User login
Breast cancer treatment linked to mild systolic dysfunction
AMSTERDAM – Breast cancer patients who underwent chemotherapy or radiotherapy had about a two-fold increased prevalence of mild systolic cardiac dysfunction a median of 10 years after treatment, compared with age-matched controls in a study that included a total of 700 people.
But even longer follow-up of treated breast cancer patients is needed to determine whether the excess mild cardiac dysfunction seen in this analysis eventually progresses to more severe cardiac impairment, Liselotte M. Boerman said at the European Breast Cancer Conference.
Data from the Breast Cancer Long-term Outcome of Cardiac Dysfunction (BLOC) study showed that 175 breast cancer patients who received chemotherapy (and may have also received radiotherapy) had a 2.5-fold higher prevalence of a left ventricular ejection fraction (LVEF) below 54% (95% confidence interval, 1.2-5.4) when measured by echocardiography a median of 10 years after treatment, compared with an equal number of age-matched individuals from the general population.
A separate group of 175 patients treated with radiotherapy only and evaluated by echocardiography a median of 10 years later had a 2.3-fold increased prevalence (1.1-4.7) of a LVEF below 54% when compared with an equal number of age-matched individuals, said Ms. Boerman, an epidemiology researcher at the University of Groningen (the Netherlands).
This degree of left-ventricular dysfunction was found in 15% of the chemotherapy patients and 6% of their controls, and in 16% of the radiotherapy patients and 8% of their controls.
However, the treated breast cancer patients had no long-term increase in their prevalence of more significant systolic cardiac dysfunction, defined as a LVEF of less than 45%, compared with the controls, and the overall rate of systolic dysfunction of this severity was low, affecting fewer than 1% of patients.
Also, the chemotherapy and radiotherapy patients showed no significant increase in the prevalence of diastolic cardiac dysfunction, defined as delayed cardiac relaxation beyond the age-appropriate range. Treated patients did show, after 10 years, a suggestion of an increased prevalence of diagnosed cardiovascular disease, which was 2.3-fold higher (1.0-4.9) in the chemotherapy-receiving patients, compared with their controls; and 70% higher (0.9-3.4) among the patients treated with radiotherapy, compared with their controls, Ms. Boerman said.
The study used data collected from breast cancer patients younger than 80 years old treated after 1980 and controls seen by general practice Dutch physicians. The chemotherapy patients were diagnosed at an average age of 49 years old (range 26-66 years old). About 78% had received treatment with an anthracycline agent and 7% had received trastuzumab (Herceptin). Radiotherapy had also been administered to 70%, while 62% had also received hormonal therapy, and 7% either had a recurrence or developed a tumor in their contralateral breast.
None of the radiotherapy-only patients had received chemotherapy, but 21% had also received hormonal therapy. Their average age at diagnosis was 54 years old (range 32-79 years old), and 10% had a recurrence or a contralateral tumor.
Follow-up echocardiography occurred 5-34 years after the index treatment, at a median age of 60 years old. Echocardiography follow-up occurred in 70% of the chemotherapy breast cancer patients contacted, and in 63% of those who received radiotherapy only. Among controls, about half of those selected by age matching, and contacted, agreed to participate.
Rates of cardiovascular-disease risk factors – dyslipidemia, hypertension, and diabetes – were at roughly similar levels in the cases and controls at the time of breast cancer diagnosis. But the rate of current smoking at the time of diagnosis appeared higher in the cases (30% among those who received chemotherapy and 33% among those on radiotherapy), compared with their respective control groups (22% and 30%). Ms. Boerman said that a multivariate analysis had not yet been run on the data but should occur soon.
“The prevalence of cardiac dysfunction was higher [in treated patients] than I would have expected, but there is potential bias as only 70% of invited patients actually participated,” commented Dr. Robert Mansel, a professor at the Institute of Cancer & Genetics at Cardiff University (Wales). He also noted the very low rate of patients who developed severe cardiac dysfunction.
Ms. Boerman and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – Breast cancer patients who underwent chemotherapy or radiotherapy had about a two-fold increased prevalence of mild systolic cardiac dysfunction a median of 10 years after treatment, compared with age-matched controls in a study that included a total of 700 people.
But even longer follow-up of treated breast cancer patients is needed to determine whether the excess mild cardiac dysfunction seen in this analysis eventually progresses to more severe cardiac impairment, Liselotte M. Boerman said at the European Breast Cancer Conference.
Data from the Breast Cancer Long-term Outcome of Cardiac Dysfunction (BLOC) study showed that 175 breast cancer patients who received chemotherapy (and may have also received radiotherapy) had a 2.5-fold higher prevalence of a left ventricular ejection fraction (LVEF) below 54% (95% confidence interval, 1.2-5.4) when measured by echocardiography a median of 10 years after treatment, compared with an equal number of age-matched individuals from the general population.
A separate group of 175 patients treated with radiotherapy only and evaluated by echocardiography a median of 10 years later had a 2.3-fold increased prevalence (1.1-4.7) of a LVEF below 54% when compared with an equal number of age-matched individuals, said Ms. Boerman, an epidemiology researcher at the University of Groningen (the Netherlands).
This degree of left-ventricular dysfunction was found in 15% of the chemotherapy patients and 6% of their controls, and in 16% of the radiotherapy patients and 8% of their controls.
However, the treated breast cancer patients had no long-term increase in their prevalence of more significant systolic cardiac dysfunction, defined as a LVEF of less than 45%, compared with the controls, and the overall rate of systolic dysfunction of this severity was low, affecting fewer than 1% of patients.
Also, the chemotherapy and radiotherapy patients showed no significant increase in the prevalence of diastolic cardiac dysfunction, defined as delayed cardiac relaxation beyond the age-appropriate range. Treated patients did show, after 10 years, a suggestion of an increased prevalence of diagnosed cardiovascular disease, which was 2.3-fold higher (1.0-4.9) in the chemotherapy-receiving patients, compared with their controls; and 70% higher (0.9-3.4) among the patients treated with radiotherapy, compared with their controls, Ms. Boerman said.
The study used data collected from breast cancer patients younger than 80 years old treated after 1980 and controls seen by general practice Dutch physicians. The chemotherapy patients were diagnosed at an average age of 49 years old (range 26-66 years old). About 78% had received treatment with an anthracycline agent and 7% had received trastuzumab (Herceptin). Radiotherapy had also been administered to 70%, while 62% had also received hormonal therapy, and 7% either had a recurrence or developed a tumor in their contralateral breast.
None of the radiotherapy-only patients had received chemotherapy, but 21% had also received hormonal therapy. Their average age at diagnosis was 54 years old (range 32-79 years old), and 10% had a recurrence or a contralateral tumor.
Follow-up echocardiography occurred 5-34 years after the index treatment, at a median age of 60 years old. Echocardiography follow-up occurred in 70% of the chemotherapy breast cancer patients contacted, and in 63% of those who received radiotherapy only. Among controls, about half of those selected by age matching, and contacted, agreed to participate.
Rates of cardiovascular-disease risk factors – dyslipidemia, hypertension, and diabetes – were at roughly similar levels in the cases and controls at the time of breast cancer diagnosis. But the rate of current smoking at the time of diagnosis appeared higher in the cases (30% among those who received chemotherapy and 33% among those on radiotherapy), compared with their respective control groups (22% and 30%). Ms. Boerman said that a multivariate analysis had not yet been run on the data but should occur soon.
“The prevalence of cardiac dysfunction was higher [in treated patients] than I would have expected, but there is potential bias as only 70% of invited patients actually participated,” commented Dr. Robert Mansel, a professor at the Institute of Cancer & Genetics at Cardiff University (Wales). He also noted the very low rate of patients who developed severe cardiac dysfunction.
Ms. Boerman and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – Breast cancer patients who underwent chemotherapy or radiotherapy had about a two-fold increased prevalence of mild systolic cardiac dysfunction a median of 10 years after treatment, compared with age-matched controls in a study that included a total of 700 people.
But even longer follow-up of treated breast cancer patients is needed to determine whether the excess mild cardiac dysfunction seen in this analysis eventually progresses to more severe cardiac impairment, Liselotte M. Boerman said at the European Breast Cancer Conference.
Data from the Breast Cancer Long-term Outcome of Cardiac Dysfunction (BLOC) study showed that 175 breast cancer patients who received chemotherapy (and may have also received radiotherapy) had a 2.5-fold higher prevalence of a left ventricular ejection fraction (LVEF) below 54% (95% confidence interval, 1.2-5.4) when measured by echocardiography a median of 10 years after treatment, compared with an equal number of age-matched individuals from the general population.
A separate group of 175 patients treated with radiotherapy only and evaluated by echocardiography a median of 10 years later had a 2.3-fold increased prevalence (1.1-4.7) of a LVEF below 54% when compared with an equal number of age-matched individuals, said Ms. Boerman, an epidemiology researcher at the University of Groningen (the Netherlands).
This degree of left-ventricular dysfunction was found in 15% of the chemotherapy patients and 6% of their controls, and in 16% of the radiotherapy patients and 8% of their controls.
However, the treated breast cancer patients had no long-term increase in their prevalence of more significant systolic cardiac dysfunction, defined as a LVEF of less than 45%, compared with the controls, and the overall rate of systolic dysfunction of this severity was low, affecting fewer than 1% of patients.
Also, the chemotherapy and radiotherapy patients showed no significant increase in the prevalence of diastolic cardiac dysfunction, defined as delayed cardiac relaxation beyond the age-appropriate range. Treated patients did show, after 10 years, a suggestion of an increased prevalence of diagnosed cardiovascular disease, which was 2.3-fold higher (1.0-4.9) in the chemotherapy-receiving patients, compared with their controls; and 70% higher (0.9-3.4) among the patients treated with radiotherapy, compared with their controls, Ms. Boerman said.
The study used data collected from breast cancer patients younger than 80 years old treated after 1980 and controls seen by general practice Dutch physicians. The chemotherapy patients were diagnosed at an average age of 49 years old (range 26-66 years old). About 78% had received treatment with an anthracycline agent and 7% had received trastuzumab (Herceptin). Radiotherapy had also been administered to 70%, while 62% had also received hormonal therapy, and 7% either had a recurrence or developed a tumor in their contralateral breast.
None of the radiotherapy-only patients had received chemotherapy, but 21% had also received hormonal therapy. Their average age at diagnosis was 54 years old (range 32-79 years old), and 10% had a recurrence or a contralateral tumor.
Follow-up echocardiography occurred 5-34 years after the index treatment, at a median age of 60 years old. Echocardiography follow-up occurred in 70% of the chemotherapy breast cancer patients contacted, and in 63% of those who received radiotherapy only. Among controls, about half of those selected by age matching, and contacted, agreed to participate.
Rates of cardiovascular-disease risk factors – dyslipidemia, hypertension, and diabetes – were at roughly similar levels in the cases and controls at the time of breast cancer diagnosis. But the rate of current smoking at the time of diagnosis appeared higher in the cases (30% among those who received chemotherapy and 33% among those on radiotherapy), compared with their respective control groups (22% and 30%). Ms. Boerman said that a multivariate analysis had not yet been run on the data but should occur soon.
“The prevalence of cardiac dysfunction was higher [in treated patients] than I would have expected, but there is potential bias as only 70% of invited patients actually participated,” commented Dr. Robert Mansel, a professor at the Institute of Cancer & Genetics at Cardiff University (Wales). He also noted the very low rate of patients who developed severe cardiac dysfunction.
Ms. Boerman and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AT EBCC10
Key clinical point: Breast cancer patients treated with chemotherapy or radiotherapy showed a doubled rate of mild left-ventricular dysfunction, compared with matched controls 10 years after treatment.
