User login
Patient navigators’ personal experiences with cancer: does it have an impact on treatment?
Patient navigation has emerged in the past decade as a strategy to decrease cancer disparities among low-income, minority populations. Patient navigators help individuals who face personal and systemtic barriers to gaining access to care.1 Their role is to help patients find their way through a complex health care system,2,3 including logistic support of rescheduling appointments, assistance with transportation, and child care needs. They provide personal support, including coaching patients on their clinical visits, educating them about the cancer treatment process, and addressing their fears of diagnosis and treatment. Patient navigation has shown improvement in cancer screening rates, time to diagnostic resolution for those patients who have abnormal cancer screening tests, and quality of cancer care.4,5
In hiring patient navigators, it is not clear which professional training and skill sets and what personal experiences are most useful to becoming an effective navigator. Personal cancer experience can include a personal diagnosis, the experience of serving as a primary caregiver for a patient during treatment, or having a family member or close friend with cancer. Several current support programs specifically recruit cancer survivors on the assumption that their cancer treatment experience can provide helpful insights to a current patient for both emotional and logistical support.6 In this paper, we sought to address whether patient navigation promotes more timely diagnostic care if the navigator has experience with cancer.
Methods
This is a secondary analysis of the patients with abnormal cancer screening in the navigation arm of the national Patient Navigation Research Program (PNRP) study,1, 5 a collaborative effort across 10 centers to investigate the efficacy of patient navigation on improving patient-level outcomes for those who have abnormal results from a breast, cervical, colorectal, or prostate cancer screening test. The study demonstrated that patient navigation was effective in reducing delays in diagnosis and treatment5 and resulting in a higher quality of care,4 especially among vulnerable populations.7 The Institutional Review Board of each respective institution approved the research.
All of the patient navigators were paid employees with a minimum high-school diploma or equivalent. Navigators’ activities were standardized across centers through a national training program.8 Navigators used the care management model to identify and address barriers to care and to track participants throughout the course of their diagnostic evaluation,9 with the primary aim of timely diagnostic resolution. Most navigation programs were embedded within the clinical care system and interacted with patients through mail, by phone, and face-to-face contact.1
Data collection
Each center used agreed-upon inclusion and exclusion criteria and collected and coded the same patient-level data. Medical records were abstracted for pertinent clinical data on patients. Demographic data were collected through a patient survey or extracted from medical record registration. The central data coordinating center collected navigator information including demographic characteristics and experience with cancer.
We created a new variable, Personal experience with cancer. Personal experience with cancer was based on three questions asked of navigators: whether they were a cancer survivor; whether they were the primary caregiver to a family member or close friend with cancer; and whether they had a family member with cancer. Because of the small sample size, responses from navigators who were cancer survivors (n = 6) or primary caregivers to a family member with cancer (n = 4) were collapsed into a single category, referred to as personal experience with cancer, to compare with navigators who had no personal experience with cancer, which included those who reported a family member with cancer but who were not serving as a primary caregiver.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Each clinical center received approved from their institution’s human subjects review board. Informed consent was obtained from all patient navigator participants included in the study. Participating patients completed informed consent at some centers. At other centers where the study design was an implementation of a system intervention, a waiver of informed consent was approved by the Institutional Review Board.
Data analysis
The primary outcome variable was time to diagnostic resolution. We included only participants supported by a single navigator. A Fisher exact test by cancer type was used to compare the two groups (personal experience vs none) in the proportion of patients who achieved diagnostic resolution by 365 days. We reviewed the percentage of patients resolved for the total population as well as stratified by cancer site (breast, cervical, prostate, and colorectal), owing to the known mean differences in time to diagnostic resolution by type of cancer.
Cox proportional hazard models and adjusted hazard ratios were developed and calculated to examine the impact of navigator’s personal experience with cancer on time to resolution, controlling for patient gender, race, age, and cancer type in the models. The analysis controlled for the individual effect of navigators through clustering. We used P < .05 as the cut-off for significance, and used Stata 10.1 (StataCorp, College Station Texas 77845) for all analyses.
