User login
To Cut or Not to Cut? Evaluating Surgical Criteria for Benign & Nondiagnostic Thyroid Nodules
A new-onset thyroid nodule, found on exam or incidentally on imaging, is a common presentation at primary care and specialist clinics. Palpable nodules are present in 4% to 7% of the population.1 However, more sensitive evaluation with thyroid ultrasound (US) suggests an incidence as high as 70%.2
According to the American Cancer Society, in 2015, there were approximately 62,450 new cases of thyroid cancer in the United States (with 2.5 times as many occurring in women as in men).3 In fact, thyroid cancer is the most rapidly increasing cancer in the United States—attributable in part to the increased use of thyroid US and incidental detection.3
The high prevalence of thyroid nodules makes appropriate evaluation and treatment crucial. This article, through a case study, explores the evaluation of a thyroid nodule and the recommendation for and against thyroidectomy.
Felicia, 49, presents to the endocrine clinic as a new patient with questions about multinodular goiter (MNG). She has been advised by ENT to have a left-sided dominant nodule surgically removed while under anesthesia during her upcoming chronic sinusitis surgery. Felicia would like to avoid thyroid surgery, if possible. Her most recent thyroid US, performed three months ago, showed a right lobe with multiple colloid nodules with inspissated colloid, the largest of which is 1.5 cm, and a 4-cm complex, solid, cystic nodule with inspissated colloid in the cystic spaces replacing the entire left thyroid lobe.
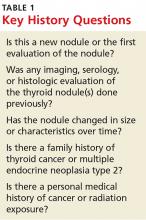
HistoryThe first step is establishing a history of the nodule(s) in question. Key questions are listed in Table 1. The onset and progression of a thyroid nodule must be determined; ideally, the provider should review any previous studies related to the thyroid gland. This will help determine if the nodule is new, if it has been evaluated in the past, and if it has changed significantly.
A thorough history can identify risk factors for malignancy, which include a personal history of cancer or radiation exposure, as well as a family history of thyroid cancer or malignant endocrine syndromes.
Felicia denies any family or personal medical history concerning for malignancy. She notes that she has two sisters with MNG. She denies any neck pain, compressive/obstructive symptoms, and hypo- or hyperthyroid symptoms.
She reports that she was found to have a goiter on exam and was subsequently diagnosed with MNG in 2008. Thyroid US showed a 2.3-cm complex, largely solid mass in the right mid-pole and a 3.3-cm largely cystic lesion in the left mid-pole. She was referred for right-sided fine-needle aspiration (FNA); results were consistent with benign colloid nodule. The left-sided nodule was not biopsied at that time, due to a largely cystic component.
Felicia underwent a follow-up US in 2011; it showed a 1.6-cm right mid-pole nodule with multiple nonspecific echogenic areas; a 1-cm benign-appearing nodule; and a 3.7-cm highly vascular heterogeneous mass with some colloid components with indeterminate component in the left lower and mid-pole. She reports that she did not follow up in 2011. Her next evaluation was the current thyroid US. She has never had FNA of the left-sided dominant nodule.
Continue for symptomatic vs asymptomatic thyroid nodules >>
Symptomatic vs Asymptomatic Thyroid NodulesEvaluation of a symptomatic thyroid nodule can help to determine the need for surgery, as well as assess the level of interference with a patient’s activities of daily living and the potential for functional abnormalities. However, both local neck and constitutional symptoms may be nonspecific and unrelated to the thyroid gland’s structure or function. Therefore, the provider should exercise caution in making recommendations based on reported symptoms alone.
Symptoms indicative of the need for surgical intervention include neck pain, increased neck pressure, foreign body sensation, dysphonia, dyspnea, and dysphagia. However, it is essential to determine if these symptoms are likely due to a thyroid nodule or if they can be attributed to a secondary cause (eg, postnasal drip, vocal cord dysfunction, gastroesophageal reflux disease, or esophageal stricture).
