User login
sNDA gets priority review for CLL/SLL
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
The U.S. Food and Drug Administration (FDA) has accepted for priority review a supplemental new drug application (sNDA) for ibrutinib (Imbruvica®).
With this sNDA, Pharmacyclics LLC (an AbbVie company) and Janssen Biotech, Inc., are seeking approval for ibrutinib in combination with obinutuzumab (Gazyva®) in previously untreated adults with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The agency intends to take action on a priority review application within 6 months of receiving it rather than the standard 10 months.
Ibrutinib is already FDA-approved as monotherapy for adults with CLL/SLL (previously treated or untreated), with and without 17p deletion. Ibrutinib is also approved in combination with bendamustine and rituximab for adults with previously treated CLL/SLL.
Obinutuzumab is FDA-approved for use in combination with chlorambucil to treat previously untreated CLL.
The sNDA for ibrutinib in combination with obinutuzumab is based on results from the phase 3 iLLUMINATE trial (NCT02264574).
The trial is a comparison of ibrutinib plus obinutuzumab and chlorambucil plus obinutuzumab in patients with previously untreated CLL/SLL.
In May, AbbVie announced that the trial’s primary endpoint was met. Specifically, ibrutinib plus obinutuzumab was associated with significantly longer progression-free survival than chlorambucil plus obinutuzumab.
Data from the trial have not been released. Pharmacyclics and Janssen said they plan to present the data in a future publication or at a medical congress.
Understanding the role of HSCT in PTCL
DUBROVNIK, CROATIA—Hematopoietic stem cell transplant (HSCT) can be hit-or-miss in patients with peripheral T-cell lymphomas (PTCLs), according to a speaker at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Ali Bazarbachi, MD, PhD, of the American University of Beirut in Lebanon, noted that the success of HSCT varies according to the subtype of PTCL and the type of transplant.
For example, autologous (auto) HSCT given as frontline consolidation can be considered the standard of care for PTCL-not otherwise specified (NOS), angioimmunoblastic T-cell lymphoma (AITL), and certain patients with anaplastic large-cell lymphoma (ALCL), according to Dr. Bazarbachi.
On the other hand, auto-HSCT should never be used in patients with adult T-cell leukemia/lymphoma (ATLL).
Both auto-HSCT and allogeneic (allo) HSCT are options for patients with non-localized, extranodal natural killer T-cell lymphoma (ENKTL), nasal type, but only at certain times.
State of PTCL treatment
Dr. Bazarbachi began his presentation by pointing out that patients with newly diagnosed PTCL are no longer treated like patients with B-cell lymphoma, but treatment outcomes in PTCL still leave a lot to be desired.
He noted that, with any of the chemotherapy regimens used, typically, about a third of patients are primary refractory, a third relapse, and a quarter are cured. Only two forms of PTCL are frequently curable—localized ENKTL and ALK-positive ALCL.
Current treatment strategies for PTCL do include HSCT, but recommendations vary. Dr. Bazarbachi made the following recommendations, supported by evidence from clinical trials.
HSCT in PTCL-NOS, AITL, and ALCL
For patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL, auto-HSCT as frontline consolidation can be considered the standard of care in patients who responded to induction, Dr. Bazarbachi said.
In a study published in 20121, high-dose chemotherapy and auto-HSCT as consolidation improved 5-year overall survival—compared to previous results with CHOP2—in patients with ALK-negative ALCL, AITL, PTCL-NOS, and enteropathy-associated T-cell lymphoma.
Allo-HSCT may also be an option for frontline consolidation in patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL, according to Dr. Bazarbachi.
“Allo-transplant is not dead in this indication,” he said. “But it should be either part of a clinical trial or [given] to some selected patients—those with persistent bone marrow involvement, very young patients, or patients with primary refractory disease.”
Results from the COMPLETE study3 showed improved survival in patients who received consolidation with auto- or allo-HSCT, as compared to patients who did not receive a transplant.
COMPLETE patients with AITL or PTCL-NOS had improvements in progression-free and overall survival with HSCT. The survival advantage was “less evident” in patients with ALCL, the researchers said, but this trial included both ALK-negative and ALK-positive patients.
Dr. Bazarbachi noted that allo- and auto-HSCT can be options after relapse in patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL.
However, chemosensitive patients who have relapsed should only receive auto-HSCT if they did not receive it frontline. Patients who have already undergone auto-HSCT can receive allo-HSCT, Dr. Bazarbachi said.
He added that refractory patients should not undergo auto-HSCT and should receive allo-HSCT only within the context of a clinical trial.
HSCT in ATLL
Dr. Bazarbachi noted that ATLL has a dismal prognosis, but allo-HSCT as frontline consolidation is potentially curative.4,5 It is most effective in patients who have achieved a complete or partial response to induction.
However, allo-HSCT should not be given as consolidation to ATLL patients who have received prior mogamulizumab. These patients have an increased risk of morbidity and mortality if they undergo allo-HSCT.
Allo-HSCT should not be given to refractory ATLL patients, although it may be an option for relapsed patients.
Dr. Bazarbachi stressed that ATLL patients should not receive auto-HSCT at any time—as frontline consolidation, after relapse, or if they have refractory disease.
Auto-HSCT “does not work in this disease,” he said. In a study published in 20145, all four ATLL patients who underwent auto-HSCT “rapidly” died.
HSCT in ENKTL
Dr. Bazarbachi said frontline consolidation with auto-HSCT should be considered the standard of care for patients with non-localized ENKTL, nasal type.
Auto-HSCT has been shown to improve survival in these patients6, and it is most effective when patients have achieved a complete response to induction.
Allo-HSCT is also an option for frontline consolidation in patients with non-localized ENKTL, nasal type, Dr. Bazarbachi said.
He added that chemosensitive patients who have relapsed can receive allo-HSCT, but they should only receive auto-HSCT if they did not receive it in the frontline setting. Both types of transplant should take place when patients are in complete remission.
Patients with refractory, non-localized ENKTL, nasal type should not receive auto-HSCT, but allo-HSCT is an option, Dr. Bazarbachi said.
He did not declare any conflicts of interest.
1. d’Amore F et al. J Clin Oncol. 2012 Sep 1;30(25):3093-9. doi: 10.1200/JCO.2011.40.2719
2. AbouYabis AN et al. ISRN Hematol. 2011 Jun 16. doi: 10.5402/2011/623924
3. Park SI et al. Blood 2017 130:342
4. Ishida T et al. Blood 2012 Aug 23;120(8):1734-41. doi: 10.1182/blood-2012-03-414490
5. Bazarbachi A et al. Bone Marrow Transplant. 2014 Oct;49(10):1266-8. doi: 10.1038/bmt.2014.143
6. Lee J et al. Biol Blood Marrow Transplant. 2008 Dec;14(12):1356-64. doi: 10.1016/j.bbmt.2008.09.014
DUBROVNIK, CROATIA—Hematopoietic stem cell transplant (HSCT) can be hit-or-miss in patients with peripheral T-cell lymphomas (PTCLs), according to a speaker at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Ali Bazarbachi, MD, PhD, of the American University of Beirut in Lebanon, noted that the success of HSCT varies according to the subtype of PTCL and the type of transplant.
For example, autologous (auto) HSCT given as frontline consolidation can be considered the standard of care for PTCL-not otherwise specified (NOS), angioimmunoblastic T-cell lymphoma (AITL), and certain patients with anaplastic large-cell lymphoma (ALCL), according to Dr. Bazarbachi.
On the other hand, auto-HSCT should never be used in patients with adult T-cell leukemia/lymphoma (ATLL).
Both auto-HSCT and allogeneic (allo) HSCT are options for patients with non-localized, extranodal natural killer T-cell lymphoma (ENKTL), nasal type, but only at certain times.
