User login
Considering work as an expert witness? Look before you leap!
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
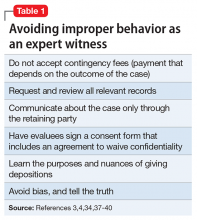
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
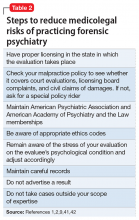
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
What is your liability for involuntary commitment based on faulty information?
Dear Dr. Mossman,
Last week, I hospitalized a patient against her will, based in part on what her family members told me she had threatened to do. The patient threatened to sue me and said I should have known that her relatives were lying. What if my patient is right? Could I face liability if I involuntarily hospitalized her based on bad collateral information?
Submitted by “Dr. R”
In all U.S. states, laws permit psychiatrists to involuntarily hospitalize persons who pose a danger to themselves or others because of mental illness.1 But taking this step can be tough. Deciding to hospitalize a patient against her will involves weighing her wants and freedom against your duty to look out for her long-term welfare and the community’s safety.2,3 Often, psychiatrists make these decisions under pressure because the family wants something done immediately, other patients also need attention, the clinical picture is incomplete, or potential dispositions (eg, crisis care and inpatient beds) are limited.3 Given such constraints, you can’t always make perfect decisions.
Dr. R’s question has 2 parts:
- What liabilities can a clinician face if a patient is wrongfully committed?
- What liabilities could arise from relying on inaccurate information or making a false petition in order to hospitalize a patient?
We hope that as you and Dr. R read our answers, you’ll have a clearer understanding of:
- the rationale for civil commitment
- how patients, doctors, and courts view civil commitment
- the role of collateral information in decision-making
- relevant legal concepts and case law.
Rationale for civil commitment
For centuries, society has used civil commitment as one of its legal methods for intervening when persons pose a danger to themselves or others because of their mental illness.4 Because incapacitation or death could result from a “false-negative” decision to release a dangerous patient, psychiatrists err on the side of caution and tolerate many “false-positive” hospitalizations of persons who wouldn’t have hurt anyone.5
We can never know if a patient would have done harm had she not been hospitalized. Measures of suicidality and hostility tend to subside during involuntary hospital treatment.6 After hospitalization, many patients cite protection from harm as a reason they are thankful for their treatment.7-9 Some involuntary inpatients want to be hospitalized but hide this for conscious or unconscious reasons,10,11 and involuntary treatment sometimes is the only way to help persons whose illness-induced anosognosia12 prevents them from understanding why they need treatment.13 Involuntary inpatient care leads to modest symptom reduction14,15 and produces treatment outcomes no worse than those of non-coerced patients.10
Patients’ views
Patients often view commitment as unjustified.16 They and their advocates object to what some view as the ultimate infringement on civil liberty.7,17 By its nature, involuntary commitment eliminates patients’ involvement in a major treatment decision,8 disempowers them,18 and influences their relationship with the treatment team.15
Some involuntary patients feel disrespected by staff members8 or experience inadvertent psychological harm, including “loss of self-esteem, identity, self-control, and self-efficacy, as well as diminished hope in the possibility of recovery.”15 Involuntary hospitalization also can have serious practical consequences. Commitment can lead to social stigma, loss of gun rights, increased risks of losing child custody, housing problems, and possible disqualification from some professions.19
Having seen many involuntary patients undergo a change of heart after treatment, psychiatrist Alan Stone proposed the “Thank You Theory” of civil commitment: involuntary hospitalization can be justified by showing that the patient is grateful after recovering.20 Studies show, however, that gratitude is far from universal.1
How coercion is experienced often depends on how it is communicated. The less coercion patients perceive, the better they feel about the treatment they received.21 Satisfaction is important because it leads to less compulsory readmission,22 and dissatisfaction makes malpractice lawsuits more likely.23
Commitment decision-making
States’ laws, judges’ attitudes, and court decisions establish each jurisdiction’s legal methods for instituting emergency holds and willingness to tolerate “false-positive” involuntary hospitalization,4,24 all of which create variation between and within states in how civil commitment laws are applied. As a result, clinicians’ decisions are influenced “by a range of social, political, and economic factors,”25 including patients’ sex, race, age, homelessness, employment status, living situation, diagnoses, previous involuntary treatment, and dissatisfaction with mental health treatment.22,26-32 Furthermore, the potential for coercion often blurs the line between an offer of voluntary admission and an involuntary hospitalization.18
Collateral information
Psychiatrists owe each patient a sound clinical assessment before deciding to initiate involuntarily hospitalization. During a psychiatric crisis, a patient might not be forthcoming or could have impaired memory or judgment. Information from friends or family can help fill in gaps in a patient’s self-report.33 As Dr. R’s question illustrates, adequate assessment often includes seeking information from persons familiar with the patient.1 A report on the Virginia Tech shootings by the Virginia Office of the Inspector General describes how collateral sources can provide otherwise missing evidence of dangerousness,34 and it often leads clinicians toward favoring admission.35
Yet clinicians should regard third-party reports with caution.36 As one attorney warns, “Psychiatrists should be cautious of the underlying motives of well-meaning family members and relatives.”37 If you make a decision to hospitalize a patient involuntarily based on collateral information that turns out to be flawed, are you at fault and potentially liable for harm to the patient?
False petitions and liability
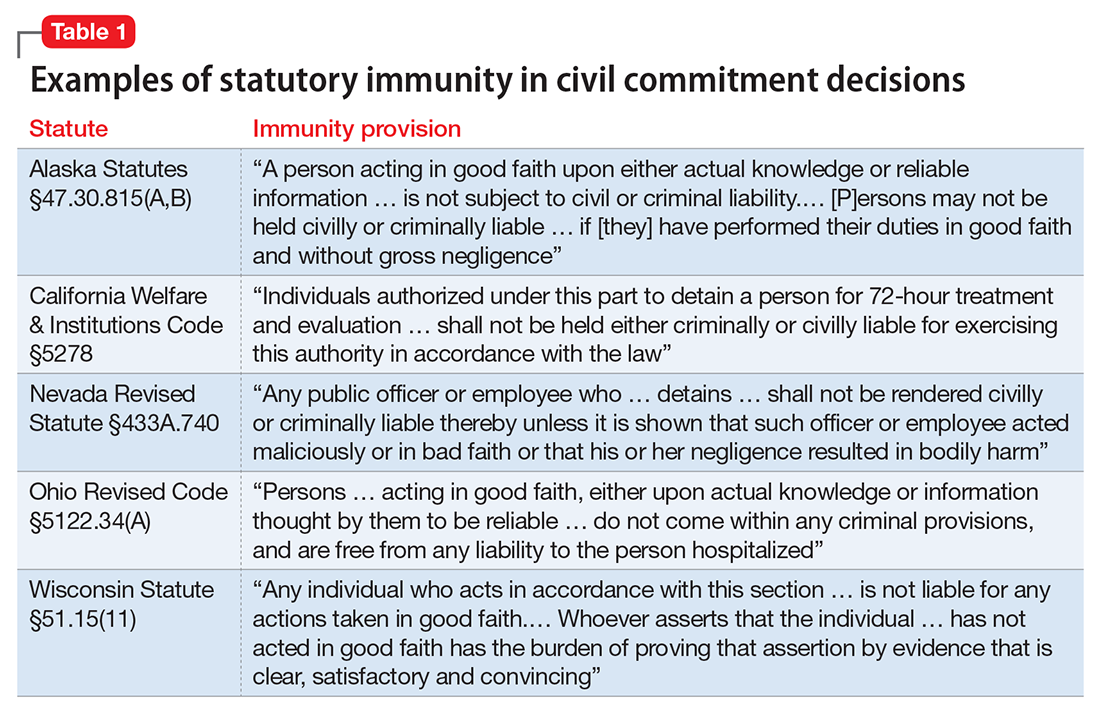
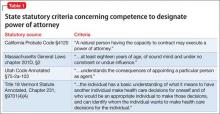
If you’re in a situation similar to the one Dr. R describes, you can take solace in knowing that courts generally provide immunity to a psychiatrist who makes a reasonable, well-intentioned decision to commit someone. The degree of immunity offered varies by jurisdiction. Table 1 provides examples of immunity language from several states’ statutes.
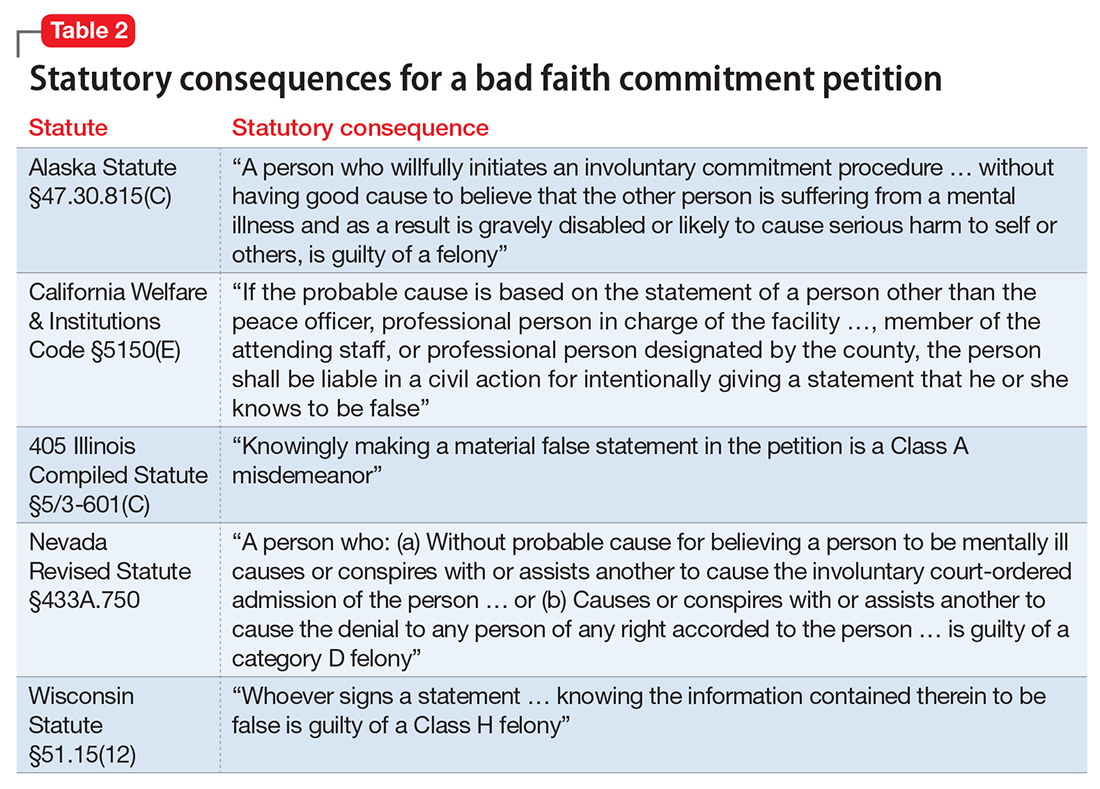
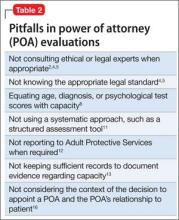
Many states’ statutes also lay out the potential consequences if a psychiatrist takes action to involuntarily hospitalize someone in bad faith or with malicious intent. In some jurisdictions, such actions can lead to criminal sanctions against the doctor or against the party who made a false petition (eg, a devious family member) (Table 2). Commenting on Texas’s statute, attorney Jeffrey Anderson explains, “The touchstone for causes of action based upon a wrongful civil commitment require that the psychiatrist[’s] conduct be found to be unreasonable and negligent. [Immunity…] still requires that a psychiatrist[’s] diagnosis of a patient[’s] threat to harm himself or others be a reasonable and prudent one.”37
The immunity extended through such statutes usually is limited to claims arising directly from the detention. For example, in the California case of Jacobs v Grossmont Hospital, a patient under a 72-hour hold fell and fractured her leg, and she sought damages. The trial court dismissed the suit under the immunity statute applicable to commitment decisions, but the appellate court held that “the immunity did not extend to other negligent acts.… The trial court erred in assuming that … the hospital was exempt from all liability for any negligence that occurred during the lawful hold.”38
Bingham v Cedars-Sinai Health Systems illustrates how physicians can lose immunity.39 A nurse contacted her supervisor to report a colleague who had stolen narcotics from work and compromised patient care. In response, the supervisor, hospital, and several physicians agreed to have her involuntarily committed. Later, it was confirmed that the colleague had taken the narcotics. She later sued the hospital system, claiming—in addition to malpractice—retaliation, invasion of privacy, assault and battery, false imprisonment, defamation, intentional infliction of emotional distress, disability-based harassment, and violation of her civil rights. Citing California’s immunity statute, the trial court granted summary judgment to the clinicians and hospital system. On appeal, however, the appellate court reversed the judgment, holding that the defendants had not shown that “the decision to detain Bingham was based on probable cause, a prerequisite to the exemption from liability,” and that Bingham had some legitimate grounds for her lawsuit.
A key point for Dr. R to consider is that, although some states provide immunity if the psychiatrist’s admitting decision was based on an evaluation “performed in good faith,”40 other states’ immunity provisions apply only if the psychiatrist had probable cause to make a decision to detain.41
Ways to reduce liability risk
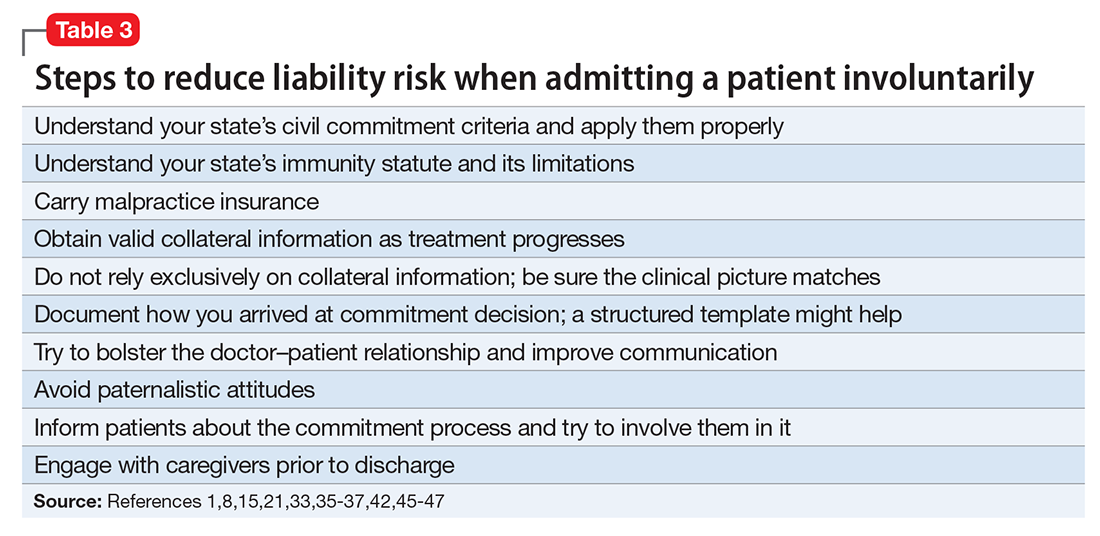
Although an involuntary hospitalization could have an uncertain basis, psychiatrists can reduce the risk of legal liability for their decisions. Good documentation is important. Admitting psychiatrists usually make sound decisions, but the corresponding documentation frequently lacks clinical justification.42-44 As the rate of appropriate documentation of admission decision-making improves, the rate of commitment falls,44 and patients’ legal rights enjoy greater protection.43 Poor communication can decrease the quality of care and increase the risk of a malpractice lawsuit.45 This is just one of many reasons why you should explain your reasons for involuntary hospitalization and inform patients of the procedures for judicial review.8,9 Table 3 summarizes other steps to reduce liability risk when committing patients to the hospital.1,8,15,21,33,35-37,42,45-47
1. Pinals DA, Mossman D. Evaluation for civil commitment: best practices for forensic mental health assessments. New York, NY: Oxford University Press; 2011.
2. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgemont). 2010;7(10):30-40.
3. Hedman LC, Petrila J, Fisher WH, et al. State laws on emergency holds for mental health stabilization. Psychiatr Serv. 2016;67(5):529-535.
4. Groendyk Z. “It takes a lot to get into Bellevue”: a pro-rights critique of New York’s involuntary commitment law. Fordham Urban Law J. 2013;40(1):548-585.
5. Brooks RA. U.S. psychiatrists’ beliefs and wants about involuntary civil commitment grounds. Int J Law Psychiatry. 2006;29(1):13-21.
6. Giacco D, Priebe S. Suicidality and hostility following involuntary hospital treatment. PLoS One. 2016;11(5):e0154458. doi: 10.1371/journal.pone.0154458.
7. Wyder M, Bland R, Herriot A, et al. The experiences of the legal processes of involuntary treatment orders: tension between the legal and medical frameworks. Int J Law Psychiatry. 2015;38:44-50.
8. Valenti E, Giacco D, Katasakou C, et al. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics. 2014;40(12):832-836.
9. Katsakou C, Rose D, Amos T, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;42(7):1169-1179.
10. Kaltiala-Heino R, Laippala P, Salokangas RK. Impact of coercion on treatment outcome. Int J Law Psychiatry. 1997;20(3):311-322.
11. Hoge SK, Lidz CW, Eisenberg M, et al. Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiatry. 1997;20(2):167-181.
12. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):10-17. 13. Gordon S. The danger zone: how the dangerousness standard in civil commitment proceedings harms people with serious mental illness. Case Western Reserve Law Review. 2016;66(3):657-700.
14. Kallert TW, Katsakou C, Adamowski T, et al. Coerced hospital admission and symptom change—a prospective observational multi-centre study. PLoS One. 2011;6(11):e28191. doi: 10.1371/journal.pone.0028191.
15. Danzer G, Wilkus-Stone A. The give and take of freedom: the role of involuntary hospitalization and treatment in recovery from mental illness. Bull Menninger Clin. 2015;79(3):255-280.
16. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
17. Amidov T. Involuntary commitment is unnecessary and discriminatory. In: Berlatsky N, ed. Mental illness. Farmington Hills, MI: Greenhaven Press; 2016;140-145.
18. Monahan J, Hoge SK, Lidz C, et al. Coercion and commitment: understanding involuntary mental hospital admission. Int J Law Psychiatry. 1995;18(3):249-263.
19. Guest Pryal KR. Heller’s scapegoats. North Carolina Law Review. 2015;93(5):1439-1473.
20. Stone AA. Mental health and law: a system in transition. Washington, DC: U.S. Government Printing Office; 1975:75-176.
21. Katsakou C, Bowers L, Amos T, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286-292.
22. Setkowski K, van der Post LF, Peen J, et al. Changing patient perspectives after compulsory admission and the risk of re-admission during 5 years of follow-up: the Amsterdam study of acute psychiatry IX. Int J Soc Psychiatry. 2016;62(6):578-588.
23. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
24. Goldman A. Continued overreliance on involuntary commitment: the need for a less restrictive alternative. J Leg Med. 2015;36(2):233-251.
25. Fisher WH, Grisso T. Commentary: civil commitment statutes—40 years of circumvention. J Am Acad Psychiatry Law. 2010;38(3):365-368.
26. Curley A, Agada E, Emechebe A, et al. Exploring and explaining involuntary care: the relationship between psychiatric admission status, gender and other demographic and clinical variables. Int J Law Psychiatry. 2016;47:53-59.
27. Muroff JR, Jackson JS, Mowbray CT, et al. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry. 2007;29(6):481-488.
28. Muroff JR, Edelsohn GA, Joe S, et al. The role of race in diagnostic and disposition decision making in a pediatric psychiatric emergency service. Gen Hosp Psychiatry. 2008;30(3):269-276.
29. Unick GJ, Kessell E, Woodard EK, et al. Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. Gen Hosp Psychiatry. 2011;33(6):618-625.
30. Ng XT, Kelly BD. Voluntary and involuntary care: three-year study of demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatry. 2012;35(4):317-326.
31. Lo TT, Woo BK. The impact of unemployment on utilization of psychiatric emergency services. Gen Hosp Psychiatry. 2011;33(3):e7-e8. doi: 10.1016/j.genhosppsych.2010.10.010.
32. van der Post LFM, Peen J, Dekker JJ. A prediction model for the incidence of civil detention for crisis patients with psychiatric illnesses; the Amsterdam study of acute psychiatry VII. Soc Psychiatry Psychiatr Epidemiol. 2014;49(2):283-290.
33. Heilbrun K, NeMoyer A, King C, et al. Using third-party information in forensic mental health assessment: a critical review. Court Review. 2015;51(1):16-35.
34. Mass shootings at Virginia Tech, April 16, 2007 report of the Virginia Tech Review Panel presented to Timothy M. Kaine, Governor, Commonwealth of Virginia. http://cdm16064.contentdm.oclc.org/cdm/ref/collection/p266901coll4/id/904. Accessed February 2, 2017.
35. Segal SP, Laurie TA, Segal MJ. Factors in the use of coercive retention in civil commitment evaluations in psychiatric emergency services. Psychiatr Serv. 2001;52(4):514-520.
36. Lincoln A, Allen MH. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
37. Anderson JC. How I decided to sue you: misadventures in psychiatry. Reprinted in part from: Moody CE, Smith MT, Maedgen BJ. Litigation of psychiatric malpractice claims. Presented at: Medical Malpractice Conference; April 15, 1993; San Antonio, TX. http://www.texaslawfirm.com/Articles/How_I_Decided_to_Sue_You__Misadventrues_in_Psychiatry.pdf. Accessed December 27, 2016.
38. Jacobs v Grossmont Hospital, 108 Cal App 4th 69, 133 Cal Rptr 2d9 (2003).
39. Bingham v Cedars Sinai Health Systems, WL 2137442, Cal App 2 Dist (2004).
40. Ohio Revised Code §5122.34.
41. California Welfare & Institutions Code §5150(E).
42. Hashmi A, Shad M, Rhoades HM, et al. Involuntary detention: do psychiatrists clinically justify continuing involuntary hospitalization? Psychiatr Q. 2014;85(3):285-293.
43. Brayley J, Alston A, Rogers K. Legal criteria for involuntary mental health admission: clinician performance in recording grounds for decision. Med J Aust. 2015;203(8):334.
44. Perrigo TL, Williams KA. Implementation of an evidence based guideline for assessment and documentation of the civil commitment process. Community Ment Health J. 2016;52(8):1033-1036.
45. Mor S, Rabinovich-Einy O. Relational malpractice. Seton Hall Law Rev. 2012;42(2):601-642.
46. Tate v Kaiser Foundation Hospitals, WL 176625, U.S. Dist. LEXIS 5891 (CD Cal 2014).
47. Ranieri V, Madigan K, Roche E, et al. Caregivers’ perceptions of coercion in psychiatric hospital admission. Psychiatry Res. 2015;22(3)8:380-385.
Dear Dr. Mossman,
Last week, I hospitalized a patient against her will, based in part on what her family members told me she had threatened to do. The patient threatened to sue me and said I should have known that her relatives were lying. What if my patient is right? Could I face liability if I involuntarily hospitalized her based on bad collateral information?
Submitted by “Dr. R”
In all U.S. states, laws permit psychiatrists to involuntarily hospitalize persons who pose a danger to themselves or others because of mental illness.1 But taking this step can be tough. Deciding to hospitalize a patient against her will involves weighing her wants and freedom against your duty to look out for her long-term welfare and the community’s safety.2,3 Often, psychiatrists make these decisions under pressure because the family wants something done immediately, other patients also need attention, the clinical picture is incomplete, or potential dispositions (eg, crisis care and inpatient beds) are limited.3 Given such constraints, you can’t always make perfect decisions.
Dr. R’s question has 2 parts:
- What liabilities can a clinician face if a patient is wrongfully committed?
- What liabilities could arise from relying on inaccurate information or making a false petition in order to hospitalize a patient?
We hope that as you and Dr. R read our answers, you’ll have a clearer understanding of:
- the rationale for civil commitment
- how patients, doctors, and courts view civil commitment
- the role of collateral information in decision-making
- relevant legal concepts and case law.
Rationale for civil commitment
For centuries, society has used civil commitment as one of its legal methods for intervening when persons pose a danger to themselves or others because of their mental illness.4 Because incapacitation or death could result from a “false-negative” decision to release a dangerous patient, psychiatrists err on the side of caution and tolerate many “false-positive” hospitalizations of persons who wouldn’t have hurt anyone.5
We can never know if a patient would have done harm had she not been hospitalized. Measures of suicidality and hostility tend to subside during involuntary hospital treatment.6 After hospitalization, many patients cite protection from harm as a reason they are thankful for their treatment.7-9 Some involuntary inpatients want to be hospitalized but hide this for conscious or unconscious reasons,10,11 and involuntary treatment sometimes is the only way to help persons whose illness-induced anosognosia12 prevents them from understanding why they need treatment.13 Involuntary inpatient care leads to modest symptom reduction14,15 and produces treatment outcomes no worse than those of non-coerced patients.10
Patients’ views
Patients often view commitment as unjustified.16 They and their advocates object to what some view as the ultimate infringement on civil liberty.7,17 By its nature, involuntary commitment eliminates patients’ involvement in a major treatment decision,8 disempowers them,18 and influences their relationship with the treatment team.15
Some involuntary patients feel disrespected by staff members8 or experience inadvertent psychological harm, including “loss of self-esteem, identity, self-control, and self-efficacy, as well as diminished hope in the possibility of recovery.”15 Involuntary hospitalization also can have serious practical consequences. Commitment can lead to social stigma, loss of gun rights, increased risks of losing child custody, housing problems, and possible disqualification from some professions.19
Having seen many involuntary patients undergo a change of heart after treatment, psychiatrist Alan Stone proposed the “Thank You Theory” of civil commitment: involuntary hospitalization can be justified by showing that the patient is grateful after recovering.20 Studies show, however, that gratitude is far from universal.1
How coercion is experienced often depends on how it is communicated. The less coercion patients perceive, the better they feel about the treatment they received.21 Satisfaction is important because it leads to less compulsory readmission,22 and dissatisfaction makes malpractice lawsuits more likely.23
Commitment decision-making
States’ laws, judges’ attitudes, and court decisions establish each jurisdiction’s legal methods for instituting emergency holds and willingness to tolerate “false-positive” involuntary hospitalization,4,24 all of which create variation between and within states in how civil commitment laws are applied. As a result, clinicians’ decisions are influenced “by a range of social, political, and economic factors,”25 including patients’ sex, race, age, homelessness, employment status, living situation, diagnoses, previous involuntary treatment, and dissatisfaction with mental health treatment.22,26-32 Furthermore, the potential for coercion often blurs the line between an offer of voluntary admission and an involuntary hospitalization.18
Collateral information
Psychiatrists owe each patient a sound clinical assessment before deciding to initiate involuntarily hospitalization. During a psychiatric crisis, a patient might not be forthcoming or could have impaired memory or judgment. Information from friends or family can help fill in gaps in a patient’s self-report.33 As Dr. R’s question illustrates, adequate assessment often includes seeking information from persons familiar with the patient.1 A report on the Virginia Tech shootings by the Virginia Office of the Inspector General describes how collateral sources can provide otherwise missing evidence of dangerousness,34 and it often leads clinicians toward favoring admission.35
Yet clinicians should regard third-party reports with caution.36 As one attorney warns, “Psychiatrists should be cautious of the underlying motives of well-meaning family members and relatives.”37 If you make a decision to hospitalize a patient involuntarily based on collateral information that turns out to be flawed, are you at fault and potentially liable for harm to the patient?
False petitions and liability
If you’re in a situation similar to the one Dr. R describes, you can take solace in knowing that courts generally provide immunity to a psychiatrist who makes a reasonable, well-intentioned decision to commit someone. The degree of immunity offered varies by jurisdiction. Table 1 provides examples of immunity language from several states’ statutes.
