User login
Is the doctor in?
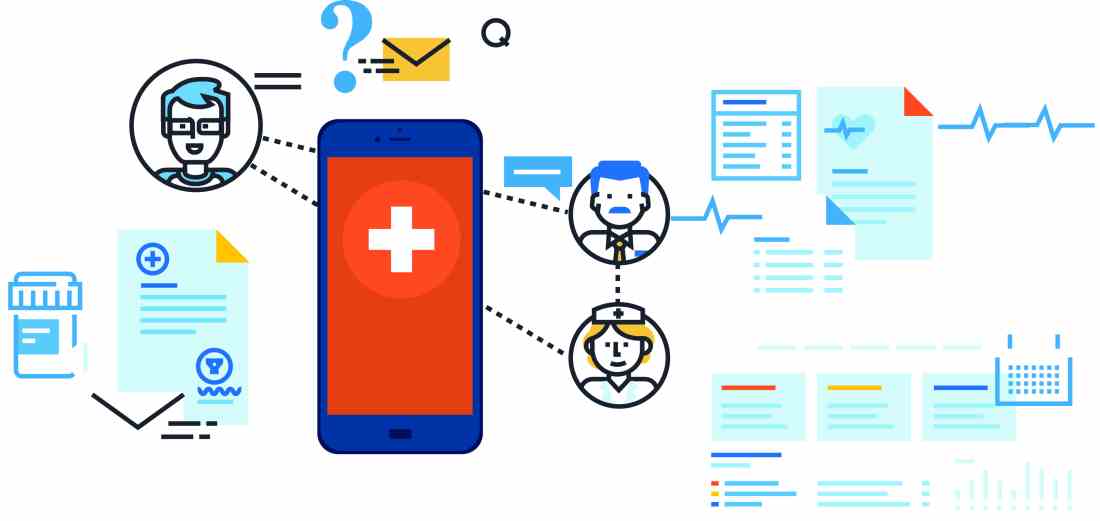
Within hospital medicine, there has been a recent increase in programs that provide virtual or telehealth hospitalists, primarily to hospitals that are small, remote, and/or understaffed. According to a 2013 Cisco health care customer experience report, the number of telehealth consumers will likely markedly increase to at least 7 million by 2018.1
Since telehospitalist programs are still relatively new, there are many questions about why and how they exist and how they are (and can be) funded. Questions also remain about some limitations of telehospitalist programs for both the “givers” and the “receivers” of the services. I tackle some of these questions in this article.
What is a telehospitalist?
What are the drivers of telehospitalist programs?
One primary driver of telehealth (and specifically telehospitalist) programs is an ongoing shortage of hospitalists, especially in remote areas and critical access hospitals where coverage issues are especially prominent at night and/or on weekends. In many hospitals, there is also a growing unwillingness on the part of physicians to be routinely on call at night. Although working on call used to be on par with being a physician, many younger-generation physicians are less willing to blur “work and life.” This increases the need for dedicated night coverage in many hospitals.
Another driver for some programs (especially at tertiary care medical centers) is a desire to more thoroughly assess patients prior to transfer to their respective centers (the alternative being a phone conversation with the transferring center about the patient’s status). There is also a growing desire to keep patients local if possible, which is usually better for the patient and the family and can decrease the total cost of their care.
Another catalyst to telehospitalist program growth is the growing cultural comfort level with two-way video interactions, such as Skype and FaceTime. Since videoconferencing has permeated most of our professional and personal lives, telehealth seems familiar and comfortable for both providers and patients. In a recent consumer survey, three out of every four consumers responded that they are very comfortable communicating with providers via technology, as opposed to seeing them in person.1
Another driver for some programs is financial. Depending on the way the program is structured, it can be not only financially feasible but financially beneficial, especially if the program can consolidate coverage across multiple sites (more on this later).
One other driver for some health care systems is the need to cover areas with on-site nurse practitioners and physician assistants. Using a telehospitalist makes it easier to get appropriate and required oversight for this coverage model across time and space.
What are the advantages of being a telehospitalist?
Some of the career advantages of being a telehospitalist include the shift flexibility and convenience. This work allows a hospitalist to serve a shift from anywhere in the world and from the convenience of their home. Some telehospitalists can easily work local night shifts when they live many time zones away (and therefore, don’t actually have to work a night shift). Many programs are designed to have a single hospitalist cover many hospitals over a wide geography, which would be logistically impossible to do in person. This is especially appealing for multihospital systems that cannot afford to have a hospitalist on site at each location.
The earning potential can also be appealing, depending on the number of shifts a hospitalist is willing to work.
What are the limitations of being a telehospitalist?
There are limits to what a telehospitalist can perform, many of which depend on the manner in which the program and the technology are arranged. Telehealth can vary from a cart-based videoconferencing system that is transported into a patient’s room to an independent robot that travels throughout sites. The primary limitation is the need to rely on someone in the patient’s room to act as virtual hands. This usually falls to the bedside nurse and requires a good working relationship and patience on their part. The bedside nurses have to “buy into” the program in advance and may need to have scripting for how to explain the process to the patients.
Another major challenge is interacting with different electronic health record systems. Becoming agile with a single EHR is challenging enough, but maneuvering several of them in a single shift can be extremely trying. Telehospitalists can also be challenged by technology glitches or failures that need troubleshooting both on their end and on-site. Although these problems are rare, there will always be a concern that the patient will not get his or her needs met if the technology fails.
How does the financing work?
Although this is a rapidly changing landscape, telehospitalists are not currently able to generate much revenue from professional billing. Unlike in-person visits, Medicare will not reimburse professional fees for telehospitalist visits. Although each payer is unique, most other (nonMedicare) payers are also not willing to reimburse for televisits. This may change in the future, however, as Medicare does pay for virtual specialty services such as telestroke. In addition, many states have enacted telemedicine parity laws, which require private payers to pay for all health care services equally, regardless of modality (audio, video, or in person).
For now, the financial case for employing telehospitalists for most programs has to be made using benfits other than the generation of professional fees. For telehospitalist programs that can cover several sites, the cost is substantially less than employing individual on-site hospitalists to do low-volume work. Telehospitalist programs are also, likely, less costly than is locum tenens staffing. For programs that evaluate the need for transfers, a case can be made that keeping a patient in a smaller, low-cost venue, rather than transferring them to a larger, higher-cost venue, can also reduce overall cost for a health care system.
What about licensing and credentialing?
Telehospitalists can be hindered by the need to have a license in several states and to be credentialed in several systems. This can be cumbersome, time-consuming, and expensive. To ease the multistate licensing burden, the Interstate Medical Licensure Compact has been established.2 This is an accelerated licensure process for eligible physicians that improves license portability across states. There are currently 18 states that participate, and the number continues to increase.
For credentialing, most hospitals require initial credentialing and full recredentialing every 2 years. Maintaining credentials at several sites can be extremely time consuming. To ease this burden, some hospitals with telehealth programs have adopted “credentialing by proxy,” which means that one hospital will accept the credentialing process of another facility.
What next?
In summary, there has been and will likely continue to be explosive growth of telehospitalist programs and providers for all the reasons outlined above. Although some barriers to efficient and effective practice do exist, many of those barriers are being overcome quite rapidly. I expect this growth to continue for the betterment of hospitalists, our patients, and the systems in which we work. For a more in-depth look into telemedicine in hospital medicine, view a report created by a work group of SHM's Practice Management Committee.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
1.Cisco. (2013 March 4). Cisco Study Reveals 74 Percent of Consumers Open to Virtual Doctor Visit. Cisco: The Network. Retrieved from https://newsroom.cisco.com/press-release-content?type=webcontent&articleId=1148539.
2. Interstate Medical Licensure Compact Commission. (2017). Interstate Medical Licensure Compact. Retrieved from http://www.licenseportability.org/index.html.
Within hospital medicine, there has been a recent increase in programs that provide virtual or telehealth hospitalists, primarily to hospitals that are small, remote, and/or understaffed. According to a 2013 Cisco health care customer experience report, the number of telehealth consumers will likely markedly increase to at least 7 million by 2018.1
Since telehospitalist programs are still relatively new, there are many questions about why and how they exist and how they are (and can be) funded. Questions also remain about some limitations of telehospitalist programs for both the “givers” and the “receivers” of the services. I tackle some of these questions in this article.
What is a telehospitalist?
What are the drivers of telehospitalist programs?
One primary driver of telehealth (and specifically telehospitalist) programs is an ongoing shortage of hospitalists, especially in remote areas and critical access hospitals where coverage issues are especially prominent at night and/or on weekends. In many hospitals, there is also a growing unwillingness on the part of physicians to be routinely on call at night. Although working on call used to be on par with being a physician, many younger-generation physicians are less willing to blur “work and life.” This increases the need for dedicated night coverage in many hospitals.
Another driver for some programs (especially at tertiary care medical centers) is a desire to more thoroughly assess patients prior to transfer to their respective centers (the alternative being a phone conversation with the transferring center about the patient’s status). There is also a growing desire to keep patients local if possible, which is usually better for the patient and the family and can decrease the total cost of their care.
Another catalyst to telehospitalist program growth is the growing cultural comfort level with two-way video interactions, such as Skype and FaceTime. Since videoconferencing has permeated most of our professional and personal lives, telehealth seems familiar and comfortable for both providers and patients. In a recent consumer survey, three out of every four consumers responded that they are very comfortable communicating with providers via technology, as opposed to seeing them in person.1
Another driver for some programs is financial. Depending on the way the program is structured, it can be not only financially feasible but financially beneficial, especially if the program can consolidate coverage across multiple sites (more on this later).
One other driver for some health care systems is the need to cover areas with on-site nurse practitioners and physician assistants. Using a telehospitalist makes it easier to get appropriate and required oversight for this coverage model across time and space.
