User login
Opt for redo root surgery, not TAVI, in young patients
CHICAGO – Whether to perform transcatheter aortic valve implantation in a 57-year-old patient with a severely calcified aortic homograft was the subject of a case report presented at Heart Valve Summit 2012.
"In our center, even though we do a huge number of TAVIs [transcatheter aortic valve implantations], we still believe TAVI should be left for the older patients and those with a restricted life expectancy, because the long-term results are not known," said Dr. Michael Borger, assistant director of the Leipzig (Germany) Heart Center.
The patient in this case was a 57 year-old woman who presented with increased shortness of breath and was found to have NYHA II-III heart failure. At age 40, she had received a homograft aortic root replacement for destructive endocarditis.
Her ejection fraction and left ventricular dimensions were preserved, her AV gradient was 86/52 mm Hg, and her effective orifice area (EOA) was 0.6 cm2. She had no other risk factors and was taking no medications. A coronary angiogram showed a severely calcified homograft and isolated proximal stenosis of the right coronary artery.
Dr. Borger discussed two options: redo root replacement surgery with a bypass to the right coronary artery or a transcatheter aortic valve replacement (TAVR) with a PCI to the right coronary artery.
The decision was to perform conventional surgery. "The patient underwent a redo Bentall operation with a mechanical valve, as well as a RIMA (right internal mammary artery) to RCA (right coronary artery) bypass. She did very well postoperatively without any complications," he said.
Aortic root replacements with aortic homografts are not without risk, and the literature shows relatively high mortality for homograft reoperations. Reoperation after stentless AVR also has been performed, but it often requires replacement of the aortic root and is associated with increased mortality (Ann. Thorac. Surg. 2007;84:737-43).
"Most of those [stentless] operations are difficult because of the inability to get a good plane of cleavage between the stentless valve and the native aortic root," said Dr. Borger. "The large majority of those patients end up leaving the OR with a full root replacement."
Dr. Borger’s fellow panelist, Dr. Michael Reardon, agreed. "I was a real fan of the Toronto SPV valve, and ... I’ve taken a couple out," said Dr. Reardon, professor and vice chair of the Methodist DeBakey Heart and Vascular Center in Houston. "They all end up in root replacements. By the time you’re finished you end up having these shards of tissue ... and porcine tissue incites a huge dermoplastic reaction. ... I personally found it very difficult."
Dr. Borger noted, "In Leipzig we have put in a large number of Toronto roots and, knock on wood, have not reoperated on one of them yet. However, they have not yet reached the period whereby you expect to observe structural valve dysfunction."
A study of valve-related events after aortic root replacement with cryopreserved aortic homografts examined risk after placement of a homograft and found that a heavily calcified homograft at the time of reoperation was a significant predictor of death (Ann. Thorac. Surg. 2005;79:1491-5).
"I’m not saying that TAVI is not an option for all young patients," said Dr. Borger. "If you’ve got a young patient who is at very high risk for conventional surgery with lots of comorbidities, whose life expectancy is 5 years or less, then sure, do a TAVI. But for this particular patient, if she survives the operation, you’re going to put her back on an almost normal survival curve."
Dr. Borger disclosed consultant fees and honoraria from Medtronic, St. Jude Medical, and Edwards Lifesciences.
CHICAGO – Whether to perform transcatheter aortic valve implantation in a 57-year-old patient with a severely calcified aortic homograft was the subject of a case report presented at Heart Valve Summit 2012.
"In our center, even though we do a huge number of TAVIs [transcatheter aortic valve implantations], we still believe TAVI should be left for the older patients and those with a restricted life expectancy, because the long-term results are not known," said Dr. Michael Borger, assistant director of the Leipzig (Germany) Heart Center.
The patient in this case was a 57 year-old woman who presented with increased shortness of breath and was found to have NYHA II-III heart failure. At age 40, she had received a homograft aortic root replacement for destructive endocarditis.
Her ejection fraction and left ventricular dimensions were preserved, her AV gradient was 86/52 mm Hg, and her effective orifice area (EOA) was 0.6 cm2. She had no other risk factors and was taking no medications. A coronary angiogram showed a severely calcified homograft and isolated proximal stenosis of the right coronary artery.
Dr. Borger discussed two options: redo root replacement surgery with a bypass to the right coronary artery or a transcatheter aortic valve replacement (TAVR) with a PCI to the right coronary artery.
The decision was to perform conventional surgery. "The patient underwent a redo Bentall operation with a mechanical valve, as well as a RIMA (right internal mammary artery) to RCA (right coronary artery) bypass. She did very well postoperatively without any complications," he said.
