User login
Beyond a Purple Journal: Improving Hospital-Based Addiction Care
Rosa* was one of my first patients as an intern rotating at the county hospital. Her marriage had disintegrated years earlier. To cope with depression, she hid a daily ritual of orange juice and vodka from her children. She worked as a cashier, until nausea and fatigue overwhelmed her.
The first time I met her she sat on the gurney: petite, tanned, and pregnant. Then I saw her yellow eyes and revised: temporal wasting, jaundiced, and swollen with ascites. Rosa didn’t know that alcohol could cause liver disease. Without insurance or access to primary care, her untreated alcohol use disorder (AUD) and depression had snowballed for years.
Midway through my intern year, I’d taken care of many people with AUD. However, I’d barely learned anything about it as a medical student, though we’d spent weeks studying esoteric diseases, that now––9 years after medical school––I still have not encountered.
Among the 28.3 million individuals in the United States with AUD, only 1% receive medication treatment.1 In the United States, unhealthy alcohol use accounts for more than 95,000 deaths each year.2 This number likely under-captures alcohol-related mortality and is higher now given recent reports of increasing alcohol-related deaths and prevalence of unhealthy alcohol use, especially among women, younger age groups, and marginalized populations.3-5
Rosa had alcohol-related hepatitis, which can cause severe inflammation and liver failure and quickly lead to death. As her liver failure progressed, I asked the gastroenterologists, “What other treatments can we offer? Is she a liver transplant candidate?” “Nothing” and “No” they answered.
Later, I emailed the hepatologist and transplant surgeon begging them to reevaluate her transplantation candidacy, but they told me there was no exception to the institution’s 6-month sobriety rule.
Maintaining a 6-month sobriety period is not an evidence-based criterion for transplantation. However, 50% of transplant centers do not perform transplantation prior to 6 months of alcohol abstinence for alcohol-related hepatitis due to concern for return to drinking after transplant.6 This practice may promote bias in patient selection for transplantation. A recent study found that individuals with alcohol-related liver disease transplanted before 6 months of abstinence had similar rates of survival and return to drinking compared to those who abstained from alcohol for 6 months and participated in AUD treatment before transplantation.7
There are other liver transplant practices that result in inequities for individuals with substance use disorders (SUD). Some liver transplant centers consider being on a medication for opioid use disorder a contraindication for transplantation—even if the individual is in recovery and abstaining from substances.8 Others mandate that individuals with alcohol-related liver disease attend Alcoholics Anonymous (AA) meetings prior to transplant. While mutual help groups, including AA, may benefit some individuals, different approaches work for different people.9 Other psychosocial interventions (eg, cognitive-behavioral therapy, contingency management, and residential treatment) and medications also help individuals reduce or stop drinking. Some meet their goals without any treatment. Addiction care works best when it respects autonomy and meets individuals where they are by allowing them to decide among options.
While organ allocations are a crystalized example of inequities in addiction care, they are also ethically complex. Many individuals—with and without SUD—die on waiting lists and must meet stringent transplantation criteria. However, we can at least remove the unnecessary biases that compound inequities in care people with SUD already face.
As Rosa’s liver succumbed, her kidneys failed too, and she required dialysis. She sensed what was coming. “I want everything…for now. I need to take care of my children.” I, too, wanted Rosa to live and see her youngest start kindergarten.
A few days before her discharge, I walked to the pharmacy and bought a purple journal. In a rare moment, I found Rosa alone in her room, without her ex-husband, sister, and mother, who rarely left her bedside. Together, we called AA and explored whether she could start participating in phone meetings from the hospital. I explained that one way to document a commitment to sobriety, as the transplant center’s rules dictated, was to attend and document AA meetings in this notebook. “In 5 months, you will be a liver transplant candidate,” I remember saying, wishing it to fruition.
I became Rosa’s primary care physician and saw her in clinic. Over the next few weeks, her skin took on an ashen tone. Sleep escaped her and her thoughts and speech blurred. Her walk slowed and she needed a wheelchair. The quiet fierceness that had defined her dissipated as encephalopathy took over. But until our last visit, she brought her purple journal, tracking the AA meetings she’d attended. Dialysis became intolerable, but not before Rosa made care arrangements for her girls. When that happened, she stopped dialysis and went to Mexico, where she died in her sleep after saying good-bye to her father.
Earlier access to healthcare and effective depression and AUD treatment could have saved Rosa’s life. While it was too late for her, as hospitalists we care for many others with substance-related complications and may miss opportunities to discuss and offer evidence-based addiction treatment. For example, we initiate the most up-to-date management for a patient’s gastrointestinal bleed but may leave the alcohol discussion for someone else. It is similar for other SUD: we treat cellulitis, epidural abscesses, bacteremia, chronic obstructive pulmonary disease, heart failure exacerbations, and other complications of SUD without addressing the root cause of the hospitalization—other than to prescribe abstinence from substance use or, at our worst, scold individuals for continuing to use.
But what can we offer? Most healthcare professionals still do not receive addiction education during training. Without tools, we enact temporizing measures, until patients return to the hospital or die.
In addition to increasing alcohol-related morbidity, there have also been increases in drug-related overdoses, fueled by COVID-19, synthetic opioids like fentanyl, and stimulants.10 In the 12-month period ending April 2021, more than 100,000 individuals died of drug-related overdoses, the highest number of deaths ever recorded in a year.11 Despite this, most healthcare systems remain unequipped to provide addiction services during hospitalization due to inadequate training, stigma, and lack of systems-based care.
Hospitalists and healthcare systems cannot be bystanders amid our worsening addiction crisis. We must empower clinicians with addiction education and ensure health systems offer evidence-based SUD services.
Educational efforts can close the knowledge gaps for both medical students and hospitalists. Medical schools should include foundational curricular content in screening, assessing, diagnosing, and treating SUD in alignment with standards set by the Liaison Committee on Medical Education, which accredits US medical schools. Residency programs can offer educational conferences, cased-based discussions, and addiction medicine rotations. Hospitalists can participate in educational didactics and review evidence-based addiction guidelines.12,13 While the focus here is on hospitalists, clinicians across practice settings and specialties will encounter patients with SUD, and all need to be well-versed in the diagnosis and treatment of addiction given the all-hands-on deck approach necessary amidst our worsening addiction crisis.
With one in nine hospitalizations involving individuals with SUD, and this number quickly rising, and with an annual cost to US hospitals of $13.2 billion, healthcare system leaders must invest in addiction care.14,15 Hospital-based addiction services could pay for themselves and save healthcare systems money while improving the patient and clinician experience.16One way to implement hospital-based addiction care is through an addiction consult team (ACT).17 While ACT compositions vary, most are interprofessional, offer evidence-based addiction treatment, and connect patients to community care.18 Our hospital’s ACT has nurses, patient navigators, and physicians who assess, diagnose, and treat SUD, and arrange follow-up addiction care.19 In addition to caring for individual patients, our ACT has led systems change. For example, we created order sets to guide clinicians, added medications to our hospital formulary to ensure access to evidence-based addiction treatment, and partnered with community stakeholders to streamline care transitions and access to psychosocial and medication treatment. Our team also worked with hospital leadership, nursing, and a syringe service program to integrate hospital harm reduction education and supply provision. Additionally, we are building capacity among staff, trainees, and clinicians through education and systems changes.
In hospitals without an ACT, leadership can finance SUD champions and integrate them into policy-level decision-making to implement best practices in addiction care and lead hospital-wide educational efforts. This will transform hospital culture and improve care as all clinicians develop essential addiction skills.
Addiction champions and ACTs could also advocate for equitable practices for patients with SUD to reduce the stigma that both prevents patients from seeking care and results in self-discharges.20 For example, with interprofessional support, we revised our in-hospital substance use policy. It previously entailed hospital security responding to substance use concerns, which unintentionally harmed patients and perpetuated stigma. Our revised policy ensures we offer medications for cravings and withdrawal, adequate pain management, and other services that address patients’ reasons for in-hospital substance use.
With the increasing prevalence of SUD among hospitalized patients, escalating substance-related deaths, rising healthcare costs, and the impact of addiction on health and well-being, addiction care, including ACTs and champions, must be adequately funded. However, sustainable financing remains a challenge.18
Caring for Rosa and others with SUD sparked my desire to learn about addiction, obtain addiction medicine board certification as a practicing hospitalist, and create an ACT that offers evidence-based addiction treatment. While much remains to be done, by collaborating with addiction champions and engaging hospital leadership, we have transformed our hospital’s approach to substance use care.
With the knowledge and resources I now have as an addiction medicine physician, I reimagine the possibilities for patients like Rosa.
Rosa died when living was possible.
*Name has been changed for patient privacy.
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. HHS Publication No. PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Accessed December 1, 2021. www.samhsa.gov/data/
2. Centers for Disease Control and Prevention. Alcohol and public health: alcohol-related disease impact (ARDI) application, 2013. Average for United States 2006–2010 alcohol-attributable deaths due to excessive alcohol use. Accessed December 1, 2021. www.cdc.gov/ARDI
3. Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Netw Open. 2020;3(2):e1921451. https://doi.org/ 10.1001/jamanetworkopen.2019.21451
4. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161 https://doi.org/10.1001/jamapsychiatry.2017.2161
5. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the covid-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. https://doi.org/10.1001/jamanetworkopen.2020.22942
6. Bangaru S, Pedersen MR, Macconmara MP, Singal AG, Mufti AR. Survey of liver transplantation practices for severe acute alcoholic hepatitis. Liver Transpl. 2018;24(10):1357-1362. https://doi.org/10.1002/lt.25285
7. Herrick-Reynolds KM, Punchhi G, Greenberg RS, et al. Evaluation of early vs standard liver transplant for alcohol-associated liver disease. JAMA Surg. 2021;156(11):1026-1034. https://doi.org/10.1001/jamasurg.2021.3748
8. Fleming JN, Lai JC, Te HS, Said A, Spengler EK, Rogal SS. Opioid and opioid substitution therapy in liver transplant candidates: A survey of center policies and practices. Clin Transplant. 2017;31(12):e13119. https://doi.org/10.1111/ctr.13119
9. Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev. 2018;12(12):CD009269. https://doi.org/10.1002/14651858.CD009269.pub4
10. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. https://doi.org/10.15585/mmwr.mm7006a4
11. Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. Accessed November 18, 2021. www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
12. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
13. California Bridge Program. Tools: Treat substance use disorders from the acute care setting. Accessed August 20, 2021. https://cabridge.org/tools
14. Peterson C, Li M, Xu L, Mikosz CA, Luo F. Assessment of annual cost of substance use disorder in US hospitals. JAMA Netw Open. 2021;4(3):e210242. https://doi.org/10.1001/jamanetworkopen.2021.0242
15. Suen LW, Makam AN, Snyder HR, et al. National prevalence of alcohol and other substance use disorders among emergency department visits and hospitalizations: NHAMCS 2014-2018. J Gen Intern Med. 2021;13:1-9. https://doi.org/10.1007/s11606-021-07069-w
16. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: Qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993
17. Priest KC, McCarty D. Making the business case for an addiction medicine consult service: a qualitative analysis. BMC Health Services Research. 2019;19(1):822. https://doi.org/10.1186/s12913-019-4670-4
18. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496
19. Martin M, Snyder HR, Coffa D, et al. Time to ACT: launching an Addiction Care Team (ACT) in an urban safety-net health system. BMJ Open Qual. 2021;10(1):e001111. https://doi.org/10.1136/bmjoq-2020-001111
20. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abus. 2020;41(4):519-525. https://doi.org/10.1080/08897077.2019.1671942
Rosa* was one of my first patients as an intern rotating at the county hospital. Her marriage had disintegrated years earlier. To cope with depression, she hid a daily ritual of orange juice and vodka from her children. She worked as a cashier, until nausea and fatigue overwhelmed her.
The first time I met her she sat on the gurney: petite, tanned, and pregnant. Then I saw her yellow eyes and revised: temporal wasting, jaundiced, and swollen with ascites. Rosa didn’t know that alcohol could cause liver disease. Without insurance or access to primary care, her untreated alcohol use disorder (AUD) and depression had snowballed for years.
Midway through my intern year, I’d taken care of many people with AUD. However, I’d barely learned anything about it as a medical student, though we’d spent weeks studying esoteric diseases, that now––9 years after medical school––I still have not encountered.
Among the 28.3 million individuals in the United States with AUD, only 1% receive medication treatment.1 In the United States, unhealthy alcohol use accounts for more than 95,000 deaths each year.2 This number likely under-captures alcohol-related mortality and is higher now given recent reports of increasing alcohol-related deaths and prevalence of unhealthy alcohol use, especially among women, younger age groups, and marginalized populations.3-5
Rosa had alcohol-related hepatitis, which can cause severe inflammation and liver failure and quickly lead to death. As her liver failure progressed, I asked the gastroenterologists, “What other treatments can we offer? Is she a liver transplant candidate?” “Nothing” and “No” they answered.
Later, I emailed the hepatologist and transplant surgeon begging them to reevaluate her transplantation candidacy, but they told me there was no exception to the institution’s 6-month sobriety rule.
Maintaining a 6-month sobriety period is not an evidence-based criterion for transplantation. However, 50% of transplant centers do not perform transplantation prior to 6 months of alcohol abstinence for alcohol-related hepatitis due to concern for return to drinking after transplant.6 This practice may promote bias in patient selection for transplantation. A recent study found that individuals with alcohol-related liver disease transplanted before 6 months of abstinence had similar rates of survival and return to drinking compared to those who abstained from alcohol for 6 months and participated in AUD treatment before transplantation.7
There are other liver transplant practices that result in inequities for individuals with substance use disorders (SUD). Some liver transplant centers consider being on a medication for opioid use disorder a contraindication for transplantation—even if the individual is in recovery and abstaining from substances.8 Others mandate that individuals with alcohol-related liver disease attend Alcoholics Anonymous (AA) meetings prior to transplant. While mutual help groups, including AA, may benefit some individuals, different approaches work for different people.9 Other psychosocial interventions (eg, cognitive-behavioral therapy, contingency management, and residential treatment) and medications also help individuals reduce or stop drinking. Some meet their goals without any treatment. Addiction care works best when it respects autonomy and meets individuals where they are by allowing them to decide among options.
While organ allocations are a crystalized example of inequities in addiction care, they are also ethically complex. Many individuals—with and without SUD—die on waiting lists and must meet stringent transplantation criteria. However, we can at least remove the unnecessary biases that compound inequities in care people with SUD already face.
As Rosa’s liver succumbed, her kidneys failed too, and she required dialysis. She sensed what was coming. “I want everything…for now. I need to take care of my children.” I, too, wanted Rosa to live and see her youngest start kindergarten.
A few days before her discharge, I walked to the pharmacy and bought a purple journal. In a rare moment, I found Rosa alone in her room, without her ex-husband, sister, and mother, who rarely left her bedside. Together, we called AA and explored whether she could start participating in phone meetings from the hospital. I explained that one way to document a commitment to sobriety, as the transplant center’s rules dictated, was to attend and document AA meetings in this notebook. “In 5 months, you will be a liver transplant candidate,” I remember saying, wishing it to fruition.
I became Rosa’s primary care physician and saw her in clinic. Over the next few weeks, her skin took on an ashen tone. Sleep escaped her and her thoughts and speech blurred. Her walk slowed and she needed a wheelchair. The quiet fierceness that had defined her dissipated as encephalopathy took over. But until our last visit, she brought her purple journal, tracking the AA meetings she’d attended. Dialysis became intolerable, but not before Rosa made care arrangements for her girls. When that happened, she stopped dialysis and went to Mexico, where she died in her sleep after saying good-bye to her father.
Earlier access to healthcare and effective depression and AUD treatment could have saved Rosa’s life. While it was too late for her, as hospitalists we care for many others with substance-related complications and may miss opportunities to discuss and offer evidence-based addiction treatment. For example, we initiate the most up-to-date management for a patient’s gastrointestinal bleed but may leave the alcohol discussion for someone else. It is similar for other SUD: we treat cellulitis, epidural abscesses, bacteremia, chronic obstructive pulmonary disease, heart failure exacerbations, and other complications of SUD without addressing the root cause of the hospitalization—other than to prescribe abstinence from substance use or, at our worst, scold individuals for continuing to use.
But what can we offer? Most healthcare professionals still do not receive addiction education during training. Without tools, we enact temporizing measures, until patients return to the hospital or die.
In addition to increasing alcohol-related morbidity, there have also been increases in drug-related overdoses, fueled by COVID-19, synthetic opioids like fentanyl, and stimulants.10 In the 12-month period ending April 2021, more than 100,000 individuals died of drug-related overdoses, the highest number of deaths ever recorded in a year.11 Despite this, most healthcare systems remain unequipped to provide addiction services during hospitalization due to inadequate training, stigma, and lack of systems-based care.
Hospitalists and healthcare systems cannot be bystanders amid our worsening addiction crisis. We must empower clinicians with addiction education and ensure health systems offer evidence-based SUD services.
Educational efforts can close the knowledge gaps for both medical students and hospitalists. Medical schools should include foundational curricular content in screening, assessing, diagnosing, and treating SUD in alignment with standards set by the Liaison Committee on Medical Education, which accredits US medical schools. Residency programs can offer educational conferences, cased-based discussions, and addiction medicine rotations. Hospitalists can participate in educational didactics and review evidence-based addiction guidelines.12,13 While the focus here is on hospitalists, clinicians across practice settings and specialties will encounter patients with SUD, and all need to be well-versed in the diagnosis and treatment of addiction given the all-hands-on deck approach necessary amidst our worsening addiction crisis.
With one in nine hospitalizations involving individuals with SUD, and this number quickly rising, and with an annual cost to US hospitals of $13.2 billion, healthcare system leaders must invest in addiction care.14,15 Hospital-based addiction services could pay for themselves and save healthcare systems money while improving the patient and clinician experience.16One way to implement hospital-based addiction care is through an addiction consult team (ACT).17 While ACT compositions vary, most are interprofessional, offer evidence-based addiction treatment, and connect patients to community care.18 Our hospital’s ACT has nurses, patient navigators, and physicians who assess, diagnose, and treat SUD, and arrange follow-up addiction care.19 In addition to caring for individual patients, our ACT has led systems change. For example, we created order sets to guide clinicians, added medications to our hospital formulary to ensure access to evidence-based addiction treatment, and partnered with community stakeholders to streamline care transitions and access to psychosocial and medication treatment. Our team also worked with hospital leadership, nursing, and a syringe service program to integrate hospital harm reduction education and supply provision. Additionally, we are building capacity among staff, trainees, and clinicians through education and systems changes.
In hospitals without an ACT, leadership can finance SUD champions and integrate them into policy-level decision-making to implement best practices in addiction care and lead hospital-wide educational efforts. This will transform hospital culture and improve care as all clinicians develop essential addiction skills.
Addiction champions and ACTs could also advocate for equitable practices for patients with SUD to reduce the stigma that both prevents patients from seeking care and results in self-discharges.20 For example, with interprofessional support, we revised our in-hospital substance use policy. It previously entailed hospital security responding to substance use concerns, which unintentionally harmed patients and perpetuated stigma. Our revised policy ensures we offer medications for cravings and withdrawal, adequate pain management, and other services that address patients’ reasons for in-hospital substance use.
With the increasing prevalence of SUD among hospitalized patients, escalating substance-related deaths, rising healthcare costs, and the impact of addiction on health and well-being, addiction care, including ACTs and champions, must be adequately funded. However, sustainable financing remains a challenge.18
Caring for Rosa and others with SUD sparked my desire to learn about addiction, obtain addiction medicine board certification as a practicing hospitalist, and create an ACT that offers evidence-based addiction treatment. While much remains to be done, by collaborating with addiction champions and engaging hospital leadership, we have transformed our hospital’s approach to substance use care.
With the knowledge and resources I now have as an addiction medicine physician, I reimagine the possibilities for patients like Rosa.
Rosa died when living was possible.
*Name has been changed for patient privacy.
Rosa* was one of my first patients as an intern rotating at the county hospital. Her marriage had disintegrated years earlier. To cope with depression, she hid a daily ritual of orange juice and vodka from her children. She worked as a cashier, until nausea and fatigue overwhelmed her.
The first time I met her she sat on the gurney: petite, tanned, and pregnant. Then I saw her yellow eyes and revised: temporal wasting, jaundiced, and swollen with ascites. Rosa didn’t know that alcohol could cause liver disease. Without insurance or access to primary care, her untreated alcohol use disorder (AUD) and depression had snowballed for years.
Midway through my intern year, I’d taken care of many people with AUD. However, I’d barely learned anything about it as a medical student, though we’d spent weeks studying esoteric diseases, that now––9 years after medical school––I still have not encountered.
Among the 28.3 million individuals in the United States with AUD, only 1% receive medication treatment.1 In the United States, unhealthy alcohol use accounts for more than 95,000 deaths each year.2 This number likely under-captures alcohol-related mortality and is higher now given recent reports of increasing alcohol-related deaths and prevalence of unhealthy alcohol use, especially among women, younger age groups, and marginalized populations.3-5
Rosa had alcohol-related hepatitis, which can cause severe inflammation and liver failure and quickly lead to death. As her liver failure progressed, I asked the gastroenterologists, “What other treatments can we offer? Is she a liver transplant candidate?” “Nothing” and “No” they answered.
Later, I emailed the hepatologist and transplant surgeon begging them to reevaluate her transplantation candidacy, but they told me there was no exception to the institution’s 6-month sobriety rule.
Maintaining a 6-month sobriety period is not an evidence-based criterion for transplantation. However, 50% of transplant centers do not perform transplantation prior to 6 months of alcohol abstinence for alcohol-related hepatitis due to concern for return to drinking after transplant.6 This practice may promote bias in patient selection for transplantation. A recent study found that individuals with alcohol-related liver disease transplanted before 6 months of abstinence had similar rates of survival and return to drinking compared to those who abstained from alcohol for 6 months and participated in AUD treatment before transplantation.7
There are other liver transplant practices that result in inequities for individuals with substance use disorders (SUD). Some liver transplant centers consider being on a medication for opioid use disorder a contraindication for transplantation—even if the individual is in recovery and abstaining from substances.8 Others mandate that individuals with alcohol-related liver disease attend Alcoholics Anonymous (AA) meetings prior to transplant. While mutual help groups, including AA, may benefit some individuals, different approaches work for different people.9 Other psychosocial interventions (eg, cognitive-behavioral therapy, contingency management, and residential treatment) and medications also help individuals reduce or stop drinking. Some meet their goals without any treatment. Addiction care works best when it respects autonomy and meets individuals where they are by allowing them to decide among options.
While organ allocations are a crystalized example of inequities in addiction care, they are also ethically complex. Many individuals—with and without SUD—die on waiting lists and must meet stringent transplantation criteria. However, we can at least remove the unnecessary biases that compound inequities in care people with SUD already face.
As Rosa’s liver succumbed, her kidneys failed too, and she required dialysis. She sensed what was coming. “I want everything…for now. I need to take care of my children.” I, too, wanted Rosa to live and see her youngest start kindergarten.
A few days before her discharge, I walked to the pharmacy and bought a purple journal. In a rare moment, I found Rosa alone in her room, without her ex-husband, sister, and mother, who rarely left her bedside. Together, we called AA and explored whether she could start participating in phone meetings from the hospital. I explained that one way to document a commitment to sobriety, as the transplant center’s rules dictated, was to attend and document AA meetings in this notebook. “In 5 months, you will be a liver transplant candidate,” I remember saying, wishing it to fruition.
I became Rosa’s primary care physician and saw her in clinic. Over the next few weeks, her skin took on an ashen tone. Sleep escaped her and her thoughts and speech blurred. Her walk slowed and she needed a wheelchair. The quiet fierceness that had defined her dissipated as encephalopathy took over. But until our last visit, she brought her purple journal, tracking the AA meetings she’d attended. Dialysis became intolerable, but not before Rosa made care arrangements for her girls. When that happened, she stopped dialysis and went to Mexico, where she died in her sleep after saying good-bye to her father.
Earlier access to healthcare and effective depression and AUD treatment could have saved Rosa’s life. While it was too late for her, as hospitalists we care for many others with substance-related complications and may miss opportunities to discuss and offer evidence-based addiction treatment. For example, we initiate the most up-to-date management for a patient’s gastrointestinal bleed but may leave the alcohol discussion for someone else. It is similar for other SUD: we treat cellulitis, epidural abscesses, bacteremia, chronic obstructive pulmonary disease, heart failure exacerbations, and other complications of SUD without addressing the root cause of the hospitalization—other than to prescribe abstinence from substance use or, at our worst, scold individuals for continuing to use.
But what can we offer? Most healthcare professionals still do not receive addiction education during training. Without tools, we enact temporizing measures, until patients return to the hospital or die.
In addition to increasing alcohol-related morbidity, there have also been increases in drug-related overdoses, fueled by COVID-19, synthetic opioids like fentanyl, and stimulants.10 In the 12-month period ending April 2021, more than 100,000 individuals died of drug-related overdoses, the highest number of deaths ever recorded in a year.11 Despite this, most healthcare systems remain unequipped to provide addiction services during hospitalization due to inadequate training, stigma, and lack of systems-based care.
Hospitalists and healthcare systems cannot be bystanders amid our worsening addiction crisis. We must empower clinicians with addiction education and ensure health systems offer evidence-based SUD services.
Educational efforts can close the knowledge gaps for both medical students and hospitalists. Medical schools should include foundational curricular content in screening, assessing, diagnosing, and treating SUD in alignment with standards set by the Liaison Committee on Medical Education, which accredits US medical schools. Residency programs can offer educational conferences, cased-based discussions, and addiction medicine rotations. Hospitalists can participate in educational didactics and review evidence-based addiction guidelines.12,13 While the focus here is on hospitalists, clinicians across practice settings and specialties will encounter patients with SUD, and all need to be well-versed in the diagnosis and treatment of addiction given the all-hands-on deck approach necessary amidst our worsening addiction crisis.
