User login
The end of the line: Concluding your practice when facing serious illness
Dear Dr. Mossman,
I have a possibly fatal disease. So far, my symptoms and treatment haven’t kept me from my usual activities. But if my illness worsens, I’ll have to quit practicing psychiatry. What should I be doing now to make sure I fulfill my ethical and legal obligations to my patients?
Submitted by “Dr. F”
“Remember, with great power comes great responsibility.”
- Peter Parker, Spider-Man (2002)
Peter Parker’s movie-ending statement applies to doctors as well as Spider-Man. Although we don’t swing from building to building to save cities from heinous villains, practicing medicine is a privilege that society bestows only upon physicians who retain the knowledge, skills, and ability to treat patients competently.
Doctors retire from practice for many reasons, including when deteriorating physical health or cognitive capacity prevents them from performing clinical duties properly. Dr. F’s situation is not rare. As the physician population ages,1,2 a growing number of his colleagues will face similar circumstances,3,4 and with them, the responsibility and emotional turmoil of arranging to end their medical practices.
In many ways, concluding a psychiatric practice is similar to retiring from practice in other specialties. But because we care for patients’ minds as well as their bodies, retirement affects psychiatrists in distinctive ways that reflect our patients’ feelings toward us and our feelings toward them. To answer Dr. F’s question, this article considers having to stop practicing from 3 vantage points:
- the emotional impact on patients
- the emotional impact on the psychiatrist
- fulfilling one’s legal obligations while attending to the emotions of patients as well as oneself.
Emotional impact on patients
A content analysis study suggests that the traits patients appreciate in family physicians include the availability to listen, caring and compassion, trusted medical judgment, conveying the patient’s importance during encounters, feelings of connectedness, knowledge and understanding of the patient’s family, and relationship longevity.5 The same factors likely apply to relationships between psychiatrists and their patients, particularly if treatment encounters have extended over years and have involved conversations beyond those needed merely to write prescriptions.
Psychoanalytic publications offer many descriptions of patients’ reactions to the illness or death of their mental health professional. A 1978 study of 27 analysands whose physicians died during ongoing therapy reported reactions that ranged from a minimal impact to protracted mourning accompanied by helplessness, intense crying, and recurrent dreams about the analyst.6 Although a few patients were relieved that death had ended a difficult treatment, many were angry at their doctor for not attending to self-care and for breaking their treatment agreement, or because they had missed out on hoped-for benefits.
A 2010 study described the pain and distress that patients may experience following the death of their analyst or psychotherapist. These accounts emphasized the emotional isolation of grieving patients, who do not have the social support that bereaved persons receive after losing a loved one.7 Successful psychotherapy provides a special relationship characterized by trust, intimacy, and safety. But if the therapist suddenly dies, this relationship “is transformed into a solitude like no other.”8
Because the sudden “rupture of an analytic process is bound to be traumatic and may cause iatrogenic injury to the patient,” Traesdal9 advocates that therapists in situations similar to Dr. F’s discuss their possible death “on the reality level at least once during any analysis or psychotherapy.… It is extremely helpful to a patient to have discussed … how to handle the situation” if the therapist dies. This discussion also offers the patient an opportunity to confront a cultural taboo around death and to increase capacity to tolerate pain, illness, and aging.10,11
Most psychiatric care today is not psychoanalysis; psychiatrists provide other forms of care that create less intense doctor–patient relationships. Yet knowledge of these kinds of reactions may help Dr. F stay attuned to his patients’ concerns and to contemplate what they may experience, to greater or lesser degrees, if his health declines.
Retirement’s emotional impact on the psychiatrist
Published guidance on concluding a psychiatric practice is sparse, considering that all psychiatrists are mortal and stop practicing at some point.12Not thinking about or planning for retirement is a psychiatric tradition that started with Freud. He saw patients until shortly before his death and did not seem to have planned for ending his practice, despite suffering with jaw cancer for 16 years.13
Practicing medicine often is more than just a career; it is a core aspect of many physicians’ identity.14 Most of us spend a large fraction of our waking hours caring for patients and meeting other job requirements (eg, teaching, maintaining knowledge and skills), and many of us have scant time to pursue nonmedical interests. An intense prioritization of one’s “medical identity” makes retirement a blow to a doctor’s self-worth and sense of meaning in life.15,16
Because their work is not physically demanding, most psychiatrists continue to practice beyond the age of 65 years.12,17 More important, perhaps, is that being a psychiatrist is uniquely rewarding. As Benjamin Rush observed in an 1810 letter to Pennsylvania Hospital, successfully treating any medical disease is gratifying, but “what is this pleasure compared with that of restoring a fellow creature from the anguish and folly of madness and of reviving in him the knowledge of himself, his family, his friends, and his God!”18
Physicians in any specialty that involves repeated contact with the same patients form emotional bonds with their patients that retirement breaks.14 Psychiatrists’ interest in how patients think, feel, and cope with problems creates special attachments17 that can make some terminations “emotionally excruciating.”12
Psychiatrists with serious illness
What guidance might Dr. F find regarding whether to broach the subject of his illness with patients, and if so, how? No one has conducted controlled trials to answer these questions. Rather, published discussion of psychiatrists’ serious illness is found mainly in the psychotherapy literature. What’s available consists of individual accounts and case series that lack scientific rigor and offer little clarity about what the therapist should say, when to say it, and how to initiate the discussion.19,20 Yet Dr. F may find some of these authors’ ideas and suggestions helpful, particularly if his psychiatric practice includes providing psychotherapy.
As a rule, psychiatrists avoid talking about themselves, but having a serious illness that could affect treatment often justifies deviating from this practice. Although Dr. F (like many psychiatrists) may be concerned that discussing his health will make patients anxious or “contaminate” what they are able or willing to say,21 not providing information or avoiding discussion (especially if a patient asks about your health) may quickly undermine a patient’s trust.21,22 Even in psychoanalytic treatment, it makes little sense to encourage patients “to speak freely on the pretense that all is well, despite obvious evidence to the contrary.”19
Physicians often deny—or at least avoid thinking about—their own mortality.23 But avoiding talking about something so important (and often so obvious) as one’s illness may risk supporting patients’ denial of crucial matters in their own lives.19,21 Moreover, Dr. F’s inadvertent self-disclosure (eg, by displaying obvious signs of illness) may do more harm to therapy than a planned statement in which Dr. F has prepared what he’ll say to answer his patients’ questions.20
That Dr. F has continued working while suffering from a potentially fatal illness seems noble. Yet by doing so, he accepts not only the burdens of his illness but also the obligation to continue to serve his patients competently. This requires maintaining emotional steadiness and not using patients for emotional support, but instead obtaining and using the support of his friends, colleagues, family, consultants, and caregivers.20
Legal obligations
Retirement does not end a physician’s professional legal obligations.24 The legal rules and duties for psychiatrists who leave their practices are similar to those that apply to other physicians. Mishandling these aspects of retirement can result in various legal, licensure-related, or economic consequences, depending on your circumstances and employment arrangements.
Employment contracts in hospital or group practices often require notice of impending departures. If applicable to Dr. F’s situation, failure to comply with such conditions may lead to forfeiture of buyout payments, paying for malpractice tail coverage, or lawsuits claiming violation of contractual agreements.25
Retirement also creates practical and legal responsibilities to patients that are separate from the interpersonal and emotional issues previously discussed. How will those who need ongoing care and coverage be cared for? When withdrawing from a patient’s care (because of retirement or other reasons), a physician should give the patient enough advance notice to set up satisfactory treatment arrangements elsewhere and should facilitate transfer of the patient’s care, if appropriate.26 Failure to meet this ethical obligation may lead to a malpractice action alleging abandonment, which is defined as “the unilateral severance of the professional relationship … without reasonable notice at a time when there is still the necessity of continuing medical attention.”27
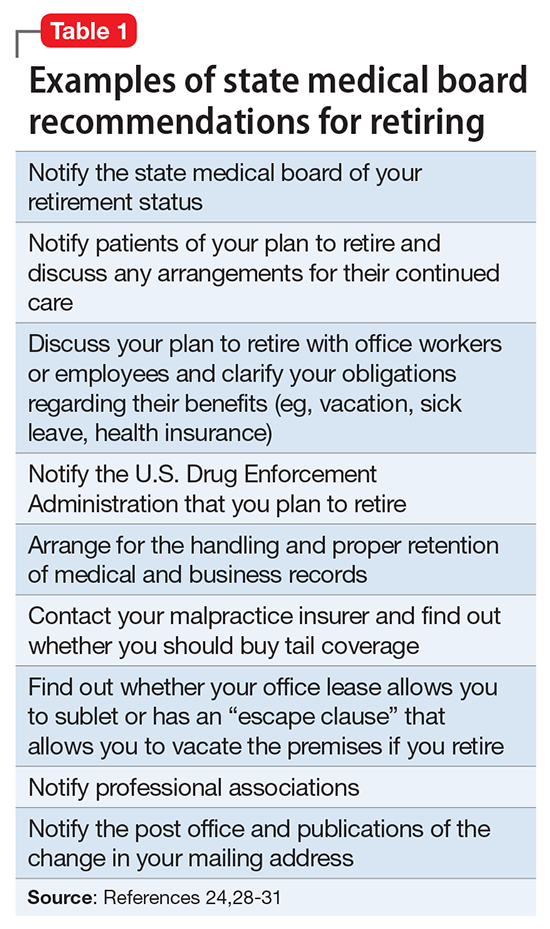
Further obligations come from medical licensing boards, which, in many states, have established time frames and specific procedures for informing patients and the public when a physician is leaving practice. Table 124,28-31 lists examples of these. If Dr. F works in a state where the board hasn’t promulgated such regulations, Table 124,28-31 may still help him think through how to discharge his ethical responsibilities to notify patients, colleagues, and business entities that he is ending his practice. References 28-30 and 32 discuss several of these matters, suggest timetables for various steps of a practice closure, and provide sample letters for notifying patients.
Physicians also must preserve their medical records for a certain period after they retire. States with rules on this matter require record preservation for 5 to 10 years or until 2 or 3 years after minor patients reach the age of majority.33 The Health Insurance Portability and Accountability Act of 1996 requires covered entities, which include most psychiatrists, to retain records for 6 years,34 and certain Medicare programs require retention for 10 years.35
Depending on Dr. F’s location and type of practice, his records should be preserved for the longest period that applies. If he is leaving a group practice that owns the records, arranging for this should be easy. If leaving an independent practice, he may need to ask another practice to perform this function.25
A ‘professional will’
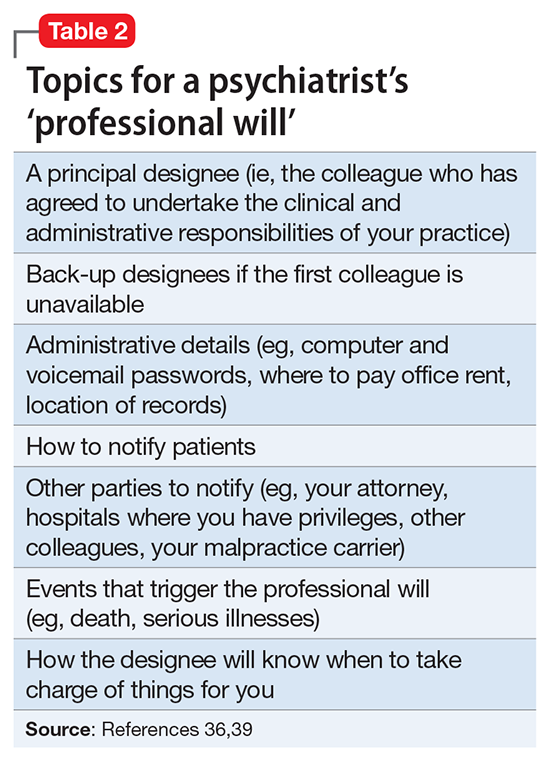
Dr. F also might consider a measure that many psychotherapists recommend13,19,36 and that in some states is required by mental health licensing boards or professional codes37,38: creating a “professional will” that contains instructions for handling practice matters in case of death or disability.39
1. LoboPrabhu SM, Molinari VA, Hamilton JD, et al. The aging physician with cognitive impairment: approaches to oversight, prevention, and remediation. Am J Geriatr Psychiatry. 2009;17(6):445-454.
2. Dellinger EP, Pellegrini CA, Gallagher TH. The aging physician and the medical profession: a review. JAMA Surg. 2017;152(10):967-971.
3. Dall T, West T, Chakrabarti R, et al. The complexities of physician supply and demand: projections from 2014 to 2025. Association of American Medical Colleges. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published 2016. Accessed September 26, 2017.
4. Draper B, Winfield S, Luscombe G. The older psychiatrist and retirement. Int J Geriatr Psychiatry. 1997;12(2):233-239.
5. Merenstein B, Merenstein J. Patient reflections: saying good-bye to a retiring family doctor. J Am Board Fam Med. 2008;21(5):461-465.
6. Lord R, Ritvo S, Solnit AJ. Patients’ reactions to the death of the psychoanalyst. Intern J Psychoanal. 1978;59(2-3):189-197.
7. Power A. Forced endings in psychotherapy and psychoanalysis: attachment and loss in retirement. New York, NY: Routledge; 2016.
8. Robutti A. When the patient loses his/her analyst. Italian Psychoanalytic Annual. 2010;4:129-145.
9. Traesdal T. When the analyst dies: dealing with the aftermath. J Am Psychoanal Assoc. 2005;53(4):1235-1255.
10. Deutsch RA. A voice lost, a voice found: after the death of the analyst. In: Deutsch RA, ed. Traumatic ruptures: abandonment and betrayal in the analytic relationship. New York, NY: Routledge; 2014:32-45.
11. Ward VP. On Yoda, trouble, and transformation: the cultural context of therapy and supervision. Contemp Fam Ther. 2009;31(3):171-176.
12. Moffic HS. Mental bootcamp: today is the first day of your retirement! Psychiatr Times. http://www.psychiatrictimes.com/blogs/couch-crisis/mental-bootcamp-today-first-day-your-retirement. Published June 25, 2012. Accessed October 31, 2017.
13. Shatsky P. Everything ends: identity and the therapist’s retirement. Clin Soc Work J. 2016;44(2):143-149.
14. Collier R.
15. Onyura B, Bohnen J, Wasylenki D, et al. Reimagining the self at late-career transitions: how identity threat influences academic physicians’ retirement considerations. Acad Med. 2015;90(6):794-801.
16. Silver MP. Critical reflection on physician retirement. Can Fam Physician. 2016;62(10):783-784.
17. Clemens NA. A psychiatrist retires: an oxymoron? J Psychiatr Pract. 2011;17(5):351-354.
18. Packard FR. The earliest hospitals. In: Packard FR. History of medicine in the United States. Philadelphia, PA: Lippincott; 1901:348.
19. Galatzer-Levy RM. The death of the analyst: patients whose previous analyst died while they were in treatment. J Amer Psychoanalytic Assoc. 2004;52(4):999-1024.
20. Fajardo B. Life-threatening illness in the analyst. J Am Psychoanal Assoc. 2001;49(2):569-586.
21. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
22. Howe E. Should psychiatrists self disclose? Innov Clin Neurosci. 2011;8(12):14-17.
23. Rizq R, Voller D. ‘Who is the third who walks always beside you?’ On the death of a psychoanalyst. Psychodyn Pract. 2013;19(2):143-167.
24. Babitsky S, Mangraviti JJ. The biggest legal mistakes physicians make—and how to avoid them. Falmouth, MA: SEAK, Inc.; 2005.
25. Armon BD, Bayus K. Legal considerations when making a practice change. Chest. 2014;146(1):215-219.
26. American Medical Association. Opinions on patient-physician relationships: 1.1.5 terminating a patient-physician relationship. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethics-chapter-1.pdf. Published 2016. Accessed September 29, 2017.
27. Lee v Dewbre, 362 S.W. 2d 900 (Tex Civ App 7th Dist 1962).
28. Medical Association of Georgia. Issues for the retiring physician. https://www.mag.org/georgia/uploadedfiles/issues-retiring-physicians.pdf. Accessed October 1, 2017.
29. Massachusetts Medical Society. Issues for the retiring physician. http://www.massmed.org/physicians/practice-management/practice-ownership-and-operations/issues-for-the-retiring-physician-(pdf). Published 2012. Accessed October 1, 2017.
30. North Carolina Medical Board. The doctor is out: a physician’s guide to closing a practice. https://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 1, 2017.
31. 243 Code of Mass. Regulations §2.06(4)(a).
32. Sampson K. Physician’s guide to closing a practice. Maine Medical Association. https://www.mainemed.com/sites/default/files/content/Closing%20Practice%20Guide%20FINAL%206.2014.pdf. Published 2014. Accessed October 1, 2017.
33. HealthIT.gov. State medical record laws: minimum medical record retention periods for records held by medical doctors and hospitals. https://www.healthit.gov/sites/default/files/appa7-1.pdf. Accessed September 29, 2017.
34. 45 CFR §164.316(b)(2).
35. 42 CFR §422.504(d)(2)(iii).
36. Pope KS, Vasquez MJT. How to survive and thrive as a therapist: information, ideas, and resources for psychologists in practice. Washington, DC: American Psychological Association; 2005.
37. Becher EH, Ogasawara T, Harris SM. Death of a clinician: the personal, practical and clinical implications of therapist mortality. Contemp Fam Ther. 2012;34(3):313-321.
38. Hovey JK. Mortality practices: how clinical social workers interact with their mortality within their clinical and professional practice. Theses, Dissertations, and Projects.Paper 1081. http://scholarworks.smith.edu/cgi/viewcontent.cgi?article=2158&context=theses. Published 2014. Accessed October 1, 2017.
39. Frankel AS, Alban A. Professional wills: protecting patients, family members and colleagues. The Steve Frankel Group. https://www.sfrankelgroup.com/professional-wills.html. Accessed October 31, 2017.
Dear Dr. Mossman,
I have a possibly fatal disease. So far, my symptoms and treatment haven’t kept me from my usual activities. But if my illness worsens, I’ll have to quit practicing psychiatry. What should I be doing now to make sure I fulfill my ethical and legal obligations to my patients?
Submitted by “Dr. F”
“Remember, with great power comes great responsibility.”
- Peter Parker, Spider-Man (2002)
Peter Parker’s movie-ending statement applies to doctors as well as Spider-Man. Although we don’t swing from building to building to save cities from heinous villains, practicing medicine is a privilege that society bestows only upon physicians who retain the knowledge, skills, and ability to treat patients competently.
Doctors retire from practice for many reasons, including when deteriorating physical health or cognitive capacity prevents them from performing clinical duties properly. Dr. F’s situation is not rare. As the physician population ages,1,2 a growing number of his colleagues will face similar circumstances,3,4 and with them, the responsibility and emotional turmoil of arranging to end their medical practices.
In many ways, concluding a psychiatric practice is similar to retiring from practice in other specialties. But because we care for patients’ minds as well as their bodies, retirement affects psychiatrists in distinctive ways that reflect our patients’ feelings toward us and our feelings toward them. To answer Dr. F’s question, this article considers having to stop practicing from 3 vantage points:
- the emotional impact on patients
- the emotional impact on the psychiatrist
- fulfilling one’s legal obligations while attending to the emotions of patients as well as oneself.
Emotional impact on patients
A content analysis study suggests that the traits patients appreciate in family physicians include the availability to listen, caring and compassion, trusted medical judgment, conveying the patient’s importance during encounters, feelings of connectedness, knowledge and understanding of the patient’s family, and relationship longevity.5 The same factors likely apply to relationships between psychiatrists and their patients, particularly if treatment encounters have extended over years and have involved conversations beyond those needed merely to write prescriptions.
Psychoanalytic publications offer many descriptions of patients’ reactions to the illness or death of their mental health professional. A 1978 study of 27 analysands whose physicians died during ongoing therapy reported reactions that ranged from a minimal impact to protracted mourning accompanied by helplessness, intense crying, and recurrent dreams about the analyst.6 Although a few patients were relieved that death had ended a difficult treatment, many were angry at their doctor for not attending to self-care and for breaking their treatment agreement, or because they had missed out on hoped-for benefits.
A 2010 study described the pain and distress that patients may experience following the death of their analyst or psychotherapist. These accounts emphasized the emotional isolation of grieving patients, who do not have the social support that bereaved persons receive after losing a loved one.7 Successful psychotherapy provides a special relationship characterized by trust, intimacy, and safety. But if the therapist suddenly dies, this relationship “is transformed into a solitude like no other.”8
Because the sudden “rupture of an analytic process is bound to be traumatic and may cause iatrogenic injury to the patient,” Traesdal9 advocates that therapists in situations similar to Dr. F’s discuss their possible death “on the reality level at least once during any analysis or psychotherapy.… It is extremely helpful to a patient to have discussed … how to handle the situation” if the therapist dies. This discussion also offers the patient an opportunity to confront a cultural taboo around death and to increase capacity to tolerate pain, illness, and aging.10,11
Most psychiatric care today is not psychoanalysis; psychiatrists provide other forms of care that create less intense doctor–patient relationships. Yet knowledge of these kinds of reactions may help Dr. F stay attuned to his patients’ concerns and to contemplate what they may experience, to greater or lesser degrees, if his health declines.
Retirement’s emotional impact on the psychiatrist
Published guidance on concluding a psychiatric practice is sparse, considering that all psychiatrists are mortal and stop practicing at some point.12Not thinking about or planning for retirement is a psychiatric tradition that started with Freud. He saw patients until shortly before his death and did not seem to have planned for ending his practice, despite suffering with jaw cancer for 16 years.13
Practicing medicine often is more than just a career; it is a core aspect of many physicians’ identity.14 Most of us spend a large fraction of our waking hours caring for patients and meeting other job requirements (eg, teaching, maintaining knowledge and skills), and many of us have scant time to pursue nonmedical interests. An intense prioritization of one’s “medical identity” makes retirement a blow to a doctor’s self-worth and sense of meaning in life.15,16
Because their work is not physically demanding, most psychiatrists continue to practice beyond the age of 65 years.12,17 More important, perhaps, is that being a psychiatrist is uniquely rewarding. As Benjamin Rush observed in an 1810 letter to Pennsylvania Hospital, successfully treating any medical disease is gratifying, but “what is this pleasure compared with that of restoring a fellow creature from the anguish and folly of madness and of reviving in him the knowledge of himself, his family, his friends, and his God!”18
Physicians in any specialty that involves repeated contact with the same patients form emotional bonds with their patients that retirement breaks.14 Psychiatrists’ interest in how patients think, feel, and cope with problems creates special attachments17 that can make some terminations “emotionally excruciating.”12
Psychiatrists with serious illness
What guidance might Dr. F find regarding whether to broach the subject of his illness with patients, and if so, how? No one has conducted controlled trials to answer these questions. Rather, published discussion of psychiatrists’ serious illness is found mainly in the psychotherapy literature. What’s available consists of individual accounts and case series that lack scientific rigor and offer little clarity about what the therapist should say, when to say it, and how to initiate the discussion.19,20 Yet Dr. F may find some of these authors’ ideas and suggestions helpful, particularly if his psychiatric practice includes providing psychotherapy.
As a rule, psychiatrists avoid talking about themselves, but having a serious illness that could affect treatment often justifies deviating from this practice. Although Dr. F (like many psychiatrists) may be concerned that discussing his health will make patients anxious or “contaminate” what they are able or willing to say,21 not providing information or avoiding discussion (especially if a patient asks about your health) may quickly undermine a patient’s trust.21,22 Even in psychoanalytic treatment, it makes little sense to encourage patients “to speak freely on the pretense that all is well, despite obvious evidence to the contrary.”19
Physicians often deny—or at least avoid thinking about—their own mortality.23 But avoiding talking about something so important (and often so obvious) as one’s illness may risk supporting patients’ denial of crucial matters in their own lives.19,21 Moreover, Dr. F’s inadvertent self-disclosure (eg, by displaying obvious signs of illness) may do more harm to therapy than a planned statement in which Dr. F has prepared what he’ll say to answer his patients’ questions.20
That Dr. F has continued working while suffering from a potentially fatal illness seems noble. Yet by doing so, he accepts not only the burdens of his illness but also the obligation to continue to serve his patients competently. This requires maintaining emotional steadiness and not using patients for emotional support, but instead obtaining and using the support of his friends, colleagues, family, consultants, and caregivers.20
Legal obligations
Retirement does not end a physician’s professional legal obligations.24 The legal rules and duties for psychiatrists who leave their practices are similar to those that apply to other physicians. Mishandling these aspects of retirement can result in various legal, licensure-related, or economic consequences, depending on your circumstances and employment arrangements.
Employment contracts in hospital or group practices often require notice of impending departures. If applicable to Dr. F’s situation, failure to comply with such conditions may lead to forfeiture of buyout payments, paying for malpractice tail coverage, or lawsuits claiming violation of contractual agreements.25
Retirement also creates practical and legal responsibilities to patients that are separate from the interpersonal and emotional issues previously discussed. How will those who need ongoing care and coverage be cared for? When withdrawing from a patient’s care (because of retirement or other reasons), a physician should give the patient enough advance notice to set up satisfactory treatment arrangements elsewhere and should facilitate transfer of the patient’s care, if appropriate.26 Failure to meet this ethical obligation may lead to a malpractice action alleging abandonment, which is defined as “the unilateral severance of the professional relationship … without reasonable notice at a time when there is still the necessity of continuing medical attention.”27
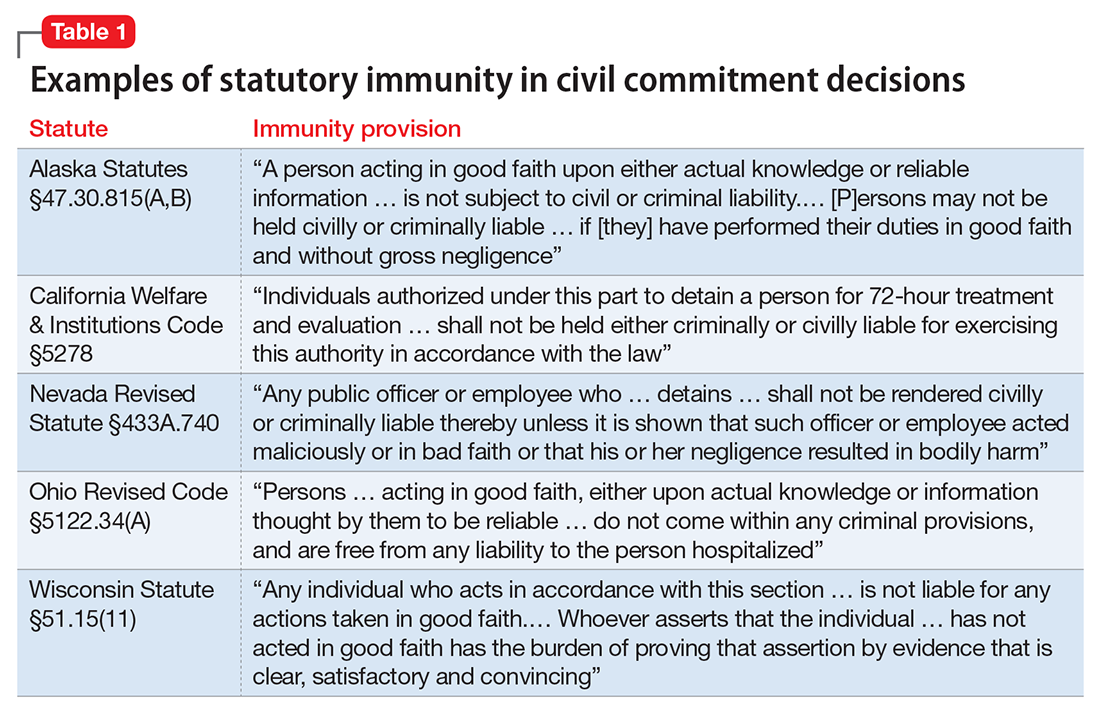
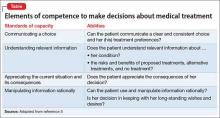
Further obligations come from medical licensing boards, which, in many states, have established time frames and specific procedures for informing patients and the public when a physician is leaving practice. Table 124,28-31 lists examples of these. If Dr. F works in a state where the board hasn’t promulgated such regulations, Table 124,28-31 may still help him think through how to discharge his ethical responsibilities to notify patients, colleagues, and business entities that he is ending his practice. References 28-30 and 32 discuss several of these matters, suggest timetables for various steps of a practice closure, and provide sample letters for notifying patients.
Physicians also must preserve their medical records for a certain period after they retire. States with rules on this matter require record preservation for 5 to 10 years or until 2 or 3 years after minor patients reach the age of majority.33 The Health Insurance Portability and Accountability Act of 1996 requires covered entities, which include most psychiatrists, to retain records for 6 years,34 and certain Medicare programs require retention for 10 years.35
Depending on Dr. F’s location and type of practice, his records should be preserved for the longest period that applies. If he is leaving a group practice that owns the records, arranging for this should be easy. If leaving an independent practice, he may need to ask another practice to perform this function.25
A ‘professional will’
Dr. F also might consider a measure that many psychotherapists recommend13,19,36 and that in some states is required by mental health licensing boards or professional codes37,38: creating a “professional will” that contains instructions for handling practice matters in case of death or disability.39
Dear Dr. Mossman,
I have a possibly fatal disease. So far, my symptoms and treatment haven’t kept me from my usual activities. But if my illness worsens, I’ll have to quit practicing psychiatry. What should I be doing now to make sure I fulfill my ethical and legal obligations to my patients?
Submitted by “Dr. F”
“Remember, with great power comes great responsibility.”
- Peter Parker, Spider-Man (2002)
Peter Parker’s movie-ending statement applies to doctors as well as Spider-Man. Although we don’t swing from building to building to save cities from heinous villains, practicing medicine is a privilege that society bestows only upon physicians who retain the knowledge, skills, and ability to treat patients competently.
Doctors retire from practice for many reasons, including when deteriorating physical health or cognitive capacity prevents them from performing clinical duties properly. Dr. F’s situation is not rare. As the physician population ages,1,2 a growing number of his colleagues will face similar circumstances,3,4 and with them, the responsibility and emotional turmoil of arranging to end their medical practices.