Results
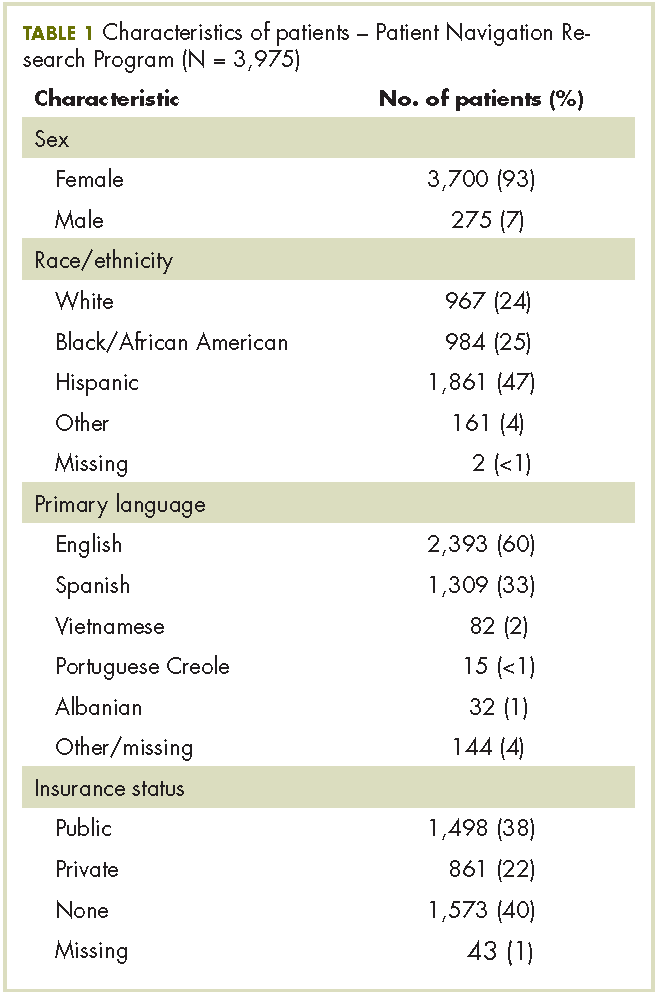
Our analytic sample included the 3,975 patients with only 1 navigator over the course of the study, 79% of the navigation (n = 5,063) arm. Most of the patients were women (93%), and most were from racial and ethnic minority communities. Most patients spoke English (60%), with Spanish (33%) as the next most common language. Most patients were publically insured (38%) or uninsured (40%) (Table 1).
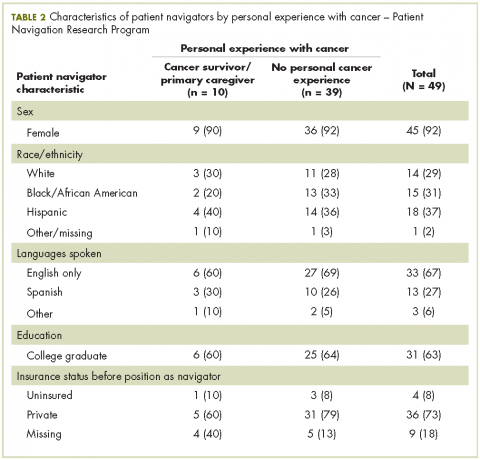
Of the total 49 navigators, 6 were cancer survivors and 4 were primary caregivers to a family member with cancer; an additional 19 reported that they had family members with cancer (Table 2). Most of the navigators were women. The racial/ethnic distribution mirrored the populations they served: white (29%); black or African American (31%); and Hispanic (37%). English was the only spoken language of 67% of the navigators; 27% spoke Spanish, and 6% reported speaking another language. Most had a college degree (63%).
