User login
Variation in Printed Handoff Documents
Handoffs among hospital providers are highly error prone and can result in serious morbidity and mortality. Best practices for verbal handoffs have been described[1, 2, 3, 4] and include conducting verbal handoffs face to face, providing opportunities for questions, having the receiver perform a readback, as well as specific content recommendations including action items. Far less research has focused on best practices for printed handoff documents,[5, 6] despite the routine use of written handoff tools as a reference by on‐call physicians.[7, 8] Erroneous or outdated information on the written handoff can mislead on‐call providers, potentially leading to serious medical errors.
In their most basic form, printed handoff documents list patients for whom a provider is responsible. Typically, they also contain demographic information, reason for hospital admission, and a task list for each patient. They may also contain more detailed information on patient history, hospital course, and/or care plan, and may vary among specialties.[9] They come in various forms, ranging from index cards with handwritten notes, to word‐processor or spreadsheet documents, to printed documents that are autopopulated from the electronic health record (EHR).[2] Importantly, printed handoff documents supplement the verbal handoff by allowing receivers to follow along as patients are presented. The concurrent use of written and verbal handoffs may improve retention of clinical information as compared with either alone.[10, 11]
The Joint Commission requires an institutional approach to patient handoffs.[12] The requirements state that handoff communication solutions should take a standardized form, but they do not provide details regarding what data elements should be included in printed or verbal handoffs. Accreditation Council for Graduate Medical Education Common Program Requirements likewise require that residents must become competent in patient handoffs[13] but do not provide specific details or measurement tools. Absent widely accepted guidelines, decisions regarding which elements to include in printed handoff documents are currently made at an individual or institutional level.
The I‐PASS study is a federally funded multi‐institutional project that demonstrated a decrease in medical errors and preventable adverse events after implementation of a standardized resident handoff bundle.[14, 15] The I‐PASS Study Group developed a bundle of handoff interventions, beginning with a handoff and teamwork training program (based in part on TeamSTEPPS [Team Strategies and Tools to Enhance Performance and Patient Safety]),[16] a novel verbal mnemonic, I‐PASS (Illness Severity, Patient Summary, Action List, Situation Awareness and Contingency Planning, and Synthesis by Receiver),[17] and changes to the verbal handoff process, in addition to several other elements.
We hypothesized that developing a standardized printed handoff template would reinforce the handoff training and enhance the value of the verbal handoff process changes. Given the paucity of data on best printed handoff practices, however, we first conducted a needs assessment to identify which data elements were currently contained in printed handoffs across sites, and to allow an expert panel to make recommendations for best practices.
METHODS
I‐PASS Study sites included 9 pediatric residency programs at academic medical centers from across North America. Programs were identified through professional networks and invited to participate. The nonintensive care unit hospitalist services at these medical centers are primarily staffed by residents and medical students with attending supervision. At 1 site, nurse practitioners also participate in care. Additional details about study sites can be found in the study descriptions previously published.[14, 15] All sites received local institutional review board approval.
We began by inviting members of the I‐PASS Education Executive Committee (EEC)[14] to build a collective, comprehensive list of possible data elements for printed handoff documents. This committee included pediatric residency program directors, pediatric hospitalists, education researchers, health services researchers, and patient safety experts. We obtained sample handoff documents from pediatric hospitalist services at each of 9 institutions in the United States and Canada (with protected health information redacted). We reviewed these sample handoff documents to characterize their format and to determine what discrete data elements appeared in each site's printed handoff document. Presence or absence of each data element across sites was tabulated. We also queried sites to determine the feasibility of including elements that were not presently included.
Subsequently, I‐PASS site investigators led structured group interviews at participating sites to gather additional information about handoff practices at each site. These structured group interviews included diverse representation from residents, faculty, and residency program leadership, as well as hospitalists and medical students, to ensure the comprehensive acquisition of information regarding site‐specific characteristics. Each group provided answers to a standardized set of open‐ended questions that addressed current practices, handoff education, simulation use, team structure, and the nature of current written handoff tools, if applicable, at each site. One member of the structured group interview served as a scribe and created a document that summarized the content of the structured group interview meeting and answers to the standardized questions.
Consensus on Content
The initial data collection also included a multivote process[18] of the full I‐PASS EEC to help prioritize data elements. Committee members brainstormed a list of all possible data elements for a printed handoff document. Each member (n=14) was given 10 votes to distribute among the elements. Committee members could assign more than 1 vote to an element to emphasize its importance.
The results of this process as well as the current data elements included in each printed handoff tool were reviewed by a subgroup of the I‐PASS EEC. These expert panel members participated in a series of conference calls during which they tabulated categorical information, reviewed narrative comments, discussed existing evidence, and conducted simple content analysis to identify areas of concordance or discordance. Areas of discordance were discussed by the committee. Disagreements were resolved with group consensus with attention to published evidence or best practices, if available.
Elements were divided into those that were essential (unanimous consensus, no conflicting literature) and those that were recommended (majority supported inclusion of element, no conflicting literature). Ratings were assigned using the American College of Cardiology/American Heart Association framework for practice guidelines,[19] in which each element is assigned a classification (I=effective, II=conflicting evidence/opinion, III=not effective) and a level of evidence to support that classification (A=multiple large randomized controlled trials, B=single randomized trial, or nonrandomized studies, C=expert consensus).
The expert panel reached consensus, through active discussion, on a list of data elements that should be included in an ideal printed handoff document. Elements were chosen based on perceived importance, with attention to published best practices[1, 16] and the multivoting results. In making recommendations, consideration was given to whether data elements could be electronically imported into the printed handoff document from the EHR, or whether they would be entered manually. The potential for serious medical errors due to possible errors in manual entry of data was an important aspect of recommendations made. The list of candidate elements was then reviewed by a larger group of investigators from the I‐PASS Education Executive Committee and Coordinating Council for additional input.
The panel asked site investigators from each participating hospital to gather data on the feasibility of redesigning the printed handoff at that hospital to include each recommended element. Site investigators reported whether each element was already included, possible to include but not included currently, or not currently possible to include within that site's printed handoff tool. Site investigators also reported how data elements were populated in their handoff documents, with options including: (1) autopopulated from administrative data (eg, pharmacy‐entered medication list, demographic data entered by admitting office), (2) autoimported from physicians' free‐text entries elsewhere in the EHR (eg, progress notes), (3) free text entered specifically for the printed handoff, or (4) not applicable (element cannot be included).
RESULTS
Nine programs (100%) provided data on the structure and contents of their printed handoff documents. We found wide variation in structure across the 9 sites. Three sites used a word‐processorbased document that required manual entry of all data elements. The other 6 institutions had a direct link with the EHR to enable autopopulation of between 10 and 20 elements on the printed handoff document.
The content of written handoff documents, as well as the sources of data included in them (present or future), likewise varied substantially across sites (Table 1). Only 4 data elements (name, age, weight, and a list of medications) were universally included at all 9 sites. Among the 6 institutions that linked the printed handoff to the EHR, there was also substantial variation in which elements were autoimported. Only 7 elements were universally autoimported at these 6 sites: patient name, medical record number, room number, weight, date of birth, age, and date of admission. Two elements from the original brainstorming were not presently included in any sites' documents (emergency contact and primary language).
| Data Elements | Sites With Data Element Included at Initial Needs Assessment (Out of Nine Sites) | Data Source (Current or Anticipated) | ||
|---|---|---|---|---|
| Autoimported* | Manually Entered | Not Applicable | ||
| ||||
| Name | 9 | 6 | 3 | 0 |
| Medical record number | 8 | 6 | 3 | 0 |
| Room number | 8 | 6 | 3 | 0 |
| Allergies | 6 | 4 | 5 | 0 |
| Weight | 9 | 6 | 3 | 0 |
| Age | 9 | 6 | 3 | 0 |
| Date of birth | 6 | 6 | 3 | 0 |
| Admission date | 8 | 6 | 3 | 0 |
| Attending name | 5 | 4 | 5 | 0 |
| Team/service | 7 | 4 | 5 | 0 |
| Illness severity | 1 | 0 | 9 | 0 |
| Patient summary | 8 | 0 | 9 | 0 |
| Action items | 8 | 0 | 9 | 0 |
| Situation monitoring/contingency plan | 5 | 0 | 9 | 0 |
| Medication name | 9 | 4 | 5 | 0 |
| Medication name and dose/route/frequency | 4 | 4 | 5 | 0 |
| Code status | 2 | 2 | 7 | 0 |
| Labs | 6 | 5 | 4 | 0 |
| Access | 2 | 2 | 7 | 0 |
| Ins/outs | 2 | 4 | 4 | 1 |
| Primary language | 0 | 3 | 6 | 0 |
| Vital signs | 3 | 4 | 4 | 1 |
| Emergency contact | 0 | 2 | 7 | 0 |
| Primary care provider | 4 | 4 | 5 | 0 |
Nine institutions (100%) conducted structured group interviews, ranging in size from 4 to 27 individuals with a median of 5 participants. The documents containing information from each site were provided to the authors. The authors then tabulated categorical information, reviewed narrative comments to understand current institutional practices, and conducted simple content analysis to identify areas of concordance or discordance, particularly with respect to data elements and EHR usage. Based on the results of the printed handoff document review and structured group interviews, with additional perspectives provided by the I‐PASS EEC, the expert panel came to consensus on a list of 23 elements that should be included in printed handoff documents, including 15 essential data elements and 8 additional recommended elements (Table 2).
|
| Essential Elements |
| Patient identifiers |
| Patient name (class I, level of evidence C) |
| Medical record number (class I, level of evidence C) |
| Date of birth (class I, level of evidence C) |
| Hospital service identifiers |
| Attending name (class I, level of evidence C) |
| Team/service (class I, level of evidence C) |
| Room number (class I, level of evidence C) |
| Admission date (class I, level of evidence C) |
| Age (class I, level of evidence C) |
| Weight (class I, level of evidence C) |
| Illness severity (class I, level of evidence B)[20, 21] |
| Patient summary (class I, level of evidence B)[21, 22] |
| Action items (class I, level of evidence B) [21, 22] |
| Situation awareness/contingency planning (class I, level of evidence B) [21, 22] |
| Allergies (class I, level of evidence C) |
| Medications |
| Autopopulation of medications (class I, level of evidence B)[22, 23, 24] |
| Free‐text entry of medications (class IIa, level of evidence C) |
| Recommended elements |
| Primary language (class IIa, level of evidence C) |
| Emergency contact (class IIa, level of evidence C) |
| Primary care provider (class IIa, level of evidence C) |
| Code status (class IIb, level of evidence C) |
| Labs (class IIa, level of evidence C) |
| Access (class IIa, level of evidence C) |
| Ins/outs (class IIa, level of evidence C) |
| Vital signs (class IIa, level of evidence C) |
Evidence ratings[19] of these elements are included. Several elements are classified as I‐B (effective, nonrandomized studies) based on either studies of individual elements, or greater than 1 study of bundled elements that could reasonably be extrapolated. These include Illness severity,[20, 21] patient summary,[21, 22] action items[21, 22] (to do lists), situation awareness and contingency plan,[21, 22] and medications[22, 23, 24] with attention to importing from the EHR. Medications entered as free text were classified as IIa‐C because of risk and potential significance of errors; in particular there was concern that transcription errors, errors of omission, or errors of commission could potentially lead to patient harms. The remaining essential elements are classified as I‐C (effective, expert consensus). Of note, date of birth was specifically included as a patient identifier, distinct from age, which was felt to be useful as a descriptor (often within a one‐liner or as part of the patient summary).
The 8 recommended elements were elements for which there was not unanimous agreement on inclusion, but the majority of the panel felt they should be included. These elements were classified as IIa‐C, with 1 exception. Code status generated significant controversy among the group. After extensive discussion among the group and consideration of safety, supervision, educational, and pediatric‐specific considerations, all members of the group agreed on the categorization as a recommended element; it is classified as IIb‐C.
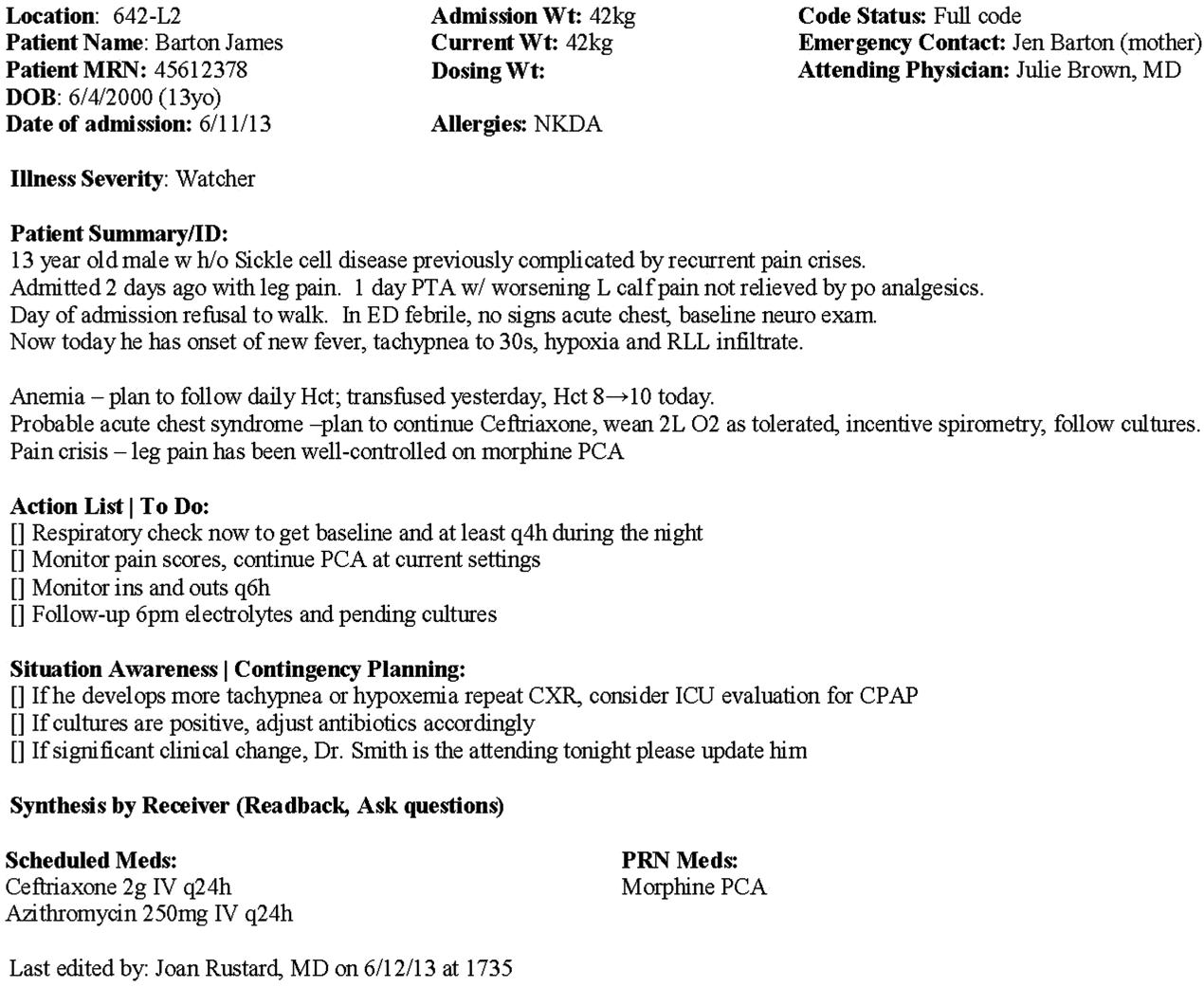
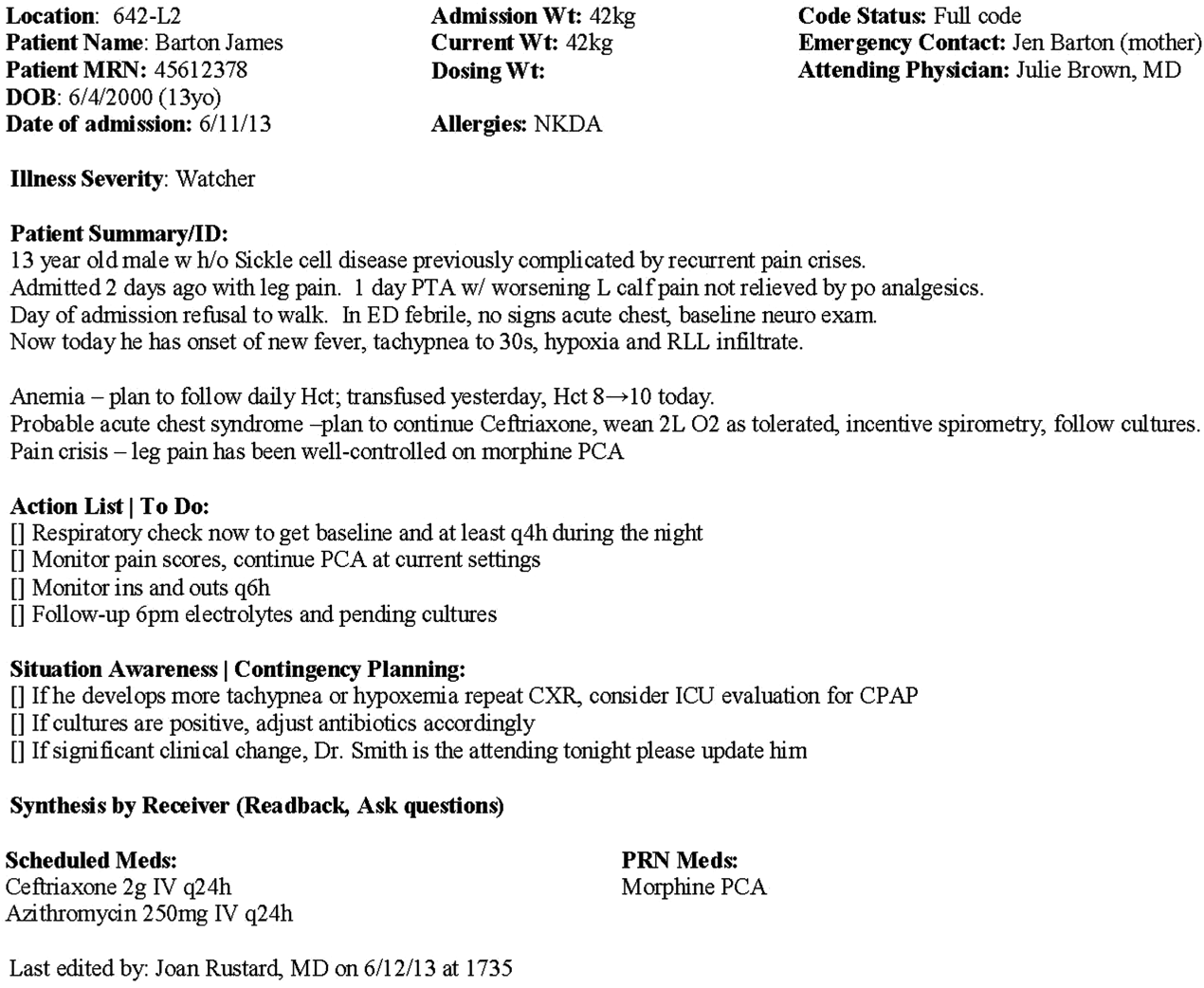
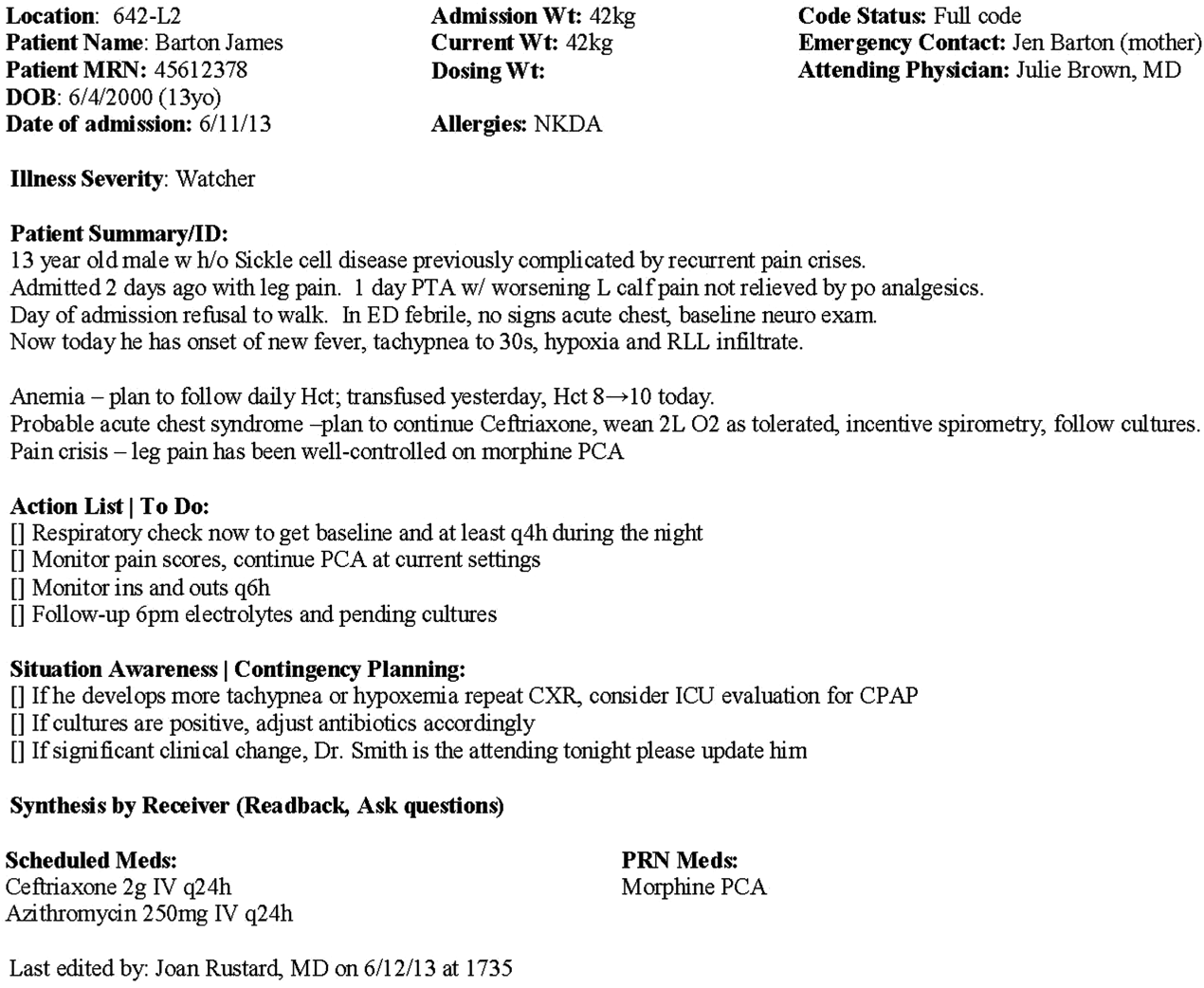
All members of the group agreed that data elements should be directly imported from the EHR whenever possible. Finally, members agreed that the elements that make up the I‐PASS mnemonic (illness severity, patient summary, action items, situation awareness/contingency planning) should be listed in that order whenever possible. A sample I‐PASS‐compliant printed handoff document is shown Figure 1.
