User login
Ruptured AAA triage to EVAR centers proposed
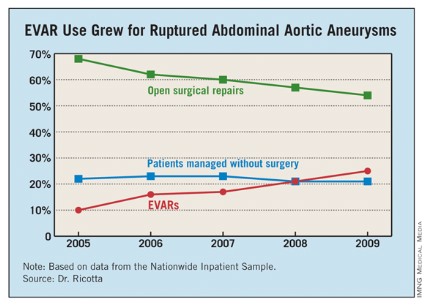
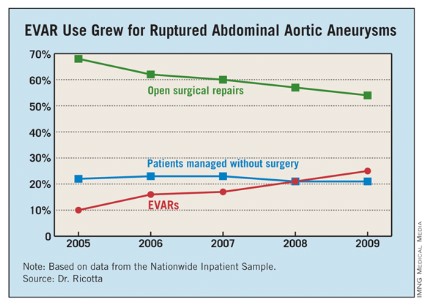
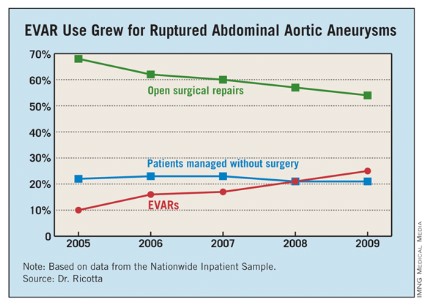
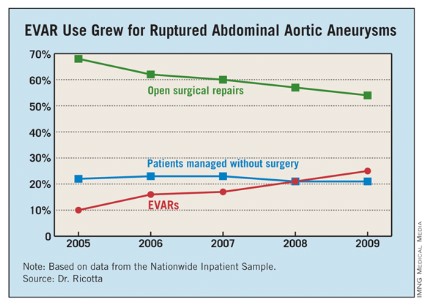
PALM BEACH, FLA. – The number of U.S. patients with ruptured abdominal aortic aneurysms who were managed with endovascular aneurysm repair more than doubled during 2005-2009, suggesting that it’s time to develop a national triage system in order to perform emergency endovascular repairs around the clock, according to Dr. John J. Ricotta.
"A strategy that promotes development of EVAR [endovascular aneurysm repair] centers with triage of stable, EVAR-suitable patients may be the best approach," said Dr. Ricotta, a vascular surgeon and chairman of surgery at MedStar Washington (D.C.) Hospital Center.
"Regionalization of EVAR services may be practical, along with a triage system to rapidly diagnose and transfer patients with RAAA [ruptured abdominal aortic aneurysm]," Dr. Ricotta said at the annual meeting of the Southern Surgical Association.
Because the time from the onset of symptoms to the start of successful EVAR repair is often more than 10 hours, stable RAAA patients could be transferred.
"The focus should be on older patients, who are more likely to survive if you do EVAR, and stable patients. Patients who are hemodynamically stable and have good anatomy [for performing EVAR] should go to an EVAR center."
Dr. Ricotta and his associates analyzed data collected from the U.S. Nationwide Inpatient Sample for all patients aged 60 years or older treated for RAAA during 2005-2009. During the 5-year period, a total of 21,218 patients in the sample underwent treatment for RAAA; 60% of the patients underwent open surgical repair, 22% had no operative repair, and 18% had EVAR.
Use of EVAR rose from 10% of RAAA patients in 2005 to 25% in 2009 (see table). Among the subset of patients who had surgical management, EVAR use rose from 13% of patients in 2005 to 32% in 2009.
EVAR was performed primarily at urban teaching hospitals and in patients under 90. Throughout the 5-year period, EVAR use at urban teaching hospitals included 25% of RAAA patients, compared with 12% of these patients managed at urban nonteaching hospitals and 7% of RAAA patients managed at rural hospitals. About 19% of RAAA patients 60-89 years old underwent EVAR, compared with 12% of those aged 90 or older.
EVAR effectively reduced mortality. Throughout the period studied, the rate of in-hospital mortality was 41% in patients managed with open surgery and 28% in those managed with EVAR, a significant difference, Dr. Ricotta said.
Furthermore, EVAR produced a mortality benefit compared with open surgery across the spectrum of patients, regardless of age. For example, among patients who were at least 90 years old, in-hospital mortality following EVAR was 36%, compared with 77% among patients who had open repair. In a multivariate analysis, EVAR was the only demographic or clinical variable associated with a significant reduction in postoperative in-hospital death, cutting mortality by 47%.
Despite EVAR’s success, use of the technique is limited by the anatomic and physiologic presentation of RAAA patients. "With current technology, EVAR is generally thought to be applicable to 30%-50% of RAAA patients," Dr. Ricotta said. "Experienced centers report the use of EVAR for about 50% of RAAA patients."
Dr. Ricotta called for regionalization and a triage and transfer model, because "widespread adoption of EVAR for RAAA is not practical," he said. "It is an expensive and evolving technology that needs a dedicated staff and a high volume of procedures." An EVAR-first program requires ready CT access and suitable imaging facilities in the operating room, a suitable stock of endografts, and an EVAR team that’s available 24/7, he said.