What are the advantages of being a telehospitalist?
Some of the career advantages of being a telehospitalist include the shift flexibility and convenience. This work allows a hospitalist to serve a shift from anywhere in the world and from the convenience of their home. Some telehospitalists can easily work local night shifts when they live many time zones away (and therefore, don’t actually have to work a night shift). Many programs are designed to have a single hospitalist cover many hospitals over a wide geography, which would be logistically impossible to do in person. This is especially appealing for multihospital systems that cannot afford to have a hospitalist on site at each location.
The earning potential can also be appealing, depending on the number of shifts a hospitalist is willing to work.
What are the limitations of being a telehospitalist?
There are limits to what a telehospitalist can perform, many of which depend on the manner in which the program and the technology are arranged. Telehealth can vary from a cart-based videoconferencing system that is transported into a patient’s room to an independent robot that travels throughout sites. The primary limitation is the need to rely on someone in the patient’s room to act as virtual hands. This usually falls to the bedside nurse and requires a good working relationship and patience on their part. The bedside nurses have to “buy into” the program in advance and may need to have scripting for how to explain the process to the patients.
Another major challenge is interacting with different electronic health record systems. Becoming agile with a single EHR is challenging enough, but maneuvering several of them in a single shift can be extremely trying. Telehospitalists can also be challenged by technology glitches or failures that need troubleshooting both on their end and on-site. Although these problems are rare, there will always be a concern that the patient will not get his or her needs met if the technology fails.
How does the financing work?
Although this is a rapidly changing landscape, telehospitalists are not currently able to generate much revenue from professional billing. Unlike in-person visits, Medicare will not reimburse professional fees for telehospitalist visits. Although each payer is unique, most other (nonMedicare) payers are also not willing to reimburse for televisits. This may change in the future, however, as Medicare does pay for virtual specialty services such as telestroke. In addition, many states have enacted telemedicine parity laws, which require private payers to pay for all health care services equally, regardless of modality (audio, video, or in person).
For now, the financial case for employing telehospitalists for most programs has to be made using benfits other than the generation of professional fees. For telehospitalist programs that can cover several sites, the cost is substantially less than employing individual on-site hospitalists to do low-volume work. Telehospitalist programs are also, likely, less costly than is locum tenens staffing. For programs that evaluate the need for transfers, a case can be made that keeping a patient in a smaller, low-cost venue, rather than transferring them to a larger, higher-cost venue, can also reduce overall cost for a health care system.
What about licensing and credentialing?
Telehospitalists can be hindered by the need to have a license in several states and to be credentialed in several systems. This can be cumbersome, time-consuming, and expensive. To ease the multistate licensing burden, the Interstate Medical Licensure Compact has been established.2 This is an accelerated licensure process for eligible physicians that improves license portability across states. There are currently 18 states that participate, and the number continues to increase.
For credentialing, most hospitals require initial credentialing and full recredentialing every 2 years. Maintaining credentials at several sites can be extremely time consuming. To ease this burden, some hospitals with telehealth programs have adopted “credentialing by proxy,” which means that one hospital will accept the credentialing process of another facility.
What next?
In summary, there has been and will likely continue to be explosive growth of telehospitalist programs and providers for all the reasons outlined above. Although some barriers to efficient and effective practice do exist, many of those barriers are being overcome quite rapidly. I expect this growth to continue for the betterment of hospitalists, our patients, and the systems in which we work. For a more in-depth look into telemedicine in hospital medicine, view a report created by a work group of SHM's Practice Management Committee.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
1.Cisco. (2013 March 4). Cisco Study Reveals 74 Percent of Consumers Open to Virtual Doctor Visit. Cisco: The Network. Retrieved from https://newsroom.cisco.com/press-release-content?type=webcontent&articleId=1148539.
2. Interstate Medical Licensure Compact Commission. (2017). Interstate Medical Licensure Compact. Retrieved from http://www.licenseportability.org/index.html.
Within hospital medicine, there has been a recent increase in programs that provide virtual or telehealth hospitalists, primarily to hospitals that are small, remote, and/or understaffed. According to a 2013 Cisco health care customer experience report, the number of telehealth consumers will likely markedly increase to at least 7 million by 2018.1
Since telehospitalist programs are still relatively new, there are many questions about why and how they exist and how they are (and can be) funded. Questions also remain about some limitations of telehospitalist programs for both the “givers” and the “receivers” of the services. I tackle some of these questions in this article.
What is a telehospitalist?
What are the drivers of telehospitalist programs?
One primary driver of telehealth (and specifically telehospitalist) programs is an ongoing shortage of hospitalists, especially in remote areas and critical access hospitals where coverage issues are especially prominent at night and/or on weekends. In many hospitals, there is also a growing unwillingness on the part of physicians to be routinely on call at night. Although working on call used to be on par with being a physician, many younger-generation physicians are less willing to blur “work and life.” This increases the need for dedicated night coverage in many hospitals.
Another driver for some programs (especially at tertiary care medical centers) is a desire to more thoroughly assess patients prior to transfer to their respective centers (the alternative being a phone conversation with the transferring center about the patient’s status). There is also a growing desire to keep patients local if possible, which is usually better for the patient and the family and can decrease the total cost of their care.
Another catalyst to telehospitalist program growth is the growing cultural comfort level with two-way video interactions, such as Skype and FaceTime. Since videoconferencing has permeated most of our professional and personal lives, telehealth seems familiar and comfortable for both providers and patients. In a recent consumer survey, three out of every four consumers responded that they are very comfortable communicating with providers via technology, as opposed to seeing them in person.1
Another driver for some programs is financial. Depending on the way the program is structured, it can be not only financially feasible but financially beneficial, especially if the program can consolidate coverage across multiple sites (more on this later).
One other driver for some health care systems is the need to cover areas with on-site nurse practitioners and physician assistants. Using a telehospitalist makes it easier to get appropriate and required oversight for this coverage model across time and space.
What are the advantages of being a telehospitalist?
Some of the career advantages of being a telehospitalist include the shift flexibility and convenience. This work allows a hospitalist to serve a shift from anywhere in the world and from the convenience of their home. Some telehospitalists can easily work local night shifts when they live many time zones away (and therefore, don’t actually have to work a night shift). Many programs are designed to have a single hospitalist cover many hospitals over a wide geography, which would be logistically impossible to do in person. This is especially appealing for multihospital systems that cannot afford to have a hospitalist on site at each location.
The earning potential can also be appealing, depending on the number of shifts a hospitalist is willing to work.
What are the limitations of being a telehospitalist?
There are limits to what a telehospitalist can perform, many of which depend on the manner in which the program and the technology are arranged. Telehealth can vary from a cart-based videoconferencing system that is transported into a patient’s room to an independent robot that travels throughout sites. The primary limitation is the need to rely on someone in the patient’s room to act as virtual hands. This usually falls to the bedside nurse and requires a good working relationship and patience on their part. The bedside nurses have to “buy into” the program in advance and may need to have scripting for how to explain the process to the patients.
Another major challenge is interacting with different electronic health record systems. Becoming agile with a single EHR is challenging enough, but maneuvering several of them in a single shift can be extremely trying. Telehospitalists can also be challenged by technology glitches or failures that need troubleshooting both on their end and on-site. Although these problems are rare, there will always be a concern that the patient will not get his or her needs met if the technology fails.
How does the financing work?
Although this is a rapidly changing landscape, telehospitalists are not currently able to generate much revenue from professional billing. Unlike in-person visits, Medicare will not reimburse professional fees for telehospitalist visits. Although each payer is unique, most other (nonMedicare) payers are also not willing to reimburse for televisits. This may change in the future, however, as Medicare does pay for virtual specialty services such as telestroke. In addition, many states have enacted telemedicine parity laws, which require private payers to pay for all health care services equally, regardless of modality (audio, video, or in person).
For now, the financial case for employing telehospitalists for most programs has to be made using benfits other than the generation of professional fees. For telehospitalist programs that can cover several sites, the cost is substantially less than employing individual on-site hospitalists to do low-volume work. Telehospitalist programs are also, likely, less costly than is locum tenens staffing. For programs that evaluate the need for transfers, a case can be made that keeping a patient in a smaller, low-cost venue, rather than transferring them to a larger, higher-cost venue, can also reduce overall cost for a health care system.
What about licensing and credentialing?
Telehospitalists can be hindered by the need to have a license in several states and to be credentialed in several systems. This can be cumbersome, time-consuming, and expensive. To ease the multistate licensing burden, the Interstate Medical Licensure Compact has been established.2 This is an accelerated licensure process for eligible physicians that improves license portability across states. There are currently 18 states that participate, and the number continues to increase.
For credentialing, most hospitals require initial credentialing and full recredentialing every 2 years. Maintaining credentials at several sites can be extremely time consuming. To ease this burden, some hospitals with telehealth programs have adopted “credentialing by proxy,” which means that one hospital will accept the credentialing process of another facility.
What next?
In summary, there has been and will likely continue to be explosive growth of telehospitalist programs and providers for all the reasons outlined above. Although some barriers to efficient and effective practice do exist, many of those barriers are being overcome quite rapidly. I expect this growth to continue for the betterment of hospitalists, our patients, and the systems in which we work. For a more in-depth look into telemedicine in hospital medicine, view a report created by a work group of SHM's Practice Management Committee.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
1.Cisco. (2013 March 4). Cisco Study Reveals 74 Percent of Consumers Open to Virtual Doctor Visit. Cisco: The Network. Retrieved from https://newsroom.cisco.com/press-release-content?type=webcontent&articleId=1148539.
2. Interstate Medical Licensure Compact Commission. (2017). Interstate Medical Licensure Compact. Retrieved from http://www.licenseportability.org/index.html.
