User login
Management strategies for patients with COVID-19 pneumonia/ARDS
Since the first SARS-CoV-2 (COVID-19) outbreak in Wuhan, China, in December 2019, more than 6.6 million deaths have occurred. . One of the strategies for those cases refractory to traditional ARDS treatments has been the use of extracorporeal membrane oxygenation (ECMO).
Before the COVID-19 pandemic, a substantial amount of data regarding the use of ECMO in ARDS was gathered during the H1N1 influenza outbreak in 2009. Mortality ranged from 8% to 65% (Zangrillo, et al. Crit Care. 2013;17[1]:R30). From these data, we learned the importance of patient selection. Young patients with few co-morbidities and less than 7 days supported by mechanical ventilation did remarkably better than elderly patients or those who had prolonged positive-pressure ventilation prior to ECMO.
To date, the mortality rate for COVID-19 patients with ARDS requiring ECMO is 48% based on data from ELSO. Interestingly though, using May 1, 2020, as a cutoff date, mortality rates for patients with COVID-19 receiving ECMO significantly increased from 37% to 52% (Barbaro, et al. Lancet. 2021;398[10307]:1230). This escalation in mortality engendered concern that ECMO may not be useful in treating patients with COVID-19 and ARDS.
Several factors can be cited for this increase in mortality. First, many new ECMO programs launched after May 1. These new programs had a higher mortality rate (59%) compared with established programs, suggesting that program and provider experience play a significant role in patient outcomes (Barbaro, et al. Lancet. 2021;398[10307]:1230). Second, patients in the latter part of 2020 experienced much longer intervals between the onset of symptoms and time of intubation. Clinicians had a tendency to delay intubation as long as possible. Subsequently, the number of days receiving high flow nasal oxygen or noninvasive ventilation (NIV) was significantly longer (Schmidt, et al. Crit Care. 2021;25[1]:355). These data suggest that prolonged NIV on high Fio2 may be a negative prognostic indicator and should be considered when assessing a patient’s candidacy for ECMO.
Early in the pandemic, clinicians realized that average ECMO run times for patients with COVID-19 and ARDS were significantly longer, 15 vs 9 days, respectively (Jacobs, et al. Ann Thorac Surg. 2022;113[5]:1452). With such long run times, beds were slow to turn over, and a shortage of ECMO beds resulted during the height of the pandemic. In a retrospective study, Gannon looked at 90 patients, all of whom were deemed medically appropriate for ECMO. Two groups were created: (1) no capacity for ECMO vs (2) ECMO provided. Mortality rates were staggering at 89% and 43%, respectively (P =.001) (Gannon, et al. Am J Respir Crit Care Med. 2022;205[11]:1354). This study demonstrated a profound point: during a pandemic, when demand overcomes supply, there is a unique opportunity to see the effect of lifesaving therapies, such as ECMO, on outcomes. This study was particularly poignant, as the average age of the patients was 40 years old.
It is now widely accepted that prone positioning has survival benefit in ARDS. Prone positioning while receiving ECMO has generally been avoided due to concern for potential complications associated with the cannula(s). However, it has been shown that prone positioning while receiving veno-venous (VV) -ECMO reduces mortality rates, 37% proned vs 50% supine positioning (P =.02) (Giani, et al. Ann Am Thorac Soc. 2021;18[3]:495). In this study, no major complications occurred, and minor complications occurred in 6% of the proning events. Prone positioning improves ventilation-perfusion mismatch and reduces hypoxic vasoconstriction, which is thought to be right-sided heart-protective.
Right-sided heart dysfunction (RHD) is common in ARDS, whether COVID-19-related or not. The pathogenesis includes hypoxic vasoconstriction, pulmonary fibrosis, and ventilator-induced lung injury. Pulmonary microthrombi and patient-specific characteristics, such as obesity, are additional factors leading to RHD in patients with COVID-19. During the pandemic, several articles described using right-sided heart protective cannulation strategies for patients with COVID-19 requiring ECMO with favorable results (Mustafa, et al. JAMA Surg. 2020;155[10]:990; Cain, et al. J Surg Res. 2021;264:81-89). This right-sided heart protective strategy involves inserting a single access dual lumen cannula into the right internal jugular vein, which is advanced into the pulmonary artery, effectively bypassing the right ventricle. This setup is more typical of right ventricle assist device (RVAD), rather than typical VV-ECMO, which returns blood to the right atrium. Unfortunately, these studies did not include echocardiographic information to evaluate the effects of this intervention on RVD, and this is an area for future research. However, this vein to pulmonary artery strategy was found to facilitate decreased sedation, earlier liberation from mechanical ventilation, reduced need for tracheostomy, improved mobilization out of bed, and ease in prone positioning (Mustafa, et al. JAMA Surg. 2020;155[10]:990).
In conclusion, there is evidence to support the use of ECMO in patients with COVID-19 patients and ARDS failing conventional mechanical ventilation. The success of ECMO therapy is highly dependent on patient selection. Prolonged use of NIV on high Fio2 may be a negative predictor of ECMO survival and should be considered when assessing a patient for ECMO candidacy. Prone positioning with ECMO has been shown to have survival benefit and should be considered in all patients receiving ECMO.
Dr. Gaillard, Dr. Staples, and Dr. Kapoor are with the Department of Anesthesiology, Section on Critical Care, at Wake Forest School of Medicine in Winston-Salem, N.C. Dr. Gaillard is also with the Department of Emergency Medicine and Department of Internal Medicine, Section on Pulmonary, Critical Care, Allergy, and Immunology at Wake Forest School of Medicine.
Since the first SARS-CoV-2 (COVID-19) outbreak in Wuhan, China, in December 2019, more than 6.6 million deaths have occurred. . One of the strategies for those cases refractory to traditional ARDS treatments has been the use of extracorporeal membrane oxygenation (ECMO).
Before the COVID-19 pandemic, a substantial amount of data regarding the use of ECMO in ARDS was gathered during the H1N1 influenza outbreak in 2009. Mortality ranged from 8% to 65% (Zangrillo, et al. Crit Care. 2013;17[1]:R30). From these data, we learned the importance of patient selection. Young patients with few co-morbidities and less than 7 days supported by mechanical ventilation did remarkably better than elderly patients or those who had prolonged positive-pressure ventilation prior to ECMO.
To date, the mortality rate for COVID-19 patients with ARDS requiring ECMO is 48% based on data from ELSO. Interestingly though, using May 1, 2020, as a cutoff date, mortality rates for patients with COVID-19 receiving ECMO significantly increased from 37% to 52% (Barbaro, et al. Lancet. 2021;398[10307]:1230). This escalation in mortality engendered concern that ECMO may not be useful in treating patients with COVID-19 and ARDS.
Several factors can be cited for this increase in mortality. First, many new ECMO programs launched after May 1. These new programs had a higher mortality rate (59%) compared with established programs, suggesting that program and provider experience play a significant role in patient outcomes (Barbaro, et al. Lancet. 2021;398[10307]:1230). Second, patients in the latter part of 2020 experienced much longer intervals between the onset of symptoms and time of intubation. Clinicians had a tendency to delay intubation as long as possible. Subsequently, the number of days receiving high flow nasal oxygen or noninvasive ventilation (NIV) was significantly longer (Schmidt, et al. Crit Care. 2021;25[1]:355). These data suggest that prolonged NIV on high Fio2 may be a negative prognostic indicator and should be considered when assessing a patient’s candidacy for ECMO.
Early in the pandemic, clinicians realized that average ECMO run times for patients with COVID-19 and ARDS were significantly longer, 15 vs 9 days, respectively (Jacobs, et al. Ann Thorac Surg. 2022;113[5]:1452). With such long run times, beds were slow to turn over, and a shortage of ECMO beds resulted during the height of the pandemic. In a retrospective study, Gannon looked at 90 patients, all of whom were deemed medically appropriate for ECMO. Two groups were created: (1) no capacity for ECMO vs (2) ECMO provided. Mortality rates were staggering at 89% and 43%, respectively (P =.001) (Gannon, et al. Am J Respir Crit Care Med. 2022;205[11]:1354). This study demonstrated a profound point: during a pandemic, when demand overcomes supply, there is a unique opportunity to see the effect of lifesaving therapies, such as ECMO, on outcomes. This study was particularly poignant, as the average age of the patients was 40 years old.
It is now widely accepted that prone positioning has survival benefit in ARDS. Prone positioning while receiving ECMO has generally been avoided due to concern for potential complications associated with the cannula(s). However, it has been shown that prone positioning while receiving veno-venous (VV) -ECMO reduces mortality rates, 37% proned vs 50% supine positioning (P =.02) (Giani, et al. Ann Am Thorac Soc. 2021;18[3]:495). In this study, no major complications occurred, and minor complications occurred in 6% of the proning events. Prone positioning improves ventilation-perfusion mismatch and reduces hypoxic vasoconstriction, which is thought to be right-sided heart-protective.
Right-sided heart dysfunction (RHD) is common in ARDS, whether COVID-19-related or not. The pathogenesis includes hypoxic vasoconstriction, pulmonary fibrosis, and ventilator-induced lung injury. Pulmonary microthrombi and patient-specific characteristics, such as obesity, are additional factors leading to RHD in patients with COVID-19. During the pandemic, several articles described using right-sided heart protective cannulation strategies for patients with COVID-19 requiring ECMO with favorable results (Mustafa, et al. JAMA Surg. 2020;155[10]:990; Cain, et al. J Surg Res. 2021;264:81-89). This right-sided heart protective strategy involves inserting a single access dual lumen cannula into the right internal jugular vein, which is advanced into the pulmonary artery, effectively bypassing the right ventricle. This setup is more typical of right ventricle assist device (RVAD), rather than typical VV-ECMO, which returns blood to the right atrium. Unfortunately, these studies did not include echocardiographic information to evaluate the effects of this intervention on RVD, and this is an area for future research. However, this vein to pulmonary artery strategy was found to facilitate decreased sedation, earlier liberation from mechanical ventilation, reduced need for tracheostomy, improved mobilization out of bed, and ease in prone positioning (Mustafa, et al. JAMA Surg. 2020;155[10]:990).
In conclusion, there is evidence to support the use of ECMO in patients with COVID-19 patients and ARDS failing conventional mechanical ventilation. The success of ECMO therapy is highly dependent on patient selection. Prolonged use of NIV on high Fio2 may be a negative predictor of ECMO survival and should be considered when assessing a patient for ECMO candidacy. Prone positioning with ECMO has been shown to have survival benefit and should be considered in all patients receiving ECMO.
Dr. Gaillard, Dr. Staples, and Dr. Kapoor are with the Department of Anesthesiology, Section on Critical Care, at Wake Forest School of Medicine in Winston-Salem, N.C. Dr. Gaillard is also with the Department of Emergency Medicine and Department of Internal Medicine, Section on Pulmonary, Critical Care, Allergy, and Immunology at Wake Forest School of Medicine.
Since the first SARS-CoV-2 (COVID-19) outbreak in Wuhan, China, in December 2019, more than 6.6 million deaths have occurred. . One of the strategies for those cases refractory to traditional ARDS treatments has been the use of extracorporeal membrane oxygenation (ECMO).
Before the COVID-19 pandemic, a substantial amount of data regarding the use of ECMO in ARDS was gathered during the H1N1 influenza outbreak in 2009. Mortality ranged from 8% to 65% (Zangrillo, et al. Crit Care. 2013;17[1]:R30). From these data, we learned the importance of patient selection. Young patients with few co-morbidities and less than 7 days supported by mechanical ventilation did remarkably better than elderly patients or those who had prolonged positive-pressure ventilation prior to ECMO.
To date, the mortality rate for COVID-19 patients with ARDS requiring ECMO is 48% based on data from ELSO. Interestingly though, using May 1, 2020, as a cutoff date, mortality rates for patients with COVID-19 receiving ECMO significantly increased from 37% to 52% (Barbaro, et al. Lancet. 2021;398[10307]:1230). This escalation in mortality engendered concern that ECMO may not be useful in treating patients with COVID-19 and ARDS.
Several factors can be cited for this increase in mortality. First, many new ECMO programs launched after May 1. These new programs had a higher mortality rate (59%) compared with established programs, suggesting that program and provider experience play a significant role in patient outcomes (Barbaro, et al. Lancet. 2021;398[10307]:1230). Second, patients in the latter part of 2020 experienced much longer intervals between the onset of symptoms and time of intubation. Clinicians had a tendency to delay intubation as long as possible. Subsequently, the number of days receiving high flow nasal oxygen or noninvasive ventilation (NIV) was significantly longer (Schmidt, et al. Crit Care. 2021;25[1]:355). These data suggest that prolonged NIV on high Fio2 may be a negative prognostic indicator and should be considered when assessing a patient’s candidacy for ECMO.
Early in the pandemic, clinicians realized that average ECMO run times for patients with COVID-19 and ARDS were significantly longer, 15 vs 9 days, respectively (Jacobs, et al. Ann Thorac Surg. 2022;113[5]:1452). With such long run times, beds were slow to turn over, and a shortage of ECMO beds resulted during the height of the pandemic. In a retrospective study, Gannon looked at 90 patients, all of whom were deemed medically appropriate for ECMO. Two groups were created: (1) no capacity for ECMO vs (2) ECMO provided. Mortality rates were staggering at 89% and 43%, respectively (P =.001) (Gannon, et al. Am J Respir Crit Care Med. 2022;205[11]:1354). This study demonstrated a profound point: during a pandemic, when demand overcomes supply, there is a unique opportunity to see the effect of lifesaving therapies, such as ECMO, on outcomes. This study was particularly poignant, as the average age of the patients was 40 years old.
It is now widely accepted that prone positioning has survival benefit in ARDS. Prone positioning while receiving ECMO has generally been avoided due to concern for potential complications associated with the cannula(s). However, it has been shown that prone positioning while receiving veno-venous (VV) -ECMO reduces mortality rates, 37% proned vs 50% supine positioning (P =.02) (Giani, et al. Ann Am Thorac Soc. 2021;18[3]:495). In this study, no major complications occurred, and minor complications occurred in 6% of the proning events. Prone positioning improves ventilation-perfusion mismatch and reduces hypoxic vasoconstriction, which is thought to be right-sided heart-protective.
Right-sided heart dysfunction (RHD) is common in ARDS, whether COVID-19-related or not. The pathogenesis includes hypoxic vasoconstriction, pulmonary fibrosis, and ventilator-induced lung injury. Pulmonary microthrombi and patient-specific characteristics, such as obesity, are additional factors leading to RHD in patients with COVID-19. During the pandemic, several articles described using right-sided heart protective cannulation strategies for patients with COVID-19 requiring ECMO with favorable results (Mustafa, et al. JAMA Surg. 2020;155[10]:990; Cain, et al. J Surg Res. 2021;264:81-89). This right-sided heart protective strategy involves inserting a single access dual lumen cannula into the right internal jugular vein, which is advanced into the pulmonary artery, effectively bypassing the right ventricle. This setup is more typical of right ventricle assist device (RVAD), rather than typical VV-ECMO, which returns blood to the right atrium. Unfortunately, these studies did not include echocardiographic information to evaluate the effects of this intervention on RVD, and this is an area for future research. However, this vein to pulmonary artery strategy was found to facilitate decreased sedation, earlier liberation from mechanical ventilation, reduced need for tracheostomy, improved mobilization out of bed, and ease in prone positioning (Mustafa, et al. JAMA Surg. 2020;155[10]:990).
In conclusion, there is evidence to support the use of ECMO in patients with COVID-19 patients and ARDS failing conventional mechanical ventilation. The success of ECMO therapy is highly dependent on patient selection. Prolonged use of NIV on high Fio2 may be a negative predictor of ECMO survival and should be considered when assessing a patient for ECMO candidacy. Prone positioning with ECMO has been shown to have survival benefit and should be considered in all patients receiving ECMO.
Dr. Gaillard, Dr. Staples, and Dr. Kapoor are with the Department of Anesthesiology, Section on Critical Care, at Wake Forest School of Medicine in Winston-Salem, N.C. Dr. Gaillard is also with the Department of Emergency Medicine and Department of Internal Medicine, Section on Pulmonary, Critical Care, Allergy, and Immunology at Wake Forest School of Medicine.
Toward a healthy and sustainable critical care workforce in the COVID-19 era: A call for action
The COVID-19 pandemic has caused unprecedented and unpredictable strain on health care systems worldwide, forcing rapid organizational modifications and innovations to ensure availability of critical care resources during acute surge events. Yet, while much attention has been paid to the availability of ICU beds and ventilators, COVID-19 has insidiously and significantly harmed the most precious critical care resource of all – the human beings who are the lifeblood of critical care delivery. We are now at a crucial moment in history to better understand the pandemic’s impact on our human resources and enact changes to reverse the damage that it has inflicted on our workforce.
ICUs, where critical care delivery predominantly occurs, increasingly utilize interprofessional staffing models in which clinicians from multiple disciplines – physicians, nurses, clinical pharmacists, respiratory therapists, and dieticians, among others – bring their unique expertise to team-based clinical decisions and care delivery. Such a multidisciplinary approach helps enable the provision of more comprehensive, higher-quality critical care. In this way, the interprofessional ICU care team is an embodiment of the notion that the “whole” is more than just the sum of its parts. Therefore, we must consider the impact of the pandemic on interprofessional critical care clinicians as the team that they are.
Even before the COVID-19 pandemic, the well-being of critical care clinicians was compromised. Across multiple disciplines, they had among the highest rates of burnout syndrome of all health care professionals (Moss M, et al. Am J Respir Crit Care Med. 2016;194[1]:106-113). As the pandemic has dragged on, their well-being has only further declined. Burnout rates are at all-time highs, and symptoms of posttraumatic stress disorder, anxiety, and depression are common and have increased with each subsequent surge (Azoulay E, et al. Chest. 2021;160[3]:944-955). Offsets to burnout, such as fulfillment and recognition, have declined over time (Kerlin MP, et al. Ann Amer Thorac Soc. 2022;19[2]:329-331). These worrisome trends pose a significant threat to critical care delivery. Clinician burnout is associated with worse patient outcomes, increased medical errors, and lower patient satisfaction (Moss M, et al. Am J Respir Crit Care Med. 2016;194[1]:106-113; Poghosyan L, et al. Res Nurs Health. 2010;33[4]:288-298). It is also associated with mental illness and substance use disorders among clinicians (Dyrbye LN, et al. Ann Intern Med. 2008;149[5]:334-341). Finally, it has contributed to a workforce crisis: nearly 500,000 health care workers have left the US health care sector since the beginning of the pandemic, and approximately two-thirds of acute and critical care nurses have considered doing so (Wong E. “Why Healthcare Workers are Quitting in Droves”. The Atlantic. Accessed November 7, 2022). Such a “brain drain” of clinicians – whose expertise cannot be easily replicated or replaced – represents a staffing crisis that threatens our ability to provide high-quality, safe care for the foreseeable future.
To combat burnout, it is first necessary to identify the mechanisms by which the pandemic has induced harm. Early during the pandemic, critical care clinicians feared for their own safety with little information of how the virus was spread. At a time when the world was under lockdown, vaccines were not yet available, and hospitals were overwhelmed with surges of critically ill patients, clinicians struggled like the rest of the world to meet their own basic needs such as childcare, grocery shopping, and time with family. They experienced distress from high volumes of patients with extreme mortality rates, helplessness due to lack of treatment options, and moral injury over restrictive visitation policies (Vranas KC, et al. Chest. 2022;162[2]:331-345; Vranas KC, et al. Chest. 2021;160[5]:1714-1728). Over time, critical care clinicians have no doubt experienced further exhaustion related to the duration of the pandemic, often without adequate time to recover and process the trauma they have experienced. More recently, a new source of distress for clinicians has emerged from variability in vaccine uptake among the public. Clinicians have experienced compassion fatigue and even moral outrage toward those who chose not to receive a vaccine that is highly effective at preventing severe illness. They also suffered from ethical conflicts over how to treat unvaccinated patients and whether they should be given equal priority and access to limited therapies (Shaw D. Bioethics. 2022;36[8]:883-890).
Furthermore, the pandemic has damaged the relationship between clinicians and their institutions. Early in the pandemic, the widespread shortages of personal protective equipment harmed trust among clinicians due to their perception that their safety was not prioritized. Hospitals have also struggled with having to make rapid decisions on how to equitably allocate fixed resources in response to unanticipated and unpredictable demands, while also maintaining financial solvency. In some cases, these challenging policy decisions (eg, whether to continue elective procedures during acute surge events) lacked transparency and input from the team at the frontlines of patient care. As a result, clinicians have felt undervalued and without a voice in decisions that directly impact both the care they can provide their patients and their own well-being.
It is incumbent upon us now to take steps to repair the damage inflicted on our critical care workforce by the pandemic. To this end, there have been calls for the urgent implementation of strategies to mitigate the psychological burden experienced by critical care clinicians. However, many of these focus on interventions to increase coping strategies and resilience among individual clinicians. While programs such as mindfulness apps and resilience training are valuable, they are not sufficient. The very nature of these solutions implies that the solution (and therefore, the problem) of burnout lies in the individual clinician. Yet, as described above, many of the mechanisms of harm to clinicians’ well-being are systems-level issues that will necessarily require systems-level solutions.
Therefore, we propose a comprehensive, layered approach to begin to reverse the damage inflicted by the pandemic on critical care clinicians’ well-being, with solutions organized by ecological levels of individual clinicians, departments, institutions, and society. With this approach, we hope to address specific aspects of our critical care delivery system that, taken together, will fortify the well-being of our critical care workforce as a whole. We offer suggestions below that are both informed by existing evidence, as well as our own opinions as intensivists and researchers.
At the level of the individual clinician:
- Proactively provide access to mental health resources. Clinicians have limited time or energy to navigate mental health and support services and find it helpful when others proactively reach out to them.
- Provide opportunities for clinicians to experience community and support among peers. Clinicians find benefit in town halls, debrief sessions, and peer support groups, particularly during times of acute strain.
At the level of the department:
- Allow more flexibility in work schedules. Even prior to the pandemic, the lack of scheduling flexibility and the number of consecutive days worked had been identified as key contributors to burnout; these have been exacerbated during times of caseload surges, when clinicians have been asked or even required to increase their hours and work extra shifts.
- Promote a culture of psychological safety in which clinicians feel empowered to say “I cannot work” for whatever reason. This will require the establishment of formalized backup systems that easily accommodate call-outs without relying on individual clinicians to find their own coverage.
At the level of the health care system:
- Prioritize transparency, and bring administrators and clinicians together for policy decisions. Break down silos between the frontline workers involved in direct patient care and hospital executives, both to inform those decisions and demonstrate the value of clinicians’ perspectives.
- Compensate clinicians for extra work. Consider hazard pay or ensure extra time off for extra time worked.
- Make it “easier” for clinicians to do their jobs by helping them meet their basic needs. Create schedules with designated breaks during shifts. Provide adequate office space and call rooms. Facilitate access to childcare. Provide parking.
- Minimize moral injury. Develop protocols for scarce resource allocation that exclude the treatment team from making decisions about allocation of scarce resources. Avoid visitor restrictions given the harm these policies inflict on patients, families, and members of the care team.
At the level of society:
- Study mechanisms to improve communication about public health with the public. Both science and communication are essential to promoting and protecting public health; more research is needed to improve the way scientific knowledge and evidence-based recommendations are communicated to the public.
In conclusion, the COVID-19 pandemic has forever changed our critical care workforce and the way we deliver care. The time is now to act on the lessons learned from the COVID-19 pandemic through implementation of systems-level solutions to combat burnout and ensure both the health and sustainability of our critical care workforce for the season ahead.
