User login
Caregiver Perspectives on Communication During Hospitalization at an Academic Pediatric Institution: A Qualitative Study
Provision of high-quality, high-value medical care hinges upon effective communication. During a hospitalization, critical information is communicated between patients, caregivers, and providers multiple times each day. This can cause inconsistent and misinterpreted messages, leaving ample room for error.1 The Joint Commission notes that communication failures occurring between medical providers account for ~60% of all sentinel or serious adverse events that result in death or harm to a patient.2 Communication that occurs between patients and/or their caregivers and medical providers is also critically important. The content and consistency of this communication is highly valued by patients and providers and can affect patient outcomes during hospitalizations and during transitions to home.3,4 Still, the multifactorial, complex nature of communication in the pediatric inpatient setting is not well understood.5,6
During hospitalization, communication happens continuously during both daytime and nighttime hours. It also precedes the particularly fragile period of transition from hospital to home. Studies have shown that nighttime communication between caregivers and medical providers (ie, nurses and physicians), as well as caregivers’ perceptions of interactions that occur between nurses and physicians, may be closely linked to that caregiver’s satisfaction and perceived quality of care.6,7 Communication that occurs between inpatient and outpatient providers is also subject to barriers (eg, limited availability for direct communication)8-12; studies have shown that patient and/or caregiver satisfaction has also been tied to perceptions of this communication.13,14 Moreover, a caregiver’s ability to understand diagnoses and adhere to postdischarge care plans is intimately tied to communication during the hospitalization and at discharge. Although many improvement efforts have aimed to enhance communication during these vulnerable time periods,3,15,16 there remains much work to be done.1,10,12
The many facets and routes of communication, and the multiple stakeholders involved, make improvement efforts challenging. We believe that more effective communication strategies could result from a deeper understanding of how caregivers view communication successes and challenges during a hospitalization. We see this as key to developing meaningful interventions that are directed towards improving communication and, by extension, patient satisfaction and safety. Here, we sought to extend findings from a broader qualitative study17 by developing an in-depth understanding of communication issues experienced by families during their child’s hospitalization and during the transition to home.
METHODS
Setting
The analyses presented here emerged from the Hospital to Home Outcomes Study (H2O). The first objective of H2O was to explore the caregiver perspective on hospital-to-home transitions. Here, we present the results related to caregiver perspectives of communication, while broader results of our qualitative investigation have been published elsewhere.17 This objective informed the latter 2 aims of the H2O study, which were to modify an existing nurse-led transitional home visit (THV) program and to study the effectiveness of the modified THV on reutilization and patient-specific outcomes via a randomized control trial. The specifics of the H2O protocol and design have been presented elsewhere.18
H2O was approved by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center (CCHMC), a free-standing, academic children’s hospital with ~600 inpatient beds. This teaching hospital has >800 total medical students, residents, and fellows. Approximately 8000 children are hospitalized annually at CCHMC for general pediatric conditions, with ~85% of such admissions staffed by hospitalists from the Division of Hospital Medicine. The division is composed of >40 providers who devote the majority of their clinical time to the hospital medicine service; 15 additional providers work on the hospital medicine service but have primary clinical responsibilities in another division.
Family-centered rounds (FCR) are the standard of care at CCHMC, involving family members at the bedside to discuss patient care plans and diagnoses with the medical team.19 On a typical day, a team conducting FCR is composed of 1 attending, 1 fellow, 2 to 3 pediatric residents, 2 to 3 medical students, a charge nurse or bedside nurse, and a pharmacist. Other ancillary staff, such as social workers, care coordinators, nurse practitioners, or dieticians, may also participate on rounds, particularly for children with greater medical complexity.
Population
Caregivers of children discharged with acute medical conditions were eligible for recruitment if they were English-speaking (we did not have access to interpreter services during focus groups/interviews), had a child admitted to 1 of 3 services (hospital medicine, neurology, or neurosurgery), and could attend a focus group within 30 days of the child’s discharge. The majority of participants had a child admitted to hospital medicine; however, caregivers with a generally healthy child admitted to either neurology or neurosurgery were eligible to participate in the study.
Study Design
As presented elsewhere,17,20 we used focus groups and individual in-depth interviews to generate consensus themes about patient and caregiver experiences during the transition from hospital to home. Because there is evidence suggesting that focus group participants are more willing to talk openly when among others of similar backgrounds, we stratified the sample by the family’s estimated socioeconomic status.21,22 Socioeconomic status was estimated by identifying the poverty rate in the census tract in which each participant lived. Census tracts, relatively homogeneous areas of ~4000 individuals, have been previously shown to effectively detect socioeconomic gradients.23-26 Here, we separated participants into 2 socioeconomically distinct groupings (those in census tracts where <15% or ≥15% of the population lived below the federal poverty level).26 This cut point ensured an equivalent number of eligible participants within each stratum and diversity within our sample.
Data Collection
Caregivers were recruited on the inpatient unit during their child’s hospitalization. Participants then returned to CCHMC facilities for the focus group within 30 days of discharge. Though efforts were made to enhance participation by scheduling sessions at multiple sites and during various days and times of the week, 4 sessions yielded just 1 participant; thus, the format for those became an individual interview. Childcare was provided, and participants received a gift card for their participation.
An open-ended, semistructured question guide,17 developed de novo by the research team, directed the discussion for focus groups and interviews. As data collection progressed, the question guide was adapted to incorporate new issues raised by participants. Questions broadly focused on aspects of the inpatient experience, discharge processes, and healthcare system and family factors thought to be most relevant to patient- and family-centered outcomes. Communication-related questions addressed information shared with families from the medical team about discharge, diagnoses, instructions, and care plans. An experienced moderator and qualitative research methodologist (SNS) used probes to further elucidate responses and expand discussion by participants. Sessions were held in private conference rooms, lasted ~90 minutes, were audiotaped, and were transcribed verbatim. Identifiers were stripped and transcripts were reviewed for accuracy. After conducting 11 focus groups (generally composed of 5-10 participants) and 4 individual interviews, the research team determined that theoretical saturation27 was achieved, and recruitment was suspended.
Data Analysis
An inductive, thematic approach was used for analysis.27 Transcripts were independently reviewed by a multidisciplinary team of 4 researchers, including 2 pediatricians (LGS and AFB), a clinical research coordinator (SAS), and a qualitative research methodologist (SNS). The study team identified emerging concepts and themes related to the transition from hospital to home; themes related to communication during hospitalization are presented here.
During the first phase of analysis, investigators independently read transcripts and later convened to identify and define initial concepts and themes. A preliminary codebook was then designed. Investigators continued to review and code transcripts independently, meeting regularly to discuss coding decisions collaboratively, resolving differences through consensus.28 As patterns in the data became apparent, the codebook was modified iteratively, adding, subtracting, and refining codes as needed and grouping related codes. Results were reviewed with key stakeholders, including parents, inpatient and outpatient pediatricians, and home health nurses, throughout the analytic process.27,28 Coded data were maintained in an electronic database accessible only to study personnel.
RESULTS
Participants
Resulting Themes
Analyses revealed the following 3 major communication-related themes with associated subthemes: (1) experiences that affect caregiver perceptions of communication between the inpatient medical team and families, (2) communication challenges for caregivers related to a teaching hospital environment, and (3) caregiver perceptions of communication between medical providers. Each theme (and subtheme) is explored below with accompanying verbatim quotes in the narrative and the tables.
Major Theme 1: Experiences that Affect Caregiver Perceptions of Communication Between the Inpatient Medical Team and Families
In contrast, some of the negative experiences shared by participants related to feeling excluded from discussions about their child’s care. One participant said, “They tell you…as much as they want to tell you. They don’t fully inform you on things.” Additionally, concerns were voiced about insufficient time for face-to-face discussions with physicians: “I forget what I have to say and it’s something really, really important…But now, my doctor is going, you can’t get the doctor back.” Finally, participants discussed how the use of medical jargon often made it more difficult to understand things, especially for those not in the medical field.
Major Theme 2: Communication Challenges for Caregivers Related to a Teaching Hospital Environment
Major Theme 3: Caregiver Perceptions of Communication Between Medical Providers
Perceptions were not isolated to the inpatient setting. Based on their experiences, caregivers similarly described their sense of how inpatient and outpatient providers were communicating with each other. In some cases, it was clear that good communication, as perceived by the participant, had occurred in situations in which the primary care physician knew “everything” about the hospitalization when they saw the patient in follow-up. One participant described, “We didn’t even realize at the time, [the medical team] had actually called our doctor and filled them in on our situation, and we got [to the follow up visit]…He already knew the entire situation.” There were others, however, who shared their uncertainty about whether the information exchange about their child’s hospitalization had actually occurred. They, therefore, voiced apprehension around who to call for advice after discharge; would their outpatient provider have their child’s hospitalization history and be able to properly advise them?
DISCUSSION
Communication during a hospitalization and at transition from hospital to home happens in both formal and informal ways; it is a vital component of appropriate, effective patient care. When done poorly, it has the potential to negatively affect a patient’s safety, care, and key outcomes.2 During a hospitalization, the multifaceted nature of communication and multidisciplinary approach to care provision can create communication challenges and make fixing challenges difficult. In order to more comprehensively move toward mitigation, it is important to gather perspectives of key stakeholders, such as caregivers. Caregivers are an integral part of their child’s care during the hospitalization and particularly at home during their child’s recovery. They are also a valued member of the team, particularly in this era of family-centered care.19,29 The perspectives of the caregivers presented here identified both successes and challenges of their communication experiences with the medical team during their child’s hospitalization. These perspectives included experiences affecting perceptions of communication between the inpatient medical team and families; communication related to the teaching hospital environment, including confusing messages associated with large multidisciplinary teams, aspects of FCR, and confusion about medical team member roles; and caregivers’ perceptions of communication between providers in and out of the hospital, including types of communication caregivers observed or believed occurred between medical providers. We believe that these qualitative results are crucial to developing better, more targeted interventions to improve communication.
Maintaining a healthy and productive relationship with patients and their caregivers is critical to providing comprehensive and safe patient care. As supported in the literature, we found that when caregivers were included in conversations, they felt appreciated and valued; in addition, when answers were not directly shared by providers or there were lingering questions, nurses often served as “interpreters.”29,30 Indeed, nurses were seen as a critical touchpoint for many participants, individuals that could not only answer questions but also be a trusted source of information. Supporting such a relationship, and helping enhance the relationship between the family and other team members, may be particularly important considering the degree to which a hospitalization can stress a patient, caregiver, and family.31-34 Developing rapport with families and facilitating relationships with the inclusion of nursing during FCR can be particularly helpful. Though this can be challenging with the many competing priorities of medical providers and the fast-paced, acute nature of inpatient care, making an effort to include nursing staff on rounds can cut down on confusion and assist the family in understanding care plans. This, in turn, can minimize the stress associated with hospitalization and improve the patient and family experience.