If the findings are inconsistent with the clinical picture, secondary evaluation is prudent to avoid an unnecessary procedure.
Physical ExamPalpation of a thyroid nodule is an unreliable indicator of risk for malignancy. Palpation alone does not allow for detection of all nodules, particularly smaller ones, and specific characteristics are not discernible. Imaging studies are required to accurately evaluate a thyroid nodule and determine the most appropriate course of action.
Palpation can be used to evaluate for a larger and/or fixed nodule, thyroid gland/nodule tenderness, and cervical lymphadenopathy. Physical exam can also assess for signs of hypo- or hyperthyroidism, including abnormal pulse rate or blood pressure, tremor, hypo- or hyperreflexia, and integumentary abnormalities (eg, hair loss, abnormal skin temperature, and nail changes).
Continue for serologic evaluation >>
Serologic Evaluation
If a thyroid nodule is suspected on exam or found on imaging, assessment of thyroid function, via thyroid-stimulating hormone (TSH) measurement, is the recommended first step. If TSH is elevated, further evaluation for hypothyroidism is recommended, with testing for free thyroxine (T4) and antithyroid peroxidase (TPO) antibodies.4 If TSH is suppressed, further evaluation with free T4 and assessment for underlying causes of hyperthyroidism are indicated, including work-up for toxic nodular goiter.
Routine monitoring of serum calcitonin level is not recommended. However, if there is suspicion for medullary thyroid cancer—based on either US findings or family history—serologic screening for abnormal calcitonin level may be indicated.4,5
Felicia’s lab results include a TSH of 1.30 µIU/mL (reference range, 0.30-3.00 µIU/mL). Based on this finding, what (if any) further serologic testing is recommended? None: With normal TSH and no concerning family or personal history, additional laboratory evaluation is not indicated.
Imaging a Thyroid Nodule
Thyroid US is the most sensitive imaging study for evaluating thyroid nodule characteristics. Thyroid uptake and scan is not indicated unless TSH is suppressed and evaluation for toxic nodular goiter is needed. Additional imaging studies, such as CT or MRI, are not recommended for thyroid nodule evaluation.
Based on the thyroid US, what characteristics of Felicia’s nodule are suggestive of a benign nodule? Of a malignant nodule? (See Table 2.)
FNA of the left-sided dominant nodule is indicated, based on the US findings of a partially solid component and size > 1 cm. Unfortunately, FNA is nondiagnostic, because it yielded cystic fluid only with scant follicular cells for evaluation.
Continue to now what? >>
Now What?
While FNA most definitively distinguishes between benign and malignant nodules, the test is limited. An indeterminate, or nondiagnostic, finding occurs in 10% to 15% of cases and is more likely in nodules with a large cystic component.1
Even a benign finding on FNA of a larger nodule should be viewed with caution, since aspiration is unlikely to pinpoint small insidious malignant cells nestled among a larger collection of benign tissue.3 In many situations, a patient receives FNA results and asks, “What should we do now?”
Nondiagnostic nodules
When FNA is indeterminate, the next step depends on the characteristics of the nodule. For a solid nodule, repeat FNA is recommended.4,5 For nodules with repeatedly nondiagnostic FNAs, the American Academy of Clinical Endocrinologists and the American Thyroid Association recommend that a solid nodule be considered for surgical removal unless the nodule has “clearly favorable clinical and US features.”4,5
Surgical excision should be considered for cysts that recur, those that are larger (> 4 cm), and those that are repeatedly nondiagnostic on FNA. Personal and family history should be taken into account when nodules that are nondiagnostic on FNA demonstrate suspicious characteristics on US.6
An analysis by Renshaw determined that risk for malignancy in a nodule with a single nondiagnostic FNA was about 20%. For nodules that underwent repeat FNA, the risk was 0% for those that were again nondiagnostic. This significant difference led the author to conclude that “patients with two sequential nondiagnostic thyroid aspirates have a very low risk of malignancy.”7
Consider the time commitment, financial burden, and emotional cost for the patient of repeated evaluation with thyroid US and possibly FNA. In recurrent cases, the risks associated with surgery begin to be outweighed by the cost and burden of prolonged observation.