Dr. Vranas is with the Center to Improve Veteran Involvement in Care, VA Portland Health Care System, the Division of Pulmonary and Critical Care, Oregon Health & Science University; Portland, OR; and the Palliative and Advanced Illness Research (PAIR) Center, University of Pennsylvania; Philadelphia, PA. Dr. Kerlin is with the Palliative and Advanced Illness Research (PAIR) Center, and Division of Pulmonary, Allergy and Critical Care, Perelman School of Medicine, University of Pennsylvania; Philadelphia, PA.
The COVID-19 pandemic has caused unprecedented and unpredictable strain on health care systems worldwide, forcing rapid organizational modifications and innovations to ensure availability of critical care resources during acute surge events. Yet, while much attention has been paid to the availability of ICU beds and ventilators, COVID-19 has insidiously and significantly harmed the most precious critical care resource of all – the human beings who are the lifeblood of critical care delivery. We are now at a crucial moment in history to better understand the pandemic’s impact on our human resources and enact changes to reverse the damage that it has inflicted on our workforce.
ICUs, where critical care delivery predominantly occurs, increasingly utilize interprofessional staffing models in which clinicians from multiple disciplines – physicians, nurses, clinical pharmacists, respiratory therapists, and dieticians, among others – bring their unique expertise to team-based clinical decisions and care delivery. Such a multidisciplinary approach helps enable the provision of more comprehensive, higher-quality critical care. In this way, the interprofessional ICU care team is an embodiment of the notion that the “whole” is more than just the sum of its parts. Therefore, we must consider the impact of the pandemic on interprofessional critical care clinicians as the team that they are.
Even before the COVID-19 pandemic, the well-being of critical care clinicians was compromised. Across multiple disciplines, they had among the highest rates of burnout syndrome of all health care professionals (Moss M, et al. Am J Respir Crit Care Med. 2016;194[1]:106-113). As the pandemic has dragged on, their well-being has only further declined. Burnout rates are at all-time highs, and symptoms of posttraumatic stress disorder, anxiety, and depression are common and have increased with each subsequent surge (Azoulay E, et al. Chest. 2021;160[3]:944-955). Offsets to burnout, such as fulfillment and recognition, have declined over time (Kerlin MP, et al. Ann Amer Thorac Soc. 2022;19[2]:329-331). These worrisome trends pose a significant threat to critical care delivery. Clinician burnout is associated with worse patient outcomes, increased medical errors, and lower patient satisfaction (Moss M, et al. Am J Respir Crit Care Med. 2016;194[1]:106-113; Poghosyan L, et al. Res Nurs Health. 2010;33[4]:288-298). It is also associated with mental illness and substance use disorders among clinicians (Dyrbye LN, et al. Ann Intern Med. 2008;149[5]:334-341). Finally, it has contributed to a workforce crisis: nearly 500,000 health care workers have left the US health care sector since the beginning of the pandemic, and approximately two-thirds of acute and critical care nurses have considered doing so (Wong E. “Why Healthcare Workers are Quitting in Droves”. The Atlantic. Accessed November 7, 2022). Such a “brain drain” of clinicians – whose expertise cannot be easily replicated or replaced – represents a staffing crisis that threatens our ability to provide high-quality, safe care for the foreseeable future.
To combat burnout, it is first necessary to identify the mechanisms by which the pandemic has induced harm. Early during the pandemic, critical care clinicians feared for their own safety with little information of how the virus was spread. At a time when the world was under lockdown, vaccines were not yet available, and hospitals were overwhelmed with surges of critically ill patients, clinicians struggled like the rest of the world to meet their own basic needs such as childcare, grocery shopping, and time with family. They experienced distress from high volumes of patients with extreme mortality rates, helplessness due to lack of treatment options, and moral injury over restrictive visitation policies (Vranas KC, et al. Chest. 2022;162[2]:331-345; Vranas KC, et al. Chest. 2021;160[5]:1714-1728). Over time, critical care clinicians have no doubt experienced further exhaustion related to the duration of the pandemic, often without adequate time to recover and process the trauma they have experienced. More recently, a new source of distress for clinicians has emerged from variability in vaccine uptake among the public. Clinicians have experienced compassion fatigue and even moral outrage toward those who chose not to receive a vaccine that is highly effective at preventing severe illness. They also suffered from ethical conflicts over how to treat unvaccinated patients and whether they should be given equal priority and access to limited therapies (Shaw D. Bioethics. 2022;36[8]:883-890).
Furthermore, the pandemic has damaged the relationship between clinicians and their institutions. Early in the pandemic, the widespread shortages of personal protective equipment harmed trust among clinicians due to their perception that their safety was not prioritized. Hospitals have also struggled with having to make rapid decisions on how to equitably allocate fixed resources in response to unanticipated and unpredictable demands, while also maintaining financial solvency. In some cases, these challenging policy decisions (eg, whether to continue elective procedures during acute surge events) lacked transparency and input from the team at the frontlines of patient care. As a result, clinicians have felt undervalued and without a voice in decisions that directly impact both the care they can provide their patients and their own well-being.
It is incumbent upon us now to take steps to repair the damage inflicted on our critical care workforce by the pandemic. To this end, there have been calls for the urgent implementation of strategies to mitigate the psychological burden experienced by critical care clinicians. However, many of these focus on interventions to increase coping strategies and resilience among individual clinicians. While programs such as mindfulness apps and resilience training are valuable, they are not sufficient. The very nature of these solutions implies that the solution (and therefore, the problem) of burnout lies in the individual clinician. Yet, as described above, many of the mechanisms of harm to clinicians’ well-being are systems-level issues that will necessarily require systems-level solutions.
Therefore, we propose a comprehensive, layered approach to begin to reverse the damage inflicted by the pandemic on critical care clinicians’ well-being, with solutions organized by ecological levels of individual clinicians, departments, institutions, and society. With this approach, we hope to address specific aspects of our critical care delivery system that, taken together, will fortify the well-being of our critical care workforce as a whole. We offer suggestions below that are both informed by existing evidence, as well as our own opinions as intensivists and researchers.
At the level of the individual clinician:
- Proactively provide access to mental health resources. Clinicians have limited time or energy to navigate mental health and support services and find it helpful when others proactively reach out to them.
- Provide opportunities for clinicians to experience community and support among peers. Clinicians find benefit in town halls, debrief sessions, and peer support groups, particularly during times of acute strain.
At the level of the department:
- Allow more flexibility in work schedules. Even prior to the pandemic, the lack of scheduling flexibility and the number of consecutive days worked had been identified as key contributors to burnout; these have been exacerbated during times of caseload surges, when clinicians have been asked or even required to increase their hours and work extra shifts.
- Promote a culture of psychological safety in which clinicians feel empowered to say “I cannot work” for whatever reason. This will require the establishment of formalized backup systems that easily accommodate call-outs without relying on individual clinicians to find their own coverage.
At the level of the health care system:
- Prioritize transparency, and bring administrators and clinicians together for policy decisions. Break down silos between the frontline workers involved in direct patient care and hospital executives, both to inform those decisions and demonstrate the value of clinicians’ perspectives.
- Compensate clinicians for extra work. Consider hazard pay or ensure extra time off for extra time worked.
- Make it “easier” for clinicians to do their jobs by helping them meet their basic needs. Create schedules with designated breaks during shifts. Provide adequate office space and call rooms. Facilitate access to childcare. Provide parking.
- Minimize moral injury. Develop protocols for scarce resource allocation that exclude the treatment team from making decisions about allocation of scarce resources. Avoid visitor restrictions given the harm these policies inflict on patients, families, and members of the care team.
At the level of society:
- Study mechanisms to improve communication about public health with the public. Both science and communication are essential to promoting and protecting public health; more research is needed to improve the way scientific knowledge and evidence-based recommendations are communicated to the public.
In conclusion, the COVID-19 pandemic has forever changed our critical care workforce and the way we deliver care. The time is now to act on the lessons learned from the COVID-19 pandemic through implementation of systems-level solutions to combat burnout and ensure both the health and sustainability of our critical care workforce for the season ahead.
Dr. Vranas is with the Center to Improve Veteran Involvement in Care, VA Portland Health Care System, the Division of Pulmonary and Critical Care, Oregon Health & Science University; Portland, OR; and the Palliative and Advanced Illness Research (PAIR) Center, University of Pennsylvania; Philadelphia, PA. Dr. Kerlin is with the Palliative and Advanced Illness Research (PAIR) Center, and Division of Pulmonary, Allergy and Critical Care, Perelman School of Medicine, University of Pennsylvania; Philadelphia, PA.
The COVID-19 pandemic has caused unprecedented and unpredictable strain on health care systems worldwide, forcing rapid organizational modifications and innovations to ensure availability of critical care resources during acute surge events. Yet, while much attention has been paid to the availability of ICU beds and ventilators, COVID-19 has insidiously and significantly harmed the most precious critical care resource of all – the human beings who are the lifeblood of critical care delivery. We are now at a crucial moment in history to better understand the pandemic’s impact on our human resources and enact changes to reverse the damage that it has inflicted on our workforce.
ICUs, where critical care delivery predominantly occurs, increasingly utilize interprofessional staffing models in which clinicians from multiple disciplines – physicians, nurses, clinical pharmacists, respiratory therapists, and dieticians, among others – bring their unique expertise to team-based clinical decisions and care delivery. Such a multidisciplinary approach helps enable the provision of more comprehensive, higher-quality critical care. In this way, the interprofessional ICU care team is an embodiment of the notion that the “whole” is more than just the sum of its parts. Therefore, we must consider the impact of the pandemic on interprofessional critical care clinicians as the team that they are.
Even before the COVID-19 pandemic, the well-being of critical care clinicians was compromised. Across multiple disciplines, they had among the highest rates of burnout syndrome of all health care professionals (Moss M, et al. Am J Respir Crit Care Med. 2016;194[1]:106-113). As the pandemic has dragged on, their well-being has only further declined. Burnout rates are at all-time highs, and symptoms of posttraumatic stress disorder, anxiety, and depression are common and have increased with each subsequent surge (Azoulay E, et al. Chest. 2021;160[3]:944-955). Offsets to burnout, such as fulfillment and recognition, have declined over time (Kerlin MP, et al. Ann Amer Thorac Soc. 2022;19[2]:329-331). These worrisome trends pose a significant threat to critical care delivery. Clinician burnout is associated with worse patient outcomes, increased medical errors, and lower patient satisfaction (Moss M, et al. Am J Respir Crit Care Med. 2016;194[1]:106-113; Poghosyan L, et al. Res Nurs Health. 2010;33[4]:288-298). It is also associated with mental illness and substance use disorders among clinicians (Dyrbye LN, et al. Ann Intern Med. 2008;149[5]:334-341). Finally, it has contributed to a workforce crisis: nearly 500,000 health care workers have left the US health care sector since the beginning of the pandemic, and approximately two-thirds of acute and critical care nurses have considered doing so (Wong E. “Why Healthcare Workers are Quitting in Droves”. The Atlantic. Accessed November 7, 2022). Such a “brain drain” of clinicians – whose expertise cannot be easily replicated or replaced – represents a staffing crisis that threatens our ability to provide high-quality, safe care for the foreseeable future.
To combat burnout, it is first necessary to identify the mechanisms by which the pandemic has induced harm. Early during the pandemic, critical care clinicians feared for their own safety with little information of how the virus was spread. At a time when the world was under lockdown, vaccines were not yet available, and hospitals were overwhelmed with surges of critically ill patients, clinicians struggled like the rest of the world to meet their own basic needs such as childcare, grocery shopping, and time with family. They experienced distress from high volumes of patients with extreme mortality rates, helplessness due to lack of treatment options, and moral injury over restrictive visitation policies (Vranas KC, et al. Chest. 2022;162[2]:331-345; Vranas KC, et al. Chest. 2021;160[5]:1714-1728). Over time, critical care clinicians have no doubt experienced further exhaustion related to the duration of the pandemic, often without adequate time to recover and process the trauma they have experienced. More recently, a new source of distress for clinicians has emerged from variability in vaccine uptake among the public. Clinicians have experienced compassion fatigue and even moral outrage toward those who chose not to receive a vaccine that is highly effective at preventing severe illness. They also suffered from ethical conflicts over how to treat unvaccinated patients and whether they should be given equal priority and access to limited therapies (Shaw D. Bioethics. 2022;36[8]:883-890).
Furthermore, the pandemic has damaged the relationship between clinicians and their institutions. Early in the pandemic, the widespread shortages of personal protective equipment harmed trust among clinicians due to their perception that their safety was not prioritized. Hospitals have also struggled with having to make rapid decisions on how to equitably allocate fixed resources in response to unanticipated and unpredictable demands, while also maintaining financial solvency. In some cases, these challenging policy decisions (eg, whether to continue elective procedures during acute surge events) lacked transparency and input from the team at the frontlines of patient care. As a result, clinicians have felt undervalued and without a voice in decisions that directly impact both the care they can provide their patients and their own well-being.
It is incumbent upon us now to take steps to repair the damage inflicted on our critical care workforce by the pandemic. To this end, there have been calls for the urgent implementation of strategies to mitigate the psychological burden experienced by critical care clinicians. However, many of these focus on interventions to increase coping strategies and resilience among individual clinicians. While programs such as mindfulness apps and resilience training are valuable, they are not sufficient. The very nature of these solutions implies that the solution (and therefore, the problem) of burnout lies in the individual clinician. Yet, as described above, many of the mechanisms of harm to clinicians’ well-being are systems-level issues that will necessarily require systems-level solutions.
Therefore, we propose a comprehensive, layered approach to begin to reverse the damage inflicted by the pandemic on critical care clinicians’ well-being, with solutions organized by ecological levels of individual clinicians, departments, institutions, and society. With this approach, we hope to address specific aspects of our critical care delivery system that, taken together, will fortify the well-being of our critical care workforce as a whole. We offer suggestions below that are both informed by existing evidence, as well as our own opinions as intensivists and researchers.
At the level of the individual clinician:
- Proactively provide access to mental health resources. Clinicians have limited time or energy to navigate mental health and support services and find it helpful when others proactively reach out to them.
- Provide opportunities for clinicians to experience community and support among peers. Clinicians find benefit in town halls, debrief sessions, and peer support groups, particularly during times of acute strain.
At the level of the department:
- Allow more flexibility in work schedules. Even prior to the pandemic, the lack of scheduling flexibility and the number of consecutive days worked had been identified as key contributors to burnout; these have been exacerbated during times of caseload surges, when clinicians have been asked or even required to increase their hours and work extra shifts.
- Promote a culture of psychological safety in which clinicians feel empowered to say “I cannot work” for whatever reason. This will require the establishment of formalized backup systems that easily accommodate call-outs without relying on individual clinicians to find their own coverage.
At the level of the health care system:
- Prioritize transparency, and bring administrators and clinicians together for policy decisions. Break down silos between the frontline workers involved in direct patient care and hospital executives, both to inform those decisions and demonstrate the value of clinicians’ perspectives.
- Compensate clinicians for extra work. Consider hazard pay or ensure extra time off for extra time worked.
- Make it “easier” for clinicians to do their jobs by helping them meet their basic needs. Create schedules with designated breaks during shifts. Provide adequate office space and call rooms. Facilitate access to childcare. Provide parking.
- Minimize moral injury. Develop protocols for scarce resource allocation that exclude the treatment team from making decisions about allocation of scarce resources. Avoid visitor restrictions given the harm these policies inflict on patients, families, and members of the care team.
At the level of society:
- Study mechanisms to improve communication about public health with the public. Both science and communication are essential to promoting and protecting public health; more research is needed to improve the way scientific knowledge and evidence-based recommendations are communicated to the public.
In conclusion, the COVID-19 pandemic has forever changed our critical care workforce and the way we deliver care. The time is now to act on the lessons learned from the COVID-19 pandemic through implementation of systems-level solutions to combat burnout and ensure both the health and sustainability of our critical care workforce for the season ahead.
Dr. Vranas is with the Center to Improve Veteran Involvement in Care, VA Portland Health Care System, the Division of Pulmonary and Critical Care, Oregon Health & Science University; Portland, OR; and the Palliative and Advanced Illness Research (PAIR) Center, University of Pennsylvania; Philadelphia, PA. Dr. Kerlin is with the Palliative and Advanced Illness Research (PAIR) Center, and Division of Pulmonary, Allergy and Critical Care, Perelman School of Medicine, University of Pennsylvania; Philadelphia, PA.
ICU telemedicine turns 40
connected with intensivists at the University Hospitals of Cleveland (Grundy, et al. Crit Care Med. 1982;10[7]:471). After this proof-of-concept report, however, ICU telemedicine gained little traction for nearly 20 years, until Johns Hopkins Hospital established a continuously monitored ICU telemedicine service in a nonintensivist staffed surgical ICU. Their pre/post analysis suggested a 64% decrease in severity-adjusted ICU mortality and greater than 30% decrease in ICU length of stay, ICU complications, and costs (Rosenfeld, et al. Crit Care Med. 2000;28[12]:3925).
Along with better and less costly telemedicine technology, rapid adoption of electronic medical records, and a nationwide intensivist shortage, this and other evidence for the service’s clinical and cost effectiveness has spurred explosive growth in ICU telemedicine in the succeeding 2 decades, with at least 18% of hospitals and 28% of ICU beds supported by ICU telemedicine by 2018 (Ofoma, et al. Crit Care Explor. 2021;4[3]:e0468).
Importantly, what “ICU telemedicine” represents varies substantially across hospitals and even across ICUs within systems. Two-way audiovisual technology is the defining feature, and at a minimum, programs provide intensivists and/or nurses who respond to consultation requests. Commonly, telemedicine clinicians directly connect with patients; monitor labs, hemodynamics, and alarms; and proactively contact on-site clinicians with recommendations or place orders directly into the electronic health record depending on whether the clinician acts as the patients’ primary, co-managing, or consultant provider. A centralized hub and spoke model with telemedicine personnel located at a single, remote center is the most common and best studied ICU telemedicine design. Additional staffing may include respiratory therapists, pharmacists, and advanced practice clinicians in coverage models that range from 24/7 to nocturnal and can also differ in whether patients are monitored continuously or on an as needed basis, triggered by alarms or clinician/nursing concerns.
On-demand services may extend to support for teams responding to medical emergencies inside and sometimes outside the ICU. Another equally important role that ICU telemedicine can provide is helping ensure facilities adhere to ICU quality metrics, such as ventilator bundles, DVT prophylaxis, and daily SAT/SBT.
Unsurprisingly, integrating ICU telemedicine into an existing system is very costly and complex, requiring substantial and thoughtful process redesign to maximize fiscal and clinical return on investment. One vendor of proprietary telemedicine technology, Philips eICU, estimates an implementation cost of $50,000 to $100,000 per bed with annual overhead, software maintenance, and IT staffing of ~20% of implementation costs in addition to clinician staffing of $1-2 million per 100 beds. However, some (but not all) evidence suggests that ICU telemedicine programs pay for themselves over time. An influential report from Sentara Healthcare, an early adopter of ICU telemedicine, described equipment costs of more than $1 million for a total of 103 critical care beds but attributed savings of $460,000 per month to decreased length of stay (Coustasse, et al. The Permanente Journal. 2014;18[4]:76).
Cost savings are great, of course, but ICU telemedicine’s potential to improve clinical outcomes is the real priority. While Sentara’s early report included a 27% decrease in ICU mortality after telemedicine adoption, a 2011 meta-analysis of 13 studies, including 35 ICUs and over 40,000 patients, suggested decreased ICU mortality and LOS with a statistically significant effect on overall hospital mortality and LOS (Young, et al. Arch Intern Med. 2011;171[6]:498). This highlights the Achilles heel of ICU telemedicine evidence: the pretest/posttest studies that dominate this field and likely contribute substantially to the inconsistencies in the evidence base.
In the absence of risk adjustment and control groups, many studies observed postimplementation changes that may reflect trends in patient mix or the effects of unrelated practice changes rather than the causal influence of ICU telemedicine. In fact, in studies using more robust methods, ICU telemedicine’s effect size has been smaller or nonexistent. For example, in 2016, Kahn and colleagues used CMS data to evaluate 132 ICU telemedicine programs using 389 matched controlled hospitals. There was a slight reduction in 90-day mortality (OR=0.96, CI 0.94-0.98) with only 12% showing a statistically significant reduction in mortality. Interestingly, hospitals in urban areas demonstrated greater benefit than rural facilities (Kahn, et al. Medical Care. 2016;54[3]:319).
The heterogeneity of the studied programs (e.g., primary vs consultative role, on-demand vs proactive involvement) and recipient ICUs (e.g., rural vs tertiary care facility, presence of bedside intensivists) further hinders a clear answer to the key question: Would ICU telemedicine benefit my hospital? Fortunately, some recent, well-designed studies have attempted to understand which attributes of ICU telemedicine programs provide results and which ICUs will see the most benefit. In a cohort of 118,990 patients across 56 ICUs, four interventions were associated with lower mortality and reduced LOS: (1) evaluation of patients within 1 hour of ICU admission, (2) frequent leadership review of performance data, (3) ICU best practice compliance, and (4) prompt response to alerts (Lilly, et al. Chest. 2014;145[3]:500). Kahn and colleagues have also investigated this issue, conducting an in-depth ethnographic evaluation of 10 hospitals identified in their 2016 study to have positive, neutral, or negative outcomes after ICU telemedicine implementation (Kahn, et al. Am J Respir Crit Care Med. 2019;199[8]:970). They found that successful programs:
(1) provided consistent services matched to recipient needs;
(2) provided services both proactively and reactively without being obtrusive;
(3) embedded routine engagements unobtrusively into usual routines;
(4) had engaged leadership who set clear expectations and mediated conflicts; and
(5) had bedside clinicians who valued and sought out telemedicine participation in care.
The authors concluded that, “the true value of ICU telemedicine lies not in whether the technology exists but in how it is applied.” However, another recent analysis also suggested that, rather than telemedicine or recipient ICU design, targeting underperforming recipient ICU performance may be the key determinant of whether ICU telemedicine implementation improves outcomes (Fusaro, et al. Crit Care Med. 2019; 47[4]:501). While the finding may reflect regression to the mean, the idea that ICUs with above-expected mortality derive greater benefit from ICU telemedicine support than already well-performing ICUs is certainly logical.
As COVID-19 strained health care systems across the country, we and others found ways to use ICU telemedicine to preserve optimal care delivery for critically ill patients. Our program at Intermountain Healthcare – already supporting 17 ICUs within our 24-hospital health system, as well as 10 external ICUs with experienced critical care physicians, nurses, respiratory therapists, and pharmacists – took on increased responsibility for ICU load balancing and interhospital transfers.
Leveraging telemedicine services also helped community ICUs care for sicker, more complex patients than usual and aided nonintensivist physicians called upon to manage critically ill patients in ad hoc ICUs at referral hospitals. While the pandemic certainly stressed ICU staff, we suspect that telemedicine’s ability to balance caseloads and distribute clinical tasks helped mitigate these stresses. At age 40, ICU telemedicine is both mature and still growing, with continued expansion of bed coverage and the range of services available. Looking ahead, as we confront a national shortage of intensivists, ICU telemedicine likely represents a cost effective and efficient strategy to maintain critical care capacity with the potential to ensure low-cost, high-quality care for all, regardless of location.