DISCUSSION
We identified substantial variability in the structure and content of printed handoff documents used by 9 pediatric hospitalist teaching services, reflective of a lack of standardization. We found that institutional printed handoff documents shared some demographic elements (eg, name, room, medical record number) but also varied in clinical content (eg, vital signs, lab tests, code status). Our expert panel developed a list of 15 essential and 8 recommended data elements for printed handoff documents. Although this is a large number of fields, the majority of the essential fields were already included by most sites, and many are basic demographic identifiers. Illness severity is the 1 essential field that was not routinely included; however, including this type of overview is consistently recommended[2, 4] and supported by evidence,[20, 21] and contributes to building a shared mental model.[16] We recommend the categories of stable/watcher/unstable.[17]
Several prior single‐center studies have found that introducing a printed handoff document can lead to improvements in workflow, communication, and patient safety. In an early study, Petersen et al.[25] showed an association between use of a computerized sign‐out program and reduced odds of preventable adverse events during periods of cross‐coverage. Wayne et al.[26] reported fewer perceived inaccuracies in handoff documents as well as improved clarity at the time of transfer, supporting the role for standardization. Van Eaton et al.[27] demonstrated rapid uptake and desirability of a computerized handoff document, which combined autoimportation of information from an EHR with resident‐entered patient details, reflecting the importance of both data sources. In addition, they demonstrated improvements in both the rounding and sign‐out processes.[28]
Two studies specifically reported the increased use of specific fields after implementation. Payne et al. implemented a Web‐based handoff tool and documented significant increases in the number of handoffs containing problem lists, medication lists, and code status, accompanied by perceived improvements in quality of handoffs and fewer near‐miss events.[24] Starmer et al. found that introduction of a resident handoff bundle that included a printed handoff tool led to reduction in medical errors and adverse events.[22] The study group using the tool populated 11 data elements more often after implementation, and introduction of this printed handoff tool in particular was associated with reductions in written handoff miscommunications. Neither of these studies included subanalysis to indicate which data elements may have been most important.
In contrast to previous single‐institution studies, our recommendations for a printed handoff template come from evaluations of tools and discussions with front line providers across 9 institutions. We had substantial overlap with data elements recommended by Van Eaton et al.[27] However, there were several areas in which we did not have overlap with published templates including weight, ins/outs, primary language, emergency contact information, or primary care provider. Other published handoff tools have been highly specialized (eg, for cardiac intensive care) or included many fewer data elements than our group felt were essential. These differences may reflect the unique aspects of caring for pediatric patients (eg, need for weights) and the absence of defined protocols for many pediatric conditions. In addition, the level of detail needed for contingency planning may vary between teaching and nonteaching services.
Resident physicians may provide valuable information in the development of standardized handoff documents. Clark et al.,[29] at Virginia Mason University, utilized resident‐driven continuous quality improvement processes including real‐time feedback to implement an electronic template. They found that engagement of both senior leaders and front‐line users was an important component of their success in uptake. Our study utilized residents as essential members of structured group interviews to ensure that front‐line users' needs were represented as recommendations for a printed handoff tool template were developed.
As previously described,[17] our study group had identified several key data elements that should be included in verbal handoffs: illness severity, a patient summary, a discrete action list, situation awareness/contingency planning, and a synthesis by receiver. With consideration of the multivoting results as well as known best practices,[1, 4, 12] the expert panel for this study agreed that each of these elements should also be highlighted in the printed template to ensure consistency between the printed document and the verbal handoff, and to have each reinforce the other. On the printed handoff tool, the final S in the I‐PASS mnemonic (synthesis by receiver) cannot be prepopulated, but considering the importance of this step,[16, 30, 31, 32] it should be printed as synthesis by receiver to serve as a text‐reminder to both givers and receivers.
The panel also felt, however, that the printed handoff document should provide additional background information not routinely included in a verbal handoff. It should serve as a reference tool both at the time of verbal handoff and throughout the day and night, and therefore should include more comprehensive information than is necessary or appropriate to convey during the verbal handoff. We identified 10 data elements that are essential in a printed handoff document in addition to the I‐PASS elements (Table 2).
Patient demographic data elements, as well as team assignments and attending physician, were uniformly supported for inclusion. The medication list was viewed as essential; however, the panel also recognized the potential for medical errors due to inaccuracies in the medication list. In particular, there was concern that including all fields of a medication order (drug, dose, route, frequency) would result in handoffs containing a high proportion of inaccurate information, particularly for complex patients whose medication regimens may vary over the course of hospitalization. Therefore, the panel agreed that if medication lists were entered manually, then only the medication name should be included as they did not wish to perpetuate inaccurate or potentially harmful information. If medication lists were autoimported from an EHR, then they should include drug name, dose, route, and frequency if possible.
In the I‐PASS study,[15] all institutions implemented printed handoff documents that included fields for the essential data elements. After implementation, there was a significant increase in completion of all essential fields. Although there is limited evidence to support any individual data element, increased usage of these elements was associated with the overall study finding of decreased rates of medical errors and preventable adverse events.
EHRs have the potential to help standardize printed handoff documents[5, 6, 33, 34, 35]; all participants in our study agreed that printed handoff documents should ideally be linked with the EHR and should autoimport data wherever appropriate. Manually populated (eg, word processor‐ or spreadsheet‐based) handoff tools have important limitations, particularly related to the potential for typographical errors as well as accidental omission of data fields, and lead to unnecessary duplication of work (eg, re‐entering data already included in a progress note) that can waste providers' time. It was also acknowledged that word processor‐ or spreadsheet‐based documents may have flexibility that is lacking in EHR‐based handoff documents. For example, formatting can more easily be adjusted to increase the number of patients per printed page. As technology advances, printed documents may be phased out in favor of EHR‐based on‐screen reports, which by their nature would be more accurate due to real‐time autoupdates.
In making recommendations about essential versus recommended items for inclusion in the printed handoff template, the only data element that generated controversy among our experts was code status. Some felt that it should be included as an essential element, whereas others did not. We believe that this was unique to our practice in pediatric hospital ward settings, as codes in most pediatric ward settings are rare. Among the concerns expressed with including code status for all patients were that residents might assume patients were full‐code without verifying. The potential inaccuracy created by this might have severe implications. Alternatively, residents might feel obligated to have code discussions with all patients regardless of severity of illness, which may be inappropriate in a pediatric population. Several educators expressed concerns about trainees having unsupervised code‐status conversations with families of pediatric patients. Conversely, although codes are rare in pediatric ward settings, concerns were raised that not including code status could be problematic during these rare but critically important events. Other fields, such as weight, might have less relevance for an adult population in which emergency drug doses are standardized.
Limitations
Our study has several limitations. We only collected data from hospitalist services at pediatric sites. It is likely that providers in other specialties would have specific data elements they felt were essential (eg, postoperative day, code status). Our methodology was expert consensus based, driven by data collection from sites that were already participating in the I‐PASS study. Although the I‐PASS study demonstrated decreased rates of medical errors and preventable adverse events with inclusion of these data elements as part of a bundle, future research will be required to evaluate whether some of these items are more important than others in improving written communication and ultimately patient safety. In spite of these limitations, our work represents an important starting point for the development of standards for written handoff documents that should be used in patient handoffs, particularly those generated from EHRs.
CONCLUSIONS
In this article we describe the results of a needs assessment that informed expert consensus‐based recommendations for data elements to include in a printed handoff document. We recommend that pediatric programs include the elements identified as part of a standardized written handoff tool. Although many of these elements are also applicable to other specialties, future work should be conducted to adapt the printed handoff document elements described here for use in other specialties and settings. Future studies should work to validate the importance of these elements, studying the manner in which their inclusion affects the quality of written handoffs, and ultimately patient safety.
Acknowledgements
Members of the I‐PASS Study Education Executive Committee who contributed to this manuscript include: Boston Children's Hospital/Harvard Medical School (primary site) (Christopher P. Landrigan, MD, MPH, Elizabeth L. Noble, BA. Theodore C. Sectish, MD. Lisa L. Tse, BA). Cincinnati Children's Hospital Medical Center/University of Cincinnati College of Medicine (Jennifer K. O'Toole, MD, MEd). Doernbecher Children's Hospital/Oregon Health and Science University (Amy J. Starmer, MD, MPH). Hospital for Sick Children/University of Toronto (Zia Bismilla, MD. Maitreya Coffey, MD). Lucile Packard Children's Hospital/Stanford University (Lauren A. Destino, MD. Jennifer L. Everhart, MD. Shilpa J. Patel, MD [currently at Kapi'olani Children's Hospital/University of Hawai'i School of Medicine]). National Capital Consortium (Jennifer H. Hepps, MD. Joseph O. Lopreiato, MD, MPH. Clifton E. Yu, MD). Primary Children's Medical Center/University of Utah (James F. Bale, Jr., MD. Adam T. Stevenson, MD). St. Louis Children's Hospital/Washington University (F. Sessions Cole, MD). St. Christopher's Hospital for Children/Drexel University College of Medicine (Sharon Calaman, MD. Nancy D. Spector, MD). Benioff Children's Hospital/University of California San Francisco School of Medicine (Glenn Rosenbluth, MD. Daniel C. West, MD).
Additional I‐PASS Study Group members who contributed to this manuscript include April D. Allen, MPA, MA (Heller School for Social Policy and Management, Brandeis University, previously affiliated with Boston Children's Hospital), Madelyn D. Kahana, MD (The Children's Hospital at Montefiore/Albert Einstein College of Medicine, previously affiliated with Lucile Packard Children's Hospital/Stanford University), Robert S. McGregor, MD (Akron Children's Hospital/Northeast Ohio Medical University, previously affiliated with St. Christopher's Hospital for Children/Drexel University), and John S. Webster, MD, MBA, MS (Webster Healthcare Consulting Inc., formerly of the Department of Defense).
Members of the I‐PASS Study Group include individuals from the institutions listed below as follows: Boston Children's Hospital/Harvard Medical School (primary site): April D. Allen, MPA, MA (currently at Heller School for Social Policy and Management, Brandeis University), Angela M. Feraco, MD, Christopher P. Landrigan, MD, MPH, Elizabeth L. Noble, BA, Theodore C. Sectish, MD, Lisa L. Tse, BA. Brigham and Women's Hospital (data coordinating center): Anuj K. Dalal, MD, Carol A. Keohane, BSN, RN, Stuart Lipsitz, PhD, Jeffrey M. Rothschild, MD, MPH, Matt F. Wien, BS, Catherine S. Yoon, MS, Katherine R. Zigmont, BSN, RN. Cincinnati Children's Hospital Medical Center/University of Cincinnati College of Medicine: Javier Gonzalez del Rey, MD, MEd, Jennifer K. O'Toole, MD, MEd, Lauren G. Solan, MD. Doernbecher Children's Hospital/Oregon Health and Science University: Megan E. Aylor, MD, Amy J. Starmer, MD, MPH, Windy Stevenson, MD, Tamara Wagner, MD. Hospital for Sick Children/University of Toronto: Zia Bismilla, MD, Maitreya Coffey, MD, Sanjay Mahant, MD, MSc. Lucile Packard Children's Hospital/Stanford University: Rebecca L. Blankenburg, MD, MPH, Lauren A. Destino, MD, Jennifer L. Everhart, MD, Madelyn Kahana, MD, Shilpa J. Patel, MD (currently at Kapi'olani Children's Hospital/University of Hawaii School of Medicine). National Capital Consortium: Jennifer H. Hepps, MD, Joseph O. Lopreiato, MD, MPH, Clifton E. Yu, MD. Primary Children's Hospital/University of Utah: James F. Bale, Jr., MD, Jaime Blank Spackman, MSHS, CCRP, Rajendu Srivastava, MD, FRCP(C), MPH, Adam Stevenson, MD. St. Louis Children's Hospital/Washington University: Kevin Barton, MD, Kathleen Berchelmann, MD, F. Sessions Cole, MD, Christine Hrach, MD, Kyle S. Schultz, MD, Michael P. Turmelle, MD, Andrew J. White, MD. St. Christopher's Hospital for Children/Drexel University: Sharon Calaman, MD, Bronwyn D. Carlson, MD, Robert S. McGregor, MD (currently at Akron Children's Hospital/Northeast Ohio Medical University), Vahideh Nilforoshan, MD, Nancy D. Spector, MD. and Benioff Children's Hospital/University of California San Francisco School of Medicine: Glenn Rosenbluth, MD, Daniel C. West, MD. Dorene Balmer, PhD, RD, Carol L. Carraccio, MD, MA, Laura Degnon, CAE, and David McDonald, and Alan Schwartz PhD serve the I‐PASS Study Group as part of the IIPE. Karen M. Wilson, MD, MPH serves the I‐PASS Study Group as part of the advisory board from the PRIS Executive Council. John Webster served the I‐PASS Study Group and Education Executive Committee as a representative from TeamSTEPPS.
Disclosures: The I‐PASS Study was primarily supported by the US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation (1R18AE000029‐01). The opinions and conclusions expressed herein are solely those of the author(s) and should not be constructed as representing the opinions or policy of any agency of the federal government. Developed with input from the Initiative for Innovation in Pediatric Education and the Pediatric Research in Inpatient Settings Network (supported by the Children's Hospital Association, the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine). A. J. S. was supported by the Agency for Healthcare Research and Quality/Oregon Comparative Effectiveness Research K12 Program (1K12HS019456‐01). Additional funding for the I‐PASS Study was provided by the Medical Research Foundation of Oregon, Physician Services Incorporated Foundation (Ontario, Canada), and Pfizer (unrestricted medical education grant to N.D.S.). C.P.L, A.J.S. were supported by the Oregon Comparative Effectiveness Research K12 Program (1K12HS019456 from the Agency for Healthcare Research and Quality). A.J.S. was also supported by the Medical Research Foundation of Oregon. The authors report no conflicts of interest.
- , , , , . Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16(2):125–132.
- , , , , . Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out. J Hosp Med. 2006;1(4):257–266.
- , , . Development and implementation of an oral sign‐out skills curriculum. J Gen Intern Med. 2007;22(10):1470–1474.
- , , , , , . Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440.
- , , . A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc. 2014;21(1):154–162.
- , , , , . Review of computerized physician handoff tools for improving the quality of patient care. J Hosp Med. 2013;8(8):456–463.
- , , , , . Answering questions on call: pediatric resident physicians' use of handoffs and other resources. J Hosp Med. 2013;8(6):328–333.
- , , , . Effectiveness of written hospitalist sign‐outs in answering overnight inquiries. J Hosp Med. 2013;8(11):609–614.
- , , . Sign‐out snapshot: cross‐sectional evaluation of written sign‐outs among specialties. BMJ Qual Saf. 2014;23(1):66–72.
- , , , . An experimental comparison of handover methods. Ann R Coll Surg Engl. 2007;89(3):298–300.
- , , , . Pilot study to show the loss of important data in nursing handover. Br J Nurs. 2005;14(20):1090–1093.
- The Joint Commission. Hospital Accreditation Standards 2015: Joint Commission Resources; 2015:PC.02.02.01.
- Accreditation Council for Graduate Medical Education. Common Program Requirements. 2013; http://acgme.org/acgmeweb/tabid/429/ProgramandInstitutionalAccreditation/CommonProgramRequirements.aspx. Accessed May 11, 2015.
- , , , . Establishing a multisite education and research project requires leadership, expertise, collaboration, and an important aim. Pediatrics. 2010;126(4):619–622.
- , , , et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812.
