User login
Is the limit of viability shifting again?
Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5:e2233331. doi:10.1001/jamanet workopen.2022.33331.
EXPERT COMMENTARY
The single most important intervention available in obstetrics to improve the health outcomes of preterm newborns is the maternal administration of corticosteroids. The 27 randomized controlled trials that formed the basis for this knowledge1 did not include infants delivered at 24 weeks’ gestation or less. This has not dissuaded us, over the last several decades, from using corticosteroids for impending delivery at 24 weeks’ gestation; in the absence of randomized data, this has been based on observational evidence of benefit.
Following the 2011 publication of a retrospective cohort study that analyzed data collected by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network between 1993 and 2009 (the Carlo study),2 ACS started to be used widely even for impending delivery at 23 weeks’ gestation. That study had found that the odds of death and neurodevelopmental impairment at 18 to 22 months of age were significantly lower in cases that received ACS and were born at 23 weeks (n = 1,978). The same benefit could not be verified for infants born at 22 weeks’ gestational age (n = 402).
In a recent study conducted by the same NICHD Neonatal Research Network, antenatal steroid exposure at 21 to 22 weeks of gestation was examined.

Details of the study
Using prospectively collected data from 2016 to 2019, Chawla and colleagues conducted a retrospective cohort study that analyzed data from 431 infants who were born between 22 0/7 and 23 6/7 weeks’ gestation and received neonatal intensive care (179 infants born at 22 weeks’ gestation).3 The infants not exposed to ACS were compared with those who had partial exposure (only 1 dose) and those with complete ACS exposure (2 doses).
Complete ACS exposure proved to be beneficial, increasing survival to discharge from 35.5% in the no-exposure group to 53.9% (adjusted odds ratio [aOR], 1.95; 95% confidence interval [CI], 1.07–3.56). Of the survivors, 26.9% in the complete-exposure group had no major morbidities compared with 10% in the no-exposure group (aOR, 2.74; 95% CI, 1.19–6.30).
Study strengths and limitations
The strengths of this study include the use of a diverse, multicenter cohort, with contemporary delivery data, which increases the generalizability of the findings. The analysis included aspects often overlooked in other similar studies, such as the dose of ACS exposure and the gestational age at the time of exposure.
The observational study design, however, can suggest only associations rather than causal relationships. Observational studies also are apt to be affected by residual confounding. Such limitations can only be overcome by a randomized controlled trial, but such a trial of ACS at periviable gestational ages seems unfeasible due to limited ethical justification.
Another limitation is the reporting on outcomes as a collective group (22–23 weeks’ gestation). It is important to consider each gestational age week separately due to differences in physiology and potential biological limitations. It cannot be assumed that 22 weeks behaves like 23 weeks, just as 21 weeks is not equivalent to 22 weeks.
The study results suggest that the protective effect of ACS was dose dependent. However, the interpretation that only a complete ACS exposure was beneficial should be viewed cautiously because the study had no power to assess the impact of a partial exposure.
A further limitation is the lack of consideration in analysis for maternal comorbidities and fetal growth restriction. In the Carlo study, the beneficial effect of corticosteroids in 23-week gestational age deliveries was not demonstrable in pregnancies affected by fetal growth restriction or maternal hypertension.
Other studies considered
Given all its limitations, can we assume that the study by Chawla and colleagues has reliably refuted the Carlo study’s suggestion of lack of ACS efficacy in infants born at 22 weeks’ gestation? Taken by itself, probably not. In the context of other recent investigations, yes.
A retrospective registry study that used data from the Vermont Oxford Network for the period 2012–2016 on 1,058 infants born at 22 weeks’ gestation found that infants who were exposed to ACS and received postnatal life support were more likely to survive to hospital discharge without major morbidity compared with infants who received postnatal life support alone.4 Overall survival was 38.5% versus 17.7% (adjusted risk ratio [aRR], 2.11; 95% CI, 1.68–2.65), and survival without major morbidity was 4.4% versus 1.0% (aRR, 4.35; 95% CI, 1.84–10.28).
An even larger cohort study that used data from the National Center for Health Statistics concluded that survival at age 1 year for infants born at 22 weeks (n = 2,635) during 2009–2014 was improved in those exposed to ACS followed by postnatal life support compared with postnatal life support alone (45.2% vs 27.8%; aRR, 1.6; 95% CI, 1.2–2.1).5
A meta-analysis of observational studies that reported on infants born between 22 0/7 and 22 6/7 weeks’ gestation (n = 2,226) who received proactive neonatal treatment found that administration of ACS doubled the rate of survival when compared with no ACS administration (39% vs 19.5%; P<.01).6
In September 2021, the recommendations from the American College of Obstetricians and Gynecologists changed, stating that ACS can be considered at 22 weeks’ gestation when active postnatal management is desired.7 This recommendation is largely congruent with those from several other national and international medical organizations, including the World Association of Perinatal Medicine, the Royal Collegeof Obstetricians and Gynaecologists, and the German, Austrian and Swiss societies of gynecology and obstetrics. The implication is that the limit of viability may have shifted again, from 23 to 22 weeks’ gestation, and considering the importance of adequate timing in ACS administration (within 1 week from delivery), Chawla and colleagues posited that ACS administration can be considered as early as 21 weeks’ gestation when birth is anticipated at 22 weeks and active postnatal management is planned (notably, this should be the correct interpretation of the article title, not that ACS may be beneficial in 21-weeks’ gestational age births). ●
In 2001, the Institute of Medicine of the National Academies introduced the concept of shared decision-making as a key component of quality care. In very few other clinical situations is shared decision-making as critical as in the context of planning intervention when delivery is anticipated at 22 weeks’ gestation. The truth remains that even with the coordinated provision of ACS and active postnatal care, survival at this gestational age is still a toss-up, and survivors face a high probability of neurodevelopmental impairment and other long-term adverse health outcomes. In this setting, decision-making is complex, with the need to balance patient autonomy and nonmaleficence. On the other hand, the concept of patient autonomy is blurred because the patient (fetus) is incompetent and the negotiation is conducted between physicians and parents. However, no intervention should be undertaken unless the parents so desire. Since parental wishes are frequently emotional, overwhelmingly driving intervention, thorough and timely interdisciplinary counseling is needed. Evidence indicates that both obstetricians and neonatologists may, at times, underestimate the chance of a favorable health outcome for infants born extremely preterm.8,9 Early involvement of the neonatal and obstetric team is pivotal to put forward a coherent, nonconfusing, nonpaternalistic, balanced message. When outcomes information is shared during prenatal counseling, it should be based on local, not only national, data. Following appropriate consultation with the parents, the physicians will adjust the expectations to the local standards, outcomes data, and availability regarding periviable neonatal support.
Recent data suggest that the rate of cesarean delivery (CD) in the periviable period is increasing.10 There is no clear evidence in favor of CD to improve neonatal outcomes, whereas there is concern that periviable CD is associated with significantly increased maternal risks. Regardless of uterine incision type, periviable CD results in an increased risk of uterine rupture in a subsequent pregnancy.11 Consistent with the principle of nonmaleficence, a discussion of these risks should be included in shared decision-making.
ALEX C. VIDAEFF, MD, MPH, AND NATHAN C. SUNDGREN, MD, PHD
- McGoldrick E, Stewart F, Parker R, et al. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12(12):CD004454.
- Carlo WA, McDonald SA, Fanaroff AA, et al; Eunice Kennedy Schriver National Institute for Child Health and Human Development Neonatal Research Network. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22-25 weeks gestation. JAMA. 2011;306:2348-2358.
- Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5(9):e2233331. doi:10.1001/ jamanetworkopen.2022.33331.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks’ gestation. JAMA Netw Open. 2018;1(6):e183235. doi:10.1001/ jamanetworkopen.2018.3235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks. Am J Perinatol. November 28, 2021. doi:10.1055/s-0041-1740062.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Cahill AG, Kaimal AJ, Kuller JA, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Practice advisory: Use of antenatal corticosteroids at 22 weeks of gestation. Accessed December 7, 2022. https://www.acog.org/clinical/clinical-guidance /practice-advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation#
- Boland RA, Davis PG, Dawson JA, et al. What are we telling the parents of extremely preterm babies? Aust N Z J Obstet Gynaecol. 2016;56:274-281.
- Blanco F, Suresh G, Howard D, et al. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics. 2005;115:e478-e487.
- Rossi RM, Hall E, DeFranco EA. Contemporary trends in cesarean delivery utilization for live births between 22 0/7 and 23 6/7 weeks of gestation. Obstet Gynecol. 2019;133:451-458.
- Lannon SMR, Guthrie KA, Vanderhoeven JP, et al. Uterine rupture risk after periviable cesarean delivery. Obstet Gynecol. 2015;125:1095-1100.
Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5:e2233331. doi:10.1001/jamanet workopen.2022.33331.
EXPERT COMMENTARY
The single most important intervention available in obstetrics to improve the health outcomes of preterm newborns is the maternal administration of corticosteroids. The 27 randomized controlled trials that formed the basis for this knowledge1 did not include infants delivered at 24 weeks’ gestation or less. This has not dissuaded us, over the last several decades, from using corticosteroids for impending delivery at 24 weeks’ gestation; in the absence of randomized data, this has been based on observational evidence of benefit.
Following the 2011 publication of a retrospective cohort study that analyzed data collected by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network between 1993 and 2009 (the Carlo study),2 ACS started to be used widely even for impending delivery at 23 weeks’ gestation. That study had found that the odds of death and neurodevelopmental impairment at 18 to 22 months of age were significantly lower in cases that received ACS and were born at 23 weeks (n = 1,978). The same benefit could not be verified for infants born at 22 weeks’ gestational age (n = 402).
In a recent study conducted by the same NICHD Neonatal Research Network, antenatal steroid exposure at 21 to 22 weeks of gestation was examined.

Details of the study
Using prospectively collected data from 2016 to 2019, Chawla and colleagues conducted a retrospective cohort study that analyzed data from 431 infants who were born between 22 0/7 and 23 6/7 weeks’ gestation and received neonatal intensive care (179 infants born at 22 weeks’ gestation).3 The infants not exposed to ACS were compared with those who had partial exposure (only 1 dose) and those with complete ACS exposure (2 doses).
Complete ACS exposure proved to be beneficial, increasing survival to discharge from 35.5% in the no-exposure group to 53.9% (adjusted odds ratio [aOR], 1.95; 95% confidence interval [CI], 1.07–3.56). Of the survivors, 26.9% in the complete-exposure group had no major morbidities compared with 10% in the no-exposure group (aOR, 2.74; 95% CI, 1.19–6.30).
Study strengths and limitations
The strengths of this study include the use of a diverse, multicenter cohort, with contemporary delivery data, which increases the generalizability of the findings. The analysis included aspects often overlooked in other similar studies, such as the dose of ACS exposure and the gestational age at the time of exposure.
The observational study design, however, can suggest only associations rather than causal relationships. Observational studies also are apt to be affected by residual confounding. Such limitations can only be overcome by a randomized controlled trial, but such a trial of ACS at periviable gestational ages seems unfeasible due to limited ethical justification.
Another limitation is the reporting on outcomes as a collective group (22–23 weeks’ gestation). It is important to consider each gestational age week separately due to differences in physiology and potential biological limitations. It cannot be assumed that 22 weeks behaves like 23 weeks, just as 21 weeks is not equivalent to 22 weeks.
The study results suggest that the protective effect of ACS was dose dependent. However, the interpretation that only a complete ACS exposure was beneficial should be viewed cautiously because the study had no power to assess the impact of a partial exposure.
A further limitation is the lack of consideration in analysis for maternal comorbidities and fetal growth restriction. In the Carlo study, the beneficial effect of corticosteroids in 23-week gestational age deliveries was not demonstrable in pregnancies affected by fetal growth restriction or maternal hypertension.
Other studies considered
Given all its limitations, can we assume that the study by Chawla and colleagues has reliably refuted the Carlo study’s suggestion of lack of ACS efficacy in infants born at 22 weeks’ gestation? Taken by itself, probably not. In the context of other recent investigations, yes.
A retrospective registry study that used data from the Vermont Oxford Network for the period 2012–2016 on 1,058 infants born at 22 weeks’ gestation found that infants who were exposed to ACS and received postnatal life support were more likely to survive to hospital discharge without major morbidity compared with infants who received postnatal life support alone.4 Overall survival was 38.5% versus 17.7% (adjusted risk ratio [aRR], 2.11; 95% CI, 1.68–2.65), and survival without major morbidity was 4.4% versus 1.0% (aRR, 4.35; 95% CI, 1.84–10.28).
An even larger cohort study that used data from the National Center for Health Statistics concluded that survival at age 1 year for infants born at 22 weeks (n = 2,635) during 2009–2014 was improved in those exposed to ACS followed by postnatal life support compared with postnatal life support alone (45.2% vs 27.8%; aRR, 1.6; 95% CI, 1.2–2.1).5
A meta-analysis of observational studies that reported on infants born between 22 0/7 and 22 6/7 weeks’ gestation (n = 2,226) who received proactive neonatal treatment found that administration of ACS doubled the rate of survival when compared with no ACS administration (39% vs 19.5%; P<.01).6
In September 2021, the recommendations from the American College of Obstetricians and Gynecologists changed, stating that ACS can be considered at 22 weeks’ gestation when active postnatal management is desired.7 This recommendation is largely congruent with those from several other national and international medical organizations, including the World Association of Perinatal Medicine, the Royal Collegeof Obstetricians and Gynaecologists, and the German, Austrian and Swiss societies of gynecology and obstetrics. The implication is that the limit of viability may have shifted again, from 23 to 22 weeks’ gestation, and considering the importance of adequate timing in ACS administration (within 1 week from delivery), Chawla and colleagues posited that ACS administration can be considered as early as 21 weeks’ gestation when birth is anticipated at 22 weeks and active postnatal management is planned (notably, this should be the correct interpretation of the article title, not that ACS may be beneficial in 21-weeks’ gestational age births). ●
In 2001, the Institute of Medicine of the National Academies introduced the concept of shared decision-making as a key component of quality care. In very few other clinical situations is shared decision-making as critical as in the context of planning intervention when delivery is anticipated at 22 weeks’ gestation. The truth remains that even with the coordinated provision of ACS and active postnatal care, survival at this gestational age is still a toss-up, and survivors face a high probability of neurodevelopmental impairment and other long-term adverse health outcomes. In this setting, decision-making is complex, with the need to balance patient autonomy and nonmaleficence. On the other hand, the concept of patient autonomy is blurred because the patient (fetus) is incompetent and the negotiation is conducted between physicians and parents. However, no intervention should be undertaken unless the parents so desire. Since parental wishes are frequently emotional, overwhelmingly driving intervention, thorough and timely interdisciplinary counseling is needed. Evidence indicates that both obstetricians and neonatologists may, at times, underestimate the chance of a favorable health outcome for infants born extremely preterm.8,9 Early involvement of the neonatal and obstetric team is pivotal to put forward a coherent, nonconfusing, nonpaternalistic, balanced message. When outcomes information is shared during prenatal counseling, it should be based on local, not only national, data. Following appropriate consultation with the parents, the physicians will adjust the expectations to the local standards, outcomes data, and availability regarding periviable neonatal support.
Recent data suggest that the rate of cesarean delivery (CD) in the periviable period is increasing.10 There is no clear evidence in favor of CD to improve neonatal outcomes, whereas there is concern that periviable CD is associated with significantly increased maternal risks. Regardless of uterine incision type, periviable CD results in an increased risk of uterine rupture in a subsequent pregnancy.11 Consistent with the principle of nonmaleficence, a discussion of these risks should be included in shared decision-making.
ALEX C. VIDAEFF, MD, MPH, AND NATHAN C. SUNDGREN, MD, PHD
Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5:e2233331. doi:10.1001/jamanet workopen.2022.33331.
EXPERT COMMENTARY
The single most important intervention available in obstetrics to improve the health outcomes of preterm newborns is the maternal administration of corticosteroids. The 27 randomized controlled trials that formed the basis for this knowledge1 did not include infants delivered at 24 weeks’ gestation or less. This has not dissuaded us, over the last several decades, from using corticosteroids for impending delivery at 24 weeks’ gestation; in the absence of randomized data, this has been based on observational evidence of benefit.
Following the 2011 publication of a retrospective cohort study that analyzed data collected by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Neonatal Research Network between 1993 and 2009 (the Carlo study),2 ACS started to be used widely even for impending delivery at 23 weeks’ gestation. That study had found that the odds of death and neurodevelopmental impairment at 18 to 22 months of age were significantly lower in cases that received ACS and were born at 23 weeks (n = 1,978). The same benefit could not be verified for infants born at 22 weeks’ gestational age (n = 402).
In a recent study conducted by the same NICHD Neonatal Research Network, antenatal steroid exposure at 21 to 22 weeks of gestation was examined.

Details of the study
Using prospectively collected data from 2016 to 2019, Chawla and colleagues conducted a retrospective cohort study that analyzed data from 431 infants who were born between 22 0/7 and 23 6/7 weeks’ gestation and received neonatal intensive care (179 infants born at 22 weeks’ gestation).3 The infants not exposed to ACS were compared with those who had partial exposure (only 1 dose) and those with complete ACS exposure (2 doses).
Complete ACS exposure proved to be beneficial, increasing survival to discharge from 35.5% in the no-exposure group to 53.9% (adjusted odds ratio [aOR], 1.95; 95% confidence interval [CI], 1.07–3.56). Of the survivors, 26.9% in the complete-exposure group had no major morbidities compared with 10% in the no-exposure group (aOR, 2.74; 95% CI, 1.19–6.30).
Study strengths and limitations
The strengths of this study include the use of a diverse, multicenter cohort, with contemporary delivery data, which increases the generalizability of the findings. The analysis included aspects often overlooked in other similar studies, such as the dose of ACS exposure and the gestational age at the time of exposure.
The observational study design, however, can suggest only associations rather than causal relationships. Observational studies also are apt to be affected by residual confounding. Such limitations can only be overcome by a randomized controlled trial, but such a trial of ACS at periviable gestational ages seems unfeasible due to limited ethical justification.
Another limitation is the reporting on outcomes as a collective group (22–23 weeks’ gestation). It is important to consider each gestational age week separately due to differences in physiology and potential biological limitations. It cannot be assumed that 22 weeks behaves like 23 weeks, just as 21 weeks is not equivalent to 22 weeks.
The study results suggest that the protective effect of ACS was dose dependent. However, the interpretation that only a complete ACS exposure was beneficial should be viewed cautiously because the study had no power to assess the impact of a partial exposure.
A further limitation is the lack of consideration in analysis for maternal comorbidities and fetal growth restriction. In the Carlo study, the beneficial effect of corticosteroids in 23-week gestational age deliveries was not demonstrable in pregnancies affected by fetal growth restriction or maternal hypertension.
Other studies considered
Given all its limitations, can we assume that the study by Chawla and colleagues has reliably refuted the Carlo study’s suggestion of lack of ACS efficacy in infants born at 22 weeks’ gestation? Taken by itself, probably not. In the context of other recent investigations, yes.
A retrospective registry study that used data from the Vermont Oxford Network for the period 2012–2016 on 1,058 infants born at 22 weeks’ gestation found that infants who were exposed to ACS and received postnatal life support were more likely to survive to hospital discharge without major morbidity compared with infants who received postnatal life support alone.4 Overall survival was 38.5% versus 17.7% (adjusted risk ratio [aRR], 2.11; 95% CI, 1.68–2.65), and survival without major morbidity was 4.4% versus 1.0% (aRR, 4.35; 95% CI, 1.84–10.28).
An even larger cohort study that used data from the National Center for Health Statistics concluded that survival at age 1 year for infants born at 22 weeks (n = 2,635) during 2009–2014 was improved in those exposed to ACS followed by postnatal life support compared with postnatal life support alone (45.2% vs 27.8%; aRR, 1.6; 95% CI, 1.2–2.1).5
A meta-analysis of observational studies that reported on infants born between 22 0/7 and 22 6/7 weeks’ gestation (n = 2,226) who received proactive neonatal treatment found that administration of ACS doubled the rate of survival when compared with no ACS administration (39% vs 19.5%; P<.01).6
In September 2021, the recommendations from the American College of Obstetricians and Gynecologists changed, stating that ACS can be considered at 22 weeks’ gestation when active postnatal management is desired.7 This recommendation is largely congruent with those from several other national and international medical organizations, including the World Association of Perinatal Medicine, the Royal Collegeof Obstetricians and Gynaecologists, and the German, Austrian and Swiss societies of gynecology and obstetrics. The implication is that the limit of viability may have shifted again, from 23 to 22 weeks’ gestation, and considering the importance of adequate timing in ACS administration (within 1 week from delivery), Chawla and colleagues posited that ACS administration can be considered as early as 21 weeks’ gestation when birth is anticipated at 22 weeks and active postnatal management is planned (notably, this should be the correct interpretation of the article title, not that ACS may be beneficial in 21-weeks’ gestational age births). ●
In 2001, the Institute of Medicine of the National Academies introduced the concept of shared decision-making as a key component of quality care. In very few other clinical situations is shared decision-making as critical as in the context of planning intervention when delivery is anticipated at 22 weeks’ gestation. The truth remains that even with the coordinated provision of ACS and active postnatal care, survival at this gestational age is still a toss-up, and survivors face a high probability of neurodevelopmental impairment and other long-term adverse health outcomes. In this setting, decision-making is complex, with the need to balance patient autonomy and nonmaleficence. On the other hand, the concept of patient autonomy is blurred because the patient (fetus) is incompetent and the negotiation is conducted between physicians and parents. However, no intervention should be undertaken unless the parents so desire. Since parental wishes are frequently emotional, overwhelmingly driving intervention, thorough and timely interdisciplinary counseling is needed. Evidence indicates that both obstetricians and neonatologists may, at times, underestimate the chance of a favorable health outcome for infants born extremely preterm.8,9 Early involvement of the neonatal and obstetric team is pivotal to put forward a coherent, nonconfusing, nonpaternalistic, balanced message. When outcomes information is shared during prenatal counseling, it should be based on local, not only national, data. Following appropriate consultation with the parents, the physicians will adjust the expectations to the local standards, outcomes data, and availability regarding periviable neonatal support.
Recent data suggest that the rate of cesarean delivery (CD) in the periviable period is increasing.10 There is no clear evidence in favor of CD to improve neonatal outcomes, whereas there is concern that periviable CD is associated with significantly increased maternal risks. Regardless of uterine incision type, periviable CD results in an increased risk of uterine rupture in a subsequent pregnancy.11 Consistent with the principle of nonmaleficence, a discussion of these risks should be included in shared decision-making.
ALEX C. VIDAEFF, MD, MPH, AND NATHAN C. SUNDGREN, MD, PHD
- McGoldrick E, Stewart F, Parker R, et al. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12(12):CD004454.
- Carlo WA, McDonald SA, Fanaroff AA, et al; Eunice Kennedy Schriver National Institute for Child Health and Human Development Neonatal Research Network. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22-25 weeks gestation. JAMA. 2011;306:2348-2358.
- Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5(9):e2233331. doi:10.1001/ jamanetworkopen.2022.33331.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks’ gestation. JAMA Netw Open. 2018;1(6):e183235. doi:10.1001/ jamanetworkopen.2018.3235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks. Am J Perinatol. November 28, 2021. doi:10.1055/s-0041-1740062.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Cahill AG, Kaimal AJ, Kuller JA, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Practice advisory: Use of antenatal corticosteroids at 22 weeks of gestation. Accessed December 7, 2022. https://www.acog.org/clinical/clinical-guidance /practice-advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation#
- Boland RA, Davis PG, Dawson JA, et al. What are we telling the parents of extremely preterm babies? Aust N Z J Obstet Gynaecol. 2016;56:274-281.
- Blanco F, Suresh G, Howard D, et al. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics. 2005;115:e478-e487.
- Rossi RM, Hall E, DeFranco EA. Contemporary trends in cesarean delivery utilization for live births between 22 0/7 and 23 6/7 weeks of gestation. Obstet Gynecol. 2019;133:451-458.
- Lannon SMR, Guthrie KA, Vanderhoeven JP, et al. Uterine rupture risk after periviable cesarean delivery. Obstet Gynecol. 2015;125:1095-1100.
- McGoldrick E, Stewart F, Parker R, et al. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12(12):CD004454.
- Carlo WA, McDonald SA, Fanaroff AA, et al; Eunice Kennedy Schriver National Institute for Child Health and Human Development Neonatal Research Network. Association of antenatal corticosteroids with mortality and neurodevelopmental outcomes among infants born at 22-25 weeks gestation. JAMA. 2011;306:2348-2358.
- Chawla S, Wyckoff MH, Rysavy MA, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Association of antenatal steroid exposure at 21 to 22 weeks of gestation with neonatal survival and survival without morbidities. JAMA Netw Open. 2022;5(9):e2233331. doi:10.1001/ jamanetworkopen.2022.33331.
- Ehret DEY, Edwards EM, Greenberg LT, et al. Association of antenatal steroid exposure with survival among infants receiving postnatal life support at 22 to 25 weeks’ gestation. JAMA Netw Open. 2018;1(6):e183235. doi:10.1001/ jamanetworkopen.2018.3235.
- Rossi RM, DeFranco EA, Hall ES. Association of antenatal corticosteroid exposure and infant survival at 22 and 23 weeks. Am J Perinatol. November 28, 2021. doi:10.1055/s-0041-1740062.
- Backes CH, Rivera BK, Pavlek L, et al. Proactive neonatal treatment at 22 weeks of gestation: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224:158-174.
- Cahill AG, Kaimal AJ, Kuller JA, et al; American College of Obstetricians and Gynecologists and Society for Maternal-Fetal Medicine. Practice advisory: Use of antenatal corticosteroids at 22 weeks of gestation. Accessed December 7, 2022. https://www.acog.org/clinical/clinical-guidance /practice-advisory/articles/2021/09/use-of-antenatal -corticosteroids-at-22-weeks-of-gestation#
- Boland RA, Davis PG, Dawson JA, et al. What are we telling the parents of extremely preterm babies? Aust N Z J Obstet Gynaecol. 2016;56:274-281.
- Blanco F, Suresh G, Howard D, et al. Ensuring accurate knowledge of prematurity outcomes for prenatal counseling. Pediatrics. 2005;115:e478-e487.
- Rossi RM, Hall E, DeFranco EA. Contemporary trends in cesarean delivery utilization for live births between 22 0/7 and 23 6/7 weeks of gestation. Obstet Gynecol. 2019;133:451-458.
- Lannon SMR, Guthrie KA, Vanderhoeven JP, et al. Uterine rupture risk after periviable cesarean delivery. Obstet Gynecol. 2015;125:1095-1100.
Progesterone for preterm delivery prevention
Researchers have been studying the use of exogenous progestins for prevention of preterm delivery (PTD) for almost 60 years, but conflicting results contribute to an ongoing debate. Interpretation of the available data is particularly difficult because different forms and doses of progestins have been used in disparate study populations.
Based on available data, progesterone supplementation is not effective as a primary prevention strategy for PTD in the general low-risk obstetric population. PTD is a complex problem with varied and incompletely elucidated pathogenic pathways, making it unlikely that one interventional approach would be effective for all pregnant women. As a result, emerging indications for the use of progesterone are based on risk factors for PTD (ie, prior PTD and/or short cervix). However, this secondary prevention approach is a limiting factor in itself because 50% of women destined to have a PTD have no identifiable risk factors.1 In addition, researchers have found that progestins are ineffective at delaying delivery for women with multiple gestation, suggesting that a distinct underlying mechanism of early parturition is present in these women, and that this mechanism is unresponsive to progestins.2
The formulations used in the study of progestin supplementation for PTD prevention have been almost exclusively either the synthetic 17 alpha-hydroxyprogesterone caproate (17-OHPC) or natural progesterone administered orally or vaginally. In 2003, the American College of Obstetricians and Gynecologists (ACOG) supported the use of progesterone to reduce the rate of PTD,3 and in 2011, the US Food and Drug Administration (FDA) approved 17-OHPC for use as prophylaxis against recurrent PTD. As a result, in recent years, the perceived standard of care for a majority of practitioners in the United States had been that all women with a previous preterm birth should be offered 17-OHPC. It may be interesting to note that in other parts of the world, the same enthusiastic adoption did not occur. For example, in Australia and New Zealand in 2007, only 5% of practitioners were using progesterone for this indication.4 Further, 17-OHPC is not recommended by professional guidelines in the United Kingdom and has remained unavailable in Germany.
The publication in 2019 of the PROLONG trial called into question the use of 17-OHPC for the prevention of PTD.5 In the December 2019 issue of OBG Management (“Managing preterm birth in those at risk: Expert strategies”), I expressed the opinion that with only rare exceptions, 17-OHPC is no longer a viable option for recurrent PTD prevention.6 In light of these developments, what scientific evidence is relevant and applicable to the care of women at risk for PTD?
Continue to: Case 1 Previous spontaneous PTD at 31 weeks...
Case 1 Previous spontaneous PTD at 31 weeks
MC is an asymptomatic 32-year-old woman with a singleton pregnancy at 13 weeks’ gestation. You see her for a maternal-fetal medicine consultation because 2 years ago she had a spontaneous PTD at 31 weeks’ gestation. What management recommendations can you make to decrease her risk of recurrent PTD?
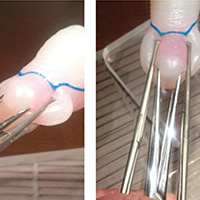
Cervical length measurement narrows in on risk
The indication “previous preterm birth” is largely meaningless because of the heterogeneity in preterm birth pathways (preterm birth as a syndrome7) and inadequate risk characterization. Among women who experience a spontaneous PTD, 70% to 80% do not deliver prematurely in subsequent pregnancies.8 To better characterize the risk of PTD recurrence, ultrasound assessment of cervical length should be used. Research has shown that among women with a prior spontaneous PTD who maintain a normal cervical length until 24 weeks’ gestation, more than 90% will deliver at 35 weeks or after without intervention.9 Such an approach not only identifies the subgroup of women at significantly increased risk of recurrence but also eliminates unnecessary interventions.
Cervical ultrasound surveillance should be initiated at 16 weeks’ gestation. A short cervix before 16 weeks is not associated with a statistically significant increase in risk for PTD.10 Shortening of the cervix begins approximately 10 weeks before delivery in any gestational age group.11 Therefore, ultrasound assessment of the cervix at 28 weeks and after is irrelevant. In addition, after 28 weeks, cervical length varies greatly leading to loss in the predictive power of the cervical measurement.12 Based on these considerations, cervical surveillance may be extended up to 26 weeks. Although cervical cerclage is not an option in the United States in cases in which a short cervix is detected between 24 and 26 weeks, vaginal progesterone supplementation may still be considered.
Case 1 Continued
MC was started on ultrasound cervical surveillance at 16 weeks’ gestation. Her cervical length was initially normal (> 2.5 cm), but at 18 weeks the measurement was 2.2 cm. What is your recommendation?
The value of vaginal progesterone
There appears to be increasing consensus on the value of vaginal progesterone for women with a midtrimester short cervix on sonography, with or without a history of PTD. An individual patient data meta-analysis demonstrated the benefits of vaginal progesterone.13 Although there was no evidence of an effect on PTD at less than 37 weeks, the rates of PTD at less than 36 weeks and spontaneous PTD at less than 34 weeks were significantly reduced (by 20% and 28%, respectively). Also, there was a significant reduction in the risk of respiratory distress syndrome (53%) and composite neonatal morbidity and mortality (41%), with no significant impact on infant development up to the second year of life.13
The lack of generalizable evidence of benefit on childhood outcomes, combined with considerable uncertainty about the exact role and mechanism of action of exogenous progestins, contribute to the ongoing debate. Vaginal progesterone dosage regimens have been based on extrapolations from experience with progesterone in nonpregnant women, and recent pharmacokinetic studies have revealed how precarious such extrapolations may be. As an example, in nonpregnant women, the bioavailability of oral and vaginal progesterone is similar.14 In pregnancy, however, while daily oral progesterone doubles a pregnant woman’s serum progesterone level,15 daily vaginal administration of progesterone results in only a modest rise in serum progesterone, with a coefficient of variation among individuals that is double that outside of pregnancy.16 It is, therefore, considered that vaginal progesterone in pregnancy may have a local action secondary to the uterine first-pass effect. The uterine first-pass effect for vaginal progesterone was described in nonpregnant women and is only assumed to occur in pregnancy as well. 17
After evaluating the data from the largest available study of vaginal progesterone,18 the FDA concluded in 2012 that the study did not meet the statistical significance generally expected to support the approval of a new product. However, according to a more comprehensive evidence review developed in 2019 by the National Guideline Alliance in the United Kingdom, women with a history of PTD and women with a short cervix derive an important benefit from the use of vaginal progesterone; thus, this intervention should be offered to them.19 At this time, a short cervix and PTD prevention are not considered FDA-approved indications for progesterone supplementation in pregnancy. However, vaginal progesterone is FDA approved for use in pregnant women with a history of infertility.
Continue to: Case 1 Continued...
Case 1 Continued
MC initiated treatment with daily vaginal progesterone at 18 weeks’ gestation and returned for ultrasound cervical length examination weekly instead of every other week. At 20 weeks’ gestation, cervical length was 2.0 cm; the following week it was 1.4 cm. What would you recommend at this point?
When to consider cerclage
If cervical shortening progresses to about 1.5 cm while a woman is being treated with vaginal progesterone, cerclage may be considered. The benefit of cerclage in patients with prior PTD and a short cervix was highlighted in a 2018 Cochrane Review.20 In this stepwise management approach to a short cervix, waiting for a cervix to be less than 1.5 cm may be unadvisable. Under conditions of a very short cervix that is frequently dilated with exposure of fetal membranes, ascending subclinical intra-amniotic infection may already be present, reducing the efficacy of any preventive measures. Preferential consideration for cerclage from the start over initial vaginal progesterone also may be appropriate when there is a history of 2 spontaneous PTDs or mid-trimester losses, a history of a successful cerclage, or with a very short cervix (< 1.0 cm) at the initial evaluation. As for the latter, a 2018 individual patient data meta-analysis of vaginal progesterone found no benefit when the cervix was less than 1.0 cm.13
Progesterone plus cerclage likely to add benefit
The results of an adjusted indirect comparison meta-analysis suggest that both interventions—vaginal progesterone and cerclage—are equally effective.21 Assuming that there is no clinically meaningful difference in benefit associated with these 2 treatments, the next logical question is whether combining the 2 therapies provides any added benefit; limited observational data seem to suggest that it does. In a retrospective cohort of 86 consecutive singleton pregnancies among women who underwent ultrasound-indicated cerclage, those who used vaginal progesterone after cerclage (n = 45) had a lower rate of PTD.22 Also, a small (66 cases) case-control study demonstrated the benefit of administration of vaginal progesterone as a rescue intervention in women with cerclage and progressive cervical shortening despite cerclage.23
Case 2 Woman experiences adverse effects from vaginal progesterone
MS is a 25-year-old G2P0101 who was started on vaginal progesterone as prophylaxis for recurrent PTD. She is now at 20 weeks’ gestation, with a stable remnant cervical length of 2.0 cm. She is reporting an increasing vaginal burning sensation and vaginal discharge caused by the nightly vaginal progesterone applications, to the point that she is unwilling to continue the treatment. She asks if any alternatives to vaginal progesterone are available to decrease her risk of PTD.
Continue to: Is oral progesterone an option?...
Is oral progesterone an option?
In the 1980s and 1990s, oral micronized progesterone was widely used in France at doses of 900 to 1,200 mg/d for women at risk for PTD. The practice was stopped when secondary hepatic effects, including cholestasis of pregnancy, were reported at a higher rate in treated women.24 A rise in the serum concentration of progesterone metabolites has been associated with impaired biliary excretion and subsequent accumulation of bile acids.25 In other reports, elevated serum transaminase activity was found in pregnant women treated with oral micronized progesterone, and withdrawal of treatment frequently has led to improvement in transaminase levels.26 The synthesis of endogenous progesterone during normal pregnancy is between 250 and 500 mg/d,26 and experts have expressed concern that exogenous progesterone supplementation may impose an additional load on the hepatic transport of sulfated metabolites. Unlike orally administered progesterone, progestins given by the vaginal route avoid the hepatic first-pass effect. For this reason, they may be associated with less hepatic dysfunction.
Although not recommended by professional guidelines, oral progesterone administration for the prevention of PTD has been used in the United States. A 2015 survey of Wisconsin prenatal care providers found that of those who prescribed any progesterone for PTD prevention, oral progesterone was prescribed by 13.1% of obstetricians, 24.4% of midwives, and 40.7% of family medicine practitioners.27
Some limited recent evidence from a meta-analysis of 3 trials investigating oral progesterone versus placebo suggests effectiveness in the prevention of recurrent PTD and reduction in perinatal morbidity and mortality.15 However, the number of cases included in the meta-analysis (386) was too small to support definitive clinical recommendations. Furthermore, questions have been raised in the literature about the reliability of the largest trial included in that meta-analysis.28
Case 3 Two previous spontaneous PTDs
A 29-year-old G3P0201 presents for her first prenatal appointment at 10 weeks’ gestation. With her first pregnancy she had a spontaneous PTD at 23 weeks, and the neonate did not survive. In her second pregnancy, she was treated with 17-OHPC from 16 weeks’ gestation. She had a spontaneous PTD at 29 weeks, and that child is developing normally by her report. She believes that 17-OHPC helped her in her last pregnancy and is anxious about the risk for still another PTD. Consistent with the concept of shared decision-making, you inform her of the results of the recent PROLONG trial and statements on the subject released by professional organizations such as ACOG and the Society for Maternal-Fetal Medicine (SMFM). What options does she have?
