User login
Ask Alzheimer's Patient Caregiver: Patch or Pill Therapy?
LAS VEGAS – If you’re stumped about which cholinesterase inhibitor to prescribe for your patients with newly diagnosed Alzheimer’s disease, rest assured that the clinical effects are similar with all such agents.
"There is no substantive scientific evidence that says one of the cholinesterase inhibitors is better than another, so get comfortable with one or two of them," Dr. Jeffrey L. Cummings advised during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "The effect is demonstrable late in the disease, so if you take patients with Mini-Mental State Exam scores of less than 10, you still get the same response that you do in somebody whose Mini-Mental State Exam score is 20. There’s no proven effect on the underlying disease state."
Clinical evidence from nearly 20 years of cholinesterase inhibitor use suggests that 25% of patients who take them will experience modest cognitive improvements, defined as a 2-4 point increase on the Alzheimer’s Disease Assessment Scale-cognitive subscale or a 1-2 point increase on the Mini-Mental State Exam. This "makes it very difficult to see a response if it’s not on the upper end of that [response]," Dr. Cummings said. "But about 80% of patients on cholinesterase inhibitors have a delay in decline of 6-9 months. That’s worthwhile, because patients are usually only on therapy for about 5 or 6 years over the course of their disease. So if you can delay almost 20% of that, that’s fantastic."
Dr. Cummings, director of the Cleveland Clinic’s Lou Ruvo Center for Brain Health, lets convenience drive the choice of which cholinesterase inhibitor to prescribe. "I sit with the patient and the caregiver and I ask: ‘Do you want a pill or a transdermal patch?’ If they say, ‘I want a pill,’ I give them donepezil. If they say, ‘I want a patch,’ I give them the rivastigmine transdermal patch," he said.
"I’m trying to respond to the perceived convenience of the caregiver. That’s the question I pose, and those are the two drugs I use."
He went on to note that donepezil "is more likely to give you diarrhea than rivastigmine is, and the rivastigmine patch will give you a rash in 5-10% of patients. Bradycardia is a contraindication for all cholinesterase inhibitors."
Donepezil is available in 5-mg, 10-mg, and 23-mg formulations. The 23-mg form is approved only for patients with moderate to severe disease. "There is more diarrhea with the 23-mg dose; maybe 15% of patients will get diarrhea with that higher dose," he said. "To ameliorate this, for 1 month I have patients go from 10 mg to 15 mg before jumping to the 23-mg dose. I think that helps rather than going directly from 10 mg to 23 mg."
Rivastigmine is approved for mild to moderate Alzheimer’s and for patients with mild to moderate Parkinson’s disease dementia. It’s available in 1.5-mg, 3-mg, 4.5-mg, and 6-mg capsules, or as a 4.6-mg or 9.5-mg transdermal patch.
Galantamine is another cholinesterase inhibitor approved for patients with mild to moderate Alzheimer’s disease, and it has dosing options of 6 mg, 8 mg, or 12 mg b.i.d. Extended formulations are available in 12-mg and 24-mg doses.
The NMDA (N-methyl-d-aspartate) receptor antagonist memantine is also approved for patients with mild to moderate Alzheimer’s, with optimal dosing titration to 10 mg b.i.d. "Side effects are quite rare, but can include somnolence, headache, and dizziness," said Dr. Cummings, who is also chair of neurotherapeutics at the Cleveland Clinic’s Neurological Institute. "Most patients, by the time they reach mid-disease, are on both a cholinesterase inhibitor and memantine."
Other treatment options include the medical foods CerefolinNAC and Axona, which are generally recognized as safe by the Food and Drug Administration and are available by prescription. "No demonstration of clinical benefit is required for these agents," Dr. Cummings said. "The data set supporting medical foods is not as robust as the data set supporting cholinesterase inhibitors."
CerefolinNAC is a combination of vitamin B6, vitamin B12, and folate that Dr. Cummings uses for hyperhomocysteinemia. "I know that high levels of homocysteine are correlated with cognitive impairment, so I try to reduce that by giving CerefolinNAC," he said. "However, there are no data which prove that lowering will necessarily improve the prognosis of the patient. What you are doing is piecing together various types of data to support that use, but it’s not as strong as a double-blind, placebo-controlled trial showing a direct benefit."
Axona is a proprietary formulation of medium-chain triglycerides that increase plasma concentrations of ketone bodies. "This is considered an energy source for neurons," Dr. Cummings said.
Dr. Cummings disclosed that he has provided consultation to the following pharmaceutical companies: Abbott, Acadia, Adamas, Anavex, Astellas, Avanir, Bayer, BMS, Eisai, EnVivo, ExonHit, Janssen, Forest, Genentech, GSK, Lundbeck, Merck, Neurokos, Novartis, Otsuka, Pfizer, Prana, QR Pharma, Sanofi-Aventis, and Takeda.
LAS VEGAS – If you’re stumped about which cholinesterase inhibitor to prescribe for your patients with newly diagnosed Alzheimer’s disease, rest assured that the clinical effects are similar with all such agents.
"There is no substantive scientific evidence that says one of the cholinesterase inhibitors is better than another, so get comfortable with one or two of them," Dr. Jeffrey L. Cummings advised during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "The effect is demonstrable late in the disease, so if you take patients with Mini-Mental State Exam scores of less than 10, you still get the same response that you do in somebody whose Mini-Mental State Exam score is 20. There’s no proven effect on the underlying disease state."
Clinical evidence from nearly 20 years of cholinesterase inhibitor use suggests that 25% of patients who take them will experience modest cognitive improvements, defined as a 2-4 point increase on the Alzheimer’s Disease Assessment Scale-cognitive subscale or a 1-2 point increase on the Mini-Mental State Exam. This "makes it very difficult to see a response if it’s not on the upper end of that [response]," Dr. Cummings said. "But about 80% of patients on cholinesterase inhibitors have a delay in decline of 6-9 months. That’s worthwhile, because patients are usually only on therapy for about 5 or 6 years over the course of their disease. So if you can delay almost 20% of that, that’s fantastic."
Dr. Cummings, director of the Cleveland Clinic’s Lou Ruvo Center for Brain Health, lets convenience drive the choice of which cholinesterase inhibitor to prescribe. "I sit with the patient and the caregiver and I ask: ‘Do you want a pill or a transdermal patch?’ If they say, ‘I want a pill,’ I give them donepezil. If they say, ‘I want a patch,’ I give them the rivastigmine transdermal patch," he said.
"I’m trying to respond to the perceived convenience of the caregiver. That’s the question I pose, and those are the two drugs I use."
He went on to note that donepezil "is more likely to give you diarrhea than rivastigmine is, and the rivastigmine patch will give you a rash in 5-10% of patients. Bradycardia is a contraindication for all cholinesterase inhibitors."
Donepezil is available in 5-mg, 10-mg, and 23-mg formulations. The 23-mg form is approved only for patients with moderate to severe disease. "There is more diarrhea with the 23-mg dose; maybe 15% of patients will get diarrhea with that higher dose," he said. "To ameliorate this, for 1 month I have patients go from 10 mg to 15 mg before jumping to the 23-mg dose. I think that helps rather than going directly from 10 mg to 23 mg."
Rivastigmine is approved for mild to moderate Alzheimer’s and for patients with mild to moderate Parkinson’s disease dementia. It’s available in 1.5-mg, 3-mg, 4.5-mg, and 6-mg capsules, or as a 4.6-mg or 9.5-mg transdermal patch.
Galantamine is another cholinesterase inhibitor approved for patients with mild to moderate Alzheimer’s disease, and it has dosing options of 6 mg, 8 mg, or 12 mg b.i.d. Extended formulations are available in 12-mg and 24-mg doses.
The NMDA (N-methyl-d-aspartate) receptor antagonist memantine is also approved for patients with mild to moderate Alzheimer’s, with optimal dosing titration to 10 mg b.i.d. "Side effects are quite rare, but can include somnolence, headache, and dizziness," said Dr. Cummings, who is also chair of neurotherapeutics at the Cleveland Clinic’s Neurological Institute. "Most patients, by the time they reach mid-disease, are on both a cholinesterase inhibitor and memantine."
Other treatment options include the medical foods CerefolinNAC and Axona, which are generally recognized as safe by the Food and Drug Administration and are available by prescription. "No demonstration of clinical benefit is required for these agents," Dr. Cummings said. "The data set supporting medical foods is not as robust as the data set supporting cholinesterase inhibitors."
CerefolinNAC is a combination of vitamin B6, vitamin B12, and folate that Dr. Cummings uses for hyperhomocysteinemia. "I know that high levels of homocysteine are correlated with cognitive impairment, so I try to reduce that by giving CerefolinNAC," he said. "However, there are no data which prove that lowering will necessarily improve the prognosis of the patient. What you are doing is piecing together various types of data to support that use, but it’s not as strong as a double-blind, placebo-controlled trial showing a direct benefit."
Axona is a proprietary formulation of medium-chain triglycerides that increase plasma concentrations of ketone bodies. "This is considered an energy source for neurons," Dr. Cummings said.
Dr. Cummings disclosed that he has provided consultation to the following pharmaceutical companies: Abbott, Acadia, Adamas, Anavex, Astellas, Avanir, Bayer, BMS, Eisai, EnVivo, ExonHit, Janssen, Forest, Genentech, GSK, Lundbeck, Merck, Neurokos, Novartis, Otsuka, Pfizer, Prana, QR Pharma, Sanofi-Aventis, and Takeda.
LAS VEGAS – If you’re stumped about which cholinesterase inhibitor to prescribe for your patients with newly diagnosed Alzheimer’s disease, rest assured that the clinical effects are similar with all such agents.
"There is no substantive scientific evidence that says one of the cholinesterase inhibitors is better than another, so get comfortable with one or two of them," Dr. Jeffrey L. Cummings advised during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "The effect is demonstrable late in the disease, so if you take patients with Mini-Mental State Exam scores of less than 10, you still get the same response that you do in somebody whose Mini-Mental State Exam score is 20. There’s no proven effect on the underlying disease state."
Clinical evidence from nearly 20 years of cholinesterase inhibitor use suggests that 25% of patients who take them will experience modest cognitive improvements, defined as a 2-4 point increase on the Alzheimer’s Disease Assessment Scale-cognitive subscale or a 1-2 point increase on the Mini-Mental State Exam. This "makes it very difficult to see a response if it’s not on the upper end of that [response]," Dr. Cummings said. "But about 80% of patients on cholinesterase inhibitors have a delay in decline of 6-9 months. That’s worthwhile, because patients are usually only on therapy for about 5 or 6 years over the course of their disease. So if you can delay almost 20% of that, that’s fantastic."
Dr. Cummings, director of the Cleveland Clinic’s Lou Ruvo Center for Brain Health, lets convenience drive the choice of which cholinesterase inhibitor to prescribe. "I sit with the patient and the caregiver and I ask: ‘Do you want a pill or a transdermal patch?’ If they say, ‘I want a pill,’ I give them donepezil. If they say, ‘I want a patch,’ I give them the rivastigmine transdermal patch," he said.
"I’m trying to respond to the perceived convenience of the caregiver. That’s the question I pose, and those are the two drugs I use."
He went on to note that donepezil "is more likely to give you diarrhea than rivastigmine is, and the rivastigmine patch will give you a rash in 5-10% of patients. Bradycardia is a contraindication for all cholinesterase inhibitors."
Donepezil is available in 5-mg, 10-mg, and 23-mg formulations. The 23-mg form is approved only for patients with moderate to severe disease. "There is more diarrhea with the 23-mg dose; maybe 15% of patients will get diarrhea with that higher dose," he said. "To ameliorate this, for 1 month I have patients go from 10 mg to 15 mg before jumping to the 23-mg dose. I think that helps rather than going directly from 10 mg to 23 mg."
Rivastigmine is approved for mild to moderate Alzheimer’s and for patients with mild to moderate Parkinson’s disease dementia. It’s available in 1.5-mg, 3-mg, 4.5-mg, and 6-mg capsules, or as a 4.6-mg or 9.5-mg transdermal patch.
Galantamine is another cholinesterase inhibitor approved for patients with mild to moderate Alzheimer’s disease, and it has dosing options of 6 mg, 8 mg, or 12 mg b.i.d. Extended formulations are available in 12-mg and 24-mg doses.
The NMDA (N-methyl-d-aspartate) receptor antagonist memantine is also approved for patients with mild to moderate Alzheimer’s, with optimal dosing titration to 10 mg b.i.d. "Side effects are quite rare, but can include somnolence, headache, and dizziness," said Dr. Cummings, who is also chair of neurotherapeutics at the Cleveland Clinic’s Neurological Institute. "Most patients, by the time they reach mid-disease, are on both a cholinesterase inhibitor and memantine."
Other treatment options include the medical foods CerefolinNAC and Axona, which are generally recognized as safe by the Food and Drug Administration and are available by prescription. "No demonstration of clinical benefit is required for these agents," Dr. Cummings said. "The data set supporting medical foods is not as robust as the data set supporting cholinesterase inhibitors."
CerefolinNAC is a combination of vitamin B6, vitamin B12, and folate that Dr. Cummings uses for hyperhomocysteinemia. "I know that high levels of homocysteine are correlated with cognitive impairment, so I try to reduce that by giving CerefolinNAC," he said. "However, there are no data which prove that lowering will necessarily improve the prognosis of the patient. What you are doing is piecing together various types of data to support that use, but it’s not as strong as a double-blind, placebo-controlled trial showing a direct benefit."
Axona is a proprietary formulation of medium-chain triglycerides that increase plasma concentrations of ketone bodies. "This is considered an energy source for neurons," Dr. Cummings said.