In many ways, concluding a psychiatric practice is similar to retiring from practice in other specialties. But because we care for patients’ minds as well as their bodies, retirement affects psychiatrists in distinctive ways that reflect our patients’ feelings toward us and our feelings toward them. To answer Dr. F’s question, this article considers having to stop practicing from 3 vantage points:
- the emotional impact on patients
- the emotional impact on the psychiatrist
- fulfilling one’s legal obligations while attending to the emotions of patients as well as oneself.
Emotional impact on patients
A content analysis study suggests that the traits patients appreciate in family physicians include the availability to listen, caring and compassion, trusted medical judgment, conveying the patient’s importance during encounters, feelings of connectedness, knowledge and understanding of the patient’s family, and relationship longevity.5 The same factors likely apply to relationships between psychiatrists and their patients, particularly if treatment encounters have extended over years and have involved conversations beyond those needed merely to write prescriptions.
Psychoanalytic publications offer many descriptions of patients’ reactions to the illness or death of their mental health professional. A 1978 study of 27 analysands whose physicians died during ongoing therapy reported reactions that ranged from a minimal impact to protracted mourning accompanied by helplessness, intense crying, and recurrent dreams about the analyst.6 Although a few patients were relieved that death had ended a difficult treatment, many were angry at their doctor for not attending to self-care and for breaking their treatment agreement, or because they had missed out on hoped-for benefits.
A 2010 study described the pain and distress that patients may experience following the death of their analyst or psychotherapist. These accounts emphasized the emotional isolation of grieving patients, who do not have the social support that bereaved persons receive after losing a loved one.7 Successful psychotherapy provides a special relationship characterized by trust, intimacy, and safety. But if the therapist suddenly dies, this relationship “is transformed into a solitude like no other.”8
Because the sudden “rupture of an analytic process is bound to be traumatic and may cause iatrogenic injury to the patient,” Traesdal9 advocates that therapists in situations similar to Dr. F’s discuss their possible death “on the reality level at least once during any analysis or psychotherapy.… It is extremely helpful to a patient to have discussed … how to handle the situation” if the therapist dies. This discussion also offers the patient an opportunity to confront a cultural taboo around death and to increase capacity to tolerate pain, illness, and aging.10,11
Most psychiatric care today is not psychoanalysis; psychiatrists provide other forms of care that create less intense doctor–patient relationships. Yet knowledge of these kinds of reactions may help Dr. F stay attuned to his patients’ concerns and to contemplate what they may experience, to greater or lesser degrees, if his health declines.
Retirement’s emotional impact on the psychiatrist
Published guidance on concluding a psychiatric practice is sparse, considering that all psychiatrists are mortal and stop practicing at some point.12Not thinking about or planning for retirement is a psychiatric tradition that started with Freud. He saw patients until shortly before his death and did not seem to have planned for ending his practice, despite suffering with jaw cancer for 16 years.13
Practicing medicine often is more than just a career; it is a core aspect of many physicians’ identity.14 Most of us spend a large fraction of our waking hours caring for patients and meeting other job requirements (eg, teaching, maintaining knowledge and skills), and many of us have scant time to pursue nonmedical interests. An intense prioritization of one’s “medical identity” makes retirement a blow to a doctor’s self-worth and sense of meaning in life.15,16
Because their work is not physically demanding, most psychiatrists continue to practice beyond the age of 65 years.12,17 More important, perhaps, is that being a psychiatrist is uniquely rewarding. As Benjamin Rush observed in an 1810 letter to Pennsylvania Hospital, successfully treating any medical disease is gratifying, but “what is this pleasure compared with that of restoring a fellow creature from the anguish and folly of madness and of reviving in him the knowledge of himself, his family, his friends, and his God!”18
Physicians in any specialty that involves repeated contact with the same patients form emotional bonds with their patients that retirement breaks.14 Psychiatrists’ interest in how patients think, feel, and cope with problems creates special attachments17 that can make some terminations “emotionally excruciating.”12
Psychiatrists with serious illness
What guidance might Dr. F find regarding whether to broach the subject of his illness with patients, and if so, how? No one has conducted controlled trials to answer these questions. Rather, published discussion of psychiatrists’ serious illness is found mainly in the psychotherapy literature. What’s available consists of individual accounts and case series that lack scientific rigor and offer little clarity about what the therapist should say, when to say it, and how to initiate the discussion.19,20 Yet Dr. F may find some of these authors’ ideas and suggestions helpful, particularly if his psychiatric practice includes providing psychotherapy.
As a rule, psychiatrists avoid talking about themselves, but having a serious illness that could affect treatment often justifies deviating from this practice. Although Dr. F (like many psychiatrists) may be concerned that discussing his health will make patients anxious or “contaminate” what they are able or willing to say,21 not providing information or avoiding discussion (especially if a patient asks about your health) may quickly undermine a patient’s trust.21,22 Even in psychoanalytic treatment, it makes little sense to encourage patients “to speak freely on the pretense that all is well, despite obvious evidence to the contrary.”19
Physicians often deny—or at least avoid thinking about—their own mortality.23 But avoiding talking about something so important (and often so obvious) as one’s illness may risk supporting patients’ denial of crucial matters in their own lives.19,21 Moreover, Dr. F’s inadvertent self-disclosure (eg, by displaying obvious signs of illness) may do more harm to therapy than a planned statement in which Dr. F has prepared what he’ll say to answer his patients’ questions.20
That Dr. F has continued working while suffering from a potentially fatal illness seems noble. Yet by doing so, he accepts not only the burdens of his illness but also the obligation to continue to serve his patients competently. This requires maintaining emotional steadiness and not using patients for emotional support, but instead obtaining and using the support of his friends, colleagues, family, consultants, and caregivers.20
Legal obligations
Retirement does not end a physician’s professional legal obligations.24 The legal rules and duties for psychiatrists who leave their practices are similar to those that apply to other physicians. Mishandling these aspects of retirement can result in various legal, licensure-related, or economic consequences, depending on your circumstances and employment arrangements.
Employment contracts in hospital or group practices often require notice of impending departures. If applicable to Dr. F’s situation, failure to comply with such conditions may lead to forfeiture of buyout payments, paying for malpractice tail coverage, or lawsuits claiming violation of contractual agreements.25
Retirement also creates practical and legal responsibilities to patients that are separate from the interpersonal and emotional issues previously discussed. How will those who need ongoing care and coverage be cared for? When withdrawing from a patient’s care (because of retirement or other reasons), a physician should give the patient enough advance notice to set up satisfactory treatment arrangements elsewhere and should facilitate transfer of the patient’s care, if appropriate.26 Failure to meet this ethical obligation may lead to a malpractice action alleging abandonment, which is defined as “the unilateral severance of the professional relationship … without reasonable notice at a time when there is still the necessity of continuing medical attention.”27
Further obligations come from medical licensing boards, which, in many states, have established time frames and specific procedures for informing patients and the public when a physician is leaving practice. Table 124,28-31 lists examples of these. If Dr. F works in a state where the board hasn’t promulgated such regulations, Table 124,28-31 may still help him think through how to discharge his ethical responsibilities to notify patients, colleagues, and business entities that he is ending his practice. References 28-30 and 32 discuss several of these matters, suggest timetables for various steps of a practice closure, and provide sample letters for notifying patients.
Physicians also must preserve their medical records for a certain period after they retire. States with rules on this matter require record preservation for 5 to 10 years or until 2 or 3 years after minor patients reach the age of majority.33 The Health Insurance Portability and Accountability Act of 1996 requires covered entities, which include most psychiatrists, to retain records for 6 years,34 and certain Medicare programs require retention for 10 years.35
Depending on Dr. F’s location and type of practice, his records should be preserved for the longest period that applies. If he is leaving a group practice that owns the records, arranging for this should be easy. If leaving an independent practice, he may need to ask another practice to perform this function.25
A ‘professional will’
Dr. F also might consider a measure that many psychotherapists recommend13,19,36 and that in some states is required by mental health licensing boards or professional codes37,38: creating a “professional will” that contains instructions for handling practice matters in case of death or disability.39
1. LoboPrabhu SM, Molinari VA, Hamilton JD, et al. The aging physician with cognitive impairment: approaches to oversight, prevention, and remediation. Am J Geriatr Psychiatry. 2009;17(6):445-454.
2. Dellinger EP, Pellegrini CA, Gallagher TH. The aging physician and the medical profession: a review. JAMA Surg. 2017;152(10):967-971.
3. Dall T, West T, Chakrabarti R, et al. The complexities of physician supply and demand: projections from 2014 to 2025. Association of American Medical Colleges. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published 2016. Accessed September 26, 2017.
4. Draper B, Winfield S, Luscombe G. The older psychiatrist and retirement. Int J Geriatr Psychiatry. 1997;12(2):233-239.
5. Merenstein B, Merenstein J. Patient reflections: saying good-bye to a retiring family doctor. J Am Board Fam Med. 2008;21(5):461-465.
6. Lord R, Ritvo S, Solnit AJ. Patients’ reactions to the death of the psychoanalyst. Intern J Psychoanal. 1978;59(2-3):189-197.
7. Power A. Forced endings in psychotherapy and psychoanalysis: attachment and loss in retirement. New York, NY: Routledge; 2016.
8. Robutti A. When the patient loses his/her analyst. Italian Psychoanalytic Annual. 2010;4:129-145.
9. Traesdal T. When the analyst dies: dealing with the aftermath. J Am Psychoanal Assoc. 2005;53(4):1235-1255.
10. Deutsch RA. A voice lost, a voice found: after the death of the analyst. In: Deutsch RA, ed. Traumatic ruptures: abandonment and betrayal in the analytic relationship. New York, NY: Routledge; 2014:32-45.
11. Ward VP. On Yoda, trouble, and transformation: the cultural context of therapy and supervision. Contemp Fam Ther. 2009;31(3):171-176.
12. Moffic HS. Mental bootcamp: today is the first day of your retirement! Psychiatr Times. http://www.psychiatrictimes.com/blogs/couch-crisis/mental-bootcamp-today-first-day-your-retirement. Published June 25, 2012. Accessed October 31, 2017.
13. Shatsky P. Everything ends: identity and the therapist’s retirement. Clin Soc Work J. 2016;44(2):143-149.
14. Collier R.
15. Onyura B, Bohnen J, Wasylenki D, et al. Reimagining the self at late-career transitions: how identity threat influences academic physicians’ retirement considerations. Acad Med. 2015;90(6):794-801.
16. Silver MP. Critical reflection on physician retirement. Can Fam Physician. 2016;62(10):783-784.
17. Clemens NA. A psychiatrist retires: an oxymoron? J Psychiatr Pract. 2011;17(5):351-354.
18. Packard FR. The earliest hospitals. In: Packard FR. History of medicine in the United States. Philadelphia, PA: Lippincott; 1901:348.
19. Galatzer-Levy RM. The death of the analyst: patients whose previous analyst died while they were in treatment. J Amer Psychoanalytic Assoc. 2004;52(4):999-1024.
20. Fajardo B. Life-threatening illness in the analyst. J Am Psychoanal Assoc. 2001;49(2):569-586.
21. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
22. Howe E. Should psychiatrists self disclose? Innov Clin Neurosci. 2011;8(12):14-17.
23. Rizq R, Voller D. ‘Who is the third who walks always beside you?’ On the death of a psychoanalyst. Psychodyn Pract. 2013;19(2):143-167.
24. Babitsky S, Mangraviti JJ. The biggest legal mistakes physicians make—and how to avoid them. Falmouth, MA: SEAK, Inc.; 2005.
25. Armon BD, Bayus K. Legal considerations when making a practice change. Chest. 2014;146(1):215-219.
26. American Medical Association. Opinions on patient-physician relationships: 1.1.5 terminating a patient-physician relationship. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethics-chapter-1.pdf. Published 2016. Accessed September 29, 2017.
27. Lee v Dewbre, 362 S.W. 2d 900 (Tex Civ App 7th Dist 1962).
28. Medical Association of Georgia. Issues for the retiring physician. https://www.mag.org/georgia/uploadedfiles/issues-retiring-physicians.pdf. Accessed October 1, 2017.
29. Massachusetts Medical Society. Issues for the retiring physician. http://www.massmed.org/physicians/practice-management/practice-ownership-and-operations/issues-for-the-retiring-physician-(pdf). Published 2012. Accessed October 1, 2017.
30. North Carolina Medical Board. The doctor is out: a physician’s guide to closing a practice. https://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 1, 2017.
31. 243 Code of Mass. Regulations §2.06(4)(a).
32. Sampson K. Physician’s guide to closing a practice. Maine Medical Association. https://www.mainemed.com/sites/default/files/content/Closing%20Practice%20Guide%20FINAL%206.2014.pdf. Published 2014. Accessed October 1, 2017.
33. HealthIT.gov. State medical record laws: minimum medical record retention periods for records held by medical doctors and hospitals. https://www.healthit.gov/sites/default/files/appa7-1.pdf. Accessed September 29, 2017.
34. 45 CFR §164.316(b)(2).
35. 42 CFR §422.504(d)(2)(iii).
36. Pope KS, Vasquez MJT. How to survive and thrive as a therapist: information, ideas, and resources for psychologists in practice. Washington, DC: American Psychological Association; 2005.
37. Becher EH, Ogasawara T, Harris SM. Death of a clinician: the personal, practical and clinical implications of therapist mortality. Contemp Fam Ther. 2012;34(3):313-321.
38. Hovey JK. Mortality practices: how clinical social workers interact with their mortality within their clinical and professional practice. Theses, Dissertations, and Projects.Paper 1081. http://scholarworks.smith.edu/cgi/viewcontent.cgi?article=2158&context=theses. Published 2014. Accessed October 1, 2017.
39. Frankel AS, Alban A. Professional wills: protecting patients, family members and colleagues. The Steve Frankel Group. https://www.sfrankelgroup.com/professional-wills.html. Accessed October 31, 2017.
1. LoboPrabhu SM, Molinari VA, Hamilton JD, et al. The aging physician with cognitive impairment: approaches to oversight, prevention, and remediation. Am J Geriatr Psychiatry. 2009;17(6):445-454.
2. Dellinger EP, Pellegrini CA, Gallagher TH. The aging physician and the medical profession: a review. JAMA Surg. 2017;152(10):967-971.
3. Dall T, West T, Chakrabarti R, et al. The complexities of physician supply and demand: projections from 2014 to 2025. Association of American Medical Colleges. https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf. Published 2016. Accessed September 26, 2017.
4. Draper B, Winfield S, Luscombe G. The older psychiatrist and retirement. Int J Geriatr Psychiatry. 1997;12(2):233-239.
5. Merenstein B, Merenstein J. Patient reflections: saying good-bye to a retiring family doctor. J Am Board Fam Med. 2008;21(5):461-465.
6. Lord R, Ritvo S, Solnit AJ. Patients’ reactions to the death of the psychoanalyst. Intern J Psychoanal. 1978;59(2-3):189-197.
7. Power A. Forced endings in psychotherapy and psychoanalysis: attachment and loss in retirement. New York, NY: Routledge; 2016.
8. Robutti A. When the patient loses his/her analyst. Italian Psychoanalytic Annual. 2010;4:129-145.
9. Traesdal T. When the analyst dies: dealing with the aftermath. J Am Psychoanal Assoc. 2005;53(4):1235-1255.
10. Deutsch RA. A voice lost, a voice found: after the death of the analyst. In: Deutsch RA, ed. Traumatic ruptures: abandonment and betrayal in the analytic relationship. New York, NY: Routledge; 2014:32-45.
11. Ward VP. On Yoda, trouble, and transformation: the cultural context of therapy and supervision. Contemp Fam Ther. 2009;31(3):171-176.
12. Moffic HS. Mental bootcamp: today is the first day of your retirement! Psychiatr Times. http://www.psychiatrictimes.com/blogs/couch-crisis/mental-bootcamp-today-first-day-your-retirement. Published June 25, 2012. Accessed October 31, 2017.
13. Shatsky P. Everything ends: identity and the therapist’s retirement. Clin Soc Work J. 2016;44(2):143-149.
14. Collier R.
15. Onyura B, Bohnen J, Wasylenki D, et al. Reimagining the self at late-career transitions: how identity threat influences academic physicians’ retirement considerations. Acad Med. 2015;90(6):794-801.
16. Silver MP. Critical reflection on physician retirement. Can Fam Physician. 2016;62(10):783-784.
17. Clemens NA. A psychiatrist retires: an oxymoron? J Psychiatr Pract. 2011;17(5):351-354.
18. Packard FR. The earliest hospitals. In: Packard FR. History of medicine in the United States. Philadelphia, PA: Lippincott; 1901:348.
19. Galatzer-Levy RM. The death of the analyst: patients whose previous analyst died while they were in treatment. J Amer Psychoanalytic Assoc. 2004;52(4):999-1024.
20. Fajardo B. Life-threatening illness in the analyst. J Am Psychoanal Assoc. 2001;49(2):569-586.
21. Dewald PA. Serious illness in the analyst: transference, countertransference, and reality responses. J Am Psychoanal Assoc. 1982;30(2):347-363.
22. Howe E. Should psychiatrists self disclose? Innov Clin Neurosci. 2011;8(12):14-17.
23. Rizq R, Voller D. ‘Who is the third who walks always beside you?’ On the death of a psychoanalyst. Psychodyn Pract. 2013;19(2):143-167.
24. Babitsky S, Mangraviti JJ. The biggest legal mistakes physicians make—and how to avoid them. Falmouth, MA: SEAK, Inc.; 2005.
25. Armon BD, Bayus K. Legal considerations when making a practice change. Chest. 2014;146(1):215-219.
26. American Medical Association. Opinions on patient-physician relationships: 1.1.5 terminating a patient-physician relationship. https://www.ama-assn.org/sites/default/files/media-browser/code-of-medical-ethics-chapter-1.pdf. Published 2016. Accessed September 29, 2017.
27. Lee v Dewbre, 362 S.W. 2d 900 (Tex Civ App 7th Dist 1962).
28. Medical Association of Georgia. Issues for the retiring physician. https://www.mag.org/georgia/uploadedfiles/issues-retiring-physicians.pdf. Accessed October 1, 2017.
29. Massachusetts Medical Society. Issues for the retiring physician. http://www.massmed.org/physicians/practice-management/practice-ownership-and-operations/issues-for-the-retiring-physician-(pdf). Published 2012. Accessed October 1, 2017.
30. North Carolina Medical Board. The doctor is out: a physician’s guide to closing a practice. https://www.ncmedboard.org/images/uploads/article_images/Physicians_Guide_to_Closing_a_Practice_05_12_2014.pdf. Published May 12, 2014. Accessed October 1, 2017.
31. 243 Code of Mass. Regulations §2.06(4)(a).
32. Sampson K. Physician’s guide to closing a practice. Maine Medical Association. https://www.mainemed.com/sites/default/files/content/Closing%20Practice%20Guide%20FINAL%206.2014.pdf. Published 2014. Accessed October 1, 2017.
33. HealthIT.gov. State medical record laws: minimum medical record retention periods for records held by medical doctors and hospitals. https://www.healthit.gov/sites/default/files/appa7-1.pdf. Accessed September 29, 2017.
34. 45 CFR §164.316(b)(2).
35. 42 CFR §422.504(d)(2)(iii).
36. Pope KS, Vasquez MJT. How to survive and thrive as a therapist: information, ideas, and resources for psychologists in practice. Washington, DC: American Psychological Association; 2005.
37. Becher EH, Ogasawara T, Harris SM. Death of a clinician: the personal, practical and clinical implications of therapist mortality. Contemp Fam Ther. 2012;34(3):313-321.
38. Hovey JK. Mortality practices: how clinical social workers interact with their mortality within their clinical and professional practice. Theses, Dissertations, and Projects.Paper 1081. http://scholarworks.smith.edu/cgi/viewcontent.cgi?article=2158&context=theses. Published 2014. Accessed October 1, 2017.
39. Frankel AS, Alban A. Professional wills: protecting patients, family members and colleagues. The Steve Frankel Group. https://www.sfrankelgroup.com/professional-wills.html. Accessed October 31, 2017.
Considering work as an expert witness? Look before you leap!
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
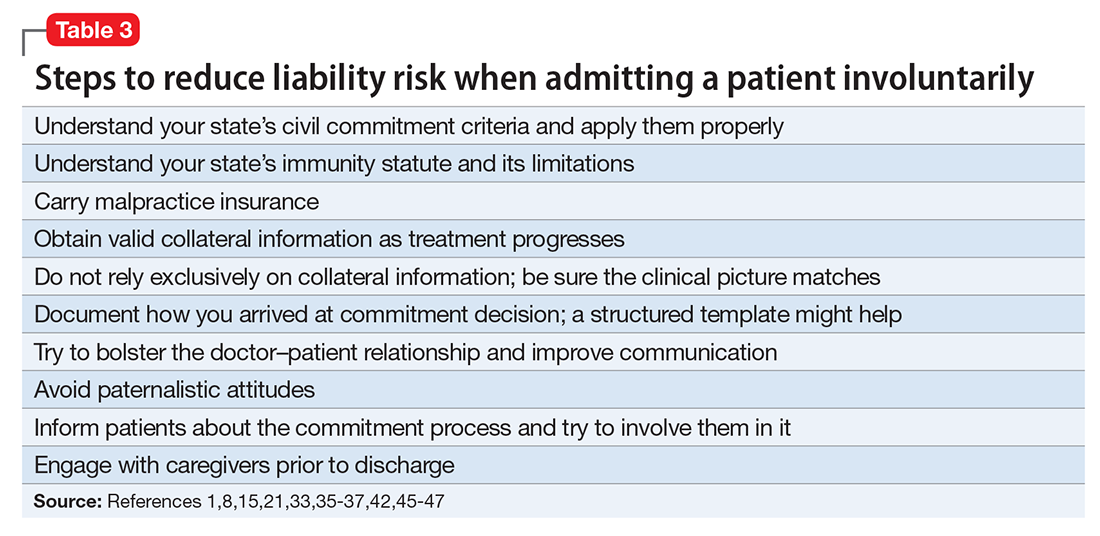
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
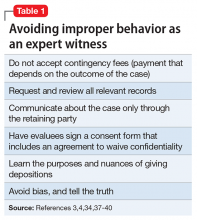
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
Other liability
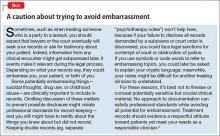
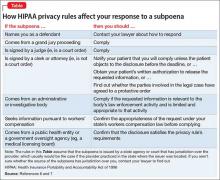
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
Dear Dr. Mossman,
I am retired, but an attorney friend of mine has asked me to help out by performing forensic evaluations. I’m tempted to try it because the work sounds meaningful and interesting. I won’t have a doctor–patient relationship with the attorney’s clients, and I expect the work will take <10 hours a week. Do I need malpractice coverage? Should I consider any other medicolegal issues before I start?
Submitted by “Dr. B”
One of the great things about being a psychiatrist is the variety of available practice options. Like Dr. B, many psychiatrists contemplate using their clinical know-how to perform forensic evaluations. For some psychiatrists, part-time work as an expert witness may provide an appealing change of pace from their other clinical duties1 and a way to supplement their income.2
But as would be true for other kinds of medical practice, Dr. B is wise to consider the possible risks before jumping into forensic work. To help Dr. B decide about getting insurance coverage, we will:
- explain briefly the subspecialty of forensic psychiatry
- review the theory of malpractice and negligence torts
- discuss whether forensic evaluations can create doctor–patient relationships
- explore the availability and limitations of immunity for forensic work
- describe other types of liability with forensic work
- summarize steps to avoid liability.
Introduction to forensic psychiatry
Some psychiatrists—and many people who are not psychiatrists—have a vague or incorrect understanding of forensic psychiatry. Put succinctly, “Forensic Psychiatry is a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts….”3 To practice forensic psychiatry well, a psychiatrist must have some understanding of the law and how to apply and translate clinical concepts to fit legal criteria.4 Psychiatrists who offer to serve as expert witnesses should be familiar with how the courtroom functions, the nuances of how expert testimony is used, and possible sources of bias.4,5
Forensic work can create role conflicts. For most types of forensic assessments, psychiatrists should not provide forensic opinions or testimony about their own patients.3 Even psychiatrists who only work as expert witnesses must balance duties of assisting the trier of fact, fulfilling the consultation role to the retaining party, upholding the standards and ethics of the profession, and striving to provide truthful, objective testimony.2
Special training usually is required
The most important qualification for being a good psychiatric expert witness is being a good psychiatrist, and courts do not require psychiatrists to have specialty training in forensic psychiatry to perform forensic psychiatric evaluations. Yet, the field of forensic psychiatry has developed over the past 50 years to the point that psychiatrists need special training to properly perform many, if not most, types of forensic evaluations.6 Much of forensic psychiatry involves writing specialized reports for lawyers and the court,7 and experts are supposed to meet professional standards, regardless of their training.8-10 Psychiatrists who perform forensic work are obligated to claim expertise only in areas where their knowledge, skills, training, and experience justify such claims. These considerations explain why, since 1999, the American Board of Psychiatry and Neurology has limited eligibility for board certification in forensic psychiatry to psychiatrists who have completed accredited forensic fellowships.11
Malpractice: A short review
To address Dr. B’s question about malpractice coverage, we first review what malpractice is.
“Tort” is a legal term for injury, and tort claims arise when one party harms another and the harmed party seeks money as compensation.9 In a tort claim alleging negligence, the plaintiff (ie, the person bringing the suit) asserts that the defendant had a legally recognized duty, that the defendant breached that duty, and that breach of duty harmed the plaintiff.8
Physicians have a legal duty to “possess the requisite knowledge and skill such as is possessed by the average member of the medical profession; … exercise ordinary and reasonable care in the application of such knowledge and skill; and … use best judgment in such application.”10 A medical malpractice lawsuit asserts that a doctor breached this duty and caused injury in the course of the medical practice.
Malpractice in forensic cases
Practicing medicine typically occurs within the context of treatment relationships. One might think, as Dr. B did, that because forensic evaluations do not involve treating patients, they do not create the kind of doctor–patient relationship that could lead to malpractice liability. This is incorrect, however, for several reasons.
Certain well-intended actions during a forensic evaluation, such as explaining the implications of a diagnosis, giving specific advice about a medication, or making a recommendation about where or how to obtain treatment, may create a doctor–patient relationship.12,13 Many states’ laws on what constitutes the practice of medicine include performing examinations, diagnosing, or referring to oneself as “Dr.” or as a medical practitioner.14-17 State courts have interpreted these laws to further define what constitutes medical practice and the creation of a doctor–patient relationship during a forensic examination.18,19 Some legal scholars20 and the American Medical Association (AMA)9 regard provision of expert testimony as practicing medicine because such testimony requires the application of medical science and rendering of diagnoses.
Immunity and shifts away from it
For many years, courts granted civil immunity to expert witnesses for several policy reasons.8,9,13,20-22 Courts recognized that losing parties might want to blame whomever they could, and immunity could provide legal protection for expert witnesses. Without such protection, witnesses might feel more pressured to give testimony favorable to their side at the loss of objectivity,23,24 or experts might be discouraged from testifying at all. This would be true especially for academic psychiatrists who testify infrequently or for retired doctors, such as Dr. B, who might not want to carry insurance for just one case.21 According to this argument, rather than using the threat of litigation to keep out improper testimony, courts should rely on both admissibility standards25,26 and the adversarial nature of proceedings.21
Those who oppose granting immunity to experts argue that admissibility rules and cross-examination do too little to prevent bad testimony; the threat of liability, however, motivates experts to be more cautious and scientifically rigorous in their approach.21 Opponents also have argued that the threat of liability might reduce improper testimony, which they believe was partly responsible for rising malpractice premiums.20
Courts vary in how they consider granting immunity and to what extent. For example:
- Some courts will not grant immunity to so-called “friendly experts,” while others have limited immunity for adversarial experts.20-22
- Some courts have applied immunity to general fact witnesses but not to professional experts.21,24,27
- When immunity is considered, it is usually regarding actual testimony. Yet, some courts have included pretrial services.21,28-30
- Some courts have considered the testimonial issue at hand when deciding whether to extend immunity. For example, immunity may not apply if the issue is loss of profits21,31 or if an experiment is conducted to demonstrate the extent of a physical injury.21,32
If you plan to serve as an expert witness, find out what, if any, immunity is available in the jurisdiction where you expect to testify. If you do not have immunity, you may be subject to various malpractice claims, including alleged physical or emotional harm resulting from the evaluation1 (perhaps caused by misuse of empathic statements33), an accusation of negligent misdiagnosis of an evaluee,8 or failing to act upon a duty to warn or protect that arises during an assessment.34
Other liability
Dr. B also asked about medicolegal issues other than malpractice. Although negligence is the claim that forensic psychiatrists most commonly encounter,10 other types of claims arise in practice-related legal actions. Potential causes of action include failure to obtain or attempt to obtain informed consent, breach of confidentiality, or not responding to a psychiatric emergency during evaluation. The plaintiff usually must show that the expert’s conduct was the cause-in-fact of injury.8
Besides civil lawsuits, forensic work may generate complaints to state medical boards.10 Occasionally, state medical boards have revoked psychiatrists’ licenses for improper testimony.20 Aggrieved parties may allege violations of the Health Insurance Portability and Accountability Act of 1996, such as mishandling protected health information. Psychiatrists also may face sanction by professional societies—for example, censure by the American Psychiatric Association9,10 or the AMA13 for ethics violations—if their improper testimony is considered unprofessional conduct. The theory behind this is that judges and jurors cannot be technical experts in every field, so the field must have a mechanism to police itself.20,35,36 Finally, forensic experts can face criminal charges for perjury if they lie under oath.8
How to protect yourself
Even when legal claims against psychiatrists turn out to be baseless, legal costs of defending oneself can mount quickly. Knowing this, Dr. B may conclude that obtaining malpractice insurance would be wise. But a malpractice policy alone may not meet all Dr. B’s needs, because some policies do not cover ordinary negligence or other potential causes of legal action against a psychiatrist.13 Some companies offer these extra types of coverage for work as an expert witness at no additional cost, and some offer access to risk management services with specialized knowledge about forensic psychiatric practice.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
1. Appelbaum PS. Law and psychiatry: liability for forensic evaluations: a word of caution. Psychiatr Serv. 2001;52(7):885-886.
2. Shuman DW, Greenberg SA. The expert witness, the adversary system, and the voice of reason: reconciling impartiality and advocacy. Professional Psychology: Research and Practice. 2003;34(3):219-224.