"Patients who are transferred might do better than patients who are not transferred," agreed Dr. Spence M. Taylor, a vascular surgeon and professor of surgery at the University of South Carolina in Greenville. But he added that patient selection may also play a role. "EVAR does better than open surgical repair in patients who can be stabilized and have this intervention compared with patients who can’t."
Dr. Ricotta and Dr. Taylor had no disclosures.
PALM BEACH, FLA. – The number of U.S. patients with ruptured abdominal aortic aneurysms who were managed with endovascular aneurysm repair more than doubled during 2005-2009, suggesting that it’s time to develop a national triage system in order to perform emergency endovascular repairs around the clock, according to Dr. John J. Ricotta.
"A strategy that promotes development of EVAR [endovascular aneurysm repair] centers with triage of stable, EVAR-suitable patients may be the best approach," said Dr. Ricotta, a vascular surgeon and chairman of surgery at MedStar Washington (D.C.) Hospital Center.
"Regionalization of EVAR services may be practical, along with a triage system to rapidly diagnose and transfer patients with RAAA [ruptured abdominal aortic aneurysm]," Dr. Ricotta said at the annual meeting of the Southern Surgical Association.
Because the time from the onset of symptoms to the start of successful EVAR repair is often more than 10 hours, stable RAAA patients could be transferred.
"The focus should be on older patients, who are more likely to survive if you do EVAR, and stable patients. Patients who are hemodynamically stable and have good anatomy [for performing EVAR] should go to an EVAR center."
Dr. Ricotta and his associates analyzed data collected from the U.S. Nationwide Inpatient Sample for all patients aged 60 years or older treated for RAAA during 2005-2009. During the 5-year period, a total of 21,218 patients in the sample underwent treatment for RAAA; 60% of the patients underwent open surgical repair, 22% had no operative repair, and 18% had EVAR.
Use of EVAR rose from 10% of RAAA patients in 2005 to 25% in 2009 (see table). Among the subset of patients who had surgical management, EVAR use rose from 13% of patients in 2005 to 32% in 2009.
EVAR was performed primarily at urban teaching hospitals and in patients under 90. Throughout the 5-year period, EVAR use at urban teaching hospitals included 25% of RAAA patients, compared with 12% of these patients managed at urban nonteaching hospitals and 7% of RAAA patients managed at rural hospitals. About 19% of RAAA patients 60-89 years old underwent EVAR, compared with 12% of those aged 90 or older.
EVAR effectively reduced mortality. Throughout the period studied, the rate of in-hospital mortality was 41% in patients managed with open surgery and 28% in those managed with EVAR, a significant difference, Dr. Ricotta said.
Furthermore, EVAR produced a mortality benefit compared with open surgery across the spectrum of patients, regardless of age. For example, among patients who were at least 90 years old, in-hospital mortality following EVAR was 36%, compared with 77% among patients who had open repair. In a multivariate analysis, EVAR was the only demographic or clinical variable associated with a significant reduction in postoperative in-hospital death, cutting mortality by 47%.
Despite EVAR’s success, use of the technique is limited by the anatomic and physiologic presentation of RAAA patients. "With current technology, EVAR is generally thought to be applicable to 30%-50% of RAAA patients," Dr. Ricotta said. "Experienced centers report the use of EVAR for about 50% of RAAA patients."
Dr. Ricotta called for regionalization and a triage and transfer model, because "widespread adoption of EVAR for RAAA is not practical," he said. "It is an expensive and evolving technology that needs a dedicated staff and a high volume of procedures." An EVAR-first program requires ready CT access and suitable imaging facilities in the operating room, a suitable stock of endografts, and an EVAR team that’s available 24/7, he said.
"Patients who are transferred might do better than patients who are not transferred," agreed Dr. Spence M. Taylor, a vascular surgeon and professor of surgery at the University of South Carolina in Greenville. But he added that patient selection may also play a role. "EVAR does better than open surgical repair in patients who can be stabilized and have this intervention compared with patients who can’t."
Dr. Ricotta and Dr. Taylor had no disclosures.
PALM BEACH, FLA. – The number of U.S. patients with ruptured abdominal aortic aneurysms who were managed with endovascular aneurysm repair more than doubled during 2005-2009, suggesting that it’s time to develop a national triage system in order to perform emergency endovascular repairs around the clock, according to Dr. John J. Ricotta.
"A strategy that promotes development of EVAR [endovascular aneurysm repair] centers with triage of stable, EVAR-suitable patients may be the best approach," said Dr. Ricotta, a vascular surgeon and chairman of surgery at MedStar Washington (D.C.) Hospital Center.
"Regionalization of EVAR services may be practical, along with a triage system to rapidly diagnose and transfer patients with RAAA [ruptured abdominal aortic aneurysm]," Dr. Ricotta said at the annual meeting of the Southern Surgical Association.
Because the time from the onset of symptoms to the start of successful EVAR repair is often more than 10 hours, stable RAAA patients could be transferred.