Many states’ statutes also lay out the potential consequences if a psychiatrist takes action to involuntarily hospitalize someone in bad faith or with malicious intent. In some jurisdictions, such actions can lead to criminal sanctions against the doctor or against the party who made a false petition (eg, a devious family member) (Table 2). Commenting on Texas’s statute, attorney Jeffrey Anderson explains, “The touchstone for causes of action based upon a wrongful civil commitment require that the psychiatrist[’s] conduct be found to be unreasonable and negligent. [Immunity…] still requires that a psychiatrist[’s] diagnosis of a patient[’s] threat to harm himself or others be a reasonable and prudent one.”37
The immunity extended through such statutes usually is limited to claims arising directly from the detention. For example, in the California case of Jacobs v Grossmont Hospital, a patient under a 72-hour hold fell and fractured her leg, and she sought damages. The trial court dismissed the suit under the immunity statute applicable to commitment decisions, but the appellate court held that “the immunity did not extend to other negligent acts.… The trial court erred in assuming that … the hospital was exempt from all liability for any negligence that occurred during the lawful hold.”38
Bingham v Cedars-Sinai Health Systems illustrates how physicians can lose immunity.39 A nurse contacted her supervisor to report a colleague who had stolen narcotics from work and compromised patient care. In response, the supervisor, hospital, and several physicians agreed to have her involuntarily committed. Later, it was confirmed that the colleague had taken the narcotics. She later sued the hospital system, claiming—in addition to malpractice—retaliation, invasion of privacy, assault and battery, false imprisonment, defamation, intentional infliction of emotional distress, disability-based harassment, and violation of her civil rights. Citing California’s immunity statute, the trial court granted summary judgment to the clinicians and hospital system. On appeal, however, the appellate court reversed the judgment, holding that the defendants had not shown that “the decision to detain Bingham was based on probable cause, a prerequisite to the exemption from liability,” and that Bingham had some legitimate grounds for her lawsuit.
A key point for Dr. R to consider is that, although some states provide immunity if the psychiatrist’s admitting decision was based on an evaluation “performed in good faith,”40 other states’ immunity provisions apply only if the psychiatrist had probable cause to make a decision to detain.41
Ways to reduce liability risk
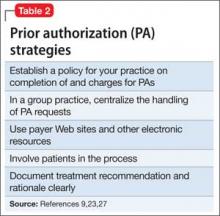
Although an involuntary hospitalization could have an uncertain basis, psychiatrists can reduce the risk of legal liability for their decisions. Good documentation is important. Admitting psychiatrists usually make sound decisions, but the corresponding documentation frequently lacks clinical justification.42-44 As the rate of appropriate documentation of admission decision-making improves, the rate of commitment falls,44 and patients’ legal rights enjoy greater protection.43 Poor communication can decrease the quality of care and increase the risk of a malpractice lawsuit.45 This is just one of many reasons why you should explain your reasons for involuntary hospitalization and inform patients of the procedures for judicial review.8,9 Table 3 summarizes other steps to reduce liability risk when committing patients to the hospital.1,8,15,21,33,35-37,42,45-47
Dear Dr. Mossman,
Last week, I hospitalized a patient against her will, based in part on what her family members told me she had threatened to do. The patient threatened to sue me and said I should have known that her relatives were lying. What if my patient is right? Could I face liability if I involuntarily hospitalized her based on bad collateral information?
Submitted by “Dr. R”
In all U.S. states, laws permit psychiatrists to involuntarily hospitalize persons who pose a danger to themselves or others because of mental illness.1 But taking this step can be tough. Deciding to hospitalize a patient against her will involves weighing her wants and freedom against your duty to look out for her long-term welfare and the community’s safety.2,3 Often, psychiatrists make these decisions under pressure because the family wants something done immediately, other patients also need attention, the clinical picture is incomplete, or potential dispositions (eg, crisis care and inpatient beds) are limited.3 Given such constraints, you can’t always make perfect decisions.
Dr. R’s question has 2 parts:
- What liabilities can a clinician face if a patient is wrongfully committed?
- What liabilities could arise from relying on inaccurate information or making a false petition in order to hospitalize a patient?
We hope that as you and Dr. R read our answers, you’ll have a clearer understanding of:
- the rationale for civil commitment
- how patients, doctors, and courts view civil commitment
- the role of collateral information in decision-making
- relevant legal concepts and case law.
Rationale for civil commitment
For centuries, society has used civil commitment as one of its legal methods for intervening when persons pose a danger to themselves or others because of their mental illness.4 Because incapacitation or death could result from a “false-negative” decision to release a dangerous patient, psychiatrists err on the side of caution and tolerate many “false-positive” hospitalizations of persons who wouldn’t have hurt anyone.5
We can never know if a patient would have done harm had she not been hospitalized. Measures of suicidality and hostility tend to subside during involuntary hospital treatment.6 After hospitalization, many patients cite protection from harm as a reason they are thankful for their treatment.7-9 Some involuntary inpatients want to be hospitalized but hide this for conscious or unconscious reasons,10,11 and involuntary treatment sometimes is the only way to help persons whose illness-induced anosognosia12 prevents them from understanding why they need treatment.13 Involuntary inpatient care leads to modest symptom reduction14,15 and produces treatment outcomes no worse than those of non-coerced patients.10
Patients’ views
Patients often view commitment as unjustified.16 They and their advocates object to what some view as the ultimate infringement on civil liberty.7,17 By its nature, involuntary commitment eliminates patients’ involvement in a major treatment decision,8 disempowers them,18 and influences their relationship with the treatment team.15
Some involuntary patients feel disrespected by staff members8 or experience inadvertent psychological harm, including “loss of self-esteem, identity, self-control, and self-efficacy, as well as diminished hope in the possibility of recovery.”15 Involuntary hospitalization also can have serious practical consequences. Commitment can lead to social stigma, loss of gun rights, increased risks of losing child custody, housing problems, and possible disqualification from some professions.19
Having seen many involuntary patients undergo a change of heart after treatment, psychiatrist Alan Stone proposed the “Thank You Theory” of civil commitment: involuntary hospitalization can be justified by showing that the patient is grateful after recovering.20 Studies show, however, that gratitude is far from universal.1
How coercion is experienced often depends on how it is communicated. The less coercion patients perceive, the better they feel about the treatment they received.21 Satisfaction is important because it leads to less compulsory readmission,22 and dissatisfaction makes malpractice lawsuits more likely.23
Commitment decision-making
States’ laws, judges’ attitudes, and court decisions establish each jurisdiction’s legal methods for instituting emergency holds and willingness to tolerate “false-positive” involuntary hospitalization,4,24 all of which create variation between and within states in how civil commitment laws are applied. As a result, clinicians’ decisions are influenced “by a range of social, political, and economic factors,”25 including patients’ sex, race, age, homelessness, employment status, living situation, diagnoses, previous involuntary treatment, and dissatisfaction with mental health treatment.22,26-32 Furthermore, the potential for coercion often blurs the line between an offer of voluntary admission and an involuntary hospitalization.18
Collateral information
Psychiatrists owe each patient a sound clinical assessment before deciding to initiate involuntarily hospitalization. During a psychiatric crisis, a patient might not be forthcoming or could have impaired memory or judgment. Information from friends or family can help fill in gaps in a patient’s self-report.33 As Dr. R’s question illustrates, adequate assessment often includes seeking information from persons familiar with the patient.1 A report on the Virginia Tech shootings by the Virginia Office of the Inspector General describes how collateral sources can provide otherwise missing evidence of dangerousness,34 and it often leads clinicians toward favoring admission.35
Yet clinicians should regard third-party reports with caution.36 As one attorney warns, “Psychiatrists should be cautious of the underlying motives of well-meaning family members and relatives.”37 If you make a decision to hospitalize a patient involuntarily based on collateral information that turns out to be flawed, are you at fault and potentially liable for harm to the patient?
False petitions and liability
If you’re in a situation similar to the one Dr. R describes, you can take solace in knowing that courts generally provide immunity to a psychiatrist who makes a reasonable, well-intentioned decision to commit someone. The degree of immunity offered varies by jurisdiction. Table 1 provides examples of immunity language from several states’ statutes.
Many states’ statutes also lay out the potential consequences if a psychiatrist takes action to involuntarily hospitalize someone in bad faith or with malicious intent. In some jurisdictions, such actions can lead to criminal sanctions against the doctor or against the party who made a false petition (eg, a devious family member) (Table 2). Commenting on Texas’s statute, attorney Jeffrey Anderson explains, “The touchstone for causes of action based upon a wrongful civil commitment require that the psychiatrist[’s] conduct be found to be unreasonable and negligent. [Immunity…] still requires that a psychiatrist[’s] diagnosis of a patient[’s] threat to harm himself or others be a reasonable and prudent one.”37
The immunity extended through such statutes usually is limited to claims arising directly from the detention. For example, in the California case of Jacobs v Grossmont Hospital, a patient under a 72-hour hold fell and fractured her leg, and she sought damages. The trial court dismissed the suit under the immunity statute applicable to commitment decisions, but the appellate court held that “the immunity did not extend to other negligent acts.… The trial court erred in assuming that … the hospital was exempt from all liability for any negligence that occurred during the lawful hold.”38
Bingham v Cedars-Sinai Health Systems illustrates how physicians can lose immunity.39 A nurse contacted her supervisor to report a colleague who had stolen narcotics from work and compromised patient care. In response, the supervisor, hospital, and several physicians agreed to have her involuntarily committed. Later, it was confirmed that the colleague had taken the narcotics. She later sued the hospital system, claiming—in addition to malpractice—retaliation, invasion of privacy, assault and battery, false imprisonment, defamation, intentional infliction of emotional distress, disability-based harassment, and violation of her civil rights. Citing California’s immunity statute, the trial court granted summary judgment to the clinicians and hospital system. On appeal, however, the appellate court reversed the judgment, holding that the defendants had not shown that “the decision to detain Bingham was based on probable cause, a prerequisite to the exemption from liability,” and that Bingham had some legitimate grounds for her lawsuit.
A key point for Dr. R to consider is that, although some states provide immunity if the psychiatrist’s admitting decision was based on an evaluation “performed in good faith,”40 other states’ immunity provisions apply only if the psychiatrist had probable cause to make a decision to detain.41
Ways to reduce liability risk
Although an involuntary hospitalization could have an uncertain basis, psychiatrists can reduce the risk of legal liability for their decisions. Good documentation is important. Admitting psychiatrists usually make sound decisions, but the corresponding documentation frequently lacks clinical justification.42-44 As the rate of appropriate documentation of admission decision-making improves, the rate of commitment falls,44 and patients’ legal rights enjoy greater protection.43 Poor communication can decrease the quality of care and increase the risk of a malpractice lawsuit.45 This is just one of many reasons why you should explain your reasons for involuntary hospitalization and inform patients of the procedures for judicial review.8,9 Table 3 summarizes other steps to reduce liability risk when committing patients to the hospital.1,8,15,21,33,35-37,42,45-47
1. Pinals DA, Mossman D. Evaluation for civil commitment: best practices for forensic mental health assessments. New York, NY: Oxford University Press; 2011.
2. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgemont). 2010;7(10):30-40.
3. Hedman LC, Petrila J, Fisher WH, et al. State laws on emergency holds for mental health stabilization. Psychiatr Serv. 2016;67(5):529-535.
4. Groendyk Z. “It takes a lot to get into Bellevue”: a pro-rights critique of New York’s involuntary commitment law. Fordham Urban Law J. 2013;40(1):548-585.
5. Brooks RA. U.S. psychiatrists’ beliefs and wants about involuntary civil commitment grounds. Int J Law Psychiatry. 2006;29(1):13-21.
6. Giacco D, Priebe S. Suicidality and hostility following involuntary hospital treatment. PLoS One. 2016;11(5):e0154458. doi: 10.1371/journal.pone.0154458.
7. Wyder M, Bland R, Herriot A, et al. The experiences of the legal processes of involuntary treatment orders: tension between the legal and medical frameworks. Int J Law Psychiatry. 2015;38:44-50.
8. Valenti E, Giacco D, Katasakou C, et al. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics. 2014;40(12):832-836.
9. Katsakou C, Rose D, Amos T, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;42(7):1169-1179.
10. Kaltiala-Heino R, Laippala P, Salokangas RK. Impact of coercion on treatment outcome. Int J Law Psychiatry. 1997;20(3):311-322.
11. Hoge SK, Lidz CW, Eisenberg M, et al. Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiatry. 1997;20(2):167-181.
12. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):10-17. 13. Gordon S. The danger zone: how the dangerousness standard in civil commitment proceedings harms people with serious mental illness. Case Western Reserve Law Review. 2016;66(3):657-700.
14. Kallert TW, Katsakou C, Adamowski T, et al. Coerced hospital admission and symptom change—a prospective observational multi-centre study. PLoS One. 2011;6(11):e28191. doi: 10.1371/journal.pone.0028191.
15. Danzer G, Wilkus-Stone A. The give and take of freedom: the role of involuntary hospitalization and treatment in recovery from mental illness. Bull Menninger Clin. 2015;79(3):255-280.
16. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
17. Amidov T. Involuntary commitment is unnecessary and discriminatory. In: Berlatsky N, ed. Mental illness. Farmington Hills, MI: Greenhaven Press; 2016;140-145.
18. Monahan J, Hoge SK, Lidz C, et al. Coercion and commitment: understanding involuntary mental hospital admission. Int J Law Psychiatry. 1995;18(3):249-263.
19. Guest Pryal KR. Heller’s scapegoats. North Carolina Law Review. 2015;93(5):1439-1473.
20. Stone AA. Mental health and law: a system in transition. Washington, DC: U.S. Government Printing Office; 1975:75-176.
21. Katsakou C, Bowers L, Amos T, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286-292.
22. Setkowski K, van der Post LF, Peen J, et al. Changing patient perspectives after compulsory admission and the risk of re-admission during 5 years of follow-up: the Amsterdam study of acute psychiatry IX. Int J Soc Psychiatry. 2016;62(6):578-588.
23. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
24. Goldman A. Continued overreliance on involuntary commitment: the need for a less restrictive alternative. J Leg Med. 2015;36(2):233-251.
25. Fisher WH, Grisso T. Commentary: civil commitment statutes—40 years of circumvention. J Am Acad Psychiatry Law. 2010;38(3):365-368.
26. Curley A, Agada E, Emechebe A, et al. Exploring and explaining involuntary care: the relationship between psychiatric admission status, gender and other demographic and clinical variables. Int J Law Psychiatry. 2016;47:53-59.
27. Muroff JR, Jackson JS, Mowbray CT, et al. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry. 2007;29(6):481-488.
28. Muroff JR, Edelsohn GA, Joe S, et al. The role of race in diagnostic and disposition decision making in a pediatric psychiatric emergency service. Gen Hosp Psychiatry. 2008;30(3):269-276.
29. Unick GJ, Kessell E, Woodard EK, et al. Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. Gen Hosp Psychiatry. 2011;33(6):618-625.
30. Ng XT, Kelly BD. Voluntary and involuntary care: three-year study of demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatry. 2012;35(4):317-326.
31. Lo TT, Woo BK. The impact of unemployment on utilization of psychiatric emergency services. Gen Hosp Psychiatry. 2011;33(3):e7-e8. doi: 10.1016/j.genhosppsych.2010.10.010.
32. van der Post LFM, Peen J, Dekker JJ. A prediction model for the incidence of civil detention for crisis patients with psychiatric illnesses; the Amsterdam study of acute psychiatry VII. Soc Psychiatry Psychiatr Epidemiol. 2014;49(2):283-290.
33. Heilbrun K, NeMoyer A, King C, et al. Using third-party information in forensic mental health assessment: a critical review. Court Review. 2015;51(1):16-35.
34. Mass shootings at Virginia Tech, April 16, 2007 report of the Virginia Tech Review Panel presented to Timothy M. Kaine, Governor, Commonwealth of Virginia. http://cdm16064.contentdm.oclc.org/cdm/ref/collection/p266901coll4/id/904. Accessed February 2, 2017.
35. Segal SP, Laurie TA, Segal MJ. Factors in the use of coercive retention in civil commitment evaluations in psychiatric emergency services. Psychiatr Serv. 2001;52(4):514-520.
36. Lincoln A, Allen MH. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
37. Anderson JC. How I decided to sue you: misadventures in psychiatry. Reprinted in part from: Moody CE, Smith MT, Maedgen BJ. Litigation of psychiatric malpractice claims. Presented at: Medical Malpractice Conference; April 15, 1993; San Antonio, TX. http://www.texaslawfirm.com/Articles/How_I_Decided_to_Sue_You__Misadventrues_in_Psychiatry.pdf. Accessed December 27, 2016.
38. Jacobs v Grossmont Hospital, 108 Cal App 4th 69, 133 Cal Rptr 2d9 (2003).
39. Bingham v Cedars Sinai Health Systems, WL 2137442, Cal App 2 Dist (2004).
40. Ohio Revised Code §5122.34.
41. California Welfare & Institutions Code §5150(E).
42. Hashmi A, Shad M, Rhoades HM, et al. Involuntary detention: do psychiatrists clinically justify continuing involuntary hospitalization? Psychiatr Q. 2014;85(3):285-293.
43. Brayley J, Alston A, Rogers K. Legal criteria for involuntary mental health admission: clinician performance in recording grounds for decision. Med J Aust. 2015;203(8):334.
44. Perrigo TL, Williams KA. Implementation of an evidence based guideline for assessment and documentation of the civil commitment process. Community Ment Health J. 2016;52(8):1033-1036.
45. Mor S, Rabinovich-Einy O. Relational malpractice. Seton Hall Law Rev. 2012;42(2):601-642.
46. Tate v Kaiser Foundation Hospitals, WL 176625, U.S. Dist. LEXIS 5891 (CD Cal 2014).
47. Ranieri V, Madigan K, Roche E, et al. Caregivers’ perceptions of coercion in psychiatric hospital admission. Psychiatry Res. 2015;22(3)8:380-385.
1. Pinals DA, Mossman D. Evaluation for civil commitment: best practices for forensic mental health assessments. New York, NY: Oxford University Press; 2011.
2. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgemont). 2010;7(10):30-40.
3. Hedman LC, Petrila J, Fisher WH, et al. State laws on emergency holds for mental health stabilization. Psychiatr Serv. 2016;67(5):529-535.
4. Groendyk Z. “It takes a lot to get into Bellevue”: a pro-rights critique of New York’s involuntary commitment law. Fordham Urban Law J. 2013;40(1):548-585.
5. Brooks RA. U.S. psychiatrists’ beliefs and wants about involuntary civil commitment grounds. Int J Law Psychiatry. 2006;29(1):13-21.
6. Giacco D, Priebe S. Suicidality and hostility following involuntary hospital treatment. PLoS One. 2016;11(5):e0154458. doi: 10.1371/journal.pone.0154458.
7. Wyder M, Bland R, Herriot A, et al. The experiences of the legal processes of involuntary treatment orders: tension between the legal and medical frameworks. Int J Law Psychiatry. 2015;38:44-50.
8. Valenti E, Giacco D, Katasakou C, et al. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics. 2014;40(12):832-836.
9. Katsakou C, Rose D, Amos T, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;42(7):1169-1179.
10. Kaltiala-Heino R, Laippala P, Salokangas RK. Impact of coercion on treatment outcome. Int J Law Psychiatry. 1997;20(3):311-322.
11. Hoge SK, Lidz CW, Eisenberg M, et al. Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiatry. 1997;20(2):167-181.
12. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):10-17. 13. Gordon S. The danger zone: how the dangerousness standard in civil commitment proceedings harms people with serious mental illness. Case Western Reserve Law Review. 2016;66(3):657-700.
14. Kallert TW, Katsakou C, Adamowski T, et al. Coerced hospital admission and symptom change—a prospective observational multi-centre study. PLoS One. 2011;6(11):e28191. doi: 10.1371/journal.pone.0028191.
15. Danzer G, Wilkus-Stone A. The give and take of freedom: the role of involuntary hospitalization and treatment in recovery from mental illness. Bull Menninger Clin. 2015;79(3):255-280.
16. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
17. Amidov T. Involuntary commitment is unnecessary and discriminatory. In: Berlatsky N, ed. Mental illness. Farmington Hills, MI: Greenhaven Press; 2016;140-145.
18. Monahan J, Hoge SK, Lidz C, et al. Coercion and commitment: understanding involuntary mental hospital admission. Int J Law Psychiatry. 1995;18(3):249-263.
19. Guest Pryal KR. Heller’s scapegoats. North Carolina Law Review. 2015;93(5):1439-1473.
20. Stone AA. Mental health and law: a system in transition. Washington, DC: U.S. Government Printing Office; 1975:75-176.
21. Katsakou C, Bowers L, Amos T, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286-292.
22. Setkowski K, van der Post LF, Peen J, et al. Changing patient perspectives after compulsory admission and the risk of re-admission during 5 years of follow-up: the Amsterdam study of acute psychiatry IX. Int J Soc Psychiatry. 2016;62(6):578-588.
23. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
24. Goldman A. Continued overreliance on involuntary commitment: the need for a less restrictive alternative. J Leg Med. 2015;36(2):233-251.
25. Fisher WH, Grisso T. Commentary: civil commitment statutes—40 years of circumvention. J Am Acad Psychiatry Law. 2010;38(3):365-368.
26. Curley A, Agada E, Emechebe A, et al. Exploring and explaining involuntary care: the relationship between psychiatric admission status, gender and other demographic and clinical variables. Int J Law Psychiatry. 2016;47:53-59.
27. Muroff JR, Jackson JS, Mowbray CT, et al. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry. 2007;29(6):481-488.
28. Muroff JR, Edelsohn GA, Joe S, et al. The role of race in diagnostic and disposition decision making in a pediatric psychiatric emergency service. Gen Hosp Psychiatry. 2008;30(3):269-276.
29. Unick GJ, Kessell E, Woodard EK, et al. Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. Gen Hosp Psychiatry. 2011;33(6):618-625.
30. Ng XT, Kelly BD. Voluntary and involuntary care: three-year study of demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatry. 2012;35(4):317-326.
31. Lo TT, Woo BK. The impact of unemployment on utilization of psychiatric emergency services. Gen Hosp Psychiatry. 2011;33(3):e7-e8. doi: 10.1016/j.genhosppsych.2010.10.010.
32. van der Post LFM, Peen J, Dekker JJ. A prediction model for the incidence of civil detention for crisis patients with psychiatric illnesses; the Amsterdam study of acute psychiatry VII. Soc Psychiatry Psychiatr Epidemiol. 2014;49(2):283-290.
33. Heilbrun K, NeMoyer A, King C, et al. Using third-party information in forensic mental health assessment: a critical review. Court Review. 2015;51(1):16-35.
34. Mass shootings at Virginia Tech, April 16, 2007 report of the Virginia Tech Review Panel presented to Timothy M. Kaine, Governor, Commonwealth of Virginia. http://cdm16064.contentdm.oclc.org/cdm/ref/collection/p266901coll4/id/904. Accessed February 2, 2017.
35. Segal SP, Laurie TA, Segal MJ. Factors in the use of coercive retention in civil commitment evaluations in psychiatric emergency services. Psychiatr Serv. 2001;52(4):514-520.
36. Lincoln A, Allen MH. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
37. Anderson JC. How I decided to sue you: misadventures in psychiatry. Reprinted in part from: Moody CE, Smith MT, Maedgen BJ. Litigation of psychiatric malpractice claims. Presented at: Medical Malpractice Conference; April 15, 1993; San Antonio, TX. http://www.texaslawfirm.com/Articles/How_I_Decided_to_Sue_You__Misadventrues_in_Psychiatry.pdf. Accessed December 27, 2016.
38. Jacobs v Grossmont Hospital, 108 Cal App 4th 69, 133 Cal Rptr 2d9 (2003).
39. Bingham v Cedars Sinai Health Systems, WL 2137442, Cal App 2 Dist (2004).
40. Ohio Revised Code §5122.34.
41. California Welfare & Institutions Code §5150(E).
42. Hashmi A, Shad M, Rhoades HM, et al. Involuntary detention: do psychiatrists clinically justify continuing involuntary hospitalization? Psychiatr Q. 2014;85(3):285-293.
43. Brayley J, Alston A, Rogers K. Legal criteria for involuntary mental health admission: clinician performance in recording grounds for decision. Med J Aust. 2015;203(8):334.
44. Perrigo TL, Williams KA. Implementation of an evidence based guideline for assessment and documentation of the civil commitment process. Community Ment Health J. 2016;52(8):1033-1036.
45. Mor S, Rabinovich-Einy O. Relational malpractice. Seton Hall Law Rev. 2012;42(2):601-642.
46. Tate v Kaiser Foundation Hospitals, WL 176625, U.S. Dist. LEXIS 5891 (CD Cal 2014).
47. Ranieri V, Madigan K, Roche E, et al. Caregivers’ perceptions of coercion in psychiatric hospital admission. Psychiatry Res. 2015;22(3)8:380-385.
Would better policing of metabolic status help you avoid medicolegal worries?
Dear Dr. Mossman,
All the psychiatrists at our clinic agree: It is hard to remember when our patients who take an antipsychotic are due for metabolic monitoring, and it’s even harder to get many of them to follow through with timely blood tests. For many, stopping their medication would be a bad idea. If we keep a patient on an antipsychotic and a metabolic problem results, how serious is our malpractice liability risk?
Submitted by “Dr. V”
Antipsychotics, the mainstay of treatment for schizophrenia,1 put patients at risk of gaining weight and developing metabolic syndrome, including type 2 diabetes mellitus, hypertension, and dyslipidemia.2 Second-generation antipsychotics are the biggest offenders, but taking a first-generation antipsychotic also can lead to these adverse effects.3
Most psychiatrists are aware of these risks and prefer that their patients do not experience them. However, many psychiatrists neglect proper monitoring or, like Dr. V, find it hard to ensure it happens and thus worry about clinical deterioration if patients stop taking an antipsychotic.4 If you are in the same situation as Dr. V, what medicolegal risks are you facing?
To answer this question, we will:
- review the clinical guidelines and standards for monitoring metabolic effects of antipsychotics
- examine how well (or poorly) physicians adhere to these standards
- discuss what “standard of care” means and how a practice guideline affects the standard effects
- propose how psychiatrists can do better at policing the metabolic effects of antipsychotics.
I’ll be watching you: Following guidelines
Several medical specialty societies have published guidelines for monitoring the metabolic effects of antipsychotics.5-8 These guidelines instruct physicians to obtain a thorough personal and family history; consider metabolic risks when starting a medication; and monitor weight, waist circumference, blood pressure, glucose, hemoglobin A1c, and lipids at various intervals. They also advise referral for management of detected metabolic problems.
Although the recommendations seem clear, many physicians don’t follow them. A 2012 meta-analysis of 48 studies, covering >200,000 antipsychotic-treated patients, showed that baseline measurements of cholesterol, glucose, and weight occurred in <50% of cases.9 A more recent review found that, among adults with a serious mental illness, the rate of lipid testing varied from 6% to 85% and for glucose monitoring, between 18% and 75%.10 In the first years after antipsychotic monitoring guidelines were established, they had only a modest impact on practice,9,11 and some studies showed the guidelines made no difference at all.12-14
Monitoring compliance varies with the type of insurance coverage patients have but remains suboptimal among the commercially insured,11 Medicaid patients,14-16 and veterans.17,18 Studies on antipsychotic treatment in children, adolescents, patients with dementia, and patients with an intellectual disability show insufficient monitoring as well.9,14,17,19-21 The reasons for these gaps are manifold, but one commonly cited factor is uncertainty about whether the psychiatrist or primary care physician should handle monitoring.22
Every claim you stake: The ‘standard of care’
In a medical malpractice case, the party claiming injury must show that the accused physician failed to follow “the generally recognized practices and procedures which would be exercised by ordinary competent practitioners in a defendant doctor’s field of medicine under the same or similar circumstances.”23 In the studies mentioned above,9-14 a large fraction of psychiatrists—many of whom, we can presume, are “competent practitioners”—don’t follow the antipsychotic monitoring guidelines in actual practice. Could failing to follow those guidelines still be the basis for a successful lawsuit?