17-OHPC may be a possibility in very high-risk women
According to a SMFM statement released in the wake of the PROLONG trial publication, “. . . SMFM believes that it is reasonable for providers to use 17-OHPC in women with a profile more representative of the very high-risk population reported in the Meis trial”.29 Only a few women will have a recurrence risk of PTD over 50%, as was the background event rate in the Meis trial.30 Such a risk level may be suspected, as an example, in women with 2 or more prior early (before 34 weeks) PTDs without intervening term deliveries. Even in those cases, if treatment with 17-OHPC is decided upon, ultrasound cervical surveillance should be added as an additional safety measure. ●
- Iams JD, Goldenberg RL, Mercer BM, et al. The preterm prediction study: can low-risk women destined for spontaneous preterm birth be identified? Am J Obstet Gynecol. 2001;184:652-655.
- Murray SR, Stock SJ, Cowan S, et al. Spontaneous preterm birth prevention in multiple pregnancy. Obstet Gynecol. 2018;20:57-63.
- American College of Obstetricians and Gynecologists. ACOG committee opinion. Use of progesterone to reduce preterm birth. Obstet Gynecol. 2003;102:1115-1116.
- Dodd JM, Ashwood P, Flenady V, et al. A survey of clinician and patient attitudes towards the use of progesterone for women at risk of preterm birth. Aust N Z J Obstet Gynaecol. 2007;47:106-109.
- Blackwell SC, Gyamfi -Bannerman C, Biggio JR, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2020;37:127-136.
- Duff P, Vidaeff AC, Ross MG, Norwitz ER. Managing preterm birth in those at risk: expert strategies. OBG Manag. 2019;31:39-42.
- Romero R, Mazor M, Munoz H, et al. The preterm labor syndrome. Ann N Y Acad Sci. 1994;734:414-429.
- Phillips C, Velji Z, Hanly C, et al. Risk of recurrent spontaneous preterm birth: a systematic review and meta-analysis. BMJ Open. 2017;7:e015402.
- Berghella V, Seibel-Seamon J. Contemporary use of cervical cerclage. Clin Obstet Gynecol. 2007;50:468-477.
- Naim A, Haberman S, Burgess T, et al. Changes in cervical length and the risk of preterm labor. Am J Obstet Gynecol. 2002;186:887-889.
- Zilianti M, Azuaga A, Calderon F, et al. Monitoring the effacement of the uterine cervix by transperineal sonography: a new perspective. J Ultrasound Med. 1995;14:719-724.
- Goldenberg RL, Iams JD, Miodovnik M, et al. The preterm prediction study: risk factors in twin gestation. Am J Obstet Gynecol. 1996;175:1047-1053.
- Romero R, Conde-Agudelo A, Da Fonseca E, et al. Vaginal progesterone for preventing preterm birth and adverse perinatal outcomes in singleton gestations with a short cervix: a meta-analysis of individual patient data. Am J Obstet Gynecol. 2018;218:161-180.
- Norman T, Morse C, Dennerstein L. Comparative bioavailability of orally and vaginally administered progesterone. Fertil Steril. 1991;56:1034-1039.
- Boelig RC, Della Corte L, Ashoush S, et al. Oral progesterone for the prevention of recurrent preterm birth: systematic review and metaanalysis. Am J Obstet Gynecol MFM. 2019;1:50-62.
- Boelig RC, Zuppa AF, Kraft WK, et al. Pharmacokinetics of vaginal progesterone in pregnancy. Am J Obstet Gynecol. 2019;221:263.e1-7.
- Bulletti C, de Ziegler D, Flamigni C, et al. Targeted drug delivery in gynaecology: the first uterine pass effect. Hum Reprod. 1997;12:1073-1079.
- Hassan SS, Romero R, Vidyadhari D, et al. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebocontrolled trial. Ultrasound Obstet Gynecol. 2011;38:18-31.
- Preterm labour and birth. Evidence review for clinical effectiveness of prophylactic progesterone in preventing preterm labour. London: National Institute for Health and Care Excellence (UK); August 2019.
- Alfirevic Z, Stampalija T, Medley N. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2017;6:CD008991.
- Conde-Agudelo A, Romero R, Da Fonseca E, et al. Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: updated indirect comparison meta-analysis. Am J Obstet Gynecol. 2018;219:10-25.
- Park JY, Jung YM, Kook S-Y, et al. The effect of postoperative vaginal progesterone in ultrasound-indicated cerclage to prevent preterm birth. J Matern Fetal Neonatal Med. 2019:1-8.
- Roman AR, Da Silva Costa F, et al. Rescue adjuvant vaginal progesterone may improve outcomes in cervical cerclage failure. Geburt Frauen. 2018;78:785-790.
- Benifle JL, Dumont M, Levardon M, et al. Effects of natural micronized progesterone on the liver in the third trimester of pregnancy. Contracept Fertil Sex. 1997;25:165-169.
- Vallejo M, Briz O, Serrano MA, et al. Potential role of transinhibition of the bile salt export pump by progesterone metabolites in the etiopathogenesis of intrahepatic cholestasis of pregnancy. J Hepatol. 2006;44:1150-1157.
- Bacq Y, Sapey T, Bréchot MC, et al. Intrahepatic cholestasis of pregnancy: a French prospective study. Hepatology. 1997;26:358-364.
- Hoppe K, Kramer RD, Ha B, et al. Progesterone supplementation for the prevention of preterm birth: provider practice in Wisconsin. WMJ. 2019;118:126-131.
- Katsanevakis E, Mol BW, Thornton J. A question about the reliability of a recent trial of progesterone for preterm birth prevention, published in Acta. Acta Obstet Gynecol Scand. 2020;99:426.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. SMFM Statement: use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://www.smfm.org/publications/280smfm-statement-use-of-17-alpha-hydroxyprogesteronecaproate-for-prevention-of-recurrent-preterm-birth. Accessed March 23, 2020.
- Meis PJ, Klebanoff M, Thom E, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;384:2379-2385.
Researchers have been studying the use of exogenous progestins for prevention of preterm delivery (PTD) for almost 60 years, but conflicting results contribute to an ongoing debate. Interpretation of the available data is particularly difficult because different forms and doses of progestins have been used in disparate study populations.
Based on available data, progesterone supplementation is not effective as a primary prevention strategy for PTD in the general low-risk obstetric population. PTD is a complex problem with varied and incompletely elucidated pathogenic pathways, making it unlikely that one interventional approach would be effective for all pregnant women. As a result, emerging indications for the use of progesterone are based on risk factors for PTD (ie, prior PTD and/or short cervix). However, this secondary prevention approach is a limiting factor in itself because 50% of women destined to have a PTD have no identifiable risk factors.1 In addition, researchers have found that progestins are ineffective at delaying delivery for women with multiple gestation, suggesting that a distinct underlying mechanism of early parturition is present in these women, and that this mechanism is unresponsive to progestins.2
The formulations used in the study of progestin supplementation for PTD prevention have been almost exclusively either the synthetic 17 alpha-hydroxyprogesterone caproate (17-OHPC) or natural progesterone administered orally or vaginally. In 2003, the American College of Obstetricians and Gynecologists (ACOG) supported the use of progesterone to reduce the rate of PTD,3 and in 2011, the US Food and Drug Administration (FDA) approved 17-OHPC for use as prophylaxis against recurrent PTD. As a result, in recent years, the perceived standard of care for a majority of practitioners in the United States had been that all women with a previous preterm birth should be offered 17-OHPC. It may be interesting to note that in other parts of the world, the same enthusiastic adoption did not occur. For example, in Australia and New Zealand in 2007, only 5% of practitioners were using progesterone for this indication.4 Further, 17-OHPC is not recommended by professional guidelines in the United Kingdom and has remained unavailable in Germany.
The publication in 2019 of the PROLONG trial called into question the use of 17-OHPC for the prevention of PTD.5 In the December 2019 issue of OBG Management (“Managing preterm birth in those at risk: Expert strategies”), I expressed the opinion that with only rare exceptions, 17-OHPC is no longer a viable option for recurrent PTD prevention.6 In light of these developments, what scientific evidence is relevant and applicable to the care of women at risk for PTD?
Continue to: Case 1 Previous spontaneous PTD at 31 weeks...
Case 1 Previous spontaneous PTD at 31 weeks
MC is an asymptomatic 32-year-old woman with a singleton pregnancy at 13 weeks’ gestation. You see her for a maternal-fetal medicine consultation because 2 years ago she had a spontaneous PTD at 31 weeks’ gestation. What management recommendations can you make to decrease her risk of recurrent PTD?
Cervical length measurement narrows in on risk
The indication “previous preterm birth” is largely meaningless because of the heterogeneity in preterm birth pathways (preterm birth as a syndrome7) and inadequate risk characterization. Among women who experience a spontaneous PTD, 70% to 80% do not deliver prematurely in subsequent pregnancies.8 To better characterize the risk of PTD recurrence, ultrasound assessment of cervical length should be used. Research has shown that among women with a prior spontaneous PTD who maintain a normal cervical length until 24 weeks’ gestation, more than 90% will deliver at 35 weeks or after without intervention.9 Such an approach not only identifies the subgroup of women at significantly increased risk of recurrence but also eliminates unnecessary interventions.
Cervical ultrasound surveillance should be initiated at 16 weeks’ gestation. A short cervix before 16 weeks is not associated with a statistically significant increase in risk for PTD.10 Shortening of the cervix begins approximately 10 weeks before delivery in any gestational age group.11 Therefore, ultrasound assessment of the cervix at 28 weeks and after is irrelevant. In addition, after 28 weeks, cervical length varies greatly leading to loss in the predictive power of the cervical measurement.12 Based on these considerations, cervical surveillance may be extended up to 26 weeks. Although cervical cerclage is not an option in the United States in cases in which a short cervix is detected between 24 and 26 weeks, vaginal progesterone supplementation may still be considered.
Case 1 Continued
MC was started on ultrasound cervical surveillance at 16 weeks’ gestation. Her cervical length was initially normal (> 2.5 cm), but at 18 weeks the measurement was 2.2 cm. What is your recommendation?
The value of vaginal progesterone
There appears to be increasing consensus on the value of vaginal progesterone for women with a midtrimester short cervix on sonography, with or without a history of PTD. An individual patient data meta-analysis demonstrated the benefits of vaginal progesterone.13 Although there was no evidence of an effect on PTD at less than 37 weeks, the rates of PTD at less than 36 weeks and spontaneous PTD at less than 34 weeks were significantly reduced (by 20% and 28%, respectively). Also, there was a significant reduction in the risk of respiratory distress syndrome (53%) and composite neonatal morbidity and mortality (41%), with no significant impact on infant development up to the second year of life.13
The lack of generalizable evidence of benefit on childhood outcomes, combined with considerable uncertainty about the exact role and mechanism of action of exogenous progestins, contribute to the ongoing debate. Vaginal progesterone dosage regimens have been based on extrapolations from experience with progesterone in nonpregnant women, and recent pharmacokinetic studies have revealed how precarious such extrapolations may be. As an example, in nonpregnant women, the bioavailability of oral and vaginal progesterone is similar.14 In pregnancy, however, while daily oral progesterone doubles a pregnant woman’s serum progesterone level,15 daily vaginal administration of progesterone results in only a modest rise in serum progesterone, with a coefficient of variation among individuals that is double that outside of pregnancy.16 It is, therefore, considered that vaginal progesterone in pregnancy may have a local action secondary to the uterine first-pass effect. The uterine first-pass effect for vaginal progesterone was described in nonpregnant women and is only assumed to occur in pregnancy as well. 17
After evaluating the data from the largest available study of vaginal progesterone,18 the FDA concluded in 2012 that the study did not meet the statistical significance generally expected to support the approval of a new product. However, according to a more comprehensive evidence review developed in 2019 by the National Guideline Alliance in the United Kingdom, women with a history of PTD and women with a short cervix derive an important benefit from the use of vaginal progesterone; thus, this intervention should be offered to them.19 At this time, a short cervix and PTD prevention are not considered FDA-approved indications for progesterone supplementation in pregnancy. However, vaginal progesterone is FDA approved for use in pregnant women with a history of infertility.
Continue to: Case 1 Continued...
Case 1 Continued
MC initiated treatment with daily vaginal progesterone at 18 weeks’ gestation and returned for ultrasound cervical length examination weekly instead of every other week. At 20 weeks’ gestation, cervical length was 2.0 cm; the following week it was 1.4 cm. What would you recommend at this point?
When to consider cerclage
If cervical shortening progresses to about 1.5 cm while a woman is being treated with vaginal progesterone, cerclage may be considered. The benefit of cerclage in patients with prior PTD and a short cervix was highlighted in a 2018 Cochrane Review.20 In this stepwise management approach to a short cervix, waiting for a cervix to be less than 1.5 cm may be unadvisable. Under conditions of a very short cervix that is frequently dilated with exposure of fetal membranes, ascending subclinical intra-amniotic infection may already be present, reducing the efficacy of any preventive measures. Preferential consideration for cerclage from the start over initial vaginal progesterone also may be appropriate when there is a history of 2 spontaneous PTDs or mid-trimester losses, a history of a successful cerclage, or with a very short cervix (< 1.0 cm) at the initial evaluation. As for the latter, a 2018 individual patient data meta-analysis of vaginal progesterone found no benefit when the cervix was less than 1.0 cm.13
Progesterone plus cerclage likely to add benefit
The results of an adjusted indirect comparison meta-analysis suggest that both interventions—vaginal progesterone and cerclage—are equally effective.21 Assuming that there is no clinically meaningful difference in benefit associated with these 2 treatments, the next logical question is whether combining the 2 therapies provides any added benefit; limited observational data seem to suggest that it does. In a retrospective cohort of 86 consecutive singleton pregnancies among women who underwent ultrasound-indicated cerclage, those who used vaginal progesterone after cerclage (n = 45) had a lower rate of PTD.22 Also, a small (66 cases) case-control study demonstrated the benefit of administration of vaginal progesterone as a rescue intervention in women with cerclage and progressive cervical shortening despite cerclage.23
Case 2 Woman experiences adverse effects from vaginal progesterone
MS is a 25-year-old G2P0101 who was started on vaginal progesterone as prophylaxis for recurrent PTD. She is now at 20 weeks’ gestation, with a stable remnant cervical length of 2.0 cm. She is reporting an increasing vaginal burning sensation and vaginal discharge caused by the nightly vaginal progesterone applications, to the point that she is unwilling to continue the treatment. She asks if any alternatives to vaginal progesterone are available to decrease her risk of PTD.
Continue to: Is oral progesterone an option?...
Is oral progesterone an option?
In the 1980s and 1990s, oral micronized progesterone was widely used in France at doses of 900 to 1,200 mg/d for women at risk for PTD. The practice was stopped when secondary hepatic effects, including cholestasis of pregnancy, were reported at a higher rate in treated women.24 A rise in the serum concentration of progesterone metabolites has been associated with impaired biliary excretion and subsequent accumulation of bile acids.25 In other reports, elevated serum transaminase activity was found in pregnant women treated with oral micronized progesterone, and withdrawal of treatment frequently has led to improvement in transaminase levels.26 The synthesis of endogenous progesterone during normal pregnancy is between 250 and 500 mg/d,26 and experts have expressed concern that exogenous progesterone supplementation may impose an additional load on the hepatic transport of sulfated metabolites. Unlike orally administered progesterone, progestins given by the vaginal route avoid the hepatic first-pass effect. For this reason, they may be associated with less hepatic dysfunction.
Although not recommended by professional guidelines, oral progesterone administration for the prevention of PTD has been used in the United States. A 2015 survey of Wisconsin prenatal care providers found that of those who prescribed any progesterone for PTD prevention, oral progesterone was prescribed by 13.1% of obstetricians, 24.4% of midwives, and 40.7% of family medicine practitioners.27
Some limited recent evidence from a meta-analysis of 3 trials investigating oral progesterone versus placebo suggests effectiveness in the prevention of recurrent PTD and reduction in perinatal morbidity and mortality.15 However, the number of cases included in the meta-analysis (386) was too small to support definitive clinical recommendations. Furthermore, questions have been raised in the literature about the reliability of the largest trial included in that meta-analysis.28
Case 3 Two previous spontaneous PTDs
A 29-year-old G3P0201 presents for her first prenatal appointment at 10 weeks’ gestation. With her first pregnancy she had a spontaneous PTD at 23 weeks, and the neonate did not survive. In her second pregnancy, she was treated with 17-OHPC from 16 weeks’ gestation. She had a spontaneous PTD at 29 weeks, and that child is developing normally by her report. She believes that 17-OHPC helped her in her last pregnancy and is anxious about the risk for still another PTD. Consistent with the concept of shared decision-making, you inform her of the results of the recent PROLONG trial and statements on the subject released by professional organizations such as ACOG and the Society for Maternal-Fetal Medicine (SMFM). What options does she have?
17-OHPC may be a possibility in very high-risk women
According to a SMFM statement released in the wake of the PROLONG trial publication, “. . . SMFM believes that it is reasonable for providers to use 17-OHPC in women with a profile more representative of the very high-risk population reported in the Meis trial”.29 Only a few women will have a recurrence risk of PTD over 50%, as was the background event rate in the Meis trial.30 Such a risk level may be suspected, as an example, in women with 2 or more prior early (before 34 weeks) PTDs without intervening term deliveries. Even in those cases, if treatment with 17-OHPC is decided upon, ultrasound cervical surveillance should be added as an additional safety measure. ●
Researchers have been studying the use of exogenous progestins for prevention of preterm delivery (PTD) for almost 60 years, but conflicting results contribute to an ongoing debate. Interpretation of the available data is particularly difficult because different forms and doses of progestins have been used in disparate study populations.
Based on available data, progesterone supplementation is not effective as a primary prevention strategy for PTD in the general low-risk obstetric population. PTD is a complex problem with varied and incompletely elucidated pathogenic pathways, making it unlikely that one interventional approach would be effective for all pregnant women. As a result, emerging indications for the use of progesterone are based on risk factors for PTD (ie, prior PTD and/or short cervix). However, this secondary prevention approach is a limiting factor in itself because 50% of women destined to have a PTD have no identifiable risk factors.1 In addition, researchers have found that progestins are ineffective at delaying delivery for women with multiple gestation, suggesting that a distinct underlying mechanism of early parturition is present in these women, and that this mechanism is unresponsive to progestins.2
The formulations used in the study of progestin supplementation for PTD prevention have been almost exclusively either the synthetic 17 alpha-hydroxyprogesterone caproate (17-OHPC) or natural progesterone administered orally or vaginally. In 2003, the American College of Obstetricians and Gynecologists (ACOG) supported the use of progesterone to reduce the rate of PTD,3 and in 2011, the US Food and Drug Administration (FDA) approved 17-OHPC for use as prophylaxis against recurrent PTD. As a result, in recent years, the perceived standard of care for a majority of practitioners in the United States had been that all women with a previous preterm birth should be offered 17-OHPC. It may be interesting to note that in other parts of the world, the same enthusiastic adoption did not occur. For example, in Australia and New Zealand in 2007, only 5% of practitioners were using progesterone for this indication.4 Further, 17-OHPC is not recommended by professional guidelines in the United Kingdom and has remained unavailable in Germany.
The publication in 2019 of the PROLONG trial called into question the use of 17-OHPC for the prevention of PTD.5 In the December 2019 issue of OBG Management (“Managing preterm birth in those at risk: Expert strategies”), I expressed the opinion that with only rare exceptions, 17-OHPC is no longer a viable option for recurrent PTD prevention.6 In light of these developments, what scientific evidence is relevant and applicable to the care of women at risk for PTD?
Continue to: Case 1 Previous spontaneous PTD at 31 weeks...
Case 1 Previous spontaneous PTD at 31 weeks
MC is an asymptomatic 32-year-old woman with a singleton pregnancy at 13 weeks’ gestation. You see her for a maternal-fetal medicine consultation because 2 years ago she had a spontaneous PTD at 31 weeks’ gestation. What management recommendations can you make to decrease her risk of recurrent PTD?
Cervical length measurement narrows in on risk
The indication “previous preterm birth” is largely meaningless because of the heterogeneity in preterm birth pathways (preterm birth as a syndrome7) and inadequate risk characterization. Among women who experience a spontaneous PTD, 70% to 80% do not deliver prematurely in subsequent pregnancies.8 To better characterize the risk of PTD recurrence, ultrasound assessment of cervical length should be used. Research has shown that among women with a prior spontaneous PTD who maintain a normal cervical length until 24 weeks’ gestation, more than 90% will deliver at 35 weeks or after without intervention.9 Such an approach not only identifies the subgroup of women at significantly increased risk of recurrence but also eliminates unnecessary interventions.
Cervical ultrasound surveillance should be initiated at 16 weeks’ gestation. A short cervix before 16 weeks is not associated with a statistically significant increase in risk for PTD.10 Shortening of the cervix begins approximately 10 weeks before delivery in any gestational age group.11 Therefore, ultrasound assessment of the cervix at 28 weeks and after is irrelevant. In addition, after 28 weeks, cervical length varies greatly leading to loss in the predictive power of the cervical measurement.12 Based on these considerations, cervical surveillance may be extended up to 26 weeks. Although cervical cerclage is not an option in the United States in cases in which a short cervix is detected between 24 and 26 weeks, vaginal progesterone supplementation may still be considered.
Case 1 Continued
MC was started on ultrasound cervical surveillance at 16 weeks’ gestation. Her cervical length was initially normal (> 2.5 cm), but at 18 weeks the measurement was 2.2 cm. What is your recommendation?
The value of vaginal progesterone
There appears to be increasing consensus on the value of vaginal progesterone for women with a midtrimester short cervix on sonography, with or without a history of PTD. An individual patient data meta-analysis demonstrated the benefits of vaginal progesterone.13 Although there was no evidence of an effect on PTD at less than 37 weeks, the rates of PTD at less than 36 weeks and spontaneous PTD at less than 34 weeks were significantly reduced (by 20% and 28%, respectively). Also, there was a significant reduction in the risk of respiratory distress syndrome (53%) and composite neonatal morbidity and mortality (41%), with no significant impact on infant development up to the second year of life.13
The lack of generalizable evidence of benefit on childhood outcomes, combined with considerable uncertainty about the exact role and mechanism of action of exogenous progestins, contribute to the ongoing debate. Vaginal progesterone dosage regimens have been based on extrapolations from experience with progesterone in nonpregnant women, and recent pharmacokinetic studies have revealed how precarious such extrapolations may be. As an example, in nonpregnant women, the bioavailability of oral and vaginal progesterone is similar.14 In pregnancy, however, while daily oral progesterone doubles a pregnant woman’s serum progesterone level,15 daily vaginal administration of progesterone results in only a modest rise in serum progesterone, with a coefficient of variation among individuals that is double that outside of pregnancy.16 It is, therefore, considered that vaginal progesterone in pregnancy may have a local action secondary to the uterine first-pass effect. The uterine first-pass effect for vaginal progesterone was described in nonpregnant women and is only assumed to occur in pregnancy as well. 17
After evaluating the data from the largest available study of vaginal progesterone,18 the FDA concluded in 2012 that the study did not meet the statistical significance generally expected to support the approval of a new product. However, according to a more comprehensive evidence review developed in 2019 by the National Guideline Alliance in the United Kingdom, women with a history of PTD and women with a short cervix derive an important benefit from the use of vaginal progesterone; thus, this intervention should be offered to them.19 At this time, a short cervix and PTD prevention are not considered FDA-approved indications for progesterone supplementation in pregnancy. However, vaginal progesterone is FDA approved for use in pregnant women with a history of infertility.
Continue to: Case 1 Continued...
Case 1 Continued
MC initiated treatment with daily vaginal progesterone at 18 weeks’ gestation and returned for ultrasound cervical length examination weekly instead of every other week. At 20 weeks’ gestation, cervical length was 2.0 cm; the following week it was 1.4 cm. What would you recommend at this point?
When to consider cerclage
If cervical shortening progresses to about 1.5 cm while a woman is being treated with vaginal progesterone, cerclage may be considered. The benefit of cerclage in patients with prior PTD and a short cervix was highlighted in a 2018 Cochrane Review.20 In this stepwise management approach to a short cervix, waiting for a cervix to be less than 1.5 cm may be unadvisable. Under conditions of a very short cervix that is frequently dilated with exposure of fetal membranes, ascending subclinical intra-amniotic infection may already be present, reducing the efficacy of any preventive measures. Preferential consideration for cerclage from the start over initial vaginal progesterone also may be appropriate when there is a history of 2 spontaneous PTDs or mid-trimester losses, a history of a successful cerclage, or with a very short cervix (< 1.0 cm) at the initial evaluation. As for the latter, a 2018 individual patient data meta-analysis of vaginal progesterone found no benefit when the cervix was less than 1.0 cm.13
Progesterone plus cerclage likely to add benefit
The results of an adjusted indirect comparison meta-analysis suggest that both interventions—vaginal progesterone and cerclage—are equally effective.21 Assuming that there is no clinically meaningful difference in benefit associated with these 2 treatments, the next logical question is whether combining the 2 therapies provides any added benefit; limited observational data seem to suggest that it does. In a retrospective cohort of 86 consecutive singleton pregnancies among women who underwent ultrasound-indicated cerclage, those who used vaginal progesterone after cerclage (n = 45) had a lower rate of PTD.22 Also, a small (66 cases) case-control study demonstrated the benefit of administration of vaginal progesterone as a rescue intervention in women with cerclage and progressive cervical shortening despite cerclage.23
Case 2 Woman experiences adverse effects from vaginal progesterone
MS is a 25-year-old G2P0101 who was started on vaginal progesterone as prophylaxis for recurrent PTD. She is now at 20 weeks’ gestation, with a stable remnant cervical length of 2.0 cm. She is reporting an increasing vaginal burning sensation and vaginal discharge caused by the nightly vaginal progesterone applications, to the point that she is unwilling to continue the treatment. She asks if any alternatives to vaginal progesterone are available to decrease her risk of PTD.
Continue to: Is oral progesterone an option?...
Is oral progesterone an option?
In the 1980s and 1990s, oral micronized progesterone was widely used in France at doses of 900 to 1,200 mg/d for women at risk for PTD. The practice was stopped when secondary hepatic effects, including cholestasis of pregnancy, were reported at a higher rate in treated women.24 A rise in the serum concentration of progesterone metabolites has been associated with impaired biliary excretion and subsequent accumulation of bile acids.25 In other reports, elevated serum transaminase activity was found in pregnant women treated with oral micronized progesterone, and withdrawal of treatment frequently has led to improvement in transaminase levels.26 The synthesis of endogenous progesterone during normal pregnancy is between 250 and 500 mg/d,26 and experts have expressed concern that exogenous progesterone supplementation may impose an additional load on the hepatic transport of sulfated metabolites. Unlike orally administered progesterone, progestins given by the vaginal route avoid the hepatic first-pass effect. For this reason, they may be associated with less hepatic dysfunction.
Although not recommended by professional guidelines, oral progesterone administration for the prevention of PTD has been used in the United States. A 2015 survey of Wisconsin prenatal care providers found that of those who prescribed any progesterone for PTD prevention, oral progesterone was prescribed by 13.1% of obstetricians, 24.4% of midwives, and 40.7% of family medicine practitioners.27
Some limited recent evidence from a meta-analysis of 3 trials investigating oral progesterone versus placebo suggests effectiveness in the prevention of recurrent PTD and reduction in perinatal morbidity and mortality.15 However, the number of cases included in the meta-analysis (386) was too small to support definitive clinical recommendations. Furthermore, questions have been raised in the literature about the reliability of the largest trial included in that meta-analysis.28
Case 3 Two previous spontaneous PTDs
A 29-year-old G3P0201 presents for her first prenatal appointment at 10 weeks’ gestation. With her first pregnancy she had a spontaneous PTD at 23 weeks, and the neonate did not survive. In her second pregnancy, she was treated with 17-OHPC from 16 weeks’ gestation. She had a spontaneous PTD at 29 weeks, and that child is developing normally by her report. She believes that 17-OHPC helped her in her last pregnancy and is anxious about the risk for still another PTD. Consistent with the concept of shared decision-making, you inform her of the results of the recent PROLONG trial and statements on the subject released by professional organizations such as ACOG and the Society for Maternal-Fetal Medicine (SMFM). What options does she have?
17-OHPC may be a possibility in very high-risk women
According to a SMFM statement released in the wake of the PROLONG trial publication, “. . . SMFM believes that it is reasonable for providers to use 17-OHPC in women with a profile more representative of the very high-risk population reported in the Meis trial”.29 Only a few women will have a recurrence risk of PTD over 50%, as was the background event rate in the Meis trial.30 Such a risk level may be suspected, as an example, in women with 2 or more prior early (before 34 weeks) PTDs without intervening term deliveries. Even in those cases, if treatment with 17-OHPC is decided upon, ultrasound cervical surveillance should be added as an additional safety measure. ●
- Iams JD, Goldenberg RL, Mercer BM, et al. The preterm prediction study: can low-risk women destined for spontaneous preterm birth be identified? Am J Obstet Gynecol. 2001;184:652-655.
- Murray SR, Stock SJ, Cowan S, et al. Spontaneous preterm birth prevention in multiple pregnancy. Obstet Gynecol. 2018;20:57-63.
- American College of Obstetricians and Gynecologists. ACOG committee opinion. Use of progesterone to reduce preterm birth. Obstet Gynecol. 2003;102:1115-1116.
- Dodd JM, Ashwood P, Flenady V, et al. A survey of clinician and patient attitudes towards the use of progesterone for women at risk of preterm birth. Aust N Z J Obstet Gynaecol. 2007;47:106-109.
- Blackwell SC, Gyamfi -Bannerman C, Biggio JR, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2020;37:127-136.
- Duff P, Vidaeff AC, Ross MG, Norwitz ER. Managing preterm birth in those at risk: expert strategies. OBG Manag. 2019;31:39-42.
- Romero R, Mazor M, Munoz H, et al. The preterm labor syndrome. Ann N Y Acad Sci. 1994;734:414-429.
- Phillips C, Velji Z, Hanly C, et al. Risk of recurrent spontaneous preterm birth: a systematic review and meta-analysis. BMJ Open. 2017;7:e015402.
- Berghella V, Seibel-Seamon J. Contemporary use of cervical cerclage. Clin Obstet Gynecol. 2007;50:468-477.
- Naim A, Haberman S, Burgess T, et al. Changes in cervical length and the risk of preterm labor. Am J Obstet Gynecol. 2002;186:887-889.
- Zilianti M, Azuaga A, Calderon F, et al. Monitoring the effacement of the uterine cervix by transperineal sonography: a new perspective. J Ultrasound Med. 1995;14:719-724.
- Goldenberg RL, Iams JD, Miodovnik M, et al. The preterm prediction study: risk factors in twin gestation. Am J Obstet Gynecol. 1996;175:1047-1053.
- Romero R, Conde-Agudelo A, Da Fonseca E, et al. Vaginal progesterone for preventing preterm birth and adverse perinatal outcomes in singleton gestations with a short cervix: a meta-analysis of individual patient data. Am J Obstet Gynecol. 2018;218:161-180.
- Norman T, Morse C, Dennerstein L. Comparative bioavailability of orally and vaginally administered progesterone. Fertil Steril. 1991;56:1034-1039.
- Boelig RC, Della Corte L, Ashoush S, et al. Oral progesterone for the prevention of recurrent preterm birth: systematic review and metaanalysis. Am J Obstet Gynecol MFM. 2019;1:50-62.
- Boelig RC, Zuppa AF, Kraft WK, et al. Pharmacokinetics of vaginal progesterone in pregnancy. Am J Obstet Gynecol. 2019;221:263.e1-7.
- Bulletti C, de Ziegler D, Flamigni C, et al. Targeted drug delivery in gynaecology: the first uterine pass effect. Hum Reprod. 1997;12:1073-1079.
- Hassan SS, Romero R, Vidyadhari D, et al. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebocontrolled trial. Ultrasound Obstet Gynecol. 2011;38:18-31.
- Preterm labour and birth. Evidence review for clinical effectiveness of prophylactic progesterone in preventing preterm labour. London: National Institute for Health and Care Excellence (UK); August 2019.
- Alfirevic Z, Stampalija T, Medley N. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2017;6:CD008991.
- Conde-Agudelo A, Romero R, Da Fonseca E, et al. Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: updated indirect comparison meta-analysis. Am J Obstet Gynecol. 2018;219:10-25.
- Park JY, Jung YM, Kook S-Y, et al. The effect of postoperative vaginal progesterone in ultrasound-indicated cerclage to prevent preterm birth. J Matern Fetal Neonatal Med. 2019:1-8.
- Roman AR, Da Silva Costa F, et al. Rescue adjuvant vaginal progesterone may improve outcomes in cervical cerclage failure. Geburt Frauen. 2018;78:785-790.
- Benifle JL, Dumont M, Levardon M, et al. Effects of natural micronized progesterone on the liver in the third trimester of pregnancy. Contracept Fertil Sex. 1997;25:165-169.
- Vallejo M, Briz O, Serrano MA, et al. Potential role of transinhibition of the bile salt export pump by progesterone metabolites in the etiopathogenesis of intrahepatic cholestasis of pregnancy. J Hepatol. 2006;44:1150-1157.
- Bacq Y, Sapey T, Bréchot MC, et al. Intrahepatic cholestasis of pregnancy: a French prospective study. Hepatology. 1997;26:358-364.
- Hoppe K, Kramer RD, Ha B, et al. Progesterone supplementation for the prevention of preterm birth: provider practice in Wisconsin. WMJ. 2019;118:126-131.
- Katsanevakis E, Mol BW, Thornton J. A question about the reliability of a recent trial of progesterone for preterm birth prevention, published in Acta. Acta Obstet Gynecol Scand. 2020;99:426.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. SMFM Statement: use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://www.smfm.org/publications/280smfm-statement-use-of-17-alpha-hydroxyprogesteronecaproate-for-prevention-of-recurrent-preterm-birth. Accessed March 23, 2020.
- Meis PJ, Klebanoff M, Thom E, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;384:2379-2385.
- Iams JD, Goldenberg RL, Mercer BM, et al. The preterm prediction study: can low-risk women destined for spontaneous preterm birth be identified? Am J Obstet Gynecol. 2001;184:652-655.
- Murray SR, Stock SJ, Cowan S, et al. Spontaneous preterm birth prevention in multiple pregnancy. Obstet Gynecol. 2018;20:57-63.
- American College of Obstetricians and Gynecologists. ACOG committee opinion. Use of progesterone to reduce preterm birth. Obstet Gynecol. 2003;102:1115-1116.
- Dodd JM, Ashwood P, Flenady V, et al. A survey of clinician and patient attitudes towards the use of progesterone for women at risk of preterm birth. Aust N Z J Obstet Gynaecol. 2007;47:106-109.
- Blackwell SC, Gyamfi -Bannerman C, Biggio JR, et al. 17-OHPC to prevent recurrent preterm birth in singleton gestations (PROLONG study): a multicenter, international, randomized double-blind trial. Am J Perinatol. 2020;37:127-136.
- Duff P, Vidaeff AC, Ross MG, Norwitz ER. Managing preterm birth in those at risk: expert strategies. OBG Manag. 2019;31:39-42.
- Romero R, Mazor M, Munoz H, et al. The preterm labor syndrome. Ann N Y Acad Sci. 1994;734:414-429.
- Phillips C, Velji Z, Hanly C, et al. Risk of recurrent spontaneous preterm birth: a systematic review and meta-analysis. BMJ Open. 2017;7:e015402.
- Berghella V, Seibel-Seamon J. Contemporary use of cervical cerclage. Clin Obstet Gynecol. 2007;50:468-477.
- Naim A, Haberman S, Burgess T, et al. Changes in cervical length and the risk of preterm labor. Am J Obstet Gynecol. 2002;186:887-889.
- Zilianti M, Azuaga A, Calderon F, et al. Monitoring the effacement of the uterine cervix by transperineal sonography: a new perspective. J Ultrasound Med. 1995;14:719-724.
- Goldenberg RL, Iams JD, Miodovnik M, et al. The preterm prediction study: risk factors in twin gestation. Am J Obstet Gynecol. 1996;175:1047-1053.
- Romero R, Conde-Agudelo A, Da Fonseca E, et al. Vaginal progesterone for preventing preterm birth and adverse perinatal outcomes in singleton gestations with a short cervix: a meta-analysis of individual patient data. Am J Obstet Gynecol. 2018;218:161-180.
- Norman T, Morse C, Dennerstein L. Comparative bioavailability of orally and vaginally administered progesterone. Fertil Steril. 1991;56:1034-1039.
- Boelig RC, Della Corte L, Ashoush S, et al. Oral progesterone for the prevention of recurrent preterm birth: systematic review and metaanalysis. Am J Obstet Gynecol MFM. 2019;1:50-62.
- Boelig RC, Zuppa AF, Kraft WK, et al. Pharmacokinetics of vaginal progesterone in pregnancy. Am J Obstet Gynecol. 2019;221:263.e1-7.
- Bulletti C, de Ziegler D, Flamigni C, et al. Targeted drug delivery in gynaecology: the first uterine pass effect. Hum Reprod. 1997;12:1073-1079.
- Hassan SS, Romero R, Vidyadhari D, et al. Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebocontrolled trial. Ultrasound Obstet Gynecol. 2011;38:18-31.
- Preterm labour and birth. Evidence review for clinical effectiveness of prophylactic progesterone in preventing preterm labour. London: National Institute for Health and Care Excellence (UK); August 2019.
- Alfirevic Z, Stampalija T, Medley N. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2017;6:CD008991.
- Conde-Agudelo A, Romero R, Da Fonseca E, et al. Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: updated indirect comparison meta-analysis. Am J Obstet Gynecol. 2018;219:10-25.
- Park JY, Jung YM, Kook S-Y, et al. The effect of postoperative vaginal progesterone in ultrasound-indicated cerclage to prevent preterm birth. J Matern Fetal Neonatal Med. 2019:1-8.
- Roman AR, Da Silva Costa F, et al. Rescue adjuvant vaginal progesterone may improve outcomes in cervical cerclage failure. Geburt Frauen. 2018;78:785-790.
- Benifle JL, Dumont M, Levardon M, et al. Effects of natural micronized progesterone on the liver in the third trimester of pregnancy. Contracept Fertil Sex. 1997;25:165-169.
