening is not recommended in current guidelines. Perhaps this finding is the first step to get guidelines committees to address the use of BNP for screening," commented Dr. Sanjay Kaul, director of the vascular physiology and thrombosis research laboratory at the Burns and Allen Research Institute at Cedars Sinai Medical Center in Los Angeles.
Among the 1,374 patients enrolled in the STOP-HF (Screening to Prevent Heart Failure) trial, annual BNP measurement found 498 (36%) with a BNP level that rose above 50 pg/mL in at least one annual test. This included 235 patients randomized to the control arm and 263 randomized to the intervention group. The overall age of patients in the study averaged 65 years, but the age of those with elevated BNP averaged closer to 70 years.
During average follow-up of just over 4 years, patients referred to the cardiology program had 25 cases (10%) of heart failure or asymptomatic left ventricular dysfunction, compared with 44 cases (19%) in the control arm, a 54% odds ratio reduction that was statistically significant for the study’s primary endpoint. For the entire study group of 1,374 randomized patients, participation in the group eligible for referred care cut the primary endpoint by a relative 41%, compared with the controls, a statistically significant difference.
A secondary efficacy analysis that tallied the combined rate of incident heart failure, arrhythmia, myocardial infarction, unstable angina, cerebrovascular events, peripheral thrombosis, or pulmonary embolism found 51 events (7%) in the entire intervention group compared with 71 events (10%) in the control group, a 46% odds rate reduction that was statistically significant.
A study limitation was the large percentage of patients in both arms either lost to follow-up, 10%; or who withdrew their consent to participate, another 16%. "It challenges interpretation of the results," commented Dr. Kaul.
But Dr. McDonald and his associates were convinced by their findings.
"We believe the results are conclusive enough to roll this out as a clinical program," he said in an interview. "We are now extending this to another region of Ireland, and we will try to get this disseminated nationally."
He also foresees additional refinements to the program, possibly identifying other risk markers that can compliment BNP and further focus intervention.
"We have shown benefit, but a question is the cost of getting that benefit. BNP is clearly a step up from where we were, but that doesn’t mean we are as good as we could make it."
Dr. McDonald said that he had no disclosures.
On Twitter @mitchelzoler
AT ACC 13
Major finding: BNP-driven referral to intensive preventive care cut heart failures and left ventricular dysfunctions 54%, compared with standard care.
Data source: The STOP-HF trial, which randomized 1,374 adults in 39 primary-care practices around Dublin, Ireland.
Disclosures: Dr. McDonald said that he had no disclosures.
STREAM trial endorses fibrinolysis-first in selected STEMIs
SAN FRANCISCO – Selected patients with ST-elevation myocardial infarction fare just as well with a treatment strategy of early fibrinolysis followed by transfer to a PCI center for timely coronary angiography as they do with primary PCI, according to the landmark STREAM trial.
The large patient population for whom this so-called "pharmacoinvasive" or fibrinolysis-first strategy is applicable comprises those STEMI patients whose symptoms are less than 3 hours old at first medical contact and who cannot undergo primary percutaneous coronary intervention (PCI) within the following hour, Dr. Frans Van de Werf explained in presenting the results of the STREAM (Strategic Reperfusion Early After Myocardial infarction) trial at the annual meeting of the American College of Cardiology.
Guidelines are clear that primary PCI is the preferred reperfusion method in STEMI patients with recent onset of symptoms, but only when the intervention can be performed promptly by an experienced team. That’s a huge caveat. The fact is that primary PCI doesn’t get done within guideline-recommended times for most patients who present to a non–PCI-capable hospital. Large registries consistently show this to be the case because of lengthy transfer times and other logistic issues, noted Dr. Van de Werf, professor of cardiology at the Catholic University of Leuven (Belgium).
"This study is not a challenge to primary PCI, it’s a study in a population who can’t get primary PCI in a short period of time," he stressed.
STREAM was an international, prospective, randomized trial involving 1,892 STEMI patients who presented to a non-PCI center within 3 hours of symptom onset and were unable to undergo primary PCI within the next hour. They were randomized to direct transfer for primary PCI or to fibrinolytic therapy with tenecteplase along with clopidogrel and enoxaparin, followed by transfer to a PCI-capable center.
If an ECG obtained 90 minutes after bolus tenecteplase showed at least 50% ST resolution, patients underwent coronary angiography 6-24 hours later – after the increased procedural bleeding risk associated with fibrinolytic therapy had worn off – with PCI or coronary artery bypass graft (CABG) surgery if indicated. However, if the ECG did not show reperfusion, emergency angiography was performed with an eye toward PCI.
The median time to the start of reperfusion therapy was 100 minutes from symptom onset in the pharmacoinvasive group, compared with 178 minutes in patients assigned to primary PCI.
The primary study endpoint was the 30-day cumulative rate of death, shock, congestive heart failure, or reinfarction. It occurred in 12.4% of the fibrinolysis-first group and 14.3% of those who underwent primary PCI, a nonsignificant difference (P = .21).
The ECG showed that fibrinolysis failed, requiring emergency angiography, in 36% of patients, with rescue PCI performed an average of 2.2 hours after randomization. The other 64% of patients in the pharmacoinvasive group underwent nonurgent catheterization at a median of 17 hours.