While academic institutions’ resources and access to subspecialties are often thought to be advantageous, there are other challenges inherent to providing care in such complex environments. Some caregivers cited confusion related to large teams of providers with, to them, indistinguishable roles asking redundant questions. These experiences affected their perceptions of FCR, generally leading to a fixation on its overwhelming aspects. Certain caregivers highlighted that FCR caused them, and their child, to feel overwhelmed and more confused about the plan for the day. It is important to find ways to mitigate these feelings while simultaneously continuing to support the inclusion of caregivers during their child’s hospitalization and understanding of care plans. Some initiatives (in addition to including nursing on FCR as discussed above) focus on improving the ways in which providers communicate with families during rounds and throughout the day, seeking to decrease miscommunications and medical errors while also striving for better quality of care and patient/family satisfaction.35 Other initiatives seek to clarify identities and roles of the often large and confusing medical team. One such example of this is the development of a face sheet tool, which provides families with medical team members’ photos and role descriptions. Unaka et al.36 found that the use of the face sheet tool improved the ability of caregivers to correctly identify providers and their roles. Thinking beyond interventions at the bedside, it is also important to include caregivers on higher level committees within the institution, such as on family advisory boards and/or peer support groups, to inform systems-wide interventions that support the tenants of family-centered care.29 Efforts such as these are worth trialing in order to improve the patient and family experience and quality of communication.
Multiple studies have evaluated the challenges with ensuring consistent and useful handoffs across the inpatient-to-outpatient transition,8-10,12 but few have looked at it from the perspective of the caregiver.13 After leaving the hospital to care for their recovering child, caregivers often feel overwhelmed; they may want, or need, to rely on the support of others in the outpatient environment. This support can be enhanced when outpatient providers are intimately aware of what occurred during the hospitalization; trust erodes if this is not the case. Given the value caregivers place on this communication occurring and occurring well, interventions supporting this communication are critical. Furthermore, as providers, we should also inform families that communication with outpatient providers is happening. Examples of efforts that have worked to improve the quality and consistency of communication with outpatient providers include improving discharge summary documentation, ensuring timely faxing of documentation to outpatient providers, and reliably making phone calls to outpatient providers.37-39 These types of interventions seek to bridge the gap between inpatient and outpatient care and facilitate a smooth transfer of information in order to provide optimal quality of care and avoid undesired outcomes (eg, emergency department revisits, readmissions, medication errors, etc) and can be adopted by institutions to address the issue of communication between inpatient and outpatient providers.
We acknowledge limitations to our study. This was done at a single academic institution with only English-speaking participants. Thus, our results may not be reflective of caregivers of children cared for in different, more ethnically or linguistically diverse settings. The patient population at CCHMC, however, is diverse both demographically and clinically, which was reflected in the composition of our focus groups and interviews. Additionally, the inclusion of participants who received a nurse home visit after discharge may limit generalizability. However, only 4 participants had a nurse home visit; thus, the overwhelming majority of participants did not receive such an intervention. We also acknowledge that those willing to participate may have differed from nonparticipants, specifically sharing more positive experiences. We believe that our sampling strategy and use of an unbiased, nonhospital affiliated moderator minimized this possibility. Recall bias is possible, as participants were asked to reflect back on a discharge experience occurring in their past. We attempted to minimize this by holding sessions no more than 30 days from the day of discharge. Finally, we present data on caregivers’ perception of communication and not directly observed communication occurrences. Still, we expect that perception is powerful in and of itself, relevant to both outcomes and to interventions.
CONCLUSION
Communication during hospitalization influences how caregivers understand diagnoses and care plans. Communication perceived as effective fosters mutual understandings and positive relationships with the potential to result in better care and improved outcomes. Communication perceived as ineffective negatively affects experiences of patients and their caregivers and can adversely affect patient outcomes. Learning from caregivers’ experiences with communication during their child’s hospitalization can help identify modifiable factors and inform strategies to improve communication, support families through hospitalization, and facilitate a smooth reentry home.
ACKNOWLEDGMENTS
This manuscript is submitted on behalf of the H2O study group: Katherine A. Auger, MD, MSc, JoAnne Bachus, BSN, Monica L. Borell, BSN, Lenisa V. Chang, MA, PhD, Jennifer M. Gold, BSN, Judy A. Heilman, RN, Joseph A. Jabour, BS, Jane C. Khoury, PhD, Margo J. Moore, BSN, CCRP, Rita H. Pickler, PNP, PhD, Anita N. Shah, DO, Angela M. Statile, MD, MEd, Heidi J. Sucharew, PhD, Karen P. Sullivan, BSN, Heather L. Tubbs-Cooley, RN, PhD, Susan Wade-Murphy, MSN, and Christine M. White, MD, MAT.
Disclaimer
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors, or Methodology Committee.
Disclosure
This work was (partially) supported through a Patient-Centered Outcomes Research Institute (PCORI) Award (HIS-1306-0081). The authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest to disclose.
1. Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and Attending Physicians’ Handoffs: A Systematic Review of the Literature. Acad Med. 2009;84(12):1775-1787. PubMed
6. Comp D. Improving parent satisfaction by sharing the inpatient daily plan of care: an evidence review with implications for practice and research. Pediatr Nurs. 2011;37(5):237-242. PubMed
30. Latta LC, Dick R, Parry C, Tamura GS. Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292-297. PubMed
Provision of high-quality, high-value medical care hinges upon effective communication. During a hospitalization, critical information is communicated between patients, caregivers, and providers multiple times each day. This can cause inconsistent and misinterpreted messages, leaving ample room for error.1 The Joint Commission notes that communication failures occurring between medical providers account for ~60% of all sentinel or serious adverse events that result in death or harm to a patient.2 Communication that occurs between patients and/or their caregivers and medical providers is also critically important. The content and consistency of this communication is highly valued by patients and providers and can affect patient outcomes during hospitalizations and during transitions to home.3,4 Still, the multifactorial, complex nature of communication in the pediatric inpatient setting is not well understood.5,6
During hospitalization, communication happens continuously during both daytime and nighttime hours. It also precedes the particularly fragile period of transition from hospital to home. Studies have shown that nighttime communication between caregivers and medical providers (ie, nurses and physicians), as well as caregivers’ perceptions of interactions that occur between nurses and physicians, may be closely linked to that caregiver’s satisfaction and perceived quality of care.6,7 Communication that occurs between inpatient and outpatient providers is also subject to barriers (eg, limited availability for direct communication)8-12; studies have shown that patient and/or caregiver satisfaction has also been tied to perceptions of this communication.13,14 Moreover, a caregiver’s ability to understand diagnoses and adhere to postdischarge care plans is intimately tied to communication during the hospitalization and at discharge. Although many improvement efforts have aimed to enhance communication during these vulnerable time periods,3,15,16 there remains much work to be done.1,10,12
The many facets and routes of communication, and the multiple stakeholders involved, make improvement efforts challenging. We believe that more effective communication strategies could result from a deeper understanding of how caregivers view communication successes and challenges during a hospitalization. We see this as key to developing meaningful interventions that are directed towards improving communication and, by extension, patient satisfaction and safety. Here, we sought to extend findings from a broader qualitative study17 by developing an in-depth understanding of communication issues experienced by families during their child’s hospitalization and during the transition to home.
METHODS
Setting
The analyses presented here emerged from the Hospital to Home Outcomes Study (H2O). The first objective of H2O was to explore the caregiver perspective on hospital-to-home transitions. Here, we present the results related to caregiver perspectives of communication, while broader results of our qualitative investigation have been published elsewhere.17 This objective informed the latter 2 aims of the H2O study, which were to modify an existing nurse-led transitional home visit (THV) program and to study the effectiveness of the modified THV on reutilization and patient-specific outcomes via a randomized control trial. The specifics of the H2O protocol and design have been presented elsewhere.18
H2O was approved by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center (CCHMC), a free-standing, academic children’s hospital with ~600 inpatient beds. This teaching hospital has >800 total medical students, residents, and fellows. Approximately 8000 children are hospitalized annually at CCHMC for general pediatric conditions, with ~85% of such admissions staffed by hospitalists from the Division of Hospital Medicine. The division is composed of >40 providers who devote the majority of their clinical time to the hospital medicine service; 15 additional providers work on the hospital medicine service but have primary clinical responsibilities in another division.
Family-centered rounds (FCR) are the standard of care at CCHMC, involving family members at the bedside to discuss patient care plans and diagnoses with the medical team.19 On a typical day, a team conducting FCR is composed of 1 attending, 1 fellow, 2 to 3 pediatric residents, 2 to 3 medical students, a charge nurse or bedside nurse, and a pharmacist. Other ancillary staff, such as social workers, care coordinators, nurse practitioners, or dieticians, may also participate on rounds, particularly for children with greater medical complexity.
Population
Caregivers of children discharged with acute medical conditions were eligible for recruitment if they were English-speaking (we did not have access to interpreter services during focus groups/interviews), had a child admitted to 1 of 3 services (hospital medicine, neurology, or neurosurgery), and could attend a focus group within 30 days of the child’s discharge. The majority of participants had a child admitted to hospital medicine; however, caregivers with a generally healthy child admitted to either neurology or neurosurgery were eligible to participate in the study.
Study Design
As presented elsewhere,17,20 we used focus groups and individual in-depth interviews to generate consensus themes about patient and caregiver experiences during the transition from hospital to home. Because there is evidence suggesting that focus group participants are more willing to talk openly when among others of similar backgrounds, we stratified the sample by the family’s estimated socioeconomic status.21,22 Socioeconomic status was estimated by identifying the poverty rate in the census tract in which each participant lived. Census tracts, relatively homogeneous areas of ~4000 individuals, have been previously shown to effectively detect socioeconomic gradients.23-26 Here, we separated participants into 2 socioeconomically distinct groupings (those in census tracts where <15% or ≥15% of the population lived below the federal poverty level).26 This cut point ensured an equivalent number of eligible participants within each stratum and diversity within our sample.