Aortic root replacements with aortic homografts are not without risk, and the literature shows relatively high mortality for homograft reoperations. Reoperation after stentless AVR also has been performed, but it often requires replacement of the aortic root and is associated with increased mortality (Ann. Thorac. Surg. 2007;84:737-43).
"Most of those [stentless] operations are difficult because of the inability to get a good plane of cleavage between the stentless valve and the native aortic root," said Dr. Borger. "The large majority of those patients end up leaving the OR with a full root replacement."
Dr. Borger’s fellow panelist, Dr. Michael Reardon, agreed. "I was a real fan of the Toronto SPV valve, and ... I’ve taken a couple out," said Dr. Reardon, professor and vice chair of the Methodist DeBakey Heart and Vascular Center in Houston. "They all end up in root replacements. By the time you’re finished you end up having these shards of tissue ... and porcine tissue incites a huge dermoplastic reaction. ... I personally found it very difficult."
Dr. Borger noted, "In Leipzig we have put in a large number of Toronto roots and, knock on wood, have not reoperated on one of them yet. However, they have not yet reached the period whereby you expect to observe structural valve dysfunction."
A study of valve-related events after aortic root replacement with cryopreserved aortic homografts examined risk after placement of a homograft and found that a heavily calcified homograft at the time of reoperation was a significant predictor of death (Ann. Thorac. Surg. 2005;79:1491-5).
"I’m not saying that TAVI is not an option for all young patients," said Dr. Borger. "If you’ve got a young patient who is at very high risk for conventional surgery with lots of comorbidities, whose life expectancy is 5 years or less, then sure, do a TAVI. But for this particular patient, if she survives the operation, you’re going to put her back on an almost normal survival curve."
Dr. Borger disclosed consultant fees and honoraria from Medtronic, St. Jude Medical, and Edwards Lifesciences.
CHICAGO – Whether to perform transcatheter aortic valve implantation in a 57-year-old patient with a severely calcified aortic homograft was the subject of a case report presented at Heart Valve Summit 2012.
"In our center, even though we do a huge number of TAVIs [transcatheter aortic valve implantations], we still believe TAVI should be left for the older patients and those with a restricted life expectancy, because the long-term results are not known," said Dr. Michael Borger, assistant director of the Leipzig (Germany) Heart Center.
The patient in this case was a 57 year-old woman who presented with increased shortness of breath and was found to have NYHA II-III heart failure. At age 40, she had received a homograft aortic root replacement for destructive endocarditis.
Her ejection fraction and left ventricular dimensions were preserved, her AV gradient was 86/52 mm Hg, and her effective orifice area (EOA) was 0.6 cm2. She had no other risk factors and was taking no medications. A coronary angiogram showed a severely calcified homograft and isolated proximal stenosis of the right coronary artery.
Dr. Borger discussed two options: redo root replacement surgery with a bypass to the right coronary artery or a transcatheter aortic valve replacement (TAVR) with a PCI to the right coronary artery.
The decision was to perform conventional surgery. "The patient underwent a redo Bentall operation with a mechanical valve, as well as a RIMA (right internal mammary artery) to RCA (right coronary artery) bypass. She did very well postoperatively without any complications," he said.
Aortic root replacements with aortic homografts are not without risk, and the literature shows relatively high mortality for homograft reoperations. Reoperation after stentless AVR also has been performed, but it often requires replacement of the aortic root and is associated with increased mortality (Ann. Thorac. Surg. 2007;84:737-43).
"Most of those [stentless] operations are difficult because of the inability to get a good plane of cleavage between the stentless valve and the native aortic root," said Dr. Borger. "The large majority of those patients end up leaving the OR with a full root replacement."
Dr. Borger’s fellow panelist, Dr. Michael Reardon, agreed. "I was a real fan of the Toronto SPV valve, and ... I’ve taken a couple out," said Dr. Reardon, professor and vice chair of the Methodist DeBakey Heart and Vascular Center in Houston. "They all end up in root replacements. By the time you’re finished you end up having these shards of tissue ... and porcine tissue incites a huge dermoplastic reaction. ... I personally found it very difficult."
Dr. Borger noted, "In Leipzig we have put in a large number of Toronto roots and, knock on wood, have not reoperated on one of them yet. However, they have not yet reached the period whereby you expect to observe structural valve dysfunction."
A study of valve-related events after aortic root replacement with cryopreserved aortic homografts examined risk after placement of a homograft and found that a heavily calcified homograft at the time of reoperation was a significant predictor of death (Ann. Thorac. Surg. 2005;79:1491-5).
"I’m not saying that TAVI is not an option for all young patients," said Dr. Borger. "If you’ve got a young patient who is at very high risk for conventional surgery with lots of comorbidities, whose life expectancy is 5 years or less, then sure, do a TAVI. But for this particular patient, if she survives the operation, you’re going to put her back on an almost normal survival curve."