Dr. Cummings disclosed that he has provided consultation to the following pharmaceutical companies: Abbott, Acadia, Adamas, Anavex, Astellas, Avanir, Bayer, BMS, Eisai, EnVivo, ExonHit, Janssen, Forest, Genentech, GSK, Lundbeck, Merck, Neurokos, Novartis, Otsuka, Pfizer, Prana, QR Pharma, Sanofi-Aventis, and Takeda.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION
Education a Cornerstone of Effective Opioid Management
LAS VEGAS – Even the most careful clinical pain management cannot eliminate the risk of opioid misuse in patients with a history of addiction, but good communication can help reduce the risk significantly, Dr. Sean Mackey said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association.
"Some of the basic tenets of managing patients with chronic opioids are education, education, and education," said Dr. Mackey, chief of the pain management division at Stanford (Calif.) University. "It’s important to set expectations for people with chronic pain. The cure is not the goal; we’re there to help improve quality of life and get people back in control of their lives, better manage pain, and improve physical functioning."
According to best estimates from existing medical literature, the prevalence of comorbid chronic pain and opioid addiction in the United States ranges between 0.6-1.2 million people, mainly affecting young adults and the elderly. But that estimate might be conservative. A June 2011 report from the Institute of Medicine noted that chronic pain affects 116 million Americans – more than the total affected by heart disease, cancer and diabetes combined – at a cost of $560-$630 billion per year. Chronic pain "is the No. 1 reason people are out of work, hitting people often at their most productive ages, and also hitting people more and more as we advance in years," Dr. Mackey said.
In his opinion, optimal management of patients with chronic pain consists of a multidisciplinary approach "in which we bring together specialists who take care of pharmacologic aspects to pain management, physical and occupational therapy approaches, psychological/behavioral approaches, and complementary and alternative medicine approaches. It’s a team-based approach. A lot of this is dealing with body education: helping people understand what is safe for them to do and what is not safe for them to do, alleviating their fears about their body.
"We do procedural approaches as well, everything from simple trigger-point injections to spinal cord stimulation – all in the context of a functional rehabilitation approach."
Psychological approaches include giving patients time-contingent dosing of medications, "on-the-clock rather than when they are experiencing pain," said Dr. Mackey, who also directs the Stanford Systems Neuroscience and Pain Lab. "We also give positive reinforcement for healthy behaviors, negative reinforcement for unhealthy behaviors, and we get their spouse involved, because their involvement is crucial to success."
To responsibly prescribe opioids, Dr. Mackey recommends that physicians become familiar with the Federation of State Medical Boards’ Model Policy for the Treatment of Pain. He also recommends the book "Responsible Opioid Prescribing: A Physician’s Guide," by pain expert Dr. Scott M. Fishman (Waterford, Mich.: Waterford Life Sciences, 2007). This book incorporates the tenets set out in the FSMB’s model policy. "The basic tenet of this model is that pain management is a moral imperative; we should all be aware of the problems of pain management and the use of opioids may be necessary for our patients in pain," Dr. Mackey said.
The model also emphasizes that the use of opioids other than for a legitimate medical purpose "does pose a problem, that we have a responsibility to minimize the abuse and diversion with risk mitigation, [and] that physicians may deviate from recommended treatment when they have good cause. That means we’re not trying to box people in to rigid policies."
His recommended strategy for prescribing opioids in patients with a history of substance abuse starts with a careful assessment and formation of an appropriate differential diagnosis and a psychological assessment, including risk of addictive disorders. Next, have patients sign an informed consent for opioid treatment. "Our consent form has changed somewhat," Dr. Mackey said. "I’m giving patients more information about the potential for organ toxicity and the endocrine abnormalities that can occur as a consequence of opioid use, such as depression of sex hormones."
This is followed by asking patients to sign an opioid treatment agreement that informs them about your standard opioid prescribing policy, such as stating that medication will be refilled during regular office hours, Mondays through Fridays, that lost narcotic medication cannot be replaced, and that stolen narcotic medication may be replaced provided they obtain a police report and are seen in the office.
Dr. Mackey then begins patients on an appropriate trial of opioid therapy with or without adjunctive medications.
"I use the word ‘trial’ because people often think this is meant to be a long-term use of these medications when we try to make it clear right up front that use is for the short term," he explained. "I then assess and reassess their level of pain and function."
He also recommends that clinicians follow the "four As" for ongoing monitoring of pain treatment outcomes, a system developed by Steven D. Passik, Ph.D. These are analgesia (pain relief), activities of daily living (psychosocial functioning), adverse events (side effects), and aberrant drug taking (addiction-related outcomes).
"If you focus on those four As and document them, you can usually stay out of trouble when prescribing these medications," Dr. Mackey said. "Document everything in the medical record, because 95% of the problems that doctors run into with their state medical board have to do with failure to appropriately document."
Other efforts to mitigate risk include using predictive tools, urine drug testing when appropriate, and using your state’s prescription monitoring program. "Use family and friends and others to gather information to make sure that the patient is using the medication appropriately," he advised.
Potential signs of abuse and diversion include patients "who show up at the end of office hours and arrive without an appointment, or who often arrive right when your staff is trying to leave for the day," Dr. Mackey said. "They’re typically reluctant to have a thorough physical exam and don’t give you past medical records, they don’t follow up with appointments, and they have very unusual stories."
Dr. Mackey disclosed that he has received research funding from the National Institutes of Health, the Dodie and John Rosekrans Pain Research Endowment, and the Redlich Pain Research Endowment.
LAS VEGAS – Even the most careful clinical pain management cannot eliminate the risk of opioid misuse in patients with a history of addiction, but good communication can help reduce the risk significantly, Dr. Sean Mackey said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association.
"Some of the basic tenets of managing patients with chronic opioids are education, education, and education," said Dr. Mackey, chief of the pain management division at Stanford (Calif.) University. "It’s important to set expectations for people with chronic pain. The cure is not the goal; we’re there to help improve quality of life and get people back in control of their lives, better manage pain, and improve physical functioning."
According to best estimates from existing medical literature, the prevalence of comorbid chronic pain and opioid addiction in the United States ranges between 0.6-1.2 million people, mainly affecting young adults and the elderly. But that estimate might be conservative. A June 2011 report from the Institute of Medicine noted that chronic pain affects 116 million Americans – more than the total affected by heart disease, cancer and diabetes combined – at a cost of $560-$630 billion per year. Chronic pain "is the No. 1 reason people are out of work, hitting people often at their most productive ages, and also hitting people more and more as we advance in years," Dr. Mackey said.
In his opinion, optimal management of patients with chronic pain consists of a multidisciplinary approach "in which we bring together specialists who take care of pharmacologic aspects to pain management, physical and occupational therapy approaches, psychological/behavioral approaches, and complementary and alternative medicine approaches. It’s a team-based approach. A lot of this is dealing with body education: helping people understand what is safe for them to do and what is not safe for them to do, alleviating their fears about their body.
"We do procedural approaches as well, everything from simple trigger-point injections to spinal cord stimulation – all in the context of a functional rehabilitation approach."
Psychological approaches include giving patients time-contingent dosing of medications, "on-the-clock rather than when they are experiencing pain," said Dr. Mackey, who also directs the Stanford Systems Neuroscience and Pain Lab. "We also give positive reinforcement for healthy behaviors, negative reinforcement for unhealthy behaviors, and we get their spouse involved, because their involvement is crucial to success."
To responsibly prescribe opioids, Dr. Mackey recommends that physicians become familiar with the Federation of State Medical Boards’ Model Policy for the Treatment of Pain. He also recommends the book "Responsible Opioid Prescribing: A Physician’s Guide," by pain expert Dr. Scott M. Fishman (Waterford, Mich.: Waterford Life Sciences, 2007). This book incorporates the tenets set out in the FSMB’s model policy. "The basic tenet of this model is that pain management is a moral imperative; we should all be aware of the problems of pain management and the use of opioids may be necessary for our patients in pain," Dr. Mackey said.
The model also emphasizes that the use of opioids other than for a legitimate medical purpose "does pose a problem, that we have a responsibility to minimize the abuse and diversion with risk mitigation, [and] that physicians may deviate from recommended treatment when they have good cause. That means we’re not trying to box people in to rigid policies."
His recommended strategy for prescribing opioids in patients with a history of substance abuse starts with a careful assessment and formation of an appropriate differential diagnosis and a psychological assessment, including risk of addictive disorders. Next, have patients sign an informed consent for opioid treatment. "Our consent form has changed somewhat," Dr. Mackey said. "I’m giving patients more information about the potential for organ toxicity and the endocrine abnormalities that can occur as a consequence of opioid use, such as depression of sex hormones."
This is followed by asking patients to sign an opioid treatment agreement that informs them about your standard opioid prescribing policy, such as stating that medication will be refilled during regular office hours, Mondays through Fridays, that lost narcotic medication cannot be replaced, and that stolen narcotic medication may be replaced provided they obtain a police report and are seen in the office.
Dr. Mackey then begins patients on an appropriate trial of opioid therapy with or without adjunctive medications.
"I use the word ‘trial’ because people often think this is meant to be a long-term use of these medications when we try to make it clear right up front that use is for the short term," he explained. "I then assess and reassess their level of pain and function."
He also recommends that clinicians follow the "four As" for ongoing monitoring of pain treatment outcomes, a system developed by Steven D. Passik, Ph.D. These are analgesia (pain relief), activities of daily living (psychosocial functioning), adverse events (side effects), and aberrant drug taking (addiction-related outcomes).
"If you focus on those four As and document them, you can usually stay out of trouble when prescribing these medications," Dr. Mackey said. "Document everything in the medical record, because 95% of the problems that doctors run into with their state medical board have to do with failure to appropriately document."
Other efforts to mitigate risk include using predictive tools, urine drug testing when appropriate, and using your state’s prescription monitoring program. "Use family and friends and others to gather information to make sure that the patient is using the medication appropriately," he advised.
Potential signs of abuse and diversion include patients "who show up at the end of office hours and arrive without an appointment, or who often arrive right when your staff is trying to leave for the day," Dr. Mackey said. "They’re typically reluctant to have a thorough physical exam and don’t give you past medical records, they don’t follow up with appointments, and they have very unusual stories."
Dr. Mackey disclosed that he has received research funding from the National Institutes of Health, the Dodie and John Rosekrans Pain Research Endowment, and the Redlich Pain Research Endowment.
LAS VEGAS – Even the most careful clinical pain management cannot eliminate the risk of opioid misuse in patients with a history of addiction, but good communication can help reduce the risk significantly, Dr. Sean Mackey said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association.
"Some of the basic tenets of managing patients with chronic opioids are education, education, and education," said Dr. Mackey, chief of the pain management division at Stanford (Calif.) University. "It’s important to set expectations for people with chronic pain. The cure is not the goal; we’re there to help improve quality of life and get people back in control of their lives, better manage pain, and improve physical functioning."
According to best estimates from existing medical literature, the prevalence of comorbid chronic pain and opioid addiction in the United States ranges between 0.6-1.2 million people, mainly affecting young adults and the elderly. But that estimate might be conservative. A June 2011 report from the Institute of Medicine noted that chronic pain affects 116 million Americans – more than the total affected by heart disease, cancer and diabetes combined – at a cost of $560-$630 billion per year. Chronic pain "is the No. 1 reason people are out of work, hitting people often at their most productive ages, and also hitting people more and more as we advance in years," Dr. Mackey said.
In his opinion, optimal management of patients with chronic pain consists of a multidisciplinary approach "in which we bring together specialists who take care of pharmacologic aspects to pain management, physical and occupational therapy approaches, psychological/behavioral approaches, and complementary and alternative medicine approaches. It’s a team-based approach. A lot of this is dealing with body education: helping people understand what is safe for them to do and what is not safe for them to do, alleviating their fears about their body.
"We do procedural approaches as well, everything from simple trigger-point injections to spinal cord stimulation – all in the context of a functional rehabilitation approach."
Psychological approaches include giving patients time-contingent dosing of medications, "on-the-clock rather than when they are experiencing pain," said Dr. Mackey, who also directs the Stanford Systems Neuroscience and Pain Lab. "We also give positive reinforcement for healthy behaviors, negative reinforcement for unhealthy behaviors, and we get their spouse involved, because their involvement is crucial to success."
To responsibly prescribe opioids, Dr. Mackey recommends that physicians become familiar with the Federation of State Medical Boards’ Model Policy for the Treatment of Pain. He also recommends the book "Responsible Opioid Prescribing: A Physician’s Guide," by pain expert Dr. Scott M. Fishman (Waterford, Mich.: Waterford Life Sciences, 2007). This book incorporates the tenets set out in the FSMB’s model policy. "The basic tenet of this model is that pain management is a moral imperative; we should all be aware of the problems of pain management and the use of opioids may be necessary for our patients in pain," Dr. Mackey said.
The model also emphasizes that the use of opioids other than for a legitimate medical purpose "does pose a problem, that we have a responsibility to minimize the abuse and diversion with risk mitigation, [and] that physicians may deviate from recommended treatment when they have good cause. That means we’re not trying to box people in to rigid policies."
His recommended strategy for prescribing opioids in patients with a history of substance abuse starts with a careful assessment and formation of an appropriate differential diagnosis and a psychological assessment, including risk of addictive disorders. Next, have patients sign an informed consent for opioid treatment. "Our consent form has changed somewhat," Dr. Mackey said. "I’m giving patients more information about the potential for organ toxicity and the endocrine abnormalities that can occur as a consequence of opioid use, such as depression of sex hormones."