With one in nine hospitalizations involving individuals with SUD, and this number quickly rising, and with an annual cost to US hospitals of $13.2 billion, healthcare system leaders must invest in addiction care.14,15 Hospital-based addiction services could pay for themselves and save healthcare systems money while improving the patient and clinician experience.16One way to implement hospital-based addiction care is through an addiction consult team (ACT).17 While ACT compositions vary, most are interprofessional, offer evidence-based addiction treatment, and connect patients to community care.18 Our hospital’s ACT has nurses, patient navigators, and physicians who assess, diagnose, and treat SUD, and arrange follow-up addiction care.19 In addition to caring for individual patients, our ACT has led systems change. For example, we created order sets to guide clinicians, added medications to our hospital formulary to ensure access to evidence-based addiction treatment, and partnered with community stakeholders to streamline care transitions and access to psychosocial and medication treatment. Our team also worked with hospital leadership, nursing, and a syringe service program to integrate hospital harm reduction education and supply provision. Additionally, we are building capacity among staff, trainees, and clinicians through education and systems changes.
In hospitals without an ACT, leadership can finance SUD champions and integrate them into policy-level decision-making to implement best practices in addiction care and lead hospital-wide educational efforts. This will transform hospital culture and improve care as all clinicians develop essential addiction skills.
Addiction champions and ACTs could also advocate for equitable practices for patients with SUD to reduce the stigma that both prevents patients from seeking care and results in self-discharges.20 For example, with interprofessional support, we revised our in-hospital substance use policy. It previously entailed hospital security responding to substance use concerns, which unintentionally harmed patients and perpetuated stigma. Our revised policy ensures we offer medications for cravings and withdrawal, adequate pain management, and other services that address patients’ reasons for in-hospital substance use.
With the increasing prevalence of SUD among hospitalized patients, escalating substance-related deaths, rising healthcare costs, and the impact of addiction on health and well-being, addiction care, including ACTs and champions, must be adequately funded. However, sustainable financing remains a challenge.18
Caring for Rosa and others with SUD sparked my desire to learn about addiction, obtain addiction medicine board certification as a practicing hospitalist, and create an ACT that offers evidence-based addiction treatment. While much remains to be done, by collaborating with addiction champions and engaging hospital leadership, we have transformed our hospital’s approach to substance use care.
With the knowledge and resources I now have as an addiction medicine physician, I reimagine the possibilities for patients like Rosa.
Rosa died when living was possible.
*Name has been changed for patient privacy.
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. HHS Publication No. PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Accessed December 1, 2021. www.samhsa.gov/data/
2. Centers for Disease Control and Prevention. Alcohol and public health: alcohol-related disease impact (ARDI) application, 2013. Average for United States 2006–2010 alcohol-attributable deaths due to excessive alcohol use. Accessed December 1, 2021. www.cdc.gov/ARDI
3. Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Netw Open. 2020;3(2):e1921451. https://doi.org/ 10.1001/jamanetworkopen.2019.21451
4. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161 https://doi.org/10.1001/jamapsychiatry.2017.2161
5. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the covid-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. https://doi.org/10.1001/jamanetworkopen.2020.22942
6. Bangaru S, Pedersen MR, Macconmara MP, Singal AG, Mufti AR. Survey of liver transplantation practices for severe acute alcoholic hepatitis. Liver Transpl. 2018;24(10):1357-1362. https://doi.org/10.1002/lt.25285
7. Herrick-Reynolds KM, Punchhi G, Greenberg RS, et al. Evaluation of early vs standard liver transplant for alcohol-associated liver disease. JAMA Surg. 2021;156(11):1026-1034. https://doi.org/10.1001/jamasurg.2021.3748
8. Fleming JN, Lai JC, Te HS, Said A, Spengler EK, Rogal SS. Opioid and opioid substitution therapy in liver transplant candidates: A survey of center policies and practices. Clin Transplant. 2017;31(12):e13119. https://doi.org/10.1111/ctr.13119
9. Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev. 2018;12(12):CD009269. https://doi.org/10.1002/14651858.CD009269.pub4
10. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. https://doi.org/10.15585/mmwr.mm7006a4
11. Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. Accessed November 18, 2021. www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
12. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
13. California Bridge Program. Tools: Treat substance use disorders from the acute care setting. Accessed August 20, 2021. https://cabridge.org/tools
14. Peterson C, Li M, Xu L, Mikosz CA, Luo F. Assessment of annual cost of substance use disorder in US hospitals. JAMA Netw Open. 2021;4(3):e210242. https://doi.org/10.1001/jamanetworkopen.2021.0242
15. Suen LW, Makam AN, Snyder HR, et al. National prevalence of alcohol and other substance use disorders among emergency department visits and hospitalizations: NHAMCS 2014-2018. J Gen Intern Med. 2021;13:1-9. https://doi.org/10.1007/s11606-021-07069-w
16. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: Qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993
17. Priest KC, McCarty D. Making the business case for an addiction medicine consult service: a qualitative analysis. BMC Health Services Research. 2019;19(1):822. https://doi.org/10.1186/s12913-019-4670-4
18. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496
19. Martin M, Snyder HR, Coffa D, et al. Time to ACT: launching an Addiction Care Team (ACT) in an urban safety-net health system. BMJ Open Qual. 2021;10(1):e001111. https://doi.org/10.1136/bmjoq-2020-001111
20. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abus. 2020;41(4):519-525. https://doi.org/10.1080/08897077.2019.1671942
1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. HHS Publication No. PEP21-07-01-003, NSDUH Series H-56. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Accessed December 1, 2021. www.samhsa.gov/data/
2. Centers for Disease Control and Prevention. Alcohol and public health: alcohol-related disease impact (ARDI) application, 2013. Average for United States 2006–2010 alcohol-attributable deaths due to excessive alcohol use. Accessed December 1, 2021. www.cdc.gov/ARDI
3. Spillane S, Shiels MS, Best AF, et al. Trends in alcohol-induced deaths in the United States, 2000-2016. JAMA Netw Open. 2020;3(2):e1921451. https://doi.org/ 10.1001/jamanetworkopen.2019.21451
4. Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161 https://doi.org/10.1001/jamapsychiatry.2017.2161
5. Pollard MS, Tucker JS, Green HD Jr. Changes in adult alcohol use and consequences during the covid-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. https://doi.org/10.1001/jamanetworkopen.2020.22942
6. Bangaru S, Pedersen MR, Macconmara MP, Singal AG, Mufti AR. Survey of liver transplantation practices for severe acute alcoholic hepatitis. Liver Transpl. 2018;24(10):1357-1362. https://doi.org/10.1002/lt.25285
7. Herrick-Reynolds KM, Punchhi G, Greenberg RS, et al. Evaluation of early vs standard liver transplant for alcohol-associated liver disease. JAMA Surg. 2021;156(11):1026-1034. https://doi.org/10.1001/jamasurg.2021.3748
8. Fleming JN, Lai JC, Te HS, Said A, Spengler EK, Rogal SS. Opioid and opioid substitution therapy in liver transplant candidates: A survey of center policies and practices. Clin Transplant. 2017;31(12):e13119. https://doi.org/10.1111/ctr.13119
9. Klimas J, Fairgrieve C, Tobin H, et al. Psychosocial interventions to reduce alcohol consumption in concurrent problem alcohol and illicit drug users. Cochrane Database Syst Rev. 2018;12(12):CD009269. https://doi.org/10.1002/14651858.CD009269.pub4
10. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70:202–207. https://doi.org/10.15585/mmwr.mm7006a4
11. Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. Accessed November 18, 2021. www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
12. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
13. California Bridge Program. Tools: Treat substance use disorders from the acute care setting. Accessed August 20, 2021. https://cabridge.org/tools
14. Peterson C, Li M, Xu L, Mikosz CA, Luo F. Assessment of annual cost of substance use disorder in US hospitals. JAMA Netw Open. 2021;4(3):e210242. https://doi.org/10.1001/jamanetworkopen.2021.0242
15. Suen LW, Makam AN, Snyder HR, et al. National prevalence of alcohol and other substance use disorders among emergency department visits and hospitalizations: NHAMCS 2014-2018. J Gen Intern Med. 2021;13:1-9. https://doi.org/10.1007/s11606-021-07069-w
16. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: Qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993
17. Priest KC, McCarty D. Making the business case for an addiction medicine consult service: a qualitative analysis. BMC Health Services Research. 2019;19(1):822. https://doi.org/10.1186/s12913-019-4670-4
18. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496
19. Martin M, Snyder HR, Coffa D, et al. Time to ACT: launching an Addiction Care Team (ACT) in an urban safety-net health system. BMJ Open Qual. 2021;10(1):e001111. https://doi.org/10.1136/bmjoq-2020-001111
20. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abus. 2020;41(4):519-525. https://doi.org/10.1080/08897077.2019.1671942
© 2021 Society of Hospital Medicine
Things We Do for No Reason™: Prescribing Thiamine, Folate and Multivitamins on Discharge for Patients With Alcohol Use Disorder
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 56-year-old man with alcohol use disorder (AUD) is admitted with decompensated heart failure and experiences alcohol withdrawal during the hospitalization. He improves with guideline-directed heart failure therapy and benzodiazepines for alcohol withdrawal. Discharge medications are metoprolol succinate, lisinopril, furosemide, aspirin, atorvastatin, thiamine, folic acid, and a multivitamin. No medications are offered for AUD treatment. At follow-up a week later, he presents with dyspnea and reports poor medication adherence and a return to heavy drinking.
WHY YOU MIGHT THINK IT IS HELPFUL TO PRESCRIBE VITAMIN SUPPLEMENTATION TO PATIENTS WITH AUD AT HOSPITAL DISCHARGE
AUD is common among hospitalized patients.1 AUD increases the risk of vitamin deficiencies due to the toxic effects of alcohol on the gastrointestinal tract and liver, causing impaired digestion, reduced absorption, and increased degradation of key micronutrients.2,3 Other risk factors for AUD-associated vitamin deficiencies include food insecurity and the replacement of nutrient-rich food with alcohol. Since the body does not readily store water-soluble vitamins, including thiamine (vitamin B1) and folate (vitamin B9), people require regular dietary replenishment of these nutrients. Thus, if individuals with AUD eat less fortified food, they risk developing thiamine, folate, niacin, and other vitamin deficiencies. Since AUD puts patients at risk for vitamin deficiencies, hospitalized patients typically receive vitamin supplementation, including thiamine, folic acid, and a multivitamin (most formulations contain water-soluble vitamins B and C and micronutrients).1 Hospitalists often continue these medications at discharge.
Thiamine deficiency may manifest as Wernicke encephalopathy (WE), peripheral neuropathy, or a high-output heart failure state.
Hospitalists empirically treat with thiamine, folate, and other vitamins upon hospital admission with the intent of reducing morbidity associated with nutritional deficiencies.1 Repletion poses few risks to patients since the kidneys eliminate water-soluble vitamins. Multivitamins also have a low potential for direct harm and a low cost. Given the consequences of missing a deficiency, alcohol withdrawal–management order sets commonly embed vitamin repletion orders.6
WHY ROUTINELY PRESCRIBING VITAMIN SUPPLEMENTATION AT HOSPITAL DISCHARGE IN PATIENTS WITH AUD IS A TWDFNR
Hospitalists often reflexively continue vitamin supplementation on discharge. Unfortunately, there is no evidence that prescribing vitamin supplementation leads to clinically significant improvements for people with AUD, and patients can experience harms.
Literature and specialty guidelines lack consensus on rational vitamin supplementation in patients with AUD.2,7,8 Folate testing is not recommended due to inaccuracies.9 In fact, clinical data, such as body mass index, more accurately predict alcohol-related cognitive impairment than blood levels of vitamins.10 In one small study of vitamin deficiencies among patients with acute alcohol intoxication, none had low B12 or folate levels.11 A systematic review among people experiencing homelessness with unhealthy alcohol use showed no clear pattern of vitamin deficiencies across studies, although vitamin C and thiamine deficiencies predominated.12
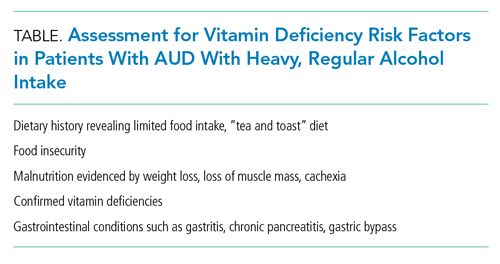
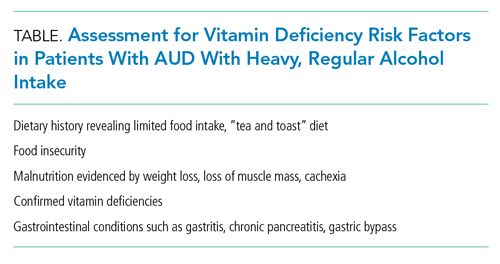
In the absence of reliable thiamine and folate testing to confirm deficiencies, clinicians must use their clinical assessment skills. Clinicians rarely evaluate patients with AUD for vitamin deficiency risk factors and instead reflexively prescribe vitamin supplementation. An AUD diagnosis may serve as a sensitive, but not specific, risk factor for those in need of vitamin supplementation.
Other limitations make prescribing oral vitamins reflexively at discharge a low-value practice. Thiamine, often prescribed orally in the hospital and on discharge, has poor oral bioavailability.13 Unfortunately, people with AUD have decreased and variable thiamine absorption. To prevent WE, thiamine must cross the blood-brain barrier, and the literature provides insufficient evidence to guide clinicians on an appropriate oral thiamine dose, frequency, or duration of treatment.14 While early high-dose IV thiamine may treat or prevent WE during hospitalization, low-dose oral thiamine may not provide benefit to patients with AUD.5
The literature also provides sparse evidence for folate supplementation and its optimal dose. Since 1998, when the United States mandated fortifying grain products with folic acid, people rarely have low serum folate levels. Though patients with AUD have lower folate levels relative to the general population,15 this difference does not seem clinically significant. While limited data show an association between oral multivitamin supplementation and improved serum nutrient levels among people with AUD, we lack evidence on clinical outcomes.16
Most importantly, for a practice lacking strong evidence, prescribing multiple vitamins at discharge may result in harm from polypharmacy and unnecessary costs for the recently hospitalized patient. Alcohol use is associated with decreased adherence to medications for chronic conditions,17 including HIV, hypertension, hyperlipidemia, and psychiatric diseases. In addition, research shows an association between an increased number of discharge medications and higher risk for hospital readmission. The harm may actually correlate with the number of medications and complexity of the regimen rather than the risk profile of the medications themselves.18 Providers underestimate the impact of adding multiple vitamins at discharge, especially for patients who have several co-occurring medical conditions that require other medications. Furthermore, insurance rarely covers vitamins, leading hospitals or patients to incur the costs at discharge.
WHEN TO CONSIDER VITAMIN SUPPLEMENTATION AT DISCHARGE FOR PATIENTS WITH AUD
When treating patients with AUD, consider the potential benefit of vitamin supplementation for the individual. If a patient with regular, heavy alcohol use is at high risk of vitamin deficiencies due to ongoing risk factors (Table), hospitalists should discuss vitamin therapy via a patient-centered risk-benefit process.
When considering discharge vitamins, make concurrent efforts to enhance patient nutrition via decreased alcohol consumption and improved healthy food intake. While some patients do not have a goal of abstaining from alcohol, providing resources to food access may help decrease the harms of drinking. Education may help patients learn that vitamin deficiencies can result from heavy alcohol use.
Multivitamin formulations have variable doses of vitamins but can contain 100% or more of the daily value of thiamine and folic acid. For patients with AUD at lower risk of vitamin deficiencies (ie, mild alcohol use disorder with a healthy diet), discuss risks and benefits of supplementation. If they desire supplementation, a single thiamine-containing vitamin alone may be highest yield since it is the most morbid vitamin deficiency. Conversely, a patient with heavy alcohol intake and other risk factors for malnutrition may benefit from a higher dose of supplementation, achieved by prescribing a multivitamin alongside additional doses of thiamine and folate. However, the literature lacks evidence to guide clinicians on optimal vitamin dosing and formulations.
WHAT WE SHOULD DO INSTEAD
Instead of reflexively prescribing thiamine, folate, and multivitamin, clinicians can assess patients for AUD, provide motivational interviewing, and offer AUD treatment. Hospitalists should initiate and prescribe evidence-based medications for AUD for patients interested in reducing or stopping their alcohol intake. We can choose from Food and Drug Administration–approved AUD medications, including naltrexone and acamprosate. Unfortunately, less than 3% of patients with AUD receive medication therapy.19 Our healthcare systems can also refer individuals to community psychosocial treatment.
For patients with risk factors, prescribe empiric IV thiamine during hospitalization. Clinicians should then perform a risk-benefit assessment rather than reflexively prescribe vitamins to patients with AUD at discharge. We should also counsel patients to eat food when drinking to decrease alcohol-related harms.20 Patients experiencing food insecurity should be linked to food resources through inpatient nutritional and social work consultations.
Elicit patient preference around vitamin supplementation after discharge. For patients with AUD who desire supplementation without risk factors for malnutrition (Table), consider prescribing a single thiamine-containing vitamin for prevention of thiamine deficiency, which, unlike other vitamin deficiencies, has the potential to be irreversible and life-threatening. Though no evidence currently supports this practice, it stands to reason that prescribing a single tablet could decrease the number of pills for patients who struggle with pill burden.
RECOMMENDATIONS
- Offer evidence-based medication treatment for AUD.
- Connect patients experiencing food insecurity with appropriate resources.
- For patients initiated on a multivitamin, folate, and high-dose IV thiamine at admission, perform vitamin de-escalation during hospitalization.
- Risk-stratify hospitalized patients with AUD for additional risk factors for vitamin deficiencies (Table). In those with additional risk factors, offer supplementation if consistent with patient preference. Balance the benefits of vitamin supplementation with the risks of polypharmacy, particularly if the patient has conditions requiring multiple medications.
CONCLUSION
Returning to our case, the hospitalist initiates IV thiamine, folate, and a multivitamin at admission and assesses the patient’s nutritional status and food insecurity. The hospitalist deems the patient—who eats regular, balanced meals—to be at low risk for vitamin deficiencies. The medical team discontinues folate and multivitamins before discharge and continues IV thiamine throughout the 3-day hospitalization. The patient and clinician agree that unaddressed AUD played a key role in the patient’s heart failure exacerbation. The clinician elicits the patient’s goals around their alcohol use, discusses AUD treatment, and initiates naltrexone for AUD.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
1. Makdissi R, Stewart SH. Care for hospitalized patients with unhealthy alcohol use: a narrative review. Addict Sci Clin Pract. 2013;8(1):11. https://doi.org/10.1186/1940-0640-8-11
2. Lewis MJ. Alcoholism and nutrition: a review of vitamin supplementation and treatment. Curr Opin Clin Nutr Metab Care. 2020;23(2):138-144. https://doi.org/10.1097/mco.0000000000000622
3. Bergmans RS, Coughlin L, Wilson T, Malecki K. Cross-sectional associations of food insecurity with smoking cigarettes and heavy alcohol use in a population-based sample of adults. Drug Alcohol Depend. 2019;205:107646. https://doi.org/10.1016/j.drugalcdep.2019.107646
4. Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014;44(9):911-915. https://doi.org/10.1111/imj.12522
5. Flannery AH, Adkins DA, Cook AM. Unpeeling the evidence for the banana bag: evidence-based recommendations for the management of alcohol-associated vitamin and electrolyte deficiencies in the ICU. Crit Care Med. 2016;44(8):1545-1552. https://doi.org/10.1097/ccm.0000000000001659
6. Wai JM, Aloezos C, Mowrey WB, Baron SW, Cregin R, Forman HL. Using clinical decision support through the electronic medical record to increase prescribing of high-dose parenteral thiamine in hospitalized patients with alcohol use disorder. J Subst Abuse Treat. 2019;99:117-123. https://doi.org/10.1016/j.jsat.2019.01.017
7. American Society of Addiction Medicine. The ASAM Clinical Practice Guideline on Alcohol Withdrawal Management. January 2020. https://www.asam.org/docs/default-source/quality-science/the_asam_clinical_practice_guideline_on_alcohol-1.pdf?sfvrsn=ba255c2_2
8. O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Hepatology. 2010;51(1):307-328. https://doi.org/10.1002/hep.23258
9. Breu AC, Theisen-Toupal J, Feldman LS. Serum and red blood cell folate testing on hospitalized patients. J Hosp Med. 2015;10(11):753-755. https://doi.org/10.1002/jhm.2385
10. Gautron M-A, Questel F, Lejoyeux M, Bellivier F, Vorspan F. Nutritional status during inpatient alcohol detoxification. Alcohol Alcohol. 2018;53(1):64-70. https://doi.org/10.1093/alcalc/agx086
11. Li SF, Jacob J, Feng J, Kulkarni M. Vitamin deficiencies in acutely intoxicated patients in the ED. Am J Emerg Med. 2008;26(7):792-795. https://doi.org/10.1016/j.ajem.2007.10.003
12. Ijaz S, Jackson J, Thorley H, et al. Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health. 2017;16(1):71. https://doi.org/10.1186/s12939-017-0564-4
13. Day GS, Ladak S, Curley K, et al. Thiamine prescribing practices within university-affiliated hospitals: a multicenter retrospective review. J Hosp Med. 2015;10(4):246-253. https://doi.org/10.1002/jhm.2324
14. Day E, Bentham PW, Callaghan R, Kuruvilla T, George S. Thiamine for prevention and treatment of Wernicke-Korsakoff syndrome in people who abuse alcohol. Cochrane Database Syst Rev. 2013;2013(7):CD004033. https://doi.org/10.1002/14651858.CD004033.pub3
15. Medici V, Halsted CH. Folate, alcohol, and liver disease. Mol Nutr Food Res. 2013;57(4):596-606. https://doi.org/10.1002/mnfr.201200077
16. Ijaz S, Thorley H, Porter K, et al. Interventions for preventing or treating malnutrition in homeless problem-drinkers: a systematic review. Int J Equity Health. 2018;17(1):8. https://doi.org/10.1186/s12939-018-0722-3
17. Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008;149(11):795-803. https://doi.org/10.7326/0003-4819-149-11-200812020-00004
18. Picker D, Heard K, Bailey TC, Martin NR, LaRossa GN, Kollef MH. The number of discharge medications predicts thirty-day hospital readmission: a cohort study. BMC Health Serv Res. 2015;15:282. https://doi.org/10.1186/s12913-015-0950-9
19. Han B, Jones CM, Einstein EB, Powell PA, Compton WM. Use of medications for alcohol use disorder in the US: results From the 2019 National Survey on Drug Use and Health. JAMA Psychiatry. 2021;78(8):922–4. https://doi.org/10.1001/jamapsychiatry.2021.1271
20. Collins SE, Duncan MH, Saxon AJ, et al. Combining behavioral harm-reduction treatment and extended-release naltrexone for people experiencing homelessness and alcohol use disorder in the USA: a randomised clinical trial. Lancet Psychiatry. 2021;8(4):287-300. https://doi.org/10.1016/S2215-0366(20)30489-2
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 56-year-old man with alcohol use disorder (AUD) is admitted with decompensated heart failure and experiences alcohol withdrawal during the hospitalization. He improves with guideline-directed heart failure therapy and benzodiazepines for alcohol withdrawal. Discharge medications are metoprolol succinate, lisinopril, furosemide, aspirin, atorvastatin, thiamine, folic acid, and a multivitamin. No medications are offered for AUD treatment. At follow-up a week later, he presents with dyspnea and reports poor medication adherence and a return to heavy drinking.
WHY YOU MIGHT THINK IT IS HELPFUL TO PRESCRIBE VITAMIN SUPPLEMENTATION TO PATIENTS WITH AUD AT HOSPITAL DISCHARGE
AUD is common among hospitalized patients.1 AUD increases the risk of vitamin deficiencies due to the toxic effects of alcohol on the gastrointestinal tract and liver, causing impaired digestion, reduced absorption, and increased degradation of key micronutrients.2,3 Other risk factors for AUD-associated vitamin deficiencies include food insecurity and the replacement of nutrient-rich food with alcohol. Since the body does not readily store water-soluble vitamins, including thiamine (vitamin B1) and folate (vitamin B9), people require regular dietary replenishment of these nutrients. Thus, if individuals with AUD eat less fortified food, they risk developing thiamine, folate, niacin, and other vitamin deficiencies. Since AUD puts patients at risk for vitamin deficiencies, hospitalized patients typically receive vitamin supplementation, including thiamine, folic acid, and a multivitamin (most formulations contain water-soluble vitamins B and C and micronutrients).1 Hospitalists often continue these medications at discharge.
Thiamine deficiency may manifest as Wernicke encephalopathy (WE), peripheral neuropathy, or a high-output heart failure state.
Hospitalists empirically treat with thiamine, folate, and other vitamins upon hospital admission with the intent of reducing morbidity associated with nutritional deficiencies.1 Repletion poses few risks to patients since the kidneys eliminate water-soluble vitamins. Multivitamins also have a low potential for direct harm and a low cost. Given the consequences of missing a deficiency, alcohol withdrawal–management order sets commonly embed vitamin repletion orders.6
WHY ROUTINELY PRESCRIBING VITAMIN SUPPLEMENTATION AT HOSPITAL DISCHARGE IN PATIENTS WITH AUD IS A TWDFNR
Hospitalists often reflexively continue vitamin supplementation on discharge. Unfortunately, there is no evidence that prescribing vitamin supplementation leads to clinically significant improvements for people with AUD, and patients can experience harms.