State of PTCL treatment
Dr. Bazarbachi began his presentation by pointing out that patients with newly diagnosed PTCL are no longer treated like patients with B-cell lymphoma, but treatment outcomes in PTCL still leave a lot to be desired.
He noted that, with any of the chemotherapy regimens used, typically, about a third of patients are primary refractory, a third relapse, and a quarter are cured. Only two forms of PTCL are frequently curable—localized ENKTL and ALK-positive ALCL.
Current treatment strategies for PTCL do include HSCT, but recommendations vary. Dr. Bazarbachi made the following recommendations, supported by evidence from clinical trials.
HSCT in PTCL-NOS, AITL, and ALCL
For patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL, auto-HSCT as frontline consolidation can be considered the standard of care in patients who responded to induction, Dr. Bazarbachi said.
In a study published in 20121, high-dose chemotherapy and auto-HSCT as consolidation improved 5-year overall survival—compared to previous results with CHOP2—in patients with ALK-negative ALCL, AITL, PTCL-NOS, and enteropathy-associated T-cell lymphoma.
Allo-HSCT may also be an option for frontline consolidation in patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL, according to Dr. Bazarbachi.
“Allo-transplant is not dead in this indication,” he said. “But it should be either part of a clinical trial or [given] to some selected patients—those with persistent bone marrow involvement, very young patients, or patients with primary refractory disease.”
Results from the COMPLETE study3 showed improved survival in patients who received consolidation with auto- or allo-HSCT, as compared to patients who did not receive a transplant.
COMPLETE patients with AITL or PTCL-NOS had improvements in progression-free and overall survival with HSCT. The survival advantage was “less evident” in patients with ALCL, the researchers said, but this trial included both ALK-negative and ALK-positive patients.
Dr. Bazarbachi noted that allo- and auto-HSCT can be options after relapse in patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL.
However, chemosensitive patients who have relapsed should only receive auto-HSCT if they did not receive it frontline. Patients who have already undergone auto-HSCT can receive allo-HSCT, Dr. Bazarbachi said.
He added that refractory patients should not undergo auto-HSCT and should receive allo-HSCT only within the context of a clinical trial.
HSCT in ATLL
Dr. Bazarbachi noted that ATLL has a dismal prognosis, but allo-HSCT as frontline consolidation is potentially curative.4,5 It is most effective in patients who have achieved a complete or partial response to induction.
However, allo-HSCT should not be given as consolidation to ATLL patients who have received prior mogamulizumab. These patients have an increased risk of morbidity and mortality if they undergo allo-HSCT.
Allo-HSCT should not be given to refractory ATLL patients, although it may be an option for relapsed patients.
Dr. Bazarbachi stressed that ATLL patients should not receive auto-HSCT at any time—as frontline consolidation, after relapse, or if they have refractory disease.
Auto-HSCT “does not work in this disease,” he said. In a study published in 20145, all four ATLL patients who underwent auto-HSCT “rapidly” died.
HSCT in ENKTL
Dr. Bazarbachi said frontline consolidation with auto-HSCT should be considered the standard of care for patients with non-localized ENKTL, nasal type.
Auto-HSCT has been shown to improve survival in these patients6, and it is most effective when patients have achieved a complete response to induction.
Allo-HSCT is also an option for frontline consolidation in patients with non-localized ENKTL, nasal type, Dr. Bazarbachi said.
He added that chemosensitive patients who have relapsed can receive allo-HSCT, but they should only receive auto-HSCT if they did not receive it in the frontline setting. Both types of transplant should take place when patients are in complete remission.
Patients with refractory, non-localized ENKTL, nasal type should not receive auto-HSCT, but allo-HSCT is an option, Dr. Bazarbachi said.
He did not declare any conflicts of interest.
1. d’Amore F et al. J Clin Oncol. 2012 Sep 1;30(25):3093-9. doi: 10.1200/JCO.2011.40.2719
2. AbouYabis AN et al. ISRN Hematol. 2011 Jun 16. doi: 10.5402/2011/623924
3. Park SI et al. Blood 2017 130:342
4. Ishida T et al. Blood 2012 Aug 23;120(8):1734-41. doi: 10.1182/blood-2012-03-414490
5. Bazarbachi A et al. Bone Marrow Transplant. 2014 Oct;49(10):1266-8. doi: 10.1038/bmt.2014.143
6. Lee J et al. Biol Blood Marrow Transplant. 2008 Dec;14(12):1356-64. doi: 10.1016/j.bbmt.2008.09.014
DUBROVNIK, CROATIA—Hematopoietic stem cell transplant (HSCT) can be hit-or-miss in patients with peripheral T-cell lymphomas (PTCLs), according to a speaker at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Ali Bazarbachi, MD, PhD, of the American University of Beirut in Lebanon, noted that the success of HSCT varies according to the subtype of PTCL and the type of transplant.
For example, autologous (auto) HSCT given as frontline consolidation can be considered the standard of care for PTCL-not otherwise specified (NOS), angioimmunoblastic T-cell lymphoma (AITL), and certain patients with anaplastic large-cell lymphoma (ALCL), according to Dr. Bazarbachi.
On the other hand, auto-HSCT should never be used in patients with adult T-cell leukemia/lymphoma (ATLL).
Both auto-HSCT and allogeneic (allo) HSCT are options for patients with non-localized, extranodal natural killer T-cell lymphoma (ENKTL), nasal type, but only at certain times.
State of PTCL treatment
Dr. Bazarbachi began his presentation by pointing out that patients with newly diagnosed PTCL are no longer treated like patients with B-cell lymphoma, but treatment outcomes in PTCL still leave a lot to be desired.
He noted that, with any of the chemotherapy regimens used, typically, about a third of patients are primary refractory, a third relapse, and a quarter are cured. Only two forms of PTCL are frequently curable—localized ENKTL and ALK-positive ALCL.
Current treatment strategies for PTCL do include HSCT, but recommendations vary. Dr. Bazarbachi made the following recommendations, supported by evidence from clinical trials.
HSCT in PTCL-NOS, AITL, and ALCL
For patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL, auto-HSCT as frontline consolidation can be considered the standard of care in patients who responded to induction, Dr. Bazarbachi said.
In a study published in 20121, high-dose chemotherapy and auto-HSCT as consolidation improved 5-year overall survival—compared to previous results with CHOP2—in patients with ALK-negative ALCL, AITL, PTCL-NOS, and enteropathy-associated T-cell lymphoma.
Allo-HSCT may also be an option for frontline consolidation in patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL, according to Dr. Bazarbachi.
“Allo-transplant is not dead in this indication,” he said. “But it should be either part of a clinical trial or [given] to some selected patients—those with persistent bone marrow involvement, very young patients, or patients with primary refractory disease.”
Results from the COMPLETE study3 showed improved survival in patients who received consolidation with auto- or allo-HSCT, as compared to patients who did not receive a transplant.
COMPLETE patients with AITL or PTCL-NOS had improvements in progression-free and overall survival with HSCT. The survival advantage was “less evident” in patients with ALCL, the researchers said, but this trial included both ALK-negative and ALK-positive patients.
Dr. Bazarbachi noted that allo- and auto-HSCT can be options after relapse in patients with PTCL-NOS, AITL, or ALK-negative, non-DUSP22 ALCL.
However, chemosensitive patients who have relapsed should only receive auto-HSCT if they did not receive it frontline. Patients who have already undergone auto-HSCT can receive allo-HSCT, Dr. Bazarbachi said.
He added that refractory patients should not undergo auto-HSCT and should receive allo-HSCT only within the context of a clinical trial.
HSCT in ATLL
Dr. Bazarbachi noted that ATLL has a dismal prognosis, but allo-HSCT as frontline consolidation is potentially curative.4,5 It is most effective in patients who have achieved a complete or partial response to induction.
However, allo-HSCT should not be given as consolidation to ATLL patients who have received prior mogamulizumab. These patients have an increased risk of morbidity and mortality if they undergo allo-HSCT.