Benign nodules
With a biopsy-proven benign nodule, observation is recommended unless certain criteria are present: local neck compressive/obstructive symptoms that can be confidently attributed to a thyroid nodule; patient preference (eg, due to anxiety or aesthetics); or higher index of suspicion (eg, history of previous radiation exposure, progressive nodule growth, or suspicious characteristics on US).4,5
If surgical removal of a benign thyroid nodule is recommended, it is imperative to discuss the risks with patients. In addition to traditional surgery risks, thyroidectomy is associated with transient or permanent postoperative hypoparathyroidism, as well as vocal hoarseness or changes in vocal quality due to the proximity of the recurrent laryngeal nerve. Additionally, patients should be advised of the potential for surgical hypothyroidism with hemithyroidectomy and certain irreversible hypothyroidism with total thyroidectomy.
After a discussion of the risks and cost of observation versus surgery, an informed decision between provider and patient can ultimately be reached.
Would thyroidectomy be recommended for Felicia? After a thorough discussion, it is decided that surgery is not indicated at this time. Relevant factors include the benign thyroid US characteristics, lack of clinical neck compressive symptoms, and patient preference.
According to the American Thyroid Association guidelines, Felicia’s risk for malignancy for the nodule in question is < 3%, since it is a partially cystic nodule without any suspicious sonographic features. By foregoing surgery, Felicia will need repeated imaging studies and possibly repeat serologic studies and FNA in the future.
References
1. Stang MT, Carty SE. Recent developments in predicting thyroid malignancy. Curr Opin Oncol. 2008;21(1):11-17.
2. Hambleton C, Kandil E. Appropriate and accurate diagnosis of thyroid nodules: a review of thyroid fine-needle aspiration. Int J Clin Exp Med. 2013;6(6):413-422.
3. American Cancer Society. Thyroid cancer (2014). www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf. Accessed June 29, 2016.
4. Gharib H, Papini E, Garber J, et al; AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules—2016 Update. Endocrine Pract. 2016;22(suppl 1):1-60.
5. Haugen BR, Alexander EK, Bible KC, et al; The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26(1):1-133.
6. Yeung MJ, Serpell JW. Management of the solitary thyroid nodule. Oncologist. 2008; 13(2):105-112.
7. Renshaw A. Significance of repeatedly nondiagnostic thyroid fine-needle aspirations. Am J Clin Pathol. 2011;135(5):750-752.
A new-onset thyroid nodule, found on exam or incidentally on imaging, is a common presentation at primary care and specialist clinics. Palpable nodules are present in 4% to 7% of the population.1 However, more sensitive evaluation with thyroid ultrasound (US) suggests an incidence as high as 70%.2
According to the American Cancer Society, in 2015, there were approximately 62,450 new cases of thyroid cancer in the United States (with 2.5 times as many occurring in women as in men).3 In fact, thyroid cancer is the most rapidly increasing cancer in the United States—attributable in part to the increased use of thyroid US and incidental detection.3
The high prevalence of thyroid nodules makes appropriate evaluation and treatment crucial. This article, through a case study, explores the evaluation of a thyroid nodule and the recommendation for and against thyroidectomy.
Felicia, 49, presents to the endocrine clinic as a new patient with questions about multinodular goiter (MNG). She has been advised by ENT to have a left-sided dominant nodule surgically removed while under anesthesia during her upcoming chronic sinusitis surgery. Felicia would like to avoid thyroid surgery, if possible. Her most recent thyroid US, performed three months ago, showed a right lobe with multiple colloid nodules with inspissated colloid, the largest of which is 1.5 cm, and a 4-cm complex, solid, cystic nodule with inspissated colloid in the cystic spaces replacing the entire left thyroid lobe.