Literature and specialty guidelines lack consensus on rational vitamin supplementation in patients with AUD.2,7,8 Folate testing is not recommended due to inaccuracies.9 In fact, clinical data, such as body mass index, more accurately predict alcohol-related cognitive impairment than blood levels of vitamins.10 In one small study of vitamin deficiencies among patients with acute alcohol intoxication, none had low B12 or folate levels.11 A systematic review among people experiencing homelessness with unhealthy alcohol use showed no clear pattern of vitamin deficiencies across studies, although vitamin C and thiamine deficiencies predominated.12
In the absence of reliable thiamine and folate testing to confirm deficiencies, clinicians must use their clinical assessment skills. Clinicians rarely evaluate patients with AUD for vitamin deficiency risk factors and instead reflexively prescribe vitamin supplementation. An AUD diagnosis may serve as a sensitive, but not specific, risk factor for those in need of vitamin supplementation.
Other limitations make prescribing oral vitamins reflexively at discharge a low-value practice. Thiamine, often prescribed orally in the hospital and on discharge, has poor oral bioavailability.13 Unfortunately, people with AUD have decreased and variable thiamine absorption. To prevent WE, thiamine must cross the blood-brain barrier, and the literature provides insufficient evidence to guide clinicians on an appropriate oral thiamine dose, frequency, or duration of treatment.14 While early high-dose IV thiamine may treat or prevent WE during hospitalization, low-dose oral thiamine may not provide benefit to patients with AUD.5
The literature also provides sparse evidence for folate supplementation and its optimal dose. Since 1998, when the United States mandated fortifying grain products with folic acid, people rarely have low serum folate levels. Though patients with AUD have lower folate levels relative to the general population,15 this difference does not seem clinically significant. While limited data show an association between oral multivitamin supplementation and improved serum nutrient levels among people with AUD, we lack evidence on clinical outcomes.16
Most importantly, for a practice lacking strong evidence, prescribing multiple vitamins at discharge may result in harm from polypharmacy and unnecessary costs for the recently hospitalized patient. Alcohol use is associated with decreased adherence to medications for chronic conditions,17 including HIV, hypertension, hyperlipidemia, and psychiatric diseases. In addition, research shows an association between an increased number of discharge medications and higher risk for hospital readmission. The harm may actually correlate with the number of medications and complexity of the regimen rather than the risk profile of the medications themselves.18 Providers underestimate the impact of adding multiple vitamins at discharge, especially for patients who have several co-occurring medical conditions that require other medications. Furthermore, insurance rarely covers vitamins, leading hospitals or patients to incur the costs at discharge.
WHEN TO CONSIDER VITAMIN SUPPLEMENTATION AT DISCHARGE FOR PATIENTS WITH AUD
When treating patients with AUD, consider the potential benefit of vitamin supplementation for the individual. If a patient with regular, heavy alcohol use is at high risk of vitamin deficiencies due to ongoing risk factors (Table), hospitalists should discuss vitamin therapy via a patient-centered risk-benefit process.
When considering discharge vitamins, make concurrent efforts to enhance patient nutrition via decreased alcohol consumption and improved healthy food intake. While some patients do not have a goal of abstaining from alcohol, providing resources to food access may help decrease the harms of drinking. Education may help patients learn that vitamin deficiencies can result from heavy alcohol use.
Multivitamin formulations have variable doses of vitamins but can contain 100% or more of the daily value of thiamine and folic acid. For patients with AUD at lower risk of vitamin deficiencies (ie, mild alcohol use disorder with a healthy diet), discuss risks and benefits of supplementation. If they desire supplementation, a single thiamine-containing vitamin alone may be highest yield since it is the most morbid vitamin deficiency. Conversely, a patient with heavy alcohol intake and other risk factors for malnutrition may benefit from a higher dose of supplementation, achieved by prescribing a multivitamin alongside additional doses of thiamine and folate. However, the literature lacks evidence to guide clinicians on optimal vitamin dosing and formulations.
WHAT WE SHOULD DO INSTEAD
Instead of reflexively prescribing thiamine, folate, and multivitamin, clinicians can assess patients for AUD, provide motivational interviewing, and offer AUD treatment. Hospitalists should initiate and prescribe evidence-based medications for AUD for patients interested in reducing or stopping their alcohol intake. We can choose from Food and Drug Administration–approved AUD medications, including naltrexone and acamprosate. Unfortunately, less than 3% of patients with AUD receive medication therapy.19 Our healthcare systems can also refer individuals to community psychosocial treatment.
For patients with risk factors, prescribe empiric IV thiamine during hospitalization. Clinicians should then perform a risk-benefit assessment rather than reflexively prescribe vitamins to patients with AUD at discharge. We should also counsel patients to eat food when drinking to decrease alcohol-related harms.20 Patients experiencing food insecurity should be linked to food resources through inpatient nutritional and social work consultations.
Elicit patient preference around vitamin supplementation after discharge. For patients with AUD who desire supplementation without risk factors for malnutrition (Table), consider prescribing a single thiamine-containing vitamin for prevention of thiamine deficiency, which, unlike other vitamin deficiencies, has the potential to be irreversible and life-threatening. Though no evidence currently supports this practice, it stands to reason that prescribing a single tablet could decrease the number of pills for patients who struggle with pill burden.
RECOMMENDATIONS
- Offer evidence-based medication treatment for AUD.
- Connect patients experiencing food insecurity with appropriate resources.
- For patients initiated on a multivitamin, folate, and high-dose IV thiamine at admission, perform vitamin de-escalation during hospitalization.
- Risk-stratify hospitalized patients with AUD for additional risk factors for vitamin deficiencies (Table). In those with additional risk factors, offer supplementation if consistent with patient preference. Balance the benefits of vitamin supplementation with the risks of polypharmacy, particularly if the patient has conditions requiring multiple medications.
CONCLUSION
Returning to our case, the hospitalist initiates IV thiamine, folate, and a multivitamin at admission and assesses the patient’s nutritional status and food insecurity. The hospitalist deems the patient—who eats regular, balanced meals—to be at low risk for vitamin deficiencies. The medical team discontinues folate and multivitamins before discharge and continues IV thiamine throughout the 3-day hospitalization. The patient and clinician agree that unaddressed AUD played a key role in the patient’s heart failure exacerbation. The clinician elicits the patient’s goals around their alcohol use, discusses AUD treatment, and initiates naltrexone for AUD.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR series do not represent clear-cut conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 56-year-old man with alcohol use disorder (AUD) is admitted with decompensated heart failure and experiences alcohol withdrawal during the hospitalization. He improves with guideline-directed heart failure therapy and benzodiazepines for alcohol withdrawal. Discharge medications are metoprolol succinate, lisinopril, furosemide, aspirin, atorvastatin, thiamine, folic acid, and a multivitamin. No medications are offered for AUD treatment. At follow-up a week later, he presents with dyspnea and reports poor medication adherence and a return to heavy drinking.
WHY YOU MIGHT THINK IT IS HELPFUL TO PRESCRIBE VITAMIN SUPPLEMENTATION TO PATIENTS WITH AUD AT HOSPITAL DISCHARGE
AUD is common among hospitalized patients.1 AUD increases the risk of vitamin deficiencies due to the toxic effects of alcohol on the gastrointestinal tract and liver, causing impaired digestion, reduced absorption, and increased degradation of key micronutrients.2,3 Other risk factors for AUD-associated vitamin deficiencies include food insecurity and the replacement of nutrient-rich food with alcohol. Since the body does not readily store water-soluble vitamins, including thiamine (vitamin B1) and folate (vitamin B9), people require regular dietary replenishment of these nutrients. Thus, if individuals with AUD eat less fortified food, they risk developing thiamine, folate, niacin, and other vitamin deficiencies. Since AUD puts patients at risk for vitamin deficiencies, hospitalized patients typically receive vitamin supplementation, including thiamine, folic acid, and a multivitamin (most formulations contain water-soluble vitamins B and C and micronutrients).1 Hospitalists often continue these medications at discharge.
Thiamine deficiency may manifest as Wernicke encephalopathy (WE), peripheral neuropathy, or a high-output heart failure state.
Hospitalists empirically treat with thiamine, folate, and other vitamins upon hospital admission with the intent of reducing morbidity associated with nutritional deficiencies.1 Repletion poses few risks to patients since the kidneys eliminate water-soluble vitamins. Multivitamins also have a low potential for direct harm and a low cost. Given the consequences of missing a deficiency, alcohol withdrawal–management order sets commonly embed vitamin repletion orders.6
WHY ROUTINELY PRESCRIBING VITAMIN SUPPLEMENTATION AT HOSPITAL DISCHARGE IN PATIENTS WITH AUD IS A TWDFNR
Hospitalists often reflexively continue vitamin supplementation on discharge. Unfortunately, there is no evidence that prescribing vitamin supplementation leads to clinically significant improvements for people with AUD, and patients can experience harms.
Literature and specialty guidelines lack consensus on rational vitamin supplementation in patients with AUD.2,7,8 Folate testing is not recommended due to inaccuracies.9 In fact, clinical data, such as body mass index, more accurately predict alcohol-related cognitive impairment than blood levels of vitamins.10 In one small study of vitamin deficiencies among patients with acute alcohol intoxication, none had low B12 or folate levels.11 A systematic review among people experiencing homelessness with unhealthy alcohol use showed no clear pattern of vitamin deficiencies across studies, although vitamin C and thiamine deficiencies predominated.12
In the absence of reliable thiamine and folate testing to confirm deficiencies, clinicians must use their clinical assessment skills. Clinicians rarely evaluate patients with AUD for vitamin deficiency risk factors and instead reflexively prescribe vitamin supplementation. An AUD diagnosis may serve as a sensitive, but not specific, risk factor for those in need of vitamin supplementation.
Other limitations make prescribing oral vitamins reflexively at discharge a low-value practice. Thiamine, often prescribed orally in the hospital and on discharge, has poor oral bioavailability.13 Unfortunately, people with AUD have decreased and variable thiamine absorption. To prevent WE, thiamine must cross the blood-brain barrier, and the literature provides insufficient evidence to guide clinicians on an appropriate oral thiamine dose, frequency, or duration of treatment.14 While early high-dose IV thiamine may treat or prevent WE during hospitalization, low-dose oral thiamine may not provide benefit to patients with AUD.5
The literature also provides sparse evidence for folate supplementation and its optimal dose. Since 1998, when the United States mandated fortifying grain products with folic acid, people rarely have low serum folate levels. Though patients with AUD have lower folate levels relative to the general population,15 this difference does not seem clinically significant. While limited data show an association between oral multivitamin supplementation and improved serum nutrient levels among people with AUD, we lack evidence on clinical outcomes.16
Most importantly, for a practice lacking strong evidence, prescribing multiple vitamins at discharge may result in harm from polypharmacy and unnecessary costs for the recently hospitalized patient. Alcohol use is associated with decreased adherence to medications for chronic conditions,17 including HIV, hypertension, hyperlipidemia, and psychiatric diseases. In addition, research shows an association between an increased number of discharge medications and higher risk for hospital readmission. The harm may actually correlate with the number of medications and complexity of the regimen rather than the risk profile of the medications themselves.18 Providers underestimate the impact of adding multiple vitamins at discharge, especially for patients who have several co-occurring medical conditions that require other medications. Furthermore, insurance rarely covers vitamins, leading hospitals or patients to incur the costs at discharge.
WHEN TO CONSIDER VITAMIN SUPPLEMENTATION AT DISCHARGE FOR PATIENTS WITH AUD
When treating patients with AUD, consider the potential benefit of vitamin supplementation for the individual. If a patient with regular, heavy alcohol use is at high risk of vitamin deficiencies due to ongoing risk factors (Table), hospitalists should discuss vitamin therapy via a patient-centered risk-benefit process.
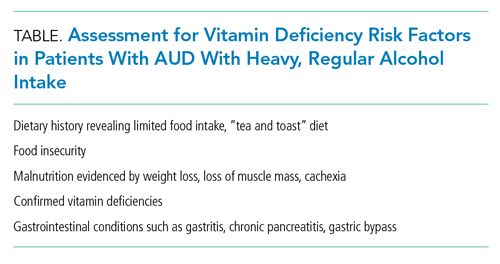
When considering discharge vitamins, make concurrent efforts to enhance patient nutrition via decreased alcohol consumption and improved healthy food intake. While some patients do not have a goal of abstaining from alcohol, providing resources to food access may help decrease the harms of drinking. Education may help patients learn that vitamin deficiencies can result from heavy alcohol use.
Multivitamin formulations have variable doses of vitamins but can contain 100% or more of the daily value of thiamine and folic acid. For patients with AUD at lower risk of vitamin deficiencies (ie, mild alcohol use disorder with a healthy diet), discuss risks and benefits of supplementation. If they desire supplementation, a single thiamine-containing vitamin alone may be highest yield since it is the most morbid vitamin deficiency. Conversely, a patient with heavy alcohol intake and other risk factors for malnutrition may benefit from a higher dose of supplementation, achieved by prescribing a multivitamin alongside additional doses of thiamine and folate. However, the literature lacks evidence to guide clinicians on optimal vitamin dosing and formulations.
WHAT WE SHOULD DO INSTEAD
Instead of reflexively prescribing thiamine, folate, and multivitamin, clinicians can assess patients for AUD, provide motivational interviewing, and offer AUD treatment. Hospitalists should initiate and prescribe evidence-based medications for AUD for patients interested in reducing or stopping their alcohol intake. We can choose from Food and Drug Administration–approved AUD medications, including naltrexone and acamprosate. Unfortunately, less than 3% of patients with AUD receive medication therapy.19 Our healthcare systems can also refer individuals to community psychosocial treatment.
For patients with risk factors, prescribe empiric IV thiamine during hospitalization. Clinicians should then perform a risk-benefit assessment rather than reflexively prescribe vitamins to patients with AUD at discharge. We should also counsel patients to eat food when drinking to decrease alcohol-related harms.20 Patients experiencing food insecurity should be linked to food resources through inpatient nutritional and social work consultations.
Elicit patient preference around vitamin supplementation after discharge. For patients with AUD who desire supplementation without risk factors for malnutrition (Table), consider prescribing a single thiamine-containing vitamin for prevention of thiamine deficiency, which, unlike other vitamin deficiencies, has the potential to be irreversible and life-threatening. Though no evidence currently supports this practice, it stands to reason that prescribing a single tablet could decrease the number of pills for patients who struggle with pill burden.
RECOMMENDATIONS
- Offer evidence-based medication treatment for AUD.
- Connect patients experiencing food insecurity with appropriate resources.
- For patients initiated on a multivitamin, folate, and high-dose IV thiamine at admission, perform vitamin de-escalation during hospitalization.
- Risk-stratify hospitalized patients with AUD for additional risk factors for vitamin deficiencies (Table). In those with additional risk factors, offer supplementation if consistent with patient preference. Balance the benefits of vitamin supplementation with the risks of polypharmacy, particularly if the patient has conditions requiring multiple medications.
CONCLUSION
Returning to our case, the hospitalist initiates IV thiamine, folate, and a multivitamin at admission and assesses the patient’s nutritional status and food insecurity. The hospitalist deems the patient—who eats regular, balanced meals—to be at low risk for vitamin deficiencies. The medical team discontinues folate and multivitamins before discharge and continues IV thiamine throughout the 3-day hospitalization. The patient and clinician agree that unaddressed AUD played a key role in the patient’s heart failure exacerbation. The clinician elicits the patient’s goals around their alcohol use, discusses AUD treatment, and initiates naltrexone for AUD.
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™”? Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
1. Makdissi R, Stewart SH. Care for hospitalized patients with unhealthy alcohol use: a narrative review. Addict Sci Clin Pract. 2013;8(1):11. https://doi.org/10.1186/1940-0640-8-11
2. Lewis MJ. Alcoholism and nutrition: a review of vitamin supplementation and treatment. Curr Opin Clin Nutr Metab Care. 2020;23(2):138-144. https://doi.org/10.1097/mco.0000000000000622
3. Bergmans RS, Coughlin L, Wilson T, Malecki K. Cross-sectional associations of food insecurity with smoking cigarettes and heavy alcohol use in a population-based sample of adults. Drug Alcohol Depend. 2019;205:107646. https://doi.org/10.1016/j.drugalcdep.2019.107646
4. Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014;44(9):911-915. https://doi.org/10.1111/imj.12522
5. Flannery AH, Adkins DA, Cook AM. Unpeeling the evidence for the banana bag: evidence-based recommendations for the management of alcohol-associated vitamin and electrolyte deficiencies in the ICU. Crit Care Med. 2016;44(8):1545-1552. https://doi.org/10.1097/ccm.0000000000001659
6. Wai JM, Aloezos C, Mowrey WB, Baron SW, Cregin R, Forman HL. Using clinical decision support through the electronic medical record to increase prescribing of high-dose parenteral thiamine in hospitalized patients with alcohol use disorder. J Subst Abuse Treat. 2019;99:117-123. https://doi.org/10.1016/j.jsat.2019.01.017
7. American Society of Addiction Medicine. The ASAM Clinical Practice Guideline on Alcohol Withdrawal Management. January 2020. https://www.asam.org/docs/default-source/quality-science/the_asam_clinical_practice_guideline_on_alcohol-1.pdf?sfvrsn=ba255c2_2
8. O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Hepatology. 2010;51(1):307-328. https://doi.org/10.1002/hep.23258
9. Breu AC, Theisen-Toupal J, Feldman LS. Serum and red blood cell folate testing on hospitalized patients. J Hosp Med. 2015;10(11):753-755. https://doi.org/10.1002/jhm.2385
10. Gautron M-A, Questel F, Lejoyeux M, Bellivier F, Vorspan F. Nutritional status during inpatient alcohol detoxification. Alcohol Alcohol. 2018;53(1):64-70. https://doi.org/10.1093/alcalc/agx086
11. Li SF, Jacob J, Feng J, Kulkarni M. Vitamin deficiencies in acutely intoxicated patients in the ED. Am J Emerg Med. 2008;26(7):792-795. https://doi.org/10.1016/j.ajem.2007.10.003
12. Ijaz S, Jackson J, Thorley H, et al. Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health. 2017;16(1):71. https://doi.org/10.1186/s12939-017-0564-4
13. Day GS, Ladak S, Curley K, et al. Thiamine prescribing practices within university-affiliated hospitals: a multicenter retrospective review. J Hosp Med. 2015;10(4):246-253. https://doi.org/10.1002/jhm.2324
14. Day E, Bentham PW, Callaghan R, Kuruvilla T, George S. Thiamine for prevention and treatment of Wernicke-Korsakoff syndrome in people who abuse alcohol. Cochrane Database Syst Rev. 2013;2013(7):CD004033. https://doi.org/10.1002/14651858.CD004033.pub3
15. Medici V, Halsted CH. Folate, alcohol, and liver disease. Mol Nutr Food Res. 2013;57(4):596-606. https://doi.org/10.1002/mnfr.201200077
16. Ijaz S, Thorley H, Porter K, et al. Interventions for preventing or treating malnutrition in homeless problem-drinkers: a systematic review. Int J Equity Health. 2018;17(1):8. https://doi.org/10.1186/s12939-018-0722-3
17. Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008;149(11):795-803. https://doi.org/10.7326/0003-4819-149-11-200812020-00004
18. Picker D, Heard K, Bailey TC, Martin NR, LaRossa GN, Kollef MH. The number of discharge medications predicts thirty-day hospital readmission: a cohort study. BMC Health Serv Res. 2015;15:282. https://doi.org/10.1186/s12913-015-0950-9
19. Han B, Jones CM, Einstein EB, Powell PA, Compton WM. Use of medications for alcohol use disorder in the US: results From the 2019 National Survey on Drug Use and Health. JAMA Psychiatry. 2021;78(8):922–4. https://doi.org/10.1001/jamapsychiatry.2021.1271
20. Collins SE, Duncan MH, Saxon AJ, et al. Combining behavioral harm-reduction treatment and extended-release naltrexone for people experiencing homelessness and alcohol use disorder in the USA: a randomised clinical trial. Lancet Psychiatry. 2021;8(4):287-300. https://doi.org/10.1016/S2215-0366(20)30489-2
1. Makdissi R, Stewart SH. Care for hospitalized patients with unhealthy alcohol use: a narrative review. Addict Sci Clin Pract. 2013;8(1):11. https://doi.org/10.1186/1940-0640-8-11
2. Lewis MJ. Alcoholism and nutrition: a review of vitamin supplementation and treatment. Curr Opin Clin Nutr Metab Care. 2020;23(2):138-144. https://doi.org/10.1097/mco.0000000000000622
3. Bergmans RS, Coughlin L, Wilson T, Malecki K. Cross-sectional associations of food insecurity with smoking cigarettes and heavy alcohol use in a population-based sample of adults. Drug Alcohol Depend. 2019;205:107646. https://doi.org/10.1016/j.drugalcdep.2019.107646
4. Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. Intern Med J. 2014;44(9):911-915. https://doi.org/10.1111/imj.12522
5. Flannery AH, Adkins DA, Cook AM. Unpeeling the evidence for the banana bag: evidence-based recommendations for the management of alcohol-associated vitamin and electrolyte deficiencies in the ICU. Crit Care Med. 2016;44(8):1545-1552. https://doi.org/10.1097/ccm.0000000000001659
6. Wai JM, Aloezos C, Mowrey WB, Baron SW, Cregin R, Forman HL. Using clinical decision support through the electronic medical record to increase prescribing of high-dose parenteral thiamine in hospitalized patients with alcohol use disorder. J Subst Abuse Treat. 2019;99:117-123. https://doi.org/10.1016/j.jsat.2019.01.017
7. American Society of Addiction Medicine. The ASAM Clinical Practice Guideline on Alcohol Withdrawal Management. January 2020. https://www.asam.org/docs/default-source/quality-science/the_asam_clinical_practice_guideline_on_alcohol-1.pdf?sfvrsn=ba255c2_2
8. O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Hepatology. 2010;51(1):307-328. https://doi.org/10.1002/hep.23258
9. Breu AC, Theisen-Toupal J, Feldman LS. Serum and red blood cell folate testing on hospitalized patients. J Hosp Med. 2015;10(11):753-755. https://doi.org/10.1002/jhm.2385
10. Gautron M-A, Questel F, Lejoyeux M, Bellivier F, Vorspan F. Nutritional status during inpatient alcohol detoxification. Alcohol Alcohol. 2018;53(1):64-70. https://doi.org/10.1093/alcalc/agx086
11. Li SF, Jacob J, Feng J, Kulkarni M. Vitamin deficiencies in acutely intoxicated patients in the ED. Am J Emerg Med. 2008;26(7):792-795. https://doi.org/10.1016/j.ajem.2007.10.003
12. Ijaz S, Jackson J, Thorley H, et al. Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health. 2017;16(1):71. https://doi.org/10.1186/s12939-017-0564-4
13. Day GS, Ladak S, Curley K, et al. Thiamine prescribing practices within university-affiliated hospitals: a multicenter retrospective review. J Hosp Med. 2015;10(4):246-253. https://doi.org/10.1002/jhm.2324
14. Day E, Bentham PW, Callaghan R, Kuruvilla T, George S. Thiamine for prevention and treatment of Wernicke-Korsakoff syndrome in people who abuse alcohol. Cochrane Database Syst Rev. 2013;2013(7):CD004033. https://doi.org/10.1002/14651858.CD004033.pub3
15. Medici V, Halsted CH. Folate, alcohol, and liver disease. Mol Nutr Food Res. 2013;57(4):596-606. https://doi.org/10.1002/mnfr.201200077
16. Ijaz S, Thorley H, Porter K, et al. Interventions for preventing or treating malnutrition in homeless problem-drinkers: a systematic review. Int J Equity Health. 2018;17(1):8. https://doi.org/10.1186/s12939-018-0722-3
17. Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008;149(11):795-803. https://doi.org/10.7326/0003-4819-149-11-200812020-00004
18. Picker D, Heard K, Bailey TC, Martin NR, LaRossa GN, Kollef MH. The number of discharge medications predicts thirty-day hospital readmission: a cohort study. BMC Health Serv Res. 2015;15:282. https://doi.org/10.1186/s12913-015-0950-9
19. Han B, Jones CM, Einstein EB, Powell PA, Compton WM. Use of medications for alcohol use disorder in the US: results From the 2019 National Survey on Drug Use and Health. JAMA Psychiatry. 2021;78(8):922–4. https://doi.org/10.1001/jamapsychiatry.2021.1271
20. Collins SE, Duncan MH, Saxon AJ, et al. Combining behavioral harm-reduction treatment and extended-release naltrexone for people experiencing homelessness and alcohol use disorder in the USA: a randomised clinical trial. Lancet Psychiatry. 2021;8(4):287-300. https://doi.org/10.1016/S2215-0366(20)30489-2
© 2021 Society of Hospital Medicine
When the X-Waiver gets X’ed: Implications for hospitalists
There are two pandemics permeating the United States: COVID-19 and addiction. To date, more than 468,000 people have died from COVID-19 in the U.S. In the 12-month period ending in May 2020, over 80,000 died from a drug related cause – the highest number ever recorded in a year. Many of these deaths involved opioids.
COVID-19 has worsened outcomes for people with addiction. There is less access to treatment, increased isolation, and worsening psychosocial and economic stressors. These factors may drive new, increased, or more risky substance use and return to use for people in recovery. As hospitalists, we have been responders in both COVID-19 and our country’s worsening overdose and addiction crisis.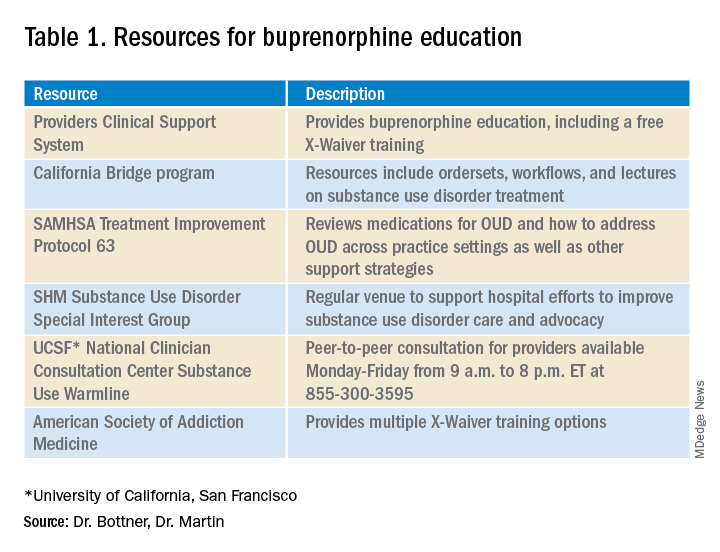
In December 2020’s Journal of Hospital Medicine article “Converging Crises: Caring for hospitalized adults with substance use disorder in the time of COVID-19”, Dr. Honora Englander and her coauthors called on hospitalists to actively engage patients with substance use disorders during hospitalization. The article highlights the colliding crises of addiction and COVID-19 and provides eight practical approaches for hospitalists to address substance use disorders during the pandemic, including initiating buprenorphine for opioid withdrawal and prescribing it for opioid use disorder (OUD) treatment.