"The focus should be on older patients, who are more likely to survive if you do EVAR, and stable patients. Patients who are hemodynamically stable and have good anatomy [for performing EVAR] should go to an EVAR center."
Dr. Ricotta and his associates analyzed data collected from the U.S. Nationwide Inpatient Sample for all patients aged 60 years or older treated for RAAA during 2005-2009. During the 5-year period, a total of 21,218 patients in the sample underwent treatment for RAAA; 60% of the patients underwent open surgical repair, 22% had no operative repair, and 18% had EVAR.
Use of EVAR rose from 10% of RAAA patients in 2005 to 25% in 2009 (see table). Among the subset of patients who had surgical management, EVAR use rose from 13% of patients in 2005 to 32% in 2009.
EVAR was performed primarily at urban teaching hospitals and in patients under 90. Throughout the 5-year period, EVAR use at urban teaching hospitals included 25% of RAAA patients, compared with 12% of these patients managed at urban nonteaching hospitals and 7% of RAAA patients managed at rural hospitals. About 19% of RAAA patients 60-89 years old underwent EVAR, compared with 12% of those aged 90 or older.
EVAR effectively reduced mortality. Throughout the period studied, the rate of in-hospital mortality was 41% in patients managed with open surgery and 28% in those managed with EVAR, a significant difference, Dr. Ricotta said.
Furthermore, EVAR produced a mortality benefit compared with open surgery across the spectrum of patients, regardless of age. For example, among patients who were at least 90 years old, in-hospital mortality following EVAR was 36%, compared with 77% among patients who had open repair. In a multivariate analysis, EVAR was the only demographic or clinical variable associated with a significant reduction in postoperative in-hospital death, cutting mortality by 47%.
Despite EVAR’s success, use of the technique is limited by the anatomic and physiologic presentation of RAAA patients. "With current technology, EVAR is generally thought to be applicable to 30%-50% of RAAA patients," Dr. Ricotta said. "Experienced centers report the use of EVAR for about 50% of RAAA patients."
Dr. Ricotta called for regionalization and a triage and transfer model, because "widespread adoption of EVAR for RAAA is not practical," he said. "It is an expensive and evolving technology that needs a dedicated staff and a high volume of procedures." An EVAR-first program requires ready CT access and suitable imaging facilities in the operating room, a suitable stock of endografts, and an EVAR team that’s available 24/7, he said.
"Patients who are transferred might do better than patients who are not transferred," agreed Dr. Spence M. Taylor, a vascular surgeon and professor of surgery at the University of South Carolina in Greenville. But he added that patient selection may also play a role. "EVAR does better than open surgical repair in patients who can be stabilized and have this intervention compared with patients who can’t."
Dr. Ricotta and Dr. Taylor had no disclosures.
AT THE ANNUAL MEETING OF THE SOUTHERN SURGICAL ASSOCIATION
Major Finding: From 2005 to 2009, the percentage of hospitalized U.S. patients with a ruptured AAA who underwent EVAR grew from 10% to 25%.
Data Source: The data came from an analysis of 21,218 U.S. patients hospitalized for a ruptured abdominal aortic aneurysm during 2005-2009 and included in the Nationwide Inpatient Sample.
Disclosures: Dr. Ricotta and Dr. Taylor had no disclosures.
Antibiotic prophylaxis reduces colorectal surgery readmissions
PALM BEACH, FLA. – Administering a brief oral antibiotic regimen preoperatively to colorectal surgery patients cut the average postoperative hospitalization by more than a day and reduced 30-day readmissions by about 3% compared with no presurgical bowel preparation, a review of more than 8,000 patients found.
The primary driver of these beneficial effects was a reduced rate of surgical site infections, Dr. Mary T. Hawn said at the annual meeting of the Southern Surgical Association.
"Efforts to improve adherence with the use of oral antibiotic preparation may improve the efficiency of care for colorectal surgery," said Dr. Hawn, chief of gastrointestinal surgery at the University of Alabama, Birmingham. "Further research is needed to determine the best protocol for bowel prep prior to colorectal surgery, and to prospectively monitor the rate of Clostridium difficile infection."
The findings by Dr. Hawn’s group also showed that oral antibiotic bowel preparation (OABP) led to a small but statistically significant increase in the rate of hospital readmissions among patients with a principal diagnostic code of colitis caused by C. difficile infection. The OABP patients had a 0.5% readmission rate, compared with a 0.1% rate among patients who received no presurgical bowel preparation.
The value of OABP as shown in this study is particularly important because the use of OABP before colorectal surgery has declined in the United States over the past 20 years, Dr. Hawn added.
Using data collected as part of the VA Surgical Quality Improvement Program, Dr. Hawn and her colleagues analyzed results for 8,180 patients who underwent elective colorectal resection at any of 112 participating VA hospitals during 2005-2009. Patients who had a partial or total colectomy, a rectal resection, or an ostomy were included. Patients were excluded if they had a preoperative stay of more than 2 days, a postoperative stay of more than 30 days, or an American Surgical Association 5 classification, or if they died before hospital discharge.