Data Collection
Caregivers were recruited on the inpatient unit during their child’s hospitalization. Participants then returned to CCHMC facilities for the focus group within 30 days of discharge. Though efforts were made to enhance participation by scheduling sessions at multiple sites and during various days and times of the week, 4 sessions yielded just 1 participant; thus, the format for those became an individual interview. Childcare was provided, and participants received a gift card for their participation.
An open-ended, semistructured question guide,17 developed de novo by the research team, directed the discussion for focus groups and interviews. As data collection progressed, the question guide was adapted to incorporate new issues raised by participants. Questions broadly focused on aspects of the inpatient experience, discharge processes, and healthcare system and family factors thought to be most relevant to patient- and family-centered outcomes. Communication-related questions addressed information shared with families from the medical team about discharge, diagnoses, instructions, and care plans. An experienced moderator and qualitative research methodologist (SNS) used probes to further elucidate responses and expand discussion by participants. Sessions were held in private conference rooms, lasted ~90 minutes, were audiotaped, and were transcribed verbatim. Identifiers were stripped and transcripts were reviewed for accuracy. After conducting 11 focus groups (generally composed of 5-10 participants) and 4 individual interviews, the research team determined that theoretical saturation27 was achieved, and recruitment was suspended.
Data Analysis
An inductive, thematic approach was used for analysis.27 Transcripts were independently reviewed by a multidisciplinary team of 4 researchers, including 2 pediatricians (LGS and AFB), a clinical research coordinator (SAS), and a qualitative research methodologist (SNS). The study team identified emerging concepts and themes related to the transition from hospital to home; themes related to communication during hospitalization are presented here.
During the first phase of analysis, investigators independently read transcripts and later convened to identify and define initial concepts and themes. A preliminary codebook was then designed. Investigators continued to review and code transcripts independently, meeting regularly to discuss coding decisions collaboratively, resolving differences through consensus.28 As patterns in the data became apparent, the codebook was modified iteratively, adding, subtracting, and refining codes as needed and grouping related codes. Results were reviewed with key stakeholders, including parents, inpatient and outpatient pediatricians, and home health nurses, throughout the analytic process.27,28 Coded data were maintained in an electronic database accessible only to study personnel.
RESULTS
Participants
Resulting Themes
Analyses revealed the following 3 major communication-related themes with associated subthemes: (1) experiences that affect caregiver perceptions of communication between the inpatient medical team and families, (2) communication challenges for caregivers related to a teaching hospital environment, and (3) caregiver perceptions of communication between medical providers. Each theme (and subtheme) is explored below with accompanying verbatim quotes in the narrative and the tables.
Major Theme 1: Experiences that Affect Caregiver Perceptions of Communication Between the Inpatient Medical Team and Families
In contrast, some of the negative experiences shared by participants related to feeling excluded from discussions about their child’s care. One participant said, “They tell you…as much as they want to tell you. They don’t fully inform you on things.” Additionally, concerns were voiced about insufficient time for face-to-face discussions with physicians: “I forget what I have to say and it’s something really, really important…But now, my doctor is going, you can’t get the doctor back.” Finally, participants discussed how the use of medical jargon often made it more difficult to understand things, especially for those not in the medical field.
Major Theme 2: Communication Challenges for Caregivers Related to a Teaching Hospital Environment
Major Theme 3: Caregiver Perceptions of Communication Between Medical Providers
Perceptions were not isolated to the inpatient setting. Based on their experiences, caregivers similarly described their sense of how inpatient and outpatient providers were communicating with each other. In some cases, it was clear that good communication, as perceived by the participant, had occurred in situations in which the primary care physician knew “everything” about the hospitalization when they saw the patient in follow-up. One participant described, “We didn’t even realize at the time, [the medical team] had actually called our doctor and filled them in on our situation, and we got [to the follow up visit]…He already knew the entire situation.” There were others, however, who shared their uncertainty about whether the information exchange about their child’s hospitalization had actually occurred. They, therefore, voiced apprehension around who to call for advice after discharge; would their outpatient provider have their child’s hospitalization history and be able to properly advise them?
DISCUSSION
Communication during a hospitalization and at transition from hospital to home happens in both formal and informal ways; it is a vital component of appropriate, effective patient care. When done poorly, it has the potential to negatively affect a patient’s safety, care, and key outcomes.2 During a hospitalization, the multifaceted nature of communication and multidisciplinary approach to care provision can create communication challenges and make fixing challenges difficult. In order to more comprehensively move toward mitigation, it is important to gather perspectives of key stakeholders, such as caregivers. Caregivers are an integral part of their child’s care during the hospitalization and particularly at home during their child’s recovery. They are also a valued member of the team, particularly in this era of family-centered care.19,29 The perspectives of the caregivers presented here identified both successes and challenges of their communication experiences with the medical team during their child’s hospitalization. These perspectives included experiences affecting perceptions of communication between the inpatient medical team and families; communication related to the teaching hospital environment, including confusing messages associated with large multidisciplinary teams, aspects of FCR, and confusion about medical team member roles; and caregivers’ perceptions of communication between providers in and out of the hospital, including types of communication caregivers observed or believed occurred between medical providers. We believe that these qualitative results are crucial to developing better, more targeted interventions to improve communication.
Maintaining a healthy and productive relationship with patients and their caregivers is critical to providing comprehensive and safe patient care. As supported in the literature, we found that when caregivers were included in conversations, they felt appreciated and valued; in addition, when answers were not directly shared by providers or there were lingering questions, nurses often served as “interpreters.”29,30 Indeed, nurses were seen as a critical touchpoint for many participants, individuals that could not only answer questions but also be a trusted source of information. Supporting such a relationship, and helping enhance the relationship between the family and other team members, may be particularly important considering the degree to which a hospitalization can stress a patient, caregiver, and family.31-34 Developing rapport with families and facilitating relationships with the inclusion of nursing during FCR can be particularly helpful. Though this can be challenging with the many competing priorities of medical providers and the fast-paced, acute nature of inpatient care, making an effort to include nursing staff on rounds can cut down on confusion and assist the family in understanding care plans. This, in turn, can minimize the stress associated with hospitalization and improve the patient and family experience.
While academic institutions’ resources and access to subspecialties are often thought to be advantageous, there are other challenges inherent to providing care in such complex environments. Some caregivers cited confusion related to large teams of providers with, to them, indistinguishable roles asking redundant questions. These experiences affected their perceptions of FCR, generally leading to a fixation on its overwhelming aspects. Certain caregivers highlighted that FCR caused them, and their child, to feel overwhelmed and more confused about the plan for the day. It is important to find ways to mitigate these feelings while simultaneously continuing to support the inclusion of caregivers during their child’s hospitalization and understanding of care plans. Some initiatives (in addition to including nursing on FCR as discussed above) focus on improving the ways in which providers communicate with families during rounds and throughout the day, seeking to decrease miscommunications and medical errors while also striving for better quality of care and patient/family satisfaction.35 Other initiatives seek to clarify identities and roles of the often large and confusing medical team. One such example of this is the development of a face sheet tool, which provides families with medical team members’ photos and role descriptions. Unaka et al.36 found that the use of the face sheet tool improved the ability of caregivers to correctly identify providers and their roles. Thinking beyond interventions at the bedside, it is also important to include caregivers on higher level committees within the institution, such as on family advisory boards and/or peer support groups, to inform systems-wide interventions that support the tenants of family-centered care.29 Efforts such as these are worth trialing in order to improve the patient and family experience and quality of communication.
Multiple studies have evaluated the challenges with ensuring consistent and useful handoffs across the inpatient-to-outpatient transition,8-10,12 but few have looked at it from the perspective of the caregiver.13 After leaving the hospital to care for their recovering child, caregivers often feel overwhelmed; they may want, or need, to rely on the support of others in the outpatient environment. This support can be enhanced when outpatient providers are intimately aware of what occurred during the hospitalization; trust erodes if this is not the case. Given the value caregivers place on this communication occurring and occurring well, interventions supporting this communication are critical. Furthermore, as providers, we should also inform families that communication with outpatient providers is happening. Examples of efforts that have worked to improve the quality and consistency of communication with outpatient providers include improving discharge summary documentation, ensuring timely faxing of documentation to outpatient providers, and reliably making phone calls to outpatient providers.37-39 These types of interventions seek to bridge the gap between inpatient and outpatient care and facilitate a smooth transfer of information in order to provide optimal quality of care and avoid undesired outcomes (eg, emergency department revisits, readmissions, medication errors, etc) and can be adopted by institutions to address the issue of communication between inpatient and outpatient providers.
We acknowledge limitations to our study. This was done at a single academic institution with only English-speaking participants. Thus, our results may not be reflective of caregivers of children cared for in different, more ethnically or linguistically diverse settings. The patient population at CCHMC, however, is diverse both demographically and clinically, which was reflected in the composition of our focus groups and interviews. Additionally, the inclusion of participants who received a nurse home visit after discharge may limit generalizability. However, only 4 participants had a nurse home visit; thus, the overwhelming majority of participants did not receive such an intervention. We also acknowledge that those willing to participate may have differed from nonparticipants, specifically sharing more positive experiences. We believe that our sampling strategy and use of an unbiased, nonhospital affiliated moderator minimized this possibility. Recall bias is possible, as participants were asked to reflect back on a discharge experience occurring in their past. We attempted to minimize this by holding sessions no more than 30 days from the day of discharge. Finally, we present data on caregivers’ perception of communication and not directly observed communication occurrences. Still, we expect that perception is powerful in and of itself, relevant to both outcomes and to interventions.
CONCLUSION
Communication during hospitalization influences how caregivers understand diagnoses and care plans. Communication perceived as effective fosters mutual understandings and positive relationships with the potential to result in better care and improved outcomes. Communication perceived as ineffective negatively affects experiences of patients and their caregivers and can adversely affect patient outcomes. Learning from caregivers’ experiences with communication during their child’s hospitalization can help identify modifiable factors and inform strategies to improve communication, support families through hospitalization, and facilitate a smooth reentry home.
ACKNOWLEDGMENTS
This manuscript is submitted on behalf of the H2O study group: Katherine A. Auger, MD, MSc, JoAnne Bachus, BSN, Monica L. Borell, BSN, Lenisa V. Chang, MA, PhD, Jennifer M. Gold, BSN, Judy A. Heilman, RN, Joseph A. Jabour, BS, Jane C. Khoury, PhD, Margo J. Moore, BSN, CCRP, Rita H. Pickler, PNP, PhD, Anita N. Shah, DO, Angela M. Statile, MD, MEd, Heidi J. Sucharew, PhD, Karen P. Sullivan, BSN, Heather L. Tubbs-Cooley, RN, PhD, Susan Wade-Murphy, MSN, and Christine M. White, MD, MAT.