Dr. Borger disclosed consultant fees and honoraria from Medtronic, St. Jude Medical, and Edwards Lifesciences.
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2012
Minimally invasive surgery with sutureless valves shows benefits
CHICAGO – European data suggest that minimally invasive aortic valve surgery has several benefits and few downsides when compared to conventional aortic valve replacement.
Bleeding is decreased, as is ICU and hospital length of stay. Cosmesis is improved. Sutureless valves may facilitate the performance of minimally invasive aortic valve replacement (AVR), and are associated with decreased ischemic times and lower transvalvular gradients – an advantage when concomitant procedures are performed or patients are high risk, according to a presentation at the 2012 Heart Valve summit.
Sutureless aortic valves facilitate minimal basic AVR and minimize myocardial ischemic time, said Dr. Michael Borger of Leipzig (Germany) Heart Center.
He described the evidence to date, as well as his personal experience, at this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
Leipzig Heart Center is one of Europe’s largest cardiac facilities, with 4,000 cardiac operations per year.
The number of patients who undergo minimally invasive aortic valve procedures is still very low, said Dr. Borger, and he urged the audience to consider this option in the future, especially when transcatheter aortic valve implantation (TAVI) becomes as widely accepted in America as it is in Europe. In Germany alone, 31% of isolated AVRs are now done by TAVI.
"Decreased myocardial ischemic time doesn’t matter for someone who needs an isolated aortic valve, [such as a] 70-year-old patient with no risk factors. It doesn’t matter if you shorten their ischemic time by 20 minutes. That’s not the point. The point is that a sutureless valve facilitates minimally invasive surgery by making it easier to do; and a marker for that is decreased ischemic time."
One subgroup of patients who do benefit from decreased ischemic times, however, are those requiring complex multivalve procedures. Patients who have a poor ejection fraction also benefit.
"We are applying lessons that we’ve learned from TAVI to these sutureless valves," said Dr. Borger. "TAVI has been in Europe – transfemoral for 10 years, transapical for 6 years – and what we know from TAVI is that a stent is able to hold an aortic valve in the left ventricular outflow tract and prevent it from embolizing afterwards. In addition, we now know that you do not need to fully decalcify the annulus. As a matter of fact, you’re better off leaving some calcification in the annulus when implanting sutureless valves ... to avoid the formation of annular tears or defects."
There are two approaches: the upper hemisternotomy approach, which is favored in Leipzig, and the upper right midlateral thoracotomy approach.
Three sutureless valves are currently in use in Europe: the Medtronic (formerly ATS) Enable sutureless valve, the Sorin Perceval S sutureless valve, and the Edwards Intuity valve.
The Medtronic Enable valve is equine pericardium and was the first sutureless valve to get CE mark approval in Europe. The literature is limited, but a study from Switzerland (J. Thorac. Cardiovasc. Surg. 2010;140:313-6) of the 3f Enable valve in 28 patients showed that the valve could be implanted safely and quickly with favorable early hemodynamics.
"Again, I just want to stress, the goal is not to go from 60 minutes down to 40 minutes of ischemia; the goal is to facilitate a minimally invasive approach," said Dr. Borger. He noted that the hemodynamics were excellent for all three sutureless valves.
The second valve to receive CE mark approval in Europe was the Sorin Perceval S, at the beginning of 2012. It has a bovine pericardial leaflet, also attached to a Nitinol stent, and is crimped at the bedside. This results in an advantage for implantation.
"You can see exactly that the valve is in the position where you want it to be before deploying it," said Dr. Borger. The long-term results of crimping the leaflets are not yet known.
This particular model is currently available in sizes of 21, 23, and 25 mm. Even a 25-mm valve can only be put in a relatively small annulus, making the Perceval valve most appropriate for the small, elderly patient.
Sorin has reported results from 186 patients who received the Perceval valve, and noted short cross-clamp times (mean cross-clamp time for isolated AVR, 28.6 minutes) and 2.8% mortality.
The third and final sutureless aortic prosthesis is the Edwards Intuity valve, whose top is a traditional design based on the Magna Ease valve, and whose bottom is stent technology borrowed from Edwards’ TAVI program. A recent study of 152 patents revealed an average cross-clamp time of 41 minutes for isolated AVR, with a perioperative mortality rate of 2.1% and a paravalvular leak rate of 1.4% (J. Thorac. Cardiovasc. Surg. 2012;145:110-16). In addition, hemodynamics were excellent, with a mean transvalvular gradient of 9.8 mm Hg.