- US Department of Health and Human Services. Agency for Healthcare Research and Quality. TeamSTEPPS website. Available at: http://teamstepps.ahrq.gov/. Accessed July 12, 2013.
- , , , , , . I‐PASS, a mnemonic to standardize verbal handoffs. Pediatrics. 2012;129(2):201–204.
- , , . The Team Handbook. 3rd ed. Middleton, WI: Oriel STAT A MATRIX; 2010.
- ACC/AHA Task Force on Practice Guidelines. Methodology Manual and Policies From the ACCF/AHA Task Force on Practice Guidelines. Available at: http://my.americanheart.org/idc/groups/ahamah‐public/@wcm/@sop/documents/downloadable/ucm_319826.pdf. Published June 2010. Accessed January 11, 2015.
- , , , et al. Effect of illness severity and comorbidity on patient safety and adverse events. Am J Med Qual. 2012;27(1):48–57.
- , , , , . Consequences of inadequate sign‐out for patient care. Arch Intern Med. 2008;168(16):1755–1760.
- , , , et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262–2270.
- , , , , . Medication discrepancies in resident sign‐outs and their potential to harm. J Gen Intern Med. 2007;22(12):1751–1755.
- , , , . Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Qual Saf. 2012;21(11):925–932.
- , , , , . Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24(2):77–87.
- , , , et al. Simple standardized patient handoff system that increases accuracy and completeness. J Surg Educ. 2008;65(6):476–485.
- , , , . Organizing the transfer of patient care information: the development of a computerized resident sign‐out system. Surgery. 2004;136(1):5–13.
- , , , , . A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200(4):538–545.
- , , . Template for success: using a resident‐designed sign‐out template in the handover of patient care. J Surg Educ. 2011;68(1):52–57.
- , , , , , . Read‐back improves information transfer in simulated clinical crises. BMJ Qual Saf. 2014;23(12):989–993.
- , , , , . Interns overestimate the effectiveness of their hand‐off communication. Pediatrics. 2010;125(3):491–496.
- , , , , , . Improving patient safety by repeating (read‐back) telephone reports of critical information. Am J Clin Pathol. 2004;121(6):801–803.
- , , , , . Content overlap in nurse and physician handoff artifacts and the potential role of electronic health records: a systematic review. J Biomed Inform. 2011;44(4):704–712.
- , , , . Clinical summarization capabilities of commercially‐available and internally‐developed electronic health records. Appl Clin Inform. 2012;3(1):80–93.
- , . An analysis and recommendations for multidisciplinary computerized handoff applications in hospitals. AMIA Annu Symp Proc. 2011;2011:588–597.
Handoffs among hospital providers are highly error prone and can result in serious morbidity and mortality. Best practices for verbal handoffs have been described[1, 2, 3, 4] and include conducting verbal handoffs face to face, providing opportunities for questions, having the receiver perform a readback, as well as specific content recommendations including action items. Far less research has focused on best practices for printed handoff documents,[5, 6] despite the routine use of written handoff tools as a reference by on‐call physicians.[7, 8] Erroneous or outdated information on the written handoff can mislead on‐call providers, potentially leading to serious medical errors.
In their most basic form, printed handoff documents list patients for whom a provider is responsible. Typically, they also contain demographic information, reason for hospital admission, and a task list for each patient. They may also contain more detailed information on patient history, hospital course, and/or care plan, and may vary among specialties.[9] They come in various forms, ranging from index cards with handwritten notes, to word‐processor or spreadsheet documents, to printed documents that are autopopulated from the electronic health record (EHR).[2] Importantly, printed handoff documents supplement the verbal handoff by allowing receivers to follow along as patients are presented. The concurrent use of written and verbal handoffs may improve retention of clinical information as compared with either alone.[10, 11]
The Joint Commission requires an institutional approach to patient handoffs.[12] The requirements state that handoff communication solutions should take a standardized form, but they do not provide details regarding what data elements should be included in printed or verbal handoffs. Accreditation Council for Graduate Medical Education Common Program Requirements likewise require that residents must become competent in patient handoffs[13] but do not provide specific details or measurement tools. Absent widely accepted guidelines, decisions regarding which elements to include in printed handoff documents are currently made at an individual or institutional level.
The I‐PASS study is a federally funded multi‐institutional project that demonstrated a decrease in medical errors and preventable adverse events after implementation of a standardized resident handoff bundle.[14, 15] The I‐PASS Study Group developed a bundle of handoff interventions, beginning with a handoff and teamwork training program (based in part on TeamSTEPPS [Team Strategies and Tools to Enhance Performance and Patient Safety]),[16] a novel verbal mnemonic, I‐PASS (Illness Severity, Patient Summary, Action List, Situation Awareness and Contingency Planning, and Synthesis by Receiver),[17] and changes to the verbal handoff process, in addition to several other elements.
We hypothesized that developing a standardized printed handoff template would reinforce the handoff training and enhance the value of the verbal handoff process changes. Given the paucity of data on best printed handoff practices, however, we first conducted a needs assessment to identify which data elements were currently contained in printed handoffs across sites, and to allow an expert panel to make recommendations for best practices.
METHODS
I‐PASS Study sites included 9 pediatric residency programs at academic medical centers from across North America. Programs were identified through professional networks and invited to participate. The nonintensive care unit hospitalist services at these medical centers are primarily staffed by residents and medical students with attending supervision. At 1 site, nurse practitioners also participate in care. Additional details about study sites can be found in the study descriptions previously published.[14, 15] All sites received local institutional review board approval.
We began by inviting members of the I‐PASS Education Executive Committee (EEC)[14] to build a collective, comprehensive list of possible data elements for printed handoff documents. This committee included pediatric residency program directors, pediatric hospitalists, education researchers, health services researchers, and patient safety experts. We obtained sample handoff documents from pediatric hospitalist services at each of 9 institutions in the United States and Canada (with protected health information redacted). We reviewed these sample handoff documents to characterize their format and to determine what discrete data elements appeared in each site's printed handoff document. Presence or absence of each data element across sites was tabulated. We also queried sites to determine the feasibility of including elements that were not presently included.
Subsequently, I‐PASS site investigators led structured group interviews at participating sites to gather additional information about handoff practices at each site. These structured group interviews included diverse representation from residents, faculty, and residency program leadership, as well as hospitalists and medical students, to ensure the comprehensive acquisition of information regarding site‐specific characteristics. Each group provided answers to a standardized set of open‐ended questions that addressed current practices, handoff education, simulation use, team structure, and the nature of current written handoff tools, if applicable, at each site. One member of the structured group interview served as a scribe and created a document that summarized the content of the structured group interview meeting and answers to the standardized questions.
Consensus on Content
The initial data collection also included a multivote process[18] of the full I‐PASS EEC to help prioritize data elements. Committee members brainstormed a list of all possible data elements for a printed handoff document. Each member (n=14) was given 10 votes to distribute among the elements. Committee members could assign more than 1 vote to an element to emphasize its importance.
The results of this process as well as the current data elements included in each printed handoff tool were reviewed by a subgroup of the I‐PASS EEC. These expert panel members participated in a series of conference calls during which they tabulated categorical information, reviewed narrative comments, discussed existing evidence, and conducted simple content analysis to identify areas of concordance or discordance. Areas of discordance were discussed by the committee. Disagreements were resolved with group consensus with attention to published evidence or best practices, if available.
Elements were divided into those that were essential (unanimous consensus, no conflicting literature) and those that were recommended (majority supported inclusion of element, no conflicting literature). Ratings were assigned using the American College of Cardiology/American Heart Association framework for practice guidelines,[19] in which each element is assigned a classification (I=effective, II=conflicting evidence/opinion, III=not effective) and a level of evidence to support that classification (A=multiple large randomized controlled trials, B=single randomized trial, or nonrandomized studies, C=expert consensus).
The expert panel reached consensus, through active discussion, on a list of data elements that should be included in an ideal printed handoff document. Elements were chosen based on perceived importance, with attention to published best practices[1, 16] and the multivoting results. In making recommendations, consideration was given to whether data elements could be electronically imported into the printed handoff document from the EHR, or whether they would be entered manually. The potential for serious medical errors due to possible errors in manual entry of data was an important aspect of recommendations made. The list of candidate elements was then reviewed by a larger group of investigators from the I‐PASS Education Executive Committee and Coordinating Council for additional input.
The panel asked site investigators from each participating hospital to gather data on the feasibility of redesigning the printed handoff at that hospital to include each recommended element. Site investigators reported whether each element was already included, possible to include but not included currently, or not currently possible to include within that site's printed handoff tool. Site investigators also reported how data elements were populated in their handoff documents, with options including: (1) autopopulated from administrative data (eg, pharmacy‐entered medication list, demographic data entered by admitting office), (2) autoimported from physicians' free‐text entries elsewhere in the EHR (eg, progress notes), (3) free text entered specifically for the printed handoff, or (4) not applicable (element cannot be included).
RESULTS
Nine programs (100%) provided data on the structure and contents of their printed handoff documents. We found wide variation in structure across the 9 sites. Three sites used a word‐processorbased document that required manual entry of all data elements. The other 6 institutions had a direct link with the EHR to enable autopopulation of between 10 and 20 elements on the printed handoff document.
The content of written handoff documents, as well as the sources of data included in them (present or future), likewise varied substantially across sites (Table 1). Only 4 data elements (name, age, weight, and a list of medications) were universally included at all 9 sites. Among the 6 institutions that linked the printed handoff to the EHR, there was also substantial variation in which elements were autoimported. Only 7 elements were universally autoimported at these 6 sites: patient name, medical record number, room number, weight, date of birth, age, and date of admission. Two elements from the original brainstorming were not presently included in any sites' documents (emergency contact and primary language).
| Data Elements | Sites With Data Element Included at Initial Needs Assessment (Out of Nine Sites) | Data Source (Current or Anticipated) | ||
|---|---|---|---|---|
| Autoimported* | Manually Entered | Not Applicable | ||
| ||||
| Name | 9 | 6 | 3 | 0 |
| Medical record number | 8 | 6 | 3 | 0 |
| Room number | 8 | 6 | 3 | 0 |
| Allergies | 6 | 4 | 5 | 0 |
| Weight | 9 | 6 | 3 | 0 |
| Age | 9 | 6 | 3 | 0 |
| Date of birth | 6 | 6 | 3 | 0 |
| Admission date | 8 | 6 | 3 | 0 |
| Attending name | 5 | 4 | 5 | 0 |
| Team/service | 7 | 4 | 5 | 0 |
| Illness severity | 1 | 0 | 9 | 0 |
| Patient summary | 8 | 0 | 9 | 0 |
| Action items | 8 | 0 | 9 | 0 |
| Situation monitoring/contingency plan | 5 | 0 | 9 | 0 |
| Medication name | 9 | 4 | 5 | 0 |
| Medication name and dose/route/frequency | 4 | 4 | 5 | 0 |
| Code status | 2 | 2 | 7 | 0 |
| Labs | 6 | 5 | 4 | 0 |
| Access | 2 | 2 | 7 | 0 |
| Ins/outs | 2 | 4 | 4 | 1 |
| Primary language | 0 | 3 | 6 | 0 |
| Vital signs | 3 | 4 | 4 | 1 |
| Emergency contact | 0 | 2 | 7 | 0 |
| Primary care provider | 4 | 4 | 5 | 0 |
Nine institutions (100%) conducted structured group interviews, ranging in size from 4 to 27 individuals with a median of 5 participants. The documents containing information from each site were provided to the authors. The authors then tabulated categorical information, reviewed narrative comments to understand current institutional practices, and conducted simple content analysis to identify areas of concordance or discordance, particularly with respect to data elements and EHR usage. Based on the results of the printed handoff document review and structured group interviews, with additional perspectives provided by the I‐PASS EEC, the expert panel came to consensus on a list of 23 elements that should be included in printed handoff documents, including 15 essential data elements and 8 additional recommended elements (Table 2).
|
| Essential Elements |
| Patient identifiers |
| Patient name (class I, level of evidence C) |
| Medical record number (class I, level of evidence C) |
| Date of birth (class I, level of evidence C) |
| Hospital service identifiers |
| Attending name (class I, level of evidence C) |
| Team/service (class I, level of evidence C) |
| Room number (class I, level of evidence C) |
| Admission date (class I, level of evidence C) |
| Age (class I, level of evidence C) |
| Weight (class I, level of evidence C) |
| Illness severity (class I, level of evidence B)[20, 21] |
| Patient summary (class I, level of evidence B)[21, 22] |
| Action items (class I, level of evidence B) [21, 22] |
| Situation awareness/contingency planning (class I, level of evidence B) [21, 22] |
| Allergies (class I, level of evidence C) |
| Medications |
| Autopopulation of medications (class I, level of evidence B)[22, 23, 24] |
| Free‐text entry of medications (class IIa, level of evidence C) |
| Recommended elements |
| Primary language (class IIa, level of evidence C) |
| Emergency contact (class IIa, level of evidence C) |
| Primary care provider (class IIa, level of evidence C) |
| Code status (class IIb, level of evidence C) |
| Labs (class IIa, level of evidence C) |
| Access (class IIa, level of evidence C) |
| Ins/outs (class IIa, level of evidence C) |
| Vital signs (class IIa, level of evidence C) |
Evidence ratings[19] of these elements are included. Several elements are classified as I‐B (effective, nonrandomized studies) based on either studies of individual elements, or greater than 1 study of bundled elements that could reasonably be extrapolated. These include Illness severity,[20, 21] patient summary,[21, 22] action items[21, 22] (to do lists), situation awareness and contingency plan,[21, 22] and medications[22, 23, 24] with attention to importing from the EHR. Medications entered as free text were classified as IIa‐C because of risk and potential significance of errors; in particular there was concern that transcription errors, errors of omission, or errors of commission could potentially lead to patient harms. The remaining essential elements are classified as I‐C (effective, expert consensus). Of note, date of birth was specifically included as a patient identifier, distinct from age, which was felt to be useful as a descriptor (often within a one‐liner or as part of the patient summary).
The 8 recommended elements were elements for which there was not unanimous agreement on inclusion, but the majority of the panel felt they should be included. These elements were classified as IIa‐C, with 1 exception. Code status generated significant controversy among the group. After extensive discussion among the group and consideration of safety, supervision, educational, and pediatric‐specific considerations, all members of the group agreed on the categorization as a recommended element; it is classified as IIb‐C.
All members of the group agreed that data elements should be directly imported from the EHR whenever possible. Finally, members agreed that the elements that make up the I‐PASS mnemonic (illness severity, patient summary, action items, situation awareness/contingency planning) should be listed in that order whenever possible. A sample I‐PASS‐compliant printed handoff document is shown Figure 1.
DISCUSSION
We identified substantial variability in the structure and content of printed handoff documents used by 9 pediatric hospitalist teaching services, reflective of a lack of standardization. We found that institutional printed handoff documents shared some demographic elements (eg, name, room, medical record number) but also varied in clinical content (eg, vital signs, lab tests, code status). Our expert panel developed a list of 15 essential and 8 recommended data elements for printed handoff documents. Although this is a large number of fields, the majority of the essential fields were already included by most sites, and many are basic demographic identifiers. Illness severity is the 1 essential field that was not routinely included; however, including this type of overview is consistently recommended[2, 4] and supported by evidence,[20, 21] and contributes to building a shared mental model.[16] We recommend the categories of stable/watcher/unstable.[17]
Several prior single‐center studies have found that introducing a printed handoff document can lead to improvements in workflow, communication, and patient safety. In an early study, Petersen et al.[25] showed an association between use of a computerized sign‐out program and reduced odds of preventable adverse events during periods of cross‐coverage. Wayne et al.[26] reported fewer perceived inaccuracies in handoff documents as well as improved clarity at the time of transfer, supporting the role for standardization. Van Eaton et al.[27] demonstrated rapid uptake and desirability of a computerized handoff document, which combined autoimportation of information from an EHR with resident‐entered patient details, reflecting the importance of both data sources. In addition, they demonstrated improvements in both the rounding and sign‐out processes.[28]
Two studies specifically reported the increased use of specific fields after implementation. Payne et al. implemented a Web‐based handoff tool and documented significant increases in the number of handoffs containing problem lists, medication lists, and code status, accompanied by perceived improvements in quality of handoffs and fewer near‐miss events.[24] Starmer et al. found that introduction of a resident handoff bundle that included a printed handoff tool led to reduction in medical errors and adverse events.[22] The study group using the tool populated 11 data elements more often after implementation, and introduction of this printed handoff tool in particular was associated with reductions in written handoff miscommunications. Neither of these studies included subanalysis to indicate which data elements may have been most important.
In contrast to previous single‐institution studies, our recommendations for a printed handoff template come from evaluations of tools and discussions with front line providers across 9 institutions. We had substantial overlap with data elements recommended by Van Eaton et al.[27] However, there were several areas in which we did not have overlap with published templates including weight, ins/outs, primary language, emergency contact information, or primary care provider. Other published handoff tools have been highly specialized (eg, for cardiac intensive care) or included many fewer data elements than our group felt were essential. These differences may reflect the unique aspects of caring for pediatric patients (eg, need for weights) and the absence of defined protocols for many pediatric conditions. In addition, the level of detail needed for contingency planning may vary between teaching and nonteaching services.
Resident physicians may provide valuable information in the development of standardized handoff documents. Clark et al.,[29] at Virginia Mason University, utilized resident‐driven continuous quality improvement processes including real‐time feedback to implement an electronic template. They found that engagement of both senior leaders and front‐line users was an important component of their success in uptake. Our study utilized residents as essential members of structured group interviews to ensure that front‐line users' needs were represented as recommendations for a printed handoff tool template were developed.
As previously described,[17] our study group had identified several key data elements that should be included in verbal handoffs: illness severity, a patient summary, a discrete action list, situation awareness/contingency planning, and a synthesis by receiver. With consideration of the multivoting results as well as known best practices,[1, 4, 12] the expert panel for this study agreed that each of these elements should also be highlighted in the printed template to ensure consistency between the printed document and the verbal handoff, and to have each reinforce the other. On the printed handoff tool, the final S in the I‐PASS mnemonic (synthesis by receiver) cannot be prepopulated, but considering the importance of this step,[16, 30, 31, 32] it should be printed as synthesis by receiver to serve as a text‐reminder to both givers and receivers.
The panel also felt, however, that the printed handoff document should provide additional background information not routinely included in a verbal handoff. It should serve as a reference tool both at the time of verbal handoff and throughout the day and night, and therefore should include more comprehensive information than is necessary or appropriate to convey during the verbal handoff. We identified 10 data elements that are essential in a printed handoff document in addition to the I‐PASS elements (Table 2).
Patient demographic data elements, as well as team assignments and attending physician, were uniformly supported for inclusion. The medication list was viewed as essential; however, the panel also recognized the potential for medical errors due to inaccuracies in the medication list. In particular, there was concern that including all fields of a medication order (drug, dose, route, frequency) would result in handoffs containing a high proportion of inaccurate information, particularly for complex patients whose medication regimens may vary over the course of hospitalization. Therefore, the panel agreed that if medication lists were entered manually, then only the medication name should be included as they did not wish to perpetuate inaccurate or potentially harmful information. If medication lists were autoimported from an EHR, then they should include drug name, dose, route, and frequency if possible.
In the I‐PASS study,[15] all institutions implemented printed handoff documents that included fields for the essential data elements. After implementation, there was a significant increase in completion of all essential fields. Although there is limited evidence to support any individual data element, increased usage of these elements was associated with the overall study finding of decreased rates of medical errors and preventable adverse events.