Dr. Graham and Dr. Peltan are with the Division of Pulmonary & Critical Care Medicine, Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City, Utah; and Dr. Peltan is also with the Division of Pulmonary & Critical Care Medicine, Department of Medicine, Intermountain Medical Center, Murray, Utah.
connected with intensivists at the University Hospitals of Cleveland (Grundy, et al. Crit Care Med. 1982;10[7]:471). After this proof-of-concept report, however, ICU telemedicine gained little traction for nearly 20 years, until Johns Hopkins Hospital established a continuously monitored ICU telemedicine service in a nonintensivist staffed surgical ICU. Their pre/post analysis suggested a 64% decrease in severity-adjusted ICU mortality and greater than 30% decrease in ICU length of stay, ICU complications, and costs (Rosenfeld, et al. Crit Care Med. 2000;28[12]:3925).
Along with better and less costly telemedicine technology, rapid adoption of electronic medical records, and a nationwide intensivist shortage, this and other evidence for the service’s clinical and cost effectiveness has spurred explosive growth in ICU telemedicine in the succeeding 2 decades, with at least 18% of hospitals and 28% of ICU beds supported by ICU telemedicine by 2018 (Ofoma, et al. Crit Care Explor. 2021;4[3]:e0468).
Importantly, what “ICU telemedicine” represents varies substantially across hospitals and even across ICUs within systems. Two-way audiovisual technology is the defining feature, and at a minimum, programs provide intensivists and/or nurses who respond to consultation requests. Commonly, telemedicine clinicians directly connect with patients; monitor labs, hemodynamics, and alarms; and proactively contact on-site clinicians with recommendations or place orders directly into the electronic health record depending on whether the clinician acts as the patients’ primary, co-managing, or consultant provider. A centralized hub and spoke model with telemedicine personnel located at a single, remote center is the most common and best studied ICU telemedicine design. Additional staffing may include respiratory therapists, pharmacists, and advanced practice clinicians in coverage models that range from 24/7 to nocturnal and can also differ in whether patients are monitored continuously or on an as needed basis, triggered by alarms or clinician/nursing concerns.
On-demand services may extend to support for teams responding to medical emergencies inside and sometimes outside the ICU. Another equally important role that ICU telemedicine can provide is helping ensure facilities adhere to ICU quality metrics, such as ventilator bundles, DVT prophylaxis, and daily SAT/SBT.
Unsurprisingly, integrating ICU telemedicine into an existing system is very costly and complex, requiring substantial and thoughtful process redesign to maximize fiscal and clinical return on investment. One vendor of proprietary telemedicine technology, Philips eICU, estimates an implementation cost of $50,000 to $100,000 per bed with annual overhead, software maintenance, and IT staffing of ~20% of implementation costs in addition to clinician staffing of $1-2 million per 100 beds. However, some (but not all) evidence suggests that ICU telemedicine programs pay for themselves over time. An influential report from Sentara Healthcare, an early adopter of ICU telemedicine, described equipment costs of more than $1 million for a total of 103 critical care beds but attributed savings of $460,000 per month to decreased length of stay (Coustasse, et al. The Permanente Journal. 2014;18[4]:76).
Cost savings are great, of course, but ICU telemedicine’s potential to improve clinical outcomes is the real priority. While Sentara’s early report included a 27% decrease in ICU mortality after telemedicine adoption, a 2011 meta-analysis of 13 studies, including 35 ICUs and over 40,000 patients, suggested decreased ICU mortality and LOS with a statistically significant effect on overall hospital mortality and LOS (Young, et al. Arch Intern Med. 2011;171[6]:498). This highlights the Achilles heel of ICU telemedicine evidence: the pretest/posttest studies that dominate this field and likely contribute substantially to the inconsistencies in the evidence base.
In the absence of risk adjustment and control groups, many studies observed postimplementation changes that may reflect trends in patient mix or the effects of unrelated practice changes rather than the causal influence of ICU telemedicine. In fact, in studies using more robust methods, ICU telemedicine’s effect size has been smaller or nonexistent. For example, in 2016, Kahn and colleagues used CMS data to evaluate 132 ICU telemedicine programs using 389 matched controlled hospitals. There was a slight reduction in 90-day mortality (OR=0.96, CI 0.94-0.98) with only 12% showing a statistically significant reduction in mortality. Interestingly, hospitals in urban areas demonstrated greater benefit than rural facilities (Kahn, et al. Medical Care. 2016;54[3]:319).
The heterogeneity of the studied programs (e.g., primary vs consultative role, on-demand vs proactive involvement) and recipient ICUs (e.g., rural vs tertiary care facility, presence of bedside intensivists) further hinders a clear answer to the key question: Would ICU telemedicine benefit my hospital? Fortunately, some recent, well-designed studies have attempted to understand which attributes of ICU telemedicine programs provide results and which ICUs will see the most benefit. In a cohort of 118,990 patients across 56 ICUs, four interventions were associated with lower mortality and reduced LOS: (1) evaluation of patients within 1 hour of ICU admission, (2) frequent leadership review of performance data, (3) ICU best practice compliance, and (4) prompt response to alerts (Lilly, et al. Chest. 2014;145[3]:500). Kahn and colleagues have also investigated this issue, conducting an in-depth ethnographic evaluation of 10 hospitals identified in their 2016 study to have positive, neutral, or negative outcomes after ICU telemedicine implementation (Kahn, et al. Am J Respir Crit Care Med. 2019;199[8]:970). They found that successful programs:
(1) provided consistent services matched to recipient needs;
(2) provided services both proactively and reactively without being obtrusive;
(3) embedded routine engagements unobtrusively into usual routines;
(4) had engaged leadership who set clear expectations and mediated conflicts; and
(5) had bedside clinicians who valued and sought out telemedicine participation in care.
The authors concluded that, “the true value of ICU telemedicine lies not in whether the technology exists but in how it is applied.” However, another recent analysis also suggested that, rather than telemedicine or recipient ICU design, targeting underperforming recipient ICU performance may be the key determinant of whether ICU telemedicine implementation improves outcomes (Fusaro, et al. Crit Care Med. 2019; 47[4]:501). While the finding may reflect regression to the mean, the idea that ICUs with above-expected mortality derive greater benefit from ICU telemedicine support than already well-performing ICUs is certainly logical.
As COVID-19 strained health care systems across the country, we and others found ways to use ICU telemedicine to preserve optimal care delivery for critically ill patients. Our program at Intermountain Healthcare – already supporting 17 ICUs within our 24-hospital health system, as well as 10 external ICUs with experienced critical care physicians, nurses, respiratory therapists, and pharmacists – took on increased responsibility for ICU load balancing and interhospital transfers.
Leveraging telemedicine services also helped community ICUs care for sicker, more complex patients than usual and aided nonintensivist physicians called upon to manage critically ill patients in ad hoc ICUs at referral hospitals. While the pandemic certainly stressed ICU staff, we suspect that telemedicine’s ability to balance caseloads and distribute clinical tasks helped mitigate these stresses. At age 40, ICU telemedicine is both mature and still growing, with continued expansion of bed coverage and the range of services available. Looking ahead, as we confront a national shortage of intensivists, ICU telemedicine likely represents a cost effective and efficient strategy to maintain critical care capacity with the potential to ensure low-cost, high-quality care for all, regardless of location.
Dr. Graham and Dr. Peltan are with the Division of Pulmonary & Critical Care Medicine, Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City, Utah; and Dr. Peltan is also with the Division of Pulmonary & Critical Care Medicine, Department of Medicine, Intermountain Medical Center, Murray, Utah.
connected with intensivists at the University Hospitals of Cleveland (Grundy, et al. Crit Care Med. 1982;10[7]:471). After this proof-of-concept report, however, ICU telemedicine gained little traction for nearly 20 years, until Johns Hopkins Hospital established a continuously monitored ICU telemedicine service in a nonintensivist staffed surgical ICU. Their pre/post analysis suggested a 64% decrease in severity-adjusted ICU mortality and greater than 30% decrease in ICU length of stay, ICU complications, and costs (Rosenfeld, et al. Crit Care Med. 2000;28[12]:3925).
Along with better and less costly telemedicine technology, rapid adoption of electronic medical records, and a nationwide intensivist shortage, this and other evidence for the service’s clinical and cost effectiveness has spurred explosive growth in ICU telemedicine in the succeeding 2 decades, with at least 18% of hospitals and 28% of ICU beds supported by ICU telemedicine by 2018 (Ofoma, et al. Crit Care Explor. 2021;4[3]:e0468).
Importantly, what “ICU telemedicine” represents varies substantially across hospitals and even across ICUs within systems. Two-way audiovisual technology is the defining feature, and at a minimum, programs provide intensivists and/or nurses who respond to consultation requests. Commonly, telemedicine clinicians directly connect with patients; monitor labs, hemodynamics, and alarms; and proactively contact on-site clinicians with recommendations or place orders directly into the electronic health record depending on whether the clinician acts as the patients’ primary, co-managing, or consultant provider. A centralized hub and spoke model with telemedicine personnel located at a single, remote center is the most common and best studied ICU telemedicine design. Additional staffing may include respiratory therapists, pharmacists, and advanced practice clinicians in coverage models that range from 24/7 to nocturnal and can also differ in whether patients are monitored continuously or on an as needed basis, triggered by alarms or clinician/nursing concerns.
On-demand services may extend to support for teams responding to medical emergencies inside and sometimes outside the ICU. Another equally important role that ICU telemedicine can provide is helping ensure facilities adhere to ICU quality metrics, such as ventilator bundles, DVT prophylaxis, and daily SAT/SBT.
Unsurprisingly, integrating ICU telemedicine into an existing system is very costly and complex, requiring substantial and thoughtful process redesign to maximize fiscal and clinical return on investment. One vendor of proprietary telemedicine technology, Philips eICU, estimates an implementation cost of $50,000 to $100,000 per bed with annual overhead, software maintenance, and IT staffing of ~20% of implementation costs in addition to clinician staffing of $1-2 million per 100 beds. However, some (but not all) evidence suggests that ICU telemedicine programs pay for themselves over time. An influential report from Sentara Healthcare, an early adopter of ICU telemedicine, described equipment costs of more than $1 million for a total of 103 critical care beds but attributed savings of $460,000 per month to decreased length of stay (Coustasse, et al. The Permanente Journal. 2014;18[4]:76).
Cost savings are great, of course, but ICU telemedicine’s potential to improve clinical outcomes is the real priority. While Sentara’s early report included a 27% decrease in ICU mortality after telemedicine adoption, a 2011 meta-analysis of 13 studies, including 35 ICUs and over 40,000 patients, suggested decreased ICU mortality and LOS with a statistically significant effect on overall hospital mortality and LOS (Young, et al. Arch Intern Med. 2011;171[6]:498). This highlights the Achilles heel of ICU telemedicine evidence: the pretest/posttest studies that dominate this field and likely contribute substantially to the inconsistencies in the evidence base.
In the absence of risk adjustment and control groups, many studies observed postimplementation changes that may reflect trends in patient mix or the effects of unrelated practice changes rather than the causal influence of ICU telemedicine. In fact, in studies using more robust methods, ICU telemedicine’s effect size has been smaller or nonexistent. For example, in 2016, Kahn and colleagues used CMS data to evaluate 132 ICU telemedicine programs using 389 matched controlled hospitals. There was a slight reduction in 90-day mortality (OR=0.96, CI 0.94-0.98) with only 12% showing a statistically significant reduction in mortality. Interestingly, hospitals in urban areas demonstrated greater benefit than rural facilities (Kahn, et al. Medical Care. 2016;54[3]:319).
The heterogeneity of the studied programs (e.g., primary vs consultative role, on-demand vs proactive involvement) and recipient ICUs (e.g., rural vs tertiary care facility, presence of bedside intensivists) further hinders a clear answer to the key question: Would ICU telemedicine benefit my hospital? Fortunately, some recent, well-designed studies have attempted to understand which attributes of ICU telemedicine programs provide results and which ICUs will see the most benefit. In a cohort of 118,990 patients across 56 ICUs, four interventions were associated with lower mortality and reduced LOS: (1) evaluation of patients within 1 hour of ICU admission, (2) frequent leadership review of performance data, (3) ICU best practice compliance, and (4) prompt response to alerts (Lilly, et al. Chest. 2014;145[3]:500). Kahn and colleagues have also investigated this issue, conducting an in-depth ethnographic evaluation of 10 hospitals identified in their 2016 study to have positive, neutral, or negative outcomes after ICU telemedicine implementation (Kahn, et al. Am J Respir Crit Care Med. 2019;199[8]:970). They found that successful programs:
(1) provided consistent services matched to recipient needs;
(2) provided services both proactively and reactively without being obtrusive;
(3) embedded routine engagements unobtrusively into usual routines;
(4) had engaged leadership who set clear expectations and mediated conflicts; and
(5) had bedside clinicians who valued and sought out telemedicine participation in care.
The authors concluded that, “the true value of ICU telemedicine lies not in whether the technology exists but in how it is applied.” However, another recent analysis also suggested that, rather than telemedicine or recipient ICU design, targeting underperforming recipient ICU performance may be the key determinant of whether ICU telemedicine implementation improves outcomes (Fusaro, et al. Crit Care Med. 2019; 47[4]:501). While the finding may reflect regression to the mean, the idea that ICUs with above-expected mortality derive greater benefit from ICU telemedicine support than already well-performing ICUs is certainly logical.
As COVID-19 strained health care systems across the country, we and others found ways to use ICU telemedicine to preserve optimal care delivery for critically ill patients. Our program at Intermountain Healthcare – already supporting 17 ICUs within our 24-hospital health system, as well as 10 external ICUs with experienced critical care physicians, nurses, respiratory therapists, and pharmacists – took on increased responsibility for ICU load balancing and interhospital transfers.
Leveraging telemedicine services also helped community ICUs care for sicker, more complex patients than usual and aided nonintensivist physicians called upon to manage critically ill patients in ad hoc ICUs at referral hospitals. While the pandemic certainly stressed ICU staff, we suspect that telemedicine’s ability to balance caseloads and distribute clinical tasks helped mitigate these stresses. At age 40, ICU telemedicine is both mature and still growing, with continued expansion of bed coverage and the range of services available. Looking ahead, as we confront a national shortage of intensivists, ICU telemedicine likely represents a cost effective and efficient strategy to maintain critical care capacity with the potential to ensure low-cost, high-quality care for all, regardless of location.
Dr. Graham and Dr. Peltan are with the Division of Pulmonary & Critical Care Medicine, Department of Internal Medicine, University of Utah School of Medicine, Salt Lake City, Utah; and Dr. Peltan is also with the Division of Pulmonary & Critical Care Medicine, Department of Medicine, Intermountain Medical Center, Murray, Utah.
Addressing racial bias in pulse oximetry
Pulse oximetry is a vital monitoring tool in the ICU and in pulmonary medicine. Regrettably, re-emerging data show that pulse oximeters do not accurately measure blood oxygen levels in Black patients, presumably due to their skin tone. (i.e., low arterial oxygen saturation despite a seemingly normal pulse oximetry reading). While inaccuracy of pulse oximeter measurements in patients with darker skin has been recognized for decades, recent studies have highlighted this as an ongoing problem with potentially severe consequences for Black patients and other patients of color.
One recent study found that Black patients had almost three times the likelihood of occult hypoxemia compared with White patients (Sjoding, MW, et al. N Engl J Med. 2020;383[25]:2477-8).
Subsequent studies have confirmed this to be a widespread problem across various clinical settings in hundreds of hospitals (Wong AI, et al. JAMA Netw Open. 2021;4[11]:e2131674; Valbuena VS, et al. Chest. 2022;161[4]:971-8). A recent retrospective cohort study of patients with COVID-19 found that occult hypoxemia in Black and Hispanic patients was associated with delayed eligibility for potentially lifesaving COVID-19 therapies (Fawzy AF, et al. JAMA Intern Med. 2022; published online May 31, 2022).
Now that numerous studies have demonstrated the inaccuracy of pulse oximetry with the potential to cause harm to historically marginalized racial and ethnic groups, must we abandon the use of pulse oximetry? We would argue that pulse oximeters remain valuable tools, but for now, we must adapt our practice until better devices are widely adopted.
First, it is crucial that health professionals are aware that pulse oximeters may underestimate the true extent of hypoxemia for all patients, but particularly for patients with darker skin. Acknowledging this device flaw is essential to avoid harm to our patients.
Second, clinicians must have heightened skepticism for seemingly normal pulse oximetry values when caring for symptomatic patients at risk of occult hypoxemia.
Until better pulse oximeters are widely available, clinicians must consider workarounds aimed at ensuring timely identification of hypoxemia in Black patients and other patients of color.
These patients may need invasive monitoring of arterial oxygenation, including arterial blood gas checks or an arterial catheter. However, invasive monitoring comes at the cost of discomfort to patients and potential complications, such as vessel or nerve damage.
Invasive monitoring of patients at risk for occult hypoxemia is not an equitable or acceptable long-term solution for this problem. As advocates for patients, clinicians and professional organizations should lobby regulatory bodies to ensure pulse oximeters are accurate for all patients.
We must also call on government leaders to move this process forward. For example, in response to efforts by the United Kingdom’s Intensive Care Society, the Health Secretary of the UK, Sajid Javid, has called for a review of pulse oximeters as part of a larger review assessing structural issues in health care that lead to worse outcomes in racial and ethnic minorities (BBC News. https://www.bbc.com/news/uk-59363544. Published online Nov. 21, 2021).
Device companies are largely for-profit corporations with obligations to their shareholders. It seems that existing incentives are insufficient to motivate investment in less biased technology and real-world evaluations of their devices.
We previously called for buyers of pulse oximeters to change the incentives of device companies – that is, for “hospitals to commit to only purchasing pulse oximeters that have been shown to work equally well in patients of colour.” (Hidalgo DC, et al. Lancet Respir Med. 2021;9[4]:E37). And, indeed, we worry that hospitals are putting themselves at medicolegal risk by not raising their purchasing standards. Since it is now widely known that pulse oximeters are inaccurate in certain patients, could there be liability for hospitals that continue to use devices we know to be disproportionately inaccurate by race?
Device companies must commit to fixing racial bias in pulse oximeters. Change is feasible, and pulse oximeters can be redesigned to be accurate and reliable among all patients using existing technology that is decades-old.
In the 1960s and 1970s, Hewlett Packard worked with NASA to noninvasively measure oxygen saturation in astronauts (Moran-Thomas, M. Wired. Published online June 4, 2021. https://www.wired.com/story/pulse-oximeters-equity). The device was designed to work for all skin tones and could be calibrated based on an individual’s skin tone. However, Hewlett Packard moved away from medical devices in the 1980s, shelving their design while other companies took over the oximeter market.
Lastly, as new devices are designed, they must be proven to work for all patients. Testing should be conducted in real-world clinical settings using metrics aligned with clinical care, since we know testing in artificial environments may not generalize to critically ill patients. Testing standards historically used by the FDA, such as only requiring device testing in a small number of non-White individuals, may miss clinically relevant hypoxemia. Non-inferiority studies are particularly susceptible to poor design or under-powering, and rigorous standards are needed from unbiased sources.
While potential solutions are currently being evaluated, the fact remains that the inaccuracy of pulse oximeters has been known for decades without any meaningful action taken to correct the problem.
As Valeria Valbuena, author of a study demonstrating inaccuracy of pulse oximetry in patients about to undergo ECMO, points out, “Using White patients as the standard in biomedical design has led to both differential care and innovation inertia for optimizing the way devices and algorithms work for patients of racial and ethnic minoritized groups” (Valbuena VS. JAMA Intern Med. 2022. doi: 10.1001/jamainternmed.2022.1903).
We know that hypoxemia is dangerous for our patients and that this is only one example of the long-standing systemic racism leading to harm in historically marginalized racial and ethnic groups. It is unacceptable that the devices we rely on to care for our patients are disproportionately inaccurate in non-White patients.
We hope that with increased awareness of this problem, meaningful action will be taken by device companies to ensure pulse oximeters work accurately for all patients.
From the Division of Pulmonary and Critical Care, Department of Medicine and the Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School (Drs. Harlan and Valley), and the Institute for Healthcare Policy and Innovation (Dr. Valley), University of Michigan, Ann Arbor, MI; and the Division of Pulmonary Sciences and Critical Care Medicine, University of Colorado School of Medicine, Aurora, CO (Dr. Colon Hidalgo).
Pulse oximetry is a vital monitoring tool in the ICU and in pulmonary medicine. Regrettably, re-emerging data show that pulse oximeters do not accurately measure blood oxygen levels in Black patients, presumably due to their skin tone. (i.e., low arterial oxygen saturation despite a seemingly normal pulse oximetry reading). While inaccuracy of pulse oximeter measurements in patients with darker skin has been recognized for decades, recent studies have highlighted this as an ongoing problem with potentially severe consequences for Black patients and other patients of color.
One recent study found that Black patients had almost three times the likelihood of occult hypoxemia compared with White patients (Sjoding, MW, et al. N Engl J Med. 2020;383[25]:2477-8).
Subsequent studies have confirmed this to be a widespread problem across various clinical settings in hundreds of hospitals (Wong AI, et al. JAMA Netw Open. 2021;4[11]:e2131674; Valbuena VS, et al. Chest. 2022;161[4]:971-8). A recent retrospective cohort study of patients with COVID-19 found that occult hypoxemia in Black and Hispanic patients was associated with delayed eligibility for potentially lifesaving COVID-19 therapies (Fawzy AF, et al. JAMA Intern Med. 2022; published online May 31, 2022).
Now that numerous studies have demonstrated the inaccuracy of pulse oximetry with the potential to cause harm to historically marginalized racial and ethnic groups, must we abandon the use of pulse oximetry? We would argue that pulse oximeters remain valuable tools, but for now, we must adapt our practice until better devices are widely adopted.
First, it is crucial that health professionals are aware that pulse oximeters may underestimate the true extent of hypoxemia for all patients, but particularly for patients with darker skin. Acknowledging this device flaw is essential to avoid harm to our patients.
Second, clinicians must have heightened skepticism for seemingly normal pulse oximetry values when caring for symptomatic patients at risk of occult hypoxemia.
Until better pulse oximeters are widely available, clinicians must consider workarounds aimed at ensuring timely identification of hypoxemia in Black patients and other patients of color.
These patients may need invasive monitoring of arterial oxygenation, including arterial blood gas checks or an arterial catheter. However, invasive monitoring comes at the cost of discomfort to patients and potential complications, such as vessel or nerve damage.
Invasive monitoring of patients at risk for occult hypoxemia is not an equitable or acceptable long-term solution for this problem. As advocates for patients, clinicians and professional organizations should lobby regulatory bodies to ensure pulse oximeters are accurate for all patients.
We must also call on government leaders to move this process forward. For example, in response to efforts by the United Kingdom’s Intensive Care Society, the Health Secretary of the UK, Sajid Javid, has called for a review of pulse oximeters as part of a larger review assessing structural issues in health care that lead to worse outcomes in racial and ethnic minorities (BBC News. https://www.bbc.com/news/uk-59363544. Published online Nov. 21, 2021).
Device companies are largely for-profit corporations with obligations to their shareholders. It seems that existing incentives are insufficient to motivate investment in less biased technology and real-world evaluations of their devices.
We previously called for buyers of pulse oximeters to change the incentives of device companies – that is, for “hospitals to commit to only purchasing pulse oximeters that have been shown to work equally well in patients of colour.” (Hidalgo DC, et al. Lancet Respir Med. 2021;9[4]:E37). And, indeed, we worry that hospitals are putting themselves at medicolegal risk by not raising their purchasing standards. Since it is now widely known that pulse oximeters are inaccurate in certain patients, could there be liability for hospitals that continue to use devices we know to be disproportionately inaccurate by race?