Most of the patients (83%) underwent surgery for neoplasms; the next most common reason for surgery was diverticulitis, in 6%. OABP was the most common form of presurgical preparation, used on 44% of patients; mechanical preparation only was used on 39%, and no preparation was done in 17%. Ninety percent of the OABP patients also underwent mechanical preparation, while the other 10% had OABP only.
The average postoperative length of stay was 9.1 days among those who received no preparation, 8.6 days for those who got mechanical preparation only, and 7.9 days for those who had OABP – a statistically significant advantage for OABP. In a multivariate regression analysis that controlled for indication, age, and wound class, OABP cut length of stay by an average of 12% compared with no preparation, a statistically significant reduction. In the same analysis, mechanical preparation cut length of stay by only 4% compared with no preparation, also a significant effect.
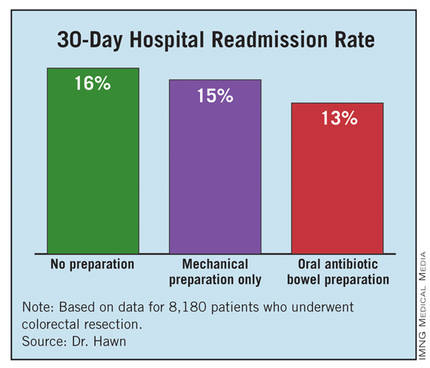
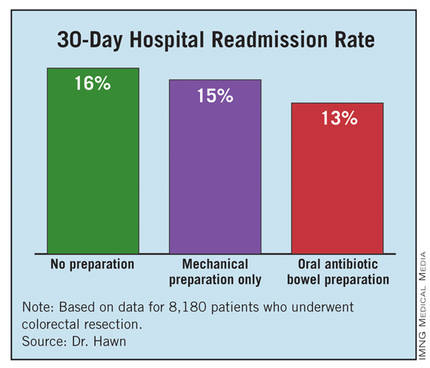
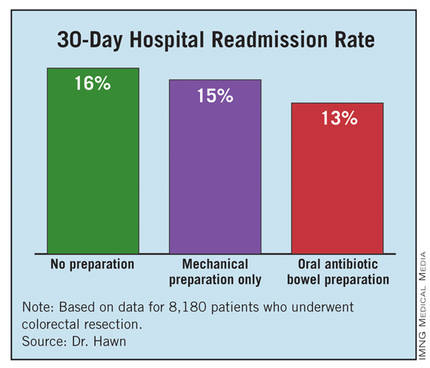
The hospital readmission rate was 16% with no preparation, 15% with mechanical preparation only, and 13% with OABP. In the multivariate regression analysis with adjustment for procedure, age, and wound class, OABP cut the readmission rate by 19% compared with no preparation, a statistically significant reduction. Mechanical preparation only did not have a statistically significant effect.
Further analyses showed that the most common reason for readmission among all patients studied was postoperative infection, in 18%, followed by digestive-system complications, in 10%. C. difficile infection caused 3% of readmissions.
In addition, infections were responsible for readmissions among 6% of patients who underwent no presurgical preparation and in 4% of those who underwent OABP, a statistically significant difference. In contrast, use of OABP produced no statistically significant decline in noninfectious causes of readmission. This rate ran 10% among patients with no preparation, and 9% in patients who underwent OABP.
Dr. Hawn said that she had no disclosures.
Surgical site infections (SSIs) remain a vexing problem despite the significant efforts by hospitals to increase compliance with measures of the Surgical Care Improvement Project. These efforts have so far failed to translate into improved outcomes. We need to identify additional processes that can be changed to improve surgical outcomes.
Elizabeth C. Wick |
At Johns Hopkins, we addressed SSIs by implementing the Comprehensive Unit-Based Safety Program for patients undergoing colorectal surgery. Interventions included standardization of skin preparation, administration of preoperative chlorhexidine showers, selective elimination of mechanical bowel preparation, warming of patients in the preanesthesia area, adoption of enhanced sterile techniques for skin and fascial closure, and addressing previously unrecognized lapses in antibiotic prophylaxis. The program was modeled on ICU processes designed to prevent central line bloodstream infections.
Our program improved the operating room culture by engaging and empowering front-line staff to address deficits and improve processes. A recent review of the rate of SSIs during the 12 months prior to and the 12 months after implementation of this program found that infection rates fell from 27% before implementation to 18% afterward – a 33% relative decrease (J. Am. Coll. Surg. 2012;215:193-200).
We are expanding this program to colon surgery programs at more than 100 U.S. hospitals. Hospitals want to institute new processes proven to improve patient outcomes. The report by Dr. Hawn and her associates is an important step toward identifying a new approach that might further reduce SSIs.
Dr. Elizabeth C. Wick is a colorectal surgeon at Johns Hopkins Hospital in Baltimore. She had no disclosures. She made these comments as a designated discussant for Dr. Hawn’s report.
Surgical site infections (SSIs) remain a vexing problem despite the significant efforts by hospitals to increase compliance with measures of the Surgical Care Improvement Project. These efforts have so far failed to translate into improved outcomes. We need to identify additional processes that can be changed to improve surgical outcomes.