VIDEO: Attaining the tools to start your own quality improvement project
Quality improvement at the program level is a major concern for most hospitalists. That’s exactly why Venkata Dontaraju, MD, MRCP, FHM, attended a Tuesday afternoon HM17 workshop entitled “Adding to Your Toolbox: QI Methodologies.”
Dr. Dontaraju, a hospitalist for 7 years with Rockford Health Physicians in Loves Park, Ill., wants to begin QI projects of his own. He planned to attend a number of QI-focused sessions at the annual meeting, with the toolbox session laying the foundation for such work.
“There is a lot of emphasis on cutting down the waste in health care, and also improving the processes,” he said. “That is where the role of QI comes into place. I want to do QI projects at my own hospital, but I first want to get the tools necessary for a successful project.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Quality improvement at the program level is a major concern for most hospitalists. That’s exactly why Venkata Dontaraju, MD, MRCP, FHM, attended a Tuesday afternoon HM17 workshop entitled “Adding to Your Toolbox: QI Methodologies.”
Dr. Dontaraju, a hospitalist for 7 years with Rockford Health Physicians in Loves Park, Ill., wants to begin QI projects of his own. He planned to attend a number of QI-focused sessions at the annual meeting, with the toolbox session laying the foundation for such work.
“There is a lot of emphasis on cutting down the waste in health care, and also improving the processes,” he said. “That is where the role of QI comes into place. I want to do QI projects at my own hospital, but I first want to get the tools necessary for a successful project.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Quality improvement at the program level is a major concern for most hospitalists. That’s exactly why Venkata Dontaraju, MD, MRCP, FHM, attended a Tuesday afternoon HM17 workshop entitled “Adding to Your Toolbox: QI Methodologies.”
Dr. Dontaraju, a hospitalist for 7 years with Rockford Health Physicians in Loves Park, Ill., wants to begin QI projects of his own. He planned to attend a number of QI-focused sessions at the annual meeting, with the toolbox session laying the foundation for such work.
“There is a lot of emphasis on cutting down the waste in health care, and also improving the processes,” he said. “That is where the role of QI comes into place. I want to do QI projects at my own hospital, but I first want to get the tools necessary for a successful project.”
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Hospitalists offer tips on QI projects
Anjala Tess, MD, a hospitalist at Beth Israel Deaconess Medical Center and assistant professor of medicine at Harvard Medical School, Boston, asked the audience how many of them had done a quality improvement project that had failed. It was not a time to be bashful: Almost half the hospitalists in the room admitted that it had happened to them.
Dr. Tess and Darlene Tad-y, MD, chair of the Physicians-in-Training Committee and an assistant professor of medicine at the University of Colorado, were there to offer help in their session, “Adding to Your QI Toolbox.”
They highlighted three tools that they say are crucial to a project’s success: Creating a process map for clearly outlining how the project will work, interacting with stakeholders productively, and displaying data in a meaningful way.
Process mapping is a way of visualizing work or a process as distinct, ordered, and related steps, Dr. Tess said. Arranged on Post-It notes or written on a white board, the process should be one that can easily be updated. Seen objectively as a set of steps, it helps remove bias in how a process is viewed, she said.
“I would encourage you to do this on every QI project that you do where you are trying to accomplish something, because it makes a huge difference in understanding the work,” she said.
Stakeholder analysis – understanding the key people whose support could determine the success of the project – is also critical, she said. This can help get buy-in for the change, and it make a project stronger – and without it, you could doom your project, Dr. Tess said.
Doing this well involves understanding their financial and emotional interests, all the way down to whether they prefer face-to-face communication or e-mail, she said.
Then there’s the data. For it to matter, it must be presented well, and that requires context, Dr. Tad-y said.
“Data are just raw facts and figures,” she said. “Data are not the same as information.”
She suggested using run charts, in which data are plotted in some kind of order, usually chronological order. This kind of chart will typically include a median line, showing practice patterns before the QI project began, as well as a “goal line” to aim for, and notations on the timeline when changes were made, she said.
Others will be looking to the project manager for the meaning behind the data, she said.
“The story is going to come from you,” she said. “Otherwise, it’s just numbers.”
Anjala Tess, MD, a hospitalist at Beth Israel Deaconess Medical Center and assistant professor of medicine at Harvard Medical School, Boston, asked the audience how many of them had done a quality improvement project that had failed. It was not a time to be bashful: Almost half the hospitalists in the room admitted that it had happened to them.
Dr. Tess and Darlene Tad-y, MD, chair of the Physicians-in-Training Committee and an assistant professor of medicine at the University of Colorado, were there to offer help in their session, “Adding to Your QI Toolbox.”
They highlighted three tools that they say are crucial to a project’s success: Creating a process map for clearly outlining how the project will work, interacting with stakeholders productively, and displaying data in a meaningful way.
Process mapping is a way of visualizing work or a process as distinct, ordered, and related steps, Dr. Tess said. Arranged on Post-It notes or written on a white board, the process should be one that can easily be updated. Seen objectively as a set of steps, it helps remove bias in how a process is viewed, she said.
“I would encourage you to do this on every QI project that you do where you are trying to accomplish something, because it makes a huge difference in understanding the work,” she said.
Stakeholder analysis – understanding the key people whose support could determine the success of the project – is also critical, she said. This can help get buy-in for the change, and it make a project stronger – and without it, you could doom your project, Dr. Tess said.
Doing this well involves understanding their financial and emotional interests, all the way down to whether they prefer face-to-face communication or e-mail, she said.
Then there’s the data. For it to matter, it must be presented well, and that requires context, Dr. Tad-y said.
“Data are just raw facts and figures,” she said. “Data are not the same as information.”
She suggested using run charts, in which data are plotted in some kind of order, usually chronological order. This kind of chart will typically include a median line, showing practice patterns before the QI project began, as well as a “goal line” to aim for, and notations on the timeline when changes were made, she said.
Others will be looking to the project manager for the meaning behind the data, she said.
“The story is going to come from you,” she said. “Otherwise, it’s just numbers.”
Anjala Tess, MD, a hospitalist at Beth Israel Deaconess Medical Center and assistant professor of medicine at Harvard Medical School, Boston, asked the audience how many of them had done a quality improvement project that had failed. It was not a time to be bashful: Almost half the hospitalists in the room admitted that it had happened to them.
Dr. Tess and Darlene Tad-y, MD, chair of the Physicians-in-Training Committee and an assistant professor of medicine at the University of Colorado, were there to offer help in their session, “Adding to Your QI Toolbox.”
They highlighted three tools that they say are crucial to a project’s success: Creating a process map for clearly outlining how the project will work, interacting with stakeholders productively, and displaying data in a meaningful way.
Process mapping is a way of visualizing work or a process as distinct, ordered, and related steps, Dr. Tess said. Arranged on Post-It notes or written on a white board, the process should be one that can easily be updated. Seen objectively as a set of steps, it helps remove bias in how a process is viewed, she said.
“I would encourage you to do this on every QI project that you do where you are trying to accomplish something, because it makes a huge difference in understanding the work,” she said.
Stakeholder analysis – understanding the key people whose support could determine the success of the project – is also critical, she said. This can help get buy-in for the change, and it make a project stronger – and without it, you could doom your project, Dr. Tess said.
Doing this well involves understanding their financial and emotional interests, all the way down to whether they prefer face-to-face communication or e-mail, she said.
Then there’s the data. For it to matter, it must be presented well, and that requires context, Dr. Tad-y said.
“Data are just raw facts and figures,” she said. “Data are not the same as information.”
She suggested using run charts, in which data are plotted in some kind of order, usually chronological order. This kind of chart will typically include a median line, showing practice patterns before the QI project began, as well as a “goal line” to aim for, and notations on the timeline when changes were made, she said.
Others will be looking to the project manager for the meaning behind the data, she said.
“The story is going to come from you,” she said. “Otherwise, it’s just numbers.”
Crossing the personal quality chasm: QI enthusiast to QI leader
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s Note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Jennifer Myers, director of quality and safety education at the University of Pennsylvania, Philadelphia.
Even as a junior physician, Jennifer Myers, MD, FHM, embraced the complexities of the hospital system and the opportunity to transform patient care. She was one of the first hospitalists to participate in and lead quality improvement (QI) work at the University of Pennsylvania Medical Center more than 10 years ago, where, “in that role, I got to know almost everyone in the hospital and got an up-close view of how the hospital works administratively,” she recalled.
The experience taught Dr. Myers how little she knew at that time about hospital operations, and she convinced hospital administrators that a mechanism was needed to prepare the next generation of leaders in QI and patient safety. In 2011, with the support of a career development award from the Josiah Macy Jr. Foundation, Dr. Myers formulated a quality and patient safety curriculum for residents of Penn Medicine, as well as a more basic introductory program for medical students.
“You will always do your best in work that you are passionate about,” she said, advising others to do the same when choosing their career pathways. “Find others who are interested in – or frustrated by – the same things that you are, and work with them as you begin to shape your projects. If it’s the opioid epidemic, partner with someone in the hospital with an interest in making informed prescribing decisions. If it’s working with residents in quality, find a chief resident to help you develop an educational pathway or elective.”
Dr. Myers says that hospitalists who function at the intersection of the ICU, the ER, and inpatient care are naturally suited for leadership positions in quality and patient safety, “but, if you are a hospitalist aspiring to be a chief quality or medical officer or (someone) who wants to know the field more deeply, I recommend getting advanced training.”
Hospitalists now have multiple educational opportunities in QI to choose from, but that was not the case 7 years ago when SHM leaders invited Dr. Myers to develop and lead the Quality and Safety Educators Academy (QSEA). The 2.5-day program trains medical educators to develop curricula that incorporate quality improvement and safety principles into their local institutions. “We give them the core quality and safety knowledge but also the skills to develop and assess curricula,” Dr. Myers said. “The program also focuses on professional development and community building.”