3. American Academy of Psychiatry and the Law. Ethics guidelines for the practice of forensic psychiatry. http://www.aapl.org/ethics.htm. Published May 2005. Accessed July 11, 2017.
4. Gutheil TG. Forensic psychiatry as a specialty. Psychiatric Times. http://www.psychiatrictimes.com/articles/forensic-psychiatry-sp
5. Knoll J, Gerbasi J. Psychiatric malpractice case analysis: striving for objectivity. J Am Acad Psychiatry Law. 2006;34(2):215-223.
6. Sadoff RL. The practice of forensic psychiatry: perils, problems, and pitfalls. J Am Acad Psychiatry Law. 1998;26(2):305-314.
7. Simon RI. Authorship in forensic psychiatry: a perspective. J Am Acad Psychiatry Law. 2007;35(1):18-26.
8. Masterson LR. Witness immunity or malpractice liability for professionals hired as experts? Rev Litig. 1998;17(2):393-418.
9. Binder RL. Liability for the psychiatrist expert witness. Am J Psychiatry. 2002;159(11):1819-1825.
10. Gold LH, Davidson JE. Do you understand your risk? Liability and third-party evaluations in civil litigation. J Am Acad Psychiatry Law. 2007;35(2):200-210.
11. American Academy of Psychiatry and the Law. ABPN certification in the subspecialty of forensic psychiatry. http://www.aapl.org/abpn-certification. Accessed July 9, 2017.
12. Marett CP, Mossman D. What are your responsibilities after a screening call? Current Psychiatry. 2014;13(9):54-57.
13. Weinstock R, Garrick T. Is liability possible for forensic psychiatrists? Bull Am Acad Psychiatry Law. 1995;23(2):183-193.
14. Ohio Revised Code §4731.34.
15. Kentucky Revised Statutes §311.550(10) (2017).
16. California Business & Professions Code §2052.5 (through 2012 Leg Sess).
17. Oregon Revised Statutes §677.085 (2013).
18. Blake V. When is a patient-physician relationship established? Virtual Mentor. 2012;14(5):403-406.
19. Zettler PJ. Toward coherent federal oversight of medicine. San Diego Law Review. 2015;52:427-500.
20. Turner JA. Going after the ‘hired guns’: is improper expert witness testimony unprofessional conduct or the negligent practice of medicine? Spec Law Dig Health Care Law. 2006;328:9-43.
21. Weiss LS, Orrick H. Expert witness malpractice actions: emerging trend or aberration? Practical Litigator. 2004;15(2):27-38.
22. McAbee GN. Improper expert medical testimony. Existing and proposed mechanisms of oversight. J Leg Med. 1998;19(2):257-272.
23. Panitz v Behrend, 632 A 2d 562 (Pa Super Ct 1993).
24. Murphy v A.A. Mathews, 841 S.W. 2d 671 (Mo 1992).
25. Daubert v Merrell Dow Pharmaceuticals, 509 U.S. 579 (1993).
26. Rule 702. Testimony by expert witnesses. In: Michigan Legal Publishing Ltd. Federal Rules of evidence. Grand Rapids, MI: Michigan Legal Publishing Ltd; 2017:21.
27. Committee on Medical Liability and Risk Management. Policy statement—expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
28. Mattco Forge, Inc., v Arthur Young & Co., 6 Cal Rptr 2d 781 (Cal Ct App 1992).
29. Marrogi v Howard, 248 F 3d 382 (5th Cir 2001).
30. Boyes-Bogie v Horvitz, 2001 WL 1771989 (Mass Super 2001).
31. LLMD of Michigan, Inc., v Jackson-Cross Co., 740 A. 2d 186 (Pa 1999).
32. Pollock v Panjabi, 781 A 2d 518 (Conn Super Ct 2000).
33. Brodsky SL, Wilson JK. Empathy in forensic evaluations: a systematic reconsideration. Behav Sci Law. 2013;31(2):192-202.
34. Heilbrun K, DeMatteo D, Marczyk G, et al. Standards of practice and care in forensic mental health assessment: legal, professional, and principles-based consideration. Psych Pub Pol L. 2008;14(1):1-26.
35. Appelbaum PS. Law & psychiatry: policing expert testimony: the role of professional organizations. Psychiatr Serv. 2002;53(4):389-390,399.
36. Austin v American Association of Neurological Surgeons, 253 F 3d 967 (7th Cir 2001).
37. Gutheil TG, Simon RI. Attorneys’ pressures on the expert witness: early warning signs of endangered honesty, objectivity, and fair compensation. J Am Acad Psychiatry Law. 1999;27(4):546-553; discussion 554-562.
38. Gold LH, Anfang SA, Drukteinis AM, et al. AAPL practice guideline for the forensic evaluation of psychiatric disability. J Am Acad Psychiatry Law. 2008;36(suppl 4):S3-S50.
39. Knoll JL IV, Resnick PJ. Deposition dos and don’ts: how to answer 8 tricky questions. Current Psychiatry. 2008;7(3):25-28,36,39-40.
40. Hoge MA, Tebes JK, Davidson L, et al. The roles of behavioral health professionals in class action litigation. J Am Acad Psychiatry Law. 2002;30(1):49-58; discussion 59-64.
41. Simon RI, Shuman DW. Conducting forensic examinations on the road: are you practicing your profession without a license? Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2001;29(1):75-82.
42. Reid WH. Licensure requirements for out-of-state forensic examinations. J Am Acad Psychiatry Law. 2000;28(4):433-437.
43. Collins B, ed. When in doubt, tell the truth: and other quotations from Mark Twain. New York, NY: Columbia University Press; 1997.
‘3 Strikes ‘n’ yer out’: Dismissing no-show patients
Dear Dr. Mossman,
The clinic where I work initiated a “3 misses and out” policy: If a patient doesn’t show for 3 appointments in a 12-month period, the clinic removes him from the patient rolls. I’ve heard such policies are common, but I worry: Is this abandonment?
Submitted by “Dr. C”
The short answer to Dr. C’s question is, “Handled properly, it’s not abandonment.” But if this response really was satisfactory, Dr. C probably would not have asked the question. Dealing with no-show patients has bothered psychiatrists, other mental health professionals, and other physicians for decades.1
Clinicians worry when patients miss important follow-up, and unreimbursed office time won’t help pay a clinician’s salary or office expenses.2 But a policy such as the one Dr. C describes may not be the best response—clinically or financially—for many patients who miss appointments repeatedly.
If no-show patients worry you or cause problems where you practice, read on as I cover:
- charging for missed appointments
- why patients miss appointments
- evidence-based methods to improve show-up rates
- when ending a treatment relationship unilaterally is not abandonment
- how to dismiss no-show patients from a practice properly.
Before the mid-1980s, most office-based psychiatrists worked in solo or small group and required patients to pay cash for treatment; approximately 40% of psychiatrists still practice this way.3 Often, private practice clinicians require payment for appointments missed without 24 hours’ notice. This well-accepted practice2,4,5 reinforces the notion that psychotherapy involves making a commitment to work on problems. It also protects clinicians’ financial interests and mitigates possible resentment that might arise if office time committed to a patient went unreimbursed.6 Clinicians who charge for missed appointments should inform patients of this at the beginning of treatment, explaining clearly that the patient—not the insurer—will be paying for unused treatment time.2,4
Since the 1980s, outpatient psychiatrists have increasingly worked in public agencies or other organizational practice settings7 where patients—whose care is funded by public monies or third-party payors—cannot afford to pay for missed appointments. If you work in a clinic such as the one where Dr. C provides services, you probably are paid an hourly wage whether your patients show up or not. To pay you and remain solvent, your clinic must find ways other than charging patients to address and reduce no-shows.
The literature abounds with research on why no-shows occur. But no-shows seem to be more common in psychiatry than in other medical specialties.8 The frequency of no-shows varies considerably, but it’s a big problem in some mental health treatment contexts, with reported rates ranging from 12% to 60%.9 A recent, comprehensive review reported that approximately 30% of patients refuse, drop out, or prematurely disengage from services after first-episode psychosis.10 No-shows and drop outs are linked to clinical deterioration11 and heightened risk of hospitalization.12
Jaeschke et al15 suggests that no-shows, dropping out of treatment, and other forms of what doctors call “noncompliance” or “nonadherence” might be better conceptualized as a lack of “concordance,” “mutuality,” or “shared ideology” about what ails patients and the role of their physicians. For this reason, striving for a “partnership between a physician and a patient,” with the patient “fully engaged in the two-way communication with a doctor … seems to be a much more suitable way of achieving therapeutic progress in the discipline of psychiatry.”15
Reducing no-shows: Evidence-based methods
Many medical and mental health articles describe evidence-based methods for lowering no-show rates. Studies document the value of assertive outreach, home visits, avoiding scheduling on religious holidays, scheduling appointments in the afternoon rather than the morning, providing assistance with transportation,8 sending reminder letters,16 or making telephone calls.17 Growing evidence suggests that text messages reduce missed appointments, even among patients with severe disorders (eg, schizophrenia) that compromise cognitive functioning.18
The measures I’ve described won’t prevent every patient from no-showing repeatedly. If you or your employer have tried some of these proven methods and they haven’t reduced a patient’s persistent no-shows, and if it makes sense from a clinical and financial standpoint, then it’s all right to dismiss the patient.
To understand why you are permitted to dismiss a patient from your practice, it helps to understand how the law views the doctor–patient relationship. A doctor has no legal duty to treat anyone—even someone who desperately needs care—unless the doctor has taken some action to establish a treatment relationship with that person. Having previously treated the patient establishes a treatment relationship, as could other actions such as giving specific advice or (in some cases) making an appointment for a person. Once you have a treatment relationship with someone, you usually must continue to provide necessary medical attention until either the treatment episode has concluded or you and the patient agree to end treatment.20
For many chronic mental illnesses, a treatment episode could last years. But this does not force you to continue caring for a patient indefinitely if your circumstances change or if the patient’s behavior causes you to want to withdraw from providing care.
To ethically end care of a patient while a treatment episode is ongoing, you must either transfer care to another competent physician, or give your patient adequate notice and opportunity to obtain appropriate treatment elsewhere.20 If you fail to do either, however, you are guilty of “abandonment” and potentially subject to discipline by state licensing authorities21 or, if harm results, a malpractice lawsuit.22
In many states, statutes or regulations describe what you must do to end a treatment relationship properly. Ohio’s rule is typical: You must send the patient a certified letter explaining that the treatment relationship is ending, that you will remain available to provide care for 30 days, and that you will send treatment records to another provider upon receiving the patient’s signed authorization.21
One note of caution, however: If you practice in hospitals or groups, or if you or the agency where you work has signed provider contracts, you may have agreed to terms of practice that make dismissing a patient more complicated.23 Whether you practice individually or in a large organization, it’s usually wise to get advice from an attorney and/or your malpractice carrier to make sure you’re handling a patient dismissal the right way.
1. Adler LM, Yamamoto J, Goin M. Failed psychiatric clinic appointments. Relationship to social class. Calif Med. 1963;99:388-392.
2. Buppert C. How to deal with missed appointments. Dermatol Nurs 2009;21(4):207-208.
3. National Council Medical Director Institute. The psychiatric shortage: causes and solutions. https://www.thenationalcouncil.org/wp-content/uploads/2017/03/Psychiatric-Shortage_National-Council-.pdf. Published March 28, 2017. Accessed April 6, 2017.
4. Legal & Regulatory Affairs staff. Practitioner pointer: how to handle late and missed appointments. http://www.apapracticecentral.org/update/2014/11-06/late-missed-appoitments.aspx. Published November 6, 2004. Accessed April 7, 2017.
5. Centers for Medicare & Medicaid Services. MLN Matters Number: MM5613. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM5613.pdf. Updated November 12, 2014. Accessed April 7, 2017.
6. MacCutcheon M. Why I charge for late cancellations and no-shows to therapy. http://www.goodtherapy.org/blog/why-i-charge-for-late-cancellations-no-shows-to-therapy-0921164. Published September 21, 2016. Accessed April 6, 2017.
7. Kalman TP, Goldstein MA. Satisfaction of Manhattan psychiatrists with private practice: assessing the impact of managed care. http://www.medscape.com/viewarticle/430759_4. Accessed April 6, 2017.
8. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat. 2007;13(6):423-434.
9. Long J, Sakauye K, Chisty K, et al. The empty chair appointment. SAGE Open. 2016;6:1-5.
10. Doyle R, Turner N, Fanning F, et al. First-episode psychosis and disengagement from treatment: a systematic review. Psychiatr Serv. 2014;65(5):603-611.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51(7):885-889.
12. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. Br J Psychiatry. 2000;176:160-165.
13. Williamson AE, Ellis DA, Wilson P, et al. Understanding repeated non-attendance in health services: a pilot analysis of administrative data and full study protocol for a national retrospective cohort. BMJ Open. 2017;7(2):e014120. doi: 10.1136/bmjopen-2016-014120.
14. Binnie J, Boden Z. Non-attendance at psychological therapy appointments. Mental Health Rev J. 2016;21(3):231-248.
15. Jaeschke R, Siwek M, Dudek D. Various ways of understanding compliance: a psychiatrist’s view. Arch Psychiatr Psychother. 2011;13(3):49-55.
16. Boland B, Burnett F. Optimising outpatient efficiency – development of an innovative ‘Did Not Attend’ management approach. Int J Psychiatry Clin Pract. 2014;18(3):217-219.
17. Pennington D, Hodgson J. Non‐attendance and invitation methods within a CBT service. Mental Health Rev J. 2012;17(3):145-151.
18. Sims H, Sanghara H, Hayes D, et al. Text message reminders of appointments: a pilot intervention at four community mental health clinics in London. Psychiatr Serv. 2012;63(2):161-168.
19. Oldham M, Kellett S, Miles E, et al. Interventions to increase attendance at psychotherapy: a meta-analysis of randomized controlled trials. J Consult Clin Psychol. 2012;80(5):928-939.
20. Gore AG, Grossman EL, Martin L, et al. Physicians, surgeons, and other healers. In: American Jurisprudence. 2nd ed, §130. Eagan, MN: West Publishing; 2017:61.
21. Ohio Administrative Code §4731-27-02.
22. Lowery v Miller, 157 Wis 2d 503, 460 N.W. 2d 446 (Wis App 1990).
23. Brockway LH. Terminating patient relationships: how to dismiss without abandoning. TMLT. https://www.tmlt.org/tmlt/tmlt-resources/newscenter/blog/2009/Terminating-patient-relationships.html. Published June 19, 2009. Accessed April 3, 2017.
Dear Dr. Mossman,
The clinic where I work initiated a “3 misses and out” policy: If a patient doesn’t show for 3 appointments in a 12-month period, the clinic removes him from the patient rolls. I’ve heard such policies are common, but I worry: Is this abandonment?
Submitted by “Dr. C”
The short answer to Dr. C’s question is, “Handled properly, it’s not abandonment.” But if this response really was satisfactory, Dr. C probably would not have asked the question. Dealing with no-show patients has bothered psychiatrists, other mental health professionals, and other physicians for decades.1
Clinicians worry when patients miss important follow-up, and unreimbursed office time won’t help pay a clinician’s salary or office expenses.2 But a policy such as the one Dr. C describes may not be the best response—clinically or financially—for many patients who miss appointments repeatedly.
If no-show patients worry you or cause problems where you practice, read on as I cover:
- charging for missed appointments
- why patients miss appointments
- evidence-based methods to improve show-up rates
- when ending a treatment relationship unilaterally is not abandonment
- how to dismiss no-show patients from a practice properly.
Before the mid-1980s, most office-based psychiatrists worked in solo or small group and required patients to pay cash for treatment; approximately 40% of psychiatrists still practice this way.3 Often, private practice clinicians require payment for appointments missed without 24 hours’ notice. This well-accepted practice2,4,5 reinforces the notion that psychotherapy involves making a commitment to work on problems. It also protects clinicians’ financial interests and mitigates possible resentment that might arise if office time committed to a patient went unreimbursed.6 Clinicians who charge for missed appointments should inform patients of this at the beginning of treatment, explaining clearly that the patient—not the insurer—will be paying for unused treatment time.2,4
Since the 1980s, outpatient psychiatrists have increasingly worked in public agencies or other organizational practice settings7 where patients—whose care is funded by public monies or third-party payors—cannot afford to pay for missed appointments. If you work in a clinic such as the one where Dr. C provides services, you probably are paid an hourly wage whether your patients show up or not. To pay you and remain solvent, your clinic must find ways other than charging patients to address and reduce no-shows.
The literature abounds with research on why no-shows occur. But no-shows seem to be more common in psychiatry than in other medical specialties.8 The frequency of no-shows varies considerably, but it’s a big problem in some mental health treatment contexts, with reported rates ranging from 12% to 60%.9 A recent, comprehensive review reported that approximately 30% of patients refuse, drop out, or prematurely disengage from services after first-episode psychosis.10 No-shows and drop outs are linked to clinical deterioration11 and heightened risk of hospitalization.12
Jaeschke et al15 suggests that no-shows, dropping out of treatment, and other forms of what doctors call “noncompliance” or “nonadherence” might be better conceptualized as a lack of “concordance,” “mutuality,” or “shared ideology” about what ails patients and the role of their physicians. For this reason, striving for a “partnership between a physician and a patient,” with the patient “fully engaged in the two-way communication with a doctor … seems to be a much more suitable way of achieving therapeutic progress in the discipline of psychiatry.”15
Reducing no-shows: Evidence-based methods
Many medical and mental health articles describe evidence-based methods for lowering no-show rates. Studies document the value of assertive outreach, home visits, avoiding scheduling on religious holidays, scheduling appointments in the afternoon rather than the morning, providing assistance with transportation,8 sending reminder letters,16 or making telephone calls.17 Growing evidence suggests that text messages reduce missed appointments, even among patients with severe disorders (eg, schizophrenia) that compromise cognitive functioning.18
The measures I’ve described won’t prevent every patient from no-showing repeatedly. If you or your employer have tried some of these proven methods and they haven’t reduced a patient’s persistent no-shows, and if it makes sense from a clinical and financial standpoint, then it’s all right to dismiss the patient.
To understand why you are permitted to dismiss a patient from your practice, it helps to understand how the law views the doctor–patient relationship. A doctor has no legal duty to treat anyone—even someone who desperately needs care—unless the doctor has taken some action to establish a treatment relationship with that person. Having previously treated the patient establishes a treatment relationship, as could other actions such as giving specific advice or (in some cases) making an appointment for a person. Once you have a treatment relationship with someone, you usually must continue to provide necessary medical attention until either the treatment episode has concluded or you and the patient agree to end treatment.20
For many chronic mental illnesses, a treatment episode could last years. But this does not force you to continue caring for a patient indefinitely if your circumstances change or if the patient’s behavior causes you to want to withdraw from providing care.
To ethically end care of a patient while a treatment episode is ongoing, you must either transfer care to another competent physician, or give your patient adequate notice and opportunity to obtain appropriate treatment elsewhere.20 If you fail to do either, however, you are guilty of “abandonment” and potentially subject to discipline by state licensing authorities21 or, if harm results, a malpractice lawsuit.22
In many states, statutes or regulations describe what you must do to end a treatment relationship properly. Ohio’s rule is typical: You must send the patient a certified letter explaining that the treatment relationship is ending, that you will remain available to provide care for 30 days, and that you will send treatment records to another provider upon receiving the patient’s signed authorization.21
One note of caution, however: If you practice in hospitals or groups, or if you or the agency where you work has signed provider contracts, you may have agreed to terms of practice that make dismissing a patient more complicated.23 Whether you practice individually or in a large organization, it’s usually wise to get advice from an attorney and/or your malpractice carrier to make sure you’re handling a patient dismissal the right way.
Dear Dr. Mossman,
The clinic where I work initiated a “3 misses and out” policy: If a patient doesn’t show for 3 appointments in a 12-month period, the clinic removes him from the patient rolls. I’ve heard such policies are common, but I worry: Is this abandonment?
Submitted by “Dr. C”
The short answer to Dr. C’s question is, “Handled properly, it’s not abandonment.” But if this response really was satisfactory, Dr. C probably would not have asked the question. Dealing with no-show patients has bothered psychiatrists, other mental health professionals, and other physicians for decades.1
Clinicians worry when patients miss important follow-up, and unreimbursed office time won’t help pay a clinician’s salary or office expenses.2 But a policy such as the one Dr. C describes may not be the best response—clinically or financially—for many patients who miss appointments repeatedly.
If no-show patients worry you or cause problems where you practice, read on as I cover:
- charging for missed appointments
- why patients miss appointments
- evidence-based methods to improve show-up rates
- when ending a treatment relationship unilaterally is not abandonment
- how to dismiss no-show patients from a practice properly.
Before the mid-1980s, most office-based psychiatrists worked in solo or small group and required patients to pay cash for treatment; approximately 40% of psychiatrists still practice this way.3 Often, private practice clinicians require payment for appointments missed without 24 hours’ notice. This well-accepted practice2,4,5 reinforces the notion that psychotherapy involves making a commitment to work on problems. It also protects clinicians’ financial interests and mitigates possible resentment that might arise if office time committed to a patient went unreimbursed.6 Clinicians who charge for missed appointments should inform patients of this at the beginning of treatment, explaining clearly that the patient—not the insurer—will be paying for unused treatment time.2,4
Since the 1980s, outpatient psychiatrists have increasingly worked in public agencies or other organizational practice settings7 where patients—whose care is funded by public monies or third-party payors—cannot afford to pay for missed appointments. If you work in a clinic such as the one where Dr. C provides services, you probably are paid an hourly wage whether your patients show up or not. To pay you and remain solvent, your clinic must find ways other than charging patients to address and reduce no-shows.
The literature abounds with research on why no-shows occur. But no-shows seem to be more common in psychiatry than in other medical specialties.8 The frequency of no-shows varies considerably, but it’s a big problem in some mental health treatment contexts, with reported rates ranging from 12% to 60%.9 A recent, comprehensive review reported that approximately 30% of patients refuse, drop out, or prematurely disengage from services after first-episode psychosis.10 No-shows and drop outs are linked to clinical deterioration11 and heightened risk of hospitalization.12
Jaeschke et al15 suggests that no-shows, dropping out of treatment, and other forms of what doctors call “noncompliance” or “nonadherence” might be better conceptualized as a lack of “concordance,” “mutuality,” or “shared ideology” about what ails patients and the role of their physicians. For this reason, striving for a “partnership between a physician and a patient,” with the patient “fully engaged in the two-way communication with a doctor … seems to be a much more suitable way of achieving therapeutic progress in the discipline of psychiatry.”15
Reducing no-shows: Evidence-based methods
Many medical and mental health articles describe evidence-based methods for lowering no-show rates. Studies document the value of assertive outreach, home visits, avoiding scheduling on religious holidays, scheduling appointments in the afternoon rather than the morning, providing assistance with transportation,8 sending reminder letters,16 or making telephone calls.17 Growing evidence suggests that text messages reduce missed appointments, even among patients with severe disorders (eg, schizophrenia) that compromise cognitive functioning.18
The measures I’ve described won’t prevent every patient from no-showing repeatedly. If you or your employer have tried some of these proven methods and they haven’t reduced a patient’s persistent no-shows, and if it makes sense from a clinical and financial standpoint, then it’s all right to dismiss the patient.
To understand why you are permitted to dismiss a patient from your practice, it helps to understand how the law views the doctor–patient relationship. A doctor has no legal duty to treat anyone—even someone who desperately needs care—unless the doctor has taken some action to establish a treatment relationship with that person. Having previously treated the patient establishes a treatment relationship, as could other actions such as giving specific advice or (in some cases) making an appointment for a person. Once you have a treatment relationship with someone, you usually must continue to provide necessary medical attention until either the treatment episode has concluded or you and the patient agree to end treatment.20
For many chronic mental illnesses, a treatment episode could last years. But this does not force you to continue caring for a patient indefinitely if your circumstances change or if the patient’s behavior causes you to want to withdraw from providing care.
To ethically end care of a patient while a treatment episode is ongoing, you must either transfer care to another competent physician, or give your patient adequate notice and opportunity to obtain appropriate treatment elsewhere.20 If you fail to do either, however, you are guilty of “abandonment” and potentially subject to discipline by state licensing authorities21 or, if harm results, a malpractice lawsuit.22
In many states, statutes or regulations describe what you must do to end a treatment relationship properly. Ohio’s rule is typical: You must send the patient a certified letter explaining that the treatment relationship is ending, that you will remain available to provide care for 30 days, and that you will send treatment records to another provider upon receiving the patient’s signed authorization.21
One note of caution, however: If you practice in hospitals or groups, or if you or the agency where you work has signed provider contracts, you may have agreed to terms of practice that make dismissing a patient more complicated.23 Whether you practice individually or in a large organization, it’s usually wise to get advice from an attorney and/or your malpractice carrier to make sure you’re handling a patient dismissal the right way.
1. Adler LM, Yamamoto J, Goin M. Failed psychiatric clinic appointments. Relationship to social class. Calif Med. 1963;99:388-392.
2. Buppert C. How to deal with missed appointments. Dermatol Nurs 2009;21(4):207-208.
3. National Council Medical Director Institute. The psychiatric shortage: causes and solutions. https://www.thenationalcouncil.org/wp-content/uploads/2017/03/Psychiatric-Shortage_National-Council-.pdf. Published March 28, 2017. Accessed April 6, 2017.
4. Legal & Regulatory Affairs staff. Practitioner pointer: how to handle late and missed appointments. http://www.apapracticecentral.org/update/2014/11-06/late-missed-appoitments.aspx. Published November 6, 2004. Accessed April 7, 2017.
5. Centers for Medicare & Medicaid Services. MLN Matters Number: MM5613. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM5613.pdf. Updated November 12, 2014. Accessed April 7, 2017.
6. MacCutcheon M. Why I charge for late cancellations and no-shows to therapy. http://www.goodtherapy.org/blog/why-i-charge-for-late-cancellations-no-shows-to-therapy-0921164. Published September 21, 2016. Accessed April 6, 2017.
7. Kalman TP, Goldstein MA. Satisfaction of Manhattan psychiatrists with private practice: assessing the impact of managed care. http://www.medscape.com/viewarticle/430759_4. Accessed April 6, 2017.
8. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat. 2007;13(6):423-434.
9. Long J, Sakauye K, Chisty K, et al. The empty chair appointment. SAGE Open. 2016;6:1-5.
10. Doyle R, Turner N, Fanning F, et al. First-episode psychosis and disengagement from treatment: a systematic review. Psychiatr Serv. 2014;65(5):603-611.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51(7):885-889.
12. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. Br J Psychiatry. 2000;176:160-165.
13. Williamson AE, Ellis DA, Wilson P, et al. Understanding repeated non-attendance in health services: a pilot analysis of administrative data and full study protocol for a national retrospective cohort. BMJ Open. 2017;7(2):e014120. doi: 10.1136/bmjopen-2016-014120.
14. Binnie J, Boden Z. Non-attendance at psychological therapy appointments. Mental Health Rev J. 2016;21(3):231-248.
15. Jaeschke R, Siwek M, Dudek D. Various ways of understanding compliance: a psychiatrist’s view. Arch Psychiatr Psychother. 2011;13(3):49-55.
16. Boland B, Burnett F. Optimising outpatient efficiency – development of an innovative ‘Did Not Attend’ management approach. Int J Psychiatry Clin Pract. 2014;18(3):217-219.
17. Pennington D, Hodgson J. Non‐attendance and invitation methods within a CBT service. Mental Health Rev J. 2012;17(3):145-151.
18. Sims H, Sanghara H, Hayes D, et al. Text message reminders of appointments: a pilot intervention at four community mental health clinics in London. Psychiatr Serv. 2012;63(2):161-168.
19. Oldham M, Kellett S, Miles E, et al. Interventions to increase attendance at psychotherapy: a meta-analysis of randomized controlled trials. J Consult Clin Psychol. 2012;80(5):928-939.
20. Gore AG, Grossman EL, Martin L, et al. Physicians, surgeons, and other healers. In: American Jurisprudence. 2nd ed, §130. Eagan, MN: West Publishing; 2017:61.
21. Ohio Administrative Code §4731-27-02.
22. Lowery v Miller, 157 Wis 2d 503, 460 N.W. 2d 446 (Wis App 1990).
23. Brockway LH. Terminating patient relationships: how to dismiss without abandoning. TMLT. https://www.tmlt.org/tmlt/tmlt-resources/newscenter/blog/2009/Terminating-patient-relationships.html. Published June 19, 2009. Accessed April 3, 2017.
1. Adler LM, Yamamoto J, Goin M. Failed psychiatric clinic appointments. Relationship to social class. Calif Med. 1963;99:388-392.
2. Buppert C. How to deal with missed appointments. Dermatol Nurs 2009;21(4):207-208.
3. National Council Medical Director Institute. The psychiatric shortage: causes and solutions. https://www.thenationalcouncil.org/wp-content/uploads/2017/03/Psychiatric-Shortage_National-Council-.pdf. Published March 28, 2017. Accessed April 6, 2017.
4. Legal & Regulatory Affairs staff. Practitioner pointer: how to handle late and missed appointments. http://www.apapracticecentral.org/update/2014/11-06/late-missed-appoitments.aspx. Published November 6, 2004. Accessed April 7, 2017.
5. Centers for Medicare & Medicaid Services. MLN Matters Number: MM5613. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM5613.pdf. Updated November 12, 2014. Accessed April 7, 2017.
6. MacCutcheon M. Why I charge for late cancellations and no-shows to therapy. http://www.goodtherapy.org/blog/why-i-charge-for-late-cancellations-no-shows-to-therapy-0921164. Published September 21, 2016. Accessed April 6, 2017.
7. Kalman TP, Goldstein MA. Satisfaction of Manhattan psychiatrists with private practice: assessing the impact of managed care. http://www.medscape.com/viewarticle/430759_4. Accessed April 6, 2017.
8. Mitchell AJ, Selmes T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv Psychiatr Treat. 2007;13(6):423-434.
9. Long J, Sakauye K, Chisty K, et al. The empty chair appointment. SAGE Open. 2016;6:1-5.
10. Doyle R, Turner N, Fanning F, et al. First-episode psychosis and disengagement from treatment: a systematic review. Psychiatr Serv. 2014;65(5):603-611.
11. Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51(7):885-889.
12. Killaspy H, Banerjee S, King M, et al. Prospective controlled study of psychiatric out-patient non-attendance. Characteristics and outcome. Br J Psychiatry. 2000;176:160-165.