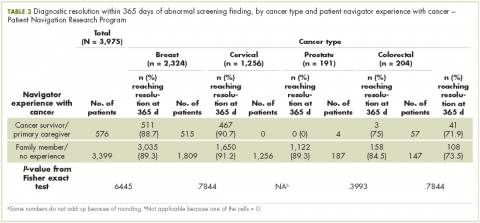
The unadjusted bivariate comparison of patients who achieved diagnostic resolution within 365 days, by navigator experience with cancer, are shown in Table 3. We found no difference in time to diagnostic resolution for those patients for whom navigators had personal experience with cancer compared with those whose navigators had no experience. When stratified by type of cancer screening abnormality (breast, cervical, prostate, or colorectal), the results also did not reveal a significant difference in the proportion of patients achieving diagnostic resolution by 365 days by navigator experience with cancer.
In the Cox proportional hazard model adjusting for patient gender, age, race/ethnicity, cancer type, and adjusting for navigator using clustering, there was no difference between patients whose navigators had experience with cancer care, and those who did not (adjusted hazard ratio, 1.03; 95% confidence interval, .83-1.3). The level of education of navigators was not significantly associated with time to diagnostic resolution for patients.
Discussion
Although several cancer support programs have explicitly used cancer survivors as patient navigators or other supports for patients in active cancer care, there are scant data on whether this expertise improves care. Our study was not able to identify that navigators with previous experience with cancer care, either as a patient or as the primary caregiver, was associated with improved time to diagnostic resolution.
As patient navigation has become the standard of cancer diagnostic and treatment practices, there is a need to develop competencies and standards for hiring and training navigators. Part of this hiring process is to determine what past experience and training are relevant for effective navigation. There is little previous research on relevant skills of navigators, with only one study having demonstrated that language and racial/ ethnic concordance between patients and navigators was associated with more timely care. The national PNRP program hired mostly lay navigators with minimal medical experience, but with affiliations to the communities of the patients receiving care. Our program has demonstrated that lay individuals can be trained in the logistic aspects of navigation.5 Although it may seem intuitive that the experience of being a cancer survivor may make a navigator more empathetic, it is also possible that being too close to the experience of survivorship can also pose challenges to a navigator. Alternatively, navigation may be equally effective with proper training regardless of previous experience with cancer.
Our study is limited to addressing the outcome of timely resolution in the diagnostic phase of care after abnormal cancer screening. It is possible that past experience with cancer care will be beneficial when providing navigation for cancer care. While this study represents one of the largest groups of navigators who have been studied, the small sample may have limited our ability to detect differences. Our study has the benefit of a diverse group of navigators from a nationally representative, multi-site study. We suggest that prior experience with cancer care is not a prerequisite to supporting diagnostic care after abnormal cancer screening. Providing appropriate training to navigators may be sufficient to ensure effective and appropriate care is provided by patient navigators.
Acknowledgments
The authors acknowledge the contributions of the following members of the Patient Navigation Research Program:Clinical centers Boston Medical Center and Boston University: Karen M Freund (principal investigator [PI]), Tracy A Battaglia (co-PI); Denver Health and Hospital Authority: Peter Raich (PI), Elizabeth Whitley (co-PI); George Washington University Cancer Institute: Steven R Patierno (PI), Lisa M Alexander, Paul H Levine, Heather A Young, Heather J Hoffman, Nancy L LaVerda; H Lee Moffitt Cancer Center and Research Institute: Richard G Roetzheim (PI), Cathy Meade, Kristen J Wells; Northwest Portland Area Indian Health Board: Victoria Warren-Mears (PI); Northwestern University Robert H Lurie Comprehensive Cancer Center: Steven Rosen (PI), Melissa Simon; The Ohio State University Comprehensive Cancer Center: Electra Paskett (PI); University of Illinois at Chicago and Access Community Health Center: Elizabeth Calhoun (PI), Julie Darnell. University of Rochester: Kevin Fiscella (PI), Samantha Hendren; University of Texas Health Science Center at San Antonio Cancer Therapy and Research Center: Donald Dudley (PI), Kevin Hall, Anand Karnard, Amelie Ramirez. Program office National Cancer Institute, Center to Reduce Cancer Health Disparities: Martha Hare, Mollie Howerton, Ken Chu, Emmanuel Taylor, Mary Ann Van Dyun. Evaluation contractor NOVA Research Company: Paul Young, Frederick Snyder
6. Macvean ML, White VM, Sanson-Fisher R. One-to-one volunteer support programs for people with cancer: a review of the literature. Patient Educ Couns. 2008;70:10-24.