The answer seems to be ‘yes.’ Published legal decisions describe malpractice lawsuits alleging physicians’ failure to follow antipsychotic guidelines,24,25 and online advertisements show that attorneys believe such cases can generate a payout.26,27 This may seem odd, given what studies say about psychiatrists’ monitoring practices. But determining the “standard of care” in a malpractice case is not an empirical question; it is a legal matter that is decided based on the testimony of expert witnesses.28 Here, customary practice matters, but it’s not the whole story.
Although the standard of care against which courts measure a physician’s actions “is that of a reasonably prudent practitioner …, The degree of care actually practiced by members of the profession is only some evidence of what is reasonably prudent—it is not dispositive.”29 To support their opinion concerning the standard of care, testifying medical witnesses sometimes use practice guidelines. In this case, an explanation of why a particular guideline was chosen is crucial.30
Using guidelines to establish the standard is controversial. On one hand, using guidelines in malpractice litigation allows for some consistency about expectations of practitioners.31,32 Although guidelines are not identical to evidenced-based medicine, they generally reflect an evidence-based expert consensus about sound medical practice. If a hospital uses a guideline to train its employees, the guideline provides the courts with clear information on what should have happened.33,34 Laws in some states allow clinicians to invoke their adherence to a guideline in defense against malpractice claims.35
On the other hand, critics contend that guidelines may not set an accurate standard for the quality of care, nor do they necessarily reflect a proper balance of the conflicting interests of patients and the health care system.36 The American Psychiatric Association states that its practice guidelines “are not intended to serve or be construed as a ‘standard of medical care.’”37
Conformity is not the only measure of prudent practice, and following guidelines does not immunize a clinician from lawsuit if a particular clinical situation demands a different course of action.32 Guidelines can be costly to implement,36 compliance with guidelines generally is low,35 and national guidelines do not necessarily improve the quality of care.38 Last, relying on guidelines to determine the standard of care might stifle innovation or development of alternate approaches by silencing viewpoints.39,40 Table 133-35,39,41 (page 60)summarizes variables that make a guideline more indicative of the standard of care.
Every step you take: Better monitoring
Medical professionals often are slow to update their practice to reflect new knowledge about optimal treatment. But practice guidelines influence the court’s views about the standard of care, and Dr. V’s question shows that he and his colleagues agree that metabolic status needs to be better monitored when patients take antipsychotic drugs. The following discussion and Table 242-45 offer suggestions for how psychiatrists and their practice settings could better accomplish this.
Electronic health records (EHRs). Monitoring health indices often is the largest hurdle that health care professionals face.46 However, large health care systems with EHRs are in a good position to develop and implement automated computer routines that track which patients need monitoring and note due dates, abnormal results, and management interventions.42 Some studies suggest that monitoring rates in both inpatient47 and outpatient48 settings improve with built-in EHR reminders. However, if a system uses too many reminders, the resulting “alert fatigue” will limit their value.22 Providing individual feedback about monitoring practices may enhance physicians’ buy-in to reminder systems.48
Integrated care systems can improve patient outcomes, particularly antipsychotic monitoring. Advantages include shared funding streams, a unified medical record, coordinated scheduling of psychiatric and primary care appointments, and addressing blood-draw refusals.43 More frequent primary care visits make antipsychotic monitoring more likely.11 Ultimately, integrated care could resolve problems related to determining which clinicians are responsible for monitoring and managing adverse metabolic effects.
Third-party payers. Managed care interventions also could improve monitoring rates.44 Prior authorization often requires physicians to obtain appropriate lab work. Insurers might contact physicians with educational interventions, including free webinars, provider alerts, and letters about monitoring rates in their region. Some insurers also provide disease management programs for patients and their caregivers.
Individual and small group practices. Psychiatrists who practice outside a large health care system might designate 2 months each year as “physical health months.” In the “Let’s Get Physical” program,45 physicians were given longer appointment times during these months to address metabolic monitoring, provide education about managing side effects of medication, and encourage better diets and exercise.
Overall, the best techniques might be those implicit to good doctoring: clear and open communication with patients, effective patient education, respect of informed consent, and thorough follow-up.49
1. Mossman D, Steinberg JL. Promoting, prescribing, and pushing pills: understanding the lessons of antipsychotic drug litigation. Michigan St U J Med & Law. 2009;13:263-334.
2. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation: evaluating the risk/benefit equation and improving the standard of care. J Clin Psychopharmacol. 2004;24(5 suppl 1):S7-S14.
3. De Hert M, Schreurs V, Sweers K, et al. Typical and atypical antipsychotics differentially affect long-term incidence rates of the metabolic syndrome in first-episode patients with schizophrenia: a retrospective chart review. Schizophr Res. 2008;101(1-3):295-303.
4. Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.
5. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65(2):267-272.
6. Pappadopulos E, Macintyre JC II, Crismon ML, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. J Am Acad Child Adolesc Psychiatry. 2003;42(2):145-161.
7. Pringsheim T, Panagiotopoulos C, Davidson J, et al; CAMESA guideline group. Evidence-based recommendations for monitoring safety of second generation antipsychotics in children and youth [Erratum in: J Can Acad Adolesc Psychiatry. 2011;20(3):1-2]. J Can Acad Child Adolesc Psychiatry. 2011;20(3):218-233.
8. Gleason MM, Egger HL, Emslie GJ, et al. Psychopharmacological treatment for very young children: contexts and guidelines. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1532-1572.
9. Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychol Med. 2012;42(1):125-147.
10. Baller JB, McGinty EE, Azrin ST, et al. Screening for cardiovascular risk factors in adults with serious mental illness: a review of the evidence. BMC Psychiatry. 2015;15:55.
11. Haupt DW, Rosenblatt LC, Kim E, et al. Prevalence and predictors of lipid monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166(3):345-353.
12. Dhamane AD, Martin BC, Brixner DI, et al. Metabolic monitoring of patients prescribed second-generation antipsychotics. J Psychiatr Pract. 2013;19(5):360-374.
13. Morrato EH, Newcomer JW, Kamat S, et al. Metabolic screening after the American Diabetes Association’s consensus statement on antipsychotic drugs and diabetes. Diabetes Care. 2009;32(6):1037-1042.
14. Morrato EH, Druss B, Hartung DM, et al. Metabolic testing rates in 3 state Medicaid programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Arch Gen Psychiatry. 2010;67(1):17-24.
15. Moeller KE, Rigler SK, Mayorga A, et al. Quality of monitoring for metabolic effects associated with second generation antipsychotics in patients with schizophrenia on public insurance. Schizophr Res. 2011;126(1-3):117-123.
16. Barnett M, VonMuenster S, Wehring H, et al. Assessment of monitoring for glucose and lipid dysregulation in adult Medi-Cal patients newly started on antipsychotics. Ann Clin Psychiatry. 2010;22(1):9-18.
17. Mittal D, Li C, Viverito K, et al. Monitoring for metabolic side effects among outpatients with dementia receiving antipsychotics. Psychiatr Serv. 2014;65(9):1147-1153.
18. Hsu C, Ried LD, Bengtson MA, et al. Metabolic monitoring in veterans with schizophrenia-related disorders and treated with second-generation antipsychotics: findings from a Veterans Affairs-based population. J Am Pharm Assoc. 2008;48(3):393-400.
19. Raebel MA, Penfold R, McMahon AW, et al. Adherence to guidelines for glucose assessment in starting second-generation antipsychotics. Pediatrics. 2014;134(5):e1308-e1314.
20. Connolly JG, Toomey TJ, Schneeweiss MC. Metabolic monitoring for youths initiating use of second-generation antipsychotics, 2003-2011. Psychiatr Serv. 2015;66(6):604-609.
21. Teeluckdharry S, Sharma S, O’Rourke E, et al. Monitoring metabolic side effects of atypical antipsychotics in people with an intellectual disability. J Intellect Disabil. 2013;17(3):223-235.
22. Lee J, Dalack GW, Casher MI, et al. Persistence of metabolic monitoring for psychiatry inpatients treated with second-generation antipsychotics utilizing a computer-based intervention. J Clin Pharm Ther. 2016;41(2):209-213.
23. McCourt v Abernathy, 457 SE2d 603 (SC 1995).
24. Schultz v AstraZeneca Pharma LP, LEXIS 94534, 2006 WL 3797932, (ND Cal 2006).
25. Redmond v AstraZeneca Pharma LP, 492 F Supp 2d 575 (SD Miss 2007).
26. Goguen D. Risperdal, Seroquel, Symbyax, Zyprexa, and other antipsychotic drugs. http://www.nolo.com/legal-encyclopedia/risperdal-seroquel-symbyax-zyprexa-antipsychotics-29866.html. Accessed April 4, 2016.
27. FreeAdvice staff. Risperdal medical malpractice lawsuits: Risperdal injury lawyer explains what you need to know. http://injury-law.freeadvice.com/injury-law/drug-toxic_chemicals/risperdal.htm. Accessed April 4, 2016.
28. Lewis MK, Gohagan JK, Merenstein DJ. The locality rule and the physician’s dilemma: local medical practices vs the national standard of care. JAMA. 2007;297(23):2633-2637.
29. Harris v Groth, 99 Wn2d 438, 663 P2d 113 (1983).
30. Moffett P, Moore G. The standard of care: legal history and definitions: the bad and good news. West J Emerg Med. 2011;12(1):109-112.
31. Taylor C. The use of clinical practice guidelines in determining standard of care. J Legal Med. 2014;35(2):273-290.
32. Bal BS, Brenner LH. Medicolegal sidebar: the law and social values: conformity to norms. Clin Orthop Relat Res. 2015;473(5):1555-1559.
33. Recupero PR. Clinical practice guidelines as learned treatises: understanding their use as evidence in the courtroom. J Am Acad Psychiatry Law. 2008;36(3):290-301.
34. Price v Cleveland Clinic Found, 515 NE2d 931 (Ohio Ct App 1986).
35. Zonana H. Commentary: when is a practice guideline only a guideline? J Am Acad Psychiatry Law. 2008;36(3):302-305.
36. Guillod O. Clinical guidelines and professional liability: a short comment from the legal side. ORL J Otorhinolaryngol Relat Spec. 2010;72(3):133-136; discussion 136-137.
37. American Psychiatric Association. Practice guidelines for the psychiatric evaluation of adults. 3rd ed. Arlington, VA: American Psychiatric Association; 2016.
38. Brouwers MC, Kho ME, Browman GP, et al; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839-E842.
39. Vermaas AM. Liability in relation to the use of professional medical guidelines. Med Law. 2003;22(2):233-238.
40. Strauss DC, Thomas JM. What does the medical profession mean by “standard of care?”. J Clin Oncol. 2009;27(32):e192-e193.
41. Kozlick D. Clinical practice guidelines and the legal standard of care: warnings, predictions, and interdisciplinary encounters. Health Law J. 2011;19:125-151.
42. Owen RR, Drummond KL, Viverito KM, et al. Monitoring and managing metabolic effects of antipsychotics: a cluster randomized trial of an intervention combining evidence-based quality improvement and external facilitation. Implement Sci. 2013;8:120.
43. Ruiz LM, Damron M, Jones KB, et al. Antipsychotic use and metabolic monitoring in individuals with developmental disabilities served in a Medicaid medical home [published online January 27, 2016]. J Autism Dev Disord. doi: 10.1007/s10803-016-2712-x.
44. Edelsohn GA, Parthasarathy M, Terhorst L, et al. Measurement of metabolic monitoring in youth and adult Medicaid recipients prescribed antipsychotics. J Manag Care Spec Pharm. 2015;21(9):769-77,777a-777cc.
45. Wilson E, Randall C, Patterson S, et al. Monitoring and management of metabolic abnormalities: mixed-method evaluation of a successful intervention. Australas Psychiatry. 2014;22(3):248-253.
46. Cohn TA, Sernyak MJ. Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry. 2006;51(8):492-501.
47. DelMonte MT, Bostwick JR, Bess JD, et al. Evaluation of a computer-based intervention to enhance metabolic monitoring in psychiatry inpatients treated with second-generation antipsychotics. J Clin Pharm Ther. 2012;37(6):668-673.
48. Lai CL, Chan HY, Pan YJ, et al. The effectiveness of a computer reminder system for laboratory monitoring of metabolic syndrome in schizophrenic outpatients using second-generation antipsychotics. Pharmacopsychiatry. 2015;48(1):25-29.
49. Bailey RK, Adams JB, Unger DM. Atypical antipsychotics: a case study in new era risk management. J Psychiatr Pract. 2006;12(4):253-258.
Dear Dr. Mossman,
All the psychiatrists at our clinic agree: It is hard to remember when our patients who take an antipsychotic are due for metabolic monitoring, and it’s even harder to get many of them to follow through with timely blood tests. For many, stopping their medication would be a bad idea. If we keep a patient on an antipsychotic and a metabolic problem results, how serious is our malpractice liability risk?
Submitted by “Dr. V”
Antipsychotics, the mainstay of treatment for schizophrenia,1 put patients at risk of gaining weight and developing metabolic syndrome, including type 2 diabetes mellitus, hypertension, and dyslipidemia.2 Second-generation antipsychotics are the biggest offenders, but taking a first-generation antipsychotic also can lead to these adverse effects.3
Most psychiatrists are aware of these risks and prefer that their patients do not experience them. However, many psychiatrists neglect proper monitoring or, like Dr. V, find it hard to ensure it happens and thus worry about clinical deterioration if patients stop taking an antipsychotic.4 If you are in the same situation as Dr. V, what medicolegal risks are you facing?
To answer this question, we will:
- review the clinical guidelines and standards for monitoring metabolic effects of antipsychotics
- examine how well (or poorly) physicians adhere to these standards
- discuss what “standard of care” means and how a practice guideline affects the standard effects
- propose how psychiatrists can do better at policing the metabolic effects of antipsychotics.
I’ll be watching you: Following guidelines
Several medical specialty societies have published guidelines for monitoring the metabolic effects of antipsychotics.5-8 These guidelines instruct physicians to obtain a thorough personal and family history; consider metabolic risks when starting a medication; and monitor weight, waist circumference, blood pressure, glucose, hemoglobin A1c, and lipids at various intervals. They also advise referral for management of detected metabolic problems.
Although the recommendations seem clear, many physicians don’t follow them. A 2012 meta-analysis of 48 studies, covering >200,000 antipsychotic-treated patients, showed that baseline measurements of cholesterol, glucose, and weight occurred in <50% of cases.9 A more recent review found that, among adults with a serious mental illness, the rate of lipid testing varied from 6% to 85% and for glucose monitoring, between 18% and 75%.10 In the first years after antipsychotic monitoring guidelines were established, they had only a modest impact on practice,9,11 and some studies showed the guidelines made no difference at all.12-14
Monitoring compliance varies with the type of insurance coverage patients have but remains suboptimal among the commercially insured,11 Medicaid patients,14-16 and veterans.17,18 Studies on antipsychotic treatment in children, adolescents, patients with dementia, and patients with an intellectual disability show insufficient monitoring as well.9,14,17,19-21 The reasons for these gaps are manifold, but one commonly cited factor is uncertainty about whether the psychiatrist or primary care physician should handle monitoring.22
Every claim you stake: The ‘standard of care’
In a medical malpractice case, the party claiming injury must show that the accused physician failed to follow “the generally recognized practices and procedures which would be exercised by ordinary competent practitioners in a defendant doctor’s field of medicine under the same or similar circumstances.”23 In the studies mentioned above,9-14 a large fraction of psychiatrists—many of whom, we can presume, are “competent practitioners”—don’t follow the antipsychotic monitoring guidelines in actual practice. Could failing to follow those guidelines still be the basis for a successful lawsuit?
The answer seems to be ‘yes.’ Published legal decisions describe malpractice lawsuits alleging physicians’ failure to follow antipsychotic guidelines,24,25 and online advertisements show that attorneys believe such cases can generate a payout.26,27 This may seem odd, given what studies say about psychiatrists’ monitoring practices. But determining the “standard of care” in a malpractice case is not an empirical question; it is a legal matter that is decided based on the testimony of expert witnesses.28 Here, customary practice matters, but it’s not the whole story.
Although the standard of care against which courts measure a physician’s actions “is that of a reasonably prudent practitioner …, The degree of care actually practiced by members of the profession is only some evidence of what is reasonably prudent—it is not dispositive.”29 To support their opinion concerning the standard of care, testifying medical witnesses sometimes use practice guidelines. In this case, an explanation of why a particular guideline was chosen is crucial.30
Using guidelines to establish the standard is controversial. On one hand, using guidelines in malpractice litigation allows for some consistency about expectations of practitioners.31,32 Although guidelines are not identical to evidenced-based medicine, they generally reflect an evidence-based expert consensus about sound medical practice. If a hospital uses a guideline to train its employees, the guideline provides the courts with clear information on what should have happened.33,34 Laws in some states allow clinicians to invoke their adherence to a guideline in defense against malpractice claims.35
On the other hand, critics contend that guidelines may not set an accurate standard for the quality of care, nor do they necessarily reflect a proper balance of the conflicting interests of patients and the health care system.36 The American Psychiatric Association states that its practice guidelines “are not intended to serve or be construed as a ‘standard of medical care.’”37
Conformity is not the only measure of prudent practice, and following guidelines does not immunize a clinician from lawsuit if a particular clinical situation demands a different course of action.32 Guidelines can be costly to implement,36 compliance with guidelines generally is low,35 and national guidelines do not necessarily improve the quality of care.38 Last, relying on guidelines to determine the standard of care might stifle innovation or development of alternate approaches by silencing viewpoints.39,40 Table 133-35,39,41 (page 60)summarizes variables that make a guideline more indicative of the standard of care.
Every step you take: Better monitoring
Medical professionals often are slow to update their practice to reflect new knowledge about optimal treatment. But practice guidelines influence the court’s views about the standard of care, and Dr. V’s question shows that he and his colleagues agree that metabolic status needs to be better monitored when patients take antipsychotic drugs. The following discussion and Table 242-45 offer suggestions for how psychiatrists and their practice settings could better accomplish this.
Electronic health records (EHRs). Monitoring health indices often is the largest hurdle that health care professionals face.46 However, large health care systems with EHRs are in a good position to develop and implement automated computer routines that track which patients need monitoring and note due dates, abnormal results, and management interventions.42 Some studies suggest that monitoring rates in both inpatient47 and outpatient48 settings improve with built-in EHR reminders. However, if a system uses too many reminders, the resulting “alert fatigue” will limit their value.22 Providing individual feedback about monitoring practices may enhance physicians’ buy-in to reminder systems.48
Integrated care systems can improve patient outcomes, particularly antipsychotic monitoring. Advantages include shared funding streams, a unified medical record, coordinated scheduling of psychiatric and primary care appointments, and addressing blood-draw refusals.43 More frequent primary care visits make antipsychotic monitoring more likely.11 Ultimately, integrated care could resolve problems related to determining which clinicians are responsible for monitoring and managing adverse metabolic effects.
Third-party payers. Managed care interventions also could improve monitoring rates.44 Prior authorization often requires physicians to obtain appropriate lab work. Insurers might contact physicians with educational interventions, including free webinars, provider alerts, and letters about monitoring rates in their region. Some insurers also provide disease management programs for patients and their caregivers.
Individual and small group practices. Psychiatrists who practice outside a large health care system might designate 2 months each year as “physical health months.” In the “Let’s Get Physical” program,45 physicians were given longer appointment times during these months to address metabolic monitoring, provide education about managing side effects of medication, and encourage better diets and exercise.
Overall, the best techniques might be those implicit to good doctoring: clear and open communication with patients, effective patient education, respect of informed consent, and thorough follow-up.49
Dear Dr. Mossman,
All the psychiatrists at our clinic agree: It is hard to remember when our patients who take an antipsychotic are due for metabolic monitoring, and it’s even harder to get many of them to follow through with timely blood tests. For many, stopping their medication would be a bad idea. If we keep a patient on an antipsychotic and a metabolic problem results, how serious is our malpractice liability risk?
Submitted by “Dr. V”
Antipsychotics, the mainstay of treatment for schizophrenia,1 put patients at risk of gaining weight and developing metabolic syndrome, including type 2 diabetes mellitus, hypertension, and dyslipidemia.2 Second-generation antipsychotics are the biggest offenders, but taking a first-generation antipsychotic also can lead to these adverse effects.3
Most psychiatrists are aware of these risks and prefer that their patients do not experience them. However, many psychiatrists neglect proper monitoring or, like Dr. V, find it hard to ensure it happens and thus worry about clinical deterioration if patients stop taking an antipsychotic.4 If you are in the same situation as Dr. V, what medicolegal risks are you facing?
To answer this question, we will:
- review the clinical guidelines and standards for monitoring metabolic effects of antipsychotics
- examine how well (or poorly) physicians adhere to these standards
- discuss what “standard of care” means and how a practice guideline affects the standard effects
- propose how psychiatrists can do better at policing the metabolic effects of antipsychotics.
I’ll be watching you: Following guidelines
Several medical specialty societies have published guidelines for monitoring the metabolic effects of antipsychotics.5-8 These guidelines instruct physicians to obtain a thorough personal and family history; consider metabolic risks when starting a medication; and monitor weight, waist circumference, blood pressure, glucose, hemoglobin A1c, and lipids at various intervals. They also advise referral for management of detected metabolic problems.
Although the recommendations seem clear, many physicians don’t follow them. A 2012 meta-analysis of 48 studies, covering >200,000 antipsychotic-treated patients, showed that baseline measurements of cholesterol, glucose, and weight occurred in <50% of cases.9 A more recent review found that, among adults with a serious mental illness, the rate of lipid testing varied from 6% to 85% and for glucose monitoring, between 18% and 75%.10 In the first years after antipsychotic monitoring guidelines were established, they had only a modest impact on practice,9,11 and some studies showed the guidelines made no difference at all.12-14
Monitoring compliance varies with the type of insurance coverage patients have but remains suboptimal among the commercially insured,11 Medicaid patients,14-16 and veterans.17,18 Studies on antipsychotic treatment in children, adolescents, patients with dementia, and patients with an intellectual disability show insufficient monitoring as well.9,14,17,19-21 The reasons for these gaps are manifold, but one commonly cited factor is uncertainty about whether the psychiatrist or primary care physician should handle monitoring.22
Every claim you stake: The ‘standard of care’
In a medical malpractice case, the party claiming injury must show that the accused physician failed to follow “the generally recognized practices and procedures which would be exercised by ordinary competent practitioners in a defendant doctor’s field of medicine under the same or similar circumstances.”23 In the studies mentioned above,9-14 a large fraction of psychiatrists—many of whom, we can presume, are “competent practitioners”—don’t follow the antipsychotic monitoring guidelines in actual practice. Could failing to follow those guidelines still be the basis for a successful lawsuit?
The answer seems to be ‘yes.’ Published legal decisions describe malpractice lawsuits alleging physicians’ failure to follow antipsychotic guidelines,24,25 and online advertisements show that attorneys believe such cases can generate a payout.26,27 This may seem odd, given what studies say about psychiatrists’ monitoring practices. But determining the “standard of care” in a malpractice case is not an empirical question; it is a legal matter that is decided based on the testimony of expert witnesses.28 Here, customary practice matters, but it’s not the whole story.
Although the standard of care against which courts measure a physician’s actions “is that of a reasonably prudent practitioner …, The degree of care actually practiced by members of the profession is only some evidence of what is reasonably prudent—it is not dispositive.”29 To support their opinion concerning the standard of care, testifying medical witnesses sometimes use practice guidelines. In this case, an explanation of why a particular guideline was chosen is crucial.30
Using guidelines to establish the standard is controversial. On one hand, using guidelines in malpractice litigation allows for some consistency about expectations of practitioners.31,32 Although guidelines are not identical to evidenced-based medicine, they generally reflect an evidence-based expert consensus about sound medical practice. If a hospital uses a guideline to train its employees, the guideline provides the courts with clear information on what should have happened.33,34 Laws in some states allow clinicians to invoke their adherence to a guideline in defense against malpractice claims.35
On the other hand, critics contend that guidelines may not set an accurate standard for the quality of care, nor do they necessarily reflect a proper balance of the conflicting interests of patients and the health care system.36 The American Psychiatric Association states that its practice guidelines “are not intended to serve or be construed as a ‘standard of medical care.’”37
Conformity is not the only measure of prudent practice, and following guidelines does not immunize a clinician from lawsuit if a particular clinical situation demands a different course of action.32 Guidelines can be costly to implement,36 compliance with guidelines generally is low,35 and national guidelines do not necessarily improve the quality of care.38 Last, relying on guidelines to determine the standard of care might stifle innovation or development of alternate approaches by silencing viewpoints.39,40 Table 133-35,39,41 (page 60)summarizes variables that make a guideline more indicative of the standard of care.
Every step you take: Better monitoring
Medical professionals often are slow to update their practice to reflect new knowledge about optimal treatment. But practice guidelines influence the court’s views about the standard of care, and Dr. V’s question shows that he and his colleagues agree that metabolic status needs to be better monitored when patients take antipsychotic drugs. The following discussion and Table 242-45 offer suggestions for how psychiatrists and their practice settings could better accomplish this.
Electronic health records (EHRs). Monitoring health indices often is the largest hurdle that health care professionals face.46 However, large health care systems with EHRs are in a good position to develop and implement automated computer routines that track which patients need monitoring and note due dates, abnormal results, and management interventions.42 Some studies suggest that monitoring rates in both inpatient47 and outpatient48 settings improve with built-in EHR reminders. However, if a system uses too many reminders, the resulting “alert fatigue” will limit their value.22 Providing individual feedback about monitoring practices may enhance physicians’ buy-in to reminder systems.48
Integrated care systems can improve patient outcomes, particularly antipsychotic monitoring. Advantages include shared funding streams, a unified medical record, coordinated scheduling of psychiatric and primary care appointments, and addressing blood-draw refusals.43 More frequent primary care visits make antipsychotic monitoring more likely.11 Ultimately, integrated care could resolve problems related to determining which clinicians are responsible for monitoring and managing adverse metabolic effects.
Third-party payers. Managed care interventions also could improve monitoring rates.44 Prior authorization often requires physicians to obtain appropriate lab work. Insurers might contact physicians with educational interventions, including free webinars, provider alerts, and letters about monitoring rates in their region. Some insurers also provide disease management programs for patients and their caregivers.
Individual and small group practices. Psychiatrists who practice outside a large health care system might designate 2 months each year as “physical health months.” In the “Let’s Get Physical” program,45 physicians were given longer appointment times during these months to address metabolic monitoring, provide education about managing side effects of medication, and encourage better diets and exercise.
Overall, the best techniques might be those implicit to good doctoring: clear and open communication with patients, effective patient education, respect of informed consent, and thorough follow-up.49
1. Mossman D, Steinberg JL. Promoting, prescribing, and pushing pills: understanding the lessons of antipsychotic drug litigation. Michigan St U J Med & Law. 2009;13:263-334.
2. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation: evaluating the risk/benefit equation and improving the standard of care. J Clin Psychopharmacol. 2004;24(5 suppl 1):S7-S14.
3. De Hert M, Schreurs V, Sweers K, et al. Typical and atypical antipsychotics differentially affect long-term incidence rates of the metabolic syndrome in first-episode patients with schizophrenia: a retrospective chart review. Schizophr Res. 2008;101(1-3):295-303.
4. Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.
5. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65(2):267-272.
6. Pappadopulos E, Macintyre JC II, Crismon ML, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. J Am Acad Child Adolesc Psychiatry. 2003;42(2):145-161.
7. Pringsheim T, Panagiotopoulos C, Davidson J, et al; CAMESA guideline group. Evidence-based recommendations for monitoring safety of second generation antipsychotics in children and youth [Erratum in: J Can Acad Adolesc Psychiatry. 2011;20(3):1-2]. J Can Acad Child Adolesc Psychiatry. 2011;20(3):218-233.