"The study results provide the opportunity for a measured approach to invasive coronary interventions, circumventing an urgent procedure in about two-thirds of fibrinolytic-treated STEMI patients," Dr. Van de Werf observed. "Drug therapy before transfer is at least as effective as PCI, and an urgent catheterization was avoided in two-thirds of patients. This gives physicians time to consider other options, such as CABG and medical therapy."
Indeed, CABG was significantly more frequent in the pharmacoinvasive strategy group than with primary PCI, by a margin of 4.7% to 2.1%. As CABG is probably a better revascularization procedure, this is a good thing, the cardiologist continued.
Intracranial hemorrhage occurred significantly more frequently in the fibrinolysis group than with primary PCI, by a margin of 1.0% to 0.2%. However, after one-fifth of STREAM participants had been enrolled, investigators realized that those aged 75 years or older had an excess risk of intracranial hemorrhage with full-dose bolus tenectaplase. Thereafter, the tenectaplase dose was reduced by 50% in elderly patients. It’s worth noting that in the more than 1,500 patients enrolled after the dosing adjustment, the intracranial hemorrhage rate was similar in both study arms and the fibrinolysis-first group’s lower rate of the study’s primary composite endpoint nearly reached statistical significance, Dr. Van de Werf said.
Probably as a result of earlier recanalization in the fibrinolysis group, their rate of heart failure was 6.1%, compared with 7.6% with primary PCI. Cardiogenic shock was also less common in the fibrinolysis group, by a margin of 4.4% to 5.9%.
"These are important observations. They were not statistically significant differences, but nonetheless I think we might see an effect on long-term mortality. So we are collecting long-term mortality data," he continued.
Discussant Dr. Freek Verheugt called STREAM "an important step forward" and applauded the investigators for pursuing "a courageous trial to do in this era of primary PCI."
"This was the first trial to show that early fibrinolysis followed by mandatory timely angiography is as effective as primary PCI in patients who are more than 1 hour away from a PCI hospital. The strength of this study is two-thirds of patients don’t need urgent intervention when they have the lytic before. I think that’s very important because we know that off-hours primary PCI procedures have a worse outcome than daytime procedures. And you have more patients getting deferred intervention and CABG with the lytic strategy. It’s good for the patients, good for their relatives, and good for the interventional cardiologists and the cath lab personnel," said Dr. Verheugt, professor of cardiology at Nijmegen (the Netherlands) University.
"I don’t think STREAM will change the guidelines because it is within the guidelines, but I think it will change practice in certain parts of the world with long drive times to PCI hospitals," he predicted.
Dr. C. Michael Gibson noted that out of more than a dozen prespecified patient subgroups analyzed in STREAM, the outcomes for the two treatment strategies differed significantly in only one: patients with an inferior infarct location. They accounted for roughly half of study participants, and their primary endpoint rate was 7.3% with fibrinolysis compared with 12.3% with primary PCI. It seems counterintuitive that they would do significantly better with the pharmacoinvasive strategy, observed Dr. Gibson, professor of medicine at Harvard University, Boston.
Dr. Van de Werf replied that while the explanation for this finding is unclear, there is some evidence from earlier studies that fibrinolysis is more effective in reperfusing an occluded right rather than left coronary artery.
ACC conference cochair Dr. Neal Kleiman of Methodist Hospital, Houston, declared STREAM "a fantastic study on a very important issue. I think you’ve provided a beacon of light in the fog here."
Simultaneous with his presentation of the STREAM data in San Francisco, the study results were published online (N. Engl. J. Med. 2013 March 10 [doi: 10.1056/NEJMoa1301092]).
STREAM was funded by Boehringer Ingelheim. Dr. Van de Werf is a consultant to the company.
SAN FRANCISCO – Selected patients with ST-elevation myocardial infarction fare just as well with a treatment strategy of early fibrinolysis followed by transfer to a PCI center for timely coronary angiography as they do with primary PCI, according to the landmark STREAM trial.
The large patient population for whom this so-called "pharmacoinvasive" or fibrinolysis-first strategy is applicable comprises those STEMI patients whose symptoms are less than 3 hours old at first medical contact and who cannot undergo primary percutaneous coronary intervention (PCI) within the following hour, Dr. Frans Van de Werf explained in presenting the results of the STREAM (Strategic Reperfusion Early After Myocardial infarction) trial at the annual meeting of the American College of Cardiology.
Guidelines are clear that primary PCI is the preferred reperfusion method in STEMI patients with recent onset of symptoms, but only when the intervention can be performed promptly by an experienced team. That’s a huge caveat. The fact is that primary PCI doesn’t get done within guideline-recommended times for most patients who present to a non–PCI-capable hospital. Large registries consistently show this to be the case because of lengthy transfer times and other logistic issues, noted Dr. Van de Werf, professor of cardiology at the Catholic University of Leuven (Belgium).
"This study is not a challenge to primary PCI, it’s a study in a population who can’t get primary PCI in a short period of time," he stressed.
STREAM was an international, prospective, randomized trial involving 1,892 STEMI patients who presented to a non-PCI center within 3 hours of symptom onset and were unable to undergo primary PCI within the next hour. They were randomized to direct transfer for primary PCI or to fibrinolytic therapy with tenecteplase along with clopidogrel and enoxaparin, followed by transfer to a PCI-capable center.
If an ECG obtained 90 minutes after bolus tenecteplase showed at least 50% ST resolution, patients underwent coronary angiography 6-24 hours later – after the increased procedural bleeding risk associated with fibrinolytic therapy had worn off – with PCI or coronary artery bypass graft (CABG) surgery if indicated. However, if the ECG did not show reperfusion, emergency angiography was performed with an eye toward PCI.