Allo-HSCT should not be given to refractory ATLL patients, although it may be an option for relapsed patients.
Dr. Bazarbachi stressed that ATLL patients should not receive auto-HSCT at any time—as frontline consolidation, after relapse, or if they have refractory disease.
Auto-HSCT “does not work in this disease,” he said. In a study published in 20145, all four ATLL patients who underwent auto-HSCT “rapidly” died.
HSCT in ENKTL
Dr. Bazarbachi said frontline consolidation with auto-HSCT should be considered the standard of care for patients with non-localized ENKTL, nasal type.
Auto-HSCT has been shown to improve survival in these patients6, and it is most effective when patients have achieved a complete response to induction.
Allo-HSCT is also an option for frontline consolidation in patients with non-localized ENKTL, nasal type, Dr. Bazarbachi said.
He added that chemosensitive patients who have relapsed can receive allo-HSCT, but they should only receive auto-HSCT if they did not receive it in the frontline setting. Both types of transplant should take place when patients are in complete remission.
Patients with refractory, non-localized ENKTL, nasal type should not receive auto-HSCT, but allo-HSCT is an option, Dr. Bazarbachi said.
He did not declare any conflicts of interest.
1. d’Amore F et al. J Clin Oncol. 2012 Sep 1;30(25):3093-9. doi: 10.1200/JCO.2011.40.2719
2. AbouYabis AN et al. ISRN Hematol. 2011 Jun 16. doi: 10.5402/2011/623924
3. Park SI et al. Blood 2017 130:342
4. Ishida T et al. Blood 2012 Aug 23;120(8):1734-41. doi: 10.1182/blood-2012-03-414490
5. Bazarbachi A et al. Bone Marrow Transplant. 2014 Oct;49(10):1266-8. doi: 10.1038/bmt.2014.143
6. Lee J et al. Biol Blood Marrow Transplant. 2008 Dec;14(12):1356-64. doi: 10.1016/j.bbmt.2008.09.014
FDA issues draft guidance on MRD
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
The U.S. Food and Drug Administration (FDA) has issued a draft guidance on the use of minimal residual disease (MRD) assessment in trials of patients with hematologic malignancies.
The FDA said it developed this guidance to assist sponsors who are planning to use MRD as a biomarker in clinical trials conducted under an investigational new drug application or to support FDA approval of products intended to treat hematologic malignancies.
“As a result of important workshops where we’ve heard from stakeholders and an analysis of marketing applications showing inconsistent quality of MRD data, the FDA identified a need to provide sponsors with guidance on the use of MRD as a biomarker in regulatory submissions,” said FDA Commissioner Scott Gottlieb, MD.
The guidance explains how MRD might be used in clinical trials, highlights considerations for MRD assessment that are specific to certain hematologic malignancies, and lists requirements for regulatory submissions that utilize MRD.
The full document, “Hematologic Malignancies: Regulatory Considerations for Use of Minimal Residual Disease in Development of Drug and Biological Products for Treatment,” is available for download from the FDA website.
How MRD can be used
The guidance notes that MRD could potentially be used as a biomarker in clinical trials, specifically, as a diagnostic, prognostic, predictive, efficacy-response, or monitoring biomarker.
MRD could also be used as a surrogate endpoint, and there are two mechanisms for obtaining FDA feedback on the use of a novel surrogate endpoint to support approval of a product:
- The drug development tool qualification process
- Discussions with the specific Center for Drug Evaluation and Research or Center for Biologics Evaluation and Research review division.
Furthermore, a sponsor can use MRD “to select patients at high risk or to enrich the trial population,” according to the guidance.
Disease specifics
The guidance also details specific considerations for MRD assessment in individual hematologic malignancies. For example:
- In acute lymphoblastic leukemia, a patient with an MRD level of 0.1% or more in first or second complete remission has a high risk of relapse.
- In trials of acute myeloid leukemia, the sponsor should provide data showing that the marker selected to assess MRD “reflects the leukemia and not underlying clonal hematopoiesis.”
- Patients with low-risk acute promyelocytic leukemia who achieve MRD negativity after arsenic/tretinoin-based therapy are generally considered cured.
- In chronic lymphocytic leukemia, MRD can be assessed in the peripheral blood or bone marrow, but the sample source should remain the same throughout a trial.
- In chronic myeloid leukemia, MRD can be used to select and monitor patients who are eligible to discontinue treatment with tyrosine kinase inhibitors.
- In multiple myeloma, imaging techniques may be combined with MRD assessment of the bone marrow to assess patient response to treatment.
Types of technology
The guidance lists the four general technologies used for MRD assessment in hematologic malignancies:
- Multiparametric flow cytometry
- Next-generation sequencing
- Quantitative reverse transcription polymerase chain reaction of specific gene fusions
- Allele-specific oligonucleotide polymerase chain reaction.
The FDA said it does not have a preference as to which technology is used in a trial. However, the sponsor must pre-specify the technology used and should utilize the same technology throughout a trial.
The FDA also said it “does not foresee the need for co-development of an MRD assay with a drug product.” However, the assay must be analytically valid for results important to the trial, and MRD assessment must be a clinically valid biomarker in the context in which it’s used.
If the MRD assay used is not FDA-cleared or -approved, additional information about the assay must be provided to the FDA.
Inhibitor receives orphan designation for PTCL
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
Phase 1 NHL, ALL trials placed on clinical hold
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Update: On October 12, 2018, Affimed N.V. received a notification from the U.S. Food and Drug Administration (FDA) saying the agency concurred with Affimed’s decision and formally placed the investigational new drug application for AFM11 on full clinical hold. Affimed said it will comply with the FDA and other global health authorities’ requests for information to resolve the clinical hold.
Affimed N.V. has placed trials of AFM11 on clinical hold and notified the global health authorities of its decision.
AFM11 is a CD19/CD3-targeting T-cell engager being evaluated in two phase 1 trials—one in patients with relapsed or refractory, CD19-positive B-cell non-Hodgkin lymphoma (NHL) and one in adults with relapsed or refractory B-precursor acute lymphoblastic leukemia (ALL).
Affimed initiated the clinical hold on these trials after serious adverse events occurred in three patients treated with AFM11.
This included a death in the ALL study and two life-threatening events in the NHL study.
The serious adverse events occurred in patients enrolled in the highest dose cohorts of each study.
A total of 33 patients have been treated in the two studies (NCT02848911 and NCT02106091), and preliminary signs of clinical activity have been observed in several patients.
Affimed said it will be working closely with the global health authorities, safety monitoring committees, and the studies’ clinical investigators to review the adverse events, assess all the data, and determine next steps for the AFM11 program.
Affimed intends to provide an update on AFM11 upon completing the evaluation.
Variant not associated with CLL, AIHA, or ITP in certain patients
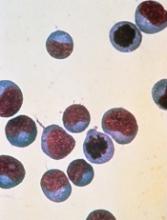
DUBROVNIK, CROATIA—New research suggests there is no association between the PTPN22 R620W polymorphism and chronic lymphocytic leukemia (CLL) or autoimmune hematologic disorders in patients from the Republic of Macedonia.
Past studies have shown an association between the PTPN22 R620W variant and both CLL1 and autoimmune diseases2 in patients from Northwest Europe.
However, a study of Macedonian patients suggests there is no association between the variant and CLL, autoimmune hemolytic anemia (AIHA), or idiopathic thrombocytopenic purpura (ITP) for patients from Southeast Europe.
Irina Panovska-Stavridis, PhD, of Ss. Cyril and Methodius University in Skopje, Republic of Macedonia, and her colleagues presented this finding at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
“A lot of data from the literature suggests [the PTPN22 R620W variant ] has a role in developing multiple immune diseases, but it is validated just in patients from Northwest Europe,” Dr. Panovska-Stavridis noted.
