User login
Inhibitor outperforms rivals in leukemia, lymphoma
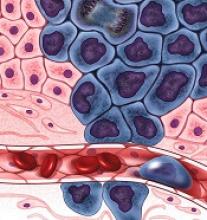
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
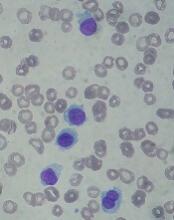
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
CHICAGO—Preclinical research suggests the pan-FLT3/pan-BTK inhibitor CG’806 is more effective than other kinase inhibitors in fighting certain hematologic malignancies.
In one study, CG’806 proved more potent than comparator drugs in primary samples of acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
In another study, CG’806 demonstrated greater cytotoxicity than comparators in a range of malignant B cell lines.
Data from both studies were presented at the AACR Annual Meeting 2018 (abstracts 791 and 794).
The research was supported by Aptose Biosciences, Inc., the company developing CG’806.
CG’806 is a small molecule that inhibits wild-type (WT) FLT3, as well as FLT3 housing the ITD mutation or with point mutations in the tyrosine kinase domain (TKD, including D835G, D835Y, D835H) or in the gatekeeper region (F691L). CG’806 also inhibits BTK-WT and BTK-C481S.
Stephen E. Kurtz, PhD, of Oregon Health & Science University in Portland, and his colleagues presented results with CG’806 in primary patient samples.
The team found that CG’806 demonstrated greater potency against AML samples relative to other FLT3 inhibitors.
Median IC50 values in 188 AML patient samples were 0.0765 µM for CG’806, 0.125 µM for gilteritinib, 0.199 µM for quizartinib, 0.551 µM for dovitinib, 2.25 µM for midostaurin, 2.93 µM for sorafenib, and 5.01 µM for crenolanib.
The researchers said CG’806 sensitivity was enhanced in FLT3-ITD and FLT3-TKD positive cases.
In CLL patient samples, CG’806 exhibited greater potency and a greater range of activity than the BTK inhibitor ibrutinib. Across 95 CLL samples, the median IC50 values were 0.114 µM for CG’806 and 4.09 µM for ibrutinib.
The researchers said this greater potency of CG’806 may be due to the activity of CG’806 on CSF1R, which has been identified as a therapeutic target in CLL.
“The clinical benefit of current FLT3 inhibitors in AML is transient, as resistance develops after several months of treatment,” Dr Kurtz noted. “Similarly, ibrutinib . . . is limited by acquired resistance as well as refractory disease and tolerance challenges. As a pan-FLT3/pan-BTK inhibitor . . ., CG’806 offers important potential to address these limitations.”
Hongying Zhang, MD, PhD, of Aptose Biosciences, and her colleagues presented results with CG’806 in malignant B-cell and AML cell lines.
The researchers found that CG’806 inhibited FLT3-ITD signaling and induced apoptosis more effectively than quizartinib in FLT3-ITD AML cells (MV4-11). The team noted that CG’806 caused G0/G1 cell-cycle arrest in the cells.
CG’806 also exhibited greater cytotoxic activity than quizartinib in FLT3-WT AML cell lines (KG-1 and NOMO-1).
In addition, CG’806 was more potent than quizartinib, gilteritinib, and crenolanib in Ba/F3 cells transfected with FLT3-WT, ITD, D835Y, and ITD-F691. CG’806 was more potent than quizartinib and crenolanib—but not gilteritinib—in Ba/F3 cells transfected with FLT3-ITD-D835Y.
The researchers said they found that CG’806 inhibits BTK, AURK, and downstream signals in FLT3-WT AML cells.
The team also found that CG’806 decreased BTK phosphorylation in all tested cell lines of B-cell malignancies. This included acute lymphoblastic leukemia, mantle cell lymphoma, Burkitt lymphoma, diffuse large B-cell lymphoma, and follicular lymphoma cell lines.
Across all cell lines, CG’806 killed malignant B cells more effectively than ibrutinib. And CG’806 was “equally potent” against WT and C481S-mutant BTK, according to the researchers.
The team also said CG’806 inhibited AURK and induced polyploidy in B-cell malignancies.
“[C]G’806 has demonstrated the ability to kill a broad range of AML and B-cell malignancies through inhibition of multiple oncogenic pathways,” said William G. Rice, PhD, chairman and chief executive officer of Aptose.
“These studies are critical for understanding how to develop and position CG’806 as we prepare for clinical development in these challenging hematologic malignancies.”
Team uses iPSCs to create ‘universal’ CAR T cells
CHICAGO—Researchers have used induced pluripotent stem cells (iPSCs) to create a “universal” chimeric antigen receptor (CAR) T-cell therapy known as FT819.
The team says FT819 has the potential to be mass-produced, stored, and made readily available for cancer patients.
In in vitro experiments, FT819 demonstrated activity against leukemia and lymphoma.
These results were presented at the AACR Annual Meeting 2018 (abstract LB-108).
The research was conducted by employees of Fate Therapeutics, Inc., the company developing FT819, as well as Memorial Sloan-Kettering Cancer Center.
About FT819
FT819 is produced from a master iPSC line generated using T cells from healthy donors.
“A master iPSC line has unlimited capacity to self-renew and can be banked and renewably used,” said Bob Valamehr, PhD, vice-president of cancer immunotherapy at Fate Therapeutics, Inc.
“We started with cells from a healthy donor rather than the patient, created a master cell line, and used the master cell line to produce large quantities of ‘universal’ CAR19 T cells that are not patient-restricted. These first-of-kind CAR19 T cells, called FT819, can be packaged, stored, and made readily available for treatment of a large number of patients.”
FT819 has 2 targeting receptors—a CAR targeting CD19-positive tumor cells and a CD16 Fc receptor that can engage other therapies (such as tumor antigen-targeting monoclonal antibodies) to overcome antigen escape.
The master iPSC line used for the production of FT819 is engineered in a one-time event to insert a CD19 CAR into the T-cell receptor α constant (TRAC) locus. This is done to eliminate T-cell receptor expression and reduce the likelihood of graft-versus-host disease.
Previous research showed that targeting a CAR to the TRAC locus results in uniform CAR expression and enhances T-cell potency. In fact, TRAC-CAR T cells outperformed conventionally generated CAR T cells by preventing T-cell exhaustion in a mouse model of acute lymphoblastic leukemia.
In vitro experiments
With the current work, the researchers found that FT819 displayed an efficient cytotoxic T-cell response when challenged with CD19-positive tumor cells. FT819 produced cytokines (IFN-gamma, TNF-alpha, and IL-2) and mediators of cell death (CD107a/b, perforin, and granzyme B).
FT819 was also target-specific, attacking only CD19-positive tumor cells and sparing CD19-negative tumor cells in experiments with Raji (Burkitt lymphoma) and Nalm-6 (B-cell acute lymphoblastic leukemia) cell lines.
The researchers said they observed consistent antigen-specific cytotoxicity against Nalm-6 cells with FT819 but variability in antigen-specific cytotoxicity with conventional CAR T cells.
In addition, when combined with rituximab, FT819 elicited antibody-dependent cell-mediated cytotoxicity against CD19-negative, CD20-positive tumor cells.
“Through the development of FT819, we believe there is significant opportunity to lower the cost of CAR T-cell manufacture, enhance the quality of the product, and create a readily available supply of a more efficacious product to reach more patients in need,” Dr Valamehr said.
CHICAGO—Researchers have used induced pluripotent stem cells (iPSCs) to create a “universal” chimeric antigen receptor (CAR) T-cell therapy known as FT819.
The team says FT819 has the potential to be mass-produced, stored, and made readily available for cancer patients.
In in vitro experiments, FT819 demonstrated activity against leukemia and lymphoma.
These results were presented at the AACR Annual Meeting 2018 (abstract LB-108).
The research was conducted by employees of Fate Therapeutics, Inc., the company developing FT819, as well as Memorial Sloan-Kettering Cancer Center.
About FT819
FT819 is produced from a master iPSC line generated using T cells from healthy donors.
“A master iPSC line has unlimited capacity to self-renew and can be banked and renewably used,” said Bob Valamehr, PhD, vice-president of cancer immunotherapy at Fate Therapeutics, Inc.
“We started with cells from a healthy donor rather than the patient, created a master cell line, and used the master cell line to produce large quantities of ‘universal’ CAR19 T cells that are not patient-restricted. These first-of-kind CAR19 T cells, called FT819, can be packaged, stored, and made readily available for treatment of a large number of patients.”
FT819 has 2 targeting receptors—a CAR targeting CD19-positive tumor cells and a CD16 Fc receptor that can engage other therapies (such as tumor antigen-targeting monoclonal antibodies) to overcome antigen escape.
The master iPSC line used for the production of FT819 is engineered in a one-time event to insert a CD19 CAR into the T-cell receptor α constant (TRAC) locus. This is done to eliminate T-cell receptor expression and reduce the likelihood of graft-versus-host disease.
Previous research showed that targeting a CAR to the TRAC locus results in uniform CAR expression and enhances T-cell potency. In fact, TRAC-CAR T cells outperformed conventionally generated CAR T cells by preventing T-cell exhaustion in a mouse model of acute lymphoblastic leukemia.
In vitro experiments
With the current work, the researchers found that FT819 displayed an efficient cytotoxic T-cell response when challenged with CD19-positive tumor cells. FT819 produced cytokines (IFN-gamma, TNF-alpha, and IL-2) and mediators of cell death (CD107a/b, perforin, and granzyme B).
FT819 was also target-specific, attacking only CD19-positive tumor cells and sparing CD19-negative tumor cells in experiments with Raji (Burkitt lymphoma) and Nalm-6 (B-cell acute lymphoblastic leukemia) cell lines.
The researchers said they observed consistent antigen-specific cytotoxicity against Nalm-6 cells with FT819 but variability in antigen-specific cytotoxicity with conventional CAR T cells.
In addition, when combined with rituximab, FT819 elicited antibody-dependent cell-mediated cytotoxicity against CD19-negative, CD20-positive tumor cells.
“Through the development of FT819, we believe there is significant opportunity to lower the cost of CAR T-cell manufacture, enhance the quality of the product, and create a readily available supply of a more efficacious product to reach more patients in need,” Dr Valamehr said.
CHICAGO—Researchers have used induced pluripotent stem cells (iPSCs) to create a “universal” chimeric antigen receptor (CAR) T-cell therapy known as FT819.
The team says FT819 has the potential to be mass-produced, stored, and made readily available for cancer patients.
In in vitro experiments, FT819 demonstrated activity against leukemia and lymphoma.
These results were presented at the AACR Annual Meeting 2018 (abstract LB-108).
The research was conducted by employees of Fate Therapeutics, Inc., the company developing FT819, as well as Memorial Sloan-Kettering Cancer Center.
About FT819
FT819 is produced from a master iPSC line generated using T cells from healthy donors.
“A master iPSC line has unlimited capacity to self-renew and can be banked and renewably used,” said Bob Valamehr, PhD, vice-president of cancer immunotherapy at Fate Therapeutics, Inc.
