User login
Can we stop worrying about the age of blood?
Blood transfusions are common in critically ill patients; two in five adults admitted to an ICU receive at least one transfusion during their hospitalization (Corwin HL, et al. Crit Care Med. 2004;32[1]:39). Recently, there has been growing concern about the potential dangers involved with prolonged blood storage. Several provocative observational and retrospective studies found that prolonged storage time (ie, the age of the blood being transfused) negatively affects clinical outcomes (Wang D, et al. Transfusion. 2012;52[6]:1184). But now, some newly published trials on blood transfusion practice, including one published in late September 2017 (Cooper DJ, et al. N Engl J Med. Published online, September 27, 2017) seem to debunk much of this literature. Was all of the concern about age of blood overblown?
The appeal of “fresh” blood is intuitive. As consumers, we’re conditioned that the fresher the better. Fresh food tastes best. Carbonated beverages go “flat” over time. The newest iPhone® device is superior to your old one. So, of course, it follows that fresh blood is also better for your health than older blood.
But, in order to have a viable transfusion service, blood has to be stored. Blood is a scarce resource, and blood banks need to keep an adequate supply on hand for expected clinical necessities, as well as for emergencies. Donors can’t be on standby, waiting in the hospital to provide immediate whole blood transfusion. Also, blood needs to be tested for infections and for potential interactions with the patient, and whole blood must be broken down into individual components for transfusion. All of this requires time and storage.
In a randomized study of 100 critically ill adults supported by mechanical ventilation, 50 were randomized to receive “fresh” blood (median storage age 4 days, interquartile range 3-5 days) and 50 were randomized to receive “standard” blood (median storage age 26.5 days, interquartile range 21-36 days) (Kor DJ, et al. Am J Respir Crit Care Med. 2012;185[8]:842). The primary outcome was gas exchange, as prolonged storage of red blood cells could potentially lead to an increased inflammatory response in patients. However, the authors found no difference in gas exchange between the two groups, and there were no differences in immunologic function or coagulation status.
The ABLE (Age of Blood Evaluation) trial was a randomized, blinded trial of transfusion practices in critically ill patients (Lacroix J, et al. N Engl J Med. 2015;372:1410). In 64 centers in Canada and Europe, 2,430 critically ill adults were randomized to receive either “fresh” blood (mean storage age 6.1 ± 4.9 days) or “standard” blood (mean storage age 22.0 ± 8.4 days). The primary outcome was 90-day mortality, with a power of 90% to detect a 5% change in mortality between the two groups. The investigators found no statistically significant difference in 90-day mortality between the “fresh” and “standard” groups (37% vs 35.3%; hazard ratio 1.1; 95% CI 0.9 – 1.2). Additionally, there were no differences in secondary outcomes, including multiorgan system dysfunction, duration of supportive care, or development of nosocomial infections.
The INFORM (Informing Fresh versus Old Red Cell Management) trial was a randomized study of patients hospitalized in six centers in Canada, Australia, Israel, and the United States (Heddle NM, et al. N Engl J Med. 2016;375[2]:1937). A total of 24,736 patients received transfusions with either “fresh” blood (median storage age 11 days) or “standard” blood (median storage age 23 days). The primary outcome was in-hospital death, with a 90% power to detect a 15% lower relative risk. When comparing the 8,215 patients who received “fresh” blood and the 16,521 patients who received “standard” blood, the authors found no difference in mortality between the two groups (9.1% vs 8.8%; odds ratio 1.04; 95% CI 0.95 to 1.14). Furthermore, there were no differences in outcomes in the high-risk subgroups that included patients with cancer, patients in the ICU, and patients undergoing cardiovascular surgery.
A meta-analysis examined 12 trials of patients who received “fresh” blood compared with those who received “older” or “standard” blood (Alexander PE, et al. Blood. 2016;127[4]:400); 5,229 patients were included in these trials, in which “fresh” blood was defined as blood stored for 3 to 10 days and “older” blood was stored for longer durations. There was no difference in mortality between the two groups (relative risk 1.04; 95% CI 0.94 - 1.14), and no difference in adverse events (relative risk 1.02; 95% CI 0.91 - 1.14). However, perhaps surprisingly, “fresh” blood was associated with an increased risk of nosocomial infections (relative risk 1.09; 95% CI 1.00 - 1.18).
