Article

Skin Cancer Screening: The Paradox of Melanoma and Improved All-Cause Mortality
- Author:
- Binh T. Ngo, MD
In April 2023, the US Preventive Services Task Force (USPSTF) issued a controversial recommendation that the current evidence is insufficient to...
Article
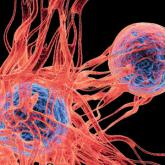
Gene Expression Profiling for Melanoma Prognosis: Going Beyond What We See With Our Eyes
- Author:
- Binh T. Ngo, MD
Gene expression panels have now been approved by numerous third-party insurers to help predict future clinical evolution of biopsied melanomas....