While education is important, Dr. Myers says that a willingness to take risks is a greater predictor of success in QI. “It’s a very experiential field where you learn by doing. What you have done, and are willing to do, is more important than the training that you’ve had. Can you lead an initiative? Do you communicate well with people and teams? Can you articulate the value equation?”
She also advises hospitalists to find multiple mentors in quality work. “We talk a lot about that at QSEA,” Dr. Myers said. “It’s important to have the perspectives of people inside and outside of your institution. That’s also where the SHM network is helpful. Mentorship is a pillar of [many activities] at the annual meeting ... and [at] programs like the Academic Hospitalist Academy and QSEA.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Battling biases with the 5 Rs of cultural humility
How do we, as hospitalists, win the hearts and minds of patients, families, and care team members whom we do not know? What are the obstacles that we face when encountering patients and gaining the trust needed to improve patient care and patient experience?
With these questions in mind, the Cultural Humility Work Group, part of SHM’s Practice Management Committee, set out to develop a simple, universal framework to provide a foundation for strengthening communication skills and raising awareness of the basic tenets of cultural humility. According to Tervalon and Murray-Garcia, cultural humility is defined as a “process that requires humility as individuals continually engage in self-reflection and self-critique as lifelong learners and reflective practitioners. It requires humility in how physicians bring into check the power imbalances that exist in the dynamics of physician-patient communication by using patient-focused interviewing and care, and it is a process that requires humility to develop and maintain mutually respectful and dynamic partnerships with communities” (Tervalon, M. & Murray-García, J. “Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education.” J Health Care Poor Underserved. 1998;9[2]:117-25).
How do we win this battle? The first step is to simply be aware that everyone is a victim of unconscious biases. Once we come to this (often uncomfortable) realization, we must make a conscious effort to change our mindset and make conscious decisions to not allow these biases to manifest.
Practicing cultural humility is extremely important in this process. It puts everyone on the same platform because there is no “minority,” “majority,” or “ethnicity” associated with it. It takes away the need to know everything about a certain culture and encourages us to approach every patient encounter acknowledging that we will humble ourselves, learn what is important to the patient, and leave having learned something from the interaction.
The work group developed “The 5 Rs of Cultural Humility” as a simple tool for hospitalists to incorporate into their practice. The first four Rs (Reflection, Respect, Regard and Relevance) are extrinsically focused, while the 5th R (Resiliency) is intrinsic. Our theory posits that, if you attain the first 4 Rs in every interaction, these will serve to build on and develop your own personal resiliency. Here are the 5 Rs:
- Reflection – Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Respect – Hospitalists will treat every person with the utmost respect and strive to preserve dignity at all times.
- Regard – Hospitalists will hold every person in their highest regard while being aware of and not allowing unconscious biases to interfere in any interactions.
- Relevance – Hospitalists will expect cultural humility to be relevant to the patient and apply this practice to every encounter.
- Resiliency – Hospitalists will embody the practice of cultural humility to enhance personal resilience and globally focused compassion.
The content will be available as a downloadable pocket card that can be easily referenced on rounds and shared with colleagues. Our hope is to achieve heightened awareness of effective interaction. In addition to the definitions of each of the Rs, the card will feature questions to ask yourself before, during, and after every interaction to aid in attaining cultural humility.
The card will be printed and disseminated at Hospital Medicine 2017, and the 5 Rs will be discussed in a few sessions: “Making ‘Everything We Say and Do’ a Positive Patient Experience” in the Practice Management track on Thursday, May 4, and during a 20-minute “MEDtalk” in Product Theater 1 on May 3, at 10:15 a.m.
Keep on the lookout for future blog posts, where you’ll read about the 5 R’s in action through vignettes and a deeper dive into each aspect.
For more information and the downloadable pocket card, visit www.hospitalmedicine.org/5Rs.
Dr. Ansari is associate professor and associate division director of hospital medicine at Loyola University Medical Center, Maywood, Ill., and serves on SHM’s Cultural Humility Work Group.
How do we, as hospitalists, win the hearts and minds of patients, families, and care team members whom we do not know? What are the obstacles that we face when encountering patients and gaining the trust needed to improve patient care and patient experience?
With these questions in mind, the Cultural Humility Work Group, part of SHM’s Practice Management Committee, set out to develop a simple, universal framework to provide a foundation for strengthening communication skills and raising awareness of the basic tenets of cultural humility. According to Tervalon and Murray-Garcia, cultural humility is defined as a “process that requires humility as individuals continually engage in self-reflection and self-critique as lifelong learners and reflective practitioners. It requires humility in how physicians bring into check the power imbalances that exist in the dynamics of physician-patient communication by using patient-focused interviewing and care, and it is a process that requires humility to develop and maintain mutually respectful and dynamic partnerships with communities” (Tervalon, M. & Murray-García, J. “Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education.” J Health Care Poor Underserved. 1998;9[2]:117-25).
How do we win this battle? The first step is to simply be aware that everyone is a victim of unconscious biases. Once we come to this (often uncomfortable) realization, we must make a conscious effort to change our mindset and make conscious decisions to not allow these biases to manifest.
Practicing cultural humility is extremely important in this process. It puts everyone on the same platform because there is no “minority,” “majority,” or “ethnicity” associated with it. It takes away the need to know everything about a certain culture and encourages us to approach every patient encounter acknowledging that we will humble ourselves, learn what is important to the patient, and leave having learned something from the interaction.
The work group developed “The 5 Rs of Cultural Humility” as a simple tool for hospitalists to incorporate into their practice. The first four Rs (Reflection, Respect, Regard and Relevance) are extrinsically focused, while the 5th R (Resiliency) is intrinsic. Our theory posits that, if you attain the first 4 Rs in every interaction, these will serve to build on and develop your own personal resiliency. Here are the 5 Rs:
- Reflection – Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Respect – Hospitalists will treat every person with the utmost respect and strive to preserve dignity at all times.
- Regard – Hospitalists will hold every person in their highest regard while being aware of and not allowing unconscious biases to interfere in any interactions.
- Relevance – Hospitalists will expect cultural humility to be relevant to the patient and apply this practice to every encounter.
- Resiliency – Hospitalists will embody the practice of cultural humility to enhance personal resilience and globally focused compassion.
The content will be available as a downloadable pocket card that can be easily referenced on rounds and shared with colleagues. Our hope is to achieve heightened awareness of effective interaction. In addition to the definitions of each of the Rs, the card will feature questions to ask yourself before, during, and after every interaction to aid in attaining cultural humility.
The card will be printed and disseminated at Hospital Medicine 2017, and the 5 Rs will be discussed in a few sessions: “Making ‘Everything We Say and Do’ a Positive Patient Experience” in the Practice Management track on Thursday, May 4, and during a 20-minute “MEDtalk” in Product Theater 1 on May 3, at 10:15 a.m.
Keep on the lookout for future blog posts, where you’ll read about the 5 R’s in action through vignettes and a deeper dive into each aspect.
For more information and the downloadable pocket card, visit www.hospitalmedicine.org/5Rs.
Dr. Ansari is associate professor and associate division director of hospital medicine at Loyola University Medical Center, Maywood, Ill., and serves on SHM’s Cultural Humility Work Group.
How do we, as hospitalists, win the hearts and minds of patients, families, and care team members whom we do not know? What are the obstacles that we face when encountering patients and gaining the trust needed to improve patient care and patient experience?
With these questions in mind, the Cultural Humility Work Group, part of SHM’s Practice Management Committee, set out to develop a simple, universal framework to provide a foundation for strengthening communication skills and raising awareness of the basic tenets of cultural humility. According to Tervalon and Murray-Garcia, cultural humility is defined as a “process that requires humility as individuals continually engage in self-reflection and self-critique as lifelong learners and reflective practitioners. It requires humility in how physicians bring into check the power imbalances that exist in the dynamics of physician-patient communication by using patient-focused interviewing and care, and it is a process that requires humility to develop and maintain mutually respectful and dynamic partnerships with communities” (Tervalon, M. & Murray-García, J. “Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education.” J Health Care Poor Underserved. 1998;9[2]:117-25).
How do we win this battle? The first step is to simply be aware that everyone is a victim of unconscious biases. Once we come to this (often uncomfortable) realization, we must make a conscious effort to change our mindset and make conscious decisions to not allow these biases to manifest.
Practicing cultural humility is extremely important in this process. It puts everyone on the same platform because there is no “minority,” “majority,” or “ethnicity” associated with it. It takes away the need to know everything about a certain culture and encourages us to approach every patient encounter acknowledging that we will humble ourselves, learn what is important to the patient, and leave having learned something from the interaction.
The work group developed “The 5 Rs of Cultural Humility” as a simple tool for hospitalists to incorporate into their practice. The first four Rs (Reflection, Respect, Regard and Relevance) are extrinsically focused, while the 5th R (Resiliency) is intrinsic. Our theory posits that, if you attain the first 4 Rs in every interaction, these will serve to build on and develop your own personal resiliency. Here are the 5 Rs:
- Reflection – Hospitalists will approach every encounter with humility and understanding that there is always something to learn from everyone.
- Respect – Hospitalists will treat every person with the utmost respect and strive to preserve dignity at all times.
- Regard – Hospitalists will hold every person in their highest regard while being aware of and not allowing unconscious biases to interfere in any interactions.
- Relevance – Hospitalists will expect cultural humility to be relevant to the patient and apply this practice to every encounter.
- Resiliency – Hospitalists will embody the practice of cultural humility to enhance personal resilience and globally focused compassion.
The content will be available as a downloadable pocket card that can be easily referenced on rounds and shared with colleagues. Our hope is to achieve heightened awareness of effective interaction. In addition to the definitions of each of the Rs, the card will feature questions to ask yourself before, during, and after every interaction to aid in attaining cultural humility.