7. Rodday AM, Parsons SK, Snyder F, et al. The impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121(22):4025-4034.
10. Charlot M, Santana MC, Chen CA, et al. Impact of patient and navigator race and language concordance on care after cancer screening abnormalities. Cancer. 2015;121(9):1477-1483.
Patient navigation has emerged in the past decade as a strategy to decrease cancer disparities among low-income, minority populations. Patient navigators help individuals who face personal and systemtic barriers to gaining access to care.1 Their role is to help patients find their way through a complex health care system,2,3 including logistic support of rescheduling appointments, assistance with transportation, and child care needs. They provide personal support, including coaching patients on their clinical visits, educating them about the cancer treatment process, and addressing their fears of diagnosis and treatment. Patient navigation has shown improvement in cancer screening rates, time to diagnostic resolution for those patients who have abnormal cancer screening tests, and quality of cancer care.4,5
In hiring patient navigators, it is not clear which professional training and skill sets and what personal experiences are most useful to becoming an effective navigator. Personal cancer experience can include a personal diagnosis, the experience of serving as a primary caregiver for a patient during treatment, or having a family member or close friend with cancer. Several current support programs specifically recruit cancer survivors on the assumption that their cancer treatment experience can provide helpful insights to a current patient for both emotional and logistical support.6 In this paper, we sought to address whether patient navigation promotes more timely diagnostic care if the navigator has experience with cancer.
Methods
This is a secondary analysis of the patients with abnormal cancer screening in the navigation arm of the national Patient Navigation Research Program (PNRP) study,1, 5 a collaborative effort across 10 centers to investigate the efficacy of patient navigation on improving patient-level outcomes for those who have abnormal results from a breast, cervical, colorectal, or prostate cancer screening test. The study demonstrated that patient navigation was effective in reducing delays in diagnosis and treatment5 and resulting in a higher quality of care,4 especially among vulnerable populations.7 The Institutional Review Board of each respective institution approved the research.
All of the patient navigators were paid employees with a minimum high-school diploma or equivalent. Navigators’ activities were standardized across centers through a national training program.8 Navigators used the care management model to identify and address barriers to care and to track participants throughout the course of their diagnostic evaluation,9 with the primary aim of timely diagnostic resolution. Most navigation programs were embedded within the clinical care system and interacted with patients through mail, by phone, and face-to-face contact.1
Data collection
Each center used agreed-upon inclusion and exclusion criteria and collected and coded the same patient-level data. Medical records were abstracted for pertinent clinical data on patients. Demographic data were collected through a patient survey or extracted from medical record registration. The central data coordinating center collected navigator information including demographic characteristics and experience with cancer.
We created a new variable, Personal experience with cancer. Personal experience with cancer was based on three questions asked of navigators: whether they were a cancer survivor; whether they were the primary caregiver to a family member or close friend with cancer; and whether they had a family member with cancer. Because of the small sample size, responses from navigators who were cancer survivors (n = 6) or primary caregivers to a family member with cancer (n = 4) were collapsed into a single category, referred to as personal experience with cancer, to compare with navigators who had no personal experience with cancer, which included those who reported a family member with cancer but who were not serving as a primary caregiver.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Each clinical center received approved from their institution’s human subjects review board. Informed consent was obtained from all patient navigator participants included in the study. Participating patients completed informed consent at some centers. At other centers where the study design was an implementation of a system intervention, a waiver of informed consent was approved by the Institutional Review Board.