Buprenorphine effectively treats opioid withdrawal, reduces OUD-related mortality, and decreases hospital readmissions related to OUD. To prescribe buprenorphine for OUD in the outpatient setting or on hospital discharge, providers need an X-Waiver. The X-Waiver is a result of the Drug Addiction Treatment Act 2000 (DATA 2000), which was enacted in 2000. It permits physicians to prescribe buprenorphine for OUD treatment after an 8-hour training. In 2016, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing to physician assistants (PAs) and advanced-practice nurses (APNs). However, PAs and APNs are required to complete a 24-hour training to receive the waiver.
On Jan. 14, 2021, the U.S. Department of Health and Human Services under the Trump administration announced it was removing the X-Waiver training previously required for physicians to prescribe this life-saving medication. However, on Jan. 20, 2021, the Biden administration froze the training requirement removal pending a 60-day review. The excitement about the waiver’s eradication further dampened on Jan. 25, when the plan was halted due to procedural factors coupled with the concern that HHS may not have the authority to void requirements mandated by Congress.
Many of us continue to be hopeful that the X-Waiver will soon be gone. The Substance Abuse and Mental Health Services Administration has committed to working with federal agencies to increase access to buprenorphine. The Biden administration also committed to addressing our country’s addiction crisis, including a plan to “make effective prevention, treatment, and recovery services available to all, including through a $125 billion federal investment.”
Despite the pause on HHS’s recent attempt to “X the X-Waiver,” we now have renewed attention and interest in this critical issue and an opportunity for greater and longer-lasting legislative impact. SHM supports that Congress repeal the legislative requirement for buprenorphine training dictated by DATA 2000 so that it cannot be rolled back by future administrations. To further increase access to buprenorphine treatment, the training requirement should be removed for all providers who care for individuals with OUD.
The X-Waiver has been a barrier to hospitalist adoption of this critical, life-saving medication. HHS’s stance to nix the waiver, though fleeting, should be interpreted as an urgent call to the medical community, including us as hospitalists, to learn about buprenorphine with the many resources available (see table 1). As hospital medicine providers, we can order buprenorphine for patients with OUD during hospitalization. It is discharge prescriptions that have been limited to providers with an X-Waiver.
What can we do now to prepare for the eventual X-Waiver training removal? We can start by educating ourselves with the resources listed in table 1. Those of us who are already buprenorphine champions could lead trainings in our home institutions. In a future without the waiver there will be more flexibility to develop hospitalist-focused buprenorphine trainings, as the previous ones were geared for outpatient providers. Hospitalist organizations could support hospitalist-specific buprenorphine trainings and extend the models to include additional medications for addiction.
There is a large body of evidence regarding buprenorphine’s safety and efficacy in OUD treatment. With a worsening overdose crisis, there have been increasing opioid-related hospitalizations. When new medications for diabetes, hypertension, or DVT treatment become available, as hospitalists we incorporate them into our toolbox. As buprenorphine becomes more accessible, we can be leaders in further adopting it (and other substance use disorder medications while we are at it) as our standard of care for people with OUD.
Dr. Bottner is a physician assistant in the Division of Hospital Medicine at Dell Medical School at The University of Texas at Austin and director of the hospital’s Buprenorphine Team. Dr. Martin is a board-certified addiction medicine physician and hospitalist at University of California, San Francisco, and director of the Addiction Care Team at San Francisco General Hospital. Dr. Bottner and Dr. Martin colead the SHM Substance Use Disorder Special Interest Group.
There are two pandemics permeating the United States: COVID-19 and addiction. To date, more than 468,000 people have died from COVID-19 in the U.S. In the 12-month period ending in May 2020, over 80,000 died from a drug related cause – the highest number ever recorded in a year. Many of these deaths involved opioids.
COVID-19 has worsened outcomes for people with addiction. There is less access to treatment, increased isolation, and worsening psychosocial and economic stressors. These factors may drive new, increased, or more risky substance use and return to use for people in recovery. As hospitalists, we have been responders in both COVID-19 and our country’s worsening overdose and addiction crisis.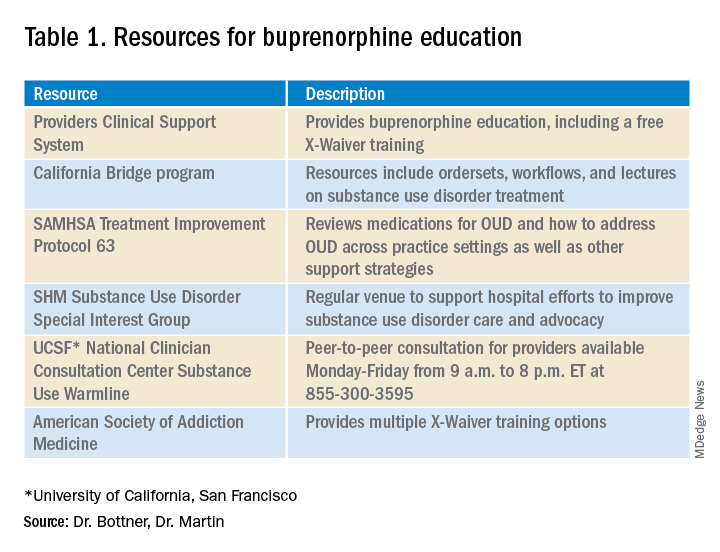
In December 2020’s Journal of Hospital Medicine article “Converging Crises: Caring for hospitalized adults with substance use disorder in the time of COVID-19”, Dr. Honora Englander and her coauthors called on hospitalists to actively engage patients with substance use disorders during hospitalization. The article highlights the colliding crises of addiction and COVID-19 and provides eight practical approaches for hospitalists to address substance use disorders during the pandemic, including initiating buprenorphine for opioid withdrawal and prescribing it for opioid use disorder (OUD) treatment.
Buprenorphine effectively treats opioid withdrawal, reduces OUD-related mortality, and decreases hospital readmissions related to OUD. To prescribe buprenorphine for OUD in the outpatient setting or on hospital discharge, providers need an X-Waiver. The X-Waiver is a result of the Drug Addiction Treatment Act 2000 (DATA 2000), which was enacted in 2000. It permits physicians to prescribe buprenorphine for OUD treatment after an 8-hour training. In 2016, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing to physician assistants (PAs) and advanced-practice nurses (APNs). However, PAs and APNs are required to complete a 24-hour training to receive the waiver.
On Jan. 14, 2021, the U.S. Department of Health and Human Services under the Trump administration announced it was removing the X-Waiver training previously required for physicians to prescribe this life-saving medication. However, on Jan. 20, 2021, the Biden administration froze the training requirement removal pending a 60-day review. The excitement about the waiver’s eradication further dampened on Jan. 25, when the plan was halted due to procedural factors coupled with the concern that HHS may not have the authority to void requirements mandated by Congress.
Many of us continue to be hopeful that the X-Waiver will soon be gone. The Substance Abuse and Mental Health Services Administration has committed to working with federal agencies to increase access to buprenorphine. The Biden administration also committed to addressing our country’s addiction crisis, including a plan to “make effective prevention, treatment, and recovery services available to all, including through a $125 billion federal investment.”
Despite the pause on HHS’s recent attempt to “X the X-Waiver,” we now have renewed attention and interest in this critical issue and an opportunity for greater and longer-lasting legislative impact. SHM supports that Congress repeal the legislative requirement for buprenorphine training dictated by DATA 2000 so that it cannot be rolled back by future administrations. To further increase access to buprenorphine treatment, the training requirement should be removed for all providers who care for individuals with OUD.
The X-Waiver has been a barrier to hospitalist adoption of this critical, life-saving medication. HHS’s stance to nix the waiver, though fleeting, should be interpreted as an urgent call to the medical community, including us as hospitalists, to learn about buprenorphine with the many resources available (see table 1). As hospital medicine providers, we can order buprenorphine for patients with OUD during hospitalization. It is discharge prescriptions that have been limited to providers with an X-Waiver.
What can we do now to prepare for the eventual X-Waiver training removal? We can start by educating ourselves with the resources listed in table 1. Those of us who are already buprenorphine champions could lead trainings in our home institutions. In a future without the waiver there will be more flexibility to develop hospitalist-focused buprenorphine trainings, as the previous ones were geared for outpatient providers. Hospitalist organizations could support hospitalist-specific buprenorphine trainings and extend the models to include additional medications for addiction.
There is a large body of evidence regarding buprenorphine’s safety and efficacy in OUD treatment. With a worsening overdose crisis, there have been increasing opioid-related hospitalizations. When new medications for diabetes, hypertension, or DVT treatment become available, as hospitalists we incorporate them into our toolbox. As buprenorphine becomes more accessible, we can be leaders in further adopting it (and other substance use disorder medications while we are at it) as our standard of care for people with OUD.
Dr. Bottner is a physician assistant in the Division of Hospital Medicine at Dell Medical School at The University of Texas at Austin and director of the hospital’s Buprenorphine Team. Dr. Martin is a board-certified addiction medicine physician and hospitalist at University of California, San Francisco, and director of the Addiction Care Team at San Francisco General Hospital. Dr. Bottner and Dr. Martin colead the SHM Substance Use Disorder Special Interest Group.
There are two pandemics permeating the United States: COVID-19 and addiction. To date, more than 468,000 people have died from COVID-19 in the U.S. In the 12-month period ending in May 2020, over 80,000 died from a drug related cause – the highest number ever recorded in a year. Many of these deaths involved opioids.
COVID-19 has worsened outcomes for people with addiction. There is less access to treatment, increased isolation, and worsening psychosocial and economic stressors. These factors may drive new, increased, or more risky substance use and return to use for people in recovery. As hospitalists, we have been responders in both COVID-19 and our country’s worsening overdose and addiction crisis.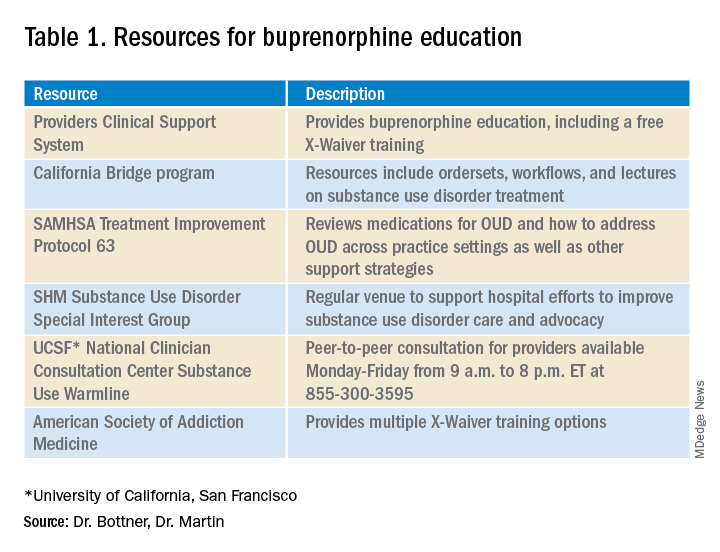
In December 2020’s Journal of Hospital Medicine article “Converging Crises: Caring for hospitalized adults with substance use disorder in the time of COVID-19”, Dr. Honora Englander and her coauthors called on hospitalists to actively engage patients with substance use disorders during hospitalization. The article highlights the colliding crises of addiction and COVID-19 and provides eight practical approaches for hospitalists to address substance use disorders during the pandemic, including initiating buprenorphine for opioid withdrawal and prescribing it for opioid use disorder (OUD) treatment.
Buprenorphine effectively treats opioid withdrawal, reduces OUD-related mortality, and decreases hospital readmissions related to OUD. To prescribe buprenorphine for OUD in the outpatient setting or on hospital discharge, providers need an X-Waiver. The X-Waiver is a result of the Drug Addiction Treatment Act 2000 (DATA 2000), which was enacted in 2000. It permits physicians to prescribe buprenorphine for OUD treatment after an 8-hour training. In 2016, the Comprehensive Addiction and Recovery Act extended buprenorphine prescribing to physician assistants (PAs) and advanced-practice nurses (APNs). However, PAs and APNs are required to complete a 24-hour training to receive the waiver.
On Jan. 14, 2021, the U.S. Department of Health and Human Services under the Trump administration announced it was removing the X-Waiver training previously required for physicians to prescribe this life-saving medication. However, on Jan. 20, 2021, the Biden administration froze the training requirement removal pending a 60-day review. The excitement about the waiver’s eradication further dampened on Jan. 25, when the plan was halted due to procedural factors coupled with the concern that HHS may not have the authority to void requirements mandated by Congress.
Many of us continue to be hopeful that the X-Waiver will soon be gone. The Substance Abuse and Mental Health Services Administration has committed to working with federal agencies to increase access to buprenorphine. The Biden administration also committed to addressing our country’s addiction crisis, including a plan to “make effective prevention, treatment, and recovery services available to all, including through a $125 billion federal investment.”
Despite the pause on HHS’s recent attempt to “X the X-Waiver,” we now have renewed attention and interest in this critical issue and an opportunity for greater and longer-lasting legislative impact. SHM supports that Congress repeal the legislative requirement for buprenorphine training dictated by DATA 2000 so that it cannot be rolled back by future administrations. To further increase access to buprenorphine treatment, the training requirement should be removed for all providers who care for individuals with OUD.
The X-Waiver has been a barrier to hospitalist adoption of this critical, life-saving medication. HHS’s stance to nix the waiver, though fleeting, should be interpreted as an urgent call to the medical community, including us as hospitalists, to learn about buprenorphine with the many resources available (see table 1). As hospital medicine providers, we can order buprenorphine for patients with OUD during hospitalization. It is discharge prescriptions that have been limited to providers with an X-Waiver.
What can we do now to prepare for the eventual X-Waiver training removal? We can start by educating ourselves with the resources listed in table 1. Those of us who are already buprenorphine champions could lead trainings in our home institutions. In a future without the waiver there will be more flexibility to develop hospitalist-focused buprenorphine trainings, as the previous ones were geared for outpatient providers. Hospitalist organizations could support hospitalist-specific buprenorphine trainings and extend the models to include additional medications for addiction.
There is a large body of evidence regarding buprenorphine’s safety and efficacy in OUD treatment. With a worsening overdose crisis, there have been increasing opioid-related hospitalizations. When new medications for diabetes, hypertension, or DVT treatment become available, as hospitalists we incorporate them into our toolbox. As buprenorphine becomes more accessible, we can be leaders in further adopting it (and other substance use disorder medications while we are at it) as our standard of care for people with OUD.
Dr. Bottner is a physician assistant in the Division of Hospital Medicine at Dell Medical School at The University of Texas at Austin and director of the hospital’s Buprenorphine Team. Dr. Martin is a board-certified addiction medicine physician and hospitalist at University of California, San Francisco, and director of the Addiction Care Team at San Francisco General Hospital. Dr. Bottner and Dr. Martin colead the SHM Substance Use Disorder Special Interest Group.
Converging Crises: Caring for Hospitalized Adults With Substance Use Disorder in the Time of COVID-19
The spread of SARS-CoV-2, the pathogen behind the COVID-19 pandemic, has converged with an unrelenting addiction epidemic. These combined crises will have profound effects on people with substance use disorders (SUD) and people in recovery. Hospitals—which were already hit hard by the addiction epidemic—are the last line of defense in the COVID-19 pandemic. Hospitalists have an important role in balancing the effects of these intersecting, synergistic crises.
People with SUD are disproportionately affected by major medical illnesses, including infections such as hepatitis C, HIV, and cardiovascular, pulmonary, and liver diseases.1 They also experience high rates of hospitalization due to drug-related infections, injury, and overdose.2 People with SUD commonly have intersecting vulnerabilities that may affect their healthcare experience and health outcomes, including housing and food insecurity, mental illness, and experiences of racism, incarceration, and other trauma. They may also harbor mistrust of healthcare providers because of previous negative encounters and discrimination with health systems.3 These vulnerabilities increase risks for COVID-19 morbidity and mortality.4,5 The COVID-19 pandemic may drive increases in use and harms from SUD among patients who already have an SUD, with widespread job loss, insurance loss,6 anxiety, and social isolation on the rise. We may also see increases in return to use among people in recovery or new substance use among those without a history of SUD.
The intersecting crises of SUD and COVID-19 are important for people with SUD and for public health. In this perspective, we describe how the COVID-19 pandemic has affected people with SUD and share practical resources for hospital providers to improve care for people with SUD during the pandemic and beyond.
CONTEXTUALIZING COVID-19 AND SUD RISK
Mistrust of Hospitals and Healthcare Providers
Fear of stigmatization is an ongoing problem for people with SUD, who often experience discrimination in hospitals and, as a result, may avoid hospital care.7 Much of this stigma is based on the false but persistent belief—widespread even among healthcare providers—that addiction is the result of bad choices and limited willpower; however, the science is clear that addiction is a disorder with neurobiological, genetic, and environmental underpinnings.3 These attitudes are likely to be amplified during COVID-19, as patients and providers experience higher levels of stress.
Increased Risks of Substance Use
Typically, people who use drugs are counseled to use with others nearby so that they might administer naloxone or call 911 in the event of an overdose.8 With physical distancing, people may be more likely to use alone. COVID-19 also introduces uncertainty into the drug supply chain through changes in drug production and trafficking.9 Further, access to alcohol may be limited as liquor stores close and public transportation becomes less available. As has been shown in other complex emergencies (such as social, political, economic, and environmental disasters), these barriers to obtaining substances may increase risks for withdrawal, for needing to exchange sex for money or drugs, for sharing syringes or drug preparation equipment,10 or for consuming other available sources of substances, like rubbing alcohol or hand sanitizer. COVID-19 may also increase risk for depression, anxiety, social isolation, and suicidality, all of which increase risk for return to use and overdose.
Changes to the Treatment Milieu
Many of the resources and services that people who use substances rely on to keep safe may be disrupted by COVID-19. Social distancing—the cornerstone of mitigating COVID-19 spread—may be challenging among people with SUD. Though federal regulations around methadone dispensing and buprenorphine prescribing have loosened in response to the pandemic,11 individuals in treatment may still be required to provide urine drug screens or be physically present to receive methadone doses, sometimes daily and in crowded waiting rooms.
Recovery support groups such as Alcoholics Anonymous (AA) and Self-Management and Recovery Training (SMART) provide social connection and are the foundation of many people’s recovery. While many in-person meetings have rapidly transformed to online and telephone support, they remain inaccessible to the most marginalized members of communities: people without smart phones, computers, or internet. This digital shift may also disproportionately affect older adults, people with limited English proficiency, and people with low technological literacy. Limits for other resources, such as syringe service programs, community centers, food pantries, housing shelters, and other places that people depend on for clean water, food, showers, soap, and safer spaces to use, may limit services or close altogether; those that remain open may see an unprecedented rise in need for services as millions of Americans file for unemployment. For many, anxiety about the pandemic, unemployment, financial strain, increased isolation, family stressors, illness, and community losses can lead to enormous personal distress and trigger return to use; loss of a recovery network may further exacerbate this.
Intersectionality of SUD and Other Structural Inequities
Many of the inequities that increase people’s risk for undertreated SUD also increase risk for COVID-19 infection, including racism,12 poverty, and homelessness.4 “Stay home and stay safe” is not an option for people who are unsheltered or whose homes are unsafe because of risks of physical, sexual, or emotional violence. Poverty commonly forces people to live in crowded communal apartments or shelters, rely on public transportation, wait in long lines at food pantries, and continue to work, even if unwell. Many shelters have had to reduce the number of people they serve to reduce crowding and support social distancing, which further compounds risks of unstable housing. Unfortunately, the same structural inequities that exacerbate SUD worsen the COVID-19 crisis.13
ROLE FOR HOSPITALISTS
The intersecting vulnerabilities of SUD and COVID-19 heighten an already urgent need to address SUD among hospitalized patients.14 While COVID-19 may increase harms of substance use, it may also increase people’s readiness to engage in treatment given changes to the drug supply and patient’s concerns about health risks. As such, it is even more critical to make treatment readily accessible and support harm reduction. Hospitalists can take important, actionable steps for patients with SUD—many of which are good general practices14 (Appendix Table).
Hospitalists should do the following:
1. Identify and treat acute withdrawal.15
2. Manage acute pain, including providing high-dose opioids if needed.16 Both practices (1 and 2) are evidence-based, can promote patient’s trust in providers,17 and can help avoid patients leaving against medical advice (AMA). Leaving AMA can lead to poor individual health and further threaten public health if patients leave with undiagnosed or unmanaged COVID-19 infection.
3. Encourage their hospitals to provide patients with tablets or other means to communicate with family, friends, and recovery supports via videolink, and refer patients to virtual peer support and recovery meetings during hospitalization.18 These practices may further support patients in tolerating hospitalization and prevent AMA discharge.
4. Initiate medication for addiction during admission and refer to addictions treatment after discharge. COVID-19–related regulatory changes such as expanded telehealth buprenorphine options and fewer daily dosing requirements for methadone may make this easier. Further, hospitalists should offer medication for alcohol and tobacco use disorders,15 especially given heightened possibility of unhealthy alcohol use and the respiratory complications associated with both tobacco and COVID-19.
5. Assess mental health and suicide risks19 given their association with social isolation, job loss, and financial insecurity.
6. Discuss relapse prevention among people in recovery.
7. Assess overdose risk and promote harm reduction.19 Specifically, this may include counseling patients to avoid sharing smoking supplies to avoid COVID-19 transmission, identifying places to access clean syringes, prescribing naloxone,20 and providing supports so that, if patients need to use alone, they can do so more safely.21
8. Consider high-risk transitions that may be exacerbated by COVID-19. COVID-19 may make safe discharge plans among people experiencing homelessness very challenging. Some communities are rapidly repurposing existing spaces or building new ones to care for people without a safe place to recover after acute hospitalization, yet many communities have no such resources. Hospital teams should consider the possibility that community services and SUD treatment resources may change rapidly during the pandemic. Hospitals can maintain updated resource lists and consider partnering with state and local health departments to improve safe care for people experiencing homelessness or lacking basic services.
COVID-19 is putting enormous strain on many US hospitals. Hospital-based addictions care is under resourced in the best of times,14 and while some hospitals have addiction consult services, many do not. To what degree hospitalists and hospital teams can address anything beyond COVID-19 emergencies will vary based on settings and resources. Furthermore, we recognize that who performs various activities will depend on individual hospital’s resources and practices. Addiction consult services, if available, can play a critical role, as can hospital social workers and care managers, nurses, residents, students, and other members of the healthcare team.
Finally, though COVID-19 adds tremendous stress to hospitals, permanent improvements in SUD treatment systems such as telephone visits for buprenorphine or eased methadone restrictions may emerge that could reduce barriers to hospital-based addictions care.11 Leveraging these changes now may help hospital providers to better support patients long-term.
CONCLUSION
Hospitalization can be a challenging time for patients with SUD and for the hospital teams who care for them. These tensions are exacerbated by the COVID-19 pandemic, yet hospitalists play a critical role in addressing the converging crises of SUD and COVID-19. Providing comprehensive, compassionate, evidence-based care for hospitalized patients with SUD is important for both individual and community health during COVID-19.
Acknowledgments
The authors would like to thank Alisa Patten for help preparing this manuscript.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
Dr King received grant support from the National Institutes of Health (UG1DA015815) and the National Institute on Drug Abuse (R01DA037441). Dr Snyder received a Public Health Institute grant payable to her institution.
1. Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated health care system. J Addict Med. 2017;11(1):3-9. https://doi.org/10.1097/adm.0000000000000260
2. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424
3. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
4. Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5(5):e240. https://doi.org/10.1016/s2468-2667(20)30085-2
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648
6. Woolhandler S, Himmelstein DU. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020;173(1):63-64. https://doi.org/10.7326/m20-1491
7. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010
8. Harm Reduction Coalition. Accessed April 24, 2020. https://harmreduction.org/
9. COVID-19 and the drug supply chain: from production and trafficking to use. Global Research Network, United Nations Office on Drugs and Crime; 2020. Accessed June 4, 2020. http://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf
10. Pouget ER, Sandoval M, Nikolopoulos GK, Friedman SR. Immediate impact of hurricane Sandy on people who inject drugs in New York City. Subst Use Misuse. 2015;50(7):878-884. https://doi.org/10.3109/10826084.2015.978675
11. FAQs: Provision of methadone and buprenorphine for the treatment of opioid use disorder in the COVID-19 emergency. Substance Abuse and Mental Health Services Administration. Updated April 21, 2020. Accessed March 27, 2020. https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf
12. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
13. Baggett TP, Lewis E, Gaeta JM. Epidemiology of COVID-19 among people experiencing homelessness: early evidence from Boston. Ann Fam Med. Preprint posted April 4, 2020. http://hdl.handle.net/2027.42/154734
14. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
15. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001
16. Quality & Science. American Society of Addiction Medicine. Accessed April 24, 2020. https://www.asam.org/Quality-Science/quality
17. Collins D, Alla J, Nicolaidis C, et al. “If it wasn’t for him, I wouldn’t have talked to them”: qualitative study of addiction peer mentorship in the hospital. J Gen Intern Med. Published online December 12, 2019. https://doi.org/10.1007/s11606-019-05311-0
18. Digital Recovery Support Services. Recovery Link. Accessed April 24, 2020. https://myrecoverylink.com/digital-recovery-support/
19. Publications and Digital Products: Suicide Assessment Five-Step Evaluation and Triage for Clinicians. Substance Abuse and Mental Health Administration. September 2009. Accessed April 4, 2020. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
20. Prescribe to Prevent: Prescribe Naloxone, Save a Life. Accessed April 24, 2020. https://prescribetoprevent.org/
21. Never Use Alone. Accessed April 24, 2020. https://neverusealone.com/
The spread of SARS-CoV-2, the pathogen behind the COVID-19 pandemic, has converged with an unrelenting addiction epidemic. These combined crises will have profound effects on people with substance use disorders (SUD) and people in recovery. Hospitals—which were already hit hard by the addiction epidemic—are the last line of defense in the COVID-19 pandemic. Hospitalists have an important role in balancing the effects of these intersecting, synergistic crises.