Dr. Borger disclosed receiving speaking honoraria from Edwards Lifesciences, Medtronic, and St. Jude Medical. He was a researcher in the Edwards Intuity and Sorin Perceval studies.
Leipzig Heart Center,
CHICAGO – European data suggest that minimally invasive aortic valve surgery has several benefits and few downsides when compared to conventional aortic valve replacement.
Bleeding is decreased, as is ICU and hospital length of stay. Cosmesis is improved. Sutureless valves may facilitate the performance of minimally invasive aortic valve replacement (AVR), and are associated with decreased ischemic times and lower transvalvular gradients – an advantage when concomitant procedures are performed or patients are high risk, according to a presentation at the 2012 Heart Valve summit.
Sutureless aortic valves facilitate minimal basic AVR and minimize myocardial ischemic time, said Dr. Michael Borger of Leipzig (Germany) Heart Center.
He described the evidence to date, as well as his personal experience, at this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
Leipzig Heart Center is one of Europe’s largest cardiac facilities, with 4,000 cardiac operations per year.
The number of patients who undergo minimally invasive aortic valve procedures is still very low, said Dr. Borger, and he urged the audience to consider this option in the future, especially when transcatheter aortic valve implantation (TAVI) becomes as widely accepted in America as it is in Europe. In Germany alone, 31% of isolated AVRs are now done by TAVI.
"Decreased myocardial ischemic time doesn’t matter for someone who needs an isolated aortic valve, [such as a] 70-year-old patient with no risk factors. It doesn’t matter if you shorten their ischemic time by 20 minutes. That’s not the point. The point is that a sutureless valve facilitates minimally invasive surgery by making it easier to do; and a marker for that is decreased ischemic time."
One subgroup of patients who do benefit from decreased ischemic times, however, are those requiring complex multivalve procedures. Patients who have a poor ejection fraction also benefit.
"We are applying lessons that we’ve learned from TAVI to these sutureless valves," said Dr. Borger. "TAVI has been in Europe – transfemoral for 10 years, transapical for 6 years – and what we know from TAVI is that a stent is able to hold an aortic valve in the left ventricular outflow tract and prevent it from embolizing afterwards. In addition, we now know that you do not need to fully decalcify the annulus. As a matter of fact, you’re better off leaving some calcification in the annulus when implanting sutureless valves ... to avoid the formation of annular tears or defects."
There are two approaches: the upper hemisternotomy approach, which is favored in Leipzig, and the upper right midlateral thoracotomy approach.
Three sutureless valves are currently in use in Europe: the Medtronic (formerly ATS) Enable sutureless valve, the Sorin Perceval S sutureless valve, and the Edwards Intuity valve.
The Medtronic Enable valve is equine pericardium and was the first sutureless valve to get CE mark approval in Europe. The literature is limited, but a study from Switzerland (J. Thorac. Cardiovasc. Surg. 2010;140:313-6) of the 3f Enable valve in 28 patients showed that the valve could be implanted safely and quickly with favorable early hemodynamics.
"Again, I just want to stress, the goal is not to go from 60 minutes down to 40 minutes of ischemia; the goal is to facilitate a minimally invasive approach," said Dr. Borger. He noted that the hemodynamics were excellent for all three sutureless valves.
The second valve to receive CE mark approval in Europe was the Sorin Perceval S, at the beginning of 2012. It has a bovine pericardial leaflet, also attached to a Nitinol stent, and is crimped at the bedside. This results in an advantage for implantation.
"You can see exactly that the valve is in the position where you want it to be before deploying it," said Dr. Borger. The long-term results of crimping the leaflets are not yet known.
This particular model is currently available in sizes of 21, 23, and 25 mm. Even a 25-mm valve can only be put in a relatively small annulus, making the Perceval valve most appropriate for the small, elderly patient.
Sorin has reported results from 186 patients who received the Perceval valve, and noted short cross-clamp times (mean cross-clamp time for isolated AVR, 28.6 minutes) and 2.8% mortality.
The third and final sutureless aortic prosthesis is the Edwards Intuity valve, whose top is a traditional design based on the Magna Ease valve, and whose bottom is stent technology borrowed from Edwards’ TAVI program. A recent study of 152 patents revealed an average cross-clamp time of 41 minutes for isolated AVR, with a perioperative mortality rate of 2.1% and a paravalvular leak rate of 1.4% (J. Thorac. Cardiovasc. Surg. 2012;145:110-16). In addition, hemodynamics were excellent, with a mean transvalvular gradient of 9.8 mm Hg.
Dr. Borger disclosed receiving speaking honoraria from Edwards Lifesciences, Medtronic, and St. Jude Medical. He was a researcher in the Edwards Intuity and Sorin Perceval studies.