Therefore, she and her colleagues decided to assess the frequency of the PTPN22 R620W variant (C1858T, rs2476601) in individuals from Southeast Europe, particularly the Republic of Macedonia.
The researchers evaluated 320 patients—168 with CLL, 66 with AIHA, and 86 with ITP—and 182 age- and sex-matched control subjects with no history of malignant or autoimmune disease.
The team found a similar frequency of the minor T allele and genotype distribution in control subjects and patients.
| CLL | AIHA | ITP | Controls | |
| Minor T allele | 0.107 | 0.067 | 0.036 | 0.05 |
| CC genotype | 0.809 | 0.166 | 0.023 | 0.901 |
| CT genotype | 0.9 | 0.067 | 0.033 | 0.099 |
| TT genotype | 0.928 | 0.072 | 0 | 0 |
Dr. Panovska-Stavridis said these results suggest the PTPN22 R620W variant is not a risk factor for the development of CLL, AIHA, or ITP in patients from Southeast Europe.
She also said the results suggest the influence of the variant on lymphocytic homeostasis is affected by certain genetic and environmental factors, and the development of CLL and autoimmune diseases is influenced by race/ethnicity-based variations in the germline composition of the IGHV locus in correlation with environmental factors.
Dr. Panovska-Stavridis did not declare any conflicts of interest.
1. Hebbring S et al. Blood. 2013 121:237-238; doi: https://doi.org/10.1182/blood-2012-08-450221
2. Burb GL et al. FEBS Lett. 2011 Dec 1;585(23):3689-98. doi: 10.1016/j.febslet.2011.04.032
DUBROVNIK, CROATIA—New research suggests there is no association between the PTPN22 R620W polymorphism and chronic lymphocytic leukemia (CLL) or autoimmune hematologic disorders in patients from the Republic of Macedonia.
Past studies have shown an association between the PTPN22 R620W variant and both CLL1 and autoimmune diseases2 in patients from Northwest Europe.
However, a study of Macedonian patients suggests there is no association between the variant and CLL, autoimmune hemolytic anemia (AIHA), or idiopathic thrombocytopenic purpura (ITP) for patients from Southeast Europe.
Irina Panovska-Stavridis, PhD, of Ss. Cyril and Methodius University in Skopje, Republic of Macedonia, and her colleagues presented this finding at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
“A lot of data from the literature suggests [the PTPN22 R620W variant ] has a role in developing multiple immune diseases, but it is validated just in patients from Northwest Europe,” Dr. Panovska-Stavridis noted.
Therefore, she and her colleagues decided to assess the frequency of the PTPN22 R620W variant (C1858T, rs2476601) in individuals from Southeast Europe, particularly the Republic of Macedonia.
The researchers evaluated 320 patients—168 with CLL, 66 with AIHA, and 86 with ITP—and 182 age- and sex-matched control subjects with no history of malignant or autoimmune disease.
The team found a similar frequency of the minor T allele and genotype distribution in control subjects and patients.
| CLL | AIHA | ITP | Controls | |
| Minor T allele | 0.107 | 0.067 | 0.036 | 0.05 |
| CC genotype | 0.809 | 0.166 | 0.023 | 0.901 |
| CT genotype | 0.9 | 0.067 | 0.033 | 0.099 |
| TT genotype | 0.928 | 0.072 | 0 | 0 |
Dr. Panovska-Stavridis said these results suggest the PTPN22 R620W variant is not a risk factor for the development of CLL, AIHA, or ITP in patients from Southeast Europe.
She also said the results suggest the influence of the variant on lymphocytic homeostasis is affected by certain genetic and environmental factors, and the development of CLL and autoimmune diseases is influenced by race/ethnicity-based variations in the germline composition of the IGHV locus in correlation with environmental factors.
Dr. Panovska-Stavridis did not declare any conflicts of interest.
1. Hebbring S et al. Blood. 2013 121:237-238; doi: https://doi.org/10.1182/blood-2012-08-450221
2. Burb GL et al. FEBS Lett. 2011 Dec 1;585(23):3689-98. doi: 10.1016/j.febslet.2011.04.032
DUBROVNIK, CROATIA—New research suggests there is no association between the PTPN22 R620W polymorphism and chronic lymphocytic leukemia (CLL) or autoimmune hematologic disorders in patients from the Republic of Macedonia.
Past studies have shown an association between the PTPN22 R620W variant and both CLL1 and autoimmune diseases2 in patients from Northwest Europe.
However, a study of Macedonian patients suggests there is no association between the variant and CLL, autoimmune hemolytic anemia (AIHA), or idiopathic thrombocytopenic purpura (ITP) for patients from Southeast Europe.
Irina Panovska-Stavridis, PhD, of Ss. Cyril and Methodius University in Skopje, Republic of Macedonia, and her colleagues presented this finding at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
“A lot of data from the literature suggests [the PTPN22 R620W variant ] has a role in developing multiple immune diseases, but it is validated just in patients from Northwest Europe,” Dr. Panovska-Stavridis noted.
Therefore, she and her colleagues decided to assess the frequency of the PTPN22 R620W variant (C1858T, rs2476601) in individuals from Southeast Europe, particularly the Republic of Macedonia.
The researchers evaluated 320 patients—168 with CLL, 66 with AIHA, and 86 with ITP—and 182 age- and sex-matched control subjects with no history of malignant or autoimmune disease.
The team found a similar frequency of the minor T allele and genotype distribution in control subjects and patients.
| CLL | AIHA | ITP | Controls | |
| Minor T allele | 0.107 | 0.067 | 0.036 | 0.05 |
| CC genotype | 0.809 | 0.166 | 0.023 | 0.901 |
| CT genotype | 0.9 | 0.067 | 0.033 | 0.099 |
| TT genotype | 0.928 | 0.072 | 0 | 0 |
Dr. Panovska-Stavridis said these results suggest the PTPN22 R620W variant is not a risk factor for the development of CLL, AIHA, or ITP in patients from Southeast Europe.
She also said the results suggest the influence of the variant on lymphocytic homeostasis is affected by certain genetic and environmental factors, and the development of CLL and autoimmune diseases is influenced by race/ethnicity-based variations in the germline composition of the IGHV locus in correlation with environmental factors.
Dr. Panovska-Stavridis did not declare any conflicts of interest.
1. Hebbring S et al. Blood. 2013 121:237-238; doi: https://doi.org/10.1182/blood-2012-08-450221
2. Burb GL et al. FEBS Lett. 2011 Dec 1;585(23):3689-98. doi: 10.1016/j.febslet.2011.04.032
System may better predict thrombosis in lymphoma
DUBROVNIK, CROATIA—An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients.
Researchers found the updated ThroLy had a positive predictive value of 22% to 25%, a negative predictive value of 96%, sensitivity of 56% to 57%, and specificity of 85% to 87%.
Darko Antić, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Dr. Antić said he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients, and the Khorana score is predominantly for solid tumor malignancies.
“It’s good . . . , but it’s not specific for lymphoma patients,” Dr. Antić said.
With this in mind, he and his colleagues developed ThroLy. They based the scoring system on variables used in the Padua and Khorana systems as well as variables that are specific to lymphoma patients.
In a past study*, the researchers found several variables that were independently associated with risk for VTE in lymphoma:
- Previous VTE
- Previous acute myocardial infarction/stroke
- Mediastinal involvement
- Body mass index > 30 kg/m2
- Reduced mobility
- Extranodal localization
- Development of neutropenia
- Hemoglobin level < 100g/L.
Previous VTE, previous acute myocardial infarction/stroke, obesity, and mediastinal involvement were all worth 2 points, and the other factors were worth a single point.
Patients with scores of 0 to 1 were considered low-risk, patients with scores of 2 to 3 were considered intermediate-risk, and patients with scores of 4 or greater were considered high-risk.