Disclaimer
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors, or Methodology Committee.
Disclosure
This work was (partially) supported through a Patient-Centered Outcomes Research Institute (PCORI) Award (HIS-1306-0081). The authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest to disclose.
Provision of high-quality, high-value medical care hinges upon effective communication. During a hospitalization, critical information is communicated between patients, caregivers, and providers multiple times each day. This can cause inconsistent and misinterpreted messages, leaving ample room for error.1 The Joint Commission notes that communication failures occurring between medical providers account for ~60% of all sentinel or serious adverse events that result in death or harm to a patient.2 Communication that occurs between patients and/or their caregivers and medical providers is also critically important. The content and consistency of this communication is highly valued by patients and providers and can affect patient outcomes during hospitalizations and during transitions to home.3,4 Still, the multifactorial, complex nature of communication in the pediatric inpatient setting is not well understood.5,6
During hospitalization, communication happens continuously during both daytime and nighttime hours. It also precedes the particularly fragile period of transition from hospital to home. Studies have shown that nighttime communication between caregivers and medical providers (ie, nurses and physicians), as well as caregivers’ perceptions of interactions that occur between nurses and physicians, may be closely linked to that caregiver’s satisfaction and perceived quality of care.6,7 Communication that occurs between inpatient and outpatient providers is also subject to barriers (eg, limited availability for direct communication)8-12; studies have shown that patient and/or caregiver satisfaction has also been tied to perceptions of this communication.13,14 Moreover, a caregiver’s ability to understand diagnoses and adhere to postdischarge care plans is intimately tied to communication during the hospitalization and at discharge. Although many improvement efforts have aimed to enhance communication during these vulnerable time periods,3,15,16 there remains much work to be done.1,10,12
The many facets and routes of communication, and the multiple stakeholders involved, make improvement efforts challenging. We believe that more effective communication strategies could result from a deeper understanding of how caregivers view communication successes and challenges during a hospitalization. We see this as key to developing meaningful interventions that are directed towards improving communication and, by extension, patient satisfaction and safety. Here, we sought to extend findings from a broader qualitative study17 by developing an in-depth understanding of communication issues experienced by families during their child’s hospitalization and during the transition to home.
METHODS
Setting
The analyses presented here emerged from the Hospital to Home Outcomes Study (H2O). The first objective of H2O was to explore the caregiver perspective on hospital-to-home transitions. Here, we present the results related to caregiver perspectives of communication, while broader results of our qualitative investigation have been published elsewhere.17 This objective informed the latter 2 aims of the H2O study, which were to modify an existing nurse-led transitional home visit (THV) program and to study the effectiveness of the modified THV on reutilization and patient-specific outcomes via a randomized control trial. The specifics of the H2O protocol and design have been presented elsewhere.18
H2O was approved by the Institutional Review Board at Cincinnati Children’s Hospital Medical Center (CCHMC), a free-standing, academic children’s hospital with ~600 inpatient beds. This teaching hospital has >800 total medical students, residents, and fellows. Approximately 8000 children are hospitalized annually at CCHMC for general pediatric conditions, with ~85% of such admissions staffed by hospitalists from the Division of Hospital Medicine. The division is composed of >40 providers who devote the majority of their clinical time to the hospital medicine service; 15 additional providers work on the hospital medicine service but have primary clinical responsibilities in another division.
Family-centered rounds (FCR) are the standard of care at CCHMC, involving family members at the bedside to discuss patient care plans and diagnoses with the medical team.19 On a typical day, a team conducting FCR is composed of 1 attending, 1 fellow, 2 to 3 pediatric residents, 2 to 3 medical students, a charge nurse or bedside nurse, and a pharmacist. Other ancillary staff, such as social workers, care coordinators, nurse practitioners, or dieticians, may also participate on rounds, particularly for children with greater medical complexity.
Population
Caregivers of children discharged with acute medical conditions were eligible for recruitment if they were English-speaking (we did not have access to interpreter services during focus groups/interviews), had a child admitted to 1 of 3 services (hospital medicine, neurology, or neurosurgery), and could attend a focus group within 30 days of the child’s discharge. The majority of participants had a child admitted to hospital medicine; however, caregivers with a generally healthy child admitted to either neurology or neurosurgery were eligible to participate in the study.
Study Design
As presented elsewhere,17,20 we used focus groups and individual in-depth interviews to generate consensus themes about patient and caregiver experiences during the transition from hospital to home. Because there is evidence suggesting that focus group participants are more willing to talk openly when among others of similar backgrounds, we stratified the sample by the family’s estimated socioeconomic status.21,22 Socioeconomic status was estimated by identifying the poverty rate in the census tract in which each participant lived. Census tracts, relatively homogeneous areas of ~4000 individuals, have been previously shown to effectively detect socioeconomic gradients.23-26 Here, we separated participants into 2 socioeconomically distinct groupings (those in census tracts where <15% or ≥15% of the population lived below the federal poverty level).26 This cut point ensured an equivalent number of eligible participants within each stratum and diversity within our sample.
Data Collection
Caregivers were recruited on the inpatient unit during their child’s hospitalization. Participants then returned to CCHMC facilities for the focus group within 30 days of discharge. Though efforts were made to enhance participation by scheduling sessions at multiple sites and during various days and times of the week, 4 sessions yielded just 1 participant; thus, the format for those became an individual interview. Childcare was provided, and participants received a gift card for their participation.
An open-ended, semistructured question guide,17 developed de novo by the research team, directed the discussion for focus groups and interviews. As data collection progressed, the question guide was adapted to incorporate new issues raised by participants. Questions broadly focused on aspects of the inpatient experience, discharge processes, and healthcare system and family factors thought to be most relevant to patient- and family-centered outcomes. Communication-related questions addressed information shared with families from the medical team about discharge, diagnoses, instructions, and care plans. An experienced moderator and qualitative research methodologist (SNS) used probes to further elucidate responses and expand discussion by participants. Sessions were held in private conference rooms, lasted ~90 minutes, were audiotaped, and were transcribed verbatim. Identifiers were stripped and transcripts were reviewed for accuracy. After conducting 11 focus groups (generally composed of 5-10 participants) and 4 individual interviews, the research team determined that theoretical saturation27 was achieved, and recruitment was suspended.
Data Analysis
An inductive, thematic approach was used for analysis.27 Transcripts were independently reviewed by a multidisciplinary team of 4 researchers, including 2 pediatricians (LGS and AFB), a clinical research coordinator (SAS), and a qualitative research methodologist (SNS). The study team identified emerging concepts and themes related to the transition from hospital to home; themes related to communication during hospitalization are presented here.
During the first phase of analysis, investigators independently read transcripts and later convened to identify and define initial concepts and themes. A preliminary codebook was then designed. Investigators continued to review and code transcripts independently, meeting regularly to discuss coding decisions collaboratively, resolving differences through consensus.28 As patterns in the data became apparent, the codebook was modified iteratively, adding, subtracting, and refining codes as needed and grouping related codes. Results were reviewed with key stakeholders, including parents, inpatient and outpatient pediatricians, and home health nurses, throughout the analytic process.27,28 Coded data were maintained in an electronic database accessible only to study personnel.
RESULTS
Participants
Resulting Themes
Analyses revealed the following 3 major communication-related themes with associated subthemes: (1) experiences that affect caregiver perceptions of communication between the inpatient medical team and families, (2) communication challenges for caregivers related to a teaching hospital environment, and (3) caregiver perceptions of communication between medical providers. Each theme (and subtheme) is explored below with accompanying verbatim quotes in the narrative and the tables.
Major Theme 1: Experiences that Affect Caregiver Perceptions of Communication Between the Inpatient Medical Team and Families
In contrast, some of the negative experiences shared by participants related to feeling excluded from discussions about their child’s care. One participant said, “They tell you…as much as they want to tell you. They don’t fully inform you on things.” Additionally, concerns were voiced about insufficient time for face-to-face discussions with physicians: “I forget what I have to say and it’s something really, really important…But now, my doctor is going, you can’t get the doctor back.” Finally, participants discussed how the use of medical jargon often made it more difficult to understand things, especially for those not in the medical field.
Major Theme 2: Communication Challenges for Caregivers Related to a Teaching Hospital Environment
Major Theme 3: Caregiver Perceptions of Communication Between Medical Providers
Perceptions were not isolated to the inpatient setting. Based on their experiences, caregivers similarly described their sense of how inpatient and outpatient providers were communicating with each other. In some cases, it was clear that good communication, as perceived by the participant, had occurred in situations in which the primary care physician knew “everything” about the hospitalization when they saw the patient in follow-up. One participant described, “We didn’t even realize at the time, [the medical team] had actually called our doctor and filled them in on our situation, and we got [to the follow up visit]…He already knew the entire situation.” There were others, however, who shared their uncertainty about whether the information exchange about their child’s hospitalization had actually occurred. They, therefore, voiced apprehension around who to call for advice after discharge; would their outpatient provider have their child’s hospitalization history and be able to properly advise them?
DISCUSSION
Communication during a hospitalization and at transition from hospital to home happens in both formal and informal ways; it is a vital component of appropriate, effective patient care. When done poorly, it has the potential to negatively affect a patient’s safety, care, and key outcomes.2 During a hospitalization, the multifaceted nature of communication and multidisciplinary approach to care provision can create communication challenges and make fixing challenges difficult. In order to more comprehensively move toward mitigation, it is important to gather perspectives of key stakeholders, such as caregivers. Caregivers are an integral part of their child’s care during the hospitalization and particularly at home during their child’s recovery. They are also a valued member of the team, particularly in this era of family-centered care.19,29 The perspectives of the caregivers presented here identified both successes and challenges of their communication experiences with the medical team during their child’s hospitalization. These perspectives included experiences affecting perceptions of communication between the inpatient medical team and families; communication related to the teaching hospital environment, including confusing messages associated with large multidisciplinary teams, aspects of FCR, and confusion about medical team member roles; and caregivers’ perceptions of communication between providers in and out of the hospital, including types of communication caregivers observed or believed occurred between medical providers. We believe that these qualitative results are crucial to developing better, more targeted interventions to improve communication.