HistoryThe first step is establishing a history of the nodule(s) in question. Key questions are listed in Table 1. The onset and progression of a thyroid nodule must be determined; ideally, the provider should review any previous studies related to the thyroid gland. This will help determine if the nodule is new, if it has been evaluated in the past, and if it has changed significantly.
A thorough history can identify risk factors for malignancy, which include a personal history of cancer or radiation exposure, as well as a family history of thyroid cancer or malignant endocrine syndromes.
Felicia denies any family or personal medical history concerning for malignancy. She notes that she has two sisters with MNG. She denies any neck pain, compressive/obstructive symptoms, and hypo- or hyperthyroid symptoms.
She reports that she was found to have a goiter on exam and was subsequently diagnosed with MNG in 2008. Thyroid US showed a 2.3-cm complex, largely solid mass in the right mid-pole and a 3.3-cm largely cystic lesion in the left mid-pole. She was referred for right-sided fine-needle aspiration (FNA); results were consistent with benign colloid nodule. The left-sided nodule was not biopsied at that time, due to a largely cystic component.
Felicia underwent a follow-up US in 2011; it showed a 1.6-cm right mid-pole nodule with multiple nonspecific echogenic areas; a 1-cm benign-appearing nodule; and a 3.7-cm highly vascular heterogeneous mass with some colloid components with indeterminate component in the left lower and mid-pole. She reports that she did not follow up in 2011. Her next evaluation was the current thyroid US. She has never had FNA of the left-sided dominant nodule.
Continue for symptomatic vs asymptomatic thyroid nodules >>
Symptomatic vs Asymptomatic Thyroid NodulesEvaluation of a symptomatic thyroid nodule can help to determine the need for surgery, as well as assess the level of interference with a patient’s activities of daily living and the potential for functional abnormalities. However, both local neck and constitutional symptoms may be nonspecific and unrelated to the thyroid gland’s structure or function. Therefore, the provider should exercise caution in making recommendations based on reported symptoms alone.
Symptoms indicative of the need for surgical intervention include neck pain, increased neck pressure, foreign body sensation, dysphonia, dyspnea, and dysphagia. However, it is essential to determine if these symptoms are likely due to a thyroid nodule or if they can be attributed to a secondary cause (eg, postnasal drip, vocal cord dysfunction, gastroesophageal reflux disease, or esophageal stricture).
If the findings are inconsistent with the clinical picture, secondary evaluation is prudent to avoid an unnecessary procedure.
Physical ExamPalpation of a thyroid nodule is an unreliable indicator of risk for malignancy. Palpation alone does not allow for detection of all nodules, particularly smaller ones, and specific characteristics are not discernible. Imaging studies are required to accurately evaluate a thyroid nodule and determine the most appropriate course of action.
Palpation can be used to evaluate for a larger and/or fixed nodule, thyroid gland/nodule tenderness, and cervical lymphadenopathy. Physical exam can also assess for signs of hypo- or hyperthyroidism, including abnormal pulse rate or blood pressure, tremor, hypo- or hyperreflexia, and integumentary abnormalities (eg, hair loss, abnormal skin temperature, and nail changes).
Continue for serologic evaluation >>
Serologic Evaluation
If a thyroid nodule is suspected on exam or found on imaging, assessment of thyroid function, via thyroid-stimulating hormone (TSH) measurement, is the recommended first step. If TSH is elevated, further evaluation for hypothyroidism is recommended, with testing for free thyroxine (T4) and antithyroid peroxidase (TPO) antibodies.4 If TSH is suppressed, further evaluation with free T4 and assessment for underlying causes of hyperthyroidism are indicated, including work-up for toxic nodular goiter.