Major finding: Mildly reduced left-ventricular function occurred in 15% of post-chemotherapy patients, compared with 6% of controls.
Data source: Echocardiography examinations conducted on 350 Dutch breast cancer patients and an equal number of age-matched controls.
Disclosures: Ms. Boerman and Dr. Mansel reported having no financial disclosures.
Phone monitoring program helps cut chemotherapy symptom severity
AMSTERDAM – A telephone-based system to monitor chemotherapy-induced symptoms when patients are home and facilitate interventions as needed led to significant cuts in symptom burden in a single-center, randomized trial with 152 breast cancer patients.
“Symptom care at home gives patients symptom care when and where they need it,” Kathi H. Mooney, Ph.D., said at the European Breast Cancer Conference. “Rarely is symptom monitoring extended to when patients are home, but that is when symptoms are most problematic for patients.”
The 30-day program was linked with significant cuts in the number of days with any of seven chemotherapy-induced symptoms. In addition, overall days with any severe symptom fell by 48% (P = .006) and the number of days with any moderate symptoms fell by 38% (P = .011), reported Dr. Mooney, professor of nursing at the University of Utah, Salt Lake City.
She and her associates designed a telephone-based system to address the usual reticence that chemotherapy patients have to report their symptoms. Prior study results had documented that patients with moderate or severe symptoms initiated calls for about 5% of episodes, even when explicitly told to report symptoms. This led the Utah researchers to develop an automated, interactive system that phoned patients daily.
The enrolled patients spanned the full spectrum of breast cancer stages; the average age was 53 years. All patients received a daily, automated call that prompted them to rate each of 11 chemotherapy symptoms on a scale of 0-10.
The calls also provided automated, self-management coaching for problematic symptoms. The investigational Symptom Care at Home intervention involved a nurse practitioner getting back to patients who reported poorly-controlled symptoms. These follow-up calls averaged just under 7 minutes in length, and on average each patient received 11 calls during the 30 days of the intervention.
After 30 days, the 83 patients in the Symptom Care at Home program had statistically-significant reductions in days with moderate or worse episodes for 7 of the 11 symptoms tallied: numbness or tingling, anxiety, nausea, pain, depressed mood, sore mouth, and fatigue. The most robust effects were a 72% drop in days with moderate or worse numbness or tingling, a 66% reduction in anxiety days, and a 61% cut in nausea days.
“I like the intervention used in this study. I think it shows what can happen when you collect symptom information in a way that is patient friendly,” said Dr. Robert Mansel, professor at the Institute of Cancer & Genetics at Cardiff University, South Wales. “I was delighted to see that this intervention really made a difference. The findings show that patients often suffer a lot more from treatment than they are usually prepared to tell us.”
In addition to the efficacy of this intervention, “patients told us that they liked having someone to talk with about their symptoms,” Dr. Mooney said in an interview. “Patients are concerned about their symptoms.”
One aspect of the Symptom Care at Home program that has not yet been analyzed is its cost efficacy. The University of Utah’s Huntsman Cancer Institute, where the program was developed, is awaiting results from a cost-benefit analysis before deciding whether to make the telephone system part of routine practice, she said.
Dr. Mooney and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – A telephone-based system to monitor chemotherapy-induced symptoms when patients are home and facilitate interventions as needed led to significant cuts in symptom burden in a single-center, randomized trial with 152 breast cancer patients.
“Symptom care at home gives patients symptom care when and where they need it,” Kathi H. Mooney, Ph.D., said at the European Breast Cancer Conference. “Rarely is symptom monitoring extended to when patients are home, but that is when symptoms are most problematic for patients.”
The 30-day program was linked with significant cuts in the number of days with any of seven chemotherapy-induced symptoms. In addition, overall days with any severe symptom fell by 48% (P = .006) and the number of days with any moderate symptoms fell by 38% (P = .011), reported Dr. Mooney, professor of nursing at the University of Utah, Salt Lake City.
She and her associates designed a telephone-based system to address the usual reticence that chemotherapy patients have to report their symptoms. Prior study results had documented that patients with moderate or severe symptoms initiated calls for about 5% of episodes, even when explicitly told to report symptoms. This led the Utah researchers to develop an automated, interactive system that phoned patients daily.
The enrolled patients spanned the full spectrum of breast cancer stages; the average age was 53 years. All patients received a daily, automated call that prompted them to rate each of 11 chemotherapy symptoms on a scale of 0-10.
The calls also provided automated, self-management coaching for problematic symptoms. The investigational Symptom Care at Home intervention involved a nurse practitioner getting back to patients who reported poorly-controlled symptoms. These follow-up calls averaged just under 7 minutes in length, and on average each patient received 11 calls during the 30 days of the intervention.
After 30 days, the 83 patients in the Symptom Care at Home program had statistically-significant reductions in days with moderate or worse episodes for 7 of the 11 symptoms tallied: numbness or tingling, anxiety, nausea, pain, depressed mood, sore mouth, and fatigue. The most robust effects were a 72% drop in days with moderate or worse numbness or tingling, a 66% reduction in anxiety days, and a 61% cut in nausea days.
“I like the intervention used in this study. I think it shows what can happen when you collect symptom information in a way that is patient friendly,” said Dr. Robert Mansel, professor at the Institute of Cancer & Genetics at Cardiff University, South Wales. “I was delighted to see that this intervention really made a difference. The findings show that patients often suffer a lot more from treatment than they are usually prepared to tell us.”
In addition to the efficacy of this intervention, “patients told us that they liked having someone to talk with about their symptoms,” Dr. Mooney said in an interview. “Patients are concerned about their symptoms.”
One aspect of the Symptom Care at Home program that has not yet been analyzed is its cost efficacy. The University of Utah’s Huntsman Cancer Institute, where the program was developed, is awaiting results from a cost-benefit analysis before deciding whether to make the telephone system part of routine practice, she said.
Dr. Mooney and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AMSTERDAM – A telephone-based system to monitor chemotherapy-induced symptoms when patients are home and facilitate interventions as needed led to significant cuts in symptom burden in a single-center, randomized trial with 152 breast cancer patients.
“Symptom care at home gives patients symptom care when and where they need it,” Kathi H. Mooney, Ph.D., said at the European Breast Cancer Conference. “Rarely is symptom monitoring extended to when patients are home, but that is when symptoms are most problematic for patients.”
The 30-day program was linked with significant cuts in the number of days with any of seven chemotherapy-induced symptoms. In addition, overall days with any severe symptom fell by 48% (P = .006) and the number of days with any moderate symptoms fell by 38% (P = .011), reported Dr. Mooney, professor of nursing at the University of Utah, Salt Lake City.
She and her associates designed a telephone-based system to address the usual reticence that chemotherapy patients have to report their symptoms. Prior study results had documented that patients with moderate or severe symptoms initiated calls for about 5% of episodes, even when explicitly told to report symptoms. This led the Utah researchers to develop an automated, interactive system that phoned patients daily.
The enrolled patients spanned the full spectrum of breast cancer stages; the average age was 53 years. All patients received a daily, automated call that prompted them to rate each of 11 chemotherapy symptoms on a scale of 0-10.
The calls also provided automated, self-management coaching for problematic symptoms. The investigational Symptom Care at Home intervention involved a nurse practitioner getting back to patients who reported poorly-controlled symptoms. These follow-up calls averaged just under 7 minutes in length, and on average each patient received 11 calls during the 30 days of the intervention.
After 30 days, the 83 patients in the Symptom Care at Home program had statistically-significant reductions in days with moderate or worse episodes for 7 of the 11 symptoms tallied: numbness or tingling, anxiety, nausea, pain, depressed mood, sore mouth, and fatigue. The most robust effects were a 72% drop in days with moderate or worse numbness or tingling, a 66% reduction in anxiety days, and a 61% cut in nausea days.
“I like the intervention used in this study. I think it shows what can happen when you collect symptom information in a way that is patient friendly,” said Dr. Robert Mansel, professor at the Institute of Cancer & Genetics at Cardiff University, South Wales. “I was delighted to see that this intervention really made a difference. The findings show that patients often suffer a lot more from treatment than they are usually prepared to tell us.”
In addition to the efficacy of this intervention, “patients told us that they liked having someone to talk with about their symptoms,” Dr. Mooney said in an interview. “Patients are concerned about their symptoms.”
One aspect of the Symptom Care at Home program that has not yet been analyzed is its cost efficacy. The University of Utah’s Huntsman Cancer Institute, where the program was developed, is awaiting results from a cost-benefit analysis before deciding whether to make the telephone system part of routine practice, she said.
Dr. Mooney and Dr. Mansel reported having no financial disclosures.
On Twitter @mitchelzoler
AT EBCC 10
VIDEO: Trastuzumab plus lapatinib erases selected breast cancers
AMSTERDAM – An unexpectedly dramatic benefit from combining trastuzumab and lapatinib when briefly treating women scheduled for breast cancer surgery has researchers focused on the best follow-up study to this promising but preliminary finding from 66 patients.
Among 66 patients with newly diagnosed HER2-positive breast cancer and scheduled for surgery, an average 11 days of treatment with a combination of trastuzumab (Herceptin) and lapatinib (Tykerb) during the period before surgery resulted in a pathologic complete response (pCR) in seven patients (11%) and 11 patients (17%) with minimal residual disease (MRD), Dr. Nigel Bundred reported at the European Breast Cancer Conference.
These patients had breast cancer tumors at baseline with a median diameter of 2 cm that with treatment for not quite 2 weeks resulted in either complete tumor disappearance or shrinkage to less than 5 mm in diameter in 18 (27%) of the patients on dual therapy, said Dr. Bundred, a professor of surgical oncology at the University Hospital of South Manchester (England).
“No cancer has ever disappeared that fast. It was flabbergasting,” Dr. Bundred said in an interview. “We need to confirm the results, and get larger numbers of patients.”
“This was a really surprising finding,” said Judith M. Bliss, professor and director of the Clinical Trials & Statistics unit of the Institute of Cancer Research in London and a co-investigator. “We knew that trastuzumab and lapatinib are effective treatments, but we had not expected to see such a dramatic effect on the structure and size of the tumor in such a short period of time,” Prof. Bliss said in a video interview.
The finding came as part of the Effect of Perioperative Anti-HER2 Therapy on Overall Survival–Biologic Phase (EPHOS-B) trial, designed to assess changes in a marker of cell proliferation (Ki67) and in a marker of cell apoptosis in relation to treatment with trastuzumab, lapatinib, or both when administered during the 10-12 days from the time patients entered the study until their scheduled surgery.
During the first phase of EPHOS-B, when 130 patients received trastuzumab monotherapy, lapatinib monotherapy, or neither, one of the 57 patients on trastuzumab (2%) had a pathologic complete response and one patient (2%) had minimal residual disease. No patients on lapatinib alone or in the control arm with no anti-HER2 drug had this sort of response.
During the second phase, 127 patients received trastuzumab alone, trastuzumab plus lapatinib in combination, or controls who received no anti-HER2 treatment. The substantial number of complete or partial responders in the 66 patients who received combined treatment with trastuzumab and lapatinib contrasted with one minimal residual disease among 32 patients (3%) who received trastuzumab alone and no responders among the 29 controls.
Patients receiving trastuzumab, alone or in the combined regimen, received a standard intravenous loading dosage of 6 mg/kg on days 1 and 8 after entry into the protocol, followed by a third dose after surgery on days 15-19; those also receiving lapatinib received 1 g/day orally for 28 days starting on entry.
“A quarter of the patients seem exquisitely sensitive to the combination of trastuzumab and lapatinib,” said Dr. David Cameron, another collaborator on the EPHOS-B study. “It’s pretty unusual to treat for 10-12 days and have 10% of the tumors disappear.”