So, can we stop worrying about the age of the blood that we are about to transfuse? Probably. Taken together, these studies suggest that differences in the duration of red blood cell storage allowed within current US FDA standards aren’t clinically relevant, even in critically ill patients. At least, for now, the current practices for age of blood and duration of storage appear unrelated to adverse clinical outcomes.
Dr. Carroll is Professor of Pediatrics, University of Connecticut, Division of Critical Care, Connecticut Children’s Medical Center, Hartford, Connecticut.
Blood transfusions are common in critically ill patients; two in five adults admitted to an ICU receive at least one transfusion during their hospitalization (Corwin HL, et al. Crit Care Med. 2004;32[1]:39). Recently, there has been growing concern about the potential dangers involved with prolonged blood storage. Several provocative observational and retrospective studies found that prolonged storage time (ie, the age of the blood being transfused) negatively affects clinical outcomes (Wang D, et al. Transfusion. 2012;52[6]:1184). But now, some newly published trials on blood transfusion practice, including one published in late September 2017 (Cooper DJ, et al. N Engl J Med. Published online, September 27, 2017) seem to debunk much of this literature. Was all of the concern about age of blood overblown?
The appeal of “fresh” blood is intuitive. As consumers, we’re conditioned that the fresher the better. Fresh food tastes best. Carbonated beverages go “flat” over time. The newest iPhone® device is superior to your old one. So, of course, it follows that fresh blood is also better for your health than older blood.
But, in order to have a viable transfusion service, blood has to be stored. Blood is a scarce resource, and blood banks need to keep an adequate supply on hand for expected clinical necessities, as well as for emergencies. Donors can’t be on standby, waiting in the hospital to provide immediate whole blood transfusion. Also, blood needs to be tested for infections and for potential interactions with the patient, and whole blood must be broken down into individual components for transfusion. All of this requires time and storage.
In a randomized study of 100 critically ill adults supported by mechanical ventilation, 50 were randomized to receive “fresh” blood (median storage age 4 days, interquartile range 3-5 days) and 50 were randomized to receive “standard” blood (median storage age 26.5 days, interquartile range 21-36 days) (Kor DJ, et al. Am J Respir Crit Care Med. 2012;185[8]:842). The primary outcome was gas exchange, as prolonged storage of red blood cells could potentially lead to an increased inflammatory response in patients. However, the authors found no difference in gas exchange between the two groups, and there were no differences in immunologic function or coagulation status.
The ABLE (Age of Blood Evaluation) trial was a randomized, blinded trial of transfusion practices in critically ill patients (Lacroix J, et al. N Engl J Med. 2015;372:1410). In 64 centers in Canada and Europe, 2,430 critically ill adults were randomized to receive either “fresh” blood (mean storage age 6.1 ± 4.9 days) or “standard” blood (mean storage age 22.0 ± 8.4 days). The primary outcome was 90-day mortality, with a power of 90% to detect a 5% change in mortality between the two groups. The investigators found no statistically significant difference in 90-day mortality between the “fresh” and “standard” groups (37% vs 35.3%; hazard ratio 1.1; 95% CI 0.9 – 1.2). Additionally, there were no differences in secondary outcomes, including multiorgan system dysfunction, duration of supportive care, or development of nosocomial infections.
The INFORM (Informing Fresh versus Old Red Cell Management) trial was a randomized study of patients hospitalized in six centers in Canada, Australia, Israel, and the United States (Heddle NM, et al. N Engl J Med. 2016;375[2]:1937). A total of 24,736 patients received transfusions with either “fresh” blood (median storage age 11 days) or “standard” blood (median storage age 23 days). The primary outcome was in-hospital death, with a 90% power to detect a 15% lower relative risk. When comparing the 8,215 patients who received “fresh” blood and the 16,521 patients who received “standard” blood, the authors found no difference in mortality between the two groups (9.1% vs 8.8%; odds ratio 1.04; 95% CI 0.95 to 1.14). Furthermore, there were no differences in outcomes in the high-risk subgroups that included patients with cancer, patients in the ICU, and patients undergoing cardiovascular surgery.