People with SUD are disproportionately affected by major medical illnesses, including infections such as hepatitis C, HIV, and cardiovascular, pulmonary, and liver diseases.1 They also experience high rates of hospitalization due to drug-related infections, injury, and overdose.2 People with SUD commonly have intersecting vulnerabilities that may affect their healthcare experience and health outcomes, including housing and food insecurity, mental illness, and experiences of racism, incarceration, and other trauma. They may also harbor mistrust of healthcare providers because of previous negative encounters and discrimination with health systems.3 These vulnerabilities increase risks for COVID-19 morbidity and mortality.4,5 The COVID-19 pandemic may drive increases in use and harms from SUD among patients who already have an SUD, with widespread job loss, insurance loss,6 anxiety, and social isolation on the rise. We may also see increases in return to use among people in recovery or new substance use among those without a history of SUD.
The intersecting crises of SUD and COVID-19 are important for people with SUD and for public health. In this perspective, we describe how the COVID-19 pandemic has affected people with SUD and share practical resources for hospital providers to improve care for people with SUD during the pandemic and beyond.
CONTEXTUALIZING COVID-19 AND SUD RISK
Mistrust of Hospitals and Healthcare Providers
Fear of stigmatization is an ongoing problem for people with SUD, who often experience discrimination in hospitals and, as a result, may avoid hospital care.7 Much of this stigma is based on the false but persistent belief—widespread even among healthcare providers—that addiction is the result of bad choices and limited willpower; however, the science is clear that addiction is a disorder with neurobiological, genetic, and environmental underpinnings.3 These attitudes are likely to be amplified during COVID-19, as patients and providers experience higher levels of stress.
Increased Risks of Substance Use
Typically, people who use drugs are counseled to use with others nearby so that they might administer naloxone or call 911 in the event of an overdose.8 With physical distancing, people may be more likely to use alone. COVID-19 also introduces uncertainty into the drug supply chain through changes in drug production and trafficking.9 Further, access to alcohol may be limited as liquor stores close and public transportation becomes less available. As has been shown in other complex emergencies (such as social, political, economic, and environmental disasters), these barriers to obtaining substances may increase risks for withdrawal, for needing to exchange sex for money or drugs, for sharing syringes or drug preparation equipment,10 or for consuming other available sources of substances, like rubbing alcohol or hand sanitizer. COVID-19 may also increase risk for depression, anxiety, social isolation, and suicidality, all of which increase risk for return to use and overdose.
Changes to the Treatment Milieu
Many of the resources and services that people who use substances rely on to keep safe may be disrupted by COVID-19. Social distancing—the cornerstone of mitigating COVID-19 spread—may be challenging among people with SUD. Though federal regulations around methadone dispensing and buprenorphine prescribing have loosened in response to the pandemic,11 individuals in treatment may still be required to provide urine drug screens or be physically present to receive methadone doses, sometimes daily and in crowded waiting rooms.
Recovery support groups such as Alcoholics Anonymous (AA) and Self-Management and Recovery Training (SMART) provide social connection and are the foundation of many people’s recovery. While many in-person meetings have rapidly transformed to online and telephone support, they remain inaccessible to the most marginalized members of communities: people without smart phones, computers, or internet. This digital shift may also disproportionately affect older adults, people with limited English proficiency, and people with low technological literacy. Limits for other resources, such as syringe service programs, community centers, food pantries, housing shelters, and other places that people depend on for clean water, food, showers, soap, and safer spaces to use, may limit services or close altogether; those that remain open may see an unprecedented rise in need for services as millions of Americans file for unemployment. For many, anxiety about the pandemic, unemployment, financial strain, increased isolation, family stressors, illness, and community losses can lead to enormous personal distress and trigger return to use; loss of a recovery network may further exacerbate this.
Intersectionality of SUD and Other Structural Inequities
Many of the inequities that increase people’s risk for undertreated SUD also increase risk for COVID-19 infection, including racism,12 poverty, and homelessness.4 “Stay home and stay safe” is not an option for people who are unsheltered or whose homes are unsafe because of risks of physical, sexual, or emotional violence. Poverty commonly forces people to live in crowded communal apartments or shelters, rely on public transportation, wait in long lines at food pantries, and continue to work, even if unwell. Many shelters have had to reduce the number of people they serve to reduce crowding and support social distancing, which further compounds risks of unstable housing. Unfortunately, the same structural inequities that exacerbate SUD worsen the COVID-19 crisis.13
ROLE FOR HOSPITALISTS
The intersecting vulnerabilities of SUD and COVID-19 heighten an already urgent need to address SUD among hospitalized patients.14 While COVID-19 may increase harms of substance use, it may also increase people’s readiness to engage in treatment given changes to the drug supply and patient’s concerns about health risks. As such, it is even more critical to make treatment readily accessible and support harm reduction. Hospitalists can take important, actionable steps for patients with SUD—many of which are good general practices14 (Appendix Table).
Hospitalists should do the following:
1. Identify and treat acute withdrawal.15
2. Manage acute pain, including providing high-dose opioids if needed.16 Both practices (1 and 2) are evidence-based, can promote patient’s trust in providers,17 and can help avoid patients leaving against medical advice (AMA). Leaving AMA can lead to poor individual health and further threaten public health if patients leave with undiagnosed or unmanaged COVID-19 infection.
3. Encourage their hospitals to provide patients with tablets or other means to communicate with family, friends, and recovery supports via videolink, and refer patients to virtual peer support and recovery meetings during hospitalization.18 These practices may further support patients in tolerating hospitalization and prevent AMA discharge.
4. Initiate medication for addiction during admission and refer to addictions treatment after discharge. COVID-19–related regulatory changes such as expanded telehealth buprenorphine options and fewer daily dosing requirements for methadone may make this easier. Further, hospitalists should offer medication for alcohol and tobacco use disorders,15 especially given heightened possibility of unhealthy alcohol use and the respiratory complications associated with both tobacco and COVID-19.
5. Assess mental health and suicide risks19 given their association with social isolation, job loss, and financial insecurity.
6. Discuss relapse prevention among people in recovery.
7. Assess overdose risk and promote harm reduction.19 Specifically, this may include counseling patients to avoid sharing smoking supplies to avoid COVID-19 transmission, identifying places to access clean syringes, prescribing naloxone,20 and providing supports so that, if patients need to use alone, they can do so more safely.21
8. Consider high-risk transitions that may be exacerbated by COVID-19. COVID-19 may make safe discharge plans among people experiencing homelessness very challenging. Some communities are rapidly repurposing existing spaces or building new ones to care for people without a safe place to recover after acute hospitalization, yet many communities have no such resources. Hospital teams should consider the possibility that community services and SUD treatment resources may change rapidly during the pandemic. Hospitals can maintain updated resource lists and consider partnering with state and local health departments to improve safe care for people experiencing homelessness or lacking basic services.
COVID-19 is putting enormous strain on many US hospitals. Hospital-based addictions care is under resourced in the best of times,14 and while some hospitals have addiction consult services, many do not. To what degree hospitalists and hospital teams can address anything beyond COVID-19 emergencies will vary based on settings and resources. Furthermore, we recognize that who performs various activities will depend on individual hospital’s resources and practices. Addiction consult services, if available, can play a critical role, as can hospital social workers and care managers, nurses, residents, students, and other members of the healthcare team.
Finally, though COVID-19 adds tremendous stress to hospitals, permanent improvements in SUD treatment systems such as telephone visits for buprenorphine or eased methadone restrictions may emerge that could reduce barriers to hospital-based addictions care.11 Leveraging these changes now may help hospital providers to better support patients long-term.
CONCLUSION
Hospitalization can be a challenging time for patients with SUD and for the hospital teams who care for them. These tensions are exacerbated by the COVID-19 pandemic, yet hospitalists play a critical role in addressing the converging crises of SUD and COVID-19. Providing comprehensive, compassionate, evidence-based care for hospitalized patients with SUD is important for both individual and community health during COVID-19.
Acknowledgments
The authors would like to thank Alisa Patten for help preparing this manuscript.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
Dr King received grant support from the National Institutes of Health (UG1DA015815) and the National Institute on Drug Abuse (R01DA037441). Dr Snyder received a Public Health Institute grant payable to her institution.
The spread of SARS-CoV-2, the pathogen behind the COVID-19 pandemic, has converged with an unrelenting addiction epidemic. These combined crises will have profound effects on people with substance use disorders (SUD) and people in recovery. Hospitals—which were already hit hard by the addiction epidemic—are the last line of defense in the COVID-19 pandemic. Hospitalists have an important role in balancing the effects of these intersecting, synergistic crises.
People with SUD are disproportionately affected by major medical illnesses, including infections such as hepatitis C, HIV, and cardiovascular, pulmonary, and liver diseases.1 They also experience high rates of hospitalization due to drug-related infections, injury, and overdose.2 People with SUD commonly have intersecting vulnerabilities that may affect their healthcare experience and health outcomes, including housing and food insecurity, mental illness, and experiences of racism, incarceration, and other trauma. They may also harbor mistrust of healthcare providers because of previous negative encounters and discrimination with health systems.3 These vulnerabilities increase risks for COVID-19 morbidity and mortality.4,5 The COVID-19 pandemic may drive increases in use and harms from SUD among patients who already have an SUD, with widespread job loss, insurance loss,6 anxiety, and social isolation on the rise. We may also see increases in return to use among people in recovery or new substance use among those without a history of SUD.
The intersecting crises of SUD and COVID-19 are important for people with SUD and for public health. In this perspective, we describe how the COVID-19 pandemic has affected people with SUD and share practical resources for hospital providers to improve care for people with SUD during the pandemic and beyond.
CONTEXTUALIZING COVID-19 AND SUD RISK
Mistrust of Hospitals and Healthcare Providers
Fear of stigmatization is an ongoing problem for people with SUD, who often experience discrimination in hospitals and, as a result, may avoid hospital care.7 Much of this stigma is based on the false but persistent belief—widespread even among healthcare providers—that addiction is the result of bad choices and limited willpower; however, the science is clear that addiction is a disorder with neurobiological, genetic, and environmental underpinnings.3 These attitudes are likely to be amplified during COVID-19, as patients and providers experience higher levels of stress.
Increased Risks of Substance Use
Typically, people who use drugs are counseled to use with others nearby so that they might administer naloxone or call 911 in the event of an overdose.8 With physical distancing, people may be more likely to use alone. COVID-19 also introduces uncertainty into the drug supply chain through changes in drug production and trafficking.9 Further, access to alcohol may be limited as liquor stores close and public transportation becomes less available. As has been shown in other complex emergencies (such as social, political, economic, and environmental disasters), these barriers to obtaining substances may increase risks for withdrawal, for needing to exchange sex for money or drugs, for sharing syringes or drug preparation equipment,10 or for consuming other available sources of substances, like rubbing alcohol or hand sanitizer. COVID-19 may also increase risk for depression, anxiety, social isolation, and suicidality, all of which increase risk for return to use and overdose.
Changes to the Treatment Milieu
Many of the resources and services that people who use substances rely on to keep safe may be disrupted by COVID-19. Social distancing—the cornerstone of mitigating COVID-19 spread—may be challenging among people with SUD. Though federal regulations around methadone dispensing and buprenorphine prescribing have loosened in response to the pandemic,11 individuals in treatment may still be required to provide urine drug screens or be physically present to receive methadone doses, sometimes daily and in crowded waiting rooms.
Recovery support groups such as Alcoholics Anonymous (AA) and Self-Management and Recovery Training (SMART) provide social connection and are the foundation of many people’s recovery. While many in-person meetings have rapidly transformed to online and telephone support, they remain inaccessible to the most marginalized members of communities: people without smart phones, computers, or internet. This digital shift may also disproportionately affect older adults, people with limited English proficiency, and people with low technological literacy. Limits for other resources, such as syringe service programs, community centers, food pantries, housing shelters, and other places that people depend on for clean water, food, showers, soap, and safer spaces to use, may limit services or close altogether; those that remain open may see an unprecedented rise in need for services as millions of Americans file for unemployment. For many, anxiety about the pandemic, unemployment, financial strain, increased isolation, family stressors, illness, and community losses can lead to enormous personal distress and trigger return to use; loss of a recovery network may further exacerbate this.
Intersectionality of SUD and Other Structural Inequities
Many of the inequities that increase people’s risk for undertreated SUD also increase risk for COVID-19 infection, including racism,12 poverty, and homelessness.4 “Stay home and stay safe” is not an option for people who are unsheltered or whose homes are unsafe because of risks of physical, sexual, or emotional violence. Poverty commonly forces people to live in crowded communal apartments or shelters, rely on public transportation, wait in long lines at food pantries, and continue to work, even if unwell. Many shelters have had to reduce the number of people they serve to reduce crowding and support social distancing, which further compounds risks of unstable housing. Unfortunately, the same structural inequities that exacerbate SUD worsen the COVID-19 crisis.13
ROLE FOR HOSPITALISTS
The intersecting vulnerabilities of SUD and COVID-19 heighten an already urgent need to address SUD among hospitalized patients.14 While COVID-19 may increase harms of substance use, it may also increase people’s readiness to engage in treatment given changes to the drug supply and patient’s concerns about health risks. As such, it is even more critical to make treatment readily accessible and support harm reduction. Hospitalists can take important, actionable steps for patients with SUD—many of which are good general practices14 (Appendix Table).
Hospitalists should do the following:
1. Identify and treat acute withdrawal.15
2. Manage acute pain, including providing high-dose opioids if needed.16 Both practices (1 and 2) are evidence-based, can promote patient’s trust in providers,17 and can help avoid patients leaving against medical advice (AMA). Leaving AMA can lead to poor individual health and further threaten public health if patients leave with undiagnosed or unmanaged COVID-19 infection.
3. Encourage their hospitals to provide patients with tablets or other means to communicate with family, friends, and recovery supports via videolink, and refer patients to virtual peer support and recovery meetings during hospitalization.18 These practices may further support patients in tolerating hospitalization and prevent AMA discharge.
4. Initiate medication for addiction during admission and refer to addictions treatment after discharge. COVID-19–related regulatory changes such as expanded telehealth buprenorphine options and fewer daily dosing requirements for methadone may make this easier. Further, hospitalists should offer medication for alcohol and tobacco use disorders,15 especially given heightened possibility of unhealthy alcohol use and the respiratory complications associated with both tobacco and COVID-19.
5. Assess mental health and suicide risks19 given their association with social isolation, job loss, and financial insecurity.
6. Discuss relapse prevention among people in recovery.
7. Assess overdose risk and promote harm reduction.19 Specifically, this may include counseling patients to avoid sharing smoking supplies to avoid COVID-19 transmission, identifying places to access clean syringes, prescribing naloxone,20 and providing supports so that, if patients need to use alone, they can do so more safely.21
8. Consider high-risk transitions that may be exacerbated by COVID-19. COVID-19 may make safe discharge plans among people experiencing homelessness very challenging. Some communities are rapidly repurposing existing spaces or building new ones to care for people without a safe place to recover after acute hospitalization, yet many communities have no such resources. Hospital teams should consider the possibility that community services and SUD treatment resources may change rapidly during the pandemic. Hospitals can maintain updated resource lists and consider partnering with state and local health departments to improve safe care for people experiencing homelessness or lacking basic services.
COVID-19 is putting enormous strain on many US hospitals. Hospital-based addictions care is under resourced in the best of times,14 and while some hospitals have addiction consult services, many do not. To what degree hospitalists and hospital teams can address anything beyond COVID-19 emergencies will vary based on settings and resources. Furthermore, we recognize that who performs various activities will depend on individual hospital’s resources and practices. Addiction consult services, if available, can play a critical role, as can hospital social workers and care managers, nurses, residents, students, and other members of the healthcare team.
Finally, though COVID-19 adds tremendous stress to hospitals, permanent improvements in SUD treatment systems such as telephone visits for buprenorphine or eased methadone restrictions may emerge that could reduce barriers to hospital-based addictions care.11 Leveraging these changes now may help hospital providers to better support patients long-term.
CONCLUSION
Hospitalization can be a challenging time for patients with SUD and for the hospital teams who care for them. These tensions are exacerbated by the COVID-19 pandemic, yet hospitalists play a critical role in addressing the converging crises of SUD and COVID-19. Providing comprehensive, compassionate, evidence-based care for hospitalized patients with SUD is important for both individual and community health during COVID-19.
Acknowledgments
The authors would like to thank Alisa Patten for help preparing this manuscript.
Disclosures
The authors have no conflicts of interest to disclose.
Funding
Dr King received grant support from the National Institutes of Health (UG1DA015815) and the National Institute on Drug Abuse (R01DA037441). Dr Snyder received a Public Health Institute grant payable to her institution.
1. Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated health care system. J Addict Med. 2017;11(1):3-9. https://doi.org/10.1097/adm.0000000000000260
2. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424
3. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
4. Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5(5):e240. https://doi.org/10.1016/s2468-2667(20)30085-2
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648
6. Woolhandler S, Himmelstein DU. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020;173(1):63-64. https://doi.org/10.7326/m20-1491
7. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010
8. Harm Reduction Coalition. Accessed April 24, 2020. https://harmreduction.org/
9. COVID-19 and the drug supply chain: from production and trafficking to use. Global Research Network, United Nations Office on Drugs and Crime; 2020. Accessed June 4, 2020. http://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf
10. Pouget ER, Sandoval M, Nikolopoulos GK, Friedman SR. Immediate impact of hurricane Sandy on people who inject drugs in New York City. Subst Use Misuse. 2015;50(7):878-884. https://doi.org/10.3109/10826084.2015.978675
11. FAQs: Provision of methadone and buprenorphine for the treatment of opioid use disorder in the COVID-19 emergency. Substance Abuse and Mental Health Services Administration. Updated April 21, 2020. Accessed March 27, 2020. https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf
12. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
13. Baggett TP, Lewis E, Gaeta JM. Epidemiology of COVID-19 among people experiencing homelessness: early evidence from Boston. Ann Fam Med. Preprint posted April 4, 2020. http://hdl.handle.net/2027.42/154734
14. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
15. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001
16. Quality & Science. American Society of Addiction Medicine. Accessed April 24, 2020. https://www.asam.org/Quality-Science/quality
17. Collins D, Alla J, Nicolaidis C, et al. “If it wasn’t for him, I wouldn’t have talked to them”: qualitative study of addiction peer mentorship in the hospital. J Gen Intern Med. Published online December 12, 2019. https://doi.org/10.1007/s11606-019-05311-0
18. Digital Recovery Support Services. Recovery Link. Accessed April 24, 2020. https://myrecoverylink.com/digital-recovery-support/
19. Publications and Digital Products: Suicide Assessment Five-Step Evaluation and Triage for Clinicians. Substance Abuse and Mental Health Administration. September 2009. Accessed April 4, 2020. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
20. Prescribe to Prevent: Prescribe Naloxone, Save a Life. Accessed April 24, 2020. https://prescribetoprevent.org/
21. Never Use Alone. Accessed April 24, 2020. https://neverusealone.com/
1. Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated health care system. J Addict Med. 2017;11(1):3-9. https://doi.org/10.1097/adm.0000000000000260
2. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424
3. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131(1-2):23-35. https://doi.org/10.1016/j.drugalcdep.2013.02.018
4. Ahmed F, Ahmed N, Pissarides C, Stiglitz J. Why inequality could spread COVID-19. Lancet Public Health. 2020;5(5):e240. https://doi.org/10.1016/s2468-2667(20)30085-2
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242. https://doi.org/10.1001/jama.2020.2648
6. Woolhandler S, Himmelstein DU. Intersecting U.S. epidemics: COVID-19 and lack of health insurance. Ann Intern Med. 2020;173(1):63-64. https://doi.org/10.7326/m20-1491
7. McNeil R, Small W, Wood E, Kerr T. Hospitals as a ‘risk environment’: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010
8. Harm Reduction Coalition. Accessed April 24, 2020. https://harmreduction.org/
9. COVID-19 and the drug supply chain: from production and trafficking to use. Global Research Network, United Nations Office on Drugs and Crime; 2020. Accessed June 4, 2020. http://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf
10. Pouget ER, Sandoval M, Nikolopoulos GK, Friedman SR. Immediate impact of hurricane Sandy on people who inject drugs in New York City. Subst Use Misuse. 2015;50(7):878-884. https://doi.org/10.3109/10826084.2015.978675
11. FAQs: Provision of methadone and buprenorphine for the treatment of opioid use disorder in the COVID-19 emergency. Substance Abuse and Mental Health Services Administration. Updated April 21, 2020. Accessed March 27, 2020. https://www.samhsa.gov/sites/default/files/faqs-for-oud-prescribing-and-dispensing.pdf
12. Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. https://doi.org/10.1001/jama.2020.6548
13. Baggett TP, Lewis E, Gaeta JM. Epidemiology of COVID-19 among people experiencing homelessness: early evidence from Boston. Ann Fam Med. Preprint posted April 4, 2020. http://hdl.handle.net/2027.42/154734
14. Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311
15. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001
16. Quality & Science. American Society of Addiction Medicine. Accessed April 24, 2020. https://www.asam.org/Quality-Science/quality
17. Collins D, Alla J, Nicolaidis C, et al. “If it wasn’t for him, I wouldn’t have talked to them”: qualitative study of addiction peer mentorship in the hospital. J Gen Intern Med. Published online December 12, 2019. https://doi.org/10.1007/s11606-019-05311-0
18. Digital Recovery Support Services. Recovery Link. Accessed April 24, 2020. https://myrecoverylink.com/digital-recovery-support/
19. Publications and Digital Products: Suicide Assessment Five-Step Evaluation and Triage for Clinicians. Substance Abuse and Mental Health Administration. September 2009. Accessed April 4, 2020. https://store.samhsa.gov/product/SAFE-T-Pocket-Card-Suicide-Assessment-Five-Step-Evaluation-and-Triage-for-Clinicians/sma09-4432
20. Prescribe to Prevent: Prescribe Naloxone, Save a Life. Accessed April 24, 2020. https://prescribetoprevent.org/
21. Never Use Alone. Accessed April 24, 2020. https://neverusealone.com/
© 2020 Society of Hospital Medicine
A Call to Action: Hospitalists’ Role in Addressing Substance Use Disorder
In 2017, the death toll from drug overdoses reached a record high, killing more Americans than the entire Vietnam War or the HIV/AIDS epidemic at its peak.1 Up to one-quarter of hospitalized patients have a substance use disorder (SUD) and SUD-related2,3 hospitalizations are surging. People with SUD have longer hospital stays, higher costs, and more readmissions.3,4 While the burden of SUD is staggering, it is far from hopeless. There are multiple evidence-based and highly effective interventions to treat SUD, including medications, behavioral interventions, and harm reduction strategies.
Hospitalization can be a reachable moment to initiate and coordinate addictions care.5 Hospital-based addictions care has the potential to engage sicker, highly vulnerable patients, many who are not engaged in primary care or outpatient addictions care.6 Studied effects of hospital-based addictions care include improved SUD treatment engagement, reduced alcohol and drug use, lower hospital readmissions, and improved provider experience.7-9
Most hospitals, however, do not treat SUD during hospitalization and do not connect people to treatment after discharge. Hospitals may lack staffing or financial resources to implement addiction care, may believe that SUDs are an outpatient concern, may want to avoid caring for people with SUD, or may simply not know where to begin. Whatever the reason, unaddressed SUD can lead to untreated withdrawal, disruptive patient behaviors, failure to complete recommended medical therapy, high rates of against medical advice discharge, poor patient experience, and widespread provider distress.8
Hospitalists—individually and collectively—are uniquely positioned to address this gap. By treating addiction effectively and compassionately, hospitalists can engage patients, improve care, improve patient and provider experience, and lower costs. This paper is a call to action that describes the current state of hospital-based addictions care, outlines key challenges to implementing SUD care in the hospital, debunks common misconceptions, and identifies actionable steps for hospitalists, hospital leaders, and hospitalist organizations.
MODELS TO DELIVER HOSPITAL-BASED ADDICTIONS CARE
Hospital-based addiction medicine consult services are emerging; they include a range of models, with variations in how patients are identified, team composition, service availability, and financing.10 Existing addiction medicine consult services commonly offer SUD assessments, psychological intervention, medical management of SUDs (eg, initiating methadone or buprenorphine), medical pain management, and linkage to SUD care after hospitalization. Some services also explicitly integrate harm reduction principles (eg, naloxone distribution, safe injection education, permitting patients to smoke).11 Additional consult service activities include hospital-wide SUD education, and creation and implementation of hospital guidance documents (eg, methadone policies).10 Some consult services utilize only physicians, while others include interprofessional providers, such as nurses, social workers, and peers with lived experience of addiction. Whereas addiction medicine physicians staff some consult services, hospitalists with less formal addiction credentials staff others.
Broadly, hospital-based addictions care cannot depend solely on consult services. Just as not all hospitals have cardiology consult services, not all hospitals will have addiction consult services. As such, hospitalists can play an even greater role by implementing order sets and guidelines, supporting partnerships with community SUD treatment, and independently initiating evidence-based medications.