- Vallejo M, Briz O, Serrano MA, et al. Potential role of transinhibition of the bile salt export pump by progesterone metabolites in the etiopathogenesis of intrahepatic cholestasis of pregnancy. J Hepatol. 2006;44:1150-1157.
- Bacq Y, Sapey T, Bréchot MC, et al. Intrahepatic cholestasis of pregnancy: a French prospective study. Hepatology. 1997;26:358-364.
- Hoppe K, Kramer RD, Ha B, et al. Progesterone supplementation for the prevention of preterm birth: provider practice in Wisconsin. WMJ. 2019;118:126-131.
- Katsanevakis E, Mol BW, Thornton J. A question about the reliability of a recent trial of progesterone for preterm birth prevention, published in Acta. Acta Obstet Gynecol Scand. 2020;99:426.
- Society for Maternal-Fetal Medicine (SMFM) Publications Committee. SMFM Statement: use of 17-alpha hydroxyprogesterone caproate for prevention of recurrent preterm birth. https://www.smfm.org/publications/280smfm-statement-use-of-17-alpha-hydroxyprogesteronecaproate-for-prevention-of-recurrent-preterm-birth. Accessed March 23, 2020.
- Meis PJ, Klebanoff M, Thom E, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;384:2379-2385.
Intra-amniotic sludge: Does its presence rule out cerclage for short cervix?
CASE: Woman with short cervix, intra-amniotic sludge, and prior preterm delivery
An asymptomatic 32-year-old woman with a prior preterm delivery, presently pregnant with a singleton at 17 weeks of gestation, underwent transvaginal ultrasonography and was found to have a cervical length of 22 mm and dense intra-amniotic sludge. She received one dose of 17α-hydroxyprogesterone caproate (17P) at 16 weeks of gestation. What are your next steps in management?
Intra-amniotic sludge is a conundrum
Intra-amniotic sludge is a sonographic finding of free-floating, hyperechoic, particulate matter in the amniotic fluid close to the internal os. The precise nature of this material varies, and it may include blood, meconium, or vernix and may signal inflammation or infection. In a retrospective case-control study, 27% of asymptomatic women with sludge and a short cervix had positive amniotic fluid cultures, and 27% had evidence of inflammation in the amniotic fluid (>50 white blood cells/mm3).1 In a separate report, the authors proposed that "the detection of amniotic fluid 'sludge' represents a sign that microbial invasion of the amniotic cavity and an inflammatory process are in progress."2
Benefit of cerclage in high-risk women. Several systematic reviews have highlighted the benefit of cerclage for women with a singleton pregnancy, short cervix, and previous preterm birth or second-trimester loss (ultrasound-indicated cerclage for high-risk women).3 Cerclage is presumed to work by providing some degree of structural support and by maintaining a barrier to protect the fetal membranes against exposure to ascending pathogens.4
Since dense intra-amniotic sludge may represent chronic intra-amniotic infection, can cerclage still be expected to be beneficial when microbiologic invasion of the amniotic cavity already has occurred? Furthermore, intra-amniotic infection has been cited as a possible complication of ultrasound-indicated cerclage, with a rate of 10%.5 The traditional view is that the presence of subclinical intra-amniotic infection may further increase this risk and therefore should be considered a contraindication to cerclage.6
Evaluating the patient for cerclage placement
The patient history and physical examination should focus on the signs and symptoms of labor, vaginal bleeding, amniotic membrane rupture, and intra-amniotic infection. Particular attention should be paid to maternal temperature, pulse, and the presence of uterine tenderness or foul-smelling vaginal discharge. A sterile speculum examination followed by digital examination would complement the ultrasonography evaluation in assessing cervical dilation and effacement. The ultrasonography evaluation should be completed to confirm a viable pregnancy with accurate dating and the absence of detectable fetal anomalies.
Currently, evidence is insufficient for recommending routine amniocentesis to exclude intra-amniotic infection in an asymptomatic woman prior to ultrasound-indicated cerclage, even in the presence of intra-amniotic sludge, as there are no data demonstrating improved outcomes.4 In addition, intra-amniotic sludge has been associated with intra-amniotic infection and/or inflammation in the form of microbial biofilms, which may prevent detection of infection by routine culture techniques.7
Related Article:
Universal cervical length screening–saving babies lives
Study results offer limited guidance
Data are limited on the clinical implications of intra-amniotic sludge in women with cervical cerclage. In a retrospective cohort of 177 patients with cerclage, 60 had evidence of sludge and 46 of those with sludge underwent ultrasound-indicated cerclage.8 There were no significant differences in the mean gestational age at delivery, neonatal outcomes, rate of preterm delivery, preterm premature rupture of membranes, or intra-amniotic infection between women with or without intra-amniotic sludge. A subanalysis was performed comparing women with sludge detected before or after cerclage and, again, no difference was found in measured outcomes.
Similarly, in a small (N = 20) retrospective review of the Arabin pessary used as a noninvasive intervention for short cervix, the presence of intra-amniotic sludge in 5 cases did not appear to impact outcomes.9
Case patient: How would you manage her care?
Based on her obstetric history and ultrasonography findings, the patient described in the case vignette is at high risk for preterm delivery. The presence of both intra-amniotic sludge and short cervix is associated with an increased risk for spontaneous preterm delivery. After evaluating for clinical intra-amniotic infection and performing a work-up for other contraindications to cerclage placement, cerclage placement may be offered--even in the presence of intra-amniotic sludge.
The next practical question is whether 17P, already started, should be continued after cerclage placement. From the literature on 17P, it is unclear whether progesterone provides additional benefit. One randomized, placebo-controlled study in women with at least 2 preterm deliveries or mid-trimester losses and cerclage in place showed that the 17P-treated women had a significant reduction in preterm delivery compared with the control group, from 37.8% to 16.1%.10
By contrast, in a secondary analysis of a randomized trial evaluating cerclage in high-risk women with short cervix in the current pregnancy, addition of 17P to cerclage was not beneficial.11 Results of 2 retrospective cohort studies showed the same lack of difference on preterm delivery rates with the addition of 17P.12,13
Accepting that the interpretation of these data is challenging, in our practice we would choose to continue the progesterone supplementation, siding with other recently expressed expert opinions.14
The bottom line
While clinical intra-amniotic infection is a contraindication to cerclage, there is no evidence to support withholding cerclage from eligible women due to the presence of intra-amniotic fluid sludge alone.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid "sludge" in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
- Romero R, Kusanovic JP, Espinoza J, et al. What is amniotic fluid "sludge"? Ultrasound Obstet Gynecol. 2007;30(5):793-798.
- Alfirevic Z, Stampalija T, Roberts D, Jorgensen AL. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012;4:CD008991.
- Abbott D, To M, Shennan A. Cervical cerclage: a review of current evidence. Aust N Z J Obstet Gynaecol. 2012;52(3):220-223.
- Drassinower D, Poggi SH, Landy HJ, Gilo N, Benson JE, Ghidini A. Perioperative complications of history-indicated and ultrasound-indicated cervical cerclage. Am J Obstet Gynecol. 2011;205(1):53.e1-e5.
- Mays JK, Figueroa R, Shah J, Khakoo H, Kaminsky S, Tejani N. Amniocentesis for selection before rescue cerclage. Obstet Gynecol. 2000;95(5):652-655.
- Vaisbuch E, Romero R, Erez IO, et al. Clinical significance of early (<20 weeks) vs late (20-24 weeks) detection of sonographic short cervix in asymptomatic women in the mid-trimester. Ultrasound Obstet Gynecol. 2010;36(4):471-481.
- Gorski LA, Huang WH, Iriye BK, Hancock J. Clinical implication of intra-amniotic sludge on ultrasound in patients with cervical cerclage. Ultrasound Obstet Gynecol. 2010;36(4):482-485.
- Ting YH, Lao TT, Wa Law LW, et al. Arabin cerclage pessary in the management of cervical insufficiency. J Matern Fetal Neonatal Med. 2012;25(12):2693-2695.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574-577.
- Berghella V, Figueroa D, Szychowski JM, et al; Vaginal Ultrasound Trial Consortium. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1-e6.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271-275.
- Stetson B, Hibbard JU, Wilkins I, Leftwich H. Outcomes with cerclage alone compared with cerclage plus 17 α-hydroxyprogesterone caproate. Obstet Gynecol. 2016;128(5):983-988.
- Iams JD. Identification of candidates for progesterone: why, who, how, and when? Obstet Gynecol. 2014;123(6):1317-1326.
CASE: Woman with short cervix, intra-amniotic sludge, and prior preterm delivery
An asymptomatic 32-year-old woman with a prior preterm delivery, presently pregnant with a singleton at 17 weeks of gestation, underwent transvaginal ultrasonography and was found to have a cervical length of 22 mm and dense intra-amniotic sludge. She received one dose of 17α-hydroxyprogesterone caproate (17P) at 16 weeks of gestation. What are your next steps in management?
Intra-amniotic sludge is a conundrum
Intra-amniotic sludge is a sonographic finding of free-floating, hyperechoic, particulate matter in the amniotic fluid close to the internal os. The precise nature of this material varies, and it may include blood, meconium, or vernix and may signal inflammation or infection. In a retrospective case-control study, 27% of asymptomatic women with sludge and a short cervix had positive amniotic fluid cultures, and 27% had evidence of inflammation in the amniotic fluid (>50 white blood cells/mm3).1 In a separate report, the authors proposed that "the detection of amniotic fluid 'sludge' represents a sign that microbial invasion of the amniotic cavity and an inflammatory process are in progress."2
Benefit of cerclage in high-risk women. Several systematic reviews have highlighted the benefit of cerclage for women with a singleton pregnancy, short cervix, and previous preterm birth or second-trimester loss (ultrasound-indicated cerclage for high-risk women).3 Cerclage is presumed to work by providing some degree of structural support and by maintaining a barrier to protect the fetal membranes against exposure to ascending pathogens.4
Since dense intra-amniotic sludge may represent chronic intra-amniotic infection, can cerclage still be expected to be beneficial when microbiologic invasion of the amniotic cavity already has occurred? Furthermore, intra-amniotic infection has been cited as a possible complication of ultrasound-indicated cerclage, with a rate of 10%.5 The traditional view is that the presence of subclinical intra-amniotic infection may further increase this risk and therefore should be considered a contraindication to cerclage.6
Evaluating the patient for cerclage placement
The patient history and physical examination should focus on the signs and symptoms of labor, vaginal bleeding, amniotic membrane rupture, and intra-amniotic infection. Particular attention should be paid to maternal temperature, pulse, and the presence of uterine tenderness or foul-smelling vaginal discharge. A sterile speculum examination followed by digital examination would complement the ultrasonography evaluation in assessing cervical dilation and effacement. The ultrasonography evaluation should be completed to confirm a viable pregnancy with accurate dating and the absence of detectable fetal anomalies.
Currently, evidence is insufficient for recommending routine amniocentesis to exclude intra-amniotic infection in an asymptomatic woman prior to ultrasound-indicated cerclage, even in the presence of intra-amniotic sludge, as there are no data demonstrating improved outcomes.4 In addition, intra-amniotic sludge has been associated with intra-amniotic infection and/or inflammation in the form of microbial biofilms, which may prevent detection of infection by routine culture techniques.7
Related Article:
Universal cervical length screening–saving babies lives
Study results offer limited guidance
Data are limited on the clinical implications of intra-amniotic sludge in women with cervical cerclage. In a retrospective cohort of 177 patients with cerclage, 60 had evidence of sludge and 46 of those with sludge underwent ultrasound-indicated cerclage.8 There were no significant differences in the mean gestational age at delivery, neonatal outcomes, rate of preterm delivery, preterm premature rupture of membranes, or intra-amniotic infection between women with or without intra-amniotic sludge. A subanalysis was performed comparing women with sludge detected before or after cerclage and, again, no difference was found in measured outcomes.
Similarly, in a small (N = 20) retrospective review of the Arabin pessary used as a noninvasive intervention for short cervix, the presence of intra-amniotic sludge in 5 cases did not appear to impact outcomes.9
Case patient: How would you manage her care?
Based on her obstetric history and ultrasonography findings, the patient described in the case vignette is at high risk for preterm delivery. The presence of both intra-amniotic sludge and short cervix is associated with an increased risk for spontaneous preterm delivery. After evaluating for clinical intra-amniotic infection and performing a work-up for other contraindications to cerclage placement, cerclage placement may be offered--even in the presence of intra-amniotic sludge.
The next practical question is whether 17P, already started, should be continued after cerclage placement. From the literature on 17P, it is unclear whether progesterone provides additional benefit. One randomized, placebo-controlled study in women with at least 2 preterm deliveries or mid-trimester losses and cerclage in place showed that the 17P-treated women had a significant reduction in preterm delivery compared with the control group, from 37.8% to 16.1%.10
By contrast, in a secondary analysis of a randomized trial evaluating cerclage in high-risk women with short cervix in the current pregnancy, addition of 17P to cerclage was not beneficial.11 Results of 2 retrospective cohort studies showed the same lack of difference on preterm delivery rates with the addition of 17P.12,13
Accepting that the interpretation of these data is challenging, in our practice we would choose to continue the progesterone supplementation, siding with other recently expressed expert opinions.14
The bottom line
While clinical intra-amniotic infection is a contraindication to cerclage, there is no evidence to support withholding cerclage from eligible women due to the presence of intra-amniotic fluid sludge alone.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
CASE: Woman with short cervix, intra-amniotic sludge, and prior preterm delivery
An asymptomatic 32-year-old woman with a prior preterm delivery, presently pregnant with a singleton at 17 weeks of gestation, underwent transvaginal ultrasonography and was found to have a cervical length of 22 mm and dense intra-amniotic sludge. She received one dose of 17α-hydroxyprogesterone caproate (17P) at 16 weeks of gestation. What are your next steps in management?
Intra-amniotic sludge is a conundrum
Intra-amniotic sludge is a sonographic finding of free-floating, hyperechoic, particulate matter in the amniotic fluid close to the internal os. The precise nature of this material varies, and it may include blood, meconium, or vernix and may signal inflammation or infection. In a retrospective case-control study, 27% of asymptomatic women with sludge and a short cervix had positive amniotic fluid cultures, and 27% had evidence of inflammation in the amniotic fluid (>50 white blood cells/mm3).1 In a separate report, the authors proposed that "the detection of amniotic fluid 'sludge' represents a sign that microbial invasion of the amniotic cavity and an inflammatory process are in progress."2
Benefit of cerclage in high-risk women. Several systematic reviews have highlighted the benefit of cerclage for women with a singleton pregnancy, short cervix, and previous preterm birth or second-trimester loss (ultrasound-indicated cerclage for high-risk women).3 Cerclage is presumed to work by providing some degree of structural support and by maintaining a barrier to protect the fetal membranes against exposure to ascending pathogens.4
Since dense intra-amniotic sludge may represent chronic intra-amniotic infection, can cerclage still be expected to be beneficial when microbiologic invasion of the amniotic cavity already has occurred? Furthermore, intra-amniotic infection has been cited as a possible complication of ultrasound-indicated cerclage, with a rate of 10%.5 The traditional view is that the presence of subclinical intra-amniotic infection may further increase this risk and therefore should be considered a contraindication to cerclage.6
Evaluating the patient for cerclage placement
The patient history and physical examination should focus on the signs and symptoms of labor, vaginal bleeding, amniotic membrane rupture, and intra-amniotic infection. Particular attention should be paid to maternal temperature, pulse, and the presence of uterine tenderness or foul-smelling vaginal discharge. A sterile speculum examination followed by digital examination would complement the ultrasonography evaluation in assessing cervical dilation and effacement. The ultrasonography evaluation should be completed to confirm a viable pregnancy with accurate dating and the absence of detectable fetal anomalies.
Currently, evidence is insufficient for recommending routine amniocentesis to exclude intra-amniotic infection in an asymptomatic woman prior to ultrasound-indicated cerclage, even in the presence of intra-amniotic sludge, as there are no data demonstrating improved outcomes.4 In addition, intra-amniotic sludge has been associated with intra-amniotic infection and/or inflammation in the form of microbial biofilms, which may prevent detection of infection by routine culture techniques.7
Related Article:
Universal cervical length screening–saving babies lives
Study results offer limited guidance
Data are limited on the clinical implications of intra-amniotic sludge in women with cervical cerclage. In a retrospective cohort of 177 patients with cerclage, 60 had evidence of sludge and 46 of those with sludge underwent ultrasound-indicated cerclage.8 There were no significant differences in the mean gestational age at delivery, neonatal outcomes, rate of preterm delivery, preterm premature rupture of membranes, or intra-amniotic infection between women with or without intra-amniotic sludge. A subanalysis was performed comparing women with sludge detected before or after cerclage and, again, no difference was found in measured outcomes.
Similarly, in a small (N = 20) retrospective review of the Arabin pessary used as a noninvasive intervention for short cervix, the presence of intra-amniotic sludge in 5 cases did not appear to impact outcomes.9
Case patient: How would you manage her care?
Based on her obstetric history and ultrasonography findings, the patient described in the case vignette is at high risk for preterm delivery. The presence of both intra-amniotic sludge and short cervix is associated with an increased risk for spontaneous preterm delivery. After evaluating for clinical intra-amniotic infection and performing a work-up for other contraindications to cerclage placement, cerclage placement may be offered--even in the presence of intra-amniotic sludge.
The next practical question is whether 17P, already started, should be continued after cerclage placement. From the literature on 17P, it is unclear whether progesterone provides additional benefit. One randomized, placebo-controlled study in women with at least 2 preterm deliveries or mid-trimester losses and cerclage in place showed that the 17P-treated women had a significant reduction in preterm delivery compared with the control group, from 37.8% to 16.1%.10
By contrast, in a secondary analysis of a randomized trial evaluating cerclage in high-risk women with short cervix in the current pregnancy, addition of 17P to cerclage was not beneficial.11 Results of 2 retrospective cohort studies showed the same lack of difference on preterm delivery rates with the addition of 17P.12,13
Accepting that the interpretation of these data is challenging, in our practice we would choose to continue the progesterone supplementation, siding with other recently expressed expert opinions.14
The bottom line
While clinical intra-amniotic infection is a contraindication to cerclage, there is no evidence to support withholding cerclage from eligible women due to the presence of intra-amniotic fluid sludge alone.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid "sludge" in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
- Romero R, Kusanovic JP, Espinoza J, et al. What is amniotic fluid "sludge"? Ultrasound Obstet Gynecol. 2007;30(5):793-798.
- Alfirevic Z, Stampalija T, Roberts D, Jorgensen AL. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012;4:CD008991.
- Abbott D, To M, Shennan A. Cervical cerclage: a review of current evidence. Aust N Z J Obstet Gynaecol. 2012;52(3):220-223.
- Drassinower D, Poggi SH, Landy HJ, Gilo N, Benson JE, Ghidini A. Perioperative complications of history-indicated and ultrasound-indicated cervical cerclage. Am J Obstet Gynecol. 2011;205(1):53.e1-e5.
- Mays JK, Figueroa R, Shah J, Khakoo H, Kaminsky S, Tejani N. Amniocentesis for selection before rescue cerclage. Obstet Gynecol. 2000;95(5):652-655.
- Vaisbuch E, Romero R, Erez IO, et al. Clinical significance of early (<20 weeks) vs late (20-24 weeks) detection of sonographic short cervix in asymptomatic women in the mid-trimester. Ultrasound Obstet Gynecol. 2010;36(4):471-481.
- Gorski LA, Huang WH, Iriye BK, Hancock J. Clinical implication of intra-amniotic sludge on ultrasound in patients with cervical cerclage. Ultrasound Obstet Gynecol. 2010;36(4):482-485.
- Ting YH, Lao TT, Wa Law LW, et al. Arabin cerclage pessary in the management of cervical insufficiency. J Matern Fetal Neonatal Med. 2012;25(12):2693-2695.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574-577.
- Berghella V, Figueroa D, Szychowski JM, et al; Vaginal Ultrasound Trial Consortium. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1-e6.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271-275.
- Stetson B, Hibbard JU, Wilkins I, Leftwich H. Outcomes with cerclage alone compared with cerclage plus 17 α-hydroxyprogesterone caproate. Obstet Gynecol. 2016;128(5):983-988.
- Iams JD. Identification of candidates for progesterone: why, who, how, and when? Obstet Gynecol. 2014;123(6):1317-1326.
- Kusanovic JP, Espinoza J, Romero R, et al. Clinical significance of the presence of amniotic fluid "sludge" in asymptomatic patients at high risk for spontaneous preterm delivery. Ultrasound Obstet Gynecol. 2007;30(5):706-714.
- Romero R, Kusanovic JP, Espinoza J, et al. What is amniotic fluid "sludge"? Ultrasound Obstet Gynecol. 2007;30(5):793-798.
- Alfirevic Z, Stampalija T, Roberts D, Jorgensen AL. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2012;4:CD008991.
- Abbott D, To M, Shennan A. Cervical cerclage: a review of current evidence. Aust N Z J Obstet Gynaecol. 2012;52(3):220-223.
- Drassinower D, Poggi SH, Landy HJ, Gilo N, Benson JE, Ghidini A. Perioperative complications of history-indicated and ultrasound-indicated cervical cerclage. Am J Obstet Gynecol. 2011;205(1):53.e1-e5.
- Mays JK, Figueroa R, Shah J, Khakoo H, Kaminsky S, Tejani N. Amniocentesis for selection before rescue cerclage. Obstet Gynecol. 2000;95(5):652-655.
- Vaisbuch E, Romero R, Erez IO, et al. Clinical significance of early (<20 weeks) vs late (20-24 weeks) detection of sonographic short cervix in asymptomatic women in the mid-trimester. Ultrasound Obstet Gynecol. 2010;36(4):471-481.
- Gorski LA, Huang WH, Iriye BK, Hancock J. Clinical implication of intra-amniotic sludge on ultrasound in patients with cervical cerclage. Ultrasound Obstet Gynecol. 2010;36(4):482-485.
- Ting YH, Lao TT, Wa Law LW, et al. Arabin cerclage pessary in the management of cervical insufficiency. J Matern Fetal Neonatal Med. 2012;25(12):2693-2695.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574-577.
- Berghella V, Figueroa D, Szychowski JM, et al; Vaginal Ultrasound Trial Consortium. 17-alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1-e6.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271-275.
- Stetson B, Hibbard JU, Wilkins I, Leftwich H. Outcomes with cerclage alone compared with cerclage plus 17 α-hydroxyprogesterone caproate. Obstet Gynecol. 2016;128(5):983-988.
- Iams JD. Identification of candidates for progesterone: why, who, how, and when? Obstet Gynecol. 2014;123(6):1317-1326.
Need for caution before extending the use of antenatal corticosteroids beyond 34 weeks’ gestation
The results of the highly anticipated Antenatal Late Preterm Study recently have become available.1 Data from this randomized controlled trial, conducted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network, demonstrated that administration of betamethasone to women at risk for preterm delivery between 34 weeks 0 days and 36 weeks 6 days of gestation significantly reduces the rate of neonatal respiratory complications. It may represent the largest study of antenatal corticosteroids (ACS) to date, with 2,827 infants studied, and its results inevitably lead to the logical practical question: Should ACS use be extended beyond the 34 weeks’ gestation limit previously recommended by professional guidelines in the United States2?
There are some issues that bear discussion before such a significant change in standard of care should be promoted.2
Antenatal Late Preterm Study outcomesThe primary outcome in the study was a composite end point describing the need for respiratory support within 72 hours after birth. Based on a pilot study, the investigators had anticipated a 33% decrease in the rate of the primary outcome; however, the reduction was only 20% (relative risk [RR], 0.80; 95% confidence interval [CI], 0.66−0.97). Although the effect size was statistically significant, one could question the clinical relevance of such a small difference.
A 33% reduction effect, more consistent with the preliminary expectations, was noted in the prespecified secondary composite outcome of severe respiratory complications (RR, 0.67; 95% CI, 0.53−0.84). Occurrences included in the secondary composite outcome that also showed significant rate reductions were:
- the use of continuous positive airway pressure (CPAP) or high-flow oxygen via nasal cannula for at least 12 hours (RR, 0.62; 95% CI, 0.48−0.80)
- need for resuscitation at birth (RR, 0.78; 95% CI, 0.66−0.92)
- surfactant use (RR, 0.59; 95% CI, 0.37−0.96)
- transient tachypnea of the newborn (RR, 0.68; 95% CI, 0.53−0.87).
The reported reduction in bronchopulmonary dysplasia (RR, 0.22; 95% CI, 0.02−0.92) cannot plausibly be attributed to ACS. Randomized data aggregated by the Cochrane Database of Systematic Reviews3 do not show improvement in chronic lung disease with ACS use. Moreover, the authors recognize that the assessment for bronchopulmonary dysplasia at only 28 days of life is only partially informative and that longer childhood follow-up is required to confirm the finding.
- Although corticosteroids have been shown to reduce the risk of the baby needing breathing support by 20%, they are associated with a 60% increase in risk for low blood sugar in the newborn (hypoglycemia). Hypoglycemia can place the baby at risk for seizures and even brain damage.
- There is an unknown safety profile for corticosteroid administration at this gestational age. The fetal brain is still developing during this period, and there is some information to suggest that corticosteroids could have an unfavorable effect on brain development.
- Corticosteroids are potent hormones and potentially can have undesired hormonal effects at this gestational age.
- If corticosteroids are given and the mother carries the baby to term (37 weeks or later) there are some studies that suggest the baby is at an increased risk for neurologic, cognitive, metabolic, and/or behavioral abnormalities in later life.
We recommend caution before changing current practiceWe propose prudence with ACS use after 34 weeks’ gestation for the following reasons: the increased risk for neonatal hypoglycemia associated with ACS, the increased risk for ACS-related harm in term-born babies, and safety concerns with ACS in the late preterm period.
Evidence shows an increased risk for neonatal hypoglycemiaThe most profound effect modification observed in the study was an adverse effect—namely, a 60% increase in neonatal hypoglycemia with ACS administration (RR, 1.6; 95% CI, 1.37−1.87). The rate of neonatal hypoglycemia was 24% in the ACS group, compared with 15% in the placebo group.
Results of prior studies have demonstrated either no increased risk of hypoglycemia with ACS use4−7 or a much smaller increase (from 4.2% to 5.7%).8 The higher rate of neonatal hypoglycemia seen in this study suggests the possibility that the late preterm population may be more vulnerable to the negative impact of ACS on neonatal glucose/insulin homeostasis. Presumed mechanisms of action are either maternal hyperglycemia or fetal adrenal suppression or both, with potential for fetal adrenal suppression resulting from betamethasone exposure to affect long-term metabolic outcomes.9
Of note, women with pregestational diabetes were excluded from the study and, in routine practice, inclusion of such patients may further increase the risk of neonatal hypoglycemia.
There are few data on the prognostic significance of neonatal hypoglycemia in preterm infants, with the exception of a single study, the results of which show that it is associated with adverse neurodevelopment at 18 months of age.10
Data reveal increased risk for harm in term-born babiesIn spite of strict protocol specifications to increase the probability of delivery before 37 weeks’ gestation, 16% of women in the trial delivered at term. Investigators of prior randomized studies of ACS, aimed at reducing the risks of prematurity, have reported a rate of term delivery of about one-third,4,11 and in routine practice, administration of ACS after 34 weeks may be associated with even higher rates of term delivery.
This is important because recent evidence shows an unfavorable impact of ACS exposure in term-born children.12 The 5-year follow-up of the largest randomized trial in which multiple ACS courses were used noted that babies born at term had a 4-fold increased odds ratio for neurosensory disability.11 There was no dose−response interaction, with the same adverse odds ratio after 1 or 4 additional ACS courses. This observation was consistent with a previously reported Swedish national cohort, pointing to an unfavorable impact of even a single course of ACS in term-born children, with a greater likelihood of harm than benefit.13
In a UK follow-up of children aged 8 to 15 years who were enrolled in an RCT of ACS before cesarean delivery at term, low academic achievement was significantly more common in the group whose mothers had received ACS.14 In another study of 304 children born at term after exposure to a single course of ACS, investigators noted significantly increased cortisol reactivity to acute psychological stress at ages 6 to 11 years in the ACS-exposed patients, compared with 212 babies of women with threatened preterm labor who did not receive ACS and 372 babies from uncomplicated term pregnancies.15
The relevance of such study findings extends beyond childhood given the fact that elevated hypothalamic-pituitary-adrenal (HPA) axis reactivity has been linked to the pathogenesis of metabolic syndrome and depression in adult life.16 As recently as 2015, investigators of a randomized trial of ACS in 6 low- and middle-income countries highlighted their concern regarding “potentially harmful use of antenatal corticosteroids for infants not delivered preterm.”17
There are safety concerns with ACS in the late preterm periodThe effects of ACS are more pleiotropic than those reflected in a lower incidence of respiratory difficulties. Knowledge of the overall consequences of ACS exposure in infants born late-preterm or at term is still limited. The close-to-term fetus exposed to exogenous corticosteroids is also exposed to the physiologic endogenous surge of cortisol known to occur in the maternal circulation in late pregnancy, which reaches levels 3 times higher than those seen in nonpregnant women.18 Although placental 11 beta-hydroxysteroid dehydrogenase type 2 plays a protective role by allowing no more than 10% to 20% of maternal corticosteroids to cross the placenta, fetal overexposure from concomitant exogenous maternal corticosteroid administration remains a theoretical concern close to term. This is especially worrisome if there is a gestational age−related increase in the sensitivity to corticosteroid-induced in utero fetal programming. It has been reported that fetal overexposure to corticosteroids in late pregnancy can permanently increase the activity of the HPA-axis, with likely consequences in adult life.19
Another concern relates to oligodendrocytes development. Although the neuronal division process in humans usually is completed by 24 weeks’ gestation, the most rapid growth for oligodendrocytes occurs between 34 and 36 weeks’ gestation; these are the cells responsible for the synthesis of myelin. Overexposure to corticosteroids at this vulnerable time in the late preterm fetus potentially may have unanticipated negative neurologic consequences.20
This is the only scenario in which we feel antenatal corticosteroids could be used in a fetus aged 34 weeks to 36 weeks 5 days. In the setting of a scheduled cesarean delivery between 34 weeks and 35 weeks, the concerns relative to term delivery after corticosteroid exposure may not apply, but the concerns in relation to the administration of corticosteroid in the late preterm period—which is a time of possibly increased neurohormonal and neurologic vulnerability—still apply. With regard to the risk of neonatal hypoglycemia, one might argue that close neonatal monitoring of babies so exposed may ensure that any associated neonatal hypoglycemia does not go unnoticed or untreated. However, the prognostic significance of even short periods of neonatal hypoglycemia has not been established.
Where should future studies focus?There is clear neonatal benefit from a single course of ACS given to women who will deliver before 34 weeks’ gestation. It is widely accepted, based on the evidence provided by the 30-year follow-up of the cohort of 534 participants from the Auckland trial (the longest follow-up for any pregnancy trial), that administration of ACS at less than 34 weeks’ gestation is not associated with any obvious major developmental risk.21−23
However, the reassurances provided by the Auckland cohort should be neither directly extrapolated to the administration of ACS in the late preterm period nor applied to term-born babies exposed to ACS, for the simple reason that these subgroups never have been analyzed separately. The risk:benefit ratio of ACS use in the late-preterm period is as yet unknown, and in term-born babies the ratio may be unfavorable.
Follow-up studies are neededWe consider that there is a vital need for long-term follow-up studies. The focus of research on the effects of ACS no longer is on the immediate neonatal outcomes and now is on safety and the long-term outcomes of this exposure.
Bottom lineWe regard the large, high-quality study conducted by the NICHD MFMU Network1 as an opportunity to answer current concerns. It is hoped that the resources necessaryfor in-depth follow-up of the children involved in this study will be provided to the investigators and to the NICHD. It is only with such follow-up that mid- and long-term adverse effects can be assessed. We believe that, at a minimum, mid-term follow-up data should be available before it is wise to make any definitive recommendations for a sweeping change in clinical practice.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery [published online ahead of print February 4, 2016]. N Engl J Med.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG Committee Opinion No. 475: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2011;117(2 pt 1):422–424.
- Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;(3):CD004454.
- Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics. 1972;50(4):515–525.
- Sann L, Burnod J, Lasne Y, Bethenod M. Antenatal administration of betamethasone: effects upon neonatal blood glucose in premature infants [in French]. Nouv Presse Med. 1979;8(39):3147–3148.
- Rokicki W, Krasnodebski J. Antenatal glucocorticoid administration and neonatal glycemia. Dev Pharmacol Ther. 1987;10(4):307–311.
- Gazquez Serrano IM, Arroyos Plana A, Diaz Morales O, Herraiz Perea C, Holgueras Bragado A. Antenatal corticosteroid therapy and late preterm infant morbidity and mortality [in Spanish]. An Pediatr (Barc). 2014;81(6):374–382.
- Pettit KE, Tran SH, Lee E, Caughey AB. The association of antenatal corticosteroids with neonatal hypoglycemia and hyperbilirubinemia. J Matern Fetal Neonatal Med. 2014;27(7):683–686.
- Aydin M, Derveci U, Hakan N. Neonatal hypoglycemia associated with the antenatal corticosteroids may be secondary to fetal adrenal suppression. J Matern Fetal Neonatal Med. 2015;28(8):892.
- Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ. 1988;297(6659):1304–1308.
- Asztalos EV, Murphy KE, Willan AR, et al; MACS-5 Collaborative Group. Multiple courses of antenatal corticosteroids for preterm birth study: outcomes in children at 5 years of age (MACS-5). JAMA Pediatr. 2013;167(12):1102–1110.
- Vidaeff AC, Belfort MA, Steer PJ. Antenatal corticosteroids: a time for more careful scrutiny of the indications [published online ahead of print January 18, 2016]. BJOG. doi:10.1111/1471-0528.13853.
- Eriksson L, Haglund B, Ewald U, Odlind V, Kieler H. Health consequences of prophylactic exposure to antenatal corticosteroids among children born late preterm or term. Acta Obstet Gynecol Scand. 2012;91(12):1415–1421.
- Stutchfield PR, Whitaker R, Gliddon AE, Hobson L, Kotecha S, Doull IJ. Behavioural, educational and respiratory outcomes of antenatal betamethasone for term caesarean section (ASTECS trial). Arch Dis Child Fetal Neonatal Ed. 2013;98(3):F195–F200.
- Alexander N, Rosenlocher F, Stalder T, et al. Impact of antenatal synthetic glucocorticoid exposure on endocrine stress reactivity in term-born children. J Clin Endocrinol Metab. 2012;97(10):3538–3544.
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5(7):374–381.
- Althabe F, Belizan JM, McClure EM, et al. A population-based, multifaceted strategy to implement antenatal corticosteroid treatment versus standard care for the reduction of neonatal mortality due to preterm birth in low-income and middle-income countries: the ACT cluster-randomised trial. Lancet. 2015;385(9968):629–639.
- Jung C, Ho JT, Torpy DJ, et al. A longitudinal study of plasma and urinary cortisol in pregnancy and postpartum. J Clin Endocrinol Metab. 2011;96(5):1533–1540.
- Welberg LA, Seckl JR, Holmes MC. Inhibition of 11ß-hydroxysteroid dehydrogenase, the foeto-placental barrier to maternal glucocorticoids, permanently programs amygdale GR mRNA expression and anxiety-like behavior in the offspring. Eur J Neurosci. 2000;12(3):1047–1054.
- Whitelaw A, Thoresen M. Antenatal steroids and the developing brain. Arch Dis Child Fetal Neonatal Ed. 2000;83(2):F154–F157.
- Dalziel SR, Walker NK, Parag V, et al. Cardiovascular risk factors after antenatal exposure to betamethasone: 30-year follow-up of a randomised controlled trial. Lancet. 2005;365(9474):1856–1862.
- Dalziel SR, Lim VK, Lambert A, et al. Antenatal exposure to betamethasone: psychological functioning and health related quality of life 31 years after inclusion in randomised controlled trial. BMJ. 2005;331(7518):665.
- Welberg LA, Seckl JR, Holmes MC. Inhibition of 11Dalziel SR, Walker NK, Parag V, et al. Dalziel SR, Lim VK, Lambert A, et al. Dalziel SR, Rea HH, Walker NK, et al.
The results of the highly anticipated Antenatal Late Preterm Study recently have become available.1 Data from this randomized controlled trial, conducted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network, demonstrated that administration of betamethasone to women at risk for preterm delivery between 34 weeks 0 days and 36 weeks 6 days of gestation significantly reduces the rate of neonatal respiratory complications. It may represent the largest study of antenatal corticosteroids (ACS) to date, with 2,827 infants studied, and its results inevitably lead to the logical practical question: Should ACS use be extended beyond the 34 weeks’ gestation limit previously recommended by professional guidelines in the United States2?
There are some issues that bear discussion before such a significant change in standard of care should be promoted.2
Antenatal Late Preterm Study outcomesThe primary outcome in the study was a composite end point describing the need for respiratory support within 72 hours after birth. Based on a pilot study, the investigators had anticipated a 33% decrease in the rate of the primary outcome; however, the reduction was only 20% (relative risk [RR], 0.80; 95% confidence interval [CI], 0.66−0.97). Although the effect size was statistically significant, one could question the clinical relevance of such a small difference.
A 33% reduction effect, more consistent with the preliminary expectations, was noted in the prespecified secondary composite outcome of severe respiratory complications (RR, 0.67; 95% CI, 0.53−0.84). Occurrences included in the secondary composite outcome that also showed significant rate reductions were:
- the use of continuous positive airway pressure (CPAP) or high-flow oxygen via nasal cannula for at least 12 hours (RR, 0.62; 95% CI, 0.48−0.80)
- need for resuscitation at birth (RR, 0.78; 95% CI, 0.66−0.92)
- surfactant use (RR, 0.59; 95% CI, 0.37−0.96)
- transient tachypnea of the newborn (RR, 0.68; 95% CI, 0.53−0.87).