Elizabeth C. Wick |
At Johns Hopkins, we addressed SSIs by implementing the Comprehensive Unit-Based Safety Program for patients undergoing colorectal surgery. Interventions included standardization of skin preparation, administration of preoperative chlorhexidine showers, selective elimination of mechanical bowel preparation, warming of patients in the preanesthesia area, adoption of enhanced sterile techniques for skin and fascial closure, and addressing previously unrecognized lapses in antibiotic prophylaxis. The program was modeled on ICU processes designed to prevent central line bloodstream infections.
Our program improved the operating room culture by engaging and empowering front-line staff to address deficits and improve processes. A recent review of the rate of SSIs during the 12 months prior to and the 12 months after implementation of this program found that infection rates fell from 27% before implementation to 18% afterward – a 33% relative decrease (J. Am. Coll. Surg. 2012;215:193-200).
We are expanding this program to colon surgery programs at more than 100 U.S. hospitals. Hospitals want to institute new processes proven to improve patient outcomes. The report by Dr. Hawn and her associates is an important step toward identifying a new approach that might further reduce SSIs.
Dr. Elizabeth C. Wick is a colorectal surgeon at Johns Hopkins Hospital in Baltimore. She had no disclosures. She made these comments as a designated discussant for Dr. Hawn’s report.
Surgical site infections (SSIs) remain a vexing problem despite the significant efforts by hospitals to increase compliance with measures of the Surgical Care Improvement Project. These efforts have so far failed to translate into improved outcomes. We need to identify additional processes that can be changed to improve surgical outcomes.
Elizabeth C. Wick |
At Johns Hopkins, we addressed SSIs by implementing the Comprehensive Unit-Based Safety Program for patients undergoing colorectal surgery. Interventions included standardization of skin preparation, administration of preoperative chlorhexidine showers, selective elimination of mechanical bowel preparation, warming of patients in the preanesthesia area, adoption of enhanced sterile techniques for skin and fascial closure, and addressing previously unrecognized lapses in antibiotic prophylaxis. The program was modeled on ICU processes designed to prevent central line bloodstream infections.
Our program improved the operating room culture by engaging and empowering front-line staff to address deficits and improve processes. A recent review of the rate of SSIs during the 12 months prior to and the 12 months after implementation of this program found that infection rates fell from 27% before implementation to 18% afterward – a 33% relative decrease (J. Am. Coll. Surg. 2012;215:193-200).
We are expanding this program to colon surgery programs at more than 100 U.S. hospitals. Hospitals want to institute new processes proven to improve patient outcomes. The report by Dr. Hawn and her associates is an important step toward identifying a new approach that might further reduce SSIs.
Dr. Elizabeth C. Wick is a colorectal surgeon at Johns Hopkins Hospital in Baltimore. She had no disclosures. She made these comments as a designated discussant for Dr. Hawn’s report.
PALM BEACH, FLA. – Administering a brief oral antibiotic regimen preoperatively to colorectal surgery patients cut the average postoperative hospitalization by more than a day and reduced 30-day readmissions by about 3% compared with no presurgical bowel preparation, a review of more than 8,000 patients found.
The primary driver of these beneficial effects was a reduced rate of surgical site infections, Dr. Mary T. Hawn said at the annual meeting of the Southern Surgical Association.
"Efforts to improve adherence with the use of oral antibiotic preparation may improve the efficiency of care for colorectal surgery," said Dr. Hawn, chief of gastrointestinal surgery at the University of Alabama, Birmingham. "Further research is needed to determine the best protocol for bowel prep prior to colorectal surgery, and to prospectively monitor the rate of Clostridium difficile infection."
The findings by Dr. Hawn’s group also showed that oral antibiotic bowel preparation (OABP) led to a small but statistically significant increase in the rate of hospital readmissions among patients with a principal diagnostic code of colitis caused by C. difficile infection. The OABP patients had a 0.5% readmission rate, compared with a 0.1% rate among patients who received no presurgical bowel preparation.
The value of OABP as shown in this study is particularly important because the use of OABP before colorectal surgery has declined in the United States over the past 20 years, Dr. Hawn added.
Using data collected as part of the VA Surgical Quality Improvement Program, Dr. Hawn and her colleagues analyzed results for 8,180 patients who underwent elective colorectal resection at any of 112 participating VA hospitals during 2005-2009. Patients who had a partial or total colectomy, a rectal resection, or an ostomy were included. Patients were excluded if they had a preoperative stay of more than 2 days, a postoperative stay of more than 30 days, or an American Surgical Association 5 classification, or if they died before hospital discharge.
Most of the patients (83%) underwent surgery for neoplasms; the next most common reason for surgery was diverticulitis, in 6%. OABP was the most common form of presurgical preparation, used on 44% of patients; mechanical preparation only was used on 39%, and no preparation was done in 17%. Ninety percent of the OABP patients also underwent mechanical preparation, while the other 10% had OABP only.