The card will be printed and disseminated at Hospital Medicine 2017, and the 5 Rs will be discussed in a few sessions: “Making ‘Everything We Say and Do’ a Positive Patient Experience” in the Practice Management track on Thursday, May 4, and during a 20-minute “MEDtalk” in Product Theater 1 on May 3, at 10:15 a.m.
Keep on the lookout for future blog posts, where you’ll read about the 5 R’s in action through vignettes and a deeper dive into each aspect.
For more information and the downloadable pocket card, visit www.hospitalmedicine.org/5Rs.
Dr. Ansari is associate professor and associate division director of hospital medicine at Loyola University Medical Center, Maywood, Ill., and serves on SHM’s Cultural Humility Work Group.
SHM receives Eisenberg Award as part of I-PASS Study Group
The Society of Hospital Medicine is part of a patient safety research group that received the prestigious 2016 John M. Eisenberg Award for Innovation in Patient Safety and Quality presented annually by The Joint Commission and the National Quality Forum, two leading organizations that set standards in patient care as part of the I-PASS Study Group.
I-PASS comprises a suite of educational materials and interventions dedicated to improving patient safety by reducing miscommunication during patient handoffs that can lead to harmful medical errors. The team in SHM’s Center for Quality Improvement has been instrumental in supporting the I-PASS Study Group, which represents more than 50 hospitals from across North America.
“The Eisenberg Award for Innovation represents the highest patient safety and quality award in the country, and we are honored to be recognized for our role in this important program,” said Jenna Goldstein, director of SHM’s Center for Quality Improvement. “Our team’s participation in developing and sustaining the SHM I-PASS mentored implementation demonstrates our commitment to ensure safe and high-quality care for hospitalized patients.”
SHM previously won the 2011 Eisenberg Award at the national level for its mentored implementation program model. Through its mentored implementation framework and project management, SHM has supported the I-PASS program across the country at 32 hospitals of varying types, including pediatric and adult hospitals, academic medical centers, and community-based hospitals. SHM has offered both an I-PASS mentored implementation program, in which a physician mentor coaches hospital team members on evidence-based best practices in process improvement and culture change for safe patient handoffs, and an implementation guide, which contains strategies and tools needed to lead the quality improvement effort in the hospital.
In a large multicenter study published in the New England Journal of Medicine, implementation of I-PASS was associated with a 30% reduction in medical errors that harm patients. An estimated 80% of the most serious medical errors can be linked to communication failures, particularly during patient handoffs.
In addition to its work with I-PASS, SHM’s Center for Quality Improvement plays a prominent role in developing tools that empower clinicians to lead quality improvement efforts in their institutions.
Brett Radler is SHM’s communications specialist.
The Society of Hospital Medicine is part of a patient safety research group that received the prestigious 2016 John M. Eisenberg Award for Innovation in Patient Safety and Quality presented annually by The Joint Commission and the National Quality Forum, two leading organizations that set standards in patient care as part of the I-PASS Study Group.
I-PASS comprises a suite of educational materials and interventions dedicated to improving patient safety by reducing miscommunication during patient handoffs that can lead to harmful medical errors. The team in SHM’s Center for Quality Improvement has been instrumental in supporting the I-PASS Study Group, which represents more than 50 hospitals from across North America.
“The Eisenberg Award for Innovation represents the highest patient safety and quality award in the country, and we are honored to be recognized for our role in this important program,” said Jenna Goldstein, director of SHM’s Center for Quality Improvement. “Our team’s participation in developing and sustaining the SHM I-PASS mentored implementation demonstrates our commitment to ensure safe and high-quality care for hospitalized patients.”
SHM previously won the 2011 Eisenberg Award at the national level for its mentored implementation program model. Through its mentored implementation framework and project management, SHM has supported the I-PASS program across the country at 32 hospitals of varying types, including pediatric and adult hospitals, academic medical centers, and community-based hospitals. SHM has offered both an I-PASS mentored implementation program, in which a physician mentor coaches hospital team members on evidence-based best practices in process improvement and culture change for safe patient handoffs, and an implementation guide, which contains strategies and tools needed to lead the quality improvement effort in the hospital.
In a large multicenter study published in the New England Journal of Medicine, implementation of I-PASS was associated with a 30% reduction in medical errors that harm patients. An estimated 80% of the most serious medical errors can be linked to communication failures, particularly during patient handoffs.
In addition to its work with I-PASS, SHM’s Center for Quality Improvement plays a prominent role in developing tools that empower clinicians to lead quality improvement efforts in their institutions.
Brett Radler is SHM’s communications specialist.
The Society of Hospital Medicine is part of a patient safety research group that received the prestigious 2016 John M. Eisenberg Award for Innovation in Patient Safety and Quality presented annually by The Joint Commission and the National Quality Forum, two leading organizations that set standards in patient care as part of the I-PASS Study Group.
I-PASS comprises a suite of educational materials and interventions dedicated to improving patient safety by reducing miscommunication during patient handoffs that can lead to harmful medical errors. The team in SHM’s Center for Quality Improvement has been instrumental in supporting the I-PASS Study Group, which represents more than 50 hospitals from across North America.
“The Eisenberg Award for Innovation represents the highest patient safety and quality award in the country, and we are honored to be recognized for our role in this important program,” said Jenna Goldstein, director of SHM’s Center for Quality Improvement. “Our team’s participation in developing and sustaining the SHM I-PASS mentored implementation demonstrates our commitment to ensure safe and high-quality care for hospitalized patients.”
SHM previously won the 2011 Eisenberg Award at the national level for its mentored implementation program model. Through its mentored implementation framework and project management, SHM has supported the I-PASS program across the country at 32 hospitals of varying types, including pediatric and adult hospitals, academic medical centers, and community-based hospitals. SHM has offered both an I-PASS mentored implementation program, in which a physician mentor coaches hospital team members on evidence-based best practices in process improvement and culture change for safe patient handoffs, and an implementation guide, which contains strategies and tools needed to lead the quality improvement effort in the hospital.
In a large multicenter study published in the New England Journal of Medicine, implementation of I-PASS was associated with a 30% reduction in medical errors that harm patients. An estimated 80% of the most serious medical errors can be linked to communication failures, particularly during patient handoffs.
In addition to its work with I-PASS, SHM’s Center for Quality Improvement plays a prominent role in developing tools that empower clinicians to lead quality improvement efforts in their institutions.
Brett Radler is SHM’s communications specialist.
How’s your postacute network doing?
By now, nearly all hospitals are developing networks of postacute facilities for some or all of their patients, such as those in ACOs, bundled payments, or other value-based programs. Commonly referred to as preferred providers, performance networks, narrow networks, or similar, these networks of skilled nursing facilities (SNFs) and other entities that provide postacute care (like home health agencies) are usually chosen because they have demonstrated that they provide high quality, cost-effective care for patients after they leave the hospital.
While case managers are often the ones who counsel patients and caregivers on the details of the network, hospitalists should have at least a high-level grasp of which facilities are on the list and what the network selection criteria are. I would argue that hospitalists should lead the discussion with patients on postacute facility selection as it relates to which facilities are in the network and why going to a network facility is advantageous. Why? Because as hospitalist practices begin to share clinical and financial risk for patients, or at least become eligible to share in savings as MACRA encourages, they will have a vested interest in network facilities’ performance.
Postacute care network selection criteria
There is a range of criteria – usually incorporating measures of quality and efficiency – for including providers like SNFs in networks. In terms of quality, criteria can include physician/provider availability, star ratings on Nursing Home Compare, care transitions measures, Department of Public Health inspection survey scores, Joint Commission accreditation, etc.
A few caveats regarding specific selection criteria:
Star ratings on Nursing Home Compare
These are derived from nursing staffing ratios, health inspections, and 16 quality measures. More than half of the quality measures pertain to long-stay residents who typically are not in the ACO or bundled payment program for which the network was created (these are usually short-stay patients).
SNF length of stay
High readmission rates from a SNF can actually lower its length of stay, so including “balancing” measures such as readmissions should be considered.
What about patient choice?
Narrow postacute networks are not only becoming the norm, but there is also broad recognition from CMS, MedPAC, and industry leaders that value-based payment programs require such networks to succeed. That said, case managers and other discharge planners may still resist networks on the grounds that they might be perceived as restricting patient choice. One approach to balancing differing views on patient choice is to give patients the traditional longer list of available postacute providers, and also furnish the shorter network list accompanied by an explanation of why certain SNFs are in the network. Thankfully, as ACOs and bundles become widespread, resistance to narrow networks is dying down.
What role should hospitalists play in network referrals?
High functioning hospitalist practices should lead the discussion with patients and the health care team on referrals to network SNFs. Why? Patients are looking for their doctors to guide them on such decisions. Only if the physician opts not to have the discussion will patients look to the case manager for direction on which postacute facility to choose. A better option still would be for the hospitalists to partner with case managers to have the conversation with patients. In such a scenario, the hospitalist can begin the discussion and cover the major points, and the case manager can follow with more detailed information. For less mature hospitalist practices, the case manager can play a larger role in the discussion. In any case, as value-based models become ubiquitous, and shared savings become a driver of hospitalist revenue, hospitalists’ knowledge of and active participation in conversations around narrow networks and referrals will be necessary.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn. He is a cofounder and past president of SHM.
By now, nearly all hospitals are developing networks of postacute facilities for some or all of their patients, such as those in ACOs, bundled payments, or other value-based programs. Commonly referred to as preferred providers, performance networks, narrow networks, or similar, these networks of skilled nursing facilities (SNFs) and other entities that provide postacute care (like home health agencies) are usually chosen because they have demonstrated that they provide high quality, cost-effective care for patients after they leave the hospital.