13. Williamson AE, Ellis DA, Wilson P, et al. Understanding repeated non-attendance in health services: a pilot analysis of administrative data and full study protocol for a national retrospective cohort. BMJ Open. 2017;7(2):e014120. doi: 10.1136/bmjopen-2016-014120.
14. Binnie J, Boden Z. Non-attendance at psychological therapy appointments. Mental Health Rev J. 2016;21(3):231-248.
15. Jaeschke R, Siwek M, Dudek D. Various ways of understanding compliance: a psychiatrist’s view. Arch Psychiatr Psychother. 2011;13(3):49-55.
16. Boland B, Burnett F. Optimising outpatient efficiency – development of an innovative ‘Did Not Attend’ management approach. Int J Psychiatry Clin Pract. 2014;18(3):217-219.
17. Pennington D, Hodgson J. Non‐attendance and invitation methods within a CBT service. Mental Health Rev J. 2012;17(3):145-151.
18. Sims H, Sanghara H, Hayes D, et al. Text message reminders of appointments: a pilot intervention at four community mental health clinics in London. Psychiatr Serv. 2012;63(2):161-168.
19. Oldham M, Kellett S, Miles E, et al. Interventions to increase attendance at psychotherapy: a meta-analysis of randomized controlled trials. J Consult Clin Psychol. 2012;80(5):928-939.
20. Gore AG, Grossman EL, Martin L, et al. Physicians, surgeons, and other healers. In: American Jurisprudence. 2nd ed, §130. Eagan, MN: West Publishing; 2017:61.
21. Ohio Administrative Code §4731-27-02.
22. Lowery v Miller, 157 Wis 2d 503, 460 N.W. 2d 446 (Wis App 1990).
23. Brockway LH. Terminating patient relationships: how to dismiss without abandoning. TMLT. https://www.tmlt.org/tmlt/tmlt-resources/newscenter/blog/2009/Terminating-patient-relationships.html. Published June 19, 2009. Accessed April 3, 2017.
What is your liability for involuntary commitment based on faulty information?
Dear Dr. Mossman,
Last week, I hospitalized a patient against her will, based in part on what her family members told me she had threatened to do. The patient threatened to sue me and said I should have known that her relatives were lying. What if my patient is right? Could I face liability if I involuntarily hospitalized her based on bad collateral information?
Submitted by “Dr. R”
In all U.S. states, laws permit psychiatrists to involuntarily hospitalize persons who pose a danger to themselves or others because of mental illness.1 But taking this step can be tough. Deciding to hospitalize a patient against her will involves weighing her wants and freedom against your duty to look out for her long-term welfare and the community’s safety.2,3 Often, psychiatrists make these decisions under pressure because the family wants something done immediately, other patients also need attention, the clinical picture is incomplete, or potential dispositions (eg, crisis care and inpatient beds) are limited.3 Given such constraints, you can’t always make perfect decisions.
Dr. R’s question has 2 parts:
- What liabilities can a clinician face if a patient is wrongfully committed?
- What liabilities could arise from relying on inaccurate information or making a false petition in order to hospitalize a patient?
We hope that as you and Dr. R read our answers, you’ll have a clearer understanding of:
- the rationale for civil commitment
- how patients, doctors, and courts view civil commitment
- the role of collateral information in decision-making
- relevant legal concepts and case law.
Rationale for civil commitment
For centuries, society has used civil commitment as one of its legal methods for intervening when persons pose a danger to themselves or others because of their mental illness.4 Because incapacitation or death could result from a “false-negative” decision to release a dangerous patient, psychiatrists err on the side of caution and tolerate many “false-positive” hospitalizations of persons who wouldn’t have hurt anyone.5
We can never know if a patient would have done harm had she not been hospitalized. Measures of suicidality and hostility tend to subside during involuntary hospital treatment.6 After hospitalization, many patients cite protection from harm as a reason they are thankful for their treatment.7-9 Some involuntary inpatients want to be hospitalized but hide this for conscious or unconscious reasons,10,11 and involuntary treatment sometimes is the only way to help persons whose illness-induced anosognosia12 prevents them from understanding why they need treatment.13 Involuntary inpatient care leads to modest symptom reduction14,15 and produces treatment outcomes no worse than those of non-coerced patients.10
Patients’ views
Patients often view commitment as unjustified.16 They and their advocates object to what some view as the ultimate infringement on civil liberty.7,17 By its nature, involuntary commitment eliminates patients’ involvement in a major treatment decision,8 disempowers them,18 and influences their relationship with the treatment team.15
Some involuntary patients feel disrespected by staff members8 or experience inadvertent psychological harm, including “loss of self-esteem, identity, self-control, and self-efficacy, as well as diminished hope in the possibility of recovery.”15 Involuntary hospitalization also can have serious practical consequences. Commitment can lead to social stigma, loss of gun rights, increased risks of losing child custody, housing problems, and possible disqualification from some professions.19
Having seen many involuntary patients undergo a change of heart after treatment, psychiatrist Alan Stone proposed the “Thank You Theory” of civil commitment: involuntary hospitalization can be justified by showing that the patient is grateful after recovering.20 Studies show, however, that gratitude is far from universal.1
How coercion is experienced often depends on how it is communicated. The less coercion patients perceive, the better they feel about the treatment they received.21 Satisfaction is important because it leads to less compulsory readmission,22 and dissatisfaction makes malpractice lawsuits more likely.23
Commitment decision-making
States’ laws, judges’ attitudes, and court decisions establish each jurisdiction’s legal methods for instituting emergency holds and willingness to tolerate “false-positive” involuntary hospitalization,4,24 all of which create variation between and within states in how civil commitment laws are applied. As a result, clinicians’ decisions are influenced “by a range of social, political, and economic factors,”25 including patients’ sex, race, age, homelessness, employment status, living situation, diagnoses, previous involuntary treatment, and dissatisfaction with mental health treatment.22,26-32 Furthermore, the potential for coercion often blurs the line between an offer of voluntary admission and an involuntary hospitalization.18
Collateral information
Psychiatrists owe each patient a sound clinical assessment before deciding to initiate involuntarily hospitalization. During a psychiatric crisis, a patient might not be forthcoming or could have impaired memory or judgment. Information from friends or family can help fill in gaps in a patient’s self-report.33 As Dr. R’s question illustrates, adequate assessment often includes seeking information from persons familiar with the patient.1 A report on the Virginia Tech shootings by the Virginia Office of the Inspector General describes how collateral sources can provide otherwise missing evidence of dangerousness,34 and it often leads clinicians toward favoring admission.35
Yet clinicians should regard third-party reports with caution.36 As one attorney warns, “Psychiatrists should be cautious of the underlying motives of well-meaning family members and relatives.”37 If you make a decision to hospitalize a patient involuntarily based on collateral information that turns out to be flawed, are you at fault and potentially liable for harm to the patient?
False petitions and liability
If you’re in a situation similar to the one Dr. R describes, you can take solace in knowing that courts generally provide immunity to a psychiatrist who makes a reasonable, well-intentioned decision to commit someone. The degree of immunity offered varies by jurisdiction. Table 1 provides examples of immunity language from several states’ statutes.
Many states’ statutes also lay out the potential consequences if a psychiatrist takes action to involuntarily hospitalize someone in bad faith or with malicious intent. In some jurisdictions, such actions can lead to criminal sanctions against the doctor or against the party who made a false petition (eg, a devious family member) (Table 2). Commenting on Texas’s statute, attorney Jeffrey Anderson explains, “The touchstone for causes of action based upon a wrongful civil commitment require that the psychiatrist[’s] conduct be found to be unreasonable and negligent. [Immunity…] still requires that a psychiatrist[’s] diagnosis of a patient[’s] threat to harm himself or others be a reasonable and prudent one.”37
The immunity extended through such statutes usually is limited to claims arising directly from the detention. For example, in the California case of Jacobs v Grossmont Hospital, a patient under a 72-hour hold fell and fractured her leg, and she sought damages. The trial court dismissed the suit under the immunity statute applicable to commitment decisions, but the appellate court held that “the immunity did not extend to other negligent acts.… The trial court erred in assuming that … the hospital was exempt from all liability for any negligence that occurred during the lawful hold.”38
Bingham v Cedars-Sinai Health Systems illustrates how physicians can lose immunity.39 A nurse contacted her supervisor to report a colleague who had stolen narcotics from work and compromised patient care. In response, the supervisor, hospital, and several physicians agreed to have her involuntarily committed. Later, it was confirmed that the colleague had taken the narcotics. She later sued the hospital system, claiming—in addition to malpractice—retaliation, invasion of privacy, assault and battery, false imprisonment, defamation, intentional infliction of emotional distress, disability-based harassment, and violation of her civil rights. Citing California’s immunity statute, the trial court granted summary judgment to the clinicians and hospital system. On appeal, however, the appellate court reversed the judgment, holding that the defendants had not shown that “the decision to detain Bingham was based on probable cause, a prerequisite to the exemption from liability,” and that Bingham had some legitimate grounds for her lawsuit.
A key point for Dr. R to consider is that, although some states provide immunity if the psychiatrist’s admitting decision was based on an evaluation “performed in good faith,”40 other states’ immunity provisions apply only if the psychiatrist had probable cause to make a decision to detain.41
Ways to reduce liability risk
Although an involuntary hospitalization could have an uncertain basis, psychiatrists can reduce the risk of legal liability for their decisions. Good documentation is important. Admitting psychiatrists usually make sound decisions, but the corresponding documentation frequently lacks clinical justification.42-44 As the rate of appropriate documentation of admission decision-making improves, the rate of commitment falls,44 and patients’ legal rights enjoy greater protection.43 Poor communication can decrease the quality of care and increase the risk of a malpractice lawsuit.45 This is just one of many reasons why you should explain your reasons for involuntary hospitalization and inform patients of the procedures for judicial review.8,9 Table 3 summarizes other steps to reduce liability risk when committing patients to the hospital.1,8,15,21,33,35-37,42,45-47
1. Pinals DA, Mossman D. Evaluation for civil commitment: best practices for forensic mental health assessments. New York, NY: Oxford University Press; 2011.
2. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgemont). 2010;7(10):30-40.
3. Hedman LC, Petrila J, Fisher WH, et al. State laws on emergency holds for mental health stabilization. Psychiatr Serv. 2016;67(5):529-535.
4. Groendyk Z. “It takes a lot to get into Bellevue”: a pro-rights critique of New York’s involuntary commitment law. Fordham Urban Law J. 2013;40(1):548-585.
5. Brooks RA. U.S. psychiatrists’ beliefs and wants about involuntary civil commitment grounds. Int J Law Psychiatry. 2006;29(1):13-21.
6. Giacco D, Priebe S. Suicidality and hostility following involuntary hospital treatment. PLoS One. 2016;11(5):e0154458. doi: 10.1371/journal.pone.0154458.
7. Wyder M, Bland R, Herriot A, et al. The experiences of the legal processes of involuntary treatment orders: tension between the legal and medical frameworks. Int J Law Psychiatry. 2015;38:44-50.
8. Valenti E, Giacco D, Katasakou C, et al. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics. 2014;40(12):832-836.
9. Katsakou C, Rose D, Amos T, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;42(7):1169-1179.
10. Kaltiala-Heino R, Laippala P, Salokangas RK. Impact of coercion on treatment outcome. Int J Law Psychiatry. 1997;20(3):311-322.
11. Hoge SK, Lidz CW, Eisenberg M, et al. Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiatry. 1997;20(2):167-181.
12. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):10-17. 13. Gordon S. The danger zone: how the dangerousness standard in civil commitment proceedings harms people with serious mental illness. Case Western Reserve Law Review. 2016;66(3):657-700.
14. Kallert TW, Katsakou C, Adamowski T, et al. Coerced hospital admission and symptom change—a prospective observational multi-centre study. PLoS One. 2011;6(11):e28191. doi: 10.1371/journal.pone.0028191.
15. Danzer G, Wilkus-Stone A. The give and take of freedom: the role of involuntary hospitalization and treatment in recovery from mental illness. Bull Menninger Clin. 2015;79(3):255-280.
16. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
17. Amidov T. Involuntary commitment is unnecessary and discriminatory. In: Berlatsky N, ed. Mental illness. Farmington Hills, MI: Greenhaven Press; 2016;140-145.
18. Monahan J, Hoge SK, Lidz C, et al. Coercion and commitment: understanding involuntary mental hospital admission. Int J Law Psychiatry. 1995;18(3):249-263.
19. Guest Pryal KR. Heller’s scapegoats. North Carolina Law Review. 2015;93(5):1439-1473.
20. Stone AA. Mental health and law: a system in transition. Washington, DC: U.S. Government Printing Office; 1975:75-176.
21. Katsakou C, Bowers L, Amos T, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286-292.
22. Setkowski K, van der Post LF, Peen J, et al. Changing patient perspectives after compulsory admission and the risk of re-admission during 5 years of follow-up: the Amsterdam study of acute psychiatry IX. Int J Soc Psychiatry. 2016;62(6):578-588.
23. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
24. Goldman A. Continued overreliance on involuntary commitment: the need for a less restrictive alternative. J Leg Med. 2015;36(2):233-251.
25. Fisher WH, Grisso T. Commentary: civil commitment statutes—40 years of circumvention. J Am Acad Psychiatry Law. 2010;38(3):365-368.
26. Curley A, Agada E, Emechebe A, et al. Exploring and explaining involuntary care: the relationship between psychiatric admission status, gender and other demographic and clinical variables. Int J Law Psychiatry. 2016;47:53-59.
27. Muroff JR, Jackson JS, Mowbray CT, et al. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry. 2007;29(6):481-488.
28. Muroff JR, Edelsohn GA, Joe S, et al. The role of race in diagnostic and disposition decision making in a pediatric psychiatric emergency service. Gen Hosp Psychiatry. 2008;30(3):269-276.
29. Unick GJ, Kessell E, Woodard EK, et al. Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. Gen Hosp Psychiatry. 2011;33(6):618-625.
30. Ng XT, Kelly BD. Voluntary and involuntary care: three-year study of demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatry. 2012;35(4):317-326.
31. Lo TT, Woo BK. The impact of unemployment on utilization of psychiatric emergency services. Gen Hosp Psychiatry. 2011;33(3):e7-e8. doi: 10.1016/j.genhosppsych.2010.10.010.
32. van der Post LFM, Peen J, Dekker JJ. A prediction model for the incidence of civil detention for crisis patients with psychiatric illnesses; the Amsterdam study of acute psychiatry VII. Soc Psychiatry Psychiatr Epidemiol. 2014;49(2):283-290.
33. Heilbrun K, NeMoyer A, King C, et al. Using third-party information in forensic mental health assessment: a critical review. Court Review. 2015;51(1):16-35.
34. Mass shootings at Virginia Tech, April 16, 2007 report of the Virginia Tech Review Panel presented to Timothy M. Kaine, Governor, Commonwealth of Virginia. http://cdm16064.contentdm.oclc.org/cdm/ref/collection/p266901coll4/id/904. Accessed February 2, 2017.
35. Segal SP, Laurie TA, Segal MJ. Factors in the use of coercive retention in civil commitment evaluations in psychiatric emergency services. Psychiatr Serv. 2001;52(4):514-520.
36. Lincoln A, Allen MH. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
37. Anderson JC. How I decided to sue you: misadventures in psychiatry. Reprinted in part from: Moody CE, Smith MT, Maedgen BJ. Litigation of psychiatric malpractice claims. Presented at: Medical Malpractice Conference; April 15, 1993; San Antonio, TX. http://www.texaslawfirm.com/Articles/How_I_Decided_to_Sue_You__Misadventrues_in_Psychiatry.pdf. Accessed December 27, 2016.
38. Jacobs v Grossmont Hospital, 108 Cal App 4th 69, 133 Cal Rptr 2d9 (2003).
39. Bingham v Cedars Sinai Health Systems, WL 2137442, Cal App 2 Dist (2004).
40. Ohio Revised Code §5122.34.
41. California Welfare & Institutions Code §5150(E).
42. Hashmi A, Shad M, Rhoades HM, et al. Involuntary detention: do psychiatrists clinically justify continuing involuntary hospitalization? Psychiatr Q. 2014;85(3):285-293.
43. Brayley J, Alston A, Rogers K. Legal criteria for involuntary mental health admission: clinician performance in recording grounds for decision. Med J Aust. 2015;203(8):334.
44. Perrigo TL, Williams KA. Implementation of an evidence based guideline for assessment and documentation of the civil commitment process. Community Ment Health J. 2016;52(8):1033-1036.
45. Mor S, Rabinovich-Einy O. Relational malpractice. Seton Hall Law Rev. 2012;42(2):601-642.
46. Tate v Kaiser Foundation Hospitals, WL 176625, U.S. Dist. LEXIS 5891 (CD Cal 2014).
47. Ranieri V, Madigan K, Roche E, et al. Caregivers’ perceptions of coercion in psychiatric hospital admission. Psychiatry Res. 2015;22(3)8:380-385.
Dear Dr. Mossman,
Last week, I hospitalized a patient against her will, based in part on what her family members told me she had threatened to do. The patient threatened to sue me and said I should have known that her relatives were lying. What if my patient is right? Could I face liability if I involuntarily hospitalized her based on bad collateral information?
Submitted by “Dr. R”
In all U.S. states, laws permit psychiatrists to involuntarily hospitalize persons who pose a danger to themselves or others because of mental illness.1 But taking this step can be tough. Deciding to hospitalize a patient against her will involves weighing her wants and freedom against your duty to look out for her long-term welfare and the community’s safety.2,3 Often, psychiatrists make these decisions under pressure because the family wants something done immediately, other patients also need attention, the clinical picture is incomplete, or potential dispositions (eg, crisis care and inpatient beds) are limited.3 Given such constraints, you can’t always make perfect decisions.
Dr. R’s question has 2 parts:
- What liabilities can a clinician face if a patient is wrongfully committed?
- What liabilities could arise from relying on inaccurate information or making a false petition in order to hospitalize a patient?
We hope that as you and Dr. R read our answers, you’ll have a clearer understanding of:
- the rationale for civil commitment
- how patients, doctors, and courts view civil commitment
- the role of collateral information in decision-making
- relevant legal concepts and case law.
Rationale for civil commitment
For centuries, society has used civil commitment as one of its legal methods for intervening when persons pose a danger to themselves or others because of their mental illness.4 Because incapacitation or death could result from a “false-negative” decision to release a dangerous patient, psychiatrists err on the side of caution and tolerate many “false-positive” hospitalizations of persons who wouldn’t have hurt anyone.5
We can never know if a patient would have done harm had she not been hospitalized. Measures of suicidality and hostility tend to subside during involuntary hospital treatment.6 After hospitalization, many patients cite protection from harm as a reason they are thankful for their treatment.7-9 Some involuntary inpatients want to be hospitalized but hide this for conscious or unconscious reasons,10,11 and involuntary treatment sometimes is the only way to help persons whose illness-induced anosognosia12 prevents them from understanding why they need treatment.13 Involuntary inpatient care leads to modest symptom reduction14,15 and produces treatment outcomes no worse than those of non-coerced patients.10
Patients’ views
Patients often view commitment as unjustified.16 They and their advocates object to what some view as the ultimate infringement on civil liberty.7,17 By its nature, involuntary commitment eliminates patients’ involvement in a major treatment decision,8 disempowers them,18 and influences their relationship with the treatment team.15
Some involuntary patients feel disrespected by staff members8 or experience inadvertent psychological harm, including “loss of self-esteem, identity, self-control, and self-efficacy, as well as diminished hope in the possibility of recovery.”15 Involuntary hospitalization also can have serious practical consequences. Commitment can lead to social stigma, loss of gun rights, increased risks of losing child custody, housing problems, and possible disqualification from some professions.19
Having seen many involuntary patients undergo a change of heart after treatment, psychiatrist Alan Stone proposed the “Thank You Theory” of civil commitment: involuntary hospitalization can be justified by showing that the patient is grateful after recovering.20 Studies show, however, that gratitude is far from universal.1
How coercion is experienced often depends on how it is communicated. The less coercion patients perceive, the better they feel about the treatment they received.21 Satisfaction is important because it leads to less compulsory readmission,22 and dissatisfaction makes malpractice lawsuits more likely.23
Commitment decision-making
States’ laws, judges’ attitudes, and court decisions establish each jurisdiction’s legal methods for instituting emergency holds and willingness to tolerate “false-positive” involuntary hospitalization,4,24 all of which create variation between and within states in how civil commitment laws are applied. As a result, clinicians’ decisions are influenced “by a range of social, political, and economic factors,”25 including patients’ sex, race, age, homelessness, employment status, living situation, diagnoses, previous involuntary treatment, and dissatisfaction with mental health treatment.22,26-32 Furthermore, the potential for coercion often blurs the line between an offer of voluntary admission and an involuntary hospitalization.18
Collateral information
Psychiatrists owe each patient a sound clinical assessment before deciding to initiate involuntarily hospitalization. During a psychiatric crisis, a patient might not be forthcoming or could have impaired memory or judgment. Information from friends or family can help fill in gaps in a patient’s self-report.33 As Dr. R’s question illustrates, adequate assessment often includes seeking information from persons familiar with the patient.1 A report on the Virginia Tech shootings by the Virginia Office of the Inspector General describes how collateral sources can provide otherwise missing evidence of dangerousness,34 and it often leads clinicians toward favoring admission.35
Yet clinicians should regard third-party reports with caution.36 As one attorney warns, “Psychiatrists should be cautious of the underlying motives of well-meaning family members and relatives.”37 If you make a decision to hospitalize a patient involuntarily based on collateral information that turns out to be flawed, are you at fault and potentially liable for harm to the patient?
False petitions and liability
If you’re in a situation similar to the one Dr. R describes, you can take solace in knowing that courts generally provide immunity to a psychiatrist who makes a reasonable, well-intentioned decision to commit someone. The degree of immunity offered varies by jurisdiction. Table 1 provides examples of immunity language from several states’ statutes.
Many states’ statutes also lay out the potential consequences if a psychiatrist takes action to involuntarily hospitalize someone in bad faith or with malicious intent. In some jurisdictions, such actions can lead to criminal sanctions against the doctor or against the party who made a false petition (eg, a devious family member) (Table 2). Commenting on Texas’s statute, attorney Jeffrey Anderson explains, “The touchstone for causes of action based upon a wrongful civil commitment require that the psychiatrist[’s] conduct be found to be unreasonable and negligent. [Immunity…] still requires that a psychiatrist[’s] diagnosis of a patient[’s] threat to harm himself or others be a reasonable and prudent one.”37
The immunity extended through such statutes usually is limited to claims arising directly from the detention. For example, in the California case of Jacobs v Grossmont Hospital, a patient under a 72-hour hold fell and fractured her leg, and she sought damages. The trial court dismissed the suit under the immunity statute applicable to commitment decisions, but the appellate court held that “the immunity did not extend to other negligent acts.… The trial court erred in assuming that … the hospital was exempt from all liability for any negligence that occurred during the lawful hold.”38
Bingham v Cedars-Sinai Health Systems illustrates how physicians can lose immunity.39 A nurse contacted her supervisor to report a colleague who had stolen narcotics from work and compromised patient care. In response, the supervisor, hospital, and several physicians agreed to have her involuntarily committed. Later, it was confirmed that the colleague had taken the narcotics. She later sued the hospital system, claiming—in addition to malpractice—retaliation, invasion of privacy, assault and battery, false imprisonment, defamation, intentional infliction of emotional distress, disability-based harassment, and violation of her civil rights. Citing California’s immunity statute, the trial court granted summary judgment to the clinicians and hospital system. On appeal, however, the appellate court reversed the judgment, holding that the defendants had not shown that “the decision to detain Bingham was based on probable cause, a prerequisite to the exemption from liability,” and that Bingham had some legitimate grounds for her lawsuit.
A key point for Dr. R to consider is that, although some states provide immunity if the psychiatrist’s admitting decision was based on an evaluation “performed in good faith,”40 other states’ immunity provisions apply only if the psychiatrist had probable cause to make a decision to detain.41
Ways to reduce liability risk
Although an involuntary hospitalization could have an uncertain basis, psychiatrists can reduce the risk of legal liability for their decisions. Good documentation is important. Admitting psychiatrists usually make sound decisions, but the corresponding documentation frequently lacks clinical justification.42-44 As the rate of appropriate documentation of admission decision-making improves, the rate of commitment falls,44 and patients’ legal rights enjoy greater protection.43 Poor communication can decrease the quality of care and increase the risk of a malpractice lawsuit.45 This is just one of many reasons why you should explain your reasons for involuntary hospitalization and inform patients of the procedures for judicial review.8,9 Table 3 summarizes other steps to reduce liability risk when committing patients to the hospital.1,8,15,21,33,35-37,42,45-47
Dear Dr. Mossman,
Last week, I hospitalized a patient against her will, based in part on what her family members told me she had threatened to do. The patient threatened to sue me and said I should have known that her relatives were lying. What if my patient is right? Could I face liability if I involuntarily hospitalized her based on bad collateral information?
Submitted by “Dr. R”
In all U.S. states, laws permit psychiatrists to involuntarily hospitalize persons who pose a danger to themselves or others because of mental illness.1 But taking this step can be tough. Deciding to hospitalize a patient against her will involves weighing her wants and freedom against your duty to look out for her long-term welfare and the community’s safety.2,3 Often, psychiatrists make these decisions under pressure because the family wants something done immediately, other patients also need attention, the clinical picture is incomplete, or potential dispositions (eg, crisis care and inpatient beds) are limited.3 Given such constraints, you can’t always make perfect decisions.
Dr. R’s question has 2 parts:
- What liabilities can a clinician face if a patient is wrongfully committed?
- What liabilities could arise from relying on inaccurate information or making a false petition in order to hospitalize a patient?
We hope that as you and Dr. R read our answers, you’ll have a clearer understanding of:
- the rationale for civil commitment
- how patients, doctors, and courts view civil commitment
- the role of collateral information in decision-making
- relevant legal concepts and case law.
Rationale for civil commitment
For centuries, society has used civil commitment as one of its legal methods for intervening when persons pose a danger to themselves or others because of their mental illness.4 Because incapacitation or death could result from a “false-negative” decision to release a dangerous patient, psychiatrists err on the side of caution and tolerate many “false-positive” hospitalizations of persons who wouldn’t have hurt anyone.5
We can never know if a patient would have done harm had she not been hospitalized. Measures of suicidality and hostility tend to subside during involuntary hospital treatment.6 After hospitalization, many patients cite protection from harm as a reason they are thankful for their treatment.7-9 Some involuntary inpatients want to be hospitalized but hide this for conscious or unconscious reasons,10,11 and involuntary treatment sometimes is the only way to help persons whose illness-induced anosognosia12 prevents them from understanding why they need treatment.13 Involuntary inpatient care leads to modest symptom reduction14,15 and produces treatment outcomes no worse than those of non-coerced patients.10
Patients’ views
Patients often view commitment as unjustified.16 They and their advocates object to what some view as the ultimate infringement on civil liberty.7,17 By its nature, involuntary commitment eliminates patients’ involvement in a major treatment decision,8 disempowers them,18 and influences their relationship with the treatment team.15
Some involuntary patients feel disrespected by staff members8 or experience inadvertent psychological harm, including “loss of self-esteem, identity, self-control, and self-efficacy, as well as diminished hope in the possibility of recovery.”15 Involuntary hospitalization also can have serious practical consequences. Commitment can lead to social stigma, loss of gun rights, increased risks of losing child custody, housing problems, and possible disqualification from some professions.19
Having seen many involuntary patients undergo a change of heart after treatment, psychiatrist Alan Stone proposed the “Thank You Theory” of civil commitment: involuntary hospitalization can be justified by showing that the patient is grateful after recovering.20 Studies show, however, that gratitude is far from universal.1
How coercion is experienced often depends on how it is communicated. The less coercion patients perceive, the better they feel about the treatment they received.21 Satisfaction is important because it leads to less compulsory readmission,22 and dissatisfaction makes malpractice lawsuits more likely.23
Commitment decision-making
States’ laws, judges’ attitudes, and court decisions establish each jurisdiction’s legal methods for instituting emergency holds and willingness to tolerate “false-positive” involuntary hospitalization,4,24 all of which create variation between and within states in how civil commitment laws are applied. As a result, clinicians’ decisions are influenced “by a range of social, political, and economic factors,”25 including patients’ sex, race, age, homelessness, employment status, living situation, diagnoses, previous involuntary treatment, and dissatisfaction with mental health treatment.22,26-32 Furthermore, the potential for coercion often blurs the line between an offer of voluntary admission and an involuntary hospitalization.18
Collateral information
Psychiatrists owe each patient a sound clinical assessment before deciding to initiate involuntarily hospitalization. During a psychiatric crisis, a patient might not be forthcoming or could have impaired memory or judgment. Information from friends or family can help fill in gaps in a patient’s self-report.33 As Dr. R’s question illustrates, adequate assessment often includes seeking information from persons familiar with the patient.1 A report on the Virginia Tech shootings by the Virginia Office of the Inspector General describes how collateral sources can provide otherwise missing evidence of dangerousness,34 and it often leads clinicians toward favoring admission.35
Yet clinicians should regard third-party reports with caution.36 As one attorney warns, “Psychiatrists should be cautious of the underlying motives of well-meaning family members and relatives.”37 If you make a decision to hospitalize a patient involuntarily based on collateral information that turns out to be flawed, are you at fault and potentially liable for harm to the patient?
False petitions and liability
If you’re in a situation similar to the one Dr. R describes, you can take solace in knowing that courts generally provide immunity to a psychiatrist who makes a reasonable, well-intentioned decision to commit someone. The degree of immunity offered varies by jurisdiction. Table 1 provides examples of immunity language from several states’ statutes.
