User login
Unmasked: How the COVID-19 Pandemic Exacerbates Disparities for People With Communication-Based Disabilities
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
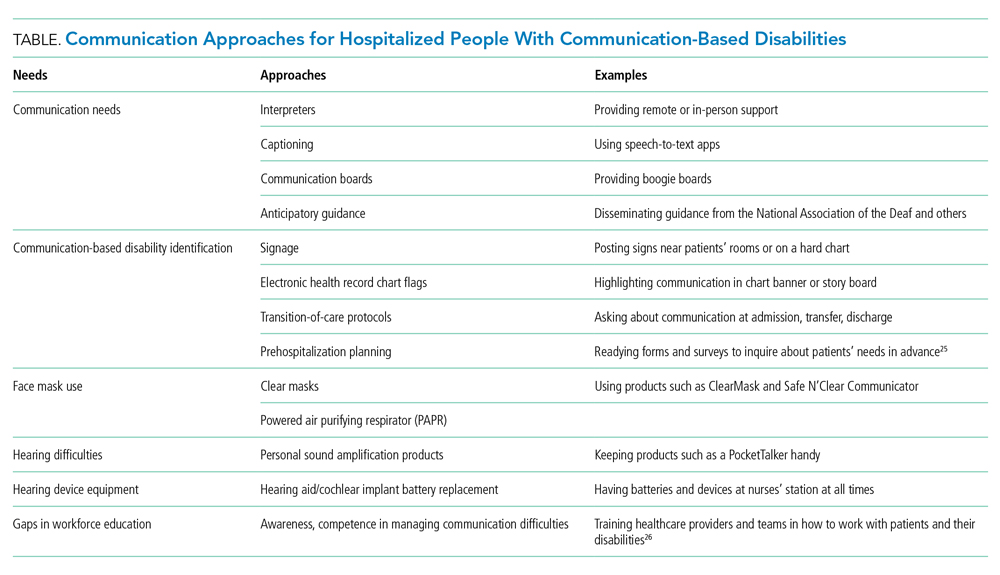
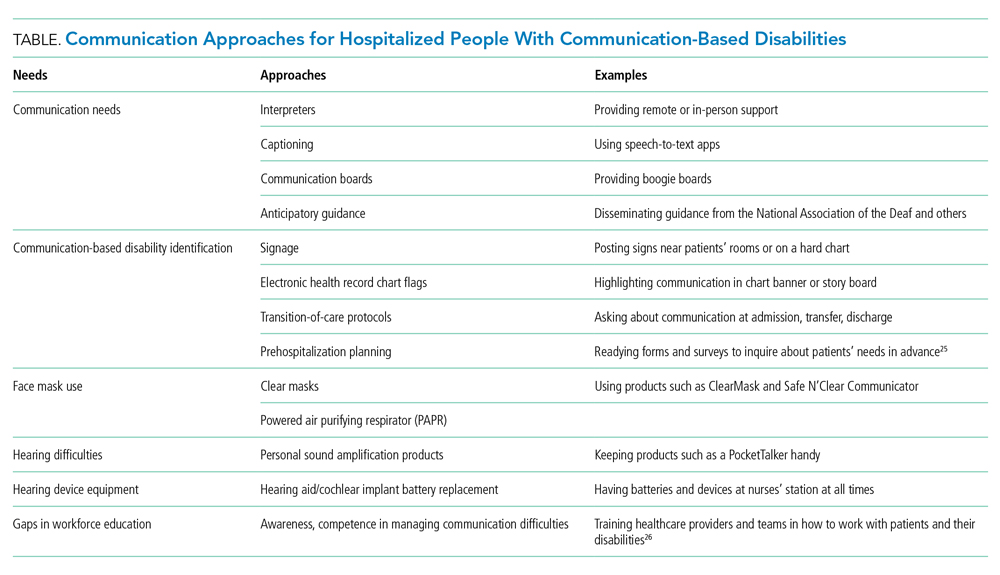
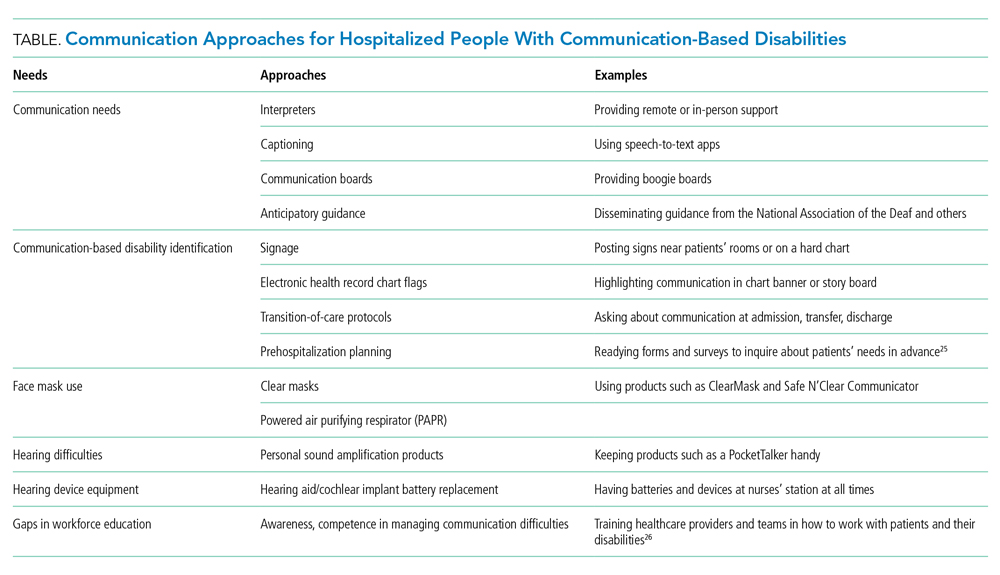
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
Adults with communication-based disabilities struggle with healthcare inequities,1-4 largely secondary to poor healthcare provider-patient communication. The prevalence of communication-based disabilities, which include speech, language, voice, and/or hearing disabilities, is relatively high yet difficult to ascertain. Ten percent of adults in the United States report having had a speech, language, or voice disability within the past year,5 and hearing loss also affects 17% of the US population.6 These individuals’ collective communication difficulties have been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic, with healthcare systems mandating personal protective equipment (PPE), including face masks, to ensure the safety of workers and patients. This change has placed patients with communication-based disabilities at even greater risk for communication breakdowns.7,8
Hospitals pose challenging communicative environments due to multiple factors (eg, noisy equipment alarms, harried healthcare teams spending less time with patients, PPE use obstructing faces and muffling sounds). Adverse communication among those with communication-based disabilities results in poorer healthcare outcomes, including higher rates of readmission and preventable adverse medical events, as well as lower healthcare satisfaction.7,9,10 Ineffective communication leads to reduced adherence, longer hospitalizations, and worse health outcomes in general.11-13 This is problematic because those with communication-based disabilities are more likely to require hospitalization due to higher rates of associated comorbidities, including frailty, cardiovascular disease, cognitive decline, and falls.4,14-16 Yet hospitals rarely screen and implement best practices to ensure effective and accessible communication for those with communication-based disabilities. The COVID-19 pandemic has exacerbated existing barriers, despite feasible solutions. Importantly, the Americans with Disabilities Act (ADA) remains in effect despite the pandemic. Therefore, hospitals should review existing policies and approaches to ensure adherence to ADA mandates. We address commonly encountered COVID-19-related communication barriers and recommend potential solutions.17