Routine monitoring of serum calcitonin level is not recommended. However, if there is suspicion for medullary thyroid cancer—based on either US findings or family history—serologic screening for abnormal calcitonin level may be indicated.4,5
Felicia’s lab results include a TSH of 1.30 µIU/mL (reference range, 0.30-3.00 µIU/mL). Based on this finding, what (if any) further serologic testing is recommended? None: With normal TSH and no concerning family or personal history, additional laboratory evaluation is not indicated.
Imaging a Thyroid Nodule
Thyroid US is the most sensitive imaging study for evaluating thyroid nodule characteristics. Thyroid uptake and scan is not indicated unless TSH is suppressed and evaluation for toxic nodular goiter is needed. Additional imaging studies, such as CT or MRI, are not recommended for thyroid nodule evaluation.
Based on the thyroid US, what characteristics of Felicia’s nodule are suggestive of a benign nodule? Of a malignant nodule? (See Table 2.)
FNA of the left-sided dominant nodule is indicated, based on the US findings of a partially solid component and size > 1 cm. Unfortunately, FNA is nondiagnostic, because it yielded cystic fluid only with scant follicular cells for evaluation.
Continue to now what? >>
Now What?
While FNA most definitively distinguishes between benign and malignant nodules, the test is limited. An indeterminate, or nondiagnostic, finding occurs in 10% to 15% of cases and is more likely in nodules with a large cystic component.1
Even a benign finding on FNA of a larger nodule should be viewed with caution, since aspiration is unlikely to pinpoint small insidious malignant cells nestled among a larger collection of benign tissue.3 In many situations, a patient receives FNA results and asks, “What should we do now?”
Nondiagnostic nodules
When FNA is indeterminate, the next step depends on the characteristics of the nodule. For a solid nodule, repeat FNA is recommended.4,5 For nodules with repeatedly nondiagnostic FNAs, the American Academy of Clinical Endocrinologists and the American Thyroid Association recommend that a solid nodule be considered for surgical removal unless the nodule has “clearly favorable clinical and US features.”4,5
Surgical excision should be considered for cysts that recur, those that are larger (> 4 cm), and those that are repeatedly nondiagnostic on FNA. Personal and family history should be taken into account when nodules that are nondiagnostic on FNA demonstrate suspicious characteristics on US.6
An analysis by Renshaw determined that risk for malignancy in a nodule with a single nondiagnostic FNA was about 20%. For nodules that underwent repeat FNA, the risk was 0% for those that were again nondiagnostic. This significant difference led the author to conclude that “patients with two sequential nondiagnostic thyroid aspirates have a very low risk of malignancy.”7
Consider the time commitment, financial burden, and emotional cost for the patient of repeated evaluation with thyroid US and possibly FNA. In recurrent cases, the risks associated with surgery begin to be outweighed by the cost and burden of prolonged observation.
Benign nodules
With a biopsy-proven benign nodule, observation is recommended unless certain criteria are present: local neck compressive/obstructive symptoms that can be confidently attributed to a thyroid nodule; patient preference (eg, due to anxiety or aesthetics); or higher index of suspicion (eg, history of previous radiation exposure, progressive nodule growth, or suspicious characteristics on US).4,5
If surgical removal of a benign thyroid nodule is recommended, it is imperative to discuss the risks with patients. In addition to traditional surgery risks, thyroidectomy is associated with transient or permanent postoperative hypoparathyroidism, as well as vocal hoarseness or changes in vocal quality due to the proximity of the recurrent laryngeal nerve. Additionally, patients should be advised of the potential for surgical hypothyroidism with hemithyroidectomy and certain irreversible hypothyroidism with total thyroidectomy.
After a discussion of the risks and cost of observation versus surgery, an informed decision between provider and patient can ultimately be reached.
Would thyroidectomy be recommended for Felicia? After a thorough discussion, it is decided that surgery is not indicated at this time. Relevant factors include the benign thyroid US characteristics, lack of clinical neck compressive symptoms, and patient preference.