Data analysis
The primary outcome variable was time to diagnostic resolution. We included only participants supported by a single navigator. A Fisher exact test by cancer type was used to compare the two groups (personal experience vs none) in the proportion of patients who achieved diagnostic resolution by 365 days. We reviewed the percentage of patients resolved for the total population as well as stratified by cancer site (breast, cervical, prostate, and colorectal), owing to the known mean differences in time to diagnostic resolution by type of cancer.
Cox proportional hazard models and adjusted hazard ratios were developed and calculated to examine the impact of navigator’s personal experience with cancer on time to resolution, controlling for patient gender, race, age, and cancer type in the models. The analysis controlled for the individual effect of navigators through clustering. We used P < .05 as the cut-off for significance, and used Stata 10.1 (StataCorp, College Station Texas 77845) for all analyses.
Results
Our analytic sample included the 3,975 patients with only 1 navigator over the course of the study, 79% of the navigation (n = 5,063) arm. Most of the patients were women (93%), and most were from racial and ethnic minority communities. Most patients spoke English (60%), with Spanish (33%) as the next most common language. Most patients were publically insured (38%) or uninsured (40%) (Table 1).
Of the total 49 navigators, 6 were cancer survivors and 4 were primary caregivers to a family member with cancer; an additional 19 reported that they had family members with cancer (Table 2). Most of the navigators were women. The racial/ethnic distribution mirrored the populations they served: white (29%); black or African American (31%); and Hispanic (37%). English was the only spoken language of 67% of the navigators; 27% spoke Spanish, and 6% reported speaking another language. Most had a college degree (63%).
The unadjusted bivariate comparison of patients who achieved diagnostic resolution within 365 days, by navigator experience with cancer, are shown in Table 3. We found no difference in time to diagnostic resolution for those patients for whom navigators had personal experience with cancer compared with those whose navigators had no experience. When stratified by type of cancer screening abnormality (breast, cervical, prostate, or colorectal), the results also did not reveal a significant difference in the proportion of patients achieving diagnostic resolution by 365 days by navigator experience with cancer.
In the Cox proportional hazard model adjusting for patient gender, age, race/ethnicity, cancer type, and adjusting for navigator using clustering, there was no difference between patients whose navigators had experience with cancer care, and those who did not (adjusted hazard ratio, 1.03; 95% confidence interval, .83-1.3). The level of education of navigators was not significantly associated with time to diagnostic resolution for patients.
Discussion
Although several cancer support programs have explicitly used cancer survivors as patient navigators or other supports for patients in active cancer care, there are scant data on whether this expertise improves care. Our study was not able to identify that navigators with previous experience with cancer care, either as a patient or as the primary caregiver, was associated with improved time to diagnostic resolution.
As patient navigation has become the standard of cancer diagnostic and treatment practices, there is a need to develop competencies and standards for hiring and training navigators. Part of this hiring process is to determine what past experience and training are relevant for effective navigation. There is little previous research on relevant skills of navigators, with only one study having demonstrated that language and racial/ ethnic concordance between patients and navigators was associated with more timely care. The national PNRP program hired mostly lay navigators with minimal medical experience, but with affiliations to the communities of the patients receiving care. Our program has demonstrated that lay individuals can be trained in the logistic aspects of navigation.5 Although it may seem intuitive that the experience of being a cancer survivor may make a navigator more empathetic, it is also possible that being too close to the experience of survivorship can also pose challenges to a navigator. Alternatively, navigation may be equally effective with proper training regardless of previous experience with cancer.