EHRs have the potential to help standardize printed handoff documents[5, 6, 33, 34, 35]; all participants in our study agreed that printed handoff documents should ideally be linked with the EHR and should autoimport data wherever appropriate. Manually populated (eg, word processor‐ or spreadsheet‐based) handoff tools have important limitations, particularly related to the potential for typographical errors as well as accidental omission of data fields, and lead to unnecessary duplication of work (eg, re‐entering data already included in a progress note) that can waste providers' time. It was also acknowledged that word processor‐ or spreadsheet‐based documents may have flexibility that is lacking in EHR‐based handoff documents. For example, formatting can more easily be adjusted to increase the number of patients per printed page. As technology advances, printed documents may be phased out in favor of EHR‐based on‐screen reports, which by their nature would be more accurate due to real‐time autoupdates.
In making recommendations about essential versus recommended items for inclusion in the printed handoff template, the only data element that generated controversy among our experts was code status. Some felt that it should be included as an essential element, whereas others did not. We believe that this was unique to our practice in pediatric hospital ward settings, as codes in most pediatric ward settings are rare. Among the concerns expressed with including code status for all patients were that residents might assume patients were full‐code without verifying. The potential inaccuracy created by this might have severe implications. Alternatively, residents might feel obligated to have code discussions with all patients regardless of severity of illness, which may be inappropriate in a pediatric population. Several educators expressed concerns about trainees having unsupervised code‐status conversations with families of pediatric patients. Conversely, although codes are rare in pediatric ward settings, concerns were raised that not including code status could be problematic during these rare but critically important events. Other fields, such as weight, might have less relevance for an adult population in which emergency drug doses are standardized.
Limitations
Our study has several limitations. We only collected data from hospitalist services at pediatric sites. It is likely that providers in other specialties would have specific data elements they felt were essential (eg, postoperative day, code status). Our methodology was expert consensus based, driven by data collection from sites that were already participating in the I‐PASS study. Although the I‐PASS study demonstrated decreased rates of medical errors and preventable adverse events with inclusion of these data elements as part of a bundle, future research will be required to evaluate whether some of these items are more important than others in improving written communication and ultimately patient safety. In spite of these limitations, our work represents an important starting point for the development of standards for written handoff documents that should be used in patient handoffs, particularly those generated from EHRs.
CONCLUSIONS
In this article we describe the results of a needs assessment that informed expert consensus‐based recommendations for data elements to include in a printed handoff document. We recommend that pediatric programs include the elements identified as part of a standardized written handoff tool. Although many of these elements are also applicable to other specialties, future work should be conducted to adapt the printed handoff document elements described here for use in other specialties and settings. Future studies should work to validate the importance of these elements, studying the manner in which their inclusion affects the quality of written handoffs, and ultimately patient safety.
Acknowledgements
Members of the I‐PASS Study Education Executive Committee who contributed to this manuscript include: Boston Children's Hospital/Harvard Medical School (primary site) (Christopher P. Landrigan, MD, MPH, Elizabeth L. Noble, BA. Theodore C. Sectish, MD. Lisa L. Tse, BA). Cincinnati Children's Hospital Medical Center/University of Cincinnati College of Medicine (Jennifer K. O'Toole, MD, MEd). Doernbecher Children's Hospital/Oregon Health and Science University (Amy J. Starmer, MD, MPH). Hospital for Sick Children/University of Toronto (Zia Bismilla, MD. Maitreya Coffey, MD). Lucile Packard Children's Hospital/Stanford University (Lauren A. Destino, MD. Jennifer L. Everhart, MD. Shilpa J. Patel, MD [currently at Kapi'olani Children's Hospital/University of Hawai'i School of Medicine]). National Capital Consortium (Jennifer H. Hepps, MD. Joseph O. Lopreiato, MD, MPH. Clifton E. Yu, MD). Primary Children's Medical Center/University of Utah (James F. Bale, Jr., MD. Adam T. Stevenson, MD). St. Louis Children's Hospital/Washington University (F. Sessions Cole, MD). St. Christopher's Hospital for Children/Drexel University College of Medicine (Sharon Calaman, MD. Nancy D. Spector, MD). Benioff Children's Hospital/University of California San Francisco School of Medicine (Glenn Rosenbluth, MD. Daniel C. West, MD).
Additional I‐PASS Study Group members who contributed to this manuscript include April D. Allen, MPA, MA (Heller School for Social Policy and Management, Brandeis University, previously affiliated with Boston Children's Hospital), Madelyn D. Kahana, MD (The Children's Hospital at Montefiore/Albert Einstein College of Medicine, previously affiliated with Lucile Packard Children's Hospital/Stanford University), Robert S. McGregor, MD (Akron Children's Hospital/Northeast Ohio Medical University, previously affiliated with St. Christopher's Hospital for Children/Drexel University), and John S. Webster, MD, MBA, MS (Webster Healthcare Consulting Inc., formerly of the Department of Defense).
Members of the I‐PASS Study Group include individuals from the institutions listed below as follows: Boston Children's Hospital/Harvard Medical School (primary site): April D. Allen, MPA, MA (currently at Heller School for Social Policy and Management, Brandeis University), Angela M. Feraco, MD, Christopher P. Landrigan, MD, MPH, Elizabeth L. Noble, BA, Theodore C. Sectish, MD, Lisa L. Tse, BA. Brigham and Women's Hospital (data coordinating center): Anuj K. Dalal, MD, Carol A. Keohane, BSN, RN, Stuart Lipsitz, PhD, Jeffrey M. Rothschild, MD, MPH, Matt F. Wien, BS, Catherine S. Yoon, MS, Katherine R. Zigmont, BSN, RN. Cincinnati Children's Hospital Medical Center/University of Cincinnati College of Medicine: Javier Gonzalez del Rey, MD, MEd, Jennifer K. O'Toole, MD, MEd, Lauren G. Solan, MD. Doernbecher Children's Hospital/Oregon Health and Science University: Megan E. Aylor, MD, Amy J. Starmer, MD, MPH, Windy Stevenson, MD, Tamara Wagner, MD. Hospital for Sick Children/University of Toronto: Zia Bismilla, MD, Maitreya Coffey, MD, Sanjay Mahant, MD, MSc. Lucile Packard Children's Hospital/Stanford University: Rebecca L. Blankenburg, MD, MPH, Lauren A. Destino, MD, Jennifer L. Everhart, MD, Madelyn Kahana, MD, Shilpa J. Patel, MD (currently at Kapi'olani Children's Hospital/University of Hawaii School of Medicine). National Capital Consortium: Jennifer H. Hepps, MD, Joseph O. Lopreiato, MD, MPH, Clifton E. Yu, MD. Primary Children's Hospital/University of Utah: James F. Bale, Jr., MD, Jaime Blank Spackman, MSHS, CCRP, Rajendu Srivastava, MD, FRCP(C), MPH, Adam Stevenson, MD. St. Louis Children's Hospital/Washington University: Kevin Barton, MD, Kathleen Berchelmann, MD, F. Sessions Cole, MD, Christine Hrach, MD, Kyle S. Schultz, MD, Michael P. Turmelle, MD, Andrew J. White, MD. St. Christopher's Hospital for Children/Drexel University: Sharon Calaman, MD, Bronwyn D. Carlson, MD, Robert S. McGregor, MD (currently at Akron Children's Hospital/Northeast Ohio Medical University), Vahideh Nilforoshan, MD, Nancy D. Spector, MD. and Benioff Children's Hospital/University of California San Francisco School of Medicine: Glenn Rosenbluth, MD, Daniel C. West, MD. Dorene Balmer, PhD, RD, Carol L. Carraccio, MD, MA, Laura Degnon, CAE, and David McDonald, and Alan Schwartz PhD serve the I‐PASS Study Group as part of the IIPE. Karen M. Wilson, MD, MPH serves the I‐PASS Study Group as part of the advisory board from the PRIS Executive Council. John Webster served the I‐PASS Study Group and Education Executive Committee as a representative from TeamSTEPPS.
Disclosures: The I‐PASS Study was primarily supported by the US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation (1R18AE000029‐01). The opinions and conclusions expressed herein are solely those of the author(s) and should not be constructed as representing the opinions or policy of any agency of the federal government. Developed with input from the Initiative for Innovation in Pediatric Education and the Pediatric Research in Inpatient Settings Network (supported by the Children's Hospital Association, the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine). A. J. S. was supported by the Agency for Healthcare Research and Quality/Oregon Comparative Effectiveness Research K12 Program (1K12HS019456‐01). Additional funding for the I‐PASS Study was provided by the Medical Research Foundation of Oregon, Physician Services Incorporated Foundation (Ontario, Canada), and Pfizer (unrestricted medical education grant to N.D.S.). C.P.L, A.J.S. were supported by the Oregon Comparative Effectiveness Research K12 Program (1K12HS019456 from the Agency for Healthcare Research and Quality). A.J.S. was also supported by the Medical Research Foundation of Oregon. The authors report no conflicts of interest.
Handoffs among hospital providers are highly error prone and can result in serious morbidity and mortality. Best practices for verbal handoffs have been described[1, 2, 3, 4] and include conducting verbal handoffs face to face, providing opportunities for questions, having the receiver perform a readback, as well as specific content recommendations including action items. Far less research has focused on best practices for printed handoff documents,[5, 6] despite the routine use of written handoff tools as a reference by on‐call physicians.[7, 8] Erroneous or outdated information on the written handoff can mislead on‐call providers, potentially leading to serious medical errors.
In their most basic form, printed handoff documents list patients for whom a provider is responsible. Typically, they also contain demographic information, reason for hospital admission, and a task list for each patient. They may also contain more detailed information on patient history, hospital course, and/or care plan, and may vary among specialties.[9] They come in various forms, ranging from index cards with handwritten notes, to word‐processor or spreadsheet documents, to printed documents that are autopopulated from the electronic health record (EHR).[2] Importantly, printed handoff documents supplement the verbal handoff by allowing receivers to follow along as patients are presented. The concurrent use of written and verbal handoffs may improve retention of clinical information as compared with either alone.[10, 11]
The Joint Commission requires an institutional approach to patient handoffs.[12] The requirements state that handoff communication solutions should take a standardized form, but they do not provide details regarding what data elements should be included in printed or verbal handoffs. Accreditation Council for Graduate Medical Education Common Program Requirements likewise require that residents must become competent in patient handoffs[13] but do not provide specific details or measurement tools. Absent widely accepted guidelines, decisions regarding which elements to include in printed handoff documents are currently made at an individual or institutional level.
The I‐PASS study is a federally funded multi‐institutional project that demonstrated a decrease in medical errors and preventable adverse events after implementation of a standardized resident handoff bundle.[14, 15] The I‐PASS Study Group developed a bundle of handoff interventions, beginning with a handoff and teamwork training program (based in part on TeamSTEPPS [Team Strategies and Tools to Enhance Performance and Patient Safety]),[16] a novel verbal mnemonic, I‐PASS (Illness Severity, Patient Summary, Action List, Situation Awareness and Contingency Planning, and Synthesis by Receiver),[17] and changes to the verbal handoff process, in addition to several other elements.
We hypothesized that developing a standardized printed handoff template would reinforce the handoff training and enhance the value of the verbal handoff process changes. Given the paucity of data on best printed handoff practices, however, we first conducted a needs assessment to identify which data elements were currently contained in printed handoffs across sites, and to allow an expert panel to make recommendations for best practices.
METHODS
I‐PASS Study sites included 9 pediatric residency programs at academic medical centers from across North America. Programs were identified through professional networks and invited to participate. The nonintensive care unit hospitalist services at these medical centers are primarily staffed by residents and medical students with attending supervision. At 1 site, nurse practitioners also participate in care. Additional details about study sites can be found in the study descriptions previously published.[14, 15] All sites received local institutional review board approval.
We began by inviting members of the I‐PASS Education Executive Committee (EEC)[14] to build a collective, comprehensive list of possible data elements for printed handoff documents. This committee included pediatric residency program directors, pediatric hospitalists, education researchers, health services researchers, and patient safety experts. We obtained sample handoff documents from pediatric hospitalist services at each of 9 institutions in the United States and Canada (with protected health information redacted). We reviewed these sample handoff documents to characterize their format and to determine what discrete data elements appeared in each site's printed handoff document. Presence or absence of each data element across sites was tabulated. We also queried sites to determine the feasibility of including elements that were not presently included.
Subsequently, I‐PASS site investigators led structured group interviews at participating sites to gather additional information about handoff practices at each site. These structured group interviews included diverse representation from residents, faculty, and residency program leadership, as well as hospitalists and medical students, to ensure the comprehensive acquisition of information regarding site‐specific characteristics. Each group provided answers to a standardized set of open‐ended questions that addressed current practices, handoff education, simulation use, team structure, and the nature of current written handoff tools, if applicable, at each site. One member of the structured group interview served as a scribe and created a document that summarized the content of the structured group interview meeting and answers to the standardized questions.
Consensus on Content
The initial data collection also included a multivote process[18] of the full I‐PASS EEC to help prioritize data elements. Committee members brainstormed a list of all possible data elements for a printed handoff document. Each member (n=14) was given 10 votes to distribute among the elements. Committee members could assign more than 1 vote to an element to emphasize its importance.
The results of this process as well as the current data elements included in each printed handoff tool were reviewed by a subgroup of the I‐PASS EEC. These expert panel members participated in a series of conference calls during which they tabulated categorical information, reviewed narrative comments, discussed existing evidence, and conducted simple content analysis to identify areas of concordance or discordance. Areas of discordance were discussed by the committee. Disagreements were resolved with group consensus with attention to published evidence or best practices, if available.
Elements were divided into those that were essential (unanimous consensus, no conflicting literature) and those that were recommended (majority supported inclusion of element, no conflicting literature). Ratings were assigned using the American College of Cardiology/American Heart Association framework for practice guidelines,[19] in which each element is assigned a classification (I=effective, II=conflicting evidence/opinion, III=not effective) and a level of evidence to support that classification (A=multiple large randomized controlled trials, B=single randomized trial, or nonrandomized studies, C=expert consensus).
The expert panel reached consensus, through active discussion, on a list of data elements that should be included in an ideal printed handoff document. Elements were chosen based on perceived importance, with attention to published best practices[1, 16] and the multivoting results. In making recommendations, consideration was given to whether data elements could be electronically imported into the printed handoff document from the EHR, or whether they would be entered manually. The potential for serious medical errors due to possible errors in manual entry of data was an important aspect of recommendations made. The list of candidate elements was then reviewed by a larger group of investigators from the I‐PASS Education Executive Committee and Coordinating Council for additional input.
The panel asked site investigators from each participating hospital to gather data on the feasibility of redesigning the printed handoff at that hospital to include each recommended element. Site investigators reported whether each element was already included, possible to include but not included currently, or not currently possible to include within that site's printed handoff tool. Site investigators also reported how data elements were populated in their handoff documents, with options including: (1) autopopulated from administrative data (eg, pharmacy‐entered medication list, demographic data entered by admitting office), (2) autoimported from physicians' free‐text entries elsewhere in the EHR (eg, progress notes), (3) free text entered specifically for the printed handoff, or (4) not applicable (element cannot be included).
RESULTS
Nine programs (100%) provided data on the structure and contents of their printed handoff documents. We found wide variation in structure across the 9 sites. Three sites used a word‐processorbased document that required manual entry of all data elements. The other 6 institutions had a direct link with the EHR to enable autopopulation of between 10 and 20 elements on the printed handoff document.
The content of written handoff documents, as well as the sources of data included in them (present or future), likewise varied substantially across sites (Table 1). Only 4 data elements (name, age, weight, and a list of medications) were universally included at all 9 sites. Among the 6 institutions that linked the printed handoff to the EHR, there was also substantial variation in which elements were autoimported. Only 7 elements were universally autoimported at these 6 sites: patient name, medical record number, room number, weight, date of birth, age, and date of admission. Two elements from the original brainstorming were not presently included in any sites' documents (emergency contact and primary language).
| Data Elements | Sites With Data Element Included at Initial Needs Assessment (Out of Nine Sites) | Data Source (Current or Anticipated) | ||
|---|---|---|---|---|
| Autoimported* | Manually Entered | Not Applicable | ||
| ||||
| Name | 9 | 6 | 3 | 0 |
| Medical record number | 8 | 6 | 3 | 0 |
| Room number | 8 | 6 | 3 | 0 |
| Allergies | 6 | 4 | 5 | 0 |
| Weight | 9 | 6 | 3 | 0 |
| Age | 9 | 6 | 3 | 0 |
| Date of birth | 6 | 6 | 3 | 0 |
| Admission date | 8 | 6 | 3 | 0 |
| Attending name | 5 | 4 | 5 | 0 |
| Team/service | 7 | 4 | 5 | 0 |
| Illness severity | 1 | 0 | 9 | 0 |
| Patient summary | 8 | 0 | 9 | 0 |
| Action items | 8 | 0 | 9 | 0 |
| Situation monitoring/contingency plan | 5 | 0 | 9 | 0 |
| Medication name | 9 | 4 | 5 | 0 |
| Medication name and dose/route/frequency | 4 | 4 | 5 | 0 |
| Code status | 2 | 2 | 7 | 0 |
| Labs | 6 | 5 | 4 | 0 |
| Access | 2 | 2 | 7 | 0 |
| Ins/outs | 2 | 4 | 4 | 1 |
| Primary language | 0 | 3 | 6 | 0 |
| Vital signs | 3 | 4 | 4 | 1 |
| Emergency contact | 0 | 2 | 7 | 0 |
| Primary care provider | 4 | 4 | 5 | 0 |
Nine institutions (100%) conducted structured group interviews, ranging in size from 4 to 27 individuals with a median of 5 participants. The documents containing information from each site were provided to the authors. The authors then tabulated categorical information, reviewed narrative comments to understand current institutional practices, and conducted simple content analysis to identify areas of concordance or discordance, particularly with respect to data elements and EHR usage. Based on the results of the printed handoff document review and structured group interviews, with additional perspectives provided by the I‐PASS EEC, the expert panel came to consensus on a list of 23 elements that should be included in printed handoff documents, including 15 essential data elements and 8 additional recommended elements (Table 2).
|
| Essential Elements |
| Patient identifiers |
| Patient name (class I, level of evidence C) |
| Medical record number (class I, level of evidence C) |
| Date of birth (class I, level of evidence C) |
| Hospital service identifiers |
| Attending name (class I, level of evidence C) |
| Team/service (class I, level of evidence C) |
| Room number (class I, level of evidence C) |
| Admission date (class I, level of evidence C) |
| Age (class I, level of evidence C) |
| Weight (class I, level of evidence C) |
| Illness severity (class I, level of evidence B)[20, 21] |
| Patient summary (class I, level of evidence B)[21, 22] |
| Action items (class I, level of evidence B) [21, 22] |
| Situation awareness/contingency planning (class I, level of evidence B) [21, 22] |
| Allergies (class I, level of evidence C) |
| Medications |
| Autopopulation of medications (class I, level of evidence B)[22, 23, 24] |
| Free‐text entry of medications (class IIa, level of evidence C) |
| Recommended elements |
| Primary language (class IIa, level of evidence C) |
| Emergency contact (class IIa, level of evidence C) |
| Primary care provider (class IIa, level of evidence C) |
| Code status (class IIb, level of evidence C) |
| Labs (class IIa, level of evidence C) |
| Access (class IIa, level of evidence C) |
| Ins/outs (class IIa, level of evidence C) |
| Vital signs (class IIa, level of evidence C) |
Evidence ratings[19] of these elements are included. Several elements are classified as I‐B (effective, nonrandomized studies) based on either studies of individual elements, or greater than 1 study of bundled elements that could reasonably be extrapolated. These include Illness severity,[20, 21] patient summary,[21, 22] action items[21, 22] (to do lists), situation awareness and contingency plan,[21, 22] and medications[22, 23, 24] with attention to importing from the EHR. Medications entered as free text were classified as IIa‐C because of risk and potential significance of errors; in particular there was concern that transcription errors, errors of omission, or errors of commission could potentially lead to patient harms. The remaining essential elements are classified as I‐C (effective, expert consensus). Of note, date of birth was specifically included as a patient identifier, distinct from age, which was felt to be useful as a descriptor (often within a one‐liner or as part of the patient summary).