Prospective validation
To validate and refine ThroLy, Dr. Antić and his colleagues used it to assess 1723 lymphoma patients treated at 8 institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma (n=467), aggressive non-Hodgkin lymphoma (n=647), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=235), and Hodgkin lymphoma (n=366). Most subjects (84%) were outpatients.
Nine percent of patients had thrombosis (n=142), with 7% having VTE (n=121).
ThroLy had a positive predictive value of 17%, compared to 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively.
The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua. The specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antić noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models.
Model 1 included the following variables:
- Type of lymphoma/clinical stage (aggressive/advanced)—1 point
- Previous VTE—5 points
- Reduced mobility—2 points
- Hemoglobin level < 100 g/L—1 point
- Presence of vascular devices—1 point.
Model 2 included all of the aforementioned variables as well as thrombophilic condition, which was worth 1 point.
With these models, patients were divided into two risk groups—low-risk (≤ 2 points) and high-risk (>2 points).
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%.
For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
Dr. Antić said there were no major differences in model discrimination and calibration according to the country in which a patient was treated or whether patients were treated in inpatient or outpatient settings.
Dr. Antić did not report any conflicts of interest.
*Antić D et al. Am J Hematol. 2016 Oct;91(10):1014-9. doi: 10.1002/ajh.24466.
DUBROVNIK, CROATIA—An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients.
Researchers found the updated ThroLy had a positive predictive value of 22% to 25%, a negative predictive value of 96%, sensitivity of 56% to 57%, and specificity of 85% to 87%.
Darko Antić, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Dr. Antić said he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients, and the Khorana score is predominantly for solid tumor malignancies.
“It’s good . . . , but it’s not specific for lymphoma patients,” Dr. Antić said.
With this in mind, he and his colleagues developed ThroLy. They based the scoring system on variables used in the Padua and Khorana systems as well as variables that are specific to lymphoma patients.
In a past study*, the researchers found several variables that were independently associated with risk for VTE in lymphoma:
- Previous VTE
- Previous acute myocardial infarction/stroke
- Mediastinal involvement
- Body mass index > 30 kg/m2
- Reduced mobility
- Extranodal localization
- Development of neutropenia
- Hemoglobin level < 100g/L.
Previous VTE, previous acute myocardial infarction/stroke, obesity, and mediastinal involvement were all worth 2 points, and the other factors were worth a single point.
Patients with scores of 0 to 1 were considered low-risk, patients with scores of 2 to 3 were considered intermediate-risk, and patients with scores of 4 or greater were considered high-risk.
Prospective validation
To validate and refine ThroLy, Dr. Antić and his colleagues used it to assess 1723 lymphoma patients treated at 8 institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma (n=467), aggressive non-Hodgkin lymphoma (n=647), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=235), and Hodgkin lymphoma (n=366). Most subjects (84%) were outpatients.
Nine percent of patients had thrombosis (n=142), with 7% having VTE (n=121).
ThroLy had a positive predictive value of 17%, compared to 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively.
The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua. The specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antić noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models.
Model 1 included the following variables:
- Type of lymphoma/clinical stage (aggressive/advanced)—1 point
- Previous VTE—5 points
- Reduced mobility—2 points
- Hemoglobin level < 100 g/L—1 point
- Presence of vascular devices—1 point.
Model 2 included all of the aforementioned variables as well as thrombophilic condition, which was worth 1 point.
With these models, patients were divided into two risk groups—low-risk (≤ 2 points) and high-risk (>2 points).
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%.
For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
Dr. Antić said there were no major differences in model discrimination and calibration according to the country in which a patient was treated or whether patients were treated in inpatient or outpatient settings.
Dr. Antić did not report any conflicts of interest.
*Antić D et al. Am J Hematol. 2016 Oct;91(10):1014-9. doi: 10.1002/ajh.24466.
DUBROVNIK, CROATIA—An updated scoring system can more accurately identify lymphoma patients who may require thromboprophylaxis, according to researchers.
The revised scoring system, ThroLy, proved more effective than other systems for predicting thromboembolic events in lymphoma patients.
Researchers found the updated ThroLy had a positive predictive value of 22% to 25%, a negative predictive value of 96%, sensitivity of 56% to 57%, and specificity of 85% to 87%.
Darko Antić, MD, PhD, of the University of Belgrade in Serbia, presented these findings at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Dr. Antić said he and his colleagues developed ThroLy because other systems used to predict venous thromboembolism (VTE) are not quite right for lymphoma. He noted that the Padua score is not designed for cancer patients, and the Khorana score is predominantly for solid tumor malignancies.
“It’s good . . . , but it’s not specific for lymphoma patients,” Dr. Antić said.
With this in mind, he and his colleagues developed ThroLy. They based the scoring system on variables used in the Padua and Khorana systems as well as variables that are specific to lymphoma patients.
In a past study*, the researchers found several variables that were independently associated with risk for VTE in lymphoma:
- Previous VTE
- Previous acute myocardial infarction/stroke
- Mediastinal involvement
- Body mass index > 30 kg/m2
- Reduced mobility
- Extranodal localization
- Development of neutropenia
- Hemoglobin level < 100g/L.
Previous VTE, previous acute myocardial infarction/stroke, obesity, and mediastinal involvement were all worth 2 points, and the other factors were worth a single point.
Patients with scores of 0 to 1 were considered low-risk, patients with scores of 2 to 3 were considered intermediate-risk, and patients with scores of 4 or greater were considered high-risk.
Prospective validation
To validate and refine ThroLy, Dr. Antić and his colleagues used it to assess 1723 lymphoma patients treated at 8 institutions in Austria, Croatia, France, Jordan, Macedonia, Spain, Switzerland, and the United States.
Patients had indolent non-Hodgkin lymphoma (n=467), aggressive non-Hodgkin lymphoma (n=647), chronic lymphocytic leukemia/small lymphocytic lymphoma (n=235), and Hodgkin lymphoma (n=366). Most subjects (84%) were outpatients.
Nine percent of patients had thrombosis (n=142), with 7% having VTE (n=121).
ThroLy had a positive predictive value of 17%, compared to 11% with Khorana and 13% with Padua. The negative predictive value was 93%, 92%, and 95%, respectively.
The sensitivity was 51% with ThroLy, 42% with Khorana, and 70% with Padua. The specificity was 72%, 64%, and 52%, respectively.
“The positive predictive value was low [with ThroLy] but definitely higher than the positive predictive value of the other two [scoring systems],” Dr. Antić noted.
Updated models
To further improve ThroLy, the researchers updated the system, creating two new models.
Model 1 included the following variables:
- Type of lymphoma/clinical stage (aggressive/advanced)—1 point
- Previous VTE—5 points
- Reduced mobility—2 points
- Hemoglobin level < 100 g/L—1 point
- Presence of vascular devices—1 point.
Model 2 included all of the aforementioned variables as well as thrombophilic condition, which was worth 1 point.
With these models, patients were divided into two risk groups—low-risk (≤ 2 points) and high-risk (>2 points).
For Model 1, the positive predictive value was 22%, the negative predictive value was 96%, the sensitivity was 56%, and the specificity was 85%.
For Model 2, the positive predictive value was 25%, the negative predictive value was 96%, the sensitivity was 57%, and the specificity was 87%.
Dr. Antić said there were no major differences in model discrimination and calibration according to the country in which a patient was treated or whether patients were treated in inpatient or outpatient settings.
Dr. Antić did not report any conflicts of interest.
*Antić D et al. Am J Hematol. 2016 Oct;91(10):1014-9. doi: 10.1002/ajh.24466.
Duvelisib bests ofatumumab as monotherapy for treatment of CLL/SLL
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
Final analysis of the phase 3 DUO trial has shown monotherapy with oral duvelisib results in a statistically significant improvement in progression-free survival (PFS) and overall response rate (ORR) compared to monotherapy with ofatumumab for patients with relapsed or refractory chronic lymphocytic leukemia/small lympchocytic lymphoma (CLL/SLL).