“We started with cells from a healthy donor rather than the patient, created a master cell line, and used the master cell line to produce large quantities of ‘universal’ CAR19 T cells that are not patient-restricted. These first-of-kind CAR19 T cells, called FT819, can be packaged, stored, and made readily available for treatment of a large number of patients.”
FT819 has 2 targeting receptors—a CAR targeting CD19-positive tumor cells and a CD16 Fc receptor that can engage other therapies (such as tumor antigen-targeting monoclonal antibodies) to overcome antigen escape.
The master iPSC line used for the production of FT819 is engineered in a one-time event to insert a CD19 CAR into the T-cell receptor α constant (TRAC) locus. This is done to eliminate T-cell receptor expression and reduce the likelihood of graft-versus-host disease.
Previous research showed that targeting a CAR to the TRAC locus results in uniform CAR expression and enhances T-cell potency. In fact, TRAC-CAR T cells outperformed conventionally generated CAR T cells by preventing T-cell exhaustion in a mouse model of acute lymphoblastic leukemia.
In vitro experiments
With the current work, the researchers found that FT819 displayed an efficient cytotoxic T-cell response when challenged with CD19-positive tumor cells. FT819 produced cytokines (IFN-gamma, TNF-alpha, and IL-2) and mediators of cell death (CD107a/b, perforin, and granzyme B).
FT819 was also target-specific, attacking only CD19-positive tumor cells and sparing CD19-negative tumor cells in experiments with Raji (Burkitt lymphoma) and Nalm-6 (B-cell acute lymphoblastic leukemia) cell lines.
The researchers said they observed consistent antigen-specific cytotoxicity against Nalm-6 cells with FT819 but variability in antigen-specific cytotoxicity with conventional CAR T cells.
In addition, when combined with rituximab, FT819 elicited antibody-dependent cell-mediated cytotoxicity against CD19-negative, CD20-positive tumor cells.
“Through the development of FT819, we believe there is significant opportunity to lower the cost of CAR T-cell manufacture, enhance the quality of the product, and create a readily available supply of a more efficacious product to reach more patients in need,” Dr Valamehr said.
Research reveals new subtypes of DLBCL
New research helps explain why some patients with diffuse large B-cell lymphoma (DLBCL) respond well to immunochemotherapy and others do not.
Researchers analyzed samples from nearly 600 DLBCL patients and identified 4 new genetic subtypes of the disease.
Patients with 2 of these subtypes had overall survival (OS) rates that were roughly twice as high as OS rates in patients with the other 2 subtypes.
Louis M. Staudt, MD, PhD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues described these findings in NEJM.
The researchers noted that the current subtypes of DLBCL—germinal center B-cell-like (GCB) and activated B-cell-like (ABC) DLBCL—are associated with OS after treatment with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
Patients with ABC DLBCL have a much lower OS rate, on average, than patients with GCB DLBCL. However, even in the GCB subgroup, many patients relapse after treatment.
“The first question we wanted to tackle was whether there were other molecular features of the tumors that could help us explain why some people were well-served by chemotherapy,” Dr Staudt said.
“And the second, related question was, if we could understand who was not responding well to treatment, could we understand the genetics of these tumors to suggest new potential therapies beyond chemotherapy? The answer to both questions was ‘yes.’”
Dr Staudt and his colleagues analyzed tumor samples from 574 patients with DLBCL, performing exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes to find recurrent aberrations.
The team also developed an algorithm to discover genetic subtypes based on the co-occurrence of genetic alterations.
In this way, they identified 4 genetic subtypes:
- MCD, which was named based on the co-occurrence of MYD88L265P and CD79B mutations
- BN2, whose name was based on the presence of BCL6 fusions and NOTCH2 mutations
- N1, named for NOTCH1 mutations
- EZB, named for EZH2 mutations and BCL2 translocations.
The researchers said aberrations in multiple genes distinguished each of these subtypes from other DLBCLs, and the subtypes differed phenotypically.
Patients with BN2 or EZB subtypes had much higher OS rates after receiving R-CHOP than patients with MCD or N1 subtypes. The predicted 5-year OS rates were 26% for MCD patients, 36% for N1 patients, 65% for BN2 patients, and 68% for EZB patients.
The researchers said they found evidence to suggest that MCD and BN2 DLBCLs rely on chronic active B-cell receptor signaling that is amenable to therapeutic inhibition.
The team also noted that some of the subtypes they identified can be found in both ABC and GCB DLBCLs. For example, a patient could have ABC DLBCL, which is associated with a lower OS rate after R-CHOP, but also have the BN2 genetic subtype that responds well to R-CHOP.
“This shows we’ve gone beyond where we were,” Dr Staudt said. “Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type, and they need to be treated aggressively.”
“Now, we can implement this kind of classification and say that, even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
Data from this study will be shared through the National Cancer Institute’s Genomic Data Commons to make it available for future research.
Dr Staudt said he and his colleagues hope their new molecular classification will be used in clinical trials so that DLBCL treatment can move toward more targeted therapies.
“The goal is to find the right drug for the right person at the right time,” Dr Staudt said. “And we feel this genetic understanding of diffuse lymphoma is a step forward in precision therapy.”
New research helps explain why some patients with diffuse large B-cell lymphoma (DLBCL) respond well to immunochemotherapy and others do not.
Researchers analyzed samples from nearly 600 DLBCL patients and identified 4 new genetic subtypes of the disease.
Patients with 2 of these subtypes had overall survival (OS) rates that were roughly twice as high as OS rates in patients with the other 2 subtypes.
Louis M. Staudt, MD, PhD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues described these findings in NEJM.
The researchers noted that the current subtypes of DLBCL—germinal center B-cell-like (GCB) and activated B-cell-like (ABC) DLBCL—are associated with OS after treatment with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
Patients with ABC DLBCL have a much lower OS rate, on average, than patients with GCB DLBCL. However, even in the GCB subgroup, many patients relapse after treatment.
“The first question we wanted to tackle was whether there were other molecular features of the tumors that could help us explain why some people were well-served by chemotherapy,” Dr Staudt said.
“And the second, related question was, if we could understand who was not responding well to treatment, could we understand the genetics of these tumors to suggest new potential therapies beyond chemotherapy? The answer to both questions was ‘yes.’”
Dr Staudt and his colleagues analyzed tumor samples from 574 patients with DLBCL, performing exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes to find recurrent aberrations.
The team also developed an algorithm to discover genetic subtypes based on the co-occurrence of genetic alterations.
In this way, they identified 4 genetic subtypes:
- MCD, which was named based on the co-occurrence of MYD88L265P and CD79B mutations
- BN2, whose name was based on the presence of BCL6 fusions and NOTCH2 mutations
- N1, named for NOTCH1 mutations
- EZB, named for EZH2 mutations and BCL2 translocations.
The researchers said aberrations in multiple genes distinguished each of these subtypes from other DLBCLs, and the subtypes differed phenotypically.
Patients with BN2 or EZB subtypes had much higher OS rates after receiving R-CHOP than patients with MCD or N1 subtypes. The predicted 5-year OS rates were 26% for MCD patients, 36% for N1 patients, 65% for BN2 patients, and 68% for EZB patients.
The researchers said they found evidence to suggest that MCD and BN2 DLBCLs rely on chronic active B-cell receptor signaling that is amenable to therapeutic inhibition.
The team also noted that some of the subtypes they identified can be found in both ABC and GCB DLBCLs. For example, a patient could have ABC DLBCL, which is associated with a lower OS rate after R-CHOP, but also have the BN2 genetic subtype that responds well to R-CHOP.
“This shows we’ve gone beyond where we were,” Dr Staudt said. “Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type, and they need to be treated aggressively.”
“Now, we can implement this kind of classification and say that, even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
Data from this study will be shared through the National Cancer Institute’s Genomic Data Commons to make it available for future research.
Dr Staudt said he and his colleagues hope their new molecular classification will be used in clinical trials so that DLBCL treatment can move toward more targeted therapies.
“The goal is to find the right drug for the right person at the right time,” Dr Staudt said. “And we feel this genetic understanding of diffuse lymphoma is a step forward in precision therapy.”
New research helps explain why some patients with diffuse large B-cell lymphoma (DLBCL) respond well to immunochemotherapy and others do not.
Researchers analyzed samples from nearly 600 DLBCL patients and identified 4 new genetic subtypes of the disease.
Patients with 2 of these subtypes had overall survival (OS) rates that were roughly twice as high as OS rates in patients with the other 2 subtypes.
Louis M. Staudt, MD, PhD, of the National Cancer Institute in Bethesda, Maryland, and his colleagues described these findings in NEJM.
The researchers noted that the current subtypes of DLBCL—germinal center B-cell-like (GCB) and activated B-cell-like (ABC) DLBCL—are associated with OS after treatment with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone).
Patients with ABC DLBCL have a much lower OS rate, on average, than patients with GCB DLBCL. However, even in the GCB subgroup, many patients relapse after treatment.
“The first question we wanted to tackle was whether there were other molecular features of the tumors that could help us explain why some people were well-served by chemotherapy,” Dr Staudt said.
“And the second, related question was, if we could understand who was not responding well to treatment, could we understand the genetics of these tumors to suggest new potential therapies beyond chemotherapy? The answer to both questions was ‘yes.’”
Dr Staudt and his colleagues analyzed tumor samples from 574 patients with DLBCL, performing exome and transcriptome sequencing, array-based DNA copy-number analysis, and targeted amplicon resequencing of 372 genes to find recurrent aberrations.
The team also developed an algorithm to discover genetic subtypes based on the co-occurrence of genetic alterations.
In this way, they identified 4 genetic subtypes:
- MCD, which was named based on the co-occurrence of MYD88L265P and CD79B mutations
- BN2, whose name was based on the presence of BCL6 fusions and NOTCH2 mutations
- N1, named for NOTCH1 mutations
- EZB, named for EZH2 mutations and BCL2 translocations.
The researchers said aberrations in multiple genes distinguished each of these subtypes from other DLBCLs, and the subtypes differed phenotypically.
Patients with BN2 or EZB subtypes had much higher OS rates after receiving R-CHOP than patients with MCD or N1 subtypes. The predicted 5-year OS rates were 26% for MCD patients, 36% for N1 patients, 65% for BN2 patients, and 68% for EZB patients.
The researchers said they found evidence to suggest that MCD and BN2 DLBCLs rely on chronic active B-cell receptor signaling that is amenable to therapeutic inhibition.
The team also noted that some of the subtypes they identified can be found in both ABC and GCB DLBCLs. For example, a patient could have ABC DLBCL, which is associated with a lower OS rate after R-CHOP, but also have the BN2 genetic subtype that responds well to R-CHOP.
“This shows we’ve gone beyond where we were,” Dr Staudt said. “Before, even with our most advanced molecular diagnosis, we would have said all ABC tumors are the ‘bad’ type, and they need to be treated aggressively.”
“Now, we can implement this kind of classification and say that, even if a patient has the ‘bad’ ABC type, they have the ‘good’ genetic type, BN2. So there’s a much better chance of chemotherapy curing the disease.”