Maintaining a healthy and productive relationship with patients and their caregivers is critical to providing comprehensive and safe patient care. As supported in the literature, we found that when caregivers were included in conversations, they felt appreciated and valued; in addition, when answers were not directly shared by providers or there were lingering questions, nurses often served as “interpreters.”29,30 Indeed, nurses were seen as a critical touchpoint for many participants, individuals that could not only answer questions but also be a trusted source of information. Supporting such a relationship, and helping enhance the relationship between the family and other team members, may be particularly important considering the degree to which a hospitalization can stress a patient, caregiver, and family.31-34 Developing rapport with families and facilitating relationships with the inclusion of nursing during FCR can be particularly helpful. Though this can be challenging with the many competing priorities of medical providers and the fast-paced, acute nature of inpatient care, making an effort to include nursing staff on rounds can cut down on confusion and assist the family in understanding care plans. This, in turn, can minimize the stress associated with hospitalization and improve the patient and family experience.
While academic institutions’ resources and access to subspecialties are often thought to be advantageous, there are other challenges inherent to providing care in such complex environments. Some caregivers cited confusion related to large teams of providers with, to them, indistinguishable roles asking redundant questions. These experiences affected their perceptions of FCR, generally leading to a fixation on its overwhelming aspects. Certain caregivers highlighted that FCR caused them, and their child, to feel overwhelmed and more confused about the plan for the day. It is important to find ways to mitigate these feelings while simultaneously continuing to support the inclusion of caregivers during their child’s hospitalization and understanding of care plans. Some initiatives (in addition to including nursing on FCR as discussed above) focus on improving the ways in which providers communicate with families during rounds and throughout the day, seeking to decrease miscommunications and medical errors while also striving for better quality of care and patient/family satisfaction.35 Other initiatives seek to clarify identities and roles of the often large and confusing medical team. One such example of this is the development of a face sheet tool, which provides families with medical team members’ photos and role descriptions. Unaka et al.36 found that the use of the face sheet tool improved the ability of caregivers to correctly identify providers and their roles. Thinking beyond interventions at the bedside, it is also important to include caregivers on higher level committees within the institution, such as on family advisory boards and/or peer support groups, to inform systems-wide interventions that support the tenants of family-centered care.29 Efforts such as these are worth trialing in order to improve the patient and family experience and quality of communication.
Multiple studies have evaluated the challenges with ensuring consistent and useful handoffs across the inpatient-to-outpatient transition,8-10,12 but few have looked at it from the perspective of the caregiver.13 After leaving the hospital to care for their recovering child, caregivers often feel overwhelmed; they may want, or need, to rely on the support of others in the outpatient environment. This support can be enhanced when outpatient providers are intimately aware of what occurred during the hospitalization; trust erodes if this is not the case. Given the value caregivers place on this communication occurring and occurring well, interventions supporting this communication are critical. Furthermore, as providers, we should also inform families that communication with outpatient providers is happening. Examples of efforts that have worked to improve the quality and consistency of communication with outpatient providers include improving discharge summary documentation, ensuring timely faxing of documentation to outpatient providers, and reliably making phone calls to outpatient providers.37-39 These types of interventions seek to bridge the gap between inpatient and outpatient care and facilitate a smooth transfer of information in order to provide optimal quality of care and avoid undesired outcomes (eg, emergency department revisits, readmissions, medication errors, etc) and can be adopted by institutions to address the issue of communication between inpatient and outpatient providers.
We acknowledge limitations to our study. This was done at a single academic institution with only English-speaking participants. Thus, our results may not be reflective of caregivers of children cared for in different, more ethnically or linguistically diverse settings. The patient population at CCHMC, however, is diverse both demographically and clinically, which was reflected in the composition of our focus groups and interviews. Additionally, the inclusion of participants who received a nurse home visit after discharge may limit generalizability. However, only 4 participants had a nurse home visit; thus, the overwhelming majority of participants did not receive such an intervention. We also acknowledge that those willing to participate may have differed from nonparticipants, specifically sharing more positive experiences. We believe that our sampling strategy and use of an unbiased, nonhospital affiliated moderator minimized this possibility. Recall bias is possible, as participants were asked to reflect back on a discharge experience occurring in their past. We attempted to minimize this by holding sessions no more than 30 days from the day of discharge. Finally, we present data on caregivers’ perception of communication and not directly observed communication occurrences. Still, we expect that perception is powerful in and of itself, relevant to both outcomes and to interventions.
CONCLUSION
Communication during hospitalization influences how caregivers understand diagnoses and care plans. Communication perceived as effective fosters mutual understandings and positive relationships with the potential to result in better care and improved outcomes. Communication perceived as ineffective negatively affects experiences of patients and their caregivers and can adversely affect patient outcomes. Learning from caregivers’ experiences with communication during their child’s hospitalization can help identify modifiable factors and inform strategies to improve communication, support families through hospitalization, and facilitate a smooth reentry home.
ACKNOWLEDGMENTS
This manuscript is submitted on behalf of the H2O study group: Katherine A. Auger, MD, MSc, JoAnne Bachus, BSN, Monica L. Borell, BSN, Lenisa V. Chang, MA, PhD, Jennifer M. Gold, BSN, Judy A. Heilman, RN, Joseph A. Jabour, BS, Jane C. Khoury, PhD, Margo J. Moore, BSN, CCRP, Rita H. Pickler, PNP, PhD, Anita N. Shah, DO, Angela M. Statile, MD, MEd, Heidi J. Sucharew, PhD, Karen P. Sullivan, BSN, Heather L. Tubbs-Cooley, RN, PhD, Susan Wade-Murphy, MSN, and Christine M. White, MD, MAT.
Disclaimer
All statements in this report, including its findings and conclusions, are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors, or Methodology Committee.
Disclosure
This work was (partially) supported through a Patient-Centered Outcomes Research Institute (PCORI) Award (HIS-1306-0081). The authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest to disclose.
1. Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and Attending Physicians’ Handoffs: A Systematic Review of the Literature. Acad Med. 2009;84(12):1775-1787. PubMed
6. Comp D. Improving parent satisfaction by sharing the inpatient daily plan of care: an evidence review with implications for practice and research. Pediatr Nurs. 2011;37(5):237-242. PubMed
30. Latta LC, Dick R, Parry C, Tamura GS. Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292-297. PubMed
1. Riesenberg LA, Leitzsch J, Massucci JL, et al. Residents’ and Attending Physicians’ Handoffs: A Systematic Review of the Literature. Acad Med. 2009;84(12):1775-1787. PubMed
6. Comp D. Improving parent satisfaction by sharing the inpatient daily plan of care: an evidence review with implications for practice and research. Pediatr Nurs. 2011;37(5):237-242. PubMed
30. Latta LC, Dick R, Parry C, Tamura GS. Parental responses to involvement in rounds on a pediatric inpatient unit at a teaching hospital: a qualitative study. Acad Med. 2008;83(3):292-297. PubMed
© 2018 Society of Hospital Medicine
Assessment of readability, understandability, and completeness of pediatric hospital medicine discharge instructions
The average American adult reads at an 8th-grade level.1 Limited general literacy can affect health literacy, which is defined as the “degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”2,3 Adults with limited health literacy are at risk for poorer outcomes, including overuse of the emergency department and lower adherence to preventive care recommendations.4
Children transitioning from hospital to home depend on their adult caregivers (and their caregivers’ health literacy) to carry out discharge instructions. During the immediate postdischarge period, complex care needs can involve new or changed medications, follow-up instructions, home care instructions, and suggestions regarding when and why to seek additional care.
The discharge education provided to patients in the hospital is often subpar because of lack of standardization and divided responsibility among providers.5 Communication of vital information to patients with low health literacy has been noted to be particularly poor,6 as many patient education materials are written at 10th-, 11th-, and 12th-grade reading levels.4 Evidence supports providing materials written at 6th-grade level or lower to increase comprehension.7 Several studies have evaluated the quality and readability of discharge instructions for hospitalized adults,8,9 and one study found a link between poorly written instructions for adult patients and readmission risk.10 Less is known about readability in pediatrics, in which education may be more important for families of children most commonly hospitalized for acute illness.
We conducted a study to describe readability levels, understandability scores, and completeness of written instructions given to families at hospital discharge.
METHODS
Study Design and Setting
In this study, we performed a cross-sectional review of discharge instructions within electronic health records at Cincinnati Children’s Hospital Medical Center (CCHMC). The study was reviewed and approved by CCHMC’s Institutional Review Board. Charts were randomly selected from all hospital medicine service discharges during two 3-month periods of high patient volume: January-March 2014 and January-March 2015.
CCHMC is a large urban academic referral center that is the sole provider of general, subspecialty, and critical pediatric inpatient care for a large geographical area. CCHMC, which has 600 beds, provides cares for many children who live in impoverished settings. Its hospital medicine service consists of 4 teams that care for approximately 7000 children hospitalized with general pediatric illnesses each year. Each team consists of 5 or 6 pediatric residents supervised by a hospital medicine attending.
Providers, most commonly pediatric interns, generate discharge instructions in electronic health records. In this nonautomated process, they use free-text or nonstandardized templates to create content. At discharge, instructions are printed as part of the postvisit summary, which includes updates on medications and scheduled follow-up appointments. Bedside nurses verbally review the instructions with families and provide printed copies for home use.
Data Collection and Analysis
A random sequence generator was used to select charts for review. Instructions written in a language other than English were excluded. Written discharge instructions and clinical information, including age, sex, primary diagnosis, insurance type, number of discharge medications, number of scheduled appointments at discharge, and hospital length of stay, were abstracted from electronic health records and anonymized before analysis. The primary outcomes assessed were discharge instruction readability, understandability, and completeness. Readability was calculated with Fry Readability Scale (FRS) scores,11 which range from 1 to 17 and correspond to reading levels (score 1 = 1st-grade reading level). Health literacy experts have used the FRS to assess readability in health care environments.12
Understandability was measured with the Patient Education Materials Assessment Tool (PEMAT), a validated scoring system provided by the Agency for Healthcare Research and Quality.13 The PEMAT measures the understandability of print materials on a scale ranging from 0% to 100%. Higher scores indicate increased understandability, and scores under 70% indicate instructions are difficult to understand.