A meta-analysis examined 12 trials of patients who received “fresh” blood compared with those who received “older” or “standard” blood (Alexander PE, et al. Blood. 2016;127[4]:400); 5,229 patients were included in these trials, in which “fresh” blood was defined as blood stored for 3 to 10 days and “older” blood was stored for longer durations. There was no difference in mortality between the two groups (relative risk 1.04; 95% CI 0.94 - 1.14), and no difference in adverse events (relative risk 1.02; 95% CI 0.91 - 1.14). However, perhaps surprisingly, “fresh” blood was associated with an increased risk of nosocomial infections (relative risk 1.09; 95% CI 1.00 - 1.18).
So, can we stop worrying about the age of the blood that we are about to transfuse? Probably. Taken together, these studies suggest that differences in the duration of red blood cell storage allowed within current US FDA standards aren’t clinically relevant, even in critically ill patients. At least, for now, the current practices for age of blood and duration of storage appear unrelated to adverse clinical outcomes.
Dr. Carroll is Professor of Pediatrics, University of Connecticut, Division of Critical Care, Connecticut Children’s Medical Center, Hartford, Connecticut.
Blood transfusions are common in critically ill patients; two in five adults admitted to an ICU receive at least one transfusion during their hospitalization (Corwin HL, et al. Crit Care Med. 2004;32[1]:39). Recently, there has been growing concern about the potential dangers involved with prolonged blood storage. Several provocative observational and retrospective studies found that prolonged storage time (ie, the age of the blood being transfused) negatively affects clinical outcomes (Wang D, et al. Transfusion. 2012;52[6]:1184). But now, some newly published trials on blood transfusion practice, including one published in late September 2017 (Cooper DJ, et al. N Engl J Med. Published online, September 27, 2017) seem to debunk much of this literature. Was all of the concern about age of blood overblown?
The appeal of “fresh” blood is intuitive. As consumers, we’re conditioned that the fresher the better. Fresh food tastes best. Carbonated beverages go “flat” over time. The newest iPhone® device is superior to your old one. So, of course, it follows that fresh blood is also better for your health than older blood.
But, in order to have a viable transfusion service, blood has to be stored. Blood is a scarce resource, and blood banks need to keep an adequate supply on hand for expected clinical necessities, as well as for emergencies. Donors can’t be on standby, waiting in the hospital to provide immediate whole blood transfusion. Also, blood needs to be tested for infections and for potential interactions with the patient, and whole blood must be broken down into individual components for transfusion. All of this requires time and storage.
In a randomized study of 100 critically ill adults supported by mechanical ventilation, 50 were randomized to receive “fresh” blood (median storage age 4 days, interquartile range 3-5 days) and 50 were randomized to receive “standard” blood (median storage age 26.5 days, interquartile range 21-36 days) (Kor DJ, et al. Am J Respir Crit Care Med. 2012;185[8]:842). The primary outcome was gas exchange, as prolonged storage of red blood cells could potentially lead to an increased inflammatory response in patients. However, the authors found no difference in gas exchange between the two groups, and there were no differences in immunologic function or coagulation status.
The ABLE (Age of Blood Evaluation) trial was a randomized, blinded trial of transfusion practices in critically ill patients (Lacroix J, et al. N Engl J Med. 2015;372:1410). In 64 centers in Canada and Europe, 2,430 critically ill adults were randomized to receive either “fresh” blood (mean storage age 6.1 ± 4.9 days) or “standard” blood (mean storage age 22.0 ± 8.4 days). The primary outcome was 90-day mortality, with a power of 90% to detect a 5% change in mortality between the two groups. The investigators found no statistically significant difference in 90-day mortality between the “fresh” and “standard” groups (37% vs 35.3%; hazard ratio 1.1; 95% CI 0.9 – 1.2). Additionally, there were no differences in secondary outcomes, including multiorgan system dysfunction, duration of supportive care, or development of nosocomial infections.