CHICAGO – European data suggest that minimally invasive aortic valve surgery has several benefits and few downsides when compared to conventional aortic valve replacement.
Bleeding is decreased, as is ICU and hospital length of stay. Cosmesis is improved. Sutureless valves may facilitate the performance of minimally invasive aortic valve replacement (AVR), and are associated with decreased ischemic times and lower transvalvular gradients – an advantage when concomitant procedures are performed or patients are high risk, according to a presentation at the 2012 Heart Valve summit.
Sutureless aortic valves facilitate minimal basic AVR and minimize myocardial ischemic time, said Dr. Michael Borger of Leipzig (Germany) Heart Center.
He described the evidence to date, as well as his personal experience, at this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
Leipzig Heart Center is one of Europe’s largest cardiac facilities, with 4,000 cardiac operations per year.
The number of patients who undergo minimally invasive aortic valve procedures is still very low, said Dr. Borger, and he urged the audience to consider this option in the future, especially when transcatheter aortic valve implantation (TAVI) becomes as widely accepted in America as it is in Europe. In Germany alone, 31% of isolated AVRs are now done by TAVI.
"Decreased myocardial ischemic time doesn’t matter for someone who needs an isolated aortic valve, [such as a] 70-year-old patient with no risk factors. It doesn’t matter if you shorten their ischemic time by 20 minutes. That’s not the point. The point is that a sutureless valve facilitates minimally invasive surgery by making it easier to do; and a marker for that is decreased ischemic time."
One subgroup of patients who do benefit from decreased ischemic times, however, are those requiring complex multivalve procedures. Patients who have a poor ejection fraction also benefit.
"We are applying lessons that we’ve learned from TAVI to these sutureless valves," said Dr. Borger. "TAVI has been in Europe – transfemoral for 10 years, transapical for 6 years – and what we know from TAVI is that a stent is able to hold an aortic valve in the left ventricular outflow tract and prevent it from embolizing afterwards. In addition, we now know that you do not need to fully decalcify the annulus. As a matter of fact, you’re better off leaving some calcification in the annulus when implanting sutureless valves ... to avoid the formation of annular tears or defects."
There are two approaches: the upper hemisternotomy approach, which is favored in Leipzig, and the upper right midlateral thoracotomy approach.
Three sutureless valves are currently in use in Europe: the Medtronic (formerly ATS) Enable sutureless valve, the Sorin Perceval S sutureless valve, and the Edwards Intuity valve.
The Medtronic Enable valve is equine pericardium and was the first sutureless valve to get CE mark approval in Europe. The literature is limited, but a study from Switzerland (J. Thorac. Cardiovasc. Surg. 2010;140:313-6) of the 3f Enable valve in 28 patients showed that the valve could be implanted safely and quickly with favorable early hemodynamics.
"Again, I just want to stress, the goal is not to go from 60 minutes down to 40 minutes of ischemia; the goal is to facilitate a minimally invasive approach," said Dr. Borger. He noted that the hemodynamics were excellent for all three sutureless valves.
The second valve to receive CE mark approval in Europe was the Sorin Perceval S, at the beginning of 2012. It has a bovine pericardial leaflet, also attached to a Nitinol stent, and is crimped at the bedside. This results in an advantage for implantation.
"You can see exactly that the valve is in the position where you want it to be before deploying it," said Dr. Borger. The long-term results of crimping the leaflets are not yet known.
This particular model is currently available in sizes of 21, 23, and 25 mm. Even a 25-mm valve can only be put in a relatively small annulus, making the Perceval valve most appropriate for the small, elderly patient.
Sorin has reported results from 186 patients who received the Perceval valve, and noted short cross-clamp times (mean cross-clamp time for isolated AVR, 28.6 minutes) and 2.8% mortality.
The third and final sutureless aortic prosthesis is the Edwards Intuity valve, whose top is a traditional design based on the Magna Ease valve, and whose bottom is stent technology borrowed from Edwards’ TAVI program. A recent study of 152 patents revealed an average cross-clamp time of 41 minutes for isolated AVR, with a perioperative mortality rate of 2.1% and a paravalvular leak rate of 1.4% (J. Thorac. Cardiovasc. Surg. 2012;145:110-16). In addition, hemodynamics were excellent, with a mean transvalvular gradient of 9.8 mm Hg.
Dr. Borger disclosed receiving speaking honoraria from Edwards Lifesciences, Medtronic, and St. Jude Medical. He was a researcher in the Edwards Intuity and Sorin Perceval studies.
Leipzig Heart Center,
Leipzig Heart Center,
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2012
Progress Limited in Transcatheter Repair of Mitral Regurgitation
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
CHICAGO – Within narrow limits, transcatheter repair of mitral regurgitation can have outcomes meeting or even exceeding those of surgery.