This is followed by asking patients to sign an opioid treatment agreement that informs them about your standard opioid prescribing policy, such as stating that medication will be refilled during regular office hours, Mondays through Fridays, that lost narcotic medication cannot be replaced, and that stolen narcotic medication may be replaced provided they obtain a police report and are seen in the office.
Dr. Mackey then begins patients on an appropriate trial of opioid therapy with or without adjunctive medications.
"I use the word ‘trial’ because people often think this is meant to be a long-term use of these medications when we try to make it clear right up front that use is for the short term," he explained. "I then assess and reassess their level of pain and function."
He also recommends that clinicians follow the "four As" for ongoing monitoring of pain treatment outcomes, a system developed by Steven D. Passik, Ph.D. These are analgesia (pain relief), activities of daily living (psychosocial functioning), adverse events (side effects), and aberrant drug taking (addiction-related outcomes).
"If you focus on those four As and document them, you can usually stay out of trouble when prescribing these medications," Dr. Mackey said. "Document everything in the medical record, because 95% of the problems that doctors run into with their state medical board have to do with failure to appropriately document."
Other efforts to mitigate risk include using predictive tools, urine drug testing when appropriate, and using your state’s prescription monitoring program. "Use family and friends and others to gather information to make sure that the patient is using the medication appropriately," he advised.
Potential signs of abuse and diversion include patients "who show up at the end of office hours and arrive without an appointment, or who often arrive right when your staff is trying to leave for the day," Dr. Mackey said. "They’re typically reluctant to have a thorough physical exam and don’t give you past medical records, they don’t follow up with appointments, and they have very unusual stories."
Dr. Mackey disclosed that he has received research funding from the National Institutes of Health, the Dodie and John Rosekrans Pain Research Endowment, and the Redlich Pain Research Endowment.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION
Five Factors Flag Antipsychotic Prescribing for Teens
LAS VEGAS – Nearly 45% of children and adolescents admitted as inpatients to a psychiatric hospital were prescribed antipsychotics over a 10-year period.
The top five variables significantly associated with use of antipsychotics were a diagnosis of psychosis (odds ratio, 7.2), taking anticonvulsants (OR, 2.7), taking lithium (OR, 2.5), having posttraumatic stress disorder (PTSD; OR, 2.3), and taking benzodiazepines (OR, 2.0).
Those are key findings from a single-center study that set out to examine antipsychotic prescribing practices for patients under age 18 between 2000 and 2010. The study, thought to be the largest of its kind, was undertaken at the Hartford, Conn.–based Institute of Living, part of Hartford Hospital.
"This is an important issue because these antipsychotic medications are commonly prescribed," Dr. John W. Goethe said at a psychopharmacology conference sponsored by the Nevada Psychiatric Association. The amount of published data about antipsychotic use in children and adolescents who are inpatients is scant, he said. Most of the literature has focused on outpatients.
In addition, Dr. Goethe said, antipsychotics are commonly used for indications that have not been approved by the Food and Drug Administration. The clinical rationale for this type of use is not well understood
Dr. Goethe, director of the Burlingame Center for Psychiatric Research and Education at the Institute of Living, went on to note that outpatient visit rates for second-generation antipsychotics quadrupled between 1997 and 2002. As a result, he said, concern has been rising about the metabolic syndrome side effects of the second-generation antipsychotics, and about the cardiovascular and hepatic effects of these drugs. Prolonged elevations of prolactin also have occurred as a side effect of some of these drugs. The literature documenting concern about the use of these drugs in children and adolescents is extensive, he said.
Using a computerized clinical evaluation and monitoring system that has been employed at the institute since 2000, Dr. Goethe and his associates analyzed antipsychotic prescribing practices in 3,851 consecutive inpatient admissions of children and adolescents aged 5-17 years. They also examined a subsample of 2,816 patients for whom antipsychotic dose at discharge was available. In addition, they examined two subsamples to determine changes in prescribing patterns over time: a group of 1,422 patients between 2000 and 2003, and a group of 2,120 patients between 2006 and 2010. Data collected included age, gender, race/ethnicity, clinical diagnosis, antipsychotic type at discharge, antipsychotic dose at discharge, use of other psychotropic medications at discharge, and length of stay.
The mean age of the 3,851 patients was 14 years. Of these, 74% were adolescents aged 13-17 years, and 26% were children aged 5-12 years. A slightly higher proportion of the patients was girls (51%). However, there were significantly more boys than girls among the 5- to 12-year-olds (67% vs. 33%, respectively), and significantly more girls than boys among the 13- to 17-year-olds (58% vs. 42%).
More than half of all the patients (56%) were white, 24% were Latino, 12% were black, and the remaining 8% were from other ethnic groups.
By diagnostic category, 40.7% had psychosis, 20.7% had behavioral disorders, 17.7% had mood disorders, 17% had PTSD, 2.9% had other anxiety disorders, and 0.9% had other disorders.
Dr. Goethe reported that the prevalence of antipsychotic use was 44% overall, and was higher among children than adolescents (52% vs. 42%, respectively). The top five antipsychotics used and the mean dosing at discharge were aripiprazole (11.8 mg), quetiapine (205.9 mg), risperidone (1.5 mg), chlorpromazine (146.1 mg), and ziprasidone (82.1 mg).
Second-generation antipsychotics (SGAs) were prescribed in 94.1% of cases. Of those prescribed SGAs, 3.6% of the overall sample of children and adolescents also received first-generation antipsychotics (FGAs). However, the use of FGAs in children was 7.5%. "We were surprised at this finding but could not determine from the data a reason for this difference," Dr. Goethe said in a later interview.
By diagnostic category, 77% of patients with a psychosis diagnosis received an antipsychotic, compared with 46% of those with PTSD, 45% of those with a behavioral disorder, 31% of those with other anxiety disorders, 24% of those who had a mood disorder without psychosis, and 20% who had other disorders.
Among the 1,707 patients who received an antipsychotic, the four most commonly coprescribed psychotropic agents were antidepressants (58%), anticonvulsants (31%), lithium (8%), and benzodiazepines (7%).
Hospital length of stay was significantly longer for children and adolescents who received antipsychotics than for those who did not: 19 vs. 11 days, respectively, in those with psychosis; 14 vs. 7 days in those with a mood disorder without psychosis; 20 vs. 8 days in those with a behavioral disorder; and 22 vs. 10 days among those with PTSD.
Variables significantly associated with antipsychotic use included a diagnosis of psychosis (odds ratio, 7.2), taking anticonvulsants (OR, 2.7), taking lithium (OR, 2.5), having PTSD (OR, 2.3), taking benzodiazepines (OR, 2.0), having a diagnosis of behavioral disorder (OR, 1.93), taking antidepressants (OR, 1.8), and being male (OR, 1.76).
More than three-quarters of patients (82%) received one of the three antipsychotics approved for some indication for patients under age 18 (aripiprazole, quetiapine, and risperidone). However, in 92% of all patients the antipsychotic was still "off label" based on the patient’s age and/or diagnosis.
Use of antipsychotics did not change significantly over the two time periods (47% in the earlier time period vs. 44% in the later time period). There were no significant changes in antipsychotic use for any diagnostic group.
"The prevalence of antipsychotic use varies widely by diagnosis and several other parameters," Dr. Goethe concluded. "Some of these are new findings, and to us they further support the need for clarity and uniformity in reporting prevalence [of antipsychotic use in children and adolescents], both overall and with respect to off-label use.
"We need common definitions, and we need to have clarity about when we’re quoting FDA guidelines and when we are quoting generally accepted guidelines," he said. "The specific antipsychotics that were used were not surprising with regard to the data about second-generation drugs, but were about first-generation drugs."
Also, the high rate of off-label use "was expected, and these findings are consistent with previous reports," he continued. "Calculating off-label prevalence is complicated because definitions vary widely; FDA-approved indications change over time; and some of the reported rates in the literature are misleading in that you can read the rates as reflecting FDA approval, but in fact what they’re reporting is being consistent with or not being consistent with one or more of the published guidelines, so we need to be clear about that."
Dr. Goethe acknowledged certain limitations of the study. It was conducted on a single site, some relevant variables might not have been included, and no posthospital follow-up was conducted. "We are assuming that the discharge medication was one that would be continued, but we don’t know that for a fact," he said. "Further research in this area is needed."
The study was funded by the Burlingame Center Endowment and the Hartford Hospital Research Fund. Dr. Goethe disclosed that he also has received research support from the National Institutes of Health, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Eisai, Hoffmann-La Roche, Shire, Schering-Plough, Johnson & Johnson, Merck, Neuronetics, Novartis, Otsuka, Pfizer, and Takeda.
LAS VEGAS – Nearly 45% of children and adolescents admitted as inpatients to a psychiatric hospital were prescribed antipsychotics over a 10-year period.
The top five variables significantly associated with use of antipsychotics were a diagnosis of psychosis (odds ratio, 7.2), taking anticonvulsants (OR, 2.7), taking lithium (OR, 2.5), having posttraumatic stress disorder (PTSD; OR, 2.3), and taking benzodiazepines (OR, 2.0).
Those are key findings from a single-center study that set out to examine antipsychotic prescribing practices for patients under age 18 between 2000 and 2010. The study, thought to be the largest of its kind, was undertaken at the Hartford, Conn.–based Institute of Living, part of Hartford Hospital.
"This is an important issue because these antipsychotic medications are commonly prescribed," Dr. John W. Goethe said at a psychopharmacology conference sponsored by the Nevada Psychiatric Association. The amount of published data about antipsychotic use in children and adolescents who are inpatients is scant, he said. Most of the literature has focused on outpatients.
In addition, Dr. Goethe said, antipsychotics are commonly used for indications that have not been approved by the Food and Drug Administration. The clinical rationale for this type of use is not well understood
Dr. Goethe, director of the Burlingame Center for Psychiatric Research and Education at the Institute of Living, went on to note that outpatient visit rates for second-generation antipsychotics quadrupled between 1997 and 2002. As a result, he said, concern has been rising about the metabolic syndrome side effects of the second-generation antipsychotics, and about the cardiovascular and hepatic effects of these drugs. Prolonged elevations of prolactin also have occurred as a side effect of some of these drugs. The literature documenting concern about the use of these drugs in children and adolescents is extensive, he said.
Using a computerized clinical evaluation and monitoring system that has been employed at the institute since 2000, Dr. Goethe and his associates analyzed antipsychotic prescribing practices in 3,851 consecutive inpatient admissions of children and adolescents aged 5-17 years. They also examined a subsample of 2,816 patients for whom antipsychotic dose at discharge was available. In addition, they examined two subsamples to determine changes in prescribing patterns over time: a group of 1,422 patients between 2000 and 2003, and a group of 2,120 patients between 2006 and 2010. Data collected included age, gender, race/ethnicity, clinical diagnosis, antipsychotic type at discharge, antipsychotic dose at discharge, use of other psychotropic medications at discharge, and length of stay.
The mean age of the 3,851 patients was 14 years. Of these, 74% were adolescents aged 13-17 years, and 26% were children aged 5-12 years. A slightly higher proportion of the patients was girls (51%). However, there were significantly more boys than girls among the 5- to 12-year-olds (67% vs. 33%, respectively), and significantly more girls than boys among the 13- to 17-year-olds (58% vs. 42%).
More than half of all the patients (56%) were white, 24% were Latino, 12% were black, and the remaining 8% were from other ethnic groups.
By diagnostic category, 40.7% had psychosis, 20.7% had behavioral disorders, 17.7% had mood disorders, 17% had PTSD, 2.9% had other anxiety disorders, and 0.9% had other disorders.
Dr. Goethe reported that the prevalence of antipsychotic use was 44% overall, and was higher among children than adolescents (52% vs. 42%, respectively). The top five antipsychotics used and the mean dosing at discharge were aripiprazole (11.8 mg), quetiapine (205.9 mg), risperidone (1.5 mg), chlorpromazine (146.1 mg), and ziprasidone (82.1 mg).
Second-generation antipsychotics (SGAs) were prescribed in 94.1% of cases. Of those prescribed SGAs, 3.6% of the overall sample of children and adolescents also received first-generation antipsychotics (FGAs). However, the use of FGAs in children was 7.5%. "We were surprised at this finding but could not determine from the data a reason for this difference," Dr. Goethe said in a later interview.
By diagnostic category, 77% of patients with a psychosis diagnosis received an antipsychotic, compared with 46% of those with PTSD, 45% of those with a behavioral disorder, 31% of those with other anxiety disorders, 24% of those who had a mood disorder without psychosis, and 20% who had other disorders.
Among the 1,707 patients who received an antipsychotic, the four most commonly coprescribed psychotropic agents were antidepressants (58%), anticonvulsants (31%), lithium (8%), and benzodiazepines (7%).
Hospital length of stay was significantly longer for children and adolescents who received antipsychotics than for those who did not: 19 vs. 11 days, respectively, in those with psychosis; 14 vs. 7 days in those with a mood disorder without psychosis; 20 vs. 8 days in those with a behavioral disorder; and 22 vs. 10 days among those with PTSD.
Variables significantly associated with antipsychotic use included a diagnosis of psychosis (odds ratio, 7.2), taking anticonvulsants (OR, 2.7), taking lithium (OR, 2.5), having PTSD (OR, 2.3), taking benzodiazepines (OR, 2.0), having a diagnosis of behavioral disorder (OR, 1.93), taking antidepressants (OR, 1.8), and being male (OR, 1.76).
More than three-quarters of patients (82%) received one of the three antipsychotics approved for some indication for patients under age 18 (aripiprazole, quetiapine, and risperidone). However, in 92% of all patients the antipsychotic was still "off label" based on the patient’s age and/or diagnosis.