Although recent efforts have focused on the development of quality metrics for hospital-to-home transitions of pediatric patients,14 during our study there were no standard items to include in pediatric discharge instructions. Five criteria for completeness were determined by consensus of 3 pediatric hospital medicine faculty and were informed by qualitative results of work performed at our institution—work in which families noted challenges with information overload and a desire for pertinent and usable information that would enhance caregiver confidence and discharge preparedness.15 The criteria included statement of diagnosis, description of diagnosis, signs and symptoms indicative of the need for escalation of care (warning signs), the person caregivers should call if worried, and contact information for the primary care provider, subspecialist, and/or emergency department. Each set of discharge instructions was manually evaluated for completeness (presence of each individual component, number of components present, presence of all components). All charts were scored by the same investigator. A convenience sample of 20 charts was evaluated by a different investigator to ensure rating parameters were clear and classification was consistent (defined as perfect agreement). If the primary rater was undecided on a discharge instruction score, the secondary rater rated the instruction, and consensus was reached.
Means, medians, and ranges were calculated to enumerate the distribution of readability levels, understandability scores, and completeness of discharge instructions. Instructions were classified as readable if the FRS score was 6 or under, as understandable if the PEMAT score was under 70%, and as complete if all 5 criteria were satisfied. Descriptive statistics were generated for all demographic and clinical variables.
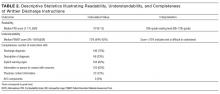
RESULTS
Of the study period’s 3819 discharges, 200 were randomly selected for review. Table 1 lists the demographic and clinical information of patients included in the analyses. Median FRS score was 10, indicating a 10th-grade reading level (interquartile range, 8-12; range, 1-13) (Table 2). Only 14 (7%) of 200 discharge instructions had a score of 6 or under. Median PEMAT understandability score was 73% (interquartile range, 64%-82%), and 36% of instructions had a PEMAT score under 70%. No instruction satisfied all 5 of the defined characteristics of complete discharge instructions (Table 2).
DISCUSSION
To our knowledge, this is the first study of the readability, understandability, and completeness of discharge instructions in a pediatric population. We found that the majority of discharge instruction readability levels were 10th grade or higher, that many instructions were difficult to understand, and that important information was missing from many instructions.
Discharge instruction readability levels were higher than the literacy level of many families in surrounding communities. The high school dropout rates in Cincinnati are staggering; they range from 22% to 64% in the 10 neighborhoods with the largest proportion of residents not completing high school.16 However, such findings are not unique to Cincinnati; low literacy is prevalent throughout the United States. Caregivers with limited literacy skills may struggle to navigate complex health systems, understand medical instructions and anticipatory guidance, perform child care and self-care tasks, and understand issues related to consent, medical authorization, and risk communication.17
Although readability is important, other factors also correlate with comprehension and execution of discharge tasks.18 Information must be understandable, or presented in a way that makes sense and can inform appropriate action. In many cases in our study, instructions were incomplete, despite previous investigators’ emphasizing caregivers’ desire and need for written instructions that are complete, informative, and inclusive of clearly outlined contingency plans.15,19 In addition, families may differ in the level of support needed after discharge; standardizing elements and including families in the development of discharge instructions may improve communication.8
This study had several limitations. First, the discharge instructions randomly selected for review were all written during the winter months. As the census on the hospital medicine teams is particularly high during that time, authors with competing responsibilities may not have had enough time to write effective discharge instructions then. We selected the winter period in order to capture real-world instructions written during a busy clinical time, when providers care for a high volume of patients. Second, caregiver health literacy and English-language proficiency were not assessed, and information regarding caregivers’ race/ethnicity, educational attainment, and socioeconomic status was unavailable. Third, interrater agreement was not formally evaluated. Fourth, this was a single-center study with results that may not be generalizable.
In conclusion, discharge instructions for pediatric patients are often difficult to read and understand, and incomplete. Efforts to address these communication gaps—including educational initiatives for physician trainees focused on health literacy, and quality improvement work directed at standardization and creation of readable, understandable, and complete discharge instructions—are crucial in providing safe, high-value care. Researchers need to evaluate the relationship between discharge instruction quality and outcomes, including unplanned office visits, emergency department visits, and readmissions.
Disclosure
Nothing to report.
1. Kutner MA, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy. Washington, DC: US Dept of Education, National Center for Education Statistics; 2006. NCES publication 2006-483. https://nces.ed.gov/pubs2006/2006483.pdf. Published September 2006. Accessed December 21, 2016.
2. Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan S, Parker RM, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2000:v-vi. NLM publication CBM 2000-1. https://www.nlm.nih.gov/archive//20061214/pubs/cbm/hliteracy.pdf. Published February 2000. Accessed December 21, 2016.
3. Arora VM, Schaninger C, D’Arcy M, et al. Improving inpatients’ identification of their doctors: use of FACE cards. Jt Comm J Qual Patient Saf. 2009;35(12):613-619. PubMed
4. Berkman ND, Sheridan SL, Donahue KE, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess (Full Rep). 2011;(199):1-941. PubMed
5. Ashbrook L, Mourad M, Sehgal N. Communicating discharge instructions to patients: a survey of nurse, intern, and hospitalist practices. J Hosp Med. 2013;8(1):36-41. PubMed
6. Kripalani S, Jacobson TA, Mugalla IC, Cawthon CR, Niesner KJ, Vaccarino V. Health literacy and the quality of physician–patient communication during hospitalization. J Hosp Med. 2010;5(5):269-275. PubMed
7. Nielsen-Bohlman L, Panzer AM, Kindig DA, eds; Committee on Health Literacy, Board on Neuroscience and Behavioral Health, Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
8. Hahn-Goldberg S, Okrainec K, Huynh T, Zahr N, Abrams H. Co-creating patient-oriented discharge instructions with patients, caregivers, and healthcare providers. J Hosp Med. 2015;10(12):804-807. PubMed
9. Lauster CD, Gibson JM, DiNella JV, DiNardo M, Korytkowski MT, Donihi AC. Implementation of standardized instructions for insulin at hospital discharge. J Hosp Med. 2009;4(8):E41-E42. PubMed
10. Howard-Anderson J, Busuttil A, Lonowski S, Vangala S, Afsar-Manesh N. From discharge to readmission: understanding the process from the patient perspective. J Hosp Med. 2016;11(6):407-412. PubMed
11. Fry E. A readability formula that saves time. J Reading. 1968;11:513-516, 575-578.
12. D’Alessandro DM, Kingsley P, Johnson-West J. The readability of pediatric patient education materials on the World Wide Web. Arch Pediatr Adolesc Med. 2001;155(7):807-812. PubMed
13. Shoemaker SJ, Wolf MS, Brach C. The Patient Education Materials Assessment Tool (PEMAT) and User’s Guide: An Instrument to Assess the Understandability and Actionability of Print and Audiovisual Patient Education Materials. Rockville, MD: US Dept of Health and Human Services, Agency for Healthcare Research and Quality; 2013. http://www.ahrq.gov/professionals/prevention-chronic-care/improve/self-mgmt/pemat/index.html. Published October 2013. Accessed November 27, 2013.
14. Leyenaar JK, Desai AD, Burkhart Q, et al. Quality measures to assess care transitions for hospitalized children. Pediatrics. 2016;138(2). PubMed
15. Solan LG, Beck AF, Brunswick SA, et al; H2O Study Group. The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136(6):e1539-e1549. PubMed
16. Maloney M, Auffrey C. The Social Areas of Cincinnati: An Analysis of Social Needs: Patterns for Five Census Decades. 5th ed. Cincinnati, OH: University of Cincinnati School of Planning/United Way/University of Cincinnati Community Research Collaborative; 2013. http://www.socialareasofcincinnati.org/files/FifthEdition/SASBook.pdf. Published April 2013. Accessed December 21, 2016.
17. Rothman RL, Yin HS, Mulvaney S, Co JP, Homer C, Lannon C. Health literacy and quality: focus on chronic illness care and patient safety. Pediatrics. 2009;124(suppl 3):S315-S326. PubMed
18. Moon RY, Cheng TL, Patel KM, Baumhaft K, Scheidt PC. Parental literacy level and understanding of medical information. Pediatrics. 1998;102(2):e25. PubMed
19. Desai AD, Durkin LK, Jacob-Files EA, Mangione-Smith R. Caregiver perceptions of hospital to home transitions according to medical complexity: a qualitative study. Acad Pediatr. 2016;16(2):136-144. PubMed
The average American adult reads at an 8th-grade level.1 Limited general literacy can affect health literacy, which is defined as the “degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”2,3 Adults with limited health literacy are at risk for poorer outcomes, including overuse of the emergency department and lower adherence to preventive care recommendations.4
Children transitioning from hospital to home depend on their adult caregivers (and their caregivers’ health literacy) to carry out discharge instructions. During the immediate postdischarge period, complex care needs can involve new or changed medications, follow-up instructions, home care instructions, and suggestions regarding when and why to seek additional care.
The discharge education provided to patients in the hospital is often subpar because of lack of standardization and divided responsibility among providers.5 Communication of vital information to patients with low health literacy has been noted to be particularly poor,6 as many patient education materials are written at 10th-, 11th-, and 12th-grade reading levels.4 Evidence supports providing materials written at 6th-grade level or lower to increase comprehension.7 Several studies have evaluated the quality and readability of discharge instructions for hospitalized adults,8,9 and one study found a link between poorly written instructions for adult patients and readmission risk.10 Less is known about readability in pediatrics, in which education may be more important for families of children most commonly hospitalized for acute illness.
We conducted a study to describe readability levels, understandability scores, and completeness of written instructions given to families at hospital discharge.
METHODS
Study Design and Setting
In this study, we performed a cross-sectional review of discharge instructions within electronic health records at Cincinnati Children’s Hospital Medical Center (CCHMC). The study was reviewed and approved by CCHMC’s Institutional Review Board. Charts were randomly selected from all hospital medicine service discharges during two 3-month periods of high patient volume: January-March 2014 and January-March 2015.
CCHMC is a large urban academic referral center that is the sole provider of general, subspecialty, and critical pediatric inpatient care for a large geographical area. CCHMC, which has 600 beds, provides cares for many children who live in impoverished settings. Its hospital medicine service consists of 4 teams that care for approximately 7000 children hospitalized with general pediatric illnesses each year. Each team consists of 5 or 6 pediatric residents supervised by a hospital medicine attending.
Providers, most commonly pediatric interns, generate discharge instructions in electronic health records. In this nonautomated process, they use free-text or nonstandardized templates to create content. At discharge, instructions are printed as part of the postvisit summary, which includes updates on medications and scheduled follow-up appointments. Bedside nurses verbally review the instructions with families and provide printed copies for home use.