PFS for all patients as assessed by Independent Review Committee (IRC) was a median 13.3 months with duvelisib compared to 9.9 months with ofatumumab (P<0.0001).
ORR was significantly higher with duvelisib, 74% compared to 45%, P<0.0001, regardless of deletion 17p status.
Duvelisib (Copiktra™) was recently approved by the U.S. Food and Drug Administration for CLL/SLL based in part on this head-to-head trial.
The investigators reported the results in Blood.
"The way we treat patients with CLL is changing rapidly as we move from standard chemotherapy-based approaches to more targeted therapies," said principal investigator Ian W. Flinn, MD, PhD, of Sarah Cannon Research Institute in Nashville.
"Based on these data, duvelisib may offer a new treatment option for patients who otherwise may have limited options."
Duvelisib is an oral, dual inhibitor of phosphoinositide 3-kinase (PI3K)-δ and -γ, which means it blocks the survival and proliferation of malignant B cells and also disrupts the recruitment and differentiation of T cells and macrophages within the tumor microenvironment.
Ofatumumab is a humanized anti-CD20 antibody with single-agent efficacy in refractory CLL. It is approved by the FDA as a treatment option in CLL.
Study design
Investigators randomized 319 relapsed or refractory CLL/SLL patients, 160 to the duvelisib arm and 159 to the ofatumumab arm.
Patients in the duvelisib arm self-administered 25 mg capsules twice daily continuously in 28-day cycles. They could take duvelisib for up to 18 cycles, until disease progression or unacceptable toxicity.
Ofatumumab-treated patients received infusions as approved in the product labeling for monotherapy in relapsed CLL. Dosing of ofatumumab could not exceed 12 doses in 7 cycles.
Prophylaxis for Pneumocystis jirovecci was required for all patients on both treatment arms.
Patients were allowed to crossover to a separate extension study to receive the opposite therapy if they had progressive disease.
They were followed for a median of 22.4 months.
Patient characteristics
According to the investigators, patient characteristics were well balanced between the arms.
The majority (60%) were male and the median age in both arms was 69. Most had an ECOG performance status of 0 or 1; 7% in the duvelisib arm and 10% in the ofatumumab arm had a performance status of 2.
Other patient characteristics in the duvelisib and ofatumumab arms, respectively, were:
- Time from initial diagnosis: 7.5 years, 6.7 years
- CLL/SLL, %: 97/5, 99/2
- Bulky disease: 46%, 45%
- Baseline lymphocyte counts: 38x109/L, 35x109/L
- Deletion 17p and/or TP53 mutation: 31%, 33%
- Median number of prior therapies: 2 in each arm
- Previous alkylating agent: 93%, 95%
- Previous monoclonal antibody: 78%, 83%
- Prior purine analog: 60%, 71%
Of the total patients enrolled, 158 patients in the duvelisib arm and 155 in the ofatumumab arm received treatment, for a median exposure of 50 weeks and 23 weeks, respectively.
Efficacy
In addition to the significantly improved overall PFS and ORR with duvelisib, further analysis revealed that PFS also improved for all predefined subgroups.
High-risk patients with deletion 17p/TP53 mutations also experienced a significant improvement in PFS with duvelisib of 12.7 months compared to 9.0 months with ofatumumab by IRC (P=0.0002).
The estimated probability of being progression-free for these patients at 6 and 12 moths was 73% and 55% with duvelisib and 63% and 30% with ofatumumab.
The investigators pointed out that duvelisib treatment was particularly effective in eliciting a lymph node response—85.0% compared to 15.7% with ofatumumab as assessed by IRC (P<0.0001).
Median overall survival was not reached in either arm. The 12-month probability of survival was 86% for both treatments.
Safety
Median treatment exposure was almost twice as long in the duvelisib arm because ofatumumab treatment was not allowed to exceed 12 doses as specified in the prescribing information.
The investigators explained this resulted in a longer adverse event (AE) reporting period for duvelisib.
One hundred twenty-four duvelisib-treated patients discontinued treatment, most commonly due to AEs (35%), disease progression (22%), subject withdrawal (8%), and death (8%).
All ofatumumab-treated patients discontinued treatment by the time of data cutoff, and 67% had completed treatment as per protocol. Others discontinued due to disease progression (20%), subject withdrawal (5%), and AEs (4%).
Eight (5%) duvelisib patients crossed over to ofatumumab therapy at the time of disease progression, and 89 (57%) ofatumumab-treated patients crossed over to duvelisib.
Nearly all patients in both arms experienced an AE.
The most common hematologic malignancies with duvelisib and ofatumumab, respectively, occurring in 10% or more patients were neutropenia (33%, 21%), anemia (23%, 10%), and thrombocytopenia (15%, 6%).
The most common nonhematologic AES with duvelisib were diarrhea (51%), pyrexia (29%), nausea (23%), and cough (21%).
With ofatumumab, the most common nonhematologic AES were infusion-related reaction (19%), cough (14%), and diarrhea, rash, and fatigue (12% each).
Grade 3 or greater AEs occurred in 87% of duvelisib-treated patients and 48% in the ofatumumab arm.
The most common grade 3 or greater events with duvelisib were neutropenia (30%), diarrhea (15%), pneumonia (14%), and anemia (13%).
With ofatumumab, only neutropenia (17%) of grade 3 or higher occurred in 10% or more patients.
Severe immune-related toxicities with duvelisib included colitis (12%) and pneumonitis, alanine transaminase (ALT) or aspartate transaminase (AST) increase (3% each). The events were managed with dose interruptions and steroid therapy for pneumonitis or colitis. All reported events resolved, and none was fatal.
Infectious AEs occurred more frequently with duvelisib, 69% compared to 43% in the ofatumumab arm. Pneumonia (18%) and upper respiratory tract infection (16%) were the most common events.
Three patients in the duvelisib arm and 1 in the ofatumumab arm contracted Pneumocystis jirovecii.
The most frequently reported serious AE was pneumonia (duvelisib 15%; ofatumumab 3%).
Nineteen fatal AEs occurred in patients on the duvelisib arm, 4 of which were related to the study drug: staphylococcal pneumonia (n = 2), sepsis (n=1), and general health deterioration (n = 1).
Seven fatal AEs occurred in patients on the ofatumumab arm, although none was attributed to ofatumumab.
The DUO trial was sponsored by Verastem Oncology and Infinity Pharmaceuticals , Inc.
FDA lifts partial hold on tazemetostat trials
The U.S. Food and Drug Administration (FDA) has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The FDA had placed the hold in April, and this halted U.S.-based enrollment of new patients in tazemetostat clinical trials.
Now, Epizyme, Inc., the company developing tazemetostat, is in the process of reopening enrollment in all company-sponsored trials in the U.S.
The FDA had placed the partial hold on tazemetostat trials after an adverse event was observed in a pediatric patient on a phase 1 study.
The patient, who had advanced poorly differentiated chordoma, developed secondary T-cell lymphoblastic lymphoma (T-LBL) while taking tazemetostat. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” said Robert Bazemore, president and chief executive officer of Epizyme.
Due to this adverse event and the partial clinical hold, Epizyme began to assess the risk of T-LBL and other secondary malignancies potentially associated with tazemetostat.
The company also assessed the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials.
Epizyme concluded that the benefits of tazemetostat outweigh the risks, and the risk of T-LBL appears confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
Epizyme convened a panel of external scientific and medical experts who reviewed and validated the company’s findings.
“The team at Epizyme has worked diligently in collaboration with external experts and FDA over the past several months, culminating in decisions . . . to lift the partial clinical hold and allow re-opening of enrollment in our clinical trials,” Bazemore said.
He noted that the company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials.
However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies.
Bazemore said the lifting of the partial clinical hold allows Epizyme to turn its full attention to key priorities, including plans to submit a new drug application for tazemetostat in epithelioid sarcoma.
