User login
Beyond a Purple Journal: Improving Hospital-Based Addiction Care
Rosa* was one of my first patients as an intern rotating at the county hospital. Her marriage had disintegrated years earlier. To cope with depression, she hid a daily ritual of orange juice and vodka from her children. She worked as a cashier, until nausea and fatigue overwhelmed her.
The first time I met her she sat on the gurney: petite, tanned, and pregnant. Then I saw her yellow eyes and revised: temporal wasting, jaundiced, and swollen with ascites. Rosa didn’t know that alcohol could cause liver disease. Without insurance or access to primary care, her untreated alcohol use disorder (AUD) and depression had snowballed for years.
Midway through my intern year, I’d taken care of many people with AUD. However, I’d barely learned anything about it as a medical student, though we’d spent weeks studying esoteric diseases, that now––9 years after medical school––I still have not encountered.
Among the 28.3 million individuals in the United States with AUD, only 1% receive medication treatment.1 In the United States, unhealthy alcohol use accounts for more than 95,000 deaths each year.2 This number likely under-captures alcohol-related mortality and is higher now given recent reports of increasing alcohol-related deaths and prevalence of unhealthy alcohol use, especially among women, younger age groups, and marginalized populations.3-5
Rosa had alcohol-related hepatitis, which can cause severe inflammation and liver failure and quickly lead to death. As her liver failure progressed, I asked the gastroenterologists, “What other treatments can we offer? Is she a liver transplant candidate?” “Nothing” and “No” they answered.
Later, I emailed the hepatologist and transplant surgeon begging them to reevaluate her transplantation candidacy, but they told me there was no exception to the institution’s 6-month sobriety rule.
Maintaining a 6-month sobriety period is not an evidence-based criterion for transplantation. However, 50% of transplant centers do not perform transplantation prior to 6 months of alcohol abstinence for alcohol-related hepatitis due to concern for return to drinking after transplant.6 This practice may promote bias in patient selection for transplantation. A recent study found that individuals with alcohol-related liver disease transplanted before 6 months of abstinence had similar rates of survival and return to drinking compared to those who abstained from alcohol for 6 months and participated in AUD treatment before transplantation.7
There are other liver transplant practices that result in inequities for individuals with substance use disorders (SUD). Some liver transplant centers consider being on a medication for opioid use disorder a contraindication for transplantation—even if the individual is in recovery and abstaining from substances.8 Others mandate that individuals with alcohol-related liver disease attend Alcoholics Anonymous (AA) meetings prior to transplant. While mutual help groups, including AA, may benefit some individuals, different approaches work for different people.9 Other psychosocial interventions (eg, cognitive-behavioral therapy, contingency management, and residential treatment) and medications also help individuals reduce or stop drinking. Some meet their goals without any treatment. Addiction care works best when it respects autonomy and meets individuals where they are by allowing them to decide among options.
While organ allocations are a crystalized example of inequities in addiction care, they are also ethically complex. Many individuals—with and without SUD—die on waiting lists and must meet stringent transplantation criteria. However, we can at least remove the unnecessary biases that compound inequities in care people with SUD already face.
As Rosa’s liver succumbed, her kidneys failed too, and she required dialysis. She sensed what was coming. “I want everything…for now. I need to take care of my children.” I, too, wanted Rosa to live and see her youngest start kindergarten.
A few days before her discharge, I walked to the pharmacy and bought a purple journal. In a rare moment, I found Rosa alone in her room, without her ex-husband, sister, and mother, who rarely left her bedside. Together, we called AA and explored whether she could start participating in phone meetings from the hospital. I explained that one way to document a commitment to sobriety, as the transplant center’s rules dictated, was to attend and document AA meetings in this notebook. “In 5 months, you will be a liver transplant candidate,” I remember saying, wishing it to fruition.
I became Rosa’s primary care physician and saw her in clinic. Over the next few weeks, her skin took on an ashen tone. Sleep escaped her and her thoughts and speech blurred. Her walk slowed and she needed a wheelchair. The quiet fierceness that had defined her dissipated as encephalopathy took over. But until our last visit, she brought her purple journal, tracking the AA meetings she’d attended. Dialysis became intolerable, but not before Rosa made care arrangements for her girls. When that happened, she stopped dialysis and went to Mexico, where she died in her sleep after saying good-bye to her father.
Earlier access to healthcare and effective depression and AUD treatment could have saved Rosa’s life. While it was too late for her, as hospitalists we care for many others with substance-related complications and may miss opportunities to discuss and offer evidence-based addiction treatment. For example, we initiate the most up-to-date management for a patient’s gastrointestinal bleed but may leave the alcohol discussion for someone else. It is similar for other SUD: we treat cellulitis, epidural abscesses, bacteremia, chronic obstructive pulmonary disease, heart failure exacerbations, and other complications of SUD without addressing the root cause of the hospitalization—other than to prescribe abstinence from substance use or, at our worst, scold individuals for continuing to use.
But what can we offer? Most healthcare professionals still do not receive addiction education during training. Without tools, we enact temporizing measures, until patients return to the hospital or die.
In addition to increasing alcohol-related morbidity, there have also been increases in drug-related overdoses, fueled by COVID-19, synthetic opioids like fentanyl, and stimulants.10 In the 12-month period ending April 2021, more than 100,000 individuals died of drug-related overdoses, the highest number of deaths ever recorded in a year.11 Despite this, most healthcare systems remain unequipped to provide addiction services during hospitalization due to inadequate training, stigma, and lack of systems-based care.
Hospitalists and healthcare systems cannot be bystanders amid our worsening addiction crisis. We must empower clinicians with addiction education and ensure health systems offer evidence-based SUD services.
Educational efforts can close the knowledge gaps for both medical students and hospitalists. Medical schools should include foundational curricular content in screening, assessing, diagnosing, and treating SUD in alignment with standards set by the Liaison Committee on Medical Education, which accredits US medical schools. Residency programs can offer educational conferences, cased-based discussions, and addiction medicine rotations. Hospitalists can participate in educational didactics and review evidence-based addiction guidelines.12,13 While the focus here is on hospitalists, clinicians across practice settings and specialties will encounter patients with SUD, and all need to be well-versed in the diagnosis and treatment of addiction given the all-hands-on deck approach necessary amidst our worsening addiction crisis.
With one in nine hospitalizations involving individuals with SUD, and this number quickly rising, and with an annual cost to US hospitals of $13.2 billion, healthcare system leaders must invest in addiction care.14,15 Hospital-based addiction services could pay for themselves and save healthcare systems money while improving the patient and clinician experience.16One way to implement hospital-based addiction care is through an addiction consult team (ACT).17 While ACT compositions vary, most are interprofessional, offer evidence-based addiction treatment, and connect patients to community care.18 Our hospital’s ACT has nurses, patient navigators, and physicians who assess, diagnose, and treat SUD, and arrange follow-up addiction care.19 In addition to caring for individual patients, our ACT has led systems change. For example, we created order sets to guide clinicians, added medications to our hospital formulary to ensure access to evidence-based addiction treatment, and partnered with community stakeholders to streamline care transitions and access to psychosocial and medication treatment. Our team also worked with hospital leadership, nursing, and a syringe service program to integrate hospital harm reduction education and supply provision. Additionally, we are building capacity among staff, trainees, and clinicians through education and systems changes.
In hospitals without an ACT, leadership can finance SUD champions and integrate them into policy-level decision-making to implement best practices in addiction care and lead hospital-wide educational efforts. This will transform hospital culture and improve care as all clinicians develop essential addiction skills.
Addiction champions and ACTs could also advocate for equitable practices for patients with SUD to reduce the stigma that both prevents patients from seeking care and results in self-discharges.20 For example, with interprofessional support, we revised our in-hospital substance use policy. It previously entailed hospital security responding to substance use concerns, which unintentionally harmed patients and perpetuated stigma. Our revised policy ensures we offer medications for cravings and withdrawal, adequate pain management, and other services that address patients’ reasons for in-hospital substance use.
With the increasing prevalence of SUD among hospitalized patients, escalating substance-related deaths, rising healthcare costs, and the impact of addiction on health and well-being, addiction care, including ACTs and champions, must be adequately funded. However, sustainable financing remains a challenge.18
Caring for Rosa and others with SUD sparked my desire to learn about addiction, obtain addiction medicine board certification as a practicing hospitalist, and create an ACT that offers evidence-based addiction treatment. While much remains to be done, by collaborating with addiction champions and engaging hospital leadership, we have transformed our hospital’s approach to substance use care.
With the knowledge and resources I now have as an addiction medicine physician, I reimagine the possibilities for patients like Rosa.
Rosa died when living was possible.
*Name has been changed for patient privacy.
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. HHS Publication No. PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Accessed December 1, 2021. www.samhsa.gov/data/
2. Centers for Disease Control and Prevention. Alcohol and public health: alcohol-related disease impact (ARDI) application, 2013. Average for United States 2006–2010 alcohol-attributable deaths due to excessive alcohol use. Accessed December 1, 2021. www.cdc.gov/ARDI
3. Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Netw Open. 2020;3(2):e1921451. https://doi.org/ 10.1001/jamanetworkopen.2019.21451
4. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161 https://doi.org/10.1001/jamapsychiatry.2017.2161
5. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the covid-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. https://doi.org/10.1001/jamanetworkopen.2020.22942
6. Bangaru S, Pedersen MR, Macconmara MP, Singal AG, Mufti AR. Survey of liver transplantation practices for severe acute alcoholic hepatitis. Liver Transpl. 2018;24(10):1357-1362. https://doi.org/10.1002/lt.25285
7. Herrick-Reynolds KM, Punchhi G, Greenberg RS, et al. Evaluation of early vs standard liver transplant for alcohol-associated liver disease. JAMA Surg. 2021;156(11):1026-1034. https://doi.org/10.1001/jamasurg.2021.3748
8. Fleming JN, Lai JC, Te HS, Said A, Spengler EK, Rogal SS. Opioid and opioid substitution therapy in liver transplant candidates: A survey of center policies and practices. Clin Transplant. 2017;31(12):e13119. https://doi.org/10.1111/ctr.13119
9. Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev. 2018;12(12):CD009269. https://doi.org/10.1002/14651858.CD009269.pub4
10. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. https://doi.org/10.15585/mmwr.mm7006a4
11. Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. Accessed November 18, 2021. www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
12. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
13. California Bridge Program. Tools: Treat substance use disorders from the acute care setting. Accessed August 20, 2021. https://cabridge.org/tools
14. Peterson C, Li M, Xu L, Mikosz CA, Luo F. Assessment of annual cost of substance use disorder in US hospitals. JAMA Netw Open. 2021;4(3):e210242. https://doi.org/10.1001/jamanetworkopen.2021.0242
15. Suen LW, Makam AN, Snyder HR, et al. National prevalence of alcohol and other substance use disorders among emergency department visits and hospitalizations: NHAMCS 2014-2018. J Gen Intern Med. 2021;13:1-9. https://doi.org/10.1007/s11606-021-07069-w
16. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: Qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993
17. Priest KC, McCarty D. Making the business case for an addiction medicine consult service: a qualitative analysis. BMC Health Services Research. 2019;19(1):822. https://doi.org/10.1186/s12913-019-4670-4
18. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496
19. Martin M, Snyder HR, Coffa D, et al. Time to ACT: launching an Addiction Care Team (ACT) in an urban safety-net health system. BMJ Open Qual. 2021;10(1):e001111. https://doi.org/10.1136/bmjoq-2020-001111
20. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abus. 2020;41(4):519-525. https://doi.org/10.1080/08897077.2019.1671942
Rosa* was one of my first patients as an intern rotating at the county hospital. Her marriage had disintegrated years earlier. To cope with depression, she hid a daily ritual of orange juice and vodka from her children. She worked as a cashier, until nausea and fatigue overwhelmed her.
The first time I met her she sat on the gurney: petite, tanned, and pregnant. Then I saw her yellow eyes and revised: temporal wasting, jaundiced, and swollen with ascites. Rosa didn’t know that alcohol could cause liver disease. Without insurance or access to primary care, her untreated alcohol use disorder (AUD) and depression had snowballed for years.
Midway through my intern year, I’d taken care of many people with AUD. However, I’d barely learned anything about it as a medical student, though we’d spent weeks studying esoteric diseases, that now––9 years after medical school––I still have not encountered.
Among the 28.3 million individuals in the United States with AUD, only 1% receive medication treatment.1 In the United States, unhealthy alcohol use accounts for more than 95,000 deaths each year.2 This number likely under-captures alcohol-related mortality and is higher now given recent reports of increasing alcohol-related deaths and prevalence of unhealthy alcohol use, especially among women, younger age groups, and marginalized populations.3-5
Rosa had alcohol-related hepatitis, which can cause severe inflammation and liver failure and quickly lead to death. As her liver failure progressed, I asked the gastroenterologists, “What other treatments can we offer? Is she a liver transplant candidate?” “Nothing” and “No” they answered.
Later, I emailed the hepatologist and transplant surgeon begging them to reevaluate her transplantation candidacy, but they told me there was no exception to the institution’s 6-month sobriety rule.
Maintaining a 6-month sobriety period is not an evidence-based criterion for transplantation. However, 50% of transplant centers do not perform transplantation prior to 6 months of alcohol abstinence for alcohol-related hepatitis due to concern for return to drinking after transplant.6 This practice may promote bias in patient selection for transplantation. A recent study found that individuals with alcohol-related liver disease transplanted before 6 months of abstinence had similar rates of survival and return to drinking compared to those who abstained from alcohol for 6 months and participated in AUD treatment before transplantation.7
There are other liver transplant practices that result in inequities for individuals with substance use disorders (SUD). Some liver transplant centers consider being on a medication for opioid use disorder a contraindication for transplantation—even if the individual is in recovery and abstaining from substances.8 Others mandate that individuals with alcohol-related liver disease attend Alcoholics Anonymous (AA) meetings prior to transplant. While mutual help groups, including AA, may benefit some individuals, different approaches work for different people.9 Other psychosocial interventions (eg, cognitive-behavioral therapy, contingency management, and residential treatment) and medications also help individuals reduce or stop drinking. Some meet their goals without any treatment. Addiction care works best when it respects autonomy and meets individuals where they are by allowing them to decide among options.
While organ allocations are a crystalized example of inequities in addiction care, they are also ethically complex. Many individuals—with and without SUD—die on waiting lists and must meet stringent transplantation criteria. However, we can at least remove the unnecessary biases that compound inequities in care people with SUD already face.
As Rosa’s liver succumbed, her kidneys failed too, and she required dialysis. She sensed what was coming. “I want everything…for now. I need to take care of my children.” I, too, wanted Rosa to live and see her youngest start kindergarten.
A few days before her discharge, I walked to the pharmacy and bought a purple journal. In a rare moment, I found Rosa alone in her room, without her ex-husband, sister, and mother, who rarely left her bedside. Together, we called AA and explored whether she could start participating in phone meetings from the hospital. I explained that one way to document a commitment to sobriety, as the transplant center’s rules dictated, was to attend and document AA meetings in this notebook. “In 5 months, you will be a liver transplant candidate,” I remember saying, wishing it to fruition.
I became Rosa’s primary care physician and saw her in clinic. Over the next few weeks, her skin took on an ashen tone. Sleep escaped her and her thoughts and speech blurred. Her walk slowed and she needed a wheelchair. The quiet fierceness that had defined her dissipated as encephalopathy took over. But until our last visit, she brought her purple journal, tracking the AA meetings she’d attended. Dialysis became intolerable, but not before Rosa made care arrangements for her girls. When that happened, she stopped dialysis and went to Mexico, where she died in her sleep after saying good-bye to her father.
Earlier access to healthcare and effective depression and AUD treatment could have saved Rosa’s life. While it was too late for her, as hospitalists we care for many others with substance-related complications and may miss opportunities to discuss and offer evidence-based addiction treatment. For example, we initiate the most up-to-date management for a patient’s gastrointestinal bleed but may leave the alcohol discussion for someone else. It is similar for other SUD: we treat cellulitis, epidural abscesses, bacteremia, chronic obstructive pulmonary disease, heart failure exacerbations, and other complications of SUD without addressing the root cause of the hospitalization—other than to prescribe abstinence from substance use or, at our worst, scold individuals for continuing to use.
But what can we offer? Most healthcare professionals still do not receive addiction education during training. Without tools, we enact temporizing measures, until patients return to the hospital or die.
In addition to increasing alcohol-related morbidity, there have also been increases in drug-related overdoses, fueled by COVID-19, synthetic opioids like fentanyl, and stimulants.10 In the 12-month period ending April 2021, more than 100,000 individuals died of drug-related overdoses, the highest number of deaths ever recorded in a year.11 Despite this, most healthcare systems remain unequipped to provide addiction services during hospitalization due to inadequate training, stigma, and lack of systems-based care.
Hospitalists and healthcare systems cannot be bystanders amid our worsening addiction crisis. We must empower clinicians with addiction education and ensure health systems offer evidence-based SUD services.
Educational efforts can close the knowledge gaps for both medical students and hospitalists. Medical schools should include foundational curricular content in screening, assessing, diagnosing, and treating SUD in alignment with standards set by the Liaison Committee on Medical Education, which accredits US medical schools. Residency programs can offer educational conferences, cased-based discussions, and addiction medicine rotations. Hospitalists can participate in educational didactics and review evidence-based addiction guidelines.12,13 While the focus here is on hospitalists, clinicians across practice settings and specialties will encounter patients with SUD, and all need to be well-versed in the diagnosis and treatment of addiction given the all-hands-on deck approach necessary amidst our worsening addiction crisis.
With one in nine hospitalizations involving individuals with SUD, and this number quickly rising, and with an annual cost to US hospitals of $13.2 billion, healthcare system leaders must invest in addiction care.14,15 Hospital-based addiction services could pay for themselves and save healthcare systems money while improving the patient and clinician experience.16One way to implement hospital-based addiction care is through an addiction consult team (ACT).17 While ACT compositions vary, most are interprofessional, offer evidence-based addiction treatment, and connect patients to community care.18 Our hospital’s ACT has nurses, patient navigators, and physicians who assess, diagnose, and treat SUD, and arrange follow-up addiction care.19 In addition to caring for individual patients, our ACT has led systems change. For example, we created order sets to guide clinicians, added medications to our hospital formulary to ensure access to evidence-based addiction treatment, and partnered with community stakeholders to streamline care transitions and access to psychosocial and medication treatment. Our team also worked with hospital leadership, nursing, and a syringe service program to integrate hospital harm reduction education and supply provision. Additionally, we are building capacity among staff, trainees, and clinicians through education and systems changes.
In hospitals without an ACT, leadership can finance SUD champions and integrate them into policy-level decision-making to implement best practices in addiction care and lead hospital-wide educational efforts. This will transform hospital culture and improve care as all clinicians develop essential addiction skills.
Addiction champions and ACTs could also advocate for equitable practices for patients with SUD to reduce the stigma that both prevents patients from seeking care and results in self-discharges.20 For example, with interprofessional support, we revised our in-hospital substance use policy. It previously entailed hospital security responding to substance use concerns, which unintentionally harmed patients and perpetuated stigma. Our revised policy ensures we offer medications for cravings and withdrawal, adequate pain management, and other services that address patients’ reasons for in-hospital substance use.
With the increasing prevalence of SUD among hospitalized patients, escalating substance-related deaths, rising healthcare costs, and the impact of addiction on health and well-being, addiction care, including ACTs and champions, must be adequately funded. However, sustainable financing remains a challenge.18
Caring for Rosa and others with SUD sparked my desire to learn about addiction, obtain addiction medicine board certification as a practicing hospitalist, and create an ACT that offers evidence-based addiction treatment. While much remains to be done, by collaborating with addiction champions and engaging hospital leadership, we have transformed our hospital’s approach to substance use care.
With the knowledge and resources I now have as an addiction medicine physician, I reimagine the possibilities for patients like Rosa.
Rosa died when living was possible.
*Name has been changed for patient privacy.
Rosa* was one of my first patients as an intern rotating at the county hospital. Her marriage had disintegrated years earlier. To cope with depression, she hid a daily ritual of orange juice and vodka from her children. She worked as a cashier, until nausea and fatigue overwhelmed her.
The first time I met her she sat on the gurney: petite, tanned, and pregnant. Then I saw her yellow eyes and revised: temporal wasting, jaundiced, and swollen with ascites. Rosa didn’t know that alcohol could cause liver disease. Without insurance or access to primary care, her untreated alcohol use disorder (AUD) and depression had snowballed for years.
Midway through my intern year, I’d taken care of many people with AUD. However, I’d barely learned anything about it as a medical student, though we’d spent weeks studying esoteric diseases, that now––9 years after medical school––I still have not encountered.
Among the 28.3 million individuals in the United States with AUD, only 1% receive medication treatment.1 In the United States, unhealthy alcohol use accounts for more than 95,000 deaths each year.2 This number likely under-captures alcohol-related mortality and is higher now given recent reports of increasing alcohol-related deaths and prevalence of unhealthy alcohol use, especially among women, younger age groups, and marginalized populations.3-5
Rosa had alcohol-related hepatitis, which can cause severe inflammation and liver failure and quickly lead to death. As her liver failure progressed, I asked the gastroenterologists, “What other treatments can we offer? Is she a liver transplant candidate?” “Nothing” and “No” they answered.
Later, I emailed the hepatologist and transplant surgeon begging them to reevaluate her transplantation candidacy, but they told me there was no exception to the institution’s 6-month sobriety rule.
Maintaining a 6-month sobriety period is not an evidence-based criterion for transplantation. However, 50% of transplant centers do not perform transplantation prior to 6 months of alcohol abstinence for alcohol-related hepatitis due to concern for return to drinking after transplant.6 This practice may promote bias in patient selection for transplantation. A recent study found that individuals with alcohol-related liver disease transplanted before 6 months of abstinence had similar rates of survival and return to drinking compared to those who abstained from alcohol for 6 months and participated in AUD treatment before transplantation.7
There are other liver transplant practices that result in inequities for individuals with substance use disorders (SUD). Some liver transplant centers consider being on a medication for opioid use disorder a contraindication for transplantation—even if the individual is in recovery and abstaining from substances.8 Others mandate that individuals with alcohol-related liver disease attend Alcoholics Anonymous (AA) meetings prior to transplant. While mutual help groups, including AA, may benefit some individuals, different approaches work for different people.9 Other psychosocial interventions (eg, cognitive-behavioral therapy, contingency management, and residential treatment) and medications also help individuals reduce or stop drinking. Some meet their goals without any treatment. Addiction care works best when it respects autonomy and meets individuals where they are by allowing them to decide among options.
While organ allocations are a crystalized example of inequities in addiction care, they are also ethically complex. Many individuals—with and without SUD—die on waiting lists and must meet stringent transplantation criteria. However, we can at least remove the unnecessary biases that compound inequities in care people with SUD already face.
As Rosa’s liver succumbed, her kidneys failed too, and she required dialysis. She sensed what was coming. “I want everything…for now. I need to take care of my children.” I, too, wanted Rosa to live and see her youngest start kindergarten.
A few days before her discharge, I walked to the pharmacy and bought a purple journal. In a rare moment, I found Rosa alone in her room, without her ex-husband, sister, and mother, who rarely left her bedside. Together, we called AA and explored whether she could start participating in phone meetings from the hospital. I explained that one way to document a commitment to sobriety, as the transplant center’s rules dictated, was to attend and document AA meetings in this notebook. “In 5 months, you will be a liver transplant candidate,” I remember saying, wishing it to fruition.
I became Rosa’s primary care physician and saw her in clinic. Over the next few weeks, her skin took on an ashen tone. Sleep escaped her and her thoughts and speech blurred. Her walk slowed and she needed a wheelchair. The quiet fierceness that had defined her dissipated as encephalopathy took over. But until our last visit, she brought her purple journal, tracking the AA meetings she’d attended. Dialysis became intolerable, but not before Rosa made care arrangements for her girls. When that happened, she stopped dialysis and went to Mexico, where she died in her sleep after saying good-bye to her father.
Earlier access to healthcare and effective depression and AUD treatment could have saved Rosa’s life. While it was too late for her, as hospitalists we care for many others with substance-related complications and may miss opportunities to discuss and offer evidence-based addiction treatment. For example, we initiate the most up-to-date management for a patient’s gastrointestinal bleed but may leave the alcohol discussion for someone else. It is similar for other SUD: we treat cellulitis, epidural abscesses, bacteremia, chronic obstructive pulmonary disease, heart failure exacerbations, and other complications of SUD without addressing the root cause of the hospitalization—other than to prescribe abstinence from substance use or, at our worst, scold individuals for continuing to use.
But what can we offer? Most healthcare professionals still do not receive addiction education during training. Without tools, we enact temporizing measures, until patients return to the hospital or die.
In addition to increasing alcohol-related morbidity, there have also been increases in drug-related overdoses, fueled by COVID-19, synthetic opioids like fentanyl, and stimulants.10 In the 12-month period ending April 2021, more than 100,000 individuals died of drug-related overdoses, the highest number of deaths ever recorded in a year.11 Despite this, most healthcare systems remain unequipped to provide addiction services during hospitalization due to inadequate training, stigma, and lack of systems-based care.
Hospitalists and healthcare systems cannot be bystanders amid our worsening addiction crisis. We must empower clinicians with addiction education and ensure health systems offer evidence-based SUD services.
Educational efforts can close the knowledge gaps for both medical students and hospitalists. Medical schools should include foundational curricular content in screening, assessing, diagnosing, and treating SUD in alignment with standards set by the Liaison Committee on Medical Education, which accredits US medical schools. Residency programs can offer educational conferences, cased-based discussions, and addiction medicine rotations. Hospitalists can participate in educational didactics and review evidence-based addiction guidelines.12,13 While the focus here is on hospitalists, clinicians across practice settings and specialties will encounter patients with SUD, and all need to be well-versed in the diagnosis and treatment of addiction given the all-hands-on deck approach necessary amidst our worsening addiction crisis.
With one in nine hospitalizations involving individuals with SUD, and this number quickly rising, and with an annual cost to US hospitals of $13.2 billion, healthcare system leaders must invest in addiction care.14,15 Hospital-based addiction services could pay for themselves and save healthcare systems money while improving the patient and clinician experience.16One way to implement hospital-based addiction care is through an addiction consult team (ACT).17 While ACT compositions vary, most are interprofessional, offer evidence-based addiction treatment, and connect patients to community care.18 Our hospital’s ACT has nurses, patient navigators, and physicians who assess, diagnose, and treat SUD, and arrange follow-up addiction care.19 In addition to caring for individual patients, our ACT has led systems change. For example, we created order sets to guide clinicians, added medications to our hospital formulary to ensure access to evidence-based addiction treatment, and partnered with community stakeholders to streamline care transitions and access to psychosocial and medication treatment. Our team also worked with hospital leadership, nursing, and a syringe service program to integrate hospital harm reduction education and supply provision. Additionally, we are building capacity among staff, trainees, and clinicians through education and systems changes.
In hospitals without an ACT, leadership can finance SUD champions and integrate them into policy-level decision-making to implement best practices in addiction care and lead hospital-wide educational efforts. This will transform hospital culture and improve care as all clinicians develop essential addiction skills.
Addiction champions and ACTs could also advocate for equitable practices for patients with SUD to reduce the stigma that both prevents patients from seeking care and results in self-discharges.20 For example, with interprofessional support, we revised our in-hospital substance use policy. It previously entailed hospital security responding to substance use concerns, which unintentionally harmed patients and perpetuated stigma. Our revised policy ensures we offer medications for cravings and withdrawal, adequate pain management, and other services that address patients’ reasons for in-hospital substance use.
With the increasing prevalence of SUD among hospitalized patients, escalating substance-related deaths, rising healthcare costs, and the impact of addiction on health and well-being, addiction care, including ACTs and champions, must be adequately funded. However, sustainable financing remains a challenge.18
Caring for Rosa and others with SUD sparked my desire to learn about addiction, obtain addiction medicine board certification as a practicing hospitalist, and create an ACT that offers evidence-based addiction treatment. While much remains to be done, by collaborating with addiction champions and engaging hospital leadership, we have transformed our hospital’s approach to substance use care.
With the knowledge and resources I now have as an addiction medicine physician, I reimagine the possibilities for patients like Rosa.
Rosa died when living was possible.
*Name has been changed for patient privacy.
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. HHS Publication No. PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Accessed December 1, 2021. www.samhsa.gov/data/
2. Centers for Disease Control and Prevention. Alcohol and public health: alcohol-related disease impact (ARDI) application, 2013. Average for United States 2006–2010 alcohol-attributable deaths due to excessive alcohol use. Accessed December 1, 2021. www.cdc.gov/ARDI
3. Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Netw Open. 2020;3(2):e1921451. https://doi.org/ 10.1001/jamanetworkopen.2019.21451
4. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161 https://doi.org/10.1001/jamapsychiatry.2017.2161
5. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the covid-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. https://doi.org/10.1001/jamanetworkopen.2020.22942
6. Bangaru S, Pedersen MR, Macconmara MP, Singal AG, Mufti AR. Survey of liver transplantation practices for severe acute alcoholic hepatitis. Liver Transpl. 2018;24(10):1357-1362. https://doi.org/10.1002/lt.25285
7. Herrick-Reynolds KM, Punchhi G, Greenberg RS, et al. Evaluation of early vs standard liver transplant for alcohol-associated liver disease. JAMA Surg. 2021;156(11):1026-1034. https://doi.org/10.1001/jamasurg.2021.3748
8. Fleming JN, Lai JC, Te HS, Said A, Spengler EK, Rogal SS. Opioid and opioid substitution therapy in liver transplant candidates: A survey of center policies and practices. Clin Transplant. 2017;31(12):e13119. https://doi.org/10.1111/ctr.13119
9. Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev. 2018;12(12):CD009269. https://doi.org/10.1002/14651858.CD009269.pub4
10. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. https://doi.org/10.15585/mmwr.mm7006a4
11. Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. Accessed November 18, 2021. www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
12. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
13. California Bridge Program. Tools: Treat substance use disorders from the acute care setting. Accessed August 20, 2021. https://cabridge.org/tools
14. Peterson C, Li M, Xu L, Mikosz CA, Luo F. Assessment of annual cost of substance use disorder in US hospitals. JAMA Netw Open. 2021;4(3):e210242. https://doi.org/10.1001/jamanetworkopen.2021.0242
15. Suen LW, Makam AN, Snyder HR, et al. National prevalence of alcohol and other substance use disorders among emergency department visits and hospitalizations: NHAMCS 2014-2018. J Gen Intern Med. 2021;13:1-9. https://doi.org/10.1007/s11606-021-07069-w
16. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: Qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993
17. Priest KC, McCarty D. Making the business case for an addiction medicine consult service: a qualitative analysis. BMC Health Services Research. 2019;19(1):822. https://doi.org/10.1186/s12913-019-4670-4
18. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496
19. Martin M, Snyder HR, Coffa D, et al. Time to ACT: launching an Addiction Care Team (ACT) in an urban safety-net health system. BMJ Open Qual. 2021;10(1):e001111. https://doi.org/10.1136/bmjoq-2020-001111
20. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abus. 2020;41(4):519-525. https://doi.org/10.1080/08897077.2019.1671942
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. HHS Publication No. PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Accessed December 1, 2021. www.samhsa.gov/data/
2. Centers for Disease Control and Prevention. Alcohol and public health: alcohol-related disease impact (ARDI) application, 2013. Average for United States 2006–2010 alcohol-attributable deaths due to excessive alcohol use. Accessed December 1, 2021. www.cdc.gov/ARDI
3. Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Netw Open. 2020;3(2):e1921451. https://doi.org/ 10.1001/jamanetworkopen.2019.21451
4. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161 https://doi.org/10.1001/jamapsychiatry.2017.2161
5. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the covid-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. https://doi.org/10.1001/jamanetworkopen.2020.22942
6. Bangaru S, Pedersen MR, Macconmara MP, Singal AG, Mufti AR. Survey of liver transplantation practices for severe acute alcoholic hepatitis. Liver Transpl. 2018;24(10):1357-1362. https://doi.org/10.1002/lt.25285
7. Herrick-Reynolds KM, Punchhi G, Greenberg RS, et al. Evaluation of early vs standard liver transplant for alcohol-associated liver disease. JAMA Surg. 2021;156(11):1026-1034. https://doi.org/10.1001/jamasurg.2021.3748
8. Fleming JN, Lai JC, Te HS, Said A, Spengler EK, Rogal SS. Opioid and opioid substitution therapy in liver transplant candidates: A survey of center policies and practices. Clin Transplant. 2017;31(12):e13119. https://doi.org/10.1111/ctr.13119
9. Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev. 2018;12(12):CD009269. https://doi.org/10.1002/14651858.CD009269.pub4
10. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. https://doi.org/10.15585/mmwr.mm7006a4
11. Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. Accessed November 18, 2021. www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
12. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
13. California Bridge Program. Tools: Treat substance use disorders from the acute care setting. Accessed August 20, 2021. https://cabridge.org/tools
14. Peterson C, Li M, Xu L, Mikosz CA, Luo F. Assessment of annual cost of substance use disorder in US hospitals. JAMA Netw Open. 2021;4(3):e210242. https://doi.org/10.1001/jamanetworkopen.2021.0242
15. Suen LW, Makam AN, Snyder HR, et al. National prevalence of alcohol and other substance use disorders among emergency department visits and hospitalizations: NHAMCS 2014-2018. J Gen Intern Med. 2021;13:1-9. https://doi.org/10.1007/s11606-021-07069-w
16. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: Qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993
17. Priest KC, McCarty D. Making the business case for an addiction medicine consult service: a qualitative analysis. BMC Health Services Research. 2019;19(1):822. https://doi.org/10.1186/s12913-019-4670-4
18. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496
19. Martin M, Snyder HR, Coffa D, et al. Time to ACT: launching an Addiction Care Team (ACT) in an urban safety-net health system. BMJ Open Qual. 2021;10(1):e001111. https://doi.org/10.1136/bmjoq-2020-001111
20. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abus. 2020;41(4):519-525. https://doi.org/10.1080/08897077.2019.1671942
© 2021 Society of Hospital Medicine
The Kids Are Not Alright
“...but it all started to get worse during the pandemic.”
As the patient’s† door closed, I (JS) thought about what his father had shared: his 12-year-old son had experienced a slow decline in his mental health since March 2020. There had been a gradual loss of all the things his son needed for psychological well-being: school went virtual and extracurricular activities ceased, and with them went any sense of routine, normalcy, or authentic opportunities to socialize. His feelings of isolation and depression culminated in an attempt to end his own life. My mind shifted to other patients under our care: an 8-year-old with behavioral outbursts intensifying after school-based therapy ended, a 13-year-old who became suicidal from isolation and virtual bullying. These children’s families sought emergent care because they no longer had the resources to care for their children at home. My team left each of these rooms heartbroken, unsure of exactly what to say and aware of the limitations of our current healthcare system.
Before and during the COVID-19 pandemic, many pediatric providers have had similar experiences caring for countless patients who are “boarding”—awaiting transfer to a psychiatric facility for their primary acute psychiatric issue, initially in the emergency room, often for 5 days or more,1 then ultimately admitted to a general medical floor if an appropriate psychiatric bed is still not available.2 Unfortunately, just as parents have run out of resources to care for their children’s psychiatric needs, so too is our medical system lacking in resources to provide the acute care these children need in general hospitals.
This mental health crisis began before the COVID-19 pandemic3 but has only worsened in the wake of its resulting social isolation. During the pandemic, suicide hotlines had a 1000% increase in call volumes.4 COVID-19–induced bed closures simultaneously worsened an existing critical bed shortage5,6 and led to an increase in the average length of stay (LOS) for patients boarding in the emergency department (ED).7 In the state of Massachusetts, for example, psychiatric patients awaiting inpatient beds boarded for more than 10,000 hours in January 2021—more than ever before, and up approximately 4000 hours since January 2017.6 For pediatric patients, the average wait time is now 59 hours.6 In the first 6 months of the pandemic, 39% of children presenting to EDs for mental health complaints ended up boarding, which is an astounding figure and is unfortunately 7% higher than in 2019.8 Even these staggering numbers do not capture the full range of experiences, as many statistics do not account for time spent on inpatient units by patients who do not receive a bed placement after waiting hours to several days in the ED.
Shortages of space, as well as an underfunded and understaffed mental health workforce, lead to these prolonged, often traumatic boarding periods in hospitals designed to care for acute medical, rather than acute psychiatric, conditions. Patients awaiting psychiatric placement are waiting in settings that are chaotic, inconsistent, and lacking in privacy. A patient in the throes of psychosis or suicidality needs a therapeutic milieu, not one that interrupts their daily routine,2 disconnects them from their existing support networks, and is punctuated by the incessant clangs of bedside monitors and the hubbub of code teams. These environments are not therapeutic3 for young infants with fevers, let alone for teenagers battling suicidality and eating disorders. In fact, for these reasons, we suspect that many of our patients’ inpatient ”behavioral escalations” are in fact triggered by their hospital environment, which may contribute to the 300% increase in the number of pharmacological restraints used during mental health visits in the ED over the past 10 years.9
None of us imagined when we chose to pursue pediatrics a that significant—and at times predominant—portion of our training would encompass caring for patients with acute mental health concerns. And although we did not anticipate this crisis, we have now been tasked with managing it. Throughout the day, when we are called to see our patients with primarily psychiatric pathology, we are often at war with ourselves. We weigh forming deeply meaningful relationships with these patients against the potential of unintentionally retraumatizing them or forming bonds that will be abruptly severed when patients are transferred to a psychiatric facility, which often occurs with barely a few hours’ notice. Moreover, many healthcare workers have training ill-suited to meet the needs of these patients. Just as emergency physicians can diagnose appendicitis but rely on surgeons to provide timely surgical treatment, general pediatricians identify psychiatric crises but rely on psychiatrists for ideal treatment plans. And almost daily, we are called to an “escalating” patient and arrive minutes into a stressful situation that others expect us to extinguish expeditiously. Along with nursing colleagues and the behavioral response team, we enact the treatment plan laid out by our psychiatry colleagues and wonder whether there is a better way.