The median time to the start of reperfusion therapy was 100 minutes from symptom onset in the pharmacoinvasive group, compared with 178 minutes in patients assigned to primary PCI.
The primary study endpoint was the 30-day cumulative rate of death, shock, congestive heart failure, or reinfarction. It occurred in 12.4% of the fibrinolysis-first group and 14.3% of those who underwent primary PCI, a nonsignificant difference (P = .21).
The ECG showed that fibrinolysis failed, requiring emergency angiography, in 36% of patients, with rescue PCI performed an average of 2.2 hours after randomization. The other 64% of patients in the pharmacoinvasive group underwent nonurgent catheterization at a median of 17 hours.
"The study results provide the opportunity for a measured approach to invasive coronary interventions, circumventing an urgent procedure in about two-thirds of fibrinolytic-treated STEMI patients," Dr. Van de Werf observed. "Drug therapy before transfer is at least as effective as PCI, and an urgent catheterization was avoided in two-thirds of patients. This gives physicians time to consider other options, such as CABG and medical therapy."
Indeed, CABG was significantly more frequent in the pharmacoinvasive strategy group than with primary PCI, by a margin of 4.7% to 2.1%. As CABG is probably a better revascularization procedure, this is a good thing, the cardiologist continued.
Intracranial hemorrhage occurred significantly more frequently in the fibrinolysis group than with primary PCI, by a margin of 1.0% to 0.2%. However, after one-fifth of STREAM participants had been enrolled, investigators realized that those aged 75 years or older had an excess risk of intracranial hemorrhage with full-dose bolus tenectaplase. Thereafter, the tenectaplase dose was reduced by 50% in elderly patients. It’s worth noting that in the more than 1,500 patients enrolled after the dosing adjustment, the intracranial hemorrhage rate was similar in both study arms and the fibrinolysis-first group’s lower rate of the study’s primary composite endpoint nearly reached statistical significance, Dr. Van de Werf said.
Probably as a result of earlier recanalization in the fibrinolysis group, their rate of heart failure was 6.1%, compared with 7.6% with primary PCI. Cardiogenic shock was also less common in the fibrinolysis group, by a margin of 4.4% to 5.9%.
"These are important observations. They were not statistically significant differences, but nonetheless I think we might see an effect on long-term mortality. So we are collecting long-term mortality data," he continued.
Discussant Dr. Freek Verheugt called STREAM "an important step forward" and applauded the investigators for pursuing "a courageous trial to do in this era of primary PCI."
"This was the first trial to show that early fibrinolysis followed by mandatory timely angiography is as effective as primary PCI in patients who are more than 1 hour away from a PCI hospital. The strength of this study is two-thirds of patients don’t need urgent intervention when they have the lytic before. I think that’s very important because we know that off-hours primary PCI procedures have a worse outcome than daytime procedures. And you have more patients getting deferred intervention and CABG with the lytic strategy. It’s good for the patients, good for their relatives, and good for the interventional cardiologists and the cath lab personnel," said Dr. Verheugt, professor of cardiology at Nijmegen (the Netherlands) University.
"I don’t think STREAM will change the guidelines because it is within the guidelines, but I think it will change practice in certain parts of the world with long drive times to PCI hospitals," he predicted.
Dr. C. Michael Gibson noted that out of more than a dozen prespecified patient subgroups analyzed in STREAM, the outcomes for the two treatment strategies differed significantly in only one: patients with an inferior infarct location. They accounted for roughly half of study participants, and their primary endpoint rate was 7.3% with fibrinolysis compared with 12.3% with primary PCI. It seems counterintuitive that they would do significantly better with the pharmacoinvasive strategy, observed Dr. Gibson, professor of medicine at Harvard University, Boston.
Dr. Van de Werf replied that while the explanation for this finding is unclear, there is some evidence from earlier studies that fibrinolysis is more effective in reperfusing an occluded right rather than left coronary artery.
ACC conference cochair Dr. Neal Kleiman of Methodist Hospital, Houston, declared STREAM "a fantastic study on a very important issue. I think you’ve provided a beacon of light in the fog here."
Simultaneous with his presentation of the STREAM data in San Francisco, the study results were published online (N. Engl. J. Med. 2013 March 10 [doi: 10.1056/NEJMoa1301092]).
STREAM was funded by Boehringer Ingelheim. Dr. Van de Werf is a consultant to the company.
SAN FRANCISCO – Selected patients with ST-elevation myocardial infarction fare just as well with a treatment strategy of early fibrinolysis followed by transfer to a PCI center for timely coronary angiography as they do with primary PCI, according to the landmark STREAM trial.
The large patient population for whom this so-called "pharmacoinvasive" or fibrinolysis-first strategy is applicable comprises those STEMI patients whose symptoms are less than 3 hours old at first medical contact and who cannot undergo primary percutaneous coronary intervention (PCI) within the following hour, Dr. Frans Van de Werf explained in presenting the results of the STREAM (Strategic Reperfusion Early After Myocardial infarction) trial at the annual meeting of the American College of Cardiology.