Use of antipsychotics did not change significantly over the two time periods (47% in the earlier time period vs. 44% in the later time period). There were no significant changes in antipsychotic use for any diagnostic group.
"The prevalence of antipsychotic use varies widely by diagnosis and several other parameters," Dr. Goethe concluded. "Some of these are new findings, and to us they further support the need for clarity and uniformity in reporting prevalence [of antipsychotic use in children and adolescents], both overall and with respect to off-label use.
"We need common definitions, and we need to have clarity about when we’re quoting FDA guidelines and when we are quoting generally accepted guidelines," he said. "The specific antipsychotics that were used were not surprising with regard to the data about second-generation drugs, but were about first-generation drugs."
Also, the high rate of off-label use "was expected, and these findings are consistent with previous reports," he continued. "Calculating off-label prevalence is complicated because definitions vary widely; FDA-approved indications change over time; and some of the reported rates in the literature are misleading in that you can read the rates as reflecting FDA approval, but in fact what they’re reporting is being consistent with or not being consistent with one or more of the published guidelines, so we need to be clear about that."
Dr. Goethe acknowledged certain limitations of the study. It was conducted on a single site, some relevant variables might not have been included, and no posthospital follow-up was conducted. "We are assuming that the discharge medication was one that would be continued, but we don’t know that for a fact," he said. "Further research in this area is needed."
The study was funded by the Burlingame Center Endowment and the Hartford Hospital Research Fund. Dr. Goethe disclosed that he also has received research support from the National Institutes of Health, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Eisai, Hoffmann-La Roche, Shire, Schering-Plough, Johnson & Johnson, Merck, Neuronetics, Novartis, Otsuka, Pfizer, and Takeda.
LAS VEGAS – Nearly 45% of children and adolescents admitted as inpatients to a psychiatric hospital were prescribed antipsychotics over a 10-year period.
The top five variables significantly associated with use of antipsychotics were a diagnosis of psychosis (odds ratio, 7.2), taking anticonvulsants (OR, 2.7), taking lithium (OR, 2.5), having posttraumatic stress disorder (PTSD; OR, 2.3), and taking benzodiazepines (OR, 2.0).
Those are key findings from a single-center study that set out to examine antipsychotic prescribing practices for patients under age 18 between 2000 and 2010. The study, thought to be the largest of its kind, was undertaken at the Hartford, Conn.–based Institute of Living, part of Hartford Hospital.
"This is an important issue because these antipsychotic medications are commonly prescribed," Dr. John W. Goethe said at a psychopharmacology conference sponsored by the Nevada Psychiatric Association. The amount of published data about antipsychotic use in children and adolescents who are inpatients is scant, he said. Most of the literature has focused on outpatients.
In addition, Dr. Goethe said, antipsychotics are commonly used for indications that have not been approved by the Food and Drug Administration. The clinical rationale for this type of use is not well understood
Dr. Goethe, director of the Burlingame Center for Psychiatric Research and Education at the Institute of Living, went on to note that outpatient visit rates for second-generation antipsychotics quadrupled between 1997 and 2002. As a result, he said, concern has been rising about the metabolic syndrome side effects of the second-generation antipsychotics, and about the cardiovascular and hepatic effects of these drugs. Prolonged elevations of prolactin also have occurred as a side effect of some of these drugs. The literature documenting concern about the use of these drugs in children and adolescents is extensive, he said.
Using a computerized clinical evaluation and monitoring system that has been employed at the institute since 2000, Dr. Goethe and his associates analyzed antipsychotic prescribing practices in 3,851 consecutive inpatient admissions of children and adolescents aged 5-17 years. They also examined a subsample of 2,816 patients for whom antipsychotic dose at discharge was available. In addition, they examined two subsamples to determine changes in prescribing patterns over time: a group of 1,422 patients between 2000 and 2003, and a group of 2,120 patients between 2006 and 2010. Data collected included age, gender, race/ethnicity, clinical diagnosis, antipsychotic type at discharge, antipsychotic dose at discharge, use of other psychotropic medications at discharge, and length of stay.
The mean age of the 3,851 patients was 14 years. Of these, 74% were adolescents aged 13-17 years, and 26% were children aged 5-12 years. A slightly higher proportion of the patients was girls (51%). However, there were significantly more boys than girls among the 5- to 12-year-olds (67% vs. 33%, respectively), and significantly more girls than boys among the 13- to 17-year-olds (58% vs. 42%).
More than half of all the patients (56%) were white, 24% were Latino, 12% were black, and the remaining 8% were from other ethnic groups.
By diagnostic category, 40.7% had psychosis, 20.7% had behavioral disorders, 17.7% had mood disorders, 17% had PTSD, 2.9% had other anxiety disorders, and 0.9% had other disorders.
Dr. Goethe reported that the prevalence of antipsychotic use was 44% overall, and was higher among children than adolescents (52% vs. 42%, respectively). The top five antipsychotics used and the mean dosing at discharge were aripiprazole (11.8 mg), quetiapine (205.9 mg), risperidone (1.5 mg), chlorpromazine (146.1 mg), and ziprasidone (82.1 mg).
Second-generation antipsychotics (SGAs) were prescribed in 94.1% of cases. Of those prescribed SGAs, 3.6% of the overall sample of children and adolescents also received first-generation antipsychotics (FGAs). However, the use of FGAs in children was 7.5%. "We were surprised at this finding but could not determine from the data a reason for this difference," Dr. Goethe said in a later interview.
By diagnostic category, 77% of patients with a psychosis diagnosis received an antipsychotic, compared with 46% of those with PTSD, 45% of those with a behavioral disorder, 31% of those with other anxiety disorders, 24% of those who had a mood disorder without psychosis, and 20% who had other disorders.
Among the 1,707 patients who received an antipsychotic, the four most commonly coprescribed psychotropic agents were antidepressants (58%), anticonvulsants (31%), lithium (8%), and benzodiazepines (7%).
Hospital length of stay was significantly longer for children and adolescents who received antipsychotics than for those who did not: 19 vs. 11 days, respectively, in those with psychosis; 14 vs. 7 days in those with a mood disorder without psychosis; 20 vs. 8 days in those with a behavioral disorder; and 22 vs. 10 days among those with PTSD.
Variables significantly associated with antipsychotic use included a diagnosis of psychosis (odds ratio, 7.2), taking anticonvulsants (OR, 2.7), taking lithium (OR, 2.5), having PTSD (OR, 2.3), taking benzodiazepines (OR, 2.0), having a diagnosis of behavioral disorder (OR, 1.93), taking antidepressants (OR, 1.8), and being male (OR, 1.76).
More than three-quarters of patients (82%) received one of the three antipsychotics approved for some indication for patients under age 18 (aripiprazole, quetiapine, and risperidone). However, in 92% of all patients the antipsychotic was still "off label" based on the patient’s age and/or diagnosis.
Use of antipsychotics did not change significantly over the two time periods (47% in the earlier time period vs. 44% in the later time period). There were no significant changes in antipsychotic use for any diagnostic group.
"The prevalence of antipsychotic use varies widely by diagnosis and several other parameters," Dr. Goethe concluded. "Some of these are new findings, and to us they further support the need for clarity and uniformity in reporting prevalence [of antipsychotic use in children and adolescents], both overall and with respect to off-label use.
"We need common definitions, and we need to have clarity about when we’re quoting FDA guidelines and when we are quoting generally accepted guidelines," he said. "The specific antipsychotics that were used were not surprising with regard to the data about second-generation drugs, but were about first-generation drugs."
Also, the high rate of off-label use "was expected, and these findings are consistent with previous reports," he continued. "Calculating off-label prevalence is complicated because definitions vary widely; FDA-approved indications change over time; and some of the reported rates in the literature are misleading in that you can read the rates as reflecting FDA approval, but in fact what they’re reporting is being consistent with or not being consistent with one or more of the published guidelines, so we need to be clear about that."
Dr. Goethe acknowledged certain limitations of the study. It was conducted on a single site, some relevant variables might not have been included, and no posthospital follow-up was conducted. "We are assuming that the discharge medication was one that would be continued, but we don’t know that for a fact," he said. "Further research in this area is needed."
The study was funded by the Burlingame Center Endowment and the Hartford Hospital Research Fund. Dr. Goethe disclosed that he also has received research support from the National Institutes of Health, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Eisai, Hoffmann-La Roche, Shire, Schering-Plough, Johnson & Johnson, Merck, Neuronetics, Novartis, Otsuka, Pfizer, and Takeda.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION
What to Do When Common Dysthymia Treatments Fail
LAS VEGAS – When it comes to the pharmacologic treatment of patients with dysthymic disorder, the best scientific evidence points to selective serotonin reuptake inhibitors as a first-line treatment, Dr. Hagop S. Akiskal said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. This includes fluoxetine, sertraline, and citalopram, to a maximum of 40 mg/per day.
Suggested second-line interventions include mirtazapine, duloxetine, venlafaxine, and bupropion, said Dr. Akiskal, professor of psychiatry at the University of California, San Diego.
When first- and second-line interventions for dysthymic disorder fail, consider trying the tricyclic antidepressants desipramine or nortriptyline. Another option is the reversible monoamine oxidase inhibitor (MAOI) moclobemide, though this agent is not approved for use in the United States. "Don’t forget phenelzine and tranylcypromine, with certain dietary/pharmacologic restrictions," Dr. Akiskal said. "There’s also selegiline, which has been used for a long time to treat Parkinson’s disease, but it’s controversial as to whether dietary and pharmacologic restrictions should be as vigorous with this agent as with phenelzine and tranylcypromine. I would use it thinking it’s less problematic than those two agents, but still be on your guard."
He went on to highlight certain dietary and drug restrictions with irreversible MAOIs to avoid hypertensive crises. These include aged cheeses, concentrated yeast extracts, sauerkraut, broad bean pods, tap beers (though other alcoholic beverages "might be safe if consumed in moderation"), some aged meats, which "contain relatively high levels of tyramine and require closer scrutiny," pickled fish, and concomitant serotonergic antidepressants.
Dr. Akiskal, who is also editor in chief of the Journal of Affective Disorders, noted that dysthymic disorder shares many similarities to major depressive disorder, including a familial association, phase advance of REM sleep, diurnal variation, effects on thyroid-stimulating hormone and thyrotropin-releasing hormone, elevated levels of plasma corticotrophin-releasing factor, sleep deprivation response, response to antidepressants, and treatment-emergent hypomania.
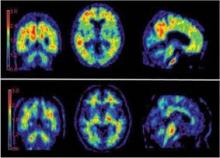
On functional MRI, dysthymic patients show significantly more right amygdala, right thalamic, right fusiform gyrus, and left cerebellar activity, compared with controls for the negative-neutral contrast. "The point is, dysthymia is presented in the brain; it’s not in the ‘mind’ of the patient," Dr. Akiskal said.
Dr. Akiskal disclosed that he is a consultant for the Lilly and the Lundbeck foundations. He also is a member of the speakers bureau for AstraZeneca, BioMarin, Bristol-Meyers Squibb, Dey Pharma, GlaxoSmithKline, Merck, and Sanofi.
LAS VEGAS – When it comes to the pharmacologic treatment of patients with dysthymic disorder, the best scientific evidence points to selective serotonin reuptake inhibitors as a first-line treatment, Dr. Hagop S. Akiskal said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. This includes fluoxetine, sertraline, and citalopram, to a maximum of 40 mg/per day.
Suggested second-line interventions include mirtazapine, duloxetine, venlafaxine, and bupropion, said Dr. Akiskal, professor of psychiatry at the University of California, San Diego.
When first- and second-line interventions for dysthymic disorder fail, consider trying the tricyclic antidepressants desipramine or nortriptyline. Another option is the reversible monoamine oxidase inhibitor (MAOI) moclobemide, though this agent is not approved for use in the United States. "Don’t forget phenelzine and tranylcypromine, with certain dietary/pharmacologic restrictions," Dr. Akiskal said. "There’s also selegiline, which has been used for a long time to treat Parkinson’s disease, but it’s controversial as to whether dietary and pharmacologic restrictions should be as vigorous with this agent as with phenelzine and tranylcypromine. I would use it thinking it’s less problematic than those two agents, but still be on your guard."
He went on to highlight certain dietary and drug restrictions with irreversible MAOIs to avoid hypertensive crises. These include aged cheeses, concentrated yeast extracts, sauerkraut, broad bean pods, tap beers (though other alcoholic beverages "might be safe if consumed in moderation"), some aged meats, which "contain relatively high levels of tyramine and require closer scrutiny," pickled fish, and concomitant serotonergic antidepressants.
Dr. Akiskal, who is also editor in chief of the Journal of Affective Disorders, noted that dysthymic disorder shares many similarities to major depressive disorder, including a familial association, phase advance of REM sleep, diurnal variation, effects on thyroid-stimulating hormone and thyrotropin-releasing hormone, elevated levels of plasma corticotrophin-releasing factor, sleep deprivation response, response to antidepressants, and treatment-emergent hypomania.
On functional MRI, dysthymic patients show significantly more right amygdala, right thalamic, right fusiform gyrus, and left cerebellar activity, compared with controls for the negative-neutral contrast. "The point is, dysthymia is presented in the brain; it’s not in the ‘mind’ of the patient," Dr. Akiskal said.
Dr. Akiskal disclosed that he is a consultant for the Lilly and the Lundbeck foundations. He also is a member of the speakers bureau for AstraZeneca, BioMarin, Bristol-Meyers Squibb, Dey Pharma, GlaxoSmithKline, Merck, and Sanofi.