The 8 recommended elements were elements for which there was not unanimous agreement on inclusion, but the majority of the panel felt they should be included. These elements were classified as IIa‐C, with 1 exception. Code status generated significant controversy among the group. After extensive discussion among the group and consideration of safety, supervision, educational, and pediatric‐specific considerations, all members of the group agreed on the categorization as a recommended element; it is classified as IIb‐C.
All members of the group agreed that data elements should be directly imported from the EHR whenever possible. Finally, members agreed that the elements that make up the I‐PASS mnemonic (illness severity, patient summary, action items, situation awareness/contingency planning) should be listed in that order whenever possible. A sample I‐PASS‐compliant printed handoff document is shown Figure 1.
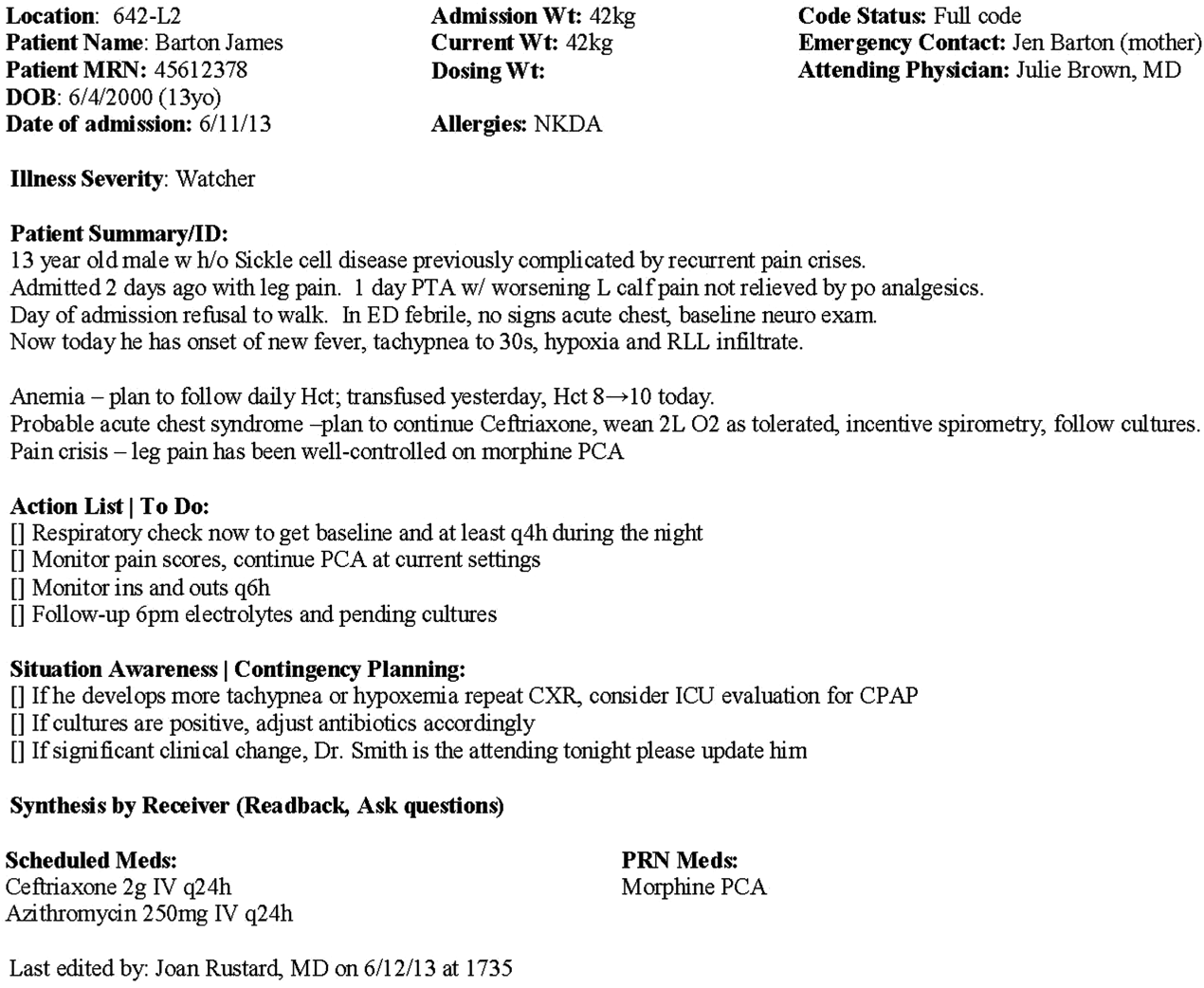
DISCUSSION
We identified substantial variability in the structure and content of printed handoff documents used by 9 pediatric hospitalist teaching services, reflective of a lack of standardization. We found that institutional printed handoff documents shared some demographic elements (eg, name, room, medical record number) but also varied in clinical content (eg, vital signs, lab tests, code status). Our expert panel developed a list of 15 essential and 8 recommended data elements for printed handoff documents. Although this is a large number of fields, the majority of the essential fields were already included by most sites, and many are basic demographic identifiers. Illness severity is the 1 essential field that was not routinely included; however, including this type of overview is consistently recommended[2, 4] and supported by evidence,[20, 21] and contributes to building a shared mental model.[16] We recommend the categories of stable/watcher/unstable.[17]
Several prior single‐center studies have found that introducing a printed handoff document can lead to improvements in workflow, communication, and patient safety. In an early study, Petersen et al.[25] showed an association between use of a computerized sign‐out program and reduced odds of preventable adverse events during periods of cross‐coverage. Wayne et al.[26] reported fewer perceived inaccuracies in handoff documents as well as improved clarity at the time of transfer, supporting the role for standardization. Van Eaton et al.[27] demonstrated rapid uptake and desirability of a computerized handoff document, which combined autoimportation of information from an EHR with resident‐entered patient details, reflecting the importance of both data sources. In addition, they demonstrated improvements in both the rounding and sign‐out processes.[28]
Two studies specifically reported the increased use of specific fields after implementation. Payne et al. implemented a Web‐based handoff tool and documented significant increases in the number of handoffs containing problem lists, medication lists, and code status, accompanied by perceived improvements in quality of handoffs and fewer near‐miss events.[24] Starmer et al. found that introduction of a resident handoff bundle that included a printed handoff tool led to reduction in medical errors and adverse events.[22] The study group using the tool populated 11 data elements more often after implementation, and introduction of this printed handoff tool in particular was associated with reductions in written handoff miscommunications. Neither of these studies included subanalysis to indicate which data elements may have been most important.
In contrast to previous single‐institution studies, our recommendations for a printed handoff template come from evaluations of tools and discussions with front line providers across 9 institutions. We had substantial overlap with data elements recommended by Van Eaton et al.[27] However, there were several areas in which we did not have overlap with published templates including weight, ins/outs, primary language, emergency contact information, or primary care provider. Other published handoff tools have been highly specialized (eg, for cardiac intensive care) or included many fewer data elements than our group felt were essential. These differences may reflect the unique aspects of caring for pediatric patients (eg, need for weights) and the absence of defined protocols for many pediatric conditions. In addition, the level of detail needed for contingency planning may vary between teaching and nonteaching services.
Resident physicians may provide valuable information in the development of standardized handoff documents. Clark et al.,[29] at Virginia Mason University, utilized resident‐driven continuous quality improvement processes including real‐time feedback to implement an electronic template. They found that engagement of both senior leaders and front‐line users was an important component of their success in uptake. Our study utilized residents as essential members of structured group interviews to ensure that front‐line users' needs were represented as recommendations for a printed handoff tool template were developed.
As previously described,[17] our study group had identified several key data elements that should be included in verbal handoffs: illness severity, a patient summary, a discrete action list, situation awareness/contingency planning, and a synthesis by receiver. With consideration of the multivoting results as well as known best practices,[1, 4, 12] the expert panel for this study agreed that each of these elements should also be highlighted in the printed template to ensure consistency between the printed document and the verbal handoff, and to have each reinforce the other. On the printed handoff tool, the final S in the I‐PASS mnemonic (synthesis by receiver) cannot be prepopulated, but considering the importance of this step,[16, 30, 31, 32] it should be printed as synthesis by receiver to serve as a text‐reminder to both givers and receivers.
The panel also felt, however, that the printed handoff document should provide additional background information not routinely included in a verbal handoff. It should serve as a reference tool both at the time of verbal handoff and throughout the day and night, and therefore should include more comprehensive information than is necessary or appropriate to convey during the verbal handoff. We identified 10 data elements that are essential in a printed handoff document in addition to the I‐PASS elements (Table 2).
Patient demographic data elements, as well as team assignments and attending physician, were uniformly supported for inclusion. The medication list was viewed as essential; however, the panel also recognized the potential for medical errors due to inaccuracies in the medication list. In particular, there was concern that including all fields of a medication order (drug, dose, route, frequency) would result in handoffs containing a high proportion of inaccurate information, particularly for complex patients whose medication regimens may vary over the course of hospitalization. Therefore, the panel agreed that if medication lists were entered manually, then only the medication name should be included as they did not wish to perpetuate inaccurate or potentially harmful information. If medication lists were autoimported from an EHR, then they should include drug name, dose, route, and frequency if possible.
In the I‐PASS study,[15] all institutions implemented printed handoff documents that included fields for the essential data elements. After implementation, there was a significant increase in completion of all essential fields. Although there is limited evidence to support any individual data element, increased usage of these elements was associated with the overall study finding of decreased rates of medical errors and preventable adverse events.
EHRs have the potential to help standardize printed handoff documents[5, 6, 33, 34, 35]; all participants in our study agreed that printed handoff documents should ideally be linked with the EHR and should autoimport data wherever appropriate. Manually populated (eg, word processor‐ or spreadsheet‐based) handoff tools have important limitations, particularly related to the potential for typographical errors as well as accidental omission of data fields, and lead to unnecessary duplication of work (eg, re‐entering data already included in a progress note) that can waste providers' time. It was also acknowledged that word processor‐ or spreadsheet‐based documents may have flexibility that is lacking in EHR‐based handoff documents. For example, formatting can more easily be adjusted to increase the number of patients per printed page. As technology advances, printed documents may be phased out in favor of EHR‐based on‐screen reports, which by their nature would be more accurate due to real‐time autoupdates.
In making recommendations about essential versus recommended items for inclusion in the printed handoff template, the only data element that generated controversy among our experts was code status. Some felt that it should be included as an essential element, whereas others did not. We believe that this was unique to our practice in pediatric hospital ward settings, as codes in most pediatric ward settings are rare. Among the concerns expressed with including code status for all patients were that residents might assume patients were full‐code without verifying. The potential inaccuracy created by this might have severe implications. Alternatively, residents might feel obligated to have code discussions with all patients regardless of severity of illness, which may be inappropriate in a pediatric population. Several educators expressed concerns about trainees having unsupervised code‐status conversations with families of pediatric patients. Conversely, although codes are rare in pediatric ward settings, concerns were raised that not including code status could be problematic during these rare but critically important events. Other fields, such as weight, might have less relevance for an adult population in which emergency drug doses are standardized.
Limitations
Our study has several limitations. We only collected data from hospitalist services at pediatric sites. It is likely that providers in other specialties would have specific data elements they felt were essential (eg, postoperative day, code status). Our methodology was expert consensus based, driven by data collection from sites that were already participating in the I‐PASS study. Although the I‐PASS study demonstrated decreased rates of medical errors and preventable adverse events with inclusion of these data elements as part of a bundle, future research will be required to evaluate whether some of these items are more important than others in improving written communication and ultimately patient safety. In spite of these limitations, our work represents an important starting point for the development of standards for written handoff documents that should be used in patient handoffs, particularly those generated from EHRs.
CONCLUSIONS
In this article we describe the results of a needs assessment that informed expert consensus‐based recommendations for data elements to include in a printed handoff document. We recommend that pediatric programs include the elements identified as part of a standardized written handoff tool. Although many of these elements are also applicable to other specialties, future work should be conducted to adapt the printed handoff document elements described here for use in other specialties and settings. Future studies should work to validate the importance of these elements, studying the manner in which their inclusion affects the quality of written handoffs, and ultimately patient safety.
Acknowledgements
Members of the I‐PASS Study Education Executive Committee who contributed to this manuscript include: Boston Children's Hospital/Harvard Medical School (primary site) (Christopher P. Landrigan, MD, MPH, Elizabeth L. Noble, BA. Theodore C. Sectish, MD. Lisa L. Tse, BA). Cincinnati Children's Hospital Medical Center/University of Cincinnati College of Medicine (Jennifer K. O'Toole, MD, MEd). Doernbecher Children's Hospital/Oregon Health and Science University (Amy J. Starmer, MD, MPH). Hospital for Sick Children/University of Toronto (Zia Bismilla, MD. Maitreya Coffey, MD). Lucile Packard Children's Hospital/Stanford University (Lauren A. Destino, MD. Jennifer L. Everhart, MD. Shilpa J. Patel, MD [currently at Kapi'olani Children's Hospital/University of Hawai'i School of Medicine]). National Capital Consortium (Jennifer H. Hepps, MD. Joseph O. Lopreiato, MD, MPH. Clifton E. Yu, MD). Primary Children's Medical Center/University of Utah (James F. Bale, Jr., MD. Adam T. Stevenson, MD). St. Louis Children's Hospital/Washington University (F. Sessions Cole, MD). St. Christopher's Hospital for Children/Drexel University College of Medicine (Sharon Calaman, MD. Nancy D. Spector, MD). Benioff Children's Hospital/University of California San Francisco School of Medicine (Glenn Rosenbluth, MD. Daniel C. West, MD).
Additional I‐PASS Study Group members who contributed to this manuscript include April D. Allen, MPA, MA (Heller School for Social Policy and Management, Brandeis University, previously affiliated with Boston Children's Hospital), Madelyn D. Kahana, MD (The Children's Hospital at Montefiore/Albert Einstein College of Medicine, previously affiliated with Lucile Packard Children's Hospital/Stanford University), Robert S. McGregor, MD (Akron Children's Hospital/Northeast Ohio Medical University, previously affiliated with St. Christopher's Hospital for Children/Drexel University), and John S. Webster, MD, MBA, MS (Webster Healthcare Consulting Inc., formerly of the Department of Defense).
Members of the I‐PASS Study Group include individuals from the institutions listed below as follows: Boston Children's Hospital/Harvard Medical School (primary site): April D. Allen, MPA, MA (currently at Heller School for Social Policy and Management, Brandeis University), Angela M. Feraco, MD, Christopher P. Landrigan, MD, MPH, Elizabeth L. Noble, BA, Theodore C. Sectish, MD, Lisa L. Tse, BA. Brigham and Women's Hospital (data coordinating center): Anuj K. Dalal, MD, Carol A. Keohane, BSN, RN, Stuart Lipsitz, PhD, Jeffrey M. Rothschild, MD, MPH, Matt F. Wien, BS, Catherine S. Yoon, MS, Katherine R. Zigmont, BSN, RN. Cincinnati Children's Hospital Medical Center/University of Cincinnati College of Medicine: Javier Gonzalez del Rey, MD, MEd, Jennifer K. O'Toole, MD, MEd, Lauren G. Solan, MD. Doernbecher Children's Hospital/Oregon Health and Science University: Megan E. Aylor, MD, Amy J. Starmer, MD, MPH, Windy Stevenson, MD, Tamara Wagner, MD. Hospital for Sick Children/University of Toronto: Zia Bismilla, MD, Maitreya Coffey, MD, Sanjay Mahant, MD, MSc. Lucile Packard Children's Hospital/Stanford University: Rebecca L. Blankenburg, MD, MPH, Lauren A. Destino, MD, Jennifer L. Everhart, MD, Madelyn Kahana, MD, Shilpa J. Patel, MD (currently at Kapi'olani Children's Hospital/University of Hawaii School of Medicine). National Capital Consortium: Jennifer H. Hepps, MD, Joseph O. Lopreiato, MD, MPH, Clifton E. Yu, MD. Primary Children's Hospital/University of Utah: James F. Bale, Jr., MD, Jaime Blank Spackman, MSHS, CCRP, Rajendu Srivastava, MD, FRCP(C), MPH, Adam Stevenson, MD. St. Louis Children's Hospital/Washington University: Kevin Barton, MD, Kathleen Berchelmann, MD, F. Sessions Cole, MD, Christine Hrach, MD, Kyle S. Schultz, MD, Michael P. Turmelle, MD, Andrew J. White, MD. St. Christopher's Hospital for Children/Drexel University: Sharon Calaman, MD, Bronwyn D. Carlson, MD, Robert S. McGregor, MD (currently at Akron Children's Hospital/Northeast Ohio Medical University), Vahideh Nilforoshan, MD, Nancy D. Spector, MD. and Benioff Children's Hospital/University of California San Francisco School of Medicine: Glenn Rosenbluth, MD, Daniel C. West, MD. Dorene Balmer, PhD, RD, Carol L. Carraccio, MD, MA, Laura Degnon, CAE, and David McDonald, and Alan Schwartz PhD serve the I‐PASS Study Group as part of the IIPE. Karen M. Wilson, MD, MPH serves the I‐PASS Study Group as part of the advisory board from the PRIS Executive Council. John Webster served the I‐PASS Study Group and Education Executive Committee as a representative from TeamSTEPPS.
Disclosures: The I‐PASS Study was primarily supported by the US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation (1R18AE000029‐01). The opinions and conclusions expressed herein are solely those of the author(s) and should not be constructed as representing the opinions or policy of any agency of the federal government. Developed with input from the Initiative for Innovation in Pediatric Education and the Pediatric Research in Inpatient Settings Network (supported by the Children's Hospital Association, the Academic Pediatric Association, the American Academy of Pediatrics, and the Society of Hospital Medicine). A. J. S. was supported by the Agency for Healthcare Research and Quality/Oregon Comparative Effectiveness Research K12 Program (1K12HS019456‐01). Additional funding for the I‐PASS Study was provided by the Medical Research Foundation of Oregon, Physician Services Incorporated Foundation (Ontario, Canada), and Pfizer (unrestricted medical education grant to N.D.S.). C.P.L, A.J.S. were supported by the Oregon Comparative Effectiveness Research K12 Program (1K12HS019456 from the Agency for Healthcare Research and Quality). A.J.S. was also supported by the Medical Research Foundation of Oregon. The authors report no conflicts of interest.
- , , , , . Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16(2):125–132.
- , , , , . Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out. J Hosp Med. 2006;1(4):257–266.
- , , . Development and implementation of an oral sign‐out skills curriculum. J Gen Intern Med. 2007;22(10):1470–1474.
- , , , , , . Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440.
- , , . A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc. 2014;21(1):154–162.
- , , , , . Review of computerized physician handoff tools for improving the quality of patient care. J Hosp Med. 2013;8(8):456–463.