Follow-up studies will be needed to determine whether patients with a pathologic complete response or minimal residual disease can forgo some or all of the chemotherapy that would usually follow surgery and still have good long-term disease-free survival. “We will focus on optimizing the short-term effect, and then modulate subsequent treatments,” said Dr. Cameron, professor and clinical director of oncology at the University of Edinburgh.
“We think these are patients who don’t need chemotherapy and are particularly sensitive to anti-HER2 drugs,” but so far that hasn’t been proven, cautioned Ms. Bliss.
The striking efficacy of trastuzumab combined with lapatinib in these 66 patients contrasts with the previously reported results from the ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) study, which failed to show an advantage in disease-free survival with trastuzumab plus lapatinib, compared with either of these two agents used individually during 1 year of adjuvant treatment in more than 8,000 randomized patients (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), But the EPHOS-B results did agree with results from the much smaller NeoALTTO study, which showed in a randomized, multicenter, phase III study with 455 patients a significant incremental increase in pathologic complete response rate in patients on combined trastuzumab plus lapatinib, compared with patients on either drug alone (Lancet. 2012;379 [9816]:633-40).
Another promising finding from EPHOS-B was that among the 64 patients who had their left ventricular ejection fraction assessed prior to the second phase, none of 32 patients on the combined regimen showed signs of cardiotoxicity with a reduced ejection fraction following treatment, Dr. Bundred reported.
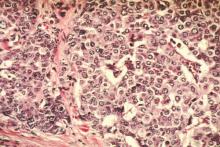
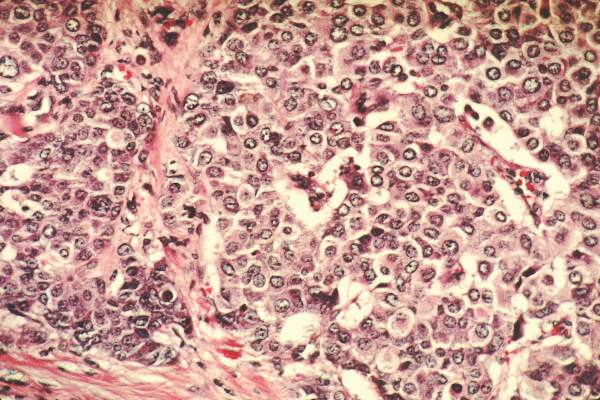
Until now, not much was known about the beneficial mechanisms of anti-HER2 drugs, he noted. The results from EPHOS-B “tell us that combined treatment does more than just shut down cell replication. It might be that trastuzumab induces an immune response.” The former tumor beds of patients with pathologic complete response as well as regions with minimal residual disease showed large numbers of tumor infiltrating lymphocytes, a sign of a robust immune response.
Trastuzumab and lapatinib work by different mechanisms, Dr. Bundred stressed. “The only way you can combine drugs is by understanding their mechanisms. We’re still looking for the mechanisms of the anti-HER2 drugs.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
The significant proportion of patients treated with trastuzumab plus lapatinib for about 11 days who developed a pathologic complete response or minimal residual disease was largely unexpected.
The finding raises questions: Can we identify patients after 11 days of treatment who are good responders to this combined treatment and will have an excellent relapse-free survival without ongoing combination anti-HER2 treatment or anti-HER2 escalation, and who will be eligible for chemotherapy de-escalation similar to the regimen tested by Tolaney and her associates (N Engl J Med. 2015 Jan;372:134-41)?
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Hervé Bonnefoi |
We clearly need more data on the impact of the combined anti-HER2 regimen on the rate of long-term, relapse-free survival, and data from many more patients treated with a combined anti-HER2 regimen. The EPHOS-B results seem to contradict the results of the ALTTO study (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), but they confirm results of the NeoALTTO study, a randomized, multicenter, phase III study with 455 patients (Lancet. 2012 Jan;379[9816]:633-40).
The EPHOS-B researchers modeled their study after the presurgical treatment studies run using hormonal therapies. The results from studies of anti-HER2 treatments during this presurgical time window have been much harder to interpret.
Dr. Hervé Bonnefoi is a professor of medical oncology at Bordeaux University (France). He reported having no financial disclosures. He made these comments as the designated discussant for the EPHOS-B study.
The significant proportion of patients treated with trastuzumab plus lapatinib for about 11 days who developed a pathologic complete response or minimal residual disease was largely unexpected.
The finding raises questions: Can we identify patients after 11 days of treatment who are good responders to this combined treatment and will have an excellent relapse-free survival without ongoing combination anti-HER2 treatment or anti-HER2 escalation, and who will be eligible for chemotherapy de-escalation similar to the regimen tested by Tolaney and her associates (N Engl J Med. 2015 Jan;372:134-41)?
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Hervé Bonnefoi |
We clearly need more data on the impact of the combined anti-HER2 regimen on the rate of long-term, relapse-free survival, and data from many more patients treated with a combined anti-HER2 regimen. The EPHOS-B results seem to contradict the results of the ALTTO study (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), but they confirm results of the NeoALTTO study, a randomized, multicenter, phase III study with 455 patients (Lancet. 2012 Jan;379[9816]:633-40).
The EPHOS-B researchers modeled their study after the presurgical treatment studies run using hormonal therapies. The results from studies of anti-HER2 treatments during this presurgical time window have been much harder to interpret.
Dr. Hervé Bonnefoi is a professor of medical oncology at Bordeaux University (France). He reported having no financial disclosures. He made these comments as the designated discussant for the EPHOS-B study.
The significant proportion of patients treated with trastuzumab plus lapatinib for about 11 days who developed a pathologic complete response or minimal residual disease was largely unexpected.
The finding raises questions: Can we identify patients after 11 days of treatment who are good responders to this combined treatment and will have an excellent relapse-free survival without ongoing combination anti-HER2 treatment or anti-HER2 escalation, and who will be eligible for chemotherapy de-escalation similar to the regimen tested by Tolaney and her associates (N Engl J Med. 2015 Jan;372:134-41)?
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Hervé Bonnefoi |
We clearly need more data on the impact of the combined anti-HER2 regimen on the rate of long-term, relapse-free survival, and data from many more patients treated with a combined anti-HER2 regimen. The EPHOS-B results seem to contradict the results of the ALTTO study (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), but they confirm results of the NeoALTTO study, a randomized, multicenter, phase III study with 455 patients (Lancet. 2012 Jan;379[9816]:633-40).
The EPHOS-B researchers modeled their study after the presurgical treatment studies run using hormonal therapies. The results from studies of anti-HER2 treatments during this presurgical time window have been much harder to interpret.
Dr. Hervé Bonnefoi is a professor of medical oncology at Bordeaux University (France). He reported having no financial disclosures. He made these comments as the designated discussant for the EPHOS-B study.
AMSTERDAM – An unexpectedly dramatic benefit from combining trastuzumab and lapatinib when briefly treating women scheduled for breast cancer surgery has researchers focused on the best follow-up study to this promising but preliminary finding from 66 patients.
Among 66 patients with newly diagnosed HER2-positive breast cancer and scheduled for surgery, an average 11 days of treatment with a combination of trastuzumab (Herceptin) and lapatinib (Tykerb) during the period before surgery resulted in a pathologic complete response (pCR) in seven patients (11%) and 11 patients (17%) with minimal residual disease (MRD), Dr. Nigel Bundred reported at the European Breast Cancer Conference.
These patients had breast cancer tumors at baseline with a median diameter of 2 cm that with treatment for not quite 2 weeks resulted in either complete tumor disappearance or shrinkage to less than 5 mm in diameter in 18 (27%) of the patients on dual therapy, said Dr. Bundred, a professor of surgical oncology at the University Hospital of South Manchester (England).
“No cancer has ever disappeared that fast. It was flabbergasting,” Dr. Bundred said in an interview. “We need to confirm the results, and get larger numbers of patients.”
“This was a really surprising finding,” said Judith M. Bliss, professor and director of the Clinical Trials & Statistics unit of the Institute of Cancer Research in London and a co-investigator. “We knew that trastuzumab and lapatinib are effective treatments, but we had not expected to see such a dramatic effect on the structure and size of the tumor in such a short period of time,” Prof. Bliss said in a video interview.
The finding came as part of the Effect of Perioperative Anti-HER2 Therapy on Overall Survival–Biologic Phase (EPHOS-B) trial, designed to assess changes in a marker of cell proliferation (Ki67) and in a marker of cell apoptosis in relation to treatment with trastuzumab, lapatinib, or both when administered during the 10-12 days from the time patients entered the study until their scheduled surgery.
During the first phase of EPHOS-B, when 130 patients received trastuzumab monotherapy, lapatinib monotherapy, or neither, one of the 57 patients on trastuzumab (2%) had a pathologic complete response and one patient (2%) had minimal residual disease. No patients on lapatinib alone or in the control arm with no anti-HER2 drug had this sort of response.
During the second phase, 127 patients received trastuzumab alone, trastuzumab plus lapatinib in combination, or controls who received no anti-HER2 treatment. The substantial number of complete or partial responders in the 66 patients who received combined treatment with trastuzumab and lapatinib contrasted with one minimal residual disease among 32 patients (3%) who received trastuzumab alone and no responders among the 29 controls.
Patients receiving trastuzumab, alone or in the combined regimen, received a standard intravenous loading dosage of 6 mg/kg on days 1 and 8 after entry into the protocol, followed by a third dose after surgery on days 15-19; those also receiving lapatinib received 1 g/day orally for 28 days starting on entry.
“A quarter of the patients seem exquisitely sensitive to the combination of trastuzumab and lapatinib,” said Dr. David Cameron, another collaborator on the EPHOS-B study. “It’s pretty unusual to treat for 10-12 days and have 10% of the tumors disappear.”
Follow-up studies will be needed to determine whether patients with a pathologic complete response or minimal residual disease can forgo some or all of the chemotherapy that would usually follow surgery and still have good long-term disease-free survival. “We will focus on optimizing the short-term effect, and then modulate subsequent treatments,” said Dr. Cameron, professor and clinical director of oncology at the University of Edinburgh.
“We think these are patients who don’t need chemotherapy and are particularly sensitive to anti-HER2 drugs,” but so far that hasn’t been proven, cautioned Ms. Bliss.
The striking efficacy of trastuzumab combined with lapatinib in these 66 patients contrasts with the previously reported results from the ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) study, which failed to show an advantage in disease-free survival with trastuzumab plus lapatinib, compared with either of these two agents used individually during 1 year of adjuvant treatment in more than 8,000 randomized patients (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), But the EPHOS-B results did agree with results from the much smaller NeoALTTO study, which showed in a randomized, multicenter, phase III study with 455 patients a significant incremental increase in pathologic complete response rate in patients on combined trastuzumab plus lapatinib, compared with patients on either drug alone (Lancet. 2012;379 [9816]:633-40).
Another promising finding from EPHOS-B was that among the 64 patients who had their left ventricular ejection fraction assessed prior to the second phase, none of 32 patients on the combined regimen showed signs of cardiotoxicity with a reduced ejection fraction following treatment, Dr. Bundred reported.
Until now, not much was known about the beneficial mechanisms of anti-HER2 drugs, he noted. The results from EPHOS-B “tell us that combined treatment does more than just shut down cell replication. It might be that trastuzumab induces an immune response.” The former tumor beds of patients with pathologic complete response as well as regions with minimal residual disease showed large numbers of tumor infiltrating lymphocytes, a sign of a robust immune response.
Trastuzumab and lapatinib work by different mechanisms, Dr. Bundred stressed. “The only way you can combine drugs is by understanding their mechanisms. We’re still looking for the mechanisms of the anti-HER2 drugs.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AMSTERDAM – An unexpectedly dramatic benefit from combining trastuzumab and lapatinib when briefly treating women scheduled for breast cancer surgery has researchers focused on the best follow-up study to this promising but preliminary finding from 66 patients.