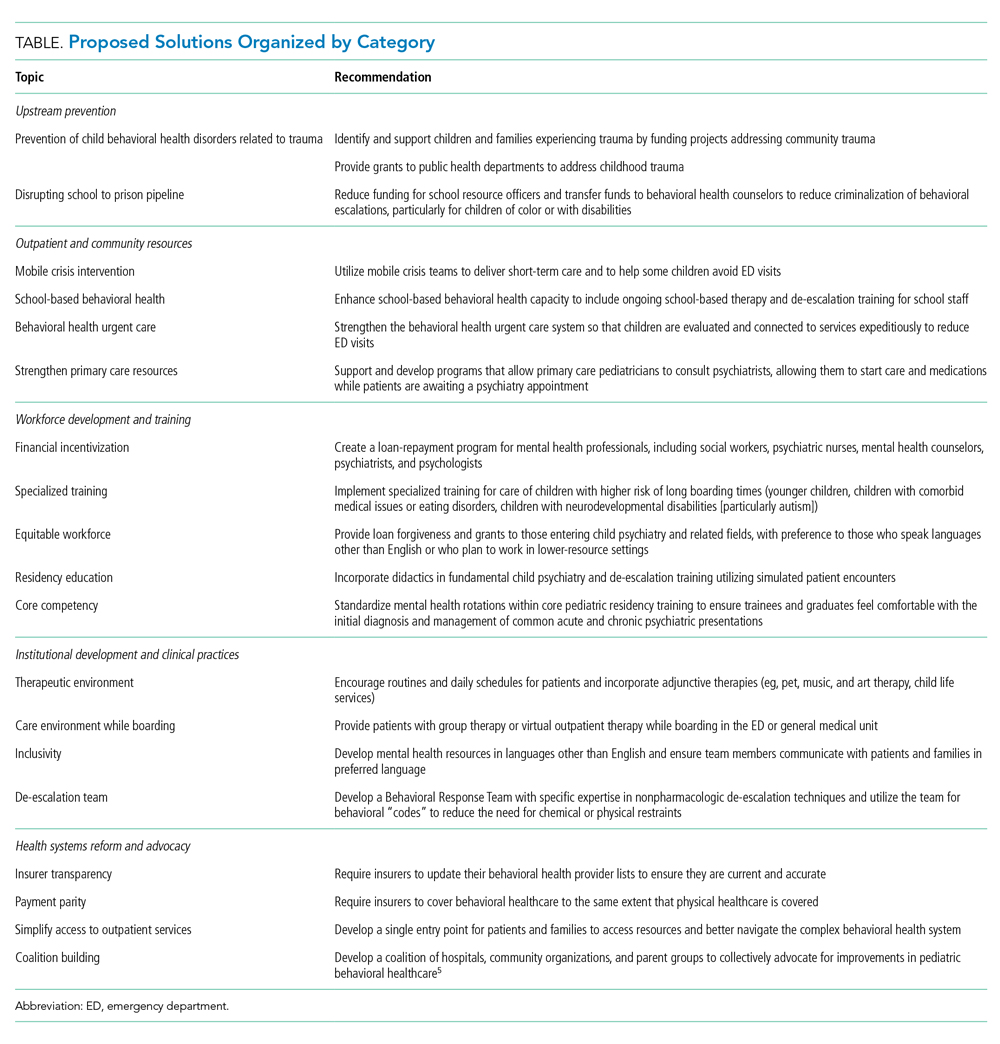
We propose the following changes to create a more ideal health system (Table). We acknowledge that each health system has unique resources, challenges, and patient populations. Thus, our recommendations are not comprehensive and are largely based on experiences within our own institutions and state, but they encompass many domains that impact and are affected by child and adolescent mental healthcare in the United States, ranging from program- and hospital-level innovation to community and legislative action.
UPSTREAM PREVENTION
Like all good health system designs, we recommend prioritizing prevention. This would entail funding programs and legislation such as H.R. 3180, the RISE from Trauma Act, and H.R. 8544, the STRONG Support for Children Act of 2020 (both currently under consideration in the US House of Representatives) that support early childhood development and prevent adverse childhood experiences and trauma, averting mental health diagnoses such as depression and attention-deficit/hyperactivity disorder before they begin.10
OUTPATIENT AND COMMUNITY RESOURCES
We recognize that schools and general pediatricians have far more exposure to children at risk for mental health crises than do subspecialists. Thus, we urge an equitable increase in access to mental healthcare in the community so that patients needing assistance are screened and diagnosed earlier in their illness, allowing for secondary prevention of worsening mental health disorders. We support increased funding for programs such as the Massachusetts Child Psychiatry Access Program, which allows primary care doctors to consult psychiatrists in real time, closing the gap between a primary care visit and specialty follow-up. Telehealth services will be key to improving access for patients themselves and to allow pediatricians to consult with mental health professionals to initiate care prior to specialist availability. We envision that strengthening school-based behavioral health resources will also help prevent ED visits. Behavioral healthcare should be integrated into schools and community centers while police presence is simultaneously reduced, as there is evidence of an increased likelihood of juvenile justice involvement for children with disabilities and mental health needs.11,12
WORKFORCE DEVELOPMENT AND TRAINING
Ensuring access necessitates increasing the capacity of our psychiatric workforce by encouraging graduates to pursue mental health occupations with concrete financial incentives such as loan repayment and training grants. We thus support legislation such as H.R. 6597, the Mental Health Professionals Workforce Shortage Loan Repayment Act of 2018 (currently under consideration in the US House of Representatives). This may also improve recruitment and retention of individuals who are underrepresented in medicine, one step in helping ensure children have access to linguistically appropriate and culturally sensitive care. Residency programs and hospital systems should expand their training and education to identify and stabilize patients in mental health in extremis through culturally sensitive curricula focused on behavioral de-escalation techniques, trauma-informed care, and psychopharmacology. Our own residency program created a 2-week mental health rotation13 that includes rotating with outpatient mental health providers and our hospital’s behavioral response team, a group of trauma-informed responders for behavioral emergencies. Similar training should be available for nursing and other allied health professionals, who are often the first responders to behavioral escalations.13
INSTITUTIONAL DEVELOPMENT AND CLINICAL PRACTICES
Ideally, patients requiring higher-intensity psychiatric care would be referred to specialized pediatric behavioral health urgent care centers so their conditions can be adequately evaluated and addressed by staff trained in psychiatric management and in therapeutic environments. We believe all providers caring for children with mental health needs should be trained in basic, but core, behavioral health and de-escalation competencies, including specialized training for children with comorbid medical and neurodevelopmental diagnoses, such as autism. These centers should have specific beds for young children and those with developmental or complex care needs, and services should be available in numerous languages and levels of health literacy to allow all families to participate in their child’s care. At the same time, even nonpsychiatric EDs and inpatient units should commit resources to developing a maximally therapeutic environment, including allowing adjunctive services such as child life services, group therapy, and pet and music therapy, and create environments that support, rather than disrupt, normal routines.
HEALTH SYSTEMS REFORM AND ADVOCACY
Underpinning all the above innovations are changes to our healthcare payment system and provider networks, including the need for insurance coverage and payment parity for behavioral health, to ensure care is not only accessible but affordable. Additionally, for durable change, we need more than just education—we need coalition building and advocacy. Many organizations, including the American Academy of Pediatrics and the Children’s Hospital Association, have begun this work, which we must all continue.14 Bringing in diverse partners, including health systems, providers, educators, hospital administrators, payors, elected officials, and communities, will prioritize children’s needs and create a more ideal pediatric behavioral healthcare system.15
The COVID-19 pandemic has highlighted the dire need for comprehensive mental healthcare in the United States, a need that existed before the pandemic and will persist in a more fragile state long after it ends. Our hope is that the pandemic serves as the catalyst necessary to promote the magnitude of investments and stakeholder buy-in necessary to improve pediatric mental health and engender a radical redesign of our behavioral healthcare system. Our patients are counting on us to act. Together, we can build a system that ensures that the kids will be alright.
†Patient details have been changed for patient privacy.
Acknowledgments
The authors thank Joanna Perdomo, MD, Amara Azubuike, JD, and Josh Greenberg, JD, for reading and providing feedback on earlier versions of this work.
1. “This is a crisis”: mom whose son has boarded 33 days for psych bed calls for state action. WBUR News. Updated March 2, 2021. Accessed August 4, 2021. www.wbur.org/news/2021/02/26/mental-health-boarding-hospitals
2. Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813-824. https://doi.org/10.1016/S2215-0366(20)30307-2
3. Nash KA, Zima BT, Rothenberg C, et al. Prolonged emergency department length of stay for US pediatric mental health visits (2005-2015). Pediatrics. 2021;147(5):e2020030692. https://doi.org/10.1542/peds.2020-030692
4. Cloutier RL, Marshaall R. A dangerous pandemic pair: Covid19 and adolescent mental health emergencies. Am J Emerg Med. 2021;46:776-777. https://doi.org/10.1016/j.ajem.2020.09.008
5. Schoenberg S. Lack of mental health beds means long ER waits. CommonWealth Magazine. April 15, 2021. Accessed August 5, 2021. https://commonwealthmagazine.org/health-care/lack-of-mental-health-beds-means-long-er-waits/
6. Jolicoeur L, Mullins L. Mass. physicians call on state to address ER “boarding” of patients awaiting admission. WBUR News. Updated February 3, 2021. Accessed August 5, 2021. www.wbur.org/news/2021/02/02/emergency-department-er-inpatient-beds-boarding
7. Krass P, Dalton E, Doupnik SK, Esposito J. US pediatric emergency department visits for mental health conditions during the COVID-19 pandemic. JAMA Netw Open. 2021;4(4):e218533. https://doi.org/10.1001/jamanetworkopen.2021.8533
8. Impact of COVID-19 on the Massachusetts Health Care System: Interim Report. Massachusetts Health Policy Commission. April 2021. Accessed September 25, 2021. www.mass.gov/doc/impact-of-covid-19-on-the-massachusetts-health-care-system-interim-report/download
9. Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic restraint use during mental health visits in pediatric emergency departments. J Pediatr. 2021;236:276-283.e2. https://doi.org/10.1016/j.jpeds.2021.03.027
10. Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, Oyeku SO. Associations between adverse childhood experiences and ADHD diagnosis and severity. Acad Pediatr. 2017;17(4):349-355. https://doi.org/10.1016/j.acap.2016.08.013
11. Harper K, Ryberg R, Temkin D. Black students and students with disabilities remain more likely to receive out-of-school suspensions, despite overall declines. Child Trends. April 29, 2019. Accessed August 5, 2021. www.childtrends.org/publications/black-students-disabilities-out-of-school-suspensions
12. Whitaker A, Torres-Guillén S, Morton M, et al. Cops and no counselors: how the lack of school mental health staff is harming students. American Civil Liberties Union. Accessed August 6, 2021. www.aclu.org/report/cops-and-no-counselors
13. Education. Boston Combined Residence Program. Accessed August 5, 2021. https://msbcrp.wpengine.com/program/education/
14. American Academy of Pediatrics. Interim guidance on supporting the emotional and behavioral health needs of children, adolescents, and families during the COVID-19 pandemic. Updated July 28, 2021. Accessed August 5, 2021. http://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/interim-guidance-on-supporting-the-emotional-and-behavioral-health-needs-of-children-adolescents-and-families-during-the-covid-19-pandemic/
15. Advocacy. Children’s Mental Health Campaign. Accessed August 4, 2021. https://childrensmentalhealthcampaign.org/advocacy
“...but it all started to get worse during the pandemic.”
As the patient’s† door closed, I (JS) thought about what his father had shared: his 12-year-old son had experienced a slow decline in his mental health since March 2020. There had been a gradual loss of all the things his son needed for psychological well-being: school went virtual and extracurricular activities ceased, and with them went any sense of routine, normalcy, or authentic opportunities to socialize. His feelings of isolation and depression culminated in an attempt to end his own life. My mind shifted to other patients under our care: an 8-year-old with behavioral outbursts intensifying after school-based therapy ended, a 13-year-old who became suicidal from isolation and virtual bullying. These children’s families sought emergent care because they no longer had the resources to care for their children at home. My team left each of these rooms heartbroken, unsure of exactly what to say and aware of the limitations of our current healthcare system.
Before and during the COVID-19 pandemic, many pediatric providers have had similar experiences caring for countless patients who are “boarding”—awaiting transfer to a psychiatric facility for their primary acute psychiatric issue, initially in the emergency room, often for 5 days or more,1 then ultimately admitted to a general medical floor if an appropriate psychiatric bed is still not available.2 Unfortunately, just as parents have run out of resources to care for their children’s psychiatric needs, so too is our medical system lacking in resources to provide the acute care these children need in general hospitals.
This mental health crisis began before the COVID-19 pandemic3 but has only worsened in the wake of its resulting social isolation. During the pandemic, suicide hotlines had a 1000% increase in call volumes.4 COVID-19–induced bed closures simultaneously worsened an existing critical bed shortage5,6 and led to an increase in the average length of stay (LOS) for patients boarding in the emergency department (ED).7 In the state of Massachusetts, for example, psychiatric patients awaiting inpatient beds boarded for more than 10,000 hours in January 2021—more than ever before, and up approximately 4000 hours since January 2017.6 For pediatric patients, the average wait time is now 59 hours.6 In the first 6 months of the pandemic, 39% of children presenting to EDs for mental health complaints ended up boarding, which is an astounding figure and is unfortunately 7% higher than in 2019.8 Even these staggering numbers do not capture the full range of experiences, as many statistics do not account for time spent on inpatient units by patients who do not receive a bed placement after waiting hours to several days in the ED.
Shortages of space, as well as an underfunded and understaffed mental health workforce, lead to these prolonged, often traumatic boarding periods in hospitals designed to care for acute medical, rather than acute psychiatric, conditions. Patients awaiting psychiatric placement are waiting in settings that are chaotic, inconsistent, and lacking in privacy. A patient in the throes of psychosis or suicidality needs a therapeutic milieu, not one that interrupts their daily routine,2 disconnects them from their existing support networks, and is punctuated by the incessant clangs of bedside monitors and the hubbub of code teams. These environments are not therapeutic3 for young infants with fevers, let alone for teenagers battling suicidality and eating disorders. In fact, for these reasons, we suspect that many of our patients’ inpatient ”behavioral escalations” are in fact triggered by their hospital environment, which may contribute to the 300% increase in the number of pharmacological restraints used during mental health visits in the ED over the past 10 years.9
None of us imagined when we chose to pursue pediatrics a that significant—and at times predominant—portion of our training would encompass caring for patients with acute mental health concerns. And although we did not anticipate this crisis, we have now been tasked with managing it. Throughout the day, when we are called to see our patients with primarily psychiatric pathology, we are often at war with ourselves. We weigh forming deeply meaningful relationships with these patients against the potential of unintentionally retraumatizing them or forming bonds that will be abruptly severed when patients are transferred to a psychiatric facility, which often occurs with barely a few hours’ notice. Moreover, many healthcare workers have training ill-suited to meet the needs of these patients. Just as emergency physicians can diagnose appendicitis but rely on surgeons to provide timely surgical treatment, general pediatricians identify psychiatric crises but rely on psychiatrists for ideal treatment plans. And almost daily, we are called to an “escalating” patient and arrive minutes into a stressful situation that others expect us to extinguish expeditiously. Along with nursing colleagues and the behavioral response team, we enact the treatment plan laid out by our psychiatry colleagues and wonder whether there is a better way.
We propose the following changes to create a more ideal health system (Table). We acknowledge that each health system has unique resources, challenges, and patient populations. Thus, our recommendations are not comprehensive and are largely based on experiences within our own institutions and state, but they encompass many domains that impact and are affected by child and adolescent mental healthcare in the United States, ranging from program- and hospital-level innovation to community and legislative action.
UPSTREAM PREVENTION
Like all good health system designs, we recommend prioritizing prevention. This would entail funding programs and legislation such as H.R. 3180, the RISE from Trauma Act, and H.R. 8544, the STRONG Support for Children Act of 2020 (both currently under consideration in the US House of Representatives) that support early childhood development and prevent adverse childhood experiences and trauma, averting mental health diagnoses such as depression and attention-deficit/hyperactivity disorder before they begin.10
OUTPATIENT AND COMMUNITY RESOURCES
We recognize that schools and general pediatricians have far more exposure to children at risk for mental health crises than do subspecialists. Thus, we urge an equitable increase in access to mental healthcare in the community so that patients needing assistance are screened and diagnosed earlier in their illness, allowing for secondary prevention of worsening mental health disorders. We support increased funding for programs such as the Massachusetts Child Psychiatry Access Program, which allows primary care doctors to consult psychiatrists in real time, closing the gap between a primary care visit and specialty follow-up. Telehealth services will be key to improving access for patients themselves and to allow pediatricians to consult with mental health professionals to initiate care prior to specialist availability. We envision that strengthening school-based behavioral health resources will also help prevent ED visits. Behavioral healthcare should be integrated into schools and community centers while police presence is simultaneously reduced, as there is evidence of an increased likelihood of juvenile justice involvement for children with disabilities and mental health needs.11,12
WORKFORCE DEVELOPMENT AND TRAINING
Ensuring access necessitates increasing the capacity of our psychiatric workforce by encouraging graduates to pursue mental health occupations with concrete financial incentives such as loan repayment and training grants. We thus support legislation such as H.R. 6597, the Mental Health Professionals Workforce Shortage Loan Repayment Act of 2018 (currently under consideration in the US House of Representatives). This may also improve recruitment and retention of individuals who are underrepresented in medicine, one step in helping ensure children have access to linguistically appropriate and culturally sensitive care. Residency programs and hospital systems should expand their training and education to identify and stabilize patients in mental health in extremis through culturally sensitive curricula focused on behavioral de-escalation techniques, trauma-informed care, and psychopharmacology. Our own residency program created a 2-week mental health rotation13 that includes rotating with outpatient mental health providers and our hospital’s behavioral response team, a group of trauma-informed responders for behavioral emergencies. Similar training should be available for nursing and other allied health professionals, who are often the first responders to behavioral escalations.13
INSTITUTIONAL DEVELOPMENT AND CLINICAL PRACTICES
Ideally, patients requiring higher-intensity psychiatric care would be referred to specialized pediatric behavioral health urgent care centers so their conditions can be adequately evaluated and addressed by staff trained in psychiatric management and in therapeutic environments. We believe all providers caring for children with mental health needs should be trained in basic, but core, behavioral health and de-escalation competencies, including specialized training for children with comorbid medical and neurodevelopmental diagnoses, such as autism. These centers should have specific beds for young children and those with developmental or complex care needs, and services should be available in numerous languages and levels of health literacy to allow all families to participate in their child’s care. At the same time, even nonpsychiatric EDs and inpatient units should commit resources to developing a maximally therapeutic environment, including allowing adjunctive services such as child life services, group therapy, and pet and music therapy, and create environments that support, rather than disrupt, normal routines.
HEALTH SYSTEMS REFORM AND ADVOCACY
Underpinning all the above innovations are changes to our healthcare payment system and provider networks, including the need for insurance coverage and payment parity for behavioral health, to ensure care is not only accessible but affordable. Additionally, for durable change, we need more than just education—we need coalition building and advocacy. Many organizations, including the American Academy of Pediatrics and the Children’s Hospital Association, have begun this work, which we must all continue.14 Bringing in diverse partners, including health systems, providers, educators, hospital administrators, payors, elected officials, and communities, will prioritize children’s needs and create a more ideal pediatric behavioral healthcare system.15
The COVID-19 pandemic has highlighted the dire need for comprehensive mental healthcare in the United States, a need that existed before the pandemic and will persist in a more fragile state long after it ends. Our hope is that the pandemic serves as the catalyst necessary to promote the magnitude of investments and stakeholder buy-in necessary to improve pediatric mental health and engender a radical redesign of our behavioral healthcare system. Our patients are counting on us to act. Together, we can build a system that ensures that the kids will be alright.
†Patient details have been changed for patient privacy.
Acknowledgments
The authors thank Joanna Perdomo, MD, Amara Azubuike, JD, and Josh Greenberg, JD, for reading and providing feedback on earlier versions of this work.
“...but it all started to get worse during the pandemic.”
As the patient’s† door closed, I (JS) thought about what his father had shared: his 12-year-old son had experienced a slow decline in his mental health since March 2020. There had been a gradual loss of all the things his son needed for psychological well-being: school went virtual and extracurricular activities ceased, and with them went any sense of routine, normalcy, or authentic opportunities to socialize. His feelings of isolation and depression culminated in an attempt to end his own life. My mind shifted to other patients under our care: an 8-year-old with behavioral outbursts intensifying after school-based therapy ended, a 13-year-old who became suicidal from isolation and virtual bullying. These children’s families sought emergent care because they no longer had the resources to care for their children at home. My team left each of these rooms heartbroken, unsure of exactly what to say and aware of the limitations of our current healthcare system.
Before and during the COVID-19 pandemic, many pediatric providers have had similar experiences caring for countless patients who are “boarding”—awaiting transfer to a psychiatric facility for their primary acute psychiatric issue, initially in the emergency room, often for 5 days or more,1 then ultimately admitted to a general medical floor if an appropriate psychiatric bed is still not available.2 Unfortunately, just as parents have run out of resources to care for their children’s psychiatric needs, so too is our medical system lacking in resources to provide the acute care these children need in general hospitals.
This mental health crisis began before the COVID-19 pandemic3 but has only worsened in the wake of its resulting social isolation. During the pandemic, suicide hotlines had a 1000% increase in call volumes.4 COVID-19–induced bed closures simultaneously worsened an existing critical bed shortage5,6 and led to an increase in the average length of stay (LOS) for patients boarding in the emergency department (ED).7 In the state of Massachusetts, for example, psychiatric patients awaiting inpatient beds boarded for more than 10,000 hours in January 2021—more than ever before, and up approximately 4000 hours since January 2017.6 For pediatric patients, the average wait time is now 59 hours.6 In the first 6 months of the pandemic, 39% of children presenting to EDs for mental health complaints ended up boarding, which is an astounding figure and is unfortunately 7% higher than in 2019.8 Even these staggering numbers do not capture the full range of experiences, as many statistics do not account for time spent on inpatient units by patients who do not receive a bed placement after waiting hours to several days in the ED.
Shortages of space, as well as an underfunded and understaffed mental health workforce, lead to these prolonged, often traumatic boarding periods in hospitals designed to care for acute medical, rather than acute psychiatric, conditions. Patients awaiting psychiatric placement are waiting in settings that are chaotic, inconsistent, and lacking in privacy. A patient in the throes of psychosis or suicidality needs a therapeutic milieu, not one that interrupts their daily routine,2 disconnects them from their existing support networks, and is punctuated by the incessant clangs of bedside monitors and the hubbub of code teams. These environments are not therapeutic3 for young infants with fevers, let alone for teenagers battling suicidality and eating disorders. In fact, for these reasons, we suspect that many of our patients’ inpatient ”behavioral escalations” are in fact triggered by their hospital environment, which may contribute to the 300% increase in the number of pharmacological restraints used during mental health visits in the ED over the past 10 years.9
None of us imagined when we chose to pursue pediatrics a that significant—and at times predominant—portion of our training would encompass caring for patients with acute mental health concerns. And although we did not anticipate this crisis, we have now been tasked with managing it. Throughout the day, when we are called to see our patients with primarily psychiatric pathology, we are often at war with ourselves. We weigh forming deeply meaningful relationships with these patients against the potential of unintentionally retraumatizing them or forming bonds that will be abruptly severed when patients are transferred to a psychiatric facility, which often occurs with barely a few hours’ notice. Moreover, many healthcare workers have training ill-suited to meet the needs of these patients. Just as emergency physicians can diagnose appendicitis but rely on surgeons to provide timely surgical treatment, general pediatricians identify psychiatric crises but rely on psychiatrists for ideal treatment plans. And almost daily, we are called to an “escalating” patient and arrive minutes into a stressful situation that others expect us to extinguish expeditiously. Along with nursing colleagues and the behavioral response team, we enact the treatment plan laid out by our psychiatry colleagues and wonder whether there is a better way.
We propose the following changes to create a more ideal health system (Table). We acknowledge that each health system has unique resources, challenges, and patient populations. Thus, our recommendations are not comprehensive and are largely based on experiences within our own institutions and state, but they encompass many domains that impact and are affected by child and adolescent mental healthcare in the United States, ranging from program- and hospital-level innovation to community and legislative action.
UPSTREAM PREVENTION
Like all good health system designs, we recommend prioritizing prevention. This would entail funding programs and legislation such as H.R. 3180, the RISE from Trauma Act, and H.R. 8544, the STRONG Support for Children Act of 2020 (both currently under consideration in the US House of Representatives) that support early childhood development and prevent adverse childhood experiences and trauma, averting mental health diagnoses such as depression and attention-deficit/hyperactivity disorder before they begin.10
OUTPATIENT AND COMMUNITY RESOURCES
We recognize that schools and general pediatricians have far more exposure to children at risk for mental health crises than do subspecialists. Thus, we urge an equitable increase in access to mental healthcare in the community so that patients needing assistance are screened and diagnosed earlier in their illness, allowing for secondary prevention of worsening mental health disorders. We support increased funding for programs such as the Massachusetts Child Psychiatry Access Program, which allows primary care doctors to consult psychiatrists in real time, closing the gap between a primary care visit and specialty follow-up. Telehealth services will be key to improving access for patients themselves and to allow pediatricians to consult with mental health professionals to initiate care prior to specialist availability. We envision that strengthening school-based behavioral health resources will also help prevent ED visits. Behavioral healthcare should be integrated into schools and community centers while police presence is simultaneously reduced, as there is evidence of an increased likelihood of juvenile justice involvement for children with disabilities and mental health needs.11,12
WORKFORCE DEVELOPMENT AND TRAINING
Ensuring access necessitates increasing the capacity of our psychiatric workforce by encouraging graduates to pursue mental health occupations with concrete financial incentives such as loan repayment and training grants. We thus support legislation such as H.R. 6597, the Mental Health Professionals Workforce Shortage Loan Repayment Act of 2018 (currently under consideration in the US House of Representatives). This may also improve recruitment and retention of individuals who are underrepresented in medicine, one step in helping ensure children have access to linguistically appropriate and culturally sensitive care. Residency programs and hospital systems should expand their training and education to identify and stabilize patients in mental health in extremis through culturally sensitive curricula focused on behavioral de-escalation techniques, trauma-informed care, and psychopharmacology. Our own residency program created a 2-week mental health rotation13 that includes rotating with outpatient mental health providers and our hospital’s behavioral response team, a group of trauma-informed responders for behavioral emergencies. Similar training should be available for nursing and other allied health professionals, who are often the first responders to behavioral escalations.13
INSTITUTIONAL DEVELOPMENT AND CLINICAL PRACTICES
Ideally, patients requiring higher-intensity psychiatric care would be referred to specialized pediatric behavioral health urgent care centers so their conditions can be adequately evaluated and addressed by staff trained in psychiatric management and in therapeutic environments. We believe all providers caring for children with mental health needs should be trained in basic, but core, behavioral health and de-escalation competencies, including specialized training for children with comorbid medical and neurodevelopmental diagnoses, such as autism. These centers should have specific beds for young children and those with developmental or complex care needs, and services should be available in numerous languages and levels of health literacy to allow all families to participate in their child’s care. At the same time, even nonpsychiatric EDs and inpatient units should commit resources to developing a maximally therapeutic environment, including allowing adjunctive services such as child life services, group therapy, and pet and music therapy, and create environments that support, rather than disrupt, normal routines.
HEALTH SYSTEMS REFORM AND ADVOCACY
Underpinning all the above innovations are changes to our healthcare payment system and provider networks, including the need for insurance coverage and payment parity for behavioral health, to ensure care is not only accessible but affordable. Additionally, for durable change, we need more than just education—we need coalition building and advocacy. Many organizations, including the American Academy of Pediatrics and the Children’s Hospital Association, have begun this work, which we must all continue.14 Bringing in diverse partners, including health systems, providers, educators, hospital administrators, payors, elected officials, and communities, will prioritize children’s needs and create a more ideal pediatric behavioral healthcare system.15
The COVID-19 pandemic has highlighted the dire need for comprehensive mental healthcare in the United States, a need that existed before the pandemic and will persist in a more fragile state long after it ends. Our hope is that the pandemic serves as the catalyst necessary to promote the magnitude of investments and stakeholder buy-in necessary to improve pediatric mental health and engender a radical redesign of our behavioral healthcare system. Our patients are counting on us to act. Together, we can build a system that ensures that the kids will be alright.
†Patient details have been changed for patient privacy.
Acknowledgments
The authors thank Joanna Perdomo, MD, Amara Azubuike, JD, and Josh Greenberg, JD, for reading and providing feedback on earlier versions of this work.
1. “This is a crisis”: mom whose son has boarded 33 days for psych bed calls for state action. WBUR News. Updated March 2, 2021. Accessed August 4, 2021. www.wbur.org/news/2021/02/26/mental-health-boarding-hospitals
2. Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813-824. https://doi.org/10.1016/S2215-0366(20)30307-2
3. Nash KA, Zima BT, Rothenberg C, et al. Prolonged emergency department length of stay for US pediatric mental health visits (2005-2015). Pediatrics. 2021;147(5):e2020030692. https://doi.org/10.1542/peds.2020-030692
4. Cloutier RL, Marshaall R. A dangerous pandemic pair: Covid19 and adolescent mental health emergencies. Am J Emerg Med. 2021;46:776-777. https://doi.org/10.1016/j.ajem.2020.09.008
5. Schoenberg S. Lack of mental health beds means long ER waits. CommonWealth Magazine. April 15, 2021. Accessed August 5, 2021. https://commonwealthmagazine.org/health-care/lack-of-mental-health-beds-means-long-er-waits/
6. Jolicoeur L, Mullins L. Mass. physicians call on state to address ER “boarding” of patients awaiting admission. WBUR News. Updated February 3, 2021. Accessed August 5, 2021. www.wbur.org/news/2021/02/02/emergency-department-er-inpatient-beds-boarding
7. Krass P, Dalton E, Doupnik SK, Esposito J. US pediatric emergency department visits for mental health conditions during the COVID-19 pandemic. JAMA Netw Open. 2021;4(4):e218533. https://doi.org/10.1001/jamanetworkopen.2021.8533
8. Impact of COVID-19 on the Massachusetts Health Care System: Interim Report. Massachusetts Health Policy Commission. April 2021. Accessed September 25, 2021. www.mass.gov/doc/impact-of-covid-19-on-the-massachusetts-health-care-system-interim-report/download
9. Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic restraint use during mental health visits in pediatric emergency departments. J Pediatr. 2021;236:276-283.e2. https://doi.org/10.1016/j.jpeds.2021.03.027
10. Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, Oyeku SO. Associations between adverse childhood experiences and ADHD diagnosis and severity. Acad Pediatr. 2017;17(4):349-355. https://doi.org/10.1016/j.acap.2016.08.013
11. Harper K, Ryberg R, Temkin D. Black students and students with disabilities remain more likely to receive out-of-school suspensions, despite overall declines. Child Trends. April 29, 2019. Accessed August 5, 2021. www.childtrends.org/publications/black-students-disabilities-out-of-school-suspensions
12. Whitaker A, Torres-Guillén S, Morton M, et al. Cops and no counselors: how the lack of school mental health staff is harming students. American Civil Liberties Union. Accessed August 6, 2021. www.aclu.org/report/cops-and-no-counselors
13. Education. Boston Combined Residence Program. Accessed August 5, 2021. https://msbcrp.wpengine.com/program/education/
14. American Academy of Pediatrics. Interim guidance on supporting the emotional and behavioral health needs of children, adolescents, and families during the COVID-19 pandemic. Updated July 28, 2021. Accessed August 5, 2021. http://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/interim-guidance-on-supporting-the-emotional-and-behavioral-health-needs-of-children-adolescents-and-families-during-the-covid-19-pandemic/
15. Advocacy. Children’s Mental Health Campaign. Accessed August 4, 2021. https://childrensmentalhealthcampaign.org/advocacy
1. “This is a crisis”: mom whose son has boarded 33 days for psych bed calls for state action. WBUR News. Updated March 2, 2021. Accessed August 4, 2021. www.wbur.org/news/2021/02/26/mental-health-boarding-hospitals
2. Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813-824. https://doi.org/10.1016/S2215-0366(20)30307-2
3. Nash KA, Zima BT, Rothenberg C, et al. Prolonged emergency department length of stay for US pediatric mental health visits (2005-2015). Pediatrics. 2021;147(5):e2020030692. https://doi.org/10.1542/peds.2020-030692
4. Cloutier RL, Marshaall R. A dangerous pandemic pair: Covid19 and adolescent mental health emergencies. Am J Emerg Med. 2021;46:776-777. https://doi.org/10.1016/j.ajem.2020.09.008
5. Schoenberg S. Lack of mental health beds means long ER waits. CommonWealth Magazine. April 15, 2021. Accessed August 5, 2021. https://commonwealthmagazine.org/health-care/lack-of-mental-health-beds-means-long-er-waits/
6. Jolicoeur L, Mullins L. Mass. physicians call on state to address ER “boarding” of patients awaiting admission. WBUR News. Updated February 3, 2021. Accessed August 5, 2021. www.wbur.org/news/2021/02/02/emergency-department-er-inpatient-beds-boarding
7. Krass P, Dalton E, Doupnik SK, Esposito J. US pediatric emergency department visits for mental health conditions during the COVID-19 pandemic. JAMA Netw Open. 2021;4(4):e218533. https://doi.org/10.1001/jamanetworkopen.2021.8533
8. Impact of COVID-19 on the Massachusetts Health Care System: Interim Report. Massachusetts Health Policy Commission. April 2021. Accessed September 25, 2021. www.mass.gov/doc/impact-of-covid-19-on-the-massachusetts-health-care-system-interim-report/download
9. Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic restraint use during mental health visits in pediatric emergency departments. J Pediatr. 2021;236:276-283.e2. https://doi.org/10.1016/j.jpeds.2021.03.027
10. Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, Oyeku SO. Associations between adverse childhood experiences and ADHD diagnosis and severity. Acad Pediatr. 2017;17(4):349-355. https://doi.org/10.1016/j.acap.2016.08.013
11. Harper K, Ryberg R, Temkin D. Black students and students with disabilities remain more likely to receive out-of-school suspensions, despite overall declines. Child Trends. April 29, 2019. Accessed August 5, 2021. www.childtrends.org/publications/black-students-disabilities-out-of-school-suspensions
12. Whitaker A, Torres-Guillén S, Morton M, et al. Cops and no counselors: how the lack of school mental health staff is harming students. American Civil Liberties Union. Accessed August 6, 2021. www.aclu.org/report/cops-and-no-counselors
13. Education. Boston Combined Residence Program. Accessed August 5, 2021. https://msbcrp.wpengine.com/program/education/
14. American Academy of Pediatrics. Interim guidance on supporting the emotional and behavioral health needs of children, adolescents, and families during the COVID-19 pandemic. Updated July 28, 2021. Accessed August 5, 2021. http://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/interim-guidance-on-supporting-the-emotional-and-behavioral-health-needs-of-children-adolescents-and-families-during-the-covid-19-pandemic/
15. Advocacy. Children’s Mental Health Campaign. Accessed August 4, 2021. https://childrensmentalhealthcampaign.org/advocacy
© 2021 Society of Hospital Medicine
Principles and Practice of Gossiping About Colleagues in Medicine
CLINICAL SCENARIO PROLOGUE
You are signing over to a colleague on the COVID-19 inpatient hospital ward. You are stressed after having failed to reach the chief medical resident who did not respond despite repeated texts. You think about mentioning this apparent professional lapse to your colleague. You pause, however, because you are uncertain about the appropriate norm, hesitant around finding the right words, and unsure about a mutual feeling of camaraderie.
OVERVIEW
Lay and scientific perspectives about gossip diverge widely. Lay definitions of gossip generally include malicious, salacious, immoral, trivial, or unfair comments that attack someone else’s reputation. Scientific definitions of gossip, in contrast, also include neutral or positive social information intended to align group dynamics.1 The common feature of both is that the named individual is not present to hear about themselves.2 A further commonality is that gossip involves informal assessments loaded with subjective judgments, unlike professional comments about patients from clinicians providing care. In contrast to stereotype remarks, gossip focuses on a specific person and not a group.
Gossip is widespread. A recent study in nonhospital settings suggests nearly all adults engage in gossip during normal interactions, averaging 52 minutes on a typical day.3 Most gossip is neutral (74%) rather than negative or positive. The content usually (92%) concerns relationships, and the typical person identified (82%) is an acquaintance. Some of the potential benefits include conveying information for social learning, defining what is socially acceptable, or promoting personal connections. Men and women gossip to nearly the same degree.4 Indeed, evolutionary theory suggests gossip is not deviant behavior and arises even in small hunter-gatherer communities.5Social psychology science provides some insights on fundamental principles of gossip that may be relevant to clinicians in medicine.6 In this article, we review three important findings from social psychology science relevant to team cooperation, the specific transmitter, and the individual receiver (Table 1). Clinicians working in groups may benefit from recognizing the prosocial function of healthy gossip and avoiding the antisocial adverse effects of harmful gossip.7 At a time when work-related conversations have radically shifted online,8 hospitalists need to be aware of positives and pitfalls of gossip to help provide effective medical care and avoid adverse events.
GOSSIP AS TEAM COMMUNICATION
Large team endeavors often require social signals to coordinate people.9 Gossip helps groups establish reputations, monitor their members, deter antisocial behavior, and protect newcomers from exploitation.10 Sharing social information can also indirectly promote cooperation because individuals place a high value on their own reputations and want to avoid embarrassment.11,12 The absence of gossip, in contrast, may lead individuals to be oblivious to team expectations and fail to do their fair share. A lack of gossip, in particular, may add to inefficiencies during the COVID-19 pandemic since exchanging gossip seems to feel awkward over email or other digital channels (albeit a chat function for side conversations in virtual meetings is a partial substitute).13,14
A paradigm for testing the positive effects of gossip involves a trust game where participants consider making small contributions for later rewards in recurrent rounds of cooperation.15-17 In one online study of volunteers, for example, individuals contributed to a group account and gained rewards equal to a doubling of total contributions shared over everyone equally (even those contributing nothing).18 Half the experiments allowed participants to send notes about other participants, whereas the other experiments allowed no such “gossip.” As predicted, gossip increased the proportion contributed (40% vs 32%, P = .020) and average total reward (64 vs 56, P = .002). In this and other studies of healthy volunteers, gossip builds trust and increases gains for the entire group.19-22
Effective medical practice inside hospitals often involves constructive gossip for pointers on how to behave (eg, how quickly to reply to a text message from the ward pharmacist). The blend of objective facts with subjective opinion provides a compelling message otherwise lacking from institutional guidelines or directives on how not to behave (eg, how quickly to complete an annual report with an arbitrary deadline). Gossip is the antithesis of a cursory interaction between strangers and is also less awkward than open flattery or public ridicule that may occur when the third person is in earshot.23 Even negative social comparisons can be constructive to listeners since people want to know how to avoid bad gossip about themselves in a world with changing morality.24
GOSSIP AND THE TRANSMITTER
Gossip can provide a distinct emotional benefit for the gossiper as a form of self-expression, an exercise of justice, and a validation of one’s perspective.25 Consider, for example, witnessing an antisocial act that leads to subsequent feelings of unfairness yet having no way to communicate personal dissatisfaction. Similarly, expressing prosocial gossip may help relieve some of the annoyance after a hassle (eg, talking with a friend after encountering a new onerous hospital protocol). The sharing of gossip might also help bolster solidarity after an offense (eg, talking with a friend on how to deal with another warning from health records).26 In contrast, lost opportunities to gossip about unfairness could be exacerbating the social isolation and emotional distress of the COVID-19 pandemic.27,28
A rigorous example of the emotional benefits of expressing gossip involves undergraduates witnessing staged behavior under laboratory conditions where one actor appeared to exploit the generosity of another actor.29 By random assignment, half the participants had an opportunity to gossip, and the other half had no such opportunity. All participants reacted to the antisocial behavior by feeling frustrated (self-report survey scale of 0-100, where higher scores indicate worse frustration). Importantly, almost all chose to engage in gossip when feasible, and those who had the opportunity to gossip experienced more relief than those who had no opportunity (absolute improvement in frustration scores, 9.69 vs 0.16; P < .01). Evidentially, engaging in prosocial gossip can sometimes provide solace.