Many states’ statutes also lay out the potential consequences if a psychiatrist takes action to involuntarily hospitalize someone in bad faith or with malicious intent. In some jurisdictions, such actions can lead to criminal sanctions against the doctor or against the party who made a false petition (eg, a devious family member) (Table 2). Commenting on Texas’s statute, attorney Jeffrey Anderson explains, “The touchstone for causes of action based upon a wrongful civil commitment require that the psychiatrist[’s] conduct be found to be unreasonable and negligent. [Immunity…] still requires that a psychiatrist[’s] diagnosis of a patient[’s] threat to harm himself or others be a reasonable and prudent one.”37
The immunity extended through such statutes usually is limited to claims arising directly from the detention. For example, in the California case of Jacobs v Grossmont Hospital, a patient under a 72-hour hold fell and fractured her leg, and she sought damages. The trial court dismissed the suit under the immunity statute applicable to commitment decisions, but the appellate court held that “the immunity did not extend to other negligent acts.… The trial court erred in assuming that … the hospital was exempt from all liability for any negligence that occurred during the lawful hold.”38
Bingham v Cedars-Sinai Health Systems illustrates how physicians can lose immunity.39 A nurse contacted her supervisor to report a colleague who had stolen narcotics from work and compromised patient care. In response, the supervisor, hospital, and several physicians agreed to have her involuntarily committed. Later, it was confirmed that the colleague had taken the narcotics. She later sued the hospital system, claiming—in addition to malpractice—retaliation, invasion of privacy, assault and battery, false imprisonment, defamation, intentional infliction of emotional distress, disability-based harassment, and violation of her civil rights. Citing California’s immunity statute, the trial court granted summary judgment to the clinicians and hospital system. On appeal, however, the appellate court reversed the judgment, holding that the defendants had not shown that “the decision to detain Bingham was based on probable cause, a prerequisite to the exemption from liability,” and that Bingham had some legitimate grounds for her lawsuit.
A key point for Dr. R to consider is that, although some states provide immunity if the psychiatrist’s admitting decision was based on an evaluation “performed in good faith,”40 other states’ immunity provisions apply only if the psychiatrist had probable cause to make a decision to detain.41
Ways to reduce liability risk
Although an involuntary hospitalization could have an uncertain basis, psychiatrists can reduce the risk of legal liability for their decisions. Good documentation is important. Admitting psychiatrists usually make sound decisions, but the corresponding documentation frequently lacks clinical justification.42-44 As the rate of appropriate documentation of admission decision-making improves, the rate of commitment falls,44 and patients’ legal rights enjoy greater protection.43 Poor communication can decrease the quality of care and increase the risk of a malpractice lawsuit.45 This is just one of many reasons why you should explain your reasons for involuntary hospitalization and inform patients of the procedures for judicial review.8,9 Table 3 summarizes other steps to reduce liability risk when committing patients to the hospital.1,8,15,21,33,35-37,42,45-47
1. Pinals DA, Mossman D. Evaluation for civil commitment: best practices for forensic mental health assessments. New York, NY: Oxford University Press; 2011.
2. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgemont). 2010;7(10):30-40.
3. Hedman LC, Petrila J, Fisher WH, et al. State laws on emergency holds for mental health stabilization. Psychiatr Serv. 2016;67(5):529-535.
4. Groendyk Z. “It takes a lot to get into Bellevue”: a pro-rights critique of New York’s involuntary commitment law. Fordham Urban Law J. 2013;40(1):548-585.
5. Brooks RA. U.S. psychiatrists’ beliefs and wants about involuntary civil commitment grounds. Int J Law Psychiatry. 2006;29(1):13-21.
6. Giacco D, Priebe S. Suicidality and hostility following involuntary hospital treatment. PLoS One. 2016;11(5):e0154458. doi: 10.1371/journal.pone.0154458.
7. Wyder M, Bland R, Herriot A, et al. The experiences of the legal processes of involuntary treatment orders: tension between the legal and medical frameworks. Int J Law Psychiatry. 2015;38:44-50.
8. Valenti E, Giacco D, Katasakou C, et al. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics. 2014;40(12):832-836.
9. Katsakou C, Rose D, Amos T, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;42(7):1169-1179.
10. Kaltiala-Heino R, Laippala P, Salokangas RK. Impact of coercion on treatment outcome. Int J Law Psychiatry. 1997;20(3):311-322.
11. Hoge SK, Lidz CW, Eisenberg M, et al. Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiatry. 1997;20(2):167-181.
12. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):10-17. 13. Gordon S. The danger zone: how the dangerousness standard in civil commitment proceedings harms people with serious mental illness. Case Western Reserve Law Review. 2016;66(3):657-700.
14. Kallert TW, Katsakou C, Adamowski T, et al. Coerced hospital admission and symptom change—a prospective observational multi-centre study. PLoS One. 2011;6(11):e28191. doi: 10.1371/journal.pone.0028191.
15. Danzer G, Wilkus-Stone A. The give and take of freedom: the role of involuntary hospitalization and treatment in recovery from mental illness. Bull Menninger Clin. 2015;79(3):255-280.
16. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
17. Amidov T. Involuntary commitment is unnecessary and discriminatory. In: Berlatsky N, ed. Mental illness. Farmington Hills, MI: Greenhaven Press; 2016;140-145.
18. Monahan J, Hoge SK, Lidz C, et al. Coercion and commitment: understanding involuntary mental hospital admission. Int J Law Psychiatry. 1995;18(3):249-263.
19. Guest Pryal KR. Heller’s scapegoats. North Carolina Law Review. 2015;93(5):1439-1473.
20. Stone AA. Mental health and law: a system in transition. Washington, DC: U.S. Government Printing Office; 1975:75-176.
21. Katsakou C, Bowers L, Amos T, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286-292.
22. Setkowski K, van der Post LF, Peen J, et al. Changing patient perspectives after compulsory admission and the risk of re-admission during 5 years of follow-up: the Amsterdam study of acute psychiatry IX. Int J Soc Psychiatry. 2016;62(6):578-588.
23. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
24. Goldman A. Continued overreliance on involuntary commitment: the need for a less restrictive alternative. J Leg Med. 2015;36(2):233-251.
25. Fisher WH, Grisso T. Commentary: civil commitment statutes—40 years of circumvention. J Am Acad Psychiatry Law. 2010;38(3):365-368.
26. Curley A, Agada E, Emechebe A, et al. Exploring and explaining involuntary care: the relationship between psychiatric admission status, gender and other demographic and clinical variables. Int J Law Psychiatry. 2016;47:53-59.
27. Muroff JR, Jackson JS, Mowbray CT, et al. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry. 2007;29(6):481-488.
28. Muroff JR, Edelsohn GA, Joe S, et al. The role of race in diagnostic and disposition decision making in a pediatric psychiatric emergency service. Gen Hosp Psychiatry. 2008;30(3):269-276.
29. Unick GJ, Kessell E, Woodard EK, et al. Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. Gen Hosp Psychiatry. 2011;33(6):618-625.
30. Ng XT, Kelly BD. Voluntary and involuntary care: three-year study of demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatry. 2012;35(4):317-326.
31. Lo TT, Woo BK. The impact of unemployment on utilization of psychiatric emergency services. Gen Hosp Psychiatry. 2011;33(3):e7-e8. doi: 10.1016/j.genhosppsych.2010.10.010.
32. van der Post LFM, Peen J, Dekker JJ. A prediction model for the incidence of civil detention for crisis patients with psychiatric illnesses; the Amsterdam study of acute psychiatry VII. Soc Psychiatry Psychiatr Epidemiol. 2014;49(2):283-290.
33. Heilbrun K, NeMoyer A, King C, et al. Using third-party information in forensic mental health assessment: a critical review. Court Review. 2015;51(1):16-35.
34. Mass shootings at Virginia Tech, April 16, 2007 report of the Virginia Tech Review Panel presented to Timothy M. Kaine, Governor, Commonwealth of Virginia. http://cdm16064.contentdm.oclc.org/cdm/ref/collection/p266901coll4/id/904. Accessed February 2, 2017.
35. Segal SP, Laurie TA, Segal MJ. Factors in the use of coercive retention in civil commitment evaluations in psychiatric emergency services. Psychiatr Serv. 2001;52(4):514-520.
36. Lincoln A, Allen MH. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
37. Anderson JC. How I decided to sue you: misadventures in psychiatry. Reprinted in part from: Moody CE, Smith MT, Maedgen BJ. Litigation of psychiatric malpractice claims. Presented at: Medical Malpractice Conference; April 15, 1993; San Antonio, TX. http://www.texaslawfirm.com/Articles/How_I_Decided_to_Sue_You__Misadventrues_in_Psychiatry.pdf. Accessed December 27, 2016.
38. Jacobs v Grossmont Hospital, 108 Cal App 4th 69, 133 Cal Rptr 2d9 (2003).
39. Bingham v Cedars Sinai Health Systems, WL 2137442, Cal App 2 Dist (2004).
40. Ohio Revised Code §5122.34.
41. California Welfare & Institutions Code §5150(E).
42. Hashmi A, Shad M, Rhoades HM, et al. Involuntary detention: do psychiatrists clinically justify continuing involuntary hospitalization? Psychiatr Q. 2014;85(3):285-293.
43. Brayley J, Alston A, Rogers K. Legal criteria for involuntary mental health admission: clinician performance in recording grounds for decision. Med J Aust. 2015;203(8):334.
44. Perrigo TL, Williams KA. Implementation of an evidence based guideline for assessment and documentation of the civil commitment process. Community Ment Health J. 2016;52(8):1033-1036.
45. Mor S, Rabinovich-Einy O. Relational malpractice. Seton Hall Law Rev. 2012;42(2):601-642.
46. Tate v Kaiser Foundation Hospitals, WL 176625, U.S. Dist. LEXIS 5891 (CD Cal 2014).
47. Ranieri V, Madigan K, Roche E, et al. Caregivers’ perceptions of coercion in psychiatric hospital admission. Psychiatry Res. 2015;22(3)8:380-385.
1. Pinals DA, Mossman D. Evaluation for civil commitment: best practices for forensic mental health assessments. New York, NY: Oxford University Press; 2011.
2. Testa M, West SG. Civil commitment in the United States. Psychiatry (Edgemont). 2010;7(10):30-40.
3. Hedman LC, Petrila J, Fisher WH, et al. State laws on emergency holds for mental health stabilization. Psychiatr Serv. 2016;67(5):529-535.
4. Groendyk Z. “It takes a lot to get into Bellevue”: a pro-rights critique of New York’s involuntary commitment law. Fordham Urban Law J. 2013;40(1):548-585.
5. Brooks RA. U.S. psychiatrists’ beliefs and wants about involuntary civil commitment grounds. Int J Law Psychiatry. 2006;29(1):13-21.
6. Giacco D, Priebe S. Suicidality and hostility following involuntary hospital treatment. PLoS One. 2016;11(5):e0154458. doi: 10.1371/journal.pone.0154458.
7. Wyder M, Bland R, Herriot A, et al. The experiences of the legal processes of involuntary treatment orders: tension between the legal and medical frameworks. Int J Law Psychiatry. 2015;38:44-50.
8. Valenti E, Giacco D, Katasakou C, et al. Which values are important for patients during involuntary treatment? A qualitative study with psychiatric inpatients. J Med Ethics. 2014;40(12):832-836.
9. Katsakou C, Rose D, Amos T, et al. Psychiatric patients’ views on why their involuntary hospitalisation was right or wrong: a qualitative study. Soc Psychiatry Psychiatr Epidemiol. 2012;42(7):1169-1179.
10. Kaltiala-Heino R, Laippala P, Salokangas RK. Impact of coercion on treatment outcome. Int J Law Psychiatry. 1997;20(3):311-322.
11. Hoge SK, Lidz CW, Eisenberg M, et al. Perceptions of coercion in the admission of voluntary and involuntary psychiatric patients. Int J Law Psychiatry. 1997;20(2):167-181.
12. Lehrer DS, Lorenz J. Anosognosia in schizophrenia: hidden in plain sight. Innov Clin Neurosci. 2014;11(5-6):10-17. 13. Gordon S. The danger zone: how the dangerousness standard in civil commitment proceedings harms people with serious mental illness. Case Western Reserve Law Review. 2016;66(3):657-700.
14. Kallert TW, Katsakou C, Adamowski T, et al. Coerced hospital admission and symptom change—a prospective observational multi-centre study. PLoS One. 2011;6(11):e28191. doi: 10.1371/journal.pone.0028191.
15. Danzer G, Wilkus-Stone A. The give and take of freedom: the role of involuntary hospitalization and treatment in recovery from mental illness. Bull Menninger Clin. 2015;79(3):255-280.
16. Roe D, Weishut DJ, Jaglom M, et al. Patients’ and staff members’ attitudes about the rights of hospitalized psychiatric patients. Psychiatr Serv. 2002;53(1):87-91.
17. Amidov T. Involuntary commitment is unnecessary and discriminatory. In: Berlatsky N, ed. Mental illness. Farmington Hills, MI: Greenhaven Press; 2016;140-145.
18. Monahan J, Hoge SK, Lidz C, et al. Coercion and commitment: understanding involuntary mental hospital admission. Int J Law Psychiatry. 1995;18(3):249-263.
19. Guest Pryal KR. Heller’s scapegoats. North Carolina Law Review. 2015;93(5):1439-1473.
20. Stone AA. Mental health and law: a system in transition. Washington, DC: U.S. Government Printing Office; 1975:75-176.
21. Katsakou C, Bowers L, Amos T, et al. Coercion and treatment satisfaction among involuntary patients. Psychiatr Serv. 2010;61(3):286-292.
22. Setkowski K, van der Post LF, Peen J, et al. Changing patient perspectives after compulsory admission and the risk of re-admission during 5 years of follow-up: the Amsterdam study of acute psychiatry IX. Int J Soc Psychiatry. 2016;62(6):578-588.
23. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):1126-1133.
24. Goldman A. Continued overreliance on involuntary commitment: the need for a less restrictive alternative. J Leg Med. 2015;36(2):233-251.
25. Fisher WH, Grisso T. Commentary: civil commitment statutes—40 years of circumvention. J Am Acad Psychiatry Law. 2010;38(3):365-368.
26. Curley A, Agada E, Emechebe A, et al. Exploring and explaining involuntary care: the relationship between psychiatric admission status, gender and other demographic and clinical variables. Int J Law Psychiatry. 2016;47:53-59.
27. Muroff JR, Jackson JS, Mowbray CT, et al. The influence of gender, patient volume and time on clinical diagnostic decision making in psychiatric emergency services. Gen Hosp Psychiatry. 2007;29(6):481-488.
28. Muroff JR, Edelsohn GA, Joe S, et al. The role of race in diagnostic and disposition decision making in a pediatric psychiatric emergency service. Gen Hosp Psychiatry. 2008;30(3):269-276.
29. Unick GJ, Kessell E, Woodard EK, et al. Factors affecting psychiatric inpatient hospitalization from a psychiatric emergency service. Gen Hosp Psychiatry. 2011;33(6):618-625.
30. Ng XT, Kelly BD. Voluntary and involuntary care: three-year study of demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatry. 2012;35(4):317-326.
31. Lo TT, Woo BK. The impact of unemployment on utilization of psychiatric emergency services. Gen Hosp Psychiatry. 2011;33(3):e7-e8. doi: 10.1016/j.genhosppsych.2010.10.010.
32. van der Post LFM, Peen J, Dekker JJ. A prediction model for the incidence of civil detention for crisis patients with psychiatric illnesses; the Amsterdam study of acute psychiatry VII. Soc Psychiatry Psychiatr Epidemiol. 2014;49(2):283-290.
33. Heilbrun K, NeMoyer A, King C, et al. Using third-party information in forensic mental health assessment: a critical review. Court Review. 2015;51(1):16-35.
34. Mass shootings at Virginia Tech, April 16, 2007 report of the Virginia Tech Review Panel presented to Timothy M. Kaine, Governor, Commonwealth of Virginia. http://cdm16064.contentdm.oclc.org/cdm/ref/collection/p266901coll4/id/904. Accessed February 2, 2017.
35. Segal SP, Laurie TA, Segal MJ. Factors in the use of coercive retention in civil commitment evaluations in psychiatric emergency services. Psychiatr Serv. 2001;52(4):514-520.
36. Lincoln A, Allen MH. The influence of collateral information on access to inpatient psychiatric services. International Journal of Psychosocial Rehabilitation. 2002;6:99-108.
37. Anderson JC. How I decided to sue you: misadventures in psychiatry. Reprinted in part from: Moody CE, Smith MT, Maedgen BJ. Litigation of psychiatric malpractice claims. Presented at: Medical Malpractice Conference; April 15, 1993; San Antonio, TX. http://www.texaslawfirm.com/Articles/How_I_Decided_to_Sue_You__Misadventrues_in_Psychiatry.pdf. Accessed December 27, 2016.
38. Jacobs v Grossmont Hospital, 108 Cal App 4th 69, 133 Cal Rptr 2d9 (2003).
39. Bingham v Cedars Sinai Health Systems, WL 2137442, Cal App 2 Dist (2004).
40. Ohio Revised Code §5122.34.
41. California Welfare & Institutions Code §5150(E).
42. Hashmi A, Shad M, Rhoades HM, et al. Involuntary detention: do psychiatrists clinically justify continuing involuntary hospitalization? Psychiatr Q. 2014;85(3):285-293.
43. Brayley J, Alston A, Rogers K. Legal criteria for involuntary mental health admission: clinician performance in recording grounds for decision. Med J Aust. 2015;203(8):334.
44. Perrigo TL, Williams KA. Implementation of an evidence based guideline for assessment and documentation of the civil commitment process. Community Ment Health J. 2016;52(8):1033-1036.
45. Mor S, Rabinovich-Einy O. Relational malpractice. Seton Hall Law Rev. 2012;42(2):601-642.
46. Tate v Kaiser Foundation Hospitals, WL 176625, U.S. Dist. LEXIS 5891 (CD Cal 2014).
47. Ranieri V, Madigan K, Roche E, et al. Caregivers’ perceptions of coercion in psychiatric hospital admission. Psychiatry Res. 2015;22(3)8:380-385.
We can work it out: Should I hire my patient?
Dear Dr. Mossman,
Each month, I see my patient, Mr. R, for a 15-minute medication management appointment. At his latest visit, Mr. R mentioned his financial difficulties. He also observed that our office needed to have some carpentry work done—not a surprise, because he’s known in our area as one of the best carpenters around. He suggested that I hire him as payment for the next 6 appointments. What risks might I encounter if I oblige him?
Submitted by “Dr. Z”
Nearly 29 million Americans are uninsured,1 and even more have trouble accessing mental health care.2 Many psychiatrists struggle to provide affordable services while remaining financially viable.3,4 For outpatients with limited means to pay for care, spacing appointments to fit their budgets might compromise treatment.5 Simply not charging patients poses its own clinical and ethical challenges.6-8
As a result, some mental health professionals make barter arrangements to help their patients enter or continue treatment. To answer Dr. Z’s question on whether exchanging services might be a way to arrange matters with some patients, we explore:
- the idea of bartering for psychiatric treatment
- related ethical and legal considerations
- when and in what situations bartering might be appropriate.
Think of what I’m saying: Bartering for treatment
“Barter” refers to exchanging commodities, products, or services of equivalent value without using money.9 In 2010, Nevada Republican Senate candidate Sue Lowden encouraged barter for health care and harkened back to an earlier time where “they would bring a chicken to the doctor; they would say ‘I’ll paint your house.’”10
Such payment arrangements have been encouraged as health care has become increasingly commoditized.11-13 This happens through both direct barter between physician and patient and barter exchanges. Barter exchange systems have been set up on Web sites (as of 2013, at least 400 such online exchanges were available14), local communities,11,15 and social programs. For example, through the “Swapping Guns for Therapy” program, psychologists in California gave free or reduced-fee care for people who traded in their guns.16
Try to see it my way: A prevailing view of barter
Several psychiatrists recommend against bartering for treatment, for a variety of reasons.7,8,17-19 Simon18 argues that a stable fee policy is part of a proper therapeutic framework, and money is “the only acceptable medium of exchange when receiving payment from patients.” Emotional distress and the power differential inherent in treatment might prevent a patient from making an accurate assessment of the value of the bartered goods or services,7,8,17,18,20 which could lead to future claims of undue influence from trading goods or services below market value.17 To avoid the possibility of exploitating the patient, Simon18 recommends that the psychiatrist’s professional fee be “the only material benefit received from the patient.”
The American Psychiatric Association’s code of ethics states that “it is not ethical to switch a doctor–patient relationship to an employer–employee one … and, in most cases, such an arrangement would be unethical.”21 In some therapeutic settings, employing a patient risks inappropriate self-disclosure and intrusion.16
More than other physicians, psychiatrists pay special attention to professional boundaries, the technical term for the “edge of appropriate behavior,” within which safe, effective care can occur.22,23 Although some boundary crossings can be harmless and even constructive, repeated boundary crossings are the forerunners to improper behavior, including sexual relationships with patients.24-26
Out of concern that bartering could become the first step down a slippery ethical slope toward patient exploitation, mental health clinicians have deemed the practice “ethically troubling,”19 said it did “not usually work out well,”7 and declared it “so fraught with risks for both parties that it seem[ed] illogical to even consider it as an option.”27
While I see it your way: What barter proponents say
Reports of bartering for chickens28 and purchasing fuel from a patient in remote Alaska29 show that not all physicians agree and why they feel that professional codes of ethics reflect an urban bias.28,29 In many rural areas and small towns, access to mental health services is limited, and patients often interact with their doctors outside of clinical encounters.23,29-31
Bartering can benefit a physician’s practice by:
- reducing the need to discount services
- eliminating bureaucratic burdens of traditional insurance arrangements
- facilitating development of a patient base
- allowing patients choice and flexibility in seeking medical care.6,16,32
Bartering could confer certain clinical benefits, such as:
- enhancing trust and empathy32
- encouraging patients to make their needs known constructively6
- modeling financial self-care6
- helping the doctor to feel fairly compensated for providing thoughtful care6
- acknowledging the patient’s cultural values15,33
- affirming that patients and doctors both produce things of value.16
I have always thought: Other ethical models
An ethical approach to bartering that requires careful thought and respect for the patient’s needs appears consistent with a primary goal of treatment: “to increase the capacity of individuals to make more rational choices in their lives and to be relatively freer from disabling conflicts.”20 Some authors criticize slippery-slope arguments and strict-rule ethical approaches as being too rigid, limiting, or risk-averse.22,26,34 In Table 1,6,8,16,18,27,29-31,35-37 we list several factors that might weigh for or against a decision to enter into a barter arrangement as payment for care.
In a similar manner, Martinez33,38 proposed a graded-risk framework that encourages examination of potential harms and benefits of a decision, potential coercive or exploitative elements, the clinician’s intentions and aspiration to professional ideals, and the context of the decision. Within this framework, some bartering arrangements might be encouraged and, perhaps, even obligatory because of the potential benefits to the patient; other arrangements (eg, trading psychotherapy for menial services) might be unjustifiable. Martinez38 argues that this approach fosters mutual decision-making with patients, discourages physician paternalism, and “demands that we struggle with the particulars with each case.”
Gottlieb’s decision-making model35 recognizes that trying to avoid all dual relationships is unrealistic and not all dual relationships are exploitative. Instead, a clinician must assess 3 dimensions of current and proposed relationships:
- the degree of power differential
- the duration of treatment
- the clarity of termination.
The decision-making process also requires involvement of the patient, who if “unable to recognize the dilemma or is unwilling to consider the issues before deciding, should be considered at risk, and the contemplated relationship rejected.”35
So I will ask you once again: Dr. Z’s decision
In the case of Dr. Z and Mr. R, a barter arrangement might work in the sense of permitting and sustaining good care. Mr. R suggested the idea and might not be able to afford care without it. Nothing in Dr. Z’s description suggests that Mr. R has personality characteristics or other conditions that would compromise his ability to give informed consent or to understand the nuances of a barter arrangement. Dr. Z is not providing a treatment (eg, psychodynamic therapy) that a barter arrangement could contaminate. That the arrangement would be circumscribed limits the effect of a power differential, as would its brief duration and defined termination endpoint. Dr. Z’s letter to the authors also shows his willingness to seek consultation.
There’s a chance that we may fall apart: Reasons for caution
Martinez’s graded-risk approach recognizes reasons for caution:
- the risk of harm to the patient or doctor–patient relationship
- the uncertain benefit to the patient
- the blurring of Dr. Z’s self-interest and Mr. R’s needs
- some ambiguity about possible exploitation.
Dr. Z and Mr. R have not discussed the value of Mr. R’s work—which might create a rift between them—and despite Mr. R’s reputation, other carpenters are available. Future med-check appointments will give them little time to explore and discuss the meanings of the barter.
Any proposed barter arrangement creates some clinical perils that can be particularly salient in mental health treatment. Patients could view themselves as “special” or entitled to enhanced access to the doctor because of exchanged services, which could take a toll on the doctor.39 The physician’s objectivity might diminish, and the business aspect of their relationship could make both parties less comfortable when discussing sensitive information relevant to treatment.31,40 Also, the suggested barter is for services to be provided at Dr. Z’s office, where confidentiality may be breeched and transference issues could arise.
A medical malpractice claim states that a doctor has breached a duty of care to a patient such that harm (or “damages”) resulted.41 Should Dr. Z and Mr. R’s barter agreement turn sour and harm follow, Mr. R could sue for recovery of damages based of a claim of duress, undue influence, or other aspects of the doctor–patient power differential.27,42,43 Given the published views we have described, a psychiatrist who barters also may be viewed as violating state regulations that measure the standard of care against generally accepted practice.
Only time will tell if I am right or I am wrong
If you face a situation similar to Dr. Z’s and want to consider a barter arrangement, you can take several steps to mitigate potential risk to your patient and ensure competent care (Table 25,6,15,16,32,35,39,40,44-47). One of the most important steps is to seek ongoing consultation, both before and after a decision to barter. Ideally, the consulting colleague would know you and your circumstances and would have sufficient clinical grasp of the patient to make an informed assessment of risks and benefits.35 This consultation, as well as your own rationale for acting on recommendations, should be thoroughly documented in the patient’s records.26,44,45
Certain types of barter should be off limits, including:
- trading prescription drugs for goods or services
- trading for services that tie into the success of one’s business (eg, business advising or marketing)16
- offering treatment in exchange for illegal or ethically unacceptable services.48
Beyond ethical considerations are some practical issues. The Internal Revenue Service has specific rules regarding taxation of bartered goods and services, which must be included as taxable income.46 If possible, an independent agent should appraise the traded goods or services before the agreement.6 When working in a group practice, the clinician might have to figure out how to allocate the received goods or services such as shared overhead costs.28 Preferably, the patient’s goods or services should be provided before care is delivered.16 If not, the duration of services rendered should be limited, and either party should have the option to disengage from the relationship if one feels dissatisfied.16
A written contract, discussed ahead of time, can be a sound way to summarize the terms of the arrangement. Both sides also should consider what would happen if an injury occurred.16 Finally, you must adhere to any relevant state laws regarding payment for services, particularly if the patient has health insurance.32
If the bartering arrangement does not work, you should take an open and non-defensive approach. If you believe you have made a mistake, consider apologizing.45
1. Kaiser Commission on Medicaid and the Uninsured. Key facts about the uninsured population. http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population. Published September 29, 2016. Accessed October 7, 2016.
2. National Alliance on Mental Illness. A long road ahead: achieving true parity in mental health and substance use care. https://www.nami.org/About-NAMI/Publications-Reports/Public-Policy-Reports/A-Long-Road-Ahead/2015-ALongRoadAhead.pdf. Published April 2015. Accessed October 7, 2016.
3. Insel T. Director’s blog: the paradox of parity. May 30, 2014. https://www.nimh.nih.gov/about/director/2014/the-paradox-of-parity.shtml. Published May 30, 2014. Accessed October 7, 2016.
4. Bishop TF, Press MJ, Keyhani S, et al. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181.
5. What do you do when patients cannot pay? Psychiatry (Edgmont). 2009;6(5):51-52.
6. Hill M. Barter: ethical considerations in psychotherapy. Women Ther. 2000;22(3):81-91.
7. Simon RI. Commentary: treatment boundaries—flexible guidelines, not rigid standards. J Am Acad Psychiatry Law. 2001;29(3):287-289.
8. Simon RI, Williams IC. Maintaining treatment boundaries in small communities and rural areas. Psychiatr Serv. 1999;50(11):1440-1446.
9. Compact edition of the Oxford English dictionary. New York, NY: Oxford University Press; 1971:171.
10. Coolican JP. Sue Lowden stands by health care plan. Las Vegas Sun. http://lasvegassun.com/news/2010/apr/20/sue-lowden-draws-fire-repeating-health-care-barter. Published April 20, 2010. Accessed September 20, 2016.
11. Consumer Reports. Barter sometimes allow patients to pay for health care they otherwise could not afford. Washington Post. https://www.washingtonpost.com/national/health-science/barter-sometimes-allow-patients-to-pay-for-health-care-they-otherwise-could-not-afford/2013/09/30/e7e5a55e-069d-11e3-88d6-d5795fab4637_story.html. Published September 20, 2013. Accessed September 27, 2016.
12. Ellis B. MediBid auction site lets doctors bid for patients. CNN Money. http://money.cnn.com/2014/01/09/pf/insurance/medibid. Published January 9, 2014. Accessed September 23, 2016.
13. Ambrosino B. Surgery for sale: the ethics of health care bartering in a social media marketplace. http://hub.jhu.edu/2014/01/16/hopkins-ethicist-ponders-medibid. Published January 16, 2014. Accessed September 23, 2016.
14. Thomas C. When patients barter for health care. https://ethicalnag.org/2013/07/30/barter. Published July 30, 2016. Accessed October 9, 2016.
15. Syme G. Fetters or freedom: dual relationships in counselling. Int J Adv Counselling. 2006;28(1):57-69.
16. Zur O. Bartering in psychotherapy and counselling: complexities, case studies and guidelines. New Therapist. 2008;58:18-26.
17. Simon RI. The psychiatrist as a fiduciary: avoiding the double agent role. Psychiatric Annals. 1987;17(9):622-626.
18. Simon RI. Treatment boundary violations: clinical, ethical, and legal considerations. Bull Am Acad Psychiatry Law. 1992;20(3):269-288.
19. Walker R, Clark JJ. Heading off boundary problems: clinical supervision as risk management. Psychiatr Serv. 1999;50(11):1435-1439.
20. Malmquist CP, Norman MT. Psychiatrist-patient boundary issues following treatment termination. Am J Psychiatry. 2001;158(7):1010-1018.
21. American Psychiatric Association. The opinions of the ethics committee on the principles of medical ethics, with annotations especially applicable to psychiatry. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2016. Accessed October 4, 2016.
22. Gutheil TG, Gabbard GO. Misuses and misunderstandings of boundary theory in clinical and regulatory settings. Am J Psychiatry. 1998;155(3):409-414.