The INFORM (Informing Fresh versus Old Red Cell Management) trial was a randomized study of patients hospitalized in six centers in Canada, Australia, Israel, and the United States (Heddle NM, et al. N Engl J Med. 2016;375[2]:1937). A total of 24,736 patients received transfusions with either “fresh” blood (median storage age 11 days) or “standard” blood (median storage age 23 days). The primary outcome was in-hospital death, with a 90% power to detect a 15% lower relative risk. When comparing the 8,215 patients who received “fresh” blood and the 16,521 patients who received “standard” blood, the authors found no difference in mortality between the two groups (9.1% vs 8.8%; odds ratio 1.04; 95% CI 0.95 to 1.14). Furthermore, there were no differences in outcomes in the high-risk subgroups that included patients with cancer, patients in the ICU, and patients undergoing cardiovascular surgery.
A meta-analysis examined 12 trials of patients who received “fresh” blood compared with those who received “older” or “standard” blood (Alexander PE, et al. Blood. 2016;127[4]:400); 5,229 patients were included in these trials, in which “fresh” blood was defined as blood stored for 3 to 10 days and “older” blood was stored for longer durations. There was no difference in mortality between the two groups (relative risk 1.04; 95% CI 0.94 - 1.14), and no difference in adverse events (relative risk 1.02; 95% CI 0.91 - 1.14). However, perhaps surprisingly, “fresh” blood was associated with an increased risk of nosocomial infections (relative risk 1.09; 95% CI 1.00 - 1.18).
So, can we stop worrying about the age of the blood that we are about to transfuse? Probably. Taken together, these studies suggest that differences in the duration of red blood cell storage allowed within current US FDA standards aren’t clinically relevant, even in critically ill patients. At least, for now, the current practices for age of blood and duration of storage appear unrelated to adverse clinical outcomes.
Dr. Carroll is Professor of Pediatrics, University of Connecticut, Division of Critical Care, Connecticut Children’s Medical Center, Hartford, Connecticut.
Hold your breath
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11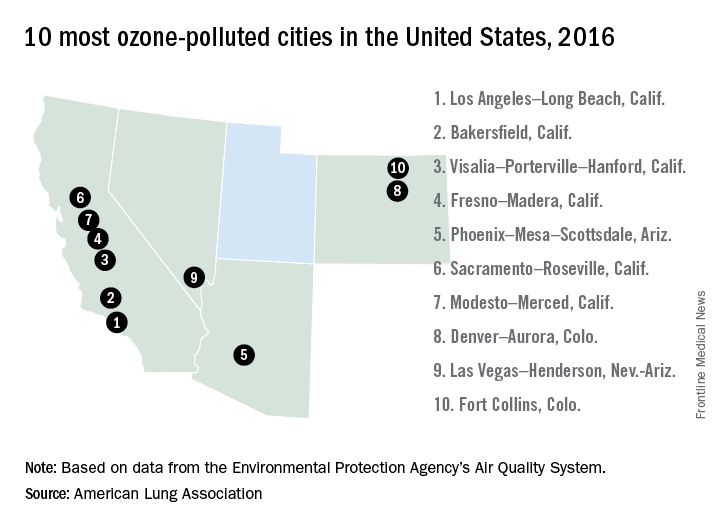
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11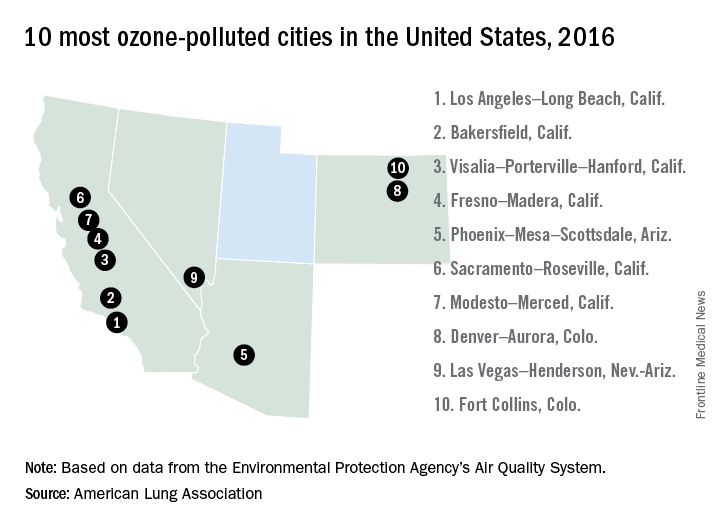
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.