"I believe that mitral regurgitation is mostly a surgical disease, but that interventional devices will, sooner or later, be able to manage some of the spectrum of mitral pathology," said Dr. Howard C. Herrmann at the Heart Valve Summit 2012. Dr. Herrmann is professor of medicine and director of interventional cardiology and cardiac catheterization at the University of Pennsylvania, Philadelphia.
"Transcatheter approaches are always going to be somewhat more limited than surgery," said Dr. Herrmann. The device that repairs a leaflet edge to edge is very different from the one that can be used to perform indirect annular dilatation via the coronary sinus, he noted.
Two devices relevant to those indications show promise, although neither is yet approved by the Food and Drug Administration (FDA), he said. These are Cardiac Dimensions’ Carillon for annular dilatation, and Abbott Vascular’s MitraClip for leaflet repair.
In the European TITAN clinical trial, 36 of 53 patients (68%) were implanted with the Carillon Mitral Contour System. The average baseline ejection fraction of all 53 patients was 28%, which Dr. Herrmann characterized as true functional mitral regurgitation (FMR). The prospective, nonrandomized, double-arm study compared results from the implanted group to results from a group without implants.
Implanted patients demonstrated significant reductions in FMR as assessed by multiple quantitative measures, including mean regurgitant volume, which decreased from 34.5 +/– 11.5 mL to 17.4 +/– 12.4 mL over 12 months (P less than .001) (Eur. J. Heart Fail. 2012;14:931-8).
These and other reductions correlated with symptomatic improvement, said Dr. Herrmann. However, the coronary sinus approach to percutaneous mitral annuloplasty is clearly limited by the variable anatomy between the coronary sinus and the posterior mitral annulus, as well as by the risk of coronary artery constriction, he said. Additionally, the long-term benefit of a surgical partial circumference ring is unknown (Circulation 2006;114:377-80).
The other device, the MitraClip, was evaluated in the EVEREST II trial for safety and efficacy in treatment of mitral valve regurgitation.
"Clearly, if you look at the primary effectiveness rate as defined by the trial, which is not a very high bar, surgery still beat the device," said Dr. Herrmann. However, he noted, the device clearly beat surgery in terms of morbidity and other safety end points.
"But when you look at it from an intent-to-treat analysis, those results are clearly inferior with MitraClip: At 2 years, 78.2% of percutaneous patients are free from mitral valve surgery, versus 96.1% of surgery patients (P less than .001).
"MitraClip should not and is not being used for low-risk patients with degenerative disease amenable to surgical repair. ... That said, in the patients who had good results with MitraClip, those results do appear to be fairly durable," he said. At 3 years, all-cause mortality was very similar between the two interventions. (J. Thorac. Cardiovasc. Surg. 2012;143:S60-3; J. Am. Coll. Cardiol. 2012;59:130-9).
Analysis of the high-surgical-risk cohort (n = 78) from EVEREST II revealed a 45% decrease in rehospitalizations (P = .02) at 12 months after intervention with MitraClip, said Dr. Herrmann. This finding led investigators to launch the COAPT trial, which has been approved by the FDA and is expected to start soon in the United States. Approximately 420 patients with significant FMR, thought to be at extremely high risk for surgery, will be randomized 1:1 to MitraClip (n = 210) or medical therapy (n = 210). The primary end point is a reduction in subsequent heart failure hospitalizations.
"This is truly a trial looking at palliative benefit, not mortality," he said.
He concluded by noting that several devices are under development, including others for leaflet repair, indirect annuloplasty, and direct annular or left ventricular remodeling; as well as direct LV shape-altering devices, transcatheter mitral valve replacement devices, and devices that mimic surgical ring annuloplasty.
The Heart Valve Summit was an educational program presented jointly by the American Association for Thoracic Surgery and the American College of Cardiology Foundation. Dr. Hermann has grant/research support from Abbott Vascular, Edwards Lifesciences, St. Jude Medical, Medtronic, and Gore, and has received consulting fees and honoraria from these and other device companies. His presentation was not sponsored.
EXPERT ANALYSIS FROM THE HEART VALVE SUMMIT 2012
What's New? The Changing Landscape of Infective Endocarditis
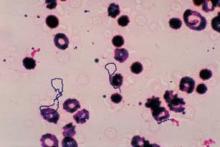
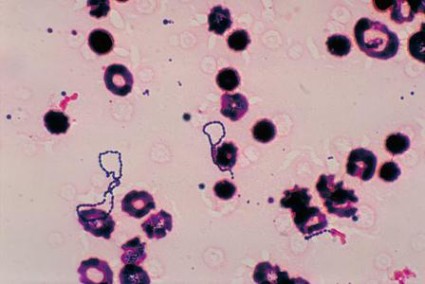
CHICAGO -- Mitral valve endocarditis is a medical-surgical problem that demands a team approach, and the landscape of the disease has changed significantly for the worst in the recent past, according to a presentation at Heart Valve Summit 2012.