KEY COMMUNICATION BARRIERS
Limited Time or Support
Patients with communication-based disabilities may need more time than others to communicate their needs, values, and preferences effectively, whether due to slower articulation (eg, movement disorders) or communicating via an intermediary (eg, family member who understands them well) or an interpreter. Due to capacity or patient acuity issues, or even concerns about minimizing time in the room of a patient infected with COVID-19, hospital staff may inadvertently spend less time than needed to develop the necessary therapeutic relationships. This concern is magnified when restrictive visitor policies limit the availability of caregivers, such as loved ones, who assist at the bedside with communication.18
Universal Masking and Face Shields
Standard face masks, now required for all in-person encounters regardless of the patient’s COVID-19 status, obstruct the view of the lips and many facial expressions. Facial cues are an important form of nonverbal communication and are critical to conveying meaning in sign language. Face masks, particularly N95 respirators, substantially degrade speech perception.19 Masking increases the difficulty of acoustically and visually understanding patients who have disorders that decrease speech intelligibility, such as dysphonia, dysarthria, or
Interpreters
For deaf and hard-of-hearing people who use American Sign Language (ASL) as their preferred healthcare communication method, interpreters play a critical role in ensuring accessible healthcare communication. Signed language interpretation can occur in person or remotely by video. For in-person interpretation, interpreters must likewise wear PPE. The use of PPE, including face masks, can obscure many of the facial cues important to ASL grammar. Similarly, patients’ face masks can make it more challenging for interpreters to interpret effectively. With remote video interpretation, technological difficulties (eg, dropped WiFi connections) and the loss of environmental cues (eg, interpreter at a remote location unable to see or hear patient surroundings) often mar opportunities for accessible and effective communication. For the DeafBlind community, the use of remote video interpretation is not feasible. DeafBlind people rely on tactile forms of ASL, requiring interpreters’ physical touch throughout the communication encounter. This potentially increases COVID-19 transmission risk.