Data Collection and Analysis
A random sequence generator was used to select charts for review. Instructions written in a language other than English were excluded. Written discharge instructions and clinical information, including age, sex, primary diagnosis, insurance type, number of discharge medications, number of scheduled appointments at discharge, and hospital length of stay, were abstracted from electronic health records and anonymized before analysis. The primary outcomes assessed were discharge instruction readability, understandability, and completeness. Readability was calculated with Fry Readability Scale (FRS) scores,11 which range from 1 to 17 and correspond to reading levels (score 1 = 1st-grade reading level). Health literacy experts have used the FRS to assess readability in health care environments.12
Understandability was measured with the Patient Education Materials Assessment Tool (PEMAT), a validated scoring system provided by the Agency for Healthcare Research and Quality.13 The PEMAT measures the understandability of print materials on a scale ranging from 0% to 100%. Higher scores indicate increased understandability, and scores under 70% indicate instructions are difficult to understand.
Although recent efforts have focused on the development of quality metrics for hospital-to-home transitions of pediatric patients,14 during our study there were no standard items to include in pediatric discharge instructions. Five criteria for completeness were determined by consensus of 3 pediatric hospital medicine faculty and were informed by qualitative results of work performed at our institution—work in which families noted challenges with information overload and a desire for pertinent and usable information that would enhance caregiver confidence and discharge preparedness.15 The criteria included statement of diagnosis, description of diagnosis, signs and symptoms indicative of the need for escalation of care (warning signs), the person caregivers should call if worried, and contact information for the primary care provider, subspecialist, and/or emergency department. Each set of discharge instructions was manually evaluated for completeness (presence of each individual component, number of components present, presence of all components). All charts were scored by the same investigator. A convenience sample of 20 charts was evaluated by a different investigator to ensure rating parameters were clear and classification was consistent (defined as perfect agreement). If the primary rater was undecided on a discharge instruction score, the secondary rater rated the instruction, and consensus was reached.
Means, medians, and ranges were calculated to enumerate the distribution of readability levels, understandability scores, and completeness of discharge instructions. Instructions were classified as readable if the FRS score was 6 or under, as understandable if the PEMAT score was under 70%, and as complete if all 5 criteria were satisfied. Descriptive statistics were generated for all demographic and clinical variables.
RESULTS
Of the study period’s 3819 discharges, 200 were randomly selected for review. Table 1 lists the demographic and clinical information of patients included in the analyses. Median FRS score was 10, indicating a 10th-grade reading level (interquartile range, 8-12; range, 1-13) (Table 2). Only 14 (7%) of 200 discharge instructions had a score of 6 or under. Median PEMAT understandability score was 73% (interquartile range, 64%-82%), and 36% of instructions had a PEMAT score under 70%. No instruction satisfied all 5 of the defined characteristics of complete discharge instructions (Table 2).
DISCUSSION
To our knowledge, this is the first study of the readability, understandability, and completeness of discharge instructions in a pediatric population. We found that the majority of discharge instruction readability levels were 10th grade or higher, that many instructions were difficult to understand, and that important information was missing from many instructions.
Discharge instruction readability levels were higher than the literacy level of many families in surrounding communities. The high school dropout rates in Cincinnati are staggering; they range from 22% to 64% in the 10 neighborhoods with the largest proportion of residents not completing high school.16 However, such findings are not unique to Cincinnati; low literacy is prevalent throughout the United States. Caregivers with limited literacy skills may struggle to navigate complex health systems, understand medical instructions and anticipatory guidance, perform child care and self-care tasks, and understand issues related to consent, medical authorization, and risk communication.17
Although readability is important, other factors also correlate with comprehension and execution of discharge tasks.18 Information must be understandable, or presented in a way that makes sense and can inform appropriate action. In many cases in our study, instructions were incomplete, despite previous investigators’ emphasizing caregivers’ desire and need for written instructions that are complete, informative, and inclusive of clearly outlined contingency plans.15,19 In addition, families may differ in the level of support needed after discharge; standardizing elements and including families in the development of discharge instructions may improve communication.8
This study had several limitations. First, the discharge instructions randomly selected for review were all written during the winter months. As the census on the hospital medicine teams is particularly high during that time, authors with competing responsibilities may not have had enough time to write effective discharge instructions then. We selected the winter period in order to capture real-world instructions written during a busy clinical time, when providers care for a high volume of patients. Second, caregiver health literacy and English-language proficiency were not assessed, and information regarding caregivers’ race/ethnicity, educational attainment, and socioeconomic status was unavailable. Third, interrater agreement was not formally evaluated. Fourth, this was a single-center study with results that may not be generalizable.
In conclusion, discharge instructions for pediatric patients are often difficult to read and understand, and incomplete. Efforts to address these communication gaps—including educational initiatives for physician trainees focused on health literacy, and quality improvement work directed at standardization and creation of readable, understandable, and complete discharge instructions—are crucial in providing safe, high-value care. Researchers need to evaluate the relationship between discharge instruction quality and outcomes, including unplanned office visits, emergency department visits, and readmissions.
Disclosure
Nothing to report.
The average American adult reads at an 8th-grade level.1 Limited general literacy can affect health literacy, which is defined as the “degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.”2,3 Adults with limited health literacy are at risk for poorer outcomes, including overuse of the emergency department and lower adherence to preventive care recommendations.4
Children transitioning from hospital to home depend on their adult caregivers (and their caregivers’ health literacy) to carry out discharge instructions. During the immediate postdischarge period, complex care needs can involve new or changed medications, follow-up instructions, home care instructions, and suggestions regarding when and why to seek additional care.
The discharge education provided to patients in the hospital is often subpar because of lack of standardization and divided responsibility among providers.5 Communication of vital information to patients with low health literacy has been noted to be particularly poor,6 as many patient education materials are written at 10th-, 11th-, and 12th-grade reading levels.4 Evidence supports providing materials written at 6th-grade level or lower to increase comprehension.7 Several studies have evaluated the quality and readability of discharge instructions for hospitalized adults,8,9 and one study found a link between poorly written instructions for adult patients and readmission risk.10 Less is known about readability in pediatrics, in which education may be more important for families of children most commonly hospitalized for acute illness.
We conducted a study to describe readability levels, understandability scores, and completeness of written instructions given to families at hospital discharge.
METHODS
Study Design and Setting
In this study, we performed a cross-sectional review of discharge instructions within electronic health records at Cincinnati Children’s Hospital Medical Center (CCHMC). The study was reviewed and approved by CCHMC’s Institutional Review Board. Charts were randomly selected from all hospital medicine service discharges during two 3-month periods of high patient volume: January-March 2014 and January-March 2015.
CCHMC is a large urban academic referral center that is the sole provider of general, subspecialty, and critical pediatric inpatient care for a large geographical area. CCHMC, which has 600 beds, provides cares for many children who live in impoverished settings. Its hospital medicine service consists of 4 teams that care for approximately 7000 children hospitalized with general pediatric illnesses each year. Each team consists of 5 or 6 pediatric residents supervised by a hospital medicine attending.
Providers, most commonly pediatric interns, generate discharge instructions in electronic health records. In this nonautomated process, they use free-text or nonstandardized templates to create content. At discharge, instructions are printed as part of the postvisit summary, which includes updates on medications and scheduled follow-up appointments. Bedside nurses verbally review the instructions with families and provide printed copies for home use.
Data Collection and Analysis
A random sequence generator was used to select charts for review. Instructions written in a language other than English were excluded. Written discharge instructions and clinical information, including age, sex, primary diagnosis, insurance type, number of discharge medications, number of scheduled appointments at discharge, and hospital length of stay, were abstracted from electronic health records and anonymized before analysis. The primary outcomes assessed were discharge instruction readability, understandability, and completeness. Readability was calculated with Fry Readability Scale (FRS) scores,11 which range from 1 to 17 and correspond to reading levels (score 1 = 1st-grade reading level). Health literacy experts have used the FRS to assess readability in health care environments.12
Understandability was measured with the Patient Education Materials Assessment Tool (PEMAT), a validated scoring system provided by the Agency for Healthcare Research and Quality.13 The PEMAT measures the understandability of print materials on a scale ranging from 0% to 100%. Higher scores indicate increased understandability, and scores under 70% indicate instructions are difficult to understand.
Although recent efforts have focused on the development of quality metrics for hospital-to-home transitions of pediatric patients,14 during our study there were no standard items to include in pediatric discharge instructions. Five criteria for completeness were determined by consensus of 3 pediatric hospital medicine faculty and were informed by qualitative results of work performed at our institution—work in which families noted challenges with information overload and a desire for pertinent and usable information that would enhance caregiver confidence and discharge preparedness.15 The criteria included statement of diagnosis, description of diagnosis, signs and symptoms indicative of the need for escalation of care (warning signs), the person caregivers should call if worried, and contact information for the primary care provider, subspecialist, and/or emergency department. Each set of discharge instructions was manually evaluated for completeness (presence of each individual component, number of components present, presence of all components). All charts were scored by the same investigator. A convenience sample of 20 charts was evaluated by a different investigator to ensure rating parameters were clear and classification was consistent (defined as perfect agreement). If the primary rater was undecided on a discharge instruction score, the secondary rater rated the instruction, and consensus was reached.
Means, medians, and ranges were calculated to enumerate the distribution of readability levels, understandability scores, and completeness of discharge instructions. Instructions were classified as readable if the FRS score was 6 or under, as understandable if the PEMAT score was under 70%, and as complete if all 5 criteria were satisfied. Descriptive statistics were generated for all demographic and clinical variables.
RESULTS
Of the study period’s 3819 discharges, 200 were randomly selected for review. Table 1 lists the demographic and clinical information of patients included in the analyses. Median FRS score was 10, indicating a 10th-grade reading level (interquartile range, 8-12; range, 1-13) (Table 2). Only 14 (7%) of 200 discharge instructions had a score of 6 or under. Median PEMAT understandability score was 73% (interquartile range, 64%-82%), and 36% of instructions had a PEMAT score under 70%. No instruction satisfied all 5 of the defined characteristics of complete discharge instructions (Table 2).
DISCUSSION
To our knowledge, this is the first study of the readability, understandability, and completeness of discharge instructions in a pediatric population. We found that the majority of discharge instruction readability levels were 10th grade or higher, that many instructions were difficult to understand, and that important information was missing from many instructions.