The reported reduction in bronchopulmonary dysplasia (RR, 0.22; 95% CI, 0.02−0.92) cannot plausibly be attributed to ACS. Randomized data aggregated by the Cochrane Database of Systematic Reviews3 do not show improvement in chronic lung disease with ACS use. Moreover, the authors recognize that the assessment for bronchopulmonary dysplasia at only 28 days of life is only partially informative and that longer childhood follow-up is required to confirm the finding.
- Although corticosteroids have been shown to reduce the risk of the baby needing breathing support by 20%, they are associated with a 60% increase in risk for low blood sugar in the newborn (hypoglycemia). Hypoglycemia can place the baby at risk for seizures and even brain damage.
- There is an unknown safety profile for corticosteroid administration at this gestational age. The fetal brain is still developing during this period, and there is some information to suggest that corticosteroids could have an unfavorable effect on brain development.
- Corticosteroids are potent hormones and potentially can have undesired hormonal effects at this gestational age.
- If corticosteroids are given and the mother carries the baby to term (37 weeks or later) there are some studies that suggest the baby is at an increased risk for neurologic, cognitive, metabolic, and/or behavioral abnormalities in later life.
We recommend caution before changing current practiceWe propose prudence with ACS use after 34 weeks’ gestation for the following reasons: the increased risk for neonatal hypoglycemia associated with ACS, the increased risk for ACS-related harm in term-born babies, and safety concerns with ACS in the late preterm period.
Evidence shows an increased risk for neonatal hypoglycemiaThe most profound effect modification observed in the study was an adverse effect—namely, a 60% increase in neonatal hypoglycemia with ACS administration (RR, 1.6; 95% CI, 1.37−1.87). The rate of neonatal hypoglycemia was 24% in the ACS group, compared with 15% in the placebo group.
Results of prior studies have demonstrated either no increased risk of hypoglycemia with ACS use4−7 or a much smaller increase (from 4.2% to 5.7%).8 The higher rate of neonatal hypoglycemia seen in this study suggests the possibility that the late preterm population may be more vulnerable to the negative impact of ACS on neonatal glucose/insulin homeostasis. Presumed mechanisms of action are either maternal hyperglycemia or fetal adrenal suppression or both, with potential for fetal adrenal suppression resulting from betamethasone exposure to affect long-term metabolic outcomes.9
Of note, women with pregestational diabetes were excluded from the study and, in routine practice, inclusion of such patients may further increase the risk of neonatal hypoglycemia.
There are few data on the prognostic significance of neonatal hypoglycemia in preterm infants, with the exception of a single study, the results of which show that it is associated with adverse neurodevelopment at 18 months of age.10
Data reveal increased risk for harm in term-born babiesIn spite of strict protocol specifications to increase the probability of delivery before 37 weeks’ gestation, 16% of women in the trial delivered at term. Investigators of prior randomized studies of ACS, aimed at reducing the risks of prematurity, have reported a rate of term delivery of about one-third,4,11 and in routine practice, administration of ACS after 34 weeks may be associated with even higher rates of term delivery.
This is important because recent evidence shows an unfavorable impact of ACS exposure in term-born children.12 The 5-year follow-up of the largest randomized trial in which multiple ACS courses were used noted that babies born at term had a 4-fold increased odds ratio for neurosensory disability.11 There was no dose−response interaction, with the same adverse odds ratio after 1 or 4 additional ACS courses. This observation was consistent with a previously reported Swedish national cohort, pointing to an unfavorable impact of even a single course of ACS in term-born children, with a greater likelihood of harm than benefit.13
In a UK follow-up of children aged 8 to 15 years who were enrolled in an RCT of ACS before cesarean delivery at term, low academic achievement was significantly more common in the group whose mothers had received ACS.14 In another study of 304 children born at term after exposure to a single course of ACS, investigators noted significantly increased cortisol reactivity to acute psychological stress at ages 6 to 11 years in the ACS-exposed patients, compared with 212 babies of women with threatened preterm labor who did not receive ACS and 372 babies from uncomplicated term pregnancies.15
The relevance of such study findings extends beyond childhood given the fact that elevated hypothalamic-pituitary-adrenal (HPA) axis reactivity has been linked to the pathogenesis of metabolic syndrome and depression in adult life.16 As recently as 2015, investigators of a randomized trial of ACS in 6 low- and middle-income countries highlighted their concern regarding “potentially harmful use of antenatal corticosteroids for infants not delivered preterm.”17
There are safety concerns with ACS in the late preterm periodThe effects of ACS are more pleiotropic than those reflected in a lower incidence of respiratory difficulties. Knowledge of the overall consequences of ACS exposure in infants born late-preterm or at term is still limited. The close-to-term fetus exposed to exogenous corticosteroids is also exposed to the physiologic endogenous surge of cortisol known to occur in the maternal circulation in late pregnancy, which reaches levels 3 times higher than those seen in nonpregnant women.18 Although placental 11 beta-hydroxysteroid dehydrogenase type 2 plays a protective role by allowing no more than 10% to 20% of maternal corticosteroids to cross the placenta, fetal overexposure from concomitant exogenous maternal corticosteroid administration remains a theoretical concern close to term. This is especially worrisome if there is a gestational age−related increase in the sensitivity to corticosteroid-induced in utero fetal programming. It has been reported that fetal overexposure to corticosteroids in late pregnancy can permanently increase the activity of the HPA-axis, with likely consequences in adult life.19
Another concern relates to oligodendrocytes development. Although the neuronal division process in humans usually is completed by 24 weeks’ gestation, the most rapid growth for oligodendrocytes occurs between 34 and 36 weeks’ gestation; these are the cells responsible for the synthesis of myelin. Overexposure to corticosteroids at this vulnerable time in the late preterm fetus potentially may have unanticipated negative neurologic consequences.20
This is the only scenario in which we feel antenatal corticosteroids could be used in a fetus aged 34 weeks to 36 weeks 5 days. In the setting of a scheduled cesarean delivery between 34 weeks and 35 weeks, the concerns relative to term delivery after corticosteroid exposure may not apply, but the concerns in relation to the administration of corticosteroid in the late preterm period—which is a time of possibly increased neurohormonal and neurologic vulnerability—still apply. With regard to the risk of neonatal hypoglycemia, one might argue that close neonatal monitoring of babies so exposed may ensure that any associated neonatal hypoglycemia does not go unnoticed or untreated. However, the prognostic significance of even short periods of neonatal hypoglycemia has not been established.
Where should future studies focus?There is clear neonatal benefit from a single course of ACS given to women who will deliver before 34 weeks’ gestation. It is widely accepted, based on the evidence provided by the 30-year follow-up of the cohort of 534 participants from the Auckland trial (the longest follow-up for any pregnancy trial), that administration of ACS at less than 34 weeks’ gestation is not associated with any obvious major developmental risk.21−23
However, the reassurances provided by the Auckland cohort should be neither directly extrapolated to the administration of ACS in the late preterm period nor applied to term-born babies exposed to ACS, for the simple reason that these subgroups never have been analyzed separately. The risk:benefit ratio of ACS use in the late-preterm period is as yet unknown, and in term-born babies the ratio may be unfavorable.
Follow-up studies are neededWe consider that there is a vital need for long-term follow-up studies. The focus of research on the effects of ACS no longer is on the immediate neonatal outcomes and now is on safety and the long-term outcomes of this exposure.
Bottom lineWe regard the large, high-quality study conducted by the NICHD MFMU Network1 as an opportunity to answer current concerns. It is hoped that the resources necessaryfor in-depth follow-up of the children involved in this study will be provided to the investigators and to the NICHD. It is only with such follow-up that mid- and long-term adverse effects can be assessed. We believe that, at a minimum, mid-term follow-up data should be available before it is wise to make any definitive recommendations for a sweeping change in clinical practice.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
The results of the highly anticipated Antenatal Late Preterm Study recently have become available.1 Data from this randomized controlled trial, conducted by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units (MFMU) Network, demonstrated that administration of betamethasone to women at risk for preterm delivery between 34 weeks 0 days and 36 weeks 6 days of gestation significantly reduces the rate of neonatal respiratory complications. It may represent the largest study of antenatal corticosteroids (ACS) to date, with 2,827 infants studied, and its results inevitably lead to the logical practical question: Should ACS use be extended beyond the 34 weeks’ gestation limit previously recommended by professional guidelines in the United States2?
There are some issues that bear discussion before such a significant change in standard of care should be promoted.2
Antenatal Late Preterm Study outcomesThe primary outcome in the study was a composite end point describing the need for respiratory support within 72 hours after birth. Based on a pilot study, the investigators had anticipated a 33% decrease in the rate of the primary outcome; however, the reduction was only 20% (relative risk [RR], 0.80; 95% confidence interval [CI], 0.66−0.97). Although the effect size was statistically significant, one could question the clinical relevance of such a small difference.
A 33% reduction effect, more consistent with the preliminary expectations, was noted in the prespecified secondary composite outcome of severe respiratory complications (RR, 0.67; 95% CI, 0.53−0.84). Occurrences included in the secondary composite outcome that also showed significant rate reductions were:
- the use of continuous positive airway pressure (CPAP) or high-flow oxygen via nasal cannula for at least 12 hours (RR, 0.62; 95% CI, 0.48−0.80)
- need for resuscitation at birth (RR, 0.78; 95% CI, 0.66−0.92)
- surfactant use (RR, 0.59; 95% CI, 0.37−0.96)
- transient tachypnea of the newborn (RR, 0.68; 95% CI, 0.53−0.87).
The reported reduction in bronchopulmonary dysplasia (RR, 0.22; 95% CI, 0.02−0.92) cannot plausibly be attributed to ACS. Randomized data aggregated by the Cochrane Database of Systematic Reviews3 do not show improvement in chronic lung disease with ACS use. Moreover, the authors recognize that the assessment for bronchopulmonary dysplasia at only 28 days of life is only partially informative and that longer childhood follow-up is required to confirm the finding.
- Although corticosteroids have been shown to reduce the risk of the baby needing breathing support by 20%, they are associated with a 60% increase in risk for low blood sugar in the newborn (hypoglycemia). Hypoglycemia can place the baby at risk for seizures and even brain damage.
- There is an unknown safety profile for corticosteroid administration at this gestational age. The fetal brain is still developing during this period, and there is some information to suggest that corticosteroids could have an unfavorable effect on brain development.
- Corticosteroids are potent hormones and potentially can have undesired hormonal effects at this gestational age.
- If corticosteroids are given and the mother carries the baby to term (37 weeks or later) there are some studies that suggest the baby is at an increased risk for neurologic, cognitive, metabolic, and/or behavioral abnormalities in later life.
We recommend caution before changing current practiceWe propose prudence with ACS use after 34 weeks’ gestation for the following reasons: the increased risk for neonatal hypoglycemia associated with ACS, the increased risk for ACS-related harm in term-born babies, and safety concerns with ACS in the late preterm period.
Evidence shows an increased risk for neonatal hypoglycemiaThe most profound effect modification observed in the study was an adverse effect—namely, a 60% increase in neonatal hypoglycemia with ACS administration (RR, 1.6; 95% CI, 1.37−1.87). The rate of neonatal hypoglycemia was 24% in the ACS group, compared with 15% in the placebo group.
Results of prior studies have demonstrated either no increased risk of hypoglycemia with ACS use4−7 or a much smaller increase (from 4.2% to 5.7%).8 The higher rate of neonatal hypoglycemia seen in this study suggests the possibility that the late preterm population may be more vulnerable to the negative impact of ACS on neonatal glucose/insulin homeostasis. Presumed mechanisms of action are either maternal hyperglycemia or fetal adrenal suppression or both, with potential for fetal adrenal suppression resulting from betamethasone exposure to affect long-term metabolic outcomes.9
Of note, women with pregestational diabetes were excluded from the study and, in routine practice, inclusion of such patients may further increase the risk of neonatal hypoglycemia.
There are few data on the prognostic significance of neonatal hypoglycemia in preterm infants, with the exception of a single study, the results of which show that it is associated with adverse neurodevelopment at 18 months of age.10
Data reveal increased risk for harm in term-born babiesIn spite of strict protocol specifications to increase the probability of delivery before 37 weeks’ gestation, 16% of women in the trial delivered at term. Investigators of prior randomized studies of ACS, aimed at reducing the risks of prematurity, have reported a rate of term delivery of about one-third,4,11 and in routine practice, administration of ACS after 34 weeks may be associated with even higher rates of term delivery.
This is important because recent evidence shows an unfavorable impact of ACS exposure in term-born children.12 The 5-year follow-up of the largest randomized trial in which multiple ACS courses were used noted that babies born at term had a 4-fold increased odds ratio for neurosensory disability.11 There was no dose−response interaction, with the same adverse odds ratio after 1 or 4 additional ACS courses. This observation was consistent with a previously reported Swedish national cohort, pointing to an unfavorable impact of even a single course of ACS in term-born children, with a greater likelihood of harm than benefit.13
In a UK follow-up of children aged 8 to 15 years who were enrolled in an RCT of ACS before cesarean delivery at term, low academic achievement was significantly more common in the group whose mothers had received ACS.14 In another study of 304 children born at term after exposure to a single course of ACS, investigators noted significantly increased cortisol reactivity to acute psychological stress at ages 6 to 11 years in the ACS-exposed patients, compared with 212 babies of women with threatened preterm labor who did not receive ACS and 372 babies from uncomplicated term pregnancies.15
The relevance of such study findings extends beyond childhood given the fact that elevated hypothalamic-pituitary-adrenal (HPA) axis reactivity has been linked to the pathogenesis of metabolic syndrome and depression in adult life.16 As recently as 2015, investigators of a randomized trial of ACS in 6 low- and middle-income countries highlighted their concern regarding “potentially harmful use of antenatal corticosteroids for infants not delivered preterm.”17
There are safety concerns with ACS in the late preterm periodThe effects of ACS are more pleiotropic than those reflected in a lower incidence of respiratory difficulties. Knowledge of the overall consequences of ACS exposure in infants born late-preterm or at term is still limited. The close-to-term fetus exposed to exogenous corticosteroids is also exposed to the physiologic endogenous surge of cortisol known to occur in the maternal circulation in late pregnancy, which reaches levels 3 times higher than those seen in nonpregnant women.18 Although placental 11 beta-hydroxysteroid dehydrogenase type 2 plays a protective role by allowing no more than 10% to 20% of maternal corticosteroids to cross the placenta, fetal overexposure from concomitant exogenous maternal corticosteroid administration remains a theoretical concern close to term. This is especially worrisome if there is a gestational age−related increase in the sensitivity to corticosteroid-induced in utero fetal programming. It has been reported that fetal overexposure to corticosteroids in late pregnancy can permanently increase the activity of the HPA-axis, with likely consequences in adult life.19
Another concern relates to oligodendrocytes development. Although the neuronal division process in humans usually is completed by 24 weeks’ gestation, the most rapid growth for oligodendrocytes occurs between 34 and 36 weeks’ gestation; these are the cells responsible for the synthesis of myelin. Overexposure to corticosteroids at this vulnerable time in the late preterm fetus potentially may have unanticipated negative neurologic consequences.20
This is the only scenario in which we feel antenatal corticosteroids could be used in a fetus aged 34 weeks to 36 weeks 5 days. In the setting of a scheduled cesarean delivery between 34 weeks and 35 weeks, the concerns relative to term delivery after corticosteroid exposure may not apply, but the concerns in relation to the administration of corticosteroid in the late preterm period—which is a time of possibly increased neurohormonal and neurologic vulnerability—still apply. With regard to the risk of neonatal hypoglycemia, one might argue that close neonatal monitoring of babies so exposed may ensure that any associated neonatal hypoglycemia does not go unnoticed or untreated. However, the prognostic significance of even short periods of neonatal hypoglycemia has not been established.
Where should future studies focus?There is clear neonatal benefit from a single course of ACS given to women who will deliver before 34 weeks’ gestation. It is widely accepted, based on the evidence provided by the 30-year follow-up of the cohort of 534 participants from the Auckland trial (the longest follow-up for any pregnancy trial), that administration of ACS at less than 34 weeks’ gestation is not associated with any obvious major developmental risk.21−23
However, the reassurances provided by the Auckland cohort should be neither directly extrapolated to the administration of ACS in the late preterm period nor applied to term-born babies exposed to ACS, for the simple reason that these subgroups never have been analyzed separately. The risk:benefit ratio of ACS use in the late-preterm period is as yet unknown, and in term-born babies the ratio may be unfavorable.
Follow-up studies are neededWe consider that there is a vital need for long-term follow-up studies. The focus of research on the effects of ACS no longer is on the immediate neonatal outcomes and now is on safety and the long-term outcomes of this exposure.
Bottom lineWe regard the large, high-quality study conducted by the NICHD MFMU Network1 as an opportunity to answer current concerns. It is hoped that the resources necessaryfor in-depth follow-up of the children involved in this study will be provided to the investigators and to the NICHD. It is only with such follow-up that mid- and long-term adverse effects can be assessed. We believe that, at a minimum, mid-term follow-up data should be available before it is wise to make any definitive recommendations for a sweeping change in clinical practice.
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery [published online ahead of print February 4, 2016]. N Engl J Med.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG Committee Opinion No. 475: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2011;117(2 pt 1):422–424.
- Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;(3):CD004454.
- Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics. 1972;50(4):515–525.
- Sann L, Burnod J, Lasne Y, Bethenod M. Antenatal administration of betamethasone: effects upon neonatal blood glucose in premature infants [in French]. Nouv Presse Med. 1979;8(39):3147–3148.
- Rokicki W, Krasnodebski J. Antenatal glucocorticoid administration and neonatal glycemia. Dev Pharmacol Ther. 1987;10(4):307–311.
- Gazquez Serrano IM, Arroyos Plana A, Diaz Morales O, Herraiz Perea C, Holgueras Bragado A. Antenatal corticosteroid therapy and late preterm infant morbidity and mortality [in Spanish]. An Pediatr (Barc). 2014;81(6):374–382.
- Pettit KE, Tran SH, Lee E, Caughey AB. The association of antenatal corticosteroids with neonatal hypoglycemia and hyperbilirubinemia. J Matern Fetal Neonatal Med. 2014;27(7):683–686.
- Aydin M, Derveci U, Hakan N. Neonatal hypoglycemia associated with the antenatal corticosteroids may be secondary to fetal adrenal suppression. J Matern Fetal Neonatal Med. 2015;28(8):892.
- Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ. 1988;297(6659):1304–1308.
- Asztalos EV, Murphy KE, Willan AR, et al; MACS-5 Collaborative Group. Multiple courses of antenatal corticosteroids for preterm birth study: outcomes in children at 5 years of age (MACS-5). JAMA Pediatr. 2013;167(12):1102–1110.
- Vidaeff AC, Belfort MA, Steer PJ. Antenatal corticosteroids: a time for more careful scrutiny of the indications [published online ahead of print January 18, 2016]. BJOG. doi:10.1111/1471-0528.13853.
- Eriksson L, Haglund B, Ewald U, Odlind V, Kieler H. Health consequences of prophylactic exposure to antenatal corticosteroids among children born late preterm or term. Acta Obstet Gynecol Scand. 2012;91(12):1415–1421.
- Stutchfield PR, Whitaker R, Gliddon AE, Hobson L, Kotecha S, Doull IJ. Behavioural, educational and respiratory outcomes of antenatal betamethasone for term caesarean section (ASTECS trial). Arch Dis Child Fetal Neonatal Ed. 2013;98(3):F195–F200.
- Alexander N, Rosenlocher F, Stalder T, et al. Impact of antenatal synthetic glucocorticoid exposure on endocrine stress reactivity in term-born children. J Clin Endocrinol Metab. 2012;97(10):3538–3544.
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5(7):374–381.
- Althabe F, Belizan JM, McClure EM, et al. A population-based, multifaceted strategy to implement antenatal corticosteroid treatment versus standard care for the reduction of neonatal mortality due to preterm birth in low-income and middle-income countries: the ACT cluster-randomised trial. Lancet. 2015;385(9968):629–639.
- Jung C, Ho JT, Torpy DJ, et al. A longitudinal study of plasma and urinary cortisol in pregnancy and postpartum. J Clin Endocrinol Metab. 2011;96(5):1533–1540.
- Welberg LA, Seckl JR, Holmes MC. Inhibition of 11ß-hydroxysteroid dehydrogenase, the foeto-placental barrier to maternal glucocorticoids, permanently programs amygdale GR mRNA expression and anxiety-like behavior in the offspring. Eur J Neurosci. 2000;12(3):1047–1054.
- Whitelaw A, Thoresen M. Antenatal steroids and the developing brain. Arch Dis Child Fetal Neonatal Ed. 2000;83(2):F154–F157.
- Dalziel SR, Walker NK, Parag V, et al. Cardiovascular risk factors after antenatal exposure to betamethasone: 30-year follow-up of a randomised controlled trial. Lancet. 2005;365(9474):1856–1862.
- Dalziel SR, Lim VK, Lambert A, et al. Antenatal exposure to betamethasone: psychological functioning and health related quality of life 31 years after inclusion in randomised controlled trial. BMJ. 2005;331(7518):665.
- Welberg LA, Seckl JR, Holmes MC. Inhibition of 11Dalziel SR, Walker NK, Parag V, et al. Dalziel SR, Lim VK, Lambert A, et al. Dalziel SR, Rea HH, Walker NK, et al.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, et al; NICHD Maternal-Fetal Medicine Units Network. Antenatal betamethasone for women at risk for late preterm delivery [published online ahead of print February 4, 2016]. N Engl J Med.
- American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG Committee Opinion No. 475: antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol. 2011;117(2 pt 1):422–424.
- Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;(3):CD004454.
- Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics. 1972;50(4):515–525.
- Sann L, Burnod J, Lasne Y, Bethenod M. Antenatal administration of betamethasone: effects upon neonatal blood glucose in premature infants [in French]. Nouv Presse Med. 1979;8(39):3147–3148.
- Rokicki W, Krasnodebski J. Antenatal glucocorticoid administration and neonatal glycemia. Dev Pharmacol Ther. 1987;10(4):307–311.
- Gazquez Serrano IM, Arroyos Plana A, Diaz Morales O, Herraiz Perea C, Holgueras Bragado A. Antenatal corticosteroid therapy and late preterm infant morbidity and mortality [in Spanish]. An Pediatr (Barc). 2014;81(6):374–382.
- Pettit KE, Tran SH, Lee E, Caughey AB. The association of antenatal corticosteroids with neonatal hypoglycemia and hyperbilirubinemia. J Matern Fetal Neonatal Med. 2014;27(7):683–686.
- Aydin M, Derveci U, Hakan N. Neonatal hypoglycemia associated with the antenatal corticosteroids may be secondary to fetal adrenal suppression. J Matern Fetal Neonatal Med. 2015;28(8):892.
- Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ. 1988;297(6659):1304–1308.
- Asztalos EV, Murphy KE, Willan AR, et al; MACS-5 Collaborative Group. Multiple courses of antenatal corticosteroids for preterm birth study: outcomes in children at 5 years of age (MACS-5). JAMA Pediatr. 2013;167(12):1102–1110.
- Vidaeff AC, Belfort MA, Steer PJ. Antenatal corticosteroids: a time for more careful scrutiny of the indications [published online ahead of print January 18, 2016]. BJOG. doi:10.1111/1471-0528.13853.
- Eriksson L, Haglund B, Ewald U, Odlind V, Kieler H. Health consequences of prophylactic exposure to antenatal corticosteroids among children born late preterm or term. Acta Obstet Gynecol Scand. 2012;91(12):1415–1421.
- Stutchfield PR, Whitaker R, Gliddon AE, Hobson L, Kotecha S, Doull IJ. Behavioural, educational and respiratory outcomes of antenatal betamethasone for term caesarean section (ASTECS trial). Arch Dis Child Fetal Neonatal Ed. 2013;98(3):F195–F200.
- Alexander N, Rosenlocher F, Stalder T, et al. Impact of antenatal synthetic glucocorticoid exposure on endocrine stress reactivity in term-born children. J Clin Endocrinol Metab. 2012;97(10):3538–3544.
- Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5(7):374–381.
- Althabe F, Belizan JM, McClure EM, et al. A population-based, multifaceted strategy to implement antenatal corticosteroid treatment versus standard care for the reduction of neonatal mortality due to preterm birth in low-income and middle-income countries: the ACT cluster-randomised trial. Lancet. 2015;385(9968):629–639.
- Jung C, Ho JT, Torpy DJ, et al. A longitudinal study of plasma and urinary cortisol in pregnancy and postpartum. J Clin Endocrinol Metab. 2011;96(5):1533–1540.
- Welberg LA, Seckl JR, Holmes MC. Inhibition of 11ß-hydroxysteroid dehydrogenase, the foeto-placental barrier to maternal glucocorticoids, permanently programs amygdale GR mRNA expression and anxiety-like behavior in the offspring. Eur J Neurosci. 2000;12(3):1047–1054.
- Whitelaw A, Thoresen M. Antenatal steroids and the developing brain. Arch Dis Child Fetal Neonatal Ed. 2000;83(2):F154–F157.
- Dalziel SR, Walker NK, Parag V, et al. Cardiovascular risk factors after antenatal exposure to betamethasone: 30-year follow-up of a randomised controlled trial. Lancet. 2005;365(9474):1856–1862.
- Dalziel SR, Lim VK, Lambert A, et al. Antenatal exposure to betamethasone: psychological functioning and health related quality of life 31 years after inclusion in randomised controlled trial. BMJ. 2005;331(7518):665.
- Welberg LA, Seckl JR, Holmes MC. Inhibition of 11Dalziel SR, Walker NK, Parag V, et al. Dalziel SR, Lim VK, Lambert A, et al. Dalziel SR, Rea HH, Walker NK, et al.
Does a second course of antenatal corticosteroids offer benefit in the setting of preterm PROM?
Gyamfi-Bannerman and Son report their secondary analysis of a randomized controlled trial (RCT) conducted through the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Maternal-Fetal Medicine Units Network. The aim of the parent RCT was to determine whether antenatal administration of magnesium sulfate decreases the rate of cerebral palsy or death in children delivered preterm. More than 80% of the women enrolled in this RCT had preterm PROM. Of these women, 98% were given antenatal corticosteroids for fetal maturation, and 9% received two courses. This aspect of the RCT provided an opportunity for Gyamfi-Bannerman and Son to study the comparative effects of one course versus two courses of ACS in the setting of preterm PROM.
Background of the study
Concern about the declining efficacy of ACS when the interval between administration and delivery exceeds 7 days prompted several randomized trials exploring the safety and efficacy of multiple ACS courses. Multiple courses were ultimately deemed to be inadvisable because of an association with reduced birth weight and neonatal head circumference.1,2 However, the unfavorable effects of ACS on anthropometrics was observed when more than three courses were administered, leaving open the possibility of giving only one additional course when needed as a “rescue” dose. Indeed, the use of a single rescue course of ACS in women with intact membranes had a favorable impact on neonatal respiratory function in two RCTs.3,4
The best available evidence (Level 1) demonstrates that the use of a single course of ACS in preterm PROM does not increase the risk of neonatal or maternal infection even in the setting of prolonged rupture of membranes.5 However, pregnant women with preterm PROM were excluded from trials of repetitive ACS dosing because earlier observational studies had suggested that they would experience a substantially increased risk of infectious morbidity when three or more courses of ACS are given.6–8 What remained debatable on a scientific level was whether a single rescue dose of ACS in women with preterm PROM would be safe and beneficial.
Findings of the analysis
Compared with a single course of ACS, exposure to two courses did not influence the rate of neonatal sepsis or chorioamnionitis. As reassuring as that finding may be, the study found no benefit for the additional course, although it was powered to do so. There was no difference in the rates of respiratory distress syndrome between the study groups.
The findings of Gyamfi-Bannerman and Son replicate those of a subgroup analysis of women in an RCT comparing weekly and single-course ACS.9 In that study, weekly courses of ACS in women with preterm PROM did not improve neonatal outcomes beyond what was achieved with single-course therapy. Similar findings have been reported by the Cochrane database.10
Ruptured versus intact membranes: When is the benefit of ACS greater?
The improvement in neonatal outcomes observed with ACS in pregnancies complicated by preterm PROM is not as pronounced as it is in gestations with intact membranes. In preterm PROM, fetuses reportedly are stressed by the presence of intrauterine inflammation or infection, or both, which accelerates lung maturity by encouraging the secretion of endogenous corticosteroids, resulting in the production of surfactant and eliminating the potential benefit of exogenous ACS.11 This theoretical consideration has not been verified in a systematic analysis of accumulated data,5 and the administration of a single course of ACS in preterm PROM now has been shown clearly to improve neonatal outcomes.12 As Gyamfi-Bannerman and Son demonstrate, the same cannot be said about the administration of a rescue dose of ACS.
Strengths and limitations of the trial
Gyamfi-Bannerman and Son did not address the same interaction as the parent study. The exposure of interest was ACS, an event that occurred in a manner unrelated to the randomization for magnesium sulfate administration. Therefore, the outcome data are no longer randomized in nature, and the study becomes a retrospective cohort analysis.
Gyamfi-Bannerman and Son recognize the limitations of such a study, especially the lack of standardization in the intervention (exact timing of intervention or type of formulation). As with any nonrandomized experiment, the potential for unintended systematic bias is present.
This study, in particular, was subject to “survivor bias,” as reflected in the significantly different intervals between membrane rupture and delivery in the two groups.
What this evidence means for practice
We must always remain cautious about basing policy or clinical decisions on cohort studies. It has been argued that basing a change in clinical practice on the findings of subgroup analyses is a deviation from fundamental scientific truth.13 Such findings should be regarded as hypothesis testing only and considered exploratory in nature.
This study’s abstract conclusion that there is a lack of association between a second dose of ACS and neonatal sepsis should not be regarded as justification to use a rescue course of ACS in women with preterm PROM. We recommend that such a practice be avoided outside the context of an approved research protocol.
— Kathleen M. Antony, MD, and Alex C. Vidaeff, MD, MPH
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Wapner RJ, Sorokin Y, Thom EA, et al. Single versus weekly courses of antenatal corticosteroids: evaluation of safety and efficacy. Am J Obstet Gynecol. 2006;195(3):633–642.
2. Murphy KE, Hannah ME, Willan AR, et al; MACS Collaborative Group. Multiple Courses of Antenatal Corticosteroids for Preterm Birth (MACS): a randomized controlled trial. Lancet. 2008;372(9656):2143–2151.
3. Garite TJ, Kurtzman, Maurel K, et al. Impact of a “rescue course” of antenatal corticosteroids: a multicenter randomized placebo-controlled trial. Am J Obstet Gynecol. 2009;200(3):248.e1–e9.
4. McEvoy C, Schilling D, Peters D, et al. Respiratory compliance in preterm infants after a single rescue course of antenatal steroids: a randomized controlled trial. Am J Obstet Gynecol. 2010;202(6):544.e1–e9.
5. Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;(3):CD004454.
6. Rotmensch S, Vishne TH, Celentano C, et al. Maternal infectious morbidity following multiple courses of betamethasone. J Infect. 1999;39(1):49–54.
7. Vermillion ST, Soper DE, Chasedunn-Roark J. Neonatal sepsis after betamethasone administration to patients with preterm premature rupture of membranes. Am J Obstet Gynecol. 1999;181(2):320–327.
8. Yang SH, Choi SJ, Roh CR, et al. Multiple courses of antenatal corticosteroid therapy in patients with preterm premature rupture of membranes. J Perinat Med. 2004;32(1):42–48.
9. Lee MJ, Davies J, Guinn D, et al. Single versus weekly courses of antenatal corticosteroids in preterm premature rupture of membranes. Obstet Gynecol. 2004;103(2):274–281.
10. Crowther CA, McKinlay CJ, Middleton P, Harding JE. Repeat doses of prenatal corticosteroids for women at risk of preterm birth for improving neonatal health outcomes. Cochrane Database Syst Rev. 2011;(6):CD003935.
11. Lyon A. Chronic lung disease of prematurity. The role of intrauterine infection. Eur J Pediatr. 2000;159(11):798–802.
12. Vidaeff AC, Ramin SM. Antenatal corticosteroids after preterm premature rupture of membranes. Clin Obstet Gynecol. 2011;54(2):337–343.
13. Bailar JC. How to distort the scientific record without actually lying: truth, and the arts of science. Eur J Oncol. 2006;11(4):217–224.
Gyamfi-Bannerman and Son report their secondary analysis of a randomized controlled trial (RCT) conducted through the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Maternal-Fetal Medicine Units Network. The aim of the parent RCT was to determine whether antenatal administration of magnesium sulfate decreases the rate of cerebral palsy or death in children delivered preterm. More than 80% of the women enrolled in this RCT had preterm PROM. Of these women, 98% were given antenatal corticosteroids for fetal maturation, and 9% received two courses. This aspect of the RCT provided an opportunity for Gyamfi-Bannerman and Son to study the comparative effects of one course versus two courses of ACS in the setting of preterm PROM.
Background of the study
Concern about the declining efficacy of ACS when the interval between administration and delivery exceeds 7 days prompted several randomized trials exploring the safety and efficacy of multiple ACS courses. Multiple courses were ultimately deemed to be inadvisable because of an association with reduced birth weight and neonatal head circumference.1,2 However, the unfavorable effects of ACS on anthropometrics was observed when more than three courses were administered, leaving open the possibility of giving only one additional course when needed as a “rescue” dose. Indeed, the use of a single rescue course of ACS in women with intact membranes had a favorable impact on neonatal respiratory function in two RCTs.3,4
The best available evidence (Level 1) demonstrates that the use of a single course of ACS in preterm PROM does not increase the risk of neonatal or maternal infection even in the setting of prolonged rupture of membranes.5 However, pregnant women with preterm PROM were excluded from trials of repetitive ACS dosing because earlier observational studies had suggested that they would experience a substantially increased risk of infectious morbidity when three or more courses of ACS are given.6–8 What remained debatable on a scientific level was whether a single rescue dose of ACS in women with preterm PROM would be safe and beneficial.
Findings of the analysis
Compared with a single course of ACS, exposure to two courses did not influence the rate of neonatal sepsis or chorioamnionitis. As reassuring as that finding may be, the study found no benefit for the additional course, although it was powered to do so. There was no difference in the rates of respiratory distress syndrome between the study groups.
The findings of Gyamfi-Bannerman and Son replicate those of a subgroup analysis of women in an RCT comparing weekly and single-course ACS.9 In that study, weekly courses of ACS in women with preterm PROM did not improve neonatal outcomes beyond what was achieved with single-course therapy. Similar findings have been reported by the Cochrane database.10
Ruptured versus intact membranes: When is the benefit of ACS greater?
The improvement in neonatal outcomes observed with ACS in pregnancies complicated by preterm PROM is not as pronounced as it is in gestations with intact membranes. In preterm PROM, fetuses reportedly are stressed by the presence of intrauterine inflammation or infection, or both, which accelerates lung maturity by encouraging the secretion of endogenous corticosteroids, resulting in the production of surfactant and eliminating the potential benefit of exogenous ACS.11 This theoretical consideration has not been verified in a systematic analysis of accumulated data,5 and the administration of a single course of ACS in preterm PROM now has been shown clearly to improve neonatal outcomes.12 As Gyamfi-Bannerman and Son demonstrate, the same cannot be said about the administration of a rescue dose of ACS.
Strengths and limitations of the trial
Gyamfi-Bannerman and Son did not address the same interaction as the parent study. The exposure of interest was ACS, an event that occurred in a manner unrelated to the randomization for magnesium sulfate administration. Therefore, the outcome data are no longer randomized in nature, and the study becomes a retrospective cohort analysis.
Gyamfi-Bannerman and Son recognize the limitations of such a study, especially the lack of standardization in the intervention (exact timing of intervention or type of formulation). As with any nonrandomized experiment, the potential for unintended systematic bias is present.
This study, in particular, was subject to “survivor bias,” as reflected in the significantly different intervals between membrane rupture and delivery in the two groups.
What this evidence means for practice
We must always remain cautious about basing policy or clinical decisions on cohort studies. It has been argued that basing a change in clinical practice on the findings of subgroup analyses is a deviation from fundamental scientific truth.13 Such findings should be regarded as hypothesis testing only and considered exploratory in nature.
This study’s abstract conclusion that there is a lack of association between a second dose of ACS and neonatal sepsis should not be regarded as justification to use a rescue course of ACS in women with preterm PROM. We recommend that such a practice be avoided outside the context of an approved research protocol.
— Kathleen M. Antony, MD, and Alex C. Vidaeff, MD, MPH
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Gyamfi-Bannerman and Son report their secondary analysis of a randomized controlled trial (RCT) conducted through the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Maternal-Fetal Medicine Units Network. The aim of the parent RCT was to determine whether antenatal administration of magnesium sulfate decreases the rate of cerebral palsy or death in children delivered preterm. More than 80% of the women enrolled in this RCT had preterm PROM. Of these women, 98% were given antenatal corticosteroids for fetal maturation, and 9% received two courses. This aspect of the RCT provided an opportunity for Gyamfi-Bannerman and Son to study the comparative effects of one course versus two courses of ACS in the setting of preterm PROM.
Background of the study
Concern about the declining efficacy of ACS when the interval between administration and delivery exceeds 7 days prompted several randomized trials exploring the safety and efficacy of multiple ACS courses. Multiple courses were ultimately deemed to be inadvisable because of an association with reduced birth weight and neonatal head circumference.1,2 However, the unfavorable effects of ACS on anthropometrics was observed when more than three courses were administered, leaving open the possibility of giving only one additional course when needed as a “rescue” dose. Indeed, the use of a single rescue course of ACS in women with intact membranes had a favorable impact on neonatal respiratory function in two RCTs.3,4
The best available evidence (Level 1) demonstrates that the use of a single course of ACS in preterm PROM does not increase the risk of neonatal or maternal infection even in the setting of prolonged rupture of membranes.5 However, pregnant women with preterm PROM were excluded from trials of repetitive ACS dosing because earlier observational studies had suggested that they would experience a substantially increased risk of infectious morbidity when three or more courses of ACS are given.6–8 What remained debatable on a scientific level was whether a single rescue dose of ACS in women with preterm PROM would be safe and beneficial.