POTENTIAL OR IMPLEMENTED SOLUTIONS
While some of the solutions listed below also apply to communication in nonpandemic times, identifying high-risk patients and anticipatory planning for communication has become even more important during the COVID-19 outbreak.
Identification and Assessment of
Hospital staff should systematically review admission and transfer protocols to ensure every patient is asked about their communication preferences, necessary accommodations, and specific needs. Any communication needs or accommodation requests (eg, interpreters, communication boards) should be documented and flagged in highly visible areas of the electronic health record. These patients should be assessed regularly to ensure their communication needs are being met and documented throughout their hospital stay.
Assistive Communication Steps
Some steps can be performed in advance. Careful consideration should be given to healthcare providers’ ability to spend additional time with patients with communication-based disabilities. Even if providers are limited physically in the room, they can still work to optimize mindful, high-quality communication by calling into the patient’s room by phone or video. The additional time is important especially when establishing rapport with patients and identifying their preferred communication approaches, as well as engaging their support networks. Patients with communication-based disabilities and their support team often have expertise on their ideal communication strategies. Healthcare providers and staff should inquire about communication preferences. Patients should also be oriented to hospital team structure and members, which could include simple solutions such as legible name tags. Hearing aids, batteries, and other assistive technology should have designated places to prevent loss and ensure ongoing working status. In addition, nurse stations should have a communication toolbox that includes replacement batteries for hearing aids along with other assistive technology devices, such as a personal sound amplification product.
Communication Strategies
Healthcare teams should be trained and reminded to use patient-centered communication strategies, including assessing their comprehension of shared health information through teach-back principles. Strategies vary by patient and may require teams’ flexibility in meeting the patient’s needs and preferences. Examples include ensuring one has the patient’s attention and uses good eye contact. Using a projected “radio voice,” which emphasizes clarity and articulation rather than volume, is helpful for those with hearing loss. For some, meaningful gestures (eg, pointing to one’s own head when asking about headaches) can aid communication. Another strategy when having difficulty understanding patients with decreased speech intelligibility is to repeat the audible speech so that the patient only needs to repeat the inaudible portions that were missed. Patients should have secure access to personal assistive devices, such as hearing aids and even smartphones with communication apps (eg, speech-to-text apps) to facilitate interpersonal communication.
Clear Face Masks
Face masks with transparent windows have been developed. Deaf and hard of hearing people’s speech perception increases when speakers use transparent versus conventional masks. The Food and Drug Administration has approved two clear face masks as American Society for Testing Materials Level 1 (Table). These two masks have limited utility for high-risk situations, such as aerosolizing procedures; in such cases, a powered air purifying respirator with a clear viewing window will be needed instead. Notably, clear mask supply has lagged behind demand, creating limited mask availability during the pandemic; their use may need to be restricted to those working with patients with communication-based disabilities.