Data from this study will be shared through the National Cancer Institute’s Genomic Data Commons to make it available for future research.
Dr Staudt said he and his colleagues hope their new molecular classification will be used in clinical trials so that DLBCL treatment can move toward more targeted therapies.
“The goal is to find the right drug for the right person at the right time,” Dr Staudt said. “And we feel this genetic understanding of diffuse lymphoma is a step forward in precision therapy.”
Tazemetostat exhibits antitumor activity in phase 1 trial
The EZH2 inhibitor tazemetostat demonstrated a “favorable safety profile and antitumor activity” in a phase 1 study, according to researchers.
The drug produced responses in 8 of 21 patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), including 3 complete responses (CRs).
The maximum tolerated dose of tazemetostat was not reached, and there were no fatal adverse events (AEs) related to treatment.
Grade 3/4 treatment-related AEs included thrombocytopenia, neutropenia, hepatocellular injury, and hypertension.
Antoine Italiano, MD, PhD, of Institut Bergonié in Bordeaux, France, and his colleagues reported these results in The Lancet Oncology. The trial was sponsored by Epizyme and Eisai.
The study enrolled 64 patients—43 with solid tumors and 21 with B-cell NHL. The following characteristics and dosing information pertain only to the patients with NHL.
Thirteen patients had diffuse large B-cell lymphoma (DLBCL), 7 had follicular lymphoma (FL), and 1 had marginal zone lymphoma (MZL).
The patients’ median age was 62 (range, 53-70), and 71% were male. They had an ECOG performance status of 0 (62%) or 1 (38%).
Most patients had received at least 3 prior therapies—38% had 3, 14% had 4, and 33% had 5 or more prior therapies. Forty-eight percent had prior hematopoietic stem cell transplant.
The patients received escalating doses of tazemetostat twice daily—100 mg (n=1), 200 mg (n=2), 400 mg (n=1), 800 mg (n=8), and 1600 mg (n=4).
The remaining 5 patients were enrolled in a substudy to evaluate food effect. These patients received a single 200 mg dose on day -8 and day -1, with or without food, followed by 400 mg twice daily starting on day 1. Specific results on the food effects were not included in the paper.
Safety
In the entire study cohort, there was 1 dose-limiting toxicity—grade 4 thrombocytopenia—at the 1600 mg dose. The maximum tolerated dose of tazemetostat was not reached, but the researchers decided upon 800 mg twice daily as the recommended phase 2 dose.
Overall, 77% (n=49) of patients had treatment-related AEs. Grade 3/4 treatment-related AEs included thrombocytopenia (4%, n=2), neutropenia (4%, n=2), hepatocellular injury (2%, n=1), and hypertension (2%, n=1).
Serious treatment-related AEs were neutropenia in 1 patient (800 mg group) and anemia and thrombocytopenia in another patient (1600 mg group).
Seven patients (11%) had fatal AEs, but none were considered treatment-related. They included general physical health deterioration (1 at 200 mg, 1 at 1600 mg, and 2 at 400 mg), respiratory distress (2 at 400 mg), and septic shock (1 at 1600 mg).
Efficacy
Eight of the 21 NHL patients responded to treatment. Three patients had a CR—1 with DLBCL and 2 with FL. Of the 5 partial responders, 3 had DLBCL, 1 had FL, and 1 had MZL.
The median time to first response was 3.5 months, and the median duration of response was 12.4 months.
The 3 complete responders remained on tazemetostat beyond 27.6 months (FL patient), 28.8 months (FL patient), and 33.6 months (DLBCL patient).
Two of the 43 patients with solid tumors responded to tazemetostat—1 with a CR and 1 with a partial response.
The complete responder had an INI1-negative malignant rhabdoid tumor, and the partial responder had a SMARCA4-negative malignant rhabdoid tumor of the ovary.
“Today’s publication in The Lancet Oncology reports the safety and tolerability endpoints for tazemetostat in this study, which enabled further evaluation of EZH2 inhibition in INI1- and SMARCA4-negative solid tumors and NHL,” Dr Italiano said. “I’m also encouraged by the preliminary antitumor activity observed in this study.”
The EZH2 inhibitor tazemetostat demonstrated a “favorable safety profile and antitumor activity” in a phase 1 study, according to researchers.
The drug produced responses in 8 of 21 patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), including 3 complete responses (CRs).
The maximum tolerated dose of tazemetostat was not reached, and there were no fatal adverse events (AEs) related to treatment.
Grade 3/4 treatment-related AEs included thrombocytopenia, neutropenia, hepatocellular injury, and hypertension.
Antoine Italiano, MD, PhD, of Institut Bergonié in Bordeaux, France, and his colleagues reported these results in The Lancet Oncology. The trial was sponsored by Epizyme and Eisai.
The study enrolled 64 patients—43 with solid tumors and 21 with B-cell NHL. The following characteristics and dosing information pertain only to the patients with NHL.
Thirteen patients had diffuse large B-cell lymphoma (DLBCL), 7 had follicular lymphoma (FL), and 1 had marginal zone lymphoma (MZL).
The patients’ median age was 62 (range, 53-70), and 71% were male. They had an ECOG performance status of 0 (62%) or 1 (38%).
Most patients had received at least 3 prior therapies—38% had 3, 14% had 4, and 33% had 5 or more prior therapies. Forty-eight percent had prior hematopoietic stem cell transplant.
The patients received escalating doses of tazemetostat twice daily—100 mg (n=1), 200 mg (n=2), 400 mg (n=1), 800 mg (n=8), and 1600 mg (n=4).
The remaining 5 patients were enrolled in a substudy to evaluate food effect. These patients received a single 200 mg dose on day -8 and day -1, with or without food, followed by 400 mg twice daily starting on day 1. Specific results on the food effects were not included in the paper.
Safety
In the entire study cohort, there was 1 dose-limiting toxicity—grade 4 thrombocytopenia—at the 1600 mg dose. The maximum tolerated dose of tazemetostat was not reached, but the researchers decided upon 800 mg twice daily as the recommended phase 2 dose.
Overall, 77% (n=49) of patients had treatment-related AEs. Grade 3/4 treatment-related AEs included thrombocytopenia (4%, n=2), neutropenia (4%, n=2), hepatocellular injury (2%, n=1), and hypertension (2%, n=1).
Serious treatment-related AEs were neutropenia in 1 patient (800 mg group) and anemia and thrombocytopenia in another patient (1600 mg group).
Seven patients (11%) had fatal AEs, but none were considered treatment-related. They included general physical health deterioration (1 at 200 mg, 1 at 1600 mg, and 2 at 400 mg), respiratory distress (2 at 400 mg), and septic shock (1 at 1600 mg).
Efficacy
Eight of the 21 NHL patients responded to treatment. Three patients had a CR—1 with DLBCL and 2 with FL. Of the 5 partial responders, 3 had DLBCL, 1 had FL, and 1 had MZL.
The median time to first response was 3.5 months, and the median duration of response was 12.4 months.
The 3 complete responders remained on tazemetostat beyond 27.6 months (FL patient), 28.8 months (FL patient), and 33.6 months (DLBCL patient).
Two of the 43 patients with solid tumors responded to tazemetostat—1 with a CR and 1 with a partial response.
The complete responder had an INI1-negative malignant rhabdoid tumor, and the partial responder had a SMARCA4-negative malignant rhabdoid tumor of the ovary.
“Today’s publication in The Lancet Oncology reports the safety and tolerability endpoints for tazemetostat in this study, which enabled further evaluation of EZH2 inhibition in INI1- and SMARCA4-negative solid tumors and NHL,” Dr Italiano said. “I’m also encouraged by the preliminary antitumor activity observed in this study.”
The EZH2 inhibitor tazemetostat demonstrated a “favorable safety profile and antitumor activity” in a phase 1 study, according to researchers.
The drug produced responses in 8 of 21 patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), including 3 complete responses (CRs).
The maximum tolerated dose of tazemetostat was not reached, and there were no fatal adverse events (AEs) related to treatment.
Grade 3/4 treatment-related AEs included thrombocytopenia, neutropenia, hepatocellular injury, and hypertension.
Antoine Italiano, MD, PhD, of Institut Bergonié in Bordeaux, France, and his colleagues reported these results in The Lancet Oncology. The trial was sponsored by Epizyme and Eisai.
The study enrolled 64 patients—43 with solid tumors and 21 with B-cell NHL. The following characteristics and dosing information pertain only to the patients with NHL.
Thirteen patients had diffuse large B-cell lymphoma (DLBCL), 7 had follicular lymphoma (FL), and 1 had marginal zone lymphoma (MZL).
The patients’ median age was 62 (range, 53-70), and 71% were male. They had an ECOG performance status of 0 (62%) or 1 (38%).
Most patients had received at least 3 prior therapies—38% had 3, 14% had 4, and 33% had 5 or more prior therapies. Forty-eight percent had prior hematopoietic stem cell transplant.
The patients received escalating doses of tazemetostat twice daily—100 mg (n=1), 200 mg (n=2), 400 mg (n=1), 800 mg (n=8), and 1600 mg (n=4).
The remaining 5 patients were enrolled in a substudy to evaluate food effect. These patients received a single 200 mg dose on day -8 and day -1, with or without food, followed by 400 mg twice daily starting on day 1. Specific results on the food effects were not included in the paper.
Safety
In the entire study cohort, there was 1 dose-limiting toxicity—grade 4 thrombocytopenia—at the 1600 mg dose. The maximum tolerated dose of tazemetostat was not reached, but the researchers decided upon 800 mg twice daily as the recommended phase 2 dose.
Overall, 77% (n=49) of patients had treatment-related AEs. Grade 3/4 treatment-related AEs included thrombocytopenia (4%, n=2), neutropenia (4%, n=2), hepatocellular injury (2%, n=1), and hypertension (2%, n=1).
Serious treatment-related AEs were neutropenia in 1 patient (800 mg group) and anemia and thrombocytopenia in another patient (1600 mg group).
Seven patients (11%) had fatal AEs, but none were considered treatment-related. They included general physical health deterioration (1 at 200 mg, 1 at 1600 mg, and 2 at 400 mg), respiratory distress (2 at 400 mg), and septic shock (1 at 1600 mg).
Efficacy
Eight of the 21 NHL patients responded to treatment. Three patients had a CR—1 with DLBCL and 2 with FL. Of the 5 partial responders, 3 had DLBCL, 1 had FL, and 1 had MZL.
The median time to first response was 3.5 months, and the median duration of response was 12.4 months.
The 3 complete responders remained on tazemetostat beyond 27.6 months (FL patient), 28.8 months (FL patient), and 33.6 months (DLBCL patient).
Two of the 43 patients with solid tumors responded to tazemetostat—1 with a CR and 1 with a partial response.
The complete responder had an INI1-negative malignant rhabdoid tumor, and the partial responder had a SMARCA4-negative malignant rhabdoid tumor of the ovary.
“Today’s publication in The Lancet Oncology reports the safety and tolerability endpoints for tazemetostat in this study, which enabled further evaluation of EZH2 inhibition in INI1- and SMARCA4-negative solid tumors and NHL,” Dr Italiano said. “I’m also encouraged by the preliminary antitumor activity observed in this study.”