Guidelines are clear that primary PCI is the preferred reperfusion method in STEMI patients with recent onset of symptoms, but only when the intervention can be performed promptly by an experienced team. That’s a huge caveat. The fact is that primary PCI doesn’t get done within guideline-recommended times for most patients who present to a non–PCI-capable hospital. Large registries consistently show this to be the case because of lengthy transfer times and other logistic issues, noted Dr. Van de Werf, professor of cardiology at the Catholic University of Leuven (Belgium).
"This study is not a challenge to primary PCI, it’s a study in a population who can’t get primary PCI in a short period of time," he stressed.
STREAM was an international, prospective, randomized trial involving 1,892 STEMI patients who presented to a non-PCI center within 3 hours of symptom onset and were unable to undergo primary PCI within the next hour. They were randomized to direct transfer for primary PCI or to fibrinolytic therapy with tenecteplase along with clopidogrel and enoxaparin, followed by transfer to a PCI-capable center.
If an ECG obtained 90 minutes after bolus tenecteplase showed at least 50% ST resolution, patients underwent coronary angiography 6-24 hours later – after the increased procedural bleeding risk associated with fibrinolytic therapy had worn off – with PCI or coronary artery bypass graft (CABG) surgery if indicated. However, if the ECG did not show reperfusion, emergency angiography was performed with an eye toward PCI.
The median time to the start of reperfusion therapy was 100 minutes from symptom onset in the pharmacoinvasive group, compared with 178 minutes in patients assigned to primary PCI.
The primary study endpoint was the 30-day cumulative rate of death, shock, congestive heart failure, or reinfarction. It occurred in 12.4% of the fibrinolysis-first group and 14.3% of those who underwent primary PCI, a nonsignificant difference (P = .21).
The ECG showed that fibrinolysis failed, requiring emergency angiography, in 36% of patients, with rescue PCI performed an average of 2.2 hours after randomization. The other 64% of patients in the pharmacoinvasive group underwent nonurgent catheterization at a median of 17 hours.
"The study results provide the opportunity for a measured approach to invasive coronary interventions, circumventing an urgent procedure in about two-thirds of fibrinolytic-treated STEMI patients," Dr. Van de Werf observed. "Drug therapy before transfer is at least as effective as PCI, and an urgent catheterization was avoided in two-thirds of patients. This gives physicians time to consider other options, such as CABG and medical therapy."
Indeed, CABG was significantly more frequent in the pharmacoinvasive strategy group than with primary PCI, by a margin of 4.7% to 2.1%. As CABG is probably a better revascularization procedure, this is a good thing, the cardiologist continued.
Intracranial hemorrhage occurred significantly more frequently in the fibrinolysis group than with primary PCI, by a margin of 1.0% to 0.2%. However, after one-fifth of STREAM participants had been enrolled, investigators realized that those aged 75 years or older had an excess risk of intracranial hemorrhage with full-dose bolus tenectaplase. Thereafter, the tenectaplase dose was reduced by 50% in elderly patients. It’s worth noting that in the more than 1,500 patients enrolled after the dosing adjustment, the intracranial hemorrhage rate was similar in both study arms and the fibrinolysis-first group’s lower rate of the study’s primary composite endpoint nearly reached statistical significance, Dr. Van de Werf said.
Probably as a result of earlier recanalization in the fibrinolysis group, their rate of heart failure was 6.1%, compared with 7.6% with primary PCI. Cardiogenic shock was also less common in the fibrinolysis group, by a margin of 4.4% to 5.9%.
"These are important observations. They were not statistically significant differences, but nonetheless I think we might see an effect on long-term mortality. So we are collecting long-term mortality data," he continued.
Discussant Dr. Freek Verheugt called STREAM "an important step forward" and applauded the investigators for pursuing "a courageous trial to do in this era of primary PCI."
"This was the first trial to show that early fibrinolysis followed by mandatory timely angiography is as effective as primary PCI in patients who are more than 1 hour away from a PCI hospital. The strength of this study is two-thirds of patients don’t need urgent intervention when they have the lytic before. I think that’s very important because we know that off-hours primary PCI procedures have a worse outcome than daytime procedures. And you have more patients getting deferred intervention and CABG with the lytic strategy. It’s good for the patients, good for their relatives, and good for the interventional cardiologists and the cath lab personnel," said Dr. Verheugt, professor of cardiology at Nijmegen (the Netherlands) University.
"I don’t think STREAM will change the guidelines because it is within the guidelines, but I think it will change practice in certain parts of the world with long drive times to PCI hospitals," he predicted.
Dr. C. Michael Gibson noted that out of more than a dozen prespecified patient subgroups analyzed in STREAM, the outcomes for the two treatment strategies differed significantly in only one: patients with an inferior infarct location. They accounted for roughly half of study participants, and their primary endpoint rate was 7.3% with fibrinolysis compared with 12.3% with primary PCI. It seems counterintuitive that they would do significantly better with the pharmacoinvasive strategy, observed Dr. Gibson, professor of medicine at Harvard University, Boston.
Dr. Van de Werf replied that while the explanation for this finding is unclear, there is some evidence from earlier studies that fibrinolysis is more effective in reperfusing an occluded right rather than left coronary artery.
ACC conference cochair Dr. Neal Kleiman of Methodist Hospital, Houston, declared STREAM "a fantastic study on a very important issue. I think you’ve provided a beacon of light in the fog here."
Simultaneous with his presentation of the STREAM data in San Francisco, the study results were published online (N. Engl. J. Med. 2013 March 10 [doi: 10.1056/NEJMoa1301092]).