Device companies must commit to fixing racial bias in pulse oximeters. Change is feasible, and pulse oximeters can be redesigned to be accurate and reliable among all patients using existing technology that is decades-old.
In the 1960s and 1970s, Hewlett Packard worked with NASA to noninvasively measure oxygen saturation in astronauts (Moran-Thomas, M. Wired. Published online June 4, 2021. https://www.wired.com/story/pulse-oximeters-equity). The device was designed to work for all skin tones and could be calibrated based on an individual’s skin tone. However, Hewlett Packard moved away from medical devices in the 1980s, shelving their design while other companies took over the oximeter market.
Lastly, as new devices are designed, they must be proven to work for all patients. Testing should be conducted in real-world clinical settings using metrics aligned with clinical care, since we know testing in artificial environments may not generalize to critically ill patients. Testing standards historically used by the FDA, such as only requiring device testing in a small number of non-White individuals, may miss clinically relevant hypoxemia. Non-inferiority studies are particularly susceptible to poor design or under-powering, and rigorous standards are needed from unbiased sources.
While potential solutions are currently being evaluated, the fact remains that the inaccuracy of pulse oximeters has been known for decades without any meaningful action taken to correct the problem.
As Valeria Valbuena, author of a study demonstrating inaccuracy of pulse oximetry in patients about to undergo ECMO, points out, “Using White patients as the standard in biomedical design has led to both differential care and innovation inertia for optimizing the way devices and algorithms work for patients of racial and ethnic minoritized groups” (Valbuena VS. JAMA Intern Med. 2022. doi: 10.1001/jamainternmed.2022.1903).
We know that hypoxemia is dangerous for our patients and that this is only one example of the long-standing systemic racism leading to harm in historically marginalized racial and ethnic groups. It is unacceptable that the devices we rely on to care for our patients are disproportionately inaccurate in non-White patients.
We hope that with increased awareness of this problem, meaningful action will be taken by device companies to ensure pulse oximeters work accurately for all patients.
From the Division of Pulmonary and Critical Care, Department of Medicine and the Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School (Drs. Harlan and Valley), and the Institute for Healthcare Policy and Innovation (Dr. Valley), University of Michigan, Ann Arbor, MI; and the Division of Pulmonary Sciences and Critical Care Medicine, University of Colorado School of Medicine, Aurora, CO (Dr. Colon Hidalgo).
Pulse oximetry is a vital monitoring tool in the ICU and in pulmonary medicine. Regrettably, re-emerging data show that pulse oximeters do not accurately measure blood oxygen levels in Black patients, presumably due to their skin tone. (i.e., low arterial oxygen saturation despite a seemingly normal pulse oximetry reading). While inaccuracy of pulse oximeter measurements in patients with darker skin has been recognized for decades, recent studies have highlighted this as an ongoing problem with potentially severe consequences for Black patients and other patients of color.
One recent study found that Black patients had almost three times the likelihood of occult hypoxemia compared with White patients (Sjoding, MW, et al. N Engl J Med. 2020;383[25]:2477-8).
Subsequent studies have confirmed this to be a widespread problem across various clinical settings in hundreds of hospitals (Wong AI, et al. JAMA Netw Open. 2021;4[11]:e2131674; Valbuena VS, et al. Chest. 2022;161[4]:971-8). A recent retrospective cohort study of patients with COVID-19 found that occult hypoxemia in Black and Hispanic patients was associated with delayed eligibility for potentially lifesaving COVID-19 therapies (Fawzy AF, et al. JAMA Intern Med. 2022; published online May 31, 2022).
Now that numerous studies have demonstrated the inaccuracy of pulse oximetry with the potential to cause harm to historically marginalized racial and ethnic groups, must we abandon the use of pulse oximetry? We would argue that pulse oximeters remain valuable tools, but for now, we must adapt our practice until better devices are widely adopted.
First, it is crucial that health professionals are aware that pulse oximeters may underestimate the true extent of hypoxemia for all patients, but particularly for patients with darker skin. Acknowledging this device flaw is essential to avoid harm to our patients.
Second, clinicians must have heightened skepticism for seemingly normal pulse oximetry values when caring for symptomatic patients at risk of occult hypoxemia.
Until better pulse oximeters are widely available, clinicians must consider workarounds aimed at ensuring timely identification of hypoxemia in Black patients and other patients of color.
These patients may need invasive monitoring of arterial oxygenation, including arterial blood gas checks or an arterial catheter. However, invasive monitoring comes at the cost of discomfort to patients and potential complications, such as vessel or nerve damage.
Invasive monitoring of patients at risk for occult hypoxemia is not an equitable or acceptable long-term solution for this problem. As advocates for patients, clinicians and professional organizations should lobby regulatory bodies to ensure pulse oximeters are accurate for all patients.
We must also call on government leaders to move this process forward. For example, in response to efforts by the United Kingdom’s Intensive Care Society, the Health Secretary of the UK, Sajid Javid, has called for a review of pulse oximeters as part of a larger review assessing structural issues in health care that lead to worse outcomes in racial and ethnic minorities (BBC News. https://www.bbc.com/news/uk-59363544. Published online Nov. 21, 2021).
Device companies are largely for-profit corporations with obligations to their shareholders. It seems that existing incentives are insufficient to motivate investment in less biased technology and real-world evaluations of their devices.
We previously called for buyers of pulse oximeters to change the incentives of device companies – that is, for “hospitals to commit to only purchasing pulse oximeters that have been shown to work equally well in patients of colour.” (Hidalgo DC, et al. Lancet Respir Med. 2021;9[4]:E37). And, indeed, we worry that hospitals are putting themselves at medicolegal risk by not raising their purchasing standards. Since it is now widely known that pulse oximeters are inaccurate in certain patients, could there be liability for hospitals that continue to use devices we know to be disproportionately inaccurate by race?
Device companies must commit to fixing racial bias in pulse oximeters. Change is feasible, and pulse oximeters can be redesigned to be accurate and reliable among all patients using existing technology that is decades-old.
In the 1960s and 1970s, Hewlett Packard worked with NASA to noninvasively measure oxygen saturation in astronauts (Moran-Thomas, M. Wired. Published online June 4, 2021. https://www.wired.com/story/pulse-oximeters-equity). The device was designed to work for all skin tones and could be calibrated based on an individual’s skin tone. However, Hewlett Packard moved away from medical devices in the 1980s, shelving their design while other companies took over the oximeter market.
Lastly, as new devices are designed, they must be proven to work for all patients. Testing should be conducted in real-world clinical settings using metrics aligned with clinical care, since we know testing in artificial environments may not generalize to critically ill patients. Testing standards historically used by the FDA, such as only requiring device testing in a small number of non-White individuals, may miss clinically relevant hypoxemia. Non-inferiority studies are particularly susceptible to poor design or under-powering, and rigorous standards are needed from unbiased sources.
While potential solutions are currently being evaluated, the fact remains that the inaccuracy of pulse oximeters has been known for decades without any meaningful action taken to correct the problem.
As Valeria Valbuena, author of a study demonstrating inaccuracy of pulse oximetry in patients about to undergo ECMO, points out, “Using White patients as the standard in biomedical design has led to both differential care and innovation inertia for optimizing the way devices and algorithms work for patients of racial and ethnic minoritized groups” (Valbuena VS. JAMA Intern Med. 2022. doi: 10.1001/jamainternmed.2022.1903).
We know that hypoxemia is dangerous for our patients and that this is only one example of the long-standing systemic racism leading to harm in historically marginalized racial and ethnic groups. It is unacceptable that the devices we rely on to care for our patients are disproportionately inaccurate in non-White patients.
We hope that with increased awareness of this problem, meaningful action will be taken by device companies to ensure pulse oximeters work accurately for all patients.
From the Division of Pulmonary and Critical Care, Department of Medicine and the Center for Bioethics and Social Sciences in Medicine, University of Michigan Medical School (Drs. Harlan and Valley), and the Institute for Healthcare Policy and Innovation (Dr. Valley), University of Michigan, Ann Arbor, MI; and the Division of Pulmonary Sciences and Critical Care Medicine, University of Colorado School of Medicine, Aurora, CO (Dr. Colon Hidalgo).
Pneumothorax, pneumomediastinum, and subcutaneous emphysema: The many faces of COVID-19 ARDS
I recall early in the pandemic being called to the bedside to examine an acutely decompensating patient with COVID-19. This was a 33-year-old, previously healthy woman, admitted to the medical ICU with hypoxemic respiratory failure requiring mechanical ventilation and undergoing treatment for severe acute respiratory distress syndrome (ARDS). I quickly realized she was seconds away from an arrest. As I examined her, one thing caught my eye. Her airway pressures had skyrocketed over the past few minutes. Could it be? I thought to myself as I reached for the ultrasound that confirmed my suspicions, tension pneumothorax. One emergent needle decompression and chest tube later and she survives, only to die a week later from overwhelming hypoxemia.
As we reflect on these past 26 months, we recall that caring for the critically ill patient with COVID-19 has posed numerous challenges. One challenge was the overwhelming incidence of the so-called “barotrauma-related complications.” However, we also recall seeing many patients develop such complications while receiving supplemental noninvasive forms of respiratory support. Perhaps, this is in agreement with prior literature that specifically discusses the presence of air outside the tracheobronchial tree and how it does not always correlate with high airway pressure and high tidal volumes, refuting the argument that these complications always fall under the umbrella of barotrauma. We will discuss these complications and attempt to shed light on the potential variables associated with their development.
The development of pneumothorax is a well-recognized complication associated with ventilator-dependent ARDS thought to be a form of barotrauma, with some reports indicating an incidence of 48.8% (Gattinoni L et al. JAMA. 1994;271[2]):1772-9) and a significantly increased mortality rate compared with postprocedural pneumothorax in the ICU (Chen K et al. Chest. 2002;122[2]:678-83). The incidence of such complication in COVID-19-related ARDS is significantly higher than in ARDS from other causes (Belletti A et al. Crit Care Med. 2022;50[3]:491-500), with a mortality rate approaching 100% (Chong WH et al. Heart Lung. 2021;50[5]:599-608).
So why are patients with COVID-19 developing these complications at a higher rate? When we examine the literature, we note that Leisman and colleagues (Am J Respir Crit Care Med. 2022;205[5]:507-19) describe higher baseline markers of alveolar damage, including RAGE (receptor for advanced glycation end-products) in mechanically ventilated patients with COVID-19 vs patients requiring mechanical ventilation for other causes. This poses a question that perhaps one of the main reasons patients with COVID-19 ARDS are at an increased risk for developing certain complications, such as pneumothorax, is inherent to the unique type of alveolar injury sustained with the infection. The authors also note that alveolar markers of injury had moderate to poor discrimination for invasive ventilation early in the disease and diminished over time in both ventilated patients receiving lung protective ventilation strategy and those spontaneously breathing. Likewise, this important finding suggests that the development of pneumothorax in patients with COVID-19 may not be entirely related to barotrauma.
Another phenomenon worth investigating is the development of pneumomediastinum and subcutaneous emphysema, with a reported seven-fold increased risk of development in patients with COVID-19. Lemmers and colleagues (ERJ Open Res. 2020;6[4]:00385-2020) found no statistically significant difference in PEEP, plateau pressure, ratio of tidal volume to ideal body weight, or compliance between patients who developed this complication and those who did not, again, signifying that perhaps there is more to the story here.
Belletti and colleagues (J Cardiothorac Vasc Anesth. 2021;35[12]:3642-51) published an article examining the predictors of pneumothorax and pneumomediastinum in patients with COVID-19. The authors found that the time from symptom onset to intubation and the total bilirubin level were the only two significant predictors for the development of these complications. They explain that longer time from symptom onset to intubation likely increased the risk for self-induced lung injury, inflammation, and fibrosis, contributing to the development of such complications. It is important to note that the authors did not find a significant difference in the ventilation parameters between patients who developed pneumothorax/pneumomediastinum and those who did not.
In our institute, we examined a total of 102 patients admitted to the ICU with COVID-19 ARDS over a 3-month period from March 2020 to May 2020. We identified a total of 36 patients who developed pneumothorax, pneumomediastinum, and/or subcutaneous emphysema. We compared these subjects to age- and gender-matched control subjects. Higher age was associated with an increased risk of development of these complications, whereas the presence of diabetes mellitus, hypertension, and chronic kidney disease at baseline was associated with lower risk. This translated into lower mSOFA scores in our subjects as opposed to the control subjects mainly due to higher creatinine levels at baseline in the control group, skewing our data and indicating that some predictive criteria may not reflect the underlying disease severity and risk for development of such complications. In analyzing our ventilator data and comparing the subjects to the control group, we found no differences in mode of ventilation, set tidal volumes, or PEEP levels between the two. The subjects had significantly higher peak airway pressures, lower compliance, and longer ventilator days. Intubation was needed significantly earlier in the subjects compared with the control group with a median of 2 days vs 6 days from admission. Our data are in concordance with prior published reports and are set to be presented in abstract form this May.
COVID-19 remains a challenging disease with the potential for morbid outcomes. As we phase out of the pandemic and move into an epidemic, future research direction will likely focus on some of the more unusually common complications, such as the ones presented here.
Dr. Abdullah is with the Henry Ford Health System, Detroit, Michigan.
I recall early in the pandemic being called to the bedside to examine an acutely decompensating patient with COVID-19. This was a 33-year-old, previously healthy woman, admitted to the medical ICU with hypoxemic respiratory failure requiring mechanical ventilation and undergoing treatment for severe acute respiratory distress syndrome (ARDS). I quickly realized she was seconds away from an arrest. As I examined her, one thing caught my eye. Her airway pressures had skyrocketed over the past few minutes. Could it be? I thought to myself as I reached for the ultrasound that confirmed my suspicions, tension pneumothorax. One emergent needle decompression and chest tube later and she survives, only to die a week later from overwhelming hypoxemia.
As we reflect on these past 26 months, we recall that caring for the critically ill patient with COVID-19 has posed numerous challenges. One challenge was the overwhelming incidence of the so-called “barotrauma-related complications.” However, we also recall seeing many patients develop such complications while receiving supplemental noninvasive forms of respiratory support. Perhaps, this is in agreement with prior literature that specifically discusses the presence of air outside the tracheobronchial tree and how it does not always correlate with high airway pressure and high tidal volumes, refuting the argument that these complications always fall under the umbrella of barotrauma. We will discuss these complications and attempt to shed light on the potential variables associated with their development.
The development of pneumothorax is a well-recognized complication associated with ventilator-dependent ARDS thought to be a form of barotrauma, with some reports indicating an incidence of 48.8% (Gattinoni L et al. JAMA. 1994;271[2]):1772-9) and a significantly increased mortality rate compared with postprocedural pneumothorax in the ICU (Chen K et al. Chest. 2002;122[2]:678-83). The incidence of such complication in COVID-19-related ARDS is significantly higher than in ARDS from other causes (Belletti A et al. Crit Care Med. 2022;50[3]:491-500), with a mortality rate approaching 100% (Chong WH et al. Heart Lung. 2021;50[5]:599-608).
So why are patients with COVID-19 developing these complications at a higher rate? When we examine the literature, we note that Leisman and colleagues (Am J Respir Crit Care Med. 2022;205[5]:507-19) describe higher baseline markers of alveolar damage, including RAGE (receptor for advanced glycation end-products) in mechanically ventilated patients with COVID-19 vs patients requiring mechanical ventilation for other causes. This poses a question that perhaps one of the main reasons patients with COVID-19 ARDS are at an increased risk for developing certain complications, such as pneumothorax, is inherent to the unique type of alveolar injury sustained with the infection. The authors also note that alveolar markers of injury had moderate to poor discrimination for invasive ventilation early in the disease and diminished over time in both ventilated patients receiving lung protective ventilation strategy and those spontaneously breathing. Likewise, this important finding suggests that the development of pneumothorax in patients with COVID-19 may not be entirely related to barotrauma.
Another phenomenon worth investigating is the development of pneumomediastinum and subcutaneous emphysema, with a reported seven-fold increased risk of development in patients with COVID-19. Lemmers and colleagues (ERJ Open Res. 2020;6[4]:00385-2020) found no statistically significant difference in PEEP, plateau pressure, ratio of tidal volume to ideal body weight, or compliance between patients who developed this complication and those who did not, again, signifying that perhaps there is more to the story here.
Belletti and colleagues (J Cardiothorac Vasc Anesth. 2021;35[12]:3642-51) published an article examining the predictors of pneumothorax and pneumomediastinum in patients with COVID-19. The authors found that the time from symptom onset to intubation and the total bilirubin level were the only two significant predictors for the development of these complications. They explain that longer time from symptom onset to intubation likely increased the risk for self-induced lung injury, inflammation, and fibrosis, contributing to the development of such complications. It is important to note that the authors did not find a significant difference in the ventilation parameters between patients who developed pneumothorax/pneumomediastinum and those who did not.
In our institute, we examined a total of 102 patients admitted to the ICU with COVID-19 ARDS over a 3-month period from March 2020 to May 2020. We identified a total of 36 patients who developed pneumothorax, pneumomediastinum, and/or subcutaneous emphysema. We compared these subjects to age- and gender-matched control subjects. Higher age was associated with an increased risk of development of these complications, whereas the presence of diabetes mellitus, hypertension, and chronic kidney disease at baseline was associated with lower risk. This translated into lower mSOFA scores in our subjects as opposed to the control subjects mainly due to higher creatinine levels at baseline in the control group, skewing our data and indicating that some predictive criteria may not reflect the underlying disease severity and risk for development of such complications. In analyzing our ventilator data and comparing the subjects to the control group, we found no differences in mode of ventilation, set tidal volumes, or PEEP levels between the two. The subjects had significantly higher peak airway pressures, lower compliance, and longer ventilator days. Intubation was needed significantly earlier in the subjects compared with the control group with a median of 2 days vs 6 days from admission. Our data are in concordance with prior published reports and are set to be presented in abstract form this May.
COVID-19 remains a challenging disease with the potential for morbid outcomes. As we phase out of the pandemic and move into an epidemic, future research direction will likely focus on some of the more unusually common complications, such as the ones presented here.
Dr. Abdullah is with the Henry Ford Health System, Detroit, Michigan.
I recall early in the pandemic being called to the bedside to examine an acutely decompensating patient with COVID-19. This was a 33-year-old, previously healthy woman, admitted to the medical ICU with hypoxemic respiratory failure requiring mechanical ventilation and undergoing treatment for severe acute respiratory distress syndrome (ARDS). I quickly realized she was seconds away from an arrest. As I examined her, one thing caught my eye. Her airway pressures had skyrocketed over the past few minutes. Could it be? I thought to myself as I reached for the ultrasound that confirmed my suspicions, tension pneumothorax. One emergent needle decompression and chest tube later and she survives, only to die a week later from overwhelming hypoxemia.
As we reflect on these past 26 months, we recall that caring for the critically ill patient with COVID-19 has posed numerous challenges. One challenge was the overwhelming incidence of the so-called “barotrauma-related complications.” However, we also recall seeing many patients develop such complications while receiving supplemental noninvasive forms of respiratory support. Perhaps, this is in agreement with prior literature that specifically discusses the presence of air outside the tracheobronchial tree and how it does not always correlate with high airway pressure and high tidal volumes, refuting the argument that these complications always fall under the umbrella of barotrauma. We will discuss these complications and attempt to shed light on the potential variables associated with their development.
The development of pneumothorax is a well-recognized complication associated with ventilator-dependent ARDS thought to be a form of barotrauma, with some reports indicating an incidence of 48.8% (Gattinoni L et al. JAMA. 1994;271[2]):1772-9) and a significantly increased mortality rate compared with postprocedural pneumothorax in the ICU (Chen K et al. Chest. 2002;122[2]:678-83). The incidence of such complication in COVID-19-related ARDS is significantly higher than in ARDS from other causes (Belletti A et al. Crit Care Med. 2022;50[3]:491-500), with a mortality rate approaching 100% (Chong WH et al. Heart Lung. 2021;50[5]:599-608).
So why are patients with COVID-19 developing these complications at a higher rate? When we examine the literature, we note that Leisman and colleagues (Am J Respir Crit Care Med. 2022;205[5]:507-19) describe higher baseline markers of alveolar damage, including RAGE (receptor for advanced glycation end-products) in mechanically ventilated patients with COVID-19 vs patients requiring mechanical ventilation for other causes. This poses a question that perhaps one of the main reasons patients with COVID-19 ARDS are at an increased risk for developing certain complications, such as pneumothorax, is inherent to the unique type of alveolar injury sustained with the infection. The authors also note that alveolar markers of injury had moderate to poor discrimination for invasive ventilation early in the disease and diminished over time in both ventilated patients receiving lung protective ventilation strategy and those spontaneously breathing. Likewise, this important finding suggests that the development of pneumothorax in patients with COVID-19 may not be entirely related to barotrauma.
Another phenomenon worth investigating is the development of pneumomediastinum and subcutaneous emphysema, with a reported seven-fold increased risk of development in patients with COVID-19. Lemmers and colleagues (ERJ Open Res. 2020;6[4]:00385-2020) found no statistically significant difference in PEEP, plateau pressure, ratio of tidal volume to ideal body weight, or compliance between patients who developed this complication and those who did not, again, signifying that perhaps there is more to the story here.
Belletti and colleagues (J Cardiothorac Vasc Anesth. 2021;35[12]:3642-51) published an article examining the predictors of pneumothorax and pneumomediastinum in patients with COVID-19. The authors found that the time from symptom onset to intubation and the total bilirubin level were the only two significant predictors for the development of these complications. They explain that longer time from symptom onset to intubation likely increased the risk for self-induced lung injury, inflammation, and fibrosis, contributing to the development of such complications. It is important to note that the authors did not find a significant difference in the ventilation parameters between patients who developed pneumothorax/pneumomediastinum and those who did not.
In our institute, we examined a total of 102 patients admitted to the ICU with COVID-19 ARDS over a 3-month period from March 2020 to May 2020. We identified a total of 36 patients who developed pneumothorax, pneumomediastinum, and/or subcutaneous emphysema. We compared these subjects to age- and gender-matched control subjects. Higher age was associated with an increased risk of development of these complications, whereas the presence of diabetes mellitus, hypertension, and chronic kidney disease at baseline was associated with lower risk. This translated into lower mSOFA scores in our subjects as opposed to the control subjects mainly due to higher creatinine levels at baseline in the control group, skewing our data and indicating that some predictive criteria may not reflect the underlying disease severity and risk for development of such complications. In analyzing our ventilator data and comparing the subjects to the control group, we found no differences in mode of ventilation, set tidal volumes, or PEEP levels between the two. The subjects had significantly higher peak airway pressures, lower compliance, and longer ventilator days. Intubation was needed significantly earlier in the subjects compared with the control group with a median of 2 days vs 6 days from admission. Our data are in concordance with prior published reports and are set to be presented in abstract form this May.
COVID-19 remains a challenging disease with the potential for morbid outcomes. As we phase out of the pandemic and move into an epidemic, future research direction will likely focus on some of the more unusually common complications, such as the ones presented here.
Dr. Abdullah is with the Henry Ford Health System, Detroit, Michigan.
What COVID-19 taught us: The challenge of maintaining contingency level care to proactively forestall crisis care
In 2014, the Task Force for Mass Critical Care (TFMCC) published a CHEST consensus statement on disaster preparedness principles in caring for the critically ill during disasters and pandemics (Christian et al. CHEST. 2014;146[4_suppl]:8s-34s). This publication attempted to guide preparedness for both single-event disasters and more prolonged events, including a feared influenza pandemic.