Combo improves outcomes in MCL
A 2-drug combination can improve outcomes in patients with mantle cell lymphoma (MCL), according to researchers.
In a phase 2 trial of MCL patients, the BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax produced an overall response rate of 71% and a complete response (CR) rate of 62%.
“This was in patients who we expected to have a poor outcome on conventional therapy, and in which treatment with either ibrutinib or venetoclax alone was expected to see only 21% of patients show a complete response,” said Constantine Tam, MBBS, MD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
The most common adverse events (AEs) in patients receiving venetoclax and ibrutinib were diarrhea (83%), fatigue (75%), and nausea/vomiting (71%). Fourteen patients (58%) had serious AEs, including 2 with tumor lysis syndrome.
Dr Tam and his colleagues reported these results in NEJM.
The study included 24 patients—23 with relapsed/refractory MCL and 1 with previously untreated MCL. They had a median age of 68 (range, 47-81).
Most patients had high-risk (75%) or intermediate-risk (21%) disease, according to the MCL International Prognostic Index. Half of patients (including the previously untreated patient) had a TP53 aberration, and 25% had an NF-κB pathway mutation.
The relapsed/refractory patients had a median of 2 prior therapies (range, 1-6), and 48% were refractory to their most recent therapy.
Patients received ibrutinib monotherapy at 560 mg daily for 4 weeks. Then, patients began receiving venetoclax as well, in increasing doses, up to 400 mg per day. Patients received treatment until progression or unacceptable toxicity.
Efficacy
The study’s primary endpoint was CR at week 16, as assessed without PET. This was to allow the researchers to compare CR results in this trial to CR results in the PCYC-1104-CA study, a phase 2 trial of ibrutinib monotherapy in MCL.
According to CT, the CR rate was 42% in patients who received venetoclax and ibrutinib. This is significantly higher than the 9% CR rate observed in the patients treated with ibrutinib alone (P<0.001).
However, according to PET/CT, the 16-week CR rate was 62% in patients who received venetoclax and ibrutinib, and the overall response rate was 71%.
Overall, the rate of minimal residual disease (MRD) negativity was 67% (n=16) in the bone marrow according to flow cytometry and 38% (n=9) in the blood according to allele-specific oligonucleotide-polymerase chain reaction (ASO-PCR). However, not all patients were evaluable for MRD.
Among evaluable patients with a CR, 93% (14/15) were MRD negative according to flow cytometry, and 82% (9/11) were negative according to ASO-PCR.
The median progression-free survival was not reached at a median follow-up of 15.9 months. The estimated progression-free survival was 75% at 12 months and 57% at 18 months.
The rate of overall survival was 79% at 12 months and 74% at 18 months.
“These very promising results have triggered additional and larger studies to better understand the synergistic benefits of the venetoclax-ibrutinib treatment combination in MCL patients,” Dr Tam said.
Safety
The most common AEs were diarrhea (83%); fatigue (75%); nausea/vomiting (71%); bleeding, bruising, or postoperative hemorrhage (54%); musculoskeletal or connective-tissue pain (50%); cough or dyspnea (46%); soft-tissue infection (42%); upper respiratory tract infection (42%); neutropenia (33%); and lower respiratory tract infection (33%).
Grade 3/4 AEs included neutropenia (33%), thrombocytopenia (17%), anemia (12%), diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), lower respiratory tract infection (8%), soft-tissue infection (8%), cough or dyspnea (4%), musculoskeletal or connective-tissue pain (4%), and bleeding, bruising, or postoperative hemorrhage (4%).
Serious AEs included diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), pyrexia (8%), pleural effusion (8%), cardiac failure (4%), and soft-tissue infection (4%).
The patients who developed tumor lysis syndrome were among the first 15 patients who started venetoclax at a dose of 50 mg per day. Because of these cases, the study protocol was amended to lower the starting dose of venetoclax to 20 mg daily. After that, there were no additional cases of tumor lysis syndrome.
There were 6 deaths during the study. Four were attributed to disease progression, 1 to malignant otitis externa, and 1 to cardiac failure in a patient in CR.
A 2-drug combination can improve outcomes in patients with mantle cell lymphoma (MCL), according to researchers.
In a phase 2 trial of MCL patients, the BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax produced an overall response rate of 71% and a complete response (CR) rate of 62%.
“This was in patients who we expected to have a poor outcome on conventional therapy, and in which treatment with either ibrutinib or venetoclax alone was expected to see only 21% of patients show a complete response,” said Constantine Tam, MBBS, MD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
The most common adverse events (AEs) in patients receiving venetoclax and ibrutinib were diarrhea (83%), fatigue (75%), and nausea/vomiting (71%). Fourteen patients (58%) had serious AEs, including 2 with tumor lysis syndrome.
Dr Tam and his colleagues reported these results in NEJM.
The study included 24 patients—23 with relapsed/refractory MCL and 1 with previously untreated MCL. They had a median age of 68 (range, 47-81).
Most patients had high-risk (75%) or intermediate-risk (21%) disease, according to the MCL International Prognostic Index. Half of patients (including the previously untreated patient) had a TP53 aberration, and 25% had an NF-κB pathway mutation.
The relapsed/refractory patients had a median of 2 prior therapies (range, 1-6), and 48% were refractory to their most recent therapy.
Patients received ibrutinib monotherapy at 560 mg daily for 4 weeks. Then, patients began receiving venetoclax as well, in increasing doses, up to 400 mg per day. Patients received treatment until progression or unacceptable toxicity.
Efficacy
The study’s primary endpoint was CR at week 16, as assessed without PET. This was to allow the researchers to compare CR results in this trial to CR results in the PCYC-1104-CA study, a phase 2 trial of ibrutinib monotherapy in MCL.
According to CT, the CR rate was 42% in patients who received venetoclax and ibrutinib. This is significantly higher than the 9% CR rate observed in the patients treated with ibrutinib alone (P<0.001).
However, according to PET/CT, the 16-week CR rate was 62% in patients who received venetoclax and ibrutinib, and the overall response rate was 71%.
Overall, the rate of minimal residual disease (MRD) negativity was 67% (n=16) in the bone marrow according to flow cytometry and 38% (n=9) in the blood according to allele-specific oligonucleotide-polymerase chain reaction (ASO-PCR). However, not all patients were evaluable for MRD.
Among evaluable patients with a CR, 93% (14/15) were MRD negative according to flow cytometry, and 82% (9/11) were negative according to ASO-PCR.
The median progression-free survival was not reached at a median follow-up of 15.9 months. The estimated progression-free survival was 75% at 12 months and 57% at 18 months.
The rate of overall survival was 79% at 12 months and 74% at 18 months.
“These very promising results have triggered additional and larger studies to better understand the synergistic benefits of the venetoclax-ibrutinib treatment combination in MCL patients,” Dr Tam said.
Safety
The most common AEs were diarrhea (83%); fatigue (75%); nausea/vomiting (71%); bleeding, bruising, or postoperative hemorrhage (54%); musculoskeletal or connective-tissue pain (50%); cough or dyspnea (46%); soft-tissue infection (42%); upper respiratory tract infection (42%); neutropenia (33%); and lower respiratory tract infection (33%).
Grade 3/4 AEs included neutropenia (33%), thrombocytopenia (17%), anemia (12%), diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), lower respiratory tract infection (8%), soft-tissue infection (8%), cough or dyspnea (4%), musculoskeletal or connective-tissue pain (4%), and bleeding, bruising, or postoperative hemorrhage (4%).
Serious AEs included diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), pyrexia (8%), pleural effusion (8%), cardiac failure (4%), and soft-tissue infection (4%).
The patients who developed tumor lysis syndrome were among the first 15 patients who started venetoclax at a dose of 50 mg per day. Because of these cases, the study protocol was amended to lower the starting dose of venetoclax to 20 mg daily. After that, there were no additional cases of tumor lysis syndrome.
There were 6 deaths during the study. Four were attributed to disease progression, 1 to malignant otitis externa, and 1 to cardiac failure in a patient in CR.
A 2-drug combination can improve outcomes in patients with mantle cell lymphoma (MCL), according to researchers.
In a phase 2 trial of MCL patients, the BTK inhibitor ibrutinib and the BCL2 inhibitor venetoclax produced an overall response rate of 71% and a complete response (CR) rate of 62%.
“This was in patients who we expected to have a poor outcome on conventional therapy, and in which treatment with either ibrutinib or venetoclax alone was expected to see only 21% of patients show a complete response,” said Constantine Tam, MBBS, MD, of the Peter MacCallum Cancer Centre in Melbourne, Victoria, Australia.
The most common adverse events (AEs) in patients receiving venetoclax and ibrutinib were diarrhea (83%), fatigue (75%), and nausea/vomiting (71%). Fourteen patients (58%) had serious AEs, including 2 with tumor lysis syndrome.
Dr Tam and his colleagues reported these results in NEJM.
The study included 24 patients—23 with relapsed/refractory MCL and 1 with previously untreated MCL. They had a median age of 68 (range, 47-81).
Most patients had high-risk (75%) or intermediate-risk (21%) disease, according to the MCL International Prognostic Index. Half of patients (including the previously untreated patient) had a TP53 aberration, and 25% had an NF-κB pathway mutation.
The relapsed/refractory patients had a median of 2 prior therapies (range, 1-6), and 48% were refractory to their most recent therapy.
Patients received ibrutinib monotherapy at 560 mg daily for 4 weeks. Then, patients began receiving venetoclax as well, in increasing doses, up to 400 mg per day. Patients received treatment until progression or unacceptable toxicity.
Efficacy
The study’s primary endpoint was CR at week 16, as assessed without PET. This was to allow the researchers to compare CR results in this trial to CR results in the PCYC-1104-CA study, a phase 2 trial of ibrutinib monotherapy in MCL.
According to CT, the CR rate was 42% in patients who received venetoclax and ibrutinib. This is significantly higher than the 9% CR rate observed in the patients treated with ibrutinib alone (P<0.001).
However, according to PET/CT, the 16-week CR rate was 62% in patients who received venetoclax and ibrutinib, and the overall response rate was 71%.
Overall, the rate of minimal residual disease (MRD) negativity was 67% (n=16) in the bone marrow according to flow cytometry and 38% (n=9) in the blood according to allele-specific oligonucleotide-polymerase chain reaction (ASO-PCR). However, not all patients were evaluable for MRD.
Among evaluable patients with a CR, 93% (14/15) were MRD negative according to flow cytometry, and 82% (9/11) were negative according to ASO-PCR.
The median progression-free survival was not reached at a median follow-up of 15.9 months. The estimated progression-free survival was 75% at 12 months and 57% at 18 months.
The rate of overall survival was 79% at 12 months and 74% at 18 months.
“These very promising results have triggered additional and larger studies to better understand the synergistic benefits of the venetoclax-ibrutinib treatment combination in MCL patients,” Dr Tam said.