Findings of the analysis
Compared with a single course of ACS, exposure to two courses did not influence the rate of neonatal sepsis or chorioamnionitis. As reassuring as that finding may be, the study found no benefit for the additional course, although it was powered to do so. There was no difference in the rates of respiratory distress syndrome between the study groups.
The findings of Gyamfi-Bannerman and Son replicate those of a subgroup analysis of women in an RCT comparing weekly and single-course ACS.9 In that study, weekly courses of ACS in women with preterm PROM did not improve neonatal outcomes beyond what was achieved with single-course therapy. Similar findings have been reported by the Cochrane database.10
Ruptured versus intact membranes: When is the benefit of ACS greater?
The improvement in neonatal outcomes observed with ACS in pregnancies complicated by preterm PROM is not as pronounced as it is in gestations with intact membranes. In preterm PROM, fetuses reportedly are stressed by the presence of intrauterine inflammation or infection, or both, which accelerates lung maturity by encouraging the secretion of endogenous corticosteroids, resulting in the production of surfactant and eliminating the potential benefit of exogenous ACS.11 This theoretical consideration has not been verified in a systematic analysis of accumulated data,5 and the administration of a single course of ACS in preterm PROM now has been shown clearly to improve neonatal outcomes.12 As Gyamfi-Bannerman and Son demonstrate, the same cannot be said about the administration of a rescue dose of ACS.
Strengths and limitations of the trial
Gyamfi-Bannerman and Son did not address the same interaction as the parent study. The exposure of interest was ACS, an event that occurred in a manner unrelated to the randomization for magnesium sulfate administration. Therefore, the outcome data are no longer randomized in nature, and the study becomes a retrospective cohort analysis.
Gyamfi-Bannerman and Son recognize the limitations of such a study, especially the lack of standardization in the intervention (exact timing of intervention or type of formulation). As with any nonrandomized experiment, the potential for unintended systematic bias is present.
This study, in particular, was subject to “survivor bias,” as reflected in the significantly different intervals between membrane rupture and delivery in the two groups.
What this evidence means for practice
We must always remain cautious about basing policy or clinical decisions on cohort studies. It has been argued that basing a change in clinical practice on the findings of subgroup analyses is a deviation from fundamental scientific truth.13 Such findings should be regarded as hypothesis testing only and considered exploratory in nature.
This study’s abstract conclusion that there is a lack of association between a second dose of ACS and neonatal sepsis should not be regarded as justification to use a rescue course of ACS in women with preterm PROM. We recommend that such a practice be avoided outside the context of an approved research protocol.
— Kathleen M. Antony, MD, and Alex C. Vidaeff, MD, MPH
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Wapner RJ, Sorokin Y, Thom EA, et al. Single versus weekly courses of antenatal corticosteroids: evaluation of safety and efficacy. Am J Obstet Gynecol. 2006;195(3):633–642.
2. Murphy KE, Hannah ME, Willan AR, et al; MACS Collaborative Group. Multiple Courses of Antenatal Corticosteroids for Preterm Birth (MACS): a randomized controlled trial. Lancet. 2008;372(9656):2143–2151.
3. Garite TJ, Kurtzman, Maurel K, et al. Impact of a “rescue course” of antenatal corticosteroids: a multicenter randomized placebo-controlled trial. Am J Obstet Gynecol. 2009;200(3):248.e1–e9.
4. McEvoy C, Schilling D, Peters D, et al. Respiratory compliance in preterm infants after a single rescue course of antenatal steroids: a randomized controlled trial. Am J Obstet Gynecol. 2010;202(6):544.e1–e9.
5. Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;(3):CD004454.
6. Rotmensch S, Vishne TH, Celentano C, et al. Maternal infectious morbidity following multiple courses of betamethasone. J Infect. 1999;39(1):49–54.
7. Vermillion ST, Soper DE, Chasedunn-Roark J. Neonatal sepsis after betamethasone administration to patients with preterm premature rupture of membranes. Am J Obstet Gynecol. 1999;181(2):320–327.
8. Yang SH, Choi SJ, Roh CR, et al. Multiple courses of antenatal corticosteroid therapy in patients with preterm premature rupture of membranes. J Perinat Med. 2004;32(1):42–48.
9. Lee MJ, Davies J, Guinn D, et al. Single versus weekly courses of antenatal corticosteroids in preterm premature rupture of membranes. Obstet Gynecol. 2004;103(2):274–281.
10. Crowther CA, McKinlay CJ, Middleton P, Harding JE. Repeat doses of prenatal corticosteroids for women at risk of preterm birth for improving neonatal health outcomes. Cochrane Database Syst Rev. 2011;(6):CD003935.
11. Lyon A. Chronic lung disease of prematurity. The role of intrauterine infection. Eur J Pediatr. 2000;159(11):798–802.
12. Vidaeff AC, Ramin SM. Antenatal corticosteroids after preterm premature rupture of membranes. Clin Obstet Gynecol. 2011;54(2):337–343.
13. Bailar JC. How to distort the scientific record without actually lying: truth, and the arts of science. Eur J Oncol. 2006;11(4):217–224.
1. Wapner RJ, Sorokin Y, Thom EA, et al. Single versus weekly courses of antenatal corticosteroids: evaluation of safety and efficacy. Am J Obstet Gynecol. 2006;195(3):633–642.
2. Murphy KE, Hannah ME, Willan AR, et al; MACS Collaborative Group. Multiple Courses of Antenatal Corticosteroids for Preterm Birth (MACS): a randomized controlled trial. Lancet. 2008;372(9656):2143–2151.
3. Garite TJ, Kurtzman, Maurel K, et al. Impact of a “rescue course” of antenatal corticosteroids: a multicenter randomized placebo-controlled trial. Am J Obstet Gynecol. 2009;200(3):248.e1–e9.
4. McEvoy C, Schilling D, Peters D, et al. Respiratory compliance in preterm infants after a single rescue course of antenatal steroids: a randomized controlled trial. Am J Obstet Gynecol. 2010;202(6):544.e1–e9.
5. Roberts D, Dalziel S. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2006;(3):CD004454.
6. Rotmensch S, Vishne TH, Celentano C, et al. Maternal infectious morbidity following multiple courses of betamethasone. J Infect. 1999;39(1):49–54.
7. Vermillion ST, Soper DE, Chasedunn-Roark J. Neonatal sepsis after betamethasone administration to patients with preterm premature rupture of membranes. Am J Obstet Gynecol. 1999;181(2):320–327.
8. Yang SH, Choi SJ, Roh CR, et al. Multiple courses of antenatal corticosteroid therapy in patients with preterm premature rupture of membranes. J Perinat Med. 2004;32(1):42–48.
9. Lee MJ, Davies J, Guinn D, et al. Single versus weekly courses of antenatal corticosteroids in preterm premature rupture of membranes. Obstet Gynecol. 2004;103(2):274–281.
10. Crowther CA, McKinlay CJ, Middleton P, Harding JE. Repeat doses of prenatal corticosteroids for women at risk of preterm birth for improving neonatal health outcomes. Cochrane Database Syst Rev. 2011;(6):CD003935.
11. Lyon A. Chronic lung disease of prematurity. The role of intrauterine infection. Eur J Pediatr. 2000;159(11):798–802.
12. Vidaeff AC, Ramin SM. Antenatal corticosteroids after preterm premature rupture of membranes. Clin Obstet Gynecol. 2011;54(2):337–343.
13. Bailar JC. How to distort the scientific record without actually lying: truth, and the arts of science. Eur J Oncol. 2006;11(4):217–224.
Which perioperative strategies for transvaginal cervical cerclage are backed by data?
In contemporary medical practice, we expect our clinical actions to reflect the best and most current evidence. In many cases, however, the evidence available to us is weak or irrelevant. In their investigation, Berghella and colleagues set out to assess the quality of evidence in the setting of transvaginal cervical cerclage by reviewing the published data on selected perioperative strategies. They elected to perform a systematic review, as opposed to a narrative review (a simple opinion piece), because this approach follows an explicit process designed to limit bias and random error in the interpretation of scientific research.
The studies they analyzed vary from observational investigations to randomized trials, generating considerable heterogeneity in the data. Therefore, it would not have been feasible or appropriate for them to combine the results in a quantitative review (ie, meta-analysis). Their solution: to limit the analysis to a qualitative systematic review.
The term “systematic review” implies that investigators have an accurate and comprehensive understanding of existent data, with each study representing one contribution to a much larger body of knowledge. Over the years, Berghella and colleagues have contributed extensively to the literature on cervical cerclage and are well qualified to provide an analytic framework for the flood of published information on this practice. Although they focused primarily on how to perform cerclage, a discussion of when to perform cerclage cannot be separated from any consideration of efficacy.
When, exactly, is cerclage indicated?
The original indication for cerclage, established more than 50 years ago, required both a history of second-trimester loss and asymptomatic cervical changes in the current pregnancy. Since then, many cerclages have been performed on the basis of history alone or on current cervical changes regardless of history. However, the most recent professional guidelines reconfirm that any cerclage procedure should be supported by both historical and contemporaneous findings.1,2
Investigators have demonstrated that the measurement of cervical length by transvaginal ultrasound should generally be an integral part of clinical evaluation for asymptomatic cervical changes. Indeed, sonographic assessment has emerged as a tool capable of reducing “overcall” and unnecessary intervention.3 On the other hand, a meta-analysis of four randomized trials of ultrasound-indicated cerclage found it to be beneficial in women with a short cervix only if they also had a history of preterm delivery.4
In addition, randomized trials have documented a benefit for cerclage in two other clinical contexts:
- Results from a secondary analysis of data from a large randomized trial published in 1993 suggest that elective cerclage can be based on history alone in women with three or more second-trimester losses or preterm births.5
- Authors of a randomized trial published in 2003 suggested that women with advanced cervical changes, such as dilatation of the external os with exposure of the fetal membranes, may benefit from “emergency” cerclage even in the absence of a prior preterm delivery.6
How the data were analyzed
The data included in the review were analyzed separately, according to three widely accepted indications for cerclage:
- history-indicated: a history of three or more second-trimester losses and/or preterm births
- ultrasound-indicated: ultrasonographic detection of a cervical length of less than 25 mm, as measured by transvaginal ultrasound, in a woman with a history of second-trimester loss or preterm birth
- physical-examination–indicated: physical examination (manual or with a speculum) that confirms a dilated cervix.
Granted, this terminology can be confusing, as in the case of ultrasound-indicated cerclage, which includes aspects of the patient’s history. Moreover, I doubt that the studies included in this analysis always adhered to these definitions. The heterogeneity of the study population and the ambiguity of these definitions may limit the applicability of findings. In fact, they constitute the major (albeit practically unavoidable) limitation of this review.
The optimal approach to subclinical infection is unclear
Although there is a consensus that overt intra-amniotic infection is an absolute contraindication to cerclage, the implications of subclinical intra-amniotic infection in asymptomatic women are unclear. About 50% of women considered for emergency cerclage are likely to have intra-amniotic infection.7 An ongoing randomized trial is expected to elucidate the benefit of precerclage amniocentesis in such cases.
The sonographic detection of sludge in the amniotic fluid also has been associated with intra-amniotic infection. However, after analyzing the data, Berghella and colleagues did not find adequate justification for amniocentesis in this setting. A more practical question might be whether cerclage is advisable at all when sludge is present. Data from a recently reported abstract suggest that the presence of sludge increases the likelihood of early preterm birth independent of cervical length.8
Other gray areas
Another absolute contraindication to cerclage is the presence of painful uterine contractions in a woman exhibiting cervical change. The study findings seemed to imply that when uterine contractions are detected via tocodynamometric monitoring but are not experienced by the patient, cerclage may be appropriate. In my opinion, this issue represents another open clinical question.
On at least one occasion, I have discovered that the patient scheduled for cerclage has not undergone preoperative screening for genital tract infections. In such a scenario, it is unclear whether it is best to cancel the procedure or to proceed. Berghella and colleagues concluded that evidence is insufficient to support routine, universal screening for genital tract infection prior to cerclage. In the absence of risk factors for infection, it may be appropriate to proceed with cerclage.
The issue of combined use of cerclage and 17α hydroxyprogesterone caproate also was addressed in this review. Berghella and colleagues recommended that progestin supplementation be continued if cerclage is subsequently performed. I, too, follow this approach, although the two interventions (progestin followed by cerclage) have not been studied in this sequence.
Related article: A stepwise approach to cervical cerclage (June 2012)
Data are limited, and conflicting, on the use of 17α hydroxyprogesterone caproate after cerclage. A small randomized trial suggested benefit,9 while a retrospective cohort study10 and a secondary analysis of data from a randomized trial of cerclage11 found no benefit for the addition of 17α hydroxyprogesterone caproate.
Berghella and colleagues advocated against reinforcing (second or repeat) cerclage, an intervention that may be associated with a higher incidence of preterm birth.12 Accordingly, continuing sonographic assessment of cervical length after cerclage may be futile. What this evidence means for practice
Increasing evidence suggests that cervical shortening is not limited to an innate or acquired cervical weakness but represents an early, asymptomatic phase on the pathway to preterm birth. Nevertheless, cerclage continues to be practiced widely and has been shown to be beneficial in selected populations.
We clinicians often face complex cases of presumed cervical insufficiency for which there are no simple or unequivocal recommendations. This appraisal by Berghella and colleagues will help us separate evidence-validated approaches from misconceptions in the technical aspects of cerclage.
--Alex C. Vidaeff, MD, MPH
We want to hear from you! Tell us what you think.
- Royal College of Obstetricians and Gynaecologists. Cervical cerclage [guidelines]. http://www.rcog.org.uk/womens-health/clinical-guidance/cervical-cerclage-green-top-60. Accessed September 18, 2013.
- ACOG Practice Bulletin #130: Prediction and prevention of preterm birth. Obstet Gynecol. 2012;120:964–973.
- Grimes-Dennis J, Berghella V. Cervical length and prediction of preterm delivery. Curr Opin Obstet Gynecol. 2007;19(2):191–195.
- Berghella V, Odibo AO, To MS, et al. Cerclage for short cervix on ultrasound: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
- Working Party on Cervical Cerclage. Final report of the Medical Research Council/Royal College of Obstetricians and Gynaecologists multicenter randomised trial of cervical cerclage. Br J Obstet Gynaecol. 1993;100(6):516–523.
- Althuisius SM, Dekker GA, Hummel P, van Geijin HP. Cervical incompetence prevention randomized cerclage trial: emergency cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2003;189(4):907–910.
- Romero R, Gonzalez R, Sepulveda W, et al. Infection and labor. VIII. Microbial invasion of the amniotic cavity in patients with suspected cervical incompetence: prevalence and clinical significance. Am J Obstet Gynecol. 1992(4 Pt 1);167:1086–1091.
- Saade G. Cervical funneling or intraamniotic debris and preterm birth in nulliparous women with short cervix. Am J Obstet Gynecol. 2013;208(1):S4.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574–577.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271–275.
- Berghella V, Figueroa D, Szychowski JM, et al. 17 alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1–e6.
- Baxter JK, Airoldi J, Berghella V. Short cervical length after history-indicated cerclage: is a reinforcing cerclage beneficial? Am J Obstet Gynecol. 2005;193(3 Pt 2):1204–1207.
In contemporary medical practice, we expect our clinical actions to reflect the best and most current evidence. In many cases, however, the evidence available to us is weak or irrelevant. In their investigation, Berghella and colleagues set out to assess the quality of evidence in the setting of transvaginal cervical cerclage by reviewing the published data on selected perioperative strategies. They elected to perform a systematic review, as opposed to a narrative review (a simple opinion piece), because this approach follows an explicit process designed to limit bias and random error in the interpretation of scientific research.
The studies they analyzed vary from observational investigations to randomized trials, generating considerable heterogeneity in the data. Therefore, it would not have been feasible or appropriate for them to combine the results in a quantitative review (ie, meta-analysis). Their solution: to limit the analysis to a qualitative systematic review.
The term “systematic review” implies that investigators have an accurate and comprehensive understanding of existent data, with each study representing one contribution to a much larger body of knowledge. Over the years, Berghella and colleagues have contributed extensively to the literature on cervical cerclage and are well qualified to provide an analytic framework for the flood of published information on this practice. Although they focused primarily on how to perform cerclage, a discussion of when to perform cerclage cannot be separated from any consideration of efficacy.
When, exactly, is cerclage indicated?
The original indication for cerclage, established more than 50 years ago, required both a history of second-trimester loss and asymptomatic cervical changes in the current pregnancy. Since then, many cerclages have been performed on the basis of history alone or on current cervical changes regardless of history. However, the most recent professional guidelines reconfirm that any cerclage procedure should be supported by both historical and contemporaneous findings.1,2
Investigators have demonstrated that the measurement of cervical length by transvaginal ultrasound should generally be an integral part of clinical evaluation for asymptomatic cervical changes. Indeed, sonographic assessment has emerged as a tool capable of reducing “overcall” and unnecessary intervention.3 On the other hand, a meta-analysis of four randomized trials of ultrasound-indicated cerclage found it to be beneficial in women with a short cervix only if they also had a history of preterm delivery.4
In addition, randomized trials have documented a benefit for cerclage in two other clinical contexts:
- Results from a secondary analysis of data from a large randomized trial published in 1993 suggest that elective cerclage can be based on history alone in women with three or more second-trimester losses or preterm births.5
- Authors of a randomized trial published in 2003 suggested that women with advanced cervical changes, such as dilatation of the external os with exposure of the fetal membranes, may benefit from “emergency” cerclage even in the absence of a prior preterm delivery.6
How the data were analyzed
The data included in the review were analyzed separately, according to three widely accepted indications for cerclage:
- history-indicated: a history of three or more second-trimester losses and/or preterm births
- ultrasound-indicated: ultrasonographic detection of a cervical length of less than 25 mm, as measured by transvaginal ultrasound, in a woman with a history of second-trimester loss or preterm birth
- physical-examination–indicated: physical examination (manual or with a speculum) that confirms a dilated cervix.
Granted, this terminology can be confusing, as in the case of ultrasound-indicated cerclage, which includes aspects of the patient’s history. Moreover, I doubt that the studies included in this analysis always adhered to these definitions. The heterogeneity of the study population and the ambiguity of these definitions may limit the applicability of findings. In fact, they constitute the major (albeit practically unavoidable) limitation of this review.
The optimal approach to subclinical infection is unclear
Although there is a consensus that overt intra-amniotic infection is an absolute contraindication to cerclage, the implications of subclinical intra-amniotic infection in asymptomatic women are unclear. About 50% of women considered for emergency cerclage are likely to have intra-amniotic infection.7 An ongoing randomized trial is expected to elucidate the benefit of precerclage amniocentesis in such cases.
The sonographic detection of sludge in the amniotic fluid also has been associated with intra-amniotic infection. However, after analyzing the data, Berghella and colleagues did not find adequate justification for amniocentesis in this setting. A more practical question might be whether cerclage is advisable at all when sludge is present. Data from a recently reported abstract suggest that the presence of sludge increases the likelihood of early preterm birth independent of cervical length.8
Other gray areas
Another absolute contraindication to cerclage is the presence of painful uterine contractions in a woman exhibiting cervical change. The study findings seemed to imply that when uterine contractions are detected via tocodynamometric monitoring but are not experienced by the patient, cerclage may be appropriate. In my opinion, this issue represents another open clinical question.
On at least one occasion, I have discovered that the patient scheduled for cerclage has not undergone preoperative screening for genital tract infections. In such a scenario, it is unclear whether it is best to cancel the procedure or to proceed. Berghella and colleagues concluded that evidence is insufficient to support routine, universal screening for genital tract infection prior to cerclage. In the absence of risk factors for infection, it may be appropriate to proceed with cerclage.
The issue of combined use of cerclage and 17α hydroxyprogesterone caproate also was addressed in this review. Berghella and colleagues recommended that progestin supplementation be continued if cerclage is subsequently performed. I, too, follow this approach, although the two interventions (progestin followed by cerclage) have not been studied in this sequence.
Related article: A stepwise approach to cervical cerclage (June 2012)
Data are limited, and conflicting, on the use of 17α hydroxyprogesterone caproate after cerclage. A small randomized trial suggested benefit,9 while a retrospective cohort study10 and a secondary analysis of data from a randomized trial of cerclage11 found no benefit for the addition of 17α hydroxyprogesterone caproate.
Berghella and colleagues advocated against reinforcing (second or repeat) cerclage, an intervention that may be associated with a higher incidence of preterm birth.12 Accordingly, continuing sonographic assessment of cervical length after cerclage may be futile. What this evidence means for practice
Increasing evidence suggests that cervical shortening is not limited to an innate or acquired cervical weakness but represents an early, asymptomatic phase on the pathway to preterm birth. Nevertheless, cerclage continues to be practiced widely and has been shown to be beneficial in selected populations.
We clinicians often face complex cases of presumed cervical insufficiency for which there are no simple or unequivocal recommendations. This appraisal by Berghella and colleagues will help us separate evidence-validated approaches from misconceptions in the technical aspects of cerclage.
--Alex C. Vidaeff, MD, MPH
We want to hear from you! Tell us what you think.
In contemporary medical practice, we expect our clinical actions to reflect the best and most current evidence. In many cases, however, the evidence available to us is weak or irrelevant. In their investigation, Berghella and colleagues set out to assess the quality of evidence in the setting of transvaginal cervical cerclage by reviewing the published data on selected perioperative strategies. They elected to perform a systematic review, as opposed to a narrative review (a simple opinion piece), because this approach follows an explicit process designed to limit bias and random error in the interpretation of scientific research.
The studies they analyzed vary from observational investigations to randomized trials, generating considerable heterogeneity in the data. Therefore, it would not have been feasible or appropriate for them to combine the results in a quantitative review (ie, meta-analysis). Their solution: to limit the analysis to a qualitative systematic review.
The term “systematic review” implies that investigators have an accurate and comprehensive understanding of existent data, with each study representing one contribution to a much larger body of knowledge. Over the years, Berghella and colleagues have contributed extensively to the literature on cervical cerclage and are well qualified to provide an analytic framework for the flood of published information on this practice. Although they focused primarily on how to perform cerclage, a discussion of when to perform cerclage cannot be separated from any consideration of efficacy.
When, exactly, is cerclage indicated?
The original indication for cerclage, established more than 50 years ago, required both a history of second-trimester loss and asymptomatic cervical changes in the current pregnancy. Since then, many cerclages have been performed on the basis of history alone or on current cervical changes regardless of history. However, the most recent professional guidelines reconfirm that any cerclage procedure should be supported by both historical and contemporaneous findings.1,2
Investigators have demonstrated that the measurement of cervical length by transvaginal ultrasound should generally be an integral part of clinical evaluation for asymptomatic cervical changes. Indeed, sonographic assessment has emerged as a tool capable of reducing “overcall” and unnecessary intervention.3 On the other hand, a meta-analysis of four randomized trials of ultrasound-indicated cerclage found it to be beneficial in women with a short cervix only if they also had a history of preterm delivery.4
In addition, randomized trials have documented a benefit for cerclage in two other clinical contexts:
- Results from a secondary analysis of data from a large randomized trial published in 1993 suggest that elective cerclage can be based on history alone in women with three or more second-trimester losses or preterm births.5
- Authors of a randomized trial published in 2003 suggested that women with advanced cervical changes, such as dilatation of the external os with exposure of the fetal membranes, may benefit from “emergency” cerclage even in the absence of a prior preterm delivery.6
How the data were analyzed
The data included in the review were analyzed separately, according to three widely accepted indications for cerclage:
- history-indicated: a history of three or more second-trimester losses and/or preterm births
- ultrasound-indicated: ultrasonographic detection of a cervical length of less than 25 mm, as measured by transvaginal ultrasound, in a woman with a history of second-trimester loss or preterm birth
- physical-examination–indicated: physical examination (manual or with a speculum) that confirms a dilated cervix.
Granted, this terminology can be confusing, as in the case of ultrasound-indicated cerclage, which includes aspects of the patient’s history. Moreover, I doubt that the studies included in this analysis always adhered to these definitions. The heterogeneity of the study population and the ambiguity of these definitions may limit the applicability of findings. In fact, they constitute the major (albeit practically unavoidable) limitation of this review.
The optimal approach to subclinical infection is unclear
Although there is a consensus that overt intra-amniotic infection is an absolute contraindication to cerclage, the implications of subclinical intra-amniotic infection in asymptomatic women are unclear. About 50% of women considered for emergency cerclage are likely to have intra-amniotic infection.7 An ongoing randomized trial is expected to elucidate the benefit of precerclage amniocentesis in such cases.
The sonographic detection of sludge in the amniotic fluid also has been associated with intra-amniotic infection. However, after analyzing the data, Berghella and colleagues did not find adequate justification for amniocentesis in this setting. A more practical question might be whether cerclage is advisable at all when sludge is present. Data from a recently reported abstract suggest that the presence of sludge increases the likelihood of early preterm birth independent of cervical length.8
Other gray areas
Another absolute contraindication to cerclage is the presence of painful uterine contractions in a woman exhibiting cervical change. The study findings seemed to imply that when uterine contractions are detected via tocodynamometric monitoring but are not experienced by the patient, cerclage may be appropriate. In my opinion, this issue represents another open clinical question.
On at least one occasion, I have discovered that the patient scheduled for cerclage has not undergone preoperative screening for genital tract infections. In such a scenario, it is unclear whether it is best to cancel the procedure or to proceed. Berghella and colleagues concluded that evidence is insufficient to support routine, universal screening for genital tract infection prior to cerclage. In the absence of risk factors for infection, it may be appropriate to proceed with cerclage.
The issue of combined use of cerclage and 17α hydroxyprogesterone caproate also was addressed in this review. Berghella and colleagues recommended that progestin supplementation be continued if cerclage is subsequently performed. I, too, follow this approach, although the two interventions (progestin followed by cerclage) have not been studied in this sequence.
Related article: A stepwise approach to cervical cerclage (June 2012)
Data are limited, and conflicting, on the use of 17α hydroxyprogesterone caproate after cerclage. A small randomized trial suggested benefit,9 while a retrospective cohort study10 and a secondary analysis of data from a randomized trial of cerclage11 found no benefit for the addition of 17α hydroxyprogesterone caproate.
Berghella and colleagues advocated against reinforcing (second or repeat) cerclage, an intervention that may be associated with a higher incidence of preterm birth.12 Accordingly, continuing sonographic assessment of cervical length after cerclage may be futile. What this evidence means for practice
Increasing evidence suggests that cervical shortening is not limited to an innate or acquired cervical weakness but represents an early, asymptomatic phase on the pathway to preterm birth. Nevertheless, cerclage continues to be practiced widely and has been shown to be beneficial in selected populations.
We clinicians often face complex cases of presumed cervical insufficiency for which there are no simple or unequivocal recommendations. This appraisal by Berghella and colleagues will help us separate evidence-validated approaches from misconceptions in the technical aspects of cerclage.
--Alex C. Vidaeff, MD, MPH
We want to hear from you! Tell us what you think.
- Royal College of Obstetricians and Gynaecologists. Cervical cerclage [guidelines]. http://www.rcog.org.uk/womens-health/clinical-guidance/cervical-cerclage-green-top-60. Accessed September 18, 2013.
- ACOG Practice Bulletin #130: Prediction and prevention of preterm birth. Obstet Gynecol. 2012;120:964–973.
- Grimes-Dennis J, Berghella V. Cervical length and prediction of preterm delivery. Curr Opin Obstet Gynecol. 2007;19(2):191–195.
- Berghella V, Odibo AO, To MS, et al. Cerclage for short cervix on ultrasound: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
- Working Party on Cervical Cerclage. Final report of the Medical Research Council/Royal College of Obstetricians and Gynaecologists multicenter randomised trial of cervical cerclage. Br J Obstet Gynaecol. 1993;100(6):516–523.
- Althuisius SM, Dekker GA, Hummel P, van Geijin HP. Cervical incompetence prevention randomized cerclage trial: emergency cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2003;189(4):907–910.
- Romero R, Gonzalez R, Sepulveda W, et al. Infection and labor. VIII. Microbial invasion of the amniotic cavity in patients with suspected cervical incompetence: prevalence and clinical significance. Am J Obstet Gynecol. 1992(4 Pt 1);167:1086–1091.
- Saade G. Cervical funneling or intraamniotic debris and preterm birth in nulliparous women with short cervix. Am J Obstet Gynecol. 2013;208(1):S4.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574–577.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271–275.
- Berghella V, Figueroa D, Szychowski JM, et al. 17 alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1–e6.
- Baxter JK, Airoldi J, Berghella V. Short cervical length after history-indicated cerclage: is a reinforcing cerclage beneficial? Am J Obstet Gynecol. 2005;193(3 Pt 2):1204–1207.
- Royal College of Obstetricians and Gynaecologists. Cervical cerclage [guidelines]. http://www.rcog.org.uk/womens-health/clinical-guidance/cervical-cerclage-green-top-60. Accessed September 18, 2013.
- ACOG Practice Bulletin #130: Prediction and prevention of preterm birth. Obstet Gynecol. 2012;120:964–973.
- Grimes-Dennis J, Berghella V. Cervical length and prediction of preterm delivery. Curr Opin Obstet Gynecol. 2007;19(2):191–195.
- Berghella V, Odibo AO, To MS, et al. Cerclage for short cervix on ultrasound: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106(1):181–189.
- Working Party on Cervical Cerclage. Final report of the Medical Research Council/Royal College of Obstetricians and Gynaecologists multicenter randomised trial of cervical cerclage. Br J Obstet Gynaecol. 1993;100(6):516–523.
- Althuisius SM, Dekker GA, Hummel P, van Geijin HP. Cervical incompetence prevention randomized cerclage trial: emergency cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol. 2003;189(4):907–910.
- Romero R, Gonzalez R, Sepulveda W, et al. Infection and labor. VIII. Microbial invasion of the amniotic cavity in patients with suspected cervical incompetence: prevalence and clinical significance. Am J Obstet Gynecol. 1992(4 Pt 1);167:1086–1091.
- Saade G. Cervical funneling or intraamniotic debris and preterm birth in nulliparous women with short cervix. Am J Obstet Gynecol. 2013;208(1):S4.
- Yemini M, Borenstein R, Dreazen E, et al. Prevention of premature labor by 17 alpha-hydroxyprogesterone caproate. Am J Obstet Gynecol. 1985;151(5):574–577.
- Rebarber A, Cleary-Goldman J, Istwan NB, et al. The use of 17 alpha-hydroxyprogesterone caproate (17P) in women with cervical cerclage. Am J Perinatol. 2008;25(5):271–275.
- Berghella V, Figueroa D, Szychowski JM, et al. 17 alpha-hydroxyprogesterone caproate for the prevention of preterm birth in women with prior preterm birth and a short cervical length. Am J Obstet Gynecol. 2010;202(4):351.e1–e6.
- Baxter JK, Airoldi J, Berghella V. Short cervical length after history-indicated cerclage: is a reinforcing cerclage beneficial? Am J Obstet Gynecol. 2005;193(3 Pt 2):1204–1207.
Does weekly progesterone prolong gestation in women who have PPROM?
Approximately 13 million preterm births occur annually worldwide.1 Depending on the geographic locale, PPROM is responsible for 16% to 40% of these births.2
The clinical approach to PPROM is one of the most contentious issues in obstetrics, with disagreement on virtually every aspect of it. Under debate are the lower and upper limits of the gestational age range at which intervention is warranted, as well as the use of ancillary interventions such as corticosteroids and antibiotics. Briery and colleagues add to the scientific debate now by asking whether 17P would be effective as cotreatment (with antibiotics) to prolong latency after PPROM.
According to their findings, the answer to this question is “No.”
Details of the trial
Briery and colleagues conducted a placebo-controlled, double-blind, randomized clinical trial of women with a singleton gestation complicated by PPROM. Excluded from the study were women whose pregnancy involved additional fetal or placental complications.
All women included in the study received antibiotics according to a protocol from the National Institutes of Health; they also were given betamethasone for fetal maturation. Tocolytics were not used. Because randomization did not occur until after each woman was transferred from the labor and delivery unit to the high-risk floor, we can assume that no participants were manifesting uterine contractions.
Women received weekly injections of 17P or placebo until 34 weeks’ gestation or delivery. The primary outcome was the interval from study entry to delivery.
One woman had a pregnancy of 23.5 weeks’ duration at randomization; the remainder had gestations that were 24 weeks or older. There were no other differences in demographics, cervical dilatation, gestational age at study entry, or reasons for delivery between the two study groups.
Study design may have been unrealistic
The authors calculated that they needed a sample size of 56 patients to detect a 50% increase in latency, based on population data from their institution showing that 80% of patients who have PPROM deliver within 7 days. Such a calculation may have set an unrealistic—albeit logistically convenient—goal, rendering the study underpowered to detect smaller effects. Note, for example, that when antibiotics are given to women who have PPROM, prolongation of the latency period is only 33% (pooled effect from a recent meta-analysis).3 Even so, given the findings of Briery and colleagues, latency improvement after 17P administration would appear to be unlikely even in a larger study. There was not even a trend toward a longer interval to delivery (mean of 11.2 days with 17P vs 14.5 days with placebo).
Only secondary prevention of preterm birth is effective
The indications for progesterone supplementation in pregnancy are still evolving as part of a sustained scientific effort to prevent preterm labor and delivery. Strategies to prevent preterm delivery can be categorized as primary, secondary, or tertiary, as can strategies for other public health concerns.
Because any number of variables—known and unknown—may trigger preterm labor, identifying them and providing primary preventive strategies in the entire pregnant population remain elusive tasks.
Tertiary prevention—i.e., treatment given to already symptomatic individuals—is also notoriously ineffective. There are no data supporting the use of progesterone as primary prevention (in low-risk women) or tertiary prevention (e.g., tocolytic). ACOG made note of this in 2003, and its conclusions remain valid today.4 According to a 2010 Cochrane review, there is insufficient evidence to advocate progestational agents as tocolytic agents for women who present with threatened or established preterm labor.5
In light of these data, the results reported by Briery and colleagues are hardly surprising. In women who may have already entered the irreversible phase of parturition (manifesting uterine contractions; presenting with advanced, painless cervical dilatation; or after PPROM), progesterone will remain ineffective. The only applicable use of prophylactic progesterone in pregnancy is as secondary prevention.4 In contrast to primary and tertiary prevention, the secondary level of prevention—i.e., an intervention aimed at minimizing the risk of preterm birth in women who are identified as having an elevated risk—is supported by several systematic reviews of randomized, controlled trials.6,7 According to these reviews, progesterone certainly is effective in high-risk pregnant women who have a short cervix or a history of spontaneous preterm birth. The same cannot be said about women who have PPROM.
Based on the evidence, including this study by Briery and colleagues, administration of antibiotics appears to be the only intervention available to delay delivery and reduce neonatal morbidity in the setting of PPROM.8 The use of tocolytics is not supported by the data in the clinical context of PPROM.9—Alex C. Vidaeff, MD, MPH
We want to hear from you! Tell us what you think.
1. Villar J, Abalos E, Carroli G, et al. Heterogeneity of perinatal outcomes in the preterm delivery syndrome. Obstet Gynecol. 2004;104(1):78-87.
2. Simmons LE, Rubens CE, Darmstadt GL, et al. Preventing preterm birth and neonatal mortality: exploring the epidemiology, causes, and interventions. Semin Perinatol. 2010;34(6):408-415.
3. Hutzal CE, Boyle EM, Kenyon SL, et al. Use of antibiotics for the treatment of preterm parturition and prevention of neonatal morbidity: a meta-analysis. Am J Obstet Gynecol. 2008;199(6):620.e1-8.
4. Society for Maternal Fetal Medicine Publications Committee. ACOG Committee Opinion #419. Use of progesterone to reduce preterm birth. Obstet Gynecol. 2008;112(4):963-965.
5. Su L-L, Samuel M, Chong Y-S. Progestational agents for treating threatened or established preterm labor. Cochrane Database Syst Rev. 2010;(1):CD006770.-doi: 10.1002/14651858.CD006770.
6. Dodd JM, Crowther CA. The role of progesterone in prevention of preterm birth. Int J Women Health. 2010;1:73-84.
7. Rode L, Langhoff-Roos J, Andersson C, et al. Systematic review of progesterone for the prevention of preterm birth in singleton pregnancies. Acta Obstet Gynecol Scand. 2009;88(11):1180-1189.
8. Kenyon S, Boulvain M, Neilson JP. Antibiotics for preterm rupture of membranes. Cochrane Database Syst Rev. 2003;(2):CD001058.-doi: 10.1002/14651858.CD001058.
9. Mercer BM. Is there a role for tocolytic therapy during conservative management of preterm premature rupture of the membranes? Clin Obstet Gynecol. 2007;50(2):487-496.
Approximately 13 million preterm births occur annually worldwide.1 Depending on the geographic locale, PPROM is responsible for 16% to 40% of these births.2
The clinical approach to PPROM is one of the most contentious issues in obstetrics, with disagreement on virtually every aspect of it. Under debate are the lower and upper limits of the gestational age range at which intervention is warranted, as well as the use of ancillary interventions such as corticosteroids and antibiotics. Briery and colleagues add to the scientific debate now by asking whether 17P would be effective as cotreatment (with antibiotics) to prolong latency after PPROM.
According to their findings, the answer to this question is “No.”
Details of the trial
Briery and colleagues conducted a placebo-controlled, double-blind, randomized clinical trial of women with a singleton gestation complicated by PPROM. Excluded from the study were women whose pregnancy involved additional fetal or placental complications.
All women included in the study received antibiotics according to a protocol from the National Institutes of Health; they also were given betamethasone for fetal maturation. Tocolytics were not used. Because randomization did not occur until after each woman was transferred from the labor and delivery unit to the high-risk floor, we can assume that no participants were manifesting uterine contractions.