Sharing gossip might strengthen social bonds, bolster self-esteem, promote personal power, elicit reciprocal favors, or telegraph the presence of a larger network of personal connections. Gossip is cheap and efficient compared with peer-sanctioning or formal sanctioning to control behavior.30 Airing grievances through gossip may also solve some social dilemmas more easily than channeling messages through institutional reporting structures or formal performance reviews. Gossip has another advantage of raising delicate comparative judgments without the discomfort of direct confrontation (eg, defining the appropriate level of detail for a case presentation is perhaps best done by identifying those who are judged too verbose).31
GOSSIP AND THE RECEIVER
People tend to enjoy listening to gossip despite the uneven quality where some comments are more valuable than others. The receiver, therefore, faces an irregular payoff similar to random intermittent reinforcement. Ironically, random intermittent reinforcement can be particularly addictive when compared with steady rewards with predictable payoffs. This includes cases where gossip conveys good news that helps elevate, inspire, or motivate the receiver. The thirst for more gossip may partially explain why receivers keep seeking gossip despite knowing the material may be unimportant. The shortfall of enticing gossip might also be another factor adding to a feeling of loneliness that prevails widely during the COVID-19 pandemic.32,33
Classic research on reinforcement includes experiments examining operant conditioning for creating addiction.34,35 An important distinction is the contrast between random reinforcement (eg, variable reward akin to gambling on a roulette wheel) and consistent reinforcement (eg, regular pay akin to a steady salary each week). In a study of pigeons trained to peck a lever for food, for example, random reinforcement resulted in twice the response compared with consistent reinforcement (despite an equalized total amount of food received).36 Moreover, random reinforcement was hard to extinguish, and the behavior continued long after all food ended. In general, random compared with consistent reinforcement tended to cause a more intense and persistent change of behavior.
The inconsistent quality makes the prospect of new, exciting gossip seem nearly impossible to resist; indeed, gossip from any source is surprisingly tantalizing. Moreover, the validity of gossip is rarely challenged, unlike the typical norm of lively thoughtful debate that surrounds new ideas (eg, whether to prescribe a novel medication).2 Gossip, of course, can also lead to a positive thrill where, for example, a recipient subsequently feels emboldened with passionate enthusiasm to relay the point to others. This means that spreading inaccurate characterizations may be particularly destructive for a listener who is gullible or easily provoked.37 Conversely, gossip can also lead to anxiety about future uncertainties.38
DISCUSSION
This perspective summarizes positive and negative features of gossip drawn from social psychology science on a normally hidden activity. The main benefits in medical care are to support team communication, the specific transmitter, and the individual receiver. Some specific gains are to enhance team cooperation, deter exploitation, signal trust, and convey codes of conduct. Sharing gossip might also promote honest dialogue, foster friendships, facilitate reciprocity, and curtail excessive use of force by a dominant individual. Listening to gossip possibly also reduces loneliness, affirms an innate desire for inclusion, and provides a way to share insights. Of course, gossip has downsides from direct or indirect adverse effects that merit attention and mitigation (Table 2).
A large direct downside of gossip is in propagating damaging misinformation that harms individuals.24 Toxic gossip can wreck relationships, hurt feelings, violate privacy, and manipulate others. Malicious gossip may become further accentuated because of groupthink, polarization, or selfish biases.39 Presumably, these downsides of gossip are sufficiently infrequent because regular people spend substantial time, attention, and effort engaging in gossip.3 In society, healthy gossip that propagates positive information goes by synonyms having a less negative connotation, including socializing, networking, chatting, schmoozing, friendly banter, small talk, and scuttlebutt. The net benefits must be real since one person is often both a transmitter and a receiver of gossip over time.
Another large direct limitation of gossip is that it can magnify social inequities by allowing some people but not others to access hidden information. In essence, receiving gossip is a privilege that is not universally available within a community and depends on social capital.40 Gossip helps strengthen personal bonds, so marginalized individuals can become further disempowered by not receiving gossip. Social exclusion is painful when different individuals realize they are left out of gossip circles. In summary, gossip can provide an unfair advantage because it allows only some people to learn what is going on behind their backs (eg, different hospitalists within the same institution may have differing circles of friendships for different professional advantages).
Gossip is a way to communicate priorities and regulate behavior. Without interpersonal comparisons, clinicians might find themselves adrift in a complex, difficult, and mysterious medical world. Listening to intelligent gossip can also be an effective way to learn lessons that are otherwise difficult to grasp (eg, an impolite comment may be more easily recognized in someone else than in yourself).41 Perhaps this explains why hospital executives gossip about physicians and vice versa.42 Healthy gossip tends to be positive or neutral (not malicious or negative), propagates accurate information (not hurtful falsehoods), and corrects social inequities (not worsening unearned privileges).43 We suggest that a careful practice of healthy gossip may help regulate trust, enhance social bonding, shape how people feel working together, and promote collective benefit.
CLINICAL SCENARIO EPILOGUE
Your colleague spontaneously comments that the chief medical resident is away because of a death in the family. In turn, you realize you were unaware of this personal nuance because the point was unmentioned in the (virtual) staff meeting last week. You thank your colleague for tactfully relaying the point. You also secretly wonder what other interpersonal details you might be missing during the COVID-19 pandemic.
Acknowledgments
The authors thank Cindy Kao, Fizza Manzoor, Sheharyar Raza, Lee Ross, Miriam Shuchman, and William Silverstein for helpful suggestions on specific points.
1. Foster EK. Research on gossip: taxonomy, methods, and future directions. Rev Gen Psychol. 2004;8(2):78-99. https://doi.org/10.1037/1089-2680.8.2.78
2. Eder D, Enke JL. The structure of gossip: opportunities and constraints on collective expression among adolescents. Am Sociol Rev. 1991;56(4):494-508. https://doi.org/10.2307/2096270
3. Robbins ML, Karan A. Who gossips and how in everyday life. Soc Psychol Pers Sci. 2020;11(2):185-195. https://doi.org/10.1177/1948550619837000
4. Nevo O, Nevo B, Derech-Zehavi A. The development of the Tendency to Gossip Questionnaire: construct and concurrent validation for a sample of Israeli college students. Educ Psychol Meas. 1993;53(4):973-981. https://doi.org/10.1177/0013164493053004010
5. Nishi A. Evolution and social epidemiology. Soc Sci Med. 2015;145:132-137. https://doi.org/10.1016/j.socscimed.2015.08.015
6. Redelmeier DA, Ross LD. Practicing medicine with colleagues: pitfalls from social psychology science. J Gen Intern Med. 2019;34(4):624-626. https://doi.org/10.1007/s11606-019-04839-5
7. Baumeister RF, Zhang L, Vohs KD. Gossip as cultural learning. Rev Gen Psychol. 2004;8(2):111-121. https://doi.org/10.1037/1089-2680.8.2.111
8. Kulkarni A. Navigating loneliness in the era of virtual care. N Engl J Med. 2019;380(4):307-309. https://doi.org/10.1056/NEJMp1813713
9. Nowak MA, Sigmund K. Evolution of indirect reciprocity. Nature. 2005;437(7063):1291-1298. https://doi.org/10.1038/nature04131
10. Dunbar RIM. Gossip in evolutionary perspective. Rev Gen Psychol. 2004;8(2):100-110. https://doi.org/10.1037/1089-2680.8.2.100
11. Emler N. A social psychology of reputation. Eur Rev Social Psychol. 2011;1(1):171-193. https://doi.org/10.1080/14792779108401861
12. Arendt F, Forrai M, Findl O. Dealing with negative reviews on physician-rating websites: an experimental test of how physicians can prevent reputational damage via effective response strategies. Soc Sci Med. 2020;266:113422. https://doi.org/10.1016/j.socscimed.2020.113422
13. Seo H. Blah blah blah: the lack of small talk is breaking our brains. The Walrus. April 22, 2021. Updated April 22, 2021. Accessed September 6, 2021. https://thewalrus.ca/blah-blah-blah-the-lack-of-small-talk-is-breaking-our-brains/
14. Houchens N, Tipirneni R. Compassionate communication amid the COVID-19 pandemic. J Hosp Med. 2020;15(7):437-439. https://doi.org/10.12788/jhm.3472
15. Camerer CE. Behavioral Game Theory: Experiments in Strategic Interaction. Princeton University Press; 2003.
16. Sommerfeld RD, Krambeck HJ, Semmann D, Milinski M. Gossip as an alternative for direct observation in games of indirect reciprocity. Proc Natl Acad Sci U S A. 2007;104(44):17435-17440. https://doi.org/10.1073/pnas.0704598104
17. Hendriks A. SoPHIE - Software Platform for Human Interaction Experiments. Working Paper. 2012.
18. Wu J, Balliet D, Van Lange PAM. Gossip versus punishment: the efficiency of reputation to promote and maintain cooperation. Sci Rep. 2016;6:23919. https://doi.org/10.1038/srep23919
19. Milinski M, Semmann D, Krambeck HJ. Reputation helps solve the “tragedy of the commons.” Nature. 2002;415(6870):424-426. https://doi.org/10.1038/415424a
20. Bolton GE, Katok E, Ockenfels A. Cooperation among strangers with limited information about reputation. J Publ Econ. 2005;89(8):1457-1468. https://doi.org/10.1016/j.jpubeco.2004.03.008
21. Seinen I, Schram A. Social status and group norms: indirect reciprocity in a repeated helping experiment. Eur Econ Rev. 2006;50(3):581-602. https://doi.org/10.1016/j.euroecorev.2004.10.005
22. Feinberg M, Willer R, Schultz M. Gossip and ostracism promote cooperation in groups. Psychol Sci. 2014;25(3):656-664. https://doi.org/10.1177/0956797613510184
23. Farley SD. Is gossip power? The inverse relationships between gossip, power, and likability. Eur J Soc Psychol. 2011;41(5):574-579. https://doi.org/10.1002/ejsp.821
24. Wert SR, Salovey P. A social comparison account of gossip. Rev Gen Psychol. 2004;8(2):122-137. https://doi.org/10.1037/1089-2680.8.2.122
25. Peters K, Kashima Y. From social talk to social action: shaping the social triad with emotion sharing. J Pers Soc Psychol. 2007;93(5):780-797. https://doi.org/10.1037/0022-3514.93.5.780
26. Cruz TDD, Beersma B, Dijkstra MTM, Bechtoldt MN. The bright and dark side of gossip for cooperation in groups. Front Psychol. 2019;10:1374. https://doi.org/10.3389/fpsyg.2019.01374
27. Connolly R. The year in gossip. Hazlitt. December 4, 2020. Accessed September 6, 2021. https://hazlitt.net/feature/year-gossip
28. Rosenbluth G, Good BP, Litterer KP, et al. Communicating effectively with hospitalized patients and families during the COVID-19 pandemic. J Hosp Med. 2020;15(7):440-442. https://doi.org/10.12788/jhm.3466
29. Feinberg M, Willer R, Stellar J, Keltner D. The virtues of gossip: reputational information sharing as prosocial behavior. J Pers Soc Psychol. 2012;102(5):1015-1030. https://doi.org/10.1037/a0026650
30. Panchanathan K, Boyd R. Indirect reciprocity can stabilize cooperation without the second-order free rider problem. Nature. 2004;432(7016):499-502. https://doi.org/10.1038/nature02978
31. Suls JM. Gossip as social comparison. J Commun. 1977;27(1):164-168. https://doi.org/10.1111/j.1460-2466.1977.tb01812.x
32. Gottfriend S. The science behind why people gossip—and when it can be a good thing. Time. September 25, 2019. Accessed September 6, 2021. https://time.com/5680457/why-do-people-gossip/
33. Auerbach A, O’Leary KJ, Greysen SR, et al. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15(8):483-488. https://doi.org/10.12788/jhm.3476
34. Skinner BF. Science and Human Behavior. The Macmillan Company; 1953.
35. Andrzejewski ME, Cardinal CD, Field DP, et al. Pigeons’ choices between fixed-interval and random-interval schedules: utility of variability? J Exp Anal Behav. 2005;83(2):129-145. https://doi.org/10.1901/jeab.2005.30-04
36. Kendall SB. Preference for intermittent reinforcement. J Exp Anal Behav. 1974;21(3):463-473. https://doi.org/10.1901/jeab.1974.21-463
37. Redelmeier DA, Ross LD. Pitfalls from psychology science that worsen with practice. J Gen Intern Med. 2020;35(10):3050-3052. https://doi.org/10.1007/s11606-020-05864-5
38. Rosnow RL. Inside rumor: a personal journey. Am Psychol. 1991;46(5):484-496. https://doi.org/10.1037/0003-066X.46.5.484
39. Cinelli M, De Francisci Moreales G, Galeazzi A, Quattrociocchi W, Starnini M. The echo chamber effect on social media. Proc Natl Acad Sci U S A. 2021;118(9):e2023301118. https://doi.org/10.1073/pnas.2023301118
40. Chaikof M, Tannenbaum E, Mathur S, Bodley J, Farrugia M. Approaching gossip and rumor in medical education. J Grad Med Educ. 2019;11(2):239-240. https://doi.org/10.4300/JGME-D-19-00119.1
41. Redelmeier DA, Najeeb U, Etchells EE. Understanding patient personality in medical care: five-factor model. J Gen Intern Med. 2021;36(7):2111-2114. https://doi.org/10.1007/s11606-021-06598-8
42. Ribeiro VE, Blakeley JA. The proactive management of rumor and gossip. J Nurs Adm. 1995;25(6):43-50. https://doi.org/10.1097/00005110-199506000-00010
43. Beersma B, van Kleef GA. Why people gossip: an empirical analysis of social motives, antecedents, and consequences. J Appl Soc Psychol. 2012;42(11):2640-2670. https://doi.org/10.1111/j.1559-1816.2012.00956.x
CLINICAL SCENARIO PROLOGUE
You are signing over to a colleague on the COVID-19 inpatient hospital ward. You are stressed after having failed to reach the chief medical resident who did not respond despite repeated texts. You think about mentioning this apparent professional lapse to your colleague. You pause, however, because you are uncertain about the appropriate norm, hesitant around finding the right words, and unsure about a mutual feeling of camaraderie.
OVERVIEW
Lay and scientific perspectives about gossip diverge widely. Lay definitions of gossip generally include malicious, salacious, immoral, trivial, or unfair comments that attack someone else’s reputation. Scientific definitions of gossip, in contrast, also include neutral or positive social information intended to align group dynamics.1 The common feature of both is that the named individual is not present to hear about themselves.2 A further commonality is that gossip involves informal assessments loaded with subjective judgments, unlike professional comments about patients from clinicians providing care. In contrast to stereotype remarks, gossip focuses on a specific person and not a group.
Gossip is widespread. A recent study in nonhospital settings suggests nearly all adults engage in gossip during normal interactions, averaging 52 minutes on a typical day.3 Most gossip is neutral (74%) rather than negative or positive. The content usually (92%) concerns relationships, and the typical person identified (82%) is an acquaintance. Some of the potential benefits include conveying information for social learning, defining what is socially acceptable, or promoting personal connections. Men and women gossip to nearly the same degree.4 Indeed, evolutionary theory suggests gossip is not deviant behavior and arises even in small hunter-gatherer communities.5Social psychology science provides some insights on fundamental principles of gossip that may be relevant to clinicians in medicine.6 In this article, we review three important findings from social psychology science relevant to team cooperation, the specific transmitter, and the individual receiver (Table 1). Clinicians working in groups may benefit from recognizing the prosocial function of healthy gossip and avoiding the antisocial adverse effects of harmful gossip.7 At a time when work-related conversations have radically shifted online,8 hospitalists need to be aware of positives and pitfalls of gossip to help provide effective medical care and avoid adverse events.
GOSSIP AS TEAM COMMUNICATION
Large team endeavors often require social signals to coordinate people.9 Gossip helps groups establish reputations, monitor their members, deter antisocial behavior, and protect newcomers from exploitation.10 Sharing social information can also indirectly promote cooperation because individuals place a high value on their own reputations and want to avoid embarrassment.11,12 The absence of gossip, in contrast, may lead individuals to be oblivious to team expectations and fail to do their fair share. A lack of gossip, in particular, may add to inefficiencies during the COVID-19 pandemic since exchanging gossip seems to feel awkward over email or other digital channels (albeit a chat function for side conversations in virtual meetings is a partial substitute).13,14
A paradigm for testing the positive effects of gossip involves a trust game where participants consider making small contributions for later rewards in recurrent rounds of cooperation.15-17 In one online study of volunteers, for example, individuals contributed to a group account and gained rewards equal to a doubling of total contributions shared over everyone equally (even those contributing nothing).18 Half the experiments allowed participants to send notes about other participants, whereas the other experiments allowed no such “gossip.” As predicted, gossip increased the proportion contributed (40% vs 32%, P = .020) and average total reward (64 vs 56, P = .002). In this and other studies of healthy volunteers, gossip builds trust and increases gains for the entire group.19-22
Effective medical practice inside hospitals often involves constructive gossip for pointers on how to behave (eg, how quickly to reply to a text message from the ward pharmacist). The blend of objective facts with subjective opinion provides a compelling message otherwise lacking from institutional guidelines or directives on how not to behave (eg, how quickly to complete an annual report with an arbitrary deadline). Gossip is the antithesis of a cursory interaction between strangers and is also less awkward than open flattery or public ridicule that may occur when the third person is in earshot.23 Even negative social comparisons can be constructive to listeners since people want to know how to avoid bad gossip about themselves in a world with changing morality.24
GOSSIP AND THE TRANSMITTER
Gossip can provide a distinct emotional benefit for the gossiper as a form of self-expression, an exercise of justice, and a validation of one’s perspective.25 Consider, for example, witnessing an antisocial act that leads to subsequent feelings of unfairness yet having no way to communicate personal dissatisfaction. Similarly, expressing prosocial gossip may help relieve some of the annoyance after a hassle (eg, talking with a friend after encountering a new onerous hospital protocol). The sharing of gossip might also help bolster solidarity after an offense (eg, talking with a friend on how to deal with another warning from health records).26 In contrast, lost opportunities to gossip about unfairness could be exacerbating the social isolation and emotional distress of the COVID-19 pandemic.27,28
A rigorous example of the emotional benefits of expressing gossip involves undergraduates witnessing staged behavior under laboratory conditions where one actor appeared to exploit the generosity of another actor.29 By random assignment, half the participants had an opportunity to gossip, and the other half had no such opportunity. All participants reacted to the antisocial behavior by feeling frustrated (self-report survey scale of 0-100, where higher scores indicate worse frustration). Importantly, almost all chose to engage in gossip when feasible, and those who had the opportunity to gossip experienced more relief than those who had no opportunity (absolute improvement in frustration scores, 9.69 vs 0.16; P < .01). Evidentially, engaging in prosocial gossip can sometimes provide solace.
Sharing gossip might strengthen social bonds, bolster self-esteem, promote personal power, elicit reciprocal favors, or telegraph the presence of a larger network of personal connections. Gossip is cheap and efficient compared with peer-sanctioning or formal sanctioning to control behavior.30 Airing grievances through gossip may also solve some social dilemmas more easily than channeling messages through institutional reporting structures or formal performance reviews. Gossip has another advantage of raising delicate comparative judgments without the discomfort of direct confrontation (eg, defining the appropriate level of detail for a case presentation is perhaps best done by identifying those who are judged too verbose).31
GOSSIP AND THE RECEIVER
People tend to enjoy listening to gossip despite the uneven quality where some comments are more valuable than others. The receiver, therefore, faces an irregular payoff similar to random intermittent reinforcement. Ironically, random intermittent reinforcement can be particularly addictive when compared with steady rewards with predictable payoffs. This includes cases where gossip conveys good news that helps elevate, inspire, or motivate the receiver. The thirst for more gossip may partially explain why receivers keep seeking gossip despite knowing the material may be unimportant. The shortfall of enticing gossip might also be another factor adding to a feeling of loneliness that prevails widely during the COVID-19 pandemic.32,33
Classic research on reinforcement includes experiments examining operant conditioning for creating addiction.34,35 An important distinction is the contrast between random reinforcement (eg, variable reward akin to gambling on a roulette wheel) and consistent reinforcement (eg, regular pay akin to a steady salary each week). In a study of pigeons trained to peck a lever for food, for example, random reinforcement resulted in twice the response compared with consistent reinforcement (despite an equalized total amount of food received).36 Moreover, random reinforcement was hard to extinguish, and the behavior continued long after all food ended. In general, random compared with consistent reinforcement tended to cause a more intense and persistent change of behavior.
The inconsistent quality makes the prospect of new, exciting gossip seem nearly impossible to resist; indeed, gossip from any source is surprisingly tantalizing. Moreover, the validity of gossip is rarely challenged, unlike the typical norm of lively thoughtful debate that surrounds new ideas (eg, whether to prescribe a novel medication).2 Gossip, of course, can also lead to a positive thrill where, for example, a recipient subsequently feels emboldened with passionate enthusiasm to relay the point to others. This means that spreading inaccurate characterizations may be particularly destructive for a listener who is gullible or easily provoked.37 Conversely, gossip can also lead to anxiety about future uncertainties.38
DISCUSSION
This perspective summarizes positive and negative features of gossip drawn from social psychology science on a normally hidden activity. The main benefits in medical care are to support team communication, the specific transmitter, and the individual receiver. Some specific gains are to enhance team cooperation, deter exploitation, signal trust, and convey codes of conduct. Sharing gossip might also promote honest dialogue, foster friendships, facilitate reciprocity, and curtail excessive use of force by a dominant individual. Listening to gossip possibly also reduces loneliness, affirms an innate desire for inclusion, and provides a way to share insights. Of course, gossip has downsides from direct or indirect adverse effects that merit attention and mitigation (Table 2).
A large direct downside of gossip is in propagating damaging misinformation that harms individuals.24 Toxic gossip can wreck relationships, hurt feelings, violate privacy, and manipulate others. Malicious gossip may become further accentuated because of groupthink, polarization, or selfish biases.39 Presumably, these downsides of gossip are sufficiently infrequent because regular people spend substantial time, attention, and effort engaging in gossip.3 In society, healthy gossip that propagates positive information goes by synonyms having a less negative connotation, including socializing, networking, chatting, schmoozing, friendly banter, small talk, and scuttlebutt. The net benefits must be real since one person is often both a transmitter and a receiver of gossip over time.
Another large direct limitation of gossip is that it can magnify social inequities by allowing some people but not others to access hidden information. In essence, receiving gossip is a privilege that is not universally available within a community and depends on social capital.40 Gossip helps strengthen personal bonds, so marginalized individuals can become further disempowered by not receiving gossip. Social exclusion is painful when different individuals realize they are left out of gossip circles. In summary, gossip can provide an unfair advantage because it allows only some people to learn what is going on behind their backs (eg, different hospitalists within the same institution may have differing circles of friendships for different professional advantages).
Gossip is a way to communicate priorities and regulate behavior. Without interpersonal comparisons, clinicians might find themselves adrift in a complex, difficult, and mysterious medical world. Listening to intelligent gossip can also be an effective way to learn lessons that are otherwise difficult to grasp (eg, an impolite comment may be more easily recognized in someone else than in yourself).41 Perhaps this explains why hospital executives gossip about physicians and vice versa.42 Healthy gossip tends to be positive or neutral (not malicious or negative), propagates accurate information (not hurtful falsehoods), and corrects social inequities (not worsening unearned privileges).43 We suggest that a careful practice of healthy gossip may help regulate trust, enhance social bonding, shape how people feel working together, and promote collective benefit.
CLINICAL SCENARIO EPILOGUE
Your colleague spontaneously comments that the chief medical resident is away because of a death in the family. In turn, you realize you were unaware of this personal nuance because the point was unmentioned in the (virtual) staff meeting last week. You thank your colleague for tactfully relaying the point. You also secretly wonder what other interpersonal details you might be missing during the COVID-19 pandemic.
Acknowledgments
The authors thank Cindy Kao, Fizza Manzoor, Sheharyar Raza, Lee Ross, Miriam Shuchman, and William Silverstein for helpful suggestions on specific points.
CLINICAL SCENARIO PROLOGUE
You are signing over to a colleague on the COVID-19 inpatient hospital ward. You are stressed after having failed to reach the chief medical resident who did not respond despite repeated texts. You think about mentioning this apparent professional lapse to your colleague. You pause, however, because you are uncertain about the appropriate norm, hesitant around finding the right words, and unsure about a mutual feeling of camaraderie.
OVERVIEW
Lay and scientific perspectives about gossip diverge widely. Lay definitions of gossip generally include malicious, salacious, immoral, trivial, or unfair comments that attack someone else’s reputation. Scientific definitions of gossip, in contrast, also include neutral or positive social information intended to align group dynamics.1 The common feature of both is that the named individual is not present to hear about themselves.2 A further commonality is that gossip involves informal assessments loaded with subjective judgments, unlike professional comments about patients from clinicians providing care. In contrast to stereotype remarks, gossip focuses on a specific person and not a group.
Gossip is widespread. A recent study in nonhospital settings suggests nearly all adults engage in gossip during normal interactions, averaging 52 minutes on a typical day.3 Most gossip is neutral (74%) rather than negative or positive. The content usually (92%) concerns relationships, and the typical person identified (82%) is an acquaintance. Some of the potential benefits include conveying information for social learning, defining what is socially acceptable, or promoting personal connections. Men and women gossip to nearly the same degree.4 Indeed, evolutionary theory suggests gossip is not deviant behavior and arises even in small hunter-gatherer communities.5Social psychology science provides some insights on fundamental principles of gossip that may be relevant to clinicians in medicine.6 In this article, we review three important findings from social psychology science relevant to team cooperation, the specific transmitter, and the individual receiver (Table 1). Clinicians working in groups may benefit from recognizing the prosocial function of healthy gossip and avoiding the antisocial adverse effects of harmful gossip.7 At a time when work-related conversations have radically shifted online,8 hospitalists need to be aware of positives and pitfalls of gossip to help provide effective medical care and avoid adverse events.
GOSSIP AS TEAM COMMUNICATION
Large team endeavors often require social signals to coordinate people.9 Gossip helps groups establish reputations, monitor their members, deter antisocial behavior, and protect newcomers from exploitation.10 Sharing social information can also indirectly promote cooperation because individuals place a high value on their own reputations and want to avoid embarrassment.11,12 The absence of gossip, in contrast, may lead individuals to be oblivious to team expectations and fail to do their fair share. A lack of gossip, in particular, may add to inefficiencies during the COVID-19 pandemic since exchanging gossip seems to feel awkward over email or other digital channels (albeit a chat function for side conversations in virtual meetings is a partial substitute).13,14
A paradigm for testing the positive effects of gossip involves a trust game where participants consider making small contributions for later rewards in recurrent rounds of cooperation.15-17 In one online study of volunteers, for example, individuals contributed to a group account and gained rewards equal to a doubling of total contributions shared over everyone equally (even those contributing nothing).18 Half the experiments allowed participants to send notes about other participants, whereas the other experiments allowed no such “gossip.” As predicted, gossip increased the proportion contributed (40% vs 32%, P = .020) and average total reward (64 vs 56, P = .002). In this and other studies of healthy volunteers, gossip builds trust and increases gains for the entire group.19-22
Effective medical practice inside hospitals often involves constructive gossip for pointers on how to behave (eg, how quickly to reply to a text message from the ward pharmacist). The blend of objective facts with subjective opinion provides a compelling message otherwise lacking from institutional guidelines or directives on how not to behave (eg, how quickly to complete an annual report with an arbitrary deadline). Gossip is the antithesis of a cursory interaction between strangers and is also less awkward than open flattery or public ridicule that may occur when the third person is in earshot.23 Even negative social comparisons can be constructive to listeners since people want to know how to avoid bad gossip about themselves in a world with changing morality.24
GOSSIP AND THE TRANSMITTER
Gossip can provide a distinct emotional benefit for the gossiper as a form of self-expression, an exercise of justice, and a validation of one’s perspective.25 Consider, for example, witnessing an antisocial act that leads to subsequent feelings of unfairness yet having no way to communicate personal dissatisfaction. Similarly, expressing prosocial gossip may help relieve some of the annoyance after a hassle (eg, talking with a friend after encountering a new onerous hospital protocol). The sharing of gossip might also help bolster solidarity after an offense (eg, talking with a friend on how to deal with another warning from health records).26 In contrast, lost opportunities to gossip about unfairness could be exacerbating the social isolation and emotional distress of the COVID-19 pandemic.27,28
A rigorous example of the emotional benefits of expressing gossip involves undergraduates witnessing staged behavior under laboratory conditions where one actor appeared to exploit the generosity of another actor.29 By random assignment, half the participants had an opportunity to gossip, and the other half had no such opportunity. All participants reacted to the antisocial behavior by feeling frustrated (self-report survey scale of 0-100, where higher scores indicate worse frustration). Importantly, almost all chose to engage in gossip when feasible, and those who had the opportunity to gossip experienced more relief than those who had no opportunity (absolute improvement in frustration scores, 9.69 vs 0.16; P < .01). Evidentially, engaging in prosocial gossip can sometimes provide solace.
Sharing gossip might strengthen social bonds, bolster self-esteem, promote personal power, elicit reciprocal favors, or telegraph the presence of a larger network of personal connections. Gossip is cheap and efficient compared with peer-sanctioning or formal sanctioning to control behavior.30 Airing grievances through gossip may also solve some social dilemmas more easily than channeling messages through institutional reporting structures or formal performance reviews. Gossip has another advantage of raising delicate comparative judgments without the discomfort of direct confrontation (eg, defining the appropriate level of detail for a case presentation is perhaps best done by identifying those who are judged too verbose).31
GOSSIP AND THE RECEIVER
People tend to enjoy listening to gossip despite the uneven quality where some comments are more valuable than others. The receiver, therefore, faces an irregular payoff similar to random intermittent reinforcement. Ironically, random intermittent reinforcement can be particularly addictive when compared with steady rewards with predictable payoffs. This includes cases where gossip conveys good news that helps elevate, inspire, or motivate the receiver. The thirst for more gossip may partially explain why receivers keep seeking gossip despite knowing the material may be unimportant. The shortfall of enticing gossip might also be another factor adding to a feeling of loneliness that prevails widely during the COVID-19 pandemic.32,33
Classic research on reinforcement includes experiments examining operant conditioning for creating addiction.34,35 An important distinction is the contrast between random reinforcement (eg, variable reward akin to gambling on a roulette wheel) and consistent reinforcement (eg, regular pay akin to a steady salary each week). In a study of pigeons trained to peck a lever for food, for example, random reinforcement resulted in twice the response compared with consistent reinforcement (despite an equalized total amount of food received).36 Moreover, random reinforcement was hard to extinguish, and the behavior continued long after all food ended. In general, random compared with consistent reinforcement tended to cause a more intense and persistent change of behavior.
The inconsistent quality makes the prospect of new, exciting gossip seem nearly impossible to resist; indeed, gossip from any source is surprisingly tantalizing. Moreover, the validity of gossip is rarely challenged, unlike the typical norm of lively thoughtful debate that surrounds new ideas (eg, whether to prescribe a novel medication).2 Gossip, of course, can also lead to a positive thrill where, for example, a recipient subsequently feels emboldened with passionate enthusiasm to relay the point to others. This means that spreading inaccurate characterizations may be particularly destructive for a listener who is gullible or easily provoked.37 Conversely, gossip can also lead to anxiety about future uncertainties.38
DISCUSSION
This perspective summarizes positive and negative features of gossip drawn from social psychology science on a normally hidden activity. The main benefits in medical care are to support team communication, the specific transmitter, and the individual receiver. Some specific gains are to enhance team cooperation, deter exploitation, signal trust, and convey codes of conduct. Sharing gossip might also promote honest dialogue, foster friendships, facilitate reciprocity, and curtail excessive use of force by a dominant individual. Listening to gossip possibly also reduces loneliness, affirms an innate desire for inclusion, and provides a way to share insights. Of course, gossip has downsides from direct or indirect adverse effects that merit attention and mitigation (Table 2).
A large direct downside of gossip is in propagating damaging misinformation that harms individuals.24 Toxic gossip can wreck relationships, hurt feelings, violate privacy, and manipulate others. Malicious gossip may become further accentuated because of groupthink, polarization, or selfish biases.39 Presumably, these downsides of gossip are sufficiently infrequent because regular people spend substantial time, attention, and effort engaging in gossip.3 In society, healthy gossip that propagates positive information goes by synonyms having a less negative connotation, including socializing, networking, chatting, schmoozing, friendly banter, small talk, and scuttlebutt. The net benefits must be real since one person is often both a transmitter and a receiver of gossip over time.
Another large direct limitation of gossip is that it can magnify social inequities by allowing some people but not others to access hidden information. In essence, receiving gossip is a privilege that is not universally available within a community and depends on social capital.40 Gossip helps strengthen personal bonds, so marginalized individuals can become further disempowered by not receiving gossip. Social exclusion is painful when different individuals realize they are left out of gossip circles. In summary, gossip can provide an unfair advantage because it allows only some people to learn what is going on behind their backs (eg, different hospitalists within the same institution may have differing circles of friendships for different professional advantages).
Gossip is a way to communicate priorities and regulate behavior. Without interpersonal comparisons, clinicians might find themselves adrift in a complex, difficult, and mysterious medical world. Listening to intelligent gossip can also be an effective way to learn lessons that are otherwise difficult to grasp (eg, an impolite comment may be more easily recognized in someone else than in yourself).41 Perhaps this explains why hospital executives gossip about physicians and vice versa.42 Healthy gossip tends to be positive or neutral (not malicious or negative), propagates accurate information (not hurtful falsehoods), and corrects social inequities (not worsening unearned privileges).43 We suggest that a careful practice of healthy gossip may help regulate trust, enhance social bonding, shape how people feel working together, and promote collective benefit.
CLINICAL SCENARIO EPILOGUE
Your colleague spontaneously comments that the chief medical resident is away because of a death in the family. In turn, you realize you were unaware of this personal nuance because the point was unmentioned in the (virtual) staff meeting last week. You thank your colleague for tactfully relaying the point. You also secretly wonder what other interpersonal details you might be missing during the COVID-19 pandemic.
Acknowledgments
The authors thank Cindy Kao, Fizza Manzoor, Sheharyar Raza, Lee Ross, Miriam Shuchman, and William Silverstein for helpful suggestions on specific points.