Among 66 patients with newly diagnosed HER2-positive breast cancer and scheduled for surgery, an average 11 days of treatment with a combination of trastuzumab (Herceptin) and lapatinib (Tykerb) during the period before surgery resulted in a pathologic complete response (pCR) in seven patients (11%) and 11 patients (17%) with minimal residual disease (MRD), Dr. Nigel Bundred reported at the European Breast Cancer Conference.
These patients had breast cancer tumors at baseline with a median diameter of 2 cm that with treatment for not quite 2 weeks resulted in either complete tumor disappearance or shrinkage to less than 5 mm in diameter in 18 (27%) of the patients on dual therapy, said Dr. Bundred, a professor of surgical oncology at the University Hospital of South Manchester (England).
“No cancer has ever disappeared that fast. It was flabbergasting,” Dr. Bundred said in an interview. “We need to confirm the results, and get larger numbers of patients.”
“This was a really surprising finding,” said Judith M. Bliss, professor and director of the Clinical Trials & Statistics unit of the Institute of Cancer Research in London and a co-investigator. “We knew that trastuzumab and lapatinib are effective treatments, but we had not expected to see such a dramatic effect on the structure and size of the tumor in such a short period of time,” Prof. Bliss said in a video interview.
The finding came as part of the Effect of Perioperative Anti-HER2 Therapy on Overall Survival–Biologic Phase (EPHOS-B) trial, designed to assess changes in a marker of cell proliferation (Ki67) and in a marker of cell apoptosis in relation to treatment with trastuzumab, lapatinib, or both when administered during the 10-12 days from the time patients entered the study until their scheduled surgery.
During the first phase of EPHOS-B, when 130 patients received trastuzumab monotherapy, lapatinib monotherapy, or neither, one of the 57 patients on trastuzumab (2%) had a pathologic complete response and one patient (2%) had minimal residual disease. No patients on lapatinib alone or in the control arm with no anti-HER2 drug had this sort of response.
During the second phase, 127 patients received trastuzumab alone, trastuzumab plus lapatinib in combination, or controls who received no anti-HER2 treatment. The substantial number of complete or partial responders in the 66 patients who received combined treatment with trastuzumab and lapatinib contrasted with one minimal residual disease among 32 patients (3%) who received trastuzumab alone and no responders among the 29 controls.
Patients receiving trastuzumab, alone or in the combined regimen, received a standard intravenous loading dosage of 6 mg/kg on days 1 and 8 after entry into the protocol, followed by a third dose after surgery on days 15-19; those also receiving lapatinib received 1 g/day orally for 28 days starting on entry.
“A quarter of the patients seem exquisitely sensitive to the combination of trastuzumab and lapatinib,” said Dr. David Cameron, another collaborator on the EPHOS-B study. “It’s pretty unusual to treat for 10-12 days and have 10% of the tumors disappear.”
Follow-up studies will be needed to determine whether patients with a pathologic complete response or minimal residual disease can forgo some or all of the chemotherapy that would usually follow surgery and still have good long-term disease-free survival. “We will focus on optimizing the short-term effect, and then modulate subsequent treatments,” said Dr. Cameron, professor and clinical director of oncology at the University of Edinburgh.
“We think these are patients who don’t need chemotherapy and are particularly sensitive to anti-HER2 drugs,” but so far that hasn’t been proven, cautioned Ms. Bliss.
The striking efficacy of trastuzumab combined with lapatinib in these 66 patients contrasts with the previously reported results from the ALTTO (Adjuvant Lapatinib and/or Trastuzumab Treatment Optimization) study, which failed to show an advantage in disease-free survival with trastuzumab plus lapatinib, compared with either of these two agents used individually during 1 year of adjuvant treatment in more than 8,000 randomized patients (J Clin Oncol. 2015 Nov 23. doi: 10.1200/JCO.2015.62.1797), But the EPHOS-B results did agree with results from the much smaller NeoALTTO study, which showed in a randomized, multicenter, phase III study with 455 patients a significant incremental increase in pathologic complete response rate in patients on combined trastuzumab plus lapatinib, compared with patients on either drug alone (Lancet. 2012;379 [9816]:633-40).
Another promising finding from EPHOS-B was that among the 64 patients who had their left ventricular ejection fraction assessed prior to the second phase, none of 32 patients on the combined regimen showed signs of cardiotoxicity with a reduced ejection fraction following treatment, Dr. Bundred reported.
Until now, not much was known about the beneficial mechanisms of anti-HER2 drugs, he noted. The results from EPHOS-B “tell us that combined treatment does more than just shut down cell replication. It might be that trastuzumab induces an immune response.” The former tumor beds of patients with pathologic complete response as well as regions with minimal residual disease showed large numbers of tumor infiltrating lymphocytes, a sign of a robust immune response.
Trastuzumab and lapatinib work by different mechanisms, Dr. Bundred stressed. “The only way you can combine drugs is by understanding their mechanisms. We’re still looking for the mechanisms of the anti-HER2 drugs.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @mitchelzoler
AT EBCC10
Key clinical point: Combined treatment with trastuzumab and lapatinib for 10-12 days led to complete HER2-positive breast cancer disappearance in seven of 66 patients.
Major finding: Pathologic complete responses occurred in seven of 66 patients on trastuzumab plus lapatinib, but none of 32 patients on trastuzumab alone or the 29 controls.
Data source: EPHOS-B, a multicenter, randomized, British study run in two phases with a total of 257 women with HER2-positive breast cancer.
Disclosures: GlaxoSmithKline, which at the time marketed lapatinib (Tykerb, now marketed by Novartis), made an educational grant to the Institute of Cancer Research in association with the EPHOS-B trial. Dr. Bundred served on an advisory board for Roche U.K. Ms. Bliss reported having no financial disclosures. Dr. Cameron has been a consultant to Novartis, GlaxoSmithKline, and Roche, but received no additional compensation.
Exploratory analysis provides support for Recurrence Score
AMSTERDAM – A 21-gene expression assessment tool may identify selected breast cancer patients who can safely forgo adjuvant chemotherapy, according to an exploratory analysis of data collected on Recurrence Scores and 5-year disease-free survival in a multicenter German trial primarily designed to compare different chemotherapy regimens.
Recurrence Score joined nodal status, stage, and grade as one of the four prognostic factors that each significantly linked with 5-year disease-free survival in a multivariate-adjusted analysis of 2,642 women with HER2-negative and hormone-receptor positive primary breast cancer, Dr. Oleg Gluz said at the European Breast Cancer Congress. Patients with a low Recurrence Score of 0-11 (on a scale of 0-100) had a 94% rate of disease-free survival during a median 55 months of follow-up when the vast majority of these patients received hormonal therapy only and no chemotherapy, said Dr. Gluz, an oncologist at the Breast Center Niederrhein of Evangelical Hospital Bethesda in Moenchengladbach, Germany. The Recurrence Score is calculated based on results from a RNA-based gene expression test known as Oncotype DX.
A Recurrence Score gene expression profile of 0-11 occurred in 18% of the screened patients, and 86% of these patients accepted the option of no chemotherapy. An additional 30% of the study group had a Recurrence Score of 12-18, and 30% had a score of 19-25, and all these patients with scores of 12-25 collectively had a 94% rate of disease-free survival following chemotherapy during a median 55 months of follow-up. Assigning all these patients with scores of 12-25 likely represents “overtreatment” for patients who also had negative lymph nodes or minimal lymph node involvement, Dr. Gluz said. In the remaining 22% of patients, who had Recurrence Scores of 26 or greater at baseline, the rate of disease-free survival after chemotherapy with a median 55 -month follow-up was 84%, Dr. Gluz reported.
These findings were consistent with an earlier report of disease-free survival after a median 3-year follow-up in the same patients, who were randomized to different chemotherapy alternatives in the PlanB trial, a phase III study primarily designed to assess the relative efficacy and safety of two chemotherapy alternatives in patients with high-risk clinical features including either positive lymph nodes or a high-risk clinical profile despite having negative lymph nodes (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.5383). They were also consistent with published 5-year disease-free survival results from a prospective evaluation of the Recurrence Score in more than 10,000 women with node-negative, hormone receptor–positive, HER2-negative breast cancer in the Trial Assigning Individualized Options for Treatment (TAILORx) study (New Engl J Med. 2015 Nov 19;373 [21]:2005-14).
“These results are interesting and provocative, but are not yet practice changing because in these high-risk patients with hormone receptor–positive tumors, relapses can occur several years after treatment so we need to wait for longer follow-up,” commented Dr. Angelo Di Leo, head of medical oncology at Prato (Italy) Hospital. He also cited the need to wait for results from several prospective, randomized trials now in progress that are more directly addressing the role of genetic profiling in predicting patient prognosis and treatment responses.
On Twitter @mitchelzoler
The key question about the genetic signatures of breast cancers obtained using tests like the Recurrence Score is whether gene-expression profiles provide useful information about the efficacy of currently-available treatment options. Before we start using assessment tools like Recurrence Score we need to see their value proven in prospective, randomized trials.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Jonas Bergh |
Our patients face a significant risk from recurrence if we prematurely use analyses like the Recurrence Score to guide treatment decisions. The 5-year median follow-up reported by Dr. Gluz is too short to produce completely reliable results.
I am concerned about the potential for undertreating patients by withholding chemotherapy from patients with a low Recurrence Score who also have one to three positive lymph nodes. We must intelligently balance the appeal of avoiding potentially toxic chemotherapy regimens against the risk for recurrence that patients could face if they don’t receive the chemotherapy regimen they require.
Dr. Jonas Bergh is a professor of oncology-pathology at the Karolinska Institute in Stockholm. He had no relevant disclosures. He made these comments as designated discussant for Dr. Gluz’s report.
The key question about the genetic signatures of breast cancers obtained using tests like the Recurrence Score is whether gene-expression profiles provide useful information about the efficacy of currently-available treatment options. Before we start using assessment tools like Recurrence Score we need to see their value proven in prospective, randomized trials.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Jonas Bergh |
Our patients face a significant risk from recurrence if we prematurely use analyses like the Recurrence Score to guide treatment decisions. The 5-year median follow-up reported by Dr. Gluz is too short to produce completely reliable results.
I am concerned about the potential for undertreating patients by withholding chemotherapy from patients with a low Recurrence Score who also have one to three positive lymph nodes. We must intelligently balance the appeal of avoiding potentially toxic chemotherapy regimens against the risk for recurrence that patients could face if they don’t receive the chemotherapy regimen they require.
Dr. Jonas Bergh is a professor of oncology-pathology at the Karolinska Institute in Stockholm. He had no relevant disclosures. He made these comments as designated discussant for Dr. Gluz’s report.
The key question about the genetic signatures of breast cancers obtained using tests like the Recurrence Score is whether gene-expression profiles provide useful information about the efficacy of currently-available treatment options. Before we start using assessment tools like Recurrence Score we need to see their value proven in prospective, randomized trials.
 |
| Mitchel L. Zoler/Frontline Medical News Dr. Jonas Bergh |
Our patients face a significant risk from recurrence if we prematurely use analyses like the Recurrence Score to guide treatment decisions. The 5-year median follow-up reported by Dr. Gluz is too short to produce completely reliable results.
I am concerned about the potential for undertreating patients by withholding chemotherapy from patients with a low Recurrence Score who also have one to three positive lymph nodes. We must intelligently balance the appeal of avoiding potentially toxic chemotherapy regimens against the risk for recurrence that patients could face if they don’t receive the chemotherapy regimen they require.