CHALLENGES TO ADOPTION AND IMPLEMENTATION OF HOSPITAL-BASED ADDICTIONS CARE
Pervasive individual and structural stigmas12 are perhaps the most critical barriers to incorporating addiction medicine into routine hospital practice, and they are both cause and consequence of our system failures. Most medical schools and residencies lack SUD training, which means that the understanding of addiction as a moral deficiency or lack of willpower may remain unchallenged. Stigma surrounding SUDs contributes to hospitalists’ and hospital leaders’ aversion to treating patients with SUD, and to fears that providing quality SUD care will attract patients suffering from these conditions.
Recent national efforts have focused on the problem of opioid overprescribing. Without an equal emphasis on treatment, this focus can lead to undertreatment of pain and/or opioid use disorder in hospitalized patients, particularly since most hospitalists have little to no training in diagnosing SUD, prescribing life-saving medications for opioid use disorder, or managing acute pain in patients with SUD. The focus on overprescribing also diverts attention away from trends involving stimulants,2 fentanyl contamination of the drug supply,13 and alcohol, all of which have important implications for the care of hospitalized adults.
Hospital policies are often not grounded in evidence (eg, recommending clonidine for first-line treatment of opioid withdrawal and not buprenorphine/methadone), and there are widespread misconceptions about perceived legal barriers to treating opioid use disorder in the hospital, which is both safe and legal.10 People with SUD may be unjustly viewed through a criminal justice lens. Policies focused on controlling visitors and conducting room searches disproportionately burden people with SUD, which may create further harms through reinforcing negative provider cognitive biases about SUDs. Finally, hospitals may lack inpatient social work and pharmacy supports, and they rarely have pathways to connect people to SUD care after discharge.
Funding remains a widespread challenge. While some hospital administrators support addiction medicine services because of the pressing medical need and public health crisis, most services depend on billing or demonstrated savings through reduced hospital days or readmissions.
A CALL TO ACTION: HOW HOSPITALISTS CAN IMPROVE ADDICTION CARE
Individual hospitalists, hospitalist leaders, and hospitalist organizations can engage by improving individual practice, driving systems change, and through advocacy and policy change (Table).
Individual Hospitalists
Providing basic addiction medicine care should be a core competency for all hospitalists, just as every hospitalist can initiate a goals-of-care conversation or prescribe insulin. For opioid use disorder, hospitalists should treat withdrawal and offer treatment initiation with opioid agonist therapy (ie, methadone, buprenorphine), which reduces mortality by over half. Commonly, hospitalized patients are subjected to harmful, nonevidence-based treatments, such as mandated rapid methadone tapers,25 which can lead to undertreated withdrawal, increased pain, and opioid cravings. This increases patients’ risk for overdose after discharge and precludes them from receiving life-saving, evidence-based methadone maintenance, or buprenorphine treatment. Though widely misunderstood, prescribing methadone in the hospital is legal, and providers need no special waiver to prescribe buprenorphine during admission. Current laws require that hospitalists have a waiver to prescribe buprenorphine at discharge and prohibit hospitalists (or anyone outside of an opioid treatment program) from prescribing methadone for the treatment of opioid use disorder at discharge. Further, hospitalists should offer medication for alcohol use disorder (eg, naltrexone) and be good stewards of opioids during hospitalization, avoiding intravenous opioids where appropriate and curbing excessive prescribing at discharge. Given high rates of overdose and fentanyl contamination of stimulants, opioids, and benzodiazepines, hospitalists should prescribe naloxone at discharge to every patient with SUD, on chronic opioids, or who uses any nonmedical substances.
Resources exist for individual hospitalists seeking mentorship or additional training (Table). Though not necessary for in-hospital prescribing, hospitalists can obtain a waiver to prescribe buprenorphine at discharge (commonly called the X-waiver). To qualify, physicians must complete eight hours of accredited training (online and/or in-person), after which they must request a waiver from the Drug Enforcement Administration. Advanced-practice practitioners must complete 24 hours of training. Many have argued that policymakers should end this waiver requirement.26 While we support efforts to “X the X” and urgently expand treatment access, additional training can enrich providers’ knowledge and confidence to prescribe buprenorphine, and is a relatively simple way that all hospitalists could act. Finally, by treating addiction and modeling patient-centered addictions care, hospitalists can legitimize and destigmatize the disease of addiction,8 and have the potential to mentor and train students, residents, nurses, and other staff.27
Hospitalist Leaders
As leaders, hospitalists can play a key role in promoting hospital-based addictions care and tailoring solutions to meet local needs. Leaders can promote a cultural shift away from stigma, and promote evidence-based, life-saving care. Hospitalist leaders could require all hospitalists to obtain buprenorphine waivers. Leaders could initiate quality improvement projects related to SUD service delivery, develop policies that support inpatient SUD treatment, develop order sets for medication initiation, engage community substance use treatment partners, build pathways to timely addiction care after discharge, and champion development of addiction medicine consult services.
Hospitalist leaders can reference open-source guidelines, order sets, assessment and treatment tools, patient materials, pharmacy and therapeutics committee materials, and other resources for implementing services for hospitalized patients with SUD (Table).21,22 Hospitalist leaders who understand financial and quality drivers can also champion the business and quality case for hospital-based addictions care, and help pursue local and national funding opportunities.
Hospitalist Organizations
Hospitalist societies could provide training at regional and national conferences to upskill hospitalists to care for people with SUD; support addiction medicine interest groups; and partner with addiction medicine societies, harm reduction organizations, and organizations focused on trauma-informed care. They could endorse practice guidelines and position statements describing the crucial role of hospitalists in addressing the overdose crisis and offering medication for addiction (Table). Hospitalist organizations can engage national and state hospital associations, lobby medical specialties to include addiction medicine competencies in board certification requirements, and advocate with governmental leaders to reduce barriers that restrict treatment access such as the X-waiver.
MOVING FORWARD
Regardless of whether a hospitalist is serving as an individual provider, a hospitalist leader, or as part of a hospitalist organization, hospitalists can take critical steps to advance the care of people with SUD. These steps shift the culture of hospitals from one where patients are afraid to discuss their substance use, to one that creates space for connection, treatment engagement, and healing. By starting medications, utilizing widely accessible resources, and collaborating with community treatment and harm reduction organizations, each one of us can play a part in addressing the epidemic.
Acknowledgments
The authors thank Alisa Patten for help preparing this manuscript. Dr. Englander would like to thank Dr. David Bangsberg and Dr. Christina Nicolaidis for their mentorship.
1. Weiss A, Elixhauser A, Barrett M, Steiner C, Bailey M, O’Malley L. Opioid-related inpatient stays and emergency department visits by state, 2009-2014. Statistical Brief #219. Healthcare Cost and Utilization Project. 2016. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.jsp. Accessed May 21, 2019.
2. Winkelman TA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of amphetamine-related hospitalizations and associated clinical outcomes and costs in the United States. JAMA Netw Open. 2018;1(6):e183758. https://doi.org/10.1001/jamanetworkopen.2018.3758.
3. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424.
4. Walley AY, Paasche-Orlow M, Lee EC, et al. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6(1):50-56. https://doi.org/10.1097/ADM.0b013e318231de51.
5. Englander H, Weimer M, Solotaroff R, et al. Planning and designing the Improving Addiction Care Team (IMPACT) for hospitalized adults with substance use disorder. J Hosp Med. 2017;12(5):339-342. https://doi.org/10.12788/jhm.2736.
6. Velez C, Nicolaidis C, Korthuis P, Englander H. “It’s been an experience, a life learning experience”: a qualitative study of hospitalized patients with substance use disorders. J Gen Intern Med. 2017;32(3):296-303. doi 10.1007/s11606-016-3919-4.
7. Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient addiction consultation for hospitalized patients increases post-discharge abstinence and reduces addiction severity. J Gen Intern Med. 2017;32(8):909-916. https://doi.org/10.1007/s11606-017-4077-z.
8. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993.
9. McQueen J, Howe TE, Allan L, Mains D, Hardy V. Brief interventions for heavy alcohol users admitted to general hospital wards. Cochrane Database Syst Rev. 2011;10(8):CD005191 https://doi.org/10.1002/14651858.CD005191.pub3.
10. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496.
11. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001.
12. McNeil R, Small W, Wood E, Kerr T. Hospitals as a “risk environment”: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010.
13. Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019. pii: S0955-3959(19)30018-0. [Epub ahead of print]. https://doi.org/10.1016/j.drugpo.2019.01.010.
14. Substance Abuse and Mental Health Services Administration. TIP 63: Medications for Opioid Use Disorder-Executive Summary. February 2018. https://store.samhsa.gov/product/TIP-63-Medications-for-Opioid-Use-Disorder-Executive-Summary/sma18-5063exsumm. Accessed August 8, 2019.
15. Providers Clinical Support System. Discover the rewards of treating patients with Opioid Use Disorders. https://pcssnow.org/. Accessed August 8, 2019.
16. California Bridge Program. Treatment Starts Here: Resources for the Treatment of Substance Use Disorders from the Acute Care Setting. https://www.bridgetotreatment.org/resources. Accessed August 7, 2019.
17. Clinical Consultation Center. Substance Use Resources. 2019. https://nccc.ucsf.edu/clinical-resources/substance-use-resources/. Accessed August 8, 2019.
18. Thakarar K, Weinstein ZM, Walley AY. Optimising health and safety of people who inject drugs during transition from acute to outpatient care: narrative review with clinical checklist. Postgrad Med J. 2016;92(1088):356-363. https://doi.org/10.1136/postgradmedj-2015-133720.
19. Office of National Drug Control Policy. Changing the Language of Addiction. Washington, D.C. 2017. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Memo%20-%20Changing%20Federal%20Terminology%20Regrading%20Substance%20Use%20and%20Substance%20Use%20Disorders.pdf. Accessed August 8, 2019.
20. The University of New Mexico. Project ECHO: A Revolution in Medical Education and Care Delivery. 2019. https://echo.unm.edu/. Accessed August 8, 2019.
21. Englander H, Mahoney S, Brandt K, et al. Tools to support hospital-based addiction care: core components, values, and activities of the Improving Addiction Care Team. J Addict Med. 2019;13(2):85-89. https://doi.org/10.1097/ADM.0000000000000487.
22. Englander H, Gregg J, Gollickson J, et al. Recommendations for intergrating peer mentors in hospital-based addiction care. Subst Abus. In press. https://doi.org/10.1080/08897077.2019.1635968.
23. American College of Medical Toxicology. ACMT Position Statement: Buprenorphine Administration in the Emergency Department. https://www.acep.org/globalassets/sites/acep/media/equal-documents/policy_acmt_bupeadministration.pdf. Accessed May 21, 2019.
24. Herzig SJ, Mosher HJ, Calcaterra SL, Jena AB, Nuckols TK. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018;13(4):263-271. https://doi.org/10.12788/jhm.2980.
25. Winetsky D, Weinrieb RM, Perrone J. Expanding treatment opportunities for hospitalized patients with opioid use disorders. J Hosp Med. 2018;13(1):62-64. https://doi.org/10.12788/jhm.2861.
26. Frank JW, Wakeman SE, Gordon AJ. No end to the crisis without an end to the waiver. Subst Abus. 2018;39(3):263-265. https://doi.org/10.1080/08897077.2018.1543382.
27. Gorfinkel L, Klimas J, Reel B, et al. In-hospital training in addiction medicine: a mixed-methods study of health care provider benefits and differences. Subst Abus. 2019. In press. https://doi.org/10.1080/08897077.2018.1561596.
In 2017, the death toll from drug overdoses reached a record high, killing more Americans than the entire Vietnam War or the HIV/AIDS epidemic at its peak.1 Up to one-quarter of hospitalized patients have a substance use disorder (SUD) and SUD-related2,3 hospitalizations are surging. People with SUD have longer hospital stays, higher costs, and more readmissions.3,4 While the burden of SUD is staggering, it is far from hopeless. There are multiple evidence-based and highly effective interventions to treat SUD, including medications, behavioral interventions, and harm reduction strategies.
Hospitalization can be a reachable moment to initiate and coordinate addictions care.5 Hospital-based addictions care has the potential to engage sicker, highly vulnerable patients, many who are not engaged in primary care or outpatient addictions care.6 Studied effects of hospital-based addictions care include improved SUD treatment engagement, reduced alcohol and drug use, lower hospital readmissions, and improved provider experience.7-9
Most hospitals, however, do not treat SUD during hospitalization and do not connect people to treatment after discharge. Hospitals may lack staffing or financial resources to implement addiction care, may believe that SUDs are an outpatient concern, may want to avoid caring for people with SUD, or may simply not know where to begin. Whatever the reason, unaddressed SUD can lead to untreated withdrawal, disruptive patient behaviors, failure to complete recommended medical therapy, high rates of against medical advice discharge, poor patient experience, and widespread provider distress.8
Hospitalists—individually and collectively—are uniquely positioned to address this gap. By treating addiction effectively and compassionately, hospitalists can engage patients, improve care, improve patient and provider experience, and lower costs. This paper is a call to action that describes the current state of hospital-based addictions care, outlines key challenges to implementing SUD care in the hospital, debunks common misconceptions, and identifies actionable steps for hospitalists, hospital leaders, and hospitalist organizations.
MODELS TO DELIVER HOSPITAL-BASED ADDICTIONS CARE
Hospital-based addiction medicine consult services are emerging; they include a range of models, with variations in how patients are identified, team composition, service availability, and financing.10 Existing addiction medicine consult services commonly offer SUD assessments, psychological intervention, medical management of SUDs (eg, initiating methadone or buprenorphine), medical pain management, and linkage to SUD care after hospitalization. Some services also explicitly integrate harm reduction principles (eg, naloxone distribution, safe injection education, permitting patients to smoke).11 Additional consult service activities include hospital-wide SUD education, and creation and implementation of hospital guidance documents (eg, methadone policies).10 Some consult services utilize only physicians, while others include interprofessional providers, such as nurses, social workers, and peers with lived experience of addiction. Whereas addiction medicine physicians staff some consult services, hospitalists with less formal addiction credentials staff others.
Broadly, hospital-based addictions care cannot depend solely on consult services. Just as not all hospitals have cardiology consult services, not all hospitals will have addiction consult services. As such, hospitalists can play an even greater role by implementing order sets and guidelines, supporting partnerships with community SUD treatment, and independently initiating evidence-based medications.
CHALLENGES TO ADOPTION AND IMPLEMENTATION OF HOSPITAL-BASED ADDICTIONS CARE
Pervasive individual and structural stigmas12 are perhaps the most critical barriers to incorporating addiction medicine into routine hospital practice, and they are both cause and consequence of our system failures. Most medical schools and residencies lack SUD training, which means that the understanding of addiction as a moral deficiency or lack of willpower may remain unchallenged. Stigma surrounding SUDs contributes to hospitalists’ and hospital leaders’ aversion to treating patients with SUD, and to fears that providing quality SUD care will attract patients suffering from these conditions.
Recent national efforts have focused on the problem of opioid overprescribing. Without an equal emphasis on treatment, this focus can lead to undertreatment of pain and/or opioid use disorder in hospitalized patients, particularly since most hospitalists have little to no training in diagnosing SUD, prescribing life-saving medications for opioid use disorder, or managing acute pain in patients with SUD. The focus on overprescribing also diverts attention away from trends involving stimulants,2 fentanyl contamination of the drug supply,13 and alcohol, all of which have important implications for the care of hospitalized adults.
Hospital policies are often not grounded in evidence (eg, recommending clonidine for first-line treatment of opioid withdrawal and not buprenorphine/methadone), and there are widespread misconceptions about perceived legal barriers to treating opioid use disorder in the hospital, which is both safe and legal.10 People with SUD may be unjustly viewed through a criminal justice lens. Policies focused on controlling visitors and conducting room searches disproportionately burden people with SUD, which may create further harms through reinforcing negative provider cognitive biases about SUDs. Finally, hospitals may lack inpatient social work and pharmacy supports, and they rarely have pathways to connect people to SUD care after discharge.
Funding remains a widespread challenge. While some hospital administrators support addiction medicine services because of the pressing medical need and public health crisis, most services depend on billing or demonstrated savings through reduced hospital days or readmissions.
A CALL TO ACTION: HOW HOSPITALISTS CAN IMPROVE ADDICTION CARE
Individual hospitalists, hospitalist leaders, and hospitalist organizations can engage by improving individual practice, driving systems change, and through advocacy and policy change (Table).
Individual Hospitalists
Providing basic addiction medicine care should be a core competency for all hospitalists, just as every hospitalist can initiate a goals-of-care conversation or prescribe insulin. For opioid use disorder, hospitalists should treat withdrawal and offer treatment initiation with opioid agonist therapy (ie, methadone, buprenorphine), which reduces mortality by over half. Commonly, hospitalized patients are subjected to harmful, nonevidence-based treatments, such as mandated rapid methadone tapers,25 which can lead to undertreated withdrawal, increased pain, and opioid cravings. This increases patients’ risk for overdose after discharge and precludes them from receiving life-saving, evidence-based methadone maintenance, or buprenorphine treatment. Though widely misunderstood, prescribing methadone in the hospital is legal, and providers need no special waiver to prescribe buprenorphine during admission. Current laws require that hospitalists have a waiver to prescribe buprenorphine at discharge and prohibit hospitalists (or anyone outside of an opioid treatment program) from prescribing methadone for the treatment of opioid use disorder at discharge. Further, hospitalists should offer medication for alcohol use disorder (eg, naltrexone) and be good stewards of opioids during hospitalization, avoiding intravenous opioids where appropriate and curbing excessive prescribing at discharge. Given high rates of overdose and fentanyl contamination of stimulants, opioids, and benzodiazepines, hospitalists should prescribe naloxone at discharge to every patient with SUD, on chronic opioids, or who uses any nonmedical substances.
Resources exist for individual hospitalists seeking mentorship or additional training (Table). Though not necessary for in-hospital prescribing, hospitalists can obtain a waiver to prescribe buprenorphine at discharge (commonly called the X-waiver). To qualify, physicians must complete eight hours of accredited training (online and/or in-person), after which they must request a waiver from the Drug Enforcement Administration. Advanced-practice practitioners must complete 24 hours of training. Many have argued that policymakers should end this waiver requirement.26 While we support efforts to “X the X” and urgently expand treatment access, additional training can enrich providers’ knowledge and confidence to prescribe buprenorphine, and is a relatively simple way that all hospitalists could act. Finally, by treating addiction and modeling patient-centered addictions care, hospitalists can legitimize and destigmatize the disease of addiction,8 and have the potential to mentor and train students, residents, nurses, and other staff.27
Hospitalist Leaders
As leaders, hospitalists can play a key role in promoting hospital-based addictions care and tailoring solutions to meet local needs. Leaders can promote a cultural shift away from stigma, and promote evidence-based, life-saving care. Hospitalist leaders could require all hospitalists to obtain buprenorphine waivers. Leaders could initiate quality improvement projects related to SUD service delivery, develop policies that support inpatient SUD treatment, develop order sets for medication initiation, engage community substance use treatment partners, build pathways to timely addiction care after discharge, and champion development of addiction medicine consult services.
Hospitalist leaders can reference open-source guidelines, order sets, assessment and treatment tools, patient materials, pharmacy and therapeutics committee materials, and other resources for implementing services for hospitalized patients with SUD (Table).21,22 Hospitalist leaders who understand financial and quality drivers can also champion the business and quality case for hospital-based addictions care, and help pursue local and national funding opportunities.
Hospitalist Organizations
Hospitalist societies could provide training at regional and national conferences to upskill hospitalists to care for people with SUD; support addiction medicine interest groups; and partner with addiction medicine societies, harm reduction organizations, and organizations focused on trauma-informed care. They could endorse practice guidelines and position statements describing the crucial role of hospitalists in addressing the overdose crisis and offering medication for addiction (Table). Hospitalist organizations can engage national and state hospital associations, lobby medical specialties to include addiction medicine competencies in board certification requirements, and advocate with governmental leaders to reduce barriers that restrict treatment access such as the X-waiver.
MOVING FORWARD
Regardless of whether a hospitalist is serving as an individual provider, a hospitalist leader, or as part of a hospitalist organization, hospitalists can take critical steps to advance the care of people with SUD. These steps shift the culture of hospitals from one where patients are afraid to discuss their substance use, to one that creates space for connection, treatment engagement, and healing. By starting medications, utilizing widely accessible resources, and collaborating with community treatment and harm reduction organizations, each one of us can play a part in addressing the epidemic.
Acknowledgments
The authors thank Alisa Patten for help preparing this manuscript. Dr. Englander would like to thank Dr. David Bangsberg and Dr. Christina Nicolaidis for their mentorship.
In 2017, the death toll from drug overdoses reached a record high, killing more Americans than the entire Vietnam War or the HIV/AIDS epidemic at its peak.1 Up to one-quarter of hospitalized patients have a substance use disorder (SUD) and SUD-related2,3 hospitalizations are surging. People with SUD have longer hospital stays, higher costs, and more readmissions.3,4 While the burden of SUD is staggering, it is far from hopeless. There are multiple evidence-based and highly effective interventions to treat SUD, including medications, behavioral interventions, and harm reduction strategies.
Hospitalization can be a reachable moment to initiate and coordinate addictions care.5 Hospital-based addictions care has the potential to engage sicker, highly vulnerable patients, many who are not engaged in primary care or outpatient addictions care.6 Studied effects of hospital-based addictions care include improved SUD treatment engagement, reduced alcohol and drug use, lower hospital readmissions, and improved provider experience.7-9
Most hospitals, however, do not treat SUD during hospitalization and do not connect people to treatment after discharge. Hospitals may lack staffing or financial resources to implement addiction care, may believe that SUDs are an outpatient concern, may want to avoid caring for people with SUD, or may simply not know where to begin. Whatever the reason, unaddressed SUD can lead to untreated withdrawal, disruptive patient behaviors, failure to complete recommended medical therapy, high rates of against medical advice discharge, poor patient experience, and widespread provider distress.8
Hospitalists—individually and collectively—are uniquely positioned to address this gap. By treating addiction effectively and compassionately, hospitalists can engage patients, improve care, improve patient and provider experience, and lower costs. This paper is a call to action that describes the current state of hospital-based addictions care, outlines key challenges to implementing SUD care in the hospital, debunks common misconceptions, and identifies actionable steps for hospitalists, hospital leaders, and hospitalist organizations.
MODELS TO DELIVER HOSPITAL-BASED ADDICTIONS CARE
Hospital-based addiction medicine consult services are emerging; they include a range of models, with variations in how patients are identified, team composition, service availability, and financing.10 Existing addiction medicine consult services commonly offer SUD assessments, psychological intervention, medical management of SUDs (eg, initiating methadone or buprenorphine), medical pain management, and linkage to SUD care after hospitalization. Some services also explicitly integrate harm reduction principles (eg, naloxone distribution, safe injection education, permitting patients to smoke).11 Additional consult service activities include hospital-wide SUD education, and creation and implementation of hospital guidance documents (eg, methadone policies).10 Some consult services utilize only physicians, while others include interprofessional providers, such as nurses, social workers, and peers with lived experience of addiction. Whereas addiction medicine physicians staff some consult services, hospitalists with less formal addiction credentials staff others.
Broadly, hospital-based addictions care cannot depend solely on consult services. Just as not all hospitals have cardiology consult services, not all hospitals will have addiction consult services. As such, hospitalists can play an even greater role by implementing order sets and guidelines, supporting partnerships with community SUD treatment, and independently initiating evidence-based medications.
CHALLENGES TO ADOPTION AND IMPLEMENTATION OF HOSPITAL-BASED ADDICTIONS CARE
Pervasive individual and structural stigmas12 are perhaps the most critical barriers to incorporating addiction medicine into routine hospital practice, and they are both cause and consequence of our system failures. Most medical schools and residencies lack SUD training, which means that the understanding of addiction as a moral deficiency or lack of willpower may remain unchallenged. Stigma surrounding SUDs contributes to hospitalists’ and hospital leaders’ aversion to treating patients with SUD, and to fears that providing quality SUD care will attract patients suffering from these conditions.
Recent national efforts have focused on the problem of opioid overprescribing. Without an equal emphasis on treatment, this focus can lead to undertreatment of pain and/or opioid use disorder in hospitalized patients, particularly since most hospitalists have little to no training in diagnosing SUD, prescribing life-saving medications for opioid use disorder, or managing acute pain in patients with SUD. The focus on overprescribing also diverts attention away from trends involving stimulants,2 fentanyl contamination of the drug supply,13 and alcohol, all of which have important implications for the care of hospitalized adults.
Hospital policies are often not grounded in evidence (eg, recommending clonidine for first-line treatment of opioid withdrawal and not buprenorphine/methadone), and there are widespread misconceptions about perceived legal barriers to treating opioid use disorder in the hospital, which is both safe and legal.10 People with SUD may be unjustly viewed through a criminal justice lens. Policies focused on controlling visitors and conducting room searches disproportionately burden people with SUD, which may create further harms through reinforcing negative provider cognitive biases about SUDs. Finally, hospitals may lack inpatient social work and pharmacy supports, and they rarely have pathways to connect people to SUD care after discharge.
Funding remains a widespread challenge. While some hospital administrators support addiction medicine services because of the pressing medical need and public health crisis, most services depend on billing or demonstrated savings through reduced hospital days or readmissions.
A CALL TO ACTION: HOW HOSPITALISTS CAN IMPROVE ADDICTION CARE
Individual hospitalists, hospitalist leaders, and hospitalist organizations can engage by improving individual practice, driving systems change, and through advocacy and policy change (Table).