Safety
The most common AEs were diarrhea (83%); fatigue (75%); nausea/vomiting (71%); bleeding, bruising, or postoperative hemorrhage (54%); musculoskeletal or connective-tissue pain (50%); cough or dyspnea (46%); soft-tissue infection (42%); upper respiratory tract infection (42%); neutropenia (33%); and lower respiratory tract infection (33%).
Grade 3/4 AEs included neutropenia (33%), thrombocytopenia (17%), anemia (12%), diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), lower respiratory tract infection (8%), soft-tissue infection (8%), cough or dyspnea (4%), musculoskeletal or connective-tissue pain (4%), and bleeding, bruising, or postoperative hemorrhage (4%).
Serious AEs included diarrhea (12%), tumor lysis syndrome (8%), atrial fibrillation (8%), pyrexia (8%), pleural effusion (8%), cardiac failure (4%), and soft-tissue infection (4%).
The patients who developed tumor lysis syndrome were among the first 15 patients who started venetoclax at a dose of 50 mg per day. Because of these cases, the study protocol was amended to lower the starting dose of venetoclax to 20 mg daily. After that, there were no additional cases of tumor lysis syndrome.
There were 6 deaths during the study. Four were attributed to disease progression, 1 to malignant otitis externa, and 1 to cardiac failure in a patient in CR.
Tenalisib receives orphan designation for CTCL
The US Food and Drug Administration (FDA) has granted orphan drug designation to tenalisib for treatment of cutaneous T-cell lymphoma (CTCL).
Tenalisib (formerly RP6530) is a dual PI3K delta/gamma inhibitor under development by Rhizen Pharmaceuticals SA.
The FDA previously granted tenalisib fast track and orphan drug designations for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib has been investigated in a phase 1 trial of patients with relapsed/refractory PTCL and CTCL. Results from this trial were presented at the 10th Annual T-cell Lymphoma Forum in February.
The data included 55 patients—28 with CTCL and 27 with PTCL—who received varying doses of tenalisib. The maximum tolerated dose was an 800 mg daily fasting dose.
Fourteen PTCL patients were evaluable for efficacy, and 7 responded (50%) to treatment. Three patients had a complete response, and 4 had a partial response.
Eighteen CTCL patients were evaluable for efficacy. Eight patients responded (44%), all with partial responses.
In the entire cohort, treatment-related adverse events (AEs) of grade 3 or higher included transaminitis (20%), rash (5%), neutropenia (2%), hypophosphatemia (2%), international normalized ratio increase (2%), sepsis (2%), pyrexia (2%), and diplopia secondary to neuropathy (2%).
Four CTCL patients stopped tenalisib due to a treatment-related AE—transaminitis, sepsis, diarrhea, and diplopia secondary to neuropathy. One PTCL patient stopped treatment due to a related AE, which was transaminitis.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
The US Food and Drug Administration (FDA) has granted orphan drug designation to tenalisib for treatment of cutaneous T-cell lymphoma (CTCL).
Tenalisib (formerly RP6530) is a dual PI3K delta/gamma inhibitor under development by Rhizen Pharmaceuticals SA.
The FDA previously granted tenalisib fast track and orphan drug designations for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib has been investigated in a phase 1 trial of patients with relapsed/refractory PTCL and CTCL. Results from this trial were presented at the 10th Annual T-cell Lymphoma Forum in February.
The data included 55 patients—28 with CTCL and 27 with PTCL—who received varying doses of tenalisib. The maximum tolerated dose was an 800 mg daily fasting dose.
Fourteen PTCL patients were evaluable for efficacy, and 7 responded (50%) to treatment. Three patients had a complete response, and 4 had a partial response.
Eighteen CTCL patients were evaluable for efficacy. Eight patients responded (44%), all with partial responses.
In the entire cohort, treatment-related adverse events (AEs) of grade 3 or higher included transaminitis (20%), rash (5%), neutropenia (2%), hypophosphatemia (2%), international normalized ratio increase (2%), sepsis (2%), pyrexia (2%), and diplopia secondary to neuropathy (2%).
Four CTCL patients stopped tenalisib due to a treatment-related AE—transaminitis, sepsis, diarrhea, and diplopia secondary to neuropathy. One PTCL patient stopped treatment due to a related AE, which was transaminitis.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
The US Food and Drug Administration (FDA) has granted orphan drug designation to tenalisib for treatment of cutaneous T-cell lymphoma (CTCL).
Tenalisib (formerly RP6530) is a dual PI3K delta/gamma inhibitor under development by Rhizen Pharmaceuticals SA.
The FDA previously granted tenalisib fast track and orphan drug designations for the treatment of peripheral T-cell lymphoma (PTCL).
Tenalisib has been investigated in a phase 1 trial of patients with relapsed/refractory PTCL and CTCL. Results from this trial were presented at the 10th Annual T-cell Lymphoma Forum in February.
The data included 55 patients—28 with CTCL and 27 with PTCL—who received varying doses of tenalisib. The maximum tolerated dose was an 800 mg daily fasting dose.
Fourteen PTCL patients were evaluable for efficacy, and 7 responded (50%) to treatment. Three patients had a complete response, and 4 had a partial response.
Eighteen CTCL patients were evaluable for efficacy. Eight patients responded (44%), all with partial responses.
In the entire cohort, treatment-related adverse events (AEs) of grade 3 or higher included transaminitis (20%), rash (5%), neutropenia (2%), hypophosphatemia (2%), international normalized ratio increase (2%), sepsis (2%), pyrexia (2%), and diplopia secondary to neuropathy (2%).
Four CTCL patients stopped tenalisib due to a treatment-related AE—transaminitis, sepsis, diarrhea, and diplopia secondary to neuropathy. One PTCL patient stopped treatment due to a related AE, which was transaminitis.
About orphan and fast track designations
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The FDA’s fast track drug development program is designed to expedite clinical development and submission of new drug applications for medicines with the potential to treat serious or life-threatening conditions and address unmet medical needs.
Fast track designation facilitates frequent interactions with the FDA review team, including meetings to discuss all aspects of development to support a drug’s approval, and also provides the opportunity to submit sections of a new drug application on a rolling basis as data become available.
Duvelisib NDA granted priority review
The US Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for duvelisib, a dual PI3K delta/gamma inhibitor.
With this NDA, Verastem, Inc., is seeking full approval of duvelisib for the treatment of relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval of the drug for the treatment of relapsed or refractory follicular lymphoma (FL).
The FDA expects to make a decision on the NDA by October 5, 2018.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The application for duvelisib is supported by data from DUO™, a randomized, phase 3 study of patients with relapsed or refractory CLL/SLL, and DYNAMO™, a phase 2 study of patients with refractory indolent non-Hodgkin lymphoma.
Phase 3 DUO trial
Results from DUO were presented at the 2017 ASH Annual Meeting in December.
This study included 319 CLL/SLL patients who were randomized 1:1 to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The study’s primary endpoint was met, as duvelisib conferred a significant improvement in median progression-free survival (PFS) over ofatumumab.
Per an independent review committee, the median PFS was 13.3 months with duvelisib and 9.9 months with ofatumumab (hazard ratio=0.52; P<0.0001). Duvelisib maintained a PFS advantage in all patient subgroups analyzed.
The overall response rate was 73.8% with duvelisib and 45.3% with ofatumumab (P<0.0001). The complete response rate was 0.6% in both arms.
Overall survival (OS) was similar in the duvelisib and ofatumumab arms (hazard ratio=0.99; P=0.4807). The median OS was not reached in either arm.
The most common grade 3 or higher adverse events (AEs)—in the duvelisib and ofatumumab arms, respectively—were neutropenia (30% vs 17%), anemia (13% vs 5%), diarrhea (15% vs 1%), pneumonia (14% vs 1%), and colitis (12% vs 1%).
Thirty-five percent of patients discontinued duvelisib due to an AE.
Severe opportunistic infections occurred in 6% of duvelisib recipients—bronchopulmonary aspergillosis (n=4), fungal infection (n=2), Pneumocystis jirovecii pneumonia (n=2), and cytomegalovirus colitis (n=1).
There were 4 deaths related to duvelisib—staphylococcal pneumonia (n=2), general physical health deterioration (n=1), and sepsis (n=1).
Phase 2 DYNAMO trial
Results from DYNAMO were presented at the 22nd EHA Congress (abstract S777) in June 2017.
This trial enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate, per an independent review committee, was 43%. One patient achieved a complete response, and 35 had a partial response. The median duration of response was 7.9 months.
The median PFS was 8.3 months, and the median OS was 27.8 months.
The most common grade 3 or higher AEs were neutropenia (22%), anemia (13%), diarrhea (16%), lipase increase (10%), and thrombocytopenia (9%).
There were 2 serious opportunistic infections—Pneumocystis pneumonia and fungal pneumonia.
There were 3 deaths attributed to duvelisib—toxic epidermal necrolysis/sepsis syndrome (n=1), drug reaction/eosinophilia/systemic symptoms (n=1), and pneumonitis/pneumonia (n=1).
The US Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for duvelisib, a dual PI3K delta/gamma inhibitor.
With this NDA, Verastem, Inc., is seeking full approval of duvelisib for the treatment of relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval of the drug for the treatment of relapsed or refractory follicular lymphoma (FL).
The FDA expects to make a decision on the NDA by October 5, 2018.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The application for duvelisib is supported by data from DUO™, a randomized, phase 3 study of patients with relapsed or refractory CLL/SLL, and DYNAMO™, a phase 2 study of patients with refractory indolent non-Hodgkin lymphoma.
Phase 3 DUO trial
Results from DUO were presented at the 2017 ASH Annual Meeting in December.
This study included 319 CLL/SLL patients who were randomized 1:1 to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The study’s primary endpoint was met, as duvelisib conferred a significant improvement in median progression-free survival (PFS) over ofatumumab.
Per an independent review committee, the median PFS was 13.3 months with duvelisib and 9.9 months with ofatumumab (hazard ratio=0.52; P<0.0001). Duvelisib maintained a PFS advantage in all patient subgroups analyzed.
The overall response rate was 73.8% with duvelisib and 45.3% with ofatumumab (P<0.0001). The complete response rate was 0.6% in both arms.
Overall survival (OS) was similar in the duvelisib and ofatumumab arms (hazard ratio=0.99; P=0.4807). The median OS was not reached in either arm.
The most common grade 3 or higher adverse events (AEs)—in the duvelisib and ofatumumab arms, respectively—were neutropenia (30% vs 17%), anemia (13% vs 5%), diarrhea (15% vs 1%), pneumonia (14% vs 1%), and colitis (12% vs 1%).
Thirty-five percent of patients discontinued duvelisib due to an AE.
Severe opportunistic infections occurred in 6% of duvelisib recipients—bronchopulmonary aspergillosis (n=4), fungal infection (n=2), Pneumocystis jirovecii pneumonia (n=2), and cytomegalovirus colitis (n=1).
There were 4 deaths related to duvelisib—staphylococcal pneumonia (n=2), general physical health deterioration (n=1), and sepsis (n=1).
Phase 2 DYNAMO trial
Results from DYNAMO were presented at the 22nd EHA Congress (abstract S777) in June 2017.