8. Gleason MM, Egger HL, Emslie GJ, et al. Psychopharmacological treatment for very young children: contexts and guidelines. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1532-1572.
9. Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychol Med. 2012;42(1):125-147.
10. Baller JB, McGinty EE, Azrin ST, et al. Screening for cardiovascular risk factors in adults with serious mental illness: a review of the evidence. BMC Psychiatry. 2015;15:55.
11. Haupt DW, Rosenblatt LC, Kim E, et al. Prevalence and predictors of lipid monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166(3):345-353.
12. Dhamane AD, Martin BC, Brixner DI, et al. Metabolic monitoring of patients prescribed second-generation antipsychotics. J Psychiatr Pract. 2013;19(5):360-374.
13. Morrato EH, Newcomer JW, Kamat S, et al. Metabolic screening after the American Diabetes Association’s consensus statement on antipsychotic drugs and diabetes. Diabetes Care. 2009;32(6):1037-1042.
14. Morrato EH, Druss B, Hartung DM, et al. Metabolic testing rates in 3 state Medicaid programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Arch Gen Psychiatry. 2010;67(1):17-24.
15. Moeller KE, Rigler SK, Mayorga A, et al. Quality of monitoring for metabolic effects associated with second generation antipsychotics in patients with schizophrenia on public insurance. Schizophr Res. 2011;126(1-3):117-123.
16. Barnett M, VonMuenster S, Wehring H, et al. Assessment of monitoring for glucose and lipid dysregulation in adult Medi-Cal patients newly started on antipsychotics. Ann Clin Psychiatry. 2010;22(1):9-18.
17. Mittal D, Li C, Viverito K, et al. Monitoring for metabolic side effects among outpatients with dementia receiving antipsychotics. Psychiatr Serv. 2014;65(9):1147-1153.
18. Hsu C, Ried LD, Bengtson MA, et al. Metabolic monitoring in veterans with schizophrenia-related disorders and treated with second-generation antipsychotics: findings from a Veterans Affairs-based population. J Am Pharm Assoc. 2008;48(3):393-400.
19. Raebel MA, Penfold R, McMahon AW, et al. Adherence to guidelines for glucose assessment in starting second-generation antipsychotics. Pediatrics. 2014;134(5):e1308-e1314.
20. Connolly JG, Toomey TJ, Schneeweiss MC. Metabolic monitoring for youths initiating use of second-generation antipsychotics, 2003-2011. Psychiatr Serv. 2015;66(6):604-609.
21. Teeluckdharry S, Sharma S, O’Rourke E, et al. Monitoring metabolic side effects of atypical antipsychotics in people with an intellectual disability. J Intellect Disabil. 2013;17(3):223-235.
22. Lee J, Dalack GW, Casher MI, et al. Persistence of metabolic monitoring for psychiatry inpatients treated with second-generation antipsychotics utilizing a computer-based intervention. J Clin Pharm Ther. 2016;41(2):209-213.
23. McCourt v Abernathy, 457 SE2d 603 (SC 1995).
24. Schultz v AstraZeneca Pharma LP, LEXIS 94534, 2006 WL 3797932, (ND Cal 2006).
25. Redmond v AstraZeneca Pharma LP, 492 F Supp 2d 575 (SD Miss 2007).
26. Goguen D. Risperdal, Seroquel, Symbyax, Zyprexa, and other antipsychotic drugs. http://www.nolo.com/legal-encyclopedia/risperdal-seroquel-symbyax-zyprexa-antipsychotics-29866.html. Accessed April 4, 2016.
27. FreeAdvice staff. Risperdal medical malpractice lawsuits: Risperdal injury lawyer explains what you need to know. http://injury-law.freeadvice.com/injury-law/drug-toxic_chemicals/risperdal.htm. Accessed April 4, 2016.
28. Lewis MK, Gohagan JK, Merenstein DJ. The locality rule and the physician’s dilemma: local medical practices vs the national standard of care. JAMA. 2007;297(23):2633-2637.
29. Harris v Groth, 99 Wn2d 438, 663 P2d 113 (1983).
30. Moffett P, Moore G. The standard of care: legal history and definitions: the bad and good news. West J Emerg Med. 2011;12(1):109-112.
31. Taylor C. The use of clinical practice guidelines in determining standard of care. J Legal Med. 2014;35(2):273-290.
32. Bal BS, Brenner LH. Medicolegal sidebar: the law and social values: conformity to norms. Clin Orthop Relat Res. 2015;473(5):1555-1559.
33. Recupero PR. Clinical practice guidelines as learned treatises: understanding their use as evidence in the courtroom. J Am Acad Psychiatry Law. 2008;36(3):290-301.
34. Price v Cleveland Clinic Found, 515 NE2d 931 (Ohio Ct App 1986).
35. Zonana H. Commentary: when is a practice guideline only a guideline? J Am Acad Psychiatry Law. 2008;36(3):302-305.
36. Guillod O. Clinical guidelines and professional liability: a short comment from the legal side. ORL J Otorhinolaryngol Relat Spec. 2010;72(3):133-136; discussion 136-137.
37. American Psychiatric Association. Practice guidelines for the psychiatric evaluation of adults. 3rd ed. Arlington, VA: American Psychiatric Association; 2016.
38. Brouwers MC, Kho ME, Browman GP, et al; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839-E842.
39. Vermaas AM. Liability in relation to the use of professional medical guidelines. Med Law. 2003;22(2):233-238.
40. Strauss DC, Thomas JM. What does the medical profession mean by “standard of care?”. J Clin Oncol. 2009;27(32):e192-e193.
41. Kozlick D. Clinical practice guidelines and the legal standard of care: warnings, predictions, and interdisciplinary encounters. Health Law J. 2011;19:125-151.
42. Owen RR, Drummond KL, Viverito KM, et al. Monitoring and managing metabolic effects of antipsychotics: a cluster randomized trial of an intervention combining evidence-based quality improvement and external facilitation. Implement Sci. 2013;8:120.
43. Ruiz LM, Damron M, Jones KB, et al. Antipsychotic use and metabolic monitoring in individuals with developmental disabilities served in a Medicaid medical home [published online January 27, 2016]. J Autism Dev Disord. doi: 10.1007/s10803-016-2712-x.
44. Edelsohn GA, Parthasarathy M, Terhorst L, et al. Measurement of metabolic monitoring in youth and adult Medicaid recipients prescribed antipsychotics. J Manag Care Spec Pharm. 2015;21(9):769-77,777a-777cc.
45. Wilson E, Randall C, Patterson S, et al. Monitoring and management of metabolic abnormalities: mixed-method evaluation of a successful intervention. Australas Psychiatry. 2014;22(3):248-253.
46. Cohn TA, Sernyak MJ. Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry. 2006;51(8):492-501.
47. DelMonte MT, Bostwick JR, Bess JD, et al. Evaluation of a computer-based intervention to enhance metabolic monitoring in psychiatry inpatients treated with second-generation antipsychotics. J Clin Pharm Ther. 2012;37(6):668-673.
48. Lai CL, Chan HY, Pan YJ, et al. The effectiveness of a computer reminder system for laboratory monitoring of metabolic syndrome in schizophrenic outpatients using second-generation antipsychotics. Pharmacopsychiatry. 2015;48(1):25-29.
49. Bailey RK, Adams JB, Unger DM. Atypical antipsychotics: a case study in new era risk management. J Psychiatr Pract. 2006;12(4):253-258.
1. Mossman D, Steinberg JL. Promoting, prescribing, and pushing pills: understanding the lessons of antipsychotic drug litigation. Michigan St U J Med & Law. 2009;13:263-334.
2. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation: evaluating the risk/benefit equation and improving the standard of care. J Clin Psychopharmacol. 2004;24(5 suppl 1):S7-S14.
3. De Hert M, Schreurs V, Sweers K, et al. Typical and atypical antipsychotics differentially affect long-term incidence rates of the metabolic syndrome in first-episode patients with schizophrenia: a retrospective chart review. Schizophr Res. 2008;101(1-3):295-303.
4. Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.
5. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65(2):267-272.
6. Pappadopulos E, Macintyre JC II, Crismon ML, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. J Am Acad Child Adolesc Psychiatry. 2003;42(2):145-161.
7. Pringsheim T, Panagiotopoulos C, Davidson J, et al; CAMESA guideline group. Evidence-based recommendations for monitoring safety of second generation antipsychotics in children and youth [Erratum in: J Can Acad Adolesc Psychiatry. 2011;20(3):1-2]. J Can Acad Child Adolesc Psychiatry. 2011;20(3):218-233.
8. Gleason MM, Egger HL, Emslie GJ, et al. Psychopharmacological treatment for very young children: contexts and guidelines. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1532-1572.
9. Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychol Med. 2012;42(1):125-147.
10. Baller JB, McGinty EE, Azrin ST, et al. Screening for cardiovascular risk factors in adults with serious mental illness: a review of the evidence. BMC Psychiatry. 2015;15:55.
11. Haupt DW, Rosenblatt LC, Kim E, et al. Prevalence and predictors of lipid monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166(3):345-353.
12. Dhamane AD, Martin BC, Brixner DI, et al. Metabolic monitoring of patients prescribed second-generation antipsychotics. J Psychiatr Pract. 2013;19(5):360-374.
13. Morrato EH, Newcomer JW, Kamat S, et al. Metabolic screening after the American Diabetes Association’s consensus statement on antipsychotic drugs and diabetes. Diabetes Care. 2009;32(6):1037-1042.
14. Morrato EH, Druss B, Hartung DM, et al. Metabolic testing rates in 3 state Medicaid programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Arch Gen Psychiatry. 2010;67(1):17-24.
15. Moeller KE, Rigler SK, Mayorga A, et al. Quality of monitoring for metabolic effects associated with second generation antipsychotics in patients with schizophrenia on public insurance. Schizophr Res. 2011;126(1-3):117-123.
16. Barnett M, VonMuenster S, Wehring H, et al. Assessment of monitoring for glucose and lipid dysregulation in adult Medi-Cal patients newly started on antipsychotics. Ann Clin Psychiatry. 2010;22(1):9-18.
17. Mittal D, Li C, Viverito K, et al. Monitoring for metabolic side effects among outpatients with dementia receiving antipsychotics. Psychiatr Serv. 2014;65(9):1147-1153.
18. Hsu C, Ried LD, Bengtson MA, et al. Metabolic monitoring in veterans with schizophrenia-related disorders and treated with second-generation antipsychotics: findings from a Veterans Affairs-based population. J Am Pharm Assoc. 2008;48(3):393-400.
19. Raebel MA, Penfold R, McMahon AW, et al. Adherence to guidelines for glucose assessment in starting second-generation antipsychotics. Pediatrics. 2014;134(5):e1308-e1314.
20. Connolly JG, Toomey TJ, Schneeweiss MC. Metabolic monitoring for youths initiating use of second-generation antipsychotics, 2003-2011. Psychiatr Serv. 2015;66(6):604-609.
21. Teeluckdharry S, Sharma S, O’Rourke E, et al. Monitoring metabolic side effects of atypical antipsychotics in people with an intellectual disability. J Intellect Disabil. 2013;17(3):223-235.
22. Lee J, Dalack GW, Casher MI, et al. Persistence of metabolic monitoring for psychiatry inpatients treated with second-generation antipsychotics utilizing a computer-based intervention. J Clin Pharm Ther. 2016;41(2):209-213.
23. McCourt v Abernathy, 457 SE2d 603 (SC 1995).
24. Schultz v AstraZeneca Pharma LP, LEXIS 94534, 2006 WL 3797932, (ND Cal 2006).
25. Redmond v AstraZeneca Pharma LP, 492 F Supp 2d 575 (SD Miss 2007).
26. Goguen D. Risperdal, Seroquel, Symbyax, Zyprexa, and other antipsychotic drugs. http://www.nolo.com/legal-encyclopedia/risperdal-seroquel-symbyax-zyprexa-antipsychotics-29866.html. Accessed April 4, 2016.
27. FreeAdvice staff. Risperdal medical malpractice lawsuits: Risperdal injury lawyer explains what you need to know. http://injury-law.freeadvice.com/injury-law/drug-toxic_chemicals/risperdal.htm. Accessed April 4, 2016.
28. Lewis MK, Gohagan JK, Merenstein DJ. The locality rule and the physician’s dilemma: local medical practices vs the national standard of care. JAMA. 2007;297(23):2633-2637.
29. Harris v Groth, 99 Wn2d 438, 663 P2d 113 (1983).
30. Moffett P, Moore G. The standard of care: legal history and definitions: the bad and good news. West J Emerg Med. 2011;12(1):109-112.
31. Taylor C. The use of clinical practice guidelines in determining standard of care. J Legal Med. 2014;35(2):273-290.
32. Bal BS, Brenner LH. Medicolegal sidebar: the law and social values: conformity to norms. Clin Orthop Relat Res. 2015;473(5):1555-1559.
33. Recupero PR. Clinical practice guidelines as learned treatises: understanding their use as evidence in the courtroom. J Am Acad Psychiatry Law. 2008;36(3):290-301.
34. Price v Cleveland Clinic Found, 515 NE2d 931 (Ohio Ct App 1986).
35. Zonana H. Commentary: when is a practice guideline only a guideline? J Am Acad Psychiatry Law. 2008;36(3):302-305.
36. Guillod O. Clinical guidelines and professional liability: a short comment from the legal side. ORL J Otorhinolaryngol Relat Spec. 2010;72(3):133-136; discussion 136-137.
37. American Psychiatric Association. Practice guidelines for the psychiatric evaluation of adults. 3rd ed. Arlington, VA: American Psychiatric Association; 2016.
38. Brouwers MC, Kho ME, Browman GP, et al; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839-E842.
39. Vermaas AM. Liability in relation to the use of professional medical guidelines. Med Law. 2003;22(2):233-238.
40. Strauss DC, Thomas JM. What does the medical profession mean by “standard of care?”. J Clin Oncol. 2009;27(32):e192-e193.
41. Kozlick D. Clinical practice guidelines and the legal standard of care: warnings, predictions, and interdisciplinary encounters. Health Law J. 2011;19:125-151.
42. Owen RR, Drummond KL, Viverito KM, et al. Monitoring and managing metabolic effects of antipsychotics: a cluster randomized trial of an intervention combining evidence-based quality improvement and external facilitation. Implement Sci. 2013;8:120.
43. Ruiz LM, Damron M, Jones KB, et al. Antipsychotic use and metabolic monitoring in individuals with developmental disabilities served in a Medicaid medical home [published online January 27, 2016]. J Autism Dev Disord. doi: 10.1007/s10803-016-2712-x.
44. Edelsohn GA, Parthasarathy M, Terhorst L, et al. Measurement of metabolic monitoring in youth and adult Medicaid recipients prescribed antipsychotics. J Manag Care Spec Pharm. 2015;21(9):769-77,777a-777cc.
45. Wilson E, Randall C, Patterson S, et al. Monitoring and management of metabolic abnormalities: mixed-method evaluation of a successful intervention. Australas Psychiatry. 2014;22(3):248-253.
46. Cohn TA, Sernyak MJ. Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry. 2006;51(8):492-501.
47. DelMonte MT, Bostwick JR, Bess JD, et al. Evaluation of a computer-based intervention to enhance metabolic monitoring in psychiatry inpatients treated with second-generation antipsychotics. J Clin Pharm Ther. 2012;37(6):668-673.
48. Lai CL, Chan HY, Pan YJ, et al. The effectiveness of a computer reminder system for laboratory monitoring of metabolic syndrome in schizophrenic outpatients using second-generation antipsychotics. Pharmacopsychiatry. 2015;48(1):25-29.
49. Bailey RK, Adams JB, Unger DM. Atypical antipsychotics: a case study in new era risk management. J Psychiatr Pract. 2006;12(4):253-258.
Peaceful feeling, or up in smoke? Medical marijuana in medicolegal context
Dear Dr. Mossman,
I practice in a state that allows medical marijuana use. A few of my patients have asked me to help them obtain marijuana for their conditions. How risky would it be to oblige?
Submitted by “Dr. J”
In recent years, public debate about marijuana has acquired 2 new dimensions: (1) the wishes and medical needs of people who seek marijuana for its purported health benefits, and (2) the role of physicians who practice where “medical marijuana” is legal. This article, the authors’ joint effort to address Dr. J’s concerns, hits 3 topics:
• the intersection of marijuana policy and health care in the United States
• the risks and possible benefits of marijuana use
• the medicolegal problems faced by physicians who might advise patients to use marijuana.
Legal haze
Two cannabinoids—dronabinol and nabilone—have received FDA approval as appetite enhancers and anti-nausea agents. Third-party payors usually cover these types of medications, but no insurer pays for medical marijuana.1 The Controlled Substances Act of 19702 classified marijuana as a Schedule I drug because of its abuse potential, lack of accepted medical applications, and uncertain safety. The FDA has not approved marijuana use for any medical condition.
Although people commonly speak of “prescribing” marijuana, physicians cannot legally do this in the United States. What physicians may do, in the 23 states that allow medical marijuana, is recommend or certify a patient’s marijuana use—an action that has constitutional protection under the First Amendment’s freedom of speech clause.3,4
A physician may complete documentation that a patient has one of the qualifying medical conditions for which the jurisdiction has legalized medical marijuana. Either the patient or the physician then submits that documentation to the appropriate government agency (eg, the state’s department of health).
If the documentation receives approval, the agency will issue the patient a registration card that allows possession of medical marijuana, with which the patient can obtain or grow a small amount of marijuana. The cannabinoid content of marijuana products varies considerably,5 and physicians who certify marijuana typically defer dosage recommendations to the patient or the dispensary.1
In states that allow medical marijuana, users may assert an affirmative defense of medical necessity if they face criminal prosecution.3,6 Possession of marijuana remains illegal under federal law, however, regardless of one’s reason for having it.7,8 Since October 2009, the Attorney General’s office has discouraged federal prosecutions of persons “whose actions are in clear and unambiguous compliance with existing state laws providing for the medical use of marijuana.”9 But given the remaining conflicts between state and federal laws, “the legal implications of certifying patients for medical marijuana remain unclear.”10
Physicians have few resources to instruct them on the legal risks of certifying medical marijuana. When Canada legalized medical marijuana, the organization that provides malpractice insurance to Canadian physicians told its members that “prescribing medical marijuana cannot be compared to prescribing prescription drugs” and recommended that physicians obtain signed release forms documenting that they have discussed the risks of medical marijuana with patients.11 For some risky approved drugs, the FDA has established a risk evaluation and mitigation strategy, but no such guidance is available for marijuana.
Highlighting the benefits and risks
Proponents of medical marijuana claim that Cannabis can help patients, and dispassionate experts acknowledge that at least modest evidence supports the benefits of using “marijuana for nausea and vomiting related to chemotherapy, specific pain syndromes, and spasticity from multiple sclerosis.”10 For several other conditions— HIV/AIDS, depression, anxiety disorders, sleep disorders, psychosis, Tourette syndrome—evidence of benefit is poor.12 Rigorous evaluation of medical marijuana is difficult because the plant contains hundreds of active chemical compounds. The chemical content of marijuana is highly variable, depending on its preparation and administration,10,13—one reason why only a few good randomized controlled trials of marijuana have been conducted.
Marijuana has several side effects and carries many health risks (Table 1).4,14-20
On the highway: Marijuana and driving
Marijuana use impairs driving ability.14 Following enactment of more lenient marijuana laws, several states have reported higher numbers of fatally injured drivers who tested positive for Cannabis21-23 and had a positive screen of tetrahydrocannabinol (THC) in driving under the influence cases.24,25 One study showed that a blood THC concentration >5 ng/mL (comparable to a blood alcohol concentration of 0.15%) increased the crash odds ratio to 6.6.25,26
Marijuana impairs reaction time, information processing, motor performance, attention, and visual processing.14,16,27,28 Drivers who are under the influence of marijuana make more driving errors, despite being cautious about how they react to traffic.29 Even after weeks of abstinence, previous daily users of marijuana display some cognitive processing and driving-related impairments.30,31
Courts have found physicians negligent if their patients’ treatment-induced driving impairments injured others when the risk of driving-related injury was foreseeable.32 The Massachusetts case of Coombes v Florio33 likened the physician’s duty to that of a liquor store that sells alcohol to a minor who subsequently crashes, or to a father who did not lock his firearms away from his violent adult son.
Three variables influence a court’s judgment about whether risk is “foreseeable”: “the relative knowledge of the risk as between lay persons and physicians, whether the patient has previously used the medication and/or experienced the adverse effect, and whether a warning would otherwise have been futile.”34 A physician who certified a patient to use marijuana without adequately explaining the risks of driving might be vulnerable to a lawsuit if the patient’s driving accident occurred while the patient was under the influence of the drug. Recommending marijuana as a treatment also could lead to a malpractice action if a patient experienced and was harmed by the drug’s adverse effects.
Other drags
Another malpractice risk stems from marijuana’s addiction potential. Although many people think Cannabis isn’t addictive, nearly 10% of all marijuana users develop dependence.10,17 Regular Cannabis users are more likely to use alcohol, tobacco, and “recreational” drugs,17,35 and using alcohol and marijuana together greatly heightens the risk of driving accidents.14,15 Although we know of no case that relates directly to marijuana, physicians have faced lawsuits for injuries stemming from a patient’s addiction to prescription drugs,36 particularly when the patient’s behavior should have led the physician to suspect abuse or overuse.37
When certifying marijuana use, physicians have the same obligations that apply to more conventional medical treatment:
• establishing a proper physician–patient relationship
• taking an appropriate history
• conducting a proper examination
• reviewing records
• developing a comprehensive treatment plan
• weighing risks and alternatives
• providing follow-up care.
Neglecting these steps could lead to medical board sanctions and suspension or revocation of a medical license.13
The blunt reality
We advise against recommending marijuana for your patients. But if you have exhausted the alternatives, see marijuana as the last resort, and believe that taking the risk is worth the potential benefit, you can take some steps to reduce your legal risk (Table 2,1,32,37,38 and Table 313).
Bottom LinE
Medical marijuana is a controversial topic that demands more rigorous research and regulatory consideration. In the present climate, cautious physicians will avoid recommending marijuana to their patients. If you think that a patient has a medical indication, with no treatment option better than medical marijuana, be sure to understand the medical and legal ramifications before you authorize its use.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474-2483.
2. Controlled Substances Act title 21, §801.
3. Frezza C. Medical marijuana: a drug without a medical model. Georgetown Law J. 2013;101:1117-1145.
4. Conant v Walters, 309 F3d 629, 637 (9th Cir 2002).
5. Vandrey R, Raber JC, Raber ME, et al. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313(24):2491-2493.
6. Thompson AE. JAMA patient page. Medical marijuana. JAMA. 2015;313(24):2508.
7. United States v Oakland Cannabis Buyers’ Cooperative, 532 U.S. 483 (2001).
8. Gonzales v Raich, 545 U.S. 1 (2005).
9. Ogden DW. Memorandum for selected United States Attorneys on investigations and prosecutions in states authorizing the medical use of marijuana. http://www. justice.gov/opa/blog/memorandum-selected-united-state-attorneys-investigations-and-prosecutions-states. Published October 19, 2009. Accessed July 11, 2015.
10. D’Souza DC, Ranganathan M. Medical marijuana: is the cart before the horse? JAMA. 2015;313(24):2431-2432.
11. Picard A. Pot-prescribing doctors warned. The Globe and Mail. http://www.theglobeandmail.com/news/national/ pot-prescribing-doctors-warned/article22506373. Published October 19, 2005. Accessed July 21, 2015.
12. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
13. Barthwell AG, Baxter LE, Cermak T, et al. The role of the physician in “medical” marijuana: American Society of Addiction Medicine. http://www.aoaam.org/usr/ ASAM_Med_Marijuana_White_Paper_Final.pdf. Published September 2010. Accessed July 11, 2015.
14. Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109-119.
15. Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478-492.
16. Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52-60.
17. Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19-35.
18. Huang YH, Zhang ZF, Tashkin DP, et al. An epidemiologic review of marijuana and cancer: an update. Cancer Epidemiol Biomarkers Prev. 2015;24(1):15-31.
19. Delforterie MJ, Lynskey MT, Huizink AC, et al. The relationship between cannabis involvement and suicidal thoughts and behaviors. Drug Alcohol Depend. 2015;150:98-104.
20. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot-a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54.
21. Masten SV, Guenzburger GV. Changes in driver cannabinoid prevalence in 12 U.S. states after implementing medical marijuana laws. J Safety Res. 2014;50:35-52.
22. Pollini RA, Romano E, Johnson MB, et al. The impact of marijuana decriminalization on California drivers. Drug Alcohol Depend. 2015;150:135-140.
23. Salomonsen-Sautel S, Min SJ, Sakai JT, et al. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144.
24. Urfer S, Morton J, Beall V, et al. Analysis of Δ9- tetrahydrocannabinol driving under the influence of drug cases in Colorado from January 2011 to February 2014. J Anal Toxicol. 2014;38(8):575-581.
25. Couper FJ, Peterson BL. The prevalence of marijuana in suspected impaired driving cases in Washington state. J Anal Toxicol. 2014;38(8):569-574.
26. Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239-248.
27. Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101-106.
28. Schwitzer T, Schwan R, Angioi-Duprez K, et al. The cannabinoid system and visual processing: a review on experimental findings and clinical presumptions. Eur Neuropsychopharmacol. 2015;25(1):100-112.
29. Neavyn MJ, Blohm E, Babu KM, et al. Medical marijuana and driving: a review. J Med Toxicol. 2014;10(3):269-279.
30. Bosker WM, Karschner EL, Lee D, et al. Sustained abstinence improves psychomotor function in chronic daily cannabis smokers. Paper presented at: SOFT 2012: Society of Forensic Toxicologists 2012 Annual Meeting; July 1-6, 2012; Boston, MA.
31. Fabritius M, Augsburger M, Chtioui H, et al. Fitness to drive and cannabis: validation of two blood THCCOOH thresholds to distinguish occasional users from heavy users. Forensic Sci Int. 2014;242:1-8.
32. Annas GJ. Doctors, drugs, and driving—tort liability for patient-caused accidents. New Engl J Med. 2008;359(5):521-525.
33. Coombes v Florio, 877 NE2d 567 (Mass 2007).
34. McKenzie v Hawaii Permanente Medical Group, Inc. 47 P3d 209 (Haw 2002).
35. Ilgen MA, Bohnert K, Kleinberg F, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 2013;132(3):654-659.
36. Osborne v United States, 166 F Supp 2d 479 (SDW Va 2001).
37. Conrad-Hutsell v Colturi, 2002 Ohio App. LEXIS 2740 (2002).
38. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
Dear Dr. Mossman,
I practice in a state that allows medical marijuana use. A few of my patients have asked me to help them obtain marijuana for their conditions. How risky would it be to oblige?
Submitted by “Dr. J”
In recent years, public debate about marijuana has acquired 2 new dimensions: (1) the wishes and medical needs of people who seek marijuana for its purported health benefits, and (2) the role of physicians who practice where “medical marijuana” is legal. This article, the authors’ joint effort to address Dr. J’s concerns, hits 3 topics:
• the intersection of marijuana policy and health care in the United States
• the risks and possible benefits of marijuana use
• the medicolegal problems faced by physicians who might advise patients to use marijuana.
Legal haze
Two cannabinoids—dronabinol and nabilone—have received FDA approval as appetite enhancers and anti-nausea agents. Third-party payors usually cover these types of medications, but no insurer pays for medical marijuana.1 The Controlled Substances Act of 19702 classified marijuana as a Schedule I drug because of its abuse potential, lack of accepted medical applications, and uncertain safety. The FDA has not approved marijuana use for any medical condition.