Dr. Jonas Bergh is a professor of oncology-pathology at the Karolinska Institute in Stockholm. He had no relevant disclosures. He made these comments as designated discussant for Dr. Gluz’s report.
AMSTERDAM – A 21-gene expression assessment tool may identify selected breast cancer patients who can safely forgo adjuvant chemotherapy, according to an exploratory analysis of data collected on Recurrence Scores and 5-year disease-free survival in a multicenter German trial primarily designed to compare different chemotherapy regimens.
Recurrence Score joined nodal status, stage, and grade as one of the four prognostic factors that each significantly linked with 5-year disease-free survival in a multivariate-adjusted analysis of 2,642 women with HER2-negative and hormone-receptor positive primary breast cancer, Dr. Oleg Gluz said at the European Breast Cancer Congress. Patients with a low Recurrence Score of 0-11 (on a scale of 0-100) had a 94% rate of disease-free survival during a median 55 months of follow-up when the vast majority of these patients received hormonal therapy only and no chemotherapy, said Dr. Gluz, an oncologist at the Breast Center Niederrhein of Evangelical Hospital Bethesda in Moenchengladbach, Germany. The Recurrence Score is calculated based on results from a RNA-based gene expression test known as Oncotype DX.
A Recurrence Score gene expression profile of 0-11 occurred in 18% of the screened patients, and 86% of these patients accepted the option of no chemotherapy. An additional 30% of the study group had a Recurrence Score of 12-18, and 30% had a score of 19-25, and all these patients with scores of 12-25 collectively had a 94% rate of disease-free survival following chemotherapy during a median 55 months of follow-up. Assigning all these patients with scores of 12-25 likely represents “overtreatment” for patients who also had negative lymph nodes or minimal lymph node involvement, Dr. Gluz said. In the remaining 22% of patients, who had Recurrence Scores of 26 or greater at baseline, the rate of disease-free survival after chemotherapy with a median 55 -month follow-up was 84%, Dr. Gluz reported.
These findings were consistent with an earlier report of disease-free survival after a median 3-year follow-up in the same patients, who were randomized to different chemotherapy alternatives in the PlanB trial, a phase III study primarily designed to assess the relative efficacy and safety of two chemotherapy alternatives in patients with high-risk clinical features including either positive lymph nodes or a high-risk clinical profile despite having negative lymph nodes (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.5383). They were also consistent with published 5-year disease-free survival results from a prospective evaluation of the Recurrence Score in more than 10,000 women with node-negative, hormone receptor–positive, HER2-negative breast cancer in the Trial Assigning Individualized Options for Treatment (TAILORx) study (New Engl J Med. 2015 Nov 19;373 [21]:2005-14).
“These results are interesting and provocative, but are not yet practice changing because in these high-risk patients with hormone receptor–positive tumors, relapses can occur several years after treatment so we need to wait for longer follow-up,” commented Dr. Angelo Di Leo, head of medical oncology at Prato (Italy) Hospital. He also cited the need to wait for results from several prospective, randomized trials now in progress that are more directly addressing the role of genetic profiling in predicting patient prognosis and treatment responses.
On Twitter @mitchelzoler
AMSTERDAM – A 21-gene expression assessment tool may identify selected breast cancer patients who can safely forgo adjuvant chemotherapy, according to an exploratory analysis of data collected on Recurrence Scores and 5-year disease-free survival in a multicenter German trial primarily designed to compare different chemotherapy regimens.
Recurrence Score joined nodal status, stage, and grade as one of the four prognostic factors that each significantly linked with 5-year disease-free survival in a multivariate-adjusted analysis of 2,642 women with HER2-negative and hormone-receptor positive primary breast cancer, Dr. Oleg Gluz said at the European Breast Cancer Congress. Patients with a low Recurrence Score of 0-11 (on a scale of 0-100) had a 94% rate of disease-free survival during a median 55 months of follow-up when the vast majority of these patients received hormonal therapy only and no chemotherapy, said Dr. Gluz, an oncologist at the Breast Center Niederrhein of Evangelical Hospital Bethesda in Moenchengladbach, Germany. The Recurrence Score is calculated based on results from a RNA-based gene expression test known as Oncotype DX.
A Recurrence Score gene expression profile of 0-11 occurred in 18% of the screened patients, and 86% of these patients accepted the option of no chemotherapy. An additional 30% of the study group had a Recurrence Score of 12-18, and 30% had a score of 19-25, and all these patients with scores of 12-25 collectively had a 94% rate of disease-free survival following chemotherapy during a median 55 months of follow-up. Assigning all these patients with scores of 12-25 likely represents “overtreatment” for patients who also had negative lymph nodes or minimal lymph node involvement, Dr. Gluz said. In the remaining 22% of patients, who had Recurrence Scores of 26 or greater at baseline, the rate of disease-free survival after chemotherapy with a median 55 -month follow-up was 84%, Dr. Gluz reported.
These findings were consistent with an earlier report of disease-free survival after a median 3-year follow-up in the same patients, who were randomized to different chemotherapy alternatives in the PlanB trial, a phase III study primarily designed to assess the relative efficacy and safety of two chemotherapy alternatives in patients with high-risk clinical features including either positive lymph nodes or a high-risk clinical profile despite having negative lymph nodes (J Clin Oncol. 2016 Feb 29. doi: 10.1200/JCO.2015.63.5383). They were also consistent with published 5-year disease-free survival results from a prospective evaluation of the Recurrence Score in more than 10,000 women with node-negative, hormone receptor–positive, HER2-negative breast cancer in the Trial Assigning Individualized Options for Treatment (TAILORx) study (New Engl J Med. 2015 Nov 19;373 [21]:2005-14).
“These results are interesting and provocative, but are not yet practice changing because in these high-risk patients with hormone receptor–positive tumors, relapses can occur several years after treatment so we need to wait for longer follow-up,” commented Dr. Angelo Di Leo, head of medical oncology at Prato (Italy) Hospital. He also cited the need to wait for results from several prospective, randomized trials now in progress that are more directly addressing the role of genetic profiling in predicting patient prognosis and treatment responses.
On Twitter @mitchelzoler
AT EBCC10
Key clinical point: A commercialized assessment of gene expression, the Recurrence Score, identified high-risk breast cancer patients who could forgo chemotherapy and receive hormonal treatment only and still have a good level of 5-year recurrence-free survival.
Major finding: Patients with a Recurrence Score of 0-11 had a 94% 5-year disease-free survival rate while largely avoiding chemotherapy.
Data source: The Plan B study, which included 2,642 German patients with hormone receptor–positive, HER2-negative breast cancer.
Disclosures: The Plan B trial was sponsored by Sanofi-Aventis, Amgen, and Genomic Health, the company that markets the Recurrence Score assay. Dr. Gluz said that he has been a speaker on behalf of Genomic Health and Nanostring. Dr. Di Leo said that he has been a lecturer on behalf of Genomic Health and has been a lecturer or advisor for seven drug companies.
Dose-dense chemotherapy boosts premenopausal breast cancer survival
AMSTERDAM – Premenopausal women with breast cancer at high risk for recurrence had a significantly improved 10-year rate of overall survival when they received a dose-dense chemotherapy regimen, compared with women treated with a standard dosage schedule.
This post hoc analysis of 1,549 premenopausal patients, a subgroup drawn from two separate trials run a decade apart, helps further confirm the benefit of the dose-dense approach in this population. “I think that European practice will now change,” based on this new analysis plus other recent findings from smaller studies, predicted Dr. Matteo Lambertini, who reported the analysis at the European Breast Cancer Congress.
“Dose-dense adjuvant chemotherapy may be considered the preferred treatment option and should be proposed to all high-risk, premenopausal breast cancer patients who are candidates for chemotherapy,” said Dr. Lambertini of Azienda University Hospital in Genoa, Italy. Although dose-dense regimens are common in U.S. practice for these patients and used at certain European Centers, many other European cancer programs still use standard-dose chemotherapy, he said.
The findings also showed that when treatment induced amenorrhea, it had no bearing on subsequent survival, and that the dose-dense regimen did not cause amenorrhea.
The analysis run by Dr. Lambertini and his associates pieced together data from premenopausal women who formed subgroups in two large Italian trials of dose-dense regimens as adjuvant chemotherapy for women of all ages with early-stage breast cancer: the Mammella InterGruppo (MIG) 1 trial and the Gruppo Italiano Mammella (GIM) 2 trial. MIG1 randomized 1,214 patients with early-stage breast cancer to standard chemotherapy given in 3-week cycles or in dose-dense 2-week cycles. At a median 10-year follow-up, the results showed a nonsignificant difference in overall survival between the two arms; the findings primarily demonstrated the safety of the dose-dense regimen (J Nat Cancer Inst. 2005 Dec 7;97 [23]:1724-33). GIM2 randomized 2,019 patients with early-stage breast cancer to the same alternatives, standard chemotherapy administered either every 2 or every 3 weeks and followed them for a median of 7 years. Its results showed a statistically significant improvement in disease-free survival after 5 years with the dose-dense regimen (Lancet. 2015 May 9;385[9980]:1863-72).
All patients in both studies routinely received ongoing treatment with a granulocyte colony–stimulating factor analogue during chemotherapy to help avoid the development of anemia or leukopenia.
Dr. Lambertini’s analysis focused on the 1,549 women from both studies who were premenopausal at the time they received treatment, with more than half of these patients younger than 45 years old. In this population, treatment with the dose-dense regimen resulted in a statistically significant increased rate of 10-year overall survival, expressed as a 29% reduced hazard ratio for death with dose-dense treatment (P = .021), he reported. The benefit was greatest in women with hormone receptor–negative tumors, with a hazard ratio for death reduced by 35% among women with a hormone receptor–negative tumor; overall mortality fell by 22% after a dose-dense regimen, compared with women who received chemotherapy with a standard interval between treatments.
The analysis also showed no impact from development of amenorrhea, with a nonsignificant hazard ratio of 16% separating the mortality rates in women who developed treatment-related amenorrhea and those who did not.
“This meta-analysis provides important information that has the potential to change and improve treatment of breast cancer in premenopausal patients,” commented Dr. Fátima Cardoso, director of the breast unit at the Champalimaud Clinical Center, Lisbon. The new findings “give us evidence-based answers as to whether or not dose-dense chemotherapy can be used in these patients without increasing their risk of treatment-induced amenorrhea, as well as showing a survival benefit,” Dr. Cardoso said in a written statement.
On Twitter@mitchelzoler
This analysis confirms the appropriateness of dose-dense chemotherapy regimens for premenopausal patients, an approach that is already routinely used in women with high-risk breast cancer who require chemotherapy. Dose-dense regimens are currently used more widely in the United States than in Europe, but these new findings should help further convince European oncologists to use dose-dense treatment schedules. The disadvantage of these regimens is that they involve more clinic visits and are more costly.
One of the factors increasing the cost is the need for greater bone marrow support by concurrent treatment with a granulocyte colony–stimulating factor analogue. It is important to have data like these to convince payers that dose-dense regimens are worth their extra cost.
By focusing specifically on premenopausal women, this analysis also showed that dose-dense regimens do not trigger more episodes of amenorrhea, nor were episodes of amenorrhea needed to get the greatest survival benefit.
Dr. Emiel J.T. Rutgers is a surgical oncologist and clinical director of the Netherlands Cancer Institute in Amsterdam. He had no relevant financial disclosures. He made these comments during a video interview with this news organization.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This analysis confirms the appropriateness of dose-dense chemotherapy regimens for premenopausal patients, an approach that is already routinely used in women with high-risk breast cancer who require chemotherapy. Dose-dense regimens are currently used more widely in the United States than in Europe, but these new findings should help further convince European oncologists to use dose-dense treatment schedules. The disadvantage of these regimens is that they involve more clinic visits and are more costly.