While case managers are often the ones who counsel patients and caregivers on the details of the network, hospitalists should have at least a high-level grasp of which facilities are on the list and what the network selection criteria are. I would argue that hospitalists should lead the discussion with patients on postacute facility selection as it relates to which facilities are in the network and why going to a network facility is advantageous. Why? Because as hospitalist practices begin to share clinical and financial risk for patients, or at least become eligible to share in savings as MACRA encourages, they will have a vested interest in network facilities’ performance.
Postacute care network selection criteria
There is a range of criteria – usually incorporating measures of quality and efficiency – for including providers like SNFs in networks. In terms of quality, criteria can include physician/provider availability, star ratings on Nursing Home Compare, care transitions measures, Department of Public Health inspection survey scores, Joint Commission accreditation, etc.
A few caveats regarding specific selection criteria:
Star ratings on Nursing Home Compare
These are derived from nursing staffing ratios, health inspections, and 16 quality measures. More than half of the quality measures pertain to long-stay residents who typically are not in the ACO or bundled payment program for which the network was created (these are usually short-stay patients).
SNF length of stay
High readmission rates from a SNF can actually lower its length of stay, so including “balancing” measures such as readmissions should be considered.
What about patient choice?
Narrow postacute networks are not only becoming the norm, but there is also broad recognition from CMS, MedPAC, and industry leaders that value-based payment programs require such networks to succeed. That said, case managers and other discharge planners may still resist networks on the grounds that they might be perceived as restricting patient choice. One approach to balancing differing views on patient choice is to give patients the traditional longer list of available postacute providers, and also furnish the shorter network list accompanied by an explanation of why certain SNFs are in the network. Thankfully, as ACOs and bundles become widespread, resistance to narrow networks is dying down.
What role should hospitalists play in network referrals?
High functioning hospitalist practices should lead the discussion with patients and the health care team on referrals to network SNFs. Why? Patients are looking for their doctors to guide them on such decisions. Only if the physician opts not to have the discussion will patients look to the case manager for direction on which postacute facility to choose. A better option still would be for the hospitalists to partner with case managers to have the conversation with patients. In such a scenario, the hospitalist can begin the discussion and cover the major points, and the case manager can follow with more detailed information. For less mature hospitalist practices, the case manager can play a larger role in the discussion. In any case, as value-based models become ubiquitous, and shared savings become a driver of hospitalist revenue, hospitalists’ knowledge of and active participation in conversations around narrow networks and referrals will be necessary.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn. He is a cofounder and past president of SHM.
By now, nearly all hospitals are developing networks of postacute facilities for some or all of their patients, such as those in ACOs, bundled payments, or other value-based programs. Commonly referred to as preferred providers, performance networks, narrow networks, or similar, these networks of skilled nursing facilities (SNFs) and other entities that provide postacute care (like home health agencies) are usually chosen because they have demonstrated that they provide high quality, cost-effective care for patients after they leave the hospital.
While case managers are often the ones who counsel patients and caregivers on the details of the network, hospitalists should have at least a high-level grasp of which facilities are on the list and what the network selection criteria are. I would argue that hospitalists should lead the discussion with patients on postacute facility selection as it relates to which facilities are in the network and why going to a network facility is advantageous. Why? Because as hospitalist practices begin to share clinical and financial risk for patients, or at least become eligible to share in savings as MACRA encourages, they will have a vested interest in network facilities’ performance.
Postacute care network selection criteria
There is a range of criteria – usually incorporating measures of quality and efficiency – for including providers like SNFs in networks. In terms of quality, criteria can include physician/provider availability, star ratings on Nursing Home Compare, care transitions measures, Department of Public Health inspection survey scores, Joint Commission accreditation, etc.
A few caveats regarding specific selection criteria:
Star ratings on Nursing Home Compare
These are derived from nursing staffing ratios, health inspections, and 16 quality measures. More than half of the quality measures pertain to long-stay residents who typically are not in the ACO or bundled payment program for which the network was created (these are usually short-stay patients).
SNF length of stay
High readmission rates from a SNF can actually lower its length of stay, so including “balancing” measures such as readmissions should be considered.
What about patient choice?
Narrow postacute networks are not only becoming the norm, but there is also broad recognition from CMS, MedPAC, and industry leaders that value-based payment programs require such networks to succeed. That said, case managers and other discharge planners may still resist networks on the grounds that they might be perceived as restricting patient choice. One approach to balancing differing views on patient choice is to give patients the traditional longer list of available postacute providers, and also furnish the shorter network list accompanied by an explanation of why certain SNFs are in the network. Thankfully, as ACOs and bundles become widespread, resistance to narrow networks is dying down.
What role should hospitalists play in network referrals?
High functioning hospitalist practices should lead the discussion with patients and the health care team on referrals to network SNFs. Why? Patients are looking for their doctors to guide them on such decisions. Only if the physician opts not to have the discussion will patients look to the case manager for direction on which postacute facility to choose. A better option still would be for the hospitalists to partner with case managers to have the conversation with patients. In such a scenario, the hospitalist can begin the discussion and cover the major points, and the case manager can follow with more detailed information. For less mature hospitalist practices, the case manager can play a larger role in the discussion. In any case, as value-based models become ubiquitous, and shared savings become a driver of hospitalist revenue, hospitalists’ knowledge of and active participation in conversations around narrow networks and referrals will be necessary.
Dr. Whitcomb is chief medical officer at Remedy Partners in Darien, Conn. He is a cofounder and past president of SHM.
QI enthusiast turns QI leader
Editor’s note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Kevin O’Leary, MD, MS, SFHM, chief of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago.
Kevin O’Leary, MD, MS, SFHM, chose a career path in hospital medicine for the reasons that attract many to the specialty – a love of “a little bit of everything, clinically” and the opportunity to problem-solve a diverse range of professional challenges on a daily basis.
“I was frustrated with our internal inefficiencies, and motivated by wanting to provide optimal care to patients,” Dr. O’Leary said, recalling his entry into the world of quality improvement. “It was the first time as a physician that I felt like quality was a problem that I owned – and if anyone was going to address it, it would have to be a hospitalist.”
That epiphany 16 years ago led Dr. O’Leary, now chief of hospital medicine at the same institution, on a path of enacting change. He began volunteering on small improvement projects around the hospital, which led to an invitation to chair the Quality Management Committee in the hospital medicine department. He continued to build his skills by enrolling in Six Sigma training and in Northwestern University’s Master in Healthcare Quality and Patient Safety program.
“That was transformative,” Dr. O’Leary said. “The master’s program, coupled with performance training, changed the trajectory of my career in quality improvement.”
While he encourages anyone with an interest in QI to seek additional training opportunities, he says personal qualities – tenacity, curiosity, and a willingness to collaborate—are better predictors of success. For those wondering how to get started, “look for a niche, an unmet need that is valuable to your organization, and fill it,” he advised. “You don’t have to be an expert in that area, but you can become one.”
Making strong connections within the hospital system is essential. Reach out to the contacts you know, he said, and if they are not the ones to help you solve the problem, they often know who can.
“That’s key to quality improvement success, as well as career success,” he said. “Find a mentor. It might be someone who is more senior within the hospitalist group, in medicine, or even outside the hospital. Meet with them regularly and ask them for feedback on your ideas.”
Newcomers to QI should embrace opportunities to change care and not get discouraged when a project has unintended outcomes.
“Failure is when a team never gets to the point of implementing the intervention or when a team doesn’t know whether the intervention has actually changed results,” he said. “Learning why an intervention isn’t effective can be as valuable as implementing one that is. If every project is successful, it just means that you’re not taking enough risks.”
Dr. O’Leary spends about 25% of his professional time providing clinical care, and another 15% meeting his responsibilities as division chief. He uses the other protected time in his schedule to lead QI and teach QI skills in programs like Northwestern Medicine’s Academy for Quality and Safety Improvement (AQSI).
As a former faculty member in SHM’s Quality and Safety Educator’s Academy (QSEA), he has trained medical educators to develop curricula in quality improvement and patient safety. He says both AQSI and QSEA are especially effective because they encourage interaction, which is valuable to professionals at all levels looking to advance their skill in QI.
“Even in a teaching capacity,” he noted, “what I learned from other faculty and participants in QSEA was critical.”
Residents and junior hospitalists often have the impression that they lack the skills to lead quality initiatives, but Dr. O’Leary says medical school provides the nuts and bolts – analytical skills, statistical knowledge, critical thinking. He encouraged hospitalists to move ahead, even without formal QI training.
“If you have strong interpersonal skills – the willingness to make friends and build connections – you will be successful,” he said.
It’s also an excellent way to learn about the ins and outs of the hospital system and the work of other departments and specialties. Dr. O’Leary especially enjoys that aspect of his work, as well as the ability to address systemic issues that he values.
“I get the greatest fulfillment from the opportunity to be creative … and to implement projects that are important to me and help patients,” he said. “As long as the projects align with organizational goals, I can usually find the support we need to be successful.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Kevin O’Leary, MD, MS, SFHM, chief of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago.
Kevin O’Leary, MD, MS, SFHM, chose a career path in hospital medicine for the reasons that attract many to the specialty – a love of “a little bit of everything, clinically” and the opportunity to problem-solve a diverse range of professional challenges on a daily basis.
“I was frustrated with our internal inefficiencies, and motivated by wanting to provide optimal care to patients,” Dr. O’Leary said, recalling his entry into the world of quality improvement. “It was the first time as a physician that I felt like quality was a problem that I owned – and if anyone was going to address it, it would have to be a hospitalist.”