According to the American Thyroid Association guidelines, Felicia’s risk for malignancy for the nodule in question is < 3%, since it is a partially cystic nodule without any suspicious sonographic features. By foregoing surgery, Felicia will need repeated imaging studies and possibly repeat serologic studies and FNA in the future.
References
1. Stang MT, Carty SE. Recent developments in predicting thyroid malignancy. Curr Opin Oncol. 2008;21(1):11-17.
2. Hambleton C, Kandil E. Appropriate and accurate diagnosis of thyroid nodules: a review of thyroid fine-needle aspiration. Int J Clin Exp Med. 2013;6(6):413-422.
3. American Cancer Society. Thyroid cancer (2014). www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf. Accessed June 29, 2016.
4. Gharib H, Papini E, Garber J, et al; AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules—2016 Update. Endocrine Pract. 2016;22(suppl 1):1-60.
5. Haugen BR, Alexander EK, Bible KC, et al; The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26(1):1-133.
6. Yeung MJ, Serpell JW. Management of the solitary thyroid nodule. Oncologist. 2008; 13(2):105-112.
7. Renshaw A. Significance of repeatedly nondiagnostic thyroid fine-needle aspirations. Am J Clin Pathol. 2011;135(5):750-752.
A new-onset thyroid nodule, found on exam or incidentally on imaging, is a common presentation at primary care and specialist clinics. Palpable nodules are present in 4% to 7% of the population.1 However, more sensitive evaluation with thyroid ultrasound (US) suggests an incidence as high as 70%.2
According to the American Cancer Society, in 2015, there were approximately 62,450 new cases of thyroid cancer in the United States (with 2.5 times as many occurring in women as in men).3 In fact, thyroid cancer is the most rapidly increasing cancer in the United States—attributable in part to the increased use of thyroid US and incidental detection.3
The high prevalence of thyroid nodules makes appropriate evaluation and treatment crucial. This article, through a case study, explores the evaluation of a thyroid nodule and the recommendation for and against thyroidectomy.
Felicia, 49, presents to the endocrine clinic as a new patient with questions about multinodular goiter (MNG). She has been advised by ENT to have a left-sided dominant nodule surgically removed while under anesthesia during her upcoming chronic sinusitis surgery. Felicia would like to avoid thyroid surgery, if possible. Her most recent thyroid US, performed three months ago, showed a right lobe with multiple colloid nodules with inspissated colloid, the largest of which is 1.5 cm, and a 4-cm complex, solid, cystic nodule with inspissated colloid in the cystic spaces replacing the entire left thyroid lobe.
HistoryThe first step is establishing a history of the nodule(s) in question. Key questions are listed in Table 1. The onset and progression of a thyroid nodule must be determined; ideally, the provider should review any previous studies related to the thyroid gland. This will help determine if the nodule is new, if it has been evaluated in the past, and if it has changed significantly.
A thorough history can identify risk factors for malignancy, which include a personal history of cancer or radiation exposure, as well as a family history of thyroid cancer or malignant endocrine syndromes.
Felicia denies any family or personal medical history concerning for malignancy. She notes that she has two sisters with MNG. She denies any neck pain, compressive/obstructive symptoms, and hypo- or hyperthyroid symptoms.
She reports that she was found to have a goiter on exam and was subsequently diagnosed with MNG in 2008. Thyroid US showed a 2.3-cm complex, largely solid mass in the right mid-pole and a 3.3-cm largely cystic lesion in the left mid-pole. She was referred for right-sided fine-needle aspiration (FNA); results were consistent with benign colloid nodule. The left-sided nodule was not biopsied at that time, due to a largely cystic component.
Felicia underwent a follow-up US in 2011; it showed a 1.6-cm right mid-pole nodule with multiple nonspecific echogenic areas; a 1-cm benign-appearing nodule; and a 3.7-cm highly vascular heterogeneous mass with some colloid components with indeterminate component in the left lower and mid-pole. She reports that she did not follow up in 2011. Her next evaluation was the current thyroid US. She has never had FNA of the left-sided dominant nodule.