Although people commonly speak of “prescribing” marijuana, physicians cannot legally do this in the United States. What physicians may do, in the 23 states that allow medical marijuana, is recommend or certify a patient’s marijuana use—an action that has constitutional protection under the First Amendment’s freedom of speech clause.3,4
A physician may complete documentation that a patient has one of the qualifying medical conditions for which the jurisdiction has legalized medical marijuana. Either the patient or the physician then submits that documentation to the appropriate government agency (eg, the state’s department of health).
If the documentation receives approval, the agency will issue the patient a registration card that allows possession of medical marijuana, with which the patient can obtain or grow a small amount of marijuana. The cannabinoid content of marijuana products varies considerably,5 and physicians who certify marijuana typically defer dosage recommendations to the patient or the dispensary.1
In states that allow medical marijuana, users may assert an affirmative defense of medical necessity if they face criminal prosecution.3,6 Possession of marijuana remains illegal under federal law, however, regardless of one’s reason for having it.7,8 Since October 2009, the Attorney General’s office has discouraged federal prosecutions of persons “whose actions are in clear and unambiguous compliance with existing state laws providing for the medical use of marijuana.”9 But given the remaining conflicts between state and federal laws, “the legal implications of certifying patients for medical marijuana remain unclear.”10
Physicians have few resources to instruct them on the legal risks of certifying medical marijuana. When Canada legalized medical marijuana, the organization that provides malpractice insurance to Canadian physicians told its members that “prescribing medical marijuana cannot be compared to prescribing prescription drugs” and recommended that physicians obtain signed release forms documenting that they have discussed the risks of medical marijuana with patients.11 For some risky approved drugs, the FDA has established a risk evaluation and mitigation strategy, but no such guidance is available for marijuana.
Highlighting the benefits and risks
Proponents of medical marijuana claim that Cannabis can help patients, and dispassionate experts acknowledge that at least modest evidence supports the benefits of using “marijuana for nausea and vomiting related to chemotherapy, specific pain syndromes, and spasticity from multiple sclerosis.”10 For several other conditions— HIV/AIDS, depression, anxiety disorders, sleep disorders, psychosis, Tourette syndrome—evidence of benefit is poor.12 Rigorous evaluation of medical marijuana is difficult because the plant contains hundreds of active chemical compounds. The chemical content of marijuana is highly variable, depending on its preparation and administration,10,13—one reason why only a few good randomized controlled trials of marijuana have been conducted.
Marijuana has several side effects and carries many health risks (Table 1).4,14-20
On the highway: Marijuana and driving
Marijuana use impairs driving ability.14 Following enactment of more lenient marijuana laws, several states have reported higher numbers of fatally injured drivers who tested positive for Cannabis21-23 and had a positive screen of tetrahydrocannabinol (THC) in driving under the influence cases.24,25 One study showed that a blood THC concentration >5 ng/mL (comparable to a blood alcohol concentration of 0.15%) increased the crash odds ratio to 6.6.25,26
Marijuana impairs reaction time, information processing, motor performance, attention, and visual processing.14,16,27,28 Drivers who are under the influence of marijuana make more driving errors, despite being cautious about how they react to traffic.29 Even after weeks of abstinence, previous daily users of marijuana display some cognitive processing and driving-related impairments.30,31
Courts have found physicians negligent if their patients’ treatment-induced driving impairments injured others when the risk of driving-related injury was foreseeable.32 The Massachusetts case of Coombes v Florio33 likened the physician’s duty to that of a liquor store that sells alcohol to a minor who subsequently crashes, or to a father who did not lock his firearms away from his violent adult son.
Three variables influence a court’s judgment about whether risk is “foreseeable”: “the relative knowledge of the risk as between lay persons and physicians, whether the patient has previously used the medication and/or experienced the adverse effect, and whether a warning would otherwise have been futile.”34 A physician who certified a patient to use marijuana without adequately explaining the risks of driving might be vulnerable to a lawsuit if the patient’s driving accident occurred while the patient was under the influence of the drug. Recommending marijuana as a treatment also could lead to a malpractice action if a patient experienced and was harmed by the drug’s adverse effects.
Other drags
Another malpractice risk stems from marijuana’s addiction potential. Although many people think Cannabis isn’t addictive, nearly 10% of all marijuana users develop dependence.10,17 Regular Cannabis users are more likely to use alcohol, tobacco, and “recreational” drugs,17,35 and using alcohol and marijuana together greatly heightens the risk of driving accidents.14,15 Although we know of no case that relates directly to marijuana, physicians have faced lawsuits for injuries stemming from a patient’s addiction to prescription drugs,36 particularly when the patient’s behavior should have led the physician to suspect abuse or overuse.37
When certifying marijuana use, physicians have the same obligations that apply to more conventional medical treatment:
• establishing a proper physician–patient relationship
• taking an appropriate history
• conducting a proper examination
• reviewing records
• developing a comprehensive treatment plan
• weighing risks and alternatives
• providing follow-up care.
Neglecting these steps could lead to medical board sanctions and suspension or revocation of a medical license.13
The blunt reality
We advise against recommending marijuana for your patients. But if you have exhausted the alternatives, see marijuana as the last resort, and believe that taking the risk is worth the potential benefit, you can take some steps to reduce your legal risk (Table 2,1,32,37,38 and Table 313).
Bottom LinE
Medical marijuana is a controversial topic that demands more rigorous research and regulatory consideration. In the present climate, cautious physicians will avoid recommending marijuana to their patients. If you think that a patient has a medical indication, with no treatment option better than medical marijuana, be sure to understand the medical and legal ramifications before you authorize its use.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
I practice in a state that allows medical marijuana use. A few of my patients have asked me to help them obtain marijuana for their conditions. How risky would it be to oblige?
Submitted by “Dr. J”
In recent years, public debate about marijuana has acquired 2 new dimensions: (1) the wishes and medical needs of people who seek marijuana for its purported health benefits, and (2) the role of physicians who practice where “medical marijuana” is legal. This article, the authors’ joint effort to address Dr. J’s concerns, hits 3 topics:
• the intersection of marijuana policy and health care in the United States
• the risks and possible benefits of marijuana use
• the medicolegal problems faced by physicians who might advise patients to use marijuana.
Legal haze
Two cannabinoids—dronabinol and nabilone—have received FDA approval as appetite enhancers and anti-nausea agents. Third-party payors usually cover these types of medications, but no insurer pays for medical marijuana.1 The Controlled Substances Act of 19702 classified marijuana as a Schedule I drug because of its abuse potential, lack of accepted medical applications, and uncertain safety. The FDA has not approved marijuana use for any medical condition.
Although people commonly speak of “prescribing” marijuana, physicians cannot legally do this in the United States. What physicians may do, in the 23 states that allow medical marijuana, is recommend or certify a patient’s marijuana use—an action that has constitutional protection under the First Amendment’s freedom of speech clause.3,4
A physician may complete documentation that a patient has one of the qualifying medical conditions for which the jurisdiction has legalized medical marijuana. Either the patient or the physician then submits that documentation to the appropriate government agency (eg, the state’s department of health).
If the documentation receives approval, the agency will issue the patient a registration card that allows possession of medical marijuana, with which the patient can obtain or grow a small amount of marijuana. The cannabinoid content of marijuana products varies considerably,5 and physicians who certify marijuana typically defer dosage recommendations to the patient or the dispensary.1
In states that allow medical marijuana, users may assert an affirmative defense of medical necessity if they face criminal prosecution.3,6 Possession of marijuana remains illegal under federal law, however, regardless of one’s reason for having it.7,8 Since October 2009, the Attorney General’s office has discouraged federal prosecutions of persons “whose actions are in clear and unambiguous compliance with existing state laws providing for the medical use of marijuana.”9 But given the remaining conflicts between state and federal laws, “the legal implications of certifying patients for medical marijuana remain unclear.”10
Physicians have few resources to instruct them on the legal risks of certifying medical marijuana. When Canada legalized medical marijuana, the organization that provides malpractice insurance to Canadian physicians told its members that “prescribing medical marijuana cannot be compared to prescribing prescription drugs” and recommended that physicians obtain signed release forms documenting that they have discussed the risks of medical marijuana with patients.11 For some risky approved drugs, the FDA has established a risk evaluation and mitigation strategy, but no such guidance is available for marijuana.
Highlighting the benefits and risks
Proponents of medical marijuana claim that Cannabis can help patients, and dispassionate experts acknowledge that at least modest evidence supports the benefits of using “marijuana for nausea and vomiting related to chemotherapy, specific pain syndromes, and spasticity from multiple sclerosis.”10 For several other conditions— HIV/AIDS, depression, anxiety disorders, sleep disorders, psychosis, Tourette syndrome—evidence of benefit is poor.12 Rigorous evaluation of medical marijuana is difficult because the plant contains hundreds of active chemical compounds. The chemical content of marijuana is highly variable, depending on its preparation and administration,10,13—one reason why only a few good randomized controlled trials of marijuana have been conducted.
Marijuana has several side effects and carries many health risks (Table 1).4,14-20
On the highway: Marijuana and driving
Marijuana use impairs driving ability.14 Following enactment of more lenient marijuana laws, several states have reported higher numbers of fatally injured drivers who tested positive for Cannabis21-23 and had a positive screen of tetrahydrocannabinol (THC) in driving under the influence cases.24,25 One study showed that a blood THC concentration >5 ng/mL (comparable to a blood alcohol concentration of 0.15%) increased the crash odds ratio to 6.6.25,26
Marijuana impairs reaction time, information processing, motor performance, attention, and visual processing.14,16,27,28 Drivers who are under the influence of marijuana make more driving errors, despite being cautious about how they react to traffic.29 Even after weeks of abstinence, previous daily users of marijuana display some cognitive processing and driving-related impairments.30,31
Courts have found physicians negligent if their patients’ treatment-induced driving impairments injured others when the risk of driving-related injury was foreseeable.32 The Massachusetts case of Coombes v Florio33 likened the physician’s duty to that of a liquor store that sells alcohol to a minor who subsequently crashes, or to a father who did not lock his firearms away from his violent adult son.
Three variables influence a court’s judgment about whether risk is “foreseeable”: “the relative knowledge of the risk as between lay persons and physicians, whether the patient has previously used the medication and/or experienced the adverse effect, and whether a warning would otherwise have been futile.”34 A physician who certified a patient to use marijuana without adequately explaining the risks of driving might be vulnerable to a lawsuit if the patient’s driving accident occurred while the patient was under the influence of the drug. Recommending marijuana as a treatment also could lead to a malpractice action if a patient experienced and was harmed by the drug’s adverse effects.
Other drags
Another malpractice risk stems from marijuana’s addiction potential. Although many people think Cannabis isn’t addictive, nearly 10% of all marijuana users develop dependence.10,17 Regular Cannabis users are more likely to use alcohol, tobacco, and “recreational” drugs,17,35 and using alcohol and marijuana together greatly heightens the risk of driving accidents.14,15 Although we know of no case that relates directly to marijuana, physicians have faced lawsuits for injuries stemming from a patient’s addiction to prescription drugs,36 particularly when the patient’s behavior should have led the physician to suspect abuse or overuse.37
When certifying marijuana use, physicians have the same obligations that apply to more conventional medical treatment:
• establishing a proper physician–patient relationship
• taking an appropriate history
• conducting a proper examination
• reviewing records
• developing a comprehensive treatment plan
• weighing risks and alternatives
• providing follow-up care.
Neglecting these steps could lead to medical board sanctions and suspension or revocation of a medical license.13
The blunt reality
We advise against recommending marijuana for your patients. But if you have exhausted the alternatives, see marijuana as the last resort, and believe that taking the risk is worth the potential benefit, you can take some steps to reduce your legal risk (Table 2,1,32,37,38 and Table 313).
Bottom LinE
Medical marijuana is a controversial topic that demands more rigorous research and regulatory consideration. In the present climate, cautious physicians will avoid recommending marijuana to their patients. If you think that a patient has a medical indication, with no treatment option better than medical marijuana, be sure to understand the medical and legal ramifications before you authorize its use.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474-2483.
2. Controlled Substances Act title 21, §801.
3. Frezza C. Medical marijuana: a drug without a medical model. Georgetown Law J. 2013;101:1117-1145.
4. Conant v Walters, 309 F3d 629, 637 (9th Cir 2002).
5. Vandrey R, Raber JC, Raber ME, et al. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313(24):2491-2493.
6. Thompson AE. JAMA patient page. Medical marijuana. JAMA. 2015;313(24):2508.
7. United States v Oakland Cannabis Buyers’ Cooperative, 532 U.S. 483 (2001).
8. Gonzales v Raich, 545 U.S. 1 (2005).
9. Ogden DW. Memorandum for selected United States Attorneys on investigations and prosecutions in states authorizing the medical use of marijuana. http://www. justice.gov/opa/blog/memorandum-selected-united-state-attorneys-investigations-and-prosecutions-states. Published October 19, 2009. Accessed July 11, 2015.
10. D’Souza DC, Ranganathan M. Medical marijuana: is the cart before the horse? JAMA. 2015;313(24):2431-2432.
11. Picard A. Pot-prescribing doctors warned. The Globe and Mail. http://www.theglobeandmail.com/news/national/ pot-prescribing-doctors-warned/article22506373. Published October 19, 2005. Accessed July 21, 2015.
12. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
13. Barthwell AG, Baxter LE, Cermak T, et al. The role of the physician in “medical” marijuana: American Society of Addiction Medicine. http://www.aoaam.org/usr/ ASAM_Med_Marijuana_White_Paper_Final.pdf. Published September 2010. Accessed July 11, 2015.
14. Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109-119.
15. Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478-492.
16. Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52-60.
17. Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19-35.
18. Huang YH, Zhang ZF, Tashkin DP, et al. An epidemiologic review of marijuana and cancer: an update. Cancer Epidemiol Biomarkers Prev. 2015;24(1):15-31.
19. Delforterie MJ, Lynskey MT, Huizink AC, et al. The relationship between cannabis involvement and suicidal thoughts and behaviors. Drug Alcohol Depend. 2015;150:98-104.
20. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot-a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54.
21. Masten SV, Guenzburger GV. Changes in driver cannabinoid prevalence in 12 U.S. states after implementing medical marijuana laws. J Safety Res. 2014;50:35-52.
22. Pollini RA, Romano E, Johnson MB, et al. The impact of marijuana decriminalization on California drivers. Drug Alcohol Depend. 2015;150:135-140.
23. Salomonsen-Sautel S, Min SJ, Sakai JT, et al. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144.
24. Urfer S, Morton J, Beall V, et al. Analysis of Δ9- tetrahydrocannabinol driving under the influence of drug cases in Colorado from January 2011 to February 2014. J Anal Toxicol. 2014;38(8):575-581.
25. Couper FJ, Peterson BL. The prevalence of marijuana in suspected impaired driving cases in Washington state. J Anal Toxicol. 2014;38(8):569-574.
26. Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239-248.
27. Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101-106.
28. Schwitzer T, Schwan R, Angioi-Duprez K, et al. The cannabinoid system and visual processing: a review on experimental findings and clinical presumptions. Eur Neuropsychopharmacol. 2015;25(1):100-112.
29. Neavyn MJ, Blohm E, Babu KM, et al. Medical marijuana and driving: a review. J Med Toxicol. 2014;10(3):269-279.
30. Bosker WM, Karschner EL, Lee D, et al. Sustained abstinence improves psychomotor function in chronic daily cannabis smokers. Paper presented at: SOFT 2012: Society of Forensic Toxicologists 2012 Annual Meeting; July 1-6, 2012; Boston, MA.
31. Fabritius M, Augsburger M, Chtioui H, et al. Fitness to drive and cannabis: validation of two blood THCCOOH thresholds to distinguish occasional users from heavy users. Forensic Sci Int. 2014;242:1-8.
32. Annas GJ. Doctors, drugs, and driving—tort liability for patient-caused accidents. New Engl J Med. 2008;359(5):521-525.
33. Coombes v Florio, 877 NE2d 567 (Mass 2007).
34. McKenzie v Hawaii Permanente Medical Group, Inc. 47 P3d 209 (Haw 2002).
35. Ilgen MA, Bohnert K, Kleinberg F, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 2013;132(3):654-659.
36. Osborne v United States, 166 F Supp 2d 479 (SDW Va 2001).
37. Conrad-Hutsell v Colturi, 2002 Ohio App. LEXIS 2740 (2002).
38. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
1. Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474-2483.
2. Controlled Substances Act title 21, §801.
3. Frezza C. Medical marijuana: a drug without a medical model. Georgetown Law J. 2013;101:1117-1145.
4. Conant v Walters, 309 F3d 629, 637 (9th Cir 2002).
5. Vandrey R, Raber JC, Raber ME, et al. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313(24):2491-2493.
6. Thompson AE. JAMA patient page. Medical marijuana. JAMA. 2015;313(24):2508.
7. United States v Oakland Cannabis Buyers’ Cooperative, 532 U.S. 483 (2001).
8. Gonzales v Raich, 545 U.S. 1 (2005).
9. Ogden DW. Memorandum for selected United States Attorneys on investigations and prosecutions in states authorizing the medical use of marijuana. http://www. justice.gov/opa/blog/memorandum-selected-united-state-attorneys-investigations-and-prosecutions-states. Published October 19, 2009. Accessed July 11, 2015.
10. D’Souza DC, Ranganathan M. Medical marijuana: is the cart before the horse? JAMA. 2015;313(24):2431-2432.
11. Picard A. Pot-prescribing doctors warned. The Globe and Mail. http://www.theglobeandmail.com/news/national/ pot-prescribing-doctors-warned/article22506373. Published October 19, 2005. Accessed July 21, 2015.
12. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
13. Barthwell AG, Baxter LE, Cermak T, et al. The role of the physician in “medical” marijuana: American Society of Addiction Medicine. http://www.aoaam.org/usr/ ASAM_Med_Marijuana_White_Paper_Final.pdf. Published September 2010. Accessed July 11, 2015.
14. Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109-119.
15. Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478-492.
16. Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52-60.
17. Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19-35.
18. Huang YH, Zhang ZF, Tashkin DP, et al. An epidemiologic review of marijuana and cancer: an update. Cancer Epidemiol Biomarkers Prev. 2015;24(1):15-31.
19. Delforterie MJ, Lynskey MT, Huizink AC, et al. The relationship between cannabis involvement and suicidal thoughts and behaviors. Drug Alcohol Depend. 2015;150:98-104.
20. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot-a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54.
21. Masten SV, Guenzburger GV. Changes in driver cannabinoid prevalence in 12 U.S. states after implementing medical marijuana laws. J Safety Res. 2014;50:35-52.
22. Pollini RA, Romano E, Johnson MB, et al. The impact of marijuana decriminalization on California drivers. Drug Alcohol Depend. 2015;150:135-140.
23. Salomonsen-Sautel S, Min SJ, Sakai JT, et al. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144.
24. Urfer S, Morton J, Beall V, et al. Analysis of Δ9- tetrahydrocannabinol driving under the influence of drug cases in Colorado from January 2011 to February 2014. J Anal Toxicol. 2014;38(8):575-581.
25. Couper FJ, Peterson BL. The prevalence of marijuana in suspected impaired driving cases in Washington state. J Anal Toxicol. 2014;38(8):569-574.
26. Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239-248.
27. Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101-106.
28. Schwitzer T, Schwan R, Angioi-Duprez K, et al. The cannabinoid system and visual processing: a review on experimental findings and clinical presumptions. Eur Neuropsychopharmacol. 2015;25(1):100-112.
29. Neavyn MJ, Blohm E, Babu KM, et al. Medical marijuana and driving: a review. J Med Toxicol. 2014;10(3):269-279.
30. Bosker WM, Karschner EL, Lee D, et al. Sustained abstinence improves psychomotor function in chronic daily cannabis smokers. Paper presented at: SOFT 2012: Society of Forensic Toxicologists 2012 Annual Meeting; July 1-6, 2012; Boston, MA.
31. Fabritius M, Augsburger M, Chtioui H, et al. Fitness to drive and cannabis: validation of two blood THCCOOH thresholds to distinguish occasional users from heavy users. Forensic Sci Int. 2014;242:1-8.
32. Annas GJ. Doctors, drugs, and driving—tort liability for patient-caused accidents. New Engl J Med. 2008;359(5):521-525.
33. Coombes v Florio, 877 NE2d 567 (Mass 2007).
34. McKenzie v Hawaii Permanente Medical Group, Inc. 47 P3d 209 (Haw 2002).
35. Ilgen MA, Bohnert K, Kleinberg F, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 2013;132(3):654-659.
36. Osborne v United States, 166 F Supp 2d 479 (SDW Va 2001).
37. Conrad-Hutsell v Colturi, 2002 Ohio App. LEXIS 2740 (2002).
38. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
Autonomy vs abuse: Can a patient choose a new power of attorney?
Dear Dr. Mossman,
At the hospital where I serve as the psychiatric consultant, a medical team asked me to evaluate a patient’s capacity to designate a new power of attorney (POA) for health care. The patient’s relatives want the change because they think the current POA—also a relative—is stealing the patient’s funds. The contentious family situation made me wonder: What legal risks might I face after I assess the patient’s capacity to choose a new POA?
Submitted by “Dr. P”
As America’s population ages, situations like the one Dr. P has encountered will become more common. Many variables—time constraints, patients’ cognitive impairments, lack of prior relationships with patients, complex medical situations, and strained family dynamics— can make these clinical situations complex and daunting.
Dr. P realizes that feuding relatives can redirect their anger toward a well-meaning physician who might appear to take sides in a dispute. Yet staying silent isn’t a good option, either: If the patient is being mistreated or abused, Dr. P may have a duty to initiate appropriate protective action.
In this article, we’ll respond to Dr. P’s question by examining these topics:
• what a POA is and the rationale for having one
• standards for capacity to choose a POA
• characteristics and dynamics of potential surrogates
• responding to possible elder abuse.
Surrogate decision-makers
People can lose their decision-making capacity because of dementia, acute or chronic illness, or sudden injury. Although autonomy and respecting decisions of mentally capable people are paramount American values, our legal system has several mechanisms that can be activated on behalf of people who have lost their decision-making capabilities.
When a careful evaluation suggests that a patient cannot make informed medical decisions, one solution is to turn to a surrogate decision-maker whom the patient previously has designated to act on his (her) behalf, should he (she) become incapacitated. A surrogate can make decisions based on the incapacitated person’s current utterances (eg, expressions of pain), previously expressed wishes about what should happen under certain circumstances, or the surrogate’s judgment of the person’s best interest.1
States have varied legal frameworks for establishing surrogacy and refer to a surrogate using terms such as proxy, agent, attorney-in-fact, and power of attorney.2 POA responsibilities can encompass a broad array of decision-making tasks or can be limited, for example, to handling banking transactions or managing estate planning.3,4 A POA can be “durable” and grant lasting power regardless of disability, or “springing” and operational only when the designator has lost capacity.
A health care POA designates a substitute decision-maker for medical care. The Patient Self-Determination Act and the Joint Commission obligate health care professionals to follow the decisions made by a legally valid POA. Generally, providers who follow a surrogate’s decision in good faith have legal immunity, but they must challenge a surrogate’s decision if it deviates widely from usual protocol.2
Legal standards
Dr. P received a consultation request that asked whether a patient with compromised medical decision-making powers nonetheless had the current capacity to choose a new POA.
To evaluate the patient’s capacity to designate a new POA, Dr. P must know what having this capacity means. What determines if someone has the capacity to designate a POA is a legal matter, and unless Dr. P is sure what the laws in her state say about this, she should consult a lawyer who can explain the jurisdiction’s applicable legal standards to her.5
The law generally presumes that adults are competent to make health care decisions, including decisions about appointing a POA.5 The law also recognizes that people with cognitive impairments or mental illnesses still can be competent to appoint POAs.4
Most states don’t have statutes that define the capacity to appoint a health care POA. In these jurisdictions, courts may apply standards similar to those concerning competence to enter into a contract.6Table 1 describes criteria in 4 states that do have statutory provisions concerning competence to designate a health care POA.
Approaching the evaluation
Before evaluating a person’s capacity to designate a POA, you should first understand the person’s medical condition and learn what powers the surrogate would have. A detailed description of the evaluation process lies beyond the scope of this article. For more information, please consult the structured interviews described by Moye et al4 and Soliman’s guide to the evaluation process.7
In addition to examining the patient’s psychological status and cognitive capacity, you also might have to consider contextual variables, such as:
• potential risks of not allowing the appointment of POA, including a delay in needed care
• the person’s relationship to the proposed POA
• possible power imbalances or evidence of coercion
• how the person would benefit from having the POA.8
People who have good marital or parent-child relationships are more likely to select loved ones as their POAs.9 Family members who have not previously served as surrogates or have not had talked with their loved ones about their preferences feel less confident exercising the duties of a POA.10 An evaluation, therefore, should consider the prior relationship between the designator and proposed surrogate, and particularly whether these parties have discussed the designator’s health care preferences. Table 2 lists potential pitfalls in POA evaluations.2,4,5,8,11-13,16
Responding to abuse
Accompanying the request for Dr. P’s evaluation were reports that the current POA had been stealing the patient’s funds. Financial exploitation of older people is not a rare phenomenon.14,15 Yet only about 1 in 25 cases is reported,16,17 and physicians discover as few as 2% of all reported cases.15
Many variables—the stress of the situation,8 pre-existing relationship dynamics,18 and caregiver psychopathology11—lead POAs to exploit their designator. Sometimes, family members believe that they are entitled to a relative’s money because of real or imagined transgressions19 or because they regard themselves as eventual heirs to their relative’s estate.16 Some designated POAs use designators’ funds simply because they need money. Kemp and Mosqueda20 have developed an evaluation framework for assessing possible financial abuse (Table 3).
Although reporting financial abuse can strain alliances between patients and their families, psychiatrists bear a responsibility to look out for the welfare of their older patients.8 Indeed, all 50 states have elder abuse statutes, most of which mandate reporting by physicians.21
Suspicion of financial abuse could indicate the need to evaluate the susceptible person’s capacity to make financial decisions.12 Depending on the patient’s circumstances and medical problems, further steps might include:
• contacting proper authorities, such as Adult Protective Services or the Department of Human Services
• contacting local law enforcement
• instituting procedures for emergency guardianship
• arranging for more in-home services for the patient or recommending a higher level of care
• developing a treatment plan for the patient’s medical and psychiatric problems
• communicating with other trusted family members.12,18
Bottom Line
Evaluating the capacity to appoint a power of attorney (POA) often requires awareness of social systems, family dynamics, and legal requirements, combined with the psychiatric data from a systematic individual assessment. Evaluating psychiatrists should understand what type of POA is being considered and the applicable legal standards in the jurisdictions where they work.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Black PG, Derse AR, Derrington S, et al. Can a patient designate his doctor as his proxy decision maker? Pediatrics. 2013;131(5):986-990.
2. Pope TM. Legal fundamentals of surrogate decision making. Chest. 2012;141(4):1074-1081.
3. Araj V. Types of power of attorney: which POA is right for me? http://www.quickenloans.com/blog/types-power-attorney-poa#4zvT8F58fd6zVb2v.99. Published December 29, 2011. Accessed January 11, 2015.
4. Moye J, Sabatino CP, Weintraub Brendel R. Evaluation of the capacity to appoint a healthcare proxy. Am J Geriatr Psychiatry. 2013;21(4):326-336.
5. Whitman R. Capacity for lifetime and estate planning. Penn State L Rev. 2013;117(4):1061-1080.
6. Duke v Kindred Healthcare Operating, Inc., 2011 WL 864321 (Tenn. Ct. App).
7. Soliman S. Evaluating older adults’ capacity and need for guardianship. Current Psychiatry. 2012;11(4):39-42,52-53,A.
8. Katona C, Chiu E, Adelman S, et al. World psychiatric association section of old age psychiatry consensus statement on ethics and capacity in older people with mental disorders. Int J Geriatr Psychiatry. 2009;24(12):1319-1324.
9. Carr D, Moorman SM, Boerner K. End-of-life planning in a family context: does relationship quality affect whether (and with whom) older adults plan? J Gerontol B Psychol Sci Soc Sci. 2013;68(4):586-592.