23. Crowden A. Professional boundaries and the ethics of dual and multiple overlapping relationships in psychotherapy. Monash Bioeth Rev. 2008;27(4):10-27.
24. Gabbard GO. Commentary: boundaries, culture, and psychotherapy. J Am Acad Psychiatry Law. 2001;29(3):284-286.
25. Kroll J. Boundary violations: a culture-bound syndrome. J Am Acad Psychiatry Law. 2001;29(3):274-283.
26. Gottlieb MC, Younggren JN. Is there a slippery slope? Considerations regarding multiple relationships and risk management. Professional Psychology: Research and Practice. 2009;40(6):564-557.
27. Woody RH. Bartering for psychological services. Professional Psychology: Research and Practice. 1998;29(2):174-178.
28. Bartering for medical care. MGMA Connex. 2008;8(6):11.
29. Roberts LW, Battaglia J, Epstein RS. Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatr Serv. 1994;50(4):497-503.
30. Endacott R, Wood A, Judd F, et al. Impact and management of dual relationships in metropolitan, regional and rural mental health practice. Aust N Z J Psychiatry. 2006;40(11-12):987-994.
31. Scopelliti J, Judd F, Grigg M, et al. Dual relationships in mental health practice: issues for clinicians in rural settings. Aust N Z J Psychiatry. 2004;38(11-12):953-959.
32. Ayers AA. Bartering basics for the urgent care operator. http://www.alanayersurgentcare.com/Linked_Files/2013_Articles/Ayers_UCAOA_Bartering_%20Basics_2012_01_09.pdf. Accessed September 23, 2016.
33. Savin D, Martinez R. Cross-cultural boundary dilemmas: a graded-risk assessment approach. Transcult Psychiatry. 2006;42(2):243-258.
34. Glass LL. The gray areas of boundary crossings and violations. Am J Psychother. 2003;57(4):429-444.
35. Gottlieb MC. Avoiding exploitive dual relationships: a decision-making model. Psychotherapy (Chic). 1993;30(1):41-48.
36. Lane JA. The ethical implications of bartering for mental health services: examining interdisciplinary ethical standards. http://pdxscholar.library.pdx.edu/coun_fac/36. Published 2012. Accessed October 17, 2016.
37. Miller RD, Maier GJ. Nonsexual boundary violations: sauce for the gander. J Psychiatry Law. 2002;30(3):309-329.
38. Martinez R. A model for boundary dilemmas: ethical decision-making in the patient-professional relationship. Ethical Hum Sci Serv. 2000;2(1):43-61.
39. Salmon K, Klijnsma M. Boundary issues: employing patients as staff? Br J Gen Pract. 2009;59(558):56-57.
40. College of Physicians and Surgeons Ontario. Hiring patients may compromise physician-patient relationship. Dialogue. 2015;3:47.
41. Bal S. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467(2):339-347.
42. What puts a psychiatrist at risk for a malpractice lawsuit? Psychiatry (Edgmont). 2009;6(8):38-39.
43. Geis v Landau, 117 Misc2d 396 (NY Misc 1983).
44. Nisselle P. Danger zone. When boundaries are crossed in the doctor-patient relationship. Aust Fam Physician. 2000;29(6):541-544.
45. Pope KS, Keith-Spiegel P. A practical approach to boundaries in psychotherapy: making decisions, bypassing blunders, and mending fences. J Clin Psychol. 2008;64(5):638-652.
46. IRS Publication 17. https://www.irs.gov/publications/p17/ch12.html. Published 2015. Accessed October 5, 2016.
47. Epstein RS, Simon RI. The exploitation index: an early warning indicator of boundary violations in psychotherapy. Bull Menninger Clin. 1990;54(4):450-465.
48. Skutch J. Savannah doctor accused of trading drugs for sex with strippers. Augusta Chronicle. http://chronicle.augusta.com/news/crime-courts/2013-01-31/savannah-doctor-accused-trading-drugs-sex-strippers. Published January 31, 2013. Accessed October 16, 2016.
Dear Dr. Mossman,
Each month, I see my patient, Mr. R, for a 15-minute medication management appointment. At his latest visit, Mr. R mentioned his financial difficulties. He also observed that our office needed to have some carpentry work done—not a surprise, because he’s known in our area as one of the best carpenters around. He suggested that I hire him as payment for the next 6 appointments. What risks might I encounter if I oblige him?
Submitted by “Dr. Z”
Nearly 29 million Americans are uninsured,1 and even more have trouble accessing mental health care.2 Many psychiatrists struggle to provide affordable services while remaining financially viable.3,4 For outpatients with limited means to pay for care, spacing appointments to fit their budgets might compromise treatment.5 Simply not charging patients poses its own clinical and ethical challenges.6-8
As a result, some mental health professionals make barter arrangements to help their patients enter or continue treatment. To answer Dr. Z’s question on whether exchanging services might be a way to arrange matters with some patients, we explore:
- the idea of bartering for psychiatric treatment
- related ethical and legal considerations
- when and in what situations bartering might be appropriate.
Think of what I’m saying: Bartering for treatment
“Barter” refers to exchanging commodities, products, or services of equivalent value without using money.9 In 2010, Nevada Republican Senate candidate Sue Lowden encouraged barter for health care and harkened back to an earlier time where “they would bring a chicken to the doctor; they would say ‘I’ll paint your house.’”10
Such payment arrangements have been encouraged as health care has become increasingly commoditized.11-13 This happens through both direct barter between physician and patient and barter exchanges. Barter exchange systems have been set up on Web sites (as of 2013, at least 400 such online exchanges were available14), local communities,11,15 and social programs. For example, through the “Swapping Guns for Therapy” program, psychologists in California gave free or reduced-fee care for people who traded in their guns.16
Try to see it my way: A prevailing view of barter
Several psychiatrists recommend against bartering for treatment, for a variety of reasons.7,8,17-19 Simon18 argues that a stable fee policy is part of a proper therapeutic framework, and money is “the only acceptable medium of exchange when receiving payment from patients.” Emotional distress and the power differential inherent in treatment might prevent a patient from making an accurate assessment of the value of the bartered goods or services,7,8,17,18,20 which could lead to future claims of undue influence from trading goods or services below market value.17 To avoid the possibility of exploitating the patient, Simon18 recommends that the psychiatrist’s professional fee be “the only material benefit received from the patient.”
The American Psychiatric Association’s code of ethics states that “it is not ethical to switch a doctor–patient relationship to an employer–employee one … and, in most cases, such an arrangement would be unethical.”21 In some therapeutic settings, employing a patient risks inappropriate self-disclosure and intrusion.16
More than other physicians, psychiatrists pay special attention to professional boundaries, the technical term for the “edge of appropriate behavior,” within which safe, effective care can occur.22,23 Although some boundary crossings can be harmless and even constructive, repeated boundary crossings are the forerunners to improper behavior, including sexual relationships with patients.24-26
Out of concern that bartering could become the first step down a slippery ethical slope toward patient exploitation, mental health clinicians have deemed the practice “ethically troubling,”19 said it did “not usually work out well,”7 and declared it “so fraught with risks for both parties that it seem[ed] illogical to even consider it as an option.”27
While I see it your way: What barter proponents say
Reports of bartering for chickens28 and purchasing fuel from a patient in remote Alaska29 show that not all physicians agree and why they feel that professional codes of ethics reflect an urban bias.28,29 In many rural areas and small towns, access to mental health services is limited, and patients often interact with their doctors outside of clinical encounters.23,29-31
Bartering can benefit a physician’s practice by:
- reducing the need to discount services
- eliminating bureaucratic burdens of traditional insurance arrangements
- facilitating development of a patient base
- allowing patients choice and flexibility in seeking medical care.6,16,32
Bartering could confer certain clinical benefits, such as:
- enhancing trust and empathy32
- encouraging patients to make their needs known constructively6
- modeling financial self-care6
- helping the doctor to feel fairly compensated for providing thoughtful care6
- acknowledging the patient’s cultural values15,33
- affirming that patients and doctors both produce things of value.16
I have always thought: Other ethical models
An ethical approach to bartering that requires careful thought and respect for the patient’s needs appears consistent with a primary goal of treatment: “to increase the capacity of individuals to make more rational choices in their lives and to be relatively freer from disabling conflicts.”20 Some authors criticize slippery-slope arguments and strict-rule ethical approaches as being too rigid, limiting, or risk-averse.22,26,34 In Table 1,6,8,16,18,27,29-31,35-37 we list several factors that might weigh for or against a decision to enter into a barter arrangement as payment for care.
In a similar manner, Martinez33,38 proposed a graded-risk framework that encourages examination of potential harms and benefits of a decision, potential coercive or exploitative elements, the clinician’s intentions and aspiration to professional ideals, and the context of the decision. Within this framework, some bartering arrangements might be encouraged and, perhaps, even obligatory because of the potential benefits to the patient; other arrangements (eg, trading psychotherapy for menial services) might be unjustifiable. Martinez38 argues that this approach fosters mutual decision-making with patients, discourages physician paternalism, and “demands that we struggle with the particulars with each case.”
Gottlieb’s decision-making model35 recognizes that trying to avoid all dual relationships is unrealistic and not all dual relationships are exploitative. Instead, a clinician must assess 3 dimensions of current and proposed relationships:
- the degree of power differential
- the duration of treatment
- the clarity of termination.
The decision-making process also requires involvement of the patient, who if “unable to recognize the dilemma or is unwilling to consider the issues before deciding, should be considered at risk, and the contemplated relationship rejected.”35
So I will ask you once again: Dr. Z’s decision
In the case of Dr. Z and Mr. R, a barter arrangement might work in the sense of permitting and sustaining good care. Mr. R suggested the idea and might not be able to afford care without it. Nothing in Dr. Z’s description suggests that Mr. R has personality characteristics or other conditions that would compromise his ability to give informed consent or to understand the nuances of a barter arrangement. Dr. Z is not providing a treatment (eg, psychodynamic therapy) that a barter arrangement could contaminate. That the arrangement would be circumscribed limits the effect of a power differential, as would its brief duration and defined termination endpoint. Dr. Z’s letter to the authors also shows his willingness to seek consultation.
There’s a chance that we may fall apart: Reasons for caution
Martinez’s graded-risk approach recognizes reasons for caution:
- the risk of harm to the patient or doctor–patient relationship
- the uncertain benefit to the patient
- the blurring of Dr. Z’s self-interest and Mr. R’s needs
- some ambiguity about possible exploitation.
Dr. Z and Mr. R have not discussed the value of Mr. R’s work—which might create a rift between them—and despite Mr. R’s reputation, other carpenters are available. Future med-check appointments will give them little time to explore and discuss the meanings of the barter.
Any proposed barter arrangement creates some clinical perils that can be particularly salient in mental health treatment. Patients could view themselves as “special” or entitled to enhanced access to the doctor because of exchanged services, which could take a toll on the doctor.39 The physician’s objectivity might diminish, and the business aspect of their relationship could make both parties less comfortable when discussing sensitive information relevant to treatment.31,40 Also, the suggested barter is for services to be provided at Dr. Z’s office, where confidentiality may be breeched and transference issues could arise.
A medical malpractice claim states that a doctor has breached a duty of care to a patient such that harm (or “damages”) resulted.41 Should Dr. Z and Mr. R’s barter agreement turn sour and harm follow, Mr. R could sue for recovery of damages based of a claim of duress, undue influence, or other aspects of the doctor–patient power differential.27,42,43 Given the published views we have described, a psychiatrist who barters also may be viewed as violating state regulations that measure the standard of care against generally accepted practice.
Only time will tell if I am right or I am wrong
If you face a situation similar to Dr. Z’s and want to consider a barter arrangement, you can take several steps to mitigate potential risk to your patient and ensure competent care (Table 25,6,15,16,32,35,39,40,44-47). One of the most important steps is to seek ongoing consultation, both before and after a decision to barter. Ideally, the consulting colleague would know you and your circumstances and would have sufficient clinical grasp of the patient to make an informed assessment of risks and benefits.35 This consultation, as well as your own rationale for acting on recommendations, should be thoroughly documented in the patient’s records.26,44,45
Certain types of barter should be off limits, including:
- trading prescription drugs for goods or services
- trading for services that tie into the success of one’s business (eg, business advising or marketing)16
- offering treatment in exchange for illegal or ethically unacceptable services.48
Beyond ethical considerations are some practical issues. The Internal Revenue Service has specific rules regarding taxation of bartered goods and services, which must be included as taxable income.46 If possible, an independent agent should appraise the traded goods or services before the agreement.6 When working in a group practice, the clinician might have to figure out how to allocate the received goods or services such as shared overhead costs.28 Preferably, the patient’s goods or services should be provided before care is delivered.16 If not, the duration of services rendered should be limited, and either party should have the option to disengage from the relationship if one feels dissatisfied.16
A written contract, discussed ahead of time, can be a sound way to summarize the terms of the arrangement. Both sides also should consider what would happen if an injury occurred.16 Finally, you must adhere to any relevant state laws regarding payment for services, particularly if the patient has health insurance.32
If the bartering arrangement does not work, you should take an open and non-defensive approach. If you believe you have made a mistake, consider apologizing.45
Dear Dr. Mossman,
Each month, I see my patient, Mr. R, for a 15-minute medication management appointment. At his latest visit, Mr. R mentioned his financial difficulties. He also observed that our office needed to have some carpentry work done—not a surprise, because he’s known in our area as one of the best carpenters around. He suggested that I hire him as payment for the next 6 appointments. What risks might I encounter if I oblige him?
Submitted by “Dr. Z”
Nearly 29 million Americans are uninsured,1 and even more have trouble accessing mental health care.2 Many psychiatrists struggle to provide affordable services while remaining financially viable.3,4 For outpatients with limited means to pay for care, spacing appointments to fit their budgets might compromise treatment.5 Simply not charging patients poses its own clinical and ethical challenges.6-8
As a result, some mental health professionals make barter arrangements to help their patients enter or continue treatment. To answer Dr. Z’s question on whether exchanging services might be a way to arrange matters with some patients, we explore:
- the idea of bartering for psychiatric treatment
- related ethical and legal considerations
- when and in what situations bartering might be appropriate.
Think of what I’m saying: Bartering for treatment
“Barter” refers to exchanging commodities, products, or services of equivalent value without using money.9 In 2010, Nevada Republican Senate candidate Sue Lowden encouraged barter for health care and harkened back to an earlier time where “they would bring a chicken to the doctor; they would say ‘I’ll paint your house.’”10
Such payment arrangements have been encouraged as health care has become increasingly commoditized.11-13 This happens through both direct barter between physician and patient and barter exchanges. Barter exchange systems have been set up on Web sites (as of 2013, at least 400 such online exchanges were available14), local communities,11,15 and social programs. For example, through the “Swapping Guns for Therapy” program, psychologists in California gave free or reduced-fee care for people who traded in their guns.16
Try to see it my way: A prevailing view of barter
Several psychiatrists recommend against bartering for treatment, for a variety of reasons.7,8,17-19 Simon18 argues that a stable fee policy is part of a proper therapeutic framework, and money is “the only acceptable medium of exchange when receiving payment from patients.” Emotional distress and the power differential inherent in treatment might prevent a patient from making an accurate assessment of the value of the bartered goods or services,7,8,17,18,20 which could lead to future claims of undue influence from trading goods or services below market value.17 To avoid the possibility of exploitating the patient, Simon18 recommends that the psychiatrist’s professional fee be “the only material benefit received from the patient.”
The American Psychiatric Association’s code of ethics states that “it is not ethical to switch a doctor–patient relationship to an employer–employee one … and, in most cases, such an arrangement would be unethical.”21 In some therapeutic settings, employing a patient risks inappropriate self-disclosure and intrusion.16
More than other physicians, psychiatrists pay special attention to professional boundaries, the technical term for the “edge of appropriate behavior,” within which safe, effective care can occur.22,23 Although some boundary crossings can be harmless and even constructive, repeated boundary crossings are the forerunners to improper behavior, including sexual relationships with patients.24-26
Out of concern that bartering could become the first step down a slippery ethical slope toward patient exploitation, mental health clinicians have deemed the practice “ethically troubling,”19 said it did “not usually work out well,”7 and declared it “so fraught with risks for both parties that it seem[ed] illogical to even consider it as an option.”27
While I see it your way: What barter proponents say
Reports of bartering for chickens28 and purchasing fuel from a patient in remote Alaska29 show that not all physicians agree and why they feel that professional codes of ethics reflect an urban bias.28,29 In many rural areas and small towns, access to mental health services is limited, and patients often interact with their doctors outside of clinical encounters.23,29-31
Bartering can benefit a physician’s practice by:
- reducing the need to discount services
- eliminating bureaucratic burdens of traditional insurance arrangements
- facilitating development of a patient base
- allowing patients choice and flexibility in seeking medical care.6,16,32
Bartering could confer certain clinical benefits, such as:
- enhancing trust and empathy32
- encouraging patients to make their needs known constructively6
- modeling financial self-care6
- helping the doctor to feel fairly compensated for providing thoughtful care6
- acknowledging the patient’s cultural values15,33
- affirming that patients and doctors both produce things of value.16
I have always thought: Other ethical models
An ethical approach to bartering that requires careful thought and respect for the patient’s needs appears consistent with a primary goal of treatment: “to increase the capacity of individuals to make more rational choices in their lives and to be relatively freer from disabling conflicts.”20 Some authors criticize slippery-slope arguments and strict-rule ethical approaches as being too rigid, limiting, or risk-averse.22,26,34 In Table 1,6,8,16,18,27,29-31,35-37 we list several factors that might weigh for or against a decision to enter into a barter arrangement as payment for care.
In a similar manner, Martinez33,38 proposed a graded-risk framework that encourages examination of potential harms and benefits of a decision, potential coercive or exploitative elements, the clinician’s intentions and aspiration to professional ideals, and the context of the decision. Within this framework, some bartering arrangements might be encouraged and, perhaps, even obligatory because of the potential benefits to the patient; other arrangements (eg, trading psychotherapy for menial services) might be unjustifiable. Martinez38 argues that this approach fosters mutual decision-making with patients, discourages physician paternalism, and “demands that we struggle with the particulars with each case.”
Gottlieb’s decision-making model35 recognizes that trying to avoid all dual relationships is unrealistic and not all dual relationships are exploitative. Instead, a clinician must assess 3 dimensions of current and proposed relationships:
- the degree of power differential
- the duration of treatment
- the clarity of termination.
The decision-making process also requires involvement of the patient, who if “unable to recognize the dilemma or is unwilling to consider the issues before deciding, should be considered at risk, and the contemplated relationship rejected.”35
So I will ask you once again: Dr. Z’s decision
In the case of Dr. Z and Mr. R, a barter arrangement might work in the sense of permitting and sustaining good care. Mr. R suggested the idea and might not be able to afford care without it. Nothing in Dr. Z’s description suggests that Mr. R has personality characteristics or other conditions that would compromise his ability to give informed consent or to understand the nuances of a barter arrangement. Dr. Z is not providing a treatment (eg, psychodynamic therapy) that a barter arrangement could contaminate. That the arrangement would be circumscribed limits the effect of a power differential, as would its brief duration and defined termination endpoint. Dr. Z’s letter to the authors also shows his willingness to seek consultation.
There’s a chance that we may fall apart: Reasons for caution
Martinez’s graded-risk approach recognizes reasons for caution:
- the risk of harm to the patient or doctor–patient relationship
- the uncertain benefit to the patient
- the blurring of Dr. Z’s self-interest and Mr. R’s needs
- some ambiguity about possible exploitation.
Dr. Z and Mr. R have not discussed the value of Mr. R’s work—which might create a rift between them—and despite Mr. R’s reputation, other carpenters are available. Future med-check appointments will give them little time to explore and discuss the meanings of the barter.
Any proposed barter arrangement creates some clinical perils that can be particularly salient in mental health treatment. Patients could view themselves as “special” or entitled to enhanced access to the doctor because of exchanged services, which could take a toll on the doctor.39 The physician’s objectivity might diminish, and the business aspect of their relationship could make both parties less comfortable when discussing sensitive information relevant to treatment.31,40 Also, the suggested barter is for services to be provided at Dr. Z’s office, where confidentiality may be breeched and transference issues could arise.
A medical malpractice claim states that a doctor has breached a duty of care to a patient such that harm (or “damages”) resulted.41 Should Dr. Z and Mr. R’s barter agreement turn sour and harm follow, Mr. R could sue for recovery of damages based of a claim of duress, undue influence, or other aspects of the doctor–patient power differential.27,42,43 Given the published views we have described, a psychiatrist who barters also may be viewed as violating state regulations that measure the standard of care against generally accepted practice.
Only time will tell if I am right or I am wrong
If you face a situation similar to Dr. Z’s and want to consider a barter arrangement, you can take several steps to mitigate potential risk to your patient and ensure competent care (Table 25,6,15,16,32,35,39,40,44-47). One of the most important steps is to seek ongoing consultation, both before and after a decision to barter. Ideally, the consulting colleague would know you and your circumstances and would have sufficient clinical grasp of the patient to make an informed assessment of risks and benefits.35 This consultation, as well as your own rationale for acting on recommendations, should be thoroughly documented in the patient’s records.26,44,45
Certain types of barter should be off limits, including:
- trading prescription drugs for goods or services
- trading for services that tie into the success of one’s business (eg, business advising or marketing)16
- offering treatment in exchange for illegal or ethically unacceptable services.48
Beyond ethical considerations are some practical issues. The Internal Revenue Service has specific rules regarding taxation of bartered goods and services, which must be included as taxable income.46 If possible, an independent agent should appraise the traded goods or services before the agreement.6 When working in a group practice, the clinician might have to figure out how to allocate the received goods or services such as shared overhead costs.28 Preferably, the patient’s goods or services should be provided before care is delivered.16 If not, the duration of services rendered should be limited, and either party should have the option to disengage from the relationship if one feels dissatisfied.16
A written contract, discussed ahead of time, can be a sound way to summarize the terms of the arrangement. Both sides also should consider what would happen if an injury occurred.16 Finally, you must adhere to any relevant state laws regarding payment for services, particularly if the patient has health insurance.32
If the bartering arrangement does not work, you should take an open and non-defensive approach. If you believe you have made a mistake, consider apologizing.45
1. Kaiser Commission on Medicaid and the Uninsured. Key facts about the uninsured population. http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population. Published September 29, 2016. Accessed October 7, 2016.
2. National Alliance on Mental Illness. A long road ahead: achieving true parity in mental health and substance use care. https://www.nami.org/About-NAMI/Publications-Reports/Public-Policy-Reports/A-Long-Road-Ahead/2015-ALongRoadAhead.pdf. Published April 2015. Accessed October 7, 2016.
3. Insel T. Director’s blog: the paradox of parity. May 30, 2014. https://www.nimh.nih.gov/about/director/2014/the-paradox-of-parity.shtml. Published May 30, 2014. Accessed October 7, 2016.
4. Bishop TF, Press MJ, Keyhani S, et al. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181.
5. What do you do when patients cannot pay? Psychiatry (Edgmont). 2009;6(5):51-52.
6. Hill M. Barter: ethical considerations in psychotherapy. Women Ther. 2000;22(3):81-91.
7. Simon RI. Commentary: treatment boundaries—flexible guidelines, not rigid standards. J Am Acad Psychiatry Law. 2001;29(3):287-289.
8. Simon RI, Williams IC. Maintaining treatment boundaries in small communities and rural areas. Psychiatr Serv. 1999;50(11):1440-1446.
9. Compact edition of the Oxford English dictionary. New York, NY: Oxford University Press; 1971:171.
10. Coolican JP. Sue Lowden stands by health care plan. Las Vegas Sun. http://lasvegassun.com/news/2010/apr/20/sue-lowden-draws-fire-repeating-health-care-barter. Published April 20, 2010. Accessed September 20, 2016.
11. Consumer Reports. Barter sometimes allow patients to pay for health care they otherwise could not afford. Washington Post. https://www.washingtonpost.com/national/health-science/barter-sometimes-allow-patients-to-pay-for-health-care-they-otherwise-could-not-afford/2013/09/30/e7e5a55e-069d-11e3-88d6-d5795fab4637_story.html. Published September 20, 2013. Accessed September 27, 2016.
12. Ellis B. MediBid auction site lets doctors bid for patients. CNN Money. http://money.cnn.com/2014/01/09/pf/insurance/medibid. Published January 9, 2014. Accessed September 23, 2016.
13. Ambrosino B. Surgery for sale: the ethics of health care bartering in a social media marketplace. http://hub.jhu.edu/2014/01/16/hopkins-ethicist-ponders-medibid. Published January 16, 2014. Accessed September 23, 2016.
14. Thomas C. When patients barter for health care. https://ethicalnag.org/2013/07/30/barter. Published July 30, 2016. Accessed October 9, 2016.
15. Syme G. Fetters or freedom: dual relationships in counselling. Int J Adv Counselling. 2006;28(1):57-69.
16. Zur O. Bartering in psychotherapy and counselling: complexities, case studies and guidelines. New Therapist. 2008;58:18-26.
17. Simon RI. The psychiatrist as a fiduciary: avoiding the double agent role. Psychiatric Annals. 1987;17(9):622-626.
18. Simon RI. Treatment boundary violations: clinical, ethical, and legal considerations. Bull Am Acad Psychiatry Law. 1992;20(3):269-288.
19. Walker R, Clark JJ. Heading off boundary problems: clinical supervision as risk management. Psychiatr Serv. 1999;50(11):1435-1439.
20. Malmquist CP, Norman MT. Psychiatrist-patient boundary issues following treatment termination. Am J Psychiatry. 2001;158(7):1010-1018.
21. American Psychiatric Association. The opinions of the ethics committee on the principles of medical ethics, with annotations especially applicable to psychiatry. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2016. Accessed October 4, 2016.
22. Gutheil TG, Gabbard GO. Misuses and misunderstandings of boundary theory in clinical and regulatory settings. Am J Psychiatry. 1998;155(3):409-414.
23. Crowden A. Professional boundaries and the ethics of dual and multiple overlapping relationships in psychotherapy. Monash Bioeth Rev. 2008;27(4):10-27.
24. Gabbard GO. Commentary: boundaries, culture, and psychotherapy. J Am Acad Psychiatry Law. 2001;29(3):284-286.
25. Kroll J. Boundary violations: a culture-bound syndrome. J Am Acad Psychiatry Law. 2001;29(3):274-283.
26. Gottlieb MC, Younggren JN. Is there a slippery slope? Considerations regarding multiple relationships and risk management. Professional Psychology: Research and Practice. 2009;40(6):564-557.
27. Woody RH. Bartering for psychological services. Professional Psychology: Research and Practice. 1998;29(2):174-178.
28. Bartering for medical care. MGMA Connex. 2008;8(6):11.
29. Roberts LW, Battaglia J, Epstein RS. Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatr Serv. 1994;50(4):497-503.
30. Endacott R, Wood A, Judd F, et al. Impact and management of dual relationships in metropolitan, regional and rural mental health practice. Aust N Z J Psychiatry. 2006;40(11-12):987-994.
31. Scopelliti J, Judd F, Grigg M, et al. Dual relationships in mental health practice: issues for clinicians in rural settings. Aust N Z J Psychiatry. 2004;38(11-12):953-959.
32. Ayers AA. Bartering basics for the urgent care operator. http://www.alanayersurgentcare.com/Linked_Files/2013_Articles/Ayers_UCAOA_Bartering_%20Basics_2012_01_09.pdf. Accessed September 23, 2016.
33. Savin D, Martinez R. Cross-cultural boundary dilemmas: a graded-risk assessment approach. Transcult Psychiatry. 2006;42(2):243-258.
34. Glass LL. The gray areas of boundary crossings and violations. Am J Psychother. 2003;57(4):429-444.
35. Gottlieb MC. Avoiding exploitive dual relationships: a decision-making model. Psychotherapy (Chic). 1993;30(1):41-48.
36. Lane JA. The ethical implications of bartering for mental health services: examining interdisciplinary ethical standards. http://pdxscholar.library.pdx.edu/coun_fac/36. Published 2012. Accessed October 17, 2016.
37. Miller RD, Maier GJ. Nonsexual boundary violations: sauce for the gander. J Psychiatry Law. 2002;30(3):309-329.
38. Martinez R. A model for boundary dilemmas: ethical decision-making in the patient-professional relationship. Ethical Hum Sci Serv. 2000;2(1):43-61.
39. Salmon K, Klijnsma M. Boundary issues: employing patients as staff? Br J Gen Pract. 2009;59(558):56-57.
40. College of Physicians and Surgeons Ontario. Hiring patients may compromise physician-patient relationship. Dialogue. 2015;3:47.
41. Bal S. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467(2):339-347.
42. What puts a psychiatrist at risk for a malpractice lawsuit? Psychiatry (Edgmont). 2009;6(8):38-39.
43. Geis v Landau, 117 Misc2d 396 (NY Misc 1983).
44. Nisselle P. Danger zone. When boundaries are crossed in the doctor-patient relationship. Aust Fam Physician. 2000;29(6):541-544.
45. Pope KS, Keith-Spiegel P. A practical approach to boundaries in psychotherapy: making decisions, bypassing blunders, and mending fences. J Clin Psychol. 2008;64(5):638-652.
46. IRS Publication 17. https://www.irs.gov/publications/p17/ch12.html. Published 2015. Accessed October 5, 2016.
47. Epstein RS, Simon RI. The exploitation index: an early warning indicator of boundary violations in psychotherapy. Bull Menninger Clin. 1990;54(4):450-465.
48. Skutch J. Savannah doctor accused of trading drugs for sex with strippers. Augusta Chronicle. http://chronicle.augusta.com/news/crime-courts/2013-01-31/savannah-doctor-accused-trading-drugs-sex-strippers. Published January 31, 2013. Accessed October 16, 2016.
1. Kaiser Commission on Medicaid and the Uninsured. Key facts about the uninsured population. http://kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population. Published September 29, 2016. Accessed October 7, 2016.
2. National Alliance on Mental Illness. A long road ahead: achieving true parity in mental health and substance use care. https://www.nami.org/About-NAMI/Publications-Reports/Public-Policy-Reports/A-Long-Road-Ahead/2015-ALongRoadAhead.pdf. Published April 2015. Accessed October 7, 2016.
3. Insel T. Director’s blog: the paradox of parity. May 30, 2014. https://www.nimh.nih.gov/about/director/2014/the-paradox-of-parity.shtml. Published May 30, 2014. Accessed October 7, 2016.