This trial enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate, per an independent review committee, was 43%. One patient achieved a complete response, and 35 had a partial response. The median duration of response was 7.9 months.
The median PFS was 8.3 months, and the median OS was 27.8 months.
The most common grade 3 or higher AEs were neutropenia (22%), anemia (13%), diarrhea (16%), lipase increase (10%), and thrombocytopenia (9%).
There were 2 serious opportunistic infections—Pneumocystis pneumonia and fungal pneumonia.
There were 3 deaths attributed to duvelisib—toxic epidermal necrolysis/sepsis syndrome (n=1), drug reaction/eosinophilia/systemic symptoms (n=1), and pneumonitis/pneumonia (n=1).
The US Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for duvelisib, a dual PI3K delta/gamma inhibitor.
With this NDA, Verastem, Inc., is seeking full approval of duvelisib for the treatment of relapsed or refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and accelerated approval of the drug for the treatment of relapsed or refractory follicular lymphoma (FL).
The FDA expects to make a decision on the NDA by October 5, 2018.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
The application for duvelisib is supported by data from DUO™, a randomized, phase 3 study of patients with relapsed or refractory CLL/SLL, and DYNAMO™, a phase 2 study of patients with refractory indolent non-Hodgkin lymphoma.
Phase 3 DUO trial
Results from DUO were presented at the 2017 ASH Annual Meeting in December.
This study included 319 CLL/SLL patients who were randomized 1:1 to receive either duvelisib (25 mg orally twice daily) or ofatumumab (initial infusion of 300 mg followed by 7 weekly infusions and 4 monthly infusions of 2000 mg).
The study’s primary endpoint was met, as duvelisib conferred a significant improvement in median progression-free survival (PFS) over ofatumumab.
Per an independent review committee, the median PFS was 13.3 months with duvelisib and 9.9 months with ofatumumab (hazard ratio=0.52; P<0.0001). Duvelisib maintained a PFS advantage in all patient subgroups analyzed.
The overall response rate was 73.8% with duvelisib and 45.3% with ofatumumab (P<0.0001). The complete response rate was 0.6% in both arms.
Overall survival (OS) was similar in the duvelisib and ofatumumab arms (hazard ratio=0.99; P=0.4807). The median OS was not reached in either arm.
The most common grade 3 or higher adverse events (AEs)—in the duvelisib and ofatumumab arms, respectively—were neutropenia (30% vs 17%), anemia (13% vs 5%), diarrhea (15% vs 1%), pneumonia (14% vs 1%), and colitis (12% vs 1%).
Thirty-five percent of patients discontinued duvelisib due to an AE.
Severe opportunistic infections occurred in 6% of duvelisib recipients—bronchopulmonary aspergillosis (n=4), fungal infection (n=2), Pneumocystis jirovecii pneumonia (n=2), and cytomegalovirus colitis (n=1).
There were 4 deaths related to duvelisib—staphylococcal pneumonia (n=2), general physical health deterioration (n=1), and sepsis (n=1).
Phase 2 DYNAMO trial
Results from DYNAMO were presented at the 22nd EHA Congress (abstract S777) in June 2017.
This trial enrolled patients with indolent non-Hodgkin lymphoma whose disease was refractory to both rituximab and chemotherapy or radioimmunotherapy.
There were 83 patients with FL. They had a median of 3 prior anticancer regimens (range, 1-10).
The patients received duvelisib at 25 mg orally twice daily until disease progression or unacceptable toxicity.
The overall response rate, per an independent review committee, was 43%. One patient achieved a complete response, and 35 had a partial response. The median duration of response was 7.9 months.
The median PFS was 8.3 months, and the median OS was 27.8 months.
The most common grade 3 or higher AEs were neutropenia (22%), anemia (13%), diarrhea (16%), lipase increase (10%), and thrombocytopenia (9%).
There were 2 serious opportunistic infections—Pneumocystis pneumonia and fungal pneumonia.
There were 3 deaths attributed to duvelisib—toxic epidermal necrolysis/sepsis syndrome (n=1), drug reaction/eosinophilia/systemic symptoms (n=1), and pneumonitis/pneumonia (n=1).
Project provides ‘unprecedented understanding’ of cancers
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Through extensive analyses of data from The Cancer Genome Atlas (TCGA), researchers have produced a new resource known as the Pan-Cancer Atlas.
Multiple research groups analyzed data on more than 10,000 tumors spanning 33 types of cancer, including acute myeloid leukemia and diffuse large B-cell lymphoma.
The work revealed new insights regarding cells of origin, oncogenic processes, and signaling pathways.
These insights make up the Pan-Cancer Atlas and are described in 27 papers published in Cell Press journals. The entire collection of papers is available through a portal on cell.com.
The Pan-Cancer Atlas is the final output of TCGA, a joint effort of the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI) to “collect, select, and analyze human tissues for genomic alterations on a very large scale.”
“This project is the culmination of more than a decade of ground-breaking work,” said Francis S. Collins, MD, PhD, director of the National Institutes of Health.
“This analysis provides cancer researchers with unprecedented understanding of how, where, and why tumors arise in humans, enabling better informed clinical trials and future treatments.”
The project focused on genome sequencing as well as other analyses, such as investigating gene and protein expression profiles and associating them with clinical and imaging data.
“The Pan-Cancer Atlas effort complements the over 30 tumor-specific papers that have been published by TCGA in the last decade and expands upon earlier pan-cancer work that was published in 2013,” said Jean Claude Zenklusen, PhD, director of the TCGA Program Office at NCI.
The Pan-Cancer Atlas is divided into 3 main categories—cell of origin, oncogenic processes, and signaling pathways—each anchored by a summary paper that recaps the core findings for the topic. Companion papers report in-depth explorations of individual topics within these categories.
Cell of origin
In the first Pan-Cancer Atlas summary paper, the authors review the findings from analyses using a technique called molecular clustering, which groups tumors by parameters such as genes being expressed, abnormality of chromosome numbers in tumor cells, and DNA modifications.
The analyses suggest that tumor types cluster by their possible cells of origin, a finding that has implications for the classification and treatment of various cancers.
“Rather than the organ of origin, we can now use molecular features to identify the cancer’s cell of origin,” said Li Ding, PhD, of Washington University School of Medicine in St. Louis, Missouri.
“We are looking at what genes are turned on in the tumor, and that brings us to a particular cell type. For example, squamous cell cancers can arise in the lung, bladder, cervix, and some tumors of the head and neck. We traditionally have treated cancers in these areas as completely different diseases, but, [by] studying their molecular features, we now know such cancers are closely related.”
“This new molecular-based classification system should greatly help in the clinic, where it is already explaining some of the similar clinical behavior of what we thought were different tumor types,” said Charles Perou, PhD, of UNC Lineberger Comprehensive Cancer Center in Chapel Hill, North Carolina.
“These findings also provide many new therapeutic opportunities, which can and will be tested in the next phase of human clinical trials.”
Oncogenic processes
The second Pan-Cancer Atlas summary paper presents a broad view of the TCGA findings on the processes that lead to cancer development and progression.
The research revealed insights into 3 critical oncogenic processes—germline and somatic mutations, the influence of the tumor’s underlying genome and epigenome on gene and protein expression, and the interplay of tumor and immune cells.
“For the 10,000 tumors we analyzed, we now know—in detail—the inherited mutations driving cancer and the genetic errors that accumulate as people age, increasing the risk of cancer,” Dr Ding said. “This is the first definitive summary of the genetics behind 33 major types of cancer.”
“TCGA has created a catalogue of alterations that occur in a variety of cancer types,” said Katherine Hoadley, PhD, of University of North Carolina at Chapel Hill.
“Having this catalogue of alterations is really important for us to look, in future studies, at why these alterations are there and to predict outcomes for patients.”
Signaling pathways
The final Pan-Cancer Atlas summary paper details TCGA research on the genomic alterations in the signaling pathways that control cell-cycle progression, cell death, and cell growth. The work highlights the similarities and differences in these processes across a range of cancers.
The researchers believe these studies have revealed new patterns of potential vulnerabilities that might aid the development of targeted and combination therapies.
Drug receives priority review for HCL
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
The US Food and Drug Administration (FDA) has accepted for priority review the biologics license application (BLA) for moxetumomab pasudotox, an investigational anti-CD22 recombinant immunotoxin.
With this BLA, AstraZeneca is seeking approval for moxetumomab pasudotox for the treatment of adults with hairy cell leukemia (HCL) who have received at least 2 prior lines of therapy.
The FDA expects to make a decision on the BLA in the third quarter of this year.
The FDA aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The agency grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
About moxetumomab pasudotox
Moxetumomab pasudotox (formerly CAT-8015 or HA22) is composed of a binding portion of an anti-CD22 antibody fused to a toxin. After binding to CD22, the molecule is internalized, processed, and releases its modified protein toxin, which inhibits protein translation and leads to apoptosis.
In addition to priority review, moxetumomab pasudotox has received orphan drug designation from the FDA.
Moxetumomab pasudotox has been tested in a phase 1 trial. Initial results from this trial were published in the Journal of Clinical Oncology in 2012. Long-term follow-up was presented at the 2017 ASH Annual Meeting.
The ASH data included 49 patients with relapsed/refractory HCL. Their median age was 57 (range, 40-77), most (n=41) were male, and they had a median of 35 (range, 1-60,444) circulating HCL cells/mm3 at baseline (in 48 evaluable patients).
Twenty-eight patients received moxetumomab pasudotox in the dose-escalation portion of the study—at 5, 10, 20, 30, 40, or 50 µg/kg—and 21 received the drug at 50 µg/kg for the extension portion of the study.
Among the 33 patients who received moxetumomab pasudotox at 50 µg/kg, the overall response rate was 88%, and the complete response (CR) rate was 64% (n=21). The median time to CR was 3.6 months, and the median duration of CR was 70.3 months.
The median follow-up was 75 months for the entire study population. At 72 months, the progression-free survival (PFS) rate was 77%.
The researchers found that minimal residual disease (MRD) negativity (via immunohistochemistry) was associated with extended response duration and prolonged PFS.
The MRD evaluation included 19 MRD+ patients and 18 MRD- patients. Forty-seven percent of the MRD+ patients (n=9) and 94% of the MRD- patients (n=17) had a CR as their best response.
The median duration of CR was 13.1 months among the MRD+ patients and was not reached among the MRD- patients (P=0.0002). The median PFS was 82.1 months among the MRD+ patients and not reached among the MRD- patients (P=0.0031).
Moxetumomab pasudotox did not undergo phase 2 testing but proceeded to a phase 3 trial. In this single-arm study, researchers evaluated the drug in HCL patients who had received at least 2 prior therapies.
According to AstraZeneca, the study’s primary endpoint—durable CR—was met. The company said the phase 3 results will be presented at an upcoming medical meeting.
ICER assesses value of CAR T-cell therapies
The Institute for Clinical and Economic Review (ICER) has made policy recommendations intended to ensure affordability and access to chimeric antigen receptor (CAR) T-cell therapies.