Continue for symptomatic vs asymptomatic thyroid nodules >>
Symptomatic vs Asymptomatic Thyroid NodulesEvaluation of a symptomatic thyroid nodule can help to determine the need for surgery, as well as assess the level of interference with a patient’s activities of daily living and the potential for functional abnormalities. However, both local neck and constitutional symptoms may be nonspecific and unrelated to the thyroid gland’s structure or function. Therefore, the provider should exercise caution in making recommendations based on reported symptoms alone.
Symptoms indicative of the need for surgical intervention include neck pain, increased neck pressure, foreign body sensation, dysphonia, dyspnea, and dysphagia. However, it is essential to determine if these symptoms are likely due to a thyroid nodule or if they can be attributed to a secondary cause (eg, postnasal drip, vocal cord dysfunction, gastroesophageal reflux disease, or esophageal stricture).
If the findings are inconsistent with the clinical picture, secondary evaluation is prudent to avoid an unnecessary procedure.
Physical ExamPalpation of a thyroid nodule is an unreliable indicator of risk for malignancy. Palpation alone does not allow for detection of all nodules, particularly smaller ones, and specific characteristics are not discernible. Imaging studies are required to accurately evaluate a thyroid nodule and determine the most appropriate course of action.
Palpation can be used to evaluate for a larger and/or fixed nodule, thyroid gland/nodule tenderness, and cervical lymphadenopathy. Physical exam can also assess for signs of hypo- or hyperthyroidism, including abnormal pulse rate or blood pressure, tremor, hypo- or hyperreflexia, and integumentary abnormalities (eg, hair loss, abnormal skin temperature, and nail changes).
Continue for serologic evaluation >>
Serologic Evaluation
If a thyroid nodule is suspected on exam or found on imaging, assessment of thyroid function, via thyroid-stimulating hormone (TSH) measurement, is the recommended first step. If TSH is elevated, further evaluation for hypothyroidism is recommended, with testing for free thyroxine (T4) and antithyroid peroxidase (TPO) antibodies.4 If TSH is suppressed, further evaluation with free T4 and assessment for underlying causes of hyperthyroidism are indicated, including work-up for toxic nodular goiter.
Routine monitoring of serum calcitonin level is not recommended. However, if there is suspicion for medullary thyroid cancer—based on either US findings or family history—serologic screening for abnormal calcitonin level may be indicated.4,5
Felicia’s lab results include a TSH of 1.30 µIU/mL (reference range, 0.30-3.00 µIU/mL). Based on this finding, what (if any) further serologic testing is recommended? None: With normal TSH and no concerning family or personal history, additional laboratory evaluation is not indicated.
Imaging a Thyroid Nodule
Thyroid US is the most sensitive imaging study for evaluating thyroid nodule characteristics. Thyroid uptake and scan is not indicated unless TSH is suppressed and evaluation for toxic nodular goiter is needed. Additional imaging studies, such as CT or MRI, are not recommended for thyroid nodule evaluation.
Based on the thyroid US, what characteristics of Felicia’s nodule are suggestive of a benign nodule? Of a malignant nodule? (See Table 2.)
FNA of the left-sided dominant nodule is indicated, based on the US findings of a partially solid component and size > 1 cm. Unfortunately, FNA is nondiagnostic, because it yielded cystic fluid only with scant follicular cells for evaluation.
Continue to now what? >>
Now What?
While FNA most definitively distinguishes between benign and malignant nodules, the test is limited. An indeterminate, or nondiagnostic, finding occurs in 10% to 15% of cases and is more likely in nodules with a large cystic component.1
Even a benign finding on FNA of a larger nodule should be viewed with caution, since aspiration is unlikely to pinpoint small insidious malignant cells nestled among a larger collection of benign tissue.3 In many situations, a patient receives FNA results and asks, “What should we do now?”