Despite the foundation of planning and support this guidance provided, the COVID-19 pandemic response revealed substantial gaps in our understanding and preparedness for these more prolonged and widespread events.
In New York City, as the first COVID-19 wave began in March and April of 2020, area hospitals responded with surge plans that prioritized what was felt to be most important (Griffin et al. Am J Respir Crit Care Med. 2020 Jun 1;201[11]:1337-44). Tiered, creative staffing structures were rapidly created with intensivists supervising non-ICU physicians and APPs. Procedure teams were created for intubation, proning, and central line placement. ICU space was created with adaptations to ORs and PACUs, and rooms on med-surg floors and step-down units underwent emergency renovations to allow creation of new “pop-up” ICUs. Triage protocols were altered: patients on high levels of supplemental oxygen, who would under normal circumstances have been admitted to an ICU, were triaged to floors and stepdown units. Equipment was reused, modified, and substituted creatively to optimize care for the maximum number of patients.
In the face of all of these struggles, many around the country and the world felt the efforts, though heroic, resulted in less than standard of care. Two subsequent publications validated this concern (Kadri et al. Ann Int Med. 2021,174;9:1240-51; Bravata DM et al. JAMA Open Network. 2021;4[1]:e2034266), demonstrating during severe surge, COVID-19 patients’ mortality increased significantly beyond that seen in non-surging or less-severe surging times, demonstrating a mortality effect of surge itself. Though these studies observed COVID-19 patients only, there is every reason to believe the findings applied to all critically ill patients cared for during these surges.
These experiences led the TFMCC to report updated strategies for remaining in contingency care levels and avoiding crisis care (Dichter JR et al. CHEST. 2022;161[2]:429-47). Contingency is equivalent to routine care though may require adaptations and employment of otherwise non-traditional resources. The ultimate goal of mass critical care in a public health emergency is to avoid crisis-operating conditions, crisis standards of care, and their associated challenging triage decisions regarding allocation of scarce resources.
The 10 suggestions included in the most recent TFMCC publication include staffing strategies and suggestions based on COVID-19 experiences for graded staff-to-patient ratios, and support processes to preserve the existing health care work force. Strategies also include reduction of redundant documentation, limiting overtime, and most importantly, approaches for improving teamwork and supporting psychological well-being and resilience. Examples include daily unit huddles to update care and share experiences, genuine intra-team recognition and appreciation, and embedding emotional health experts within teams to provide ongoing support.
Consistent communication between incident command and frontline clinicians was also a suggested priority, perhaps with a newly proposed position of physician clinical support supervisor. This would be a formal role within hospital incident command, a liaison between the two groups.
Surge strategies should include empowerment of bedside clinicians and leaders with both planning and real-time assessment of the clinical situation, as being at the front line of care enables the situational awareness to assess ICU strain most effectively. Further, ICU clinicians must recognize when progression deeper into contingency operations occurs and they become perilously close to crisis mode. At this point, decisions are made and scarce resources are modified beyond routine standards of care to preserve life. TFMCC designates this gray area between contingency and crisis as the Critical Clinical Prioritization level (Figure). 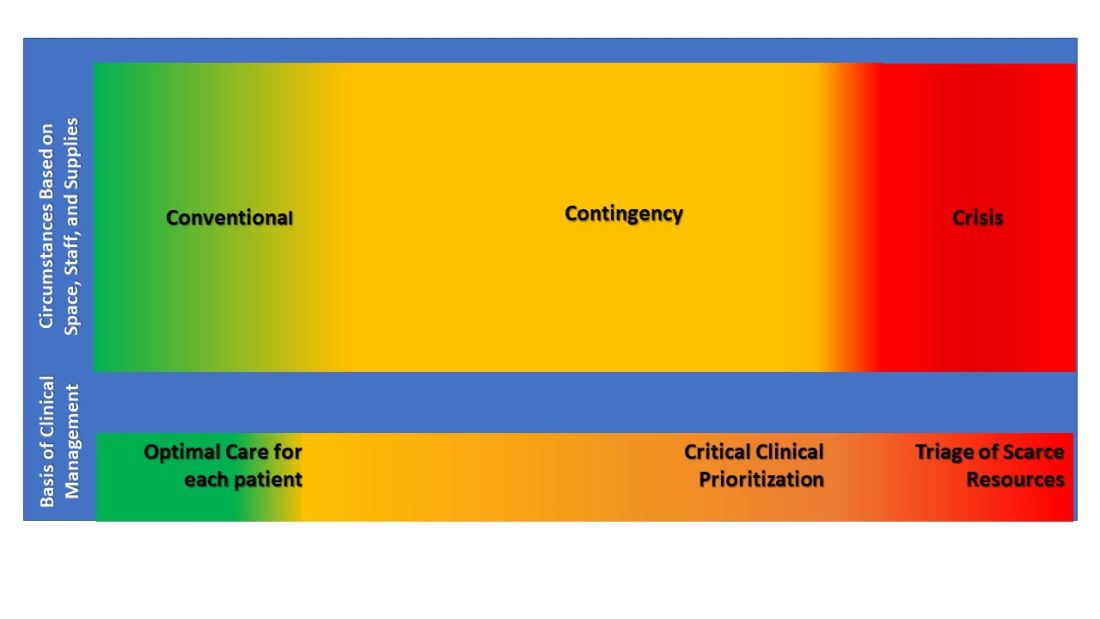
At this point, more resources must be provided, or patients must be transferred to other resourced hospitals.
Critical Clinical Prioritization is an illustration of necessity being the mother of invention, as these are adaptations clinicians devised under duress. Some particularly poignant examples are the spreading of 24 hours of continuous renal replacement therapy (CRRT) resource between two and sometimes three patients to provide life sustainment to all; and when ventilators were in short supply, determining which patients required full ICU ventilator support vs those who could manage with lower functioning ventilators, and trading them between patients when demands changed.
These adaptations can only be done by experienced clinicians proactively managing bedside critical care under duress, further underscoring the importance of our suggestion that Critical Clinical Prioritization and ICU strain be managed by bedside clinicians and leaders.
The response of early transfer of patients – load-balancing - should be considered as soon as any hospital enters contingency conditions. This strategy is commonly implemented within larger health systems, ideally before reaching Critical Clinical Prioritization. Formal, organized state or regional load-balancing coordination, now referred to as medical operations command centers (MOCCs), were highly effective and proved lifesaving for those states that implemented them (including Arizona, Washington, California, Minnesota, and others). Support for establishment of MOCC’s is crucial in prolonging contingency operations and further helps support and protect disadvantaged populations (White et al. N Engl J Med. 2021;385[24]:2211-4).
Establishment of MOCCs has met resistance due to challenges that include interhospital/intersystem competition, logistics of moving critically ill patients sometimes across significant physical distance, and the costs of assuming care of uninsured or underinsured patients. Nevertheless, the benefits to the population as a whole necessitate working through these obstacles as successful MOCCs have done, usually with government and hospital association support.
In their final suggestion of the 2022 updated strategies, TFMCC suggests that hospitals use telemedicine technology both to expand specialists’ ability to provide care and facilitate families virtually visiting their critically ill loved one when safety precludes in-person visits.
These suggestions are pivotal in planning for future public health emergencies that include mass critical care, even during events that are limited in scope and duration.
Lastly, intensivists struggled with legal and ethical concerns when mired in crisis care circumstances and decisions of allocation, and potential reallocation, of scarce resources. These issues were not well addressed during the COVID-19 pandemic, further emphasizing the importance of maintaining contingency level care and requiring further involvement from legal and medical ethics professionals for future planning.
The guiding principle of disaster preparedness is that we must do all the planning we can to ensure that we never need crisis standards of care (National Academies of Sciences, Engineering, and Medicine. 2020 Mar 28. Rapid Expert Consultation on Crisis Standards of Care for the COVID-19 Pandemic. Washington, DC: The National Academies Press.).
We must be prepared. Guidelines and suggestions laid out through decades of experience gained a real-world test in the COVID-19 pandemic. Now we must all reorganize and create new plans or augment old ones with the information we have gained. The time is now. The work must continue.
Dr. Griffin is Assistant Professor of Medicine, New York Presbyterian Hospital – Weill Cornell Medicine. Dr. Dichter is Associate Professor of Medicine, University of Minnesota.
In 2014, the Task Force for Mass Critical Care (TFMCC) published a CHEST consensus statement on disaster preparedness principles in caring for the critically ill during disasters and pandemics (Christian et al. CHEST. 2014;146[4_suppl]:8s-34s). This publication attempted to guide preparedness for both single-event disasters and more prolonged events, including a feared influenza pandemic.
Despite the foundation of planning and support this guidance provided, the COVID-19 pandemic response revealed substantial gaps in our understanding and preparedness for these more prolonged and widespread events.
In New York City, as the first COVID-19 wave began in March and April of 2020, area hospitals responded with surge plans that prioritized what was felt to be most important (Griffin et al. Am J Respir Crit Care Med. 2020 Jun 1;201[11]:1337-44). Tiered, creative staffing structures were rapidly created with intensivists supervising non-ICU physicians and APPs. Procedure teams were created for intubation, proning, and central line placement. ICU space was created with adaptations to ORs and PACUs, and rooms on med-surg floors and step-down units underwent emergency renovations to allow creation of new “pop-up” ICUs. Triage protocols were altered: patients on high levels of supplemental oxygen, who would under normal circumstances have been admitted to an ICU, were triaged to floors and stepdown units. Equipment was reused, modified, and substituted creatively to optimize care for the maximum number of patients.
In the face of all of these struggles, many around the country and the world felt the efforts, though heroic, resulted in less than standard of care. Two subsequent publications validated this concern (Kadri et al. Ann Int Med. 2021,174;9:1240-51; Bravata DM et al. JAMA Open Network. 2021;4[1]:e2034266), demonstrating during severe surge, COVID-19 patients’ mortality increased significantly beyond that seen in non-surging or less-severe surging times, demonstrating a mortality effect of surge itself. Though these studies observed COVID-19 patients only, there is every reason to believe the findings applied to all critically ill patients cared for during these surges.
These experiences led the TFMCC to report updated strategies for remaining in contingency care levels and avoiding crisis care (Dichter JR et al. CHEST. 2022;161[2]:429-47). Contingency is equivalent to routine care though may require adaptations and employment of otherwise non-traditional resources. The ultimate goal of mass critical care in a public health emergency is to avoid crisis-operating conditions, crisis standards of care, and their associated challenging triage decisions regarding allocation of scarce resources.
The 10 suggestions included in the most recent TFMCC publication include staffing strategies and suggestions based on COVID-19 experiences for graded staff-to-patient ratios, and support processes to preserve the existing health care work force. Strategies also include reduction of redundant documentation, limiting overtime, and most importantly, approaches for improving teamwork and supporting psychological well-being and resilience. Examples include daily unit huddles to update care and share experiences, genuine intra-team recognition and appreciation, and embedding emotional health experts within teams to provide ongoing support.
Consistent communication between incident command and frontline clinicians was also a suggested priority, perhaps with a newly proposed position of physician clinical support supervisor. This would be a formal role within hospital incident command, a liaison between the two groups.
Surge strategies should include empowerment of bedside clinicians and leaders with both planning and real-time assessment of the clinical situation, as being at the front line of care enables the situational awareness to assess ICU strain most effectively. Further, ICU clinicians must recognize when progression deeper into contingency operations occurs and they become perilously close to crisis mode. At this point, decisions are made and scarce resources are modified beyond routine standards of care to preserve life. TFMCC designates this gray area between contingency and crisis as the Critical Clinical Prioritization level (Figure). 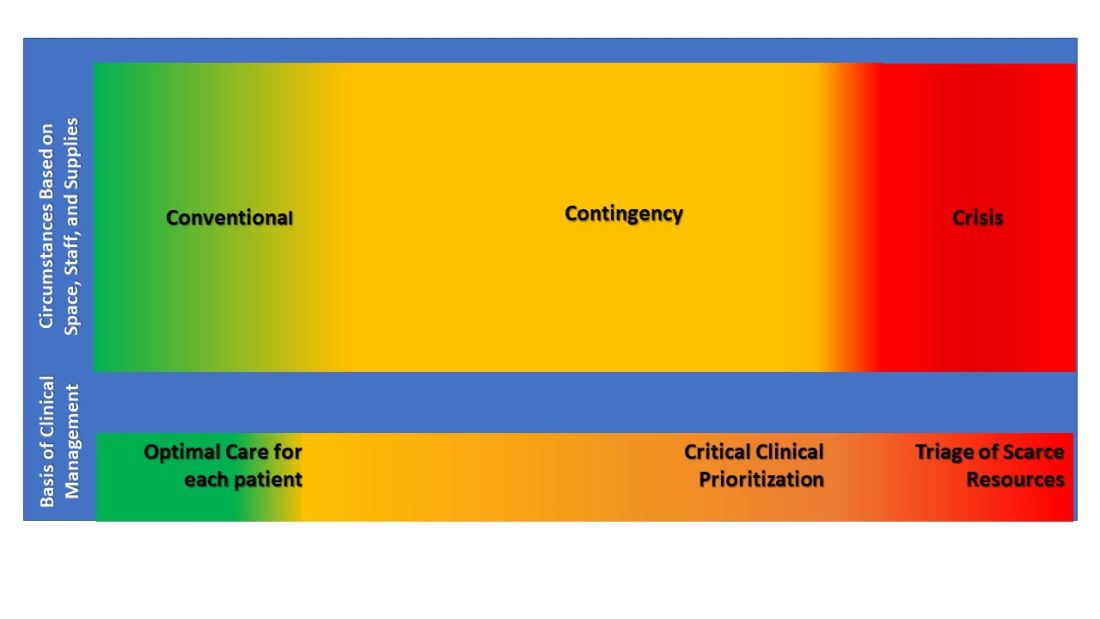
At this point, more resources must be provided, or patients must be transferred to other resourced hospitals.
Critical Clinical Prioritization is an illustration of necessity being the mother of invention, as these are adaptations clinicians devised under duress. Some particularly poignant examples are the spreading of 24 hours of continuous renal replacement therapy (CRRT) resource between two and sometimes three patients to provide life sustainment to all; and when ventilators were in short supply, determining which patients required full ICU ventilator support vs those who could manage with lower functioning ventilators, and trading them between patients when demands changed.
These adaptations can only be done by experienced clinicians proactively managing bedside critical care under duress, further underscoring the importance of our suggestion that Critical Clinical Prioritization and ICU strain be managed by bedside clinicians and leaders.
The response of early transfer of patients – load-balancing - should be considered as soon as any hospital enters contingency conditions. This strategy is commonly implemented within larger health systems, ideally before reaching Critical Clinical Prioritization. Formal, organized state or regional load-balancing coordination, now referred to as medical operations command centers (MOCCs), were highly effective and proved lifesaving for those states that implemented them (including Arizona, Washington, California, Minnesota, and others). Support for establishment of MOCC’s is crucial in prolonging contingency operations and further helps support and protect disadvantaged populations (White et al. N Engl J Med. 2021;385[24]:2211-4).
Establishment of MOCCs has met resistance due to challenges that include interhospital/intersystem competition, logistics of moving critically ill patients sometimes across significant physical distance, and the costs of assuming care of uninsured or underinsured patients. Nevertheless, the benefits to the population as a whole necessitate working through these obstacles as successful MOCCs have done, usually with government and hospital association support.
In their final suggestion of the 2022 updated strategies, TFMCC suggests that hospitals use telemedicine technology both to expand specialists’ ability to provide care and facilitate families virtually visiting their critically ill loved one when safety precludes in-person visits.
These suggestions are pivotal in planning for future public health emergencies that include mass critical care, even during events that are limited in scope and duration.
Lastly, intensivists struggled with legal and ethical concerns when mired in crisis care circumstances and decisions of allocation, and potential reallocation, of scarce resources. These issues were not well addressed during the COVID-19 pandemic, further emphasizing the importance of maintaining contingency level care and requiring further involvement from legal and medical ethics professionals for future planning.
The guiding principle of disaster preparedness is that we must do all the planning we can to ensure that we never need crisis standards of care (National Academies of Sciences, Engineering, and Medicine. 2020 Mar 28. Rapid Expert Consultation on Crisis Standards of Care for the COVID-19 Pandemic. Washington, DC: The National Academies Press.).
We must be prepared. Guidelines and suggestions laid out through decades of experience gained a real-world test in the COVID-19 pandemic. Now we must all reorganize and create new plans or augment old ones with the information we have gained. The time is now. The work must continue.
Dr. Griffin is Assistant Professor of Medicine, New York Presbyterian Hospital – Weill Cornell Medicine. Dr. Dichter is Associate Professor of Medicine, University of Minnesota.
In 2014, the Task Force for Mass Critical Care (TFMCC) published a CHEST consensus statement on disaster preparedness principles in caring for the critically ill during disasters and pandemics (Christian et al. CHEST. 2014;146[4_suppl]:8s-34s). This publication attempted to guide preparedness for both single-event disasters and more prolonged events, including a feared influenza pandemic.
Despite the foundation of planning and support this guidance provided, the COVID-19 pandemic response revealed substantial gaps in our understanding and preparedness for these more prolonged and widespread events.
In New York City, as the first COVID-19 wave began in March and April of 2020, area hospitals responded with surge plans that prioritized what was felt to be most important (Griffin et al. Am J Respir Crit Care Med. 2020 Jun 1;201[11]:1337-44). Tiered, creative staffing structures were rapidly created with intensivists supervising non-ICU physicians and APPs. Procedure teams were created for intubation, proning, and central line placement. ICU space was created with adaptations to ORs and PACUs, and rooms on med-surg floors and step-down units underwent emergency renovations to allow creation of new “pop-up” ICUs. Triage protocols were altered: patients on high levels of supplemental oxygen, who would under normal circumstances have been admitted to an ICU, were triaged to floors and stepdown units. Equipment was reused, modified, and substituted creatively to optimize care for the maximum number of patients.
In the face of all of these struggles, many around the country and the world felt the efforts, though heroic, resulted in less than standard of care. Two subsequent publications validated this concern (Kadri et al. Ann Int Med. 2021,174;9:1240-51; Bravata DM et al. JAMA Open Network. 2021;4[1]:e2034266), demonstrating during severe surge, COVID-19 patients’ mortality increased significantly beyond that seen in non-surging or less-severe surging times, demonstrating a mortality effect of surge itself. Though these studies observed COVID-19 patients only, there is every reason to believe the findings applied to all critically ill patients cared for during these surges.
These experiences led the TFMCC to report updated strategies for remaining in contingency care levels and avoiding crisis care (Dichter JR et al. CHEST. 2022;161[2]:429-47). Contingency is equivalent to routine care though may require adaptations and employment of otherwise non-traditional resources. The ultimate goal of mass critical care in a public health emergency is to avoid crisis-operating conditions, crisis standards of care, and their associated challenging triage decisions regarding allocation of scarce resources.
The 10 suggestions included in the most recent TFMCC publication include staffing strategies and suggestions based on COVID-19 experiences for graded staff-to-patient ratios, and support processes to preserve the existing health care work force. Strategies also include reduction of redundant documentation, limiting overtime, and most importantly, approaches for improving teamwork and supporting psychological well-being and resilience. Examples include daily unit huddles to update care and share experiences, genuine intra-team recognition and appreciation, and embedding emotional health experts within teams to provide ongoing support.
Consistent communication between incident command and frontline clinicians was also a suggested priority, perhaps with a newly proposed position of physician clinical support supervisor. This would be a formal role within hospital incident command, a liaison between the two groups.
Surge strategies should include empowerment of bedside clinicians and leaders with both planning and real-time assessment of the clinical situation, as being at the front line of care enables the situational awareness to assess ICU strain most effectively. Further, ICU clinicians must recognize when progression deeper into contingency operations occurs and they become perilously close to crisis mode. At this point, decisions are made and scarce resources are modified beyond routine standards of care to preserve life. TFMCC designates this gray area between contingency and crisis as the Critical Clinical Prioritization level (Figure). 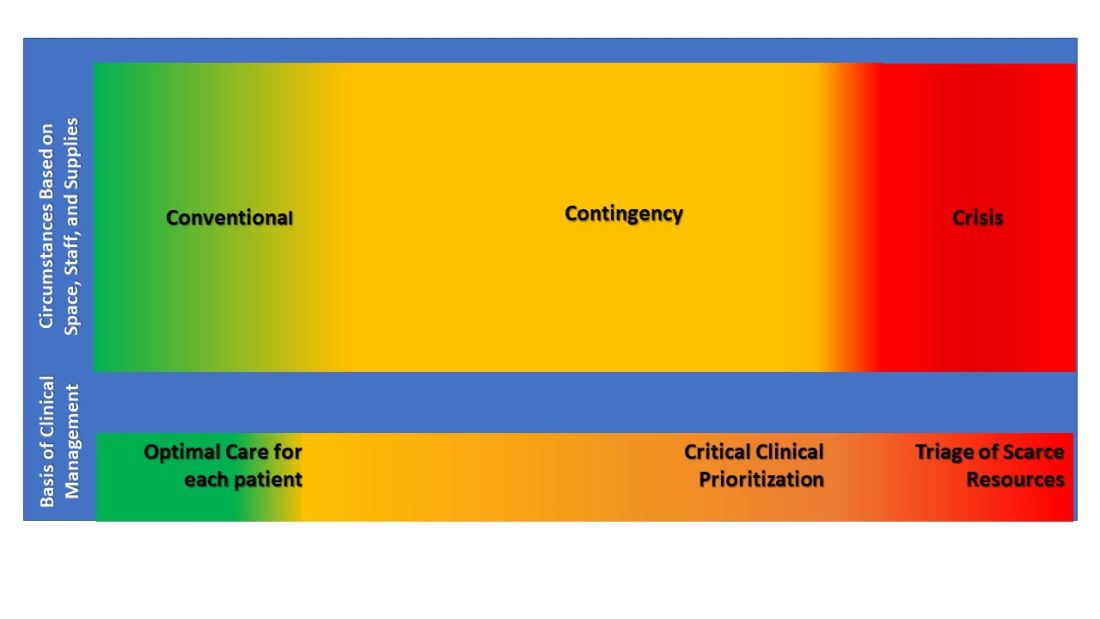
At this point, more resources must be provided, or patients must be transferred to other resourced hospitals.
Critical Clinical Prioritization is an illustration of necessity being the mother of invention, as these are adaptations clinicians devised under duress. Some particularly poignant examples are the spreading of 24 hours of continuous renal replacement therapy (CRRT) resource between two and sometimes three patients to provide life sustainment to all; and when ventilators were in short supply, determining which patients required full ICU ventilator support vs those who could manage with lower functioning ventilators, and trading them between patients when demands changed.
These adaptations can only be done by experienced clinicians proactively managing bedside critical care under duress, further underscoring the importance of our suggestion that Critical Clinical Prioritization and ICU strain be managed by bedside clinicians and leaders.
The response of early transfer of patients – load-balancing - should be considered as soon as any hospital enters contingency conditions. This strategy is commonly implemented within larger health systems, ideally before reaching Critical Clinical Prioritization. Formal, organized state or regional load-balancing coordination, now referred to as medical operations command centers (MOCCs), were highly effective and proved lifesaving for those states that implemented them (including Arizona, Washington, California, Minnesota, and others). Support for establishment of MOCC’s is crucial in prolonging contingency operations and further helps support and protect disadvantaged populations (White et al. N Engl J Med. 2021;385[24]:2211-4).