LAS VEGAS – When it comes to the pharmacologic treatment of patients with dysthymic disorder, the best scientific evidence points to selective serotonin reuptake inhibitors as a first-line treatment, Dr. Hagop S. Akiskal said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. This includes fluoxetine, sertraline, and citalopram, to a maximum of 40 mg/per day.
Suggested second-line interventions include mirtazapine, duloxetine, venlafaxine, and bupropion, said Dr. Akiskal, professor of psychiatry at the University of California, San Diego.
When first- and second-line interventions for dysthymic disorder fail, consider trying the tricyclic antidepressants desipramine or nortriptyline. Another option is the reversible monoamine oxidase inhibitor (MAOI) moclobemide, though this agent is not approved for use in the United States. "Don’t forget phenelzine and tranylcypromine, with certain dietary/pharmacologic restrictions," Dr. Akiskal said. "There’s also selegiline, which has been used for a long time to treat Parkinson’s disease, but it’s controversial as to whether dietary and pharmacologic restrictions should be as vigorous with this agent as with phenelzine and tranylcypromine. I would use it thinking it’s less problematic than those two agents, but still be on your guard."
He went on to highlight certain dietary and drug restrictions with irreversible MAOIs to avoid hypertensive crises. These include aged cheeses, concentrated yeast extracts, sauerkraut, broad bean pods, tap beers (though other alcoholic beverages "might be safe if consumed in moderation"), some aged meats, which "contain relatively high levels of tyramine and require closer scrutiny," pickled fish, and concomitant serotonergic antidepressants.
Dr. Akiskal, who is also editor in chief of the Journal of Affective Disorders, noted that dysthymic disorder shares many similarities to major depressive disorder, including a familial association, phase advance of REM sleep, diurnal variation, effects on thyroid-stimulating hormone and thyrotropin-releasing hormone, elevated levels of plasma corticotrophin-releasing factor, sleep deprivation response, response to antidepressants, and treatment-emergent hypomania.
On functional MRI, dysthymic patients show significantly more right amygdala, right thalamic, right fusiform gyrus, and left cerebellar activity, compared with controls for the negative-neutral contrast. "The point is, dysthymia is presented in the brain; it’s not in the ‘mind’ of the patient," Dr. Akiskal said.
Dr. Akiskal disclosed that he is a consultant for the Lilly and the Lundbeck foundations. He also is a member of the speakers bureau for AstraZeneca, BioMarin, Bristol-Meyers Squibb, Dey Pharma, GlaxoSmithKline, Merck, and Sanofi.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION
Expert Shares Opioid Addiction Treatment Tips
LAS VEGAS – Methadone and heroin hold two key advantages for treating patients with opioid addiction: They are inexpensive and readily endorsed by addiction patients, according to Dr. Paul H. Earley.
However, the drugs, which are pure agonists, also hold disadvantages.
"Disadvantages include pontine suppression, the potential for overdose, and prolongation of the QT interval, which, in the course of taking methadone, can lead to torsades de pointes," Dr. Earley said at a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "There’s also a lifelong commitment to pure agonists, like an insulin-dependent diabetic," he said. "They create limited mobility, and you have issues with drug diversion."
Dr. Earley, an addiction medicine physician in Atlanta, went on to discuss his approach to using mixed agonists/antagonists and pure antagonists in patients with opioid addiction. The primary mixed agonist/antagonist he uses is buprenorphine (Suboxone and Subutex), which requires a Drug Enforcement Agency waiver to use for addiction treatment.
"The interesting thing about buprenorphine is that it is an agonist at lower doses but develops more antagonist properties at higher doses," he said. "The drug is extremely safe. Overdosing on this is almost impossible, unlike with heroin and methadone. I use it a lot for detoxification but only rarely for maintenance treatment." In addition, buprenorphine can be used off label for patients with pain and addiction issues.
Establishing a clear contract with patients about this type of treatment is imperative, he said.
"My bias is that buprenorphine is not a state of abstinence," Dr. Earley said. "I think people who are on buprenorphine have a drug load, or an agonist on board, and it is classically different from an individual who does not have narcotics on board.
"It is really a more benign form of opioid maintenance therapy. If I’m going to start someone on buprenorphine, I’ll say, ‘Once you get on this drug, it’s easy to get on, but it is hard to get off of.’ It’s difficult to taper, especially the last few milligrams."
The advantages of mixed agonists/antagonists, he continued, include quick acceptance by patients, and fewer travel restrictions than exist with methadone. In addition, they’re safer than methadone, especially in regard to respiratory depression.
"The disadvantage is that a careful transition from abusable agonists is critical to prevent the inadvertent precipitation of withdrawal," he said. "Drug diversion is a problem, because these agents have a street value."
Pure antagonists used for the treatment of addiction include oral, subcutaneous pellets, or intramuscular naltrexone (Vivitrol). "The advantages are that there is no drug diversion and that you can discontinue at anytime without withdrawal," Dr. Earley said. "That’s a good thing to be able to tell your patients."
Perhaps the most impressive effect of naltrexone is its effectiveness in suppressing drug cravings, Dr. Earley said. The disadvantages include less ready endorsement by the addict, weak adherence to oral naltrexone on the part of patients, and the delicate balance of transitioning patients from detoxification or maintenance agents.
Drug screening is a central part of any addiction practice, he said. "Do not practice addiction psychiatry if you do not understand screening technology and have a high-quality screening lab behind you," he advised.
Before he switches a patient from an agonist to a partial agonist, Dr. Earley said he waits until the person enters withdrawal. "It is best to follow objective signs such as piloerection and pupillary dilation," he said. "The wait is from 6 hours (hydrocodone) to 5 days (methadone) from last dose, and is dependent on the previous agonist dose and other unknown factors, including patient temperament."
Before he switches a patient from a partial antagonist to an antagonist, Dr. Earley said he coaches the person about what to expect and encourages the presence of a "detoxification coach" in the form of a family member or a friend to sit with that person. "I say, ‘You are going to go through some withdrawal, but when we get you on this antagonist, this will be the last time you go through withdrawal, as long as you stay in recovery.’ That often will help people through the difficult times ahead."
Dr. Earley disclosed that he has been a member of the speakers bureau and has received honoraria from Alkermes.
LAS VEGAS – Methadone and heroin hold two key advantages for treating patients with opioid addiction: They are inexpensive and readily endorsed by addiction patients, according to Dr. Paul H. Earley.
However, the drugs, which are pure agonists, also hold disadvantages.
"Disadvantages include pontine suppression, the potential for overdose, and prolongation of the QT interval, which, in the course of taking methadone, can lead to torsades de pointes," Dr. Earley said at a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "There’s also a lifelong commitment to pure agonists, like an insulin-dependent diabetic," he said. "They create limited mobility, and you have issues with drug diversion."
Dr. Earley, an addiction medicine physician in Atlanta, went on to discuss his approach to using mixed agonists/antagonists and pure antagonists in patients with opioid addiction. The primary mixed agonist/antagonist he uses is buprenorphine (Suboxone and Subutex), which requires a Drug Enforcement Agency waiver to use for addiction treatment.
"The interesting thing about buprenorphine is that it is an agonist at lower doses but develops more antagonist properties at higher doses," he said. "The drug is extremely safe. Overdosing on this is almost impossible, unlike with heroin and methadone. I use it a lot for detoxification but only rarely for maintenance treatment." In addition, buprenorphine can be used off label for patients with pain and addiction issues.
Establishing a clear contract with patients about this type of treatment is imperative, he said.
"My bias is that buprenorphine is not a state of abstinence," Dr. Earley said. "I think people who are on buprenorphine have a drug load, or an agonist on board, and it is classically different from an individual who does not have narcotics on board.
"It is really a more benign form of opioid maintenance therapy. If I’m going to start someone on buprenorphine, I’ll say, ‘Once you get on this drug, it’s easy to get on, but it is hard to get off of.’ It’s difficult to taper, especially the last few milligrams."
The advantages of mixed agonists/antagonists, he continued, include quick acceptance by patients, and fewer travel restrictions than exist with methadone. In addition, they’re safer than methadone, especially in regard to respiratory depression.
"The disadvantage is that a careful transition from abusable agonists is critical to prevent the inadvertent precipitation of withdrawal," he said. "Drug diversion is a problem, because these agents have a street value."
Pure antagonists used for the treatment of addiction include oral, subcutaneous pellets, or intramuscular naltrexone (Vivitrol). "The advantages are that there is no drug diversion and that you can discontinue at anytime without withdrawal," Dr. Earley said. "That’s a good thing to be able to tell your patients."
Perhaps the most impressive effect of naltrexone is its effectiveness in suppressing drug cravings, Dr. Earley said. The disadvantages include less ready endorsement by the addict, weak adherence to oral naltrexone on the part of patients, and the delicate balance of transitioning patients from detoxification or maintenance agents.
Drug screening is a central part of any addiction practice, he said. "Do not practice addiction psychiatry if you do not understand screening technology and have a high-quality screening lab behind you," he advised.
Before he switches a patient from an agonist to a partial agonist, Dr. Earley said he waits until the person enters withdrawal. "It is best to follow objective signs such as piloerection and pupillary dilation," he said. "The wait is from 6 hours (hydrocodone) to 5 days (methadone) from last dose, and is dependent on the previous agonist dose and other unknown factors, including patient temperament."
Before he switches a patient from a partial antagonist to an antagonist, Dr. Earley said he coaches the person about what to expect and encourages the presence of a "detoxification coach" in the form of a family member or a friend to sit with that person. "I say, ‘You are going to go through some withdrawal, but when we get you on this antagonist, this will be the last time you go through withdrawal, as long as you stay in recovery.’ That often will help people through the difficult times ahead."
Dr. Earley disclosed that he has been a member of the speakers bureau and has received honoraria from Alkermes.
LAS VEGAS – Methadone and heroin hold two key advantages for treating patients with opioid addiction: They are inexpensive and readily endorsed by addiction patients, according to Dr. Paul H. Earley.
However, the drugs, which are pure agonists, also hold disadvantages.
"Disadvantages include pontine suppression, the potential for overdose, and prolongation of the QT interval, which, in the course of taking methadone, can lead to torsades de pointes," Dr. Earley said at a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "There’s also a lifelong commitment to pure agonists, like an insulin-dependent diabetic," he said. "They create limited mobility, and you have issues with drug diversion."
Dr. Earley, an addiction medicine physician in Atlanta, went on to discuss his approach to using mixed agonists/antagonists and pure antagonists in patients with opioid addiction. The primary mixed agonist/antagonist he uses is buprenorphine (Suboxone and Subutex), which requires a Drug Enforcement Agency waiver to use for addiction treatment.
"The interesting thing about buprenorphine is that it is an agonist at lower doses but develops more antagonist properties at higher doses," he said. "The drug is extremely safe. Overdosing on this is almost impossible, unlike with heroin and methadone. I use it a lot for detoxification but only rarely for maintenance treatment." In addition, buprenorphine can be used off label for patients with pain and addiction issues.
Establishing a clear contract with patients about this type of treatment is imperative, he said.
"My bias is that buprenorphine is not a state of abstinence," Dr. Earley said. "I think people who are on buprenorphine have a drug load, or an agonist on board, and it is classically different from an individual who does not have narcotics on board.
"It is really a more benign form of opioid maintenance therapy. If I’m going to start someone on buprenorphine, I’ll say, ‘Once you get on this drug, it’s easy to get on, but it is hard to get off of.’ It’s difficult to taper, especially the last few milligrams."
The advantages of mixed agonists/antagonists, he continued, include quick acceptance by patients, and fewer travel restrictions than exist with methadone. In addition, they’re safer than methadone, especially in regard to respiratory depression.
"The disadvantage is that a careful transition from abusable agonists is critical to prevent the inadvertent precipitation of withdrawal," he said. "Drug diversion is a problem, because these agents have a street value."
Pure antagonists used for the treatment of addiction include oral, subcutaneous pellets, or intramuscular naltrexone (Vivitrol). "The advantages are that there is no drug diversion and that you can discontinue at anytime without withdrawal," Dr. Earley said. "That’s a good thing to be able to tell your patients."
Perhaps the most impressive effect of naltrexone is its effectiveness in suppressing drug cravings, Dr. Earley said. The disadvantages include less ready endorsement by the addict, weak adherence to oral naltrexone on the part of patients, and the delicate balance of transitioning patients from detoxification or maintenance agents.
Drug screening is a central part of any addiction practice, he said. "Do not practice addiction psychiatry if you do not understand screening technology and have a high-quality screening lab behind you," he advised.
Before he switches a patient from an agonist to a partial agonist, Dr. Earley said he waits until the person enters withdrawal. "It is best to follow objective signs such as piloerection and pupillary dilation," he said. "The wait is from 6 hours (hydrocodone) to 5 days (methadone) from last dose, and is dependent on the previous agonist dose and other unknown factors, including patient temperament."
Before he switches a patient from a partial antagonist to an antagonist, Dr. Earley said he coaches the person about what to expect and encourages the presence of a "detoxification coach" in the form of a family member or a friend to sit with that person. "I say, ‘You are going to go through some withdrawal, but when we get you on this antagonist, this will be the last time you go through withdrawal, as long as you stay in recovery.’ That often will help people through the difficult times ahead."
Dr. Earley disclosed that he has been a member of the speakers bureau and has received honoraria from Alkermes.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION
Adjunctive Lithium Reduces Use of Newer Antipsychotics in Bipolar
LAS VEGAS – In a 6-month study, the use of adjunctive moderately dosed lithium to optimized treatment in patients with bipolar disorder was well tolerated yet did not lead to improved outcomes or decreased suicidality. However, use of adjunctive lithium resulted in a significant reduction in the use of second-generation antipsychotics.