The average postoperative length of stay was 9.1 days among those who received no preparation, 8.6 days for those who got mechanical preparation only, and 7.9 days for those who had OABP – a statistically significant advantage for OABP. In a multivariate regression analysis that controlled for indication, age, and wound class, OABP cut length of stay by an average of 12% compared with no preparation, a statistically significant reduction. In the same analysis, mechanical preparation cut length of stay by only 4% compared with no preparation, also a significant effect.
The hospital readmission rate was 16% with no preparation, 15% with mechanical preparation only, and 13% with OABP. In the multivariate regression analysis with adjustment for procedure, age, and wound class, OABP cut the readmission rate by 19% compared with no preparation, a statistically significant reduction. Mechanical preparation only did not have a statistically significant effect.
Further analyses showed that the most common reason for readmission among all patients studied was postoperative infection, in 18%, followed by digestive-system complications, in 10%. C. difficile infection caused 3% of readmissions.
In addition, infections were responsible for readmissions among 6% of patients who underwent no presurgical preparation and in 4% of those who underwent OABP, a statistically significant difference. In contrast, use of OABP produced no statistically significant decline in noninfectious causes of readmission. This rate ran 10% among patients with no preparation, and 9% in patients who underwent OABP.
Dr. Hawn said that she had no disclosures.
PALM BEACH, FLA. – Administering a brief oral antibiotic regimen preoperatively to colorectal surgery patients cut the average postoperative hospitalization by more than a day and reduced 30-day readmissions by about 3% compared with no presurgical bowel preparation, a review of more than 8,000 patients found.
The primary driver of these beneficial effects was a reduced rate of surgical site infections, Dr. Mary T. Hawn said at the annual meeting of the Southern Surgical Association.
"Efforts to improve adherence with the use of oral antibiotic preparation may improve the efficiency of care for colorectal surgery," said Dr. Hawn, chief of gastrointestinal surgery at the University of Alabama, Birmingham. "Further research is needed to determine the best protocol for bowel prep prior to colorectal surgery, and to prospectively monitor the rate of Clostridium difficile infection."
The findings by Dr. Hawn’s group also showed that oral antibiotic bowel preparation (OABP) led to a small but statistically significant increase in the rate of hospital readmissions among patients with a principal diagnostic code of colitis caused by C. difficile infection. The OABP patients had a 0.5% readmission rate, compared with a 0.1% rate among patients who received no presurgical bowel preparation.
The value of OABP as shown in this study is particularly important because the use of OABP before colorectal surgery has declined in the United States over the past 20 years, Dr. Hawn added.
Using data collected as part of the VA Surgical Quality Improvement Program, Dr. Hawn and her colleagues analyzed results for 8,180 patients who underwent elective colorectal resection at any of 112 participating VA hospitals during 2005-2009. Patients who had a partial or total colectomy, a rectal resection, or an ostomy were included. Patients were excluded if they had a preoperative stay of more than 2 days, a postoperative stay of more than 30 days, or an American Surgical Association 5 classification, or if they died before hospital discharge.
Most of the patients (83%) underwent surgery for neoplasms; the next most common reason for surgery was diverticulitis, in 6%. OABP was the most common form of presurgical preparation, used on 44% of patients; mechanical preparation only was used on 39%, and no preparation was done in 17%. Ninety percent of the OABP patients also underwent mechanical preparation, while the other 10% had OABP only.
The average postoperative length of stay was 9.1 days among those who received no preparation, 8.6 days for those who got mechanical preparation only, and 7.9 days for those who had OABP – a statistically significant advantage for OABP. In a multivariate regression analysis that controlled for indication, age, and wound class, OABP cut length of stay by an average of 12% compared with no preparation, a statistically significant reduction. In the same analysis, mechanical preparation cut length of stay by only 4% compared with no preparation, also a significant effect.
The hospital readmission rate was 16% with no preparation, 15% with mechanical preparation only, and 13% with OABP. In the multivariate regression analysis with adjustment for procedure, age, and wound class, OABP cut the readmission rate by 19% compared with no preparation, a statistically significant reduction. Mechanical preparation only did not have a statistically significant effect.
Further analyses showed that the most common reason for readmission among all patients studied was postoperative infection, in 18%, followed by digestive-system complications, in 10%. C. difficile infection caused 3% of readmissions.
In addition, infections were responsible for readmissions among 6% of patients who underwent no presurgical preparation and in 4% of those who underwent OABP, a statistically significant difference. In contrast, use of OABP produced no statistically significant decline in noninfectious causes of readmission. This rate ran 10% among patients with no preparation, and 9% in patients who underwent OABP.
Dr. Hawn said that she had no disclosures.
AT THE ANNUAL MEETING OF THE SOUTHERN SURGICAL ASSOCIATION
Major Finding: Oral antibiotic preparation before colorectal surgery cut hospital readmissions by 19% compared with no preparation.
Data Source: A review of 8,180 U.S. patients who underwent colorectal surgery during 2005-2009 at 112 VA hospitals.
Disclosures: Dr. Hawn said that she had no disclosures.