Tools for Communicating Within the Patient’s Room
Erasable whiteboards and communication boards are useful tools for simple exchanges as long as patients’ literacy and fluency are adequate. “PocketTalkers” or personalized sound amplification products may allow providers to speak into a microphone, providing amplified speech via a patient’s headphones. These amplification products are typically useful for those with mild to moderate hearing loss who are not using a hearing aid. Automatic speech recognition apps are device-based apps for converting speech to text. Speakers hold the device near the mouth to maximize accuracy while the patient reads the captions on their screen. With social distancing, lavalier microphones can increase text accuracy, but higher rates of error may still occur due to background noises or accents. For increased reliability and accuracy, Computer Access Realtime Translation stenographers can provide live speech to text on a computer screen from off-site via a computer or smartphone.
Tools for Isolation-Limited Communication
Team members can call an intermediary service to communicate with the patient via the patient’s smartphone or hospital-provided remote video interpreting service, depending on the patient’s preferred communication modality. For oral and spoken language, some services (Table) use remote stenographers to convert speech to text or sign language interpreters for those who use sign language. For both communication modes, smartphone-based videoconferencing may be beneficial while maintaining isolation precautions.
Interpreter Accessibility
Conceptualize interpreters as consulting healthcare team members. They should receive the same PPE training and monitoring as other healthcare workers. For patients using remote video interpretation, this technology needs to be optimized for best results. The room should be in a location with a strong Wi-Fi signal. Equipment should be consistently charged when not in use and rapidly accessible, even remaining in the patients’ room if possible. Healthcare teams need training to appropriately locate and set up the equipment with appropriate support from information technology staff.
Signage
Signage is useful to remind healthcare teams of the patients’ and/or caregivers’ communication-based disability. The most commonly used disability signage shows a line across an ear to indicate hearing loss (Appendix Figure).22 Appropriate signage use, even simple printed sheets documenting a communication issue, can remind healthcare team members of patients’ needs to ensure that communication is accessible and avoid misconceptions toward the patient (eg, noncompliance or cognitive issues). Chart banners, patient room doorways, and over the patients’ beds are good signage locations.
Systematic Noise Reduction
Consistent with previous calls to reduce inpatient noise,23 hospitals should systematically review and monitor protocols to reduce noise pollution. If intra-unit noise varies, patients relying on acoustic-based communication due to hearing loss or speech, language, or voice disability should be placed in quieter rooms.
Communication Concordance
Healthcare professionals and staff with disabilities are an increasingly recognized workforce segment,24 and often are experienced innovators in communicating effectively with patients with communication-based disabilities. Healthcare systems can explore whether they have healthcare team members, employees, disability resource professionals, and/or trainees with these backgrounds and, if they are available, recruit them into developing effective inpatient communication policies and processes.
CONCLUSION
People with communication disabilities experience significant healthcare disparities, now further exacerbated by COVID-19. As clinicians, staff and hospitals work to fuse safety with high-quality communication and care, we should capitalize on multipronged opportunities at the system and individual levels to identify barriers and ensure accessible and effective communication with patients who have communication-based disabilities.
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
1. McKee MM, Moreland C, Atcherson SR, Zazove P. Hearing loss: communicating with the patient who is deaf or hard of hearing. FP Essent. 2015;434:24-28.
2. Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communicating with medical providers. Disabil Rehabil Assist Technol. 2013;8(6):472-481. https://doi.org/10.3109/17483107.2012.746398
3. Steinberg AG, Barnett S, Meador HE, Wiggins EA, Zazove P. Health care system accessibility. experiences and perceptions of deaf people. J Gen Intern Med. 2006;21(3):260-266. https://doi.org/10.1111/j.1525-1497.2006.00340.x
4. Stransky ML, Jensen KM, Morris MA. Adults with communication disabilities experience poorer health and healthcare outcomes compared to persons without communication disabilities. J Gen Intern Med. 2018;33(12):2147-2155. https://doi.org/10.1007/s11606-018-4625-1
5. Morris MA, Meier SK, Griffin JM, Branda ME, Phelan SM. Prevalence and etiologies of adult communication disabilities in the United States: results from the 2012 National Health Interview Survey. Disabil Health J. 2016;9(1):140-144. https://doi.org/10.1016/j.dhjo.2015.07.004
6. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: National Health Interview Survey, 2012. Vital Health Stat. 2014(260):1-161.