- , , , , . Answering questions on call: pediatric resident physicians' use of handoffs and other resources. J Hosp Med. 2013;8(6):328–333.
- , , , . Effectiveness of written hospitalist sign‐outs in answering overnight inquiries. J Hosp Med. 2013;8(11):609–614.
- , , . Sign‐out snapshot: cross‐sectional evaluation of written sign‐outs among specialties. BMJ Qual Saf. 2014;23(1):66–72.
- , , , . An experimental comparison of handover methods. Ann R Coll Surg Engl. 2007;89(3):298–300.
- , , , . Pilot study to show the loss of important data in nursing handover. Br J Nurs. 2005;14(20):1090–1093.
- The Joint Commission. Hospital Accreditation Standards 2015: Joint Commission Resources; 2015:PC.02.02.01.
- Accreditation Council for Graduate Medical Education. Common Program Requirements. 2013; http://acgme.org/acgmeweb/tabid/429/ProgramandInstitutionalAccreditation/CommonProgramRequirements.aspx. Accessed May 11, 2015.
- , , , . Establishing a multisite education and research project requires leadership, expertise, collaboration, and an important aim. Pediatrics. 2010;126(4):619–622.
- , , , et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812.
- US Department of Health and Human Services. Agency for Healthcare Research and Quality. TeamSTEPPS website. Available at: http://teamstepps.ahrq.gov/. Accessed July 12, 2013.
- , , , , , . I‐PASS, a mnemonic to standardize verbal handoffs. Pediatrics. 2012;129(2):201–204.
- , , . The Team Handbook. 3rd ed. Middleton, WI: Oriel STAT A MATRIX; 2010.
- ACC/AHA Task Force on Practice Guidelines. Methodology Manual and Policies From the ACCF/AHA Task Force on Practice Guidelines. Available at: http://my.americanheart.org/idc/groups/ahamah‐public/@wcm/@sop/documents/downloadable/ucm_319826.pdf. Published June 2010. Accessed January 11, 2015.
- , , , et al. Effect of illness severity and comorbidity on patient safety and adverse events. Am J Med Qual. 2012;27(1):48–57.
- , , , , . Consequences of inadequate sign‐out for patient care. Arch Intern Med. 2008;168(16):1755–1760.
- , , , et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262–2270.
- , , , , . Medication discrepancies in resident sign‐outs and their potential to harm. J Gen Intern Med. 2007;22(12):1751–1755.
- , , , . Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Qual Saf. 2012;21(11):925–932.
- , , , , . Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24(2):77–87.
- , , , et al. Simple standardized patient handoff system that increases accuracy and completeness. J Surg Educ. 2008;65(6):476–485.
- , , , . Organizing the transfer of patient care information: the development of a computerized resident sign‐out system. Surgery. 2004;136(1):5–13.
- , , , , . A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200(4):538–545.
- , , . Template for success: using a resident‐designed sign‐out template in the handover of patient care. J Surg Educ. 2011;68(1):52–57.
- , , , , , . Read‐back improves information transfer in simulated clinical crises. BMJ Qual Saf. 2014;23(12):989–993.
- , , , , . Interns overestimate the effectiveness of their hand‐off communication. Pediatrics. 2010;125(3):491–496.
- , , , , , . Improving patient safety by repeating (read‐back) telephone reports of critical information. Am J Clin Pathol. 2004;121(6):801–803.
- , , , , . Content overlap in nurse and physician handoff artifacts and the potential role of electronic health records: a systematic review. J Biomed Inform. 2011;44(4):704–712.
- , , , . Clinical summarization capabilities of commercially‐available and internally‐developed electronic health records. Appl Clin Inform. 2012;3(1):80–93.
- , . An analysis and recommendations for multidisciplinary computerized handoff applications in hospitals. AMIA Annu Symp Proc. 2011;2011:588–597.
- , , , , . Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16(2):125–132.
- , , , , . Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out. J Hosp Med. 2006;1(4):257–266.
- , , . Development and implementation of an oral sign‐out skills curriculum. J Gen Intern Med. 2007;22(10):1470–1474.
- , , , , , . Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440.
- , , . A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc. 2014;21(1):154–162.
- , , , , . Review of computerized physician handoff tools for improving the quality of patient care. J Hosp Med. 2013;8(8):456–463.
- , , , , . Answering questions on call: pediatric resident physicians' use of handoffs and other resources. J Hosp Med. 2013;8(6):328–333.
- , , , . Effectiveness of written hospitalist sign‐outs in answering overnight inquiries. J Hosp Med. 2013;8(11):609–614.
- , , . Sign‐out snapshot: cross‐sectional evaluation of written sign‐outs among specialties. BMJ Qual Saf. 2014;23(1):66–72.
- , , , . An experimental comparison of handover methods. Ann R Coll Surg Engl. 2007;89(3):298–300.
- , , , . Pilot study to show the loss of important data in nursing handover. Br J Nurs. 2005;14(20):1090–1093.
- The Joint Commission. Hospital Accreditation Standards 2015: Joint Commission Resources; 2015:PC.02.02.01.
- Accreditation Council for Graduate Medical Education. Common Program Requirements. 2013; http://acgme.org/acgmeweb/tabid/429/ProgramandInstitutionalAccreditation/CommonProgramRequirements.aspx. Accessed May 11, 2015.
- , , , . Establishing a multisite education and research project requires leadership, expertise, collaboration, and an important aim. Pediatrics. 2010;126(4):619–622.
- , , , et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812.
- US Department of Health and Human Services. Agency for Healthcare Research and Quality. TeamSTEPPS website. Available at: http://teamstepps.ahrq.gov/. Accessed July 12, 2013.
- , , , , , . I‐PASS, a mnemonic to standardize verbal handoffs. Pediatrics. 2012;129(2):201–204.
- , , . The Team Handbook. 3rd ed. Middleton, WI: Oriel STAT A MATRIX; 2010.
- ACC/AHA Task Force on Practice Guidelines. Methodology Manual and Policies From the ACCF/AHA Task Force on Practice Guidelines. Available at: http://my.americanheart.org/idc/groups/ahamah‐public/@wcm/@sop/documents/downloadable/ucm_319826.pdf. Published June 2010. Accessed January 11, 2015.
- , , , et al. Effect of illness severity and comorbidity on patient safety and adverse events. Am J Med Qual. 2012;27(1):48–57.
- , , , , . Consequences of inadequate sign‐out for patient care. Arch Intern Med. 2008;168(16):1755–1760.
- , , , et al. Rates of medical errors and preventable adverse events among hospitalized children following implementation of a resident handoff bundle. JAMA. 2013;310(21):2262–2270.
- , , , , . Medication discrepancies in resident sign‐outs and their potential to harm. J Gen Intern Med. 2007;22(12):1751–1755.
- , , , . Avoiding handover fumbles: a controlled trial of a structured handover tool versus traditional handover methods. BMJ Qual Saf. 2012;21(11):925–932.
- , , , , . Using a computerized sign‐out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24(2):77–87.
- , , , et al. Simple standardized patient handoff system that increases accuracy and completeness. J Surg Educ. 2008;65(6):476–485.
- , , , . Organizing the transfer of patient care information: the development of a computerized resident sign‐out system. Surgery. 2004;136(1):5–13.
- , , , , . A randomized, controlled trial evaluating the impact of a computerized rounding and sign‐out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200(4):538–545.
- , , . Template for success: using a resident‐designed sign‐out template in the handover of patient care. J Surg Educ. 2011;68(1):52–57.
- , , , , , . Read‐back improves information transfer in simulated clinical crises. BMJ Qual Saf. 2014;23(12):989–993.
- , , , , . Interns overestimate the effectiveness of their hand‐off communication. Pediatrics. 2010;125(3):491–496.
- , , , , , . Improving patient safety by repeating (read‐back) telephone reports of critical information. Am J Clin Pathol. 2004;121(6):801–803.
- , , , , . Content overlap in nurse and physician handoff artifacts and the potential role of electronic health records: a systematic review. J Biomed Inform. 2011;44(4):704–712.
- , , , . Clinical summarization capabilities of commercially‐available and internally‐developed electronic health records. Appl Clin Inform. 2012;3(1):80–93.
- , . An analysis and recommendations for multidisciplinary computerized handoff applications in hospitals. AMIA Annu Symp Proc. 2011;2011:588–597.
© 2015 Society of Hospital Medicine
Pediatric Hospitalists' Influences
The number of pediatric hospitalists (PH) in the United States is increasing rapidly. The membership of the American Academy of Pediatrics (AAP) Section on Hospital Medicine has grown to 880 (7/10, AAP Section on Hospital Medicine), and there over 10,000 members of the Society of Hospital Medicine of which an estimated 5% care for children (7/10, Society of Hospital Medicine). Little is known about the educational contributions of pediatric hospitalists, residents' perceptions of hospitalists' roles, or how hospitalists may influence residents' eventual career plans even though 89% of pediatric hospitalists report they serve as teaching attendings.1 Teaching by hospitalists is well received and valued by residents, but, to date, all such data are from single institution studies of individual hospitalist programs.27 Less is known regarding what residents perceive about the differences in patient care provided by hospitalists as compared with traditional pediatric teaching attendings. There is a paucity of information about the level of interest of current pediatric residents in becoming hospitalists, including how many plan such a career, reasons why residents might prefer to become hospitalists, and their perceptions of Pediatric Hospital Medicine (PHM) careers as either long or short term. In addition, the effects of new residency graduates going into Hospital Medicine on the overall pediatric workforce, and how the availability of Hospital Medicine careers affects the choice of practice in Primary Care Pediatrics have not been examined.
We surveyed a national, randomly selected representative sample of pediatric residents to determine their level of exposure to hospitalist attending physicians during training. We asked the resident cohort about their educational experiences with hospitalists, patient care provided by hospitalists on their team, and career plans regarding becoming a hospitalist, including perceived needs for different or additional training. We obtained further information about reasons why hospitalist positions were appealing and about the current relationship between careers in Pediatric Hospital Medicine and Primary Care. To our knowledge, this is the first national study of how pediatric hospitalists might influence residents in the domains of education, patient care, and career planning.
METHODS
We conducted a survey of randomly selected pediatric residents from the AAP membership database. The selection was done by random generation by the AAP Department of Research from the membership database, in the same way members are selected for the annual Survey of Fellows and the annual pediatric level 3 (PL3) survey. Permission was obtained from the American Academy of Pediatrics Section on Residents (AAP SORe) to survey a selection of US pediatric residents in June 2007. The full sample of US pediatric residents included 9569 residents. The AAP SORe had 7694 e‐mail addresses from which the AAP Department of Research generated a random sample of 300 for our use, including Medicine‐Pediatric, Pediatric, and Pediatric Chief residents. One of the researchers (A.H.) sent an e‐mail with the title $200 AAP Career Raffle Survey containing a link to a SurveyMonkey survey (see Supporting Appendix AQuestionnaire in the online version of this article) and offering incentivized participation with a raffle. The need for informed consent was waived, as consent was implied by participation in the survey. The survey was taken anonymously by connecting through the link, and when it was completed, residents were asked to separately e‐mail a Section on Hospital Medicine address if they wished to participate in the raffle. Their raffle request was not linked to their survey results in any way. The $200 was supplied by the AAP Section on Hospital Medicine. The survey was sent 3 times. We analyzed responses with descriptive statistics. Institutional Review Board approval was obtained from Concord Hospital in Concord, New Hampshire.
RESULTS
The respondents are described in Figure 1 and Table 1. For their exposure to PHM, 54% (73 of 111) reported PH attendings in medical school; 90% (75 of 83) did have or will have PH attendings during residency, with no significant variation by program size (small, medium, large, or extra large). The degree of exposure was not asked. To learn about PHM, 47% (46 of 97 respondents) asked a PH in their program, while 28% (27 of 99) visited the AAP web site. Sixty‐eight percent (73 of 108) felt familiar or very familiar with PHM.
| % | Absolute Response Rate | |
|---|---|---|
| ||
| Training year | ||
| PL1 | 47.5 | 57 |
| PL2 | 35 | 42 |
| PL3 | 9 | 11 |
| PL4 | 1 | 1 |
| Skipped question | 7.5 | 9 |
| Gender | ||
| Male | 31.5 | 38 |
| Female | 61 | 73 |
| Skipped question | 7.5 | 9 |
| Specialty | ||
| Pediatrics | 79 | 95 |
| Med/Peds | 14 | 17 |
| Other (Pediatric combination residencies) | 4 | 5 |
| Skipped question | 3 | 3 |
| Program size | ||
| Less than 15 residents in program | 11 | 12 |
| 16‐30 | 38.5 | 42 |
| 31‐45 | 22.9 | 25 |
| Greater than 45 | 27.5 | 30 |
| Skipped question | 9.1 | 11 |
Table 2 summarizes the respondents' perception of PHM. They report a positive opinion of the field and overwhelmingly feel that PHM is a growing/developing field. Almost none feel PHM will not survive. A small percentage (10%, 28 of 99) felt there was no difference between PH and residents, with 25% (25 of 99) feeling some ambiguity about whether the PH role differs from that of a resident. Many (35 of 99) did not disagree that there is little difference between PH and resident positions, although most did. Sixty percent (59 of 99) agreed or strongly agreed that a PH position would be a good job for the short‐term. Forty‐seven percent (46 of 99) agreed in some form that PHM gives you something to do while you are waiting for another position. Given the choice of PHM as a long‐term opportunity, short‐term opportunity, either or not sure: 21% (21 of 98) saw PHM as a short‐term option only; 26% (25 of 98) saw PHM as a long‐term career only; 49% (48 of 98) saw it as either a short‐term option or long‐term career. Most (65%, 64 of 99) believed PH were better than primary care providers at caring for complex inpatients, but only 28% (28 of 99) thought PH provided better care for routine admissions. Most (82%, 81 of 99) agreed in some form that working with pediatric hospitalists enhances a resident's education.
| Strongly/Somewhat Disagree | Neither Disagree or Agree | Somewhat/Strongly Agree | |
|---|---|---|---|
| |||
| I think it is a great field | 2% (9/99) | 15% (15/99) | 83% (82/99) |
| It's a good job for the short‐term | 13% (13/99) | 27% (27/99) | 60% (59/99) |
| It gives you something to do while you are waiting for another position | 20% (20/99) | 33% (33/99) | 47% (46/99) |
| It's a growing/developing field | 1% (1/99) | 8% (8/99) | 91% (90/99) |
| It's a field that won't survive | 86% (85/99) | 13% (13/99) | 1% (1/99) |
| Hospitalists are better able to take care of complex inpatients than are primary care physicians | 20% (20/99) | 15% (15/99) | 65% (64/99) |
| Hospitalists are better able to take care of routine patient admissions than are primary care physicians | 39% (39/99) | 32% (32/99) | 28% (28/99) |
| There is little difference between hospitalist and resident positions | 65% (64/99) | 25% (25/99) | 10% (10/99) |
| Working with hospitalists enhances a residents education | 2% (2/99) | 16% (16/99) | 82% (81/99) |
On a 5‐point scale ranging from would definitely not include to might or might not include to would definitely include, the majority of respondents felt a PHM job would definitely include Pediatric Wards (86%, 84 of 98) and Inpatient Consultant for Specialists (54%, 52 of 97). Only 47% (46/97) felt the responsibilities would probably or definitely include Medical Student and Resident Education (47%, 46 of 97). The respondents were less certain (might or might not response) if PHM should include Normal Newborn Nursery (37%, 36 of 98), Delivery Room (42%, 41 of 98), Intensive Care Nursery (35%, 34 of 98), ED/Urgent Care (34%, 33 of 98), or Research (50%, 49 of 98). A majority of respondents felt PHM unlikely to include, or felt the job might not or might include: Outpatient Clinics (77%, 75 of 98), Outpatient Consults (81%, 79 of 98), and Pediatric Intensive Care Unit work (70%, 68 of 98).
Of categorical pediatric trainees answering the question, 35% (28 of 80) are considering a PHM career. Immediately post‐residency, 30% (24 of 80) of categorical trainees plan to enter Primary Care (PC), 4% (3 of 80) plan on PHM, and 3% (2 of 80) plan to pursue PH fellowship.
Of all respondents given the choice of whether a factor plays no role, limited role, or strong role in considering a career in PHM: flexible hours (96%, 94 of 98), opportunities to participate in education (97%, 95 of 98), and better salary than PC (94%, 91 of 97) would influence their decision to choose PHM. For 49% (48 of 98), ability to do the job without fellowship would play a strong role in choosing a career in PHM.
Forty‐five percent (44 of 97) support training in addition to residency; 16.5% (16 of 97) are against it; the remaining 38% (37 of 97) are unsure. Three percent (3 of 98) thought 3‐year fellowship best, while 28% (27 of 98) preferred 2‐year fellowship; 29% (28 of 98) would like a hospitalist‐track residency; 28% (27 of 98) believe standard residency sufficient; and 4% (4 of 98) felt a chief year adequate. If they were to pursue PHM, 31% (30 of 98) would enter PH fellowship, 34% (33 of 98) would not, and 36% (35 of 98) were unsure.
On a 5‐point scale, respondents were asked about barriers identified to choosing a career in PHM: 28% (27 of 96) agreed or strongly agreed that not feeling well‐enough trained was a barrier to entering the field; 42% (40 of 96) were agreed in some form that they were unsure of what training they needed; 39% (37 of 95) were unsure about where positions are available. Seven percent (7 of 98) of respondents were less likely to choose to practice Primary Care (PC) pediatrics because of hospitalists. Of respondents choosing PC, 59% (34 of 58) prefer or must have PH to work within their future practices, while 12% (7 of 58) prefer not to, or definitely do not want to, work with PH.
DISCUSSION
In 2006, the American Board of Pediatrics (ABP) General Pediatrics Career Survey found that 1% of first‐time applicants were taking a hospitalist position.8 In 2007, this number grew to 3% choosing a position in Pediatric Hospital Medicine.9, 10 The 2009‐2010 survey data found that 7.6% of first‐time applicants would be taking a job as hospitalist as of July 1.11 Our data suggest this number will continue to grow over the next few years. The growth of PHM has prompted an in‐depth look at the field by the ABP.1, 12, 13 PHM programs appear to have become part of the fabric of pediatric care, with the majority of hospitals with PHM programs planning to continue the programs despite the need to pay for value‐added by hospitalists beyond revenue received for their direct clinical service.13 Looking forward, when the Institute of Medicine recommendations to further restrict resident work hours to 16 hour shifts are implemented, many programs plan on increasing their PHM programs.14, 15 Therefore, residents' views of a career in PHM are important, as they give perspective on attitudes of those who might be, or interact with, hospitalists in the future, and should impact training programs for residents regardless of their interest in a career in PHM.
Our national data support local, large institution studies that hospitalists are positively impacting education.27 However, this study suggests that this is not only a local or large academic center phenomenon, but a national trend towards providing a different and positive education experience for pediatric residents. This mirrors the opinion of the majority of residency and clerkship directors who feel that hospitalists are more accessible to trainees than traditional attendings.12 Training programs should consider this impact when selecting attending hospitalists and supporting their roles as mentors and educators.
As residents finish their training and seek positions as pediatric hospitalists, programs need to be aware that a significant percentage of residents in our survey see PHM as a short‐term career option and/or fail to see a difference between a PH job and their own. Program Directors also need to be aware of the breadth of PHM practice which can include areas our respondents felt were less likely to be part of PHM, such as other inpatient areas and the expectation of research.