One of the factors increasing the cost is the need for greater bone marrow support by concurrent treatment with a granulocyte colony–stimulating factor analogue. It is important to have data like these to convince payers that dose-dense regimens are worth their extra cost.
By focusing specifically on premenopausal women, this analysis also showed that dose-dense regimens do not trigger more episodes of amenorrhea, nor were episodes of amenorrhea needed to get the greatest survival benefit.
Dr. Emiel J.T. Rutgers is a surgical oncologist and clinical director of the Netherlands Cancer Institute in Amsterdam. He had no relevant financial disclosures. He made these comments during a video interview with this news organization.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
This analysis confirms the appropriateness of dose-dense chemotherapy regimens for premenopausal patients, an approach that is already routinely used in women with high-risk breast cancer who require chemotherapy. Dose-dense regimens are currently used more widely in the United States than in Europe, but these new findings should help further convince European oncologists to use dose-dense treatment schedules. The disadvantage of these regimens is that they involve more clinic visits and are more costly.
One of the factors increasing the cost is the need for greater bone marrow support by concurrent treatment with a granulocyte colony–stimulating factor analogue. It is important to have data like these to convince payers that dose-dense regimens are worth their extra cost.
By focusing specifically on premenopausal women, this analysis also showed that dose-dense regimens do not trigger more episodes of amenorrhea, nor were episodes of amenorrhea needed to get the greatest survival benefit.
Dr. Emiel J.T. Rutgers is a surgical oncologist and clinical director of the Netherlands Cancer Institute in Amsterdam. He had no relevant financial disclosures. He made these comments during a video interview with this news organization.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AMSTERDAM – Premenopausal women with breast cancer at high risk for recurrence had a significantly improved 10-year rate of overall survival when they received a dose-dense chemotherapy regimen, compared with women treated with a standard dosage schedule.
This post hoc analysis of 1,549 premenopausal patients, a subgroup drawn from two separate trials run a decade apart, helps further confirm the benefit of the dose-dense approach in this population. “I think that European practice will now change,” based on this new analysis plus other recent findings from smaller studies, predicted Dr. Matteo Lambertini, who reported the analysis at the European Breast Cancer Congress.
“Dose-dense adjuvant chemotherapy may be considered the preferred treatment option and should be proposed to all high-risk, premenopausal breast cancer patients who are candidates for chemotherapy,” said Dr. Lambertini of Azienda University Hospital in Genoa, Italy. Although dose-dense regimens are common in U.S. practice for these patients and used at certain European Centers, many other European cancer programs still use standard-dose chemotherapy, he said.
The findings also showed that when treatment induced amenorrhea, it had no bearing on subsequent survival, and that the dose-dense regimen did not cause amenorrhea.
The analysis run by Dr. Lambertini and his associates pieced together data from premenopausal women who formed subgroups in two large Italian trials of dose-dense regimens as adjuvant chemotherapy for women of all ages with early-stage breast cancer: the Mammella InterGruppo (MIG) 1 trial and the Gruppo Italiano Mammella (GIM) 2 trial. MIG1 randomized 1,214 patients with early-stage breast cancer to standard chemotherapy given in 3-week cycles or in dose-dense 2-week cycles. At a median 10-year follow-up, the results showed a nonsignificant difference in overall survival between the two arms; the findings primarily demonstrated the safety of the dose-dense regimen (J Nat Cancer Inst. 2005 Dec 7;97 [23]:1724-33). GIM2 randomized 2,019 patients with early-stage breast cancer to the same alternatives, standard chemotherapy administered either every 2 or every 3 weeks and followed them for a median of 7 years. Its results showed a statistically significant improvement in disease-free survival after 5 years with the dose-dense regimen (Lancet. 2015 May 9;385[9980]:1863-72).
All patients in both studies routinely received ongoing treatment with a granulocyte colony–stimulating factor analogue during chemotherapy to help avoid the development of anemia or leukopenia.
Dr. Lambertini’s analysis focused on the 1,549 women from both studies who were premenopausal at the time they received treatment, with more than half of these patients younger than 45 years old. In this population, treatment with the dose-dense regimen resulted in a statistically significant increased rate of 10-year overall survival, expressed as a 29% reduced hazard ratio for death with dose-dense treatment (P = .021), he reported. The benefit was greatest in women with hormone receptor–negative tumors, with a hazard ratio for death reduced by 35% among women with a hormone receptor–negative tumor; overall mortality fell by 22% after a dose-dense regimen, compared with women who received chemotherapy with a standard interval between treatments.
The analysis also showed no impact from development of amenorrhea, with a nonsignificant hazard ratio of 16% separating the mortality rates in women who developed treatment-related amenorrhea and those who did not.
“This meta-analysis provides important information that has the potential to change and improve treatment of breast cancer in premenopausal patients,” commented Dr. Fátima Cardoso, director of the breast unit at the Champalimaud Clinical Center, Lisbon. The new findings “give us evidence-based answers as to whether or not dose-dense chemotherapy can be used in these patients without increasing their risk of treatment-induced amenorrhea, as well as showing a survival benefit,” Dr. Cardoso said in a written statement.
On Twitter@mitchelzoler
AMSTERDAM – Premenopausal women with breast cancer at high risk for recurrence had a significantly improved 10-year rate of overall survival when they received a dose-dense chemotherapy regimen, compared with women treated with a standard dosage schedule.
This post hoc analysis of 1,549 premenopausal patients, a subgroup drawn from two separate trials run a decade apart, helps further confirm the benefit of the dose-dense approach in this population. “I think that European practice will now change,” based on this new analysis plus other recent findings from smaller studies, predicted Dr. Matteo Lambertini, who reported the analysis at the European Breast Cancer Congress.
“Dose-dense adjuvant chemotherapy may be considered the preferred treatment option and should be proposed to all high-risk, premenopausal breast cancer patients who are candidates for chemotherapy,” said Dr. Lambertini of Azienda University Hospital in Genoa, Italy. Although dose-dense regimens are common in U.S. practice for these patients and used at certain European Centers, many other European cancer programs still use standard-dose chemotherapy, he said.
The findings also showed that when treatment induced amenorrhea, it had no bearing on subsequent survival, and that the dose-dense regimen did not cause amenorrhea.
The analysis run by Dr. Lambertini and his associates pieced together data from premenopausal women who formed subgroups in two large Italian trials of dose-dense regimens as adjuvant chemotherapy for women of all ages with early-stage breast cancer: the Mammella InterGruppo (MIG) 1 trial and the Gruppo Italiano Mammella (GIM) 2 trial. MIG1 randomized 1,214 patients with early-stage breast cancer to standard chemotherapy given in 3-week cycles or in dose-dense 2-week cycles. At a median 10-year follow-up, the results showed a nonsignificant difference in overall survival between the two arms; the findings primarily demonstrated the safety of the dose-dense regimen (J Nat Cancer Inst. 2005 Dec 7;97 [23]:1724-33). GIM2 randomized 2,019 patients with early-stage breast cancer to the same alternatives, standard chemotherapy administered either every 2 or every 3 weeks and followed them for a median of 7 years. Its results showed a statistically significant improvement in disease-free survival after 5 years with the dose-dense regimen (Lancet. 2015 May 9;385[9980]:1863-72).
All patients in both studies routinely received ongoing treatment with a granulocyte colony–stimulating factor analogue during chemotherapy to help avoid the development of anemia or leukopenia.
Dr. Lambertini’s analysis focused on the 1,549 women from both studies who were premenopausal at the time they received treatment, with more than half of these patients younger than 45 years old. In this population, treatment with the dose-dense regimen resulted in a statistically significant increased rate of 10-year overall survival, expressed as a 29% reduced hazard ratio for death with dose-dense treatment (P = .021), he reported. The benefit was greatest in women with hormone receptor–negative tumors, with a hazard ratio for death reduced by 35% among women with a hormone receptor–negative tumor; overall mortality fell by 22% after a dose-dense regimen, compared with women who received chemotherapy with a standard interval between treatments.
The analysis also showed no impact from development of amenorrhea, with a nonsignificant hazard ratio of 16% separating the mortality rates in women who developed treatment-related amenorrhea and those who did not.
“This meta-analysis provides important information that has the potential to change and improve treatment of breast cancer in premenopausal patients,” commented Dr. Fátima Cardoso, director of the breast unit at the Champalimaud Clinical Center, Lisbon. The new findings “give us evidence-based answers as to whether or not dose-dense chemotherapy can be used in these patients without increasing their risk of treatment-induced amenorrhea, as well as showing a survival benefit,” Dr. Cardoso said in a written statement.
On Twitter@mitchelzoler
AT EBCC10
Key clinical point: Premenopausal women with breast cancer at high risk for recurrence had a significantly improved rate of overall 10-year survival following a dose-dense chemotherapy regimen, compared with women who received a standard-treatment schedule.
Major finding: The mortality hazard ratio fell by 29% (P = .021) with dose-dense treatment, compared with standard chemotherapy.
Data source: A post hoc subgroup analysis of data collected from two large Italian chemotherapy trials that together included 1,549 premenopausal breast cancer patients.
Disclosures: Dr. Lambertini and Dr. Cardoso had no relevant financial disclosures.
VIDEO: Focused breast cancer radiation maintains efficacy, cuts AEs
AMSTERDAM – Modifying the standard radiation dosage to women with early-stage breast cancer so that the tumor-bed dosage remained the same but eliminated the dosage delivered to surrounding breast tissue led to similar 5-year efficacy and reduced adverse effects in a multicenter U.K. trial that involved more than 2,000 patients.
“Partial-breast radiotherapy was noninferior to whole-breast radiotherpy for reducing local recurrences and reduced the severity of overall breast appearance and breast hardness,” Dr. Charlotte Coles said at the European Breast Cancer Congress. “I consider this practice changing,” concluded Dr. Coles of Cambridge (England) University Hospitals.
While some experts at the meeting agreed with Dr. Coles’ assessment of the findings, others took a more skeptical view, focusing on the median follow-up of just 5 years.
“There is still some question about the long-term results for local recurrence rates,” said Dr. Robert Mansel, professor of surgical oncology at Cardiff (Wales) University. In addition, “the rationale for doing this is to reduce side effects to the whole breast, but the results showed little difference in side effects” between women who received the standard radiation dosage and those who received a reduced dosage, “so the rationale for doing this is not quite there,” said Dr. Mansel, the session’s designated discussant.
The Intensity Modulated Partial Breast Radiotherapy for Women with Early Breast Cancer (IMPORT LOW) trial enrolled 2,018 patients with early breast cancer at 30 U.K. centers during 2007-2010. Patients underwent breast conservation surgery and were at least 50 years old, had a tumor of 3 cm or less, had an invasive and unifocal adenocarcinoma that was grade I, II, or III, and had lymph nodes that were either negative or had micrometastases (pN0 or pN1). The trial randomized these women to either standard, whole-breast radiation with 40 gray, a reduced-dosage regimen that delivered 40 gray to the tumor bed but 36 gray to the rest of the breast, or a partial regimen that delivered 40 gray to the tumor bed and no radiation at all to the rest of the ipsilateral breast. All three regimens were administered as 15 fractions.
After a median follow-up of 71 months, the 674 women randomized to the reduced regimen had a 26% reduction in their absolute local recurrence rate compared with the 674 whole-breast controls. The 670 women randomized to the partial regimen had an absolute reduction of 39%. Both of these relative reductions were statistically significant. These efficacy results also met the study’s prespecified primary endpoint for noninferiority for controlling local recurrences in the ipsilateral breast, Dr. Coles reported.