Our study is limited to addressing the outcome of timely resolution in the diagnostic phase of care after abnormal cancer screening. It is possible that past experience with cancer care will be beneficial when providing navigation for cancer care. While this study represents one of the largest groups of navigators who have been studied, the small sample may have limited our ability to detect differences. Our study has the benefit of a diverse group of navigators from a nationally representative, multi-site study. We suggest that prior experience with cancer care is not a prerequisite to supporting diagnostic care after abnormal cancer screening. Providing appropriate training to navigators may be sufficient to ensure effective and appropriate care is provided by patient navigators.
Acknowledgments
The authors acknowledge the contributions of the following members of the Patient Navigation Research Program:Clinical centers Boston Medical Center and Boston University: Karen M Freund (principal investigator [PI]), Tracy A Battaglia (co-PI); Denver Health and Hospital Authority: Peter Raich (PI), Elizabeth Whitley (co-PI); George Washington University Cancer Institute: Steven R Patierno (PI), Lisa M Alexander, Paul H Levine, Heather A Young, Heather J Hoffman, Nancy L LaVerda; H Lee Moffitt Cancer Center and Research Institute: Richard G Roetzheim (PI), Cathy Meade, Kristen J Wells; Northwest Portland Area Indian Health Board: Victoria Warren-Mears (PI); Northwestern University Robert H Lurie Comprehensive Cancer Center: Steven Rosen (PI), Melissa Simon; The Ohio State University Comprehensive Cancer Center: Electra Paskett (PI); University of Illinois at Chicago and Access Community Health Center: Elizabeth Calhoun (PI), Julie Darnell. University of Rochester: Kevin Fiscella (PI), Samantha Hendren; University of Texas Health Science Center at San Antonio Cancer Therapy and Research Center: Donald Dudley (PI), Kevin Hall, Anand Karnard, Amelie Ramirez. Program office National Cancer Institute, Center to Reduce Cancer Health Disparities: Martha Hare, Mollie Howerton, Ken Chu, Emmanuel Taylor, Mary Ann Van Dyun. Evaluation contractor NOVA Research Company: Paul Young, Frederick Snyder
Patient navigation has emerged in the past decade as a strategy to decrease cancer disparities among low-income, minority populations. Patient navigators help individuals who face personal and systemtic barriers to gaining access to care.1 Their role is to help patients find their way through a complex health care system,2,3 including logistic support of rescheduling appointments, assistance with transportation, and child care needs. They provide personal support, including coaching patients on their clinical visits, educating them about the cancer treatment process, and addressing their fears of diagnosis and treatment. Patient navigation has shown improvement in cancer screening rates, time to diagnostic resolution for those patients who have abnormal cancer screening tests, and quality of cancer care.4,5
In hiring patient navigators, it is not clear which professional training and skill sets and what personal experiences are most useful to becoming an effective navigator. Personal cancer experience can include a personal diagnosis, the experience of serving as a primary caregiver for a patient during treatment, or having a family member or close friend with cancer. Several current support programs specifically recruit cancer survivors on the assumption that their cancer treatment experience can provide helpful insights to a current patient for both emotional and logistical support.6 In this paper, we sought to address whether patient navigation promotes more timely diagnostic care if the navigator has experience with cancer.
Methods
This is a secondary analysis of the patients with abnormal cancer screening in the navigation arm of the national Patient Navigation Research Program (PNRP) study,1, 5 a collaborative effort across 10 centers to investigate the efficacy of patient navigation on improving patient-level outcomes for those who have abnormal results from a breast, cervical, colorectal, or prostate cancer screening test. The study demonstrated that patient navigation was effective in reducing delays in diagnosis and treatment5 and resulting in a higher quality of care,4 especially among vulnerable populations.7 The Institutional Review Board of each respective institution approved the research.