Women received weekly injections of 17P or placebo until 34 weeks’ gestation or delivery. The primary outcome was the interval from study entry to delivery.
One woman had a pregnancy of 23.5 weeks’ duration at randomization; the remainder had gestations that were 24 weeks or older. There were no other differences in demographics, cervical dilatation, gestational age at study entry, or reasons for delivery between the two study groups.
Study design may have been unrealistic
The authors calculated that they needed a sample size of 56 patients to detect a 50% increase in latency, based on population data from their institution showing that 80% of patients who have PPROM deliver within 7 days. Such a calculation may have set an unrealistic—albeit logistically convenient—goal, rendering the study underpowered to detect smaller effects. Note, for example, that when antibiotics are given to women who have PPROM, prolongation of the latency period is only 33% (pooled effect from a recent meta-analysis).3 Even so, given the findings of Briery and colleagues, latency improvement after 17P administration would appear to be unlikely even in a larger study. There was not even a trend toward a longer interval to delivery (mean of 11.2 days with 17P vs 14.5 days with placebo).
Only secondary prevention of preterm birth is effective
The indications for progesterone supplementation in pregnancy are still evolving as part of a sustained scientific effort to prevent preterm labor and delivery. Strategies to prevent preterm delivery can be categorized as primary, secondary, or tertiary, as can strategies for other public health concerns.
Because any number of variables—known and unknown—may trigger preterm labor, identifying them and providing primary preventive strategies in the entire pregnant population remain elusive tasks.
Tertiary prevention—i.e., treatment given to already symptomatic individuals—is also notoriously ineffective. There are no data supporting the use of progesterone as primary prevention (in low-risk women) or tertiary prevention (e.g., tocolytic). ACOG made note of this in 2003, and its conclusions remain valid today.4 According to a 2010 Cochrane review, there is insufficient evidence to advocate progestational agents as tocolytic agents for women who present with threatened or established preterm labor.5
In light of these data, the results reported by Briery and colleagues are hardly surprising. In women who may have already entered the irreversible phase of parturition (manifesting uterine contractions; presenting with advanced, painless cervical dilatation; or after PPROM), progesterone will remain ineffective. The only applicable use of prophylactic progesterone in pregnancy is as secondary prevention.4 In contrast to primary and tertiary prevention, the secondary level of prevention—i.e., an intervention aimed at minimizing the risk of preterm birth in women who are identified as having an elevated risk—is supported by several systematic reviews of randomized, controlled trials.6,7 According to these reviews, progesterone certainly is effective in high-risk pregnant women who have a short cervix or a history of spontaneous preterm birth. The same cannot be said about women who have PPROM.
Based on the evidence, including this study by Briery and colleagues, administration of antibiotics appears to be the only intervention available to delay delivery and reduce neonatal morbidity in the setting of PPROM.8 The use of tocolytics is not supported by the data in the clinical context of PPROM.9—Alex C. Vidaeff, MD, MPH
We want to hear from you! Tell us what you think.
Approximately 13 million preterm births occur annually worldwide.1 Depending on the geographic locale, PPROM is responsible for 16% to 40% of these births.2
The clinical approach to PPROM is one of the most contentious issues in obstetrics, with disagreement on virtually every aspect of it. Under debate are the lower and upper limits of the gestational age range at which intervention is warranted, as well as the use of ancillary interventions such as corticosteroids and antibiotics. Briery and colleagues add to the scientific debate now by asking whether 17P would be effective as cotreatment (with antibiotics) to prolong latency after PPROM.
According to their findings, the answer to this question is “No.”
Details of the trial
Briery and colleagues conducted a placebo-controlled, double-blind, randomized clinical trial of women with a singleton gestation complicated by PPROM. Excluded from the study were women whose pregnancy involved additional fetal or placental complications.
All women included in the study received antibiotics according to a protocol from the National Institutes of Health; they also were given betamethasone for fetal maturation. Tocolytics were not used. Because randomization did not occur until after each woman was transferred from the labor and delivery unit to the high-risk floor, we can assume that no participants were manifesting uterine contractions.
Women received weekly injections of 17P or placebo until 34 weeks’ gestation or delivery. The primary outcome was the interval from study entry to delivery.
One woman had a pregnancy of 23.5 weeks’ duration at randomization; the remainder had gestations that were 24 weeks or older. There were no other differences in demographics, cervical dilatation, gestational age at study entry, or reasons for delivery between the two study groups.
Study design may have been unrealistic
The authors calculated that they needed a sample size of 56 patients to detect a 50% increase in latency, based on population data from their institution showing that 80% of patients who have PPROM deliver within 7 days. Such a calculation may have set an unrealistic—albeit logistically convenient—goal, rendering the study underpowered to detect smaller effects. Note, for example, that when antibiotics are given to women who have PPROM, prolongation of the latency period is only 33% (pooled effect from a recent meta-analysis).3 Even so, given the findings of Briery and colleagues, latency improvement after 17P administration would appear to be unlikely even in a larger study. There was not even a trend toward a longer interval to delivery (mean of 11.2 days with 17P vs 14.5 days with placebo).
Only secondary prevention of preterm birth is effective
The indications for progesterone supplementation in pregnancy are still evolving as part of a sustained scientific effort to prevent preterm labor and delivery. Strategies to prevent preterm delivery can be categorized as primary, secondary, or tertiary, as can strategies for other public health concerns.
Because any number of variables—known and unknown—may trigger preterm labor, identifying them and providing primary preventive strategies in the entire pregnant population remain elusive tasks.
Tertiary prevention—i.e., treatment given to already symptomatic individuals—is also notoriously ineffective. There are no data supporting the use of progesterone as primary prevention (in low-risk women) or tertiary prevention (e.g., tocolytic). ACOG made note of this in 2003, and its conclusions remain valid today.4 According to a 2010 Cochrane review, there is insufficient evidence to advocate progestational agents as tocolytic agents for women who present with threatened or established preterm labor.5
In light of these data, the results reported by Briery and colleagues are hardly surprising. In women who may have already entered the irreversible phase of parturition (manifesting uterine contractions; presenting with advanced, painless cervical dilatation; or after PPROM), progesterone will remain ineffective. The only applicable use of prophylactic progesterone in pregnancy is as secondary prevention.4 In contrast to primary and tertiary prevention, the secondary level of prevention—i.e., an intervention aimed at minimizing the risk of preterm birth in women who are identified as having an elevated risk—is supported by several systematic reviews of randomized, controlled trials.6,7 According to these reviews, progesterone certainly is effective in high-risk pregnant women who have a short cervix or a history of spontaneous preterm birth. The same cannot be said about women who have PPROM.
Based on the evidence, including this study by Briery and colleagues, administration of antibiotics appears to be the only intervention available to delay delivery and reduce neonatal morbidity in the setting of PPROM.8 The use of tocolytics is not supported by the data in the clinical context of PPROM.9—Alex C. Vidaeff, MD, MPH
We want to hear from you! Tell us what you think.
1. Villar J, Abalos E, Carroli G, et al. Heterogeneity of perinatal outcomes in the preterm delivery syndrome. Obstet Gynecol. 2004;104(1):78-87.
2. Simmons LE, Rubens CE, Darmstadt GL, et al. Preventing preterm birth and neonatal mortality: exploring the epidemiology, causes, and interventions. Semin Perinatol. 2010;34(6):408-415.
3. Hutzal CE, Boyle EM, Kenyon SL, et al. Use of antibiotics for the treatment of preterm parturition and prevention of neonatal morbidity: a meta-analysis. Am J Obstet Gynecol. 2008;199(6):620.e1-8.
4. Society for Maternal Fetal Medicine Publications Committee. ACOG Committee Opinion #419. Use of progesterone to reduce preterm birth. Obstet Gynecol. 2008;112(4):963-965.
5. Su L-L, Samuel M, Chong Y-S. Progestational agents for treating threatened or established preterm labor. Cochrane Database Syst Rev. 2010;(1):CD006770.-doi: 10.1002/14651858.CD006770.
6. Dodd JM, Crowther CA. The role of progesterone in prevention of preterm birth. Int J Women Health. 2010;1:73-84.
7. Rode L, Langhoff-Roos J, Andersson C, et al. Systematic review of progesterone for the prevention of preterm birth in singleton pregnancies. Acta Obstet Gynecol Scand. 2009;88(11):1180-1189.
8. Kenyon S, Boulvain M, Neilson JP. Antibiotics for preterm rupture of membranes. Cochrane Database Syst Rev. 2003;(2):CD001058.-doi: 10.1002/14651858.CD001058.
9. Mercer BM. Is there a role for tocolytic therapy during conservative management of preterm premature rupture of the membranes? Clin Obstet Gynecol. 2007;50(2):487-496.
1. Villar J, Abalos E, Carroli G, et al. Heterogeneity of perinatal outcomes in the preterm delivery syndrome. Obstet Gynecol. 2004;104(1):78-87.
2. Simmons LE, Rubens CE, Darmstadt GL, et al. Preventing preterm birth and neonatal mortality: exploring the epidemiology, causes, and interventions. Semin Perinatol. 2010;34(6):408-415.
3. Hutzal CE, Boyle EM, Kenyon SL, et al. Use of antibiotics for the treatment of preterm parturition and prevention of neonatal morbidity: a meta-analysis. Am J Obstet Gynecol. 2008;199(6):620.e1-8.
4. Society for Maternal Fetal Medicine Publications Committee. ACOG Committee Opinion #419. Use of progesterone to reduce preterm birth. Obstet Gynecol. 2008;112(4):963-965.
5. Su L-L, Samuel M, Chong Y-S. Progestational agents for treating threatened or established preterm labor. Cochrane Database Syst Rev. 2010;(1):CD006770.-doi: 10.1002/14651858.CD006770.
6. Dodd JM, Crowther CA. The role of progesterone in prevention of preterm birth. Int J Women Health. 2010;1:73-84.
7. Rode L, Langhoff-Roos J, Andersson C, et al. Systematic review of progesterone for the prevention of preterm birth in singleton pregnancies. Acta Obstet Gynecol Scand. 2009;88(11):1180-1189.
8. Kenyon S, Boulvain M, Neilson JP. Antibiotics for preterm rupture of membranes. Cochrane Database Syst Rev. 2003;(2):CD001058.-doi: 10.1002/14651858.CD001058.
9. Mercer BM. Is there a role for tocolytic therapy during conservative management of preterm premature rupture of the membranes? Clin Obstet Gynecol. 2007;50(2):487-496.
Are a short cervix and a history of preterm birth absolute indications for cervical cerclage?
- 1) a history of second-trimester loss involving painless cervical dilatation in the absence of infection, bleeding, amniorrhexis, and fetal demise
- 2) asymptomatic cervical changes in the current pregnancy.
Although our understanding of cervical insufficiency has undergone many revisions and reinterpretations in the intervening years, we still lack an accepted diagnostic test or proven criteria for diagnosis. Cerclage is placed in 1% of all pregnancies in the United States, but there is no consensus on indications, and the effectiveness is still a matter of debate.1 Cerclage placement based on ultrasonographic (US) measurement of cervical length has been proposed as the solution to this clinical quagmire, in the wake of evidence suggesting that cervical length may act as a surrogate for cervical competence.
A patient-level meta-analysis of four randomized trials of cervical cerclage, published in 2005, reconfirmed the original indication for cerclage. In women who had a cervical length below 25 mm, cerclage reduced the rate of preterm birth at less than 35 weeks’ gestation only if they had a history of preterm birth.2 This finding prompted the question: Would such women represent a truly homogeneous population in terms of therapeutic response to cerclage?
The Owen trial attempts to answer this specific question.
Details of the trial
Women who had a cervix shorter than 25 mm and a history of preterm birth and who were pregnant with a singleton gestation were eligible. Candidates for elective cerclage based on history, or for emergency cerclage based on cervical dilatation of at least 2 cm with visible membranes, were excluded from the study—possibly reducing the generalizability of the findings.
For the remaining 302 participants, cerclage appeared to have an overall benefit when survival analysis took the duration of gestation into consideration. But only women who had a cervical length below 15 mm had a significant reduction in the primary outcome (preterm birth at less than 35 weeks’ gestation) with cerclage. These results are somewhat reminiscent of the findings of a randomized comparison of cerclage and 17α-hydroxyprogesterone caproate in women who had a short cervix (measured by US), in which cerclage proved to be superior only when cervical length was less than 15 mm.3
Why the 15-mm cutoff isn’t definitive
Despite these findings, the 15-mm measurement cannot be assumed to be completely prescriptive because it was selected somewhat arbitrarily. Furthermore, it may be inadvisable to wait for cervical length to decrease below 15 mm. In pregnancies in which cervical length is below 5 mm, there is a significantly higher expression of intra-amniotic inflammation than in those in which cervical length is 6 to 25 mm, according to another recent study.4 Women who have a very short cervix may be far along the inflammatory cascade and may have already entered the irreversible phase of parturition, reducing the efficacy and even the advisability of cerclage. A positive fetal fibronectin test (as a marker of inflammation and choriodecidual disruption) and an increased level of interleukin-8 in cervical mucus reportedly identified a subgroup of women with a short cervix who would not benefit from cerclage—and who might even be harmed by it.5,6
Because preterm birth is such a complex disorder, it is unlikely that one intervention will be effective in all women—even within a certain stratum of cervical length. Rather, it may be necessary to identify subsets of pregnant women amenable to targeted or tailored intervention.
Ultrasonographic surveillance of cervical length can provide you with useful information when a woman who has a history of spontaneous preterm birth at less than 34 weeks’ gestation is pregnant with a singleton gestation. Serial sonographic surveillance of cervical length may be conducted every 1 to 2 weeks, between 16 and 24 weeks’ gestation. This approach may help identify the candidate likely to benefit from cerclage and may prevent unnecessary surgical intervention in another. Do not place cerclage “just in case”; it may benefit some gravidas but harm others.
Emerging evidence appears to show that only women who have historical risk factors plus a short cervix (—ALEX C. VIDAEFF, MD, MPH
1. Berghella V, Seibel-Seamon J. Contemporary use of cervical cerclage. Clin Obstet Gynecol. 2007;50:468-477.
2. Berghella V, Odibo AO, To MS, Rust OA, Athuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106:181-189.
3. Keeler SM, Kiefer D, Rochon M, Quinones JN, Novetsky AP, Rust O. A randomized trial of cerclage vs 17 alpha-hydroxyprogesterone caproate for treatment of short cervix. J Perinat Med. 2009;37:473-479.
4. Kiefer DG, Keeler SM, Rust OA, Wayock CP, Vintzileos AM, Hanna N. Is midtrimester short cervix a sign of intraamniotic inflammation? Am J Obstet Gynecol. 2009;200:374.e1-374.e5.
5. Keeler SM, Roman AS, Coletta JM, Kiefer DG, Feuerman M, Rust OA. Fetal fibronectin testing in patients with short cervix in the midtrimester: can it identify optimal candidates for ultrasound-indicated cerclage? Am J Obstet Gynecol. 2009;200:158.e1-158.e6.
6. Sakai M, Shiozaki A, Tabata M, et al. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol. 2006;194:14-19.
- 1) a history of second-trimester loss involving painless cervical dilatation in the absence of infection, bleeding, amniorrhexis, and fetal demise
- 2) asymptomatic cervical changes in the current pregnancy.
Although our understanding of cervical insufficiency has undergone many revisions and reinterpretations in the intervening years, we still lack an accepted diagnostic test or proven criteria for diagnosis. Cerclage is placed in 1% of all pregnancies in the United States, but there is no consensus on indications, and the effectiveness is still a matter of debate.1 Cerclage placement based on ultrasonographic (US) measurement of cervical length has been proposed as the solution to this clinical quagmire, in the wake of evidence suggesting that cervical length may act as a surrogate for cervical competence.
A patient-level meta-analysis of four randomized trials of cervical cerclage, published in 2005, reconfirmed the original indication for cerclage. In women who had a cervical length below 25 mm, cerclage reduced the rate of preterm birth at less than 35 weeks’ gestation only if they had a history of preterm birth.2 This finding prompted the question: Would such women represent a truly homogeneous population in terms of therapeutic response to cerclage?
The Owen trial attempts to answer this specific question.
Details of the trial
Women who had a cervix shorter than 25 mm and a history of preterm birth and who were pregnant with a singleton gestation were eligible. Candidates for elective cerclage based on history, or for emergency cerclage based on cervical dilatation of at least 2 cm with visible membranes, were excluded from the study—possibly reducing the generalizability of the findings.
For the remaining 302 participants, cerclage appeared to have an overall benefit when survival analysis took the duration of gestation into consideration. But only women who had a cervical length below 15 mm had a significant reduction in the primary outcome (preterm birth at less than 35 weeks’ gestation) with cerclage. These results are somewhat reminiscent of the findings of a randomized comparison of cerclage and 17α-hydroxyprogesterone caproate in women who had a short cervix (measured by US), in which cerclage proved to be superior only when cervical length was less than 15 mm.3
Why the 15-mm cutoff isn’t definitive
Despite these findings, the 15-mm measurement cannot be assumed to be completely prescriptive because it was selected somewhat arbitrarily. Furthermore, it may be inadvisable to wait for cervical length to decrease below 15 mm. In pregnancies in which cervical length is below 5 mm, there is a significantly higher expression of intra-amniotic inflammation than in those in which cervical length is 6 to 25 mm, according to another recent study.4 Women who have a very short cervix may be far along the inflammatory cascade and may have already entered the irreversible phase of parturition, reducing the efficacy and even the advisability of cerclage. A positive fetal fibronectin test (as a marker of inflammation and choriodecidual disruption) and an increased level of interleukin-8 in cervical mucus reportedly identified a subgroup of women with a short cervix who would not benefit from cerclage—and who might even be harmed by it.5,6
Because preterm birth is such a complex disorder, it is unlikely that one intervention will be effective in all women—even within a certain stratum of cervical length. Rather, it may be necessary to identify subsets of pregnant women amenable to targeted or tailored intervention.
Ultrasonographic surveillance of cervical length can provide you with useful information when a woman who has a history of spontaneous preterm birth at less than 34 weeks’ gestation is pregnant with a singleton gestation. Serial sonographic surveillance of cervical length may be conducted every 1 to 2 weeks, between 16 and 24 weeks’ gestation. This approach may help identify the candidate likely to benefit from cerclage and may prevent unnecessary surgical intervention in another. Do not place cerclage “just in case”; it may benefit some gravidas but harm others.
Emerging evidence appears to show that only women who have historical risk factors plus a short cervix (—ALEX C. VIDAEFF, MD, MPH
- 1) a history of second-trimester loss involving painless cervical dilatation in the absence of infection, bleeding, amniorrhexis, and fetal demise
- 2) asymptomatic cervical changes in the current pregnancy.
Although our understanding of cervical insufficiency has undergone many revisions and reinterpretations in the intervening years, we still lack an accepted diagnostic test or proven criteria for diagnosis. Cerclage is placed in 1% of all pregnancies in the United States, but there is no consensus on indications, and the effectiveness is still a matter of debate.1 Cerclage placement based on ultrasonographic (US) measurement of cervical length has been proposed as the solution to this clinical quagmire, in the wake of evidence suggesting that cervical length may act as a surrogate for cervical competence.
A patient-level meta-analysis of four randomized trials of cervical cerclage, published in 2005, reconfirmed the original indication for cerclage. In women who had a cervical length below 25 mm, cerclage reduced the rate of preterm birth at less than 35 weeks’ gestation only if they had a history of preterm birth.2 This finding prompted the question: Would such women represent a truly homogeneous population in terms of therapeutic response to cerclage?
The Owen trial attempts to answer this specific question.
Details of the trial
Women who had a cervix shorter than 25 mm and a history of preterm birth and who were pregnant with a singleton gestation were eligible. Candidates for elective cerclage based on history, or for emergency cerclage based on cervical dilatation of at least 2 cm with visible membranes, were excluded from the study—possibly reducing the generalizability of the findings.
For the remaining 302 participants, cerclage appeared to have an overall benefit when survival analysis took the duration of gestation into consideration. But only women who had a cervical length below 15 mm had a significant reduction in the primary outcome (preterm birth at less than 35 weeks’ gestation) with cerclage. These results are somewhat reminiscent of the findings of a randomized comparison of cerclage and 17α-hydroxyprogesterone caproate in women who had a short cervix (measured by US), in which cerclage proved to be superior only when cervical length was less than 15 mm.3
Why the 15-mm cutoff isn’t definitive
Despite these findings, the 15-mm measurement cannot be assumed to be completely prescriptive because it was selected somewhat arbitrarily. Furthermore, it may be inadvisable to wait for cervical length to decrease below 15 mm. In pregnancies in which cervical length is below 5 mm, there is a significantly higher expression of intra-amniotic inflammation than in those in which cervical length is 6 to 25 mm, according to another recent study.4 Women who have a very short cervix may be far along the inflammatory cascade and may have already entered the irreversible phase of parturition, reducing the efficacy and even the advisability of cerclage. A positive fetal fibronectin test (as a marker of inflammation and choriodecidual disruption) and an increased level of interleukin-8 in cervical mucus reportedly identified a subgroup of women with a short cervix who would not benefit from cerclage—and who might even be harmed by it.5,6
Because preterm birth is such a complex disorder, it is unlikely that one intervention will be effective in all women—even within a certain stratum of cervical length. Rather, it may be necessary to identify subsets of pregnant women amenable to targeted or tailored intervention.
Ultrasonographic surveillance of cervical length can provide you with useful information when a woman who has a history of spontaneous preterm birth at less than 34 weeks’ gestation is pregnant with a singleton gestation. Serial sonographic surveillance of cervical length may be conducted every 1 to 2 weeks, between 16 and 24 weeks’ gestation. This approach may help identify the candidate likely to benefit from cerclage and may prevent unnecessary surgical intervention in another. Do not place cerclage “just in case”; it may benefit some gravidas but harm others.
Emerging evidence appears to show that only women who have historical risk factors plus a short cervix (—ALEX C. VIDAEFF, MD, MPH
1. Berghella V, Seibel-Seamon J. Contemporary use of cervical cerclage. Clin Obstet Gynecol. 2007;50:468-477.
2. Berghella V, Odibo AO, To MS, Rust OA, Athuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106:181-189.
3. Keeler SM, Kiefer D, Rochon M, Quinones JN, Novetsky AP, Rust O. A randomized trial of cerclage vs 17 alpha-hydroxyprogesterone caproate for treatment of short cervix. J Perinat Med. 2009;37:473-479.
4. Kiefer DG, Keeler SM, Rust OA, Wayock CP, Vintzileos AM, Hanna N. Is midtrimester short cervix a sign of intraamniotic inflammation? Am J Obstet Gynecol. 2009;200:374.e1-374.e5.
5. Keeler SM, Roman AS, Coletta JM, Kiefer DG, Feuerman M, Rust OA. Fetal fibronectin testing in patients with short cervix in the midtrimester: can it identify optimal candidates for ultrasound-indicated cerclage? Am J Obstet Gynecol. 2009;200:158.e1-158.e6.
6. Sakai M, Shiozaki A, Tabata M, et al. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol. 2006;194:14-19.
1. Berghella V, Seibel-Seamon J. Contemporary use of cervical cerclage. Clin Obstet Gynecol. 2007;50:468-477.
2. Berghella V, Odibo AO, To MS, Rust OA, Athuisius SM. Cerclage for short cervix on ultrasonography: meta-analysis of trials using individual patient-level data. Obstet Gynecol. 2005;106:181-189.
3. Keeler SM, Kiefer D, Rochon M, Quinones JN, Novetsky AP, Rust O. A randomized trial of cerclage vs 17 alpha-hydroxyprogesterone caproate for treatment of short cervix. J Perinat Med. 2009;37:473-479.
4. Kiefer DG, Keeler SM, Rust OA, Wayock CP, Vintzileos AM, Hanna N. Is midtrimester short cervix a sign of intraamniotic inflammation? Am J Obstet Gynecol. 2009;200:374.e1-374.e5.
5. Keeler SM, Roman AS, Coletta JM, Kiefer DG, Feuerman M, Rust OA. Fetal fibronectin testing in patients with short cervix in the midtrimester: can it identify optimal candidates for ultrasound-indicated cerclage? Am J Obstet Gynecol. 2009;200:158.e1-158.e6.
6. Sakai M, Shiozaki A, Tabata M, et al. Evaluation of effectiveness of prophylactic cerclage of a short cervix according to interleukin-8 in cervical mucus. Am J Obstet Gynecol. 2006;194:14-19.
Fetal pulse oximetry: 8 vital questions
- The value of this new technology might not be so much the prediction of acidosis but identification of the well-oxygenated fetus so that labor may be safely continued in the presence of a concerning—but not ominous—fetal heart rate tracing.
- The only randomized study published so far did not determine whether clinical decisions can be based solely on fetal pulse oximetry. The investigators did suggest that sensitivity and specificity for metabolic acidemia was improved in the intervention group—a promising appraisal, in contrast with previous observational data.
When a teenage nullipara underwent labor induction for preeclampsia at 37 weeks, she was given epidural analgesia and seizure prophylaxis with magnesium sulfate. Her electronic fetal heart rate (FHR) tracing was initially reassuring, with only occasional variable decelerations, but subsequently revealed a baseline of 140 beats per minute (bpm), minimal to absent variability, no accelerations, and variable decelerations to 90 bpm with rapid return to baseline.
The tracing was interpreted as nonreassuring, and a fetal pulse oximeter was inserted. It revealed a fetal oxygen saturation rate between 45% and 50%, and labor was allowed to continue. After 3.5 hours in the second stage, the patient was delivered by outlet forceps. Her infant had Apgar scores of 8 at 1 minute and 9 at 5 minutes. The umbilical arterial pH was 7.25, and base excess was–4.9.
Fetal pulse oximetry made it possible to manage this case without resorting to emergent cesarean. But is this noninvasive technology truly a step forward in intrapartum assessment of fetal well-being?
We describe what the evidence (a single randomized study and a number of observational studies) reveals about these questions:
- How accurately does fetal pulse oximetry reflect the fetal condition?
- What is the critical threshold for fetal oxygen desaturation?
- Is a single reading reliable?
- Does oximetry correlate with acid-base status?
- Does the combination of oximetry and electronic monitoring improve accuracy?
- Will fetal pulse oximetry improve neonatal outcomes?
- How precise is it?
- Is it easy to use?
Needed: Effective adjunct to electronic monitoring
Except in the chronically hypoxic fetus (which is affected by the time labor begins), the pathophysiology of acute intrapartum events is a continuum, from hypoxemia to respiratory acidosis to metabolic acidosis and, ultimately, clinical impairment. The goal of intrapartum surveillance is to detect fetal hypoxemia before it progresses to asphyxia and perinatal mortality or long-term morbidity.
Although it is approved as an adjunct to electronic fetal monitoring (EFM), fetal pulse oximetry has gained only sporadic use since it became available in the United States in 2000—even though EFM has proved disappointing as a tool for predicting fetal hypoxia. Only about 10% of US obstetrical units had fetal pulse oximetry technology as of 2002.1
Clinicians began questioning the reliability of subjective interpretation of fetal heart tracings soon after EFM went into general use. Thirty years later, a meta-analysis of 12 randomized clinical trials involving 58,855 gravidas cast doubt on the benefits of EFM,2 which is associated with an increase in operative deliveries as a result of high sensitivity but low specificity in predicting fetal hypoxia and acidosis.
FDA approval was based on sole randomized trial
The only commercially available fetal oximetry sensor, the Nellcor N-400 (Nellcor, Pleasanton, Calif), obtained US Food and Drug Administration (FDA) approval as an adjunct to EFM when the latter indicates a nonreassuring FHR pattern. That approval was based on the only randomized study3 of fetal pulse oximetry conducted, which involved 1,010 women with predefined nonreassuring FHR patterns in labor.
Goal: Reduced cesarean rate with comparable outcomes. Investigators hypothesized that adjunctive fetal oximetry would improve assessment and reduce the cesarean rate without altering neonatal outcome. Indeed, in the oximetry group, the rate of cesarean delivery performed for a nonreassuring FHR tracing (4.5% versus 10.2%; P = .007) was significantly reduced. Other findings:
- Same neonatal outcomes, with no significant differences between the 2 groups.
- Higher cesarean rate for dystocia in the intervention group, offsetting any advantage in the overall cesarean delivery rate (29% versus 26%). This unexpected increase in cesarean deliveries raises several possibilities:
- Given the unblinded design, it is possible that clinicians, circumspect of the pulse oximetry, continued to perform cesareans for nonreassuring FHR, but labeled the indication for surgery differently. The validity of the dystocia diagnosis was discredited by a subsequent partogram analysis that showed a similar rate of arrested labor in both groups.
- A nonreassuring FHR in conditions of normal fetal oxygenation is predictive of dystocia. Previous randomized studies of EFM have suggested the same thing.4
- Dystocia is the consequence of the device itself. Anecdotal observations suggest a higher rate of persistent occiput posterior positions with fetal oximetry.
Other trials underway. The ongoing Fetal Oximetry (FOX) trial of the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network, involving 10,000 nulliparous participants, is comparing cesarean delivery rates and safety outcomes in patients monitored for FHR plus pulse oximetry with a group in which the clinicians are blinded to the pulse oximetry readings. Another randomized controlled trial of fetal pulse oximetry is underway in Australia.
Potential for increased costs. The American College of Obstetricians and Gynecologists (ACOG) has raised concerns about the potential increase in costs without demonstrable improvement in outcome.5 ACOG has not endorsed fetal pulse oximetry for general practice.
Question 1How accurately does pulse oximetry reflect the fetal condition?
It yields only indirect information on the partial pressure of oxygen in the blood and no data on perfusion or acid-base status.
In other clinical settings, oxygen saturation is not an acceptable substitute for arterial blood gas analysis. The pulse oximeter is not a hemoximeter—only that device directly and reliably determines blood oxygen saturation by spectrophotometry.6 Even the calculated oxygen saturation values provided automatically by modern blood gas analyzers are inaccurate.7
Studies report varying results. In a comparison8 of fetal oxygen saturation by hemoximetry in a fetal scalp blood (FSB) sample and fetal arterial oxyhemoglobin saturation (FSpO2) by pulse oximetry immediately before the blood sampling, the FSpO2 medians were always higher than the FSB hemoximetry saturation—which led to false-negative results in hypoxic babies.
In animal studies, pulse oximetry correlated well with simultaneously measured arterial oxygen saturation (r = 0.98, P = .01),9 but data from human studies are inconsistent. While McNamara et al10 reported good correlation between FSpO2 measurements and umbilical artery blood oxygen saturation at birth (r = 0.59, P <.001), Langer et al11 found no relationship between FSpO2 levels determined during pushing efforts and oxygen saturation in umbilical vein blood at birth.
Possible reasons for the ambiguous findings:
- differences in practice, such as use of umbilical venous versus arterial blood, or measurement during pushing versus between pushes,
- different intervals from FSpO2 reading to umbilical blood sampling, or
- incomparable groups, such as all women in labor versus those with abnormal FHR.
Limitations. Fetal pulse oximetry measures arterial oxygen saturation during the systolic pulse wave in the skin microcirculation at head level. In the fetus, this is part of the preductal circulation, with oxygen saturation levels somewhere between umbilical arterial and umbilical venous blood oxygen saturation.
Theoretically, FSpO2 should be closer to FSB than to umbilical blood. Although FSB samples consist of capillary blood, which is not exactly central arterial blood, the differences are small, at least in the neonate.12 In the intrapartum period, however, several variables with unknown effect may weaken relationships:
- different intervals between the last oximetry signal and blood sampling after delivery
- differences in local tissue perfusion status13
- perfusion changes during fetal compromise, as the fetus centralizes its blood flow, with vasoconstriction in the skin circulation
Question 2What is the critical threshold for fetal oxygen desaturation?
Human studies indicate that an FSpO2 of 33% is approximately the 10th percentile on the normal distribution, and an FSpO2 of 29% to 30% represents the third to fifth percentiles in normal-outcome labor.14 Studies in catheterized fetal sheep suggest that the level below which metabolic acidosis can be anticipated is an FSpO2 of about 30%.15
The 30% threshold also is supported by prospective human data from a multicenter trial.16 According to those data, an FSpO2 of less than 30% has 100% sensitivity in predicting an FSB pH below 7.20. FSpO2 of less than 30% also correlated with a lack of variability on the FHR tracing.17
The cutoff of 30% should not be interpreted as an indication of fetal distress, however. Rather, it represents a threshold below which increasing fetal acidosis will be encountered ( FIGURE 1). Oxygen saturation is a dynamic biologic parameter with broad variation.
FIGURE 1 Tracking fetal arterial oxyhemoglobin saturation
Question 3Is a single reading reliable?
The normal fetus has a remarkable capacity to compensate for transient episodes of desaturation. Thus, a single reading cannot reflect the fetal condition; the trend in FSpO2 must be taken into account. Research indicates only FSpO2 levels below 30% for more than 2 minutes18 or more than 10 minutes19 are likely to be associated with intrapartum acidosis.
ACOG has raised concerns about the potential increase in costs without demonstrable improvement in outcome.
Gorenberg et al20 retrospectively correlated FSpO2 with umbilical artery pH and found that neither the 30% threshold alone nor the duration of FSpO2 below 30% correlated with fetal acidemia (pH below 7.20). Rather, the repetition of such episodes was more predictive. The authors concluded that more than 10 episodes of FSpO2below 30% would overcome the ability of the fetus to compensate.
The study was underpowered to detect a significant difference in acidemia, and did not allow sufficient observation time to detect the natural progression of hypoxia to metabolic acidosis, a better indicator of fetal compromise. Additional research is needed.
Question 4Does oximetry correlate with acid-base status?
Many of the studies mentioned here assumed a correlation. Whenever oxygen saturation in the umbilical artery is 30% or more, acidosis (pH below 7.13) in the same blood is rare—only 1%.21 However, the correlation between fetal pulse oximetry values and acid-base status is much weaker.8.
Leszczynska-Gorzelak et al22 found no relationship between FSpO2 levels in the first or second stage of labor and pH or partial pressure of oxygen in umbilical vein blood at delivery. Other investigators concluded similarly, considering intrapartum FSpO2 of limited use for predicting acidosis at birth, irrespective of FSpO2 cutoff.23,24
Rijnders et al24 found no significant correlation between fetal scalp or umbilical artery blood pH and mean FSpO2 for the last 30 minutes before sampling (r = 0.02, P = .9). Even the lowest FSpO2 level did not correlate with arterial pH (r = .04, P = .84). None of the study’s 3 cases of umbilical pH below 7.05 would have been detected using the mean FSpO2 before delivery, and only 1 would have been detected using the lowest FSpO2.
In another multicenter study involving the Nellcor system in 164 cases with abnormal FHR, a correlation between oximetry and FSB sampling (r = 0.29, P < .01) was noted in the first stage of labor, but second-stage FSpO2 readings did not correlate with oxygen saturation, partial pressure of oxygen, pH, or bicarbonate level in the umbilical artery at birth.25
An observational series26 of 128 fetuses with nonreassuring FHR patterns concluded that fetal distress was insufficiently identified by oximetry. Only 2 of the 11 cases with umbilical artery pH below 7.20 were detected by pulse oximetry recordings below 30% during the last 30 minutes of the second stage, and out of 5 cases with hypoxic readings in the second stage, only 2 were acidotic at birth. The calculated sensitivity was 18%, specificity 92%, positive predictive value (PPV) 40%, and negative predictive value (NPV) 80%. A low Apgar score was never predicted by fetal pulse oximetry.
Others used the same Nellcor system over the final 30 minutes of labor and a cutoff for umbilical blood acidemia of pH below 7.13 and reported similar numbers: sensitivity 28%, specificity 94%, PPV 40%, and NPV 80%.23
Vitoratos et al27 analyzed FSpO2 readings in active labor (not limited to the last 30 minutes before delivery) and obtained somewhat better values: sensitivity 72%, specificity 93%, PPV 61.5%, and NPV 95.8% for an umbilical artery blood pH below 7.15.
The impression that the validity of fetal pulse oximetry is higher in earlier labor than in the second stage is supported by data from Stiller et al. 28 Leszczynska-Gorzelak et al29 found a significant decrease in mean FSpO2 from the first stage to the second stage of normal labor (51.9% versus 43.8%, P < .001), and Dildy et al14 noted a similar difference upon analyzing 160 normal labors (59% versus 53%), but other studies failed to verify such differences.25,30
Observational studies had unrealistic pH cutoff. All the evidence presented thus far on the validity of fetal pulse oximetry in predicting acidemia is based on observational data. A common deficiency is the unrealistic cutoff for pathologic fetal acidemia—a pH of less than 7.13 to 7.20—when it is widely accepted that “pathologic fetal acidemia” reflects an umbilical artery blood pH below 7.31 Even in this group, two thirds of neonates are unaffected by morbidity.
Need to identify metabolic acidosis. It also is accepted that the presence of a metabolic component to fetal acidemia may be as important—if not more important—than a single pH cutoff.31 Only a few human studies of pulse oximetry have distinguished between respiratory and metabolic acidemia. When they did, intrapartum fetal pulse oximetry was unable to predict umbilical artery base excess.23,25
The only randomized study failed to determine whether clinical decisions can be based solely on fetal pulse oximetry. 3 The investigators did suggest that sensitivity and specificity for metabolic acidemia was improved in the intervention group—a promising appraisal, in contrast with previous observational data.
In the study, 7 neonates (3 in the intervention group and 4 controls) had umbilical artery blood pH below 7. All 4 controls had vaginal delivery. There also were 6 cases of elevated base excess (ie, -16 mEq/L or below) among controls. None were recorded in the intervention group, and the 3 cases of acidemia were recognized antepartum and led to cesareans.
Unfortunately, the study design did not guarantee that patient management was based exclusively on EFM with or without fetal pulse oximetry. Vibro-acoustic stimulation or FSB sampling was required before proceeding to cesarean delivery in both groups.
It appears that the negative predictive value of fetal oximetry is of greater practical value than other attributes.