While 1 option to address some of these issues is fellowship training, this is not a simple decision. PHM needs to determine if fellowship is truly the best option for future hospitalists and, if so, what the fellowship should look like in terms of duration and scope. While the needs of optimal training should be paramount, resident preferences to not commit to an additional 3 years of training must be considered. Many residents fail to see a difference between the role of PH and their own role during training, and feel that the current format of residency training is all the preparation needed to step into a career as a PH. This demonstrates a clear gap between resident perceptions of PHM and the accepted definition of a hospitalist,16 which reaches far beyond direct inpatient care. While The Core Competencies for Pediatric Hospital Medicine17 address a number of these areas, neither trainees nor hospitalists themselves have fully integrated these into their practice. PH must recognize and prepare for their position as mentors and role models to residents. This responsibility should differentiate PH role from that of a resident, demonstrating roles PH play in policy making, patient safety and quality initiatives, in administration, and in providing advanced thinking in direct patient care. Finally, PH and their employers must work to build programs that present PHM as a long‐term career option for residents.
There is a significant impact on the field if those who enter it see it only as something to do while waiting for a position elsewhere. While some of these new‐careerists may stay with the field once they have tried it and become significant contributors, inherent in these answers are the issues of turnover and lack of senior experience many Hospital Medicine programs currently face. Additionally, and outside the scope of this survey, it is unclear what those next positions are and how a brief experience as a hospitalist might impact their future practice.
It is a significant change that residents entering a Primary Care career expect to work with pediatric hospitalists and, in general, see this as a benefit and necessity. The 2007 American Board of Pediatrics' survey found that 27% of respondents planned a career in General Pediatrics with little or no inpatient care.10 Hospitalists of the near future will likely face a dichotomy of needs between primary care providers who trained before, and those who trained after, the existence of hospitalists. Hospitalists will need to understand and address the ongoing needs of both of these groups in order to adequately serve them and their patient‐bases.
Limitations of our study include our small sample size, with a response rate of 43% at best (individual question response rate varied). Though the group was nationally representative, it was skewed towards first year respondents, likely due to the time of year in which it was distributed. There is likely some bias due to the low response rate, in that those more interested in careers as hospitalists might be more likely to respond. This might potentially inflate the percentages of those who state they are interested in being a hospitalist. In addition, given that the last round of the survey went out at the very end of the academic year, graduating residents had a lower response rate.
We were unable to compare opinions across unexposed and exposed residents because only 6.5% reported knowing nothing about the field, and only 2 respondents had not had any exposure to pediatric hospitalists to date. Given that most residencies have PHM services,12 this distinction is unlikely to be significant. In looking at training desires, we did not compare them to residents considering entering other fields of medicine. It may be true that residents considering other fellowships do not desire to do 3 years of fellowship training. That being said, it in no way diminishes the implication that 3‐year fellowships for PHM may not be the right answer for future training.
Strengths of the study include that it is, to our knowledge, the first national study of a group of residents regarding exposure to, and career plans as related to, PH. In addition, the group is gender‐balanced, and represents residents from a range of training sites (urban, suburban, rural) and program sizes. This study offers important information that must be considered in the further development of the field of Pediatric Hospital Medicine.
CONCLUSION
This was the first national study of residents regarding Pediatric Hospital Medicine. Almost all residents are exposed to PH during their training, though a gap of no exposure still exists. More work needs to be done to improve the perception of PHM as a viable long‐term career. Nevertheless, PHM has become a career consideration for trainees. Nearly half agreed that some type of specialized training would be helpful. This information should impact on the development of PHM training programs.
Acknowledgements
Thanks to the American Academy of Pediatrics Section on Hospital Medicine for raffle funding, and Texas Children's Hospital and Dr Yong Han for use of SurveyMonkey and assistance with survey set‐up. Also thanks to Dr Vincent Chang for his guidance and review.
- ,,,;for the Research Advisory Committee of the American Board of Pediatrics.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- ,,.Establishing a pediatric hospitalist program at an academic medical center.Clin Pediatr (Phila).2000;39(4):221–227.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr (Phila).2001;40(12):653–660.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76(5):556.
- ,,,,,.Community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.Pediatrics.2005;115(1):34–38.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117(5):1736–1744.
- American Board of Pediatrics. 2006 General Pediatrics Career Survey. Available at: http://www.abp.org. Accessed on January 15, 2008.
- ,,,,;for the Research Advisory Committee of the American Board of Pediatrics.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(1 suppl):S26–S30.
- American Board of Pediatrics. 2007 General Pediatrics Career Survey. Available at: http://www.abp.org. Accessed July 10,2009.
- American Board of Pediatrics. 2009–2010 Workforce Data. Available at: http://www.abp.org. Accessed July 20,2010.
- ,,.Hospitalists' involvement in pediatrics training: perspectives from pediatric residency program and clerkship directors.Acad Med.2009;84(11):1617–1621.
- ,,.Assessing the value of pediatric hospitalist programs: the perspective of hospital leaders.Acad Pediatr.2009;9(3):192–196.
- ,,,.Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist.J Hosp Med.2011;6(in press).
- Accreditation Council for Graduate Medical Education. Available at: http://acgme‐2010standards.org/. Accessed December 15, 2010.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Hospitalist_Definition5:i–iv. doi://10.1002/jhm.776. Available at: http://www3.interscience.wiley.com. Accessed on May 11, 2011.
The number of pediatric hospitalists (PH) in the United States is increasing rapidly. The membership of the American Academy of Pediatrics (AAP) Section on Hospital Medicine has grown to 880 (7/10, AAP Section on Hospital Medicine), and there over 10,000 members of the Society of Hospital Medicine of which an estimated 5% care for children (7/10, Society of Hospital Medicine). Little is known about the educational contributions of pediatric hospitalists, residents' perceptions of hospitalists' roles, or how hospitalists may influence residents' eventual career plans even though 89% of pediatric hospitalists report they serve as teaching attendings.1 Teaching by hospitalists is well received and valued by residents, but, to date, all such data are from single institution studies of individual hospitalist programs.27 Less is known regarding what residents perceive about the differences in patient care provided by hospitalists as compared with traditional pediatric teaching attendings. There is a paucity of information about the level of interest of current pediatric residents in becoming hospitalists, including how many plan such a career, reasons why residents might prefer to become hospitalists, and their perceptions of Pediatric Hospital Medicine (PHM) careers as either long or short term. In addition, the effects of new residency graduates going into Hospital Medicine on the overall pediatric workforce, and how the availability of Hospital Medicine careers affects the choice of practice in Primary Care Pediatrics have not been examined.
We surveyed a national, randomly selected representative sample of pediatric residents to determine their level of exposure to hospitalist attending physicians during training. We asked the resident cohort about their educational experiences with hospitalists, patient care provided by hospitalists on their team, and career plans regarding becoming a hospitalist, including perceived needs for different or additional training. We obtained further information about reasons why hospitalist positions were appealing and about the current relationship between careers in Pediatric Hospital Medicine and Primary Care. To our knowledge, this is the first national study of how pediatric hospitalists might influence residents in the domains of education, patient care, and career planning.
METHODS
We conducted a survey of randomly selected pediatric residents from the AAP membership database. The selection was done by random generation by the AAP Department of Research from the membership database, in the same way members are selected for the annual Survey of Fellows and the annual pediatric level 3 (PL3) survey. Permission was obtained from the American Academy of Pediatrics Section on Residents (AAP SORe) to survey a selection of US pediatric residents in June 2007. The full sample of US pediatric residents included 9569 residents. The AAP SORe had 7694 e‐mail addresses from which the AAP Department of Research generated a random sample of 300 for our use, including Medicine‐Pediatric, Pediatric, and Pediatric Chief residents. One of the researchers (A.H.) sent an e‐mail with the title $200 AAP Career Raffle Survey containing a link to a SurveyMonkey survey (see Supporting Appendix AQuestionnaire in the online version of this article) and offering incentivized participation with a raffle. The need for informed consent was waived, as consent was implied by participation in the survey. The survey was taken anonymously by connecting through the link, and when it was completed, residents were asked to separately e‐mail a Section on Hospital Medicine address if they wished to participate in the raffle. Their raffle request was not linked to their survey results in any way. The $200 was supplied by the AAP Section on Hospital Medicine. The survey was sent 3 times. We analyzed responses with descriptive statistics. Institutional Review Board approval was obtained from Concord Hospital in Concord, New Hampshire.
RESULTS
The respondents are described in Figure 1 and Table 1. For their exposure to PHM, 54% (73 of 111) reported PH attendings in medical school; 90% (75 of 83) did have or will have PH attendings during residency, with no significant variation by program size (small, medium, large, or extra large). The degree of exposure was not asked. To learn about PHM, 47% (46 of 97 respondents) asked a PH in their program, while 28% (27 of 99) visited the AAP web site. Sixty‐eight percent (73 of 108) felt familiar or very familiar with PHM.
| % | Absolute Response Rate | |
|---|---|---|
| ||
| Training year | ||
| PL1 | 47.5 | 57 |
| PL2 | 35 | 42 |
| PL3 | 9 | 11 |
| PL4 | 1 | 1 |
| Skipped question | 7.5 | 9 |
| Gender | ||
| Male | 31.5 | 38 |
| Female | 61 | 73 |
| Skipped question | 7.5 | 9 |
| Specialty | ||
| Pediatrics | 79 | 95 |
| Med/Peds | 14 | 17 |
| Other (Pediatric combination residencies) | 4 | 5 |
| Skipped question | 3 | 3 |
| Program size | ||
| Less than 15 residents in program | 11 | 12 |
| 16‐30 | 38.5 | 42 |
| 31‐45 | 22.9 | 25 |
| Greater than 45 | 27.5 | 30 |
| Skipped question | 9.1 | 11 |
Table 2 summarizes the respondents' perception of PHM. They report a positive opinion of the field and overwhelmingly feel that PHM is a growing/developing field. Almost none feel PHM will not survive. A small percentage (10%, 28 of 99) felt there was no difference between PH and residents, with 25% (25 of 99) feeling some ambiguity about whether the PH role differs from that of a resident. Many (35 of 99) did not disagree that there is little difference between PH and resident positions, although most did. Sixty percent (59 of 99) agreed or strongly agreed that a PH position would be a good job for the short‐term. Forty‐seven percent (46 of 99) agreed in some form that PHM gives you something to do while you are waiting for another position. Given the choice of PHM as a long‐term opportunity, short‐term opportunity, either or not sure: 21% (21 of 98) saw PHM as a short‐term option only; 26% (25 of 98) saw PHM as a long‐term career only; 49% (48 of 98) saw it as either a short‐term option or long‐term career. Most (65%, 64 of 99) believed PH were better than primary care providers at caring for complex inpatients, but only 28% (28 of 99) thought PH provided better care for routine admissions. Most (82%, 81 of 99) agreed in some form that working with pediatric hospitalists enhances a resident's education.
| Strongly/Somewhat Disagree | Neither Disagree or Agree | Somewhat/Strongly Agree | |
|---|---|---|---|
| |||
| I think it is a great field | 2% (9/99) | 15% (15/99) | 83% (82/99) |
| It's a good job for the short‐term | 13% (13/99) | 27% (27/99) | 60% (59/99) |
| It gives you something to do while you are waiting for another position | 20% (20/99) | 33% (33/99) | 47% (46/99) |
| It's a growing/developing field | 1% (1/99) | 8% (8/99) | 91% (90/99) |
| It's a field that won't survive | 86% (85/99) | 13% (13/99) | 1% (1/99) |
| Hospitalists are better able to take care of complex inpatients than are primary care physicians | 20% (20/99) | 15% (15/99) | 65% (64/99) |
| Hospitalists are better able to take care of routine patient admissions than are primary care physicians | 39% (39/99) | 32% (32/99) | 28% (28/99) |
| There is little difference between hospitalist and resident positions | 65% (64/99) | 25% (25/99) | 10% (10/99) |
| Working with hospitalists enhances a residents education | 2% (2/99) | 16% (16/99) | 82% (81/99) |
On a 5‐point scale ranging from would definitely not include to might or might not include to would definitely include, the majority of respondents felt a PHM job would definitely include Pediatric Wards (86%, 84 of 98) and Inpatient Consultant for Specialists (54%, 52 of 97). Only 47% (46/97) felt the responsibilities would probably or definitely include Medical Student and Resident Education (47%, 46 of 97). The respondents were less certain (might or might not response) if PHM should include Normal Newborn Nursery (37%, 36 of 98), Delivery Room (42%, 41 of 98), Intensive Care Nursery (35%, 34 of 98), ED/Urgent Care (34%, 33 of 98), or Research (50%, 49 of 98). A majority of respondents felt PHM unlikely to include, or felt the job might not or might include: Outpatient Clinics (77%, 75 of 98), Outpatient Consults (81%, 79 of 98), and Pediatric Intensive Care Unit work (70%, 68 of 98).
Of categorical pediatric trainees answering the question, 35% (28 of 80) are considering a PHM career. Immediately post‐residency, 30% (24 of 80) of categorical trainees plan to enter Primary Care (PC), 4% (3 of 80) plan on PHM, and 3% (2 of 80) plan to pursue PH fellowship.
Of all respondents given the choice of whether a factor plays no role, limited role, or strong role in considering a career in PHM: flexible hours (96%, 94 of 98), opportunities to participate in education (97%, 95 of 98), and better salary than PC (94%, 91 of 97) would influence their decision to choose PHM. For 49% (48 of 98), ability to do the job without fellowship would play a strong role in choosing a career in PHM.
Forty‐five percent (44 of 97) support training in addition to residency; 16.5% (16 of 97) are against it; the remaining 38% (37 of 97) are unsure. Three percent (3 of 98) thought 3‐year fellowship best, while 28% (27 of 98) preferred 2‐year fellowship; 29% (28 of 98) would like a hospitalist‐track residency; 28% (27 of 98) believe standard residency sufficient; and 4% (4 of 98) felt a chief year adequate. If they were to pursue PHM, 31% (30 of 98) would enter PH fellowship, 34% (33 of 98) would not, and 36% (35 of 98) were unsure.
On a 5‐point scale, respondents were asked about barriers identified to choosing a career in PHM: 28% (27 of 96) agreed or strongly agreed that not feeling well‐enough trained was a barrier to entering the field; 42% (40 of 96) were agreed in some form that they were unsure of what training they needed; 39% (37 of 95) were unsure about where positions are available. Seven percent (7 of 98) of respondents were less likely to choose to practice Primary Care (PC) pediatrics because of hospitalists. Of respondents choosing PC, 59% (34 of 58) prefer or must have PH to work within their future practices, while 12% (7 of 58) prefer not to, or definitely do not want to, work with PH.
DISCUSSION
In 2006, the American Board of Pediatrics (ABP) General Pediatrics Career Survey found that 1% of first‐time applicants were taking a hospitalist position.8 In 2007, this number grew to 3% choosing a position in Pediatric Hospital Medicine.9, 10 The 2009‐2010 survey data found that 7.6% of first‐time applicants would be taking a job as hospitalist as of July 1.11 Our data suggest this number will continue to grow over the next few years. The growth of PHM has prompted an in‐depth look at the field by the ABP.1, 12, 13 PHM programs appear to have become part of the fabric of pediatric care, with the majority of hospitals with PHM programs planning to continue the programs despite the need to pay for value‐added by hospitalists beyond revenue received for their direct clinical service.13 Looking forward, when the Institute of Medicine recommendations to further restrict resident work hours to 16 hour shifts are implemented, many programs plan on increasing their PHM programs.14, 15 Therefore, residents' views of a career in PHM are important, as they give perspective on attitudes of those who might be, or interact with, hospitalists in the future, and should impact training programs for residents regardless of their interest in a career in PHM.
Our national data support local, large institution studies that hospitalists are positively impacting education.27 However, this study suggests that this is not only a local or large academic center phenomenon, but a national trend towards providing a different and positive education experience for pediatric residents. This mirrors the opinion of the majority of residency and clerkship directors who feel that hospitalists are more accessible to trainees than traditional attendings.12 Training programs should consider this impact when selecting attending hospitalists and supporting their roles as mentors and educators.
As residents finish their training and seek positions as pediatric hospitalists, programs need to be aware that a significant percentage of residents in our survey see PHM as a short‐term career option and/or fail to see a difference between a PH job and their own. Program Directors also need to be aware of the breadth of PHM practice which can include areas our respondents felt were less likely to be part of PHM, such as other inpatient areas and the expectation of research.
While 1 option to address some of these issues is fellowship training, this is not a simple decision. PHM needs to determine if fellowship is truly the best option for future hospitalists and, if so, what the fellowship should look like in terms of duration and scope. While the needs of optimal training should be paramount, resident preferences to not commit to an additional 3 years of training must be considered. Many residents fail to see a difference between the role of PH and their own role during training, and feel that the current format of residency training is all the preparation needed to step into a career as a PH. This demonstrates a clear gap between resident perceptions of PHM and the accepted definition of a hospitalist,16 which reaches far beyond direct inpatient care. While The Core Competencies for Pediatric Hospital Medicine17 address a number of these areas, neither trainees nor hospitalists themselves have fully integrated these into their practice. PH must recognize and prepare for their position as mentors and role models to residents. This responsibility should differentiate PH role from that of a resident, demonstrating roles PH play in policy making, patient safety and quality initiatives, in administration, and in providing advanced thinking in direct patient care. Finally, PH and their employers must work to build programs that present PHM as a long‐term career option for residents.
There is a significant impact on the field if those who enter it see it only as something to do while waiting for a position elsewhere. While some of these new‐careerists may stay with the field once they have tried it and become significant contributors, inherent in these answers are the issues of turnover and lack of senior experience many Hospital Medicine programs currently face. Additionally, and outside the scope of this survey, it is unclear what those next positions are and how a brief experience as a hospitalist might impact their future practice.
It is a significant change that residents entering a Primary Care career expect to work with pediatric hospitalists and, in general, see this as a benefit and necessity. The 2007 American Board of Pediatrics' survey found that 27% of respondents planned a career in General Pediatrics with little or no inpatient care.10 Hospitalists of the near future will likely face a dichotomy of needs between primary care providers who trained before, and those who trained after, the existence of hospitalists. Hospitalists will need to understand and address the ongoing needs of both of these groups in order to adequately serve them and their patient‐bases.
Limitations of our study include our small sample size, with a response rate of 43% at best (individual question response rate varied). Though the group was nationally representative, it was skewed towards first year respondents, likely due to the time of year in which it was distributed. There is likely some bias due to the low response rate, in that those more interested in careers as hospitalists might be more likely to respond. This might potentially inflate the percentages of those who state they are interested in being a hospitalist. In addition, given that the last round of the survey went out at the very end of the academic year, graduating residents had a lower response rate.
We were unable to compare opinions across unexposed and exposed residents because only 6.5% reported knowing nothing about the field, and only 2 respondents had not had any exposure to pediatric hospitalists to date. Given that most residencies have PHM services,12 this distinction is unlikely to be significant. In looking at training desires, we did not compare them to residents considering entering other fields of medicine. It may be true that residents considering other fellowships do not desire to do 3 years of fellowship training. That being said, it in no way diminishes the implication that 3‐year fellowships for PHM may not be the right answer for future training.
Strengths of the study include that it is, to our knowledge, the first national study of a group of residents regarding exposure to, and career plans as related to, PH. In addition, the group is gender‐balanced, and represents residents from a range of training sites (urban, suburban, rural) and program sizes. This study offers important information that must be considered in the further development of the field of Pediatric Hospital Medicine.