Establishment of MOCCs has met resistance due to challenges that include interhospital/intersystem competition, logistics of moving critically ill patients sometimes across significant physical distance, and the costs of assuming care of uninsured or underinsured patients. Nevertheless, the benefits to the population as a whole necessitate working through these obstacles as successful MOCCs have done, usually with government and hospital association support.
In their final suggestion of the 2022 updated strategies, TFMCC suggests that hospitals use telemedicine technology both to expand specialists’ ability to provide care and facilitate families virtually visiting their critically ill loved one when safety precludes in-person visits.
These suggestions are pivotal in planning for future public health emergencies that include mass critical care, even during events that are limited in scope and duration.
Lastly, intensivists struggled with legal and ethical concerns when mired in crisis care circumstances and decisions of allocation, and potential reallocation, of scarce resources. These issues were not well addressed during the COVID-19 pandemic, further emphasizing the importance of maintaining contingency level care and requiring further involvement from legal and medical ethics professionals for future planning.
The guiding principle of disaster preparedness is that we must do all the planning we can to ensure that we never need crisis standards of care (National Academies of Sciences, Engineering, and Medicine. 2020 Mar 28. Rapid Expert Consultation on Crisis Standards of Care for the COVID-19 Pandemic. Washington, DC: The National Academies Press.).
We must be prepared. Guidelines and suggestions laid out through decades of experience gained a real-world test in the COVID-19 pandemic. Now we must all reorganize and create new plans or augment old ones with the information we have gained. The time is now. The work must continue.
Dr. Griffin is Assistant Professor of Medicine, New York Presbyterian Hospital – Weill Cornell Medicine. Dr. Dichter is Associate Professor of Medicine, University of Minnesota.
Decreasing the burden of postacute sequelae of SARS-CoV-2 infection: What we know
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
On March 11, 2020, the World Health Organization (WHO) declared SARS-CoV-2 a pandemic. As of October 2021, there are over 240 million confirmed COVID-19 cases and over 4 million deaths globally, with the United States having the highest incidence of both cases and deaths (https://covid.cdc.gov/covid-data-tracker/#datatracker-home). As many as 87% of COVID-19 survivors experience persistent symptoms that last beyond the acute phase of illness (Carfi A, et al. JAMA. 2020;324[6]:603-5). In February 2021, the National Institutes of Health (NIH) called for a consensus term to describe this protracted form of COVID-19, and defined it as Post-acute Sequelae of SARS-CoV-2 infection (PASC) (https://www.nih.gov/about-nih/who-we-are/nih-director/statements/nih-launches-new-initiative-study-long-covid).
What are the PASC manifestations?
PASC has a heterogeneous presentation with a broad spectrum of manifestations and can vary from single to multiorgan system involvement. Commonly, PASC involves pulmonary abnormalities (shortness of breath, exercise intolerance, abnormal pulmonary functional test [PFT] and chest imaging), neurocognitive impairments (difficulty concentrating and memory loss), mental health disorders (anxiety, depression, and post-traumatic stress disorder), functional mobility impairments, as well as general and constitutional symptoms (fatigue and muscle weakness) (Groff D, et al. JAMA Netw Open. 2021;4[10]). The most prevalent pulmonary physiologic impairment is reduced diffusion capacity that has been shown to be associated with the severity of acute illness, while the most common radiologic abnormalities on chest CT scan are ground glass opacities. Some studies have shown a temporal improvement in pulmonary physiology and exercise capacity; however, persistent physiological and radiographic abnormalities persist in some patients up to 12 months after discharge (Wu X, et al. Lancet Respir Med. 2021;9:747-54). An abnormal or persistent hyper-inflammatory state, viral-induced autoimmune reaction, and ongoing viral activity have been proposed as possible biological mechanisms for PASC; however, the pathophysiology remains mostly unknown.
Who does PASC affect?
PASC affects patients irrespective of premorbid condition and severity of symptoms in the acute phase. It spans from those who had mild disease not requiring hospitalization to those who had critical illness requiring intensive care unit (ICU) management. COVID-19 ICU survivors seem to have an overlap of PASC and post-intensive care syndrome (PICS), defined by new or worsening physical, cognitive, and/or psychiatric impairments after critical illness. (Biehl M, et al. Cleve Clin J Med. 2020 Aug 5).
Who do we evaluate for PASC?
Given the complexity and chronicity of the associated symptoms and their impact on several major organ systems, a comprehensive and multidisciplinary approach is essential to assist with diagnosis and management of PASC. Listening empathically to patients and acknowledging their symptoms are key factors. Access to ambulatory care, establishment of rapport, effective collaboration and coordination of care among different disciplines, management of comorbidities, continuity of care, access to rehabilitation programs, and reduction of disease burden are some of the principles that guided the creation of dedicated COVID-19 clinics throughout the world. The most common services offered are primary care, pulmonology, cardiology, mental health, neurology, speech and language pathology, physical and occupational therapy, pharmacy, and case management. The involvement of specialties varies depending on the specific patient’s needs (Parker A, et al. The Lancet Respir Med. 2021;S2213-2600[21]00385-4).
The development of diagnostic and care pathways by different specialties ensures standardization of clinical assessment and management while allowing for individualized care. The commonly used tools to assess the respiratory system are the 6-minute walk test, PFT, chest imaging including radiographs and high-resolution CT scan, ventilation perfusion scan, and echocardiography. Some patients exhibit persistent cardiopulmonary symptoms with no evidence of organ injury. These patients have persistent exertional and functional limitation with normal PFT, resting echocardiography, and chest imaging. Cardiopulmonary exercise testing (CPET) and, more specifically, invasive CPET can be used to further investigate the decreased exercise capacity. CPET studies have identified an augmented exercise hyperventilation, and the causes of exercise limitation varied from anemia and reduced oxygen extraction by peripheral muscles to deconditioning, obesity, and lower ventilatory efficiency. A study looking at invasive CPET showed reduced peak exercise aerobic capacity in post COVID-19 patients compared with control participants and was associated with impaired systemic oxygen extraction and an exaggerated hyperventilatory response (Singh, et al. Chest. 2021;S0012-3692[21]03635). A subset of COVID-19 survivors presents with symptoms of autonomic dysfunction such as orthostatic intolerance and postural orthostatic tachycardia. These symptoms have been reported after other viral infections and could be secondary to gastrointestinal fluid loss, prolonged bed rest, and deconditioning of the cardiovascular system. More research is needed to characterize the dysautonomia in patients post–COVID-19.
What is the treatment?
Therapies depend on symptoms and organ involvement. The duration of pulmonary symptoms in long-haulers is not yet known, with cough and exercise intolerance/dyspnea ranking among the most common complaints in these patients. Exercise therapy plays an essential part in the rehabilitation of long-haulers and several studies are underway to assess different exercise and rehabilitation programs. For most patients with normal laboratory, physiologic, and imaging tests, post–COVID-19 clinics are offering physical therapy, occupational therapy, and neuropsychological rehabilitation. While steroids have been shown to improve mortality in hospitalized patients with COVID-19 requiring mechanical ventilation or supplemental oxygen, their role in outpatient COVID-19 infections and for post–COVID-19 lung disease/organizing pneumonia remains unclear. In a UK study of patients admitted to the hospital with COVID-19 disease of varying severity, interstitial abnormalities were noted in ~5% of patients at 6 weeks postdischarge and in 10.8% of patients with persistent respiratory symptoms (Myall, et al. Ann Am Thorac Soc. 2021;18[5]:799). The most common radiological findings (in > 50% of cases) were consistent with organizing pneumonia. Patients with persistent physiological abnormalities and interstitial findings improved with steroids. However, since the trajectory of the disease is unknown, further studies are required to understand the natural history of the disease and assess treatment strategies in patients with persistent inflammatory lung changes. Several studies looking at systemic or inhaled steroids in different phases of COVID-19 infection and varying disease severity are ongoing (ClinicalTrials.gov). Antifibrotics used to treat idiopathic pulmonary fibrosis and progressive fibrotic ILD are also being investigated in COVID-19 lung disease. The rationale for their use is to treat and prevent severe COVID-19 lung injury and prevent lung fibrosis.
The role of vaccinations
Whether patients who were infected with COVID-19, and, more specifically, patients with long-term symptoms post-COVID-19, should get vaccinated is actively being investigated. Vaccinations are protective at preventing infections and severe illness. Studies showed that patients who had COVID-19 infection and got vaccinated had a significantly higher antibody response than previously uninfected vaccine recipients. A review showed that the protective effect of prior SARS-CoV-2 infection on reinfection is high and similar to that of vaccination. However, a recent study of hospitalized patients revealed higher rates of COVID-19 among unvaccinated adults with previous infection compared with vaccinated adults (http://dx.doi.org/10.15585/mmwr.mm7044e1). On the other hand, the impact of vaccine on long-hauler symptoms has raised interest. A UK survey (not peer reviewed) on more than 800 long-haulers reported about 57% with overall improvement in their symptoms, 24% no change, and 19% with worsening symptoms after their first dose of vaccine, suggesting that the chances of experiencing an overall worsening of symptoms after vaccination is small, with more than half experiencing improvement (go.nature.com/3yfqem2). While awaiting longitudinal trials, the main argument to guide vaccination in long-haulers is that COVID-19 vaccinations provide protection from reinfection and appear to have the potential to improve symptoms.
The availability of a patient’s support system, peer support, and patient advocacy groups assist in providing equitable care and are critical in sustaining the recovery of COVID-19 survivors. Providing social, financial, and cultural support is imperative in decreasing the burden of COVID-19. The dedicated post–COVID-19 clinics will not only offer care to COVID-19 survivors, but will also help our understanding of the determinants and course of PASC, and will provide opportunities for research. Long-term longitudinal observational studies and clinical trials are critical to identify those at high risk for PASC, clarify the extent of health consequences attributable to COVID-19, and define best practices for COVID-19 survivors.
Dr. Biehl is Staff Physician, Pulmonary & Critical Care Medicine, Director, Post-ICU Recovery Clinic Respiratory Institute, Cleveland Clinic; Dr.Farha is with Respiratory and Lerner Institutes, Cleveland Clinic.
TTM2: Is there anything therapeutic about therapeutic hypothermia?
Animal and human models of the effects of therapeutic hypothermia, now called targeted temperature management (TTM), began to surface in the late 1980s. The first randomized clinical trial employing TTM as a neuroprotective strategy following cardiac arrest did not appear until the early 2000s. When compared with normothermia, the HACA trial (Holzer M, et al. N Engl J Med. 2002;346[8]:549-56) demonstrated a 14% reduction in mortality and improved neurologic outcomes following out of hospital cardiac arrest (OHCA) due to ventricular fibrillation (VF) or ventricular tachycardia (VT) when maintaining body temperature between 32˚C and 34˚C post-arrest. Following the results of this trial, TTM in comatose patients following cardiac arrest was recommended by international guidelines and became the standard of care. It was not until the publication of the TTM1 trial (Nielsen N, et al. N Engl J Med. 2013;369[23]:2197-206) about a decade later, that serious questions regarding the efficacy of TTM were raised. The TTM1 trial showed no difference in mortality or neurologic outcomes when comparing TTM at 33˚C vs 36˚C for OHCA. The results of this trial heralded widespread practice change, with many abandoning deep cooling, and often active cooling measures, in favor of fever avoidance. The HYPERION trial (Lascarrou J, et al. N Engl J Med. 2019;381:2327-37) came next, comparing TTM at 33˚C to normothermia (<37.5˚C) for cardiac arrest with non-hockable rhythm. This study did not identify any improvement in mortality with utilization of TTM but suggested it may be associated with more favorable neurologic outcomes, albeit in a small number of patients.
The TTM2 trial (Dankiewicz J, et al. N Engl J Med. 2021;384:2283-94) is the most recent trial to address the question of TTM post-cardiac arrest. The TTM2 trial was an international, randomized controlled superiority trial of TTM at 33˚C vs normothermia (≤37.8˚C) for patients with coma following OHCA with any initial rhythm. It was conducted by the same group as the TTM1 trial and, to date, represents the largest (N= 1,850) and most robust trial conducted in this area. The trial spanned 61 institutions across 14 countries and had nearly complete follow-up at 6 months. Once again, there was no significant difference in all-cause mortality at 6 months in the TTM group when compared with the normothermia group. Equally important, there were no differences observed in secondary outcomes, including functional neurologic status and health-related quality of life at 6 months. With the results of the TTM1 and TTM2 trials failing to show any neurologic or mortality benefit to TTM, we are left wondering, is there anything therapeutic about “therapeutic hypothermia”?
Both the 2020 American Heart Association (AHA) and 2021 European Resuscitation Council (ERC) guidelines predate this trial; they recommend cooling any OHCA or in-hospital cardiac arrest (IHCA) patient who remains unresponsive after return of spontaneous circulation (ROSC) regardless of initial rhythm. They further suggest maintaining a target temperature between 32˚C and 36˚C for at least 24 hours, followed by avoidance of fever (>37.7˚C) for at least 72 hours after ROSC in patients who remain comatose. While it will be interesting to see what future iterations of the guidelines recommend, the results from the TTM1 and TTM2 trials support a shift in clinical practice away from TTM and toward more active fever avoidance. Additionally, careful review of adverse events in the TTM2 trial suggests that induced hypothermia is not without risk of harm. When compared with the normothermia group in the TTM2 trial, the hypothermia group experienced higher rates of arrhythmias with hemodynamic instability (16% vs 24%), increased exposure to sedation, increased use of neuromuscular blockade, and increased duration of mechanical ventilation.
While the results of the TTM2 trial move the needle away from therapeutic hypothermia for OHCA patients, there is some nuance that warrants further discussion. First, the initial HACA trial, upon which the standard of TTM was based, included only patients with an initial shockable rhythm (VT/VF). Inherently, the etiology of these arrests is likely to be cardiac and more reversible in nature. Most subsequent landmark trials on TTM, including the TTM2 trial, have included OHCA patients with both shockable and nonshockable initial rhythms. Still, the majority of patients in the TTM2 trial had an initial shockable rhythm on presentation (72% hypothermia vs 75% normothermia). This may limit broad generalizability of study findings as an increasing number of OHCA patients are presenting with nonshockable initial rhythms. Next, it is well known that bystander CPR improves outcomes following OHCA. Impressively, over 75% of patients in both groups in the TTM2 trial received bystander CPR compared with an average of 46% of arrest patients in the US according to AHA data. Finally, like most of its predecessors, the TTM2 trial only included OHCA patients meaning no real conclusions can be drawn regarding application of TTM to IHCA patients. Of the major trials to date, only the HYPERION trial included IHCA patients – representing about 25% of the study population. Thus, the utility of TTM in the setting of IHCA remains largely unknown.
Taken in summation, recent trials, including TTM2, suggest that fever-avoidance post-cardiac arrest is likely the best option for improving mortality and neurologic outcomes while mitigating risk to the patient. We must remain vigilant in our enforcement of normothermia though as worse neurologic outcomes have been observed with hyperthermia in the early post-arrest period (Zeiner A, et al. Arch Intern Med. 2001;161[16]:2007-12). A key takeaway from recent trials is that maintaining normothermia without active temperature control measures is likely to be difficult to achieve. A criticism of the HYPERION trial was that a “substantial proportion” of patients in the normothermia group had temperatures above 38˚C. Similarly, 10% to15% of patients in the TTM2 trial had body temperatures above 37.7˚C, 40 to 72 hours after randomization and, ultimately, 46% of patients in the normothermia group required cooling with a temperature management device. Thus, we can conclude that maintenance of strict normothermia will likely continue to require active control with a temperature management device.
Despite an increasing number of well conducted studies in this area, there are several questions that remain unanswered. The first is whether cooling patients even earlier post-arrest is felt to increase the likelihood of survival with improved neurologic outcomes. Like HACA and HYPERION, the rate of cooling in the TTM2 trial was relatively quick with a time to randomization after onset of cardiac arrest of about 2 hours in both groups and a median time from intervention until reaching target temperature of 3 hours. While some retrospective data suggest ultra-early cooling may be beneficial, neither induction of therapeutic hypothermia during OHCA using a rapid infusion of cold saline (Bernard SA, et al. Circulation. 2016;134[11]:797-805) nor transnasal evaporative cooling in the pre-hospital setting (Nordeberg P, et al. JAMA. 2019;321(17):1677-85) has shown improvement in survival with good neurologic outcomes. Next, if we are going to continue TTM, the TTM2 trial does not provide guidance on optimal duration of cooling. Although the current guidelines are to cool for at least 24 hours after ROSC, it is unclear for how long strict temperature control should be continued. The currently enrolling ICECAP study aims to further elucidate the optimal duration of TTM for OHCA patients with both shockable and non-shockable initial rhythms.
Post-cardiac arrest management continues to be a significant area of interest in clinical research and for good reason. Although steady improvement has occurred with regards to survival and neurologic function for IHCA, of the approximately 350,000 nontraumatic OHCA that occur in a year in the United States, only about 10.2% of those patients will survive their initial hospitalization, and only about 8.2% of those who survive will have good functional status (American Heart Association. Circulation. 2020;142(suppl 2):S366-S468). There remains much room for continued study and improvement.
Dr. Capp is a Pulmonary and Critical Care Fellow; and Dr. Pendleton is Assistant Professor of Medicine; Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine; University of Minnesota, Minneapolis, Minnesota.
Animal and human models of the effects of therapeutic hypothermia, now called targeted temperature management (TTM), began to surface in the late 1980s. The first randomized clinical trial employing TTM as a neuroprotective strategy following cardiac arrest did not appear until the early 2000s. When compared with normothermia, the HACA trial (Holzer M, et al. N Engl J Med. 2002;346[8]:549-56) demonstrated a 14% reduction in mortality and improved neurologic outcomes following out of hospital cardiac arrest (OHCA) due to ventricular fibrillation (VF) or ventricular tachycardia (VT) when maintaining body temperature between 32˚C and 34˚C post-arrest. Following the results of this trial, TTM in comatose patients following cardiac arrest was recommended by international guidelines and became the standard of care. It was not until the publication of the TTM1 trial (Nielsen N, et al. N Engl J Med. 2013;369[23]:2197-206) about a decade later, that serious questions regarding the efficacy of TTM were raised. The TTM1 trial showed no difference in mortality or neurologic outcomes when comparing TTM at 33˚C vs 36˚C for OHCA. The results of this trial heralded widespread practice change, with many abandoning deep cooling, and often active cooling measures, in favor of fever avoidance. The HYPERION trial (Lascarrou J, et al. N Engl J Med. 2019;381:2327-37) came next, comparing TTM at 33˚C to normothermia (<37.5˚C) for cardiac arrest with non-hockable rhythm. This study did not identify any improvement in mortality with utilization of TTM but suggested it may be associated with more favorable neurologic outcomes, albeit in a small number of patients.
The TTM2 trial (Dankiewicz J, et al. N Engl J Med. 2021;384:2283-94) is the most recent trial to address the question of TTM post-cardiac arrest. The TTM2 trial was an international, randomized controlled superiority trial of TTM at 33˚C vs normothermia (≤37.8˚C) for patients with coma following OHCA with any initial rhythm. It was conducted by the same group as the TTM1 trial and, to date, represents the largest (N= 1,850) and most robust trial conducted in this area. The trial spanned 61 institutions across 14 countries and had nearly complete follow-up at 6 months. Once again, there was no significant difference in all-cause mortality at 6 months in the TTM group when compared with the normothermia group. Equally important, there were no differences observed in secondary outcomes, including functional neurologic status and health-related quality of life at 6 months. With the results of the TTM1 and TTM2 trials failing to show any neurologic or mortality benefit to TTM, we are left wondering, is there anything therapeutic about “therapeutic hypothermia”?
Both the 2020 American Heart Association (AHA) and 2021 European Resuscitation Council (ERC) guidelines predate this trial; they recommend cooling any OHCA or in-hospital cardiac arrest (IHCA) patient who remains unresponsive after return of spontaneous circulation (ROSC) regardless of initial rhythm. They further suggest maintaining a target temperature between 32˚C and 36˚C for at least 24 hours, followed by avoidance of fever (>37.7˚C) for at least 72 hours after ROSC in patients who remain comatose. While it will be interesting to see what future iterations of the guidelines recommend, the results from the TTM1 and TTM2 trials support a shift in clinical practice away from TTM and toward more active fever avoidance. Additionally, careful review of adverse events in the TTM2 trial suggests that induced hypothermia is not without risk of harm. When compared with the normothermia group in the TTM2 trial, the hypothermia group experienced higher rates of arrhythmias with hemodynamic instability (16% vs 24%), increased exposure to sedation, increased use of neuromuscular blockade, and increased duration of mechanical ventilation.
While the results of the TTM2 trial move the needle away from therapeutic hypothermia for OHCA patients, there is some nuance that warrants further discussion. First, the initial HACA trial, upon which the standard of TTM was based, included only patients with an initial shockable rhythm (VT/VF). Inherently, the etiology of these arrests is likely to be cardiac and more reversible in nature. Most subsequent landmark trials on TTM, including the TTM2 trial, have included OHCA patients with both shockable and nonshockable initial rhythms. Still, the majority of patients in the TTM2 trial had an initial shockable rhythm on presentation (72% hypothermia vs 75% normothermia). This may limit broad generalizability of study findings as an increasing number of OHCA patients are presenting with nonshockable initial rhythms. Next, it is well known that bystander CPR improves outcomes following OHCA. Impressively, over 75% of patients in both groups in the TTM2 trial received bystander CPR compared with an average of 46% of arrest patients in the US according to AHA data. Finally, like most of its predecessors, the TTM2 trial only included OHCA patients meaning no real conclusions can be drawn regarding application of TTM to IHCA patients. Of the major trials to date, only the HYPERION trial included IHCA patients – representing about 25% of the study population. Thus, the utility of TTM in the setting of IHCA remains largely unknown.
Taken in summation, recent trials, including TTM2, suggest that fever-avoidance post-cardiac arrest is likely the best option for improving mortality and neurologic outcomes while mitigating risk to the patient. We must remain vigilant in our enforcement of normothermia though as worse neurologic outcomes have been observed with hyperthermia in the early post-arrest period (Zeiner A, et al. Arch Intern Med. 2001;161[16]:2007-12). A key takeaway from recent trials is that maintaining normothermia without active temperature control measures is likely to be difficult to achieve. A criticism of the HYPERION trial was that a “substantial proportion” of patients in the normothermia group had temperatures above 38˚C. Similarly, 10% to15% of patients in the TTM2 trial had body temperatures above 37.7˚C, 40 to 72 hours after randomization and, ultimately, 46% of patients in the normothermia group required cooling with a temperature management device. Thus, we can conclude that maintenance of strict normothermia will likely continue to require active control with a temperature management device.
Despite an increasing number of well conducted studies in this area, there are several questions that remain unanswered. The first is whether cooling patients even earlier post-arrest is felt to increase the likelihood of survival with improved neurologic outcomes. Like HACA and HYPERION, the rate of cooling in the TTM2 trial was relatively quick with a time to randomization after onset of cardiac arrest of about 2 hours in both groups and a median time from intervention until reaching target temperature of 3 hours. While some retrospective data suggest ultra-early cooling may be beneficial, neither induction of therapeutic hypothermia during OHCA using a rapid infusion of cold saline (Bernard SA, et al. Circulation. 2016;134[11]:797-805) nor transnasal evaporative cooling in the pre-hospital setting (Nordeberg P, et al. JAMA. 2019;321(17):1677-85) has shown improvement in survival with good neurologic outcomes. Next, if we are going to continue TTM, the TTM2 trial does not provide guidance on optimal duration of cooling. Although the current guidelines are to cool for at least 24 hours after ROSC, it is unclear for how long strict temperature control should be continued. The currently enrolling ICECAP study aims to further elucidate the optimal duration of TTM for OHCA patients with both shockable and non-shockable initial rhythms.