STREAM was funded by Boehringer Ingelheim. Dr. Van de Werf is a consultant to the company.
AT ACC 13
Major finding: The 30-day composite rate of death, shock, congestive heart failure, or reinfarction in STEMI patients was 12.4% in those randomized to a fibrinolysis-first pharmacoinvasive strategy versus 14.3% with primary PCI.
Data source: STREAM, a randomized prospective study in 1,892 patients whose first medical contact was less than 3 hours since symptom onset and who were unable to undergo primary PCI within the next hour.
Disclosures: STREAM was funded by Boehringer Ingelheim. Dr. Van de Werf is a consultant to the company.
One-year outcomes support emergency department CCTA
SAN FRANCISCO – Coronary CT angiography works better than traditional rule-out approaches for identifying emergency department patients with chest pain who are free of significant coronary disease, according to 1-year results from a randomized comparison of more than 1,300 patients.
The results also show that relying on coronary CT angiography (CCTA) for emergency department assessment of coronary disease is safe, with a 1-year rate of death or myocardial infarction substantially below 1% in patients judged negative for coronary disease by CCTA, Dr. Judd E. Hollander said at the annual meeting of the American College of Cardiology.
The findings confirmed and extended the 30-day results reported a year ago from the same study, the American College of Radiology Imaging Network (ACRIN) PA 4005 study, which randomized 1,370 low- to intermediate-risk patients who presented with chest pain and possible acute coronary syndrome at any of five U.S. emergency departments.
Two-thirds of the patients were randomized to assessment that included CCTA when deemed necessary, while the remaining third underwent more traditional assessment that could include an exercise treadmill test, a stress test with imaging, and stress echocardiography.
While the results supported a role for routine use of CCTA for assessing the types of patients enrolled in the study, Dr. Hollander stressed that a CCTA is not needed for every ED patient with questionable chest pain.
"We try to use this as an exclusionary test for patients who need an exclusionary test," said Dr. Hollander, professor and clinical research director in the department of emergency medicine at the University of Pennsylvania in Philadelphia.
"We want to avoid making this like a d-dimer test [for thrombus] or CT perfusion [for stroke patients], where everyone who comes into the ED with appropriate signs and symptoms gets one. We don’t use CCTA on patients we normally discharge. There is the risk from radiation. You need to ask how much do you need to find out what is going on with the patient sooner rather than later," he said.
During year-long follow-up on 1,368 of the starting ACRIN patients (one patient was lost to follow-up from each randomization group), one cardiac death and one myocardial infarction occurred among the 825 patients randomized to the CCTA arm and declared free of coronary disease, a 0.2% rate that fell within the study’s prespecified safety criterion of less than 1%.
CCTA’s 1-year safety came without any boost in resource use compared with ED chest-pain patients assessed by conventional means. Overall use of cardiac testing, hospital readmissions, revascularization, and ED visits was similar during 1-year follow-up in the two treatment arms, Dr. Hollander said. Further breakdown of the resource-use data showed that the majority of medical activity following the index hospitalization occurred in the 9% of the initial patients identified with coronary disease by CCTA. Fewer resources were used in patients who had questionable coronary disease following CCTA, and the least amount of resource use occurred in patients without coronary disease by CCTA.
Because CCTA categorized 9% of patients in that study arm as having coronary disease compared with 3% of the control group, and since 77% of patients in the CCTA arm were judged free of coronary disease compared with 61% in the control arm, CCTA "shifts resources to where they are most useful, with more coronary artery disease identified and treated and more patients without disease not receiving treatment," Dr. Hollander said.
The initial, 30-day ACRIN report said that 50% of patients managed in the CCTA arm were discharged early from the ED, compared with 23% of the control group (N. Engl. J. Med. 2012;366:1393-403). Patients in the CCTA group also had a substantially shorter average length of stay during their initial hospital visit.
The ACRIN PA 4005 study was sponsored by the Pennsylvania Department of Health and the ACRIN Foundation. Dr. Hollander said that he has also been a consultant to Behring, Janssen, Luitpold, and Radiometer, and that he has received research funding from Abbott, Alere, Brahms, and Siemens.
On Twitter @mitchelzoler
SAN FRANCISCO – Coronary CT angiography works better than traditional rule-out approaches for identifying emergency department patients with chest pain who are free of significant coronary disease, according to 1-year results from a randomized comparison of more than 1,300 patients.
The results also show that relying on coronary CT angiography (CCTA) for emergency department assessment of coronary disease is safe, with a 1-year rate of death or myocardial infarction substantially below 1% in patients judged negative for coronary disease by CCTA, Dr. Judd E. Hollander said at the annual meeting of the American College of Cardiology.
The findings confirmed and extended the 30-day results reported a year ago from the same study, the American College of Radiology Imaging Network (ACRIN) PA 4005 study, which randomized 1,370 low- to intermediate-risk patients who presented with chest pain and possible acute coronary syndrome at any of five U.S. emergency departments.
Two-thirds of the patients were randomized to assessment that included CCTA when deemed necessary, while the remaining third underwent more traditional assessment that could include an exercise treadmill test, a stress test with imaging, and stress echocardiography.
While the results supported a role for routine use of CCTA for assessing the types of patients enrolled in the study, Dr. Hollander stressed that a CCTA is not needed for every ED patient with questionable chest pain.
"We try to use this as an exclusionary test for patients who need an exclusionary test," said Dr. Hollander, professor and clinical research director in the department of emergency medicine at the University of Pennsylvania in Philadelphia.