That epiphany 16 years ago led Dr. O’Leary, now chief of hospital medicine at the same institution, on a path of enacting change. He began volunteering on small improvement projects around the hospital, which led to an invitation to chair the Quality Management Committee in the hospital medicine department. He continued to build his skills by enrolling in Six Sigma training and in Northwestern University’s Master in Healthcare Quality and Patient Safety program.
“That was transformative,” Dr. O’Leary said. “The master’s program, coupled with performance training, changed the trajectory of my career in quality improvement.”
While he encourages anyone with an interest in QI to seek additional training opportunities, he says personal qualities – tenacity, curiosity, and a willingness to collaborate—are better predictors of success. For those wondering how to get started, “look for a niche, an unmet need that is valuable to your organization, and fill it,” he advised. “You don’t have to be an expert in that area, but you can become one.”
Making strong connections within the hospital system is essential. Reach out to the contacts you know, he said, and if they are not the ones to help you solve the problem, they often know who can.
“That’s key to quality improvement success, as well as career success,” he said. “Find a mentor. It might be someone who is more senior within the hospitalist group, in medicine, or even outside the hospital. Meet with them regularly and ask them for feedback on your ideas.”
Newcomers to QI should embrace opportunities to change care and not get discouraged when a project has unintended outcomes.
“Failure is when a team never gets to the point of implementing the intervention or when a team doesn’t know whether the intervention has actually changed results,” he said. “Learning why an intervention isn’t effective can be as valuable as implementing one that is. If every project is successful, it just means that you’re not taking enough risks.”
Dr. O’Leary spends about 25% of his professional time providing clinical care, and another 15% meeting his responsibilities as division chief. He uses the other protected time in his schedule to lead QI and teach QI skills in programs like Northwestern Medicine’s Academy for Quality and Safety Improvement (AQSI).
As a former faculty member in SHM’s Quality and Safety Educator’s Academy (QSEA), he has trained medical educators to develop curricula in quality improvement and patient safety. He says both AQSI and QSEA are especially effective because they encourage interaction, which is valuable to professionals at all levels looking to advance their skill in QI.
“Even in a teaching capacity,” he noted, “what I learned from other faculty and participants in QSEA was critical.”
Residents and junior hospitalists often have the impression that they lack the skills to lead quality initiatives, but Dr. O’Leary says medical school provides the nuts and bolts – analytical skills, statistical knowledge, critical thinking. He encouraged hospitalists to move ahead, even without formal QI training.
“If you have strong interpersonal skills – the willingness to make friends and build connections – you will be successful,” he said.
It’s also an excellent way to learn about the ins and outs of the hospital system and the work of other departments and specialties. Dr. O’Leary especially enjoys that aspect of his work, as well as the ability to address systemic issues that he values.
“I get the greatest fulfillment from the opportunity to be creative … and to implement projects that are important to me and help patients,” he said. “As long as the projects align with organizational goals, I can usually find the support we need to be successful.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Editor’s note: This new series highlights the professional pathways of quality improvement leaders. This month features the story of Kevin O’Leary, MD, MS, SFHM, chief of hospital medicine at Northwestern University Feinberg School of Medicine in Chicago.
Kevin O’Leary, MD, MS, SFHM, chose a career path in hospital medicine for the reasons that attract many to the specialty – a love of “a little bit of everything, clinically” and the opportunity to problem-solve a diverse range of professional challenges on a daily basis.
“I was frustrated with our internal inefficiencies, and motivated by wanting to provide optimal care to patients,” Dr. O’Leary said, recalling his entry into the world of quality improvement. “It was the first time as a physician that I felt like quality was a problem that I owned – and if anyone was going to address it, it would have to be a hospitalist.”
That epiphany 16 years ago led Dr. O’Leary, now chief of hospital medicine at the same institution, on a path of enacting change. He began volunteering on small improvement projects around the hospital, which led to an invitation to chair the Quality Management Committee in the hospital medicine department. He continued to build his skills by enrolling in Six Sigma training and in Northwestern University’s Master in Healthcare Quality and Patient Safety program.
“That was transformative,” Dr. O’Leary said. “The master’s program, coupled with performance training, changed the trajectory of my career in quality improvement.”
While he encourages anyone with an interest in QI to seek additional training opportunities, he says personal qualities – tenacity, curiosity, and a willingness to collaborate—are better predictors of success. For those wondering how to get started, “look for a niche, an unmet need that is valuable to your organization, and fill it,” he advised. “You don’t have to be an expert in that area, but you can become one.”
Making strong connections within the hospital system is essential. Reach out to the contacts you know, he said, and if they are not the ones to help you solve the problem, they often know who can.
“That’s key to quality improvement success, as well as career success,” he said. “Find a mentor. It might be someone who is more senior within the hospitalist group, in medicine, or even outside the hospital. Meet with them regularly and ask them for feedback on your ideas.”
Newcomers to QI should embrace opportunities to change care and not get discouraged when a project has unintended outcomes.
“Failure is when a team never gets to the point of implementing the intervention or when a team doesn’t know whether the intervention has actually changed results,” he said. “Learning why an intervention isn’t effective can be as valuable as implementing one that is. If every project is successful, it just means that you’re not taking enough risks.”
Dr. O’Leary spends about 25% of his professional time providing clinical care, and another 15% meeting his responsibilities as division chief. He uses the other protected time in his schedule to lead QI and teach QI skills in programs like Northwestern Medicine’s Academy for Quality and Safety Improvement (AQSI).
As a former faculty member in SHM’s Quality and Safety Educator’s Academy (QSEA), he has trained medical educators to develop curricula in quality improvement and patient safety. He says both AQSI and QSEA are especially effective because they encourage interaction, which is valuable to professionals at all levels looking to advance their skill in QI.
“Even in a teaching capacity,” he noted, “what I learned from other faculty and participants in QSEA was critical.”
Residents and junior hospitalists often have the impression that they lack the skills to lead quality initiatives, but Dr. O’Leary says medical school provides the nuts and bolts – analytical skills, statistical knowledge, critical thinking. He encouraged hospitalists to move ahead, even without formal QI training.
“If you have strong interpersonal skills – the willingness to make friends and build connections – you will be successful,” he said.
It’s also an excellent way to learn about the ins and outs of the hospital system and the work of other departments and specialties. Dr. O’Leary especially enjoys that aspect of his work, as well as the ability to address systemic issues that he values.
“I get the greatest fulfillment from the opportunity to be creative … and to implement projects that are important to me and help patients,” he said. “As long as the projects align with organizational goals, I can usually find the support we need to be successful.”
Claudia Stahl is a content manager for the Society of Hospital Medicine.
Consider apps for better patient health
Hospitalists should not overlook apps as tools for better health: Smartphone ownership is rising among all demographic groups, and more than 165,000 health apps exist in app stores. Many apps are aimed at helping caregivers and patients with complex medical conditions.
“Patient-facing mobile health applications (mHealth apps) – those intended for use by patients to manage their health – have the potential to help high-need, high-cost populations manage their health, but a variety of questions related to their utility and function have not previously been explored,” Karandeep Singh, MD, MMSc, said in “Many Mobile Health Apps Target High-Need, High-Cost Populations, But Gaps Remain.”1
- How well do apps serve the needs of patients with varying levels of engagement with their health?
- Can we infer an app’s clinical utility or usability based on its app store rating?
- Do apps appropriately respond to information entered by the user indicating that he or she might be in danger?
- How well do apps protect the privacy and security of user-entered health data?
- Are app costs a barrier to patients’ purchasing and using them?
- The study team found a variety of apps for patients with chronic conditions.
“While many apps allow users to track health information, most apps did not respond appropriately when a user entered potentially dangerous health information,” Dr. Singh says. “Consumers’ ratings of apps on the iOS and Android app stores were poor indications of the apps’ clinical utility or usability. Finally, we found that many apps enable sharing of information with others but primarily through insecure means. This is especially problematic because just under two-thirds of apps we evaluated had a privacy policy.”
He cautions hospitalists that app ratings may have little bearing on its clinical utility as judged by a physician.
“Additionally, for patients tracking health findings using apps during an inpatient stay, the most secure way of sharing this information is the old-fashioned way, in person or in print,” he explains. “Unlike hospital-based health information systems, health data stored in apps is generally not regulated by HIPAA. Hospitalists should not assume that a ‘secure messaging’ system provided by a patient-facing app is actually secure.”
The American Medical Association, American Heart Association, Healthcare Information and Management Systems Society, and digital health nonprofit DHX Group are the founders of the new guideline-writing organization called Xcertia. Xcertia will provide guidance for developing, evaluating, or recommending mHealth apps.
“I hope that hospitalists keenly interested in apps will take an active role in Xcertia, to ensure that their voices are heard in what looks to be an unprecedented large-scale effort in the United States,” Dr. Singh says. “While a medication list printed on a discharge summary cannot remind patients to take their meds, apps can do this quite well.”
Reference
1. Singh, K, Drouin, K, Newmark, L, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Affairs. 2016;35(12):2310-8.
Hospitalists should not overlook apps as tools for better health: Smartphone ownership is rising among all demographic groups, and more than 165,000 health apps exist in app stores. Many apps are aimed at helping caregivers and patients with complex medical conditions.
“Patient-facing mobile health applications (mHealth apps) – those intended for use by patients to manage their health – have the potential to help high-need, high-cost populations manage their health, but a variety of questions related to their utility and function have not previously been explored,” Karandeep Singh, MD, MMSc, said in “Many Mobile Health Apps Target High-Need, High-Cost Populations, But Gaps Remain.”1
- How well do apps serve the needs of patients with varying levels of engagement with their health?
- Can we infer an app’s clinical utility or usability based on its app store rating?
- Do apps appropriately respond to information entered by the user indicating that he or she might be in danger?
- How well do apps protect the privacy and security of user-entered health data?
- Are app costs a barrier to patients’ purchasing and using them?