For the study’s secondary endpoints of various measures of adverse effects to the normal breast tissue, the partial-dosage regimen led to a statistically significant reduction in patient assessment of changed breast appearance (P = .005) and a reduced rate of patient perception of increased breast firmness (P = .001). The adverse-effects endpoints also showed a significant reduction with the partial regimen in physician assessment of breast edema (P = .0053). The overall rate of patients free of any adverse effect in their normal breast tissue after 5 years was 72% in the control patients, 79% in those who received the reduced-dose regimen (P = .042), and 81% in those who received the partial dose (P = .004).
An expert panel is scheduled to review new evidence on breast radiotherapy later in March, and these new data may produce a change in the recommended irradiation protocol, Dr. Coles said.
On Twitter @mitchelzoler
I believe that these 5-year results are sufficient to make the partial-dose radiation regimen our new standard treatment. The advantage is to better spare the normal breast tissue from radiation damage while maintaining similar local control compared with standard radiotherapy that irradiates the entire breast.
In the results reported by Dr. Coles, partial breast irradiation produced excellent local control with more limited toxicity. It should be used for women with an early, small, low-risk breast cancer detected by screening with no or very limited lymph node metastases. I estimate that about a third of women with breast cancer fall into this category. There seems to be no reason to not apply these findings to any woman who meets the enrollment criteria for the study.
One limitation of this study is that it involved a median 5-year follow-up, whereas we usually focus on 10-year follow-up data. However, we know that local-recurrence rates are usually low during years 6-10 following breast irradiation for these types of patients, so I think the 5-year data are sufficient.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Emiel J.T. Rutgers is a surgical oncologist and clinical director of the Netherlands Cancer Institute in Amsterdam. He had no disclosures. He made these comments during an interview.
I believe that these 5-year results are sufficient to make the partial-dose radiation regimen our new standard treatment. The advantage is to better spare the normal breast tissue from radiation damage while maintaining similar local control compared with standard radiotherapy that irradiates the entire breast.
In the results reported by Dr. Coles, partial breast irradiation produced excellent local control with more limited toxicity. It should be used for women with an early, small, low-risk breast cancer detected by screening with no or very limited lymph node metastases. I estimate that about a third of women with breast cancer fall into this category. There seems to be no reason to not apply these findings to any woman who meets the enrollment criteria for the study.
One limitation of this study is that it involved a median 5-year follow-up, whereas we usually focus on 10-year follow-up data. However, we know that local-recurrence rates are usually low during years 6-10 following breast irradiation for these types of patients, so I think the 5-year data are sufficient.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Emiel J.T. Rutgers is a surgical oncologist and clinical director of the Netherlands Cancer Institute in Amsterdam. He had no disclosures. He made these comments during an interview.
I believe that these 5-year results are sufficient to make the partial-dose radiation regimen our new standard treatment. The advantage is to better spare the normal breast tissue from radiation damage while maintaining similar local control compared with standard radiotherapy that irradiates the entire breast.
In the results reported by Dr. Coles, partial breast irradiation produced excellent local control with more limited toxicity. It should be used for women with an early, small, low-risk breast cancer detected by screening with no or very limited lymph node metastases. I estimate that about a third of women with breast cancer fall into this category. There seems to be no reason to not apply these findings to any woman who meets the enrollment criteria for the study.
One limitation of this study is that it involved a median 5-year follow-up, whereas we usually focus on 10-year follow-up data. However, we know that local-recurrence rates are usually low during years 6-10 following breast irradiation for these types of patients, so I think the 5-year data are sufficient.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Emiel J.T. Rutgers is a surgical oncologist and clinical director of the Netherlands Cancer Institute in Amsterdam. He had no disclosures. He made these comments during an interview.
AMSTERDAM – Modifying the standard radiation dosage to women with early-stage breast cancer so that the tumor-bed dosage remained the same but eliminated the dosage delivered to surrounding breast tissue led to similar 5-year efficacy and reduced adverse effects in a multicenter U.K. trial that involved more than 2,000 patients.
“Partial-breast radiotherapy was noninferior to whole-breast radiotherpy for reducing local recurrences and reduced the severity of overall breast appearance and breast hardness,” Dr. Charlotte Coles said at the European Breast Cancer Congress. “I consider this practice changing,” concluded Dr. Coles of Cambridge (England) University Hospitals.
While some experts at the meeting agreed with Dr. Coles’ assessment of the findings, others took a more skeptical view, focusing on the median follow-up of just 5 years.
“There is still some question about the long-term results for local recurrence rates,” said Dr. Robert Mansel, professor of surgical oncology at Cardiff (Wales) University. In addition, “the rationale for doing this is to reduce side effects to the whole breast, but the results showed little difference in side effects” between women who received the standard radiation dosage and those who received a reduced dosage, “so the rationale for doing this is not quite there,” said Dr. Mansel, the session’s designated discussant.
The Intensity Modulated Partial Breast Radiotherapy for Women with Early Breast Cancer (IMPORT LOW) trial enrolled 2,018 patients with early breast cancer at 30 U.K. centers during 2007-2010. Patients underwent breast conservation surgery and were at least 50 years old, had a tumor of 3 cm or less, had an invasive and unifocal adenocarcinoma that was grade I, II, or III, and had lymph nodes that were either negative or had micrometastases (pN0 or pN1). The trial randomized these women to either standard, whole-breast radiation with 40 gray, a reduced-dosage regimen that delivered 40 gray to the tumor bed but 36 gray to the rest of the breast, or a partial regimen that delivered 40 gray to the tumor bed and no radiation at all to the rest of the ipsilateral breast. All three regimens were administered as 15 fractions.
After a median follow-up of 71 months, the 674 women randomized to the reduced regimen had a 26% reduction in their absolute local recurrence rate compared with the 674 whole-breast controls. The 670 women randomized to the partial regimen had an absolute reduction of 39%. Both of these relative reductions were statistically significant. These efficacy results also met the study’s prespecified primary endpoint for noninferiority for controlling local recurrences in the ipsilateral breast, Dr. Coles reported.
For the study’s secondary endpoints of various measures of adverse effects to the normal breast tissue, the partial-dosage regimen led to a statistically significant reduction in patient assessment of changed breast appearance (P = .005) and a reduced rate of patient perception of increased breast firmness (P = .001). The adverse-effects endpoints also showed a significant reduction with the partial regimen in physician assessment of breast edema (P = .0053). The overall rate of patients free of any adverse effect in their normal breast tissue after 5 years was 72% in the control patients, 79% in those who received the reduced-dose regimen (P = .042), and 81% in those who received the partial dose (P = .004).
An expert panel is scheduled to review new evidence on breast radiotherapy later in March, and these new data may produce a change in the recommended irradiation protocol, Dr. Coles said.
On Twitter @mitchelzoler
AMSTERDAM – Modifying the standard radiation dosage to women with early-stage breast cancer so that the tumor-bed dosage remained the same but eliminated the dosage delivered to surrounding breast tissue led to similar 5-year efficacy and reduced adverse effects in a multicenter U.K. trial that involved more than 2,000 patients.
“Partial-breast radiotherapy was noninferior to whole-breast radiotherpy for reducing local recurrences and reduced the severity of overall breast appearance and breast hardness,” Dr. Charlotte Coles said at the European Breast Cancer Congress. “I consider this practice changing,” concluded Dr. Coles of Cambridge (England) University Hospitals.
While some experts at the meeting agreed with Dr. Coles’ assessment of the findings, others took a more skeptical view, focusing on the median follow-up of just 5 years.
“There is still some question about the long-term results for local recurrence rates,” said Dr. Robert Mansel, professor of surgical oncology at Cardiff (Wales) University. In addition, “the rationale for doing this is to reduce side effects to the whole breast, but the results showed little difference in side effects” between women who received the standard radiation dosage and those who received a reduced dosage, “so the rationale for doing this is not quite there,” said Dr. Mansel, the session’s designated discussant.
The Intensity Modulated Partial Breast Radiotherapy for Women with Early Breast Cancer (IMPORT LOW) trial enrolled 2,018 patients with early breast cancer at 30 U.K. centers during 2007-2010. Patients underwent breast conservation surgery and were at least 50 years old, had a tumor of 3 cm or less, had an invasive and unifocal adenocarcinoma that was grade I, II, or III, and had lymph nodes that were either negative or had micrometastases (pN0 or pN1). The trial randomized these women to either standard, whole-breast radiation with 40 gray, a reduced-dosage regimen that delivered 40 gray to the tumor bed but 36 gray to the rest of the breast, or a partial regimen that delivered 40 gray to the tumor bed and no radiation at all to the rest of the ipsilateral breast. All three regimens were administered as 15 fractions.
After a median follow-up of 71 months, the 674 women randomized to the reduced regimen had a 26% reduction in their absolute local recurrence rate compared with the 674 whole-breast controls. The 670 women randomized to the partial regimen had an absolute reduction of 39%. Both of these relative reductions were statistically significant. These efficacy results also met the study’s prespecified primary endpoint for noninferiority for controlling local recurrences in the ipsilateral breast, Dr. Coles reported.
For the study’s secondary endpoints of various measures of adverse effects to the normal breast tissue, the partial-dosage regimen led to a statistically significant reduction in patient assessment of changed breast appearance (P = .005) and a reduced rate of patient perception of increased breast firmness (P = .001). The adverse-effects endpoints also showed a significant reduction with the partial regimen in physician assessment of breast edema (P = .0053). The overall rate of patients free of any adverse effect in their normal breast tissue after 5 years was 72% in the control patients, 79% in those who received the reduced-dose regimen (P = .042), and 81% in those who received the partial dose (P = .004).
An expert panel is scheduled to review new evidence on breast radiotherapy later in March, and these new data may produce a change in the recommended irradiation protocol, Dr. Coles said.
On Twitter @mitchelzoler
AT EBCC 10
Key clinical point: Maintaining the standard breast cancer radiation dosage to the tumor bed while eliminating the dosage to the rest of the breast maintained efficacy and improved posttreatment breast appearance.
Major finding: Women not receiving radiation to their normal breast tissue had a 39% reduction in local recurrences, compared with controls.
Data source: The IMPORT LOW study, which randomized 2,018 women with early breast cancer at 30 U.K. centers for a median of 5 years.
Disclosures: IMPORT LOW received no commercial support. Dr. Coles and Dr. Mansel has no disclosures.
Ultrasound bested tomosynthesis for screening dense breast tissue
Ultrasound was about 1.8 times more sensitive than tomosynthesis for the incremental detection of breast cancer in women with radiologically dense breasts and negative two-dimensional mammography screening, according to interim results from the first prospective trial to directly compare the two modalities.
“However, future application of adjunct screening should consider that tomosynthesis detected more than 50% of the additional breast cancers in these women, and could potentially be [a] primary screening modality,” wrote Dr. Alberto Tagliafico of the University of Genoa (Italy) and his associates. The study was published online March 9 in the Journal of Clinical Oncology and presented simultaneously at the European Breast Cancer Conference.
Radiologically dense breast tissue undermines the sensitivity of mammography and is itself an independent risk factor for breast cancer. Recently, many states began requiring that women be informed of their breast density and adjunct screening measures, such as ultrasound. But estimates of the sensitivity of ultrasound have ranged from about 1.9 to 4.2 cancers for every 1,000 screens, said the researchers. This variance, combined with costs and concerns about false-positive recalls, have fueled debates about the value of adjunct measures in breast cancer screening, they added. To help clarify these issues, the multicenter ASTOUND (Adjunct Screening With Tomosynthesis or Ultrasound in Women With Mammography-Negative Dense Breasts) study compared physician-performed ultrasound and tomosynthesis results for 3,231 asymptomatic women aged 44 to 71 years, whose median age was 51 years (J Clin Oncol. 2016 Mar 9. doi: 10.1200/JCO.2015.63.4147).