Post-cardiac arrest management continues to be a significant area of interest in clinical research and for good reason. Although steady improvement has occurred with regards to survival and neurologic function for IHCA, of the approximately 350,000 nontraumatic OHCA that occur in a year in the United States, only about 10.2% of those patients will survive their initial hospitalization, and only about 8.2% of those who survive will have good functional status (American Heart Association. Circulation. 2020;142(suppl 2):S366-S468). There remains much room for continued study and improvement.
Dr. Capp is a Pulmonary and Critical Care Fellow; and Dr. Pendleton is Assistant Professor of Medicine; Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine; University of Minnesota, Minneapolis, Minnesota.
Animal and human models of the effects of therapeutic hypothermia, now called targeted temperature management (TTM), began to surface in the late 1980s. The first randomized clinical trial employing TTM as a neuroprotective strategy following cardiac arrest did not appear until the early 2000s. When compared with normothermia, the HACA trial (Holzer M, et al. N Engl J Med. 2002;346[8]:549-56) demonstrated a 14% reduction in mortality and improved neurologic outcomes following out of hospital cardiac arrest (OHCA) due to ventricular fibrillation (VF) or ventricular tachycardia (VT) when maintaining body temperature between 32˚C and 34˚C post-arrest. Following the results of this trial, TTM in comatose patients following cardiac arrest was recommended by international guidelines and became the standard of care. It was not until the publication of the TTM1 trial (Nielsen N, et al. N Engl J Med. 2013;369[23]:2197-206) about a decade later, that serious questions regarding the efficacy of TTM were raised. The TTM1 trial showed no difference in mortality or neurologic outcomes when comparing TTM at 33˚C vs 36˚C for OHCA. The results of this trial heralded widespread practice change, with many abandoning deep cooling, and often active cooling measures, in favor of fever avoidance. The HYPERION trial (Lascarrou J, et al. N Engl J Med. 2019;381:2327-37) came next, comparing TTM at 33˚C to normothermia (<37.5˚C) for cardiac arrest with non-hockable rhythm. This study did not identify any improvement in mortality with utilization of TTM but suggested it may be associated with more favorable neurologic outcomes, albeit in a small number of patients.
The TTM2 trial (Dankiewicz J, et al. N Engl J Med. 2021;384:2283-94) is the most recent trial to address the question of TTM post-cardiac arrest. The TTM2 trial was an international, randomized controlled superiority trial of TTM at 33˚C vs normothermia (≤37.8˚C) for patients with coma following OHCA with any initial rhythm. It was conducted by the same group as the TTM1 trial and, to date, represents the largest (N= 1,850) and most robust trial conducted in this area. The trial spanned 61 institutions across 14 countries and had nearly complete follow-up at 6 months. Once again, there was no significant difference in all-cause mortality at 6 months in the TTM group when compared with the normothermia group. Equally important, there were no differences observed in secondary outcomes, including functional neurologic status and health-related quality of life at 6 months. With the results of the TTM1 and TTM2 trials failing to show any neurologic or mortality benefit to TTM, we are left wondering, is there anything therapeutic about “therapeutic hypothermia”?
Both the 2020 American Heart Association (AHA) and 2021 European Resuscitation Council (ERC) guidelines predate this trial; they recommend cooling any OHCA or in-hospital cardiac arrest (IHCA) patient who remains unresponsive after return of spontaneous circulation (ROSC) regardless of initial rhythm. They further suggest maintaining a target temperature between 32˚C and 36˚C for at least 24 hours, followed by avoidance of fever (>37.7˚C) for at least 72 hours after ROSC in patients who remain comatose. While it will be interesting to see what future iterations of the guidelines recommend, the results from the TTM1 and TTM2 trials support a shift in clinical practice away from TTM and toward more active fever avoidance. Additionally, careful review of adverse events in the TTM2 trial suggests that induced hypothermia is not without risk of harm. When compared with the normothermia group in the TTM2 trial, the hypothermia group experienced higher rates of arrhythmias with hemodynamic instability (16% vs 24%), increased exposure to sedation, increased use of neuromuscular blockade, and increased duration of mechanical ventilation.
While the results of the TTM2 trial move the needle away from therapeutic hypothermia for OHCA patients, there is some nuance that warrants further discussion. First, the initial HACA trial, upon which the standard of TTM was based, included only patients with an initial shockable rhythm (VT/VF). Inherently, the etiology of these arrests is likely to be cardiac and more reversible in nature. Most subsequent landmark trials on TTM, including the TTM2 trial, have included OHCA patients with both shockable and nonshockable initial rhythms. Still, the majority of patients in the TTM2 trial had an initial shockable rhythm on presentation (72% hypothermia vs 75% normothermia). This may limit broad generalizability of study findings as an increasing number of OHCA patients are presenting with nonshockable initial rhythms. Next, it is well known that bystander CPR improves outcomes following OHCA. Impressively, over 75% of patients in both groups in the TTM2 trial received bystander CPR compared with an average of 46% of arrest patients in the US according to AHA data. Finally, like most of its predecessors, the TTM2 trial only included OHCA patients meaning no real conclusions can be drawn regarding application of TTM to IHCA patients. Of the major trials to date, only the HYPERION trial included IHCA patients – representing about 25% of the study population. Thus, the utility of TTM in the setting of IHCA remains largely unknown.
Taken in summation, recent trials, including TTM2, suggest that fever-avoidance post-cardiac arrest is likely the best option for improving mortality and neurologic outcomes while mitigating risk to the patient. We must remain vigilant in our enforcement of normothermia though as worse neurologic outcomes have been observed with hyperthermia in the early post-arrest period (Zeiner A, et al. Arch Intern Med. 2001;161[16]:2007-12). A key takeaway from recent trials is that maintaining normothermia without active temperature control measures is likely to be difficult to achieve. A criticism of the HYPERION trial was that a “substantial proportion” of patients in the normothermia group had temperatures above 38˚C. Similarly, 10% to15% of patients in the TTM2 trial had body temperatures above 37.7˚C, 40 to 72 hours after randomization and, ultimately, 46% of patients in the normothermia group required cooling with a temperature management device. Thus, we can conclude that maintenance of strict normothermia will likely continue to require active control with a temperature management device.
Despite an increasing number of well conducted studies in this area, there are several questions that remain unanswered. The first is whether cooling patients even earlier post-arrest is felt to increase the likelihood of survival with improved neurologic outcomes. Like HACA and HYPERION, the rate of cooling in the TTM2 trial was relatively quick with a time to randomization after onset of cardiac arrest of about 2 hours in both groups and a median time from intervention until reaching target temperature of 3 hours. While some retrospective data suggest ultra-early cooling may be beneficial, neither induction of therapeutic hypothermia during OHCA using a rapid infusion of cold saline (Bernard SA, et al. Circulation. 2016;134[11]:797-805) nor transnasal evaporative cooling in the pre-hospital setting (Nordeberg P, et al. JAMA. 2019;321(17):1677-85) has shown improvement in survival with good neurologic outcomes. Next, if we are going to continue TTM, the TTM2 trial does not provide guidance on optimal duration of cooling. Although the current guidelines are to cool for at least 24 hours after ROSC, it is unclear for how long strict temperature control should be continued. The currently enrolling ICECAP study aims to further elucidate the optimal duration of TTM for OHCA patients with both shockable and non-shockable initial rhythms.
Post-cardiac arrest management continues to be a significant area of interest in clinical research and for good reason. Although steady improvement has occurred with regards to survival and neurologic function for IHCA, of the approximately 350,000 nontraumatic OHCA that occur in a year in the United States, only about 10.2% of those patients will survive their initial hospitalization, and only about 8.2% of those who survive will have good functional status (American Heart Association. Circulation. 2020;142(suppl 2):S366-S468). There remains much room for continued study and improvement.
Dr. Capp is a Pulmonary and Critical Care Fellow; and Dr. Pendleton is Assistant Professor of Medicine; Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine; University of Minnesota, Minneapolis, Minnesota.
Delirium in the ICU: Best sedation practices lead to the best outcomes
Delirium is a frequent form of organ failure among the critically ill, impacting up to 80% of mechanically ventilated patients (Ely EW et al. JAMA. 2004;291[14]:1753-62). Its cardinal manifestations include disturbances in attention and cognition that occur acutely (e.g., hours to days) that are not better explained by another disease process (such as a toxidrome or dementia) (American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders. 5th ed., 2013). Duration of delirium in the intensive care unit (ICU) is independently associated with poor outcomes, such as mortality and hospital length of stay, even when accounting for comorbidities, coma duration, sedative use, and severity of illness. Delirium during critical illness is an important bellwether for a patient’s clinical status, often serving as a harbinger for severe or worsening disease.
Over the last two decades, the critical care community has come to understand the importance of recognizing delirium, which is often underdiagnosed, as well as delirium prevention. In the ICU, several factors coalesce to form the perfect environment for the development of delirium. Patients often have preexisting comorbidities that predispose to delirium, such as preexisting cognitive impairment, and the severity of critical illness increases the risk of delirium further. There are also bedside factors, however, that are important for the intensivist to address, many of which are modifiable. These include routinely screening for delirium and assessing level of consciousness, implementing early mobility and rehabilitation, targeting light sedation, and avoiding deliriogenic medications such as benzodiazepines. These evidence-based care practices form the foundation of the 2018 Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU (i.e., PADIS guidelines), which aim to reduce delirium and iatrogenesis from critical care (Devlin JW et al. Crit Care Med. 2018;46[9]:e825-e873). The severe acute respiratory syndrome–coronavirus 2 (SARS-CoV-2) pathogen that has caused the coronavirus disease 2019 (COVID-19) pandemic, however, has brought unprecedented challenges to critical care. One unfortunate side effect has been increased use of deep sedation and, thus, a greater incidence of delirium (Pun BT et al. Lancet Respir Med. 2021;9[3]:239-50). While the impact of the pandemic is unprecedented, thoughtful and careful sedation use remains vital to providing optimal care for the critically ill patient.
The link between sedation and delirium
The advent of modern mechanical ventilation brought critical care medicine into a period of rapid growth. Practices derived from the operating room, such as deep sedation and paralysis, became commonplace. Yet, starting in the late 1990s and early 2000s, evidence started growing regarding the impact of delirium and the unique aspects of the ICU that made it so prevalent. Delirium is strongly linked to inpatient mortality in mechanically ventilated adults, and it is best understood as an additional form of organ failure, much like other organ failures commonly recognized and treated by intensivists, such as respiratory or renal failure. Certain medications and sedation practices are associated with the development and duration of delirium. Benzodiazepines, a common sedative medication, are strongly linked to the development of delirium. In a study comparing commonly used sedative and analgesic agents, the use of lorazepam was associated with a greater risk of delirium the following day among critically ill, mechanically ventilated patients (Pandhariphande PP et al. Anesthesiology. 2006;104[1]:21-6). Given how commonly benzodiazepines are used and delirium develops in the ICU, this association has striking implications for clinical care and outcomes such as mortality. It is also significant, given that benzodiazepine use has increased during the pandemic, potentially creating significant downstream consequences. Benzodiazepines should be actively avoided when at all possible, given their propensity to lead to delirium, in accordance with the most recent guidelines.
Which sedation agent to choose?
While the negative effects of benzodiazepine-based sedation are well established, the optimal sedation agent remains unclear. Several other drugs are commonly used in the ICU, including propofol, dexmedetomidine, and opioid agents such as fentanyl and morphine. Propofol and dexmedetomidine are used specifically for their sedative properties, though they have dramatically different effects on the depth of sedation and different mechanisms of action. Opioid agents are most commonly used for their analgesic effect; however, in higher doses or combined with other medications, they have the secondary effect of inducing sedation. No particular sedation agent, however, beyond the avoidance of benzodiazepines has been recommended for use in the most recent guidelines. In the PRODEX and MIDEX studies, dexmedetomidine was noninferior to both midazolam and propofol in achieving targeted light to moderate sedation, and dexmedetomidine was associated with a shorter duration of mechanical ventilation compared to midazolam (Jakob SM et al. JAMA. 2012;307[11]:1151-60). More recently, the SPICE-III trial studied dexmedetomidine vs. usual care and found no difference in 90-day mortality (Shehabi Y et al. N Engl J Med. 2019;380[26]:2506-17).
In choosing the best sedation agent to avoid delirium, the largest and most applicable trial to date is the “Maximizing the Efficacy of Sedation and Reducing Neurological Dysfunction and Mortality in Septic Patients with Acute Respiratory Failure,” or MENDS2 trial (Hughes CG et al. N Engl J Med. 2021;384:1424-36). This study was a double-blind, multicenter randomized controlled trial of dexmedetomidine vs propofol in critically ill patients with sepsis receiving mechanical ventilation. The primary outcome was days alive without delirium or coma over the 14-day intervention period. The study enrolled 438 patients between 13 sites, with 422 patients receiving either dexmedetomidine or propofol. Hughes and colleagues found no difference in the primary outcome of days alive without delirium or coma between the dexmedetomidine and the propofol arms. The study also found no difference in secondary outcomes, including ventilator-free days, 90-day mortality, and 6-month global cognition, as well as no difference in safety endpoints. Importantly, there was excellent compliance with guideline-recommended practices of spontaneous awakening and breathing trials and early mobility, both of which are associated with reduced sedation exposure. The study did have some notable nuances, however. The overall doses of trial drugs were relatively low, and there was a moderate use of rescue sedation. There was also a small amount of crossover use of propofol and dexmedetomidine between treatment arms (10%), although the authors note that this was lower than in prior related studies. Overall, the MENDS2 study suggests there is likely clinical equipoise between propofol and dexmedetomidine in terms of delirium outcomes when combined with best practices, such targeted light sedation, paired awakening and breathing trials, and early mobility.
How should we manage sedation to prevent delirium?
Building off of the recent MENDS2 study and earlier work in the field, along with the 2018 PADIS guidelines, the general paradigm of sedation management should be focused on using light sedation with sedation interruptions to minimize overall sedation exposure. Based on the best available evidence to date, targeting less overall sedation leads to improved outcomes in critically ill patients, including mortality and duration of mechanical ventilation. Benzodiazepines should be avoided due to their association with delirium, but currently there is no evidence to suggest one nonbenzodiazepine sedative is better than another. Intensivists can feel comfortable choosing between agents based on a patient’s individual clinical needs, especially when patients are receiving paired spontaneous awakening and breathing trials and early rehabilitation. These same principles should be applied to sedation management and delirium patients in COVID-19 patients as well. While certain circumstances will necessitate deeper sedation at times (e.g., refractory hypoxemia due to ARDS from COVID-19), clinicians should continually reassess the actual sedation needs of the patient with the goal of reducing overall sedation. Focusing effort on these evidence-based practices will help reduce the incidence of delirium and ultimately improve patient outcomes.
Dr. Mart is with the Division of Allergy, Pulmonary, and Critical Care Medicine, Vanderbilt University Medical Center; Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center; and VA Tennessee Valley Healthcare System Geriatric Research Education and Clinical Center (GRECC), Nashville, Tennessee.
Delirium is a frequent form of organ failure among the critically ill, impacting up to 80% of mechanically ventilated patients (Ely EW et al. JAMA. 2004;291[14]:1753-62). Its cardinal manifestations include disturbances in attention and cognition that occur acutely (e.g., hours to days) that are not better explained by another disease process (such as a toxidrome or dementia) (American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders. 5th ed., 2013). Duration of delirium in the intensive care unit (ICU) is independently associated with poor outcomes, such as mortality and hospital length of stay, even when accounting for comorbidities, coma duration, sedative use, and severity of illness. Delirium during critical illness is an important bellwether for a patient’s clinical status, often serving as a harbinger for severe or worsening disease.
Over the last two decades, the critical care community has come to understand the importance of recognizing delirium, which is often underdiagnosed, as well as delirium prevention. In the ICU, several factors coalesce to form the perfect environment for the development of delirium. Patients often have preexisting comorbidities that predispose to delirium, such as preexisting cognitive impairment, and the severity of critical illness increases the risk of delirium further. There are also bedside factors, however, that are important for the intensivist to address, many of which are modifiable. These include routinely screening for delirium and assessing level of consciousness, implementing early mobility and rehabilitation, targeting light sedation, and avoiding deliriogenic medications such as benzodiazepines. These evidence-based care practices form the foundation of the 2018 Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU (i.e., PADIS guidelines), which aim to reduce delirium and iatrogenesis from critical care (Devlin JW et al. Crit Care Med. 2018;46[9]:e825-e873). The severe acute respiratory syndrome–coronavirus 2 (SARS-CoV-2) pathogen that has caused the coronavirus disease 2019 (COVID-19) pandemic, however, has brought unprecedented challenges to critical care. One unfortunate side effect has been increased use of deep sedation and, thus, a greater incidence of delirium (Pun BT et al. Lancet Respir Med. 2021;9[3]:239-50). While the impact of the pandemic is unprecedented, thoughtful and careful sedation use remains vital to providing optimal care for the critically ill patient.
The link between sedation and delirium
The advent of modern mechanical ventilation brought critical care medicine into a period of rapid growth. Practices derived from the operating room, such as deep sedation and paralysis, became commonplace. Yet, starting in the late 1990s and early 2000s, evidence started growing regarding the impact of delirium and the unique aspects of the ICU that made it so prevalent. Delirium is strongly linked to inpatient mortality in mechanically ventilated adults, and it is best understood as an additional form of organ failure, much like other organ failures commonly recognized and treated by intensivists, such as respiratory or renal failure. Certain medications and sedation practices are associated with the development and duration of delirium. Benzodiazepines, a common sedative medication, are strongly linked to the development of delirium. In a study comparing commonly used sedative and analgesic agents, the use of lorazepam was associated with a greater risk of delirium the following day among critically ill, mechanically ventilated patients (Pandhariphande PP et al. Anesthesiology. 2006;104[1]:21-6). Given how commonly benzodiazepines are used and delirium develops in the ICU, this association has striking implications for clinical care and outcomes such as mortality. It is also significant, given that benzodiazepine use has increased during the pandemic, potentially creating significant downstream consequences. Benzodiazepines should be actively avoided when at all possible, given their propensity to lead to delirium, in accordance with the most recent guidelines.
Which sedation agent to choose?
While the negative effects of benzodiazepine-based sedation are well established, the optimal sedation agent remains unclear. Several other drugs are commonly used in the ICU, including propofol, dexmedetomidine, and opioid agents such as fentanyl and morphine. Propofol and dexmedetomidine are used specifically for their sedative properties, though they have dramatically different effects on the depth of sedation and different mechanisms of action. Opioid agents are most commonly used for their analgesic effect; however, in higher doses or combined with other medications, they have the secondary effect of inducing sedation. No particular sedation agent, however, beyond the avoidance of benzodiazepines has been recommended for use in the most recent guidelines. In the PRODEX and MIDEX studies, dexmedetomidine was noninferior to both midazolam and propofol in achieving targeted light to moderate sedation, and dexmedetomidine was associated with a shorter duration of mechanical ventilation compared to midazolam (Jakob SM et al. JAMA. 2012;307[11]:1151-60). More recently, the SPICE-III trial studied dexmedetomidine vs. usual care and found no difference in 90-day mortality (Shehabi Y et al. N Engl J Med. 2019;380[26]:2506-17).
In choosing the best sedation agent to avoid delirium, the largest and most applicable trial to date is the “Maximizing the Efficacy of Sedation and Reducing Neurological Dysfunction and Mortality in Septic Patients with Acute Respiratory Failure,” or MENDS2 trial (Hughes CG et al. N Engl J Med. 2021;384:1424-36). This study was a double-blind, multicenter randomized controlled trial of dexmedetomidine vs propofol in critically ill patients with sepsis receiving mechanical ventilation. The primary outcome was days alive without delirium or coma over the 14-day intervention period. The study enrolled 438 patients between 13 sites, with 422 patients receiving either dexmedetomidine or propofol. Hughes and colleagues found no difference in the primary outcome of days alive without delirium or coma between the dexmedetomidine and the propofol arms. The study also found no difference in secondary outcomes, including ventilator-free days, 90-day mortality, and 6-month global cognition, as well as no difference in safety endpoints. Importantly, there was excellent compliance with guideline-recommended practices of spontaneous awakening and breathing trials and early mobility, both of which are associated with reduced sedation exposure. The study did have some notable nuances, however. The overall doses of trial drugs were relatively low, and there was a moderate use of rescue sedation. There was also a small amount of crossover use of propofol and dexmedetomidine between treatment arms (10%), although the authors note that this was lower than in prior related studies. Overall, the MENDS2 study suggests there is likely clinical equipoise between propofol and dexmedetomidine in terms of delirium outcomes when combined with best practices, such targeted light sedation, paired awakening and breathing trials, and early mobility.
How should we manage sedation to prevent delirium?
Building off of the recent MENDS2 study and earlier work in the field, along with the 2018 PADIS guidelines, the general paradigm of sedation management should be focused on using light sedation with sedation interruptions to minimize overall sedation exposure. Based on the best available evidence to date, targeting less overall sedation leads to improved outcomes in critically ill patients, including mortality and duration of mechanical ventilation. Benzodiazepines should be avoided due to their association with delirium, but currently there is no evidence to suggest one nonbenzodiazepine sedative is better than another. Intensivists can feel comfortable choosing between agents based on a patient’s individual clinical needs, especially when patients are receiving paired spontaneous awakening and breathing trials and early rehabilitation. These same principles should be applied to sedation management and delirium patients in COVID-19 patients as well. While certain circumstances will necessitate deeper sedation at times (e.g., refractory hypoxemia due to ARDS from COVID-19), clinicians should continually reassess the actual sedation needs of the patient with the goal of reducing overall sedation. Focusing effort on these evidence-based practices will help reduce the incidence of delirium and ultimately improve patient outcomes.
Dr. Mart is with the Division of Allergy, Pulmonary, and Critical Care Medicine, Vanderbilt University Medical Center; Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center; and VA Tennessee Valley Healthcare System Geriatric Research Education and Clinical Center (GRECC), Nashville, Tennessee.
Delirium is a frequent form of organ failure among the critically ill, impacting up to 80% of mechanically ventilated patients (Ely EW et al. JAMA. 2004;291[14]:1753-62). Its cardinal manifestations include disturbances in attention and cognition that occur acutely (e.g., hours to days) that are not better explained by another disease process (such as a toxidrome or dementia) (American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders. 5th ed., 2013). Duration of delirium in the intensive care unit (ICU) is independently associated with poor outcomes, such as mortality and hospital length of stay, even when accounting for comorbidities, coma duration, sedative use, and severity of illness. Delirium during critical illness is an important bellwether for a patient’s clinical status, often serving as a harbinger for severe or worsening disease.