Nondiagnostic nodules
When FNA is indeterminate, the next step depends on the characteristics of the nodule. For a solid nodule, repeat FNA is recommended.4,5 For nodules with repeatedly nondiagnostic FNAs, the American Academy of Clinical Endocrinologists and the American Thyroid Association recommend that a solid nodule be considered for surgical removal unless the nodule has “clearly favorable clinical and US features.”4,5
Surgical excision should be considered for cysts that recur, those that are larger (> 4 cm), and those that are repeatedly nondiagnostic on FNA. Personal and family history should be taken into account when nodules that are nondiagnostic on FNA demonstrate suspicious characteristics on US.6
An analysis by Renshaw determined that risk for malignancy in a nodule with a single nondiagnostic FNA was about 20%. For nodules that underwent repeat FNA, the risk was 0% for those that were again nondiagnostic. This significant difference led the author to conclude that “patients with two sequential nondiagnostic thyroid aspirates have a very low risk of malignancy.”7
Consider the time commitment, financial burden, and emotional cost for the patient of repeated evaluation with thyroid US and possibly FNA. In recurrent cases, the risks associated with surgery begin to be outweighed by the cost and burden of prolonged observation.
Benign nodules
With a biopsy-proven benign nodule, observation is recommended unless certain criteria are present: local neck compressive/obstructive symptoms that can be confidently attributed to a thyroid nodule; patient preference (eg, due to anxiety or aesthetics); or higher index of suspicion (eg, history of previous radiation exposure, progressive nodule growth, or suspicious characteristics on US).4,5
If surgical removal of a benign thyroid nodule is recommended, it is imperative to discuss the risks with patients. In addition to traditional surgery risks, thyroidectomy is associated with transient or permanent postoperative hypoparathyroidism, as well as vocal hoarseness or changes in vocal quality due to the proximity of the recurrent laryngeal nerve. Additionally, patients should be advised of the potential for surgical hypothyroidism with hemithyroidectomy and certain irreversible hypothyroidism with total thyroidectomy.
After a discussion of the risks and cost of observation versus surgery, an informed decision between provider and patient can ultimately be reached.
Would thyroidectomy be recommended for Felicia? After a thorough discussion, it is decided that surgery is not indicated at this time. Relevant factors include the benign thyroid US characteristics, lack of clinical neck compressive symptoms, and patient preference.
According to the American Thyroid Association guidelines, Felicia’s risk for malignancy for the nodule in question is < 3%, since it is a partially cystic nodule without any suspicious sonographic features. By foregoing surgery, Felicia will need repeated imaging studies and possibly repeat serologic studies and FNA in the future.
References
1. Stang MT, Carty SE. Recent developments in predicting thyroid malignancy. Curr Opin Oncol. 2008;21(1):11-17.
2. Hambleton C, Kandil E. Appropriate and accurate diagnosis of thyroid nodules: a review of thyroid fine-needle aspiration. Int J Clin Exp Med. 2013;6(6):413-422.
3. American Cancer Society. Thyroid cancer (2014). www.cancer.org/acs/groups/cid/documents/webcontent/003144-pdf.pdf. Accessed June 29, 2016.
4. Gharib H, Papini E, Garber J, et al; AACE/AME/ETA Task Force on Thyroid Nodules. American Association of Clinical Endocrinologists, Associazione Medici Endocrinologi, and European Thyroid Association medical guidelines for clinical practice for the diagnosis and management of thyroid nodules—2016 Update. Endocrine Pract. 2016;22(suppl 1):1-60.
5. Haugen BR, Alexander EK, Bible KC, et al; The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016; 26(1):1-133.
6. Yeung MJ, Serpell JW. Management of the solitary thyroid nodule. Oncologist. 2008; 13(2):105-112.
7. Renshaw A. Significance of repeatedly nondiagnostic thyroid fine-needle aspirations. Am J Clin Pathol. 2011;135(5):750-752.