Those are key findings from the Bipolar Trials Network Lithium Treatment Moderate Dose Study, a randomized trial that compared the use of lithium plus optimized treatment with optimized treatment alone.
"Currently, only about one-third of bipolar patients take lithium," Dr. Michael E. Thase said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "And outpatients uncommonly take lithium in higher, well-established doses. Today it’s more commonly used in moderate doses in combination with newer generation therapies. However, the value of lower dose, combination strategies has not been well-studied."
For the outpatient study, known as the Lithium treatment – moderate dose use study, or LiTMUS, and led by Dr. Andrew A. Nierenberg at the Massachusetts General Hospital, investigators at six clinical sites enrolled 283 patients with bipolar I or bipolar II disorder with a Clinical Global Impressions-Bipolar Scale (CGI-BP-S) score of 3 or greater to assess whether lithium, in moderate doses, "could be a useful platform upon which other newer treatments could be evaluated," said Dr. Thase, professor of psychiatry at the University of Pennsylvania, Philadelphia.
"We were working in partnership with colleagues at the National Institute of Mental Health to do this study in a real-world, relevant way, meaning that it must be inclusive so that people with common comorbidities needed to be in the study, that it needed to be administered in an open way so that the results would be generalizable," said Dr. Thase, who also pointed out that there was no placebo control group.
The investigators compared lithium plus optimized treatment or optimized treatment without lithium. Patients in the lithium arm were started on 300 mg b.i.d. and sustained on 600 mg/day for 8 weeks, adjusted as needed thereafter. The Texas Implementation of Medication Algorithms for bipolar disorder informed care.
The two main outcomes assessed at 6 months were the CGI-BP-S and the number of Necessary Clinical Adjustments (NCAs), a measure of how difficult treatment was to implement. "This takes into account how many times you had to change the treatment in response to side effects or in response to the treatment not working," Dr. Thase explained. "The higher the NCA count, the stormier the treatment course."
A secondary measure was side effect burden as measured by the Frequency and Intensity of Side Effects Ratings, "which provides composite ratings of tolerability rather than focusing on specific side effects," he said. "These were completed at each study visit by the treating psychiatrist."
Dr. Thase reported that 84% of patients completed the 6 months of treatment. The attrition rate was not significantly different among those who received lithium, compared with those who did not receive the drug. The modal dose of lithium was 600 mg/day, and the average lithium levels ranged between 0.5-0.6 mEq/L.
Patients who received lithium did not have better outcomes compared with those who did not in terms of overall change in the CGI-BP-S (–1.5 vs. –1.2, respectively). "The average level of improvement for all of our patients was only about a 30% reduction in symptom burden," Dr. Thase said. "Thus, despite using guideline-based treatment algorithms, more patients remained ill than got better."
No statistically significant differences were found between groups in terms of depression and manic symptom severity based on the CGI-BP-S, the Quick Inventory of Depressive Symptoms Score, the Quality of Life Enjoyment and Satisfaction Questionnaire Score, and the Modified Scale for Suicidal Ideation Score.
One significant difference in the study was noted at week 2, when patients who received adjunctive lithium required fewer NCAs, compared with those who did not receive the drug. "Keep in mind, however, that the lithium dose was set at 300 b.i.d. for the first 8 weeks, so unless you were deviating from the protocol you couldn’t adjust the lithium dose," Dr. Thase said. "As a result, the fact that there are fewer adjustments of lithium in the first few weeks of treatment is determined by the [study] protocol. Across the whole 6 months there were no fewer necessary clinical adjustments in the lithium-treated group than in those who received optimized treatment without lithium."
Another significant finding was that patients who received lithium carried a slightly greater side effect burden during the initial 2 months of treatment (P less than .05), "but it was not different after that time period," he said. "The intensity of side effects was also greater in the lithium group during the first two months but was not different [than the optimized treatment without lithium group] after that time period."
There were no serious adverse events specifically related to lithium therapy, but two events (one case of dehydration and one case of acute renal failure) involved medical considerations related to lithium therapy.
The only significant difference in medication use between the two groups pertained to second-generation antipsychotics. Patients who received adjunctive lithium were 15-20% less likely to receive a second-generation antipsychotic (SGA) over the course of the study. "Put another way, if you don’t use lithium in your practice, you are going to be 15-20% more likely to be prescribing SGAs," Dr. Thase noted.
He acknowledged certain limitations of LiTMUS, including the study’s silence on "the utility of higher doses of lithium or the merits of lithium at higher doses in patients taking simpler psychopharmacology regimens."
While LiTMUS found that the use of lithium as an adjunct "did not improve the simplicity of the treatment regiment, it didn’t increase it, either," Dr. Thase said. "So if you know doctors who say ‘I don’t use lithium because it’s too complicated,’ remind them that we did not find lithium complicated in this study.
"In fact ... lithium was associated with a clinically meaningful reduction in the use of SGAs, "which means that using it lead to less patient exposure to the newer generation antipsychotics.
Dr. Thase disclosed that he has received research funding from the Agency for Healthcare Research and Quality, Eli Lilly, Forest Pharmaceuticals, GlaxoSmithKline, the National Institute of Mental Health, Otsuka Pharmaceuticals, and Sepracor. He also has received honoraria or is on the scientific board of several pharmaceutical companies.
LAS VEGAS – In a 6-month study, the use of adjunctive moderately dosed lithium to optimized treatment in patients with bipolar disorder was well tolerated yet did not lead to improved outcomes or decreased suicidality. However, use of adjunctive lithium resulted in a significant reduction in the use of second-generation antipsychotics.
Those are key findings from the Bipolar Trials Network Lithium Treatment Moderate Dose Study, a randomized trial that compared the use of lithium plus optimized treatment with optimized treatment alone.
"Currently, only about one-third of bipolar patients take lithium," Dr. Michael E. Thase said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "And outpatients uncommonly take lithium in higher, well-established doses. Today it’s more commonly used in moderate doses in combination with newer generation therapies. However, the value of lower dose, combination strategies has not been well-studied."
For the outpatient study, known as the Lithium treatment – moderate dose use study, or LiTMUS, and led by Dr. Andrew A. Nierenberg at the Massachusetts General Hospital, investigators at six clinical sites enrolled 283 patients with bipolar I or bipolar II disorder with a Clinical Global Impressions-Bipolar Scale (CGI-BP-S) score of 3 or greater to assess whether lithium, in moderate doses, "could be a useful platform upon which other newer treatments could be evaluated," said Dr. Thase, professor of psychiatry at the University of Pennsylvania, Philadelphia.
"We were working in partnership with colleagues at the National Institute of Mental Health to do this study in a real-world, relevant way, meaning that it must be inclusive so that people with common comorbidities needed to be in the study, that it needed to be administered in an open way so that the results would be generalizable," said Dr. Thase, who also pointed out that there was no placebo control group.
The investigators compared lithium plus optimized treatment or optimized treatment without lithium. Patients in the lithium arm were started on 300 mg b.i.d. and sustained on 600 mg/day for 8 weeks, adjusted as needed thereafter. The Texas Implementation of Medication Algorithms for bipolar disorder informed care.
The two main outcomes assessed at 6 months were the CGI-BP-S and the number of Necessary Clinical Adjustments (NCAs), a measure of how difficult treatment was to implement. "This takes into account how many times you had to change the treatment in response to side effects or in response to the treatment not working," Dr. Thase explained. "The higher the NCA count, the stormier the treatment course."
A secondary measure was side effect burden as measured by the Frequency and Intensity of Side Effects Ratings, "which provides composite ratings of tolerability rather than focusing on specific side effects," he said. "These were completed at each study visit by the treating psychiatrist."
Dr. Thase reported that 84% of patients completed the 6 months of treatment. The attrition rate was not significantly different among those who received lithium, compared with those who did not receive the drug. The modal dose of lithium was 600 mg/day, and the average lithium levels ranged between 0.5-0.6 mEq/L.
Patients who received lithium did not have better outcomes compared with those who did not in terms of overall change in the CGI-BP-S (–1.5 vs. –1.2, respectively). "The average level of improvement for all of our patients was only about a 30% reduction in symptom burden," Dr. Thase said. "Thus, despite using guideline-based treatment algorithms, more patients remained ill than got better."
No statistically significant differences were found between groups in terms of depression and manic symptom severity based on the CGI-BP-S, the Quick Inventory of Depressive Symptoms Score, the Quality of Life Enjoyment and Satisfaction Questionnaire Score, and the Modified Scale for Suicidal Ideation Score.
One significant difference in the study was noted at week 2, when patients who received adjunctive lithium required fewer NCAs, compared with those who did not receive the drug. "Keep in mind, however, that the lithium dose was set at 300 b.i.d. for the first 8 weeks, so unless you were deviating from the protocol you couldn’t adjust the lithium dose," Dr. Thase said. "As a result, the fact that there are fewer adjustments of lithium in the first few weeks of treatment is determined by the [study] protocol. Across the whole 6 months there were no fewer necessary clinical adjustments in the lithium-treated group than in those who received optimized treatment without lithium."
Another significant finding was that patients who received lithium carried a slightly greater side effect burden during the initial 2 months of treatment (P less than .05), "but it was not different after that time period," he said. "The intensity of side effects was also greater in the lithium group during the first two months but was not different [than the optimized treatment without lithium group] after that time period."
There were no serious adverse events specifically related to lithium therapy, but two events (one case of dehydration and one case of acute renal failure) involved medical considerations related to lithium therapy.
The only significant difference in medication use between the two groups pertained to second-generation antipsychotics. Patients who received adjunctive lithium were 15-20% less likely to receive a second-generation antipsychotic (SGA) over the course of the study. "Put another way, if you don’t use lithium in your practice, you are going to be 15-20% more likely to be prescribing SGAs," Dr. Thase noted.
He acknowledged certain limitations of LiTMUS, including the study’s silence on "the utility of higher doses of lithium or the merits of lithium at higher doses in patients taking simpler psychopharmacology regimens."
While LiTMUS found that the use of lithium as an adjunct "did not improve the simplicity of the treatment regiment, it didn’t increase it, either," Dr. Thase said. "So if you know doctors who say ‘I don’t use lithium because it’s too complicated,’ remind them that we did not find lithium complicated in this study.
"In fact ... lithium was associated with a clinically meaningful reduction in the use of SGAs, "which means that using it lead to less patient exposure to the newer generation antipsychotics.
Dr. Thase disclosed that he has received research funding from the Agency for Healthcare Research and Quality, Eli Lilly, Forest Pharmaceuticals, GlaxoSmithKline, the National Institute of Mental Health, Otsuka Pharmaceuticals, and Sepracor. He also has received honoraria or is on the scientific board of several pharmaceutical companies.
LAS VEGAS – In a 6-month study, the use of adjunctive moderately dosed lithium to optimized treatment in patients with bipolar disorder was well tolerated yet did not lead to improved outcomes or decreased suicidality. However, use of adjunctive lithium resulted in a significant reduction in the use of second-generation antipsychotics.
Those are key findings from the Bipolar Trials Network Lithium Treatment Moderate Dose Study, a randomized trial that compared the use of lithium plus optimized treatment with optimized treatment alone.
"Currently, only about one-third of bipolar patients take lithium," Dr. Michael E. Thase said during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "And outpatients uncommonly take lithium in higher, well-established doses. Today it’s more commonly used in moderate doses in combination with newer generation therapies. However, the value of lower dose, combination strategies has not been well-studied."
For the outpatient study, known as the Lithium treatment – moderate dose use study, or LiTMUS, and led by Dr. Andrew A. Nierenberg at the Massachusetts General Hospital, investigators at six clinical sites enrolled 283 patients with bipolar I or bipolar II disorder with a Clinical Global Impressions-Bipolar Scale (CGI-BP-S) score of 3 or greater to assess whether lithium, in moderate doses, "could be a useful platform upon which other newer treatments could be evaluated," said Dr. Thase, professor of psychiatry at the University of Pennsylvania, Philadelphia.
"We were working in partnership with colleagues at the National Institute of Mental Health to do this study in a real-world, relevant way, meaning that it must be inclusive so that people with common comorbidities needed to be in the study, that it needed to be administered in an open way so that the results would be generalizable," said Dr. Thase, who also pointed out that there was no placebo control group.
The investigators compared lithium plus optimized treatment or optimized treatment without lithium. Patients in the lithium arm were started on 300 mg b.i.d. and sustained on 600 mg/day for 8 weeks, adjusted as needed thereafter. The Texas Implementation of Medication Algorithms for bipolar disorder informed care.
The two main outcomes assessed at 6 months were the CGI-BP-S and the number of Necessary Clinical Adjustments (NCAs), a measure of how difficult treatment was to implement. "This takes into account how many times you had to change the treatment in response to side effects or in response to the treatment not working," Dr. Thase explained. "The higher the NCA count, the stormier the treatment course."
A secondary measure was side effect burden as measured by the Frequency and Intensity of Side Effects Ratings, "which provides composite ratings of tolerability rather than focusing on specific side effects," he said. "These were completed at each study visit by the treating psychiatrist."
Dr. Thase reported that 84% of patients completed the 6 months of treatment. The attrition rate was not significantly different among those who received lithium, compared with those who did not receive the drug. The modal dose of lithium was 600 mg/day, and the average lithium levels ranged between 0.5-0.6 mEq/L.
