Article
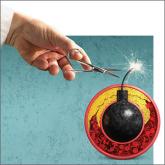
Translating AHA/ACC cholesterol guidelines into meaningful risk reduction
- Author:
- Cezary Wójcik, MD, PhD, FNLA
- Michael D. Shapiro, DO, FACC, FASPC, FNLA
The new recommendations detail refined, personalized lipid management and emphasize multiple levels of evidence. The result? Care is more complex...