All of the patient navigators were paid employees with a minimum high-school diploma or equivalent. Navigators’ activities were standardized across centers through a national training program.8 Navigators used the care management model to identify and address barriers to care and to track participants throughout the course of their diagnostic evaluation,9 with the primary aim of timely diagnostic resolution. Most navigation programs were embedded within the clinical care system and interacted with patients through mail, by phone, and face-to-face contact.1
Data collection
Each center used agreed-upon inclusion and exclusion criteria and collected and coded the same patient-level data. Medical records were abstracted for pertinent clinical data on patients. Demographic data were collected through a patient survey or extracted from medical record registration. The central data coordinating center collected navigator information including demographic characteristics and experience with cancer.
We created a new variable, Personal experience with cancer. Personal experience with cancer was based on three questions asked of navigators: whether they were a cancer survivor; whether they were the primary caregiver to a family member or close friend with cancer; and whether they had a family member with cancer. Because of the small sample size, responses from navigators who were cancer survivors (n = 6) or primary caregivers to a family member with cancer (n = 4) were collapsed into a single category, referred to as personal experience with cancer, to compare with navigators who had no personal experience with cancer, which included those who reported a family member with cancer but who were not serving as a primary caregiver.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Each clinical center received approved from their institution’s human subjects review board. Informed consent was obtained from all patient navigator participants included in the study. Participating patients completed informed consent at some centers. At other centers where the study design was an implementation of a system intervention, a waiver of informed consent was approved by the Institutional Review Board.
Data analysis
The primary outcome variable was time to diagnostic resolution. We included only participants supported by a single navigator. A Fisher exact test by cancer type was used to compare the two groups (personal experience vs none) in the proportion of patients who achieved diagnostic resolution by 365 days. We reviewed the percentage of patients resolved for the total population as well as stratified by cancer site (breast, cervical, prostate, and colorectal), owing to the known mean differences in time to diagnostic resolution by type of cancer.
Cox proportional hazard models and adjusted hazard ratios were developed and calculated to examine the impact of navigator’s personal experience with cancer on time to resolution, controlling for patient gender, race, age, and cancer type in the models. The analysis controlled for the individual effect of navigators through clustering. We used P < .05 as the cut-off for significance, and used Stata 10.1 (StataCorp, College Station Texas 77845) for all analyses.
Results
Our analytic sample included the 3,975 patients with only 1 navigator over the course of the study, 79% of the navigation (n = 5,063) arm. Most of the patients were women (93%), and most were from racial and ethnic minority communities. Most patients spoke English (60%), with Spanish (33%) as the next most common language. Most patients were publically insured (38%) or uninsured (40%) (Table 1).
Of the total 49 navigators, 6 were cancer survivors and 4 were primary caregivers to a family member with cancer; an additional 19 reported that they had family members with cancer (Table 2). Most of the navigators were women. The racial/ethnic distribution mirrored the populations they served: white (29%); black or African American (31%); and Hispanic (37%). English was the only spoken language of 67% of the navigators; 27% spoke Spanish, and 6% reported speaking another language. Most had a college degree (63%).
The unadjusted bivariate comparison of patients who achieved diagnostic resolution within 365 days, by navigator experience with cancer, are shown in Table 3. We found no difference in time to diagnostic resolution for those patients for whom navigators had personal experience with cancer compared with those whose navigators had no experience. When stratified by type of cancer screening abnormality (breast, cervical, prostate, or colorectal), the results also did not reveal a significant difference in the proportion of patients achieving diagnostic resolution by 365 days by navigator experience with cancer.
In the Cox proportional hazard model adjusting for patient gender, age, race/ethnicity, cancer type, and adjusting for navigator using clustering, there was no difference between patients whose navigators had experience with cancer care, and those who did not (adjusted hazard ratio, 1.03; 95% confidence interval, .83-1.3). The level of education of navigators was not significantly associated with time to diagnostic resolution for patients.
Discussion
Although several cancer support programs have explicitly used cancer survivors as patient navigators or other supports for patients in active cancer care, there are scant data on whether this expertise improves care. Our study was not able to identify that navigators with previous experience with cancer care, either as a patient or as the primary caregiver, was associated with improved time to diagnostic resolution.