1. Foster EK. Research on gossip: taxonomy, methods, and future directions. Rev Gen Psychol. 2004;8(2):78-99. https://doi.org/10.1037/1089-2680.8.2.78
2. Eder D, Enke JL. The structure of gossip: opportunities and constraints on collective expression among adolescents. Am Sociol Rev. 1991;56(4):494-508. https://doi.org/10.2307/2096270
3. Robbins ML, Karan A. Who gossips and how in everyday life. Soc Psychol Pers Sci. 2020;11(2):185-195. https://doi.org/10.1177/1948550619837000
4. Nevo O, Nevo B, Derech-Zehavi A. The development of the Tendency to Gossip Questionnaire: construct and concurrent validation for a sample of Israeli college students. Educ Psychol Meas. 1993;53(4):973-981. https://doi.org/10.1177/0013164493053004010
5. Nishi A. Evolution and social epidemiology. Soc Sci Med. 2015;145:132-137. https://doi.org/10.1016/j.socscimed.2015.08.015
6. Redelmeier DA, Ross LD. Practicing medicine with colleagues: pitfalls from social psychology science. J Gen Intern Med. 2019;34(4):624-626. https://doi.org/10.1007/s11606-019-04839-5
7. Baumeister RF, Zhang L, Vohs KD. Gossip as cultural learning. Rev Gen Psychol. 2004;8(2):111-121. https://doi.org/10.1037/1089-2680.8.2.111
8. Kulkarni A. Navigating loneliness in the era of virtual care. N Engl J Med. 2019;380(4):307-309. https://doi.org/10.1056/NEJMp1813713
9. Nowak MA, Sigmund K. Evolution of indirect reciprocity. Nature. 2005;437(7063):1291-1298. https://doi.org/10.1038/nature04131
10. Dunbar RIM. Gossip in evolutionary perspective. Rev Gen Psychol. 2004;8(2):100-110. https://doi.org/10.1037/1089-2680.8.2.100
11. Emler N. A social psychology of reputation. Eur Rev Social Psychol. 2011;1(1):171-193. https://doi.org/10.1080/14792779108401861
12. Arendt F, Forrai M, Findl O. Dealing with negative reviews on physician-rating websites: an experimental test of how physicians can prevent reputational damage via effective response strategies. Soc Sci Med. 2020;266:113422. https://doi.org/10.1016/j.socscimed.2020.113422
13. Seo H. Blah blah blah: the lack of small talk is breaking our brains. The Walrus. April 22, 2021. Updated April 22, 2021. Accessed September 6, 2021. https://thewalrus.ca/blah-blah-blah-the-lack-of-small-talk-is-breaking-our-brains/
14. Houchens N, Tipirneni R. Compassionate communication amid the COVID-19 pandemic. J Hosp Med. 2020;15(7):437-439. https://doi.org/10.12788/jhm.3472
15. Camerer CE. Behavioral Game Theory: Experiments in Strategic Interaction. Princeton University Press; 2003.
16. Sommerfeld RD, Krambeck HJ, Semmann D, Milinski M. Gossip as an alternative for direct observation in games of indirect reciprocity. Proc Natl Acad Sci U S A. 2007;104(44):17435-17440. https://doi.org/10.1073/pnas.0704598104
17. Hendriks A. SoPHIE - Software Platform for Human Interaction Experiments. Working Paper. 2012.
18. Wu J, Balliet D, Van Lange PAM. Gossip versus punishment: the efficiency of reputation to promote and maintain cooperation. Sci Rep. 2016;6:23919. https://doi.org/10.1038/srep23919
19. Milinski M, Semmann D, Krambeck HJ. Reputation helps solve the “tragedy of the commons.” Nature. 2002;415(6870):424-426. https://doi.org/10.1038/415424a
20. Bolton GE, Katok E, Ockenfels A. Cooperation among strangers with limited information about reputation. J Publ Econ. 2005;89(8):1457-1468. https://doi.org/10.1016/j.jpubeco.2004.03.008
21. Seinen I, Schram A. Social status and group norms: indirect reciprocity in a repeated helping experiment. Eur Econ Rev. 2006;50(3):581-602. https://doi.org/10.1016/j.euroecorev.2004.10.005
22. Feinberg M, Willer R, Schultz M. Gossip and ostracism promote cooperation in groups. Psychol Sci. 2014;25(3):656-664. https://doi.org/10.1177/0956797613510184
23. Farley SD. Is gossip power? The inverse relationships between gossip, power, and likability. Eur J Soc Psychol. 2011;41(5):574-579. https://doi.org/10.1002/ejsp.821
24. Wert SR, Salovey P. A social comparison account of gossip. Rev Gen Psychol. 2004;8(2):122-137. https://doi.org/10.1037/1089-2680.8.2.122
25. Peters K, Kashima Y. From social talk to social action: shaping the social triad with emotion sharing. J Pers Soc Psychol. 2007;93(5):780-797. https://doi.org/10.1037/0022-3514.93.5.780
26. Cruz TDD, Beersma B, Dijkstra MTM, Bechtoldt MN. The bright and dark side of gossip for cooperation in groups. Front Psychol. 2019;10:1374. https://doi.org/10.3389/fpsyg.2019.01374
27. Connolly R. The year in gossip. Hazlitt. December 4, 2020. Accessed September 6, 2021. https://hazlitt.net/feature/year-gossip
28. Rosenbluth G, Good BP, Litterer KP, et al. Communicating effectively with hospitalized patients and families during the COVID-19 pandemic. J Hosp Med. 2020;15(7):440-442. https://doi.org/10.12788/jhm.3466
29. Feinberg M, Willer R, Stellar J, Keltner D. The virtues of gossip: reputational information sharing as prosocial behavior. J Pers Soc Psychol. 2012;102(5):1015-1030. https://doi.org/10.1037/a0026650
30. Panchanathan K, Boyd R. Indirect reciprocity can stabilize cooperation without the second-order free rider problem. Nature. 2004;432(7016):499-502. https://doi.org/10.1038/nature02978
31. Suls JM. Gossip as social comparison. J Commun. 1977;27(1):164-168. https://doi.org/10.1111/j.1460-2466.1977.tb01812.x
32. Gottfriend S. The science behind why people gossip—and when it can be a good thing. Time. September 25, 2019. Accessed September 6, 2021. https://time.com/5680457/why-do-people-gossip/
33. Auerbach A, O’Leary KJ, Greysen SR, et al. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15(8):483-488. https://doi.org/10.12788/jhm.3476
34. Skinner BF. Science and Human Behavior. The Macmillan Company; 1953.
35. Andrzejewski ME, Cardinal CD, Field DP, et al. Pigeons’ choices between fixed-interval and random-interval schedules: utility of variability? J Exp Anal Behav. 2005;83(2):129-145. https://doi.org/10.1901/jeab.2005.30-04
36. Kendall SB. Preference for intermittent reinforcement. J Exp Anal Behav. 1974;21(3):463-473. https://doi.org/10.1901/jeab.1974.21-463
37. Redelmeier DA, Ross LD. Pitfalls from psychology science that worsen with practice. J Gen Intern Med. 2020;35(10):3050-3052. https://doi.org/10.1007/s11606-020-05864-5
38. Rosnow RL. Inside rumor: a personal journey. Am Psychol. 1991;46(5):484-496. https://doi.org/10.1037/0003-066X.46.5.484
39. Cinelli M, De Francisci Moreales G, Galeazzi A, Quattrociocchi W, Starnini M. The echo chamber effect on social media. Proc Natl Acad Sci U S A. 2021;118(9):e2023301118. https://doi.org/10.1073/pnas.2023301118
40. Chaikof M, Tannenbaum E, Mathur S, Bodley J, Farrugia M. Approaching gossip and rumor in medical education. J Grad Med Educ. 2019;11(2):239-240. https://doi.org/10.4300/JGME-D-19-00119.1
41. Redelmeier DA, Najeeb U, Etchells EE. Understanding patient personality in medical care: five-factor model. J Gen Intern Med. 2021;36(7):2111-2114. https://doi.org/10.1007/s11606-021-06598-8
42. Ribeiro VE, Blakeley JA. The proactive management of rumor and gossip. J Nurs Adm. 1995;25(6):43-50. https://doi.org/10.1097/00005110-199506000-00010
43. Beersma B, van Kleef GA. Why people gossip: an empirical analysis of social motives, antecedents, and consequences. J Appl Soc Psychol. 2012;42(11):2640-2670. https://doi.org/10.1111/j.1559-1816.2012.00956.x
1. Foster EK. Research on gossip: taxonomy, methods, and future directions. Rev Gen Psychol. 2004;8(2):78-99. https://doi.org/10.1037/1089-2680.8.2.78
2. Eder D, Enke JL. The structure of gossip: opportunities and constraints on collective expression among adolescents. Am Sociol Rev. 1991;56(4):494-508. https://doi.org/10.2307/2096270
3. Robbins ML, Karan A. Who gossips and how in everyday life. Soc Psychol Pers Sci. 2020;11(2):185-195. https://doi.org/10.1177/1948550619837000
4. Nevo O, Nevo B, Derech-Zehavi A. The development of the Tendency to Gossip Questionnaire: construct and concurrent validation for a sample of Israeli college students. Educ Psychol Meas. 1993;53(4):973-981. https://doi.org/10.1177/0013164493053004010
5. Nishi A. Evolution and social epidemiology. Soc Sci Med. 2015;145:132-137. https://doi.org/10.1016/j.socscimed.2015.08.015
6. Redelmeier DA, Ross LD. Practicing medicine with colleagues: pitfalls from social psychology science. J Gen Intern Med. 2019;34(4):624-626. https://doi.org/10.1007/s11606-019-04839-5
7. Baumeister RF, Zhang L, Vohs KD. Gossip as cultural learning. Rev Gen Psychol. 2004;8(2):111-121. https://doi.org/10.1037/1089-2680.8.2.111
8. Kulkarni A. Navigating loneliness in the era of virtual care. N Engl J Med. 2019;380(4):307-309. https://doi.org/10.1056/NEJMp1813713
9. Nowak MA, Sigmund K. Evolution of indirect reciprocity. Nature. 2005;437(7063):1291-1298. https://doi.org/10.1038/nature04131
10. Dunbar RIM. Gossip in evolutionary perspective. Rev Gen Psychol. 2004;8(2):100-110. https://doi.org/10.1037/1089-2680.8.2.100
11. Emler N. A social psychology of reputation. Eur Rev Social Psychol. 2011;1(1):171-193. https://doi.org/10.1080/14792779108401861
12. Arendt F, Forrai M, Findl O. Dealing with negative reviews on physician-rating websites: an experimental test of how physicians can prevent reputational damage via effective response strategies. Soc Sci Med. 2020;266:113422. https://doi.org/10.1016/j.socscimed.2020.113422
13. Seo H. Blah blah blah: the lack of small talk is breaking our brains. The Walrus. April 22, 2021. Updated April 22, 2021. Accessed September 6, 2021. https://thewalrus.ca/blah-blah-blah-the-lack-of-small-talk-is-breaking-our-brains/
14. Houchens N, Tipirneni R. Compassionate communication amid the COVID-19 pandemic. J Hosp Med. 2020;15(7):437-439. https://doi.org/10.12788/jhm.3472
15. Camerer CE. Behavioral Game Theory: Experiments in Strategic Interaction. Princeton University Press; 2003.
16. Sommerfeld RD, Krambeck HJ, Semmann D, Milinski M. Gossip as an alternative for direct observation in games of indirect reciprocity. Proc Natl Acad Sci U S A. 2007;104(44):17435-17440. https://doi.org/10.1073/pnas.0704598104
17. Hendriks A. SoPHIE - Software Platform for Human Interaction Experiments. Working Paper. 2012.
18. Wu J, Balliet D, Van Lange PAM. Gossip versus punishment: the efficiency of reputation to promote and maintain cooperation. Sci Rep. 2016;6:23919. https://doi.org/10.1038/srep23919
19. Milinski M, Semmann D, Krambeck HJ. Reputation helps solve the “tragedy of the commons.” Nature. 2002;415(6870):424-426. https://doi.org/10.1038/415424a
20. Bolton GE, Katok E, Ockenfels A. Cooperation among strangers with limited information about reputation. J Publ Econ. 2005;89(8):1457-1468. https://doi.org/10.1016/j.jpubeco.2004.03.008
21. Seinen I, Schram A. Social status and group norms: indirect reciprocity in a repeated helping experiment. Eur Econ Rev. 2006;50(3):581-602. https://doi.org/10.1016/j.euroecorev.2004.10.005
22. Feinberg M, Willer R, Schultz M. Gossip and ostracism promote cooperation in groups. Psychol Sci. 2014;25(3):656-664. https://doi.org/10.1177/0956797613510184
23. Farley SD. Is gossip power? The inverse relationships between gossip, power, and likability. Eur J Soc Psychol. 2011;41(5):574-579. https://doi.org/10.1002/ejsp.821
24. Wert SR, Salovey P. A social comparison account of gossip. Rev Gen Psychol. 2004;8(2):122-137. https://doi.org/10.1037/1089-2680.8.2.122
25. Peters K, Kashima Y. From social talk to social action: shaping the social triad with emotion sharing. J Pers Soc Psychol. 2007;93(5):780-797. https://doi.org/10.1037/0022-3514.93.5.780
26. Cruz TDD, Beersma B, Dijkstra MTM, Bechtoldt MN. The bright and dark side of gossip for cooperation in groups. Front Psychol. 2019;10:1374. https://doi.org/10.3389/fpsyg.2019.01374
27. Connolly R. The year in gossip. Hazlitt. December 4, 2020. Accessed September 6, 2021. https://hazlitt.net/feature/year-gossip
28. Rosenbluth G, Good BP, Litterer KP, et al. Communicating effectively with hospitalized patients and families during the COVID-19 pandemic. J Hosp Med. 2020;15(7):440-442. https://doi.org/10.12788/jhm.3466
29. Feinberg M, Willer R, Stellar J, Keltner D. The virtues of gossip: reputational information sharing as prosocial behavior. J Pers Soc Psychol. 2012;102(5):1015-1030. https://doi.org/10.1037/a0026650
30. Panchanathan K, Boyd R. Indirect reciprocity can stabilize cooperation without the second-order free rider problem. Nature. 2004;432(7016):499-502. https://doi.org/10.1038/nature02978
31. Suls JM. Gossip as social comparison. J Commun. 1977;27(1):164-168. https://doi.org/10.1111/j.1460-2466.1977.tb01812.x
32. Gottfriend S. The science behind why people gossip—and when it can be a good thing. Time. September 25, 2019. Accessed September 6, 2021. https://time.com/5680457/why-do-people-gossip/
33. Auerbach A, O’Leary KJ, Greysen SR, et al. Hospital ward adaptation during the COVID-19 pandemic: a national survey of academic medical centers. J Hosp Med. 2020;15(8):483-488. https://doi.org/10.12788/jhm.3476
34. Skinner BF. Science and Human Behavior. The Macmillan Company; 1953.
35. Andrzejewski ME, Cardinal CD, Field DP, et al. Pigeons’ choices between fixed-interval and random-interval schedules: utility of variability? J Exp Anal Behav. 2005;83(2):129-145. https://doi.org/10.1901/jeab.2005.30-04
36. Kendall SB. Preference for intermittent reinforcement. J Exp Anal Behav. 1974;21(3):463-473. https://doi.org/10.1901/jeab.1974.21-463
37. Redelmeier DA, Ross LD. Pitfalls from psychology science that worsen with practice. J Gen Intern Med. 2020;35(10):3050-3052. https://doi.org/10.1007/s11606-020-05864-5
38. Rosnow RL. Inside rumor: a personal journey. Am Psychol. 1991;46(5):484-496. https://doi.org/10.1037/0003-066X.46.5.484
39. Cinelli M, De Francisci Moreales G, Galeazzi A, Quattrociocchi W, Starnini M. The echo chamber effect on social media. Proc Natl Acad Sci U S A. 2021;118(9):e2023301118. https://doi.org/10.1073/pnas.2023301118
40. Chaikof M, Tannenbaum E, Mathur S, Bodley J, Farrugia M. Approaching gossip and rumor in medical education. J Grad Med Educ. 2019;11(2):239-240. https://doi.org/10.4300/JGME-D-19-00119.1
41. Redelmeier DA, Najeeb U, Etchells EE. Understanding patient personality in medical care: five-factor model. J Gen Intern Med. 2021;36(7):2111-2114. https://doi.org/10.1007/s11606-021-06598-8
42. Ribeiro VE, Blakeley JA. The proactive management of rumor and gossip. J Nurs Adm. 1995;25(6):43-50. https://doi.org/10.1097/00005110-199506000-00010
43. Beersma B, van Kleef GA. Why people gossip: an empirical analysis of social motives, antecedents, and consequences. J Appl Soc Psychol. 2012;42(11):2640-2670. https://doi.org/10.1111/j.1559-1816.2012.00956.x
© 2021 Society of Hospital Medicine
Improving Healthcare Access for Patients With Limited English Proficiency
Patients whose primary language is not English and who have a limited ability to read, speak, write, or understand English experience worse healthcare access than their English-speaking counterparts, highlighted by fewer healthcare visits and filled prescription medications.1 These patients with limited English proficiency (LEP) face additional barriers to quality healthcare during the COVID-19 pandemic, including lower rates of telehealth use,2 lower rates of COVID-19 testing,3 and challenges with implementing high-quality interpretation.4 As a result of such long-standing disparities, healthcare policy has focused on improving access to language-concordant care.
The Civil Rights Act of 1964 and Department of Health and Human Services (HHS) regulations require recipients of federal financial assistance to provide reasonable access to programs, services, and activities to persons with LEP. Section 1557 of the Affordable Care Act extends Title VI nondiscrimination standards to the entire healthcare system, including insurers and health plans. In 2016, the Obama administration implemented Section 1557 through regulations that clarified and expanded language accessibility standards, although several years later the Trump administration sought to weaken the rule’s protections.
Although the requirement to make healthcare accessible to patients with LEP is unequivocal, “reasonable access” provides clinicians who accept federal funds with flexibility in how they deliver language access services. Differing interpretations of what is considered “reasonable” drives variation in how and when medical facilities provide interpreter services. This results in inconsistency of services provided across care settings and decreased availability of language-concordant care. For example, less than one-third of outpatient providers regularly use qualified interpreters when seeing patients with LEP.5 Furthermore, only about 69% of hospitals offer language access services.6 Clinician underutilization of interpreters for patients with LEP results in poor patient satisfaction and worse health outcomes.7 In light of the Biden administration’s commitment to civil rights and healthcare access, we outline a roadmap of actions that this administration must take to ensure access to basic communication needs and improve health equity.
IDENTIFY CURRENT OPPORTUNITIES FOR IMPROVING REGULATIONS
The Trump-era rules loosened the requirement that care providers notify patients with LEP of their rights to language services and provide instructions on how to access these services. These rules also allowed providers to replace video-based interpreter services with audio-based services, which disproportionately impacts patients in rural areas, who rely on high-quality video interpretation to facilitate telehealth visits, especially during the ongoing COVID-19 pandemic, which has increased patient reliance on telehealth infrastructure for primary healthcare access. The Trump administration weakened both the standards for ensuring adequate access to language assistance services and the compliance tests used to assess whether healthcare organizations have met those standards. The revised regulations deem certain healthcare services effectively exempt from interpreter standards if the projected number of encountered patients with LEP falls below preset minimums and a healthcare entity considers the cost of compliance onerous.8 The Trump administration justified these changes as a cost-savings matter, but the suboptimal care resulting from these changes will likely offset any savings.
RESTORE AND IMPROVE LANGUAGE ACCESS PROVISIONS
To restore a strong commitment to language access, the HHS Office for Civil Rights, which the Biden administration has targeted for new investments in fiscal year 2022, should reestablish the HHS Language Access Steering Committee. This committee maintains criteria that guide covered health entities in developing language access compliance plans. Maintaining such plans should become a basic element of the revised Section 1557 compliance rules and should also become a core feature of the standards applicable to Joint Commission–accredited healthcare organizations. In addition, the Center for Medicare and Medicaid Innovation, whose mission is to identify, test, and implement major improvements in healthcare quality and efficiency, could undertake a special project to identify and incentivize adoption of the most effective language access innovations for incorporation into language access plans.
RESTRUCTURE AND STRENGTHEN COMPLIANCE FOR LANGUAGE ACCESS
Section 1557, as well as federal standards governing the conditions of participation in federal healthcare programs, should ensure that covered entities report on interpreter use and associated patient health outcomes for patients with LEP. Overall compliance measurement and reporting in connection with language access is a matter of basic health equity. Currently, any individual who believes they have experienced discrimination based on language can report a potential violation for federal investigation. But an individual remedy is insufficient because it cannot ensure the types of systemic changes essential to overcome decades of structural exclusion and achieve broader health equity. Further, barriers from digital literacy gaps and fear of legal repercussions, such as deportation, hamper individual reporting efforts. Any policy focused on improving language access use should apply to all patients, regardless of immigration status.
INCENTIVIZE LANGUAGE-CONCORDANT CARE
Ultimately, there is little benefit to imposing standards without a concomitant assurance of the resources needed to achieve full adoption and ongoing compliance. For this reason, a commitment to language access must be accompanied by payment reforms that enable Medicare and Medicaid providers to embrace this vital feature of accessible healthcare by recognizing interpreter costs as part of the clinical encounter and care management. Covered entities could use these resources either to strengthen their own staffing or contract with third-party interpreter services organizations. Currently, the Centers for Medicare & Medicaid Services (CMS) allow states to claim federal matching funds for language assistance services provided to Medicaid enrollees, though rates are dependent on how service claims are categorized. State Medicaid programs can facilitate the provision of such services by optimizing reimbursements for provider organizations under CMS policy.
The Merit-based Incentive Payment System (MIPS) provides an opportunity to incorporate the provision of interpreter services into quality measure reporting. Such efforts could improve health equity and address long-standing needs for research into how language barriers affect healthcare outcomes. Given that analyses of inaugural MIPS data revealed that safety-net practices were more likely to receive lower composite scores, additional scoring flexibility under pay-for-performance schemes (rather than strict penalties) may be necessary to ensure the solvency of safety net practices that disproportionately care for patients with LEP.9 Here, CMMI can play a critical role in expanding the use of patient-facing resources by designing new alternative payment models that reward participants for providing high-quality language concordant care.
The COVID-19 pandemic has exacerbated disparities in care for patients with LEP and even starker disparities among immigrant communities and patients of color. These disparities will only worsen if regulations aimed at improving access to language access services are not reinstated and improved. Failing to focus on healthcare access for patients with LEP hurts individual patient health and public health, as we have seen through lower rates of testing and vaccination in communities of color during this pandemic. The Biden administration can put healthcare on a more equitable pathway by expanding and strengthening language access as a core feature of healthcare, as a matter of both civil rights and health care quality.
Acknowledgments
The authors thank Jocelyn Samuels, JD, and Sara Rosenbaum, JD, for comments and guidance on an earlier draft of this article.
1. Himmelstein J, Himmelstein DU, Woolhandler S, et al. Health care spending and use among Hispanic adults with and without limited English proficiency, 1999–2018. Health Aff (Millwood). 2021;40(7):1126-1134. https://doi.org/10.1377/hlthaff.2020.02510
2. Rodriguez JA, Saadi A, Schwamm LH, Bates DW, Samal L. Disparities in telehealth use among California patients with limited English proficiency. Health Aff (Millwood). 2021;40(3):487-495. https://doi.org/10.1377/hlthaff.2020.00823
3. Kim HN, Lan KF, Nkyekyer E, et al. Assessment of disparities in COVID-19 testing and infection across language groups in Seattle, Washington. JAMA Netw Open. 2020;3(9):e2021213. https://doi.org/10.1001/jamanetworkopen.2020.21213
4. Page KR, Flores-Miller A. Lessons we’ve learned - Covid-19 and the undocumented Latinx community. N Engl J Med. 2021;384(1):5-7. https://doi.org/10.1056/NEJMp2024897
5. Schulson LB, Anderson TS. National estimates of professional interpreter use in the ambulatory setting. J Gen Intern Med. Published online November 2, 2020. https://doi.org/10.1007/s11606-020-06336-6
6. Schiaffino MK, Nara A, Mao L. Language services in hospitals vary by ownership and location. Health Aff (Millwood). 2016;35(8):1399-1403. https://doi.org/10.1377/hlthaff.2015.0955
7. Taira BR, Kim K, Mody N. Hospital and health system–level interventions to improve care for limited English proficiency patients: a systematic review. Jt Comm J Qual Patient Saf. 2019;45(6):446-458. https://doi.org/10.1016/j.jcjq.2019.02.005
8. Musumeci M, Kates J, Dawson L, Salganicoff A, Sobel L, Artiga S. The Trump administration’s final rule on Section 1557 non-discrimination regulations under the ACA and current status. Kaiser Family Foundation. September 18, 2020. Accessed September 2, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/the-trump-administrations-final-rule-on-section-1557-non-discrimination-regulations-under-the-aca-and-current-status/
9. Liao JM, Navathe AS. Does the Merit-Based Incentive Payment System disproportionately affect safety-net practices? JAMA Health Forum. 2020;1(5):e200452. https://doi.org/10.1001/jamahealthforum.2020.0452
Patients whose primary language is not English and who have a limited ability to read, speak, write, or understand English experience worse healthcare access than their English-speaking counterparts, highlighted by fewer healthcare visits and filled prescription medications.1 These patients with limited English proficiency (LEP) face additional barriers to quality healthcare during the COVID-19 pandemic, including lower rates of telehealth use,2 lower rates of COVID-19 testing,3 and challenges with implementing high-quality interpretation.4 As a result of such long-standing disparities, healthcare policy has focused on improving access to language-concordant care.
The Civil Rights Act of 1964 and Department of Health and Human Services (HHS) regulations require recipients of federal financial assistance to provide reasonable access to programs, services, and activities to persons with LEP. Section 1557 of the Affordable Care Act extends Title VI nondiscrimination standards to the entire healthcare system, including insurers and health plans. In 2016, the Obama administration implemented Section 1557 through regulations that clarified and expanded language accessibility standards, although several years later the Trump administration sought to weaken the rule’s protections.
Although the requirement to make healthcare accessible to patients with LEP is unequivocal, “reasonable access” provides clinicians who accept federal funds with flexibility in how they deliver language access services. Differing interpretations of what is considered “reasonable” drives variation in how and when medical facilities provide interpreter services. This results in inconsistency of services provided across care settings and decreased availability of language-concordant care. For example, less than one-third of outpatient providers regularly use qualified interpreters when seeing patients with LEP.5 Furthermore, only about 69% of hospitals offer language access services.6 Clinician underutilization of interpreters for patients with LEP results in poor patient satisfaction and worse health outcomes.7 In light of the Biden administration’s commitment to civil rights and healthcare access, we outline a roadmap of actions that this administration must take to ensure access to basic communication needs and improve health equity.
IDENTIFY CURRENT OPPORTUNITIES FOR IMPROVING REGULATIONS
The Trump-era rules loosened the requirement that care providers notify patients with LEP of their rights to language services and provide instructions on how to access these services. These rules also allowed providers to replace video-based interpreter services with audio-based services, which disproportionately impacts patients in rural areas, who rely on high-quality video interpretation to facilitate telehealth visits, especially during the ongoing COVID-19 pandemic, which has increased patient reliance on telehealth infrastructure for primary healthcare access. The Trump administration weakened both the standards for ensuring adequate access to language assistance services and the compliance tests used to assess whether healthcare organizations have met those standards. The revised regulations deem certain healthcare services effectively exempt from interpreter standards if the projected number of encountered patients with LEP falls below preset minimums and a healthcare entity considers the cost of compliance onerous.8 The Trump administration justified these changes as a cost-savings matter, but the suboptimal care resulting from these changes will likely offset any savings.
RESTORE AND IMPROVE LANGUAGE ACCESS PROVISIONS
To restore a strong commitment to language access, the HHS Office for Civil Rights, which the Biden administration has targeted for new investments in fiscal year 2022, should reestablish the HHS Language Access Steering Committee. This committee maintains criteria that guide covered health entities in developing language access compliance plans. Maintaining such plans should become a basic element of the revised Section 1557 compliance rules and should also become a core feature of the standards applicable to Joint Commission–accredited healthcare organizations. In addition, the Center for Medicare and Medicaid Innovation, whose mission is to identify, test, and implement major improvements in healthcare quality and efficiency, could undertake a special project to identify and incentivize adoption of the most effective language access innovations for incorporation into language access plans.
RESTRUCTURE AND STRENGTHEN COMPLIANCE FOR LANGUAGE ACCESS
Section 1557, as well as federal standards governing the conditions of participation in federal healthcare programs, should ensure that covered entities report on interpreter use and associated patient health outcomes for patients with LEP. Overall compliance measurement and reporting in connection with language access is a matter of basic health equity. Currently, any individual who believes they have experienced discrimination based on language can report a potential violation for federal investigation. But an individual remedy is insufficient because it cannot ensure the types of systemic changes essential to overcome decades of structural exclusion and achieve broader health equity. Further, barriers from digital literacy gaps and fear of legal repercussions, such as deportation, hamper individual reporting efforts. Any policy focused on improving language access use should apply to all patients, regardless of immigration status.
INCENTIVIZE LANGUAGE-CONCORDANT CARE
Ultimately, there is little benefit to imposing standards without a concomitant assurance of the resources needed to achieve full adoption and ongoing compliance. For this reason, a commitment to language access must be accompanied by payment reforms that enable Medicare and Medicaid providers to embrace this vital feature of accessible healthcare by recognizing interpreter costs as part of the clinical encounter and care management. Covered entities could use these resources either to strengthen their own staffing or contract with third-party interpreter services organizations. Currently, the Centers for Medicare & Medicaid Services (CMS) allow states to claim federal matching funds for language assistance services provided to Medicaid enrollees, though rates are dependent on how service claims are categorized. State Medicaid programs can facilitate the provision of such services by optimizing reimbursements for provider organizations under CMS policy.
The Merit-based Incentive Payment System (MIPS) provides an opportunity to incorporate the provision of interpreter services into quality measure reporting. Such efforts could improve health equity and address long-standing needs for research into how language barriers affect healthcare outcomes. Given that analyses of inaugural MIPS data revealed that safety-net practices were more likely to receive lower composite scores, additional scoring flexibility under pay-for-performance schemes (rather than strict penalties) may be necessary to ensure the solvency of safety net practices that disproportionately care for patients with LEP.9 Here, CMMI can play a critical role in expanding the use of patient-facing resources by designing new alternative payment models that reward participants for providing high-quality language concordant care.
The COVID-19 pandemic has exacerbated disparities in care for patients with LEP and even starker disparities among immigrant communities and patients of color. These disparities will only worsen if regulations aimed at improving access to language access services are not reinstated and improved. Failing to focus on healthcare access for patients with LEP hurts individual patient health and public health, as we have seen through lower rates of testing and vaccination in communities of color during this pandemic. The Biden administration can put healthcare on a more equitable pathway by expanding and strengthening language access as a core feature of healthcare, as a matter of both civil rights and health care quality.
Acknowledgments
The authors thank Jocelyn Samuels, JD, and Sara Rosenbaum, JD, for comments and guidance on an earlier draft of this article.
Patients whose primary language is not English and who have a limited ability to read, speak, write, or understand English experience worse healthcare access than their English-speaking counterparts, highlighted by fewer healthcare visits and filled prescription medications.1 These patients with limited English proficiency (LEP) face additional barriers to quality healthcare during the COVID-19 pandemic, including lower rates of telehealth use,2 lower rates of COVID-19 testing,3 and challenges with implementing high-quality interpretation.4 As a result of such long-standing disparities, healthcare policy has focused on improving access to language-concordant care.
The Civil Rights Act of 1964 and Department of Health and Human Services (HHS) regulations require recipients of federal financial assistance to provide reasonable access to programs, services, and activities to persons with LEP. Section 1557 of the Affordable Care Act extends Title VI nondiscrimination standards to the entire healthcare system, including insurers and health plans. In 2016, the Obama administration implemented Section 1557 through regulations that clarified and expanded language accessibility standards, although several years later the Trump administration sought to weaken the rule’s protections.
Although the requirement to make healthcare accessible to patients with LEP is unequivocal, “reasonable access” provides clinicians who accept federal funds with flexibility in how they deliver language access services. Differing interpretations of what is considered “reasonable” drives variation in how and when medical facilities provide interpreter services. This results in inconsistency of services provided across care settings and decreased availability of language-concordant care. For example, less than one-third of outpatient providers regularly use qualified interpreters when seeing patients with LEP.5 Furthermore, only about 69% of hospitals offer language access services.6 Clinician underutilization of interpreters for patients with LEP results in poor patient satisfaction and worse health outcomes.7 In light of the Biden administration’s commitment to civil rights and healthcare access, we outline a roadmap of actions that this administration must take to ensure access to basic communication needs and improve health equity.
IDENTIFY CURRENT OPPORTUNITIES FOR IMPROVING REGULATIONS
The Trump-era rules loosened the requirement that care providers notify patients with LEP of their rights to language services and provide instructions on how to access these services. These rules also allowed providers to replace video-based interpreter services with audio-based services, which disproportionately impacts patients in rural areas, who rely on high-quality video interpretation to facilitate telehealth visits, especially during the ongoing COVID-19 pandemic, which has increased patient reliance on telehealth infrastructure for primary healthcare access. The Trump administration weakened both the standards for ensuring adequate access to language assistance services and the compliance tests used to assess whether healthcare organizations have met those standards. The revised regulations deem certain healthcare services effectively exempt from interpreter standards if the projected number of encountered patients with LEP falls below preset minimums and a healthcare entity considers the cost of compliance onerous.8 The Trump administration justified these changes as a cost-savings matter, but the suboptimal care resulting from these changes will likely offset any savings.
RESTORE AND IMPROVE LANGUAGE ACCESS PROVISIONS
To restore a strong commitment to language access, the HHS Office for Civil Rights, which the Biden administration has targeted for new investments in fiscal year 2022, should reestablish the HHS Language Access Steering Committee. This committee maintains criteria that guide covered health entities in developing language access compliance plans. Maintaining such plans should become a basic element of the revised Section 1557 compliance rules and should also become a core feature of the standards applicable to Joint Commission–accredited healthcare organizations. In addition, the Center for Medicare and Medicaid Innovation, whose mission is to identify, test, and implement major improvements in healthcare quality and efficiency, could undertake a special project to identify and incentivize adoption of the most effective language access innovations for incorporation into language access plans.
RESTRUCTURE AND STRENGTHEN COMPLIANCE FOR LANGUAGE ACCESS
Section 1557, as well as federal standards governing the conditions of participation in federal healthcare programs, should ensure that covered entities report on interpreter use and associated patient health outcomes for patients with LEP. Overall compliance measurement and reporting in connection with language access is a matter of basic health equity. Currently, any individual who believes they have experienced discrimination based on language can report a potential violation for federal investigation. But an individual remedy is insufficient because it cannot ensure the types of systemic changes essential to overcome decades of structural exclusion and achieve broader health equity. Further, barriers from digital literacy gaps and fear of legal repercussions, such as deportation, hamper individual reporting efforts. Any policy focused on improving language access use should apply to all patients, regardless of immigration status.
INCENTIVIZE LANGUAGE-CONCORDANT CARE
Ultimately, there is little benefit to imposing standards without a concomitant assurance of the resources needed to achieve full adoption and ongoing compliance. For this reason, a commitment to language access must be accompanied by payment reforms that enable Medicare and Medicaid providers to embrace this vital feature of accessible healthcare by recognizing interpreter costs as part of the clinical encounter and care management. Covered entities could use these resources either to strengthen their own staffing or contract with third-party interpreter services organizations. Currently, the Centers for Medicare & Medicaid Services (CMS) allow states to claim federal matching funds for language assistance services provided to Medicaid enrollees, though rates are dependent on how service claims are categorized. State Medicaid programs can facilitate the provision of such services by optimizing reimbursements for provider organizations under CMS policy.
The Merit-based Incentive Payment System (MIPS) provides an opportunity to incorporate the provision of interpreter services into quality measure reporting. Such efforts could improve health equity and address long-standing needs for research into how language barriers affect healthcare outcomes. Given that analyses of inaugural MIPS data revealed that safety-net practices were more likely to receive lower composite scores, additional scoring flexibility under pay-for-performance schemes (rather than strict penalties) may be necessary to ensure the solvency of safety net practices that disproportionately care for patients with LEP.9 Here, CMMI can play a critical role in expanding the use of patient-facing resources by designing new alternative payment models that reward participants for providing high-quality language concordant care.
The COVID-19 pandemic has exacerbated disparities in care for patients with LEP and even starker disparities among immigrant communities and patients of color. These disparities will only worsen if regulations aimed at improving access to language access services are not reinstated and improved. Failing to focus on healthcare access for patients with LEP hurts individual patient health and public health, as we have seen through lower rates of testing and vaccination in communities of color during this pandemic. The Biden administration can put healthcare on a more equitable pathway by expanding and strengthening language access as a core feature of healthcare, as a matter of both civil rights and health care quality.
Acknowledgments
The authors thank Jocelyn Samuels, JD, and Sara Rosenbaum, JD, for comments and guidance on an earlier draft of this article.
1. Himmelstein J, Himmelstein DU, Woolhandler S, et al. Health care spending and use among Hispanic adults with and without limited English proficiency, 1999–2018. Health Aff (Millwood). 2021;40(7):1126-1134. https://doi.org/10.1377/hlthaff.2020.02510
2. Rodriguez JA, Saadi A, Schwamm LH, Bates DW, Samal L. Disparities in telehealth use among California patients with limited English proficiency. Health Aff (Millwood). 2021;40(3):487-495. https://doi.org/10.1377/hlthaff.2020.00823
3. Kim HN, Lan KF, Nkyekyer E, et al. Assessment of disparities in COVID-19 testing and infection across language groups in Seattle, Washington. JAMA Netw Open. 2020;3(9):e2021213. https://doi.org/10.1001/jamanetworkopen.2020.21213
4. Page KR, Flores-Miller A. Lessons we’ve learned - Covid-19 and the undocumented Latinx community. N Engl J Med. 2021;384(1):5-7. https://doi.org/10.1056/NEJMp2024897
5. Schulson LB, Anderson TS. National estimates of professional interpreter use in the ambulatory setting. J Gen Intern Med. Published online November 2, 2020. https://doi.org/10.1007/s11606-020-06336-6
6. Schiaffino MK, Nara A, Mao L. Language services in hospitals vary by ownership and location. Health Aff (Millwood). 2016;35(8):1399-1403. https://doi.org/10.1377/hlthaff.2015.0955
7. Taira BR, Kim K, Mody N. Hospital and health system–level interventions to improve care for limited English proficiency patients: a systematic review. Jt Comm J Qual Patient Saf. 2019;45(6):446-458. https://doi.org/10.1016/j.jcjq.2019.02.005
8. Musumeci M, Kates J, Dawson L, Salganicoff A, Sobel L, Artiga S. The Trump administration’s final rule on Section 1557 non-discrimination regulations under the ACA and current status. Kaiser Family Foundation. September 18, 2020. Accessed September 2, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/the-trump-administrations-final-rule-on-section-1557-non-discrimination-regulations-under-the-aca-and-current-status/
9. Liao JM, Navathe AS. Does the Merit-Based Incentive Payment System disproportionately affect safety-net practices? JAMA Health Forum. 2020;1(5):e200452. https://doi.org/10.1001/jamahealthforum.2020.0452
1. Himmelstein J, Himmelstein DU, Woolhandler S, et al. Health care spending and use among Hispanic adults with and without limited English proficiency, 1999–2018. Health Aff (Millwood). 2021;40(7):1126-1134. https://doi.org/10.1377/hlthaff.2020.02510
2. Rodriguez JA, Saadi A, Schwamm LH, Bates DW, Samal L. Disparities in telehealth use among California patients with limited English proficiency. Health Aff (Millwood). 2021;40(3):487-495. https://doi.org/10.1377/hlthaff.2020.00823
3. Kim HN, Lan KF, Nkyekyer E, et al. Assessment of disparities in COVID-19 testing and infection across language groups in Seattle, Washington. JAMA Netw Open. 2020;3(9):e2021213. https://doi.org/10.1001/jamanetworkopen.2020.21213
4. Page KR, Flores-Miller A. Lessons we’ve learned - Covid-19 and the undocumented Latinx community. N Engl J Med. 2021;384(1):5-7. https://doi.org/10.1056/NEJMp2024897
5. Schulson LB, Anderson TS. National estimates of professional interpreter use in the ambulatory setting. J Gen Intern Med. Published online November 2, 2020. https://doi.org/10.1007/s11606-020-06336-6
6. Schiaffino MK, Nara A, Mao L. Language services in hospitals vary by ownership and location. Health Aff (Millwood). 2016;35(8):1399-1403. https://doi.org/10.1377/hlthaff.2015.0955
7. Taira BR, Kim K, Mody N. Hospital and health system–level interventions to improve care for limited English proficiency patients: a systematic review. Jt Comm J Qual Patient Saf. 2019;45(6):446-458. https://doi.org/10.1016/j.jcjq.2019.02.005
8. Musumeci M, Kates J, Dawson L, Salganicoff A, Sobel L, Artiga S. The Trump administration’s final rule on Section 1557 non-discrimination regulations under the ACA and current status. Kaiser Family Foundation. September 18, 2020. Accessed September 2, 2021. https://www.kff.org/racial-equity-and-health-policy/issue-brief/the-trump-administrations-final-rule-on-section-1557-non-discrimination-regulations-under-the-aca-and-current-status/
9. Liao JM, Navathe AS. Does the Merit-Based Incentive Payment System disproportionately affect safety-net practices? JAMA Health Forum. 2020;1(5):e200452. https://doi.org/10.1001/jamahealthforum.2020.0452
© 2021 Society of Hospital Medicine
The No Judgment Zone: Building Trust Through Trustworthiness
The collective struggle felt by healthcare workers simultaneously learning about and caring for patients impacted by SARS-CoV2 infections throughout 2020 was physically and emotionally exhausting. The majority of us had never experienced a global pandemic. Beyond our work in the professional arena of ambulatory practices and hospitals, we also felt the soul-crushing impact of the pandemic in every other aspect of our lives. Preexisting health disparities were amplified by COVID-19. Some of the most affected communities also bore the weight of an additional tsunami of ongoing racial injustice.1 And as healthcare workers, we did our best to process and navigate it all while trying to avoid burnout—as well as being infected with COVID-19 ourselves. When the news of the highly effective vaccines against SARS-CoV2 receiving emergency use authorization broke late in 2020, it felt like a light at the end of a very dark tunnel.