10. Majesko A, Hong SY, Weissfeld L, et al. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281-2286.
11. Fulmer T, Guadagno L, Bitondo Dyer C, et al. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
12. Horning SM, Wilkins SS, Dhanani S, et al. A case of elder abuse and undue influence: assessment and treatment from a geriatric interdisciplinary team. Clin Case Stud. 2013;12:373-387.
13. Lui VW, Chiu CC, Ko RS, et al. The principle of assessing mental capacity for enduring power of attorney. Hong Kong Med J. 2014;20(1):59-62.
14. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
15. Wilber KH, Reynolds SL. Introducing a framework for defining financial abuse of the elderly. J Elder Abuse Negl. 1996;8(2):61-80.
16. Mukherjee D. Financial exploitation of older adults in rural settings: a family perspective. J Elder Abuse Negl. 2013; 25(5):425-437.
17. Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, New York City Department for the Aging. Under the Radar: New York State Elder Abuse Prevalence Study. http://nyceac.com/wp-content/ uploads/2011/05/UndertheRadar051211.pdf. Published May 16, 2011. Accessed January 10, 2015.
18. Hall RCW, Hall RCW, Chapman MJ. Exploitation of the elderly: undue influence as a form of elder abuse. Clin Geriatr. 2005;13(2):28-36.
19. Kemp B, Liao S. Elder financial abuse: tips for the medical director. J Am Med Dir Assoc. 2006;7(9):591-593.
20. Kemp BJ, Mosqueda LA. Elder financial abuse: an evaluation framework and supporting evidence. J Am Geriatr Soc. 2005;53(7):1123-1127.
21. Stiegel S, Klem E. Reporting requirements: provisions and citations in Adult Protective Services laws, by state. http:// www.americanbar.org/content/dam/aba/migrated/ aging/docs/MandatoryReportingProvisionsChart. authcheckdam.pdf. Published 2007. Accessed January 9, 2015.
Dear Dr. Mossman,
At the hospital where I serve as the psychiatric consultant, a medical team asked me to evaluate a patient’s capacity to designate a new power of attorney (POA) for health care. The patient’s relatives want the change because they think the current POA—also a relative—is stealing the patient’s funds. The contentious family situation made me wonder: What legal risks might I face after I assess the patient’s capacity to choose a new POA?
Submitted by “Dr. P”
As America’s population ages, situations like the one Dr. P has encountered will become more common. Many variables—time constraints, patients’ cognitive impairments, lack of prior relationships with patients, complex medical situations, and strained family dynamics— can make these clinical situations complex and daunting.
Dr. P realizes that feuding relatives can redirect their anger toward a well-meaning physician who might appear to take sides in a dispute. Yet staying silent isn’t a good option, either: If the patient is being mistreated or abused, Dr. P may have a duty to initiate appropriate protective action.
In this article, we’ll respond to Dr. P’s question by examining these topics:
• what a POA is and the rationale for having one
• standards for capacity to choose a POA
• characteristics and dynamics of potential surrogates
• responding to possible elder abuse.
Surrogate decision-makers
People can lose their decision-making capacity because of dementia, acute or chronic illness, or sudden injury. Although autonomy and respecting decisions of mentally capable people are paramount American values, our legal system has several mechanisms that can be activated on behalf of people who have lost their decision-making capabilities.
When a careful evaluation suggests that a patient cannot make informed medical decisions, one solution is to turn to a surrogate decision-maker whom the patient previously has designated to act on his (her) behalf, should he (she) become incapacitated. A surrogate can make decisions based on the incapacitated person’s current utterances (eg, expressions of pain), previously expressed wishes about what should happen under certain circumstances, or the surrogate’s judgment of the person’s best interest.1
States have varied legal frameworks for establishing surrogacy and refer to a surrogate using terms such as proxy, agent, attorney-in-fact, and power of attorney.2 POA responsibilities can encompass a broad array of decision-making tasks or can be limited, for example, to handling banking transactions or managing estate planning.3,4 A POA can be “durable” and grant lasting power regardless of disability, or “springing” and operational only when the designator has lost capacity.
A health care POA designates a substitute decision-maker for medical care. The Patient Self-Determination Act and the Joint Commission obligate health care professionals to follow the decisions made by a legally valid POA. Generally, providers who follow a surrogate’s decision in good faith have legal immunity, but they must challenge a surrogate’s decision if it deviates widely from usual protocol.2
Legal standards
Dr. P received a consultation request that asked whether a patient with compromised medical decision-making powers nonetheless had the current capacity to choose a new POA.
To evaluate the patient’s capacity to designate a new POA, Dr. P must know what having this capacity means. What determines if someone has the capacity to designate a POA is a legal matter, and unless Dr. P is sure what the laws in her state say about this, she should consult a lawyer who can explain the jurisdiction’s applicable legal standards to her.5
The law generally presumes that adults are competent to make health care decisions, including decisions about appointing a POA.5 The law also recognizes that people with cognitive impairments or mental illnesses still can be competent to appoint POAs.4
Most states don’t have statutes that define the capacity to appoint a health care POA. In these jurisdictions, courts may apply standards similar to those concerning competence to enter into a contract.6Table 1 describes criteria in 4 states that do have statutory provisions concerning competence to designate a health care POA.
Approaching the evaluation
Before evaluating a person’s capacity to designate a POA, you should first understand the person’s medical condition and learn what powers the surrogate would have. A detailed description of the evaluation process lies beyond the scope of this article. For more information, please consult the structured interviews described by Moye et al4 and Soliman’s guide to the evaluation process.7
In addition to examining the patient’s psychological status and cognitive capacity, you also might have to consider contextual variables, such as:
• potential risks of not allowing the appointment of POA, including a delay in needed care
• the person’s relationship to the proposed POA
• possible power imbalances or evidence of coercion
• how the person would benefit from having the POA.8
People who have good marital or parent-child relationships are more likely to select loved ones as their POAs.9 Family members who have not previously served as surrogates or have not had talked with their loved ones about their preferences feel less confident exercising the duties of a POA.10 An evaluation, therefore, should consider the prior relationship between the designator and proposed surrogate, and particularly whether these parties have discussed the designator’s health care preferences. Table 2 lists potential pitfalls in POA evaluations.2,4,5,8,11-13,16
Responding to abuse
Accompanying the request for Dr. P’s evaluation were reports that the current POA had been stealing the patient’s funds. Financial exploitation of older people is not a rare phenomenon.14,15 Yet only about 1 in 25 cases is reported,16,17 and physicians discover as few as 2% of all reported cases.15
Many variables—the stress of the situation,8 pre-existing relationship dynamics,18 and caregiver psychopathology11—lead POAs to exploit their designator. Sometimes, family members believe that they are entitled to a relative’s money because of real or imagined transgressions19 or because they regard themselves as eventual heirs to their relative’s estate.16 Some designated POAs use designators’ funds simply because they need money. Kemp and Mosqueda20 have developed an evaluation framework for assessing possible financial abuse (Table 3).
Although reporting financial abuse can strain alliances between patients and their families, psychiatrists bear a responsibility to look out for the welfare of their older patients.8 Indeed, all 50 states have elder abuse statutes, most of which mandate reporting by physicians.21
Suspicion of financial abuse could indicate the need to evaluate the susceptible person’s capacity to make financial decisions.12 Depending on the patient’s circumstances and medical problems, further steps might include:
• contacting proper authorities, such as Adult Protective Services or the Department of Human Services
• contacting local law enforcement
• instituting procedures for emergency guardianship
• arranging for more in-home services for the patient or recommending a higher level of care
• developing a treatment plan for the patient’s medical and psychiatric problems
• communicating with other trusted family members.12,18
Bottom Line
Evaluating the capacity to appoint a power of attorney (POA) often requires awareness of social systems, family dynamics, and legal requirements, combined with the psychiatric data from a systematic individual assessment. Evaluating psychiatrists should understand what type of POA is being considered and the applicable legal standards in the jurisdictions where they work.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
At the hospital where I serve as the psychiatric consultant, a medical team asked me to evaluate a patient’s capacity to designate a new power of attorney (POA) for health care. The patient’s relatives want the change because they think the current POA—also a relative—is stealing the patient’s funds. The contentious family situation made me wonder: What legal risks might I face after I assess the patient’s capacity to choose a new POA?
Submitted by “Dr. P”
As America’s population ages, situations like the one Dr. P has encountered will become more common. Many variables—time constraints, patients’ cognitive impairments, lack of prior relationships with patients, complex medical situations, and strained family dynamics— can make these clinical situations complex and daunting.
Dr. P realizes that feuding relatives can redirect their anger toward a well-meaning physician who might appear to take sides in a dispute. Yet staying silent isn’t a good option, either: If the patient is being mistreated or abused, Dr. P may have a duty to initiate appropriate protective action.
In this article, we’ll respond to Dr. P’s question by examining these topics:
• what a POA is and the rationale for having one
• standards for capacity to choose a POA
• characteristics and dynamics of potential surrogates
• responding to possible elder abuse.
Surrogate decision-makers
People can lose their decision-making capacity because of dementia, acute or chronic illness, or sudden injury. Although autonomy and respecting decisions of mentally capable people are paramount American values, our legal system has several mechanisms that can be activated on behalf of people who have lost their decision-making capabilities.
When a careful evaluation suggests that a patient cannot make informed medical decisions, one solution is to turn to a surrogate decision-maker whom the patient previously has designated to act on his (her) behalf, should he (she) become incapacitated. A surrogate can make decisions based on the incapacitated person’s current utterances (eg, expressions of pain), previously expressed wishes about what should happen under certain circumstances, or the surrogate’s judgment of the person’s best interest.1
States have varied legal frameworks for establishing surrogacy and refer to a surrogate using terms such as proxy, agent, attorney-in-fact, and power of attorney.2 POA responsibilities can encompass a broad array of decision-making tasks or can be limited, for example, to handling banking transactions or managing estate planning.3,4 A POA can be “durable” and grant lasting power regardless of disability, or “springing” and operational only when the designator has lost capacity.
A health care POA designates a substitute decision-maker for medical care. The Patient Self-Determination Act and the Joint Commission obligate health care professionals to follow the decisions made by a legally valid POA. Generally, providers who follow a surrogate’s decision in good faith have legal immunity, but they must challenge a surrogate’s decision if it deviates widely from usual protocol.2
Legal standards
Dr. P received a consultation request that asked whether a patient with compromised medical decision-making powers nonetheless had the current capacity to choose a new POA.
To evaluate the patient’s capacity to designate a new POA, Dr. P must know what having this capacity means. What determines if someone has the capacity to designate a POA is a legal matter, and unless Dr. P is sure what the laws in her state say about this, she should consult a lawyer who can explain the jurisdiction’s applicable legal standards to her.5
The law generally presumes that adults are competent to make health care decisions, including decisions about appointing a POA.5 The law also recognizes that people with cognitive impairments or mental illnesses still can be competent to appoint POAs.4
Most states don’t have statutes that define the capacity to appoint a health care POA. In these jurisdictions, courts may apply standards similar to those concerning competence to enter into a contract.6Table 1 describes criteria in 4 states that do have statutory provisions concerning competence to designate a health care POA.
Approaching the evaluation
Before evaluating a person’s capacity to designate a POA, you should first understand the person’s medical condition and learn what powers the surrogate would have. A detailed description of the evaluation process lies beyond the scope of this article. For more information, please consult the structured interviews described by Moye et al4 and Soliman’s guide to the evaluation process.7
In addition to examining the patient’s psychological status and cognitive capacity, you also might have to consider contextual variables, such as:
• potential risks of not allowing the appointment of POA, including a delay in needed care
• the person’s relationship to the proposed POA
• possible power imbalances or evidence of coercion
• how the person would benefit from having the POA.8
People who have good marital or parent-child relationships are more likely to select loved ones as their POAs.9 Family members who have not previously served as surrogates or have not had talked with their loved ones about their preferences feel less confident exercising the duties of a POA.10 An evaluation, therefore, should consider the prior relationship between the designator and proposed surrogate, and particularly whether these parties have discussed the designator’s health care preferences. Table 2 lists potential pitfalls in POA evaluations.2,4,5,8,11-13,16
Responding to abuse
Accompanying the request for Dr. P’s evaluation were reports that the current POA had been stealing the patient’s funds. Financial exploitation of older people is not a rare phenomenon.14,15 Yet only about 1 in 25 cases is reported,16,17 and physicians discover as few as 2% of all reported cases.15
Many variables—the stress of the situation,8 pre-existing relationship dynamics,18 and caregiver psychopathology11—lead POAs to exploit their designator. Sometimes, family members believe that they are entitled to a relative’s money because of real or imagined transgressions19 or because they regard themselves as eventual heirs to their relative’s estate.16 Some designated POAs use designators’ funds simply because they need money. Kemp and Mosqueda20 have developed an evaluation framework for assessing possible financial abuse (Table 3).
Although reporting financial abuse can strain alliances between patients and their families, psychiatrists bear a responsibility to look out for the welfare of their older patients.8 Indeed, all 50 states have elder abuse statutes, most of which mandate reporting by physicians.21
Suspicion of financial abuse could indicate the need to evaluate the susceptible person’s capacity to make financial decisions.12 Depending on the patient’s circumstances and medical problems, further steps might include:
• contacting proper authorities, such as Adult Protective Services or the Department of Human Services
• contacting local law enforcement
• instituting procedures for emergency guardianship
• arranging for more in-home services for the patient or recommending a higher level of care
• developing a treatment plan for the patient’s medical and psychiatric problems
• communicating with other trusted family members.12,18
Bottom Line
Evaluating the capacity to appoint a power of attorney (POA) often requires awareness of social systems, family dynamics, and legal requirements, combined with the psychiatric data from a systematic individual assessment. Evaluating psychiatrists should understand what type of POA is being considered and the applicable legal standards in the jurisdictions where they work.
Disclosures
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Black PG, Derse AR, Derrington S, et al. Can a patient designate his doctor as his proxy decision maker? Pediatrics. 2013;131(5):986-990.
2. Pope TM. Legal fundamentals of surrogate decision making. Chest. 2012;141(4):1074-1081.
3. Araj V. Types of power of attorney: which POA is right for me? http://www.quickenloans.com/blog/types-power-attorney-poa#4zvT8F58fd6zVb2v.99. Published December 29, 2011. Accessed January 11, 2015.
4. Moye J, Sabatino CP, Weintraub Brendel R. Evaluation of the capacity to appoint a healthcare proxy. Am J Geriatr Psychiatry. 2013;21(4):326-336.
5. Whitman R. Capacity for lifetime and estate planning. Penn State L Rev. 2013;117(4):1061-1080.
6. Duke v Kindred Healthcare Operating, Inc., 2011 WL 864321 (Tenn. Ct. App).
7. Soliman S. Evaluating older adults’ capacity and need for guardianship. Current Psychiatry. 2012;11(4):39-42,52-53,A.
8. Katona C, Chiu E, Adelman S, et al. World psychiatric association section of old age psychiatry consensus statement on ethics and capacity in older people with mental disorders. Int J Geriatr Psychiatry. 2009;24(12):1319-1324.
9. Carr D, Moorman SM, Boerner K. End-of-life planning in a family context: does relationship quality affect whether (and with whom) older adults plan? J Gerontol B Psychol Sci Soc Sci. 2013;68(4):586-592.
10. Majesko A, Hong SY, Weissfeld L, et al. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281-2286.
11. Fulmer T, Guadagno L, Bitondo Dyer C, et al. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
12. Horning SM, Wilkins SS, Dhanani S, et al. A case of elder abuse and undue influence: assessment and treatment from a geriatric interdisciplinary team. Clin Case Stud. 2013;12:373-387.
13. Lui VW, Chiu CC, Ko RS, et al. The principle of assessing mental capacity for enduring power of attorney. Hong Kong Med J. 2014;20(1):59-62.
14. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
15. Wilber KH, Reynolds SL. Introducing a framework for defining financial abuse of the elderly. J Elder Abuse Negl. 1996;8(2):61-80.
16. Mukherjee D. Financial exploitation of older adults in rural settings: a family perspective. J Elder Abuse Negl. 2013; 25(5):425-437.
17. Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, New York City Department for the Aging. Under the Radar: New York State Elder Abuse Prevalence Study. http://nyceac.com/wp-content/ uploads/2011/05/UndertheRadar051211.pdf. Published May 16, 2011. Accessed January 10, 2015.
18. Hall RCW, Hall RCW, Chapman MJ. Exploitation of the elderly: undue influence as a form of elder abuse. Clin Geriatr. 2005;13(2):28-36.
19. Kemp B, Liao S. Elder financial abuse: tips for the medical director. J Am Med Dir Assoc. 2006;7(9):591-593.
20. Kemp BJ, Mosqueda LA. Elder financial abuse: an evaluation framework and supporting evidence. J Am Geriatr Soc. 2005;53(7):1123-1127.
21. Stiegel S, Klem E. Reporting requirements: provisions and citations in Adult Protective Services laws, by state. http:// www.americanbar.org/content/dam/aba/migrated/ aging/docs/MandatoryReportingProvisionsChart. authcheckdam.pdf. Published 2007. Accessed January 9, 2015.
1. Black PG, Derse AR, Derrington S, et al. Can a patient designate his doctor as his proxy decision maker? Pediatrics. 2013;131(5):986-990.
2. Pope TM. Legal fundamentals of surrogate decision making. Chest. 2012;141(4):1074-1081.
3. Araj V. Types of power of attorney: which POA is right for me? http://www.quickenloans.com/blog/types-power-attorney-poa#4zvT8F58fd6zVb2v.99. Published December 29, 2011. Accessed January 11, 2015.
4. Moye J, Sabatino CP, Weintraub Brendel R. Evaluation of the capacity to appoint a healthcare proxy. Am J Geriatr Psychiatry. 2013;21(4):326-336.
5. Whitman R. Capacity for lifetime and estate planning. Penn State L Rev. 2013;117(4):1061-1080.
6. Duke v Kindred Healthcare Operating, Inc., 2011 WL 864321 (Tenn. Ct. App).
7. Soliman S. Evaluating older adults’ capacity and need for guardianship. Current Psychiatry. 2012;11(4):39-42,52-53,A.
8. Katona C, Chiu E, Adelman S, et al. World psychiatric association section of old age psychiatry consensus statement on ethics and capacity in older people with mental disorders. Int J Geriatr Psychiatry. 2009;24(12):1319-1324.
9. Carr D, Moorman SM, Boerner K. End-of-life planning in a family context: does relationship quality affect whether (and with whom) older adults plan? J Gerontol B Psychol Sci Soc Sci. 2013;68(4):586-592.
10. Majesko A, Hong SY, Weissfeld L, et al. Identifying family members who may struggle in the role of surrogate decision maker. Crit Care Med. 2012;40(8):2281-2286.
11. Fulmer T, Guadagno L, Bitondo Dyer C, et al. Progress in elder abuse screening and assessment instruments. J Am Geriatr Soc. 2004;52(2):297-304.
12. Horning SM, Wilkins SS, Dhanani S, et al. A case of elder abuse and undue influence: assessment and treatment from a geriatric interdisciplinary team. Clin Case Stud. 2013;12:373-387.
13. Lui VW, Chiu CC, Ko RS, et al. The principle of assessing mental capacity for enduring power of attorney. Hong Kong Med J. 2014;20(1):59-62.
14. Acierno R, Hernandez-Tejada M, Muzzy W, et al. National Elder Mistreatment Study. Washington, DC: National Institute of Justice; 2009.
15. Wilber KH, Reynolds SL. Introducing a framework for defining financial abuse of the elderly. J Elder Abuse Negl. 1996;8(2):61-80.
16. Mukherjee D. Financial exploitation of older adults in rural settings: a family perspective. J Elder Abuse Negl. 2013; 25(5):425-437.
17. Lifespan of Greater Rochester, Inc., Weill Cornell Medical Center of Cornell University, New York City Department for the Aging. Under the Radar: New York State Elder Abuse Prevalence Study. http://nyceac.com/wp-content/ uploads/2011/05/UndertheRadar051211.pdf. Published May 16, 2011. Accessed January 10, 2015.
18. Hall RCW, Hall RCW, Chapman MJ. Exploitation of the elderly: undue influence as a form of elder abuse. Clin Geriatr. 2005;13(2):28-36.
19. Kemp B, Liao S. Elder financial abuse: tips for the medical director. J Am Med Dir Assoc. 2006;7(9):591-593.
20. Kemp BJ, Mosqueda LA. Elder financial abuse: an evaluation framework and supporting evidence. J Am Geriatr Soc. 2005;53(7):1123-1127.
21. Stiegel S, Klem E. Reporting requirements: provisions and citations in Adult Protective Services laws, by state. http:// www.americanbar.org/content/dam/aba/migrated/ aging/docs/MandatoryReportingProvisionsChart. authcheckdam.pdf. Published 2007. Accessed January 9, 2015.
Good, bad, and ugly: Prior authorization and medicolegal risk
Dear Dr. Mossman,
Where I practice, most health care plans won’t pay for certain medications without giving prior authorization (PA). Completing PA forms and making telephone calls take up time that could be better spent treating patients. I’m tempted to set a new policy of not doing PAs. If I do, might I face legal trouble?
Submitted by “Dr. A”
If you provide clinical care, you’ve probably dealt with third-party payers who require prior authorization (PA) before they will pay for certain treatments. Dr. A is not alone in feeling exasperated about the time it takes to complete a PA.1 After spending several hours each month waiting on hold and wading through stacks of paperwork, you may feel like Dr. A and consider refusing to do any more PAs.
But is Dr. A’s proposed solution a good idea? To address this question and the frustration that lies behind it, we’ll take a cue from Italian film director Sergio Leone and discuss:
• how PAs affect psychiatric care: the good, the bad, and the ugly
• potential exposure to professional liability and ethics complaints that might result from refusing or failing to seek PA
• strategies to reduce the burden of PAs while providing efficient, effective care.
The good
Recent decades have witnessed huge increases in spending on prescription medication. Psychotropics are no exception; state Medicaid spending for anti-psychotic medication grew from <$1 billion in 1995 to >$5.5 billion in 2005.2
Requiring a PA for expensive drugs is one way that third-party payers try to rein in costs and hold down insurance premiums. Imposing financial constraints often is just one aim of a pharmacy benefit management (PBM) program. Insurers also justify PBMs by pointing out that feedback to practitioners whose prescribing falls well outside the norm—in the form of mailed warnings, physician second opinions, or pharmacist consultation—can improve patient safety and encourage appropriate treatment options for enrolled patients.3,4 Examples of such benefits include reducing overuse of prescription opioids5 and antipsychotics among children,3 misuse of buprenorphine,6 and adverse effects from potentially inappropriate prescriptions.7
The bad
The bad news for doctors: Cost savings for payers come at the expense of providers and their practices, in the form of time spent doing paperwork and talking on the phone to complete PAs or contest PA decisions.8 Addressing PA requests costs an estimated $83,000 per physician per year. The total administrative burden for all 835,000 physicians who practice in the United States therefore is 868,000,000 hours, or $69 billion annually.9
To make matters worse, PA requirements may increase the overall cost of care. After Georgia Medicaid instituted PA requirements for second-generation antipsychotics (SGAs), average monthly per member drug costs fell $19.62, but average monthly outpatient treatment costs rose $31.59 per member.10 Pharmacy savings that result from requiring PAs for SGAs can be offset quickly by small increases in the hospitalization rate or emergency department visits.9,11
The ugly
Many physicians believe that the PA process undermines patient care by decreasing time devoted to direct patient contact, incentivizing suboptimal treatment, and limiting medication access.1,12,13 But do any data support this belief? Do PAs impede treatment for vulnerable persons with severe mental illnesses?
The answer, some studies suggest, is “Yes.” A Maine Medicaid PA policy slowed initiation of treatment for bipolar disorder by reducing the rate of starting non-preferred medications, although the same policy had no impact on patients already receiving treatment.14 Another study examined the effect of PA processes for inpatient psychiatry treatment and found that patients were less likely to be admitted on weekends, probably because PA review was not available on those days.15 A third study showed that PA requirements and resulting impediments to getting refills were correlated with medication discontinuation by patients with schizophrenia or bipolar disorder, which can increase the risk of decompensation, work-related problems, and hospitalization.16
Problems with PAs
Whether they are helpful or counterproductive, PAs are a practice reality. Dr. A’s proposed solution sounds appealing, but it might create ethical and legal problems.
Among the fundamental elements of ethical medical practice is physicians’ obligation to give patients “guidance … as to the optimal course of action” and to “advocate for patients in dealing with third parties when appropriate.”17 It’s fine for psychiatrists to consider prescribing treatments that patients’ health care coverage favors, but we also have to help patients weigh and evaluate costs, particularly when patients’ circumstances and medical interests militate strongly for options that third-party payers balk at paying for. Patients’ interests—not what’s expedient—are always physicians’ foremost concern.18
Beyond purely ethical considerations, you might face legal consequences if you refuse or fail to seek PAs for what you think is the proper medication. As Table 1 shows, one key factor is whether you are under contract with the patient’s insurance carrier; if you are, failure to seek a PA when appropriate may constitute a breach of the contract (Donna Vanderpool, written communication, October 5, 2014).
If the prescribed medication does not meet the standard of care and your patient suffers some harm, a licensing board complaint and investigation are possible. You also face exposure to a medical malpractice action. Although we do not know of any instances in which such an action has succeeded, 2 recent court decisions suggest that harm to a patient stemmed from failing to seek PA for a medication could constitute grounds for a lawsuit.19,20 Efforts to contain medical costs have been around for decades, and courts have held that physicians, third-party payers, and utilization review intermediaries are bound by “the standard of reasonable community practice”21 and should not let cost limitations “corrupt medical judgment.”22 Physicians who do not appeal limitations at odds with their medical judgment might bear responsibility for any injuries that occur.18,22
Managing PA requests
Given the inevitability of encountering PA requests and your ethical and professional obligations to help patients, what can you do (Table 29,23,27)?
Some practitioners charge patients for time spent completing PAs.23 Although physicians should “complete without charge the appropriate ‘simplified’ insurance claim form as a part of service to the patient;” they also may consider “a charge for more complex or multiple forms … in conformity with local custom.”24 Legally, physicians’ contracts with insurance panels may preclude charging such fees, but if a patient is being seen out of network, the physician does not have a contractual obligation and may charge.9 If your practice setting lets you choose which insurances you accept, the impact and burden of seeking PAs is a factor to consider when deciding whether to participate in a particular panel.23
In an interesting twist, an Ohio physician successfully sued a medical insurance administrator for the cost of his time responding to PA inquiries.25 Reasoning that the insurance administrator “should expect to pay for the reasonable value of” the doctor’s time because the PAs “were solely intended for the benefit of the insurance administrator” or parties whom the administrator served, the judge awarded the doctor $187.50 plus 8% interest.
Considerations that are more practical relate to how to triage and address the volume of PA requests. Some large medical practices centralize PAs and try to set up pre-approved plans of care or blanket approvals for frequently encountered conditions. Centralization also allows one key administrative assistant to develop skills in processing PA requests and to build relationships with payers.26
The administrative assistant also can compile lists of preferred alternative medications, PA forms, and payer Web sites. Using and submitting requests through payer Web sites can speed up PA processing, which saves time and money.27 As electronic health records improve, they may incorporate patients’ formularies and provide automatic alerts for required PAs.23
Patients should be involved, too. They can help to obtain relevant formulary information and to weigh alternative therapies. You can help them understand your role in the PA process, the reasoning behind your treatment recommendations, and the delays in picking up prescribed medications that waiting for PA approval can create.
It’s easy to get angry about PAs
Your best response, however, is to practice prudent and—within reason— cost-effective medicine. When generic or insurer-preferred medications are clinically appropriate and meet treatment guidelines, trying them first is sensible and defensible. If your patient fails the initial low-cost treatment, or if a low-cost choice isn’t appropriate, document this clearly and seek approval for a costlier treatment.9
BOTTOM LINE
Physicians have ethical and legal obligations to advocate for their patients’ needs and best interests. This sometimes includes completing prior authorization requests. Find strategies that minimize hassle and make sense in your practice, and seek efficient ways to document the medical necessity of requested tests, procedures, or therapies.