4. Bishop TF, Press MJ, Keyhani S, et al. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181.
5. What do you do when patients cannot pay? Psychiatry (Edgmont). 2009;6(5):51-52.
6. Hill M. Barter: ethical considerations in psychotherapy. Women Ther. 2000;22(3):81-91.
7. Simon RI. Commentary: treatment boundaries—flexible guidelines, not rigid standards. J Am Acad Psychiatry Law. 2001;29(3):287-289.
8. Simon RI, Williams IC. Maintaining treatment boundaries in small communities and rural areas. Psychiatr Serv. 1999;50(11):1440-1446.
9. Compact edition of the Oxford English dictionary. New York, NY: Oxford University Press; 1971:171.
10. Coolican JP. Sue Lowden stands by health care plan. Las Vegas Sun. http://lasvegassun.com/news/2010/apr/20/sue-lowden-draws-fire-repeating-health-care-barter. Published April 20, 2010. Accessed September 20, 2016.
11. Consumer Reports. Barter sometimes allow patients to pay for health care they otherwise could not afford. Washington Post. https://www.washingtonpost.com/national/health-science/barter-sometimes-allow-patients-to-pay-for-health-care-they-otherwise-could-not-afford/2013/09/30/e7e5a55e-069d-11e3-88d6-d5795fab4637_story.html. Published September 20, 2013. Accessed September 27, 2016.
12. Ellis B. MediBid auction site lets doctors bid for patients. CNN Money. http://money.cnn.com/2014/01/09/pf/insurance/medibid. Published January 9, 2014. Accessed September 23, 2016.
13. Ambrosino B. Surgery for sale: the ethics of health care bartering in a social media marketplace. http://hub.jhu.edu/2014/01/16/hopkins-ethicist-ponders-medibid. Published January 16, 2014. Accessed September 23, 2016.
14. Thomas C. When patients barter for health care. https://ethicalnag.org/2013/07/30/barter. Published July 30, 2016. Accessed October 9, 2016.
15. Syme G. Fetters or freedom: dual relationships in counselling. Int J Adv Counselling. 2006;28(1):57-69.
16. Zur O. Bartering in psychotherapy and counselling: complexities, case studies and guidelines. New Therapist. 2008;58:18-26.
17. Simon RI. The psychiatrist as a fiduciary: avoiding the double agent role. Psychiatric Annals. 1987;17(9):622-626.
18. Simon RI. Treatment boundary violations: clinical, ethical, and legal considerations. Bull Am Acad Psychiatry Law. 1992;20(3):269-288.
19. Walker R, Clark JJ. Heading off boundary problems: clinical supervision as risk management. Psychiatr Serv. 1999;50(11):1435-1439.
20. Malmquist CP, Norman MT. Psychiatrist-patient boundary issues following treatment termination. Am J Psychiatry. 2001;158(7):1010-1018.
21. American Psychiatric Association. The opinions of the ethics committee on the principles of medical ethics, with annotations especially applicable to psychiatry. https://www.psychiatry.org/psychiatrists/practice/ethics. Published 2016. Accessed October 4, 2016.
22. Gutheil TG, Gabbard GO. Misuses and misunderstandings of boundary theory in clinical and regulatory settings. Am J Psychiatry. 1998;155(3):409-414.
23. Crowden A. Professional boundaries and the ethics of dual and multiple overlapping relationships in psychotherapy. Monash Bioeth Rev. 2008;27(4):10-27.
24. Gabbard GO. Commentary: boundaries, culture, and psychotherapy. J Am Acad Psychiatry Law. 2001;29(3):284-286.
25. Kroll J. Boundary violations: a culture-bound syndrome. J Am Acad Psychiatry Law. 2001;29(3):274-283.
26. Gottlieb MC, Younggren JN. Is there a slippery slope? Considerations regarding multiple relationships and risk management. Professional Psychology: Research and Practice. 2009;40(6):564-557.
27. Woody RH. Bartering for psychological services. Professional Psychology: Research and Practice. 1998;29(2):174-178.
28. Bartering for medical care. MGMA Connex. 2008;8(6):11.
29. Roberts LW, Battaglia J, Epstein RS. Frontier ethics: mental health care needs and ethical dilemmas in rural communities. Psychiatr Serv. 1994;50(4):497-503.
30. Endacott R, Wood A, Judd F, et al. Impact and management of dual relationships in metropolitan, regional and rural mental health practice. Aust N Z J Psychiatry. 2006;40(11-12):987-994.
31. Scopelliti J, Judd F, Grigg M, et al. Dual relationships in mental health practice: issues for clinicians in rural settings. Aust N Z J Psychiatry. 2004;38(11-12):953-959.
32. Ayers AA. Bartering basics for the urgent care operator. http://www.alanayersurgentcare.com/Linked_Files/2013_Articles/Ayers_UCAOA_Bartering_%20Basics_2012_01_09.pdf. Accessed September 23, 2016.
33. Savin D, Martinez R. Cross-cultural boundary dilemmas: a graded-risk assessment approach. Transcult Psychiatry. 2006;42(2):243-258.
34. Glass LL. The gray areas of boundary crossings and violations. Am J Psychother. 2003;57(4):429-444.
35. Gottlieb MC. Avoiding exploitive dual relationships: a decision-making model. Psychotherapy (Chic). 1993;30(1):41-48.
36. Lane JA. The ethical implications of bartering for mental health services: examining interdisciplinary ethical standards. http://pdxscholar.library.pdx.edu/coun_fac/36. Published 2012. Accessed October 17, 2016.
37. Miller RD, Maier GJ. Nonsexual boundary violations: sauce for the gander. J Psychiatry Law. 2002;30(3):309-329.
38. Martinez R. A model for boundary dilemmas: ethical decision-making in the patient-professional relationship. Ethical Hum Sci Serv. 2000;2(1):43-61.
39. Salmon K, Klijnsma M. Boundary issues: employing patients as staff? Br J Gen Pract. 2009;59(558):56-57.
40. College of Physicians and Surgeons Ontario. Hiring patients may compromise physician-patient relationship. Dialogue. 2015;3:47.
41. Bal S. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009;467(2):339-347.
42. What puts a psychiatrist at risk for a malpractice lawsuit? Psychiatry (Edgmont). 2009;6(8):38-39.
43. Geis v Landau, 117 Misc2d 396 (NY Misc 1983).
44. Nisselle P. Danger zone. When boundaries are crossed in the doctor-patient relationship. Aust Fam Physician. 2000;29(6):541-544.
45. Pope KS, Keith-Spiegel P. A practical approach to boundaries in psychotherapy: making decisions, bypassing blunders, and mending fences. J Clin Psychol. 2008;64(5):638-652.
46. IRS Publication 17. https://www.irs.gov/publications/p17/ch12.html. Published 2015. Accessed October 5, 2016.
47. Epstein RS, Simon RI. The exploitation index: an early warning indicator of boundary violations in psychotherapy. Bull Menninger Clin. 1990;54(4):450-465.
48. Skutch J. Savannah doctor accused of trading drugs for sex with strippers. Augusta Chronicle. http://chronicle.augusta.com/news/crime-courts/2013-01-31/savannah-doctor-accused-trading-drugs-sex-strippers. Published January 31, 2013. Accessed October 16, 2016.
Online dating and personal information: Pause before you post
Most adults want to have happy romantic relationships. But meeting eligible companions and finding the time to date can feel nearly impossible to many physicians, especially residents, whose 80-hour work weeks limit opportunities to meet potential partners.1
So it’s no surprise that Dr. R’s friends have suggested that she try online dating. If she does, she would be far from alone: 15% of U.S. adults have sought relationships online, and one-fourth of people in their 20s have used a mobile dating app.2,3 Online dating might work well for Dr. R, too. Between 2005 and 2012, more than one-third of U.S. marriages started online, and these marriages seemed happier and ended in separation or divorce less often than marriages that started in more traditional ways.4
Online dating is just one example of how “the permeation of online and social media into everyday life is placing doctors in new situations that they find difficult to navigate.”5 Many physicians—psychiatrists among them—date online. Yet, like Dr. R, physicians are cautious about using social media because of worries about public exposure and legal concerns.5 Moreover, medical associations haven’t developed guidelines that would help physicians reconcile their professional and personal lives if they seek companionship online.6
Although we don’t have complete answers to Dr. R’s questions, we have gathered some ideas and information that she might find helpful. Read on as we explore:
- potential benefits for psychiatrists who try online dating
- problems when physicians use social media
- how to minimize mishaps if you seek companionship online.
Advantages and benefits
Online dating is most popular among young adults. But singles and divorcees of all ages, sexual orientations, and backgrounds are increasingly seeking long-term relationships with internet-based dating tools rather than hoping to meet people through family, friends, church, and the workplace. It has become common—and no longer stigmatizing—for couples to say they met online.2,7
A dating Web site or app is a simple, fast, low-investment way to increase your opportunities to meet other singles and to make contact with more potential partners than you would meet otherwise. This is particularly helpful for people in thinner dating markets (eg, gays, lesbians, middle-age heterosexuals, and rural dwellers) or people seeking a companion of a particular type or lifestyle.7,8 Many internet dating tools claim that their matching algorithms can increase your chances of meeting someone you will find compatible (although research questions whether the algorithms really work8). Dating sites and apps also let users engage in brief, computer-mediated communications that can foster greater attraction and comfort before meeting for a first date.8
Appeal to psychiatrists
Online dating may have special appeal to young psychiatrists such as Dr. R. Oddly enough, being a mental health professional can leave you socially isolated. Many people react cautiously when they learn you are a psychiatrist—they think you are evaluating them (and let’s face it: often, this is true).9 Psychiatrists should be cordial but circumspect in conducting work relationships, which limits the type and amount of social life they might generate in the setting where many people meet their future spouses.10
Online dating can help single psychiatrists overcome these barriers. Scientifically minded physicians can find plenty of research-grounded advice for improving online dating chances.11-14 Two medical researchers even published a meta-analysis of evidence-based methods that can improve the chances of converting online contacts to a first date.15
Caution: Hazards ahead
When seeking romance online, psychiatrists shouldn’t forget their professional obligations, including the duty to maintain clear boundaries between their social and work lives.16 If Dr. R decides to try online dating, she will be making it possible for curious patients to gain access to some of her personal information. She will have to figure out how to avoid jeopardizing her professional reputation or inadvertently opening the door to sexual misconduct.17
Boundaries online. Psychiatrists use the term “boundaries” to refer to how they structure appointments and monitor their behavior during therapy to keep the treatment relationship free of personal, sexual, and romantic influences. Keeping one’s emotional life out of treatment helps prevent exploitation of patients and fosters a sense of safety and assurance that the physician is acting solely with the patient’s interest in mind. Breaching boundaries in ways that exploit patients or serve the doctor’s needs can undermine treatment, harm patients, and result in serious professional consequences.18
Maintaining appropriate boundaries can be challenging for psychiatrists who want to date online because the outside-the-office context can muddy the distinction between one’s professional and personal identity. Online dating environments make it easier for physicians to inadvertently initiate social or romantic interactions with people they have treated but don’t recognize (something the authors know has happened to colleagues). Additionally, the internet’s anonymity leaves users vulnerable to being lured into interactions with someone who is using a fictional online persona—an activity colloquially called “catfishing.”19
Although patients may play an active role in boundary breaches, the physician bears sole responsibility for maintaining proper limits within the therapeutic relationship.18 For many psychiatrists, innocuous but non-professional interactions with patients have been the first steps down a “slippery slope” toward serious boundary violations, including sexual contact—an activity that both the American Medical Association (AMA) and the American Psychiatric Association deem categorically unethical and that can lead to malpractice lawsuits, sanctions by medical license boards, and (in some jurisdictions) criminal prosecution.20 When using social media and online dating tools, psychiatrists should avoid even seemingly minor boundary violations as a safeguard against more serious transgressions.20,21
Reports of online misconduct by medical trainees and practitioners are plentiful.22,23 In response, several medical organizations, including the AMA and the American College of Physicians, have developed professional guidelines for appropriate behavior on social media by physicians.24,25 These guidelines stress the importance of maintaining a professional presence when one’s online activity is publicly viewable.
How much self-disclosure is appropriate?
Traditionally, psychiatrists (including psychoanalysts) have felt that occasional, limited, well-considered references to oneself are acceptable and even helpful in treatment.26 The majority of therapists report using therapy-relevant self-disclosure, but they are cautious about what they say. Conscientious therapists avoid self-disclosure to satisfy their own needs, and they avoid self-disclosure with patients for whom it would have detrimental effects.18,27
Dating Web sites contain a lot of personal information that physicians don’t usually share with patients. Although physicians who use social media are advised to be careful about the information they make available to the public,28 this is more difficult to do with dating applications, where revealing some information about yourself is necessary for making meaningful connections. Creating an online dating profile means that you are potentially letting patients or patients’ relatives know about your place of residence, income, sexual orientation, number of children, and interests. You will need to think about how you will respond if a patient unexpectedly comments on your dating profile during a session or asks you out.
Beyond creating awkward situations, self-disclosure can have treatment implications, and it’s impossible to know how a particular comment will affect a particular client in a particular situation.29 Psychiatrists who engage in online dating may want to limit their posted personal information only to what they would feel reasonably comfortable with having patients know about them, and hope this will suffice to capture the attention of potential partners.
Sustaining professionalism while remaining human. The term “medical professionalism” originally referred to ethical conduct during the practice of medicine30 and to sustaining one’s commitment to patients, fellow professionals, and the institutions within which health care is provided.31 More recently, however, discussions of medical professionalism have encompassed how physicians comport themselves away from work. Physicians’ actions outside the office or hospital—and especially what they say, do, or post online—have a powerful effect on perceptions of their institutions and the medical profession as a whole.25,32
Photos and comments posted by physicians can be seen by millions and can have major repercussions for employment prospects and public perceptions.25 Questionable postings by physicians on social media outlets have resulted in disciplinary actions by licensing authorities and have damaged physicians’ careers.23
What seems appropriate for a dating Web site varies from person to person. A suggestive smile or flirtatious joke that most people would find harmless may strike others as provocative. Derogatory language, depictions of intoxication or substance abuse, and inappropriate patient-related comments are clear-cut mistakes.32-34 But also keep in mind that what medical professionals find acceptable to post on social networking sites does not always match what the general public thinks.35
Bottom Line
1. Miller JA. Romance in residency: is dating even possible? Medscape. http://www.medscape.com/viewarticle/844059. Published May 5, 2016. Accessed June 27, 2016.
2. Smith A, Anderson M. 5 facts about online dating. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/02/29/5-facts-about-online-dating. Published February 29, 2016. Accessed June 27, 2016.
3. Smith A. 15% of American adults have used online dating sites or mobile dating apps. http://www.pewinternet.org/2016/02/11/15-percent-of-american-adults-have-used-online-dating-sites-or-mobile-dating-apps/. Published February 11, 2016. Accessed June 27, 2016.
4. Cacioppo JT, Cacioppo S, Gonzaga GC, et al. Marital satisfaction and break-ups differ across on-line and off-line meeting venues. Proc Natl Acad Sci U S A. 2013;110(25):10135-10140.
5. Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16(12):e267.
6. Berlin R. The professional ethics of online dating: need for guidance. J Am Acad Child Adolesc Psychiatry. 2014;53(9):935-937.
7. Rosenfeld MJ, Thomas RJ. Searching for a mate: the rise of the Internet as a social intermediary. Am Sociol Rev. 2012;77(4):523-547.
8. Finkel EJ, Eastwick PW, Karney BR, et al. Online dating: a critical analysis from the perspective of psychological science. Psychol Sci Public Interest. 2012;13(1):3-66.
9. Pierre J. A mad world: a diagnosis of mental illness is more common than ever—did psychiatrists create the problem, or just recognise it? Aeon.co. https://aeon.co/essays/do-psychiatrists-really-think-that-everyone-is-crazy. Published March 19, 2014. Accessed June 28, 2016.
10. Pearce A, Gambrell D. This chart shows who marries CEOs, doctors, chefs and janitors. Bloomberg. http://www.bloomberg.com/graphics/2016-who-marries-whom. February 11, 2016. Accessed June 28, 2016.
11. Lowin R. Proofread that text before sending! Bad grammar is a dating deal breaker, most say. Today. http://www.today.com/health/can-your-awesome-grammar-really-get-you-date-according-new-t77376. Published March 2, 2016. Accessed June 28, 2016.
12. Reilly K. This strategy will make your Tinder game much stronger. Time. http://time.com/4263598/tinder-gif-messages-response-rate. Published March 17, 2016. Accessed June 28, 2016.
13. Wotipka CD, High AC. Providing a foundation for a satisfying relationship: a direct test of warranting versus selective self-presentation as predictors of attraction to online dating profiles. Presentation at the 101st Annual Meeting of the National Communication Association; November 20, 2014; Chicago, IL.
14. Vacharkulksemsuk T, Reit E, Khambatta P, et al. Dominant, open nonverbal displays are attractive at zero-acquaintance. Proc Natl Acad Sci U S A. 2016;113(15):4009-4014.
15. Khan KS, Chaudhry S. An evidence-based approach to an ancient pursuit: systematic review on converting online contact into a first date. Evid Based Med. 2015;20(2):48-56.
16. Chretien KC, Tuck MG. Online professionalism: a synthetic review. Int Rev Psychiatry. 2015;27(2):106-117.
17. Jackson WC. When patients are normal people: strategies for managing dual relationships. Prim Care Companion J Clin Psychiatry. 2002;4(3):100-103.
18. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
19. D’Costa K. Catfishing: the truth about deception online. ScientificAmerican.com. http://blogs.scientificamerican.com/anthropology-in-practice/catfishing-the-truth-about-deception-online. Published April 25, 2014. Accessed June 29, 2016.
20. Sarkar SP. Boundary violation and sexual exploitation in psychiatry and psychotherapy: a review. Adv Psychiatr Treat. 2004;10(4):312-320.
21. Nadelson C, Notman MT. Boundaries in the doctor-patient relationship. Theor Med Bioeth. 2002;23(3):191-201.
22. Walton JM, White J, Ross S. What’s on YOUR Facebook profile? Evaluation of an educational intervention to promote appropriate use of privacy settings by medical students on social networking sites. Med Educ Online. 2015;20:28708. doi: 10.3402/meo.v20.28708.
23. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
24. Decamp M. Physicians, social media, and conflict of interest. J Gen Intern Med. 2013;28(2):299-303.
25. Farnan JM, Snyder Sulmasy L, Worster BK, et al; American College of Physicians Ethics, Professionalism and Human Rights Committee; American College of Physicians Council of Associates; Federation of State Medical Boards Special Committee on Ethics and Professionalism. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620-627.
26. Meissner WW. The problem of self-disclosure in psychoanalysis. J Am Psychoanal Assoc. 2002;50(3):827-867.
27. Henretty JR, Levitt HM. The role of therapist self-disclosure in psychotherapy: a qualitative review. Clin Psychol Rev. 2010;30(1):63-77.
28. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
29. Peterson ZD. More than a mirror: the ethics of therapist self-disclosure. Psychotherapy: Theory Research & Practice. 2002;39(1):21-31.
30. Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226-235.
31. Wass V. Doctors in society: medical professionalism in a changing world. Clin Med (Lond). 2006;6(1):109-113.
32. Langenfeld SJ, Cook G, Sudbeck C, et al. An assessment of unprofessional behavior among surgical residents on Facebook: a warning of the dangers of social media. J Surg Educ. 2014;71(6):e28-e32.
33. Chauhan B, George R, Coffin J. Social media and you: what every physician needs to know. J Med Pract Manage. 2012;28(3):206-209.
34. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
35. Jain A, Petty EM, Jaber RM, et al. What is appropriate to post on social media? Ratings from students, faculty members and the public. Med Educ. 2014;48(2):157-169.
36. Gabbard GO, Roberts LW, Crisp-Han H, et al. Professionalism in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2012.
Most adults want to have happy romantic relationships. But meeting eligible companions and finding the time to date can feel nearly impossible to many physicians, especially residents, whose 80-hour work weeks limit opportunities to meet potential partners.1
So it’s no surprise that Dr. R’s friends have suggested that she try online dating. If she does, she would be far from alone: 15% of U.S. adults have sought relationships online, and one-fourth of people in their 20s have used a mobile dating app.2,3 Online dating might work well for Dr. R, too. Between 2005 and 2012, more than one-third of U.S. marriages started online, and these marriages seemed happier and ended in separation or divorce less often than marriages that started in more traditional ways.4
Online dating is just one example of how “the permeation of online and social media into everyday life is placing doctors in new situations that they find difficult to navigate.”5 Many physicians—psychiatrists among them—date online. Yet, like Dr. R, physicians are cautious about using social media because of worries about public exposure and legal concerns.5 Moreover, medical associations haven’t developed guidelines that would help physicians reconcile their professional and personal lives if they seek companionship online.6
Although we don’t have complete answers to Dr. R’s questions, we have gathered some ideas and information that she might find helpful. Read on as we explore:
- potential benefits for psychiatrists who try online dating
- problems when physicians use social media
- how to minimize mishaps if you seek companionship online.
Advantages and benefits
Online dating is most popular among young adults. But singles and divorcees of all ages, sexual orientations, and backgrounds are increasingly seeking long-term relationships with internet-based dating tools rather than hoping to meet people through family, friends, church, and the workplace. It has become common—and no longer stigmatizing—for couples to say they met online.2,7
A dating Web site or app is a simple, fast, low-investment way to increase your opportunities to meet other singles and to make contact with more potential partners than you would meet otherwise. This is particularly helpful for people in thinner dating markets (eg, gays, lesbians, middle-age heterosexuals, and rural dwellers) or people seeking a companion of a particular type or lifestyle.7,8 Many internet dating tools claim that their matching algorithms can increase your chances of meeting someone you will find compatible (although research questions whether the algorithms really work8). Dating sites and apps also let users engage in brief, computer-mediated communications that can foster greater attraction and comfort before meeting for a first date.8
Appeal to psychiatrists
Online dating may have special appeal to young psychiatrists such as Dr. R. Oddly enough, being a mental health professional can leave you socially isolated. Many people react cautiously when they learn you are a psychiatrist—they think you are evaluating them (and let’s face it: often, this is true).9 Psychiatrists should be cordial but circumspect in conducting work relationships, which limits the type and amount of social life they might generate in the setting where many people meet their future spouses.10
Online dating can help single psychiatrists overcome these barriers. Scientifically minded physicians can find plenty of research-grounded advice for improving online dating chances.11-14 Two medical researchers even published a meta-analysis of evidence-based methods that can improve the chances of converting online contacts to a first date.15
Caution: Hazards ahead
When seeking romance online, psychiatrists shouldn’t forget their professional obligations, including the duty to maintain clear boundaries between their social and work lives.16 If Dr. R decides to try online dating, she will be making it possible for curious patients to gain access to some of her personal information. She will have to figure out how to avoid jeopardizing her professional reputation or inadvertently opening the door to sexual misconduct.17
Boundaries online. Psychiatrists use the term “boundaries” to refer to how they structure appointments and monitor their behavior during therapy to keep the treatment relationship free of personal, sexual, and romantic influences. Keeping one’s emotional life out of treatment helps prevent exploitation of patients and fosters a sense of safety and assurance that the physician is acting solely with the patient’s interest in mind. Breaching boundaries in ways that exploit patients or serve the doctor’s needs can undermine treatment, harm patients, and result in serious professional consequences.18
Maintaining appropriate boundaries can be challenging for psychiatrists who want to date online because the outside-the-office context can muddy the distinction between one’s professional and personal identity. Online dating environments make it easier for physicians to inadvertently initiate social or romantic interactions with people they have treated but don’t recognize (something the authors know has happened to colleagues). Additionally, the internet’s anonymity leaves users vulnerable to being lured into interactions with someone who is using a fictional online persona—an activity colloquially called “catfishing.”19
Although patients may play an active role in boundary breaches, the physician bears sole responsibility for maintaining proper limits within the therapeutic relationship.18 For many psychiatrists, innocuous but non-professional interactions with patients have been the first steps down a “slippery slope” toward serious boundary violations, including sexual contact—an activity that both the American Medical Association (AMA) and the American Psychiatric Association deem categorically unethical and that can lead to malpractice lawsuits, sanctions by medical license boards, and (in some jurisdictions) criminal prosecution.20 When using social media and online dating tools, psychiatrists should avoid even seemingly minor boundary violations as a safeguard against more serious transgressions.20,21
Reports of online misconduct by medical trainees and practitioners are plentiful.22,23 In response, several medical organizations, including the AMA and the American College of Physicians, have developed professional guidelines for appropriate behavior on social media by physicians.24,25 These guidelines stress the importance of maintaining a professional presence when one’s online activity is publicly viewable.
How much self-disclosure is appropriate?
Traditionally, psychiatrists (including psychoanalysts) have felt that occasional, limited, well-considered references to oneself are acceptable and even helpful in treatment.26 The majority of therapists report using therapy-relevant self-disclosure, but they are cautious about what they say. Conscientious therapists avoid self-disclosure to satisfy their own needs, and they avoid self-disclosure with patients for whom it would have detrimental effects.18,27
Dating Web sites contain a lot of personal information that physicians don’t usually share with patients. Although physicians who use social media are advised to be careful about the information they make available to the public,28 this is more difficult to do with dating applications, where revealing some information about yourself is necessary for making meaningful connections. Creating an online dating profile means that you are potentially letting patients or patients’ relatives know about your place of residence, income, sexual orientation, number of children, and interests. You will need to think about how you will respond if a patient unexpectedly comments on your dating profile during a session or asks you out.
Beyond creating awkward situations, self-disclosure can have treatment implications, and it’s impossible to know how a particular comment will affect a particular client in a particular situation.29 Psychiatrists who engage in online dating may want to limit their posted personal information only to what they would feel reasonably comfortable with having patients know about them, and hope this will suffice to capture the attention of potential partners.
Sustaining professionalism while remaining human. The term “medical professionalism” originally referred to ethical conduct during the practice of medicine30 and to sustaining one’s commitment to patients, fellow professionals, and the institutions within which health care is provided.31 More recently, however, discussions of medical professionalism have encompassed how physicians comport themselves away from work. Physicians’ actions outside the office or hospital—and especially what they say, do, or post online—have a powerful effect on perceptions of their institutions and the medical profession as a whole.25,32
Photos and comments posted by physicians can be seen by millions and can have major repercussions for employment prospects and public perceptions.25 Questionable postings by physicians on social media outlets have resulted in disciplinary actions by licensing authorities and have damaged physicians’ careers.23
What seems appropriate for a dating Web site varies from person to person. A suggestive smile or flirtatious joke that most people would find harmless may strike others as provocative. Derogatory language, depictions of intoxication or substance abuse, and inappropriate patient-related comments are clear-cut mistakes.32-34 But also keep in mind that what medical professionals find acceptable to post on social networking sites does not always match what the general public thinks.35
Bottom Line
Most adults want to have happy romantic relationships. But meeting eligible companions and finding the time to date can feel nearly impossible to many physicians, especially residents, whose 80-hour work weeks limit opportunities to meet potential partners.1
So it’s no surprise that Dr. R’s friends have suggested that she try online dating. If she does, she would be far from alone: 15% of U.S. adults have sought relationships online, and one-fourth of people in their 20s have used a mobile dating app.2,3 Online dating might work well for Dr. R, too. Between 2005 and 2012, more than one-third of U.S. marriages started online, and these marriages seemed happier and ended in separation or divorce less often than marriages that started in more traditional ways.4
Online dating is just one example of how “the permeation of online and social media into everyday life is placing doctors in new situations that they find difficult to navigate.”5 Many physicians—psychiatrists among them—date online. Yet, like Dr. R, physicians are cautious about using social media because of worries about public exposure and legal concerns.5 Moreover, medical associations haven’t developed guidelines that would help physicians reconcile their professional and personal lives if they seek companionship online.6
Although we don’t have complete answers to Dr. R’s questions, we have gathered some ideas and information that she might find helpful. Read on as we explore:
- potential benefits for psychiatrists who try online dating
- problems when physicians use social media
- how to minimize mishaps if you seek companionship online.
Advantages and benefits
Online dating is most popular among young adults. But singles and divorcees of all ages, sexual orientations, and backgrounds are increasingly seeking long-term relationships with internet-based dating tools rather than hoping to meet people through family, friends, church, and the workplace. It has become common—and no longer stigmatizing—for couples to say they met online.2,7
A dating Web site or app is a simple, fast, low-investment way to increase your opportunities to meet other singles and to make contact with more potential partners than you would meet otherwise. This is particularly helpful for people in thinner dating markets (eg, gays, lesbians, middle-age heterosexuals, and rural dwellers) or people seeking a companion of a particular type or lifestyle.7,8 Many internet dating tools claim that their matching algorithms can increase your chances of meeting someone you will find compatible (although research questions whether the algorithms really work8). Dating sites and apps also let users engage in brief, computer-mediated communications that can foster greater attraction and comfort before meeting for a first date.8
Appeal to psychiatrists
Online dating may have special appeal to young psychiatrists such as Dr. R. Oddly enough, being a mental health professional can leave you socially isolated. Many people react cautiously when they learn you are a psychiatrist—they think you are evaluating them (and let’s face it: often, this is true).9 Psychiatrists should be cordial but circumspect in conducting work relationships, which limits the type and amount of social life they might generate in the setting where many people meet their future spouses.10
Online dating can help single psychiatrists overcome these barriers. Scientifically minded physicians can find plenty of research-grounded advice for improving online dating chances.11-14 Two medical researchers even published a meta-analysis of evidence-based methods that can improve the chances of converting online contacts to a first date.15
Caution: Hazards ahead
When seeking romance online, psychiatrists shouldn’t forget their professional obligations, including the duty to maintain clear boundaries between their social and work lives.16 If Dr. R decides to try online dating, she will be making it possible for curious patients to gain access to some of her personal information. She will have to figure out how to avoid jeopardizing her professional reputation or inadvertently opening the door to sexual misconduct.17
Boundaries online. Psychiatrists use the term “boundaries” to refer to how they structure appointments and monitor their behavior during therapy to keep the treatment relationship free of personal, sexual, and romantic influences. Keeping one’s emotional life out of treatment helps prevent exploitation of patients and fosters a sense of safety and assurance that the physician is acting solely with the patient’s interest in mind. Breaching boundaries in ways that exploit patients or serve the doctor’s needs can undermine treatment, harm patients, and result in serious professional consequences.18
Maintaining appropriate boundaries can be challenging for psychiatrists who want to date online because the outside-the-office context can muddy the distinction between one’s professional and personal identity. Online dating environments make it easier for physicians to inadvertently initiate social or romantic interactions with people they have treated but don’t recognize (something the authors know has happened to colleagues). Additionally, the internet’s anonymity leaves users vulnerable to being lured into interactions with someone who is using a fictional online persona—an activity colloquially called “catfishing.”19
Although patients may play an active role in boundary breaches, the physician bears sole responsibility for maintaining proper limits within the therapeutic relationship.18 For many psychiatrists, innocuous but non-professional interactions with patients have been the first steps down a “slippery slope” toward serious boundary violations, including sexual contact—an activity that both the American Medical Association (AMA) and the American Psychiatric Association deem categorically unethical and that can lead to malpractice lawsuits, sanctions by medical license boards, and (in some jurisdictions) criminal prosecution.20 When using social media and online dating tools, psychiatrists should avoid even seemingly minor boundary violations as a safeguard against more serious transgressions.20,21
Reports of online misconduct by medical trainees and practitioners are plentiful.22,23 In response, several medical organizations, including the AMA and the American College of Physicians, have developed professional guidelines for appropriate behavior on social media by physicians.24,25 These guidelines stress the importance of maintaining a professional presence when one’s online activity is publicly viewable.