In the weeks preceding wide availability of the vaccines, it became apparent that significant numbers of people lacked confidence in the vaccines. Given the disproportionate impact of COVID-19 on racial minorities, much of the discussion centered around “vaccine hesitancy” in these communities. Reasons such as historical mistrust, belief in conspiracy theories, and misinformation emerged as the leading explanations.2 Campaigns and educational programs targeting Black Americans were quickly developed to counter this widely distributed narrative.
Vaccine uptake also became politicized, which created additional challenges. As schools and businesses reopened, the voices of those opposing pandemic mitigation mandates such as masking and vaccination were highlighted by media outlets. And though a large movement of individuals who had opted against vaccines existed well before the pandemic, with few exceptions, that number had never been great enough to impact public health to this extent.3 This primarily nonminority group of unvaccinated individuals also morphed into another monolithic identity: the “anti-vaxxer.”
The lion’s share of discussions around vaccine uptake centered on these two groups: the “vaccine hesitant” minority and the “anti-vaxxer.” The perspectives and frustration around these two stereotypical unvaccinated groups were underscored in journals and the lay press. But those working in communities and in direct care came into contact with countless COVID-19-positive patients who were unvaccinated and fell into neither of these categories. There was a large swath of vulnerable people who still had unanswered questions and mistrust in the medical system standing in their way. Awareness of health disparities among racial minorities is something that was discussed among providers, but it was something experienced and felt by patients daily in regard to so much more than just COVID-19.
With broader access to vaccines through retail, community-based, and clinical facilities, more patients who desired vaccination had the opportunity. After an initial rise in vaccine uptake, the numbers plateaued. But what remained was the repetitive messaging and sustained focus directed toward Black people and their “vaccine hesitancy.”
Grady Memorial Hospital, a public safety net hospital in Atlanta, serves a predominantly Black and uninsured patient population. We found that a “FAQ” approach with a narrow range of hypothetical ideas about unvaccinated minorities clashed with the reality of what we encountered in clinical environments and the community. While misinformation did appear to be prevalent, we appreciated that the context and level of conviction were heterogenous. We appreciated that each individual conversation could reveal something new to us about that unique patient and their personal concerns about vaccination. As time moved forward, it became clear that there was no playbook for any group, especially for historically disadvantaged communities. Importantly, it was recognized that attempts to anticipate what may be a person’s barrier to vaccination often worked to further erode trust. However, when we focused on creating a space for dialogue, we found we were able to move beyond information-sharing and instead were able to co-construct interpretations of information and co-create solutions that matched patients’ values and lived experiences.4 Through dialogue, we were better able to be transparent about our own experiences, which ultimately facilitated authentic conversations with patients.
In September 2021, we approached our hospital leadership with a patient-centered strategy aimed at providing our patients, staff, and visitors a psychologically safe place to discuss vaccine-related concerns without judgment. With their support, we set up a table in the busiest part of our hospital atrium between the information desk and vaccine-administration site. Beside it was a folding board sign with an image and these words:
“Still unsure about being vaccinated? Let’s talk about it.”
We aptly called the area the “No Judgment Zone.”
The No Judgment Zone is collaboratively staffed in 1- to 2-hour voluntary increments by physician faculty and resident physicians at Emory University School of Medicine and Morehouse School of Medicine. Our goal is to increase patient trust by honoring individual vaccine-related concerns without shame or ridicule. We also work to increase patient trust by being transparent around our own experiences with COVID-19; by sharing our own journeys, concerns, and challenges, we are better able to engage in meaningful dialogue. Also, recognizing the power of logistical barriers, in addition to answering questions, we offer physical assistance with check-in, forms, and escorts to our administration areas. The numbers of unique visits have varied from day to day, but the impact of each individual encounter cannot be overstated.
Here, we describe our approach to interactions at the No Judgment Zone. These are the instructions offered to our volunteers. Though we offer some explicit examples, each talking point is designed to open the door to a patient-centered individual dialogue. We believe that these strategies can be applied to clinical settings as well as any conversation surrounding vaccination with those who have not yet decided to be vaccinated.
THE GRADY “NO JUDGMENT ZONE” INTERACTION APPROACH
No Labels
Try to think of all who are not yet vaccinated as “on a spectrum of deliberation” about their decision—not “hesitant” or “anti-vaxxer.”
Step 1: Gratitude
- “Thank you for stopping to talk to us today.”
- “I appreciate you taking the time.”
- “Before we start—I’m glad you’re here. Thanks.”
Step 2: Determine Where They Are
- Has the person you’re speaking with been vaccinated yet?
- If no, ask: “On a scale of 0 to 10—zero being “I will never get vaccinated under any circumstances” and 10 being ‘I will definitely get vaccinated’—what number would you give yourself?”
- If the person is a firm zero: “Is there anything I might be able to share with you or tell you about that might move you away from that perspective?”
- If the answer is NO: “It sounds like you’ve thought a lot about this and are no longer deliberating about whether you will be vaccinated. If you find yourself considering it, come back to talk with us, okay?” We are not here to debate or argue. We also need to avail ourselves to those who are open to changing their mind.
- If they say anything other than zero, move to an open-ended question about #WhatsYourWhy.
Step 3: #WhatsYourWhy
- “What would you say has been your main reason for not getting vaccinated yet?”
- “Tell me what has stood in the way of you getting vaccinated.”
- Remember: Assume nothing. It may have nothing to do with misinformation, fear, or perceived threat. It could be logistics or many other things. You will not know unless you ask.
- Providers should feel encouraged to also share their why as well and the reasons they encouraged their parents/kids/loved ones to get vaccinated. Making it personal can help establish connection and be more compelling.
Step 4: Listen Completely
- Give full eye contact. Slow all body movements. Use facilitative gestures to let the person know you are listening.
- Do not plan what you wish to say next.
- Limit reactions to misinformation. Shame and judgment can be subtle. Be mindful.
- Repeat the concern back if you are not sure or want to confirm that you’ve heard correctly.
- Ask questions for clarity if you aren’t sure.
Step 5: Affirm All Concerns and Find Common Ground
- “I can only imagine how scary it must be to take a shot that you believe could cause you to not be able to have babies.”
- “You aren’t alone. That’s a concern that many of my patients have had, too. May I share some information about that with you?”
- “When I first heard about the vaccine, I worried it was too new, too. Can I share what I learned?”
Step 6: Provide Factual Information
- Without excessive medical jargon, offer factual information aimed at each concern or question. Probe to be certain your patient understands through a teach-back or question.
- If you are unsure about the answer to their question, admit that you don’t know. You can also ask a colleague or the attending with you. Another option is to call someone or say “Let’s pull this up together.” Then share your answer.
- It is okay to acknowledge that the healthcare system has not and does not always do right by minority populations, especially Black people. Use that as a pivot to why these truths make vaccination that much more important
- Have FAQ information sheets available. Confirm that the patient is comfortable with the information sheet by asking.
Step 7: Offer to Help Them Get Vaccinated Today
- “Would you like me to help you get vaccinated today?”
- “What can I do to assist you with getting vaccinated? Is today a good day?”
- Escort those who agree to the registration area.
- Affirm those plans to get vaccinated or those who feel closer to getting vaccinated after speaking with you.
Step 8: Gratitude
- Close with gratitude and an affirmation.
- “I’m so glad you took the time to talk with us today. You didn’t have to stop.”
- “Feel free to come back to talk to us if you think of any more questions. I’m grateful that you stopped.”
- We are planting seeds. Do not feel pressure to get a person to say yes. Our secret sauce is kindness, respect, and empathy.
- We do not think of our unvaccinated community members as “hesitant.” We approach all as if they are on a spectrum of deliberation.
Step 9: Reflect
- Understand the importance of your service and the potential impact each encounter has.
- Recognize the unique lived experiences of individual patients and how this may impact their deliberation process. While there is urgency and we may feel frustrated, the ultimate goal is to engender trust through respectful interactions.
- Pause for moments of quiet gratitude and self-check-ins.
Conclusion
Just as SARS-CoV2 spreads from one person to many, we recognize that information—factual and otherwise—has the potential to move quickly as well. It is important to realize that providing an opportunity for people to ask questions or receive clarification and confirmation in a safe space is critical. The No Judgement Zone, as the name indicates, offers this opportunity. The conversations that we have in this space are valuable to those who are still considering the vaccine as an option for themselves. The trust required for such conversations is less about the transmission of information and more about the social act of engaging in bidirectional dialogue. The foundation upon which trust is built is consistent trustworthy actions. One such action is respectful communication without shame or ridicule. Another is our willingness to be transparent about our own concerns, experiences, and journeys. Assumptions based upon single-story narratives of the unvaccinated—particularly those from historically marginalized groups—fracture an already fragile confidence in medical authorities.
While we understand that mitigating the ongoing spread of the virus and getting more people vaccinated will call for more than just individual conversations, we believe that respecting the unique perspectives of community members is an equally critical piece to moving forward. Throughout a healthcare worker’s typical day, we work to create personal moments of connection with patients among the immense bustle of other work that has to be done. Initiatives like this one have a focused intentionality behind creating space for patients to feel heard that is not only helpful for vaccine uptake and addressing mistrust, but can also be restorative for providers as well.
1. Manning KD. When grief and crises intersect: perspectives of a Black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
2. Young S. Black vaccine hesitancy rooted in mistrust, doubts. WebMD. February 2, 2021. Accessed November 1, 2021. https://www.webmd.com/vaccines/covid-19-vaccine/news/20210202/black-vaccine-hesitancy-rooted-in-mistrust-doubts
3. Sanyaolu A, Okorie C, Marinkovic A, et al. Measles outbreak in unvaccinated and partially vaccinated children and adults in the United States and Canada (2018-2019): a narrative review of cases. Inquiry. 2019;56:46958019894098. https://doi.org/10.1177/0046958019894098
4. O’Brien BC. Do you see what I see? Reflections on the relationship between transparency and trust. Acad Med. 2019;94(6):757-759. https://doi.org/10.1097/ACM.0000000000002710
The collective struggle felt by healthcare workers simultaneously learning about and caring for patients impacted by SARS-CoV2 infections throughout 2020 was physically and emotionally exhausting. The majority of us had never experienced a global pandemic. Beyond our work in the professional arena of ambulatory practices and hospitals, we also felt the soul-crushing impact of the pandemic in every other aspect of our lives. Preexisting health disparities were amplified by COVID-19. Some of the most affected communities also bore the weight of an additional tsunami of ongoing racial injustice.1 And as healthcare workers, we did our best to process and navigate it all while trying to avoid burnout—as well as being infected with COVID-19 ourselves. When the news of the highly effective vaccines against SARS-CoV2 receiving emergency use authorization broke late in 2020, it felt like a light at the end of a very dark tunnel.
In the weeks preceding wide availability of the vaccines, it became apparent that significant numbers of people lacked confidence in the vaccines. Given the disproportionate impact of COVID-19 on racial minorities, much of the discussion centered around “vaccine hesitancy” in these communities. Reasons such as historical mistrust, belief in conspiracy theories, and misinformation emerged as the leading explanations.2 Campaigns and educational programs targeting Black Americans were quickly developed to counter this widely distributed narrative.
Vaccine uptake also became politicized, which created additional challenges. As schools and businesses reopened, the voices of those opposing pandemic mitigation mandates such as masking and vaccination were highlighted by media outlets. And though a large movement of individuals who had opted against vaccines existed well before the pandemic, with few exceptions, that number had never been great enough to impact public health to this extent.3 This primarily nonminority group of unvaccinated individuals also morphed into another monolithic identity: the “anti-vaxxer.”
The lion’s share of discussions around vaccine uptake centered on these two groups: the “vaccine hesitant” minority and the “anti-vaxxer.” The perspectives and frustration around these two stereotypical unvaccinated groups were underscored in journals and the lay press. But those working in communities and in direct care came into contact with countless COVID-19-positive patients who were unvaccinated and fell into neither of these categories. There was a large swath of vulnerable people who still had unanswered questions and mistrust in the medical system standing in their way. Awareness of health disparities among racial minorities is something that was discussed among providers, but it was something experienced and felt by patients daily in regard to so much more than just COVID-19.
With broader access to vaccines through retail, community-based, and clinical facilities, more patients who desired vaccination had the opportunity. After an initial rise in vaccine uptake, the numbers plateaued. But what remained was the repetitive messaging and sustained focus directed toward Black people and their “vaccine hesitancy.”
Grady Memorial Hospital, a public safety net hospital in Atlanta, serves a predominantly Black and uninsured patient population. We found that a “FAQ” approach with a narrow range of hypothetical ideas about unvaccinated minorities clashed with the reality of what we encountered in clinical environments and the community. While misinformation did appear to be prevalent, we appreciated that the context and level of conviction were heterogenous. We appreciated that each individual conversation could reveal something new to us about that unique patient and their personal concerns about vaccination. As time moved forward, it became clear that there was no playbook for any group, especially for historically disadvantaged communities. Importantly, it was recognized that attempts to anticipate what may be a person’s barrier to vaccination often worked to further erode trust. However, when we focused on creating a space for dialogue, we found we were able to move beyond information-sharing and instead were able to co-construct interpretations of information and co-create solutions that matched patients’ values and lived experiences.4 Through dialogue, we were better able to be transparent about our own experiences, which ultimately facilitated authentic conversations with patients.
In September 2021, we approached our hospital leadership with a patient-centered strategy aimed at providing our patients, staff, and visitors a psychologically safe place to discuss vaccine-related concerns without judgment. With their support, we set up a table in the busiest part of our hospital atrium between the information desk and vaccine-administration site. Beside it was a folding board sign with an image and these words:
“Still unsure about being vaccinated? Let’s talk about it.”
We aptly called the area the “No Judgment Zone.”
The No Judgment Zone is collaboratively staffed in 1- to 2-hour voluntary increments by physician faculty and resident physicians at Emory University School of Medicine and Morehouse School of Medicine. Our goal is to increase patient trust by honoring individual vaccine-related concerns without shame or ridicule. We also work to increase patient trust by being transparent around our own experiences with COVID-19; by sharing our own journeys, concerns, and challenges, we are better able to engage in meaningful dialogue. Also, recognizing the power of logistical barriers, in addition to answering questions, we offer physical assistance with check-in, forms, and escorts to our administration areas. The numbers of unique visits have varied from day to day, but the impact of each individual encounter cannot be overstated.
Here, we describe our approach to interactions at the No Judgment Zone. These are the instructions offered to our volunteers. Though we offer some explicit examples, each talking point is designed to open the door to a patient-centered individual dialogue. We believe that these strategies can be applied to clinical settings as well as any conversation surrounding vaccination with those who have not yet decided to be vaccinated.
THE GRADY “NO JUDGMENT ZONE” INTERACTION APPROACH
No Labels
Try to think of all who are not yet vaccinated as “on a spectrum of deliberation” about their decision—not “hesitant” or “anti-vaxxer.”
Step 1: Gratitude
- “Thank you for stopping to talk to us today.”
- “I appreciate you taking the time.”
- “Before we start—I’m glad you’re here. Thanks.”
Step 2: Determine Where They Are
- Has the person you’re speaking with been vaccinated yet?
- If no, ask: “On a scale of 0 to 10—zero being “I will never get vaccinated under any circumstances” and 10 being ‘I will definitely get vaccinated’—what number would you give yourself?”
- If the person is a firm zero: “Is there anything I might be able to share with you or tell you about that might move you away from that perspective?”
- If the answer is NO: “It sounds like you’ve thought a lot about this and are no longer deliberating about whether you will be vaccinated. If you find yourself considering it, come back to talk with us, okay?” We are not here to debate or argue. We also need to avail ourselves to those who are open to changing their mind.
- If they say anything other than zero, move to an open-ended question about #WhatsYourWhy.
Step 3: #WhatsYourWhy
- “What would you say has been your main reason for not getting vaccinated yet?”
- “Tell me what has stood in the way of you getting vaccinated.”
- Remember: Assume nothing. It may have nothing to do with misinformation, fear, or perceived threat. It could be logistics or many other things. You will not know unless you ask.
- Providers should feel encouraged to also share their why as well and the reasons they encouraged their parents/kids/loved ones to get vaccinated. Making it personal can help establish connection and be more compelling.
Step 4: Listen Completely
- Give full eye contact. Slow all body movements. Use facilitative gestures to let the person know you are listening.
- Do not plan what you wish to say next.
- Limit reactions to misinformation. Shame and judgment can be subtle. Be mindful.
- Repeat the concern back if you are not sure or want to confirm that you’ve heard correctly.
- Ask questions for clarity if you aren’t sure.
Step 5: Affirm All Concerns and Find Common Ground
- “I can only imagine how scary it must be to take a shot that you believe could cause you to not be able to have babies.”
- “You aren’t alone. That’s a concern that many of my patients have had, too. May I share some information about that with you?”
- “When I first heard about the vaccine, I worried it was too new, too. Can I share what I learned?”
Step 6: Provide Factual Information
- Without excessive medical jargon, offer factual information aimed at each concern or question. Probe to be certain your patient understands through a teach-back or question.
- If you are unsure about the answer to their question, admit that you don’t know. You can also ask a colleague or the attending with you. Another option is to call someone or say “Let’s pull this up together.” Then share your answer.
- It is okay to acknowledge that the healthcare system has not and does not always do right by minority populations, especially Black people. Use that as a pivot to why these truths make vaccination that much more important
- Have FAQ information sheets available. Confirm that the patient is comfortable with the information sheet by asking.
Step 7: Offer to Help Them Get Vaccinated Today
- “Would you like me to help you get vaccinated today?”
- “What can I do to assist you with getting vaccinated? Is today a good day?”
- Escort those who agree to the registration area.
- Affirm those plans to get vaccinated or those who feel closer to getting vaccinated after speaking with you.
Step 8: Gratitude
- Close with gratitude and an affirmation.
- “I’m so glad you took the time to talk with us today. You didn’t have to stop.”
- “Feel free to come back to talk to us if you think of any more questions. I’m grateful that you stopped.”
- We are planting seeds. Do not feel pressure to get a person to say yes. Our secret sauce is kindness, respect, and empathy.
- We do not think of our unvaccinated community members as “hesitant.” We approach all as if they are on a spectrum of deliberation.
Step 9: Reflect
- Understand the importance of your service and the potential impact each encounter has.
- Recognize the unique lived experiences of individual patients and how this may impact their deliberation process. While there is urgency and we may feel frustrated, the ultimate goal is to engender trust through respectful interactions.
- Pause for moments of quiet gratitude and self-check-ins.
Conclusion
Just as SARS-CoV2 spreads from one person to many, we recognize that information—factual and otherwise—has the potential to move quickly as well. It is important to realize that providing an opportunity for people to ask questions or receive clarification and confirmation in a safe space is critical. The No Judgement Zone, as the name indicates, offers this opportunity. The conversations that we have in this space are valuable to those who are still considering the vaccine as an option for themselves. The trust required for such conversations is less about the transmission of information and more about the social act of engaging in bidirectional dialogue. The foundation upon which trust is built is consistent trustworthy actions. One such action is respectful communication without shame or ridicule. Another is our willingness to be transparent about our own concerns, experiences, and journeys. Assumptions based upon single-story narratives of the unvaccinated—particularly those from historically marginalized groups—fracture an already fragile confidence in medical authorities.
While we understand that mitigating the ongoing spread of the virus and getting more people vaccinated will call for more than just individual conversations, we believe that respecting the unique perspectives of community members is an equally critical piece to moving forward. Throughout a healthcare worker’s typical day, we work to create personal moments of connection with patients among the immense bustle of other work that has to be done. Initiatives like this one have a focused intentionality behind creating space for patients to feel heard that is not only helpful for vaccine uptake and addressing mistrust, but can also be restorative for providers as well.
The collective struggle felt by healthcare workers simultaneously learning about and caring for patients impacted by SARS-CoV2 infections throughout 2020 was physically and emotionally exhausting. The majority of us had never experienced a global pandemic. Beyond our work in the professional arena of ambulatory practices and hospitals, we also felt the soul-crushing impact of the pandemic in every other aspect of our lives. Preexisting health disparities were amplified by COVID-19. Some of the most affected communities also bore the weight of an additional tsunami of ongoing racial injustice.1 And as healthcare workers, we did our best to process and navigate it all while trying to avoid burnout—as well as being infected with COVID-19 ourselves. When the news of the highly effective vaccines against SARS-CoV2 receiving emergency use authorization broke late in 2020, it felt like a light at the end of a very dark tunnel.
In the weeks preceding wide availability of the vaccines, it became apparent that significant numbers of people lacked confidence in the vaccines. Given the disproportionate impact of COVID-19 on racial minorities, much of the discussion centered around “vaccine hesitancy” in these communities. Reasons such as historical mistrust, belief in conspiracy theories, and misinformation emerged as the leading explanations.2 Campaigns and educational programs targeting Black Americans were quickly developed to counter this widely distributed narrative.
Vaccine uptake also became politicized, which created additional challenges. As schools and businesses reopened, the voices of those opposing pandemic mitigation mandates such as masking and vaccination were highlighted by media outlets. And though a large movement of individuals who had opted against vaccines existed well before the pandemic, with few exceptions, that number had never been great enough to impact public health to this extent.3 This primarily nonminority group of unvaccinated individuals also morphed into another monolithic identity: the “anti-vaxxer.”
The lion’s share of discussions around vaccine uptake centered on these two groups: the “vaccine hesitant” minority and the “anti-vaxxer.” The perspectives and frustration around these two stereotypical unvaccinated groups were underscored in journals and the lay press. But those working in communities and in direct care came into contact with countless COVID-19-positive patients who were unvaccinated and fell into neither of these categories. There was a large swath of vulnerable people who still had unanswered questions and mistrust in the medical system standing in their way. Awareness of health disparities among racial minorities is something that was discussed among providers, but it was something experienced and felt by patients daily in regard to so much more than just COVID-19.
With broader access to vaccines through retail, community-based, and clinical facilities, more patients who desired vaccination had the opportunity. After an initial rise in vaccine uptake, the numbers plateaued. But what remained was the repetitive messaging and sustained focus directed toward Black people and their “vaccine hesitancy.”
Grady Memorial Hospital, a public safety net hospital in Atlanta, serves a predominantly Black and uninsured patient population. We found that a “FAQ” approach with a narrow range of hypothetical ideas about unvaccinated minorities clashed with the reality of what we encountered in clinical environments and the community. While misinformation did appear to be prevalent, we appreciated that the context and level of conviction were heterogenous. We appreciated that each individual conversation could reveal something new to us about that unique patient and their personal concerns about vaccination. As time moved forward, it became clear that there was no playbook for any group, especially for historically disadvantaged communities. Importantly, it was recognized that attempts to anticipate what may be a person’s barrier to vaccination often worked to further erode trust. However, when we focused on creating a space for dialogue, we found we were able to move beyond information-sharing and instead were able to co-construct interpretations of information and co-create solutions that matched patients’ values and lived experiences.4 Through dialogue, we were better able to be transparent about our own experiences, which ultimately facilitated authentic conversations with patients.
In September 2021, we approached our hospital leadership with a patient-centered strategy aimed at providing our patients, staff, and visitors a psychologically safe place to discuss vaccine-related concerns without judgment. With their support, we set up a table in the busiest part of our hospital atrium between the information desk and vaccine-administration site. Beside it was a folding board sign with an image and these words:
“Still unsure about being vaccinated? Let’s talk about it.”
We aptly called the area the “No Judgment Zone.”
The No Judgment Zone is collaboratively staffed in 1- to 2-hour voluntary increments by physician faculty and resident physicians at Emory University School of Medicine and Morehouse School of Medicine. Our goal is to increase patient trust by honoring individual vaccine-related concerns without shame or ridicule. We also work to increase patient trust by being transparent around our own experiences with COVID-19; by sharing our own journeys, concerns, and challenges, we are better able to engage in meaningful dialogue. Also, recognizing the power of logistical barriers, in addition to answering questions, we offer physical assistance with check-in, forms, and escorts to our administration areas. The numbers of unique visits have varied from day to day, but the impact of each individual encounter cannot be overstated.
Here, we describe our approach to interactions at the No Judgment Zone. These are the instructions offered to our volunteers. Though we offer some explicit examples, each talking point is designed to open the door to a patient-centered individual dialogue. We believe that these strategies can be applied to clinical settings as well as any conversation surrounding vaccination with those who have not yet decided to be vaccinated.
THE GRADY “NO JUDGMENT ZONE” INTERACTION APPROACH
No Labels
Try to think of all who are not yet vaccinated as “on a spectrum of deliberation” about their decision—not “hesitant” or “anti-vaxxer.”
Step 1: Gratitude
- “Thank you for stopping to talk to us today.”
- “I appreciate you taking the time.”
- “Before we start—I’m glad you’re here. Thanks.”
Step 2: Determine Where They Are
- Has the person you’re speaking with been vaccinated yet?
- If no, ask: “On a scale of 0 to 10—zero being “I will never get vaccinated under any circumstances” and 10 being ‘I will definitely get vaccinated’—what number would you give yourself?”
- If the person is a firm zero: “Is there anything I might be able to share with you or tell you about that might move you away from that perspective?”
- If the answer is NO: “It sounds like you’ve thought a lot about this and are no longer deliberating about whether you will be vaccinated. If you find yourself considering it, come back to talk with us, okay?” We are not here to debate or argue. We also need to avail ourselves to those who are open to changing their mind.
- If they say anything other than zero, move to an open-ended question about #WhatsYourWhy.
Step 3: #WhatsYourWhy
- “What would you say has been your main reason for not getting vaccinated yet?”
- “Tell me what has stood in the way of you getting vaccinated.”
- Remember: Assume nothing. It may have nothing to do with misinformation, fear, or perceived threat. It could be logistics or many other things. You will not know unless you ask.
- Providers should feel encouraged to also share their why as well and the reasons they encouraged their parents/kids/loved ones to get vaccinated. Making it personal can help establish connection and be more compelling.
Step 4: Listen Completely
- Give full eye contact. Slow all body movements. Use facilitative gestures to let the person know you are listening.
- Do not plan what you wish to say next.
- Limit reactions to misinformation. Shame and judgment can be subtle. Be mindful.
- Repeat the concern back if you are not sure or want to confirm that you’ve heard correctly.
- Ask questions for clarity if you aren’t sure.
Step 5: Affirm All Concerns and Find Common Ground
- “I can only imagine how scary it must be to take a shot that you believe could cause you to not be able to have babies.”
- “You aren’t alone. That’s a concern that many of my patients have had, too. May I share some information about that with you?”
- “When I first heard about the vaccine, I worried it was too new, too. Can I share what I learned?”
Step 6: Provide Factual Information
- Without excessive medical jargon, offer factual information aimed at each concern or question. Probe to be certain your patient understands through a teach-back or question.
- If you are unsure about the answer to their question, admit that you don’t know. You can also ask a colleague or the attending with you. Another option is to call someone or say “Let’s pull this up together.” Then share your answer.
- It is okay to acknowledge that the healthcare system has not and does not always do right by minority populations, especially Black people. Use that as a pivot to why these truths make vaccination that much more important
- Have FAQ information sheets available. Confirm that the patient is comfortable with the information sheet by asking.
Step 7: Offer to Help Them Get Vaccinated Today
- “Would you like me to help you get vaccinated today?”
- “What can I do to assist you with getting vaccinated? Is today a good day?”
- Escort those who agree to the registration area.
- Affirm those plans to get vaccinated or those who feel closer to getting vaccinated after speaking with you.
Step 8: Gratitude
- Close with gratitude and an affirmation.
- “I’m so glad you took the time to talk with us today. You didn’t have to stop.”
- “Feel free to come back to talk to us if you think of any more questions. I’m grateful that you stopped.”
- We are planting seeds. Do not feel pressure to get a person to say yes. Our secret sauce is kindness, respect, and empathy.
- We do not think of our unvaccinated community members as “hesitant.” We approach all as if they are on a spectrum of deliberation.
Step 9: Reflect
- Understand the importance of your service and the potential impact each encounter has.
- Recognize the unique lived experiences of individual patients and how this may impact their deliberation process. While there is urgency and we may feel frustrated, the ultimate goal is to engender trust through respectful interactions.
- Pause for moments of quiet gratitude and self-check-ins.
Conclusion
Just as SARS-CoV2 spreads from one person to many, we recognize that information—factual and otherwise—has the potential to move quickly as well. It is important to realize that providing an opportunity for people to ask questions or receive clarification and confirmation in a safe space is critical. The No Judgement Zone, as the name indicates, offers this opportunity. The conversations that we have in this space are valuable to those who are still considering the vaccine as an option for themselves. The trust required for such conversations is less about the transmission of information and more about the social act of engaging in bidirectional dialogue. The foundation upon which trust is built is consistent trustworthy actions. One such action is respectful communication without shame or ridicule. Another is our willingness to be transparent about our own concerns, experiences, and journeys. Assumptions based upon single-story narratives of the unvaccinated—particularly those from historically marginalized groups—fracture an already fragile confidence in medical authorities.
While we understand that mitigating the ongoing spread of the virus and getting more people vaccinated will call for more than just individual conversations, we believe that respecting the unique perspectives of community members is an equally critical piece to moving forward. Throughout a healthcare worker’s typical day, we work to create personal moments of connection with patients among the immense bustle of other work that has to be done. Initiatives like this one have a focused intentionality behind creating space for patients to feel heard that is not only helpful for vaccine uptake and addressing mistrust, but can also be restorative for providers as well.
1. Manning KD. When grief and crises intersect: perspectives of a Black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
2. Young S. Black vaccine hesitancy rooted in mistrust, doubts. WebMD. February 2, 2021. Accessed November 1, 2021. https://www.webmd.com/vaccines/covid-19-vaccine/news/20210202/black-vaccine-hesitancy-rooted-in-mistrust-doubts
3. Sanyaolu A, Okorie C, Marinkovic A, et al. Measles outbreak in unvaccinated and partially vaccinated children and adults in the United States and Canada (2018-2019): a narrative review of cases. Inquiry. 2019;56:46958019894098. https://doi.org/10.1177/0046958019894098
4. O’Brien BC. Do you see what I see? Reflections on the relationship between transparency and trust. Acad Med. 2019;94(6):757-759. https://doi.org/10.1097/ACM.0000000000002710
1. Manning KD. When grief and crises intersect: perspectives of a Black physician in the time of two pandemics. J Hosp Med. 2020;15(9):566-567. https://doi.org/10.12788/jhm.3481
2. Young S. Black vaccine hesitancy rooted in mistrust, doubts. WebMD. February 2, 2021. Accessed November 1, 2021. https://www.webmd.com/vaccines/covid-19-vaccine/news/20210202/black-vaccine-hesitancy-rooted-in-mistrust-doubts
3. Sanyaolu A, Okorie C, Marinkovic A, et al. Measles outbreak in unvaccinated and partially vaccinated children and adults in the United States and Canada (2018-2019): a narrative review of cases. Inquiry. 2019;56:46958019894098. https://doi.org/10.1177/0046958019894098
4. O’Brien BC. Do you see what I see? Reflections on the relationship between transparency and trust. Acad Med. 2019;94(6):757-759. https://doi.org/10.1097/ACM.0000000000002710
© 2021 Society of Hospital Medicine
Practicing High-Value Pediatric Care During a Pandemic: The Challenges and Opportunities
High-value care (HVC) is a philosophy and approach to medicine that focuses on achieving the best patient outcomes through evidence-based practice while minimizing harm to patients, wasted healthcare resources, and costs. Incorporating HVC principles in pediatric clinical decision-making is particularly important owing to the harms of hospitalization, overutilization, and overdiagnosis, as well as rising costs of pediatric care.1-4 How can we maintain these principles in the face of a global pandemic and new emerging syndrome, multisystem inflammatory syndrome in children (MIS-C), which has dramatically impacted healthcare systems for children?
In this article, we discuss the barriers and opportunities around practicing HVC in our evolving approach to novel COVID-19 management in hospitalized children. We also draw lessons from our experiences on how we can respond to future events that rapidly shift our approach to care.
BARRIERS TO PROVIDING HVC FOR HOSPITALIZED CHILDREN DURING COVID-19
As children’s hospitals and pediatric providers responded to the COVID-19 pandemic, practice recommendations were implemented rapidly and changed rapidly. A major challenge with an event like this is how we respond to the unknown and uncertainty, something most healthcare workers are not comfortable doing at baseline,5,6 particularly trainees and early-career physicians.7 With the benefit of hindsight, many early clinical approaches to care may now be seen as low-value care (LVC). For example, COVID-19 test availability was initially limited, and many hospitals utilized respiratory viral panels (RVPs) to potentially eliminate COVID-19 as an etiology of symptoms. RVP use increased during this time8; however, studies have shown that the co-infection rate of SARS-CoV2 with other respiratory viruses varies widely, so a positive RVP was of uncertain benefit.9 In addition, routine RVP use is often low value and may lead to overdiagnosis, additional overtesting cascades, and, at times, false reassurance and premature closure of the diagnostic workup.10
As our understanding of COVID-19 has expanded, rapid changes in treatment have also occurred. Early data were often preliminary and based on small trials of adults, and treatments ranged from inexpensive and available (dexamethasone) to quite expensive (remdesivir, monoclonal antibodies). Pragmatic randomized controlled trials (RCTs) are an important tool that may have been underutilized in pediatrics. Similar to our adult hospitalist colleagues’ experience,11 the rapid rise in cases provided an opportunity to collaborate across institutions to assess which treatments were most effective. In particular, the predictable rise in rates of MIS-C after a surge in COVID-19 cases could have provided an avenue to evaluate the relative effectiveness of the various treatments used.12 However, there were limited pediatric RCTs and thus a missed opportunity to establish an evidence-based pediatric standard of care for COVID-19 and MIS-C. This resulted in the development and dissemination of care practices before they were fully tested in children.
Similarly, the medical community has become increasingly aware of laboratory findings that may be predictive of clinical course.13 The outcomes of COVID and MIS-C are potentially severe, so looking for “early warning signs” with diagnostic testing is appealing. Clinicians responding to early data, and with a fear of missing something, may order a full panel of bloodwork for admitted patients to assist with decision-making and may underestimate the perceived minor harms and cost of unnecessary testing/admissions.3 However, most of the evidence regarding lab values came from the adult population. There is little understanding of how lab values impact pediatric-specific outcomes.14 Even for MIS-C, a pediatric-specific condition, early protocols emphasize broad testing approaches.15 A focus on grave (but rare) outcomes from a novel virus may also distract from more common causes of symptoms and lead to missed common diagnoses that are less severe.16 For both testing and treatment, having this early information before clear evidence on how it guided care may have caused more harm than benefit. Again, RCTs may have helped guide MIS-C therapies and protocol development.
Changing workflows may also create new barriers to HVC. One of the recommendations from Choosing Wisely® during the COVID-19 pandemic was to batch lab draws17 to reduce the risk of exposure to healthcare workers performing phlebotomy, as well as staff who transport, handle, and process bloodwork in the lab. This may inadvertently encourage the approach of getting a lab test “in case” we need it with a single daily blood draw. In trying to avoid multiple encounters (and conserve personal protective equipment [PPE]), we may be taking a less stepwise approach than in prepandemic times.
Finally, children’s hospitals witnessed significant financial challenges and reductions in patient volume related to the pandemic.18 Reductions in patient volume could present a potential opportunity for practicing HVC (eg, more time to discuss downstream effects) or alternatively could inadvertently incentivize low-value, low-priority care via messaging around preserving financial viability.
For clinicians and healthcare systems, these examples highlight why we may be predisposed to practicing LVC during a pandemic or similar emerging threat.
STRATEGIES FOR HVC PRACTICE DURING FUTURE MAJOR EVENTS
In light of these challenging clinical scenarios and nonclinical factors that predispose us to LVC, how can we reinforce a high-value approach to care during a pandemic or similar emerging threat? The following five specific concepts may help providers and organizations optimize HVC during this pandemic and in future situations:
- Utilize pediatric RCTs to provide evidence-based recommendations. In the face of a novel virus with unclear manifestations, treatment options were rapidly implemented without time for careful evaluation. In the future, collaboratively utilizing shared resources in the research community could help rapidly and rigorously evaluate outcomes in the pursuit of evidence-based practice.
- Use standardization as a tool to mitigate uncertainty. Knowing that uncertainty can be a driver of overuse and that during emerging threats, evidence is scarce and rapidly changing, a structured method for standardizing practice across your institution or multiple institutions can be helpful in many ways. Electronic health record–based orders and guidelines provide a standard of care to relieve uncertainty and have been shown to reduce overtesting.19 These resources can also be adapted rapidly as evidence emerges, reducing the burden on providers to know the latest evolving best practice. Experts who have reviewed the literature should have a method to quickly disseminate these findings through standardized practice, providing a venue for rapid learning and implementation.20
- Plan for active deimplementation from the outset. It is inevitable that some practices implemented early in pandemic response may need to be deimplemented later as the evidence and situation evolve. However, there is ample evidence that deimplementation can be difficult.21 Building in deimplementation mechanisms, such as standing educational sessions or hospital committees dedicated to value that review practices, from the beginning may ease these changes.