Discharge instruction readability levels were higher than the literacy level of many families in surrounding communities. The high school dropout rates in Cincinnati are staggering; they range from 22% to 64% in the 10 neighborhoods with the largest proportion of residents not completing high school.16 However, such findings are not unique to Cincinnati; low literacy is prevalent throughout the United States. Caregivers with limited literacy skills may struggle to navigate complex health systems, understand medical instructions and anticipatory guidance, perform child care and self-care tasks, and understand issues related to consent, medical authorization, and risk communication.17
Although readability is important, other factors also correlate with comprehension and execution of discharge tasks.18 Information must be understandable, or presented in a way that makes sense and can inform appropriate action. In many cases in our study, instructions were incomplete, despite previous investigators’ emphasizing caregivers’ desire and need for written instructions that are complete, informative, and inclusive of clearly outlined contingency plans.15,19 In addition, families may differ in the level of support needed after discharge; standardizing elements and including families in the development of discharge instructions may improve communication.8
This study had several limitations. First, the discharge instructions randomly selected for review were all written during the winter months. As the census on the hospital medicine teams is particularly high during that time, authors with competing responsibilities may not have had enough time to write effective discharge instructions then. We selected the winter period in order to capture real-world instructions written during a busy clinical time, when providers care for a high volume of patients. Second, caregiver health literacy and English-language proficiency were not assessed, and information regarding caregivers’ race/ethnicity, educational attainment, and socioeconomic status was unavailable. Third, interrater agreement was not formally evaluated. Fourth, this was a single-center study with results that may not be generalizable.
In conclusion, discharge instructions for pediatric patients are often difficult to read and understand, and incomplete. Efforts to address these communication gaps—including educational initiatives for physician trainees focused on health literacy, and quality improvement work directed at standardization and creation of readable, understandable, and complete discharge instructions—are crucial in providing safe, high-value care. Researchers need to evaluate the relationship between discharge instruction quality and outcomes, including unplanned office visits, emergency department visits, and readmissions.
Disclosure
Nothing to report.
1. Kutner MA, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy. Washington, DC: US Dept of Education, National Center for Education Statistics; 2006. NCES publication 2006-483. https://nces.ed.gov/pubs2006/2006483.pdf. Published September 2006. Accessed December 21, 2016.
2. Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan S, Parker RM, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2000:v-vi. NLM publication CBM 2000-1. https://www.nlm.nih.gov/archive//20061214/pubs/cbm/hliteracy.pdf. Published February 2000. Accessed December 21, 2016.
3. Arora VM, Schaninger C, D’Arcy M, et al. Improving inpatients’ identification of their doctors: use of FACE cards. Jt Comm J Qual Patient Saf. 2009;35(12):613-619. PubMed
4. Berkman ND, Sheridan SL, Donahue KE, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess (Full Rep). 2011;(199):1-941. PubMed
5. Ashbrook L, Mourad M, Sehgal N. Communicating discharge instructions to patients: a survey of nurse, intern, and hospitalist practices. J Hosp Med. 2013;8(1):36-41. PubMed
6. Kripalani S, Jacobson TA, Mugalla IC, Cawthon CR, Niesner KJ, Vaccarino V. Health literacy and the quality of physician–patient communication during hospitalization. J Hosp Med. 2010;5(5):269-275. PubMed
7. Nielsen-Bohlman L, Panzer AM, Kindig DA, eds; Committee on Health Literacy, Board on Neuroscience and Behavioral Health, Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
8. Hahn-Goldberg S, Okrainec K, Huynh T, Zahr N, Abrams H. Co-creating patient-oriented discharge instructions with patients, caregivers, and healthcare providers. J Hosp Med. 2015;10(12):804-807. PubMed
9. Lauster CD, Gibson JM, DiNella JV, DiNardo M, Korytkowski MT, Donihi AC. Implementation of standardized instructions for insulin at hospital discharge. J Hosp Med. 2009;4(8):E41-E42. PubMed
10. Howard-Anderson J, Busuttil A, Lonowski S, Vangala S, Afsar-Manesh N. From discharge to readmission: understanding the process from the patient perspective. J Hosp Med. 2016;11(6):407-412. PubMed
11. Fry E. A readability formula that saves time. J Reading. 1968;11:513-516, 575-578.
12. D’Alessandro DM, Kingsley P, Johnson-West J. The readability of pediatric patient education materials on the World Wide Web. Arch Pediatr Adolesc Med. 2001;155(7):807-812. PubMed
13. Shoemaker SJ, Wolf MS, Brach C. The Patient Education Materials Assessment Tool (PEMAT) and User’s Guide: An Instrument to Assess the Understandability and Actionability of Print and Audiovisual Patient Education Materials. Rockville, MD: US Dept of Health and Human Services, Agency for Healthcare Research and Quality; 2013. http://www.ahrq.gov/professionals/prevention-chronic-care/improve/self-mgmt/pemat/index.html. Published October 2013. Accessed November 27, 2013.
14. Leyenaar JK, Desai AD, Burkhart Q, et al. Quality measures to assess care transitions for hospitalized children. Pediatrics. 2016;138(2). PubMed
15. Solan LG, Beck AF, Brunswick SA, et al; H2O Study Group. The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136(6):e1539-e1549. PubMed
16. Maloney M, Auffrey C. The Social Areas of Cincinnati: An Analysis of Social Needs: Patterns for Five Census Decades. 5th ed. Cincinnati, OH: University of Cincinnati School of Planning/United Way/University of Cincinnati Community Research Collaborative; 2013. http://www.socialareasofcincinnati.org/files/FifthEdition/SASBook.pdf. Published April 2013. Accessed December 21, 2016.
17. Rothman RL, Yin HS, Mulvaney S, Co JP, Homer C, Lannon C. Health literacy and quality: focus on chronic illness care and patient safety. Pediatrics. 2009;124(suppl 3):S315-S326. PubMed
18. Moon RY, Cheng TL, Patel KM, Baumhaft K, Scheidt PC. Parental literacy level and understanding of medical information. Pediatrics. 1998;102(2):e25. PubMed
19. Desai AD, Durkin LK, Jacob-Files EA, Mangione-Smith R. Caregiver perceptions of hospital to home transitions according to medical complexity: a qualitative study. Acad Pediatr. 2016;16(2):136-144. PubMed
1. Kutner MA, Greenberg E, Jin Y, Paulsen C. The Health Literacy of America’s Adults: Results From the 2003 National Assessment of Adult Literacy. Washington, DC: US Dept of Education, National Center for Education Statistics; 2006. NCES publication 2006-483. https://nces.ed.gov/pubs2006/2006483.pdf. Published September 2006. Accessed December 21, 2016.
2. Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan S, Parker RM, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: US Dept of Health and Human Services, National Institutes of Health; 2000:v-vi. NLM publication CBM 2000-1. https://www.nlm.nih.gov/archive//20061214/pubs/cbm/hliteracy.pdf. Published February 2000. Accessed December 21, 2016.
3. Arora VM, Schaninger C, D’Arcy M, et al. Improving inpatients’ identification of their doctors: use of FACE cards. Jt Comm J Qual Patient Saf. 2009;35(12):613-619. PubMed
4. Berkman ND, Sheridan SL, Donahue KE, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess (Full Rep). 2011;(199):1-941. PubMed
5. Ashbrook L, Mourad M, Sehgal N. Communicating discharge instructions to patients: a survey of nurse, intern, and hospitalist practices. J Hosp Med. 2013;8(1):36-41. PubMed
6. Kripalani S, Jacobson TA, Mugalla IC, Cawthon CR, Niesner KJ, Vaccarino V. Health literacy and the quality of physician–patient communication during hospitalization. J Hosp Med. 2010;5(5):269-275. PubMed
7. Nielsen-Bohlman L, Panzer AM, Kindig DA, eds; Committee on Health Literacy, Board on Neuroscience and Behavioral Health, Institute of Medicine. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
8. Hahn-Goldberg S, Okrainec K, Huynh T, Zahr N, Abrams H. Co-creating patient-oriented discharge instructions with patients, caregivers, and healthcare providers. J Hosp Med. 2015;10(12):804-807. PubMed
9. Lauster CD, Gibson JM, DiNella JV, DiNardo M, Korytkowski MT, Donihi AC. Implementation of standardized instructions for insulin at hospital discharge. J Hosp Med. 2009;4(8):E41-E42. PubMed
10. Howard-Anderson J, Busuttil A, Lonowski S, Vangala S, Afsar-Manesh N. From discharge to readmission: understanding the process from the patient perspective. J Hosp Med. 2016;11(6):407-412. PubMed
11. Fry E. A readability formula that saves time. J Reading. 1968;11:513-516, 575-578.
12. D’Alessandro DM, Kingsley P, Johnson-West J. The readability of pediatric patient education materials on the World Wide Web. Arch Pediatr Adolesc Med. 2001;155(7):807-812. PubMed
13. Shoemaker SJ, Wolf MS, Brach C. The Patient Education Materials Assessment Tool (PEMAT) and User’s Guide: An Instrument to Assess the Understandability and Actionability of Print and Audiovisual Patient Education Materials. Rockville, MD: US Dept of Health and Human Services, Agency for Healthcare Research and Quality; 2013. http://www.ahrq.gov/professionals/prevention-chronic-care/improve/self-mgmt/pemat/index.html. Published October 2013. Accessed November 27, 2013.
14. Leyenaar JK, Desai AD, Burkhart Q, et al. Quality measures to assess care transitions for hospitalized children. Pediatrics. 2016;138(2). PubMed
15. Solan LG, Beck AF, Brunswick SA, et al; H2O Study Group. The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136(6):e1539-e1549. PubMed
16. Maloney M, Auffrey C. The Social Areas of Cincinnati: An Analysis of Social Needs: Patterns for Five Census Decades. 5th ed. Cincinnati, OH: University of Cincinnati School of Planning/United Way/University of Cincinnati Community Research Collaborative; 2013. http://www.socialareasofcincinnati.org/files/FifthEdition/SASBook.pdf. Published April 2013. Accessed December 21, 2016.
17. Rothman RL, Yin HS, Mulvaney S, Co JP, Homer C, Lannon C. Health literacy and quality: focus on chronic illness care and patient safety. Pediatrics. 2009;124(suppl 3):S315-S326. PubMed
18. Moon RY, Cheng TL, Patel KM, Baumhaft K, Scheidt PC. Parental literacy level and understanding of medical information. Pediatrics. 1998;102(2):e25. PubMed
19. Desai AD, Durkin LK, Jacob-Files EA, Mangione-Smith R. Caregiver perceptions of hospital to home transitions according to medical complexity: a qualitative study. Acad Pediatr. 2016;16(2):136-144. PubMed
© 2017 Society of Hospital Medicine