Patients who received lithium did not have better outcomes compared with those who did not in terms of overall change in the CGI-BP-S (–1.5 vs. –1.2, respectively). "The average level of improvement for all of our patients was only about a 30% reduction in symptom burden," Dr. Thase said. "Thus, despite using guideline-based treatment algorithms, more patients remained ill than got better."
No statistically significant differences were found between groups in terms of depression and manic symptom severity based on the CGI-BP-S, the Quick Inventory of Depressive Symptoms Score, the Quality of Life Enjoyment and Satisfaction Questionnaire Score, and the Modified Scale for Suicidal Ideation Score.
One significant difference in the study was noted at week 2, when patients who received adjunctive lithium required fewer NCAs, compared with those who did not receive the drug. "Keep in mind, however, that the lithium dose was set at 300 b.i.d. for the first 8 weeks, so unless you were deviating from the protocol you couldn’t adjust the lithium dose," Dr. Thase said. "As a result, the fact that there are fewer adjustments of lithium in the first few weeks of treatment is determined by the [study] protocol. Across the whole 6 months there were no fewer necessary clinical adjustments in the lithium-treated group than in those who received optimized treatment without lithium."
Another significant finding was that patients who received lithium carried a slightly greater side effect burden during the initial 2 months of treatment (P less than .05), "but it was not different after that time period," he said. "The intensity of side effects was also greater in the lithium group during the first two months but was not different [than the optimized treatment without lithium group] after that time period."
There were no serious adverse events specifically related to lithium therapy, but two events (one case of dehydration and one case of acute renal failure) involved medical considerations related to lithium therapy.
The only significant difference in medication use between the two groups pertained to second-generation antipsychotics. Patients who received adjunctive lithium were 15-20% less likely to receive a second-generation antipsychotic (SGA) over the course of the study. "Put another way, if you don’t use lithium in your practice, you are going to be 15-20% more likely to be prescribing SGAs," Dr. Thase noted.
He acknowledged certain limitations of LiTMUS, including the study’s silence on "the utility of higher doses of lithium or the merits of lithium at higher doses in patients taking simpler psychopharmacology regimens."
While LiTMUS found that the use of lithium as an adjunct "did not improve the simplicity of the treatment regiment, it didn’t increase it, either," Dr. Thase said. "So if you know doctors who say ‘I don’t use lithium because it’s too complicated,’ remind them that we did not find lithium complicated in this study.
"In fact ... lithium was associated with a clinically meaningful reduction in the use of SGAs, "which means that using it lead to less patient exposure to the newer generation antipsychotics.
Dr. Thase disclosed that he has received research funding from the Agency for Healthcare Research and Quality, Eli Lilly, Forest Pharmaceuticals, GlaxoSmithKline, the National Institute of Mental Health, Otsuka Pharmaceuticals, and Sepracor. He also has received honoraria or is on the scientific board of several pharmaceutical companies.
FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION
Major Finding: Patients with bipolar who received adjunctive lithium did not have better outcomes at 6 months, compared with those who did not in terms of overall change in the Clinical Global Impressions-Bipolar Scale (–1.5 vs. –1.2, respectively). However, those who received adjunctive lithium were 15-20% less likely to receive a second-generation antipsychotic over the course of the study, compared with those who did not.
Data Source: The multicenter, randomized study of 283 patients with bipolar I or bipolar II disorder who received either lithium plus optimized treatment or optimized treatment without lithium took place over the course of 6 months.
Disclosures: Dr. Thase disclosed that he has received research funding from the Agency for Healthcare Research and Quality, Eli Lilly, Forest Pharmaceuticals, GlaxoSmithKline, the National Institute of Mental Health, Otsuka Pharmaceuticals, and Sepracor. He has also received honoraria or is on the scientific board of a number of pharmaceutical companies.
Scan That Predicts Alzheimer's Creates Moral Dilemma
LAS VEGAS – The development of the positron emission tomography radiotracer known as AV-45, or florbetapir F18, for the diagnosis of Alzheimer’s disease carries within a certain "curse," said Dr. Jeffrey L. Cummings of the Cleveland Clinic’s Lou Rubo Center for Brain Health.
The PET scan can show positive results 5-10 years before Alzheimer’s symptoms appear, which raises a multilayered dilemma for clinicians.
"Let’s say someone comes to you and says, ‘My mom had Alzheimer’s at age 75 years. I’m now age 70, and I want to know if I’m going to have it.’ You can tell them," Dr. Cummings said at the conference. "There is going to be a moral, ethical, and cost dilemma that is brought with this scan.
"I don’t think we will use it on [cognitively] ‘normal’ people except in very special circumstances. I think we will use it to sort out those patients with mild cognitive impairment who are in the earliest stage of Alzheimer’s disease. This is going to be a great point of dialogue in the coming year."
For decades, clinicians have informed families of patients affected by Alzheimer’s disease that an autopsy is the only test that can confirm a diagnosis. The AV-45 has the potential to revolutionize the way clinicians diagnose Alzheimer’s disease. The radiotracer, developed by Avid Radiopharmaceuticals and currently under Food and Drug Administration review, enables clinicians to visualize on PET scan deposits of beta-amyloid plaques* in the brain – a hallmark feature of the illness.
"We now have a PET scan that uses ligands that were originally used to label the [amyloid] plaques at autopsy," Dr. Cummings, also chair of neurotherapeutics at the Cleveland Clinic’s Neurological Institute, said in an interview during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "It was realized that you could label these with positron imaging substances so that you could map the presence of amyloid in the brain.
"Now we can make a confident diagnosis of Alzheimer’s disease in the dementia patient. More importantly, we can make a diagnosis in the patient who has mild cognitive impairment. Some of those patients have Alzheimer’s disease; some do not. The new amyloid PET scan will help us know which of the mild cognitive impairment patients have Alzheimer’s disease, and therefore we would consider therapy."
In the meantime, clinicians are using PET in combination with the radiotracer fluorodeoxyglucose (FDG) to distinguish Alzheimer’s disease from frontotemporal dementia. This differential diagnosis is the only one which the Centers for Medicare and Medicaid Services will pay for," Dr. Cummings said. "CMS will pay for a PET scan if you write on the PET scan request, ‘I am trying to distinguish Alzheimer’s disease from frontotemporal dementia.’ If you request use of the scan to diagnose early Alzheimer’s disease, it usually will be denied." FDG PET is approved for differential diagnosis of these two similar conditions but not for the wider range of diagnostic questions such as early identification of Alzheimer’s disease.
Dr. Cummings disclosed that he has provided consultation to Abbott, Acadia, Adamas, Anavex, Astellas, Avanir, Bayer, BMS, Eisai, EnVivo, ExonHit, Janssen, Forest, Genentech, GlaxoSmithKline, Lundbeck, Merck, Neurokos, Novartis, Otsuka, Pfizer, Prana, QR Pharma, Sanofi-Aventis, and Takeda pharmaceutical companies.
*Clarification, 3/14/2012: An earlier version of this story used a less specific term.
LAS VEGAS – The development of the positron emission tomography radiotracer known as AV-45, or florbetapir F18, for the diagnosis of Alzheimer’s disease carries within a certain "curse," said Dr. Jeffrey L. Cummings of the Cleveland Clinic’s Lou Rubo Center for Brain Health.
The PET scan can show positive results 5-10 years before Alzheimer’s symptoms appear, which raises a multilayered dilemma for clinicians.
"Let’s say someone comes to you and says, ‘My mom had Alzheimer’s at age 75 years. I’m now age 70, and I want to know if I’m going to have it.’ You can tell them," Dr. Cummings said at the conference. "There is going to be a moral, ethical, and cost dilemma that is brought with this scan.
"I don’t think we will use it on [cognitively] ‘normal’ people except in very special circumstances. I think we will use it to sort out those patients with mild cognitive impairment who are in the earliest stage of Alzheimer’s disease. This is going to be a great point of dialogue in the coming year."
For decades, clinicians have informed families of patients affected by Alzheimer’s disease that an autopsy is the only test that can confirm a diagnosis. The AV-45 has the potential to revolutionize the way clinicians diagnose Alzheimer’s disease. The radiotracer, developed by Avid Radiopharmaceuticals and currently under Food and Drug Administration review, enables clinicians to visualize on PET scan deposits of beta-amyloid plaques* in the brain – a hallmark feature of the illness.
"We now have a PET scan that uses ligands that were originally used to label the [amyloid] plaques at autopsy," Dr. Cummings, also chair of neurotherapeutics at the Cleveland Clinic’s Neurological Institute, said in an interview during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "It was realized that you could label these with positron imaging substances so that you could map the presence of amyloid in the brain.
"Now we can make a confident diagnosis of Alzheimer’s disease in the dementia patient. More importantly, we can make a diagnosis in the patient who has mild cognitive impairment. Some of those patients have Alzheimer’s disease; some do not. The new amyloid PET scan will help us know which of the mild cognitive impairment patients have Alzheimer’s disease, and therefore we would consider therapy."
In the meantime, clinicians are using PET in combination with the radiotracer fluorodeoxyglucose (FDG) to distinguish Alzheimer’s disease from frontotemporal dementia. This differential diagnosis is the only one which the Centers for Medicare and Medicaid Services will pay for," Dr. Cummings said. "CMS will pay for a PET scan if you write on the PET scan request, ‘I am trying to distinguish Alzheimer’s disease from frontotemporal dementia.’ If you request use of the scan to diagnose early Alzheimer’s disease, it usually will be denied." FDG PET is approved for differential diagnosis of these two similar conditions but not for the wider range of diagnostic questions such as early identification of Alzheimer’s disease.
Dr. Cummings disclosed that he has provided consultation to Abbott, Acadia, Adamas, Anavex, Astellas, Avanir, Bayer, BMS, Eisai, EnVivo, ExonHit, Janssen, Forest, Genentech, GlaxoSmithKline, Lundbeck, Merck, Neurokos, Novartis, Otsuka, Pfizer, Prana, QR Pharma, Sanofi-Aventis, and Takeda pharmaceutical companies.
*Clarification, 3/14/2012: An earlier version of this story used a less specific term.
LAS VEGAS – The development of the positron emission tomography radiotracer known as AV-45, or florbetapir F18, for the diagnosis of Alzheimer’s disease carries within a certain "curse," said Dr. Jeffrey L. Cummings of the Cleveland Clinic’s Lou Rubo Center for Brain Health.
The PET scan can show positive results 5-10 years before Alzheimer’s symptoms appear, which raises a multilayered dilemma for clinicians.
"Let’s say someone comes to you and says, ‘My mom had Alzheimer’s at age 75 years. I’m now age 70, and I want to know if I’m going to have it.’ You can tell them," Dr. Cummings said at the conference. "There is going to be a moral, ethical, and cost dilemma that is brought with this scan.
"I don’t think we will use it on [cognitively] ‘normal’ people except in very special circumstances. I think we will use it to sort out those patients with mild cognitive impairment who are in the earliest stage of Alzheimer’s disease. This is going to be a great point of dialogue in the coming year."
For decades, clinicians have informed families of patients affected by Alzheimer’s disease that an autopsy is the only test that can confirm a diagnosis. The AV-45 has the potential to revolutionize the way clinicians diagnose Alzheimer’s disease. The radiotracer, developed by Avid Radiopharmaceuticals and currently under Food and Drug Administration review, enables clinicians to visualize on PET scan deposits of beta-amyloid plaques* in the brain – a hallmark feature of the illness.
"We now have a PET scan that uses ligands that were originally used to label the [amyloid] plaques at autopsy," Dr. Cummings, also chair of neurotherapeutics at the Cleveland Clinic’s Neurological Institute, said in an interview during a psychopharmacology conference sponsored by the Nevada Psychiatric Association. "It was realized that you could label these with positron imaging substances so that you could map the presence of amyloid in the brain.
"Now we can make a confident diagnosis of Alzheimer’s disease in the dementia patient. More importantly, we can make a diagnosis in the patient who has mild cognitive impairment. Some of those patients have Alzheimer’s disease; some do not. The new amyloid PET scan will help us know which of the mild cognitive impairment patients have Alzheimer’s disease, and therefore we would consider therapy."
In the meantime, clinicians are using PET in combination with the radiotracer fluorodeoxyglucose (FDG) to distinguish Alzheimer’s disease from frontotemporal dementia. This differential diagnosis is the only one which the Centers for Medicare and Medicaid Services will pay for," Dr. Cummings said. "CMS will pay for a PET scan if you write on the PET scan request, ‘I am trying to distinguish Alzheimer’s disease from frontotemporal dementia.’ If you request use of the scan to diagnose early Alzheimer’s disease, it usually will be denied." FDG PET is approved for differential diagnosis of these two similar conditions but not for the wider range of diagnostic questions such as early identification of Alzheimer’s disease.
Dr. Cummings disclosed that he has provided consultation to Abbott, Acadia, Adamas, Anavex, Astellas, Avanir, Bayer, BMS, Eisai, EnVivo, ExonHit, Janssen, Forest, Genentech, GlaxoSmithKline, Lundbeck, Merck, Neurokos, Novartis, Otsuka, Pfizer, Prana, QR Pharma, Sanofi-Aventis, and Takeda pharmaceutical companies.
*Clarification, 3/14/2012: An earlier version of this story used a less specific term.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION
Glutamate Receptors Are Focus of Schizophrenia Research
LAS VEGAS – In the opinion of Dr. Leslie Citrome, the clinical evidence for using adjunctive lithium and anticonvulsants in patients with schizophrenia is generally weak. Yet, clinicians continue to prescribe them.