Individual Hospitalists
Providing basic addiction medicine care should be a core competency for all hospitalists, just as every hospitalist can initiate a goals-of-care conversation or prescribe insulin. For opioid use disorder, hospitalists should treat withdrawal and offer treatment initiation with opioid agonist therapy (ie, methadone, buprenorphine), which reduces mortality by over half. Commonly, hospitalized patients are subjected to harmful, nonevidence-based treatments, such as mandated rapid methadone tapers,25 which can lead to undertreated withdrawal, increased pain, and opioid cravings. This increases patients’ risk for overdose after discharge and precludes them from receiving life-saving, evidence-based methadone maintenance, or buprenorphine treatment. Though widely misunderstood, prescribing methadone in the hospital is legal, and providers need no special waiver to prescribe buprenorphine during admission. Current laws require that hospitalists have a waiver to prescribe buprenorphine at discharge and prohibit hospitalists (or anyone outside of an opioid treatment program) from prescribing methadone for the treatment of opioid use disorder at discharge. Further, hospitalists should offer medication for alcohol use disorder (eg, naltrexone) and be good stewards of opioids during hospitalization, avoiding intravenous opioids where appropriate and curbing excessive prescribing at discharge. Given high rates of overdose and fentanyl contamination of stimulants, opioids, and benzodiazepines, hospitalists should prescribe naloxone at discharge to every patient with SUD, on chronic opioids, or who uses any nonmedical substances.
Resources exist for individual hospitalists seeking mentorship or additional training (Table). Though not necessary for in-hospital prescribing, hospitalists can obtain a waiver to prescribe buprenorphine at discharge (commonly called the X-waiver). To qualify, physicians must complete eight hours of accredited training (online and/or in-person), after which they must request a waiver from the Drug Enforcement Administration. Advanced-practice practitioners must complete 24 hours of training. Many have argued that policymakers should end this waiver requirement.26 While we support efforts to “X the X” and urgently expand treatment access, additional training can enrich providers’ knowledge and confidence to prescribe buprenorphine, and is a relatively simple way that all hospitalists could act. Finally, by treating addiction and modeling patient-centered addictions care, hospitalists can legitimize and destigmatize the disease of addiction,8 and have the potential to mentor and train students, residents, nurses, and other staff.27
Hospitalist Leaders
As leaders, hospitalists can play a key role in promoting hospital-based addictions care and tailoring solutions to meet local needs. Leaders can promote a cultural shift away from stigma, and promote evidence-based, life-saving care. Hospitalist leaders could require all hospitalists to obtain buprenorphine waivers. Leaders could initiate quality improvement projects related to SUD service delivery, develop policies that support inpatient SUD treatment, develop order sets for medication initiation, engage community substance use treatment partners, build pathways to timely addiction care after discharge, and champion development of addiction medicine consult services.
Hospitalist leaders can reference open-source guidelines, order sets, assessment and treatment tools, patient materials, pharmacy and therapeutics committee materials, and other resources for implementing services for hospitalized patients with SUD (Table).21,22 Hospitalist leaders who understand financial and quality drivers can also champion the business and quality case for hospital-based addictions care, and help pursue local and national funding opportunities.
Hospitalist Organizations
Hospitalist societies could provide training at regional and national conferences to upskill hospitalists to care for people with SUD; support addiction medicine interest groups; and partner with addiction medicine societies, harm reduction organizations, and organizations focused on trauma-informed care. They could endorse practice guidelines and position statements describing the crucial role of hospitalists in addressing the overdose crisis and offering medication for addiction (Table). Hospitalist organizations can engage national and state hospital associations, lobby medical specialties to include addiction medicine competencies in board certification requirements, and advocate with governmental leaders to reduce barriers that restrict treatment access such as the X-waiver.
MOVING FORWARD
Regardless of whether a hospitalist is serving as an individual provider, a hospitalist leader, or as part of a hospitalist organization, hospitalists can take critical steps to advance the care of people with SUD. These steps shift the culture of hospitals from one where patients are afraid to discuss their substance use, to one that creates space for connection, treatment engagement, and healing. By starting medications, utilizing widely accessible resources, and collaborating with community treatment and harm reduction organizations, each one of us can play a part in addressing the epidemic.
Acknowledgments
The authors thank Alisa Patten for help preparing this manuscript. Dr. Englander would like to thank Dr. David Bangsberg and Dr. Christina Nicolaidis for their mentorship.
1. Weiss A, Elixhauser A, Barrett M, Steiner C, Bailey M, O’Malley L. Opioid-related inpatient stays and emergency department visits by state, 2009-2014. Statistical Brief #219. Healthcare Cost and Utilization Project. 2016. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.jsp. Accessed May 21, 2019.
2. Winkelman TA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of amphetamine-related hospitalizations and associated clinical outcomes and costs in the United States. JAMA Netw Open. 2018;1(6):e183758. https://doi.org/10.1001/jamanetworkopen.2018.3758.
3. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424.
4. Walley AY, Paasche-Orlow M, Lee EC, et al. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6(1):50-56. https://doi.org/10.1097/ADM.0b013e318231de51.
5. Englander H, Weimer M, Solotaroff R, et al. Planning and designing the Improving Addiction Care Team (IMPACT) for hospitalized adults with substance use disorder. J Hosp Med. 2017;12(5):339-342. https://doi.org/10.12788/jhm.2736.
6. Velez C, Nicolaidis C, Korthuis P, Englander H. “It’s been an experience, a life learning experience”: a qualitative study of hospitalized patients with substance use disorders. J Gen Intern Med. 2017;32(3):296-303. doi 10.1007/s11606-016-3919-4.
7. Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient addiction consultation for hospitalized patients increases post-discharge abstinence and reduces addiction severity. J Gen Intern Med. 2017;32(8):909-916. https://doi.org/10.1007/s11606-017-4077-z.
8. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993.
9. McQueen J, Howe TE, Allan L, Mains D, Hardy V. Brief interventions for heavy alcohol users admitted to general hospital wards. Cochrane Database Syst Rev. 2011;10(8):CD005191 https://doi.org/10.1002/14651858.CD005191.pub3.
10. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496.
11. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001.
12. McNeil R, Small W, Wood E, Kerr T. Hospitals as a “risk environment”: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010.
13. Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019. pii: S0955-3959(19)30018-0. [Epub ahead of print]. https://doi.org/10.1016/j.drugpo.2019.01.010.
14. Substance Abuse and Mental Health Services Administration. TIP 63: Medications for Opioid Use Disorder-Executive Summary. February 2018. https://store.samhsa.gov/product/TIP-63-Medications-for-Opioid-Use-Disorder-Executive-Summary/sma18-5063exsumm. Accessed August 8, 2019.
15. Providers Clinical Support System. Discover the rewards of treating patients with Opioid Use Disorders. https://pcssnow.org/. Accessed August 8, 2019.
16. California Bridge Program. Treatment Starts Here: Resources for the Treatment of Substance Use Disorders from the Acute Care Setting. https://www.bridgetotreatment.org/resources. Accessed August 7, 2019.
17. Clinical Consultation Center. Substance Use Resources. 2019. https://nccc.ucsf.edu/clinical-resources/substance-use-resources/. Accessed August 8, 2019.
18. Thakarar K, Weinstein ZM, Walley AY. Optimising health and safety of people who inject drugs during transition from acute to outpatient care: narrative review with clinical checklist. Postgrad Med J. 2016;92(1088):356-363. https://doi.org/10.1136/postgradmedj-2015-133720.
19. Office of National Drug Control Policy. Changing the Language of Addiction. Washington, D.C. 2017. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Memo%20-%20Changing%20Federal%20Terminology%20Regrading%20Substance%20Use%20and%20Substance%20Use%20Disorders.pdf. Accessed August 8, 2019.
20. The University of New Mexico. Project ECHO: A Revolution in Medical Education and Care Delivery. 2019. https://echo.unm.edu/. Accessed August 8, 2019.
21. Englander H, Mahoney S, Brandt K, et al. Tools to support hospital-based addiction care: core components, values, and activities of the Improving Addiction Care Team. J Addict Med. 2019;13(2):85-89. https://doi.org/10.1097/ADM.0000000000000487.
22. Englander H, Gregg J, Gollickson J, et al. Recommendations for intergrating peer mentors in hospital-based addiction care. Subst Abus. In press. https://doi.org/10.1080/08897077.2019.1635968.
23. American College of Medical Toxicology. ACMT Position Statement: Buprenorphine Administration in the Emergency Department. https://www.acep.org/globalassets/sites/acep/media/equal-documents/policy_acmt_bupeadministration.pdf. Accessed May 21, 2019.
24. Herzig SJ, Mosher HJ, Calcaterra SL, Jena AB, Nuckols TK. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018;13(4):263-271. https://doi.org/10.12788/jhm.2980.
25. Winetsky D, Weinrieb RM, Perrone J. Expanding treatment opportunities for hospitalized patients with opioid use disorders. J Hosp Med. 2018;13(1):62-64. https://doi.org/10.12788/jhm.2861.
26. Frank JW, Wakeman SE, Gordon AJ. No end to the crisis without an end to the waiver. Subst Abus. 2018;39(3):263-265. https://doi.org/10.1080/08897077.2018.1543382.
27. Gorfinkel L, Klimas J, Reel B, et al. In-hospital training in addiction medicine: a mixed-methods study of health care provider benefits and differences. Subst Abus. 2019. In press. https://doi.org/10.1080/08897077.2018.1561596.
1. Weiss A, Elixhauser A, Barrett M, Steiner C, Bailey M, O’Malley L. Opioid-related inpatient stays and emergency department visits by state, 2009-2014. Statistical Brief #219. Healthcare Cost and Utilization Project. 2016. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.jsp. Accessed May 21, 2019.
2. Winkelman TA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of amphetamine-related hospitalizations and associated clinical outcomes and costs in the United States. JAMA Netw Open. 2018;1(6):e183758. https://doi.org/10.1001/jamanetworkopen.2018.3758.
3. Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Millwood). 2016;35(5):832-837. https://doi.org/10.1377/hlthaff.2015.1424.
4. Walley AY, Paasche-Orlow M, Lee EC, et al. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6(1):50-56. https://doi.org/10.1097/ADM.0b013e318231de51.
5. Englander H, Weimer M, Solotaroff R, et al. Planning and designing the Improving Addiction Care Team (IMPACT) for hospitalized adults with substance use disorder. J Hosp Med. 2017;12(5):339-342. https://doi.org/10.12788/jhm.2736.
6. Velez C, Nicolaidis C, Korthuis P, Englander H. “It’s been an experience, a life learning experience”: a qualitative study of hospitalized patients with substance use disorders. J Gen Intern Med. 2017;32(3):296-303. doi 10.1007/s11606-016-3919-4.
7. Wakeman SE, Metlay JP, Chang Y, Herman GE, Rigotti NA. Inpatient addiction consultation for hospitalized patients increases post-discharge abstinence and reduces addiction severity. J Gen Intern Med. 2017;32(8):909-916. https://doi.org/10.1007/s11606-017-4077-z.
8. Englander H, Collins D, Perry SP, Rabinowitz M, Phoutrides E, Nicolaidis C. “We’ve learned it’s a medical illness, not a moral choice”: qualitative study of the effects of a multicomponent addiction intervention on hospital providers’ attitudes and experiences. J Hosp Med. 2018;13(11):752-758. https://doi.org/10.12788/jhm.2993.
9. McQueen J, Howe TE, Allan L, Mains D, Hardy V. Brief interventions for heavy alcohol users admitted to general hospital wards. Cochrane Database Syst Rev. 2011;10(8):CD005191 https://doi.org/10.1002/14651858.CD005191.pub3.
10. Priest KC, McCarty D. Role of the hospital in the 21st century opioid overdose epidemic: the addiction medicine consult service. J Addict Med. 2019;13(2):104-112. https://doi.org/10.1097/ADM.0000000000000496.
11. Weinstein ZM, Wakeman SE, Nolan S. Inpatient addiction consult service: expertise for hospitalized patients with complex addiction problems. Med Clin North Am. 2018;102(4):587-601. https://doi.org/10.1016/j.mcna.2018.03.001.
12. McNeil R, Small W, Wood E, Kerr T. Hospitals as a “risk environment”: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59-66. https://doi.org/10.1016/j.socscimed.2014.01.010.
13. Ciccarone D. The triple wave epidemic: supply and demand drivers of the US opioid overdose crisis. Int J Drug Policy. 2019. pii: S0955-3959(19)30018-0. [Epub ahead of print]. https://doi.org/10.1016/j.drugpo.2019.01.010.
14. Substance Abuse and Mental Health Services Administration. TIP 63: Medications for Opioid Use Disorder-Executive Summary. February 2018. https://store.samhsa.gov/product/TIP-63-Medications-for-Opioid-Use-Disorder-Executive-Summary/sma18-5063exsumm. Accessed August 8, 2019.
15. Providers Clinical Support System. Discover the rewards of treating patients with Opioid Use Disorders. https://pcssnow.org/. Accessed August 8, 2019.
16. California Bridge Program. Treatment Starts Here: Resources for the Treatment of Substance Use Disorders from the Acute Care Setting. https://www.bridgetotreatment.org/resources. Accessed August 7, 2019.
17. Clinical Consultation Center. Substance Use Resources. 2019. https://nccc.ucsf.edu/clinical-resources/substance-use-resources/. Accessed August 8, 2019.
18. Thakarar K, Weinstein ZM, Walley AY. Optimising health and safety of people who inject drugs during transition from acute to outpatient care: narrative review with clinical checklist. Postgrad Med J. 2016;92(1088):356-363. https://doi.org/10.1136/postgradmedj-2015-133720.
19. Office of National Drug Control Policy. Changing the Language of Addiction. Washington, D.C. 2017. https://www.whitehouse.gov/sites/whitehouse.gov/files/images/Memo%20-%20Changing%20Federal%20Terminology%20Regrading%20Substance%20Use%20and%20Substance%20Use%20Disorders.pdf. Accessed August 8, 2019.
20. The University of New Mexico. Project ECHO: A Revolution in Medical Education and Care Delivery. 2019. https://echo.unm.edu/. Accessed August 8, 2019.
21. Englander H, Mahoney S, Brandt K, et al. Tools to support hospital-based addiction care: core components, values, and activities of the Improving Addiction Care Team. J Addict Med. 2019;13(2):85-89. https://doi.org/10.1097/ADM.0000000000000487.
22. Englander H, Gregg J, Gollickson J, et al. Recommendations for intergrating peer mentors in hospital-based addiction care. Subst Abus. In press. https://doi.org/10.1080/08897077.2019.1635968.
23. American College of Medical Toxicology. ACMT Position Statement: Buprenorphine Administration in the Emergency Department. https://www.acep.org/globalassets/sites/acep/media/equal-documents/policy_acmt_bupeadministration.pdf. Accessed May 21, 2019.
24. Herzig SJ, Mosher HJ, Calcaterra SL, Jena AB, Nuckols TK. Improving the safety of opioid use for acute noncancer pain in hospitalized adults: a consensus statement from the society of hospital medicine. J Hosp Med. 2018;13(4):263-271. https://doi.org/10.12788/jhm.2980.
25. Winetsky D, Weinrieb RM, Perrone J. Expanding treatment opportunities for hospitalized patients with opioid use disorders. J Hosp Med. 2018;13(1):62-64. https://doi.org/10.12788/jhm.2861.
26. Frank JW, Wakeman SE, Gordon AJ. No end to the crisis without an end to the waiver. Subst Abus. 2018;39(3):263-265. https://doi.org/10.1080/08897077.2018.1543382.
27. Gorfinkel L, Klimas J, Reel B, et al. In-hospital training in addiction medicine: a mixed-methods study of health care provider benefits and differences. Subst Abus. 2019. In press. https://doi.org/10.1080/08897077.2018.1561596.
© 2020 Society of Hospital Medicine
Things We Do for No Reason™: Discontinuing Buprenorphine When Treating Acute Pain

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR™) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR™ series do not represent “black and white” conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 40-year-old woman with a history of opioid use disorder (OUD) on buprenorphine-naloxone treatment is admitted to medicine following incision and drainage of a large forearm abscess with surrounding cellulitis. The patient reports severe pain following the procedure, which is not relieved by ibuprofen. The admitting hospitalist orders a pain regimen for the patient, which includes oral and intravenous hydromorphone and discontinues the patient’s buprenorphine-naloxone so that the short-acting opioids can take effect.
BACKGROUND
Medications to treat OUD include methadone, buprenorphine, and extended-release naltrexone. Buprenorphine is a Schedule III medication under the United States Food and Drug Administration that reduces opioid cravings, subsequently decreasing drug use1 and opioid-related overdose deaths.2 It has a favorable safety profile and can be prescribed for OUD in an office-based, outpatient setting since the Drug Addiction Treatment Act of 2000 (DATA 2000). Due to extensive first-pass metabolism, buprenorphine for OUD is typically administered sublingually, either alone or in a fixed combination with naloxone.
WHY YOU MIGHT THINK YOU SHOULD HOLD BUPRENORPHINE WHEN TREATING ACUTE PAIN
Buprenorphine is a partial opioid agonist with a long half-life and high affinity for the mu opioid receptor. Given these properties, prior recommendations assumed that buprenorphine blocked the effectiveness of additional opioid agonists.3,4 In 2004, guidelines by the Department of Health and Human Service Center for Substance Abuse Treatment recommended discontinuing buprenorphine in patients taking opioid pain medications.5 These suggestions were based on limited case reports describing difficulty controlling pain in patients with OUD with a high opioid tolerance who were receiving buprenorphine.6
Providers may hold buprenorphine when treating acute pain out of concern it could precipitate withdrawal by displacing full opioid agonists from the mu receptor. Providers may also believe that the naloxone component in the most commonly prescribed formulation, buprenorphine-naloxone, blocks the effects of opioid analgesics. Evolving understanding of buprenorphine pharmacology and the absence of high-quality evidence has resulted in providers holding buprenorphine in the setting of acute pain.
Finally, providers without dedicated training may feel they lack the necessary qualifications to prescribe buprenorphine in the inpatient setting. DATA 2000 requires mandatory X waiver training for physicians, nurse practitioners, and physician assistants to prescribe outpatient buprenorphine for OUD treatment outside of specialized opioid treatment programs.
WHY DISCONTINUING BUPRENORPHINE WHEN TREATING ACUTE PAIN IS NOT NECESSARY
Despite buprenorphine’s high affinity at the mu receptor, additional receptors remain available for full opioid agonists to bind and activate,6 providing effective pain relief even in patients using buprenorphine. In contrast to the 2004 Department of Health and Human Service guidelines, subsequent clinical studies have demonstrated that concurrent use of opioid analgesics is effective for patients maintained on buprenorphine, similar to patients on other forms of OUD treatment such as methadone.7,8
Precipitated withdrawal only occurs when buprenorphine is newly introduced to patients with already circulating opioids. Patients receiving buprenorphine-naloxone can also be exposed to opioids without precipitated withdrawal from the naloxone component, as naloxone is not absorbed via sublingual or buccal administration, but only present in the formulation to dissuade intravenous administration of the medication.
Even in the perioperative period, there is insufficient evidence to support the discontinuation of buprenorphine.9 Studies in this patient population have found that patients receiving buprenorphine may require higher doses of short-acting opioids to achieve adequate analgesia, but they experience similar pain control, lengths of stay, and functional outcomes to controls.10 Despite variable perioperative management of buprenorphine,11 protocols at major medical centers now recommend continuing or dose adjusting buprenorphine in the perioperative period rather than discontinuing.12-14
Patients physically dependent on opioid agonists, including buprenorphine, must be maintained on a daily equivalent opioid dose to avoid experiencing withdrawal. This maintenance requirement must be met before any analgesic effect for acute pain is obtained with additional opioids. Temporarily discontinuing buprenorphine introduces unnecessary complexity to a hospitalization, places the patient at risk of exacerbation of pain, opioid withdrawal, and predisposes the patient to return to use and overdose if not resumed before hospital discharge.5
Finally, clinicians do not require additional training or an X waiver to administer buprenorphine to hospitalized patients. These requirements are limited to providers managing buprenorphine in the outpatient setting or those prescribing buprenorphine to patients to take postdischarge. Hospitalists frequently prescribe opioid medications in the inpatient setting with similar or greater safety risk profiles to buprenorphine.
WHEN YOU SHOULD CONSIDER HOLDING BUPRENORPHINE
Providers may consider holding buprenorphine if a patient with OUD has not been taking buprenorphine before hospitalization and has severe acute pain needs. This history can be confirmed with the patient and the state’s online prescription drug monitoring program. If further clarification is needed, this can be accomplished with a pharmacist and urine testing or by verifying with the patient’s opioid treatment program, as some programs provide directly administered buprenorphine.
In cases where a patient may have stopped buprenorphine before admission but wants to restart it in the hospital, it is essential to ascertain when the patient last used an opioid. The buprenorphine reinduction should be timed to a sufficient number of hours since last opioid use and/or to when the patient shows signs of active withdrawal. The re-induction can take place before, during, or after an acute pain episode, depending on the individual circumstances.
Patient preference is extremely important in the management of both pain and OUD. After shared decision-making, some patients may ultimately opt to hold buprenorphine in certain situations or switch to an alternative treatment, such as methadone, during their hospitalization. Such adjustments should be made in conjunction with the patient, primary care provider, and pain or addiction medicine specialty consultation.
WHAT YOU SHOULD DO INSTEAD
For patients on buprenorphine admitted to the hospital with anticipated or unanticipated acute pain needs, hospitalists should continue buprenorphine. Continuation of buprenorphine meets a patient’s baseline opioid requirement while still allowing the use of additional short-acting opioid agonists as needed for pain.15
As with all pain, multimodal pain management should be provided with adjunctive medications such as acetaminophen, nonsteroidal anti-inflammatory drugs, neuropathic agents, topical analgesics, and regional anesthesia.8
Acute pain can be addressed by taking advantage of buprenorphine’s analgesic effects and adding additional short-acting opioids if needed.15 Several options are available, including:
1. Continuing daily buprenorphine and prescribing short-acting opioid agonists, preferably those with high intrinsic activity at the mu receptor (such as morphine, fentanyl, or hydromorphone). Full opioid agonist doses to achieve analgesia for patients on buprenorphine will be higher than in opioid naïve patients due to tolerance.16
2 .Dividing the total daily buprenorphine dose into three or four times per day dosing, since buprenorphine provides an analgesic effect lasting six to eight hours. Short-acting opioid agonists can still be prescribed on an as-needed basis for additional pain needs.
3. Temporarily increasing the total daily buprenorphine dose and dividing into three or four times per day dosing, as above. Short-acting opioid agonists can still be prescribed on an as-needed basis for additional pain needs.
It is essential to make a clear plan with the patient for initiation and discontinuation of short-acting opioid agonists or buprenorphine changes. Patients on buprenorphine should be managed collaboratively with the primary care provider or addiction specialist to coordinate prescribing and follow-up after discharge.
RECOMMENDATIONS
- Continue outpatient buprenorphine treatment for patients admitted with acute pain.
- Use adjunctive nonopioid pain medications and nonpharmacologic modalities to address acute pain.
- Adjust buprenorphine to address acute pain by dividing the total daily amount into three or four times a day dosing, and/or up-titrate the buprenorphine dose (federal prescribing regulations recommend a maximum of 24 mg daily, but state regulations may vary).
- Add short-acting opioid agonists on an as-needed basis in conjunction with a defined plan to discontinue short-acting opioid agonists to avoid a return to use.
- Make plans collaboratively with the patient and outpatient provider, and communicate medication changes and plan at discharge.
CONCLUSION
Concerning our case, the hospitalist can continue the patient’s buprenorphine-naloxone, even with her acute pain needs. The patient has a baseline opioid requirement, fulfilled by continuing buprenorphine. Additional short-acting opioid agonists, such as hydromorphone, will provide analgesia for the patient, though the clinician should be aware that higher doses might be required. The practice of holding buprenorphine during episodes of acute pain is not supported by current evidence and may predispose to inadequate analgesia, opioid withdrawal, and risk of return to use and death.2
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Disclosures
The authors report no conflicts of interest.
1. Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;(3):CD002207. https://doi.org/10.1002/14651858.CD002207.
2. Sordo L, Barrio G, Bravo M, et al. Morality risk during and after opioid substitution treatment: systemic review and meta-analysis of cohort studies. BMJ. 2017;357:1550. https://doi.org/10.1136/bmj.j1550.
3. Johnson RE, Fudula PJ, Payne R. Buprenorphine: considerations for pain management. J Pain Symptom Manage. 2005;29(3):297-326. https://doi.org/10.1016/j.jpainsymman.2004.07.005.
4. Marcelina JS, Rubinstein A. Continuous perioperative sublingual buprenorphine. J Pain Palliat Care Pharmacother. 2016;30(4):289-293. https://doi.org/10.1080/15360288.2016.1231734.
5. Greenwald MK, Johanson CE, Moody DE, et al. Effects of buprenorphine maintenance dose on mu-opioid receptor binding potential, plasma concentration and antagonist blockade in heroin-dependent volunteers. Neuropsychopharmacology. 2003;28(11):2000-2009. https://doi.org/10.1038/sj.npp.1300251.
6. Lembke A, Ottestad E, Schmiesing C. Patients maintained on buprenorphine for opioid use disorder should continue buprenorphine through the perioperative period. Pain Med. 2019;20(3):425-428. https://doi.org/10.1093/pm/pny019.
7. Kornfeld H, Manfredi L. Effectiveness of full agonist opioids in patients stabilized on buprenorphine undergoing major surgery: A case series. Am J Ther. 2010;17(5):523-528. https://doi.org/10.1097/MJT.0b013e3181be0804.
8. Harrison TK, Kornfeld H, Aggarwal AK, Lembke A. Perioperative considerations for the patient with opioid use disorder on buprenorphine, methadone, or naltrexone maintenance therapy. Anesthesiol Clin. 2018;36(3):345-359. https://doi.org/10.1016/j.anclin.2018.04.002.
9. Goel A, Azargive S, Lamba W, et al. The perioperative patient on buprenorphine: a systematic review of perioperative management strategies and patient outcomes. Can J Anesth. 2019; 66(2):201-217. https://doi.org/10.1007/s12630-018-1255-3.