Bariatric surgery cut vascular events in diabetes
PALM BEACH, FLA. – Add another notch to the evidence base for bariatric surgery as effective treatment for type 2 diabetes in obese patients.
Patients with type 2 diabetes who underwent any type of bariatric surgery had a 61%-78% relative risk reduction in their rate of macrovascular, microvascular, or vascular events during an average 20-month follow-up in a review of more than 15,000 cases in South Carolina.
"We are trying to get primary care physicians to spread the word [to patients] that bariatric surgery has come a long way over the past 30 or 40 years; the risk-to-reward ratio is much more beneficial to patients," Dr. John D. Scott said at the annual meeting of the Southern Surgical Association.
The new finding "adds to the extensive list of papers that show bariatric surgery mitigates the long-term effects of type 2 diabetes," Dr. Scott added in an interview. "Some front-line medical providers still see bariatric surgery as a procedure of last resort, but findings like ours show that a discussion [with patients on whether they should consider bariatric surgery] should happen a lot sooner."
Dr. Scott, a surgeon at University Medical Center in Greenville, S.C., recommended that patients with a body mass index of at least 35 kg/m2 and two or more comorbidities be told that they have the option of undergoing bariatric surgery and reducing their risk.
"We have an epidemic [of obesity and type 2 diabetes], and for the first time since tuberculosis, this is an epidemic where surgery has a real opportunity to positively intervene," commented Dr. Josef E. Fischer, a professor of surgery at Harvard Medical School in Boston.
The study used hospital billing data collected by the South Carolina Office of Research and Statistics as well as state vital records data for 1995-2009. The analysis included 2,580 obese patients who underwent any type of bariatric surgery and 13,371 obese patients who did not have surgery. The researchers extracted the data from records of nearly 34,000 obese patients, but excluded patients with type 1 diabetes, patients with incomplete data, and patients with advanced cardiovascular or microvascular disease at the time of their surgery or entry into the state records during this period.
During a median follow-up of about 20 months, the rate of new-onset macro- or microvascular events was 2% in the bariatric surgery patients and 11% in the patients who did not undergo surgery. The rate of an incident vascular disease event was 2% in the patients who had surgery and 13% in those who did not. Macrovascular events included myocardial infarction, stroke, and all-cause death. Microvascular events included blindness in at least one eye, laser eye surgery, nontraumatic amputation, or placement of access for dialysis. Other vascular events included new-onset heart failure or angina, or revascularization of a coronary, carotid, or peripheral artery.
In a multivariate-adjusted analysis, patients who underwent bariatric surgery had a 61% reduction in macrovascular events, a 78% reduction in microvascular events, a 75% reduction in vascular events, and a 64% reduction in combined macro- and microvascular events, compared with patients who did not have this surgery – all statistically significant differences, reported Dr. Spence M. Taylor, a coinvestigator with Dr. Scott on the study. A propensity-score matched analysis that compared the bariatric surgery patients and matched nonsurgical patients showed very similar reductions in all three event categories.
"Bariatric surgery has a substantial and lasting mitigating association on major complications associated with type 2 diabetes in the obese population," concluded Dr. Taylor, chairman of surgery at the University Medical Center in Greenville.
Dr. Scott, Dr. Fischer, and Dr. Taylor had no relevant disclosures.
PALM BEACH, FLA. – Add another notch to the evidence base for bariatric surgery as effective treatment for type 2 diabetes in obese patients.
Patients with type 2 diabetes who underwent any type of bariatric surgery had a 61%-78% relative risk reduction in their rate of macrovascular, microvascular, or vascular events during an average 20-month follow-up in a review of more than 15,000 cases in South Carolina.
"We are trying to get primary care physicians to spread the word [to patients] that bariatric surgery has come a long way over the past 30 or 40 years; the risk-to-reward ratio is much more beneficial to patients," Dr. John D. Scott said at the annual meeting of the Southern Surgical Association.
The new finding "adds to the extensive list of papers that show bariatric surgery mitigates the long-term effects of type 2 diabetes," Dr. Scott added in an interview. "Some front-line medical providers still see bariatric surgery as a procedure of last resort, but findings like ours show that a discussion [with patients on whether they should consider bariatric surgery] should happen a lot sooner."
Dr. Scott, a surgeon at University Medical Center in Greenville, S.C., recommended that patients with a body mass index of at least 35 kg/m2 and two or more comorbidities be told that they have the option of undergoing bariatric surgery and reducing their risk.
"We have an epidemic [of obesity and type 2 diabetes], and for the first time since tuberculosis, this is an epidemic where surgery has a real opportunity to positively intervene," commented Dr. Josef E. Fischer, a professor of surgery at Harvard Medical School in Boston.
The study used hospital billing data collected by the South Carolina Office of Research and Statistics as well as state vital records data for 1995-2009. The analysis included 2,580 obese patients who underwent any type of bariatric surgery and 13,371 obese patients who did not have surgery. The researchers extracted the data from records of nearly 34,000 obese patients, but excluded patients with type 1 diabetes, patients with incomplete data, and patients with advanced cardiovascular or microvascular disease at the time of their surgery or entry into the state records during this period.