Acknowledgment
Drs. Marett and Mossman thanks Donna Vanderpool, MBA, JD, and Annette Reynolds, MD, for their helpful input in preparing this article.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brown CM, Richards K, Rascati KL, et al. Effects of a psychotherapeutic drug prior authorization (PA) requirement on patients and providers: a providers’ perspective. Adm Policy Ment Health. 2008;35(3):181-188.
2. Law MR, Ross-Degnan D, Soumerai SB. Effect of prior authorization of second-generation antipsychotic agents on pharmacy utilization and reimbursements. Psychiatr Serv. 2008;59(5):540-546.
3. Stein BD, Leckman-Westin E, Okeke E, et al. The effects of prior authorization policies on Medicaid-enrolled children’s use of antipsychotic medications: evidence from two Mid-Atlantic states. J Child Adolesc Psychopharmacol. 2014;24(7):374-381.
4. Adams KT. Prior authorization–still used, still an issue. Biotechnol Healthc. 2010;7(4):28.
5. Garcia MM, Angelini MC, Thomas T, et al. Implementation of an opioid management initiative by a state Medicaid program. J Manag Care Pharm. 2014;20(5):447-454.
6. Clark RE, Baxter JD, Barton BA, et al. The impact of prior authorization on buprenorphine dose, relapse rates, and cost for Massachusetts Medicaid beneficiaries with opioid dependence [published online July 9, 2014]. Health Serv Res. doi: 10.1111/1475-6773.12201.
7. Dunn RL, Harrison D, Ripley TL. The beers criteria as an outpatient screening tool for potentially inappropriate medications. Consult Pharm. 2011;26(10):754-763.
8. Lennertz MD, Wertheimer AI. Is prior authorization for prescribed drugs cost-effective? Drug Benefit Trends. 2008;20:136-139.
9. Bendix J. The prior authorization predicament. Med Econ. 2014;91(13)29-30,32,34-35.
10. Farley JF, Cline RR, Schommer JC, et al. Retrospective assessment of Medicaid step-therapy prior authorization policy for atypical antipsychotic medications. Clin Ther. 2008;30(8):1524-1539; discussion 1506-1507.
11. Abouzaid S, Jutkowitz E, Foley KA, et al. Economic impact of prior authorization policies for atypical antipsychotics in the treatment of schizophrenia. Popul Health Manag. 2010;13(5):247-254.
12. Brown CM, Nwokeji E, Rascati KL, et al. Development of the burden of prior authorization of psychotherapeutics (BoPAP) scale to assess the effects of prior authorization among Texas Medicaid providers. Adm Policy Ment Health. 2009;36(4):278-287.
13. Rascati KL, Brown CM. Prior authorization for antipsychotic medications—It’s not just about the money. Clin Ther. 2008;30(8):1506-1507.
14. Lu CY, Soumerai SB, Ross-Degnan D, et al. Unintended impacts of a Medicaid prior authorization policy on access to medications for bipolar disorder. Med Care. 2010;48(1):4-9.
15. Stephens RJ, White SE, Cudnik M, et al. Factors associated with longer lengths of stay for mental health emergency department patients. J Emerg Med. 2014; 47(4):412-419.
16. Brown JD, Barrett A, Caffery E, et al. Medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder. Psychiatr Serv. 2013;64(9):878-885.
17. American Medical Association. Opinion 10.01– Fundamental elements of the patient-physician relationship. http://www.ama-assn.org/ama/pub/ physician-resources/medical-ethics/code-medical-ethics/opinion1001.page?. Accessed October 11, 2014.
18. Hall RC. Ethical and legal implications of managed care. Gen Hosp Psychiatry. 1997;19(3):200-208.
19. Porter v Thadani, 2010 U.S. Dist. LEXIS 35145 (NH 2010).
20. NB ex rel Peacock v District of Columbia, 682 F3d 77 (DC Cir 2012).
21. Wilson v Blue Cross of Southern California, 222 Cal App 3d 660, 271 Cal Rptr 876 (1990).
22. Wickline v State of California, 192 Cal App 3d 1630, 239 Cal Rptr 810 (1986).
23. Terry K. Prior authorization made easier. Med Econ. 2007;84(20):34,38,40.
24. American Medical Association. Ethics Opinion 6.07– Insurance forms completion charges. http://www. ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion607.page? Updated June 1994. Accessed October 11, 2014.
25. Gibson v Medco Health Solutions, 06-CVF-106 (OH 2008).
26. Bendix J. Curing the prior authorization headache. Med Econ. 2013;90(19):24,26-27,29-31.
27. American Medical Association. Electronic prior authorization toolkit. Available at http://www.ama-assn.org/ama/pub/advocacy/topics/administrative-simplification-initiatives/electronic-transactions-toolkit/ prior-authorization.page. Accessed October 11, 2014.
Dear Dr. Mossman,
Where I practice, most health care plans won’t pay for certain medications without giving prior authorization (PA). Completing PA forms and making telephone calls take up time that could be better spent treating patients. I’m tempted to set a new policy of not doing PAs. If I do, might I face legal trouble?
Submitted by “Dr. A”
If you provide clinical care, you’ve probably dealt with third-party payers who require prior authorization (PA) before they will pay for certain treatments. Dr. A is not alone in feeling exasperated about the time it takes to complete a PA.1 After spending several hours each month waiting on hold and wading through stacks of paperwork, you may feel like Dr. A and consider refusing to do any more PAs.
But is Dr. A’s proposed solution a good idea? To address this question and the frustration that lies behind it, we’ll take a cue from Italian film director Sergio Leone and discuss:
• how PAs affect psychiatric care: the good, the bad, and the ugly
• potential exposure to professional liability and ethics complaints that might result from refusing or failing to seek PA
• strategies to reduce the burden of PAs while providing efficient, effective care.
The good
Recent decades have witnessed huge increases in spending on prescription medication. Psychotropics are no exception; state Medicaid spending for anti-psychotic medication grew from <$1 billion in 1995 to >$5.5 billion in 2005.2
Requiring a PA for expensive drugs is one way that third-party payers try to rein in costs and hold down insurance premiums. Imposing financial constraints often is just one aim of a pharmacy benefit management (PBM) program. Insurers also justify PBMs by pointing out that feedback to practitioners whose prescribing falls well outside the norm—in the form of mailed warnings, physician second opinions, or pharmacist consultation—can improve patient safety and encourage appropriate treatment options for enrolled patients.3,4 Examples of such benefits include reducing overuse of prescription opioids5 and antipsychotics among children,3 misuse of buprenorphine,6 and adverse effects from potentially inappropriate prescriptions.7
The bad
The bad news for doctors: Cost savings for payers come at the expense of providers and their practices, in the form of time spent doing paperwork and talking on the phone to complete PAs or contest PA decisions.8 Addressing PA requests costs an estimated $83,000 per physician per year. The total administrative burden for all 835,000 physicians who practice in the United States therefore is 868,000,000 hours, or $69 billion annually.9
To make matters worse, PA requirements may increase the overall cost of care. After Georgia Medicaid instituted PA requirements for second-generation antipsychotics (SGAs), average monthly per member drug costs fell $19.62, but average monthly outpatient treatment costs rose $31.59 per member.10 Pharmacy savings that result from requiring PAs for SGAs can be offset quickly by small increases in the hospitalization rate or emergency department visits.9,11
The ugly
Many physicians believe that the PA process undermines patient care by decreasing time devoted to direct patient contact, incentivizing suboptimal treatment, and limiting medication access.1,12,13 But do any data support this belief? Do PAs impede treatment for vulnerable persons with severe mental illnesses?
The answer, some studies suggest, is “Yes.” A Maine Medicaid PA policy slowed initiation of treatment for bipolar disorder by reducing the rate of starting non-preferred medications, although the same policy had no impact on patients already receiving treatment.14 Another study examined the effect of PA processes for inpatient psychiatry treatment and found that patients were less likely to be admitted on weekends, probably because PA review was not available on those days.15 A third study showed that PA requirements and resulting impediments to getting refills were correlated with medication discontinuation by patients with schizophrenia or bipolar disorder, which can increase the risk of decompensation, work-related problems, and hospitalization.16
Problems with PAs
Whether they are helpful or counterproductive, PAs are a practice reality. Dr. A’s proposed solution sounds appealing, but it might create ethical and legal problems.
Among the fundamental elements of ethical medical practice is physicians’ obligation to give patients “guidance … as to the optimal course of action” and to “advocate for patients in dealing with third parties when appropriate.”17 It’s fine for psychiatrists to consider prescribing treatments that patients’ health care coverage favors, but we also have to help patients weigh and evaluate costs, particularly when patients’ circumstances and medical interests militate strongly for options that third-party payers balk at paying for. Patients’ interests—not what’s expedient—are always physicians’ foremost concern.18
Beyond purely ethical considerations, you might face legal consequences if you refuse or fail to seek PAs for what you think is the proper medication. As Table 1 shows, one key factor is whether you are under contract with the patient’s insurance carrier; if you are, failure to seek a PA when appropriate may constitute a breach of the contract (Donna Vanderpool, written communication, October 5, 2014).
If the prescribed medication does not meet the standard of care and your patient suffers some harm, a licensing board complaint and investigation are possible. You also face exposure to a medical malpractice action. Although we do not know of any instances in which such an action has succeeded, 2 recent court decisions suggest that harm to a patient stemmed from failing to seek PA for a medication could constitute grounds for a lawsuit.19,20 Efforts to contain medical costs have been around for decades, and courts have held that physicians, third-party payers, and utilization review intermediaries are bound by “the standard of reasonable community practice”21 and should not let cost limitations “corrupt medical judgment.”22 Physicians who do not appeal limitations at odds with their medical judgment might bear responsibility for any injuries that occur.18,22
Managing PA requests
Given the inevitability of encountering PA requests and your ethical and professional obligations to help patients, what can you do (Table 29,23,27)?
Some practitioners charge patients for time spent completing PAs.23 Although physicians should “complete without charge the appropriate ‘simplified’ insurance claim form as a part of service to the patient;” they also may consider “a charge for more complex or multiple forms … in conformity with local custom.”24 Legally, physicians’ contracts with insurance panels may preclude charging such fees, but if a patient is being seen out of network, the physician does not have a contractual obligation and may charge.9 If your practice setting lets you choose which insurances you accept, the impact and burden of seeking PAs is a factor to consider when deciding whether to participate in a particular panel.23
In an interesting twist, an Ohio physician successfully sued a medical insurance administrator for the cost of his time responding to PA inquiries.25 Reasoning that the insurance administrator “should expect to pay for the reasonable value of” the doctor’s time because the PAs “were solely intended for the benefit of the insurance administrator” or parties whom the administrator served, the judge awarded the doctor $187.50 plus 8% interest.
Considerations that are more practical relate to how to triage and address the volume of PA requests. Some large medical practices centralize PAs and try to set up pre-approved plans of care or blanket approvals for frequently encountered conditions. Centralization also allows one key administrative assistant to develop skills in processing PA requests and to build relationships with payers.26
The administrative assistant also can compile lists of preferred alternative medications, PA forms, and payer Web sites. Using and submitting requests through payer Web sites can speed up PA processing, which saves time and money.27 As electronic health records improve, they may incorporate patients’ formularies and provide automatic alerts for required PAs.23
Patients should be involved, too. They can help to obtain relevant formulary information and to weigh alternative therapies. You can help them understand your role in the PA process, the reasoning behind your treatment recommendations, and the delays in picking up prescribed medications that waiting for PA approval can create.
It’s easy to get angry about PAs
Your best response, however, is to practice prudent and—within reason— cost-effective medicine. When generic or insurer-preferred medications are clinically appropriate and meet treatment guidelines, trying them first is sensible and defensible. If your patient fails the initial low-cost treatment, or if a low-cost choice isn’t appropriate, document this clearly and seek approval for a costlier treatment.9
BOTTOM LINE
Physicians have ethical and legal obligations to advocate for their patients’ needs and best interests. This sometimes includes completing prior authorization requests. Find strategies that minimize hassle and make sense in your practice, and seek efficient ways to document the medical necessity of requested tests, procedures, or therapies.
Acknowledgment
Drs. Marett and Mossman thanks Donna Vanderpool, MBA, JD, and Annette Reynolds, MD, for their helpful input in preparing this article.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
Where I practice, most health care plans won’t pay for certain medications without giving prior authorization (PA). Completing PA forms and making telephone calls take up time that could be better spent treating patients. I’m tempted to set a new policy of not doing PAs. If I do, might I face legal trouble?
Submitted by “Dr. A”
If you provide clinical care, you’ve probably dealt with third-party payers who require prior authorization (PA) before they will pay for certain treatments. Dr. A is not alone in feeling exasperated about the time it takes to complete a PA.1 After spending several hours each month waiting on hold and wading through stacks of paperwork, you may feel like Dr. A and consider refusing to do any more PAs.
But is Dr. A’s proposed solution a good idea? To address this question and the frustration that lies behind it, we’ll take a cue from Italian film director Sergio Leone and discuss:
• how PAs affect psychiatric care: the good, the bad, and the ugly
• potential exposure to professional liability and ethics complaints that might result from refusing or failing to seek PA
• strategies to reduce the burden of PAs while providing efficient, effective care.
The good
Recent decades have witnessed huge increases in spending on prescription medication. Psychotropics are no exception; state Medicaid spending for anti-psychotic medication grew from <$1 billion in 1995 to >$5.5 billion in 2005.2
Requiring a PA for expensive drugs is one way that third-party payers try to rein in costs and hold down insurance premiums. Imposing financial constraints often is just one aim of a pharmacy benefit management (PBM) program. Insurers also justify PBMs by pointing out that feedback to practitioners whose prescribing falls well outside the norm—in the form of mailed warnings, physician second opinions, or pharmacist consultation—can improve patient safety and encourage appropriate treatment options for enrolled patients.3,4 Examples of such benefits include reducing overuse of prescription opioids5 and antipsychotics among children,3 misuse of buprenorphine,6 and adverse effects from potentially inappropriate prescriptions.7
The bad
The bad news for doctors: Cost savings for payers come at the expense of providers and their practices, in the form of time spent doing paperwork and talking on the phone to complete PAs or contest PA decisions.8 Addressing PA requests costs an estimated $83,000 per physician per year. The total administrative burden for all 835,000 physicians who practice in the United States therefore is 868,000,000 hours, or $69 billion annually.9
To make matters worse, PA requirements may increase the overall cost of care. After Georgia Medicaid instituted PA requirements for second-generation antipsychotics (SGAs), average monthly per member drug costs fell $19.62, but average monthly outpatient treatment costs rose $31.59 per member.10 Pharmacy savings that result from requiring PAs for SGAs can be offset quickly by small increases in the hospitalization rate or emergency department visits.9,11
The ugly
Many physicians believe that the PA process undermines patient care by decreasing time devoted to direct patient contact, incentivizing suboptimal treatment, and limiting medication access.1,12,13 But do any data support this belief? Do PAs impede treatment for vulnerable persons with severe mental illnesses?
The answer, some studies suggest, is “Yes.” A Maine Medicaid PA policy slowed initiation of treatment for bipolar disorder by reducing the rate of starting non-preferred medications, although the same policy had no impact on patients already receiving treatment.14 Another study examined the effect of PA processes for inpatient psychiatry treatment and found that patients were less likely to be admitted on weekends, probably because PA review was not available on those days.15 A third study showed that PA requirements and resulting impediments to getting refills were correlated with medication discontinuation by patients with schizophrenia or bipolar disorder, which can increase the risk of decompensation, work-related problems, and hospitalization.16
Problems with PAs
Whether they are helpful or counterproductive, PAs are a practice reality. Dr. A’s proposed solution sounds appealing, but it might create ethical and legal problems.
Among the fundamental elements of ethical medical practice is physicians’ obligation to give patients “guidance … as to the optimal course of action” and to “advocate for patients in dealing with third parties when appropriate.”17 It’s fine for psychiatrists to consider prescribing treatments that patients’ health care coverage favors, but we also have to help patients weigh and evaluate costs, particularly when patients’ circumstances and medical interests militate strongly for options that third-party payers balk at paying for. Patients’ interests—not what’s expedient—are always physicians’ foremost concern.18
Beyond purely ethical considerations, you might face legal consequences if you refuse or fail to seek PAs for what you think is the proper medication. As Table 1 shows, one key factor is whether you are under contract with the patient’s insurance carrier; if you are, failure to seek a PA when appropriate may constitute a breach of the contract (Donna Vanderpool, written communication, October 5, 2014).
If the prescribed medication does not meet the standard of care and your patient suffers some harm, a licensing board complaint and investigation are possible. You also face exposure to a medical malpractice action. Although we do not know of any instances in which such an action has succeeded, 2 recent court decisions suggest that harm to a patient stemmed from failing to seek PA for a medication could constitute grounds for a lawsuit.19,20 Efforts to contain medical costs have been around for decades, and courts have held that physicians, third-party payers, and utilization review intermediaries are bound by “the standard of reasonable community practice”21 and should not let cost limitations “corrupt medical judgment.”22 Physicians who do not appeal limitations at odds with their medical judgment might bear responsibility for any injuries that occur.18,22
Managing PA requests
Given the inevitability of encountering PA requests and your ethical and professional obligations to help patients, what can you do (Table 29,23,27)?
Some practitioners charge patients for time spent completing PAs.23 Although physicians should “complete without charge the appropriate ‘simplified’ insurance claim form as a part of service to the patient;” they also may consider “a charge for more complex or multiple forms … in conformity with local custom.”24 Legally, physicians’ contracts with insurance panels may preclude charging such fees, but if a patient is being seen out of network, the physician does not have a contractual obligation and may charge.9 If your practice setting lets you choose which insurances you accept, the impact and burden of seeking PAs is a factor to consider when deciding whether to participate in a particular panel.23
In an interesting twist, an Ohio physician successfully sued a medical insurance administrator for the cost of his time responding to PA inquiries.25 Reasoning that the insurance administrator “should expect to pay for the reasonable value of” the doctor’s time because the PAs “were solely intended for the benefit of the insurance administrator” or parties whom the administrator served, the judge awarded the doctor $187.50 plus 8% interest.
Considerations that are more practical relate to how to triage and address the volume of PA requests. Some large medical practices centralize PAs and try to set up pre-approved plans of care or blanket approvals for frequently encountered conditions. Centralization also allows one key administrative assistant to develop skills in processing PA requests and to build relationships with payers.26
The administrative assistant also can compile lists of preferred alternative medications, PA forms, and payer Web sites. Using and submitting requests through payer Web sites can speed up PA processing, which saves time and money.27 As electronic health records improve, they may incorporate patients’ formularies and provide automatic alerts for required PAs.23
Patients should be involved, too. They can help to obtain relevant formulary information and to weigh alternative therapies. You can help them understand your role in the PA process, the reasoning behind your treatment recommendations, and the delays in picking up prescribed medications that waiting for PA approval can create.
It’s easy to get angry about PAs
Your best response, however, is to practice prudent and—within reason— cost-effective medicine. When generic or insurer-preferred medications are clinically appropriate and meet treatment guidelines, trying them first is sensible and defensible. If your patient fails the initial low-cost treatment, or if a low-cost choice isn’t appropriate, document this clearly and seek approval for a costlier treatment.9
BOTTOM LINE
Physicians have ethical and legal obligations to advocate for their patients’ needs and best interests. This sometimes includes completing prior authorization requests. Find strategies that minimize hassle and make sense in your practice, and seek efficient ways to document the medical necessity of requested tests, procedures, or therapies.
Acknowledgment
Drs. Marett and Mossman thanks Donna Vanderpool, MBA, JD, and Annette Reynolds, MD, for their helpful input in preparing this article.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brown CM, Richards K, Rascati KL, et al. Effects of a psychotherapeutic drug prior authorization (PA) requirement on patients and providers: a providers’ perspective. Adm Policy Ment Health. 2008;35(3):181-188.
2. Law MR, Ross-Degnan D, Soumerai SB. Effect of prior authorization of second-generation antipsychotic agents on pharmacy utilization and reimbursements. Psychiatr Serv. 2008;59(5):540-546.
3. Stein BD, Leckman-Westin E, Okeke E, et al. The effects of prior authorization policies on Medicaid-enrolled children’s use of antipsychotic medications: evidence from two Mid-Atlantic states. J Child Adolesc Psychopharmacol. 2014;24(7):374-381.
4. Adams KT. Prior authorization–still used, still an issue. Biotechnol Healthc. 2010;7(4):28.
5. Garcia MM, Angelini MC, Thomas T, et al. Implementation of an opioid management initiative by a state Medicaid program. J Manag Care Pharm. 2014;20(5):447-454.
6. Clark RE, Baxter JD, Barton BA, et al. The impact of prior authorization on buprenorphine dose, relapse rates, and cost for Massachusetts Medicaid beneficiaries with opioid dependence [published online July 9, 2014]. Health Serv Res. doi: 10.1111/1475-6773.12201.
7. Dunn RL, Harrison D, Ripley TL. The beers criteria as an outpatient screening tool for potentially inappropriate medications. Consult Pharm. 2011;26(10):754-763.
8. Lennertz MD, Wertheimer AI. Is prior authorization for prescribed drugs cost-effective? Drug Benefit Trends. 2008;20:136-139.
9. Bendix J. The prior authorization predicament. Med Econ. 2014;91(13)29-30,32,34-35.
10. Farley JF, Cline RR, Schommer JC, et al. Retrospective assessment of Medicaid step-therapy prior authorization policy for atypical antipsychotic medications. Clin Ther. 2008;30(8):1524-1539; discussion 1506-1507.
11. Abouzaid S, Jutkowitz E, Foley KA, et al. Economic impact of prior authorization policies for atypical antipsychotics in the treatment of schizophrenia. Popul Health Manag. 2010;13(5):247-254.
12. Brown CM, Nwokeji E, Rascati KL, et al. Development of the burden of prior authorization of psychotherapeutics (BoPAP) scale to assess the effects of prior authorization among Texas Medicaid providers. Adm Policy Ment Health. 2009;36(4):278-287.
13. Rascati KL, Brown CM. Prior authorization for antipsychotic medications—It’s not just about the money. Clin Ther. 2008;30(8):1506-1507.
14. Lu CY, Soumerai SB, Ross-Degnan D, et al. Unintended impacts of a Medicaid prior authorization policy on access to medications for bipolar disorder. Med Care. 2010;48(1):4-9.
15. Stephens RJ, White SE, Cudnik M, et al. Factors associated with longer lengths of stay for mental health emergency department patients. J Emerg Med. 2014; 47(4):412-419.
16. Brown JD, Barrett A, Caffery E, et al. Medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder. Psychiatr Serv. 2013;64(9):878-885.
17. American Medical Association. Opinion 10.01– Fundamental elements of the patient-physician relationship. http://www.ama-assn.org/ama/pub/ physician-resources/medical-ethics/code-medical-ethics/opinion1001.page?. Accessed October 11, 2014.
18. Hall RC. Ethical and legal implications of managed care. Gen Hosp Psychiatry. 1997;19(3):200-208.
19. Porter v Thadani, 2010 U.S. Dist. LEXIS 35145 (NH 2010).
20. NB ex rel Peacock v District of Columbia, 682 F3d 77 (DC Cir 2012).
21. Wilson v Blue Cross of Southern California, 222 Cal App 3d 660, 271 Cal Rptr 876 (1990).
22. Wickline v State of California, 192 Cal App 3d 1630, 239 Cal Rptr 810 (1986).
23. Terry K. Prior authorization made easier. Med Econ. 2007;84(20):34,38,40.
24. American Medical Association. Ethics Opinion 6.07– Insurance forms completion charges. http://www. ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion607.page? Updated June 1994. Accessed October 11, 2014.
25. Gibson v Medco Health Solutions, 06-CVF-106 (OH 2008).
26. Bendix J. Curing the prior authorization headache. Med Econ. 2013;90(19):24,26-27,29-31.
27. American Medical Association. Electronic prior authorization toolkit. Available at http://www.ama-assn.org/ama/pub/advocacy/topics/administrative-simplification-initiatives/electronic-transactions-toolkit/ prior-authorization.page. Accessed October 11, 2014.
1. Brown CM, Richards K, Rascati KL, et al. Effects of a psychotherapeutic drug prior authorization (PA) requirement on patients and providers: a providers’ perspective. Adm Policy Ment Health. 2008;35(3):181-188.
2. Law MR, Ross-Degnan D, Soumerai SB. Effect of prior authorization of second-generation antipsychotic agents on pharmacy utilization and reimbursements. Psychiatr Serv. 2008;59(5):540-546.
3. Stein BD, Leckman-Westin E, Okeke E, et al. The effects of prior authorization policies on Medicaid-enrolled children’s use of antipsychotic medications: evidence from two Mid-Atlantic states. J Child Adolesc Psychopharmacol. 2014;24(7):374-381.
4. Adams KT. Prior authorization–still used, still an issue. Biotechnol Healthc. 2010;7(4):28.
5. Garcia MM, Angelini MC, Thomas T, et al. Implementation of an opioid management initiative by a state Medicaid program. J Manag Care Pharm. 2014;20(5):447-454.
6. Clark RE, Baxter JD, Barton BA, et al. The impact of prior authorization on buprenorphine dose, relapse rates, and cost for Massachusetts Medicaid beneficiaries with opioid dependence [published online July 9, 2014]. Health Serv Res. doi: 10.1111/1475-6773.12201.
7. Dunn RL, Harrison D, Ripley TL. The beers criteria as an outpatient screening tool for potentially inappropriate medications. Consult Pharm. 2011;26(10):754-763.
8. Lennertz MD, Wertheimer AI. Is prior authorization for prescribed drugs cost-effective? Drug Benefit Trends. 2008;20:136-139.
9. Bendix J. The prior authorization predicament. Med Econ. 2014;91(13)29-30,32,34-35.
10. Farley JF, Cline RR, Schommer JC, et al. Retrospective assessment of Medicaid step-therapy prior authorization policy for atypical antipsychotic medications. Clin Ther. 2008;30(8):1524-1539; discussion 1506-1507.
11. Abouzaid S, Jutkowitz E, Foley KA, et al. Economic impact of prior authorization policies for atypical antipsychotics in the treatment of schizophrenia. Popul Health Manag. 2010;13(5):247-254.
12. Brown CM, Nwokeji E, Rascati KL, et al. Development of the burden of prior authorization of psychotherapeutics (BoPAP) scale to assess the effects of prior authorization among Texas Medicaid providers. Adm Policy Ment Health. 2009;36(4):278-287.
13. Rascati KL, Brown CM. Prior authorization for antipsychotic medications—It’s not just about the money. Clin Ther. 2008;30(8):1506-1507.
14. Lu CY, Soumerai SB, Ross-Degnan D, et al. Unintended impacts of a Medicaid prior authorization policy on access to medications for bipolar disorder. Med Care. 2010;48(1):4-9.
15. Stephens RJ, White SE, Cudnik M, et al. Factors associated with longer lengths of stay for mental health emergency department patients. J Emerg Med. 2014; 47(4):412-419.
16. Brown JD, Barrett A, Caffery E, et al. Medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder. Psychiatr Serv. 2013;64(9):878-885.
17. American Medical Association. Opinion 10.01– Fundamental elements of the patient-physician relationship. http://www.ama-assn.org/ama/pub/ physician-resources/medical-ethics/code-medical-ethics/opinion1001.page?. Accessed October 11, 2014.