“Exercising my ‘reasoned judgment,’ I have no doubt that the right to a climate system capable of sustaining human life is fundamental to a free and ordered society.”
– U.S. District Judge Ann Aiken in Kelsey Cascadia Rose Juliana vs. United States of America, et al.
In many areas of the world, the simple act of breathing has become hazardous to people’s health.
According to the World Health Organization, more people die every day from air pollution than from HIV/AIDS, tuberculosis, and road injuries combined. In China, more than 1 million deaths annually are linked to polluted air (76/100,000); in India the number of deaths is more than 600,000 annually (49/100,000); and in the United States, that figure comes to more than 38,000 (12/100,000).
And yet, nonpolluting, alternative options – such as sun and wind power – are readily available.
Dirty air is visible on a hot summer day – when, mixed with other substances, it forms smog. Higher temperatures can then speed up the chemical reactions that form smog. We breathe in that polluted air, especially on days when the air is stagnant or there is temperature inversion.
The health effects of climate change
Black carbon found in air pollution leads to drug-resistant bacteria and alters antibiotic tolerance.1 The pollution also is associated with multiple cancers: lung, liver, ovarian, and, possibly, breast.2,3,4,5 It causes inflammation linked to the development of coronary artery disease (seen even in children!) and plaque formation leading to heart attacks and cardiac arrhythmias – including atrial fibrillation. Air pollution causes, triggers, or worsens respiratory illnesses – chronic obstructive pulmonary disease, emphysema, asthma, infections – and is responsible for lifelong diminished lung volume in children (a reason families are leaving Beijing.) Exponentially increased rates of autism are linked to bad air quality, as are autoimmune diseases, which also are on the rise.6,7 Polluted air causes brain inflammation – living near sources of air pollution increases the risk of dementia – and other neurodegenerative diseases such as Alzheimer’s disease, Parkinson’s, and amyotrophic lateral sclerosis.8 The blood brain barrier protects the brain from most foreign matter, but particulate matter, especially ultrafine particulate matter of less than 1 mcm such as magnetite, can cross directly into the brain via the olfactory nerve. (Magnetite has been identified in the brain tissue of residents living in areas where the substance is produced as a result of industrial waste.) While particulate matter of 2.5 mcmis measured in the United States, ultrafine particulate matter is not.
Psychiatric symptoms and chronic psychiatric disorders also are associated with polluted air: On days with poor air quality, a statistically significant increase is seen in suicide threats and visits to emergency departments for panic attacks.9,10
A rise in aggression occurs when there are abnormally high temperatures and significant changes in rainfall. More assaults, murders, suicides, domestic violence, and child abuse can be expected, and a rise in unrest around the world should come as no surprise.
As a consequence of increased CO2 in the atmosphere, temperatures have already risen by 2° F: Sixteen of the hottest years on record have occurred in the last 17 years, with 2016 as the hottest year ever recorded. In Iraq and Kuwait, the temperature last summer reached 129.2° F.
We are experiencing more frequent and extreme weather events, chronic climate conditions, and the cascading disruption of ecosystems. Drought and sea level rise are leading to physical and psychological impacts – both direct and indirect. Some regions of the world have become destabilized, triggering migrations and the refugee crisis.