"If you’re lucky enough to have a valve infection with the Strep viridans microorganism, you’re likely to do well," said Dr. Patrick T. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital, Boston.
On the other hand, patients who’ve been infected with any other type of organism, particularly Staph aureus or its increasingly frequent relative methicillin-resistant Staph aureus, could be in real trouble.
"There’s no question that these organisms are smarter than we are and can lead to destruction of the valve and death of the patient, despite our best intentions," said Dr. O’Gara. He described the evolving epidemiology, natural history, and indications for surgery for this disease to this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
"Unfortunately, despite our best efforts, and worldwide, among centers with an interest in the care of patients with endocarditis, 6-month mortality rates still approach 25%," he said. This is close to the mortality rate of a type A aortic dissection, so it is by no means trivial. Early surgery is now performed on many who present with the disease in early stages, and perioperative mortality is 12%-20%.
It is a challenge to manage a patient who is asymptomatic with respect to heart failure but who has a large mobile vegetation involving the anterior mitral leaflet, said Dr. O’Gara. Vegetations in this location are the most prone to embolize.
"This is the common question now posed to consulting cardiologists: Does my patient require early surgery for prevention of embolic complications? We don’t really get asked too much any more: ‘Does my patient need early surgery because they’ve developed heart failure?’ I guess we’re much more confident in proceeding under those circumstances."
He discussed considerations for surgery, including the level of local surgical expertise. The intervention is complex and delicate. "This is not something for the faint of heart," said Dr. O’Gara.
In the early time frame following presentation, there is a relationship between the size of the vegetation and the risk of embolization.
The risk of stroke drops rapidly after initiation of antimicrobial therapy. Patients who develop stroke as a complication of endocarditis typically do so the day before, the day of, or the day after presentation, he said. Stroke risk continues to drop quickly in the first 2 weeks after initiation of antibiotics, and by week 5 it’s almost nil.
"If you’re thinking about intervention for prevention of stroke, it makes sense to do so in the first week, after identification of a patient at risk with a large mobile vegetation. It makes much less sense to do so in weeks 2 or 3."
The size of the vegetation alone may dictate mortality. A size of 1.5 cm or greater is associated with increased risk of death at 1 year in the setting of native valve endocarditis.
The good news is that event-free survival rates have been shown to be much better for those who undergo surgery in the first 7 days after presentation with high-risk native, left-sided endocarditis. In-hospital mortality as a function of early surgery appears to have declined over the course of time.
"So, in summary, I think for our management considerations, it’s early diagnosis, risk stratification, a heart team approach, consider early surgery, particularly if you have the operative expertise. The early risk of re-infection in implanted prosthetic material is very low," Dr. O’Gara said.
Dr. O’Gara disclosed ties with the Data Safety Monitoring Board and Lantheus Medical Imaging.
CHICAGO -- Mitral valve endocarditis is a medical-surgical problem that demands a team approach, and the landscape of the disease has changed significantly for the worst in the recent past, according to a presentation at Heart Valve Summit 2012.
"If you’re lucky enough to have a valve infection with the Strep viridans microorganism, you’re likely to do well," said Dr. Patrick T. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital, Boston.
On the other hand, patients who’ve been infected with any other type of organism, particularly Staph aureus or its increasingly frequent relative methicillin-resistant Staph aureus, could be in real trouble.
"There’s no question that these organisms are smarter than we are and can lead to destruction of the valve and death of the patient, despite our best intentions," said Dr. O’Gara. He described the evolving epidemiology, natural history, and indications for surgery for this disease to this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
"Unfortunately, despite our best efforts, and worldwide, among centers with an interest in the care of patients with endocarditis, 6-month mortality rates still approach 25%," he said. This is close to the mortality rate of a type A aortic dissection, so it is by no means trivial. Early surgery is now performed on many who present with the disease in early stages, and perioperative mortality is 12%-20%.
It is a challenge to manage a patient who is asymptomatic with respect to heart failure but who has a large mobile vegetation involving the anterior mitral leaflet, said Dr. O’Gara. Vegetations in this location are the most prone to embolize.
"This is the common question now posed to consulting cardiologists: Does my patient require early surgery for prevention of embolic complications? We don’t really get asked too much any more: ‘Does my patient need early surgery because they’ve developed heart failure?’ I guess we’re much more confident in proceeding under those circumstances."
