News
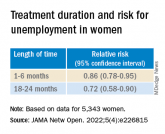
Adherence to ADHD meds may lower unemployment risk
- Author:
- Batya Swift Yasgur, MA, LSW
- Lsw
Among women in particular, longer treatment duration was associated with a lower risk of subsequent long-term unemployment.
News
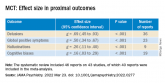
Metacognitive training an effective, durable treatment for schizophrenia
- Author:
- Batya Swift Yasgur, MA, LSW
- Lsw
MCT led to improvement in self-esteem and functioning, and all benefits were maintained up to 1 year post intervention.
News
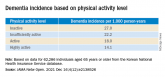
Even light physical activity linked to lower dementia risk
- Author:
- Batya Swift Yasgur, MA, LSW
- Lsw
“In older adults, an increased physical activity level, including a low amount of LPA, was associated with a...
News
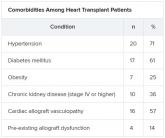
More fatalities in heart transplant patients with COVID-19
- Author:
- Batya Swift Yasgur, MA, LSW
A new study suggests a high risk for death if heart transplant patients contract COVID-19, which points to the...
News
New guidance to optimize antipsychotic treatment
- Author:
- Batya Swift Yasgur, MA, LSW
Patients receiving polypharmacy can benefit from TDM because some coprescribed medications can raise or lower antipsychotic blood levels.
News

Domestic violence amid COVID-19: Helping your patients from afar
- Author:
- Batya Swift Yasgur, MA, LSW
In the United States, 2,345 calls were placed to the National Domestic Violence Hotline during March 16–April 6, 2020.
News
New ‘atlas’ maps links between mental disorders, physical illnesses
- Author:
- Batya Swift Yasgur, MA, LSW
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke,” said Dr. John McGrath.