"We want to avoid making this like a d-dimer test [for thrombus] or CT perfusion [for stroke patients], where everyone who comes into the ED with appropriate signs and symptoms gets one. We don’t use CCTA on patients we normally discharge. There is the risk from radiation. You need to ask how much do you need to find out what is going on with the patient sooner rather than later," he said.
During year-long follow-up on 1,368 of the starting ACRIN patients (one patient was lost to follow-up from each randomization group), one cardiac death and one myocardial infarction occurred among the 825 patients randomized to the CCTA arm and declared free of coronary disease, a 0.2% rate that fell within the study’s prespecified safety criterion of less than 1%.
CCTA’s 1-year safety came without any boost in resource use compared with ED chest-pain patients assessed by conventional means. Overall use of cardiac testing, hospital readmissions, revascularization, and ED visits was similar during 1-year follow-up in the two treatment arms, Dr. Hollander said. Further breakdown of the resource-use data showed that the majority of medical activity following the index hospitalization occurred in the 9% of the initial patients identified with coronary disease by CCTA. Fewer resources were used in patients who had questionable coronary disease following CCTA, and the least amount of resource use occurred in patients without coronary disease by CCTA.
Because CCTA categorized 9% of patients in that study arm as having coronary disease compared with 3% of the control group, and since 77% of patients in the CCTA arm were judged free of coronary disease compared with 61% in the control arm, CCTA "shifts resources to where they are most useful, with more coronary artery disease identified and treated and more patients without disease not receiving treatment," Dr. Hollander said.
The initial, 30-day ACRIN report said that 50% of patients managed in the CCTA arm were discharged early from the ED, compared with 23% of the control group (N. Engl. J. Med. 2012;366:1393-403). Patients in the CCTA group also had a substantially shorter average length of stay during their initial hospital visit.
The ACRIN PA 4005 study was sponsored by the Pennsylvania Department of Health and the ACRIN Foundation. Dr. Hollander said that he has also been a consultant to Behring, Janssen, Luitpold, and Radiometer, and that he has received research funding from Abbott, Alere, Brahms, and Siemens.
On Twitter @mitchelzoler
SAN FRANCISCO – Coronary CT angiography works better than traditional rule-out approaches for identifying emergency department patients with chest pain who are free of significant coronary disease, according to 1-year results from a randomized comparison of more than 1,300 patients.
The results also show that relying on coronary CT angiography (CCTA) for emergency department assessment of coronary disease is safe, with a 1-year rate of death or myocardial infarction substantially below 1% in patients judged negative for coronary disease by CCTA, Dr. Judd E. Hollander said at the annual meeting of the American College of Cardiology.
The findings confirmed and extended the 30-day results reported a year ago from the same study, the American College of Radiology Imaging Network (ACRIN) PA 4005 study, which randomized 1,370 low- to intermediate-risk patients who presented with chest pain and possible acute coronary syndrome at any of five U.S. emergency departments.
Two-thirds of the patients were randomized to assessment that included CCTA when deemed necessary, while the remaining third underwent more traditional assessment that could include an exercise treadmill test, a stress test with imaging, and stress echocardiography.
While the results supported a role for routine use of CCTA for assessing the types of patients enrolled in the study, Dr. Hollander stressed that a CCTA is not needed for every ED patient with questionable chest pain.
"We try to use this as an exclusionary test for patients who need an exclusionary test," said Dr. Hollander, professor and clinical research director in the department of emergency medicine at the University of Pennsylvania in Philadelphia.
"We want to avoid making this like a d-dimer test [for thrombus] or CT perfusion [for stroke patients], where everyone who comes into the ED with appropriate signs and symptoms gets one. We don’t use CCTA on patients we normally discharge. There is the risk from radiation. You need to ask how much do you need to find out what is going on with the patient sooner rather than later," he said.
During year-long follow-up on 1,368 of the starting ACRIN patients (one patient was lost to follow-up from each randomization group), one cardiac death and one myocardial infarction occurred among the 825 patients randomized to the CCTA arm and declared free of coronary disease, a 0.2% rate that fell within the study’s prespecified safety criterion of less than 1%.
CCTA’s 1-year safety came without any boost in resource use compared with ED chest-pain patients assessed by conventional means. Overall use of cardiac testing, hospital readmissions, revascularization, and ED visits was similar during 1-year follow-up in the two treatment arms, Dr. Hollander said. Further breakdown of the resource-use data showed that the majority of medical activity following the index hospitalization occurred in the 9% of the initial patients identified with coronary disease by CCTA. Fewer resources were used in patients who had questionable coronary disease following CCTA, and the least amount of resource use occurred in patients without coronary disease by CCTA.
Because CCTA categorized 9% of patients in that study arm as having coronary disease compared with 3% of the control group, and since 77% of patients in the CCTA arm were judged free of coronary disease compared with 61% in the control arm, CCTA "shifts resources to where they are most useful, with more coronary artery disease identified and treated and more patients without disease not receiving treatment," Dr. Hollander said.
The initial, 30-day ACRIN report said that 50% of patients managed in the CCTA arm were discharged early from the ED, compared with 23% of the control group (N. Engl. J. Med. 2012;366:1393-403). Patients in the CCTA group also had a substantially shorter average length of stay during their initial hospital visit.