- Take advantage of novel opportunities to improve value. Early stop-gap interventions may be wasteful, but the upheaval from major events may also create novel opportunities to improve value in other ways. Some of these efforts, like PPE conservation and as-needed follow-up visits, may become useful methods to improve value even after the pandemic ends.22,23 The decreased pursuit of healthcare during the pandemic may also have given us an opportunity to better define when delayed diagnosis or even nondiagnosis for certain conditions is acceptable and when it may cause harm.
- Highlight harms of overuse. While avoiding unnecessary costs is an important aspect of reducing overuse, often the other human-centered harms of overuse are better motivators for HVC. Especially during the response to an emerging threat, the impacts of overuse may be compounded. Laboratory resources that are strained to meet COVID-19 testing demand will be further stretched by overuse of other laboratory testing. Overuse of ineffective treatments adds stress to nurses, pharmacists, and other front-line staff taking care of ill patients. Side effects of unnecessary interventions, including those that could prolong hospitalization, would also increase strain on the system. Reducing overuse is also a way to reduce workload for hospital staff during a time of crisis. Improved efficiency of practice and less time spent on practices that do not add value to patient care can insulate staff against burnout.24 Hospitalization and healthcare costs can add to the stress and financial burden of patients and families.25 Clinicians can highlight harms of overuse through openly talking about it on rounds with the patients, families, and entire care team and incorporating it into health system–wide messaging.
CONCLUSION
As vaccine distribution continues, like many clinicians, we are hopeful that the worst days of the pandemic are behind us. The crucible of the COVID-19 pandemic has undoubtedly changed us as clinicians and impacted our future practice patterns. We believe there is a need to challenge ourselves to continue to think from a value mindset even in times of crisis. Furthermore, there are important opportunities to learn from our response to the COVID-19 pandemic and find strategies for minimizing LVC outside the pandemic. We believe the lessons learned around improving value during this pandemic can strengthen our response to the next novel, widespread threat and reduce waste in our care systems, with a potential to increase the resilience of systems in the future.
1. Rokach A. Psychological, emotional and physical experiences of hospitalized children. Clin Case Rep Rev. 2016;2. https://doi.org/10.15761/CCRR.1000227
2. Stockwell DC, Landrigan CP, Toomey SL, et al. Adverse events in hospitalized pediatric patients. Pediatrics. 2018;142(2):e20173360. https://doi.org/10.1542/peds.2017-3360
3. Coon ER, Quinonez RA, Moyer VA, Schroeder AR. Overdiagnosis: how our compulsion for diagnosis may be harming children. Pediatrics. 2014;134(5):1013-1023. https://doi.org/10.1542/peds.2014-1778
4. Bui AL, Dieleman JL, Hamavid H, et al. Spending on children’s personal health care in the United States, 1996-2013. JAMA Pediatr. 2017;171(2):181-189. https://doi.org/10.1001/jamapediatrics.2016.4086
5. Ilgen JS, Eva KW, de Bruin A, Cook DA, Regehr G. Comfort with uncertainty: reframing our conceptions of how clinicians navigate complex clinical situations. Adv Health Sci Theory Pract. 2019;24(4):797-809. https://doi.org/10.1007/s10459-018-9859-5
6. Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making. 1998;18(3):320-329. https://doi.org/10.1177/0272989X9801800310
7. Beck JB, Long M, Ryan MS. Into the unknown: helping learners become more comfortable with diagnostic uncertainty. Pediatrics. 2020;146(5):e2020027300. https://doi.org/10.1542/peds.2020-027300
8. Marshall NC, Kariyawasam RM, Zelyas N, Kanji JN, Diggle MA. Broad respiratory testing to identify SARS-CoV-2 viral co-circulation and inform diagnostic stewardship in the COVID-19 pandemic. Virol J. 2021;18(1):93. https://doi.org/10.1186/s12985-021-01545-9
9. Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39(5):355-368. https://doi.org/10.1097/INF.0000000000002660
10. Morrison JM, Dudas RA, Collins K. The power and peril of panels. Hosp Pediatr. 2018;8(11):729-732. https://doi.org/10.1542/hpeds.2018-0093
11. Wise J, Coombes R. Covid-19: the inside story of the RECOVERY trial. BMJ. 2020;370:m2670. https://doi.org/10.1136/bmj.m2670.
12. Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020;383(4):334-346.
13. Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta. 2020;510:475-482. https://doi.org/10.1056/NEJMoa2021680
14. Henry BM, Benoit SW, de Oliveira MHS, et al. Laboratory abnormalities in children with mild and severe coronavirus disease 2019 (COVID-19): a pooled analysis and review. Clin Biochem. 2020;81:1-8. https://doi.org/10.1016/j.clinbiochem.2020.05.012
15. Centers for Disease Control and Prevention. Information for healthcare providers about multisystem inflammatory syndrome in children (MIS-C). Accessed July 7, 2021. https://www.cdc.gov/mis/hcp/index.html
16. Molloy M, Jerardi K, Marshall T. What are we missing in our search for MIS-C? Hosp Pediatr. 2021;11(4):e66-e69. https://doi.org/10.1542/hpeds.2020-005579
17. Cho HJ, Feldman LS, Keller S, Hoffman A, Pahwa AK, Krouss M. Choosing Wisely in the COVID-19 era: preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-362. https://doi.org/10.12788/jhm.3457
18. Synhorst DC, Bettenhausen JL, Hall M, et al. Healthcare encounter and financial impact of COVID-19 on children’s hospitals. J Hosp Med. 2021;16(4):223-226. https://doi.org/10.12788/jhm.3572
19. Algaze CA, Wood M, Pageler NM, Sharek PJ, Longhurst CA, Shin AY. Use of a checklist and clinical decision support tool reduces laboratory use and improves cost. Pediatrics. 2016;137(1). https://doi.org/10.1542/peds.2014-3019
20. Rao S, Kwan BM, Curtis DJ, et al. Implementation of a rapid evidence assessment infrastructure during the coronavirus disease 2019 (COVID-19) pandemic to develop policies, clinical pathways, stimulate academic research, and create educational opportunities. J Pediatr. 2021;230:4-8.e2. https://doi.org/10.1016/j.jpeds.2020.10.029
21. Gill PJ, Mahant S. Deimplementation of established medical practice without intervention: does it actually happen? J Hosp Med. 2020;15(12):765-766. https://doi.org/10.12788/jhm.3467
22. Coon ER, Destino LA, Greene TH, Vukin E, Stoddard G, Schroeder AR. Comparison of as-needed and scheduled posthospitalization follow-up for children hospitalized for bronchiolitis: the Bronchiolitis Follow-up Intervention Trial (BeneFIT) randomized clinical trial. JAMA Pediatr. 2020;174(9):e201937. https://doi.org/10.1001/jamapediatrics.2020.1937
23. Steuart R, Huang FS, Schaffzin JK, Thomson J. Finding the value in personal protective equipment for hospitalized patients during a pandemic and beyond. J Hosp Med. 2020;15(5):295-298. https://doi.org/10.12788/jhm.3429
24. Pierce RG, Diaz M, Kneeland P. Optimizing well-being, practice culture, and professional thriving in an era of turbulence. J Hosp Med. 2019;14(2):126-128. https://doi.org/10.12788/jhm.3101
25. Commodari E. Children staying in hospital: a research on psychological stress of caregivers. Ital J Pediatr. 2010;36:40. https://doi.org/10.1186/1824-7288-36-40
High-value care (HVC) is a philosophy and approach to medicine that focuses on achieving the best patient outcomes through evidence-based practice while minimizing harm to patients, wasted healthcare resources, and costs. Incorporating HVC principles in pediatric clinical decision-making is particularly important owing to the harms of hospitalization, overutilization, and overdiagnosis, as well as rising costs of pediatric care.1-4 How can we maintain these principles in the face of a global pandemic and new emerging syndrome, multisystem inflammatory syndrome in children (MIS-C), which has dramatically impacted healthcare systems for children?
In this article, we discuss the barriers and opportunities around practicing HVC in our evolving approach to novel COVID-19 management in hospitalized children. We also draw lessons from our experiences on how we can respond to future events that rapidly shift our approach to care.
BARRIERS TO PROVIDING HVC FOR HOSPITALIZED CHILDREN DURING COVID-19
As children’s hospitals and pediatric providers responded to the COVID-19 pandemic, practice recommendations were implemented rapidly and changed rapidly. A major challenge with an event like this is how we respond to the unknown and uncertainty, something most healthcare workers are not comfortable doing at baseline,5,6 particularly trainees and early-career physicians.7 With the benefit of hindsight, many early clinical approaches to care may now be seen as low-value care (LVC). For example, COVID-19 test availability was initially limited, and many hospitals utilized respiratory viral panels (RVPs) to potentially eliminate COVID-19 as an etiology of symptoms. RVP use increased during this time8; however, studies have shown that the co-infection rate of SARS-CoV2 with other respiratory viruses varies widely, so a positive RVP was of uncertain benefit.9 In addition, routine RVP use is often low value and may lead to overdiagnosis, additional overtesting cascades, and, at times, false reassurance and premature closure of the diagnostic workup.10
As our understanding of COVID-19 has expanded, rapid changes in treatment have also occurred. Early data were often preliminary and based on small trials of adults, and treatments ranged from inexpensive and available (dexamethasone) to quite expensive (remdesivir, monoclonal antibodies). Pragmatic randomized controlled trials (RCTs) are an important tool that may have been underutilized in pediatrics. Similar to our adult hospitalist colleagues’ experience,11 the rapid rise in cases provided an opportunity to collaborate across institutions to assess which treatments were most effective. In particular, the predictable rise in rates of MIS-C after a surge in COVID-19 cases could have provided an avenue to evaluate the relative effectiveness of the various treatments used.12 However, there were limited pediatric RCTs and thus a missed opportunity to establish an evidence-based pediatric standard of care for COVID-19 and MIS-C. This resulted in the development and dissemination of care practices before they were fully tested in children.
Similarly, the medical community has become increasingly aware of laboratory findings that may be predictive of clinical course.13 The outcomes of COVID and MIS-C are potentially severe, so looking for “early warning signs” with diagnostic testing is appealing. Clinicians responding to early data, and with a fear of missing something, may order a full panel of bloodwork for admitted patients to assist with decision-making and may underestimate the perceived minor harms and cost of unnecessary testing/admissions.3 However, most of the evidence regarding lab values came from the adult population. There is little understanding of how lab values impact pediatric-specific outcomes.14 Even for MIS-C, a pediatric-specific condition, early protocols emphasize broad testing approaches.15 A focus on grave (but rare) outcomes from a novel virus may also distract from more common causes of symptoms and lead to missed common diagnoses that are less severe.16 For both testing and treatment, having this early information before clear evidence on how it guided care may have caused more harm than benefit. Again, RCTs may have helped guide MIS-C therapies and protocol development.
Changing workflows may also create new barriers to HVC. One of the recommendations from Choosing Wisely® during the COVID-19 pandemic was to batch lab draws17 to reduce the risk of exposure to healthcare workers performing phlebotomy, as well as staff who transport, handle, and process bloodwork in the lab. This may inadvertently encourage the approach of getting a lab test “in case” we need it with a single daily blood draw. In trying to avoid multiple encounters (and conserve personal protective equipment [PPE]), we may be taking a less stepwise approach than in prepandemic times.
Finally, children’s hospitals witnessed significant financial challenges and reductions in patient volume related to the pandemic.18 Reductions in patient volume could present a potential opportunity for practicing HVC (eg, more time to discuss downstream effects) or alternatively could inadvertently incentivize low-value, low-priority care via messaging around preserving financial viability.
For clinicians and healthcare systems, these examples highlight why we may be predisposed to practicing LVC during a pandemic or similar emerging threat.
STRATEGIES FOR HVC PRACTICE DURING FUTURE MAJOR EVENTS
In light of these challenging clinical scenarios and nonclinical factors that predispose us to LVC, how can we reinforce a high-value approach to care during a pandemic or similar emerging threat? The following five specific concepts may help providers and organizations optimize HVC during this pandemic and in future situations:
- Utilize pediatric RCTs to provide evidence-based recommendations. In the face of a novel virus with unclear manifestations, treatment options were rapidly implemented without time for careful evaluation. In the future, collaboratively utilizing shared resources in the research community could help rapidly and rigorously evaluate outcomes in the pursuit of evidence-based practice.
- Use standardization as a tool to mitigate uncertainty. Knowing that uncertainty can be a driver of overuse and that during emerging threats, evidence is scarce and rapidly changing, a structured method for standardizing practice across your institution or multiple institutions can be helpful in many ways. Electronic health record–based orders and guidelines provide a standard of care to relieve uncertainty and have been shown to reduce overtesting.19 These resources can also be adapted rapidly as evidence emerges, reducing the burden on providers to know the latest evolving best practice. Experts who have reviewed the literature should have a method to quickly disseminate these findings through standardized practice, providing a venue for rapid learning and implementation.20
- Plan for active deimplementation from the outset. It is inevitable that some practices implemented early in pandemic response may need to be deimplemented later as the evidence and situation evolve. However, there is ample evidence that deimplementation can be difficult.21 Building in deimplementation mechanisms, such as standing educational sessions or hospital committees dedicated to value that review practices, from the beginning may ease these changes.
- Take advantage of novel opportunities to improve value. Early stop-gap interventions may be wasteful, but the upheaval from major events may also create novel opportunities to improve value in other ways. Some of these efforts, like PPE conservation and as-needed follow-up visits, may become useful methods to improve value even after the pandemic ends.22,23 The decreased pursuit of healthcare during the pandemic may also have given us an opportunity to better define when delayed diagnosis or even nondiagnosis for certain conditions is acceptable and when it may cause harm.
- Highlight harms of overuse. While avoiding unnecessary costs is an important aspect of reducing overuse, often the other human-centered harms of overuse are better motivators for HVC. Especially during the response to an emerging threat, the impacts of overuse may be compounded. Laboratory resources that are strained to meet COVID-19 testing demand will be further stretched by overuse of other laboratory testing. Overuse of ineffective treatments adds stress to nurses, pharmacists, and other front-line staff taking care of ill patients. Side effects of unnecessary interventions, including those that could prolong hospitalization, would also increase strain on the system. Reducing overuse is also a way to reduce workload for hospital staff during a time of crisis. Improved efficiency of practice and less time spent on practices that do not add value to patient care can insulate staff against burnout.24 Hospitalization and healthcare costs can add to the stress and financial burden of patients and families.25 Clinicians can highlight harms of overuse through openly talking about it on rounds with the patients, families, and entire care team and incorporating it into health system–wide messaging.
CONCLUSION
As vaccine distribution continues, like many clinicians, we are hopeful that the worst days of the pandemic are behind us. The crucible of the COVID-19 pandemic has undoubtedly changed us as clinicians and impacted our future practice patterns. We believe there is a need to challenge ourselves to continue to think from a value mindset even in times of crisis. Furthermore, there are important opportunities to learn from our response to the COVID-19 pandemic and find strategies for minimizing LVC outside the pandemic. We believe the lessons learned around improving value during this pandemic can strengthen our response to the next novel, widespread threat and reduce waste in our care systems, with a potential to increase the resilience of systems in the future.
High-value care (HVC) is a philosophy and approach to medicine that focuses on achieving the best patient outcomes through evidence-based practice while minimizing harm to patients, wasted healthcare resources, and costs. Incorporating HVC principles in pediatric clinical decision-making is particularly important owing to the harms of hospitalization, overutilization, and overdiagnosis, as well as rising costs of pediatric care.1-4 How can we maintain these principles in the face of a global pandemic and new emerging syndrome, multisystem inflammatory syndrome in children (MIS-C), which has dramatically impacted healthcare systems for children?
In this article, we discuss the barriers and opportunities around practicing HVC in our evolving approach to novel COVID-19 management in hospitalized children. We also draw lessons from our experiences on how we can respond to future events that rapidly shift our approach to care.
BARRIERS TO PROVIDING HVC FOR HOSPITALIZED CHILDREN DURING COVID-19
As children’s hospitals and pediatric providers responded to the COVID-19 pandemic, practice recommendations were implemented rapidly and changed rapidly. A major challenge with an event like this is how we respond to the unknown and uncertainty, something most healthcare workers are not comfortable doing at baseline,5,6 particularly trainees and early-career physicians.7 With the benefit of hindsight, many early clinical approaches to care may now be seen as low-value care (LVC). For example, COVID-19 test availability was initially limited, and many hospitals utilized respiratory viral panels (RVPs) to potentially eliminate COVID-19 as an etiology of symptoms. RVP use increased during this time8; however, studies have shown that the co-infection rate of SARS-CoV2 with other respiratory viruses varies widely, so a positive RVP was of uncertain benefit.9 In addition, routine RVP use is often low value and may lead to overdiagnosis, additional overtesting cascades, and, at times, false reassurance and premature closure of the diagnostic workup.10
As our understanding of COVID-19 has expanded, rapid changes in treatment have also occurred. Early data were often preliminary and based on small trials of adults, and treatments ranged from inexpensive and available (dexamethasone) to quite expensive (remdesivir, monoclonal antibodies). Pragmatic randomized controlled trials (RCTs) are an important tool that may have been underutilized in pediatrics. Similar to our adult hospitalist colleagues’ experience,11 the rapid rise in cases provided an opportunity to collaborate across institutions to assess which treatments were most effective. In particular, the predictable rise in rates of MIS-C after a surge in COVID-19 cases could have provided an avenue to evaluate the relative effectiveness of the various treatments used.12 However, there were limited pediatric RCTs and thus a missed opportunity to establish an evidence-based pediatric standard of care for COVID-19 and MIS-C. This resulted in the development and dissemination of care practices before they were fully tested in children.
Similarly, the medical community has become increasingly aware of laboratory findings that may be predictive of clinical course.13 The outcomes of COVID and MIS-C are potentially severe, so looking for “early warning signs” with diagnostic testing is appealing. Clinicians responding to early data, and with a fear of missing something, may order a full panel of bloodwork for admitted patients to assist with decision-making and may underestimate the perceived minor harms and cost of unnecessary testing/admissions.3 However, most of the evidence regarding lab values came from the adult population. There is little understanding of how lab values impact pediatric-specific outcomes.14 Even for MIS-C, a pediatric-specific condition, early protocols emphasize broad testing approaches.15 A focus on grave (but rare) outcomes from a novel virus may also distract from more common causes of symptoms and lead to missed common diagnoses that are less severe.16 For both testing and treatment, having this early information before clear evidence on how it guided care may have caused more harm than benefit. Again, RCTs may have helped guide MIS-C therapies and protocol development.
Changing workflows may also create new barriers to HVC. One of the recommendations from Choosing Wisely® during the COVID-19 pandemic was to batch lab draws17 to reduce the risk of exposure to healthcare workers performing phlebotomy, as well as staff who transport, handle, and process bloodwork in the lab. This may inadvertently encourage the approach of getting a lab test “in case” we need it with a single daily blood draw. In trying to avoid multiple encounters (and conserve personal protective equipment [PPE]), we may be taking a less stepwise approach than in prepandemic times.
Finally, children’s hospitals witnessed significant financial challenges and reductions in patient volume related to the pandemic.18 Reductions in patient volume could present a potential opportunity for practicing HVC (eg, more time to discuss downstream effects) or alternatively could inadvertently incentivize low-value, low-priority care via messaging around preserving financial viability.
For clinicians and healthcare systems, these examples highlight why we may be predisposed to practicing LVC during a pandemic or similar emerging threat.
STRATEGIES FOR HVC PRACTICE DURING FUTURE MAJOR EVENTS
In light of these challenging clinical scenarios and nonclinical factors that predispose us to LVC, how can we reinforce a high-value approach to care during a pandemic or similar emerging threat? The following five specific concepts may help providers and organizations optimize HVC during this pandemic and in future situations:
- Utilize pediatric RCTs to provide evidence-based recommendations. In the face of a novel virus with unclear manifestations, treatment options were rapidly implemented without time for careful evaluation. In the future, collaboratively utilizing shared resources in the research community could help rapidly and rigorously evaluate outcomes in the pursuit of evidence-based practice.
- Use standardization as a tool to mitigate uncertainty. Knowing that uncertainty can be a driver of overuse and that during emerging threats, evidence is scarce and rapidly changing, a structured method for standardizing practice across your institution or multiple institutions can be helpful in many ways. Electronic health record–based orders and guidelines provide a standard of care to relieve uncertainty and have been shown to reduce overtesting.19 These resources can also be adapted rapidly as evidence emerges, reducing the burden on providers to know the latest evolving best practice. Experts who have reviewed the literature should have a method to quickly disseminate these findings through standardized practice, providing a venue for rapid learning and implementation.20
- Plan for active deimplementation from the outset. It is inevitable that some practices implemented early in pandemic response may need to be deimplemented later as the evidence and situation evolve. However, there is ample evidence that deimplementation can be difficult.21 Building in deimplementation mechanisms, such as standing educational sessions or hospital committees dedicated to value that review practices, from the beginning may ease these changes.
- Take advantage of novel opportunities to improve value. Early stop-gap interventions may be wasteful, but the upheaval from major events may also create novel opportunities to improve value in other ways. Some of these efforts, like PPE conservation and as-needed follow-up visits, may become useful methods to improve value even after the pandemic ends.22,23 The decreased pursuit of healthcare during the pandemic may also have given us an opportunity to better define when delayed diagnosis or even nondiagnosis for certain conditions is acceptable and when it may cause harm.
- Highlight harms of overuse. While avoiding unnecessary costs is an important aspect of reducing overuse, often the other human-centered harms of overuse are better motivators for HVC. Especially during the response to an emerging threat, the impacts of overuse may be compounded. Laboratory resources that are strained to meet COVID-19 testing demand will be further stretched by overuse of other laboratory testing. Overuse of ineffective treatments adds stress to nurses, pharmacists, and other front-line staff taking care of ill patients. Side effects of unnecessary interventions, including those that could prolong hospitalization, would also increase strain on the system. Reducing overuse is also a way to reduce workload for hospital staff during a time of crisis. Improved efficiency of practice and less time spent on practices that do not add value to patient care can insulate staff against burnout.24 Hospitalization and healthcare costs can add to the stress and financial burden of patients and families.25 Clinicians can highlight harms of overuse through openly talking about it on rounds with the patients, families, and entire care team and incorporating it into health system–wide messaging.
CONCLUSION
As vaccine distribution continues, like many clinicians, we are hopeful that the worst days of the pandemic are behind us. The crucible of the COVID-19 pandemic has undoubtedly changed us as clinicians and impacted our future practice patterns. We believe there is a need to challenge ourselves to continue to think from a value mindset even in times of crisis. Furthermore, there are important opportunities to learn from our response to the COVID-19 pandemic and find strategies for minimizing LVC outside the pandemic. We believe the lessons learned around improving value during this pandemic can strengthen our response to the next novel, widespread threat and reduce waste in our care systems, with a potential to increase the resilience of systems in the future.
1. Rokach A. Psychological, emotional and physical experiences of hospitalized children. Clin Case Rep Rev. 2016;2. https://doi.org/10.15761/CCRR.1000227
2. Stockwell DC, Landrigan CP, Toomey SL, et al. Adverse events in hospitalized pediatric patients. Pediatrics. 2018;142(2):e20173360. https://doi.org/10.1542/peds.2017-3360
3. Coon ER, Quinonez RA, Moyer VA, Schroeder AR. Overdiagnosis: how our compulsion for diagnosis may be harming children. Pediatrics. 2014;134(5):1013-1023. https://doi.org/10.1542/peds.2014-1778
4. Bui AL, Dieleman JL, Hamavid H, et al. Spending on children’s personal health care in the United States, 1996-2013. JAMA Pediatr. 2017;171(2):181-189. https://doi.org/10.1001/jamapediatrics.2016.4086
5. Ilgen JS, Eva KW, de Bruin A, Cook DA, Regehr G. Comfort with uncertainty: reframing our conceptions of how clinicians navigate complex clinical situations. Adv Health Sci Theory Pract. 2019;24(4):797-809. https://doi.org/10.1007/s10459-018-9859-5
6. Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making. 1998;18(3):320-329. https://doi.org/10.1177/0272989X9801800310
7. Beck JB, Long M, Ryan MS. Into the unknown: helping learners become more comfortable with diagnostic uncertainty. Pediatrics. 2020;146(5):e2020027300. https://doi.org/10.1542/peds.2020-027300
8. Marshall NC, Kariyawasam RM, Zelyas N, Kanji JN, Diggle MA. Broad respiratory testing to identify SARS-CoV-2 viral co-circulation and inform diagnostic stewardship in the COVID-19 pandemic. Virol J. 2021;18(1):93. https://doi.org/10.1186/s12985-021-01545-9
9. Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39(5):355-368. https://doi.org/10.1097/INF.0000000000002660
10. Morrison JM, Dudas RA, Collins K. The power and peril of panels. Hosp Pediatr. 2018;8(11):729-732. https://doi.org/10.1542/hpeds.2018-0093
11. Wise J, Coombes R. Covid-19: the inside story of the RECOVERY trial. BMJ. 2020;370:m2670. https://doi.org/10.1136/bmj.m2670.
12. Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020;383(4):334-346.
13. Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta. 2020;510:475-482. https://doi.org/10.1056/NEJMoa2021680
14. Henry BM, Benoit SW, de Oliveira MHS, et al. Laboratory abnormalities in children with mild and severe coronavirus disease 2019 (COVID-19): a pooled analysis and review. Clin Biochem. 2020;81:1-8. https://doi.org/10.1016/j.clinbiochem.2020.05.012
15. Centers for Disease Control and Prevention. Information for healthcare providers about multisystem inflammatory syndrome in children (MIS-C). Accessed July 7, 2021. https://www.cdc.gov/mis/hcp/index.html
16. Molloy M, Jerardi K, Marshall T. What are we missing in our search for MIS-C? Hosp Pediatr. 2021;11(4):e66-e69. https://doi.org/10.1542/hpeds.2020-005579
17. Cho HJ, Feldman LS, Keller S, Hoffman A, Pahwa AK, Krouss M. Choosing Wisely in the COVID-19 era: preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-362. https://doi.org/10.12788/jhm.3457
18. Synhorst DC, Bettenhausen JL, Hall M, et al. Healthcare encounter and financial impact of COVID-19 on children’s hospitals. J Hosp Med. 2021;16(4):223-226. https://doi.org/10.12788/jhm.3572
19. Algaze CA, Wood M, Pageler NM, Sharek PJ, Longhurst CA, Shin AY. Use of a checklist and clinical decision support tool reduces laboratory use and improves cost. Pediatrics. 2016;137(1). https://doi.org/10.1542/peds.2014-3019
20. Rao S, Kwan BM, Curtis DJ, et al. Implementation of a rapid evidence assessment infrastructure during the coronavirus disease 2019 (COVID-19) pandemic to develop policies, clinical pathways, stimulate academic research, and create educational opportunities. J Pediatr. 2021;230:4-8.e2. https://doi.org/10.1016/j.jpeds.2020.10.029
21. Gill PJ, Mahant S. Deimplementation of established medical practice without intervention: does it actually happen? J Hosp Med. 2020;15(12):765-766. https://doi.org/10.12788/jhm.3467
22. Coon ER, Destino LA, Greene TH, Vukin E, Stoddard G, Schroeder AR. Comparison of as-needed and scheduled posthospitalization follow-up for children hospitalized for bronchiolitis: the Bronchiolitis Follow-up Intervention Trial (BeneFIT) randomized clinical trial. JAMA Pediatr. 2020;174(9):e201937. https://doi.org/10.1001/jamapediatrics.2020.1937
23. Steuart R, Huang FS, Schaffzin JK, Thomson J. Finding the value in personal protective equipment for hospitalized patients during a pandemic and beyond. J Hosp Med. 2020;15(5):295-298. https://doi.org/10.12788/jhm.3429
24. Pierce RG, Diaz M, Kneeland P. Optimizing well-being, practice culture, and professional thriving in an era of turbulence. J Hosp Med. 2019;14(2):126-128. https://doi.org/10.12788/jhm.3101
25. Commodari E. Children staying in hospital: a research on psychological stress of caregivers. Ital J Pediatr. 2010;36:40. https://doi.org/10.1186/1824-7288-36-40
1. Rokach A. Psychological, emotional and physical experiences of hospitalized children. Clin Case Rep Rev. 2016;2. https://doi.org/10.15761/CCRR.1000227
2. Stockwell DC, Landrigan CP, Toomey SL, et al. Adverse events in hospitalized pediatric patients. Pediatrics. 2018;142(2):e20173360. https://doi.org/10.1542/peds.2017-3360
3. Coon ER, Quinonez RA, Moyer VA, Schroeder AR. Overdiagnosis: how our compulsion for diagnosis may be harming children. Pediatrics. 2014;134(5):1013-1023. https://doi.org/10.1542/peds.2014-1778
4. Bui AL, Dieleman JL, Hamavid H, et al. Spending on children’s personal health care in the United States, 1996-2013. JAMA Pediatr. 2017;171(2):181-189. https://doi.org/10.1001/jamapediatrics.2016.4086
5. Ilgen JS, Eva KW, de Bruin A, Cook DA, Regehr G. Comfort with uncertainty: reframing our conceptions of how clinicians navigate complex clinical situations. Adv Health Sci Theory Pract. 2019;24(4):797-809. https://doi.org/10.1007/s10459-018-9859-5
6. Allison JJ, Kiefe CI, Cook EF, Gerrity MS, Orav EJ, Centor R. The association of physician attitudes about uncertainty and risk taking with resource use in a Medicare HMO. Med Decis Making. 1998;18(3):320-329. https://doi.org/10.1177/0272989X9801800310
7. Beck JB, Long M, Ryan MS. Into the unknown: helping learners become more comfortable with diagnostic uncertainty. Pediatrics. 2020;146(5):e2020027300. https://doi.org/10.1542/peds.2020-027300
8. Marshall NC, Kariyawasam RM, Zelyas N, Kanji JN, Diggle MA. Broad respiratory testing to identify SARS-CoV-2 viral co-circulation and inform diagnostic stewardship in the COVID-19 pandemic. Virol J. 2021;18(1):93. https://doi.org/10.1186/s12985-021-01545-9
9. Zimmermann P, Curtis N. Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children. Pediatr Infect Dis J. 2020;39(5):355-368. https://doi.org/10.1097/INF.0000000000002660
10. Morrison JM, Dudas RA, Collins K. The power and peril of panels. Hosp Pediatr. 2018;8(11):729-732. https://doi.org/10.1542/hpeds.2018-0093
11. Wise J, Coombes R. Covid-19: the inside story of the RECOVERY trial. BMJ. 2020;370:m2670. https://doi.org/10.1136/bmj.m2670.
12. Feldstein LR, Rose EB, Horwitz SM, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. N Engl J Med. 2020;383(4):334-346.
13. Pourbagheri-Sigaroodi A, Bashash D, Fateh F, Abolghasemi H. Laboratory findings in COVID-19 diagnosis and prognosis. Clin Chim Acta. 2020;510:475-482. https://doi.org/10.1056/NEJMoa2021680
14. Henry BM, Benoit SW, de Oliveira MHS, et al. Laboratory abnormalities in children with mild and severe coronavirus disease 2019 (COVID-19): a pooled analysis and review. Clin Biochem. 2020;81:1-8. https://doi.org/10.1016/j.clinbiochem.2020.05.012
15. Centers for Disease Control and Prevention. Information for healthcare providers about multisystem inflammatory syndrome in children (MIS-C). Accessed July 7, 2021. https://www.cdc.gov/mis/hcp/index.html
16. Molloy M, Jerardi K, Marshall T. What are we missing in our search for MIS-C? Hosp Pediatr. 2021;11(4):e66-e69. https://doi.org/10.1542/hpeds.2020-005579
17. Cho HJ, Feldman LS, Keller S, Hoffman A, Pahwa AK, Krouss M. Choosing Wisely in the COVID-19 era: preventing harm to healthcare workers. J Hosp Med. 2020;15(6):360-362. https://doi.org/10.12788/jhm.3457
18. Synhorst DC, Bettenhausen JL, Hall M, et al. Healthcare encounter and financial impact of COVID-19 on children’s hospitals. J Hosp Med. 2021;16(4):223-226. https://doi.org/10.12788/jhm.3572
19. Algaze CA, Wood M, Pageler NM, Sharek PJ, Longhurst CA, Shin AY. Use of a checklist and clinical decision support tool reduces laboratory use and improves cost. Pediatrics. 2016;137(1). https://doi.org/10.1542/peds.2014-3019
20. Rao S, Kwan BM, Curtis DJ, et al. Implementation of a rapid evidence assessment infrastructure during the coronavirus disease 2019 (COVID-19) pandemic to develop policies, clinical pathways, stimulate academic research, and create educational opportunities. J Pediatr. 2021;230:4-8.e2. https://doi.org/10.1016/j.jpeds.2020.10.029
21. Gill PJ, Mahant S. Deimplementation of established medical practice without intervention: does it actually happen? J Hosp Med. 2020;15(12):765-766. https://doi.org/10.12788/jhm.3467
22. Coon ER, Destino LA, Greene TH, Vukin E, Stoddard G, Schroeder AR. Comparison of as-needed and scheduled posthospitalization follow-up for children hospitalized for bronchiolitis: the Bronchiolitis Follow-up Intervention Trial (BeneFIT) randomized clinical trial. JAMA Pediatr. 2020;174(9):e201937. https://doi.org/10.1001/jamapediatrics.2020.1937
23. Steuart R, Huang FS, Schaffzin JK, Thomson J. Finding the value in personal protective equipment for hospitalized patients during a pandemic and beyond. J Hosp Med. 2020;15(5):295-298. https://doi.org/10.12788/jhm.3429
24. Pierce RG, Diaz M, Kneeland P. Optimizing well-being, practice culture, and professional thriving in an era of turbulence. J Hosp Med. 2019;14(2):126-128. https://doi.org/10.12788/jhm.3101
25. Commodari E. Children staying in hospital: a research on psychological stress of caregivers. Ital J Pediatr. 2010;36:40. https://doi.org/10.1186/1824-7288-36-40
© 2021 Society of Hospital Medicine
Tweeting Into the Void: Effective Use of Social Media for Healthcare Professionals
Communication has always played a central role in facilitating technological advances and social progress. The printing press, mail, telegraph, radio, television, electronic mail, and social media have all allowed for the exchange of ideas that led to progress, and have done so with increasing speed. But some people are beginning to question whether we are experiencing diminishing returns from making such communication easier, faster, and more widespread. Disinformation, conspiracies, inappropriate messages, and personal attacks are just as easy to communicate as truth, good ideas, and empathy. In many cases, truth and falsehood are nearly indistinguishable. Raw, nasty emotions contained in personal attacks are often provocative, thus generating even more engagement, which many people view as the purpose of social media. In this context, it is more important than ever for trusted voices, such as those of scientists and physicians, to play a role in the public sphere.
In this essay, we offer our personal recommendations on how healthcare professionals, who in our view have outsized authority and responsibility on healthcare topics, might improve communication on social media. We focus particularly on Twitter given its prominent role in the public exchange of ideas and its recognized benefits (and challenges) for scientific communication.1 We make these recommendations with some trepidation because we are sure readers will be able to find times when we have not followed our own advice. And we are sure many will disagree or feel that our advice raises the bar too high. We divide our recommendations into lists of Do’s and Don’ts. Let’s start with the Do’s.
DO
DO separate facts from inferences, ideally labeling them as such. For example, you can report that public health has found five cases of the delta variant in people in a specific nursing home as a fact. You might then infer that the variant is widespread in that facility, and that community spread in the region is likely. Stating the source of your facts helps the reader evaluate their reliability and precision.
DO state when you are quoting preliminary evidence. If posting a preprint, press release, or other non-peer-reviewed paper (even if it is your own!), make its preliminary status clear to the reader (Figure, part A).
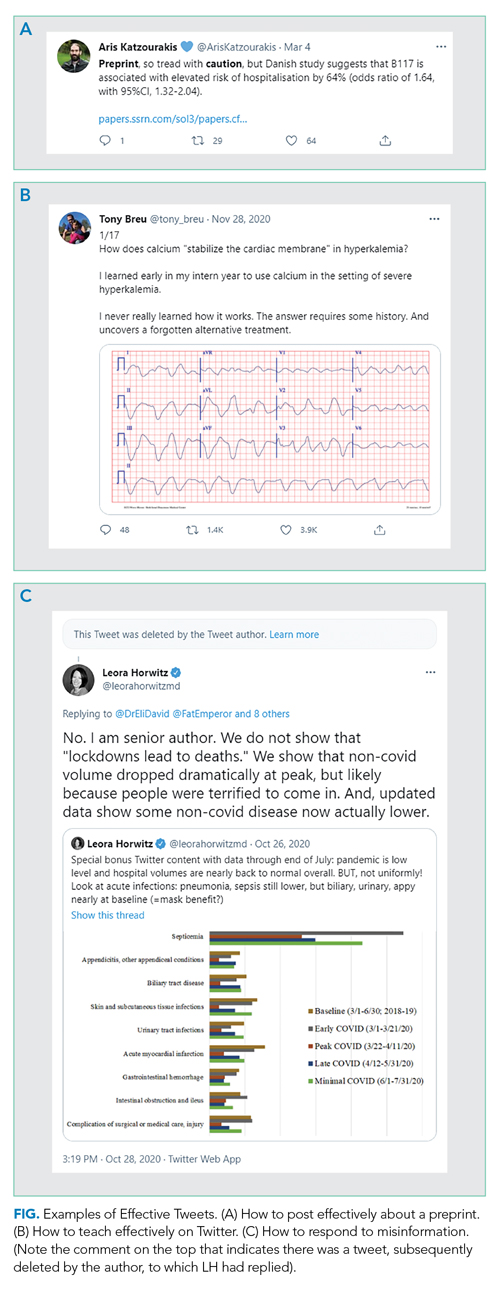
DO read the full article before posting. If you are posting an article, make sure you understand the whole context of any results you are highlighting. Avoid exaggerating, fear-mongering, or selectively picking facts or results to bolster your opinion.DO seek to add value to the public discourse. Rather than simply retweeting popular posts, consider taking the time to collate evidence (including contrary evidence) into a thread if seeking to prove a point or to teach, especially when it relates to something in your field. You likely are more knowledgeable about topics in your field than 99% of readers; use Twitter to spread your expertise. Clinical “tweetorials,” such as those popularized by @tony_breu, can be very effective teaching tools (Figure, part B).