He discussed considerations for surgery, including the level of local surgical expertise. The intervention is complex and delicate. "This is not something for the faint of heart," said Dr. O’Gara.
In the early time frame following presentation, there is a relationship between the size of the vegetation and the risk of embolization.
The risk of stroke drops rapidly after initiation of antimicrobial therapy. Patients who develop stroke as a complication of endocarditis typically do so the day before, the day of, or the day after presentation, he said. Stroke risk continues to drop quickly in the first 2 weeks after initiation of antibiotics, and by week 5 it’s almost nil.
"If you’re thinking about intervention for prevention of stroke, it makes sense to do so in the first week, after identification of a patient at risk with a large mobile vegetation. It makes much less sense to do so in weeks 2 or 3."
The size of the vegetation alone may dictate mortality. A size of 1.5 cm or greater is associated with increased risk of death at 1 year in the setting of native valve endocarditis.
The good news is that event-free survival rates have been shown to be much better for those who undergo surgery in the first 7 days after presentation with high-risk native, left-sided endocarditis. In-hospital mortality as a function of early surgery appears to have declined over the course of time.
"So, in summary, I think for our management considerations, it’s early diagnosis, risk stratification, a heart team approach, consider early surgery, particularly if you have the operative expertise. The early risk of re-infection in implanted prosthetic material is very low," Dr. O’Gara said.
Dr. O’Gara disclosed ties with the Data Safety Monitoring Board and Lantheus Medical Imaging.
CHICAGO -- Mitral valve endocarditis is a medical-surgical problem that demands a team approach, and the landscape of the disease has changed significantly for the worst in the recent past, according to a presentation at Heart Valve Summit 2012.
"If you’re lucky enough to have a valve infection with the Strep viridans microorganism, you’re likely to do well," said Dr. Patrick T. O’Gara, director of clinical cardiology at Brigham and Women’s Hospital, Boston.
On the other hand, patients who’ve been infected with any other type of organism, particularly Staph aureus or its increasingly frequent relative methicillin-resistant Staph aureus, could be in real trouble.
"There’s no question that these organisms are smarter than we are and can lead to destruction of the valve and death of the patient, despite our best intentions," said Dr. O’Gara. He described the evolving epidemiology, natural history, and indications for surgery for this disease to this educational program of the American Association for Thoracic Surgery (AATS) and the American College of Cardiology Foundation (ACCF).
"Unfortunately, despite our best efforts, and worldwide, among centers with an interest in the care of patients with endocarditis, 6-month mortality rates still approach 25%," he said. This is close to the mortality rate of a type A aortic dissection, so it is by no means trivial. Early surgery is now performed on many who present with the disease in early stages, and perioperative mortality is 12%-20%.
It is a challenge to manage a patient who is asymptomatic with respect to heart failure but who has a large mobile vegetation involving the anterior mitral leaflet, said Dr. O’Gara. Vegetations in this location are the most prone to embolize.
"This is the common question now posed to consulting cardiologists: Does my patient require early surgery for prevention of embolic complications? We don’t really get asked too much any more: ‘Does my patient need early surgery because they’ve developed heart failure?’ I guess we’re much more confident in proceeding under those circumstances."
He discussed considerations for surgery, including the level of local surgical expertise. The intervention is complex and delicate. "This is not something for the faint of heart," said Dr. O’Gara.
In the early time frame following presentation, there is a relationship between the size of the vegetation and the risk of embolization.
The risk of stroke drops rapidly after initiation of antimicrobial therapy. Patients who develop stroke as a complication of endocarditis typically do so the day before, the day of, or the day after presentation, he said. Stroke risk continues to drop quickly in the first 2 weeks after initiation of antibiotics, and by week 5 it’s almost nil.
"If you’re thinking about intervention for prevention of stroke, it makes sense to do so in the first week, after identification of a patient at risk with a large mobile vegetation. It makes much less sense to do so in weeks 2 or 3."
The size of the vegetation alone may dictate mortality. A size of 1.5 cm or greater is associated with increased risk of death at 1 year in the setting of native valve endocarditis.
The good news is that event-free survival rates have been shown to be much better for those who undergo surgery in the first 7 days after presentation with high-risk native, left-sided endocarditis. In-hospital mortality as a function of early surgery appears to have declined over the course of time.
"So, in summary, I think for our management considerations, it’s early diagnosis, risk stratification, a heart team approach, consider early surgery, particularly if you have the operative expertise. The early risk of re-infection in implanted prosthetic material is very low," Dr. O’Gara said.
Dr. O’Gara disclosed ties with the Data Safety Monitoring Board and Lantheus Medical Imaging.
EXPERT ANALYSIS FROM HEART VALVE SUMMIT 2012