7. Chang JE, Weinstein B, Chodosh J, Blustein J. Hospital readmission risk for patients with self-reported hearing loss and communication trouble. J Am Geriatr Soc. 2018;66(11):2227-2228. https://doi.org/10.1111/jgs.15545
8. McKee M, Moran C, Zazove P. Overcoming additional barriers to care for deaf and hard of hearing patients during COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;146(9):781-782. https://doi.org/10.1001/jamaoto.2020.1705
9. Bartlett G, Blais R, Tamblyn R, Clermont RJ, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555-1562. https://doi.org/10.1503/cmaj.070690
10. Hoffman JM, Yorkston KM, Shumway-Cook A, Ciol MA, Dudgeon BJ, Chan L. Effect of communication disability on satisfaction with health care: a survey of medicare beneficiaries. Am J Speech Lang Pathol. 2005;14(3):221-228. https://doi.org/10.1044/1058-0360(2005/022)
11. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(4):e94207. https://doi.org/10.1371/journal.pone.0094207
12. Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315-318. https://doi.org/10.1016/j.pec.2007.03.005
13. Street RL Jr, Makoul G, Arora NK, Epstein RM. How does communication heal? pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295-301. https://doi.org/10.1016/j.pec.2008.11.015
14. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013;309(22):2322-2324. https://doi.org/10.1001/jama.2013.5912
15. Lin FR, Yaffe K, Xia J, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293-299. https://doi.org/10.1001/jamainternmed.2013.1868
16. McKee MM, Stransky ML, Reichard A. Hearing loss and associated medical conditions among individuals 65 years and older. Disabil Health J. 2018;11(1):122-125. https://doi.org/10.1016/j.dhjo.2017.05.007
17. ADA requirements: effective communication. U.S. Department of Justice. January 31, 2014. Accessed February 12, 2021. https://www.ada.gov/effective-comm.htm
18. OCR resolves complaints after State of Connecticut and private hospital safeguard the rights of persons with disabilities to have reasonable access to support persons in hospital settings during COVID-19. Press Release. US Department of Health and Human Services; June 9, 2020. Accessed September 19, 2020. https://www.hhs.gov/about/news/2020/06/09/ocr-resolves-complaints-after-state-connecticut-private-hospital-safeguard-rights-persons.html
19. Goldin A, Weinstein B, Shiman N. How do medical masks degrade speech perception? The Hearing Review. April 1, 2020. Accessed September 30, 2020. https://www.hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception
20. Mendel LL, Gardino JA, Atcherson SR. Speech understanding using surgical masks: a problem in health care? J Am Acad Audiol. 2008;19(9):686-695. https://doi.org/10.3766/jaaa.19.9.4
21. Atcherson SR, Finley ET, McDowell BR, Watson C. More speech degradations and considerations in the search for transparent face coverings during the COVID-19 pandemic. American Academy of Audiology. November/December 2020. Accessed September 19, 2020. https://www.audiology.org/audiology-today-julyaugust-2020/online-feature-more-speech-degradations-and-considerations-search
22. Hearing Loss. Wikipedia. Accessed October 28, 2020. https://en.wikipedia.org/wiki/Hearing_loss
23. Kamdar BB, Martin JL, Needham DM. Noise and light pollution in the hospital: a call for action. J Hosp Med. 2017;12(10):861-862. https://doi.org/10.12788/jhm.2838
24. Meeks LM, Herzer K, Jain NR. Removing barriers and facilitating access: increasing the number of physicians with disabilities. Acad Med. 2018;93(4):540-543. https://doi.org/10.1097/acm.0000000000002112
25. Communication Access Plan (CAP): Instructions for Patients and Providers. Hearing Loss Association of America (HLAA). Accessed September 30, 2020. https://www.hearingloss.org/wp-content/uploads/HLAA_HC_CAP_Form_and_Instructions.pdf
26. How Do I Communicate with Doctors, Nurses, and Staff at the Hospital During COVID-19? Hearing Loss Association of America (HLAA). May 8, 2020. Accessed September 30, 2020. https://www.hearingloss.org/communication-access-recommendations-hospitals-covid-19/
© 2021 Society of Hospital Medicine