DO make recommendations as specific as possible. If your goal is to improve adherence to evidence-based medicine or support disadvantaged people, be explicit about how you would achieve these goals. Tell readers exactly what you have in mind so that individuals and leaders can operationalize the recommendations. Use threads to expand on your advice and its rationale.
DO consider engaging with misinformation. We suggest doing so if the misinformation is posted by someone prominent who is likely to have broad reach, but only once per post and in a factual manner. You are unlikely to convince persons who post disinformation that they are wrong; extended arguments are unhelpful. Your role here is simply to inform readers of the post, who may be more open to reason. Occasionally, you may even convince the initial poster, as seen in Figure, part C, to delete certain misinformation. But don’t count on it.
DO consider your obligation to the general public. It is fine to engage explicitly with the medical community (ie, through tweetchats),2 but also consider that your comments will be accessible to everyone. Now more than ever the public is looking to healthcare professionals for clarity, reassurance, and evidence about medical matters.
DO acknowledge when you were wrong. Update your opinions as facts change or when you realize you made a mistake. The COVID-19 pandemic has brought home the rapidity with which we can gain scientific knowledge. Many of the things we thought were right early on—and posted about on Twitter—we now know to be wrong. Be forthright about this, while making it clear that the fact that we know more now doesn’t mean no information can be trusted. (A corollary: Don’t overstate what we know to be true at any time, so that it does not feel as much of a surprise if we later learn more and need to revise an opinion or a statement.)
DO be kind. This is perhaps the most important thing. We are all experiencing stress as physicians, parents, children, and colleagues. Spend your time focusing on people’s actions rather than impugning their motives or intelligence. Most of the time you don’t really know what their motives are. We recognize that kindness may not generate the same amount of engagement as sarcasm, but at least take time to consider whether you want to be seen as mean-spirited forever.
DO pause before sending. Twitter creates a false perception of the need for speed (and doesn’t really lend itself to revising drafts). But in reality, there is no rush. The torrent of Twitter posts means that people typically only see what has been posted around the time they log in; an early post is not necessarily more likely to be noticed. So, take your time and avoid falling into a trap of writing something you will regret, or, in extreme cases, that will get you fired or otherwise ruin your career. There is no rush to be first; Twitter will still be there tomorrow.
DON’T
For some time, mentors have warned physicians (and others whose careers depend on their reputation) to be careful in their use of social media. Electronic dissemination of inappropriate words or images can come back to haunt people—sometimes immediately, sometimes many years later.3 Physicians are also at risk of falling into some pitfalls specific to the profession. That said, here are some Don’ts to avoid or be cautious about.
DON’T reveal information about patients in a recognizable fashion. Journals ask for written consent from patients when authors submit a manuscript about individual cases so readers can be sure consent has been obtained. The same standard should apply to social media; if not, you are clearly violating a professional standard. Yet, on Twitter, people may assume you have not obtained consent, conveying a false sense of invasion of privacy and undermining confidence in the profession. The safest thing to do is not tell stories about patients, or to completely disguise the story so even the patients can’t recognize themselves. If you do choose to post about a patient, obtain written permission that you save, and clearly indicate that you have that permission in the Tweet.
DON’T claim to have expertise in areas where you have little training or education. For example, just because you are an expert in critical care and have seen the ravages of COVID-19 on your patients doesn’t mean you are an expert in how to stop a pandemic, though your observations may be helpful to those who are. This does not mean you shouldn’t speak out on important moral issues like climate change, nuclear war, or injustices, which clearly reflect personal opinion and values. Rather, be cautious about commenting authoritatively on areas in which the lay reader might mistakenly think you have specific expertise.
DON’T make yourself the hero of every story. Implicitly seeking praise for doing your job (Look at me, I’m working on Christmas!) may breed resentment and undercut professionalism. Rather, state what it is about your job that works well and what doesn’t (for example, teaching tips, wellness advice, and organizational strategies) in a way that helps others emulate your successes.
DON’T let emotions get the better of you. This past year has been full of outrageous and appalling events and behavior. We do not suggest that you ignore these. Rather, make sure that if you are blaming an individual for something that it really was their fault, because they had control of the factors that led to the disastrous outcome. Consider focusing on systemic and structural explanations for unacceptable phenomena to minimize defensiveness and maximize the potential for identifying solutions. And yes, sometimes you just have to let it rip, but be selective—maybe show your post to someone else and sleep on it before you send it.
CONCLUSION
We hope that you will find these suggestions helpful in both creating and reading social media posts on important topics. We recognize that some people like the spontaneity of the social media platform and will thus find our suggestions stunting. But at least everyone ought to consider what they are trying to achieve when they make public statements. The exchange of ideas has always been a key ingredient in creating progress. Let’s optimize the usefulness of those exchanges for that purpose, and to promote knowledge and science in a way that helps us all live healthier and happier lives.
1. Choo EK, Ranney ML, Chan TM, et al. Twitter as a tool for communication and knowledge exchange in academic medicine: a guide for skeptics and novices. Med Teach. 2015;37(5):411-416. https://doi.org/10.3109/0142159X.2014.993371
2. Admon AJ, Kaul V, Cribbs SK, Guzman E, Jimenez O, Richards JB. Twelve tips for developing and implementing a medical education Twitter chat. Med Teach. 2020;42(5):500-506. https://doi.org/10.1080/0142159X.2019.1598553
3. Langenfeld SJ, Batra R. How can social media get us in trouble? Clin Colon Rectal Surg. 2017;30(4):264-269. https://doi.org/10.1055/s-0037-1604255
Communication has always played a central role in facilitating technological advances and social progress. The printing press, mail, telegraph, radio, television, electronic mail, and social media have all allowed for the exchange of ideas that led to progress, and have done so with increasing speed. But some people are beginning to question whether we are experiencing diminishing returns from making such communication easier, faster, and more widespread. Disinformation, conspiracies, inappropriate messages, and personal attacks are just as easy to communicate as truth, good ideas, and empathy. In many cases, truth and falsehood are nearly indistinguishable. Raw, nasty emotions contained in personal attacks are often provocative, thus generating even more engagement, which many people view as the purpose of social media. In this context, it is more important than ever for trusted voices, such as those of scientists and physicians, to play a role in the public sphere.
In this essay, we offer our personal recommendations on how healthcare professionals, who in our view have outsized authority and responsibility on healthcare topics, might improve communication on social media. We focus particularly on Twitter given its prominent role in the public exchange of ideas and its recognized benefits (and challenges) for scientific communication.1 We make these recommendations with some trepidation because we are sure readers will be able to find times when we have not followed our own advice. And we are sure many will disagree or feel that our advice raises the bar too high. We divide our recommendations into lists of Do’s and Don’ts. Let’s start with the Do’s.
DO
DO separate facts from inferences, ideally labeling them as such. For example, you can report that public health has found five cases of the delta variant in people in a specific nursing home as a fact. You might then infer that the variant is widespread in that facility, and that community spread in the region is likely. Stating the source of your facts helps the reader evaluate their reliability and precision.
DO state when you are quoting preliminary evidence. If posting a preprint, press release, or other non-peer-reviewed paper (even if it is your own!), make its preliminary status clear to the reader (Figure, part A).
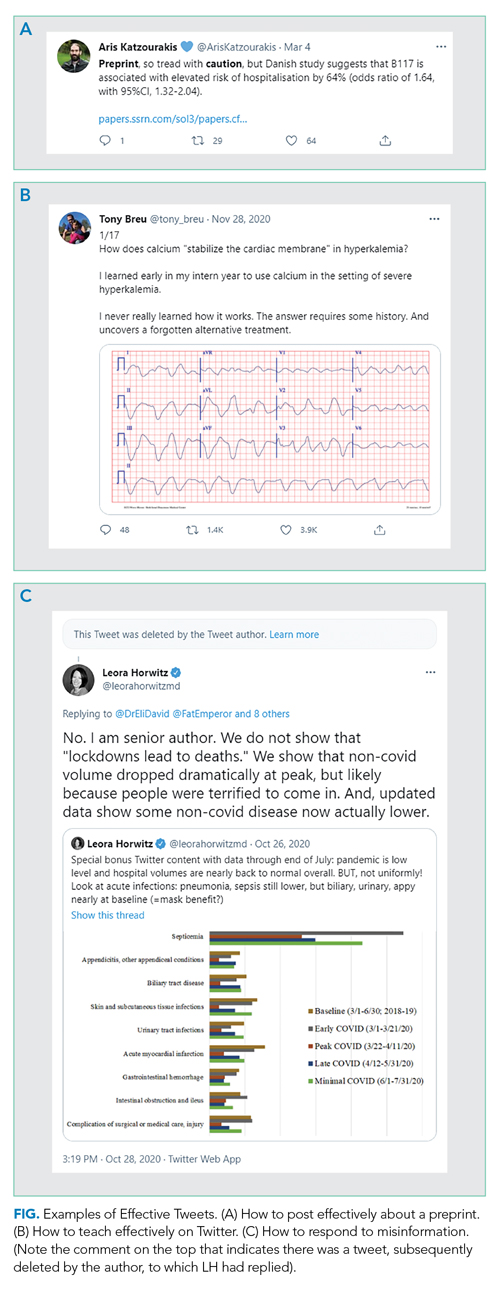
DO read the full article before posting. If you are posting an article, make sure you understand the whole context of any results you are highlighting. Avoid exaggerating, fear-mongering, or selectively picking facts or results to bolster your opinion.DO seek to add value to the public discourse. Rather than simply retweeting popular posts, consider taking the time to collate evidence (including contrary evidence) into a thread if seeking to prove a point or to teach, especially when it relates to something in your field. You likely are more knowledgeable about topics in your field than 99% of readers; use Twitter to spread your expertise. Clinical “tweetorials,” such as those popularized by @tony_breu, can be very effective teaching tools (Figure, part B).
DO make recommendations as specific as possible. If your goal is to improve adherence to evidence-based medicine or support disadvantaged people, be explicit about how you would achieve these goals. Tell readers exactly what you have in mind so that individuals and leaders can operationalize the recommendations. Use threads to expand on your advice and its rationale.
DO consider engaging with misinformation. We suggest doing so if the misinformation is posted by someone prominent who is likely to have broad reach, but only once per post and in a factual manner. You are unlikely to convince persons who post disinformation that they are wrong; extended arguments are unhelpful. Your role here is simply to inform readers of the post, who may be more open to reason. Occasionally, you may even convince the initial poster, as seen in Figure, part C, to delete certain misinformation. But don’t count on it.
DO consider your obligation to the general public. It is fine to engage explicitly with the medical community (ie, through tweetchats),2 but also consider that your comments will be accessible to everyone. Now more than ever the public is looking to healthcare professionals for clarity, reassurance, and evidence about medical matters.
DO acknowledge when you were wrong. Update your opinions as facts change or when you realize you made a mistake. The COVID-19 pandemic has brought home the rapidity with which we can gain scientific knowledge. Many of the things we thought were right early on—and posted about on Twitter—we now know to be wrong. Be forthright about this, while making it clear that the fact that we know more now doesn’t mean no information can be trusted. (A corollary: Don’t overstate what we know to be true at any time, so that it does not feel as much of a surprise if we later learn more and need to revise an opinion or a statement.)
DO be kind. This is perhaps the most important thing. We are all experiencing stress as physicians, parents, children, and colleagues. Spend your time focusing on people’s actions rather than impugning their motives or intelligence. Most of the time you don’t really know what their motives are. We recognize that kindness may not generate the same amount of engagement as sarcasm, but at least take time to consider whether you want to be seen as mean-spirited forever.
DO pause before sending. Twitter creates a false perception of the need for speed (and doesn’t really lend itself to revising drafts). But in reality, there is no rush. The torrent of Twitter posts means that people typically only see what has been posted around the time they log in; an early post is not necessarily more likely to be noticed. So, take your time and avoid falling into a trap of writing something you will regret, or, in extreme cases, that will get you fired or otherwise ruin your career. There is no rush to be first; Twitter will still be there tomorrow.
DON’T
For some time, mentors have warned physicians (and others whose careers depend on their reputation) to be careful in their use of social media. Electronic dissemination of inappropriate words or images can come back to haunt people—sometimes immediately, sometimes many years later.3 Physicians are also at risk of falling into some pitfalls specific to the profession. That said, here are some Don’ts to avoid or be cautious about.
DON’T reveal information about patients in a recognizable fashion. Journals ask for written consent from patients when authors submit a manuscript about individual cases so readers can be sure consent has been obtained. The same standard should apply to social media; if not, you are clearly violating a professional standard. Yet, on Twitter, people may assume you have not obtained consent, conveying a false sense of invasion of privacy and undermining confidence in the profession. The safest thing to do is not tell stories about patients, or to completely disguise the story so even the patients can’t recognize themselves. If you do choose to post about a patient, obtain written permission that you save, and clearly indicate that you have that permission in the Tweet.
DON’T claim to have expertise in areas where you have little training or education. For example, just because you are an expert in critical care and have seen the ravages of COVID-19 on your patients doesn’t mean you are an expert in how to stop a pandemic, though your observations may be helpful to those who are. This does not mean you shouldn’t speak out on important moral issues like climate change, nuclear war, or injustices, which clearly reflect personal opinion and values. Rather, be cautious about commenting authoritatively on areas in which the lay reader might mistakenly think you have specific expertise.
DON’T make yourself the hero of every story. Implicitly seeking praise for doing your job (Look at me, I’m working on Christmas!) may breed resentment and undercut professionalism. Rather, state what it is about your job that works well and what doesn’t (for example, teaching tips, wellness advice, and organizational strategies) in a way that helps others emulate your successes.
DON’T let emotions get the better of you. This past year has been full of outrageous and appalling events and behavior. We do not suggest that you ignore these. Rather, make sure that if you are blaming an individual for something that it really was their fault, because they had control of the factors that led to the disastrous outcome. Consider focusing on systemic and structural explanations for unacceptable phenomena to minimize defensiveness and maximize the potential for identifying solutions. And yes, sometimes you just have to let it rip, but be selective—maybe show your post to someone else and sleep on it before you send it.
CONCLUSION
We hope that you will find these suggestions helpful in both creating and reading social media posts on important topics. We recognize that some people like the spontaneity of the social media platform and will thus find our suggestions stunting. But at least everyone ought to consider what they are trying to achieve when they make public statements. The exchange of ideas has always been a key ingredient in creating progress. Let’s optimize the usefulness of those exchanges for that purpose, and to promote knowledge and science in a way that helps us all live healthier and happier lives.
Communication has always played a central role in facilitating technological advances and social progress. The printing press, mail, telegraph, radio, television, electronic mail, and social media have all allowed for the exchange of ideas that led to progress, and have done so with increasing speed. But some people are beginning to question whether we are experiencing diminishing returns from making such communication easier, faster, and more widespread. Disinformation, conspiracies, inappropriate messages, and personal attacks are just as easy to communicate as truth, good ideas, and empathy. In many cases, truth and falsehood are nearly indistinguishable. Raw, nasty emotions contained in personal attacks are often provocative, thus generating even more engagement, which many people view as the purpose of social media. In this context, it is more important than ever for trusted voices, such as those of scientists and physicians, to play a role in the public sphere.
In this essay, we offer our personal recommendations on how healthcare professionals, who in our view have outsized authority and responsibility on healthcare topics, might improve communication on social media. We focus particularly on Twitter given its prominent role in the public exchange of ideas and its recognized benefits (and challenges) for scientific communication.1 We make these recommendations with some trepidation because we are sure readers will be able to find times when we have not followed our own advice. And we are sure many will disagree or feel that our advice raises the bar too high. We divide our recommendations into lists of Do’s and Don’ts. Let’s start with the Do’s.
DO
DO separate facts from inferences, ideally labeling them as such. For example, you can report that public health has found five cases of the delta variant in people in a specific nursing home as a fact. You might then infer that the variant is widespread in that facility, and that community spread in the region is likely. Stating the source of your facts helps the reader evaluate their reliability and precision.
DO state when you are quoting preliminary evidence. If posting a preprint, press release, or other non-peer-reviewed paper (even if it is your own!), make its preliminary status clear to the reader (Figure, part A).
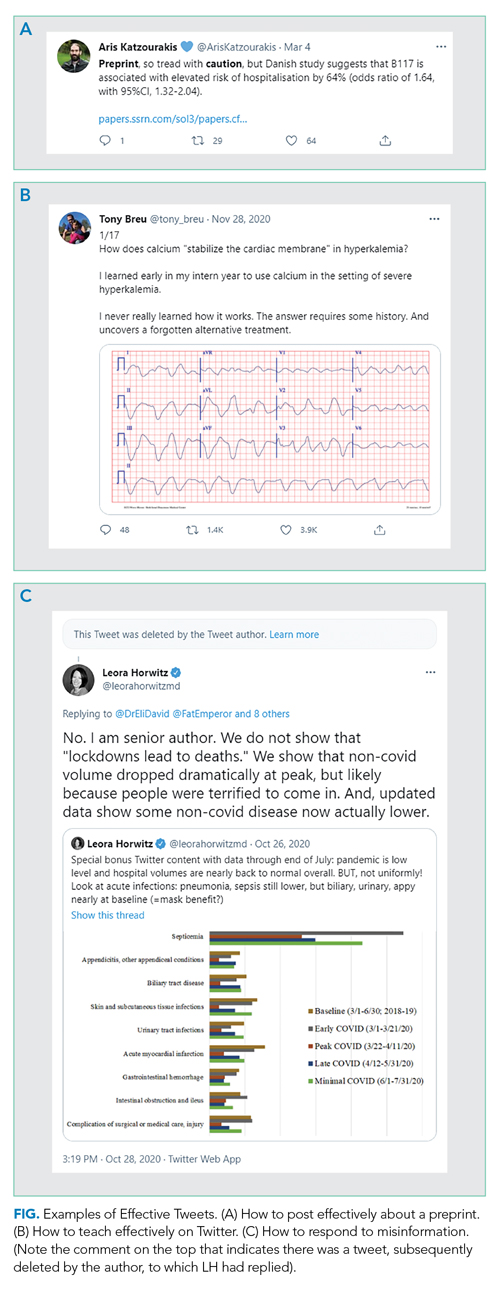
DO read the full article before posting. If you are posting an article, make sure you understand the whole context of any results you are highlighting. Avoid exaggerating, fear-mongering, or selectively picking facts or results to bolster your opinion.DO seek to add value to the public discourse. Rather than simply retweeting popular posts, consider taking the time to collate evidence (including contrary evidence) into a thread if seeking to prove a point or to teach, especially when it relates to something in your field. You likely are more knowledgeable about topics in your field than 99% of readers; use Twitter to spread your expertise. Clinical “tweetorials,” such as those popularized by @tony_breu, can be very effective teaching tools (Figure, part B).
DO make recommendations as specific as possible. If your goal is to improve adherence to evidence-based medicine or support disadvantaged people, be explicit about how you would achieve these goals. Tell readers exactly what you have in mind so that individuals and leaders can operationalize the recommendations. Use threads to expand on your advice and its rationale.
DO consider engaging with misinformation. We suggest doing so if the misinformation is posted by someone prominent who is likely to have broad reach, but only once per post and in a factual manner. You are unlikely to convince persons who post disinformation that they are wrong; extended arguments are unhelpful. Your role here is simply to inform readers of the post, who may be more open to reason. Occasionally, you may even convince the initial poster, as seen in Figure, part C, to delete certain misinformation. But don’t count on it.
DO consider your obligation to the general public. It is fine to engage explicitly with the medical community (ie, through tweetchats),2 but also consider that your comments will be accessible to everyone. Now more than ever the public is looking to healthcare professionals for clarity, reassurance, and evidence about medical matters.
DO acknowledge when you were wrong. Update your opinions as facts change or when you realize you made a mistake. The COVID-19 pandemic has brought home the rapidity with which we can gain scientific knowledge. Many of the things we thought were right early on—and posted about on Twitter—we now know to be wrong. Be forthright about this, while making it clear that the fact that we know more now doesn’t mean no information can be trusted. (A corollary: Don’t overstate what we know to be true at any time, so that it does not feel as much of a surprise if we later learn more and need to revise an opinion or a statement.)
DO be kind. This is perhaps the most important thing. We are all experiencing stress as physicians, parents, children, and colleagues. Spend your time focusing on people’s actions rather than impugning their motives or intelligence. Most of the time you don’t really know what their motives are. We recognize that kindness may not generate the same amount of engagement as sarcasm, but at least take time to consider whether you want to be seen as mean-spirited forever.
DO pause before sending. Twitter creates a false perception of the need for speed (and doesn’t really lend itself to revising drafts). But in reality, there is no rush. The torrent of Twitter posts means that people typically only see what has been posted around the time they log in; an early post is not necessarily more likely to be noticed. So, take your time and avoid falling into a trap of writing something you will regret, or, in extreme cases, that will get you fired or otherwise ruin your career. There is no rush to be first; Twitter will still be there tomorrow.
DON’T
For some time, mentors have warned physicians (and others whose careers depend on their reputation) to be careful in their use of social media. Electronic dissemination of inappropriate words or images can come back to haunt people—sometimes immediately, sometimes many years later.3 Physicians are also at risk of falling into some pitfalls specific to the profession. That said, here are some Don’ts to avoid or be cautious about.
DON’T reveal information about patients in a recognizable fashion. Journals ask for written consent from patients when authors submit a manuscript about individual cases so readers can be sure consent has been obtained. The same standard should apply to social media; if not, you are clearly violating a professional standard. Yet, on Twitter, people may assume you have not obtained consent, conveying a false sense of invasion of privacy and undermining confidence in the profession. The safest thing to do is not tell stories about patients, or to completely disguise the story so even the patients can’t recognize themselves. If you do choose to post about a patient, obtain written permission that you save, and clearly indicate that you have that permission in the Tweet.
DON’T claim to have expertise in areas where you have little training or education. For example, just because you are an expert in critical care and have seen the ravages of COVID-19 on your patients doesn’t mean you are an expert in how to stop a pandemic, though your observations may be helpful to those who are. This does not mean you shouldn’t speak out on important moral issues like climate change, nuclear war, or injustices, which clearly reflect personal opinion and values. Rather, be cautious about commenting authoritatively on areas in which the lay reader might mistakenly think you have specific expertise.
DON’T make yourself the hero of every story. Implicitly seeking praise for doing your job (Look at me, I’m working on Christmas!) may breed resentment and undercut professionalism. Rather, state what it is about your job that works well and what doesn’t (for example, teaching tips, wellness advice, and organizational strategies) in a way that helps others emulate your successes.
DON’T let emotions get the better of you. This past year has been full of outrageous and appalling events and behavior. We do not suggest that you ignore these. Rather, make sure that if you are blaming an individual for something that it really was their fault, because they had control of the factors that led to the disastrous outcome. Consider focusing on systemic and structural explanations for unacceptable phenomena to minimize defensiveness and maximize the potential for identifying solutions. And yes, sometimes you just have to let it rip, but be selective—maybe show your post to someone else and sleep on it before you send it.
CONCLUSION
We hope that you will find these suggestions helpful in both creating and reading social media posts on important topics. We recognize that some people like the spontaneity of the social media platform and will thus find our suggestions stunting. But at least everyone ought to consider what they are trying to achieve when they make public statements. The exchange of ideas has always been a key ingredient in creating progress. Let’s optimize the usefulness of those exchanges for that purpose, and to promote knowledge and science in a way that helps us all live healthier and happier lives.
1. Choo EK, Ranney ML, Chan TM, et al. Twitter as a tool for communication and knowledge exchange in academic medicine: a guide for skeptics and novices. Med Teach. 2015;37(5):411-416. https://doi.org/10.3109/0142159X.2014.993371
2. Admon AJ, Kaul V, Cribbs SK, Guzman E, Jimenez O, Richards JB. Twelve tips for developing and implementing a medical education Twitter chat. Med Teach. 2020;42(5):500-506. https://doi.org/10.1080/0142159X.2019.1598553
3. Langenfeld SJ, Batra R. How can social media get us in trouble? Clin Colon Rectal Surg. 2017;30(4):264-269. https://doi.org/10.1055/s-0037-1604255
1. Choo EK, Ranney ML, Chan TM, et al. Twitter as a tool for communication and knowledge exchange in academic medicine: a guide for skeptics and novices. Med Teach. 2015;37(5):411-416. https://doi.org/10.3109/0142159X.2014.993371
2. Admon AJ, Kaul V, Cribbs SK, Guzman E, Jimenez O, Richards JB. Twelve tips for developing and implementing a medical education Twitter chat. Med Teach. 2020;42(5):500-506. https://doi.org/10.1080/0142159X.2019.1598553
3. Langenfeld SJ, Batra R. How can social media get us in trouble? Clin Colon Rectal Surg. 2017;30(4):264-269. https://doi.org/10.1055/s-0037-1604255
© 2021 Society of Hospital Medicine
Rebuttal: Routine Daily Physical Exam
While we agree that a well-honed physical exam is one of the most important diagnostic tools than an internist can use, we have several responses to Drs Kanjee and McNamara’s point that a routine physical exam is essential for hospitalized patients.1 They argue that this exam might be helpful as a deliberate practice to improve skills for effective diagnostic exams. To this, we have two responses: the first is that the typical “routine” exam—a brief auscultation of the chest and abdomen—is performed frequently enough that additional practice should not be necessary for any practicing hospitalist. Performing a true full exam that would hone infrequently used skills, such as a full neurological exam, an orthopedic knee exam, or fundoscopy, comes at the expense of time spent talking to patients, as well as the potential harm of downstream testing cascades leading to adverse events. Second, we would argue that the real skill being developed is not “recognizing normal” but instead learning how to appropriately use physical diagnostic skills. Knowing precisely what exam maneuvers might be beneficial in a given hospitalized patient is incredibly complex, far more so than charts in evidence-based exam textbooks would suggest. It is this skill, not “recognizing normal,” that requires deliberate practice.
We agree that even during routine hospitalizations, daily exams may help detect complications of therapy, such as a patient with cellulitis on intravenous fluids developing volume overload. We are not against performing physical exams for diagnostic or monitoring purposes. In fact, it may be that most hospitalized patients would benefit from some sort of daily exam. However, rarely performed maneuvers, such as walking with patients or performing a validated delirium screen, are likely to have a higher yield than routine lung auscultation. It may also be true that hospitalized patients would benefit from certain screening exam maneuvers, but again, evidence is lacking, and decades of experience in the outpatient world would suggest the contrary.
Finally, and most ardently, we disagree that performing a routine daily physical exam can somehow inoculate against burnout. That is a view wholly unsupported by any evidence. The physical exam was originally developed as a diagnostic tool, not as a method to connect with patients. However, this traditional “routine” exam has been taught in medical schools as normal ever since, with very little serious interrogation of its utility or downstream effects. Increased cynicism about the exam’s usefulness, in our opinion, reflects physician cognizance of actual disutility of routine exams, rather than pining for a halcyon era that never existed. In fact, we believe a more hypothesis-driven diagnostic use of exams enriches physical diagnosis. For instance, listening to the chest of a patient with cellulitis on intravenous fluids is no longer “just listening,” it is an exercise specifically looking for a finding that affects management. Patient-centered care means tailoring all of our care—including the physical exam—to the needs of the patient. Doing a cursory, routine exam day after day for every patient with the goal of “recognizing normal” is not patient-centered, but rather physician-centered.
We do not doubt the importance of ritual, especially in such a stressful situation as a modern hospitalization. But rather than use a diagnostic procedure with downstream effects, we urge hospitalists to consider instead a ritual dating back to the time of Hippocrates—the compassionate physician sitting at the bedside, laying a hand on the shoulder, and listening to the patient’s concerns. That is authentic human connection rather than performance.
Acknowledgment
The authors of this point-counterpoint to thank Chris Smith, MD, and the members of the BIDMC Internal Medicine Residency Clinician Educator Track for thoughtful discussion around these topics.
1. McNamara LC, Kanjee Z. Counterpoint: routine daily physical exams add value for the hospitalist and patient. J Hosp Med. Published online August 18, 2021. https://doi.org/10.12788/jhm.3671
While we agree that a well-honed physical exam is one of the most important diagnostic tools than an internist can use, we have several responses to Drs Kanjee and McNamara’s point that a routine physical exam is essential for hospitalized patients.1 They argue that this exam might be helpful as a deliberate practice to improve skills for effective diagnostic exams. To this, we have two responses: the first is that the typical “routine” exam—a brief auscultation of the chest and abdomen—is performed frequently enough that additional practice should not be necessary for any practicing hospitalist. Performing a true full exam that would hone infrequently used skills, such as a full neurological exam, an orthopedic knee exam, or fundoscopy, comes at the expense of time spent talking to patients, as well as the potential harm of downstream testing cascades leading to adverse events. Second, we would argue that the real skill being developed is not “recognizing normal” but instead learning how to appropriately use physical diagnostic skills. Knowing precisely what exam maneuvers might be beneficial in a given hospitalized patient is incredibly complex, far more so than charts in evidence-based exam textbooks would suggest. It is this skill, not “recognizing normal,” that requires deliberate practice.
We agree that even during routine hospitalizations, daily exams may help detect complications of therapy, such as a patient with cellulitis on intravenous fluids developing volume overload. We are not against performing physical exams for diagnostic or monitoring purposes. In fact, it may be that most hospitalized patients would benefit from some sort of daily exam. However, rarely performed maneuvers, such as walking with patients or performing a validated delirium screen, are likely to have a higher yield than routine lung auscultation. It may also be true that hospitalized patients would benefit from certain screening exam maneuvers, but again, evidence is lacking, and decades of experience in the outpatient world would suggest the contrary.
Finally, and most ardently, we disagree that performing a routine daily physical exam can somehow inoculate against burnout. That is a view wholly unsupported by any evidence. The physical exam was originally developed as a diagnostic tool, not as a method to connect with patients. However, this traditional “routine” exam has been taught in medical schools as normal ever since, with very little serious interrogation of its utility or downstream effects. Increased cynicism about the exam’s usefulness, in our opinion, reflects physician cognizance of actual disutility of routine exams, rather than pining for a halcyon era that never existed. In fact, we believe a more hypothesis-driven diagnostic use of exams enriches physical diagnosis. For instance, listening to the chest of a patient with cellulitis on intravenous fluids is no longer “just listening,” it is an exercise specifically looking for a finding that affects management. Patient-centered care means tailoring all of our care—including the physical exam—to the needs of the patient. Doing a cursory, routine exam day after day for every patient with the goal of “recognizing normal” is not patient-centered, but rather physician-centered.
We do not doubt the importance of ritual, especially in such a stressful situation as a modern hospitalization. But rather than use a diagnostic procedure with downstream effects, we urge hospitalists to consider instead a ritual dating back to the time of Hippocrates—the compassionate physician sitting at the bedside, laying a hand on the shoulder, and listening to the patient’s concerns. That is authentic human connection rather than performance.
Acknowledgment
The authors of this point-counterpoint to thank Chris Smith, MD, and the members of the BIDMC Internal Medicine Residency Clinician Educator Track for thoughtful discussion around these topics.
While we agree that a well-honed physical exam is one of the most important diagnostic tools than an internist can use, we have several responses to Drs Kanjee and McNamara’s point that a routine physical exam is essential for hospitalized patients.1 They argue that this exam might be helpful as a deliberate practice to improve skills for effective diagnostic exams. To this, we have two responses: the first is that the typical “routine” exam—a brief auscultation of the chest and abdomen—is performed frequently enough that additional practice should not be necessary for any practicing hospitalist. Performing a true full exam that would hone infrequently used skills, such as a full neurological exam, an orthopedic knee exam, or fundoscopy, comes at the expense of time spent talking to patients, as well as the potential harm of downstream testing cascades leading to adverse events. Second, we would argue that the real skill being developed is not “recognizing normal” but instead learning how to appropriately use physical diagnostic skills. Knowing precisely what exam maneuvers might be beneficial in a given hospitalized patient is incredibly complex, far more so than charts in evidence-based exam textbooks would suggest. It is this skill, not “recognizing normal,” that requires deliberate practice.
We agree that even during routine hospitalizations, daily exams may help detect complications of therapy, such as a patient with cellulitis on intravenous fluids developing volume overload. We are not against performing physical exams for diagnostic or monitoring purposes. In fact, it may be that most hospitalized patients would benefit from some sort of daily exam. However, rarely performed maneuvers, such as walking with patients or performing a validated delirium screen, are likely to have a higher yield than routine lung auscultation. It may also be true that hospitalized patients would benefit from certain screening exam maneuvers, but again, evidence is lacking, and decades of experience in the outpatient world would suggest the contrary.
Finally, and most ardently, we disagree that performing a routine daily physical exam can somehow inoculate against burnout. That is a view wholly unsupported by any evidence. The physical exam was originally developed as a diagnostic tool, not as a method to connect with patients. However, this traditional “routine” exam has been taught in medical schools as normal ever since, with very little serious interrogation of its utility or downstream effects. Increased cynicism about the exam’s usefulness, in our opinion, reflects physician cognizance of actual disutility of routine exams, rather than pining for a halcyon era that never existed. In fact, we believe a more hypothesis-driven diagnostic use of exams enriches physical diagnosis. For instance, listening to the chest of a patient with cellulitis on intravenous fluids is no longer “just listening,” it is an exercise specifically looking for a finding that affects management. Patient-centered care means tailoring all of our care—including the physical exam—to the needs of the patient. Doing a cursory, routine exam day after day for every patient with the goal of “recognizing normal” is not patient-centered, but rather physician-centered.
We do not doubt the importance of ritual, especially in such a stressful situation as a modern hospitalization. But rather than use a diagnostic procedure with downstream effects, we urge hospitalists to consider instead a ritual dating back to the time of Hippocrates—the compassionate physician sitting at the bedside, laying a hand on the shoulder, and listening to the patient’s concerns. That is authentic human connection rather than performance.
Acknowledgment
The authors of this point-counterpoint to thank Chris Smith, MD, and the members of the BIDMC Internal Medicine Residency Clinician Educator Track for thoughtful discussion around these topics.
1. McNamara LC, Kanjee Z. Counterpoint: routine daily physical exams add value for the hospitalist and patient. J Hosp Med. Published online August 18, 2021. https://doi.org/10.12788/jhm.3671
1. McNamara LC, Kanjee Z. Counterpoint: routine daily physical exams add value for the hospitalist and patient. J Hosp Med. Published online August 18, 2021. https://doi.org/10.12788/jhm.3671
© 2021 Society of Hospital Medicine
Counterpoint: Routine Daily Physical Exams Add Value for the Hospitalist and Patient
We read with interest the perspective of Drs Rodman and Warnock,1 but disagree with the authors on several points. We find that the routine daily physical examination, often neglected or unappreciated amidst technological advances and new diagnostic testing, provides significant value to both hospitalist and patient in terms of diagnosis, treatment, patient-centered care, and maintaining the patient-doctor relationship.
First, the daily physical exam provides the practice that hospitalists need to develop and maintain necessary diagnostic finesse. We are taught fundamental physical exam maneuvers in medical school, but these skills often atrophy during residency and throughout our careers.2 This leaves us, as practicing physicians, potentially worse at these competencies than when we were students. The daily physical exam, on the other hand, provides frequent and effective practice to keep up and build upon these skills. We gain in part from our repeated normal exams, which help us to skillfully recognize the rare abnormal finding; a hospitalist must likely feel hundreds of normal abdomens to reliably discover a furtive abdominal mass. Our exams also benefit from several forms of prompt and relevant feedback, including that which is provided by subspecialist consultants (like a cardiologist agreeing with your assessment of jugular venous pressure) and other diagnostic tests (like the echocardiogram without the valvulopathy thought to be detected at the bedside). The physical examination is best learned at the bedside, and the daily exam offers an unparalleled opportunity to do so. Such continual skill improvement is necessary for hospitalists to accurately apply data from the evidence-based physical diagnosis literature. Many studies of the utility of various physical exam findings3 involve maneuvers performed by experts; to truly apply their results to our generalist practice, we are required to push ourselves to obtain the diagnostic expertise of the specialist. The daily physical examination, being the most concrete way for hospitalists to do so, is therefore essential to practicing better evidence-based physical diagnosis.
Beyond these larger benefits of the daily physical examination on our own practice and skills, patients in our care benefit diagnostically from these exams as well. Time and again, we see an inadequate or incomplete physical exam leading to errors or adverse patient outcomes.4,5 Even after completion of initial laboratory and imaging tests, laying of hands and stethoscope can lead to dramatic changes in inpatient diagnosis and management.6 The subsequent routine daily physical provides fresh opportunities to reexamine the evidence for or against our own working diagnoses and management plans. The adage that “you don’t know what you don’t know” is especially fitting here. We often do not know to look for and rule a disease process in or out if it is not on our initial differential on hospital day one or two; the daily physical exam allows us to be on the lookout for diagnoses we have not yet considered. The two of us have more than once made a serendipitous discovery of a new rash or other physical finding on hospital day three or four that helps suggest another, and ultimately correct, final diagnosis. Particularly in a setting in which so many inpatient diagnoses are wrong and can lead to patient harm,7 the daily physical examination provides an important check on our own diagnostic reasoning.
Even if we are right about the diagnosis, the daily exam also allows for timely recognition of complications from our management. Listening to each patient’s lungs every day, including those of patients with seemingly unrelated lower-extremity cellulitis, means we will more promptly notice when they retain fluid due to as yet unknown underlying heart failure. Those subtle bibasilar crackles not only become diagnostically useful, but also allow us the possibility of intervening and changing course even before the patient reports shortness of breath or the nurse notes hypoxemia on routine vital signs a day or two later. In an era when our treatment regimens are more complex, with frequent off-target results and side effects, the daily exam is a key screening tool for adverse outcomes in an increasingly ill population. Having a frequently updated and accurate baseline exam is also exceptionally important in the event of sudden neurologic deficits; an inpatient with new facial droop and left-arm weakness at 10
Finally, the daily physical examination is important to patient-centered care and potentially preventing physician burnout.8 Patients have more confidence in us when we conduct a thorough exam. The ritual of the physical exam is also an important contributor to the patient-doctor relationship, and a daily exam can help strengthen that bond each morning.9 Such benefits also extend to physicians. Hospitalists are spending less and less time at the bedside,10 a reality at least partially responsible for rising rates of burnout.11 We all went into clinical medicine to take care of and connect with people. The daily physical examination offers valuable time to show our patients we care about them while also giving us the opportunity to spend time with them, rather than with the “iPatient” that can otherwise become our focus.12 In this way, the daily physical examination can be immensely satisfying and may not only inoculate against burnout but also contribute to a stronger patient-doctor relationship.