10. Hansen LE, Stone GL, Matson CA, Tybor DJ, Pevear ME, Smith EL. Total joint arthroplasty in patients taking methadone or buprenorphine/naloxone preoperatively for prior heroin addiction: a prospective matched cohort study. J Arthroplasty. 2016;31(8):1698-1701. https://doi.org/10.1016/j.arth.2016.01.032.
11. Jonan AB, Kaye AD, Urman RD. Buprenorphine formulations: clinical best practice strategies recommendations for perioperative management of patients undergoing surgical or interventional pain procedures. Pain Physician. 2018;21(1):E1-12. PubMed
12. Quaye AN, Zhang Y. Perioperative management of buprenorphine: solving the conundrum. Pain Med. 2018. https://doi.org/10.1093/pm/pny217.
13. Silva MJ, Rubinstein A. Continuous perioperative sublingual buprenorphine. J Pain Palliative Care Pharmacother. 2016;30(4):289-293. https://doi.org/10.1080/15360288.2016.1231734.
14. Kampman K, Jarvis M. ASAM National practice guidelines for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358-367. https://doi.org/10.1097/ADM.0000000000000166.
15. Childers JW, Arnold RM. Treatment of pain in patients taking buprenorphine for opioid addiction. J Palliat Med. 2012;15(5):613-614. https://doi.org/10.1089/jpm.2012.9591.
16. Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med. 2006;144(2):127-134. https://doi.org/10.7326/0003-4819-144-2-200601170-00010

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR™) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR™ series do not represent “black and white” conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 40-year-old woman with a history of opioid use disorder (OUD) on buprenorphine-naloxone treatment is admitted to medicine following incision and drainage of a large forearm abscess with surrounding cellulitis. The patient reports severe pain following the procedure, which is not relieved by ibuprofen. The admitting hospitalist orders a pain regimen for the patient, which includes oral and intravenous hydromorphone and discontinues the patient’s buprenorphine-naloxone so that the short-acting opioids can take effect.
BACKGROUND
Medications to treat OUD include methadone, buprenorphine, and extended-release naltrexone. Buprenorphine is a Schedule III medication under the United States Food and Drug Administration that reduces opioid cravings, subsequently decreasing drug use1 and opioid-related overdose deaths.2 It has a favorable safety profile and can be prescribed for OUD in an office-based, outpatient setting since the Drug Addiction Treatment Act of 2000 (DATA 2000). Due to extensive first-pass metabolism, buprenorphine for OUD is typically administered sublingually, either alone or in a fixed combination with naloxone.
WHY YOU MIGHT THINK YOU SHOULD HOLD BUPRENORPHINE WHEN TREATING ACUTE PAIN
Buprenorphine is a partial opioid agonist with a long half-life and high affinity for the mu opioid receptor. Given these properties, prior recommendations assumed that buprenorphine blocked the effectiveness of additional opioid agonists.3,4 In 2004, guidelines by the Department of Health and Human Service Center for Substance Abuse Treatment recommended discontinuing buprenorphine in patients taking opioid pain medications.5 These suggestions were based on limited case reports describing difficulty controlling pain in patients with OUD with a high opioid tolerance who were receiving buprenorphine.6
Providers may hold buprenorphine when treating acute pain out of concern it could precipitate withdrawal by displacing full opioid agonists from the mu receptor. Providers may also believe that the naloxone component in the most commonly prescribed formulation, buprenorphine-naloxone, blocks the effects of opioid analgesics. Evolving understanding of buprenorphine pharmacology and the absence of high-quality evidence has resulted in providers holding buprenorphine in the setting of acute pain.
Finally, providers without dedicated training may feel they lack the necessary qualifications to prescribe buprenorphine in the inpatient setting. DATA 2000 requires mandatory X waiver training for physicians, nurse practitioners, and physician assistants to prescribe outpatient buprenorphine for OUD treatment outside of specialized opioid treatment programs.
WHY DISCONTINUING BUPRENORPHINE WHEN TREATING ACUTE PAIN IS NOT NECESSARY
Despite buprenorphine’s high affinity at the mu receptor, additional receptors remain available for full opioid agonists to bind and activate,6 providing effective pain relief even in patients using buprenorphine. In contrast to the 2004 Department of Health and Human Service guidelines, subsequent clinical studies have demonstrated that concurrent use of opioid analgesics is effective for patients maintained on buprenorphine, similar to patients on other forms of OUD treatment such as methadone.7,8
Precipitated withdrawal only occurs when buprenorphine is newly introduced to patients with already circulating opioids. Patients receiving buprenorphine-naloxone can also be exposed to opioids without precipitated withdrawal from the naloxone component, as naloxone is not absorbed via sublingual or buccal administration, but only present in the formulation to dissuade intravenous administration of the medication.
Even in the perioperative period, there is insufficient evidence to support the discontinuation of buprenorphine.9 Studies in this patient population have found that patients receiving buprenorphine may require higher doses of short-acting opioids to achieve adequate analgesia, but they experience similar pain control, lengths of stay, and functional outcomes to controls.10 Despite variable perioperative management of buprenorphine,11 protocols at major medical centers now recommend continuing or dose adjusting buprenorphine in the perioperative period rather than discontinuing.12-14
Patients physically dependent on opioid agonists, including buprenorphine, must be maintained on a daily equivalent opioid dose to avoid experiencing withdrawal. This maintenance requirement must be met before any analgesic effect for acute pain is obtained with additional opioids. Temporarily discontinuing buprenorphine introduces unnecessary complexity to a hospitalization, places the patient at risk of exacerbation of pain, opioid withdrawal, and predisposes the patient to return to use and overdose if not resumed before hospital discharge.5
Finally, clinicians do not require additional training or an X waiver to administer buprenorphine to hospitalized patients. These requirements are limited to providers managing buprenorphine in the outpatient setting or those prescribing buprenorphine to patients to take postdischarge. Hospitalists frequently prescribe opioid medications in the inpatient setting with similar or greater safety risk profiles to buprenorphine.
WHEN YOU SHOULD CONSIDER HOLDING BUPRENORPHINE
Providers may consider holding buprenorphine if a patient with OUD has not been taking buprenorphine before hospitalization and has severe acute pain needs. This history can be confirmed with the patient and the state’s online prescription drug monitoring program. If further clarification is needed, this can be accomplished with a pharmacist and urine testing or by verifying with the patient’s opioid treatment program, as some programs provide directly administered buprenorphine.
In cases where a patient may have stopped buprenorphine before admission but wants to restart it in the hospital, it is essential to ascertain when the patient last used an opioid. The buprenorphine reinduction should be timed to a sufficient number of hours since last opioid use and/or to when the patient shows signs of active withdrawal. The re-induction can take place before, during, or after an acute pain episode, depending on the individual circumstances.
Patient preference is extremely important in the management of both pain and OUD. After shared decision-making, some patients may ultimately opt to hold buprenorphine in certain situations or switch to an alternative treatment, such as methadone, during their hospitalization. Such adjustments should be made in conjunction with the patient, primary care provider, and pain or addiction medicine specialty consultation.
WHAT YOU SHOULD DO INSTEAD
For patients on buprenorphine admitted to the hospital with anticipated or unanticipated acute pain needs, hospitalists should continue buprenorphine. Continuation of buprenorphine meets a patient’s baseline opioid requirement while still allowing the use of additional short-acting opioid agonists as needed for pain.15
As with all pain, multimodal pain management should be provided with adjunctive medications such as acetaminophen, nonsteroidal anti-inflammatory drugs, neuropathic agents, topical analgesics, and regional anesthesia.8
Acute pain can be addressed by taking advantage of buprenorphine’s analgesic effects and adding additional short-acting opioids if needed.15 Several options are available, including:
1. Continuing daily buprenorphine and prescribing short-acting opioid agonists, preferably those with high intrinsic activity at the mu receptor (such as morphine, fentanyl, or hydromorphone). Full opioid agonist doses to achieve analgesia for patients on buprenorphine will be higher than in opioid naïve patients due to tolerance.16
2 .Dividing the total daily buprenorphine dose into three or four times per day dosing, since buprenorphine provides an analgesic effect lasting six to eight hours. Short-acting opioid agonists can still be prescribed on an as-needed basis for additional pain needs.
3. Temporarily increasing the total daily buprenorphine dose and dividing into three or four times per day dosing, as above. Short-acting opioid agonists can still be prescribed on an as-needed basis for additional pain needs.
It is essential to make a clear plan with the patient for initiation and discontinuation of short-acting opioid agonists or buprenorphine changes. Patients on buprenorphine should be managed collaboratively with the primary care provider or addiction specialist to coordinate prescribing and follow-up after discharge.
RECOMMENDATIONS
- Continue outpatient buprenorphine treatment for patients admitted with acute pain.
- Use adjunctive nonopioid pain medications and nonpharmacologic modalities to address acute pain.
- Adjust buprenorphine to address acute pain by dividing the total daily amount into three or four times a day dosing, and/or up-titrate the buprenorphine dose (federal prescribing regulations recommend a maximum of 24 mg daily, but state regulations may vary).
- Add short-acting opioid agonists on an as-needed basis in conjunction with a defined plan to discontinue short-acting opioid agonists to avoid a return to use.
- Make plans collaboratively with the patient and outpatient provider, and communicate medication changes and plan at discharge.
CONCLUSION
Concerning our case, the hospitalist can continue the patient’s buprenorphine-naloxone, even with her acute pain needs. The patient has a baseline opioid requirement, fulfilled by continuing buprenorphine. Additional short-acting opioid agonists, such as hydromorphone, will provide analgesia for the patient, though the clinician should be aware that higher doses might be required. The practice of holding buprenorphine during episodes of acute pain is not supported by current evidence and may predispose to inadequate analgesia, opioid withdrawal, and risk of return to use and death.2
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Disclosures
The authors report no conflicts of interest.

Inspired by the ABIM Foundation’s Choosing Wisely® campaign, the “Things We Do for No Reason™” (TWDFNR™) series reviews practices that have become common parts of hospital care but may provide little value to our patients. Practices reviewed in the TWDFNR™ series do not represent “black and white” conclusions or clinical practice standards but are meant as a starting place for research and active discussions among hospitalists and patients. We invite you to be part of that discussion.
CLINICAL SCENARIO
A 40-year-old woman with a history of opioid use disorder (OUD) on buprenorphine-naloxone treatment is admitted to medicine following incision and drainage of a large forearm abscess with surrounding cellulitis. The patient reports severe pain following the procedure, which is not relieved by ibuprofen. The admitting hospitalist orders a pain regimen for the patient, which includes oral and intravenous hydromorphone and discontinues the patient’s buprenorphine-naloxone so that the short-acting opioids can take effect.
BACKGROUND
Medications to treat OUD include methadone, buprenorphine, and extended-release naltrexone. Buprenorphine is a Schedule III medication under the United States Food and Drug Administration that reduces opioid cravings, subsequently decreasing drug use1 and opioid-related overdose deaths.2 It has a favorable safety profile and can be prescribed for OUD in an office-based, outpatient setting since the Drug Addiction Treatment Act of 2000 (DATA 2000). Due to extensive first-pass metabolism, buprenorphine for OUD is typically administered sublingually, either alone or in a fixed combination with naloxone.
WHY YOU MIGHT THINK YOU SHOULD HOLD BUPRENORPHINE WHEN TREATING ACUTE PAIN
Buprenorphine is a partial opioid agonist with a long half-life and high affinity for the mu opioid receptor. Given these properties, prior recommendations assumed that buprenorphine blocked the effectiveness of additional opioid agonists.3,4 In 2004, guidelines by the Department of Health and Human Service Center for Substance Abuse Treatment recommended discontinuing buprenorphine in patients taking opioid pain medications.5 These suggestions were based on limited case reports describing difficulty controlling pain in patients with OUD with a high opioid tolerance who were receiving buprenorphine.6
Providers may hold buprenorphine when treating acute pain out of concern it could precipitate withdrawal by displacing full opioid agonists from the mu receptor. Providers may also believe that the naloxone component in the most commonly prescribed formulation, buprenorphine-naloxone, blocks the effects of opioid analgesics. Evolving understanding of buprenorphine pharmacology and the absence of high-quality evidence has resulted in providers holding buprenorphine in the setting of acute pain.
Finally, providers without dedicated training may feel they lack the necessary qualifications to prescribe buprenorphine in the inpatient setting. DATA 2000 requires mandatory X waiver training for physicians, nurse practitioners, and physician assistants to prescribe outpatient buprenorphine for OUD treatment outside of specialized opioid treatment programs.
WHY DISCONTINUING BUPRENORPHINE WHEN TREATING ACUTE PAIN IS NOT NECESSARY
Despite buprenorphine’s high affinity at the mu receptor, additional receptors remain available for full opioid agonists to bind and activate,6 providing effective pain relief even in patients using buprenorphine. In contrast to the 2004 Department of Health and Human Service guidelines, subsequent clinical studies have demonstrated that concurrent use of opioid analgesics is effective for patients maintained on buprenorphine, similar to patients on other forms of OUD treatment such as methadone.7,8
Precipitated withdrawal only occurs when buprenorphine is newly introduced to patients with already circulating opioids. Patients receiving buprenorphine-naloxone can also be exposed to opioids without precipitated withdrawal from the naloxone component, as naloxone is not absorbed via sublingual or buccal administration, but only present in the formulation to dissuade intravenous administration of the medication.
Even in the perioperative period, there is insufficient evidence to support the discontinuation of buprenorphine.9 Studies in this patient population have found that patients receiving buprenorphine may require higher doses of short-acting opioids to achieve adequate analgesia, but they experience similar pain control, lengths of stay, and functional outcomes to controls.10 Despite variable perioperative management of buprenorphine,11 protocols at major medical centers now recommend continuing or dose adjusting buprenorphine in the perioperative period rather than discontinuing.12-14
Patients physically dependent on opioid agonists, including buprenorphine, must be maintained on a daily equivalent opioid dose to avoid experiencing withdrawal. This maintenance requirement must be met before any analgesic effect for acute pain is obtained with additional opioids. Temporarily discontinuing buprenorphine introduces unnecessary complexity to a hospitalization, places the patient at risk of exacerbation of pain, opioid withdrawal, and predisposes the patient to return to use and overdose if not resumed before hospital discharge.5
Finally, clinicians do not require additional training or an X waiver to administer buprenorphine to hospitalized patients. These requirements are limited to providers managing buprenorphine in the outpatient setting or those prescribing buprenorphine to patients to take postdischarge. Hospitalists frequently prescribe opioid medications in the inpatient setting with similar or greater safety risk profiles to buprenorphine.
WHEN YOU SHOULD CONSIDER HOLDING BUPRENORPHINE
Providers may consider holding buprenorphine if a patient with OUD has not been taking buprenorphine before hospitalization and has severe acute pain needs. This history can be confirmed with the patient and the state’s online prescription drug monitoring program. If further clarification is needed, this can be accomplished with a pharmacist and urine testing or by verifying with the patient’s opioid treatment program, as some programs provide directly administered buprenorphine.
In cases where a patient may have stopped buprenorphine before admission but wants to restart it in the hospital, it is essential to ascertain when the patient last used an opioid. The buprenorphine reinduction should be timed to a sufficient number of hours since last opioid use and/or to when the patient shows signs of active withdrawal. The re-induction can take place before, during, or after an acute pain episode, depending on the individual circumstances.
Patient preference is extremely important in the management of both pain and OUD. After shared decision-making, some patients may ultimately opt to hold buprenorphine in certain situations or switch to an alternative treatment, such as methadone, during their hospitalization. Such adjustments should be made in conjunction with the patient, primary care provider, and pain or addiction medicine specialty consultation.
WHAT YOU SHOULD DO INSTEAD
For patients on buprenorphine admitted to the hospital with anticipated or unanticipated acute pain needs, hospitalists should continue buprenorphine. Continuation of buprenorphine meets a patient’s baseline opioid requirement while still allowing the use of additional short-acting opioid agonists as needed for pain.15
As with all pain, multimodal pain management should be provided with adjunctive medications such as acetaminophen, nonsteroidal anti-inflammatory drugs, neuropathic agents, topical analgesics, and regional anesthesia.8
Acute pain can be addressed by taking advantage of buprenorphine’s analgesic effects and adding additional short-acting opioids if needed.15 Several options are available, including:
1. Continuing daily buprenorphine and prescribing short-acting opioid agonists, preferably those with high intrinsic activity at the mu receptor (such as morphine, fentanyl, or hydromorphone). Full opioid agonist doses to achieve analgesia for patients on buprenorphine will be higher than in opioid naïve patients due to tolerance.16
2 .Dividing the total daily buprenorphine dose into three or four times per day dosing, since buprenorphine provides an analgesic effect lasting six to eight hours. Short-acting opioid agonists can still be prescribed on an as-needed basis for additional pain needs.
3. Temporarily increasing the total daily buprenorphine dose and dividing into three or four times per day dosing, as above. Short-acting opioid agonists can still be prescribed on an as-needed basis for additional pain needs.
It is essential to make a clear plan with the patient for initiation and discontinuation of short-acting opioid agonists or buprenorphine changes. Patients on buprenorphine should be managed collaboratively with the primary care provider or addiction specialist to coordinate prescribing and follow-up after discharge.
RECOMMENDATIONS
- Continue outpatient buprenorphine treatment for patients admitted with acute pain.
- Use adjunctive nonopioid pain medications and nonpharmacologic modalities to address acute pain.
- Adjust buprenorphine to address acute pain by dividing the total daily amount into three or four times a day dosing, and/or up-titrate the buprenorphine dose (federal prescribing regulations recommend a maximum of 24 mg daily, but state regulations may vary).
- Add short-acting opioid agonists on an as-needed basis in conjunction with a defined plan to discontinue short-acting opioid agonists to avoid a return to use.
- Make plans collaboratively with the patient and outpatient provider, and communicate medication changes and plan at discharge.
CONCLUSION
Concerning our case, the hospitalist can continue the patient’s buprenorphine-naloxone, even with her acute pain needs. The patient has a baseline opioid requirement, fulfilled by continuing buprenorphine. Additional short-acting opioid agonists, such as hydromorphone, will provide analgesia for the patient, though the clinician should be aware that higher doses might be required. The practice of holding buprenorphine during episodes of acute pain is not supported by current evidence and may predispose to inadequate analgesia, opioid withdrawal, and risk of return to use and death.2
Do you think this is a low-value practice? Is this truly a “Thing We Do for No Reason™?” Share what you do in your practice and join in the conversation online by retweeting it on Twitter (#TWDFNR) and liking it on Facebook. We invite you to propose ideas for other “Things We Do for No Reason™” topics by emailing TWDFNR@hospitalmedicine.org.
Disclosures
The authors report no conflicts of interest.
1. Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;(3):CD002207. https://doi.org/10.1002/14651858.CD002207.
2. Sordo L, Barrio G, Bravo M, et al. Morality risk during and after opioid substitution treatment: systemic review and meta-analysis of cohort studies. BMJ. 2017;357:1550. https://doi.org/10.1136/bmj.j1550.
3. Johnson RE, Fudula PJ, Payne R. Buprenorphine: considerations for pain management. J Pain Symptom Manage. 2005;29(3):297-326. https://doi.org/10.1016/j.jpainsymman.2004.07.005.
4. Marcelina JS, Rubinstein A. Continuous perioperative sublingual buprenorphine. J Pain Palliat Care Pharmacother. 2016;30(4):289-293. https://doi.org/10.1080/15360288.2016.1231734.
5. Greenwald MK, Johanson CE, Moody DE, et al. Effects of buprenorphine maintenance dose on mu-opioid receptor binding potential, plasma concentration and antagonist blockade in heroin-dependent volunteers. Neuropsychopharmacology. 2003;28(11):2000-2009. https://doi.org/10.1038/sj.npp.1300251.
6. Lembke A, Ottestad E, Schmiesing C. Patients maintained on buprenorphine for opioid use disorder should continue buprenorphine through the perioperative period. Pain Med. 2019;20(3):425-428. https://doi.org/10.1093/pm/pny019.
7. Kornfeld H, Manfredi L. Effectiveness of full agonist opioids in patients stabilized on buprenorphine undergoing major surgery: A case series. Am J Ther. 2010;17(5):523-528. https://doi.org/10.1097/MJT.0b013e3181be0804.
8. Harrison TK, Kornfeld H, Aggarwal AK, Lembke A. Perioperative considerations for the patient with opioid use disorder on buprenorphine, methadone, or naltrexone maintenance therapy. Anesthesiol Clin. 2018;36(3):345-359. https://doi.org/10.1016/j.anclin.2018.04.002.
9. Goel A, Azargive S, Lamba W, et al. The perioperative patient on buprenorphine: a systematic review of perioperative management strategies and patient outcomes. Can J Anesth. 2019; 66(2):201-217. https://doi.org/10.1007/s12630-018-1255-3.
10. Hansen LE, Stone GL, Matson CA, Tybor DJ, Pevear ME, Smith EL. Total joint arthroplasty in patients taking methadone or buprenorphine/naloxone preoperatively for prior heroin addiction: a prospective matched cohort study. J Arthroplasty. 2016;31(8):1698-1701. https://doi.org/10.1016/j.arth.2016.01.032.
11. Jonan AB, Kaye AD, Urman RD. Buprenorphine formulations: clinical best practice strategies recommendations for perioperative management of patients undergoing surgical or interventional pain procedures. Pain Physician. 2018;21(1):E1-12. PubMed
12. Quaye AN, Zhang Y. Perioperative management of buprenorphine: solving the conundrum. Pain Med. 2018. https://doi.org/10.1093/pm/pny217.
13. Silva MJ, Rubinstein A. Continuous perioperative sublingual buprenorphine. J Pain Palliative Care Pharmacother. 2016;30(4):289-293. https://doi.org/10.1080/15360288.2016.1231734.
14. Kampman K, Jarvis M. ASAM National practice guidelines for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358-367. https://doi.org/10.1097/ADM.0000000000000166.
15. Childers JW, Arnold RM. Treatment of pain in patients taking buprenorphine for opioid addiction. J Palliat Med. 2012;15(5):613-614. https://doi.org/10.1089/jpm.2012.9591.
16. Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med. 2006;144(2):127-134. https://doi.org/10.7326/0003-4819-144-2-200601170-00010
1. Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;(3):CD002207. https://doi.org/10.1002/14651858.CD002207.
2. Sordo L, Barrio G, Bravo M, et al. Morality risk during and after opioid substitution treatment: systemic review and meta-analysis of cohort studies. BMJ. 2017;357:1550. https://doi.org/10.1136/bmj.j1550.
3. Johnson RE, Fudula PJ, Payne R. Buprenorphine: considerations for pain management. J Pain Symptom Manage. 2005;29(3):297-326. https://doi.org/10.1016/j.jpainsymman.2004.07.005.
4. Marcelina JS, Rubinstein A. Continuous perioperative sublingual buprenorphine. J Pain Palliat Care Pharmacother. 2016;30(4):289-293. https://doi.org/10.1080/15360288.2016.1231734.
5. Greenwald MK, Johanson CE, Moody DE, et al. Effects of buprenorphine maintenance dose on mu-opioid receptor binding potential, plasma concentration and antagonist blockade in heroin-dependent volunteers. Neuropsychopharmacology. 2003;28(11):2000-2009. https://doi.org/10.1038/sj.npp.1300251.
6. Lembke A, Ottestad E, Schmiesing C. Patients maintained on buprenorphine for opioid use disorder should continue buprenorphine through the perioperative period. Pain Med. 2019;20(3):425-428. https://doi.org/10.1093/pm/pny019.
7. Kornfeld H, Manfredi L. Effectiveness of full agonist opioids in patients stabilized on buprenorphine undergoing major surgery: A case series. Am J Ther. 2010;17(5):523-528. https://doi.org/10.1097/MJT.0b013e3181be0804.
8. Harrison TK, Kornfeld H, Aggarwal AK, Lembke A. Perioperative considerations for the patient with opioid use disorder on buprenorphine, methadone, or naltrexone maintenance therapy. Anesthesiol Clin. 2018;36(3):345-359. https://doi.org/10.1016/j.anclin.2018.04.002.
9. Goel A, Azargive S, Lamba W, et al. The perioperative patient on buprenorphine: a systematic review of perioperative management strategies and patient outcomes. Can J Anesth. 2019; 66(2):201-217. https://doi.org/10.1007/s12630-018-1255-3.
10. Hansen LE, Stone GL, Matson CA, Tybor DJ, Pevear ME, Smith EL. Total joint arthroplasty in patients taking methadone or buprenorphine/naloxone preoperatively for prior heroin addiction: a prospective matched cohort study. J Arthroplasty. 2016;31(8):1698-1701. https://doi.org/10.1016/j.arth.2016.01.032.
11. Jonan AB, Kaye AD, Urman RD. Buprenorphine formulations: clinical best practice strategies recommendations for perioperative management of patients undergoing surgical or interventional pain procedures. Pain Physician. 2018;21(1):E1-12. PubMed
12. Quaye AN, Zhang Y. Perioperative management of buprenorphine: solving the conundrum. Pain Med. 2018. https://doi.org/10.1093/pm/pny217.
13. Silva MJ, Rubinstein A. Continuous perioperative sublingual buprenorphine. J Pain Palliative Care Pharmacother. 2016;30(4):289-293. https://doi.org/10.1080/15360288.2016.1231734.
14. Kampman K, Jarvis M. ASAM National practice guidelines for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358-367. https://doi.org/10.1097/ADM.0000000000000166.
15. Childers JW, Arnold RM. Treatment of pain in patients taking buprenorphine for opioid addiction. J Palliat Med. 2012;15(5):613-614. https://doi.org/10.1089/jpm.2012.9591.
16. Alford DP, Compton P, Samet JH. Acute pain management for patients receiving maintenance methadone or buprenorphine therapy. Ann Intern Med. 2006;144(2):127-134. https://doi.org/10.7326/0003-4819-144-2-200601170-00010
© 2019 Society of Hospital Medicine