The company also plans to begin preparing for a potential new drug application for tazemetostat in follicular lymphoma.
Tazemetostat is currently under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid tumor malignancies. The drug is also being studied as part of combination therapy for non-small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Now that Epizyme has resolved the U.S. hold on tazemetostat trials, the company is working to resolve partial clinical holds placed in France and Germany to resume trial enrollment in those countries.
The U.S. Food and Drug Administration (FDA) has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The FDA had placed the hold in April, and this halted U.S.-based enrollment of new patients in tazemetostat clinical trials.
Now, Epizyme, Inc., the company developing tazemetostat, is in the process of reopening enrollment in all company-sponsored trials in the U.S.
The FDA had placed the partial hold on tazemetostat trials after an adverse event was observed in a pediatric patient on a phase 1 study.
The patient, who had advanced poorly differentiated chordoma, developed secondary T-cell lymphoblastic lymphoma (T-LBL) while taking tazemetostat. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” said Robert Bazemore, president and chief executive officer of Epizyme.
Due to this adverse event and the partial clinical hold, Epizyme began to assess the risk of T-LBL and other secondary malignancies potentially associated with tazemetostat.
The company also assessed the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials.
Epizyme concluded that the benefits of tazemetostat outweigh the risks, and the risk of T-LBL appears confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
Epizyme convened a panel of external scientific and medical experts who reviewed and validated the company’s findings.
“The team at Epizyme has worked diligently in collaboration with external experts and FDA over the past several months, culminating in decisions . . . to lift the partial clinical hold and allow re-opening of enrollment in our clinical trials,” Bazemore said.
He noted that the company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials.
However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies.
Bazemore said the lifting of the partial clinical hold allows Epizyme to turn its full attention to key priorities, including plans to submit a new drug application for tazemetostat in epithelioid sarcoma.
The company also plans to begin preparing for a potential new drug application for tazemetostat in follicular lymphoma.
Tazemetostat is currently under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid tumor malignancies. The drug is also being studied as part of combination therapy for non-small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Now that Epizyme has resolved the U.S. hold on tazemetostat trials, the company is working to resolve partial clinical holds placed in France and Germany to resume trial enrollment in those countries.
The U.S. Food and Drug Administration (FDA) has lifted the partial clinical hold on trials of tazemetostat, an EZH2 inhibitor being developed to treat solid tumors and lymphomas.
The FDA had placed the hold in April, and this halted U.S.-based enrollment of new patients in tazemetostat clinical trials.
Now, Epizyme, Inc., the company developing tazemetostat, is in the process of reopening enrollment in all company-sponsored trials in the U.S.
The FDA had placed the partial hold on tazemetostat trials after an adverse event was observed in a pediatric patient on a phase 1 study.
The patient, who had advanced poorly differentiated chordoma, developed secondary T-cell lymphoblastic lymphoma (T-LBL) while taking tazemetostat. The patient has since discontinued tazemetostat and responded to treatment for T-LBL.
“This remains the only case of T-LBL we’ve seen in more than 750 patients treated with tazemetostat,” said Robert Bazemore, president and chief executive officer of Epizyme.
Due to this adverse event and the partial clinical hold, Epizyme began to assess the risk of T-LBL and other secondary malignancies potentially associated with tazemetostat.
The company also assessed the overall risks and benefits of tazemetostat treatment, conducting a review of the published literature and an examination of efficacy and safety data across all of its tazemetostat trials.
Epizyme concluded that the benefits of tazemetostat outweigh the risks, and the risk of T-LBL appears confined to pediatric patients who received higher doses of the drug. The phase 1 pediatric study in which the patient developed T-LBL included higher doses of tazemetostat than those used in the phase 2 adult studies.
Epizyme convened a panel of external scientific and medical experts who reviewed and validated the company’s findings.
“The team at Epizyme has worked diligently in collaboration with external experts and FDA over the past several months, culminating in decisions . . . to lift the partial clinical hold and allow re-opening of enrollment in our clinical trials,” Bazemore said.
He noted that the company is not making any substantial changes to trial designs or the patient populations involved in tazemetostat trials.
However, Epizyme is modifying dosing in the pediatric studies, improving patient monitoring, and making changes to exclusion criteria to reduce the potential risk of T-LBL and other secondary malignancies.
Bazemore said the lifting of the partial clinical hold allows Epizyme to turn its full attention to key priorities, including plans to submit a new drug application for tazemetostat in epithelioid sarcoma.
The company also plans to begin preparing for a potential new drug application for tazemetostat in follicular lymphoma.
Tazemetostat is currently under investigation as monotherapy in phase 2 trials of follicular lymphoma and solid tumor malignancies. The drug is also being studied as part of combination therapy for non-small cell lung cancer and diffuse large B-cell lymphoma (DLBCL).
In August, Epizyme announced its decision to stop developing tazemetostat for use as monotherapy or in combination with prednisolone for patients with DLBCL. However, tazemetostat is still under investigation as a potential treatment for DLBCL as part of other combination regimens.
Now that Epizyme has resolved the U.S. hold on tazemetostat trials, the company is working to resolve partial clinical holds placed in France and Germany to resume trial enrollment in those countries.
FDA approves duvelisib for CLL/SLL and FL
The U.S. Food and Drug Administration (FDA) has approved duvelisib (Copiktra™), a dual PI3K delta/gamma inhibitor, for two indications.
Duvelisib has full FDA approval to treat adults with relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) who have received at least two prior therapies.
Duvelisib also has accelerated approval to treat adults with relapsed or refractory follicular lymphoma (FL) who have received at least two prior systemic therapies.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit. Continued approval of duvelisib in FL may be contingent upon results of confirmatory trials verifying that the drug provides a clinical benefit.
Duvelisib will be available in the U.S. immediately, according to Verastem Inc., the company marketing the drug.
Verastem said it will help patients access duvelisib through the Verastem Cares™ program, which is designed to provide information and assistance to patients who are prescribed duvelisib.
The prescribing information for duvelisib includes a boxed warning detailing four fatal and/or serious toxicities associated with the drug—infections, diarrhea or colitis, cutaneous reactions, and pneumonitis.
Verastem said it is implementing an informational risk evaluation and mitigation strategy to provide appropriate dosing and safety information for duvelisib.
The recommended dose of duvelisib is 25 mg orally twice daily, taken continuously in 28-day treatment cycles.
The FDA assessed the new drug application for duvelisib under priority review. The FDA also granted duvelisib fast track designation in CLL and FL as well as orphan drug designation for CLL/SLL and FL.
The FDA’s approval of duvelisib is supported by data from the phase 3 DUO trial and the phase 2 DYNAMO trial. Updated results from both studies are available in the prescribing information for duvelisib.
DUO trial
DUO included 319 patients with CLL (n=312) or SLL (n=7) who had received at least one prior therapy. They were randomized to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The following efficacy results were observed in patients who had received at least two prior therapies, which includes 95 patients in the duvelisib arm and 101 in the ofatumumab arm.
The overall response rate was 78% in the duvelisib arm and 39% in the ofatumumab arm. All responses in both arms were partial responses.
The median progression-free survival was 16.4 months with duvelisib and 9.1 months with ofatumumab (hazard ratio=0.40).
The safety results include all patients treated with duvelisib or ofatumumab.
Twelve percent of patients in the duvelisib arm had fatal adverse events (AEs) within 30 days of the last dose. The same was true of 4% of patients treated with ofatumumab.
Serious AEs occurred in 73% of patients treated with duvelisib. The most common were infection (38%) and diarrhea/colitis (23%).
Thirty-six percent of patients discontinued duvelisib. Most discontinuations were due to diarrhea/ colitis, infection, and rash. Twenty-nine percent of patients in the duvelisib arm required dose reductions, most often due to diarrhea/colitis and rash.