The ACRIN PA 4005 study was sponsored by the Pennsylvania Department of Health and the ACRIN Foundation. Dr. Hollander said that he has also been a consultant to Behring, Janssen, Luitpold, and Radiometer, and that he has received research funding from Abbott, Alere, Brahms, and Siemens.
On Twitter @mitchelzoler
AT ACC 13
Major finding: Patients negative for coronary disease by CT angiography had a 0.2% rate of cardiac death or myocardial infarction at 1-year follow-up.
Data source: The ACRIN PA 4005 study, which followed 1,368 chest-pain patients for 1 year after randomization to coronary CT angiography or conventional emergency department assessment.
Disclosures: The ACRIN PA 4005 study was sponsored by the Pennsylvania Department of Health and the ACRIN Foundation. Dr. Hollander said that he has also been a consultant to Behring, Janssen, Luitpold, and Radiometer, and that he has received research funding from Abbott, Alere, Brahms, and Siemens.
Digoxin linked to doubled mortality in atrial fib
SAN FRANCISCO – Starting digoxin treatment in patients with newly diagnosed atrial fibrillation was linked with a doubled risk of death during the subsequent 8 months, on the basis of an observation of more than 23,000 patients in a California health system.
"This is a very big deal. We will tell Kaiser physicians not to prescribe digoxin to patients with atrial fibrillation," Dr. James V. Freeman said while presenting a poster at the annual meeting of the American College of Cardiology.
Although the mechanism is not known, he said he suspects it may involve arrhythmia generation and sudden death. The hospitalization rate among patients who began digoxin ran the same as in those not on the drug, even though mortality doubled.
While not widely used, digoxin received significant interest from the treating physicians in California during January 2006 through June 2009, with 13% of newly diagnosed atrial fibrillation patients receiving prescriptions. The analysis excluded patients who were already on digoxin at the time of their incident atrial fibrillation, so "these were not just physicians keeping patients on digoxin for years," Dr. Freeman said in an interview.
Existing recommendations from the ACC, last updated in 2012, list digoxin as one of eight drug choices for heart rate and rhythm control in atrial fibrillation patients. The college lists the eight drugs alphabetically and does not rate any drug as better or worse than the others.
The study presented by Dr. Freeman involved 23,272 adults aged 21 years or older with an index diagnosis of atrial fibrillation in the Kaiser Permanente Northern California and Southern California health plans during the 3.5-year period examined. Among these patients who had never used digoxin before and who were without heart failure, 2,997 filled at least one prescription for the drug.
During a median follow-up of 10 months, the mortality rate was 9.49/100 person-years of follow-up among those who received digoxin, versus 4.27/100 person-years in nonusers. After adjusting for a list of possible demographic and clinical confounders, the investigators found that patients who received digoxin had a 2.06 higher mortality rate, a statistically significant difference, reported Dr. Freeman, a cardiologist at Stanford (Calif.) University. Subgroup analyses showed similar increased mortality rates with digoxin use across both women and men and among patients younger than 75 years, 75-84, and 85 years or older.
The hospitalization rate was roughly 3 cases for every 100 person-years of follow-up in both groups.
Dr. Freeman conceded that as an observational study, the analysis was vulnerable to possible confounding factors, but in this case he thought that the risk of significant confounding was minimal. The Kaiser system collects voluminous data on comorbidities and other treatments that patients received, and the pattern showed a slight tilt toward sicker patients with more comorbidity among those who did not receive digoxin. For example, the nonusers had a 76% prevalence of hypertension, a 4% prevalence of prior coronary stenting, and a 4% rate of prior stroke, compared with prevalence rates of 74%, 3%, and 3%, respectively, among digoxin recipients. However, the digoxin recipients had slightly higher rates of cancer and lung disease, 7% compared with 6%, and 23% vs. 20%, respectively.
The patients not on digoxin also had slightly higher rates of medication with other potentially beneficial drugs. For example, treatment with an ACE inhibitor occurred in 31% of digoxin nonusers compared with 29% of the digoxin users; beta-blocker treatment occurred in 46% of digoxin nonusers, compared with 40% of the digoxin users.
Dr. Freeman said he had no relevant financial disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – Starting digoxin treatment in patients with newly diagnosed atrial fibrillation was linked with a doubled risk of death during the subsequent 8 months, on the basis of an observation of more than 23,000 patients in a California health system.
"This is a very big deal. We will tell Kaiser physicians not to prescribe digoxin to patients with atrial fibrillation," Dr. James V. Freeman said while presenting a poster at the annual meeting of the American College of Cardiology.
Although the mechanism is not known, he said he suspects it may involve arrhythmia generation and sudden death. The hospitalization rate among patients who began digoxin ran the same as in those not on the drug, even though mortality doubled.
While not widely used, digoxin received significant interest from the treating physicians in California during January 2006 through June 2009, with 13% of newly diagnosed atrial fibrillation patients receiving prescriptions. The analysis excluded patients who were already on digoxin at the time of their incident atrial fibrillation, so "these were not just physicians keeping patients on digoxin for years," Dr. Freeman said in an interview.
Existing recommendations from the ACC, last updated in 2012, list digoxin as one of eight drug choices for heart rate and rhythm control in atrial fibrillation patients. The college lists the eight drugs alphabetically and does not rate any drug as better or worse than the others.
The study presented by Dr. Freeman involved 23,272 adults aged 21 years or older with an index diagnosis of atrial fibrillation in the Kaiser Permanente Northern California and Southern California health plans during the 3.5-year period examined. Among these patients who had never used digoxin before and who were without heart failure, 2,997 filled at least one prescription for the drug.