Over the last two decades, the critical care community has come to understand the importance of recognizing delirium, which is often underdiagnosed, as well as delirium prevention. In the ICU, several factors coalesce to form the perfect environment for the development of delirium. Patients often have preexisting comorbidities that predispose to delirium, such as preexisting cognitive impairment, and the severity of critical illness increases the risk of delirium further. There are also bedside factors, however, that are important for the intensivist to address, many of which are modifiable. These include routinely screening for delirium and assessing level of consciousness, implementing early mobility and rehabilitation, targeting light sedation, and avoiding deliriogenic medications such as benzodiazepines. These evidence-based care practices form the foundation of the 2018 Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU (i.e., PADIS guidelines), which aim to reduce delirium and iatrogenesis from critical care (Devlin JW et al. Crit Care Med. 2018;46[9]:e825-e873). The severe acute respiratory syndrome–coronavirus 2 (SARS-CoV-2) pathogen that has caused the coronavirus disease 2019 (COVID-19) pandemic, however, has brought unprecedented challenges to critical care. One unfortunate side effect has been increased use of deep sedation and, thus, a greater incidence of delirium (Pun BT et al. Lancet Respir Med. 2021;9[3]:239-50). While the impact of the pandemic is unprecedented, thoughtful and careful sedation use remains vital to providing optimal care for the critically ill patient.
The link between sedation and delirium
The advent of modern mechanical ventilation brought critical care medicine into a period of rapid growth. Practices derived from the operating room, such as deep sedation and paralysis, became commonplace. Yet, starting in the late 1990s and early 2000s, evidence started growing regarding the impact of delirium and the unique aspects of the ICU that made it so prevalent. Delirium is strongly linked to inpatient mortality in mechanically ventilated adults, and it is best understood as an additional form of organ failure, much like other organ failures commonly recognized and treated by intensivists, such as respiratory or renal failure. Certain medications and sedation practices are associated with the development and duration of delirium. Benzodiazepines, a common sedative medication, are strongly linked to the development of delirium. In a study comparing commonly used sedative and analgesic agents, the use of lorazepam was associated with a greater risk of delirium the following day among critically ill, mechanically ventilated patients (Pandhariphande PP et al. Anesthesiology. 2006;104[1]:21-6). Given how commonly benzodiazepines are used and delirium develops in the ICU, this association has striking implications for clinical care and outcomes such as mortality. It is also significant, given that benzodiazepine use has increased during the pandemic, potentially creating significant downstream consequences. Benzodiazepines should be actively avoided when at all possible, given their propensity to lead to delirium, in accordance with the most recent guidelines.
Which sedation agent to choose?
While the negative effects of benzodiazepine-based sedation are well established, the optimal sedation agent remains unclear. Several other drugs are commonly used in the ICU, including propofol, dexmedetomidine, and opioid agents such as fentanyl and morphine. Propofol and dexmedetomidine are used specifically for their sedative properties, though they have dramatically different effects on the depth of sedation and different mechanisms of action. Opioid agents are most commonly used for their analgesic effect; however, in higher doses or combined with other medications, they have the secondary effect of inducing sedation. No particular sedation agent, however, beyond the avoidance of benzodiazepines has been recommended for use in the most recent guidelines. In the PRODEX and MIDEX studies, dexmedetomidine was noninferior to both midazolam and propofol in achieving targeted light to moderate sedation, and dexmedetomidine was associated with a shorter duration of mechanical ventilation compared to midazolam (Jakob SM et al. JAMA. 2012;307[11]:1151-60). More recently, the SPICE-III trial studied dexmedetomidine vs. usual care and found no difference in 90-day mortality (Shehabi Y et al. N Engl J Med. 2019;380[26]:2506-17).
In choosing the best sedation agent to avoid delirium, the largest and most applicable trial to date is the “Maximizing the Efficacy of Sedation and Reducing Neurological Dysfunction and Mortality in Septic Patients with Acute Respiratory Failure,” or MENDS2 trial (Hughes CG et al. N Engl J Med. 2021;384:1424-36). This study was a double-blind, multicenter randomized controlled trial of dexmedetomidine vs propofol in critically ill patients with sepsis receiving mechanical ventilation. The primary outcome was days alive without delirium or coma over the 14-day intervention period. The study enrolled 438 patients between 13 sites, with 422 patients receiving either dexmedetomidine or propofol. Hughes and colleagues found no difference in the primary outcome of days alive without delirium or coma between the dexmedetomidine and the propofol arms. The study also found no difference in secondary outcomes, including ventilator-free days, 90-day mortality, and 6-month global cognition, as well as no difference in safety endpoints. Importantly, there was excellent compliance with guideline-recommended practices of spontaneous awakening and breathing trials and early mobility, both of which are associated with reduced sedation exposure. The study did have some notable nuances, however. The overall doses of trial drugs were relatively low, and there was a moderate use of rescue sedation. There was also a small amount of crossover use of propofol and dexmedetomidine between treatment arms (10%), although the authors note that this was lower than in prior related studies. Overall, the MENDS2 study suggests there is likely clinical equipoise between propofol and dexmedetomidine in terms of delirium outcomes when combined with best practices, such targeted light sedation, paired awakening and breathing trials, and early mobility.
How should we manage sedation to prevent delirium?
Building off of the recent MENDS2 study and earlier work in the field, along with the 2018 PADIS guidelines, the general paradigm of sedation management should be focused on using light sedation with sedation interruptions to minimize overall sedation exposure. Based on the best available evidence to date, targeting less overall sedation leads to improved outcomes in critically ill patients, including mortality and duration of mechanical ventilation. Benzodiazepines should be avoided due to their association with delirium, but currently there is no evidence to suggest one nonbenzodiazepine sedative is better than another. Intensivists can feel comfortable choosing between agents based on a patient’s individual clinical needs, especially when patients are receiving paired spontaneous awakening and breathing trials and early rehabilitation. These same principles should be applied to sedation management and delirium patients in COVID-19 patients as well. While certain circumstances will necessitate deeper sedation at times (e.g., refractory hypoxemia due to ARDS from COVID-19), clinicians should continually reassess the actual sedation needs of the patient with the goal of reducing overall sedation. Focusing effort on these evidence-based practices will help reduce the incidence of delirium and ultimately improve patient outcomes.
Dr. Mart is with the Division of Allergy, Pulmonary, and Critical Care Medicine, Vanderbilt University Medical Center; Critical Illness, Brain Dysfunction, and Survivorship (CIBS) Center; and VA Tennessee Valley Healthcare System Geriatric Research Education and Clinical Center (GRECC), Nashville, Tennessee.
Reclaiming patient-centered care from the grip of COVID-19
Over a year has passed since the first case of COVID-19 was reported in the United States, with over 114 million cases now reported worldwide, and over 2.5 million deaths at the time of this writing (Dong E, et al. Lancet Infect Dis. doi: 10.1016/S1473-3099[20]30120-1). While our vaccination efforts here in the United States have provided a much-needed glimmer of hope, it has been bittersweet, as we recently surpassed the grim milestone of 500,000 COVID-19-related deaths.
The infectious nature of SARS-CoV-2, coupled with the lack of adequate PPE early in the pandemic, led to radical changes in most hospital visitor policies. Rather than welcoming families into the care setting as we have been accustomed, we were forced to restrict access. While well-intentioned, the impact of this on patients, their families – and as we later learned, ourselves – has been devastating. Patients found themselves alone in an unfamiliar environment, infected with a disease there was no effective treatment for, hearing dismal news regarding inpatient and ICU mortality rates on news networks, and families could not see for themselves how their loved ones were progressing in their hospital course.
The impact on patient-centered care
The impact of this pandemic on patients and health care providers alike cannot be overstated. Arguably, one of the greatest challenges created by COVID-19 has been its direct assault on the core values of patient-centered care that we have spent decades striving to promote and embody.
Since its identification as a quality gap by the Institute of Medicine in 2001, the definition of patient-centered care has been tweaked over the past 20 years (Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001). Most frameworks include the active participation of patients and their families as part of the health care team, encouraging and facilitating the presence of family members in the care setting, and focusing on patients’ physical comfort and emotional well-being as fundamental tenets of patient centeredness (NEJM Catalyst: What is Patient-Centered Care? Explore the definition, benefits, and examples of patient-centered care. How does patient-centered care translate to new delivery models? January 1,2017).
Families, the “F” in the ABCDEF Bundle, have been recognized as an integral part of care in the ICU setting (Ely EW. Crit Care Med. 2017;45[2]:321). While engagement of family members began with our recognition of their role in emotionally supporting patients and efforts to improve communication, we have also seen the impact of family participation on reducing ICU delirium through frequent re-orientation and encouragement of early mobility (McKenzie J, et al. Australas J Ageing. 2020;39:21). In fact, a recent study has suggested that family members could play an even more active role in detecting and assessing ICU delirium using objective assessment tools (Fiest K, et al. Crit Care Med. 2020;48[7]:954). Post-ICU PTSD has been well described in both ICU survivors as well as in their family members, with evidence that family participation in care of patients during their ICU stay leads to its reduction (Amass TH, et al. Crit Care Med. 2020[Feb];48[2]:176).
The emotional toll
Comforting patients and families in times of distress and suffering is something that comes naturally to many in critical care, and our training further improves our ability to do this effectively. No amount of training, however, could have prepared us for the degree and volume of suffering we bore witness to this past year and the resulting moral injury many are still dealing with. We were present for families’ most intimate moments, holding phones and tablets up to patients so their families could say their goodbyes, listening to the “I love yous,” “I’ll miss yous,” “I’m sorrys,” and “Please don’t gos.” Nurses held patients’ hands as they took their last breaths so they wouldn’t die alone and worked to move husbands and wives into the same room so they could be together in their final moments. Entrenched in each of our identities is the role of healer, and we found ourselves questioning our effectiveness in rising to meet suffering on a scale we had never seen before. Little did we understand that while our paradigms were reinforcing the benefits of patient-centered care for patients and their families, that framework was also serving to facilitate our role as healers – that without it, we all suffer.
Rising to the challenge
These unprecedented circumstances led to creative efforts to bridge some of these barriers. Health systems created photo lanyards that providers wore over their PPE so patients could identify their health care team and connect with them on a more human level. Video conferencing technology was brought to the patient bedside using smartphones and tablets to assist them in communicating with their families. Doctors and nurses coordinated multiple calls throughout the day to ensure families felt included in the care plans and were always abreast of any new developments.
All these initiatives were our way of attempting to alleviate some of the suffering we were witnessing, and in some ways felt complicit in. It is in hindsight that we can look back and question if we could have done things differently. We treated family as visitors, when in fact, they are fundamental members of the care team who play an active and critical role in patient care. This was, in part, driven by national unpreparedness when it came to PPE supplies, in addition to misinformation and inconsistent messaging early in the pandemic with regards to the mechanism of transmission of disease from various health organizations. While we did our best given the circumstances, we must not allow this experience to lead us away from the tenets we know to be essential to patient, family, and health care provider well-being.
All in health care met the call to action – nurses, physicians, advanced practice providers, respiratory therapists, nutritionists, pharmacists, physical therapists, patient transporters, environmental service workers, and all others who kept our hospitals and patient care facilities open through this pandemic and embarked on what amounted to a collective, global, ongoing “code-blue alert,” resuscitating patient after patient, hotspot after hotspot, region after region, and country after country. We expanded hospital bed capacities, created ICU beds where there were none, developed novel process protocols, and learned in real time what seemed to help (or not) in treating this novel disease, all while participating in incredible international scientific collaboration and information sharing that has contributed in getting the collective “us” through this first year of the pandemic. We did what we were trained and called to do.
Preparing for the future
There will inevitably be another public health crisis, and we must advocate for better preparedness next time, insisting on overall stronger public health systems and pandemic preparedness. We must address our PPE stores and supply chains. We must have disaster preparedness plans that go beyond the scope of mass casualty events and bioterrorism. Beyond physical recovery, we must tend to the factors that impact patients’ long-term recovery, with attention to emotional and psychological well-being. We must advocate for all of this now, while the memories are fresh and before the impact of this collective suffering begins to fade. It can never again be acceptable to exclude families from the health care setting. We must advocate for our patients and for the resources, systems, processes, and support that will allow us to do better.
Dr. Hegab is Associate Director, Pulmonary Hypertension Program, Medical Director, Pulmonary Embolism Response Team, Division of Pulmonary and Critical Care Medicine, Henry Ford Hospital; and Assistant Professor, Wayne State University School of Medicine, Detroit.
Over a year has passed since the first case of COVID-19 was reported in the United States, with over 114 million cases now reported worldwide, and over 2.5 million deaths at the time of this writing (Dong E, et al. Lancet Infect Dis. doi: 10.1016/S1473-3099[20]30120-1). While our vaccination efforts here in the United States have provided a much-needed glimmer of hope, it has been bittersweet, as we recently surpassed the grim milestone of 500,000 COVID-19-related deaths.
The infectious nature of SARS-CoV-2, coupled with the lack of adequate PPE early in the pandemic, led to radical changes in most hospital visitor policies. Rather than welcoming families into the care setting as we have been accustomed, we were forced to restrict access. While well-intentioned, the impact of this on patients, their families – and as we later learned, ourselves – has been devastating. Patients found themselves alone in an unfamiliar environment, infected with a disease there was no effective treatment for, hearing dismal news regarding inpatient and ICU mortality rates on news networks, and families could not see for themselves how their loved ones were progressing in their hospital course.
The impact on patient-centered care
The impact of this pandemic on patients and health care providers alike cannot be overstated. Arguably, one of the greatest challenges created by COVID-19 has been its direct assault on the core values of patient-centered care that we have spent decades striving to promote and embody.
Since its identification as a quality gap by the Institute of Medicine in 2001, the definition of patient-centered care has been tweaked over the past 20 years (Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001). Most frameworks include the active participation of patients and their families as part of the health care team, encouraging and facilitating the presence of family members in the care setting, and focusing on patients’ physical comfort and emotional well-being as fundamental tenets of patient centeredness (NEJM Catalyst: What is Patient-Centered Care? Explore the definition, benefits, and examples of patient-centered care. How does patient-centered care translate to new delivery models? January 1,2017).
Families, the “F” in the ABCDEF Bundle, have been recognized as an integral part of care in the ICU setting (Ely EW. Crit Care Med. 2017;45[2]:321). While engagement of family members began with our recognition of their role in emotionally supporting patients and efforts to improve communication, we have also seen the impact of family participation on reducing ICU delirium through frequent re-orientation and encouragement of early mobility (McKenzie J, et al. Australas J Ageing. 2020;39:21). In fact, a recent study has suggested that family members could play an even more active role in detecting and assessing ICU delirium using objective assessment tools (Fiest K, et al. Crit Care Med. 2020;48[7]:954). Post-ICU PTSD has been well described in both ICU survivors as well as in their family members, with evidence that family participation in care of patients during their ICU stay leads to its reduction (Amass TH, et al. Crit Care Med. 2020[Feb];48[2]:176).
The emotional toll
Comforting patients and families in times of distress and suffering is something that comes naturally to many in critical care, and our training further improves our ability to do this effectively. No amount of training, however, could have prepared us for the degree and volume of suffering we bore witness to this past year and the resulting moral injury many are still dealing with. We were present for families’ most intimate moments, holding phones and tablets up to patients so their families could say their goodbyes, listening to the “I love yous,” “I’ll miss yous,” “I’m sorrys,” and “Please don’t gos.” Nurses held patients’ hands as they took their last breaths so they wouldn’t die alone and worked to move husbands and wives into the same room so they could be together in their final moments. Entrenched in each of our identities is the role of healer, and we found ourselves questioning our effectiveness in rising to meet suffering on a scale we had never seen before. Little did we understand that while our paradigms were reinforcing the benefits of patient-centered care for patients and their families, that framework was also serving to facilitate our role as healers – that without it, we all suffer.
Rising to the challenge
These unprecedented circumstances led to creative efforts to bridge some of these barriers. Health systems created photo lanyards that providers wore over their PPE so patients could identify their health care team and connect with them on a more human level. Video conferencing technology was brought to the patient bedside using smartphones and tablets to assist them in communicating with their families. Doctors and nurses coordinated multiple calls throughout the day to ensure families felt included in the care plans and were always abreast of any new developments.
All these initiatives were our way of attempting to alleviate some of the suffering we were witnessing, and in some ways felt complicit in. It is in hindsight that we can look back and question if we could have done things differently. We treated family as visitors, when in fact, they are fundamental members of the care team who play an active and critical role in patient care. This was, in part, driven by national unpreparedness when it came to PPE supplies, in addition to misinformation and inconsistent messaging early in the pandemic with regards to the mechanism of transmission of disease from various health organizations. While we did our best given the circumstances, we must not allow this experience to lead us away from the tenets we know to be essential to patient, family, and health care provider well-being.
All in health care met the call to action – nurses, physicians, advanced practice providers, respiratory therapists, nutritionists, pharmacists, physical therapists, patient transporters, environmental service workers, and all others who kept our hospitals and patient care facilities open through this pandemic and embarked on what amounted to a collective, global, ongoing “code-blue alert,” resuscitating patient after patient, hotspot after hotspot, region after region, and country after country. We expanded hospital bed capacities, created ICU beds where there were none, developed novel process protocols, and learned in real time what seemed to help (or not) in treating this novel disease, all while participating in incredible international scientific collaboration and information sharing that has contributed in getting the collective “us” through this first year of the pandemic. We did what we were trained and called to do.
Preparing for the future
There will inevitably be another public health crisis, and we must advocate for better preparedness next time, insisting on overall stronger public health systems and pandemic preparedness. We must address our PPE stores and supply chains. We must have disaster preparedness plans that go beyond the scope of mass casualty events and bioterrorism. Beyond physical recovery, we must tend to the factors that impact patients’ long-term recovery, with attention to emotional and psychological well-being. We must advocate for all of this now, while the memories are fresh and before the impact of this collective suffering begins to fade. It can never again be acceptable to exclude families from the health care setting. We must advocate for our patients and for the resources, systems, processes, and support that will allow us to do better.
Dr. Hegab is Associate Director, Pulmonary Hypertension Program, Medical Director, Pulmonary Embolism Response Team, Division of Pulmonary and Critical Care Medicine, Henry Ford Hospital; and Assistant Professor, Wayne State University School of Medicine, Detroit.
Over a year has passed since the first case of COVID-19 was reported in the United States, with over 114 million cases now reported worldwide, and over 2.5 million deaths at the time of this writing (Dong E, et al. Lancet Infect Dis. doi: 10.1016/S1473-3099[20]30120-1). While our vaccination efforts here in the United States have provided a much-needed glimmer of hope, it has been bittersweet, as we recently surpassed the grim milestone of 500,000 COVID-19-related deaths.
The infectious nature of SARS-CoV-2, coupled with the lack of adequate PPE early in the pandemic, led to radical changes in most hospital visitor policies. Rather than welcoming families into the care setting as we have been accustomed, we were forced to restrict access. While well-intentioned, the impact of this on patients, their families – and as we later learned, ourselves – has been devastating. Patients found themselves alone in an unfamiliar environment, infected with a disease there was no effective treatment for, hearing dismal news regarding inpatient and ICU mortality rates on news networks, and families could not see for themselves how their loved ones were progressing in their hospital course.
The impact on patient-centered care
The impact of this pandemic on patients and health care providers alike cannot be overstated. Arguably, one of the greatest challenges created by COVID-19 has been its direct assault on the core values of patient-centered care that we have spent decades striving to promote and embody.
Since its identification as a quality gap by the Institute of Medicine in 2001, the definition of patient-centered care has been tweaked over the past 20 years (Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001). Most frameworks include the active participation of patients and their families as part of the health care team, encouraging and facilitating the presence of family members in the care setting, and focusing on patients’ physical comfort and emotional well-being as fundamental tenets of patient centeredness (NEJM Catalyst: What is Patient-Centered Care? Explore the definition, benefits, and examples of patient-centered care. How does patient-centered care translate to new delivery models? January 1,2017).
Families, the “F” in the ABCDEF Bundle, have been recognized as an integral part of care in the ICU setting (Ely EW. Crit Care Med. 2017;45[2]:321). While engagement of family members began with our recognition of their role in emotionally supporting patients and efforts to improve communication, we have also seen the impact of family participation on reducing ICU delirium through frequent re-orientation and encouragement of early mobility (McKenzie J, et al. Australas J Ageing. 2020;39:21). In fact, a recent study has suggested that family members could play an even more active role in detecting and assessing ICU delirium using objective assessment tools (Fiest K, et al. Crit Care Med. 2020;48[7]:954). Post-ICU PTSD has been well described in both ICU survivors as well as in their family members, with evidence that family participation in care of patients during their ICU stay leads to its reduction (Amass TH, et al. Crit Care Med. 2020[Feb];48[2]:176).
The emotional toll
Comforting patients and families in times of distress and suffering is something that comes naturally to many in critical care, and our training further improves our ability to do this effectively. No amount of training, however, could have prepared us for the degree and volume of suffering we bore witness to this past year and the resulting moral injury many are still dealing with. We were present for families’ most intimate moments, holding phones and tablets up to patients so their families could say their goodbyes, listening to the “I love yous,” “I’ll miss yous,” “I’m sorrys,” and “Please don’t gos.” Nurses held patients’ hands as they took their last breaths so they wouldn’t die alone and worked to move husbands and wives into the same room so they could be together in their final moments. Entrenched in each of our identities is the role of healer, and we found ourselves questioning our effectiveness in rising to meet suffering on a scale we had never seen before. Little did we understand that while our paradigms were reinforcing the benefits of patient-centered care for patients and their families, that framework was also serving to facilitate our role as healers – that without it, we all suffer.
Rising to the challenge
These unprecedented circumstances led to creative efforts to bridge some of these barriers. Health systems created photo lanyards that providers wore over their PPE so patients could identify their health care team and connect with them on a more human level. Video conferencing technology was brought to the patient bedside using smartphones and tablets to assist them in communicating with their families. Doctors and nurses coordinated multiple calls throughout the day to ensure families felt included in the care plans and were always abreast of any new developments.
All these initiatives were our way of attempting to alleviate some of the suffering we were witnessing, and in some ways felt complicit in. It is in hindsight that we can look back and question if we could have done things differently. We treated family as visitors, when in fact, they are fundamental members of the care team who play an active and critical role in patient care. This was, in part, driven by national unpreparedness when it came to PPE supplies, in addition to misinformation and inconsistent messaging early in the pandemic with regards to the mechanism of transmission of disease from various health organizations. While we did our best given the circumstances, we must not allow this experience to lead us away from the tenets we know to be essential to patient, family, and health care provider well-being.
All in health care met the call to action – nurses, physicians, advanced practice providers, respiratory therapists, nutritionists, pharmacists, physical therapists, patient transporters, environmental service workers, and all others who kept our hospitals and patient care facilities open through this pandemic and embarked on what amounted to a collective, global, ongoing “code-blue alert,” resuscitating patient after patient, hotspot after hotspot, region after region, and country after country. We expanded hospital bed capacities, created ICU beds where there were none, developed novel process protocols, and learned in real time what seemed to help (or not) in treating this novel disease, all while participating in incredible international scientific collaboration and information sharing that has contributed in getting the collective “us” through this first year of the pandemic. We did what we were trained and called to do.
Preparing for the future
There will inevitably be another public health crisis, and we must advocate for better preparedness next time, insisting on overall stronger public health systems and pandemic preparedness. We must address our PPE stores and supply chains. We must have disaster preparedness plans that go beyond the scope of mass casualty events and bioterrorism. Beyond physical recovery, we must tend to the factors that impact patients’ long-term recovery, with attention to emotional and psychological well-being. We must advocate for all of this now, while the memories are fresh and before the impact of this collective suffering begins to fade. It can never again be acceptable to exclude families from the health care setting. We must advocate for our patients and for the resources, systems, processes, and support that will allow us to do better.
Dr. Hegab is Associate Director, Pulmonary Hypertension Program, Medical Director, Pulmonary Embolism Response Team, Division of Pulmonary and Critical Care Medicine, Henry Ford Hospital; and Assistant Professor, Wayne State University School of Medicine, Detroit.