Along with these psychological impacts, CO2 affects cognition: A recent study by the Harvard School of Public Health, Boston, shows that the indoor levels of CO2 to which American workers typically are exposed impair cognitive functioning, particularly in the areas of strategic thinking, information processing, and crisis management.11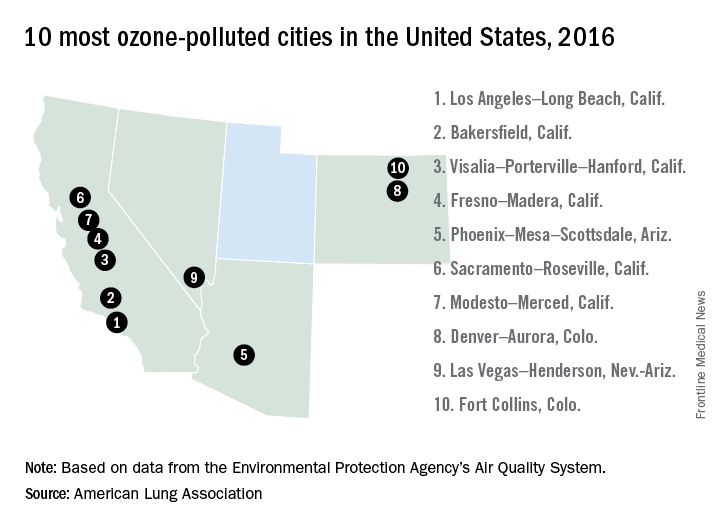
What do we do about it?
As mental health professionals, we know that aggression can be overt or passive (from inaction). Overwhelming evidence shows harm to public health from burning fossil fuels, and yet, though we are making progress, resistance still exists in the transition to clean, renewable energy critical for the health of our families and communities. When political will is what stands between us and getting back on a path to breathing clean air, how can inaction be understood as anything but an act of aggression?
This issue has reached U.S. courts: In a landmark case, 21 youths aged 9-20 years represented by “Our Children’s Trust” are suing the U.S. government in the Oregon U.S. District Court for failure to act on climate. The case, heard by Judge Ann Aiken, is now headed to trial.
All of us have a duty to collectively, repeatedly, and forcefully call on policy makers to take action.
That leads me to what we can do as doctors. In this effort to quickly transition to safe, clean renewable energy, we all have a role to play. The notion that we can’t do anything as individuals is no more credible than saying “my vote doesn’t matter.” Just as our actions as voters in a democracy demonstrate the collective civic responsibility we owe one another, so too do our actions on climate. As global citizens, all actions that we take to help us live within the planet’s means are opportunities to restore balance.
What we do collectively drives markets and determines the social norms that powerfully influence the decisions of others – sometimes even unconsciously.
As doctors, we have a unique role to play in the places we work – urging hospitals, clinics, academic centers, and other organizations and facilities to lead by example, become role models for energy efficiency, and choose clean renewable energy sources over the ones harming our health. We can start by choosing wind and solar to power our homes and influencing others to do the same.
We are the voices because this is a health message.
Dr. Van Susteren is a practicing general and forensic psychiatrist in Washington. She serves on the advisory board of the Center for Health and the Global Environment at Harvard T.H. Chan School of Public Health, Boston. Dr. Van Susteren is a former member of the board of directors of the National Wildlife Federation and coauthor of group’s report, “The Psychological Effects of Global Warming on the United States – Why the U.S. Mental Health System is Not Prepared.” In 2006, Dr. Van Susteren sought the Democratic nomination for a U.S. Senate seat in Maryland. She also founded Lucky Planet Foods, a company that provides plant-based, low carbon foods.
References
1. Environ Microbiol. 2017 Feb 14. doi: 10.1111/1462-2920.13686.
2. Environ Health Perspect. 2017 Mar;125[3]:378-84.
3. J Hepatol. 2015;63[6]:1397-1404.
4. J Toxicol Environ Health A. 2012;75[3]:174-82.
5. Environ Health Perspect. 2012 Nov; 118[11]:1578-83.
6. J Child Psychol Psychiatry. 2016; 57[3]:271-92.
7. Curr Opin Pediatr. 2010;22[2]219-25.
8. Inhal Toxicol. 2008;20[5]:499-506.
9. J Psychiatr Res. 2015 Mar;62:130-5.
10. Schizophr Res. 2016 Oct 5. doi: 10.1016/j.schres.2016.10.003.
11. Environ Health Perspect. 2016 Jun;124[6]:805-12.