During a median follow-up of 10 months, the mortality rate was 9.49/100 person-years of follow-up among those who received digoxin, versus 4.27/100 person-years in nonusers. After adjusting for a list of possible demographic and clinical confounders, the investigators found that patients who received digoxin had a 2.06 higher mortality rate, a statistically significant difference, reported Dr. Freeman, a cardiologist at Stanford (Calif.) University. Subgroup analyses showed similar increased mortality rates with digoxin use across both women and men and among patients younger than 75 years, 75-84, and 85 years or older.
The hospitalization rate was roughly 3 cases for every 100 person-years of follow-up in both groups.
Dr. Freeman conceded that as an observational study, the analysis was vulnerable to possible confounding factors, but in this case he thought that the risk of significant confounding was minimal. The Kaiser system collects voluminous data on comorbidities and other treatments that patients received, and the pattern showed a slight tilt toward sicker patients with more comorbidity among those who did not receive digoxin. For example, the nonusers had a 76% prevalence of hypertension, a 4% prevalence of prior coronary stenting, and a 4% rate of prior stroke, compared with prevalence rates of 74%, 3%, and 3%, respectively, among digoxin recipients. However, the digoxin recipients had slightly higher rates of cancer and lung disease, 7% compared with 6%, and 23% vs. 20%, respectively.
The patients not on digoxin also had slightly higher rates of medication with other potentially beneficial drugs. For example, treatment with an ACE inhibitor occurred in 31% of digoxin nonusers compared with 29% of the digoxin users; beta-blocker treatment occurred in 46% of digoxin nonusers, compared with 40% of the digoxin users.
Dr. Freeman said he had no relevant financial disclosures.
On Twitter @mitchelzoler
SAN FRANCISCO – Starting digoxin treatment in patients with newly diagnosed atrial fibrillation was linked with a doubled risk of death during the subsequent 8 months, on the basis of an observation of more than 23,000 patients in a California health system.
"This is a very big deal. We will tell Kaiser physicians not to prescribe digoxin to patients with atrial fibrillation," Dr. James V. Freeman said while presenting a poster at the annual meeting of the American College of Cardiology.
Although the mechanism is not known, he said he suspects it may involve arrhythmia generation and sudden death. The hospitalization rate among patients who began digoxin ran the same as in those not on the drug, even though mortality doubled.
While not widely used, digoxin received significant interest from the treating physicians in California during January 2006 through June 2009, with 13% of newly diagnosed atrial fibrillation patients receiving prescriptions. The analysis excluded patients who were already on digoxin at the time of their incident atrial fibrillation, so "these were not just physicians keeping patients on digoxin for years," Dr. Freeman said in an interview.
Existing recommendations from the ACC, last updated in 2012, list digoxin as one of eight drug choices for heart rate and rhythm control in atrial fibrillation patients. The college lists the eight drugs alphabetically and does not rate any drug as better or worse than the others.
The study presented by Dr. Freeman involved 23,272 adults aged 21 years or older with an index diagnosis of atrial fibrillation in the Kaiser Permanente Northern California and Southern California health plans during the 3.5-year period examined. Among these patients who had never used digoxin before and who were without heart failure, 2,997 filled at least one prescription for the drug.
During a median follow-up of 10 months, the mortality rate was 9.49/100 person-years of follow-up among those who received digoxin, versus 4.27/100 person-years in nonusers. After adjusting for a list of possible demographic and clinical confounders, the investigators found that patients who received digoxin had a 2.06 higher mortality rate, a statistically significant difference, reported Dr. Freeman, a cardiologist at Stanford (Calif.) University. Subgroup analyses showed similar increased mortality rates with digoxin use across both women and men and among patients younger than 75 years, 75-84, and 85 years or older.
The hospitalization rate was roughly 3 cases for every 100 person-years of follow-up in both groups.
Dr. Freeman conceded that as an observational study, the analysis was vulnerable to possible confounding factors, but in this case he thought that the risk of significant confounding was minimal. The Kaiser system collects voluminous data on comorbidities and other treatments that patients received, and the pattern showed a slight tilt toward sicker patients with more comorbidity among those who did not receive digoxin. For example, the nonusers had a 76% prevalence of hypertension, a 4% prevalence of prior coronary stenting, and a 4% rate of prior stroke, compared with prevalence rates of 74%, 3%, and 3%, respectively, among digoxin recipients. However, the digoxin recipients had slightly higher rates of cancer and lung disease, 7% compared with 6%, and 23% vs. 20%, respectively.
The patients not on digoxin also had slightly higher rates of medication with other potentially beneficial drugs. For example, treatment with an ACE inhibitor occurred in 31% of digoxin nonusers compared with 29% of the digoxin users; beta-blocker treatment occurred in 46% of digoxin nonusers, compared with 40% of the digoxin users.
Dr. Freeman said he had no relevant financial disclosures.
On Twitter @mitchelzoler
AT ACC 2013
Major finding: Newly diagnosed atrial fibrillation patients who received digoxin had twice the mortality of new a fib patients not on the drug.
Data source: An observational study of 23,272 patients with newly diagnosed atrial fibrillation and no history of digoxin use or heart failure in a U.S. health system during 2006-2009.
Disclosures: Dr. Freeman said he had no relevant financial disclosures.