When FSpO2 was less than 30% for the entire interval between 2 contractions, or was unobtainable, the physician was supposed to revert to interpretation of EFM. When that was persistently nonreassuring, the physician was given the option of scalp stimulation or FSB sampling. Thus, it was not determined whether clinical decisions can be based exclusively on fetal pulse oximetry. Schmidt et al26 suggested that such exclusive application of fetal pulse oximetry might actually jeopardize fetal health.
Question 5 Does the combination of oximetry and EFM improve accuracy?
Fetal pulse oximetry was not used independently in any of the studies discussed here, but in association with EFM, which has a sensitivity for fetal acidosis of 93%, specificity of 29%, PPV of 2.6%, and NPV of 99.5%.32
From a statistical point of view, whenever 2 evaluation methods with the same endpoint (fetal acidosis) are combined, sensitivity decreases while specificity increases, theoretically resulting in less unnecessary intervention. That is exactly what investigators have reported: sensitivity as low as 18%26 for fetal oximetry, and specificity as high as 94%.23 However, the value of this new technology might not be so much the prediction of acidosis but identification of the well-oxygenated fetus so that labor may be safely continued in the presence of a concerning—but not ominous—FHR tracing.
Fetal pulse oximetry employs principles of optical spectrophotometry and plethysmography to provide information on the percentage of oxygen bound to hemoglobin. Oxyhemoglobin (oxygenated hemoglobin) and deoxyhemoglobin (hemoglobin without oxygen) absorb red and infrared light differently: more red absorption by deoxyhemoglobin, and more infrared absorption by oxyhemoglobin.
By measuring the relative absorption at each wavelength, the fraction of hemoglobin that carries oxygen can be determined. The arterial oxygen saturation is expressed as a percentage. The technology has been refined to measure fetal arterial oxyhemoglobin saturation during labor.
Pulse oximetry sensors must be calibrated for fetal biological values. In the fetus, normal oxygen saturation is much lower than in the adult or neonate; hemoglobin has a higher affinity for oxygen and is in higher concentration; and there are more capillaries per unit of tissue, higher cardiac output, and a higher heart rate.
In the adult or neonate, pulse oximetry sensors can be attached to fingers, toes, ears, or the bridge of the nose, but such stable placement is not feasible in utero. Further, good contact between sensor and fetal skin is a prerequisite for avoidance of artifacts. This last aspect has presented a sizeable challenge.
Fetal sensors measure reflected light. There is disagreement about the merits of the 2 sensor types, reflectance and transmission. Both include 2 light emitters (for red and infrared light) and a detector. In the transmission sensor (the adult or neonatal type), the light produced by the light-emitting diodes (LED) is picked up by the detector after traversing the interposed tissues. Since tissue interposition is not possible in the fetus, most fetal studies have used reflectance sensors, in which the LED and detector are placed side by side, and the light to be analyzed is reflected by the tissues. This design adds variance depending on the light’s depth of tissue penetration and device position changes.
Placement of the sensor. The Nellcor N-400 includes a reflectance sensor housed in a smooth, pliable head that is advanced through the cervix with the aid of a handle. The handle has a removable stylet to stiffen it during placement.
The sensor is placed against the fetal temple, cheek, or forehead and is held in place by the uterine wall. Placement is similar to that of an internal pressure catheter. Once the stylet is removed, it should not be reinserted.
Because the sensor usually descends and rotates with the fetal head, displacements are frequent and adjustments in sensor placement may be necessary. Placement adjustments can be attempted without the stylet and, if unsuccessful, a new device can be inserted. The Nellcor sensor is not reusable.
The prerequisites for insertion are dilatation of at least 2 cm, ruptured membranes, cephalic presentation, single fetus, gestational age of at least 36 weeks, and no placenta previa.
The manufacturer reports that active genital herpes, HIV, and hepatitis B or E seropositivity preclude fetal pulse oximetry monitoring.
Placement may be impossible when the presenting part is at high station (-3 or above) or low station (+2 or below).
The Nellcor N-400 system has been commercially available in many European countries since 1995, and in Canada since 1998. It was approved for sale in the United States in early 2003.
Question 6Will it improve neonatal outcomes?
Neonatal outcome is the ultimate endpoint in obstetrical care. In the randomized trial by Garite et al,3 there was no difference in neonatal outcome between the groups using or not using fetal pulse oximetry. According to Chua et al,33 FSpO2 levels measured even 10 minutes before delivery have no relation to neonatal outcome.
Leszczynska-Gorzelak et al22 believe FSpO2 is more predictive of neonatal outcome in the first stage than the second. However, Apgar score had no relationship with FSpO2readings in the first or second stage. Butterwegge34 reported 6 cases of FSpO2 below 30% for more than 30 minutes, all with good neonatal outcome, and Alshimmiri et al23 noted that only normal FSpO2 correlates with fetal well-being. Thus, it appears that the NPV of fetal oximetry is of greater practical value than other attributes.
Question 7How precise is it?
The Nellcor system monitors the quality of FSpO2 measurement; no value is displayed if the signal lacks the characteristics of a fetal arterial plethysmographic curve or if contact between sensor and skin is insufficient. Because of fetal movements and other artifacts, posting time is always less than 100%.
In the French multicenter study,25 the mean reliable signal time in the first stage of labor was only 64.7%—even less in the second stage (54%). Signal retention was 67% in the randomized trial by Garite et al. 3
Many artifacts may impede signal acquisition and impact the reliability of a reading:
- The sensor’s position on the fetal head. For example, the difference in FSpO2 readings between the forehead and occiput may be as much as 13.4%. (The sensor is designed to go against the fetal cheek, but may move around.)
- Incomplete sensor-to-skin contact, such as with high fetal head station, -2 or above.
- Marked caput formation.
- Increased intrauterine pressure accompanying contractions, especially at presentation stations of +2 or below (FIGURE 2). FSpO2 monitoring requires detection of fetal pulses, which may be undetectable when the surrounding pressure is high, resulting in a loss of signal.
- Interposition of vernix or fetal hair.
- Presence of meconium, which behaves like a red-light filter, altering the ratio of red to infrared light and resulting in artificially low values.35 This theoretical concern is rejected by Yam et al,36 who did not observe any effect of meconium on FSpO2 values. (When the amniotic fluid is meconium-stained, Carbonne et al37 showed that fetal oximetry is a better predictor of meconium aspiration syndrome than FSB sampling.) The data on the influence of meconium on FSpO2 readings remain contradictory.
All these conditions may impair precision and contribute to poor sensitivity.
FIGURE 2 A weakening signal during pushing
Question 8Is it easy to use?
An Australian survey38 assessed clinicians’ perceptions during placement of the oximetry sensor. Ease of placement was rated as good or excellent in 71% of cases, and the patient’s comfort was rated as good or excellent in 90% of cases. Chua et al39 reported a mean insertion time of 90 seconds, with a reliable signal obtained within 5 minutes in 87% of placements. The French multicenter study25 mentioned earlier concluded that the procedure is satisfactory and easier than FSB sampling. The device itself was harmless to both mother and fetus.40
Potential research directions
Fetal pulse oximetry may be an effective tool in clinical scenarios such as:
- fetal arrhythmias with uninterpretable FHR tracing
- fetal tachycardia associated with maternal fever, thyrotoxicosis, or fetal supraventricular tachycardia, when distinguishing other contributions to tachycardia may be difficult
- fetal bradycardia caused by a complete heart block, which may render EFM undecipherable
- when amnioinfusion is attempted for variable decelerations and it is necessary to differentiate a nonreassuring FHR tracing related to transient in utero stress (eg, umbilical cord compressions) from ominous tracings
Another area not yet addressed is cost-effectiveness beyond the immediate direct costs (approximately $11,000 for the monitor and $150 for each disposable sensor). Also uncertain is whether laboring women will accept the device (how disturbing or invasive it is perceived to be) and how acceptable or applicable it is outside tertiary institutions.
Dr. Vidaeff reports no financial relationships relevant to this article. Dr. Ramin reports grant support from the US National Institutes of Health.
1. Dildy GA. A guest editorial: fetal pulse oximetry. Obstet Gynecol Surv. 2003;58:225-226.
2. Thacker SB, Stroup DF, Peterson HB. Efficacy and safety of intrapartum electronic fetal monitoring: an update. Obstet Gynecol. 1995;86:613-620.
3. Garite TJ, Dildy GA, McNamara H, et al. A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol. 2000;183:1049-1058.
4. Haverkamp AD, Orleans M, Langendoerfer S, et al. A controlled trial of the differential effects of continuous fetal heart rate monitoring in labor: a randomized trial. Am J Obstet Gynecol. 1979;134:399-412.
5. American College of Obstetricians and Gynecologists. Committee opinion: fetal pulse oximetry. Number 258, September 2001. Obstet Gynecol. 2001;98:523-524.
6. Zijlstra WG, Buursma A, Zwart A. Performance of an automated six-wavelength photometer (radiometer OSM3) for routine measurement of hemoglobin derivatives. Clin Chem. 1988;34:149-152.
7. Porath M, Sinah P, Dudenhausen JW, Luttkus AK. Systematic instrumental errors between oxygen saturation analysers in fetal blood during deep hypoxemia. Clin Chim Acta. 2001;307:151-157.
8. Luttkus AK, Lübke M, Büscher U, Porath M, Dudenhausen JW. Accuracy of fetal pulse oximetry. Acta Obstet Gynecol Scand. 2002;81:417-423.
9. Carter AM, Stiller R, König V, Jorgensen JS, Svendsen P, Huch R. Calibration of a reflectance pulse oximeter in fetal lambs for arterial oxygen saturations below 70%. J Soc Gynecol Invest. 1998;5:255-259.
10. McNamara H, Cung CD, Lilford R, Johnson N. Do fetal pulse oximetry readings at delivery correlate with cord blood oxygenation and acidemia? Br J Obstet Gynaecol. 1992;99:735-738.
11. Langer B, Boudier E, Haddad J, Pain L, Schlaeder G. Fetal pulse oximetry during labor of 62 patients. Fetal Diagn Ther. 1996;11:37-45.
12. Harrison AM, Lynch JM, Dean JM, Witte MK. Comparison of simultaneously obtained arterial and capillary blood gases in pediatric intensive care unit patients. Crit Care Med. 1997;25:1904-1908.
13. Nijland R, Jongsma HW, Nijhuis JG, Oeseburg B. Accuracy of fetal pulse oximetry and pitfalls in measurements. Eur J Obstet Gynecol Reprod Biol. 1997;72:S21-S27.
14. Dildy GA, van den Berg PP, Katz M, et al. Intrapartum fetal pulse oximetry: fetal oxygen saturation trends during labor and relation to delivery outcome. Am J Obstet Gynecol. 1994;171:679-684.
15. Nijland R, Jongsma H, Nijhuis J, van den Berg P, Oeseburg B. Arterial saturation in relation to metabolic acidosis in fetal lambs. Am J Obstet Gynecol. 1995;172:810-819.
16. Kühnert M, Seelbach-Göbel B, Butterwegge M. Predictive agreement between fetal arterial oxygen saturation and fetal scalp pH: results of the German multicenter study. Am J Obstet Gynecol. 1998;178:330-335.
17. Salamalekis E, Thomopoulos P, Giannaris D, et al. Computerised intrapartum diagnosis of fetal hypoxia based on heart rate monitoring and fetal pulse oximetry recordings utilizing wavelet analysis and neural networks. Br J Obstet Gynaecol. 2002;109:1137-1142.
18. Bloom SL, Swindle RG, McIntire DD, Leveno KJ. Fetal pulse oximetry: duration of desaturation and intrapartum outcome. Obstet Gynecol. 1999;93:1036-1040.
19. Seelbach-Göbel B, Heupel M, Kühnert M, et al. The prediction of fetal acidosis by means of intrapartum fetal pulse oximetry. Am J Obstet Gynecol. 1999;180:73-81.
20. Gorenberg DM, Patillo C, Hendi P, Rumney PJ, Garite TJ. Fetal pulse oximetry: correlation between oxygen desaturation, duration, and frequency and neonatal outcomes. Am J Obstet Gynecol. 2003;189:136-138.
21. Dildy GA, Thorp JA, Yeast JD, Clark SL. The relationship between oxygen saturation and pH in umbilical blood: implications for intrapartum fetal oxygen saturation monitoring. Am J Obstet Gynecol. 1996;175:682-687.
22. Leszczynska-Gorzelak B, Poniedzialek-Czajkowska E, Oleszczuk J. Fetal blood saturation during the 1st and 2nd stage of labor and its relation to the neonatal outcome. Gynecol Obstet Invest. 2002;54:159-163.
23. Alshimmiri M, Bocking AD, Gagnon R, Natale R, Richardson BS. Prediction of umbilical artery base excess by intrapartum fetal oxygen saturation monitoring. Am J Obstet Gynecol. 1997;177:775-779.
24. Rijnders RJ, Mol BW, Reuwer PJ, Drogtrop AP, Vernooij MM, Visser GH. Is the correlation between fetal oxygen saturation and blood pH sufficient for the use of fetal pulse oximetry? J Matern Fetal Neonatal Med. 2002;11:80-83.
25. Goffinet F, Langer B, Carbonne B, et al. Multicenter study on the clinical value of fetal pulse oximetry. I. Methodologic evaluation. The French Study Group on Fetal Pulse Oximetry. Am J Obstet Gynecol. 1997;177:1238-1246.
26. Schmidt S, Koslowski S, Sierra F, et al. Clinical usefulness of pulse oximetry in the fetus with non-reassuring heart rate pattern? J Perinat Med. 2000;28:298-305.
27. Vitoratos N, Salamalekis E, Saloum J, Makrakis E, Creatsas G. Abnormal fetal heart rate patterns during the active phase of labor and the value of fetal oxygen saturation. J Matern Fetal Neonatal Med. 2002;11:46-49.
28. Stiller R, von Mering R, König V, et al. How well does reflectance pulse oximetry reflect intrapartum fetal acidosis? Am J Obstet Gynecol. 2002;186:1351-1357.
29. Leszczynska-Gorzelak B, Poniedzialek-Czajkowska E, Zych I, Grzechnik M, Oleszczuk J. The usefulness of the intrapartum fetal pulse oximetry in anticipating the neonatal outcome. Ginekol Pol. 2001;72:1183-1188.
30. Nikolov A, Dimitrov A, Vakrilkova L, Iarkova N. Fetal oxygen saturation during normal delivery. Akush Ginekol. 2000;40:3-6.
31. Goldaber KG, Gilstrap LC III, Leveno K, Dax JS, McIntire DD. Pathologic fetal acidemia. Obstet Gynecol. 1991;78:1103-1107.
32. Low JA, Victory R, Derrick EJ. Predictive value of electronic fetal monitoring for intra-partum fetal asphyxia and metabolic acidosis. Obstet Gynecol. 1999;93:285-291.
33. Chua S, Yeong SM, Razvi K, Arulkumaran S. Fetal oxygen saturation during labour. Br J Obstet Gynaecol. 1997;104:1080-1083.
34. Butterwegge M. Fetal pulse oximetry and non-reassuring heart rate. Eur J Obstet Gynecol Reprod Biol. 1997;72:S63-S66.
35. Johnson N, Johnson VA, Bannister J, McNamara H. The effect of meconium on neonatal and fetal reflectance pulse oximetry. J Perinat Med. 1990;18:351-355.
36. Yam J, Chua S, Arulkumaran S. Intrapartum pulse oximetry: Part 1: Principles and technical issues. Obstet Gynecol Surv. 2000;55:163-172.
37. Carbonne B, Cudeville C, Sivan H, Cabrol D, Papiernik E. Fetal oxygen saturation measured by pulse oximetry during labor with clear and meconium-stained amniotic fluid. Eur J Obstet Gynecol Reprod Biol. 1997;72:S51-S55.
38. East CE, Colditz PB. Clinicians’ perceptions of placing a fetal oximetry sensor. J Qual Clin Pract. 2000;20:161-163.
39. Chua S, Yam J, Razvi K, Yeong SM, Arulkumaran S. Intrapartum fetal oxygen saturation monitoring in a busy labour ward. Eur J Obstet Gynecol Reprod Biol. 1999;82:185-189.
40. Luttkus AK, Friedmann W, Thomas S, Dimer JA, Dudenhausen JW. The safety of fetal pulse oximetry in parturients requiring fetal scalp blood sample. Obstet Gynecol. 1997;90:533-537.
- The value of this new technology might not be so much the prediction of acidosis but identification of the well-oxygenated fetus so that labor may be safely continued in the presence of a concerning—but not ominous—fetal heart rate tracing.
- The only randomized study published so far did not determine whether clinical decisions can be based solely on fetal pulse oximetry. The investigators did suggest that sensitivity and specificity for metabolic acidemia was improved in the intervention group—a promising appraisal, in contrast with previous observational data.
When a teenage nullipara underwent labor induction for preeclampsia at 37 weeks, she was given epidural analgesia and seizure prophylaxis with magnesium sulfate. Her electronic fetal heart rate (FHR) tracing was initially reassuring, with only occasional variable decelerations, but subsequently revealed a baseline of 140 beats per minute (bpm), minimal to absent variability, no accelerations, and variable decelerations to 90 bpm with rapid return to baseline.
The tracing was interpreted as nonreassuring, and a fetal pulse oximeter was inserted. It revealed a fetal oxygen saturation rate between 45% and 50%, and labor was allowed to continue. After 3.5 hours in the second stage, the patient was delivered by outlet forceps. Her infant had Apgar scores of 8 at 1 minute and 9 at 5 minutes. The umbilical arterial pH was 7.25, and base excess was–4.9.
Fetal pulse oximetry made it possible to manage this case without resorting to emergent cesarean. But is this noninvasive technology truly a step forward in intrapartum assessment of fetal well-being?
We describe what the evidence (a single randomized study and a number of observational studies) reveals about these questions:
- How accurately does fetal pulse oximetry reflect the fetal condition?
- What is the critical threshold for fetal oxygen desaturation?
- Is a single reading reliable?
- Does oximetry correlate with acid-base status?
- Does the combination of oximetry and electronic monitoring improve accuracy?
- Will fetal pulse oximetry improve neonatal outcomes?
- How precise is it?
- Is it easy to use?
Needed: Effective adjunct to electronic monitoring
Except in the chronically hypoxic fetus (which is affected by the time labor begins), the pathophysiology of acute intrapartum events is a continuum, from hypoxemia to respiratory acidosis to metabolic acidosis and, ultimately, clinical impairment. The goal of intrapartum surveillance is to detect fetal hypoxemia before it progresses to asphyxia and perinatal mortality or long-term morbidity.
Although it is approved as an adjunct to electronic fetal monitoring (EFM), fetal pulse oximetry has gained only sporadic use since it became available in the United States in 2000—even though EFM has proved disappointing as a tool for predicting fetal hypoxia. Only about 10% of US obstetrical units had fetal pulse oximetry technology as of 2002.1
Clinicians began questioning the reliability of subjective interpretation of fetal heart tracings soon after EFM went into general use. Thirty years later, a meta-analysis of 12 randomized clinical trials involving 58,855 gravidas cast doubt on the benefits of EFM,2 which is associated with an increase in operative deliveries as a result of high sensitivity but low specificity in predicting fetal hypoxia and acidosis.
FDA approval was based on sole randomized trial
The only commercially available fetal oximetry sensor, the Nellcor N-400 (Nellcor, Pleasanton, Calif), obtained US Food and Drug Administration (FDA) approval as an adjunct to EFM when the latter indicates a nonreassuring FHR pattern. That approval was based on the only randomized study3 of fetal pulse oximetry conducted, which involved 1,010 women with predefined nonreassuring FHR patterns in labor.
Goal: Reduced cesarean rate with comparable outcomes. Investigators hypothesized that adjunctive fetal oximetry would improve assessment and reduce the cesarean rate without altering neonatal outcome. Indeed, in the oximetry group, the rate of cesarean delivery performed for a nonreassuring FHR tracing (4.5% versus 10.2%; P = .007) was significantly reduced. Other findings:
- Same neonatal outcomes, with no significant differences between the 2 groups.
- Higher cesarean rate for dystocia in the intervention group, offsetting any advantage in the overall cesarean delivery rate (29% versus 26%). This unexpected increase in cesarean deliveries raises several possibilities:
- Given the unblinded design, it is possible that clinicians, circumspect of the pulse oximetry, continued to perform cesareans for nonreassuring FHR, but labeled the indication for surgery differently. The validity of the dystocia diagnosis was discredited by a subsequent partogram analysis that showed a similar rate of arrested labor in both groups.
- A nonreassuring FHR in conditions of normal fetal oxygenation is predictive of dystocia. Previous randomized studies of EFM have suggested the same thing.4
- Dystocia is the consequence of the device itself. Anecdotal observations suggest a higher rate of persistent occiput posterior positions with fetal oximetry.
Other trials underway. The ongoing Fetal Oximetry (FOX) trial of the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network, involving 10,000 nulliparous participants, is comparing cesarean delivery rates and safety outcomes in patients monitored for FHR plus pulse oximetry with a group in which the clinicians are blinded to the pulse oximetry readings. Another randomized controlled trial of fetal pulse oximetry is underway in Australia.
Potential for increased costs. The American College of Obstetricians and Gynecologists (ACOG) has raised concerns about the potential increase in costs without demonstrable improvement in outcome.5 ACOG has not endorsed fetal pulse oximetry for general practice.
Question 1How accurately does pulse oximetry reflect the fetal condition?
It yields only indirect information on the partial pressure of oxygen in the blood and no data on perfusion or acid-base status.
In other clinical settings, oxygen saturation is not an acceptable substitute for arterial blood gas analysis. The pulse oximeter is not a hemoximeter—only that device directly and reliably determines blood oxygen saturation by spectrophotometry.6 Even the calculated oxygen saturation values provided automatically by modern blood gas analyzers are inaccurate.7
Studies report varying results. In a comparison8 of fetal oxygen saturation by hemoximetry in a fetal scalp blood (FSB) sample and fetal arterial oxyhemoglobin saturation (FSpO2) by pulse oximetry immediately before the blood sampling, the FSpO2 medians were always higher than the FSB hemoximetry saturation—which led to false-negative results in hypoxic babies.
In animal studies, pulse oximetry correlated well with simultaneously measured arterial oxygen saturation (r = 0.98, P = .01),9 but data from human studies are inconsistent. While McNamara et al10 reported good correlation between FSpO2 measurements and umbilical artery blood oxygen saturation at birth (r = 0.59, P <.001), Langer et al11 found no relationship between FSpO2 levels determined during pushing efforts and oxygen saturation in umbilical vein blood at birth.
Possible reasons for the ambiguous findings:
- differences in practice, such as use of umbilical venous versus arterial blood, or measurement during pushing versus between pushes,
- different intervals from FSpO2 reading to umbilical blood sampling, or
- incomparable groups, such as all women in labor versus those with abnormal FHR.
Limitations. Fetal pulse oximetry measures arterial oxygen saturation during the systolic pulse wave in the skin microcirculation at head level. In the fetus, this is part of the preductal circulation, with oxygen saturation levels somewhere between umbilical arterial and umbilical venous blood oxygen saturation.
Theoretically, FSpO2 should be closer to FSB than to umbilical blood. Although FSB samples consist of capillary blood, which is not exactly central arterial blood, the differences are small, at least in the neonate.12 In the intrapartum period, however, several variables with unknown effect may weaken relationships:
- different intervals between the last oximetry signal and blood sampling after delivery
- differences in local tissue perfusion status13
- perfusion changes during fetal compromise, as the fetus centralizes its blood flow, with vasoconstriction in the skin circulation
Question 2What is the critical threshold for fetal oxygen desaturation?
Human studies indicate that an FSpO2 of 33% is approximately the 10th percentile on the normal distribution, and an FSpO2 of 29% to 30% represents the third to fifth percentiles in normal-outcome labor.14 Studies in catheterized fetal sheep suggest that the level below which metabolic acidosis can be anticipated is an FSpO2 of about 30%.15
The 30% threshold also is supported by prospective human data from a multicenter trial.16 According to those data, an FSpO2 of less than 30% has 100% sensitivity in predicting an FSB pH below 7.20. FSpO2 of less than 30% also correlated with a lack of variability on the FHR tracing.17
The cutoff of 30% should not be interpreted as an indication of fetal distress, however. Rather, it represents a threshold below which increasing fetal acidosis will be encountered ( FIGURE 1). Oxygen saturation is a dynamic biologic parameter with broad variation.
FIGURE 1 Tracking fetal arterial oxyhemoglobin saturation
Question 3Is a single reading reliable?
The normal fetus has a remarkable capacity to compensate for transient episodes of desaturation. Thus, a single reading cannot reflect the fetal condition; the trend in FSpO2 must be taken into account. Research indicates only FSpO2 levels below 30% for more than 2 minutes18 or more than 10 minutes19 are likely to be associated with intrapartum acidosis.
ACOG has raised concerns about the potential increase in costs without demonstrable improvement in outcome.
Gorenberg et al20 retrospectively correlated FSpO2 with umbilical artery pH and found that neither the 30% threshold alone nor the duration of FSpO2 below 30% correlated with fetal acidemia (pH below 7.20). Rather, the repetition of such episodes was more predictive. The authors concluded that more than 10 episodes of FSpO2below 30% would overcome the ability of the fetus to compensate.
The study was underpowered to detect a significant difference in acidemia, and did not allow sufficient observation time to detect the natural progression of hypoxia to metabolic acidosis, a better indicator of fetal compromise. Additional research is needed.
Question 4Does oximetry correlate with acid-base status?
Many of the studies mentioned here assumed a correlation. Whenever oxygen saturation in the umbilical artery is 30% or more, acidosis (pH below 7.13) in the same blood is rare—only 1%.21 However, the correlation between fetal pulse oximetry values and acid-base status is much weaker.8.
Leszczynska-Gorzelak et al22 found no relationship between FSpO2 levels in the first or second stage of labor and pH or partial pressure of oxygen in umbilical vein blood at delivery. Other investigators concluded similarly, considering intrapartum FSpO2 of limited use for predicting acidosis at birth, irrespective of FSpO2 cutoff.23,24
Rijnders et al24 found no significant correlation between fetal scalp or umbilical artery blood pH and mean FSpO2 for the last 30 minutes before sampling (r = 0.02, P = .9). Even the lowest FSpO2 level did not correlate with arterial pH (r = .04, P = .84). None of the study’s 3 cases of umbilical pH below 7.05 would have been detected using the mean FSpO2 before delivery, and only 1 would have been detected using the lowest FSpO2.
In another multicenter study involving the Nellcor system in 164 cases with abnormal FHR, a correlation between oximetry and FSB sampling (r = 0.29, P < .01) was noted in the first stage of labor, but second-stage FSpO2 readings did not correlate with oxygen saturation, partial pressure of oxygen, pH, or bicarbonate level in the umbilical artery at birth.25
An observational series26 of 128 fetuses with nonreassuring FHR patterns concluded that fetal distress was insufficiently identified by oximetry. Only 2 of the 11 cases with umbilical artery pH below 7.20 were detected by pulse oximetry recordings below 30% during the last 30 minutes of the second stage, and out of 5 cases with hypoxic readings in the second stage, only 2 were acidotic at birth. The calculated sensitivity was 18%, specificity 92%, positive predictive value (PPV) 40%, and negative predictive value (NPV) 80%. A low Apgar score was never predicted by fetal pulse oximetry.
Others used the same Nellcor system over the final 30 minutes of labor and a cutoff for umbilical blood acidemia of pH below 7.13 and reported similar numbers: sensitivity 28%, specificity 94%, PPV 40%, and NPV 80%.23
Vitoratos et al27 analyzed FSpO2 readings in active labor (not limited to the last 30 minutes before delivery) and obtained somewhat better values: sensitivity 72%, specificity 93%, PPV 61.5%, and NPV 95.8% for an umbilical artery blood pH below 7.15.
The impression that the validity of fetal pulse oximetry is higher in earlier labor than in the second stage is supported by data from Stiller et al. 28 Leszczynska-Gorzelak et al29 found a significant decrease in mean FSpO2 from the first stage to the second stage of normal labor (51.9% versus 43.8%, P < .001), and Dildy et al14 noted a similar difference upon analyzing 160 normal labors (59% versus 53%), but other studies failed to verify such differences.25,30
Observational studies had unrealistic pH cutoff. All the evidence presented thus far on the validity of fetal pulse oximetry in predicting acidemia is based on observational data. A common deficiency is the unrealistic cutoff for pathologic fetal acidemia—a pH of less than 7.13 to 7.20—when it is widely accepted that “pathologic fetal acidemia” reflects an umbilical artery blood pH below 7.31 Even in this group, two thirds of neonates are unaffected by morbidity.
Need to identify metabolic acidosis. It also is accepted that the presence of a metabolic component to fetal acidemia may be as important—if not more important—than a single pH cutoff.31 Only a few human studies of pulse oximetry have distinguished between respiratory and metabolic acidemia. When they did, intrapartum fetal pulse oximetry was unable to predict umbilical artery base excess.23,25
The only randomized study failed to determine whether clinical decisions can be based solely on fetal pulse oximetry. 3 The investigators did suggest that sensitivity and specificity for metabolic acidemia was improved in the intervention group—a promising appraisal, in contrast with previous observational data.
In the study, 7 neonates (3 in the intervention group and 4 controls) had umbilical artery blood pH below 7. All 4 controls had vaginal delivery. There also were 6 cases of elevated base excess (ie, -16 mEq/L or below) among controls. None were recorded in the intervention group, and the 3 cases of acidemia were recognized antepartum and led to cesareans.
Unfortunately, the study design did not guarantee that patient management was based exclusively on EFM with or without fetal pulse oximetry. Vibro-acoustic stimulation or FSB sampling was required before proceeding to cesarean delivery in both groups.
It appears that the negative predictive value of fetal oximetry is of greater practical value than other attributes.
When FSpO2 was less than 30% for the entire interval between 2 contractions, or was unobtainable, the physician was supposed to revert to interpretation of EFM. When that was persistently nonreassuring, the physician was given the option of scalp stimulation or FSB sampling. Thus, it was not determined whether clinical decisions can be based exclusively on fetal pulse oximetry. Schmidt et al26 suggested that such exclusive application of fetal pulse oximetry might actually jeopardize fetal health.
Question 5 Does the combination of oximetry and EFM improve accuracy?
Fetal pulse oximetry was not used independently in any of the studies discussed here, but in association with EFM, which has a sensitivity for fetal acidosis of 93%, specificity of 29%, PPV of 2.6%, and NPV of 99.5%.32
From a statistical point of view, whenever 2 evaluation methods with the same endpoint (fetal acidosis) are combined, sensitivity decreases while specificity increases, theoretically resulting in less unnecessary intervention. That is exactly what investigators have reported: sensitivity as low as 18%26 for fetal oximetry, and specificity as high as 94%.23 However, the value of this new technology might not be so much the prediction of acidosis but identification of the well-oxygenated fetus so that labor may be safely continued in the presence of a concerning—but not ominous—FHR tracing.
Fetal pulse oximetry employs principles of optical spectrophotometry and plethysmography to provide information on the percentage of oxygen bound to hemoglobin. Oxyhemoglobin (oxygenated hemoglobin) and deoxyhemoglobin (hemoglobin without oxygen) absorb red and infrared light differently: more red absorption by deoxyhemoglobin, and more infrared absorption by oxyhemoglobin.
By measuring the relative absorption at each wavelength, the fraction of hemoglobin that carries oxygen can be determined. The arterial oxygen saturation is expressed as a percentage. The technology has been refined to measure fetal arterial oxyhemoglobin saturation during labor.
Pulse oximetry sensors must be calibrated for fetal biological values. In the fetus, normal oxygen saturation is much lower than in the adult or neonate; hemoglobin has a higher affinity for oxygen and is in higher concentration; and there are more capillaries per unit of tissue, higher cardiac output, and a higher heart rate.
In the adult or neonate, pulse oximetry sensors can be attached to fingers, toes, ears, or the bridge of the nose, but such stable placement is not feasible in utero. Further, good contact between sensor and fetal skin is a prerequisite for avoidance of artifacts. This last aspect has presented a sizeable challenge.
Fetal sensors measure reflected light. There is disagreement about the merits of the 2 sensor types, reflectance and transmission. Both include 2 light emitters (for red and infrared light) and a detector. In the transmission sensor (the adult or neonatal type), the light produced by the light-emitting diodes (LED) is picked up by the detector after traversing the interposed tissues. Since tissue interposition is not possible in the fetus, most fetal studies have used reflectance sensors, in which the LED and detector are placed side by side, and the light to be analyzed is reflected by the tissues. This design adds variance depending on the light’s depth of tissue penetration and device position changes.
Placement of the sensor. The Nellcor N-400 includes a reflectance sensor housed in a smooth, pliable head that is advanced through the cervix with the aid of a handle. The handle has a removable stylet to stiffen it during placement.
The sensor is placed against the fetal temple, cheek, or forehead and is held in place by the uterine wall. Placement is similar to that of an internal pressure catheter. Once the stylet is removed, it should not be reinserted.
Because the sensor usually descends and rotates with the fetal head, displacements are frequent and adjustments in sensor placement may be necessary. Placement adjustments can be attempted without the stylet and, if unsuccessful, a new device can be inserted. The Nellcor sensor is not reusable.
The prerequisites for insertion are dilatation of at least 2 cm, ruptured membranes, cephalic presentation, single fetus, gestational age of at least 36 weeks, and no placenta previa.
The manufacturer reports that active genital herpes, HIV, and hepatitis B or E seropositivity preclude fetal pulse oximetry monitoring.
Placement may be impossible when the presenting part is at high station (-3 or above) or low station (+2 or below).
The Nellcor N-400 system has been commercially available in many European countries since 1995, and in Canada since 1998. It was approved for sale in the United States in early 2003.
Question 6Will it improve neonatal outcomes?
Neonatal outcome is the ultimate endpoint in obstetrical care. In the randomized trial by Garite et al,3 there was no difference in neonatal outcome between the groups using or not using fetal pulse oximetry. According to Chua et al,33 FSpO2 levels measured even 10 minutes before delivery have no relation to neonatal outcome.
Leszczynska-Gorzelak et al22 believe FSpO2 is more predictive of neonatal outcome in the first stage than the second. However, Apgar score had no relationship with FSpO2readings in the first or second stage. Butterwegge34 reported 6 cases of FSpO2 below 30% for more than 30 minutes, all with good neonatal outcome, and Alshimmiri et al23 noted that only normal FSpO2 correlates with fetal well-being. Thus, it appears that the NPV of fetal oximetry is of greater practical value than other attributes.
Question 7How precise is it?
The Nellcor system monitors the quality of FSpO2 measurement; no value is displayed if the signal lacks the characteristics of a fetal arterial plethysmographic curve or if contact between sensor and skin is insufficient. Because of fetal movements and other artifacts, posting time is always less than 100%.
In the French multicenter study,25 the mean reliable signal time in the first stage of labor was only 64.7%—even less in the second stage (54%). Signal retention was 67% in the randomized trial by Garite et al. 3
Many artifacts may impede signal acquisition and impact the reliability of a reading:
- The sensor’s position on the fetal head. For example, the difference in FSpO2 readings between the forehead and occiput may be as much as 13.4%. (The sensor is designed to go against the fetal cheek, but may move around.)
- Incomplete sensor-to-skin contact, such as with high fetal head station, -2 or above.
- Marked caput formation.
- Increased intrauterine pressure accompanying contractions, especially at presentation stations of +2 or below (FIGURE 2). FSpO2 monitoring requires detection of fetal pulses, which may be undetectable when the surrounding pressure is high, resulting in a loss of signal.
- Interposition of vernix or fetal hair.
- Presence of meconium, which behaves like a red-light filter, altering the ratio of red to infrared light and resulting in artificially low values.35 This theoretical concern is rejected by Yam et al,36 who did not observe any effect of meconium on FSpO2 values. (When the amniotic fluid is meconium-stained, Carbonne et al37 showed that fetal oximetry is a better predictor of meconium aspiration syndrome than FSB sampling.) The data on the influence of meconium on FSpO2 readings remain contradictory.
All these conditions may impair precision and contribute to poor sensitivity.
FIGURE 2 A weakening signal during pushing
Question 8Is it easy to use?
An Australian survey38 assessed clinicians’ perceptions during placement of the oximetry sensor. Ease of placement was rated as good or excellent in 71% of cases, and the patient’s comfort was rated as good or excellent in 90% of cases. Chua et al39 reported a mean insertion time of 90 seconds, with a reliable signal obtained within 5 minutes in 87% of placements. The French multicenter study25 mentioned earlier concluded that the procedure is satisfactory and easier than FSB sampling. The device itself was harmless to both mother and fetus.40
Potential research directions
Fetal pulse oximetry may be an effective tool in clinical scenarios such as:
- fetal arrhythmias with uninterpretable FHR tracing
- fetal tachycardia associated with maternal fever, thyrotoxicosis, or fetal supraventricular tachycardia, when distinguishing other contributions to tachycardia may be difficult
- fetal bradycardia caused by a complete heart block, which may render EFM undecipherable
- when amnioinfusion is attempted for variable decelerations and it is necessary to differentiate a nonreassuring FHR tracing related to transient in utero stress (eg, umbilical cord compressions) from ominous tracings
Another area not yet addressed is cost-effectiveness beyond the immediate direct costs (approximately $11,000 for the monitor and $150 for each disposable sensor). Also uncertain is whether laboring women will accept the device (how disturbing or invasive it is perceived to be) and how acceptable or applicable it is outside tertiary institutions.
Dr. Vidaeff reports no financial relationships relevant to this article. Dr. Ramin reports grant support from the US National Institutes of Health.
- The value of this new technology might not be so much the prediction of acidosis but identification of the well-oxygenated fetus so that labor may be safely continued in the presence of a concerning—but not ominous—fetal heart rate tracing.
- The only randomized study published so far did not determine whether clinical decisions can be based solely on fetal pulse oximetry. The investigators did suggest that sensitivity and specificity for metabolic acidemia was improved in the intervention group—a promising appraisal, in contrast with previous observational data.