18. Hall RC. Ethical and legal implications of managed care. Gen Hosp Psychiatry. 1997;19(3):200-208.
19. Porter v Thadani, 2010 U.S. Dist. LEXIS 35145 (NH 2010).
20. NB ex rel Peacock v District of Columbia, 682 F3d 77 (DC Cir 2012).
21. Wilson v Blue Cross of Southern California, 222 Cal App 3d 660, 271 Cal Rptr 876 (1990).
22. Wickline v State of California, 192 Cal App 3d 1630, 239 Cal Rptr 810 (1986).
23. Terry K. Prior authorization made easier. Med Econ. 2007;84(20):34,38,40.
24. American Medical Association. Ethics Opinion 6.07– Insurance forms completion charges. http://www. ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion607.page? Updated June 1994. Accessed October 11, 2014.
25. Gibson v Medco Health Solutions, 06-CVF-106 (OH 2008).
26. Bendix J. Curing the prior authorization headache. Med Econ. 2013;90(19):24,26-27,29-31.
27. American Medical Association. Electronic prior authorization toolkit. Available at http://www.ama-assn.org/ama/pub/advocacy/topics/administrative-simplification-initiatives/electronic-transactions-toolkit/ prior-authorization.page. Accessed October 11, 2014.
What are your responsibilities after a screening call?
Dear Dr. Mossman,
When I take a call from a treatment-seeker at our outpatient clinic, I ask brief screening questions to determine whether our services would be appropriate. Shortly after I screened one caller, Ms. C, she called back requesting a medication refill and asking about her diagnosis.
What obligation do I have to Ms. C? Is she my patient? Would I be liable if I didn’t help her out and something bad happened to her?
Submitted by “Dr. S”
Office and hospital Web sites, LinkedIn profiles, and Facebook pages are just a few of the ways that people find physicians and learn about their services. But most 21st century doctor-patient relationships still start with 19th century technology: a telephone call.
Talking with prospective patients before setting up an appointment makes sense. A short conversation can clarify whether you offer the services that a caller needs and increases the show-up rate for initial appointments.1
But if you ask for some personal history and information about symptoms in a screening interview, does that make the caller your patient? Ms. C seemed to have thought so. To find out whether Ms. C was right and to learn how Dr. S should handle initial telephone calls, we’ll look at:
• the rationale for screening callers before initiating treatment
• features of screening that can create a doctor-patient relationship
• how to fulfill duties that result from screening.
Why screen prospective patients?
Mental health treatment has become more diversified and specialized over the past 30 years. No psychiatrist nowadays has all the therapeutic skills that all potential patients might need.
Before speaking to you, a treatment-seeker often won’t know whether your practice style will fit his (her) needs. You might prefer not to provide medication management for another clinician’s psychotherapy patient or, if you’re like most psychiatrists, you might not offer psychotherapy.
In the absence of prior obligation (eg, agreeing to provide coverage for an emergency room), physicians may structure their practices and contract for their services as they see fit2—but this leaves you with some obligation to screen potential patients for appropriate mutual fit. In years past, some psychiatrists saw potential patients for an in-office evaluation to decide whether to provide treatment—a practicethat remains acceptable if the person is told, when the appointment is made, that the first meeting is “to meet each other and see if you want to establish a treatment relationship.”3
Good treatment plans take into account patients’ temperament, emotional state, cognitive capacity, culture, family circumstances, substance use, and medical history.4 Common mental conditions often can be identified in a telephone call.5,6 Although the diagnostic accuracy of such efforts is uncertain,7 such calls can help practitioners determine whether they offer the right services for callers. Good decisions about initiating care always take financial pressures and constraints into account,8 and a pre-appointment telephone call can address those issues, too.
For all these reasons, talking to a prospective patient before he comes to see you makes sense. Screening lets you decide:
• whether you’re the right clinician for his needs
• who the right clinician is if you are not
• whether he should seek emergency evaluation when the situation sounds urgent.
Do phone calls start treatment?
As Dr. S’s questions show, telephone screenings might leave some callers thinking that treatment has started, even before their first office appointment. Having a treatment relationship is a prerequisite to malpractice liability,9 and courts have concluded that, under the right circumstances, telephone assessments do create physician-patient relationships.
Creating a physician-patient relationship
How or when might telephone screening make someone your patient? This question doesn’t have a precise answer, but how courts decided similar questions has depended on the questions the physician asked and whether the physician offered what sounded like medical advice.10,11 A physician-patient relationship forms when the physician takes some implied or affirmative action to treat, see, examine, care for, or offer a diagnosis to the patient,9,12,13 such as:
• knowingly accepting someone as a patient14
• explicitly agreeing to treat a person
• “acting in some other way such that the patient might reasonably be led to assume a doctor-patient relationship has been established.”15
Also, the “fact that a physician does not deal directly with a patient does not necessarily preclude the existence of a physician-patient relationship,”12 so a telephone conversation can create such a relationship if it contains the right elements. Table 116 highlights actions that, during the course of screening, might constitute initiation of a physician-patient relationship. Table 2 offers suggestions for managing initial telephone contacts to reduce the chance of inadvertently creating a physician-patient relationship.
In the eyes of the law, whether a physician-patient relationship was formed depends on specific facts of the situation and may be decided by a jury.13,14 In the case of Ms. C, Dr. S might avoid premature creation of a physician-patient relationship by refraining from offering a diagnosis at the conclusion of the screening call.17
Prescribing
Although features of the original screening interview indicated that Ms. C was not yet Dr. S’s patient, prescribing certainly would commence a physician-patient relationship.18 But even if the screening had made Ms. C a patient, refilling her prescription now probably is a bad idea.
Assuming that a physician-patient relationship exists, it is unlikely that a short telephone interview gave Dr. S enough information about Ms. C’s medical history and present mental status to ensure that his diagnostic reasoning would not be faulty. It also is unlikely that telephone screening allowed Dr. S to meet the standard of care for prescribing—a process that involves choosing medications suitable to the patient’s clinical needs, checking the results of any necessary lab tests, and obtaining appropriate informed consent.19
Satisfying duties
Outpatient facilities can instruct telephone screeners to conduct interviews in ways that reduce inadvertent establishment of a treatment relationship, but establishing such a relationship cannot be avoided in all cases. If a caller is distraught or in crisis, for example, compassion dictates helping him, and some callers (eg, Ms. C) may feel they have a firmer treatment relationship than actually exists.
Once you have created a physician-patient relationship, you must continue that relationship until you end it appropriately.3 That does not mean you have to provide definitive treatment; you simply need to exercise “reasonable care according to the standards of the profession.”16,20 If a caller telephones in an emergency situation, for example, the screening clinician should take appropriate steps to ensure safety, which might include calling law enforcement or facilitating hospitalization.3
One way to fulfill the duties of a physician-patient relationship inadvertently established during initial screening is through explicit discharge (if medically appropriate) or transfer of care to another physician.15 A prudent clinic or practitioner will describe other mental health resources in the community and sometimes assist with referral if the inquiring potential patient needs services that the provider does not offer.
In many communities, finding appropriate mental health resources is difficult. Creative approaches to this problem include transitional psychiatry or crisis support clinics that serve as a “bridge” to longer-term services,21,22 preliminary process groups,23 and telepsychiatry transitional clinics.24 When a clinic does not accept a person as a patient, the clinic should clearly document 1) key features of the contact and 2) the rationale for that decision
Bottom Line
You have a right and a responsibility to screen prospective patients for good fit to your treatment services. In doing so, however, you might inadvertently create a physician-patient relationship. If this happens, you should fulfill your clinical responsibilities, as you would for any patient, by helping the patient get appropriate care from you or another provider.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Shoffner J, Staudt M, Marcus S, et al. Using telephone reminders to increase attendance at psychiatric appointments: findings of a pilot study in rural Appalachia. Psychiatr Serv. 2007;58(6):872-875.
2. Hiser v Randolph, 1980 617 P2d 774 (Ariz App).
3. American Psychiatric Association. Practice management for early career psychiatrists: a reference guide, 6th edition. http://www.psych.org/practice/managing-a-practice/ starting-a-practice. Published October 16, 2006. Accessed July 8, 2014.
4. Delgado SV, Strawn JR. Difficult psychiatric consultations: an integrated approach. New York, NY: Springer; 2014.
5. Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatric Pract. 2004;10(5): 307-313.
6. Michel C, Schimmelmann BG, Kupferschmid S, et al. Reliability of telephone assessments of at-risk criteria of psychosis: a comparison to face-to-face interviews. Schizophr Res. 2014;153(1-3):251-253.
7. Muskens EM, Lucassen P, Groenleer W, et al. Psychiatric diagnosis by telephone: is it an opportunity [published online March 15, 2014]? Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-014-0861-9.
8. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802.
9. Roberts v Sankey, 2004 813 NE2d 1195 (Ind App).
10. O’Neill v Montefiore Hospital, 1960 202 NYS 2d 436 (NY App).
11. McKinney v Schlatter, 1997 692 NE2d 1045 (Ohio App).
12. Dehn v Edgecombe, 865 A2d 603 (Md 2005).
13. Kelley v Middle Tennessee Emergency Physicians, 133 SW3d 587 (Tenn 2004).
14. Oliver v Brock, 342 So2d 1 (Ala 1976).
15. Appelbaum PS, Gutheil TG. Malpractice and other forms of liability. In: Appelbaum PS, Gutheil TG, eds. Clinical Handbook of Psychiatry and the Law, 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2007:115-116.
16. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
17. Torres A, Wagner R. Establishing the physician-patient relationship. J Dermatol Surg Oncol. 1993;19(2):147-149.
18. Aboff BM, Collier VU, Farber NJ, et al. Residents’ prescription writing for nonpatients. JAMA. 2002;288(3):381-385.
19. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
20. Brown v Koulizakis, 331 SE2d 440 (Va 1985).
21. University of Michigan Department of Psychiatry. Crisis support clinic. http://www.psych.med.umich.edu/patient-care/crisis-support-clinic. Accessed July 9, 2014.
22. UAB Department of Psychiatry. http://www.uab.edu/ medicine/psychiatry. Accessed July 9, 2014.
23. Stone WN, Klein EB. The waiting-list group. Int J Group Psychother. 1999;49(4):417-428.
24. Detweiler MB, Arif S, Candelario J, et al. A telepsychiatry transition clinic: the first 12 months experience. J Telemed Telecare. 2011;17(6):293-297.
Dear Dr. Mossman,
When I take a call from a treatment-seeker at our outpatient clinic, I ask brief screening questions to determine whether our services would be appropriate. Shortly after I screened one caller, Ms. C, she called back requesting a medication refill and asking about her diagnosis.
What obligation do I have to Ms. C? Is she my patient? Would I be liable if I didn’t help her out and something bad happened to her?
Submitted by “Dr. S”
Office and hospital Web sites, LinkedIn profiles, and Facebook pages are just a few of the ways that people find physicians and learn about their services. But most 21st century doctor-patient relationships still start with 19th century technology: a telephone call.
Talking with prospective patients before setting up an appointment makes sense. A short conversation can clarify whether you offer the services that a caller needs and increases the show-up rate for initial appointments.1
But if you ask for some personal history and information about symptoms in a screening interview, does that make the caller your patient? Ms. C seemed to have thought so. To find out whether Ms. C was right and to learn how Dr. S should handle initial telephone calls, we’ll look at:
• the rationale for screening callers before initiating treatment
• features of screening that can create a doctor-patient relationship
• how to fulfill duties that result from screening.
Why screen prospective patients?
Mental health treatment has become more diversified and specialized over the past 30 years. No psychiatrist nowadays has all the therapeutic skills that all potential patients might need.
Before speaking to you, a treatment-seeker often won’t know whether your practice style will fit his (her) needs. You might prefer not to provide medication management for another clinician’s psychotherapy patient or, if you’re like most psychiatrists, you might not offer psychotherapy.
In the absence of prior obligation (eg, agreeing to provide coverage for an emergency room), physicians may structure their practices and contract for their services as they see fit2—but this leaves you with some obligation to screen potential patients for appropriate mutual fit. In years past, some psychiatrists saw potential patients for an in-office evaluation to decide whether to provide treatment—a practicethat remains acceptable if the person is told, when the appointment is made, that the first meeting is “to meet each other and see if you want to establish a treatment relationship.”3
Good treatment plans take into account patients’ temperament, emotional state, cognitive capacity, culture, family circumstances, substance use, and medical history.4 Common mental conditions often can be identified in a telephone call.5,6 Although the diagnostic accuracy of such efforts is uncertain,7 such calls can help practitioners determine whether they offer the right services for callers. Good decisions about initiating care always take financial pressures and constraints into account,8 and a pre-appointment telephone call can address those issues, too.
For all these reasons, talking to a prospective patient before he comes to see you makes sense. Screening lets you decide:
• whether you’re the right clinician for his needs
• who the right clinician is if you are not
• whether he should seek emergency evaluation when the situation sounds urgent.
Do phone calls start treatment?
As Dr. S’s questions show, telephone screenings might leave some callers thinking that treatment has started, even before their first office appointment. Having a treatment relationship is a prerequisite to malpractice liability,9 and courts have concluded that, under the right circumstances, telephone assessments do create physician-patient relationships.
Creating a physician-patient relationship
How or when might telephone screening make someone your patient? This question doesn’t have a precise answer, but how courts decided similar questions has depended on the questions the physician asked and whether the physician offered what sounded like medical advice.10,11 A physician-patient relationship forms when the physician takes some implied or affirmative action to treat, see, examine, care for, or offer a diagnosis to the patient,9,12,13 such as:
• knowingly accepting someone as a patient14
• explicitly agreeing to treat a person
• “acting in some other way such that the patient might reasonably be led to assume a doctor-patient relationship has been established.”15
Also, the “fact that a physician does not deal directly with a patient does not necessarily preclude the existence of a physician-patient relationship,”12 so a telephone conversation can create such a relationship if it contains the right elements. Table 116 highlights actions that, during the course of screening, might constitute initiation of a physician-patient relationship. Table 2 offers suggestions for managing initial telephone contacts to reduce the chance of inadvertently creating a physician-patient relationship.
In the eyes of the law, whether a physician-patient relationship was formed depends on specific facts of the situation and may be decided by a jury.13,14 In the case of Ms. C, Dr. S might avoid premature creation of a physician-patient relationship by refraining from offering a diagnosis at the conclusion of the screening call.17
Prescribing
Although features of the original screening interview indicated that Ms. C was not yet Dr. S’s patient, prescribing certainly would commence a physician-patient relationship.18 But even if the screening had made Ms. C a patient, refilling her prescription now probably is a bad idea.
Assuming that a physician-patient relationship exists, it is unlikely that a short telephone interview gave Dr. S enough information about Ms. C’s medical history and present mental status to ensure that his diagnostic reasoning would not be faulty. It also is unlikely that telephone screening allowed Dr. S to meet the standard of care for prescribing—a process that involves choosing medications suitable to the patient’s clinical needs, checking the results of any necessary lab tests, and obtaining appropriate informed consent.19
Satisfying duties
Outpatient facilities can instruct telephone screeners to conduct interviews in ways that reduce inadvertent establishment of a treatment relationship, but establishing such a relationship cannot be avoided in all cases. If a caller is distraught or in crisis, for example, compassion dictates helping him, and some callers (eg, Ms. C) may feel they have a firmer treatment relationship than actually exists.
Once you have created a physician-patient relationship, you must continue that relationship until you end it appropriately.3 That does not mean you have to provide definitive treatment; you simply need to exercise “reasonable care according to the standards of the profession.”16,20 If a caller telephones in an emergency situation, for example, the screening clinician should take appropriate steps to ensure safety, which might include calling law enforcement or facilitating hospitalization.3
One way to fulfill the duties of a physician-patient relationship inadvertently established during initial screening is through explicit discharge (if medically appropriate) or transfer of care to another physician.15 A prudent clinic or practitioner will describe other mental health resources in the community and sometimes assist with referral if the inquiring potential patient needs services that the provider does not offer.
In many communities, finding appropriate mental health resources is difficult. Creative approaches to this problem include transitional psychiatry or crisis support clinics that serve as a “bridge” to longer-term services,21,22 preliminary process groups,23 and telepsychiatry transitional clinics.24 When a clinic does not accept a person as a patient, the clinic should clearly document 1) key features of the contact and 2) the rationale for that decision
Bottom Line
You have a right and a responsibility to screen prospective patients for good fit to your treatment services. In doing so, however, you might inadvertently create a physician-patient relationship. If this happens, you should fulfill your clinical responsibilities, as you would for any patient, by helping the patient get appropriate care from you or another provider.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
When I take a call from a treatment-seeker at our outpatient clinic, I ask brief screening questions to determine whether our services would be appropriate. Shortly after I screened one caller, Ms. C, she called back requesting a medication refill and asking about her diagnosis.
What obligation do I have to Ms. C? Is she my patient? Would I be liable if I didn’t help her out and something bad happened to her?
Submitted by “Dr. S”
Office and hospital Web sites, LinkedIn profiles, and Facebook pages are just a few of the ways that people find physicians and learn about their services. But most 21st century doctor-patient relationships still start with 19th century technology: a telephone call.
Talking with prospective patients before setting up an appointment makes sense. A short conversation can clarify whether you offer the services that a caller needs and increases the show-up rate for initial appointments.1
But if you ask for some personal history and information about symptoms in a screening interview, does that make the caller your patient? Ms. C seemed to have thought so. To find out whether Ms. C was right and to learn how Dr. S should handle initial telephone calls, we’ll look at:
• the rationale for screening callers before initiating treatment
• features of screening that can create a doctor-patient relationship
• how to fulfill duties that result from screening.
Why screen prospective patients?
Mental health treatment has become more diversified and specialized over the past 30 years. No psychiatrist nowadays has all the therapeutic skills that all potential patients might need.
Before speaking to you, a treatment-seeker often won’t know whether your practice style will fit his (her) needs. You might prefer not to provide medication management for another clinician’s psychotherapy patient or, if you’re like most psychiatrists, you might not offer psychotherapy.
In the absence of prior obligation (eg, agreeing to provide coverage for an emergency room), physicians may structure their practices and contract for their services as they see fit2—but this leaves you with some obligation to screen potential patients for appropriate mutual fit. In years past, some psychiatrists saw potential patients for an in-office evaluation to decide whether to provide treatment—a practicethat remains acceptable if the person is told, when the appointment is made, that the first meeting is “to meet each other and see if you want to establish a treatment relationship.”3
Good treatment plans take into account patients’ temperament, emotional state, cognitive capacity, culture, family circumstances, substance use, and medical history.4 Common mental conditions often can be identified in a telephone call.5,6 Although the diagnostic accuracy of such efforts is uncertain,7 such calls can help practitioners determine whether they offer the right services for callers. Good decisions about initiating care always take financial pressures and constraints into account,8 and a pre-appointment telephone call can address those issues, too.
For all these reasons, talking to a prospective patient before he comes to see you makes sense. Screening lets you decide:
• whether you’re the right clinician for his needs
• who the right clinician is if you are not
• whether he should seek emergency evaluation when the situation sounds urgent.
Do phone calls start treatment?
As Dr. S’s questions show, telephone screenings might leave some callers thinking that treatment has started, even before their first office appointment. Having a treatment relationship is a prerequisite to malpractice liability,9 and courts have concluded that, under the right circumstances, telephone assessments do create physician-patient relationships.
Creating a physician-patient relationship
How or when might telephone screening make someone your patient? This question doesn’t have a precise answer, but how courts decided similar questions has depended on the questions the physician asked and whether the physician offered what sounded like medical advice.10,11 A physician-patient relationship forms when the physician takes some implied or affirmative action to treat, see, examine, care for, or offer a diagnosis to the patient,9,12,13 such as:
• knowingly accepting someone as a patient14
• explicitly agreeing to treat a person
• “acting in some other way such that the patient might reasonably be led to assume a doctor-patient relationship has been established.”15
Also, the “fact that a physician does not deal directly with a patient does not necessarily preclude the existence of a physician-patient relationship,”12 so a telephone conversation can create such a relationship if it contains the right elements. Table 116 highlights actions that, during the course of screening, might constitute initiation of a physician-patient relationship. Table 2 offers suggestions for managing initial telephone contacts to reduce the chance of inadvertently creating a physician-patient relationship.
In the eyes of the law, whether a physician-patient relationship was formed depends on specific facts of the situation and may be decided by a jury.13,14 In the case of Ms. C, Dr. S might avoid premature creation of a physician-patient relationship by refraining from offering a diagnosis at the conclusion of the screening call.17
Prescribing
Although features of the original screening interview indicated that Ms. C was not yet Dr. S’s patient, prescribing certainly would commence a physician-patient relationship.18 But even if the screening had made Ms. C a patient, refilling her prescription now probably is a bad idea.
Assuming that a physician-patient relationship exists, it is unlikely that a short telephone interview gave Dr. S enough information about Ms. C’s medical history and present mental status to ensure that his diagnostic reasoning would not be faulty. It also is unlikely that telephone screening allowed Dr. S to meet the standard of care for prescribing—a process that involves choosing medications suitable to the patient’s clinical needs, checking the results of any necessary lab tests, and obtaining appropriate informed consent.19
Satisfying duties
Outpatient facilities can instruct telephone screeners to conduct interviews in ways that reduce inadvertent establishment of a treatment relationship, but establishing such a relationship cannot be avoided in all cases. If a caller is distraught or in crisis, for example, compassion dictates helping him, and some callers (eg, Ms. C) may feel they have a firmer treatment relationship than actually exists.
Once you have created a physician-patient relationship, you must continue that relationship until you end it appropriately.3 That does not mean you have to provide definitive treatment; you simply need to exercise “reasonable care according to the standards of the profession.”16,20 If a caller telephones in an emergency situation, for example, the screening clinician should take appropriate steps to ensure safety, which might include calling law enforcement or facilitating hospitalization.3
One way to fulfill the duties of a physician-patient relationship inadvertently established during initial screening is through explicit discharge (if medically appropriate) or transfer of care to another physician.15 A prudent clinic or practitioner will describe other mental health resources in the community and sometimes assist with referral if the inquiring potential patient needs services that the provider does not offer.
In many communities, finding appropriate mental health resources is difficult. Creative approaches to this problem include transitional psychiatry or crisis support clinics that serve as a “bridge” to longer-term services,21,22 preliminary process groups,23 and telepsychiatry transitional clinics.24 When a clinic does not accept a person as a patient, the clinic should clearly document 1) key features of the contact and 2) the rationale for that decision
Bottom Line
You have a right and a responsibility to screen prospective patients for good fit to your treatment services. In doing so, however, you might inadvertently create a physician-patient relationship. If this happens, you should fulfill your clinical responsibilities, as you would for any patient, by helping the patient get appropriate care from you or another provider.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Shoffner J, Staudt M, Marcus S, et al. Using telephone reminders to increase attendance at psychiatric appointments: findings of a pilot study in rural Appalachia. Psychiatr Serv. 2007;58(6):872-875.
2. Hiser v Randolph, 1980 617 P2d 774 (Ariz App).
3. American Psychiatric Association. Practice management for early career psychiatrists: a reference guide, 6th edition. http://www.psych.org/practice/managing-a-practice/ starting-a-practice. Published October 16, 2006. Accessed July 8, 2014.
4. Delgado SV, Strawn JR. Difficult psychiatric consultations: an integrated approach. New York, NY: Springer; 2014.
5. Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatric Pract. 2004;10(5): 307-313.
6. Michel C, Schimmelmann BG, Kupferschmid S, et al. Reliability of telephone assessments of at-risk criteria of psychosis: a comparison to face-to-face interviews. Schizophr Res. 2014;153(1-3):251-253.
7. Muskens EM, Lucassen P, Groenleer W, et al. Psychiatric diagnosis by telephone: is it an opportunity [published online March 15, 2014]? Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-014-0861-9.
8. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802.
9. Roberts v Sankey, 2004 813 NE2d 1195 (Ind App).
10. O’Neill v Montefiore Hospital, 1960 202 NYS 2d 436 (NY App).
11. McKinney v Schlatter, 1997 692 NE2d 1045 (Ohio App).
12. Dehn v Edgecombe, 865 A2d 603 (Md 2005).
13. Kelley v Middle Tennessee Emergency Physicians, 133 SW3d 587 (Tenn 2004).
14. Oliver v Brock, 342 So2d 1 (Ala 1976).
15. Appelbaum PS, Gutheil TG. Malpractice and other forms of liability. In: Appelbaum PS, Gutheil TG, eds. Clinical Handbook of Psychiatry and the Law, 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2007:115-116.
16. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
17. Torres A, Wagner R. Establishing the physician-patient relationship. J Dermatol Surg Oncol. 1993;19(2):147-149.
18. Aboff BM, Collier VU, Farber NJ, et al. Residents’ prescription writing for nonpatients. JAMA. 2002;288(3):381-385.
19. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
20. Brown v Koulizakis, 331 SE2d 440 (Va 1985).
21. University of Michigan Department of Psychiatry. Crisis support clinic. http://www.psych.med.umich.edu/patient-care/crisis-support-clinic. Accessed July 9, 2014.
22. UAB Department of Psychiatry. http://www.uab.edu/ medicine/psychiatry. Accessed July 9, 2014.
23. Stone WN, Klein EB. The waiting-list group. Int J Group Psychother. 1999;49(4):417-428.
24. Detweiler MB, Arif S, Candelario J, et al. A telepsychiatry transition clinic: the first 12 months experience. J Telemed Telecare. 2011;17(6):293-297.
1. Shoffner J, Staudt M, Marcus S, et al. Using telephone reminders to increase attendance at psychiatric appointments: findings of a pilot study in rural Appalachia. Psychiatr Serv. 2007;58(6):872-875.
2. Hiser v Randolph, 1980 617 P2d 774 (Ariz App).
3. American Psychiatric Association. Practice management for early career psychiatrists: a reference guide, 6th edition. http://www.psych.org/practice/managing-a-practice/ starting-a-practice. Published October 16, 2006. Accessed July 8, 2014.
4. Delgado SV, Strawn JR. Difficult psychiatric consultations: an integrated approach. New York, NY: Springer; 2014.
5. Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatric Pract. 2004;10(5): 307-313.
6. Michel C, Schimmelmann BG, Kupferschmid S, et al. Reliability of telephone assessments of at-risk criteria of psychosis: a comparison to face-to-face interviews. Schizophr Res. 2014;153(1-3):251-253.
7. Muskens EM, Lucassen P, Groenleer W, et al. Psychiatric diagnosis by telephone: is it an opportunity [published online March 15, 2014]? Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-014-0861-9.
8. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802.
9. Roberts v Sankey, 2004 813 NE2d 1195 (Ind App).
10. O’Neill v Montefiore Hospital, 1960 202 NYS 2d 436 (NY App).
11. McKinney v Schlatter, 1997 692 NE2d 1045 (Ohio App).
12. Dehn v Edgecombe, 865 A2d 603 (Md 2005).
13. Kelley v Middle Tennessee Emergency Physicians, 133 SW3d 587 (Tenn 2004).
14. Oliver v Brock, 342 So2d 1 (Ala 1976).
15. Appelbaum PS, Gutheil TG. Malpractice and other forms of liability. In: Appelbaum PS, Gutheil TG, eds. Clinical Handbook of Psychiatry and the Law, 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2007:115-116.
16. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
17. Torres A, Wagner R. Establishing the physician-patient relationship. J Dermatol Surg Oncol. 1993;19(2):147-149.
18. Aboff BM, Collier VU, Farber NJ, et al. Residents’ prescription writing for nonpatients. JAMA. 2002;288(3):381-385.
19. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
20. Brown v Koulizakis, 331 SE2d 440 (Va 1985).
21. University of Michigan Department of Psychiatry. Crisis support clinic. http://www.psych.med.umich.edu/patient-care/crisis-support-clinic. Accessed July 9, 2014.
22. UAB Department of Psychiatry. http://www.uab.edu/ medicine/psychiatry. Accessed July 9, 2014.
23. Stone WN, Klein EB. The waiting-list group. Int J Group Psychother. 1999;49(4):417-428.
24. Detweiler MB, Arif S, Candelario J, et al. A telepsychiatry transition clinic: the first 12 months experience. J Telemed Telecare. 2011;17(6):293-297.