As patient navigation has become the standard of cancer diagnostic and treatment practices, there is a need to develop competencies and standards for hiring and training navigators. Part of this hiring process is to determine what past experience and training are relevant for effective navigation. There is little previous research on relevant skills of navigators, with only one study having demonstrated that language and racial/ ethnic concordance between patients and navigators was associated with more timely care. The national PNRP program hired mostly lay navigators with minimal medical experience, but with affiliations to the communities of the patients receiving care. Our program has demonstrated that lay individuals can be trained in the logistic aspects of navigation.5 Although it may seem intuitive that the experience of being a cancer survivor may make a navigator more empathetic, it is also possible that being too close to the experience of survivorship can also pose challenges to a navigator. Alternatively, navigation may be equally effective with proper training regardless of previous experience with cancer.
Our study is limited to addressing the outcome of timely resolution in the diagnostic phase of care after abnormal cancer screening. It is possible that past experience with cancer care will be beneficial when providing navigation for cancer care. While this study represents one of the largest groups of navigators who have been studied, the small sample may have limited our ability to detect differences. Our study has the benefit of a diverse group of navigators from a nationally representative, multi-site study. We suggest that prior experience with cancer care is not a prerequisite to supporting diagnostic care after abnormal cancer screening. Providing appropriate training to navigators may be sufficient to ensure effective and appropriate care is provided by patient navigators.
Acknowledgments
The authors acknowledge the contributions of the following members of the Patient Navigation Research Program:Clinical centers Boston Medical Center and Boston University: Karen M Freund (principal investigator [PI]), Tracy A Battaglia (co-PI); Denver Health and Hospital Authority: Peter Raich (PI), Elizabeth Whitley (co-PI); George Washington University Cancer Institute: Steven R Patierno (PI), Lisa M Alexander, Paul H Levine, Heather A Young, Heather J Hoffman, Nancy L LaVerda; H Lee Moffitt Cancer Center and Research Institute: Richard G Roetzheim (PI), Cathy Meade, Kristen J Wells; Northwest Portland Area Indian Health Board: Victoria Warren-Mears (PI); Northwestern University Robert H Lurie Comprehensive Cancer Center: Steven Rosen (PI), Melissa Simon; The Ohio State University Comprehensive Cancer Center: Electra Paskett (PI); University of Illinois at Chicago and Access Community Health Center: Elizabeth Calhoun (PI), Julie Darnell. University of Rochester: Kevin Fiscella (PI), Samantha Hendren; University of Texas Health Science Center at San Antonio Cancer Therapy and Research Center: Donald Dudley (PI), Kevin Hall, Anand Karnard, Amelie Ramirez. Program office National Cancer Institute, Center to Reduce Cancer Health Disparities: Martha Hare, Mollie Howerton, Ken Chu, Emmanuel Taylor, Mary Ann Van Dyun. Evaluation contractor NOVA Research Company: Paul Young, Frederick Snyder
6. Macvean ML, White VM, Sanson-Fisher R. One-to-one volunteer support programs for people with cancer: a review of the literature. Patient Educ Couns. 2008;70:10-24.
7. Rodday AM, Parsons SK, Snyder F, et al. The impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121(22):4025-4034.
10. Charlot M, Santana MC, Chen CA, et al. Impact of patient and navigator race and language concordance on care after cancer screening abnormalities. Cancer. 2015;121(9):1477-1483.
6. Macvean ML, White VM, Sanson-Fisher R. One-to-one volunteer support programs for people with cancer: a review of the literature. Patient Educ Couns. 2008;70:10-24.
7. Rodday AM, Parsons SK, Snyder F, et al. The impact of patient navigation in eliminating economic disparities in cancer care. Cancer. 2015;121(22):4025-4034.
10. Charlot M, Santana MC, Chen CA, et al. Impact of patient and navigator race and language concordance on care after cancer screening abnormalities. Cancer. 2015;121(9):1477-1483.