When a teenage nullipara underwent labor induction for preeclampsia at 37 weeks, she was given epidural analgesia and seizure prophylaxis with magnesium sulfate. Her electronic fetal heart rate (FHR) tracing was initially reassuring, with only occasional variable decelerations, but subsequently revealed a baseline of 140 beats per minute (bpm), minimal to absent variability, no accelerations, and variable decelerations to 90 bpm with rapid return to baseline.
The tracing was interpreted as nonreassuring, and a fetal pulse oximeter was inserted. It revealed a fetal oxygen saturation rate between 45% and 50%, and labor was allowed to continue. After 3.5 hours in the second stage, the patient was delivered by outlet forceps. Her infant had Apgar scores of 8 at 1 minute and 9 at 5 minutes. The umbilical arterial pH was 7.25, and base excess was–4.9.
Fetal pulse oximetry made it possible to manage this case without resorting to emergent cesarean. But is this noninvasive technology truly a step forward in intrapartum assessment of fetal well-being?
We describe what the evidence (a single randomized study and a number of observational studies) reveals about these questions:
- How accurately does fetal pulse oximetry reflect the fetal condition?
- What is the critical threshold for fetal oxygen desaturation?
- Is a single reading reliable?
- Does oximetry correlate with acid-base status?
- Does the combination of oximetry and electronic monitoring improve accuracy?
- Will fetal pulse oximetry improve neonatal outcomes?
- How precise is it?
- Is it easy to use?
Needed: Effective adjunct to electronic monitoring
Except in the chronically hypoxic fetus (which is affected by the time labor begins), the pathophysiology of acute intrapartum events is a continuum, from hypoxemia to respiratory acidosis to metabolic acidosis and, ultimately, clinical impairment. The goal of intrapartum surveillance is to detect fetal hypoxemia before it progresses to asphyxia and perinatal mortality or long-term morbidity.
Although it is approved as an adjunct to electronic fetal monitoring (EFM), fetal pulse oximetry has gained only sporadic use since it became available in the United States in 2000—even though EFM has proved disappointing as a tool for predicting fetal hypoxia. Only about 10% of US obstetrical units had fetal pulse oximetry technology as of 2002.1
Clinicians began questioning the reliability of subjective interpretation of fetal heart tracings soon after EFM went into general use. Thirty years later, a meta-analysis of 12 randomized clinical trials involving 58,855 gravidas cast doubt on the benefits of EFM,2 which is associated with an increase in operative deliveries as a result of high sensitivity but low specificity in predicting fetal hypoxia and acidosis.
FDA approval was based on sole randomized trial
The only commercially available fetal oximetry sensor, the Nellcor N-400 (Nellcor, Pleasanton, Calif), obtained US Food and Drug Administration (FDA) approval as an adjunct to EFM when the latter indicates a nonreassuring FHR pattern. That approval was based on the only randomized study3 of fetal pulse oximetry conducted, which involved 1,010 women with predefined nonreassuring FHR patterns in labor.
Goal: Reduced cesarean rate with comparable outcomes. Investigators hypothesized that adjunctive fetal oximetry would improve assessment and reduce the cesarean rate without altering neonatal outcome. Indeed, in the oximetry group, the rate of cesarean delivery performed for a nonreassuring FHR tracing (4.5% versus 10.2%; P = .007) was significantly reduced. Other findings:
- Same neonatal outcomes, with no significant differences between the 2 groups.
- Higher cesarean rate for dystocia in the intervention group, offsetting any advantage in the overall cesarean delivery rate (29% versus 26%). This unexpected increase in cesarean deliveries raises several possibilities:
- Given the unblinded design, it is possible that clinicians, circumspect of the pulse oximetry, continued to perform cesareans for nonreassuring FHR, but labeled the indication for surgery differently. The validity of the dystocia diagnosis was discredited by a subsequent partogram analysis that showed a similar rate of arrested labor in both groups.
- A nonreassuring FHR in conditions of normal fetal oxygenation is predictive of dystocia. Previous randomized studies of EFM have suggested the same thing.4
- Dystocia is the consequence of the device itself. Anecdotal observations suggest a higher rate of persistent occiput posterior positions with fetal oximetry.
Other trials underway. The ongoing Fetal Oximetry (FOX) trial of the National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network, involving 10,000 nulliparous participants, is comparing cesarean delivery rates and safety outcomes in patients monitored for FHR plus pulse oximetry with a group in which the clinicians are blinded to the pulse oximetry readings. Another randomized controlled trial of fetal pulse oximetry is underway in Australia.
Potential for increased costs. The American College of Obstetricians and Gynecologists (ACOG) has raised concerns about the potential increase in costs without demonstrable improvement in outcome.5 ACOG has not endorsed fetal pulse oximetry for general practice.
Question 1How accurately does pulse oximetry reflect the fetal condition?
It yields only indirect information on the partial pressure of oxygen in the blood and no data on perfusion or acid-base status.
In other clinical settings, oxygen saturation is not an acceptable substitute for arterial blood gas analysis. The pulse oximeter is not a hemoximeter—only that device directly and reliably determines blood oxygen saturation by spectrophotometry.6 Even the calculated oxygen saturation values provided automatically by modern blood gas analyzers are inaccurate.7
Studies report varying results. In a comparison8 of fetal oxygen saturation by hemoximetry in a fetal scalp blood (FSB) sample and fetal arterial oxyhemoglobin saturation (FSpO2) by pulse oximetry immediately before the blood sampling, the FSpO2 medians were always higher than the FSB hemoximetry saturation—which led to false-negative results in hypoxic babies.
In animal studies, pulse oximetry correlated well with simultaneously measured arterial oxygen saturation (r = 0.98, P = .01),9 but data from human studies are inconsistent. While McNamara et al10 reported good correlation between FSpO2 measurements and umbilical artery blood oxygen saturation at birth (r = 0.59, P <.001), Langer et al11 found no relationship between FSpO2 levels determined during pushing efforts and oxygen saturation in umbilical vein blood at birth.
Possible reasons for the ambiguous findings:
- differences in practice, such as use of umbilical venous versus arterial blood, or measurement during pushing versus between pushes,
- different intervals from FSpO2 reading to umbilical blood sampling, or
- incomparable groups, such as all women in labor versus those with abnormal FHR.
Limitations. Fetal pulse oximetry measures arterial oxygen saturation during the systolic pulse wave in the skin microcirculation at head level. In the fetus, this is part of the preductal circulation, with oxygen saturation levels somewhere between umbilical arterial and umbilical venous blood oxygen saturation.
Theoretically, FSpO2 should be closer to FSB than to umbilical blood. Although FSB samples consist of capillary blood, which is not exactly central arterial blood, the differences are small, at least in the neonate.12 In the intrapartum period, however, several variables with unknown effect may weaken relationships:
- different intervals between the last oximetry signal and blood sampling after delivery
- differences in local tissue perfusion status13
- perfusion changes during fetal compromise, as the fetus centralizes its blood flow, with vasoconstriction in the skin circulation
Question 2What is the critical threshold for fetal oxygen desaturation?
Human studies indicate that an FSpO2 of 33% is approximately the 10th percentile on the normal distribution, and an FSpO2 of 29% to 30% represents the third to fifth percentiles in normal-outcome labor.14 Studies in catheterized fetal sheep suggest that the level below which metabolic acidosis can be anticipated is an FSpO2 of about 30%.15
The 30% threshold also is supported by prospective human data from a multicenter trial.16 According to those data, an FSpO2 of less than 30% has 100% sensitivity in predicting an FSB pH below 7.20. FSpO2 of less than 30% also correlated with a lack of variability on the FHR tracing.17
The cutoff of 30% should not be interpreted as an indication of fetal distress, however. Rather, it represents a threshold below which increasing fetal acidosis will be encountered ( FIGURE 1). Oxygen saturation is a dynamic biologic parameter with broad variation.
FIGURE 1 Tracking fetal arterial oxyhemoglobin saturation
Question 3Is a single reading reliable?
The normal fetus has a remarkable capacity to compensate for transient episodes of desaturation. Thus, a single reading cannot reflect the fetal condition; the trend in FSpO2 must be taken into account. Research indicates only FSpO2 levels below 30% for more than 2 minutes18 or more than 10 minutes19 are likely to be associated with intrapartum acidosis.
ACOG has raised concerns about the potential increase in costs without demonstrable improvement in outcome.
Gorenberg et al20 retrospectively correlated FSpO2 with umbilical artery pH and found that neither the 30% threshold alone nor the duration of FSpO2 below 30% correlated with fetal acidemia (pH below 7.20). Rather, the repetition of such episodes was more predictive. The authors concluded that more than 10 episodes of FSpO2below 30% would overcome the ability of the fetus to compensate.
The study was underpowered to detect a significant difference in acidemia, and did not allow sufficient observation time to detect the natural progression of hypoxia to metabolic acidosis, a better indicator of fetal compromise. Additional research is needed.
Question 4Does oximetry correlate with acid-base status?
Many of the studies mentioned here assumed a correlation. Whenever oxygen saturation in the umbilical artery is 30% or more, acidosis (pH below 7.13) in the same blood is rare—only 1%.21 However, the correlation between fetal pulse oximetry values and acid-base status is much weaker.8.
Leszczynska-Gorzelak et al22 found no relationship between FSpO2 levels in the first or second stage of labor and pH or partial pressure of oxygen in umbilical vein blood at delivery. Other investigators concluded similarly, considering intrapartum FSpO2 of limited use for predicting acidosis at birth, irrespective of FSpO2 cutoff.23,24
Rijnders et al24 found no significant correlation between fetal scalp or umbilical artery blood pH and mean FSpO2 for the last 30 minutes before sampling (r = 0.02, P = .9). Even the lowest FSpO2 level did not correlate with arterial pH (r = .04, P = .84). None of the study’s 3 cases of umbilical pH below 7.05 would have been detected using the mean FSpO2 before delivery, and only 1 would have been detected using the lowest FSpO2.
In another multicenter study involving the Nellcor system in 164 cases with abnormal FHR, a correlation between oximetry and FSB sampling (r = 0.29, P < .01) was noted in the first stage of labor, but second-stage FSpO2 readings did not correlate with oxygen saturation, partial pressure of oxygen, pH, or bicarbonate level in the umbilical artery at birth.25
An observational series26 of 128 fetuses with nonreassuring FHR patterns concluded that fetal distress was insufficiently identified by oximetry. Only 2 of the 11 cases with umbilical artery pH below 7.20 were detected by pulse oximetry recordings below 30% during the last 30 minutes of the second stage, and out of 5 cases with hypoxic readings in the second stage, only 2 were acidotic at birth. The calculated sensitivity was 18%, specificity 92%, positive predictive value (PPV) 40%, and negative predictive value (NPV) 80%. A low Apgar score was never predicted by fetal pulse oximetry.
Others used the same Nellcor system over the final 30 minutes of labor and a cutoff for umbilical blood acidemia of pH below 7.13 and reported similar numbers: sensitivity 28%, specificity 94%, PPV 40%, and NPV 80%.23
Vitoratos et al27 analyzed FSpO2 readings in active labor (not limited to the last 30 minutes before delivery) and obtained somewhat better values: sensitivity 72%, specificity 93%, PPV 61.5%, and NPV 95.8% for an umbilical artery blood pH below 7.15.
The impression that the validity of fetal pulse oximetry is higher in earlier labor than in the second stage is supported by data from Stiller et al. 28 Leszczynska-Gorzelak et al29 found a significant decrease in mean FSpO2 from the first stage to the second stage of normal labor (51.9% versus 43.8%, P < .001), and Dildy et al14 noted a similar difference upon analyzing 160 normal labors (59% versus 53%), but other studies failed to verify such differences.25,30
Observational studies had unrealistic pH cutoff. All the evidence presented thus far on the validity of fetal pulse oximetry in predicting acidemia is based on observational data. A common deficiency is the unrealistic cutoff for pathologic fetal acidemia—a pH of less than 7.13 to 7.20—when it is widely accepted that “pathologic fetal acidemia” reflects an umbilical artery blood pH below 7.31 Even in this group, two thirds of neonates are unaffected by morbidity.
Need to identify metabolic acidosis. It also is accepted that the presence of a metabolic component to fetal acidemia may be as important—if not more important—than a single pH cutoff.31 Only a few human studies of pulse oximetry have distinguished between respiratory and metabolic acidemia. When they did, intrapartum fetal pulse oximetry was unable to predict umbilical artery base excess.23,25
The only randomized study failed to determine whether clinical decisions can be based solely on fetal pulse oximetry. 3 The investigators did suggest that sensitivity and specificity for metabolic acidemia was improved in the intervention group—a promising appraisal, in contrast with previous observational data.
In the study, 7 neonates (3 in the intervention group and 4 controls) had umbilical artery blood pH below 7. All 4 controls had vaginal delivery. There also were 6 cases of elevated base excess (ie, -16 mEq/L or below) among controls. None were recorded in the intervention group, and the 3 cases of acidemia were recognized antepartum and led to cesareans.
Unfortunately, the study design did not guarantee that patient management was based exclusively on EFM with or without fetal pulse oximetry. Vibro-acoustic stimulation or FSB sampling was required before proceeding to cesarean delivery in both groups.
It appears that the negative predictive value of fetal oximetry is of greater practical value than other attributes.
When FSpO2 was less than 30% for the entire interval between 2 contractions, or was unobtainable, the physician was supposed to revert to interpretation of EFM. When that was persistently nonreassuring, the physician was given the option of scalp stimulation or FSB sampling. Thus, it was not determined whether clinical decisions can be based exclusively on fetal pulse oximetry. Schmidt et al26 suggested that such exclusive application of fetal pulse oximetry might actually jeopardize fetal health.
Question 5 Does the combination of oximetry and EFM improve accuracy?
Fetal pulse oximetry was not used independently in any of the studies discussed here, but in association with EFM, which has a sensitivity for fetal acidosis of 93%, specificity of 29%, PPV of 2.6%, and NPV of 99.5%.32
From a statistical point of view, whenever 2 evaluation methods with the same endpoint (fetal acidosis) are combined, sensitivity decreases while specificity increases, theoretically resulting in less unnecessary intervention. That is exactly what investigators have reported: sensitivity as low as 18%26 for fetal oximetry, and specificity as high as 94%.23 However, the value of this new technology might not be so much the prediction of acidosis but identification of the well-oxygenated fetus so that labor may be safely continued in the presence of a concerning—but not ominous—FHR tracing.
Fetal pulse oximetry employs principles of optical spectrophotometry and plethysmography to provide information on the percentage of oxygen bound to hemoglobin. Oxyhemoglobin (oxygenated hemoglobin) and deoxyhemoglobin (hemoglobin without oxygen) absorb red and infrared light differently: more red absorption by deoxyhemoglobin, and more infrared absorption by oxyhemoglobin.
By measuring the relative absorption at each wavelength, the fraction of hemoglobin that carries oxygen can be determined. The arterial oxygen saturation is expressed as a percentage. The technology has been refined to measure fetal arterial oxyhemoglobin saturation during labor.
Pulse oximetry sensors must be calibrated for fetal biological values. In the fetus, normal oxygen saturation is much lower than in the adult or neonate; hemoglobin has a higher affinity for oxygen and is in higher concentration; and there are more capillaries per unit of tissue, higher cardiac output, and a higher heart rate.
In the adult or neonate, pulse oximetry sensors can be attached to fingers, toes, ears, or the bridge of the nose, but such stable placement is not feasible in utero. Further, good contact between sensor and fetal skin is a prerequisite for avoidance of artifacts. This last aspect has presented a sizeable challenge.
Fetal sensors measure reflected light. There is disagreement about the merits of the 2 sensor types, reflectance and transmission. Both include 2 light emitters (for red and infrared light) and a detector. In the transmission sensor (the adult or neonatal type), the light produced by the light-emitting diodes (LED) is picked up by the detector after traversing the interposed tissues. Since tissue interposition is not possible in the fetus, most fetal studies have used reflectance sensors, in which the LED and detector are placed side by side, and the light to be analyzed is reflected by the tissues. This design adds variance depending on the light’s depth of tissue penetration and device position changes.
Placement of the sensor. The Nellcor N-400 includes a reflectance sensor housed in a smooth, pliable head that is advanced through the cervix with the aid of a handle. The handle has a removable stylet to stiffen it during placement.
The sensor is placed against the fetal temple, cheek, or forehead and is held in place by the uterine wall. Placement is similar to that of an internal pressure catheter. Once the stylet is removed, it should not be reinserted.
Because the sensor usually descends and rotates with the fetal head, displacements are frequent and adjustments in sensor placement may be necessary. Placement adjustments can be attempted without the stylet and, if unsuccessful, a new device can be inserted. The Nellcor sensor is not reusable.
The prerequisites for insertion are dilatation of at least 2 cm, ruptured membranes, cephalic presentation, single fetus, gestational age of at least 36 weeks, and no placenta previa.
The manufacturer reports that active genital herpes, HIV, and hepatitis B or E seropositivity preclude fetal pulse oximetry monitoring.
Placement may be impossible when the presenting part is at high station (-3 or above) or low station (+2 or below).
The Nellcor N-400 system has been commercially available in many European countries since 1995, and in Canada since 1998. It was approved for sale in the United States in early 2003.
Question 6Will it improve neonatal outcomes?
Neonatal outcome is the ultimate endpoint in obstetrical care. In the randomized trial by Garite et al,3 there was no difference in neonatal outcome between the groups using or not using fetal pulse oximetry. According to Chua et al,33 FSpO2 levels measured even 10 minutes before delivery have no relation to neonatal outcome.
Leszczynska-Gorzelak et al22 believe FSpO2 is more predictive of neonatal outcome in the first stage than the second. However, Apgar score had no relationship with FSpO2readings in the first or second stage. Butterwegge34 reported 6 cases of FSpO2 below 30% for more than 30 minutes, all with good neonatal outcome, and Alshimmiri et al23 noted that only normal FSpO2 correlates with fetal well-being. Thus, it appears that the NPV of fetal oximetry is of greater practical value than other attributes.
Question 7How precise is it?
The Nellcor system monitors the quality of FSpO2 measurement; no value is displayed if the signal lacks the characteristics of a fetal arterial plethysmographic curve or if contact between sensor and skin is insufficient. Because of fetal movements and other artifacts, posting time is always less than 100%.
In the French multicenter study,25 the mean reliable signal time in the first stage of labor was only 64.7%—even less in the second stage (54%). Signal retention was 67% in the randomized trial by Garite et al. 3
Many artifacts may impede signal acquisition and impact the reliability of a reading:
- The sensor’s position on the fetal head. For example, the difference in FSpO2 readings between the forehead and occiput may be as much as 13.4%. (The sensor is designed to go against the fetal cheek, but may move around.)
- Incomplete sensor-to-skin contact, such as with high fetal head station, -2 or above.
- Marked caput formation.
- Increased intrauterine pressure accompanying contractions, especially at presentation stations of +2 or below (FIGURE 2). FSpO2 monitoring requires detection of fetal pulses, which may be undetectable when the surrounding pressure is high, resulting in a loss of signal.
- Interposition of vernix or fetal hair.
- Presence of meconium, which behaves like a red-light filter, altering the ratio of red to infrared light and resulting in artificially low values.35 This theoretical concern is rejected by Yam et al,36 who did not observe any effect of meconium on FSpO2 values. (When the amniotic fluid is meconium-stained, Carbonne et al37 showed that fetal oximetry is a better predictor of meconium aspiration syndrome than FSB sampling.) The data on the influence of meconium on FSpO2 readings remain contradictory.
All these conditions may impair precision and contribute to poor sensitivity.
FIGURE 2 A weakening signal during pushing
Question 8Is it easy to use?
An Australian survey38 assessed clinicians’ perceptions during placement of the oximetry sensor. Ease of placement was rated as good or excellent in 71% of cases, and the patient’s comfort was rated as good or excellent in 90% of cases. Chua et al39 reported a mean insertion time of 90 seconds, with a reliable signal obtained within 5 minutes in 87% of placements. The French multicenter study25 mentioned earlier concluded that the procedure is satisfactory and easier than FSB sampling. The device itself was harmless to both mother and fetus.40
Potential research directions
Fetal pulse oximetry may be an effective tool in clinical scenarios such as:
- fetal arrhythmias with uninterpretable FHR tracing
- fetal tachycardia associated with maternal fever, thyrotoxicosis, or fetal supraventricular tachycardia, when distinguishing other contributions to tachycardia may be difficult
- fetal bradycardia caused by a complete heart block, which may render EFM undecipherable
- when amnioinfusion is attempted for variable decelerations and it is necessary to differentiate a nonreassuring FHR tracing related to transient in utero stress (eg, umbilical cord compressions) from ominous tracings
Another area not yet addressed is cost-effectiveness beyond the immediate direct costs (approximately $11,000 for the monitor and $150 for each disposable sensor). Also uncertain is whether laboring women will accept the device (how disturbing or invasive it is perceived to be) and how acceptable or applicable it is outside tertiary institutions.
Dr. Vidaeff reports no financial relationships relevant to this article. Dr. Ramin reports grant support from the US National Institutes of Health.
1. Dildy GA. A guest editorial: fetal pulse oximetry. Obstet Gynecol Surv. 2003;58:225-226.
2. Thacker SB, Stroup DF, Peterson HB. Efficacy and safety of intrapartum electronic fetal monitoring: an update. Obstet Gynecol. 1995;86:613-620.
3. Garite TJ, Dildy GA, McNamara H, et al. A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol. 2000;183:1049-1058.
4. Haverkamp AD, Orleans M, Langendoerfer S, et al. A controlled trial of the differential effects of continuous fetal heart rate monitoring in labor: a randomized trial. Am J Obstet Gynecol. 1979;134:399-412.
5. American College of Obstetricians and Gynecologists. Committee opinion: fetal pulse oximetry. Number 258, September 2001. Obstet Gynecol. 2001;98:523-524.
6. Zijlstra WG, Buursma A, Zwart A. Performance of an automated six-wavelength photometer (radiometer OSM3) for routine measurement of hemoglobin derivatives. Clin Chem. 1988;34:149-152.
7. Porath M, Sinah P, Dudenhausen JW, Luttkus AK. Systematic instrumental errors between oxygen saturation analysers in fetal blood during deep hypoxemia. Clin Chim Acta. 2001;307:151-157.
8. Luttkus AK, Lübke M, Büscher U, Porath M, Dudenhausen JW. Accuracy of fetal pulse oximetry. Acta Obstet Gynecol Scand. 2002;81:417-423.
9. Carter AM, Stiller R, König V, Jorgensen JS, Svendsen P, Huch R. Calibration of a reflectance pulse oximeter in fetal lambs for arterial oxygen saturations below 70%. J Soc Gynecol Invest. 1998;5:255-259.
10. McNamara H, Cung CD, Lilford R, Johnson N. Do fetal pulse oximetry readings at delivery correlate with cord blood oxygenation and acidemia? Br J Obstet Gynaecol. 1992;99:735-738.
11. Langer B, Boudier E, Haddad J, Pain L, Schlaeder G. Fetal pulse oximetry during labor of 62 patients. Fetal Diagn Ther. 1996;11:37-45.
12. Harrison AM, Lynch JM, Dean JM, Witte MK. Comparison of simultaneously obtained arterial and capillary blood gases in pediatric intensive care unit patients. Crit Care Med. 1997;25:1904-1908.
13. Nijland R, Jongsma HW, Nijhuis JG, Oeseburg B. Accuracy of fetal pulse oximetry and pitfalls in measurements. Eur J Obstet Gynecol Reprod Biol. 1997;72:S21-S27.
14. Dildy GA, van den Berg PP, Katz M, et al. Intrapartum fetal pulse oximetry: fetal oxygen saturation trends during labor and relation to delivery outcome. Am J Obstet Gynecol. 1994;171:679-684.
15. Nijland R, Jongsma H, Nijhuis J, van den Berg P, Oeseburg B. Arterial saturation in relation to metabolic acidosis in fetal lambs. Am J Obstet Gynecol. 1995;172:810-819.
16. Kühnert M, Seelbach-Göbel B, Butterwegge M. Predictive agreement between fetal arterial oxygen saturation and fetal scalp pH: results of the German multicenter study. Am J Obstet Gynecol. 1998;178:330-335.
17. Salamalekis E, Thomopoulos P, Giannaris D, et al. Computerised intrapartum diagnosis of fetal hypoxia based on heart rate monitoring and fetal pulse oximetry recordings utilizing wavelet analysis and neural networks. Br J Obstet Gynaecol. 2002;109:1137-1142.
18. Bloom SL, Swindle RG, McIntire DD, Leveno KJ. Fetal pulse oximetry: duration of desaturation and intrapartum outcome. Obstet Gynecol. 1999;93:1036-1040.
19. Seelbach-Göbel B, Heupel M, Kühnert M, et al. The prediction of fetal acidosis by means of intrapartum fetal pulse oximetry. Am J Obstet Gynecol. 1999;180:73-81.
20. Gorenberg DM, Patillo C, Hendi P, Rumney PJ, Garite TJ. Fetal pulse oximetry: correlation between oxygen desaturation, duration, and frequency and neonatal outcomes. Am J Obstet Gynecol. 2003;189:136-138.
21. Dildy GA, Thorp JA, Yeast JD, Clark SL. The relationship between oxygen saturation and pH in umbilical blood: implications for intrapartum fetal oxygen saturation monitoring. Am J Obstet Gynecol. 1996;175:682-687.
22. Leszczynska-Gorzelak B, Poniedzialek-Czajkowska E, Oleszczuk J. Fetal blood saturation during the 1st and 2nd stage of labor and its relation to the neonatal outcome. Gynecol Obstet Invest. 2002;54:159-163.
23. Alshimmiri M, Bocking AD, Gagnon R, Natale R, Richardson BS. Prediction of umbilical artery base excess by intrapartum fetal oxygen saturation monitoring. Am J Obstet Gynecol. 1997;177:775-779.
24. Rijnders RJ, Mol BW, Reuwer PJ, Drogtrop AP, Vernooij MM, Visser GH. Is the correlation between fetal oxygen saturation and blood pH sufficient for the use of fetal pulse oximetry? J Matern Fetal Neonatal Med. 2002;11:80-83.
25. Goffinet F, Langer B, Carbonne B, et al. Multicenter study on the clinical value of fetal pulse oximetry. I. Methodologic evaluation. The French Study Group on Fetal Pulse Oximetry. Am J Obstet Gynecol. 1997;177:1238-1246.
26. Schmidt S, Koslowski S, Sierra F, et al. Clinical usefulness of pulse oximetry in the fetus with non-reassuring heart rate pattern? J Perinat Med. 2000;28:298-305.
27. Vitoratos N, Salamalekis E, Saloum J, Makrakis E, Creatsas G. Abnormal fetal heart rate patterns during the active phase of labor and the value of fetal oxygen saturation. J Matern Fetal Neonatal Med. 2002;11:46-49.
28. Stiller R, von Mering R, König V, et al. How well does reflectance pulse oximetry reflect intrapartum fetal acidosis? Am J Obstet Gynecol. 2002;186:1351-1357.
29. Leszczynska-Gorzelak B, Poniedzialek-Czajkowska E, Zych I, Grzechnik M, Oleszczuk J. The usefulness of the intrapartum fetal pulse oximetry in anticipating the neonatal outcome. Ginekol Pol. 2001;72:1183-1188.
30. Nikolov A, Dimitrov A, Vakrilkova L, Iarkova N. Fetal oxygen saturation during normal delivery. Akush Ginekol. 2000;40:3-6.
31. Goldaber KG, Gilstrap LC III, Leveno K, Dax JS, McIntire DD. Pathologic fetal acidemia. Obstet Gynecol. 1991;78:1103-1107.
32. Low JA, Victory R, Derrick EJ. Predictive value of electronic fetal monitoring for intra-partum fetal asphyxia and metabolic acidosis. Obstet Gynecol. 1999;93:285-291.
33. Chua S, Yeong SM, Razvi K, Arulkumaran S. Fetal oxygen saturation during labour. Br J Obstet Gynaecol. 1997;104:1080-1083.
34. Butterwegge M. Fetal pulse oximetry and non-reassuring heart rate. Eur J Obstet Gynecol Reprod Biol. 1997;72:S63-S66.
35. Johnson N, Johnson VA, Bannister J, McNamara H. The effect of meconium on neonatal and fetal reflectance pulse oximetry. J Perinat Med. 1990;18:351-355.
36. Yam J, Chua S, Arulkumaran S. Intrapartum pulse oximetry: Part 1: Principles and technical issues. Obstet Gynecol Surv. 2000;55:163-172.
37. Carbonne B, Cudeville C, Sivan H, Cabrol D, Papiernik E. Fetal oxygen saturation measured by pulse oximetry during labor with clear and meconium-stained amniotic fluid. Eur J Obstet Gynecol Reprod Biol. 1997;72:S51-S55.
38. East CE, Colditz PB. Clinicians’ perceptions of placing a fetal oximetry sensor. J Qual Clin Pract. 2000;20:161-163.
39. Chua S, Yam J, Razvi K, Yeong SM, Arulkumaran S. Intrapartum fetal oxygen saturation monitoring in a busy labour ward. Eur J Obstet Gynecol Reprod Biol. 1999;82:185-189.
40. Luttkus AK, Friedmann W, Thomas S, Dimer JA, Dudenhausen JW. The safety of fetal pulse oximetry in parturients requiring fetal scalp blood sample. Obstet Gynecol. 1997;90:533-537.
1. Dildy GA. A guest editorial: fetal pulse oximetry. Obstet Gynecol Surv. 2003;58:225-226.
2. Thacker SB, Stroup DF, Peterson HB. Efficacy and safety of intrapartum electronic fetal monitoring: an update. Obstet Gynecol. 1995;86:613-620.
3. Garite TJ, Dildy GA, McNamara H, et al. A multicenter controlled trial of fetal pulse oximetry in the intrapartum management of nonreassuring fetal heart rate patterns. Am J Obstet Gynecol. 2000;183:1049-1058.
4. Haverkamp AD, Orleans M, Langendoerfer S, et al. A controlled trial of the differential effects of continuous fetal heart rate monitoring in labor: a randomized trial. Am J Obstet Gynecol. 1979;134:399-412.
5. American College of Obstetricians and Gynecologists. Committee opinion: fetal pulse oximetry. Number 258, September 2001. Obstet Gynecol. 2001;98:523-524.
6. Zijlstra WG, Buursma A, Zwart A. Performance of an automated six-wavelength photometer (radiometer OSM3) for routine measurement of hemoglobin derivatives. Clin Chem. 1988;34:149-152.
7. Porath M, Sinah P, Dudenhausen JW, Luttkus AK. Systematic instrumental errors between oxygen saturation analysers in fetal blood during deep hypoxemia. Clin Chim Acta. 2001;307:151-157.
8. Luttkus AK, Lübke M, Büscher U, Porath M, Dudenhausen JW. Accuracy of fetal pulse oximetry. Acta Obstet Gynecol Scand. 2002;81:417-423.
9. Carter AM, Stiller R, König V, Jorgensen JS, Svendsen P, Huch R. Calibration of a reflectance pulse oximeter in fetal lambs for arterial oxygen saturations below 70%. J Soc Gynecol Invest. 1998;5:255-259.
10. McNamara H, Cung CD, Lilford R, Johnson N. Do fetal pulse oximetry readings at delivery correlate with cord blood oxygenation and acidemia? Br J Obstet Gynaecol. 1992;99:735-738.
11. Langer B, Boudier E, Haddad J, Pain L, Schlaeder G. Fetal pulse oximetry during labor of 62 patients. Fetal Diagn Ther. 1996;11:37-45.
12. Harrison AM, Lynch JM, Dean JM, Witte MK. Comparison of simultaneously obtained arterial and capillary blood gases in pediatric intensive care unit patients. Crit Care Med. 1997;25:1904-1908.
13. Nijland R, Jongsma HW, Nijhuis JG, Oeseburg B. Accuracy of fetal pulse oximetry and pitfalls in measurements. Eur J Obstet Gynecol Reprod Biol. 1997;72:S21-S27.
14. Dildy GA, van den Berg PP, Katz M, et al. Intrapartum fetal pulse oximetry: fetal oxygen saturation trends during labor and relation to delivery outcome. Am J Obstet Gynecol. 1994;171:679-684.
15. Nijland R, Jongsma H, Nijhuis J, van den Berg P, Oeseburg B. Arterial saturation in relation to metabolic acidosis in fetal lambs. Am J Obstet Gynecol. 1995;172:810-819.
16. Kühnert M, Seelbach-Göbel B, Butterwegge M. Predictive agreement between fetal arterial oxygen saturation and fetal scalp pH: results of the German multicenter study. Am J Obstet Gynecol. 1998;178:330-335.
17. Salamalekis E, Thomopoulos P, Giannaris D, et al. Computerised intrapartum diagnosis of fetal hypoxia based on heart rate monitoring and fetal pulse oximetry recordings utilizing wavelet analysis and neural networks. Br J Obstet Gynaecol. 2002;109:1137-1142.
18. Bloom SL, Swindle RG, McIntire DD, Leveno KJ. Fetal pulse oximetry: duration of desaturation and intrapartum outcome. Obstet Gynecol. 1999;93:1036-1040.
19. Seelbach-Göbel B, Heupel M, Kühnert M, et al. The prediction of fetal acidosis by means of intrapartum fetal pulse oximetry. Am J Obstet Gynecol. 1999;180:73-81.
20. Gorenberg DM, Patillo C, Hendi P, Rumney PJ, Garite TJ. Fetal pulse oximetry: correlation between oxygen desaturation, duration, and frequency and neonatal outcomes. Am J Obstet Gynecol. 2003;189:136-138.
21. Dildy GA, Thorp JA, Yeast JD, Clark SL. The relationship between oxygen saturation and pH in umbilical blood: implications for intrapartum fetal oxygen saturation monitoring. Am J Obstet Gynecol. 1996;175:682-687.
22. Leszczynska-Gorzelak B, Poniedzialek-Czajkowska E, Oleszczuk J. Fetal blood saturation during the 1st and 2nd stage of labor and its relation to the neonatal outcome. Gynecol Obstet Invest. 2002;54:159-163.
23. Alshimmiri M, Bocking AD, Gagnon R, Natale R, Richardson BS. Prediction of umbilical artery base excess by intrapartum fetal oxygen saturation monitoring. Am J Obstet Gynecol. 1997;177:775-779.
24. Rijnders RJ, Mol BW, Reuwer PJ, Drogtrop AP, Vernooij MM, Visser GH. Is the correlation between fetal oxygen saturation and blood pH sufficient for the use of fetal pulse oximetry? J Matern Fetal Neonatal Med. 2002;11:80-83.
25. Goffinet F, Langer B, Carbonne B, et al. Multicenter study on the clinical value of fetal pulse oximetry. I. Methodologic evaluation. The French Study Group on Fetal Pulse Oximetry. Am J Obstet Gynecol. 1997;177:1238-1246.
26. Schmidt S, Koslowski S, Sierra F, et al. Clinical usefulness of pulse oximetry in the fetus with non-reassuring heart rate pattern? J Perinat Med. 2000;28:298-305.
27. Vitoratos N, Salamalekis E, Saloum J, Makrakis E, Creatsas G. Abnormal fetal heart rate patterns during the active phase of labor and the value of fetal oxygen saturation. J Matern Fetal Neonatal Med. 2002;11:46-49.
28. Stiller R, von Mering R, König V, et al. How well does reflectance pulse oximetry reflect intrapartum fetal acidosis? Am J Obstet Gynecol. 2002;186:1351-1357.
29. Leszczynska-Gorzelak B, Poniedzialek-Czajkowska E, Zych I, Grzechnik M, Oleszczuk J. The usefulness of the intrapartum fetal pulse oximetry in anticipating the neonatal outcome. Ginekol Pol. 2001;72:1183-1188.
30. Nikolov A, Dimitrov A, Vakrilkova L, Iarkova N. Fetal oxygen saturation during normal delivery. Akush Ginekol. 2000;40:3-6.
31. Goldaber KG, Gilstrap LC III, Leveno K, Dax JS, McIntire DD. Pathologic fetal acidemia. Obstet Gynecol. 1991;78:1103-1107.
32. Low JA, Victory R, Derrick EJ. Predictive value of electronic fetal monitoring for intra-partum fetal asphyxia and metabolic acidosis. Obstet Gynecol. 1999;93:285-291.
33. Chua S, Yeong SM, Razvi K, Arulkumaran S. Fetal oxygen saturation during labour. Br J Obstet Gynaecol. 1997;104:1080-1083.
34. Butterwegge M. Fetal pulse oximetry and non-reassuring heart rate. Eur J Obstet Gynecol Reprod Biol. 1997;72:S63-S66.
35. Johnson N, Johnson VA, Bannister J, McNamara H. The effect of meconium on neonatal and fetal reflectance pulse oximetry. J Perinat Med. 1990;18:351-355.
36. Yam J, Chua S, Arulkumaran S. Intrapartum pulse oximetry: Part 1: Principles and technical issues. Obstet Gynecol Surv. 2000;55:163-172.
37. Carbonne B, Cudeville C, Sivan H, Cabrol D, Papiernik E. Fetal oxygen saturation measured by pulse oximetry during labor with clear and meconium-stained amniotic fluid. Eur J Obstet Gynecol Reprod Biol. 1997;72:S51-S55.
38. East CE, Colditz PB. Clinicians’ perceptions of placing a fetal oximetry sensor. J Qual Clin Pract. 2000;20:161-163.
39. Chua S, Yam J, Razvi K, Yeong SM, Arulkumaran S. Intrapartum fetal oxygen saturation monitoring in a busy labour ward. Eur J Obstet Gynecol Reprod Biol. 1999;82:185-189.
40. Luttkus AK, Friedmann W, Thomas S, Dimer JA, Dudenhausen JW. The safety of fetal pulse oximetry in parturients requiring fetal scalp blood sample. Obstet Gynecol. 1997;90:533-537.