DYNAMO trial
DYNAMO enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate was 42%. One patient achieved a complete response, and 34 had a partial response.
Forty-three percent of responders maintained their response at 6 months, and 17% maintained their response at 12 months.
Serious AEs occurred in 58% of FL patients. The most common were diarrhea/colitis, pneumonia, renal insufficiency, rash, and sepsis.
AEs occurring in at least 20% of FL patients included diarrhea/colitis, nausea, fatigue, musculoskeletal pain, rash, neutropenia, cough, anemia, pyrexia, headache, mucositis, abdominal pain, vomiting, transaminase elevation, and thrombocytopenia.
Twenty-nine percent of FL patients discontinued duvelisib, and 23% had dose reductions. Most discontinuations were due to diarrhea/colitis and rash, and most dose reductions were due to transaminase elevation, diarrhea/colitis, lipase increase, and infection.
The U.S. Food and Drug Administration (FDA) has approved duvelisib (Copiktra™), a dual PI3K delta/gamma inhibitor, for two indications.
Duvelisib has full FDA approval to treat adults with relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) who have received at least two prior therapies.
Duvelisib also has accelerated approval to treat adults with relapsed or refractory follicular lymphoma (FL) who have received at least two prior systemic therapies.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit. Continued approval of duvelisib in FL may be contingent upon results of confirmatory trials verifying that the drug provides a clinical benefit.
Duvelisib will be available in the U.S. immediately, according to Verastem Inc., the company marketing the drug.
Verastem said it will help patients access duvelisib through the Verastem Cares™ program, which is designed to provide information and assistance to patients who are prescribed duvelisib.
The prescribing information for duvelisib includes a boxed warning detailing four fatal and/or serious toxicities associated with the drug—infections, diarrhea or colitis, cutaneous reactions, and pneumonitis.
Verastem said it is implementing an informational risk evaluation and mitigation strategy to provide appropriate dosing and safety information for duvelisib.
The recommended dose of duvelisib is 25 mg orally twice daily, taken continuously in 28-day treatment cycles.
The FDA assessed the new drug application for duvelisib under priority review. The FDA also granted duvelisib fast track designation in CLL and FL as well as orphan drug designation for CLL/SLL and FL.
The FDA’s approval of duvelisib is supported by data from the phase 3 DUO trial and the phase 2 DYNAMO trial. Updated results from both studies are available in the prescribing information for duvelisib.
DUO trial
DUO included 319 patients with CLL (n=312) or SLL (n=7) who had received at least one prior therapy. They were randomized to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The following efficacy results were observed in patients who had received at least two prior therapies, which includes 95 patients in the duvelisib arm and 101 in the ofatumumab arm.
The overall response rate was 78% in the duvelisib arm and 39% in the ofatumumab arm. All responses in both arms were partial responses.
The median progression-free survival was 16.4 months with duvelisib and 9.1 months with ofatumumab (hazard ratio=0.40).
The safety results include all patients treated with duvelisib or ofatumumab.
Twelve percent of patients in the duvelisib arm had fatal adverse events (AEs) within 30 days of the last dose. The same was true of 4% of patients treated with ofatumumab.
Serious AEs occurred in 73% of patients treated with duvelisib. The most common were infection (38%) and diarrhea/colitis (23%).
Thirty-six percent of patients discontinued duvelisib. Most discontinuations were due to diarrhea/ colitis, infection, and rash. Twenty-nine percent of patients in the duvelisib arm required dose reductions, most often due to diarrhea/colitis and rash.
DYNAMO trial
DYNAMO enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate was 42%. One patient achieved a complete response, and 34 had a partial response.
Forty-three percent of responders maintained their response at 6 months, and 17% maintained their response at 12 months.
Serious AEs occurred in 58% of FL patients. The most common were diarrhea/colitis, pneumonia, renal insufficiency, rash, and sepsis.
AEs occurring in at least 20% of FL patients included diarrhea/colitis, nausea, fatigue, musculoskeletal pain, rash, neutropenia, cough, anemia, pyrexia, headache, mucositis, abdominal pain, vomiting, transaminase elevation, and thrombocytopenia.
Twenty-nine percent of FL patients discontinued duvelisib, and 23% had dose reductions. Most discontinuations were due to diarrhea/colitis and rash, and most dose reductions were due to transaminase elevation, diarrhea/colitis, lipase increase, and infection.
The U.S. Food and Drug Administration (FDA) has approved duvelisib (Copiktra™), a dual PI3K delta/gamma inhibitor, for two indications.
Duvelisib has full FDA approval to treat adults with relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) who have received at least two prior therapies.
Duvelisib also has accelerated approval to treat adults with relapsed or refractory follicular lymphoma (FL) who have received at least two prior systemic therapies.
Accelerated approval is based on a surrogate or intermediate endpoint—in this case, overall response rate—that is reasonably likely to predict clinical benefit. Continued approval of duvelisib in FL may be contingent upon results of confirmatory trials verifying that the drug provides a clinical benefit.
Duvelisib will be available in the U.S. immediately, according to Verastem Inc., the company marketing the drug.
Verastem said it will help patients access duvelisib through the Verastem Cares™ program, which is designed to provide information and assistance to patients who are prescribed duvelisib.
The prescribing information for duvelisib includes a boxed warning detailing four fatal and/or serious toxicities associated with the drug—infections, diarrhea or colitis, cutaneous reactions, and pneumonitis.
Verastem said it is implementing an informational risk evaluation and mitigation strategy to provide appropriate dosing and safety information for duvelisib.
The recommended dose of duvelisib is 25 mg orally twice daily, taken continuously in 28-day treatment cycles.
The FDA assessed the new drug application for duvelisib under priority review. The FDA also granted duvelisib fast track designation in CLL and FL as well as orphan drug designation for CLL/SLL and FL.
The FDA’s approval of duvelisib is supported by data from the phase 3 DUO trial and the phase 2 DYNAMO trial. Updated results from both studies are available in the prescribing information for duvelisib.
DUO trial
DUO included 319 patients with CLL (n=312) or SLL (n=7) who had received at least one prior therapy. They were randomized to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The following efficacy results were observed in patients who had received at least two prior therapies, which includes 95 patients in the duvelisib arm and 101 in the ofatumumab arm.
The overall response rate was 78% in the duvelisib arm and 39% in the ofatumumab arm. All responses in both arms were partial responses.
The median progression-free survival was 16.4 months with duvelisib and 9.1 months with ofatumumab (hazard ratio=0.40).
The safety results include all patients treated with duvelisib or ofatumumab.
Twelve percent of patients in the duvelisib arm had fatal adverse events (AEs) within 30 days of the last dose. The same was true of 4% of patients treated with ofatumumab.
Serious AEs occurred in 73% of patients treated with duvelisib. The most common were infection (38%) and diarrhea/colitis (23%).
Thirty-six percent of patients discontinued duvelisib. Most discontinuations were due to diarrhea/ colitis, infection, and rash. Twenty-nine percent of patients in the duvelisib arm required dose reductions, most often due to diarrhea/colitis and rash.
DYNAMO trial
DYNAMO enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate was 42%. One patient achieved a complete response, and 34 had a partial response.
Forty-three percent of responders maintained their response at 6 months, and 17% maintained their response at 12 months.
Serious AEs occurred in 58% of FL patients. The most common were diarrhea/colitis, pneumonia, renal insufficiency, rash, and sepsis.
AEs occurring in at least 20% of FL patients included diarrhea/colitis, nausea, fatigue, musculoskeletal pain, rash, neutropenia, cough, anemia, pyrexia, headache, mucositis, abdominal pain, vomiting, transaminase elevation, and thrombocytopenia.
Twenty-nine percent of FL patients discontinued duvelisib, and 23% had dose reductions. Most discontinuations were due to diarrhea/colitis and rash, and most dose reductions were due to transaminase elevation, diarrhea/colitis, lipase increase, and infection.