During a median follow-up of about 20 months, the rate of new-onset macro- or microvascular events was 2% in the bariatric surgery patients and 11% in the patients who did not undergo surgery. The rate of an incident vascular disease event was 2% in the patients who had surgery and 13% in those who did not. Macrovascular events included myocardial infarction, stroke, and all-cause death. Microvascular events included blindness in at least one eye, laser eye surgery, nontraumatic amputation, or placement of access for dialysis. Other vascular events included new-onset heart failure or angina, or revascularization of a coronary, carotid, or peripheral artery.
In a multivariate-adjusted analysis, patients who underwent bariatric surgery had a 61% reduction in macrovascular events, a 78% reduction in microvascular events, a 75% reduction in vascular events, and a 64% reduction in combined macro- and microvascular events, compared with patients who did not have this surgery – all statistically significant differences, reported Dr. Spence M. Taylor, a coinvestigator with Dr. Scott on the study. A propensity-score matched analysis that compared the bariatric surgery patients and matched nonsurgical patients showed very similar reductions in all three event categories.
"Bariatric surgery has a substantial and lasting mitigating association on major complications associated with type 2 diabetes in the obese population," concluded Dr. Taylor, chairman of surgery at the University Medical Center in Greenville.
Dr. Scott, Dr. Fischer, and Dr. Taylor had no relevant disclosures.
PALM BEACH, FLA. – Add another notch to the evidence base for bariatric surgery as effective treatment for type 2 diabetes in obese patients.
Patients with type 2 diabetes who underwent any type of bariatric surgery had a 61%-78% relative risk reduction in their rate of macrovascular, microvascular, or vascular events during an average 20-month follow-up in a review of more than 15,000 cases in South Carolina.
"We are trying to get primary care physicians to spread the word [to patients] that bariatric surgery has come a long way over the past 30 or 40 years; the risk-to-reward ratio is much more beneficial to patients," Dr. John D. Scott said at the annual meeting of the Southern Surgical Association.
The new finding "adds to the extensive list of papers that show bariatric surgery mitigates the long-term effects of type 2 diabetes," Dr. Scott added in an interview. "Some front-line medical providers still see bariatric surgery as a procedure of last resort, but findings like ours show that a discussion [with patients on whether they should consider bariatric surgery] should happen a lot sooner."
Dr. Scott, a surgeon at University Medical Center in Greenville, S.C., recommended that patients with a body mass index of at least 35 kg/m2 and two or more comorbidities be told that they have the option of undergoing bariatric surgery and reducing their risk.
"We have an epidemic [of obesity and type 2 diabetes], and for the first time since tuberculosis, this is an epidemic where surgery has a real opportunity to positively intervene," commented Dr. Josef E. Fischer, a professor of surgery at Harvard Medical School in Boston.
The study used hospital billing data collected by the South Carolina Office of Research and Statistics as well as state vital records data for 1995-2009. The analysis included 2,580 obese patients who underwent any type of bariatric surgery and 13,371 obese patients who did not have surgery. The researchers extracted the data from records of nearly 34,000 obese patients, but excluded patients with type 1 diabetes, patients with incomplete data, and patients with advanced cardiovascular or microvascular disease at the time of their surgery or entry into the state records during this period.
During a median follow-up of about 20 months, the rate of new-onset macro- or microvascular events was 2% in the bariatric surgery patients and 11% in the patients who did not undergo surgery. The rate of an incident vascular disease event was 2% in the patients who had surgery and 13% in those who did not. Macrovascular events included myocardial infarction, stroke, and all-cause death. Microvascular events included blindness in at least one eye, laser eye surgery, nontraumatic amputation, or placement of access for dialysis. Other vascular events included new-onset heart failure or angina, or revascularization of a coronary, carotid, or peripheral artery.
In a multivariate-adjusted analysis, patients who underwent bariatric surgery had a 61% reduction in macrovascular events, a 78% reduction in microvascular events, a 75% reduction in vascular events, and a 64% reduction in combined macro- and microvascular events, compared with patients who did not have this surgery – all statistically significant differences, reported Dr. Spence M. Taylor, a coinvestigator with Dr. Scott on the study. A propensity-score matched analysis that compared the bariatric surgery patients and matched nonsurgical patients showed very similar reductions in all three event categories.
"Bariatric surgery has a substantial and lasting mitigating association on major complications associated with type 2 diabetes in the obese population," concluded Dr. Taylor, chairman of surgery at the University Medical Center in Greenville.
Dr. Scott, Dr. Fischer, and Dr. Taylor had no relevant disclosures.
AT THE ANNUAL MEETING OF THE SOUTHERN SURGICAL ASSOCIATION
Major Finding: Bariatric surgery was linked to a 64% decrease in macro- and microvascular events compared with no surgery in obese type 2 diabetes patients.
Data Source: Billing information collected on 15,951 obese patients in South Carolina during 1995-2009.
Disclosures: Dr. Scott, Dr. Fischer, and Dr. Taylor had no relevant disclosures.