CONCLUSION
This was the first national study of residents regarding Pediatric Hospital Medicine. Almost all residents are exposed to PH during their training, though a gap of no exposure still exists. More work needs to be done to improve the perception of PHM as a viable long‐term career. Nevertheless, PHM has become a career consideration for trainees. Nearly half agreed that some type of specialized training would be helpful. This information should impact on the development of PHM training programs.
Acknowledgements
Thanks to the American Academy of Pediatrics Section on Hospital Medicine for raffle funding, and Texas Children's Hospital and Dr Yong Han for use of SurveyMonkey and assistance with survey set‐up. Also thanks to Dr Vincent Chang for his guidance and review.
The number of pediatric hospitalists (PH) in the United States is increasing rapidly. The membership of the American Academy of Pediatrics (AAP) Section on Hospital Medicine has grown to 880 (7/10, AAP Section on Hospital Medicine), and there over 10,000 members of the Society of Hospital Medicine of which an estimated 5% care for children (7/10, Society of Hospital Medicine). Little is known about the educational contributions of pediatric hospitalists, residents' perceptions of hospitalists' roles, or how hospitalists may influence residents' eventual career plans even though 89% of pediatric hospitalists report they serve as teaching attendings.1 Teaching by hospitalists is well received and valued by residents, but, to date, all such data are from single institution studies of individual hospitalist programs.27 Less is known regarding what residents perceive about the differences in patient care provided by hospitalists as compared with traditional pediatric teaching attendings. There is a paucity of information about the level of interest of current pediatric residents in becoming hospitalists, including how many plan such a career, reasons why residents might prefer to become hospitalists, and their perceptions of Pediatric Hospital Medicine (PHM) careers as either long or short term. In addition, the effects of new residency graduates going into Hospital Medicine on the overall pediatric workforce, and how the availability of Hospital Medicine careers affects the choice of practice in Primary Care Pediatrics have not been examined.
We surveyed a national, randomly selected representative sample of pediatric residents to determine their level of exposure to hospitalist attending physicians during training. We asked the resident cohort about their educational experiences with hospitalists, patient care provided by hospitalists on their team, and career plans regarding becoming a hospitalist, including perceived needs for different or additional training. We obtained further information about reasons why hospitalist positions were appealing and about the current relationship between careers in Pediatric Hospital Medicine and Primary Care. To our knowledge, this is the first national study of how pediatric hospitalists might influence residents in the domains of education, patient care, and career planning.
METHODS
We conducted a survey of randomly selected pediatric residents from the AAP membership database. The selection was done by random generation by the AAP Department of Research from the membership database, in the same way members are selected for the annual Survey of Fellows and the annual pediatric level 3 (PL3) survey. Permission was obtained from the American Academy of Pediatrics Section on Residents (AAP SORe) to survey a selection of US pediatric residents in June 2007. The full sample of US pediatric residents included 9569 residents. The AAP SORe had 7694 e‐mail addresses from which the AAP Department of Research generated a random sample of 300 for our use, including Medicine‐Pediatric, Pediatric, and Pediatric Chief residents. One of the researchers (A.H.) sent an e‐mail with the title $200 AAP Career Raffle Survey containing a link to a SurveyMonkey survey (see Supporting Appendix AQuestionnaire in the online version of this article) and offering incentivized participation with a raffle. The need for informed consent was waived, as consent was implied by participation in the survey. The survey was taken anonymously by connecting through the link, and when it was completed, residents were asked to separately e‐mail a Section on Hospital Medicine address if they wished to participate in the raffle. Their raffle request was not linked to their survey results in any way. The $200 was supplied by the AAP Section on Hospital Medicine. The survey was sent 3 times. We analyzed responses with descriptive statistics. Institutional Review Board approval was obtained from Concord Hospital in Concord, New Hampshire.
RESULTS
The respondents are described in Figure 1 and Table 1. For their exposure to PHM, 54% (73 of 111) reported PH attendings in medical school; 90% (75 of 83) did have or will have PH attendings during residency, with no significant variation by program size (small, medium, large, or extra large). The degree of exposure was not asked. To learn about PHM, 47% (46 of 97 respondents) asked a PH in their program, while 28% (27 of 99) visited the AAP web site. Sixty‐eight percent (73 of 108) felt familiar or very familiar with PHM.
| % | Absolute Response Rate | |
|---|---|---|
| ||
| Training year | ||
| PL1 | 47.5 | 57 |
| PL2 | 35 | 42 |
| PL3 | 9 | 11 |
| PL4 | 1 | 1 |
| Skipped question | 7.5 | 9 |
| Gender | ||
| Male | 31.5 | 38 |
| Female | 61 | 73 |
| Skipped question | 7.5 | 9 |
| Specialty | ||
| Pediatrics | 79 | 95 |
| Med/Peds | 14 | 17 |
| Other (Pediatric combination residencies) | 4 | 5 |
| Skipped question | 3 | 3 |
| Program size | ||
| Less than 15 residents in program | 11 | 12 |
| 16‐30 | 38.5 | 42 |
| 31‐45 | 22.9 | 25 |
| Greater than 45 | 27.5 | 30 |
| Skipped question | 9.1 | 11 |
Table 2 summarizes the respondents' perception of PHM. They report a positive opinion of the field and overwhelmingly feel that PHM is a growing/developing field. Almost none feel PHM will not survive. A small percentage (10%, 28 of 99) felt there was no difference between PH and residents, with 25% (25 of 99) feeling some ambiguity about whether the PH role differs from that of a resident. Many (35 of 99) did not disagree that there is little difference between PH and resident positions, although most did. Sixty percent (59 of 99) agreed or strongly agreed that a PH position would be a good job for the short‐term. Forty‐seven percent (46 of 99) agreed in some form that PHM gives you something to do while you are waiting for another position. Given the choice of PHM as a long‐term opportunity, short‐term opportunity, either or not sure: 21% (21 of 98) saw PHM as a short‐term option only; 26% (25 of 98) saw PHM as a long‐term career only; 49% (48 of 98) saw it as either a short‐term option or long‐term career. Most (65%, 64 of 99) believed PH were better than primary care providers at caring for complex inpatients, but only 28% (28 of 99) thought PH provided better care for routine admissions. Most (82%, 81 of 99) agreed in some form that working with pediatric hospitalists enhances a resident's education.
| Strongly/Somewhat Disagree | Neither Disagree or Agree | Somewhat/Strongly Agree | |
|---|---|---|---|
| |||
| I think it is a great field | 2% (9/99) | 15% (15/99) | 83% (82/99) |
| It's a good job for the short‐term | 13% (13/99) | 27% (27/99) | 60% (59/99) |
| It gives you something to do while you are waiting for another position | 20% (20/99) | 33% (33/99) | 47% (46/99) |
| It's a growing/developing field | 1% (1/99) | 8% (8/99) | 91% (90/99) |
| It's a field that won't survive | 86% (85/99) | 13% (13/99) | 1% (1/99) |
| Hospitalists are better able to take care of complex inpatients than are primary care physicians | 20% (20/99) | 15% (15/99) | 65% (64/99) |
| Hospitalists are better able to take care of routine patient admissions than are primary care physicians | 39% (39/99) | 32% (32/99) | 28% (28/99) |
| There is little difference between hospitalist and resident positions | 65% (64/99) | 25% (25/99) | 10% (10/99) |
| Working with hospitalists enhances a residents education | 2% (2/99) | 16% (16/99) | 82% (81/99) |
On a 5‐point scale ranging from would definitely not include to might or might not include to would definitely include, the majority of respondents felt a PHM job would definitely include Pediatric Wards (86%, 84 of 98) and Inpatient Consultant for Specialists (54%, 52 of 97). Only 47% (46/97) felt the responsibilities would probably or definitely include Medical Student and Resident Education (47%, 46 of 97). The respondents were less certain (might or might not response) if PHM should include Normal Newborn Nursery (37%, 36 of 98), Delivery Room (42%, 41 of 98), Intensive Care Nursery (35%, 34 of 98), ED/Urgent Care (34%, 33 of 98), or Research (50%, 49 of 98). A majority of respondents felt PHM unlikely to include, or felt the job might not or might include: Outpatient Clinics (77%, 75 of 98), Outpatient Consults (81%, 79 of 98), and Pediatric Intensive Care Unit work (70%, 68 of 98).
Of categorical pediatric trainees answering the question, 35% (28 of 80) are considering a PHM career. Immediately post‐residency, 30% (24 of 80) of categorical trainees plan to enter Primary Care (PC), 4% (3 of 80) plan on PHM, and 3% (2 of 80) plan to pursue PH fellowship.
Of all respondents given the choice of whether a factor plays no role, limited role, or strong role in considering a career in PHM: flexible hours (96%, 94 of 98), opportunities to participate in education (97%, 95 of 98), and better salary than PC (94%, 91 of 97) would influence their decision to choose PHM. For 49% (48 of 98), ability to do the job without fellowship would play a strong role in choosing a career in PHM.
Forty‐five percent (44 of 97) support training in addition to residency; 16.5% (16 of 97) are against it; the remaining 38% (37 of 97) are unsure. Three percent (3 of 98) thought 3‐year fellowship best, while 28% (27 of 98) preferred 2‐year fellowship; 29% (28 of 98) would like a hospitalist‐track residency; 28% (27 of 98) believe standard residency sufficient; and 4% (4 of 98) felt a chief year adequate. If they were to pursue PHM, 31% (30 of 98) would enter PH fellowship, 34% (33 of 98) would not, and 36% (35 of 98) were unsure.
On a 5‐point scale, respondents were asked about barriers identified to choosing a career in PHM: 28% (27 of 96) agreed or strongly agreed that not feeling well‐enough trained was a barrier to entering the field; 42% (40 of 96) were agreed in some form that they were unsure of what training they needed; 39% (37 of 95) were unsure about where positions are available. Seven percent (7 of 98) of respondents were less likely to choose to practice Primary Care (PC) pediatrics because of hospitalists. Of respondents choosing PC, 59% (34 of 58) prefer or must have PH to work within their future practices, while 12% (7 of 58) prefer not to, or definitely do not want to, work with PH.
DISCUSSION
In 2006, the American Board of Pediatrics (ABP) General Pediatrics Career Survey found that 1% of first‐time applicants were taking a hospitalist position.8 In 2007, this number grew to 3% choosing a position in Pediatric Hospital Medicine.9, 10 The 2009‐2010 survey data found that 7.6% of first‐time applicants would be taking a job as hospitalist as of July 1.11 Our data suggest this number will continue to grow over the next few years. The growth of PHM has prompted an in‐depth look at the field by the ABP.1, 12, 13 PHM programs appear to have become part of the fabric of pediatric care, with the majority of hospitals with PHM programs planning to continue the programs despite the need to pay for value‐added by hospitalists beyond revenue received for their direct clinical service.13 Looking forward, when the Institute of Medicine recommendations to further restrict resident work hours to 16 hour shifts are implemented, many programs plan on increasing their PHM programs.14, 15 Therefore, residents' views of a career in PHM are important, as they give perspective on attitudes of those who might be, or interact with, hospitalists in the future, and should impact training programs for residents regardless of their interest in a career in PHM.
Our national data support local, large institution studies that hospitalists are positively impacting education.27 However, this study suggests that this is not only a local or large academic center phenomenon, but a national trend towards providing a different and positive education experience for pediatric residents. This mirrors the opinion of the majority of residency and clerkship directors who feel that hospitalists are more accessible to trainees than traditional attendings.12 Training programs should consider this impact when selecting attending hospitalists and supporting their roles as mentors and educators.
As residents finish their training and seek positions as pediatric hospitalists, programs need to be aware that a significant percentage of residents in our survey see PHM as a short‐term career option and/or fail to see a difference between a PH job and their own. Program Directors also need to be aware of the breadth of PHM practice which can include areas our respondents felt were less likely to be part of PHM, such as other inpatient areas and the expectation of research.
While 1 option to address some of these issues is fellowship training, this is not a simple decision. PHM needs to determine if fellowship is truly the best option for future hospitalists and, if so, what the fellowship should look like in terms of duration and scope. While the needs of optimal training should be paramount, resident preferences to not commit to an additional 3 years of training must be considered. Many residents fail to see a difference between the role of PH and their own role during training, and feel that the current format of residency training is all the preparation needed to step into a career as a PH. This demonstrates a clear gap between resident perceptions of PHM and the accepted definition of a hospitalist,16 which reaches far beyond direct inpatient care. While The Core Competencies for Pediatric Hospital Medicine17 address a number of these areas, neither trainees nor hospitalists themselves have fully integrated these into their practice. PH must recognize and prepare for their position as mentors and role models to residents. This responsibility should differentiate PH role from that of a resident, demonstrating roles PH play in policy making, patient safety and quality initiatives, in administration, and in providing advanced thinking in direct patient care. Finally, PH and their employers must work to build programs that present PHM as a long‐term career option for residents.
There is a significant impact on the field if those who enter it see it only as something to do while waiting for a position elsewhere. While some of these new‐careerists may stay with the field once they have tried it and become significant contributors, inherent in these answers are the issues of turnover and lack of senior experience many Hospital Medicine programs currently face. Additionally, and outside the scope of this survey, it is unclear what those next positions are and how a brief experience as a hospitalist might impact their future practice.
It is a significant change that residents entering a Primary Care career expect to work with pediatric hospitalists and, in general, see this as a benefit and necessity. The 2007 American Board of Pediatrics' survey found that 27% of respondents planned a career in General Pediatrics with little or no inpatient care.10 Hospitalists of the near future will likely face a dichotomy of needs between primary care providers who trained before, and those who trained after, the existence of hospitalists. Hospitalists will need to understand and address the ongoing needs of both of these groups in order to adequately serve them and their patient‐bases.
Limitations of our study include our small sample size, with a response rate of 43% at best (individual question response rate varied). Though the group was nationally representative, it was skewed towards first year respondents, likely due to the time of year in which it was distributed. There is likely some bias due to the low response rate, in that those more interested in careers as hospitalists might be more likely to respond. This might potentially inflate the percentages of those who state they are interested in being a hospitalist. In addition, given that the last round of the survey went out at the very end of the academic year, graduating residents had a lower response rate.
We were unable to compare opinions across unexposed and exposed residents because only 6.5% reported knowing nothing about the field, and only 2 respondents had not had any exposure to pediatric hospitalists to date. Given that most residencies have PHM services,12 this distinction is unlikely to be significant. In looking at training desires, we did not compare them to residents considering entering other fields of medicine. It may be true that residents considering other fellowships do not desire to do 3 years of fellowship training. That being said, it in no way diminishes the implication that 3‐year fellowships for PHM may not be the right answer for future training.
Strengths of the study include that it is, to our knowledge, the first national study of a group of residents regarding exposure to, and career plans as related to, PH. In addition, the group is gender‐balanced, and represents residents from a range of training sites (urban, suburban, rural) and program sizes. This study offers important information that must be considered in the further development of the field of Pediatric Hospital Medicine.
CONCLUSION
This was the first national study of residents regarding Pediatric Hospital Medicine. Almost all residents are exposed to PH during their training, though a gap of no exposure still exists. More work needs to be done to improve the perception of PHM as a viable long‐term career. Nevertheless, PHM has become a career consideration for trainees. Nearly half agreed that some type of specialized training would be helpful. This information should impact on the development of PHM training programs.
Acknowledgements
Thanks to the American Academy of Pediatrics Section on Hospital Medicine for raffle funding, and Texas Children's Hospital and Dr Yong Han for use of SurveyMonkey and assistance with survey set‐up. Also thanks to Dr Vincent Chang for his guidance and review.
- ,,,;for the Research Advisory Committee of the American Board of Pediatrics.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- ,,.Establishing a pediatric hospitalist program at an academic medical center.Clin Pediatr (Phila).2000;39(4):221–227.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr (Phila).2001;40(12):653–660.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76(5):556.
- ,,,,,.Community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.Pediatrics.2005;115(1):34–38.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117(5):1736–1744.
- American Board of Pediatrics. 2006 General Pediatrics Career Survey. Available at: http://www.abp.org. Accessed on January 15, 2008.
- ,,,,;for the Research Advisory Committee of the American Board of Pediatrics.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(1 suppl):S26–S30.
- American Board of Pediatrics. 2007 General Pediatrics Career Survey. Available at: http://www.abp.org. Accessed July 10,2009.
- American Board of Pediatrics. 2009–2010 Workforce Data. Available at: http://www.abp.org. Accessed July 20,2010.
- ,,.Hospitalists' involvement in pediatrics training: perspectives from pediatric residency program and clerkship directors.Acad Med.2009;84(11):1617–1621.
- ,,.Assessing the value of pediatric hospitalist programs: the perspective of hospital leaders.Acad Pediatr.2009;9(3):192–196.
- ,,,.Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist.J Hosp Med.2011;6(in press).
- Accreditation Council for Graduate Medical Education. Available at: http://acgme‐2010standards.org/. Accessed December 15, 2010.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Hospitalist_Definition5:i–iv. doi://10.1002/jhm.776. Available at: http://www3.interscience.wiley.com. Accessed on May 11, 2011.
- ,,,;for the Research Advisory Committee of the American Board of Pediatrics.Characteristics of the pediatric hospitalist workforce: its roles and work environment.Pediatrics.2007;120(1):33–39.
- ,,,,,.Effect of a pediatric hospitalist system on housestaff education and experience.Arch Pediatr Adolesc Med.2002;156(9):877–883.
- ,,.Establishing a pediatric hospitalist program at an academic medical center.Clin Pediatr (Phila).2000;39(4):221–227.
- ,,,,,.Restructuring an academic pediatric inpatient service using concepts developed by hospitalists.Clin Pediatr (Phila).2001;40(12):653–660.
- .Employing hospitalists to improve residents' inpatient learning.Acad Med.2001;76(5):556.
- ,,,,,.Community and hospital‐based physicians' attitudes regarding pediatric hospitalist systems.Pediatrics.2005;115(1):34–38.
- ,,,.Pediatric hospitalists: a systematic review of the literature.Pediatrics.2006;117(5):1736–1744.
- American Board of Pediatrics. 2006 General Pediatrics Career Survey. Available at: http://www.abp.org. Accessed on January 15, 2008.
- ,,,,;for the Research Advisory Committee of the American Board of Pediatrics.General pediatrics resident perspectives on training decisions and career choice.Pediatrics.2009;123(1 suppl):S26–S30.
- American Board of Pediatrics. 2007 General Pediatrics Career Survey. Available at: http://www.abp.org. Accessed July 10,2009.
- American Board of Pediatrics. 2009–2010 Workforce Data. Available at: http://www.abp.org. Accessed July 20,2010.
- ,,.Hospitalists' involvement in pediatrics training: perspectives from pediatric residency program and clerkship directors.Acad Med.2009;84(11):1617–1621.
- ,,.Assessing the value of pediatric hospitalist programs: the perspective of hospital leaders.Acad Pediatr.2009;9(3):192–196.
- ,,,.Inpatient staffing within pediatric residency programs: work hour restrictions and the evolving role of the pediatric hospitalist.J Hosp Med.2011;6(in press).
- Accreditation Council for Graduate Medical Education. Available at: http://acgme‐2010standards.org/. Accessed December 15, 2010.
- Society of Hospital Medicine. Available at: http://www.hospitalmedicine.org/AM/Template.cfm?Section=Hospitalist_Definition5:i–iv. doi://10.1002/jhm.776. Available at: http://www3.interscience.wiley.com. Accessed on May 11, 2011.
Copyright © 2011 Society of Hospital Medicine