For so many reasons, the daily physical exam is of great benefit to hospitalists looking to develop and maintain diagnostic skills, to our patients as we stay on the lookout for unexpected diagnoses and complications, and to the relationships we have with those for whom we care. It is a practice worth not only continuing but celebrating.
1. Rodman A, Warnock S. Point: routine daily physical exams in hospitalized patients are a waste of time. J Hosp Med. Published online August 18, 2021. https://doi.org/10.12788/jhm.3670
2. Vukanovic-Criley JM, Criley S, Warde CM, et al. Competency in cardiac examination skills in medical students, trainees, physicians, and faculty: a multicenter study. Arch Intern Med. 2006;166(6):610-616. https://doi.org/10.1001/archinte.166.6.610
3. McGee S. Evidence-Based Physical Diagnosis. 4th ed. Elsevier; 2018.
4. Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JPA. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med. 2015;128(12):1322-1324.e3. https://doi.org/10.1016/j.amjmed.2015.06.004
5. Singh H, Giardina TD, Meyer AND, Forjuoh SN, Reis MD, Thomas EJ. Types and origins of diagnostic errors in primary care settings. JAMA Intern Med. 2013;173(6):418-425. https://doi.org/10.1001/jamainternmed.2013.2777
6. Reilly BM. Physical examination in the care of medical inpatients: an observational study. Lancet. 2003;362(9390):1100-1105. https://doi.org/10.1016/S0140-6736(03)14464-9
7. Gunderson CG, Bilan VP, Holleck JL, et al. Prevalence of harmful diagnostic errors in hospitalised adults: a systematic review and meta-analysis. BMJ Qual Saf. 2020;29(12):1008-1018. https://doi.org/10.1136/bmjqs-2019-010822
8. Silverman B, Gertz A. Present role of the precordial examination in patient care. Am J Cardiol. 2015;115(2):253-255. https://doi.org/10.1016/j.amjcard.2014.10.031
9. Costanzo C, Verghese A. The physical examination as ritual: social sciences and embodiment in the context of the physical examination. Med Clin North Am. 2018;102(3):425-431. https://doi.org/10.1016/j.mcna.2017.12.004
10. Malkenson D, Siegal EM, Leff JA, Weber R, Struck R. Comparing academic and community-based hospitalists. J Hosp Med. 2010;5(6):349-352. https://doi.org/10.1002/jhm.793
11. Hipp DM, Rialon KL, Nevel K, Kothari AN, Jardine LDA. “Back to bedside”: Residents’ and fellows’ perspectives on finding meaning in work. J Grad Med Educ. 2017;9(2):269-273. https://doi.org/10.4300/JGME-D-17-00136.1
12. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461
We read with interest the perspective of Drs Rodman and Warnock,1 but disagree with the authors on several points. We find that the routine daily physical examination, often neglected or unappreciated amidst technological advances and new diagnostic testing, provides significant value to both hospitalist and patient in terms of diagnosis, treatment, patient-centered care, and maintaining the patient-doctor relationship.
First, the daily physical exam provides the practice that hospitalists need to develop and maintain necessary diagnostic finesse. We are taught fundamental physical exam maneuvers in medical school, but these skills often atrophy during residency and throughout our careers.2 This leaves us, as practicing physicians, potentially worse at these competencies than when we were students. The daily physical exam, on the other hand, provides frequent and effective practice to keep up and build upon these skills. We gain in part from our repeated normal exams, which help us to skillfully recognize the rare abnormal finding; a hospitalist must likely feel hundreds of normal abdomens to reliably discover a furtive abdominal mass. Our exams also benefit from several forms of prompt and relevant feedback, including that which is provided by subspecialist consultants (like a cardiologist agreeing with your assessment of jugular venous pressure) and other diagnostic tests (like the echocardiogram without the valvulopathy thought to be detected at the bedside). The physical examination is best learned at the bedside, and the daily exam offers an unparalleled opportunity to do so. Such continual skill improvement is necessary for hospitalists to accurately apply data from the evidence-based physical diagnosis literature. Many studies of the utility of various physical exam findings3 involve maneuvers performed by experts; to truly apply their results to our generalist practice, we are required to push ourselves to obtain the diagnostic expertise of the specialist. The daily physical examination, being the most concrete way for hospitalists to do so, is therefore essential to practicing better evidence-based physical diagnosis.
Beyond these larger benefits of the daily physical examination on our own practice and skills, patients in our care benefit diagnostically from these exams as well. Time and again, we see an inadequate or incomplete physical exam leading to errors or adverse patient outcomes.4,5 Even after completion of initial laboratory and imaging tests, laying of hands and stethoscope can lead to dramatic changes in inpatient diagnosis and management.6 The subsequent routine daily physical provides fresh opportunities to reexamine the evidence for or against our own working diagnoses and management plans. The adage that “you don’t know what you don’t know” is especially fitting here. We often do not know to look for and rule a disease process in or out if it is not on our initial differential on hospital day one or two; the daily physical exam allows us to be on the lookout for diagnoses we have not yet considered. The two of us have more than once made a serendipitous discovery of a new rash or other physical finding on hospital day three or four that helps suggest another, and ultimately correct, final diagnosis. Particularly in a setting in which so many inpatient diagnoses are wrong and can lead to patient harm,7 the daily physical examination provides an important check on our own diagnostic reasoning.
Even if we are right about the diagnosis, the daily exam also allows for timely recognition of complications from our management. Listening to each patient’s lungs every day, including those of patients with seemingly unrelated lower-extremity cellulitis, means we will more promptly notice when they retain fluid due to as yet unknown underlying heart failure. Those subtle bibasilar crackles not only become diagnostically useful, but also allow us the possibility of intervening and changing course even before the patient reports shortness of breath or the nurse notes hypoxemia on routine vital signs a day or two later. In an era when our treatment regimens are more complex, with frequent off-target results and side effects, the daily exam is a key screening tool for adverse outcomes in an increasingly ill population. Having a frequently updated and accurate baseline exam is also exceptionally important in the event of sudden neurologic deficits; an inpatient with new facial droop and left-arm weakness at 10
Finally, the daily physical examination is important to patient-centered care and potentially preventing physician burnout.8 Patients have more confidence in us when we conduct a thorough exam. The ritual of the physical exam is also an important contributor to the patient-doctor relationship, and a daily exam can help strengthen that bond each morning.9 Such benefits also extend to physicians. Hospitalists are spending less and less time at the bedside,10 a reality at least partially responsible for rising rates of burnout.11 We all went into clinical medicine to take care of and connect with people. The daily physical examination offers valuable time to show our patients we care about them while also giving us the opportunity to spend time with them, rather than with the “iPatient” that can otherwise become our focus.12 In this way, the daily physical examination can be immensely satisfying and may not only inoculate against burnout but also contribute to a stronger patient-doctor relationship.
For so many reasons, the daily physical exam is of great benefit to hospitalists looking to develop and maintain diagnostic skills, to our patients as we stay on the lookout for unexpected diagnoses and complications, and to the relationships we have with those for whom we care. It is a practice worth not only continuing but celebrating.
We read with interest the perspective of Drs Rodman and Warnock,1 but disagree with the authors on several points. We find that the routine daily physical examination, often neglected or unappreciated amidst technological advances and new diagnostic testing, provides significant value to both hospitalist and patient in terms of diagnosis, treatment, patient-centered care, and maintaining the patient-doctor relationship.
First, the daily physical exam provides the practice that hospitalists need to develop and maintain necessary diagnostic finesse. We are taught fundamental physical exam maneuvers in medical school, but these skills often atrophy during residency and throughout our careers.2 This leaves us, as practicing physicians, potentially worse at these competencies than when we were students. The daily physical exam, on the other hand, provides frequent and effective practice to keep up and build upon these skills. We gain in part from our repeated normal exams, which help us to skillfully recognize the rare abnormal finding; a hospitalist must likely feel hundreds of normal abdomens to reliably discover a furtive abdominal mass. Our exams also benefit from several forms of prompt and relevant feedback, including that which is provided by subspecialist consultants (like a cardiologist agreeing with your assessment of jugular venous pressure) and other diagnostic tests (like the echocardiogram without the valvulopathy thought to be detected at the bedside). The physical examination is best learned at the bedside, and the daily exam offers an unparalleled opportunity to do so. Such continual skill improvement is necessary for hospitalists to accurately apply data from the evidence-based physical diagnosis literature. Many studies of the utility of various physical exam findings3 involve maneuvers performed by experts; to truly apply their results to our generalist practice, we are required to push ourselves to obtain the diagnostic expertise of the specialist. The daily physical examination, being the most concrete way for hospitalists to do so, is therefore essential to practicing better evidence-based physical diagnosis.
Beyond these larger benefits of the daily physical examination on our own practice and skills, patients in our care benefit diagnostically from these exams as well. Time and again, we see an inadequate or incomplete physical exam leading to errors or adverse patient outcomes.4,5 Even after completion of initial laboratory and imaging tests, laying of hands and stethoscope can lead to dramatic changes in inpatient diagnosis and management.6 The subsequent routine daily physical provides fresh opportunities to reexamine the evidence for or against our own working diagnoses and management plans. The adage that “you don’t know what you don’t know” is especially fitting here. We often do not know to look for and rule a disease process in or out if it is not on our initial differential on hospital day one or two; the daily physical exam allows us to be on the lookout for diagnoses we have not yet considered. The two of us have more than once made a serendipitous discovery of a new rash or other physical finding on hospital day three or four that helps suggest another, and ultimately correct, final diagnosis. Particularly in a setting in which so many inpatient diagnoses are wrong and can lead to patient harm,7 the daily physical examination provides an important check on our own diagnostic reasoning.
Even if we are right about the diagnosis, the daily exam also allows for timely recognition of complications from our management. Listening to each patient’s lungs every day, including those of patients with seemingly unrelated lower-extremity cellulitis, means we will more promptly notice when they retain fluid due to as yet unknown underlying heart failure. Those subtle bibasilar crackles not only become diagnostically useful, but also allow us the possibility of intervening and changing course even before the patient reports shortness of breath or the nurse notes hypoxemia on routine vital signs a day or two later. In an era when our treatment regimens are more complex, with frequent off-target results and side effects, the daily exam is a key screening tool for adverse outcomes in an increasingly ill population. Having a frequently updated and accurate baseline exam is also exceptionally important in the event of sudden neurologic deficits; an inpatient with new facial droop and left-arm weakness at 10
Finally, the daily physical examination is important to patient-centered care and potentially preventing physician burnout.8 Patients have more confidence in us when we conduct a thorough exam. The ritual of the physical exam is also an important contributor to the patient-doctor relationship, and a daily exam can help strengthen that bond each morning.9 Such benefits also extend to physicians. Hospitalists are spending less and less time at the bedside,10 a reality at least partially responsible for rising rates of burnout.11 We all went into clinical medicine to take care of and connect with people. The daily physical examination offers valuable time to show our patients we care about them while also giving us the opportunity to spend time with them, rather than with the “iPatient” that can otherwise become our focus.12 In this way, the daily physical examination can be immensely satisfying and may not only inoculate against burnout but also contribute to a stronger patient-doctor relationship.
For so many reasons, the daily physical exam is of great benefit to hospitalists looking to develop and maintain diagnostic skills, to our patients as we stay on the lookout for unexpected diagnoses and complications, and to the relationships we have with those for whom we care. It is a practice worth not only continuing but celebrating.
1. Rodman A, Warnock S. Point: routine daily physical exams in hospitalized patients are a waste of time. J Hosp Med. Published online August 18, 2021. https://doi.org/10.12788/jhm.3670
2. Vukanovic-Criley JM, Criley S, Warde CM, et al. Competency in cardiac examination skills in medical students, trainees, physicians, and faculty: a multicenter study. Arch Intern Med. 2006;166(6):610-616. https://doi.org/10.1001/archinte.166.6.610
3. McGee S. Evidence-Based Physical Diagnosis. 4th ed. Elsevier; 2018.
4. Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JPA. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med. 2015;128(12):1322-1324.e3. https://doi.org/10.1016/j.amjmed.2015.06.004
5. Singh H, Giardina TD, Meyer AND, Forjuoh SN, Reis MD, Thomas EJ. Types and origins of diagnostic errors in primary care settings. JAMA Intern Med. 2013;173(6):418-425. https://doi.org/10.1001/jamainternmed.2013.2777
6. Reilly BM. Physical examination in the care of medical inpatients: an observational study. Lancet. 2003;362(9390):1100-1105. https://doi.org/10.1016/S0140-6736(03)14464-9
7. Gunderson CG, Bilan VP, Holleck JL, et al. Prevalence of harmful diagnostic errors in hospitalised adults: a systematic review and meta-analysis. BMJ Qual Saf. 2020;29(12):1008-1018. https://doi.org/10.1136/bmjqs-2019-010822
8. Silverman B, Gertz A. Present role of the precordial examination in patient care. Am J Cardiol. 2015;115(2):253-255. https://doi.org/10.1016/j.amjcard.2014.10.031
9. Costanzo C, Verghese A. The physical examination as ritual: social sciences and embodiment in the context of the physical examination. Med Clin North Am. 2018;102(3):425-431. https://doi.org/10.1016/j.mcna.2017.12.004
10. Malkenson D, Siegal EM, Leff JA, Weber R, Struck R. Comparing academic and community-based hospitalists. J Hosp Med. 2010;5(6):349-352. https://doi.org/10.1002/jhm.793
11. Hipp DM, Rialon KL, Nevel K, Kothari AN, Jardine LDA. “Back to bedside”: Residents’ and fellows’ perspectives on finding meaning in work. J Grad Med Educ. 2017;9(2):269-273. https://doi.org/10.4300/JGME-D-17-00136.1
12. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461
1. Rodman A, Warnock S. Point: routine daily physical exams in hospitalized patients are a waste of time. J Hosp Med. Published online August 18, 2021. https://doi.org/10.12788/jhm.3670
2. Vukanovic-Criley JM, Criley S, Warde CM, et al. Competency in cardiac examination skills in medical students, trainees, physicians, and faculty: a multicenter study. Arch Intern Med. 2006;166(6):610-616. https://doi.org/10.1001/archinte.166.6.610
3. McGee S. Evidence-Based Physical Diagnosis. 4th ed. Elsevier; 2018.
4. Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JPA. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med. 2015;128(12):1322-1324.e3. https://doi.org/10.1016/j.amjmed.2015.06.004
5. Singh H, Giardina TD, Meyer AND, Forjuoh SN, Reis MD, Thomas EJ. Types and origins of diagnostic errors in primary care settings. JAMA Intern Med. 2013;173(6):418-425. https://doi.org/10.1001/jamainternmed.2013.2777
6. Reilly BM. Physical examination in the care of medical inpatients: an observational study. Lancet. 2003;362(9390):1100-1105. https://doi.org/10.1016/S0140-6736(03)14464-9
7. Gunderson CG, Bilan VP, Holleck JL, et al. Prevalence of harmful diagnostic errors in hospitalised adults: a systematic review and meta-analysis. BMJ Qual Saf. 2020;29(12):1008-1018. https://doi.org/10.1136/bmjqs-2019-010822
8. Silverman B, Gertz A. Present role of the precordial examination in patient care. Am J Cardiol. 2015;115(2):253-255. https://doi.org/10.1016/j.amjcard.2014.10.031
9. Costanzo C, Verghese A. The physical examination as ritual: social sciences and embodiment in the context of the physical examination. Med Clin North Am. 2018;102(3):425-431. https://doi.org/10.1016/j.mcna.2017.12.004
10. Malkenson D, Siegal EM, Leff JA, Weber R, Struck R. Comparing academic and community-based hospitalists. J Hosp Med. 2010;5(6):349-352. https://doi.org/10.1002/jhm.793
11. Hipp DM, Rialon KL, Nevel K, Kothari AN, Jardine LDA. “Back to bedside”: Residents’ and fellows’ perspectives on finding meaning in work. J Grad Med Educ. 2017;9(2):269-273. https://doi.org/10.4300/JGME-D-17-00136.1
12. Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748-2751. https://doi.org/10.1056/NEJMp0807461
© 2021 Society of Hospital Medicine
Point: Routine Daily Physical Exams in Hospitalized Patients Are a Waste of Time
Every day, physicians engage in an elaborate performance with their patients—the routine complete physical exam. We argue that this purportedly time-tested ritual is at best a waste of time, and at worst potentially harmful.
The modern physical exam evolved throughout the 19th century as the first diagnostic tool in a medical field that was rapidly transforming from its traditional roots to a modern scientific discipline.1 Despite the vast increase in diagnostic tools since then, the physical exam remains one of the most predictive. Several decades of investigation into the “evidence-based” physical exam have attempted to calculate the test characteristics of individual exam findings, confirming that the exam remains as useful a diagnostic tool today as it was for Laënnec or Osler.2
Performing a physical exam for the purposes of diagnosis and prognosis—not only on admission, but also on a daily basis to assess treatment response—remains a fundamental part of a hospitalist’s job. For example, a daily volume assessment, including cardiac auscultation for an S3, evaluation of the jugular venous pulse, and measurement of edema, is essential in managing patients with decompensated heart failure. However, when we stray from these diagnostic purposes, we are no longer using the exam as intended.
The physical exam most frequently performed in the hospital today is the so-called routine daily exam. Generally, this involves passing a stethoscope fleetingly across the chest and abdomen, perhaps with some additional palpation of the abdomen. Cranial nerves II through XII may also occasionally be checked. This routine exam—and by extension, the templated physical exams that fill hospitalists’ documentation—not only lack an evidence base, but also are arguably harmful to patients. Such exams should not be part of a hospitalist’s daily practice.
The most concerning aspect of a routine daily exam is that examination of an asymptomatic patient—for example, auscultation of the lungs of a patient admitted with lower extremity cellulitis—is fundamentally a screening rather than a diagnostic test. While little work has been done in the inpatient setting, decades of studies on outpatient screening exams demonstrate that very few of them are effective.3 For example, a review of commonly used exam maneuvers in wellness visits concluded that “for the asymptomatic, nonpregnant adult of any age, no evidence supports the need for a complete physical exam as traditionally defined,” recommending against such popular maneuvers as lung and heart auscultation and peripheral pulse palpation.4 While the inpatient hospital medicine population has different characteristics that may warrant a routine exam, there is no evidence to support such practice.
It is often argued that the routine physical exam is “cheap” and “quick” and, therefore, should be performed regardless of evidence. While this is certainly true for many diagnostic physical exams, the literature suggests that there is no reason to think that a routine physical exam would be cost-effective.5 Even cost-effective screening physical exam tests, such as an outpatient nurse performing a 1-minute pulse palpation starting at age 55, have incremental costs measuring in the thousands of dollars.6 Furthermore, screening tests can have unexpected downstream effects that are both costly and associated with morbidity and mortality.7 For example, abdominal palpation of a “prominent” aorta can lead to imaging, where incidental findings can trigger procedures that may involve complications.
In addition to potentially adding more risk, the routine daily physical exam represents time that can be better allocated. Medical residents spend the vast majority of their day at the computer, while spending less than 10% of their time at the patient’s bedside.8 Anything that takes up that valuable time, including a “routine exam,” is time spent not talking to the patient, learning about their symptoms, their fears, and who they are as human beings.
It is also true that patients expect a physical exam to be performed, and that additional exam maneuvers, including potentially invasive exams, are associated with increasing patient satisfaction.9 However, these arguments miss much of the nuance of why patients have these expectations. Qualitative research suggests that much of a patient’s desire for unnecessary tests or exams is actually their concern about a lack of validation or empathy from the physician, as well as general skepticism about evidence-based medical decision-making.10 Perhaps spending more face time with patients discussing their issues, rather than idle time performing routine maneuvers, would lead to even greater patient satisfaction.
Finally, one of the most popular arguments in defense of a routine physical exam is that the exam is a “sacred ritual” essential to the patient-physician relationship.11 However, this is an argument not supported by historical interpretation. The physical exam was developed as an explicitly diagnostic procedure in the early 19th century, while the primacy of the doctor-physician relationship dates back millennia, long before the development of the modern physical exam. Furthermore, modern historiography has identified the development of the physical exam as part of a movement to minimize the experience of the patient in their own disease, and to situate the physician as the ultimate source of knowledge about a patient’s body rather than an attempt to strengthen a relationship.12
Ritual is indeed important, and the exam as currently practiced may indeed reinforce the physician-patient relationship. But we should also keep in mind what that relationship entails. Having full access to a patient’s unclothed body and having the ability to perform invasive procedures are far beyond regular social norms—these are powerful diagnostic tools, yes, but they also serve to reinforce an imbalance of power in the relationship. Medical rituals have also changed dramatically over time. Modern evidence suggests that pulse palpation alone, the form of the exam that was dominant for millennia, has profound physiological effects even on critically ill patients.13 Rather than a diagnostic exam that has potential downstream cost implications and consumes valuable time from an encounter, we suggest a return to a more traditional ritual of physical touch: sitting at the patient’s bedside, holding their hand, and speaking to them compassionately about their fears and hopes. This would be a far more valuable “routine” encounter to incorporate into the busy hospitalist’s day.
Acknowledgment
The authors of this point-counterpoint thank Chris Smith, MD, and the members of the BIDMC Internal Medicine Residency Clinician Educator Track for thoughtful discussion around these topics.
1. Laënnec RTH. De l’auscultation médiate ou Traité du Diagnostic des Maladies des Poumon et du Coeur fondé principalement sur ce Nouveau Moyen d’Exploration. Brosson & Chaudé; 1819.
2. McGee S. Evidence-Based Physical Diagnosis. 4th ed. Elsevier; 2018.
3. Bloomfield HE, Wilt TJ. Evidence brief: Role of the annual comprehensive physical examination in the asymptomatic adult. VA Evidence Synthesis Program Evidence Briefs. US Department of Veterans Affairs; October 2011.
4. Oboler SK, LaForce FM. The periodic physical examination in asymptomatic adults. Ann Intern Med. 1989;110(3):214-226. https://doi.org/10.7326/0003-4819-110-3-214
5. Angus S. The cost-effective evaluation of syncope. Med Clin North Am. 2016;100(5):1019-1032. https://doi.org/10.1016/j.mcna.2016.04.010
6. Welton NJ, McAleenan A, Thom HH, et al. Screening strategies for atrial fibrillation: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2017;21(29):1-236. https://doi.org/10.3310/hta21290
7. Rothberg MB. The $50 000 physical. JAMA. 2020;323(17):1682-1683. https://doi.org/10.1001/jama.2020.2866
8. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148
9. Duan L, Mukherjee EM, Federman DG. The physical examination: a survey of patient preferences and expectations during primary care visits. Postgrad Med. 2020;132(1):102-108. https://doi.org/10.1080/00325481.2020.1713618
10. Kravitz RL, Callahan EJ. Patients’ perceptions of omitted examinations and tests: a qualitative analysis. J Gen Intern Med. 2000;15(1):38-45. https://doi.org/10.1046/j.1525-1497.2000.12058.x
11. Costanzo C, Verghese A. The physical examination as ritual: social sciences and embodiment in the context of the physical examination. Med Clin North Am. 2018;102(3):425-431. https://doi.org/10.1016/j.mcna.2017.12.004
12. Jewson ND. The disappearance of the sick-man from medical cosmology, 1770–1870. Int J Epidemiol. 2009;38(3):622-633. https://doi.org/10.1093/ije/dyp180
13. Arnold MH, Komesaroff P, Kerridge I. Understanding the ethical implications of the rituals of medicine. Intern Med J. 2020;50(9):1123-1131. https://doi.org/10.1111/imj.14990
Every day, physicians engage in an elaborate performance with their patients—the routine complete physical exam. We argue that this purportedly time-tested ritual is at best a waste of time, and at worst potentially harmful.
The modern physical exam evolved throughout the 19th century as the first diagnostic tool in a medical field that was rapidly transforming from its traditional roots to a modern scientific discipline.1 Despite the vast increase in diagnostic tools since then, the physical exam remains one of the most predictive. Several decades of investigation into the “evidence-based” physical exam have attempted to calculate the test characteristics of individual exam findings, confirming that the exam remains as useful a diagnostic tool today as it was for Laënnec or Osler.2
Performing a physical exam for the purposes of diagnosis and prognosis—not only on admission, but also on a daily basis to assess treatment response—remains a fundamental part of a hospitalist’s job. For example, a daily volume assessment, including cardiac auscultation for an S3, evaluation of the jugular venous pulse, and measurement of edema, is essential in managing patients with decompensated heart failure. However, when we stray from these diagnostic purposes, we are no longer using the exam as intended.
The physical exam most frequently performed in the hospital today is the so-called routine daily exam. Generally, this involves passing a stethoscope fleetingly across the chest and abdomen, perhaps with some additional palpation of the abdomen. Cranial nerves II through XII may also occasionally be checked. This routine exam—and by extension, the templated physical exams that fill hospitalists’ documentation—not only lack an evidence base, but also are arguably harmful to patients. Such exams should not be part of a hospitalist’s daily practice.
The most concerning aspect of a routine daily exam is that examination of an asymptomatic patient—for example, auscultation of the lungs of a patient admitted with lower extremity cellulitis—is fundamentally a screening rather than a diagnostic test. While little work has been done in the inpatient setting, decades of studies on outpatient screening exams demonstrate that very few of them are effective.3 For example, a review of commonly used exam maneuvers in wellness visits concluded that “for the asymptomatic, nonpregnant adult of any age, no evidence supports the need for a complete physical exam as traditionally defined,” recommending against such popular maneuvers as lung and heart auscultation and peripheral pulse palpation.4 While the inpatient hospital medicine population has different characteristics that may warrant a routine exam, there is no evidence to support such practice.
It is often argued that the routine physical exam is “cheap” and “quick” and, therefore, should be performed regardless of evidence. While this is certainly true for many diagnostic physical exams, the literature suggests that there is no reason to think that a routine physical exam would be cost-effective.5 Even cost-effective screening physical exam tests, such as an outpatient nurse performing a 1-minute pulse palpation starting at age 55, have incremental costs measuring in the thousands of dollars.6 Furthermore, screening tests can have unexpected downstream effects that are both costly and associated with morbidity and mortality.7 For example, abdominal palpation of a “prominent” aorta can lead to imaging, where incidental findings can trigger procedures that may involve complications.
In addition to potentially adding more risk, the routine daily physical exam represents time that can be better allocated. Medical residents spend the vast majority of their day at the computer, while spending less than 10% of their time at the patient’s bedside.8 Anything that takes up that valuable time, including a “routine exam,” is time spent not talking to the patient, learning about their symptoms, their fears, and who they are as human beings.
It is also true that patients expect a physical exam to be performed, and that additional exam maneuvers, including potentially invasive exams, are associated with increasing patient satisfaction.9 However, these arguments miss much of the nuance of why patients have these expectations. Qualitative research suggests that much of a patient’s desire for unnecessary tests or exams is actually their concern about a lack of validation or empathy from the physician, as well as general skepticism about evidence-based medical decision-making.10 Perhaps spending more face time with patients discussing their issues, rather than idle time performing routine maneuvers, would lead to even greater patient satisfaction.
Finally, one of the most popular arguments in defense of a routine physical exam is that the exam is a “sacred ritual” essential to the patient-physician relationship.11 However, this is an argument not supported by historical interpretation. The physical exam was developed as an explicitly diagnostic procedure in the early 19th century, while the primacy of the doctor-physician relationship dates back millennia, long before the development of the modern physical exam. Furthermore, modern historiography has identified the development of the physical exam as part of a movement to minimize the experience of the patient in their own disease, and to situate the physician as the ultimate source of knowledge about a patient’s body rather than an attempt to strengthen a relationship.12
Ritual is indeed important, and the exam as currently practiced may indeed reinforce the physician-patient relationship. But we should also keep in mind what that relationship entails. Having full access to a patient’s unclothed body and having the ability to perform invasive procedures are far beyond regular social norms—these are powerful diagnostic tools, yes, but they also serve to reinforce an imbalance of power in the relationship. Medical rituals have also changed dramatically over time. Modern evidence suggests that pulse palpation alone, the form of the exam that was dominant for millennia, has profound physiological effects even on critically ill patients.13 Rather than a diagnostic exam that has potential downstream cost implications and consumes valuable time from an encounter, we suggest a return to a more traditional ritual of physical touch: sitting at the patient’s bedside, holding their hand, and speaking to them compassionately about their fears and hopes. This would be a far more valuable “routine” encounter to incorporate into the busy hospitalist’s day.
Acknowledgment
The authors of this point-counterpoint thank Chris Smith, MD, and the members of the BIDMC Internal Medicine Residency Clinician Educator Track for thoughtful discussion around these topics.
Every day, physicians engage in an elaborate performance with their patients—the routine complete physical exam. We argue that this purportedly time-tested ritual is at best a waste of time, and at worst potentially harmful.
The modern physical exam evolved throughout the 19th century as the first diagnostic tool in a medical field that was rapidly transforming from its traditional roots to a modern scientific discipline.1 Despite the vast increase in diagnostic tools since then, the physical exam remains one of the most predictive. Several decades of investigation into the “evidence-based” physical exam have attempted to calculate the test characteristics of individual exam findings, confirming that the exam remains as useful a diagnostic tool today as it was for Laënnec or Osler.2
Performing a physical exam for the purposes of diagnosis and prognosis—not only on admission, but also on a daily basis to assess treatment response—remains a fundamental part of a hospitalist’s job. For example, a daily volume assessment, including cardiac auscultation for an S3, evaluation of the jugular venous pulse, and measurement of edema, is essential in managing patients with decompensated heart failure. However, when we stray from these diagnostic purposes, we are no longer using the exam as intended.
The physical exam most frequently performed in the hospital today is the so-called routine daily exam. Generally, this involves passing a stethoscope fleetingly across the chest and abdomen, perhaps with some additional palpation of the abdomen. Cranial nerves II through XII may also occasionally be checked. This routine exam—and by extension, the templated physical exams that fill hospitalists’ documentation—not only lack an evidence base, but also are arguably harmful to patients. Such exams should not be part of a hospitalist’s daily practice.
The most concerning aspect of a routine daily exam is that examination of an asymptomatic patient—for example, auscultation of the lungs of a patient admitted with lower extremity cellulitis—is fundamentally a screening rather than a diagnostic test. While little work has been done in the inpatient setting, decades of studies on outpatient screening exams demonstrate that very few of them are effective.3 For example, a review of commonly used exam maneuvers in wellness visits concluded that “for the asymptomatic, nonpregnant adult of any age, no evidence supports the need for a complete physical exam as traditionally defined,” recommending against such popular maneuvers as lung and heart auscultation and peripheral pulse palpation.4 While the inpatient hospital medicine population has different characteristics that may warrant a routine exam, there is no evidence to support such practice.
It is often argued that the routine physical exam is “cheap” and “quick” and, therefore, should be performed regardless of evidence. While this is certainly true for many diagnostic physical exams, the literature suggests that there is no reason to think that a routine physical exam would be cost-effective.5 Even cost-effective screening physical exam tests, such as an outpatient nurse performing a 1-minute pulse palpation starting at age 55, have incremental costs measuring in the thousands of dollars.6 Furthermore, screening tests can have unexpected downstream effects that are both costly and associated with morbidity and mortality.7 For example, abdominal palpation of a “prominent” aorta can lead to imaging, where incidental findings can trigger procedures that may involve complications.
In addition to potentially adding more risk, the routine daily physical exam represents time that can be better allocated. Medical residents spend the vast majority of their day at the computer, while spending less than 10% of their time at the patient’s bedside.8 Anything that takes up that valuable time, including a “routine exam,” is time spent not talking to the patient, learning about their symptoms, their fears, and who they are as human beings.
It is also true that patients expect a physical exam to be performed, and that additional exam maneuvers, including potentially invasive exams, are associated with increasing patient satisfaction.9 However, these arguments miss much of the nuance of why patients have these expectations. Qualitative research suggests that much of a patient’s desire for unnecessary tests or exams is actually their concern about a lack of validation or empathy from the physician, as well as general skepticism about evidence-based medical decision-making.10 Perhaps spending more face time with patients discussing their issues, rather than idle time performing routine maneuvers, would lead to even greater patient satisfaction.
Finally, one of the most popular arguments in defense of a routine physical exam is that the exam is a “sacred ritual” essential to the patient-physician relationship.11 However, this is an argument not supported by historical interpretation. The physical exam was developed as an explicitly diagnostic procedure in the early 19th century, while the primacy of the doctor-physician relationship dates back millennia, long before the development of the modern physical exam. Furthermore, modern historiography has identified the development of the physical exam as part of a movement to minimize the experience of the patient in their own disease, and to situate the physician as the ultimate source of knowledge about a patient’s body rather than an attempt to strengthen a relationship.12
Ritual is indeed important, and the exam as currently practiced may indeed reinforce the physician-patient relationship. But we should also keep in mind what that relationship entails. Having full access to a patient’s unclothed body and having the ability to perform invasive procedures are far beyond regular social norms—these are powerful diagnostic tools, yes, but they also serve to reinforce an imbalance of power in the relationship. Medical rituals have also changed dramatically over time. Modern evidence suggests that pulse palpation alone, the form of the exam that was dominant for millennia, has profound physiological effects even on critically ill patients.13 Rather than a diagnostic exam that has potential downstream cost implications and consumes valuable time from an encounter, we suggest a return to a more traditional ritual of physical touch: sitting at the patient’s bedside, holding their hand, and speaking to them compassionately about their fears and hopes. This would be a far more valuable “routine” encounter to incorporate into the busy hospitalist’s day.
Acknowledgment
The authors of this point-counterpoint thank Chris Smith, MD, and the members of the BIDMC Internal Medicine Residency Clinician Educator Track for thoughtful discussion around these topics.
1. Laënnec RTH. De l’auscultation médiate ou Traité du Diagnostic des Maladies des Poumon et du Coeur fondé principalement sur ce Nouveau Moyen d’Exploration. Brosson & Chaudé; 1819.
2. McGee S. Evidence-Based Physical Diagnosis. 4th ed. Elsevier; 2018.
3. Bloomfield HE, Wilt TJ. Evidence brief: Role of the annual comprehensive physical examination in the asymptomatic adult. VA Evidence Synthesis Program Evidence Briefs. US Department of Veterans Affairs; October 2011.
4. Oboler SK, LaForce FM. The periodic physical examination in asymptomatic adults. Ann Intern Med. 1989;110(3):214-226. https://doi.org/10.7326/0003-4819-110-3-214
5. Angus S. The cost-effective evaluation of syncope. Med Clin North Am. 2016;100(5):1019-1032. https://doi.org/10.1016/j.mcna.2016.04.010
6. Welton NJ, McAleenan A, Thom HH, et al. Screening strategies for atrial fibrillation: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2017;21(29):1-236. https://doi.org/10.3310/hta21290
7. Rothberg MB. The $50 000 physical. JAMA. 2020;323(17):1682-1683. https://doi.org/10.1001/jama.2020.2866
8. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148
9. Duan L, Mukherjee EM, Federman DG. The physical examination: a survey of patient preferences and expectations during primary care visits. Postgrad Med. 2020;132(1):102-108. https://doi.org/10.1080/00325481.2020.1713618
10. Kravitz RL, Callahan EJ. Patients’ perceptions of omitted examinations and tests: a qualitative analysis. J Gen Intern Med. 2000;15(1):38-45. https://doi.org/10.1046/j.1525-1497.2000.12058.x
11. Costanzo C, Verghese A. The physical examination as ritual: social sciences and embodiment in the context of the physical examination. Med Clin North Am. 2018;102(3):425-431. https://doi.org/10.1016/j.mcna.2017.12.004
12. Jewson ND. The disappearance of the sick-man from medical cosmology, 1770–1870. Int J Epidemiol. 2009;38(3):622-633. https://doi.org/10.1093/ije/dyp180
13. Arnold MH, Komesaroff P, Kerridge I. Understanding the ethical implications of the rituals of medicine. Intern Med J. 2020;50(9):1123-1131. https://doi.org/10.1111/imj.14990
1. Laënnec RTH. De l’auscultation médiate ou Traité du Diagnostic des Maladies des Poumon et du Coeur fondé principalement sur ce Nouveau Moyen d’Exploration. Brosson & Chaudé; 1819.
2. McGee S. Evidence-Based Physical Diagnosis. 4th ed. Elsevier; 2018.
3. Bloomfield HE, Wilt TJ. Evidence brief: Role of the annual comprehensive physical examination in the asymptomatic adult. VA Evidence Synthesis Program Evidence Briefs. US Department of Veterans Affairs; October 2011.
4. Oboler SK, LaForce FM. The periodic physical examination in asymptomatic adults. Ann Intern Med. 1989;110(3):214-226. https://doi.org/10.7326/0003-4819-110-3-214
5. Angus S. The cost-effective evaluation of syncope. Med Clin North Am. 2016;100(5):1019-1032. https://doi.org/10.1016/j.mcna.2016.04.010
6. Welton NJ, McAleenan A, Thom HH, et al. Screening strategies for atrial fibrillation: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2017;21(29):1-236. https://doi.org/10.3310/hta21290
7. Rothberg MB. The $50 000 physical. JAMA. 2020;323(17):1682-1683. https://doi.org/10.1001/jama.2020.2866
8. Mamykina L, Vawdrey DK, Hripcsak G. How do residents spend their shift time? A time and motion study with a particular focus on the use of computers. Acad Med. 2016;91(6):827-832. https://doi.org/10.1097/ACM.0000000000001148
9. Duan L, Mukherjee EM, Federman DG. The physical examination: a survey of patient preferences and expectations during primary care visits. Postgrad Med. 2020;132(1):102-108. https://doi.org/10.1080/00325481.2020.1713618
10. Kravitz RL, Callahan EJ. Patients’ perceptions of omitted examinations and tests: a qualitative analysis. J Gen Intern Med. 2000;15(1):38-45. https://doi.org/10.1046/j.1525-1497.2000.12058.x
11. Costanzo C, Verghese A. The physical examination as ritual: social sciences and embodiment in the context of the physical examination. Med Clin North Am. 2018;102(3):425-431. https://doi.org/10.1016/j.mcna.2017.12.004
12. Jewson ND. The disappearance of the sick-man from medical cosmology, 1770–1870. Int J Epidemiol. 2009;38(3):622-633. https://doi.org/10.1093/ije/dyp180
13. Arnold MH, Komesaroff P, Kerridge I. Understanding the ethical implications of the rituals of medicine. Intern Med J. 2020;50(9):1123-1131. https://doi.org/10.1111/imj.14990
© 2021 Society of Hospital Medicine