ICER released a Final Evidence Report on tisagenlecleucel (Kymriah, Novartis) and axicabtagene ciloleucel (Yescarta, Kite Pharma/Gilead), 2 CAR T-cell therapies approved in the US to treat B-cell acute lymphoblastic leukemia (B-ALL) and non-Hodgkin lymphoma (NHL), respectively.
The report says the pricing of these therapies aligns with patient benefit, but changes will be needed in future pricing, payment, and delivery mechanisms to ensure patient access without threatening health system affordability.
“Given the currently available evidence, these therapies appear to be effective options for those with B-ALL or NHL, though uncertainty in the evidence raised questions around the long-term value for money,” said Dan Ollendorf, PhD, ICER’s chief scientific officer.
Net health benefit
ICER’s report says tisagenlecleucel provides a net health benefit for children with B-ALL, and both tisagenlecleucel and axicabtagene ciloleucel provide a net health benefit for adults with certain types of NHL. (Novartis is seeking approval for tisagenlecleucel in NHL).
The evidence suggests there is at least a small net health benefit of the CAR T-cell therapies compared to other therapies. The benefit may be substantial, but uncertainties remain.
The data show complete remission (CR), disease-free survival (DFS), and overall survival (OS) rates are superior for NHL patients who receive axicabtagene ciloleucel, compared to patients who receive standard chemoimmunotherapy regimens.
Similarly, B-ALL patients treated with tisagenlecleucel have superior CR, DFS, and OS rates to patients treated with standard therapies. CR and OS rates are also superior in NHL patients treated with tisagenlecleucel, but DFS has not been reported in this population.
The report says there is insufficient evidence to distinguish between the 2 CAR T-cell therapies for the treatment of NHL.
Toxicity and uncertainty
The report highlights the fact that cytokine release syndrome, neurological symptoms, and B-cell aplasia have been observed in patients who receive CAR T-cell therapies. However, these sometimes severe adverse events are generally “manageable.”
In addition to toxicity, the report highlights sources of uncertainty. These include the fact that studies of tisagenlecleucel and axicabtagene ciloleucel are small, single-arm trials with short follow-up; comparisons with historical controls may be misleading; and improvements in the CAR T-cell manufacturing process may change outcomes.
Cost-effectiveness
The report states that the cost-effectiveness of each therapy fell below or within commonly cited thresholds of $50,000 to $150,000 per quality-adjusted life-year (QALY) over a lifetime.
For its analyses, ICER used the wholesale acquisition cost (WAC) plus an assumed hospital mark-up. The analyses were also based on the assumption that survival benefits observed in clinical trials would continue after the trials ended.
For tisagenlecleucel in pediatric B-ALL, the WAC is $475,000. The long-term cost-effectiveness compared to clofarabine is $45,871 per QALY gained.
For axicabtagene ciloleucel in adults with NHL, the WAC is $373,000. The long-term cost-effectiveness compared to salvage chemotherapy is $136,078 per QALY gained. The effectiveness assumptions for chemotherapy were based on an average of salvage chemotherapy regimens from the SCHOLAR-1 trial, and the cost assumptions were based on the cost of the R-DHAP (rituximab, dexamethasone, cytarabine, and cisplatin) regimen.
The report says tisagenlecleucel’s price would remain in alignment with value even if price premiums of 102% to 194% were applied.
Meanwhile, axicabtagene ciloleucel’s price could be increased by up to 11% and remain in alignment with the upper threshold ($150,000 per QALY gained) but would need to be discounted by 28% to align with the lower threshold ($100,000 per QALY gained).
Tisagenlecleucel, as a treatment for B-ALL, is not expected to cross the $915 million threshold for annual budget impact.
However, the short-term costs of axicabtagene ciloleucel for relapsed/refractory NHL could exceed the threshold. Only 38% of the estimated 5900 eligible patients could receive axicabtagene ciloleucel in a year before crossing the threshold.
Because of these findings, ICER issued an “Affordability and Access Alert” for axicabtagene ciloleucel.
This alert is intended to signal when the added costs associated with a new treatment may be difficult for the healthcare system to absorb over the short-term without displacing other needed services or contributing to unsustainable growth in healthcare insurance costs.
“Based on current evidence, both therapies appear to be priced in alignment with their clinical value, but there are potential short-term affordability concerns—for axicabtagene ciloleucel under its current indication and for both treatments should they receive future approvals for broader patient populations,” Dr Ollendorf said.
Panel voting results
ICER’s report was reviewed at a public meeting of the California Technology Assessment Forum on March 2.
Most of the panel said tisagenlecleucel provides intermediate long-term value for money when treating B-ALL. However, the significant uncertainty surrounding the long-term risks and benefits of the therapy precluded a high-value vote.
After deliberating on the value of axicabtagene ciloleucel to treat NHL, the panel’s votes were split between low-value and intermediate-value, driven by similar concerns about long-term uncertainty.
Policy recommendations
Following the voting session, ICER convened a policy roundtable of experts, including physicians, patient advocates, manufacturer representatives, and payer representatives.
Based on the roundtable discussion, ICER developed recommendations for enhanced stakeholder communication, innovative payment models, generation of additional evidence, settings of care, and patient education.
“With many other potentially transformative therapies in the pipeline, stakeholders must collaborate now to develop payment and delivery systems that can ensure timely patient access, manage short-term affordability for expensive one-time treatments, and continue to reward the innovation that brings these new treatments to market,” Dr Ollendorf said.
Some of ICER’s recommendations include:
- When launching novel therapies approved with limited clinical evidence, such as CAR T-cell therapies, manufacturers and payers should consider using a lower launch price that could be increased if substantial clinical benefits are confirmed or using a higher initial price tied to a requirement for refunds or rebates if real-world evidence fails to confirm high expectations.
- Outcomes-based pricing arrangements must be linked to “meaningful clinical outcomes assessed with sufficient follow up.”
- Hospital mark-up for CAR T-cell therapies “should reflect the expected additional cost for care delivered in the hospital, rather than a percentage of the drug cost to avoid perverse incentives in choosing the treatment location.”
- Initially, CAR T-cell therapies should be delivered in “manufacturer-accredited centers to ensure the quality and appropriateness of care.” Later, “centers of excellence accredited by specialty societies” can administer these therapies, as long as providers have “sufficient expertise” to manage serious side effects.
- Centers should ensure that patients understand what to expect from CAR T-cell therapy, including long-term consequences.
- Because additional evidence on CAR T-cell therapies is needed, all patients who receive these therapies should enter into a registry with planned long-term follow-up.
- Studies should determine the optimal timing of CAR T-cell therapy in the sequence of treatments for B-ALL and NHL.
Additional recommendations and more details are available in ICER’s report.
About ICER
ICER is an independent, non-profit research institute that produces reports analyzing evidence on the effectiveness and value of drugs and other medical services.
ICER’s reports include evidence-based calculations of prices for new drugs that reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall healthcare system.
ICER’s reports incorporate input from stakeholders and are the subject of public hearings through 3 core programs: the California Technology Assessment Forum, the Midwest Comparative Effectiveness Public Advisory Council, and the New England Comparative Effectiveness Public Advisory Council.
These independent panels review ICER’s reports at public meetings to deliberate on the evidence and develop recommendations for how patients, clinicians, insurers, and policymakers can improve the quality and value of healthcare.
The Institute for Clinical and Economic Review (ICER) has made policy recommendations intended to ensure affordability and access to chimeric antigen receptor (CAR) T-cell therapies.
ICER released a Final Evidence Report on tisagenlecleucel (Kymriah, Novartis) and axicabtagene ciloleucel (Yescarta, Kite Pharma/Gilead), 2 CAR T-cell therapies approved in the US to treat B-cell acute lymphoblastic leukemia (B-ALL) and non-Hodgkin lymphoma (NHL), respectively.
The report says the pricing of these therapies aligns with patient benefit, but changes will be needed in future pricing, payment, and delivery mechanisms to ensure patient access without threatening health system affordability.
“Given the currently available evidence, these therapies appear to be effective options for those with B-ALL or NHL, though uncertainty in the evidence raised questions around the long-term value for money,” said Dan Ollendorf, PhD, ICER’s chief scientific officer.
Net health benefit
ICER’s report says tisagenlecleucel provides a net health benefit for children with B-ALL, and both tisagenlecleucel and axicabtagene ciloleucel provide a net health benefit for adults with certain types of NHL. (Novartis is seeking approval for tisagenlecleucel in NHL).
The evidence suggests there is at least a small net health benefit of the CAR T-cell therapies compared to other therapies. The benefit may be substantial, but uncertainties remain.
The data show complete remission (CR), disease-free survival (DFS), and overall survival (OS) rates are superior for NHL patients who receive axicabtagene ciloleucel, compared to patients who receive standard chemoimmunotherapy regimens.
Similarly, B-ALL patients treated with tisagenlecleucel have superior CR, DFS, and OS rates to patients treated with standard therapies. CR and OS rates are also superior in NHL patients treated with tisagenlecleucel, but DFS has not been reported in this population.
The report says there is insufficient evidence to distinguish between the 2 CAR T-cell therapies for the treatment of NHL.
Toxicity and uncertainty
The report highlights the fact that cytokine release syndrome, neurological symptoms, and B-cell aplasia have been observed in patients who receive CAR T-cell therapies. However, these sometimes severe adverse events are generally “manageable.”
In addition to toxicity, the report highlights sources of uncertainty. These include the fact that studies of tisagenlecleucel and axicabtagene ciloleucel are small, single-arm trials with short follow-up; comparisons with historical controls may be misleading; and improvements in the CAR T-cell manufacturing process may change outcomes.
Cost-effectiveness
The report states that the cost-effectiveness of each therapy fell below or within commonly cited thresholds of $50,000 to $150,000 per quality-adjusted life-year (QALY) over a lifetime.
For its analyses, ICER used the wholesale acquisition cost (WAC) plus an assumed hospital mark-up. The analyses were also based on the assumption that survival benefits observed in clinical trials would continue after the trials ended.
For tisagenlecleucel in pediatric B-ALL, the WAC is $475,000. The long-term cost-effectiveness compared to clofarabine is $45,871 per QALY gained.
For axicabtagene ciloleucel in adults with NHL, the WAC is $373,000. The long-term cost-effectiveness compared to salvage chemotherapy is $136,078 per QALY gained. The effectiveness assumptions for chemotherapy were based on an average of salvage chemotherapy regimens from the SCHOLAR-1 trial, and the cost assumptions were based on the cost of the R-DHAP (rituximab, dexamethasone, cytarabine, and cisplatin) regimen.
The report says tisagenlecleucel’s price would remain in alignment with value even if price premiums of 102% to 194% were applied.
Meanwhile, axicabtagene ciloleucel’s price could be increased by up to 11% and remain in alignment with the upper threshold ($150,000 per QALY gained) but would need to be discounted by 28% to align with the lower threshold ($100,000 per QALY gained).
Tisagenlecleucel, as a treatment for B-ALL, is not expected to cross the $915 million threshold for annual budget impact.
However, the short-term costs of axicabtagene ciloleucel for relapsed/refractory NHL could exceed the threshold. Only 38% of the estimated 5900 eligible patients could receive axicabtagene ciloleucel in a year before crossing the threshold.