"It’s kind of puzzling," Dr. Citrome said at the psychopharmacology conference sponsored by the Nevada Psychiatric Association. "When you count out the number of randomized, controlled trials, they do exist. They just don’t show a signal for efficacy, with the possible exception of lamotrigine plus clozapine. But we’re still doing it. Why? I think it’s because studies of these adjunctive agents may have not looked at chronically ill, refractory patients.
"Maybe the right trials weren’t done. Or maybe it’s so hard to gather together the right patients for that trial," said Dr. Citrome of the department of psychiatry and behavioral sciences at New York Medical College, Valhalla. "I think that is the biggest obstacle. Schizophrenia is many different diseases. It’s foolhardy to think that it’s all one pathophysiological process solved by one drug. Once we have a better idea of the different kinds of schizophrenia, then I think we’ll have greater chance and finding answers."
Until then, finding medical treatments that work "is very difficult," he said. "These are very challenging patients. By the time we end up treating them in some settings they’ve been ill for 10, 20, or 30 years."
In an effort to improve therapeutic options for patients with schizophrenia, several agents that affect glutamate receptors are being actively studied in randomized, controlled trials. If the successes that were observed in early clinical trials hold out to be true in the long term, "we are going to have drugs that affect the glutamate system directly and possibly [can be] used every day in the management of patients with schizophrenia," Dr. Citrome said. "Not today, but maybe within 5 or 10 years. This is a very active field of study."
Glutamate is distributed widely and is the primary excitatory neurotransmitter in the human central nervous system. It connects to dopamine neurons, "sometimes directly, sometimes through a [gamma-aminobutyric] interneuron, so there is a framework of how glutamate can impact on dopamine and affect the mesolimbic pathway and thus address psychotic symptoms, as well as [affect] the mesocortical pathway and impact cognition and mood," he said.
Early studies have demonstrated that antagonists to glutamate receptors exacerbate psychotic symptoms and cognitive impairment in patients with schizophrenia, and can induce positive and cognitive symptoms in healthy volunteers. Susceptibility genes for schizophrenia can influence the function of glutamate receptors.
The two main categories of glutamate receptors are ionotropic, which involve ion channels, and metabotropic, which involve G (guanine nucleotide–binding) proteins and chemical second messengers. The three different types of ionotropic glutamate receptors are AMPA (alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid), kainate, and NMDA (N-methyl-D-aspartate). "NMDA receptors won’t work without AMPA or kainate, so they’re all interrelated in some way," Dr. Citrome said. "AMPA and kainate are the ones that work quickly, while NMDA can lead to changes in plasticity over time. NMDA is really where it’s at in terms of where the research is going on, but all three types work in tandem; they don’t work in isolation."
Dr. Citrome went on to explain that for an NMDA receptor to be activated, both glutamate and glycine are required. "D-serine also has high affinity for the glycine site on NMDA receptors," he said. "An analogue of D-serine, D-cycloserine is also active at the glycine co-agonist site of NMDA receptors." In clinical trials of NMDA agonists combined with antipsychotic agents that involved a total of 300 patients, negative symptoms improved in range from 10% to nearly 40% (Clin. Schizophr. Relat. Psychoses 2010;4:189-200).
The glycine transmitter type 1 (GlyT1) reuptake pump is the major route of inactivation of synaptic glycine, Dr. Citrome said. GlyT1 inhibitors such as sarcosine "are analogous to drugs that inhibit reuptake of other neurotransmitters, such as SSRIs and their actions at the serotonin transporter," he said. "When GlyT1 pumps are blocked by a GlyT1 inhibitor, this increases the synaptic availability of glycine-enhancing NMDA neurotransmission."
Proposed agents that target the GlyT1 transport inhibitor include sarcosine and Roche’s RG1678. The latter agent is currently in phase II and phase III trials with an eye toward commercialization.
"What’s exciting about glutamatergic drugs is that it’s not about dopamine anymore," Dr. Citrome said. "These agents don’t block dopamine."
Phase II and III testing is also under way with Eli Lilly’s LY-2140023, an agent that targets metabotropic glutamate type 2/3 (mGluR2/3) receptors.
Dr. Citrome disclosed that in the past 24 months he has engaged in collaborative research with, or has received consulting or speaking fees from Alexza, Alkermes, AstraZeneca, Avanir, Bristol-Myers Squibb, Eli Lilly, Janssen, Lundbeck, Merck, Novartis, Noven, Otsuka, Pfizer, Shire, Sunovion, and Valeant.
LAS VEGAS – In the opinion of Dr. Leslie Citrome, the clinical evidence for using adjunctive lithium and anticonvulsants in patients with schizophrenia is generally weak. Yet, clinicians continue to prescribe them.
"It’s kind of puzzling," Dr. Citrome said at the psychopharmacology conference sponsored by the Nevada Psychiatric Association. "When you count out the number of randomized, controlled trials, they do exist. They just don’t show a signal for efficacy, with the possible exception of lamotrigine plus clozapine. But we’re still doing it. Why? I think it’s because studies of these adjunctive agents may have not looked at chronically ill, refractory patients.
"Maybe the right trials weren’t done. Or maybe it’s so hard to gather together the right patients for that trial," said Dr. Citrome of the department of psychiatry and behavioral sciences at New York Medical College, Valhalla. "I think that is the biggest obstacle. Schizophrenia is many different diseases. It’s foolhardy to think that it’s all one pathophysiological process solved by one drug. Once we have a better idea of the different kinds of schizophrenia, then I think we’ll have greater chance and finding answers."
Until then, finding medical treatments that work "is very difficult," he said. "These are very challenging patients. By the time we end up treating them in some settings they’ve been ill for 10, 20, or 30 years."
In an effort to improve therapeutic options for patients with schizophrenia, several agents that affect glutamate receptors are being actively studied in randomized, controlled trials. If the successes that were observed in early clinical trials hold out to be true in the long term, "we are going to have drugs that affect the glutamate system directly and possibly [can be] used every day in the management of patients with schizophrenia," Dr. Citrome said. "Not today, but maybe within 5 or 10 years. This is a very active field of study."
Glutamate is distributed widely and is the primary excitatory neurotransmitter in the human central nervous system. It connects to dopamine neurons, "sometimes directly, sometimes through a [gamma-aminobutyric] interneuron, so there is a framework of how glutamate can impact on dopamine and affect the mesolimbic pathway and thus address psychotic symptoms, as well as [affect] the mesocortical pathway and impact cognition and mood," he said.
Early studies have demonstrated that antagonists to glutamate receptors exacerbate psychotic symptoms and cognitive impairment in patients with schizophrenia, and can induce positive and cognitive symptoms in healthy volunteers. Susceptibility genes for schizophrenia can influence the function of glutamate receptors.
The two main categories of glutamate receptors are ionotropic, which involve ion channels, and metabotropic, which involve G (guanine nucleotide–binding) proteins and chemical second messengers. The three different types of ionotropic glutamate receptors are AMPA (alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid), kainate, and NMDA (N-methyl-D-aspartate). "NMDA receptors won’t work without AMPA or kainate, so they’re all interrelated in some way," Dr. Citrome said. "AMPA and kainate are the ones that work quickly, while NMDA can lead to changes in plasticity over time. NMDA is really where it’s at in terms of where the research is going on, but all three types work in tandem; they don’t work in isolation."
Dr. Citrome went on to explain that for an NMDA receptor to be activated, both glutamate and glycine are required. "D-serine also has high affinity for the glycine site on NMDA receptors," he said. "An analogue of D-serine, D-cycloserine is also active at the glycine co-agonist site of NMDA receptors." In clinical trials of NMDA agonists combined with antipsychotic agents that involved a total of 300 patients, negative symptoms improved in range from 10% to nearly 40% (Clin. Schizophr. Relat. Psychoses 2010;4:189-200).
The glycine transmitter type 1 (GlyT1) reuptake pump is the major route of inactivation of synaptic glycine, Dr. Citrome said. GlyT1 inhibitors such as sarcosine "are analogous to drugs that inhibit reuptake of other neurotransmitters, such as SSRIs and their actions at the serotonin transporter," he said. "When GlyT1 pumps are blocked by a GlyT1 inhibitor, this increases the synaptic availability of glycine-enhancing NMDA neurotransmission."
Proposed agents that target the GlyT1 transport inhibitor include sarcosine and Roche’s RG1678. The latter agent is currently in phase II and phase III trials with an eye toward commercialization.
"What’s exciting about glutamatergic drugs is that it’s not about dopamine anymore," Dr. Citrome said. "These agents don’t block dopamine."
Phase II and III testing is also under way with Eli Lilly’s LY-2140023, an agent that targets metabotropic glutamate type 2/3 (mGluR2/3) receptors.
Dr. Citrome disclosed that in the past 24 months he has engaged in collaborative research with, or has received consulting or speaking fees from Alexza, Alkermes, AstraZeneca, Avanir, Bristol-Myers Squibb, Eli Lilly, Janssen, Lundbeck, Merck, Novartis, Noven, Otsuka, Pfizer, Shire, Sunovion, and Valeant.
LAS VEGAS – In the opinion of Dr. Leslie Citrome, the clinical evidence for using adjunctive lithium and anticonvulsants in patients with schizophrenia is generally weak. Yet, clinicians continue to prescribe them.
"It’s kind of puzzling," Dr. Citrome said at the psychopharmacology conference sponsored by the Nevada Psychiatric Association. "When you count out the number of randomized, controlled trials, they do exist. They just don’t show a signal for efficacy, with the possible exception of lamotrigine plus clozapine. But we’re still doing it. Why? I think it’s because studies of these adjunctive agents may have not looked at chronically ill, refractory patients.
"Maybe the right trials weren’t done. Or maybe it’s so hard to gather together the right patients for that trial," said Dr. Citrome of the department of psychiatry and behavioral sciences at New York Medical College, Valhalla. "I think that is the biggest obstacle. Schizophrenia is many different diseases. It’s foolhardy to think that it’s all one pathophysiological process solved by one drug. Once we have a better idea of the different kinds of schizophrenia, then I think we’ll have greater chance and finding answers."
Until then, finding medical treatments that work "is very difficult," he said. "These are very challenging patients. By the time we end up treating them in some settings they’ve been ill for 10, 20, or 30 years."
In an effort to improve therapeutic options for patients with schizophrenia, several agents that affect glutamate receptors are being actively studied in randomized, controlled trials. If the successes that were observed in early clinical trials hold out to be true in the long term, "we are going to have drugs that affect the glutamate system directly and possibly [can be] used every day in the management of patients with schizophrenia," Dr. Citrome said. "Not today, but maybe within 5 or 10 years. This is a very active field of study."
Glutamate is distributed widely and is the primary excitatory neurotransmitter in the human central nervous system. It connects to dopamine neurons, "sometimes directly, sometimes through a [gamma-aminobutyric] interneuron, so there is a framework of how glutamate can impact on dopamine and affect the mesolimbic pathway and thus address psychotic symptoms, as well as [affect] the mesocortical pathway and impact cognition and mood," he said.
Early studies have demonstrated that antagonists to glutamate receptors exacerbate psychotic symptoms and cognitive impairment in patients with schizophrenia, and can induce positive and cognitive symptoms in healthy volunteers. Susceptibility genes for schizophrenia can influence the function of glutamate receptors.
The two main categories of glutamate receptors are ionotropic, which involve ion channels, and metabotropic, which involve G (guanine nucleotide–binding) proteins and chemical second messengers. The three different types of ionotropic glutamate receptors are AMPA (alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid), kainate, and NMDA (N-methyl-D-aspartate). "NMDA receptors won’t work without AMPA or kainate, so they’re all interrelated in some way," Dr. Citrome said. "AMPA and kainate are the ones that work quickly, while NMDA can lead to changes in plasticity over time. NMDA is really where it’s at in terms of where the research is going on, but all three types work in tandem; they don’t work in isolation."
Dr. Citrome went on to explain that for an NMDA receptor to be activated, both glutamate and glycine are required. "D-serine also has high affinity for the glycine site on NMDA receptors," he said. "An analogue of D-serine, D-cycloserine is also active at the glycine co-agonist site of NMDA receptors." In clinical trials of NMDA agonists combined with antipsychotic agents that involved a total of 300 patients, negative symptoms improved in range from 10% to nearly 40% (Clin. Schizophr. Relat. Psychoses 2010;4:189-200).
The glycine transmitter type 1 (GlyT1) reuptake pump is the major route of inactivation of synaptic glycine, Dr. Citrome said. GlyT1 inhibitors such as sarcosine "are analogous to drugs that inhibit reuptake of other neurotransmitters, such as SSRIs and their actions at the serotonin transporter," he said. "When GlyT1 pumps are blocked by a GlyT1 inhibitor, this increases the synaptic availability of glycine-enhancing NMDA neurotransmission."
Proposed agents that target the GlyT1 transport inhibitor include sarcosine and Roche’s RG1678. The latter agent is currently in phase II and phase III trials with an eye toward commercialization.
"What’s exciting about glutamatergic drugs is that it’s not about dopamine anymore," Dr. Citrome said. "These agents don’t block dopamine."
Phase II and III testing is also under way with Eli Lilly’s LY-2140023, an agent that targets metabotropic glutamate type 2/3 (mGluR2/3) receptors.
Dr. Citrome disclosed that in the past 24 months he has engaged in collaborative research with, or has received consulting or speaking fees from Alexza, Alkermes, AstraZeneca, Avanir, Bristol-Myers Squibb, Eli Lilly, Janssen, Lundbeck, Merck, Novartis, Noven, Otsuka, Pfizer, Shire, Sunovion, and Valeant.
EXPERT ANALYSIS FROM A PSYCHOPHARMACOLOGY CONFERENCE SPONSORED BY THE NEVADA PSYCHIATRIC ASSOCIATION