In all, the researchers detected 24 additional breast cancers, 23 of which were invasive. Thus, ultrasound detected about 7.1 additional cancers for every 1,000 screens (95% confidence interval, 4.2-10), compared with 4.0 additional cancers per 1,000 screens for tomosynthesis (95% CI, 1.8-6.2; P = .006). Only one cancer was detected by tomosynthesis alone. The rate of false-positive recalls was similar for the two modalities – 53 cases for tomosynthesis, versus 63 for ultrasound (P = .26). Rates of false-positive recalls leading to biopsy also were similar. Needle biopsies usually sufficed in recalled cases, but two women underwent surgical biopsies, both of which revealed radial scars.
If the final results of ASTOUND confirm these interim data, “it could be argued that breast tomosynthesis has little value in a setting where adjunct ultrasound is frequently used for screening women with mammography-dense breasts,” said the researchers. But tomosynthesis may have a role as a primary screening modality in other setting, especially because tomosynthesis acquisitions that also provide reconstructed 2D mammography are now available, lessening concerns about unjustified radiation exposure, they added.
The “modest” number of cancers in the interim report led to relatively wide confidence intervals, the investigators noted. Biomarker data were not available for all cancers, and both prevalent and incident ultrasound data were compared with prevalent tomosynthesis data, which might bias false-positive recall results in favor of ultrasound, they added.
Currently, 24 American states have laws requiring that women receive some level of notification about breast density with their mammography results. Dense breast tissue can hide cancer on mammography, especially when the cancer lacks calcifications, resulting in delayed diagnosis and worse outcomes. Moreover, dense breast tissue is an independent risk factor for developing breast cancer.
Because the primary goal of screening is detection of early breast cancer, ultrasound would seem the clear choice, compared with tomosynthesis. Given comparable false-positive rates in ASTOUND, the estimated cost per cancer detected would be similar or more favorable for ultrasound than tomosynthesis. Ultrasound equipment is becoming much less expensive, requires no ionizing radiation, and it is easy to guide needle biopsy of lesions seen only on ultrasound.
Preliminary results from ASTOUND are extremely important in helping to inform personalized screening choices for women with dense breasts. Guidelines on these issues are planned, but often limit recommendations to those based on evidence from randomized trials with mortality as an end point. Our knowledge of the natural history of breast cancer and results from randomized trials of mammography should inform guidelines for supplemental screening.
Dr. Wendie A. Berg is at Magee-Womens Hospital of University of Pittsburgh Medical Center. She reported serving in a consulting or advisory role with SuperSonic Imagine. These comments were taken from her accompanying editorial (J Clin Oncol. 2016 Mar 9. doi: 10.1200/JCO.2015.65.8674).
Currently, 24 American states have laws requiring that women receive some level of notification about breast density with their mammography results. Dense breast tissue can hide cancer on mammography, especially when the cancer lacks calcifications, resulting in delayed diagnosis and worse outcomes. Moreover, dense breast tissue is an independent risk factor for developing breast cancer.
Because the primary goal of screening is detection of early breast cancer, ultrasound would seem the clear choice, compared with tomosynthesis. Given comparable false-positive rates in ASTOUND, the estimated cost per cancer detected would be similar or more favorable for ultrasound than tomosynthesis. Ultrasound equipment is becoming much less expensive, requires no ionizing radiation, and it is easy to guide needle biopsy of lesions seen only on ultrasound.
Preliminary results from ASTOUND are extremely important in helping to inform personalized screening choices for women with dense breasts. Guidelines on these issues are planned, but often limit recommendations to those based on evidence from randomized trials with mortality as an end point. Our knowledge of the natural history of breast cancer and results from randomized trials of mammography should inform guidelines for supplemental screening.
Dr. Wendie A. Berg is at Magee-Womens Hospital of University of Pittsburgh Medical Center. She reported serving in a consulting or advisory role with SuperSonic Imagine. These comments were taken from her accompanying editorial (J Clin Oncol. 2016 Mar 9. doi: 10.1200/JCO.2015.65.8674).
Currently, 24 American states have laws requiring that women receive some level of notification about breast density with their mammography results. Dense breast tissue can hide cancer on mammography, especially when the cancer lacks calcifications, resulting in delayed diagnosis and worse outcomes. Moreover, dense breast tissue is an independent risk factor for developing breast cancer.
Because the primary goal of screening is detection of early breast cancer, ultrasound would seem the clear choice, compared with tomosynthesis. Given comparable false-positive rates in ASTOUND, the estimated cost per cancer detected would be similar or more favorable for ultrasound than tomosynthesis. Ultrasound equipment is becoming much less expensive, requires no ionizing radiation, and it is easy to guide needle biopsy of lesions seen only on ultrasound.
Preliminary results from ASTOUND are extremely important in helping to inform personalized screening choices for women with dense breasts. Guidelines on these issues are planned, but often limit recommendations to those based on evidence from randomized trials with mortality as an end point. Our knowledge of the natural history of breast cancer and results from randomized trials of mammography should inform guidelines for supplemental screening.
Dr. Wendie A. Berg is at Magee-Womens Hospital of University of Pittsburgh Medical Center. She reported serving in a consulting or advisory role with SuperSonic Imagine. These comments were taken from her accompanying editorial (J Clin Oncol. 2016 Mar 9. doi: 10.1200/JCO.2015.65.8674).
Ultrasound was about 1.8 times more sensitive than tomosynthesis for the incremental detection of breast cancer in women with radiologically dense breasts and negative two-dimensional mammography screening, according to interim results from the first prospective trial to directly compare the two modalities.
“However, future application of adjunct screening should consider that tomosynthesis detected more than 50% of the additional breast cancers in these women, and could potentially be [a] primary screening modality,” wrote Dr. Alberto Tagliafico of the University of Genoa (Italy) and his associates. The study was published online March 9 in the Journal of Clinical Oncology and presented simultaneously at the European Breast Cancer Conference.
Radiologically dense breast tissue undermines the sensitivity of mammography and is itself an independent risk factor for breast cancer. Recently, many states began requiring that women be informed of their breast density and adjunct screening measures, such as ultrasound. But estimates of the sensitivity of ultrasound have ranged from about 1.9 to 4.2 cancers for every 1,000 screens, said the researchers. This variance, combined with costs and concerns about false-positive recalls, have fueled debates about the value of adjunct measures in breast cancer screening, they added. To help clarify these issues, the multicenter ASTOUND (Adjunct Screening With Tomosynthesis or Ultrasound in Women With Mammography-Negative Dense Breasts) study compared physician-performed ultrasound and tomosynthesis results for 3,231 asymptomatic women aged 44 to 71 years, whose median age was 51 years (J Clin Oncol. 2016 Mar 9. doi: 10.1200/JCO.2015.63.4147).
In all, the researchers detected 24 additional breast cancers, 23 of which were invasive. Thus, ultrasound detected about 7.1 additional cancers for every 1,000 screens (95% confidence interval, 4.2-10), compared with 4.0 additional cancers per 1,000 screens for tomosynthesis (95% CI, 1.8-6.2; P = .006). Only one cancer was detected by tomosynthesis alone. The rate of false-positive recalls was similar for the two modalities – 53 cases for tomosynthesis, versus 63 for ultrasound (P = .26). Rates of false-positive recalls leading to biopsy also were similar. Needle biopsies usually sufficed in recalled cases, but two women underwent surgical biopsies, both of which revealed radial scars.
If the final results of ASTOUND confirm these interim data, “it could be argued that breast tomosynthesis has little value in a setting where adjunct ultrasound is frequently used for screening women with mammography-dense breasts,” said the researchers. But tomosynthesis may have a role as a primary screening modality in other setting, especially because tomosynthesis acquisitions that also provide reconstructed 2D mammography are now available, lessening concerns about unjustified radiation exposure, they added.
The “modest” number of cancers in the interim report led to relatively wide confidence intervals, the investigators noted. Biomarker data were not available for all cancers, and both prevalent and incident ultrasound data were compared with prevalent tomosynthesis data, which might bias false-positive recall results in favor of ultrasound, they added.
Ultrasound was about 1.8 times more sensitive than tomosynthesis for the incremental detection of breast cancer in women with radiologically dense breasts and negative two-dimensional mammography screening, according to interim results from the first prospective trial to directly compare the two modalities.
“However, future application of adjunct screening should consider that tomosynthesis detected more than 50% of the additional breast cancers in these women, and could potentially be [a] primary screening modality,” wrote Dr. Alberto Tagliafico of the University of Genoa (Italy) and his associates. The study was published online March 9 in the Journal of Clinical Oncology and presented simultaneously at the European Breast Cancer Conference.
Radiologically dense breast tissue undermines the sensitivity of mammography and is itself an independent risk factor for breast cancer. Recently, many states began requiring that women be informed of their breast density and adjunct screening measures, such as ultrasound. But estimates of the sensitivity of ultrasound have ranged from about 1.9 to 4.2 cancers for every 1,000 screens, said the researchers. This variance, combined with costs and concerns about false-positive recalls, have fueled debates about the value of adjunct measures in breast cancer screening, they added. To help clarify these issues, the multicenter ASTOUND (Adjunct Screening With Tomosynthesis or Ultrasound in Women With Mammography-Negative Dense Breasts) study compared physician-performed ultrasound and tomosynthesis results for 3,231 asymptomatic women aged 44 to 71 years, whose median age was 51 years (J Clin Oncol. 2016 Mar 9. doi: 10.1200/JCO.2015.63.4147).
In all, the researchers detected 24 additional breast cancers, 23 of which were invasive. Thus, ultrasound detected about 7.1 additional cancers for every 1,000 screens (95% confidence interval, 4.2-10), compared with 4.0 additional cancers per 1,000 screens for tomosynthesis (95% CI, 1.8-6.2; P = .006). Only one cancer was detected by tomosynthesis alone. The rate of false-positive recalls was similar for the two modalities – 53 cases for tomosynthesis, versus 63 for ultrasound (P = .26). Rates of false-positive recalls leading to biopsy also were similar. Needle biopsies usually sufficed in recalled cases, but two women underwent surgical biopsies, both of which revealed radial scars.
If the final results of ASTOUND confirm these interim data, “it could be argued that breast tomosynthesis has little value in a setting where adjunct ultrasound is frequently used for screening women with mammography-dense breasts,” said the researchers. But tomosynthesis may have a role as a primary screening modality in other setting, especially because tomosynthesis acquisitions that also provide reconstructed 2D mammography are now available, lessening concerns about unjustified radiation exposure, they added.
The “modest” number of cancers in the interim report led to relatively wide confidence intervals, the investigators noted. Biomarker data were not available for all cancers, and both prevalent and incident ultrasound data were compared with prevalent tomosynthesis data, which might bias false-positive recall results in favor of ultrasound, they added.
FROM JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Ultrasound outperformed tomosynthesis for the incremental detection of breast cancer in women with negative mammograms and radiologically dense breast tissue.
Major finding: Ultrasound detected about 7.1 additional cancers for every 1,000 screens (95% confidence interval, 4.2-10), compared with 4.0 additional cancers per 1,000 tomosynthesis screens (95% CI, 1.8-6.2; P = .006).
Data source: A multicenter, prospective trial comparing the two modalities in 3,231 women.
Disclosures: The University of Genoa sponsors the ASTOUND study. Dr. Tagliafico disclosed honoraria from Esaote-Philips, patents, royalties, or other intellectual property from Springer, and travel, accommodations, and expense support from Hologic and Technologic. Four coinvestigators reported financial relationships with several device and pharmaceutical companies. The senior author and the other seven coinvestigators had no disclosures.