Because of these findings, ICER issued an “Affordability and Access Alert” for axicabtagene ciloleucel.
This alert is intended to signal when the added costs associated with a new treatment may be difficult for the healthcare system to absorb over the short-term without displacing other needed services or contributing to unsustainable growth in healthcare insurance costs.
“Based on current evidence, both therapies appear to be priced in alignment with their clinical value, but there are potential short-term affordability concerns—for axicabtagene ciloleucel under its current indication and for both treatments should they receive future approvals for broader patient populations,” Dr Ollendorf said.
Panel voting results
ICER’s report was reviewed at a public meeting of the California Technology Assessment Forum on March 2.
Most of the panel said tisagenlecleucel provides intermediate long-term value for money when treating B-ALL. However, the significant uncertainty surrounding the long-term risks and benefits of the therapy precluded a high-value vote.
After deliberating on the value of axicabtagene ciloleucel to treat NHL, the panel’s votes were split between low-value and intermediate-value, driven by similar concerns about long-term uncertainty.
Policy recommendations
Following the voting session, ICER convened a policy roundtable of experts, including physicians, patient advocates, manufacturer representatives, and payer representatives.
Based on the roundtable discussion, ICER developed recommendations for enhanced stakeholder communication, innovative payment models, generation of additional evidence, settings of care, and patient education.
“With many other potentially transformative therapies in the pipeline, stakeholders must collaborate now to develop payment and delivery systems that can ensure timely patient access, manage short-term affordability for expensive one-time treatments, and continue to reward the innovation that brings these new treatments to market,” Dr Ollendorf said.
Some of ICER’s recommendations include:
- When launching novel therapies approved with limited clinical evidence, such as CAR T-cell therapies, manufacturers and payers should consider using a lower launch price that could be increased if substantial clinical benefits are confirmed or using a higher initial price tied to a requirement for refunds or rebates if real-world evidence fails to confirm high expectations.
- Outcomes-based pricing arrangements must be linked to “meaningful clinical outcomes assessed with sufficient follow up.”
- Hospital mark-up for CAR T-cell therapies “should reflect the expected additional cost for care delivered in the hospital, rather than a percentage of the drug cost to avoid perverse incentives in choosing the treatment location.”
- Initially, CAR T-cell therapies should be delivered in “manufacturer-accredited centers to ensure the quality and appropriateness of care.” Later, “centers of excellence accredited by specialty societies” can administer these therapies, as long as providers have “sufficient expertise” to manage serious side effects.
- Centers should ensure that patients understand what to expect from CAR T-cell therapy, including long-term consequences.
- Because additional evidence on CAR T-cell therapies is needed, all patients who receive these therapies should enter into a registry with planned long-term follow-up.
- Studies should determine the optimal timing of CAR T-cell therapy in the sequence of treatments for B-ALL and NHL.
Additional recommendations and more details are available in ICER’s report.
About ICER
ICER is an independent, non-profit research institute that produces reports analyzing evidence on the effectiveness and value of drugs and other medical services.
ICER’s reports include evidence-based calculations of prices for new drugs that reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall healthcare system.
ICER’s reports incorporate input from stakeholders and are the subject of public hearings through 3 core programs: the California Technology Assessment Forum, the Midwest Comparative Effectiveness Public Advisory Council, and the New England Comparative Effectiveness Public Advisory Council.
These independent panels review ICER’s reports at public meetings to deliberate on the evidence and develop recommendations for how patients, clinicians, insurers, and policymakers can improve the quality and value of healthcare.
The Institute for Clinical and Economic Review (ICER) has made policy recommendations intended to ensure affordability and access to chimeric antigen receptor (CAR) T-cell therapies.
ICER released a Final Evidence Report on tisagenlecleucel (Kymriah, Novartis) and axicabtagene ciloleucel (Yescarta, Kite Pharma/Gilead), 2 CAR T-cell therapies approved in the US to treat B-cell acute lymphoblastic leukemia (B-ALL) and non-Hodgkin lymphoma (NHL), respectively.
The report says the pricing of these therapies aligns with patient benefit, but changes will be needed in future pricing, payment, and delivery mechanisms to ensure patient access without threatening health system affordability.
“Given the currently available evidence, these therapies appear to be effective options for those with B-ALL or NHL, though uncertainty in the evidence raised questions around the long-term value for money,” said Dan Ollendorf, PhD, ICER’s chief scientific officer.
Net health benefit
ICER’s report says tisagenlecleucel provides a net health benefit for children with B-ALL, and both tisagenlecleucel and axicabtagene ciloleucel provide a net health benefit for adults with certain types of NHL. (Novartis is seeking approval for tisagenlecleucel in NHL).
The evidence suggests there is at least a small net health benefit of the CAR T-cell therapies compared to other therapies. The benefit may be substantial, but uncertainties remain.
The data show complete remission (CR), disease-free survival (DFS), and overall survival (OS) rates are superior for NHL patients who receive axicabtagene ciloleucel, compared to patients who receive standard chemoimmunotherapy regimens.
Similarly, B-ALL patients treated with tisagenlecleucel have superior CR, DFS, and OS rates to patients treated with standard therapies. CR and OS rates are also superior in NHL patients treated with tisagenlecleucel, but DFS has not been reported in this population.
The report says there is insufficient evidence to distinguish between the 2 CAR T-cell therapies for the treatment of NHL.
Toxicity and uncertainty
The report highlights the fact that cytokine release syndrome, neurological symptoms, and B-cell aplasia have been observed in patients who receive CAR T-cell therapies. However, these sometimes severe adverse events are generally “manageable.”
In addition to toxicity, the report highlights sources of uncertainty. These include the fact that studies of tisagenlecleucel and axicabtagene ciloleucel are small, single-arm trials with short follow-up; comparisons with historical controls may be misleading; and improvements in the CAR T-cell manufacturing process may change outcomes.
Cost-effectiveness
The report states that the cost-effectiveness of each therapy fell below or within commonly cited thresholds of $50,000 to $150,000 per quality-adjusted life-year (QALY) over a lifetime.
For its analyses, ICER used the wholesale acquisition cost (WAC) plus an assumed hospital mark-up. The analyses were also based on the assumption that survival benefits observed in clinical trials would continue after the trials ended.
For tisagenlecleucel in pediatric B-ALL, the WAC is $475,000. The long-term cost-effectiveness compared to clofarabine is $45,871 per QALY gained.
For axicabtagene ciloleucel in adults with NHL, the WAC is $373,000. The long-term cost-effectiveness compared to salvage chemotherapy is $136,078 per QALY gained. The effectiveness assumptions for chemotherapy were based on an average of salvage chemotherapy regimens from the SCHOLAR-1 trial, and the cost assumptions were based on the cost of the R-DHAP (rituximab, dexamethasone, cytarabine, and cisplatin) regimen.
The report says tisagenlecleucel’s price would remain in alignment with value even if price premiums of 102% to 194% were applied.
Meanwhile, axicabtagene ciloleucel’s price could be increased by up to 11% and remain in alignment with the upper threshold ($150,000 per QALY gained) but would need to be discounted by 28% to align with the lower threshold ($100,000 per QALY gained).
Tisagenlecleucel, as a treatment for B-ALL, is not expected to cross the $915 million threshold for annual budget impact.
However, the short-term costs of axicabtagene ciloleucel for relapsed/refractory NHL could exceed the threshold. Only 38% of the estimated 5900 eligible patients could receive axicabtagene ciloleucel in a year before crossing the threshold.
Because of these findings, ICER issued an “Affordability and Access Alert” for axicabtagene ciloleucel.
This alert is intended to signal when the added costs associated with a new treatment may be difficult for the healthcare system to absorb over the short-term without displacing other needed services or contributing to unsustainable growth in healthcare insurance costs.
“Based on current evidence, both therapies appear to be priced in alignment with their clinical value, but there are potential short-term affordability concerns—for axicabtagene ciloleucel under its current indication and for both treatments should they receive future approvals for broader patient populations,” Dr Ollendorf said.
Panel voting results
ICER’s report was reviewed at a public meeting of the California Technology Assessment Forum on March 2.
Most of the panel said tisagenlecleucel provides intermediate long-term value for money when treating B-ALL. However, the significant uncertainty surrounding the long-term risks and benefits of the therapy precluded a high-value vote.
After deliberating on the value of axicabtagene ciloleucel to treat NHL, the panel’s votes were split between low-value and intermediate-value, driven by similar concerns about long-term uncertainty.
Policy recommendations
Following the voting session, ICER convened a policy roundtable of experts, including physicians, patient advocates, manufacturer representatives, and payer representatives.
Based on the roundtable discussion, ICER developed recommendations for enhanced stakeholder communication, innovative payment models, generation of additional evidence, settings of care, and patient education.
“With many other potentially transformative therapies in the pipeline, stakeholders must collaborate now to develop payment and delivery systems that can ensure timely patient access, manage short-term affordability for expensive one-time treatments, and continue to reward the innovation that brings these new treatments to market,” Dr Ollendorf said.
Some of ICER’s recommendations include:
- When launching novel therapies approved with limited clinical evidence, such as CAR T-cell therapies, manufacturers and payers should consider using a lower launch price that could be increased if substantial clinical benefits are confirmed or using a higher initial price tied to a requirement for refunds or rebates if real-world evidence fails to confirm high expectations.
- Outcomes-based pricing arrangements must be linked to “meaningful clinical outcomes assessed with sufficient follow up.”
- Hospital mark-up for CAR T-cell therapies “should reflect the expected additional cost for care delivered in the hospital, rather than a percentage of the drug cost to avoid perverse incentives in choosing the treatment location.”
- Initially, CAR T-cell therapies should be delivered in “manufacturer-accredited centers to ensure the quality and appropriateness of care.” Later, “centers of excellence accredited by specialty societies” can administer these therapies, as long as providers have “sufficient expertise” to manage serious side effects.
- Centers should ensure that patients understand what to expect from CAR T-cell therapy, including long-term consequences.
- Because additional evidence on CAR T-cell therapies is needed, all patients who receive these therapies should enter into a registry with planned long-term follow-up.
- Studies should determine the optimal timing of CAR T-cell therapy in the sequence of treatments for B-ALL and NHL.
Additional recommendations and more details are available in ICER’s report.
About ICER
ICER is an independent, non-profit research institute that produces reports analyzing evidence on the effectiveness and value of drugs and other medical services.
ICER’s reports include evidence-based calculations of prices for new drugs that reflect the degree of improvement expected in long-term patient outcomes, while also highlighting price levels that might contribute to unaffordable short-term cost growth for the overall healthcare system.
ICER’s reports incorporate input from stakeholders and are the subject of public hearings through 3 core programs: the California Technology Assessment Forum, the Midwest Comparative Effectiveness Public Advisory Council, and the New England Comparative Effectiveness Public Advisory Council.
These independent panels review ICER’s reports at public meetings to deliberate on the evidence and develop recommendations for how patients, clinicians, insurers, and policymakers can improve the quality and value of healthcare.