- The study team found a variety of apps for patients with chronic conditions.
“While many apps allow users to track health information, most apps did not respond appropriately when a user entered potentially dangerous health information,” Dr. Singh says. “Consumers’ ratings of apps on the iOS and Android app stores were poor indications of the apps’ clinical utility or usability. Finally, we found that many apps enable sharing of information with others but primarily through insecure means. This is especially problematic because just under two-thirds of apps we evaluated had a privacy policy.”
He cautions hospitalists that app ratings may have little bearing on its clinical utility as judged by a physician.
“Additionally, for patients tracking health findings using apps during an inpatient stay, the most secure way of sharing this information is the old-fashioned way, in person or in print,” he explains. “Unlike hospital-based health information systems, health data stored in apps is generally not regulated by HIPAA. Hospitalists should not assume that a ‘secure messaging’ system provided by a patient-facing app is actually secure.”
The American Medical Association, American Heart Association, Healthcare Information and Management Systems Society, and digital health nonprofit DHX Group are the founders of the new guideline-writing organization called Xcertia. Xcertia will provide guidance for developing, evaluating, or recommending mHealth apps.
“I hope that hospitalists keenly interested in apps will take an active role in Xcertia, to ensure that their voices are heard in what looks to be an unprecedented large-scale effort in the United States,” Dr. Singh says. “While a medication list printed on a discharge summary cannot remind patients to take their meds, apps can do this quite well.”
Reference
1. Singh, K, Drouin, K, Newmark, L, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Affairs. 2016;35(12):2310-8.
Hospitalists should not overlook apps as tools for better health: Smartphone ownership is rising among all demographic groups, and more than 165,000 health apps exist in app stores. Many apps are aimed at helping caregivers and patients with complex medical conditions.
“Patient-facing mobile health applications (mHealth apps) – those intended for use by patients to manage their health – have the potential to help high-need, high-cost populations manage their health, but a variety of questions related to their utility and function have not previously been explored,” Karandeep Singh, MD, MMSc, said in “Many Mobile Health Apps Target High-Need, High-Cost Populations, But Gaps Remain.”1
- How well do apps serve the needs of patients with varying levels of engagement with their health?
- Can we infer an app’s clinical utility or usability based on its app store rating?
- Do apps appropriately respond to information entered by the user indicating that he or she might be in danger?
- How well do apps protect the privacy and security of user-entered health data?
- Are app costs a barrier to patients’ purchasing and using them?
- The study team found a variety of apps for patients with chronic conditions.
“While many apps allow users to track health information, most apps did not respond appropriately when a user entered potentially dangerous health information,” Dr. Singh says. “Consumers’ ratings of apps on the iOS and Android app stores were poor indications of the apps’ clinical utility or usability. Finally, we found that many apps enable sharing of information with others but primarily through insecure means. This is especially problematic because just under two-thirds of apps we evaluated had a privacy policy.”
He cautions hospitalists that app ratings may have little bearing on its clinical utility as judged by a physician.
“Additionally, for patients tracking health findings using apps during an inpatient stay, the most secure way of sharing this information is the old-fashioned way, in person or in print,” he explains. “Unlike hospital-based health information systems, health data stored in apps is generally not regulated by HIPAA. Hospitalists should not assume that a ‘secure messaging’ system provided by a patient-facing app is actually secure.”
The American Medical Association, American Heart Association, Healthcare Information and Management Systems Society, and digital health nonprofit DHX Group are the founders of the new guideline-writing organization called Xcertia. Xcertia will provide guidance for developing, evaluating, or recommending mHealth apps.
“I hope that hospitalists keenly interested in apps will take an active role in Xcertia, to ensure that their voices are heard in what looks to be an unprecedented large-scale effort in the United States,” Dr. Singh says. “While a medication list printed on a discharge summary cannot remind patients to take their meds, apps can do this quite well.”
Reference
1. Singh, K, Drouin, K, Newmark, L, et al. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Affairs. 2016;35(12):2310-8.
Hospitalists seek tools for more efficient admissions
Moving patients safely and efficiently through the admission process is always a priority for hospitalists. Is there a way to optimize and standardize the process?
“In hopes of improving admission efficiency, while simultaneously increasing quality of care, we decided to use Lean/Six Sigma methodology to streamline our admission process,” says Escher Howard-Williams, MD, lead author of an abstract called “Standardizing the Admission Process Using Lean/Six Sigma One Piece Flow.”1
A basic tenet of the methodology is called “one piece flow” (OPF), the idea that standardized processes are more efficient and less prone to error when completed from start to finish without interruption. In the study, hospitalists committed to performing all patient admissions in OPF, focusing on one patient from initiation of chart review through exam, order entry and documentation, without interruption. Researchers then analyzed times, including time to call back to ED, time at initiation of chart review, time of evaluation of patient, time orders were placed, and time of sign-out note completed, before and after implementation of OPF. They found a substantial reduction in time of the admission process across all time points with OPF.
“When you are trying to improve quality of care in your institution, dissecting the overall work flow will allow you to discover areas that hinder the overall process,” Dr. Howard-Williams says. “Reframing your process to focus on providing excellent quality care will allow you to find workable solutions to improve the quality of care and efficiency in your practice. As part of this process, developing a team with an appropriate variety of members lays the foundation for success.”
Dr. Howard-Williams hopes that the study will inspire others to reflect on their own practices.
“If, during that reflection, they can identify areas that they would like to improve quality, we would encourage them to join us,” she says. “They will have the opportunity to build their personal work flow maps, find choke points and devise a plan for moving forward with new solutions.”
Reference
1. Howard-Williams E, Liles A, Stephens J, lanza-Kaduce K. Standardizing the admission process using Lean/Six Sigma One Piece Flow [abstract]. J Hosp Med. 2016;11(suppl 1). Available at: http://www.shmabstracts.com/abstract/standardizing-the-admission-process-using-lean-six-sigma-one-piece-flow/. Accessed March 7, 2017.
Moving patients safely and efficiently through the admission process is always a priority for hospitalists. Is there a way to optimize and standardize the process?
“In hopes of improving admission efficiency, while simultaneously increasing quality of care, we decided to use Lean/Six Sigma methodology to streamline our admission process,” says Escher Howard-Williams, MD, lead author of an abstract called “Standardizing the Admission Process Using Lean/Six Sigma One Piece Flow.”1
A basic tenet of the methodology is called “one piece flow” (OPF), the idea that standardized processes are more efficient and less prone to error when completed from start to finish without interruption. In the study, hospitalists committed to performing all patient admissions in OPF, focusing on one patient from initiation of chart review through exam, order entry and documentation, without interruption. Researchers then analyzed times, including time to call back to ED, time at initiation of chart review, time of evaluation of patient, time orders were placed, and time of sign-out note completed, before and after implementation of OPF. They found a substantial reduction in time of the admission process across all time points with OPF.
“When you are trying to improve quality of care in your institution, dissecting the overall work flow will allow you to discover areas that hinder the overall process,” Dr. Howard-Williams says. “Reframing your process to focus on providing excellent quality care will allow you to find workable solutions to improve the quality of care and efficiency in your practice. As part of this process, developing a team with an appropriate variety of members lays the foundation for success.”
Dr. Howard-Williams hopes that the study will inspire others to reflect on their own practices.
“If, during that reflection, they can identify areas that they would like to improve quality, we would encourage them to join us,” she says. “They will have the opportunity to build their personal work flow maps, find choke points and devise a plan for moving forward with new solutions.”
Reference
1. Howard-Williams E, Liles A, Stephens J, lanza-Kaduce K. Standardizing the admission process using Lean/Six Sigma One Piece Flow [abstract]. J Hosp Med. 2016;11(suppl 1). Available at: http://www.shmabstracts.com/abstract/standardizing-the-admission-process-using-lean-six-sigma-one-piece-flow/. Accessed March 7, 2017.
Moving patients safely and efficiently through the admission process is always a priority for hospitalists. Is there a way to optimize and standardize the process?
“In hopes of improving admission efficiency, while simultaneously increasing quality of care, we decided to use Lean/Six Sigma methodology to streamline our admission process,” says Escher Howard-Williams, MD, lead author of an abstract called “Standardizing the Admission Process Using Lean/Six Sigma One Piece Flow.”1
A basic tenet of the methodology is called “one piece flow” (OPF), the idea that standardized processes are more efficient and less prone to error when completed from start to finish without interruption. In the study, hospitalists committed to performing all patient admissions in OPF, focusing on one patient from initiation of chart review through exam, order entry and documentation, without interruption. Researchers then analyzed times, including time to call back to ED, time at initiation of chart review, time of evaluation of patient, time orders were placed, and time of sign-out note completed, before and after implementation of OPF. They found a substantial reduction in time of the admission process across all time points with OPF.
“When you are trying to improve quality of care in your institution, dissecting the overall work flow will allow you to discover areas that hinder the overall process,” Dr. Howard-Williams says. “Reframing your process to focus on providing excellent quality care will allow you to find workable solutions to improve the quality of care and efficiency in your practice. As part of this process, developing a team with an appropriate variety of members lays the foundation for success.”
Dr. Howard-Williams hopes that the study will inspire others to reflect on their own practices.
“If, during that reflection, they can identify areas that they would like to improve quality, we would encourage them to join us,” she says. “They will have the opportunity to build their personal work flow maps, find choke points and devise a plan for moving forward with new solutions.”
Reference
1. Howard-Williams E, Liles A, Stephens J, lanza-Kaduce K. Standardizing the admission process using Lean/Six Sigma One Piece Flow [abstract]. J Hosp Med. 2016;11(suppl 1). Available at: http://www.shmabstracts.com/abstract/standardizing-the-admission-process-using-lean-six-sigma-one-piece-flow/. Accessed March 7, 2017.