How much self-disclosure is appropriate?
Traditionally, psychiatrists (including psychoanalysts) have felt that occasional, limited, well-considered references to oneself are acceptable and even helpful in treatment.26 The majority of therapists report using therapy-relevant self-disclosure, but they are cautious about what they say. Conscientious therapists avoid self-disclosure to satisfy their own needs, and they avoid self-disclosure with patients for whom it would have detrimental effects.18,27
Dating Web sites contain a lot of personal information that physicians don’t usually share with patients. Although physicians who use social media are advised to be careful about the information they make available to the public,28 this is more difficult to do with dating applications, where revealing some information about yourself is necessary for making meaningful connections. Creating an online dating profile means that you are potentially letting patients or patients’ relatives know about your place of residence, income, sexual orientation, number of children, and interests. You will need to think about how you will respond if a patient unexpectedly comments on your dating profile during a session or asks you out.
Beyond creating awkward situations, self-disclosure can have treatment implications, and it’s impossible to know how a particular comment will affect a particular client in a particular situation.29 Psychiatrists who engage in online dating may want to limit their posted personal information only to what they would feel reasonably comfortable with having patients know about them, and hope this will suffice to capture the attention of potential partners.
Sustaining professionalism while remaining human. The term “medical professionalism” originally referred to ethical conduct during the practice of medicine30 and to sustaining one’s commitment to patients, fellow professionals, and the institutions within which health care is provided.31 More recently, however, discussions of medical professionalism have encompassed how physicians comport themselves away from work. Physicians’ actions outside the office or hospital—and especially what they say, do, or post online—have a powerful effect on perceptions of their institutions and the medical profession as a whole.25,32
Photos and comments posted by physicians can be seen by millions and can have major repercussions for employment prospects and public perceptions.25 Questionable postings by physicians on social media outlets have resulted in disciplinary actions by licensing authorities and have damaged physicians’ careers.23
What seems appropriate for a dating Web site varies from person to person. A suggestive smile or flirtatious joke that most people would find harmless may strike others as provocative. Derogatory language, depictions of intoxication or substance abuse, and inappropriate patient-related comments are clear-cut mistakes.32-34 But also keep in mind that what medical professionals find acceptable to post on social networking sites does not always match what the general public thinks.35
Bottom Line
1. Miller JA. Romance in residency: is dating even possible? Medscape. http://www.medscape.com/viewarticle/844059. Published May 5, 2016. Accessed June 27, 2016.
2. Smith A, Anderson M. 5 facts about online dating. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/02/29/5-facts-about-online-dating. Published February 29, 2016. Accessed June 27, 2016.
3. Smith A. 15% of American adults have used online dating sites or mobile dating apps. http://www.pewinternet.org/2016/02/11/15-percent-of-american-adults-have-used-online-dating-sites-or-mobile-dating-apps/. Published February 11, 2016. Accessed June 27, 2016.
4. Cacioppo JT, Cacioppo S, Gonzaga GC, et al. Marital satisfaction and break-ups differ across on-line and off-line meeting venues. Proc Natl Acad Sci U S A. 2013;110(25):10135-10140.
5. Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16(12):e267.
6. Berlin R. The professional ethics of online dating: need for guidance. J Am Acad Child Adolesc Psychiatry. 2014;53(9):935-937.
7. Rosenfeld MJ, Thomas RJ. Searching for a mate: the rise of the Internet as a social intermediary. Am Sociol Rev. 2012;77(4):523-547.
8. Finkel EJ, Eastwick PW, Karney BR, et al. Online dating: a critical analysis from the perspective of psychological science. Psychol Sci Public Interest. 2012;13(1):3-66.
9. Pierre J. A mad world: a diagnosis of mental illness is more common than ever—did psychiatrists create the problem, or just recognise it? Aeon.co. https://aeon.co/essays/do-psychiatrists-really-think-that-everyone-is-crazy. Published March 19, 2014. Accessed June 28, 2016.
10. Pearce A, Gambrell D. This chart shows who marries CEOs, doctors, chefs and janitors. Bloomberg. http://www.bloomberg.com/graphics/2016-who-marries-whom. February 11, 2016. Accessed June 28, 2016.
11. Lowin R. Proofread that text before sending! Bad grammar is a dating deal breaker, most say. Today. http://www.today.com/health/can-your-awesome-grammar-really-get-you-date-according-new-t77376. Published March 2, 2016. Accessed June 28, 2016.
12. Reilly K. This strategy will make your Tinder game much stronger. Time. http://time.com/4263598/tinder-gif-messages-response-rate. Published March 17, 2016. Accessed June 28, 2016.
13. Wotipka CD, High AC. Providing a foundation for a satisfying relationship: a direct test of warranting versus selective self-presentation as predictors of attraction to online dating profiles. Presentation at the 101st Annual Meeting of the National Communication Association; November 20, 2014; Chicago, IL.
14. Vacharkulksemsuk T, Reit E, Khambatta P, et al. Dominant, open nonverbal displays are attractive at zero-acquaintance. Proc Natl Acad Sci U S A. 2016;113(15):4009-4014.
15. Khan KS, Chaudhry S. An evidence-based approach to an ancient pursuit: systematic review on converting online contact into a first date. Evid Based Med. 2015;20(2):48-56.
16. Chretien KC, Tuck MG. Online professionalism: a synthetic review. Int Rev Psychiatry. 2015;27(2):106-117.
17. Jackson WC. When patients are normal people: strategies for managing dual relationships. Prim Care Companion J Clin Psychiatry. 2002;4(3):100-103.
18. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
19. D’Costa K. Catfishing: the truth about deception online. ScientificAmerican.com. http://blogs.scientificamerican.com/anthropology-in-practice/catfishing-the-truth-about-deception-online. Published April 25, 2014. Accessed June 29, 2016.
20. Sarkar SP. Boundary violation and sexual exploitation in psychiatry and psychotherapy: a review. Adv Psychiatr Treat. 2004;10(4):312-320.
21. Nadelson C, Notman MT. Boundaries in the doctor-patient relationship. Theor Med Bioeth. 2002;23(3):191-201.
22. Walton JM, White J, Ross S. What’s on YOUR Facebook profile? Evaluation of an educational intervention to promote appropriate use of privacy settings by medical students on social networking sites. Med Educ Online. 2015;20:28708. doi: 10.3402/meo.v20.28708.
23. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
24. Decamp M. Physicians, social media, and conflict of interest. J Gen Intern Med. 2013;28(2):299-303.
25. Farnan JM, Snyder Sulmasy L, Worster BK, et al; American College of Physicians Ethics, Professionalism and Human Rights Committee; American College of Physicians Council of Associates; Federation of State Medical Boards Special Committee on Ethics and Professionalism. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620-627.
26. Meissner WW. The problem of self-disclosure in psychoanalysis. J Am Psychoanal Assoc. 2002;50(3):827-867.
27. Henretty JR, Levitt HM. The role of therapist self-disclosure in psychotherapy: a qualitative review. Clin Psychol Rev. 2010;30(1):63-77.
28. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
29. Peterson ZD. More than a mirror: the ethics of therapist self-disclosure. Psychotherapy: Theory Research & Practice. 2002;39(1):21-31.
30. Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226-235.
31. Wass V. Doctors in society: medical professionalism in a changing world. Clin Med (Lond). 2006;6(1):109-113.
32. Langenfeld SJ, Cook G, Sudbeck C, et al. An assessment of unprofessional behavior among surgical residents on Facebook: a warning of the dangers of social media. J Surg Educ. 2014;71(6):e28-e32.
33. Chauhan B, George R, Coffin J. Social media and you: what every physician needs to know. J Med Pract Manage. 2012;28(3):206-209.
34. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
35. Jain A, Petty EM, Jaber RM, et al. What is appropriate to post on social media? Ratings from students, faculty members and the public. Med Educ. 2014;48(2):157-169.
36. Gabbard GO, Roberts LW, Crisp-Han H, et al. Professionalism in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2012.
1. Miller JA. Romance in residency: is dating even possible? Medscape. http://www.medscape.com/viewarticle/844059. Published May 5, 2016. Accessed June 27, 2016.
2. Smith A, Anderson M. 5 facts about online dating. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/02/29/5-facts-about-online-dating. Published February 29, 2016. Accessed June 27, 2016.
3. Smith A. 15% of American adults have used online dating sites or mobile dating apps. http://www.pewinternet.org/2016/02/11/15-percent-of-american-adults-have-used-online-dating-sites-or-mobile-dating-apps/. Published February 11, 2016. Accessed June 27, 2016.
4. Cacioppo JT, Cacioppo S, Gonzaga GC, et al. Marital satisfaction and break-ups differ across on-line and off-line meeting venues. Proc Natl Acad Sci U S A. 2013;110(25):10135-10140.
5. Brown J, Ryan C, Harris A. How doctors view and use social media: a national survey. J Med Internet Res. 2014;16(12):e267.
6. Berlin R. The professional ethics of online dating: need for guidance. J Am Acad Child Adolesc Psychiatry. 2014;53(9):935-937.
7. Rosenfeld MJ, Thomas RJ. Searching for a mate: the rise of the Internet as a social intermediary. Am Sociol Rev. 2012;77(4):523-547.
8. Finkel EJ, Eastwick PW, Karney BR, et al. Online dating: a critical analysis from the perspective of psychological science. Psychol Sci Public Interest. 2012;13(1):3-66.
9. Pierre J. A mad world: a diagnosis of mental illness is more common than ever—did psychiatrists create the problem, or just recognise it? Aeon.co. https://aeon.co/essays/do-psychiatrists-really-think-that-everyone-is-crazy. Published March 19, 2014. Accessed June 28, 2016.
10. Pearce A, Gambrell D. This chart shows who marries CEOs, doctors, chefs and janitors. Bloomberg. http://www.bloomberg.com/graphics/2016-who-marries-whom. February 11, 2016. Accessed June 28, 2016.
11. Lowin R. Proofread that text before sending! Bad grammar is a dating deal breaker, most say. Today. http://www.today.com/health/can-your-awesome-grammar-really-get-you-date-according-new-t77376. Published March 2, 2016. Accessed June 28, 2016.
12. Reilly K. This strategy will make your Tinder game much stronger. Time. http://time.com/4263598/tinder-gif-messages-response-rate. Published March 17, 2016. Accessed June 28, 2016.
13. Wotipka CD, High AC. Providing a foundation for a satisfying relationship: a direct test of warranting versus selective self-presentation as predictors of attraction to online dating profiles. Presentation at the 101st Annual Meeting of the National Communication Association; November 20, 2014; Chicago, IL.
14. Vacharkulksemsuk T, Reit E, Khambatta P, et al. Dominant, open nonverbal displays are attractive at zero-acquaintance. Proc Natl Acad Sci U S A. 2016;113(15):4009-4014.
15. Khan KS, Chaudhry S. An evidence-based approach to an ancient pursuit: systematic review on converting online contact into a first date. Evid Based Med. 2015;20(2):48-56.
16. Chretien KC, Tuck MG. Online professionalism: a synthetic review. Int Rev Psychiatry. 2015;27(2):106-117.
17. Jackson WC. When patients are normal people: strategies for managing dual relationships. Prim Care Companion J Clin Psychiatry. 2002;4(3):100-103.
18. Gutheil TG, Gabbard GO. The concept of boundaries in clinical practice: theoretical and risk-management dimensions. Am J Psychiatry. 1993;150(2):188-196.
19. D’Costa K. Catfishing: the truth about deception online. ScientificAmerican.com. http://blogs.scientificamerican.com/anthropology-in-practice/catfishing-the-truth-about-deception-online. Published April 25, 2014. Accessed June 29, 2016.
20. Sarkar SP. Boundary violation and sexual exploitation in psychiatry and psychotherapy: a review. Adv Psychiatr Treat. 2004;10(4):312-320.
21. Nadelson C, Notman MT. Boundaries in the doctor-patient relationship. Theor Med Bioeth. 2002;23(3):191-201.
22. Walton JM, White J, Ross S. What’s on YOUR Facebook profile? Evaluation of an educational intervention to promote appropriate use of privacy settings by medical students on social networking sites. Med Educ Online. 2015;20:28708. doi: 10.3402/meo.v20.28708.
23. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
24. Decamp M. Physicians, social media, and conflict of interest. J Gen Intern Med. 2013;28(2):299-303.
25. Farnan JM, Snyder Sulmasy L, Worster BK, et al; American College of Physicians Ethics, Professionalism and Human Rights Committee; American College of Physicians Council of Associates; Federation of State Medical Boards Special Committee on Ethics and Professionalism. Online medical professionalism: patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med. 2013;158(8):620-627.
26. Meissner WW. The problem of self-disclosure in psychoanalysis. J Am Psychoanal Assoc. 2002;50(3):827-867.
27. Henretty JR, Levitt HM. The role of therapist self-disclosure in psychotherapy: a qualitative review. Clin Psychol Rev. 2010;30(1):63-77.
28. Ponce BA, Determann JR, Boohaker HA, et al. Social networking profiles and professionalism issues in residency applicants: an original study-cohort study. J Surg Educ. 2013;70(4):502-507.
29. Peterson ZD. More than a mirror: the ethics of therapist self-disclosure. Psychotherapy: Theory Research & Practice. 2002;39(1):21-31.
30. Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002;287(2):226-235.
31. Wass V. Doctors in society: medical professionalism in a changing world. Clin Med (Lond). 2006;6(1):109-113.
32. Langenfeld SJ, Cook G, Sudbeck C, et al. An assessment of unprofessional behavior among surgical residents on Facebook: a warning of the dangers of social media. J Surg Educ. 2014;71(6):e28-e32.
33. Chauhan B, George R, Coffin J. Social media and you: what every physician needs to know. J Med Pract Manage. 2012;28(3):206-209.
34. Greysen SR, Chretien KC, Kind T, et al. Physician violations of online professionalism and disciplinary actions: a national survey of state medical boards. JAMA. 2012;307(11):1141-1142.
35. Jain A, Petty EM, Jaber RM, et al. What is appropriate to post on social media? Ratings from students, faculty members and the public. Med Educ. 2014;48(2):157-169.
36. Gabbard GO, Roberts LW, Crisp-Han H, et al. Professionalism in psychiatry. Arlington, VA: American Psychiatric Association Publishing; 2012.
Would better policing of metabolic status help you avoid medicolegal worries?
Dear Dr. Mossman,
All the psychiatrists at our clinic agree: It is hard to remember when our patients who take an antipsychotic are due for metabolic monitoring, and it’s even harder to get many of them to follow through with timely blood tests. For many, stopping their medication would be a bad idea. If we keep a patient on an antipsychotic and a metabolic problem results, how serious is our malpractice liability risk?
Submitted by “Dr. V”
Antipsychotics, the mainstay of treatment for schizophrenia,1 put patients at risk of gaining weight and developing metabolic syndrome, including type 2 diabetes mellitus, hypertension, and dyslipidemia.2 Second-generation antipsychotics are the biggest offenders, but taking a first-generation antipsychotic also can lead to these adverse effects.3
Most psychiatrists are aware of these risks and prefer that their patients do not experience them. However, many psychiatrists neglect proper monitoring or, like Dr. V, find it hard to ensure it happens and thus worry about clinical deterioration if patients stop taking an antipsychotic.4 If you are in the same situation as Dr. V, what medicolegal risks are you facing?
To answer this question, we will:
- review the clinical guidelines and standards for monitoring metabolic effects of antipsychotics
- examine how well (or poorly) physicians adhere to these standards
- discuss what “standard of care” means and how a practice guideline affects the standard effects
- propose how psychiatrists can do better at policing the metabolic effects of antipsychotics.
I’ll be watching you: Following guidelines
Several medical specialty societies have published guidelines for monitoring the metabolic effects of antipsychotics.5-8 These guidelines instruct physicians to obtain a thorough personal and family history; consider metabolic risks when starting a medication; and monitor weight, waist circumference, blood pressure, glucose, hemoglobin A1c, and lipids at various intervals. They also advise referral for management of detected metabolic problems.
Although the recommendations seem clear, many physicians don’t follow them. A 2012 meta-analysis of 48 studies, covering >200,000 antipsychotic-treated patients, showed that baseline measurements of cholesterol, glucose, and weight occurred in <50% of cases.9 A more recent review found that, among adults with a serious mental illness, the rate of lipid testing varied from 6% to 85% and for glucose monitoring, between 18% and 75%.10 In the first years after antipsychotic monitoring guidelines were established, they had only a modest impact on practice,9,11 and some studies showed the guidelines made no difference at all.12-14
Monitoring compliance varies with the type of insurance coverage patients have but remains suboptimal among the commercially insured,11 Medicaid patients,14-16 and veterans.17,18 Studies on antipsychotic treatment in children, adolescents, patients with dementia, and patients with an intellectual disability show insufficient monitoring as well.9,14,17,19-21 The reasons for these gaps are manifold, but one commonly cited factor is uncertainty about whether the psychiatrist or primary care physician should handle monitoring.22
Every claim you stake: The ‘standard of care’
In a medical malpractice case, the party claiming injury must show that the accused physician failed to follow “the generally recognized practices and procedures which would be exercised by ordinary competent practitioners in a defendant doctor’s field of medicine under the same or similar circumstances.”23 In the studies mentioned above,9-14 a large fraction of psychiatrists—many of whom, we can presume, are “competent practitioners”—don’t follow the antipsychotic monitoring guidelines in actual practice. Could failing to follow those guidelines still be the basis for a successful lawsuit?
The answer seems to be ‘yes.’ Published legal decisions describe malpractice lawsuits alleging physicians’ failure to follow antipsychotic guidelines,24,25 and online advertisements show that attorneys believe such cases can generate a payout.26,27 This may seem odd, given what studies say about psychiatrists’ monitoring practices. But determining the “standard of care” in a malpractice case is not an empirical question; it is a legal matter that is decided based on the testimony of expert witnesses.28 Here, customary practice matters, but it’s not the whole story.
Although the standard of care against which courts measure a physician’s actions “is that of a reasonably prudent practitioner …, The degree of care actually practiced by members of the profession is only some evidence of what is reasonably prudent—it is not dispositive.”29 To support their opinion concerning the standard of care, testifying medical witnesses sometimes use practice guidelines. In this case, an explanation of why a particular guideline was chosen is crucial.30
Using guidelines to establish the standard is controversial. On one hand, using guidelines in malpractice litigation allows for some consistency about expectations of practitioners.31,32 Although guidelines are not identical to evidenced-based medicine, they generally reflect an evidence-based expert consensus about sound medical practice. If a hospital uses a guideline to train its employees, the guideline provides the courts with clear information on what should have happened.33,34 Laws in some states allow clinicians to invoke their adherence to a guideline in defense against malpractice claims.35
On the other hand, critics contend that guidelines may not set an accurate standard for the quality of care, nor do they necessarily reflect a proper balance of the conflicting interests of patients and the health care system.36 The American Psychiatric Association states that its practice guidelines “are not intended to serve or be construed as a ‘standard of medical care.’”37
Conformity is not the only measure of prudent practice, and following guidelines does not immunize a clinician from lawsuit if a particular clinical situation demands a different course of action.32 Guidelines can be costly to implement,36 compliance with guidelines generally is low,35 and national guidelines do not necessarily improve the quality of care.38 Last, relying on guidelines to determine the standard of care might stifle innovation or development of alternate approaches by silencing viewpoints.39,40 Table 133-35,39,41 (page 60)summarizes variables that make a guideline more indicative of the standard of care.
Every step you take: Better monitoring
Medical professionals often are slow to update their practice to reflect new knowledge about optimal treatment. But practice guidelines influence the court’s views about the standard of care, and Dr. V’s question shows that he and his colleagues agree that metabolic status needs to be better monitored when patients take antipsychotic drugs. The following discussion and Table 242-45 offer suggestions for how psychiatrists and their practice settings could better accomplish this.
Electronic health records (EHRs). Monitoring health indices often is the largest hurdle that health care professionals face.46 However, large health care systems with EHRs are in a good position to develop and implement automated computer routines that track which patients need monitoring and note due dates, abnormal results, and management interventions.42 Some studies suggest that monitoring rates in both inpatient47 and outpatient48 settings improve with built-in EHR reminders. However, if a system uses too many reminders, the resulting “alert fatigue” will limit their value.22 Providing individual feedback about monitoring practices may enhance physicians’ buy-in to reminder systems.48
Integrated care systems can improve patient outcomes, particularly antipsychotic monitoring. Advantages include shared funding streams, a unified medical record, coordinated scheduling of psychiatric and primary care appointments, and addressing blood-draw refusals.43 More frequent primary care visits make antipsychotic monitoring more likely.11 Ultimately, integrated care could resolve problems related to determining which clinicians are responsible for monitoring and managing adverse metabolic effects.
Third-party payers. Managed care interventions also could improve monitoring rates.44 Prior authorization often requires physicians to obtain appropriate lab work. Insurers might contact physicians with educational interventions, including free webinars, provider alerts, and letters about monitoring rates in their region. Some insurers also provide disease management programs for patients and their caregivers.
Individual and small group practices. Psychiatrists who practice outside a large health care system might designate 2 months each year as “physical health months.” In the “Let’s Get Physical” program,45 physicians were given longer appointment times during these months to address metabolic monitoring, provide education about managing side effects of medication, and encourage better diets and exercise.
Overall, the best techniques might be those implicit to good doctoring: clear and open communication with patients, effective patient education, respect of informed consent, and thorough follow-up.49
1. Mossman D, Steinberg JL. Promoting, prescribing, and pushing pills: understanding the lessons of antipsychotic drug litigation. Michigan St U J Med & Law. 2009;13:263-334.
2. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation: evaluating the risk/benefit equation and improving the standard of care. J Clin Psychopharmacol. 2004;24(5 suppl 1):S7-S14.
3. De Hert M, Schreurs V, Sweers K, et al. Typical and atypical antipsychotics differentially affect long-term incidence rates of the metabolic syndrome in first-episode patients with schizophrenia: a retrospective chart review. Schizophr Res. 2008;101(1-3):295-303.
4. Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.
5. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65(2):267-272.
6. Pappadopulos E, Macintyre JC II, Crismon ML, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. J Am Acad Child Adolesc Psychiatry. 2003;42(2):145-161.
7. Pringsheim T, Panagiotopoulos C, Davidson J, et al; CAMESA guideline group. Evidence-based recommendations for monitoring safety of second generation antipsychotics in children and youth [Erratum in: J Can Acad Adolesc Psychiatry. 2011;20(3):1-2]. J Can Acad Child Adolesc Psychiatry. 2011;20(3):218-233.
8. Gleason MM, Egger HL, Emslie GJ, et al. Psychopharmacological treatment for very young children: contexts and guidelines. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1532-1572.
9. Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychol Med. 2012;42(1):125-147.
10. Baller JB, McGinty EE, Azrin ST, et al. Screening for cardiovascular risk factors in adults with serious mental illness: a review of the evidence. BMC Psychiatry. 2015;15:55.
11. Haupt DW, Rosenblatt LC, Kim E, et al. Prevalence and predictors of lipid monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166(3):345-353.
12. Dhamane AD, Martin BC, Brixner DI, et al. Metabolic monitoring of patients prescribed second-generation antipsychotics. J Psychiatr Pract. 2013;19(5):360-374.
13. Morrato EH, Newcomer JW, Kamat S, et al. Metabolic screening after the American Diabetes Association’s consensus statement on antipsychotic drugs and diabetes. Diabetes Care. 2009;32(6):1037-1042.
14. Morrato EH, Druss B, Hartung DM, et al. Metabolic testing rates in 3 state Medicaid programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Arch Gen Psychiatry. 2010;67(1):17-24.
15. Moeller KE, Rigler SK, Mayorga A, et al. Quality of monitoring for metabolic effects associated with second generation antipsychotics in patients with schizophrenia on public insurance. Schizophr Res. 2011;126(1-3):117-123.
16. Barnett M, VonMuenster S, Wehring H, et al. Assessment of monitoring for glucose and lipid dysregulation in adult Medi-Cal patients newly started on antipsychotics. Ann Clin Psychiatry. 2010;22(1):9-18.
17. Mittal D, Li C, Viverito K, et al. Monitoring for metabolic side effects among outpatients with dementia receiving antipsychotics. Psychiatr Serv. 2014;65(9):1147-1153.
18. Hsu C, Ried LD, Bengtson MA, et al. Metabolic monitoring in veterans with schizophrenia-related disorders and treated with second-generation antipsychotics: findings from a Veterans Affairs-based population. J Am Pharm Assoc. 2008;48(3):393-400.
19. Raebel MA, Penfold R, McMahon AW, et al. Adherence to guidelines for glucose assessment in starting second-generation antipsychotics. Pediatrics. 2014;134(5):e1308-e1314.
20. Connolly JG, Toomey TJ, Schneeweiss MC. Metabolic monitoring for youths initiating use of second-generation antipsychotics, 2003-2011. Psychiatr Serv. 2015;66(6):604-609.
21. Teeluckdharry S, Sharma S, O’Rourke E, et al. Monitoring metabolic side effects of atypical antipsychotics in people with an intellectual disability. J Intellect Disabil. 2013;17(3):223-235.
22. Lee J, Dalack GW, Casher MI, et al. Persistence of metabolic monitoring for psychiatry inpatients treated with second-generation antipsychotics utilizing a computer-based intervention. J Clin Pharm Ther. 2016;41(2):209-213.
23. McCourt v Abernathy, 457 SE2d 603 (SC 1995).
24. Schultz v AstraZeneca Pharma LP, LEXIS 94534, 2006 WL 3797932, (ND Cal 2006).
25. Redmond v AstraZeneca Pharma LP, 492 F Supp 2d 575 (SD Miss 2007).
26. Goguen D. Risperdal, Seroquel, Symbyax, Zyprexa, and other antipsychotic drugs. http://www.nolo.com/legal-encyclopedia/risperdal-seroquel-symbyax-zyprexa-antipsychotics-29866.html. Accessed April 4, 2016.
27. FreeAdvice staff. Risperdal medical malpractice lawsuits: Risperdal injury lawyer explains what you need to know. http://injury-law.freeadvice.com/injury-law/drug-toxic_chemicals/risperdal.htm. Accessed April 4, 2016.
28. Lewis MK, Gohagan JK, Merenstein DJ. The locality rule and the physician’s dilemma: local medical practices vs the national standard of care. JAMA. 2007;297(23):2633-2637.
29. Harris v Groth, 99 Wn2d 438, 663 P2d 113 (1983).
30. Moffett P, Moore G. The standard of care: legal history and definitions: the bad and good news. West J Emerg Med. 2011;12(1):109-112.
31. Taylor C. The use of clinical practice guidelines in determining standard of care. J Legal Med. 2014;35(2):273-290.
32. Bal BS, Brenner LH. Medicolegal sidebar: the law and social values: conformity to norms. Clin Orthop Relat Res. 2015;473(5):1555-1559.
33. Recupero PR. Clinical practice guidelines as learned treatises: understanding their use as evidence in the courtroom. J Am Acad Psychiatry Law. 2008;36(3):290-301.
34. Price v Cleveland Clinic Found, 515 NE2d 931 (Ohio Ct App 1986).
35. Zonana H. Commentary: when is a practice guideline only a guideline? J Am Acad Psychiatry Law. 2008;36(3):302-305.
36. Guillod O. Clinical guidelines and professional liability: a short comment from the legal side. ORL J Otorhinolaryngol Relat Spec. 2010;72(3):133-136; discussion 136-137.
37. American Psychiatric Association. Practice guidelines for the psychiatric evaluation of adults. 3rd ed. Arlington, VA: American Psychiatric Association; 2016.
38. Brouwers MC, Kho ME, Browman GP, et al; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839-E842.
39. Vermaas AM. Liability in relation to the use of professional medical guidelines. Med Law. 2003;22(2):233-238.
40. Strauss DC, Thomas JM. What does the medical profession mean by “standard of care?”. J Clin Oncol. 2009;27(32):e192-e193.
41. Kozlick D. Clinical practice guidelines and the legal standard of care: warnings, predictions, and interdisciplinary encounters. Health Law J. 2011;19:125-151.
42. Owen RR, Drummond KL, Viverito KM, et al. Monitoring and managing metabolic effects of antipsychotics: a cluster randomized trial of an intervention combining evidence-based quality improvement and external facilitation. Implement Sci. 2013;8:120.
43. Ruiz LM, Damron M, Jones KB, et al. Antipsychotic use and metabolic monitoring in individuals with developmental disabilities served in a Medicaid medical home [published online January 27, 2016]. J Autism Dev Disord. doi: 10.1007/s10803-016-2712-x.
44. Edelsohn GA, Parthasarathy M, Terhorst L, et al. Measurement of metabolic monitoring in youth and adult Medicaid recipients prescribed antipsychotics. J Manag Care Spec Pharm. 2015;21(9):769-77,777a-777cc.
45. Wilson E, Randall C, Patterson S, et al. Monitoring and management of metabolic abnormalities: mixed-method evaluation of a successful intervention. Australas Psychiatry. 2014;22(3):248-253.
46. Cohn TA, Sernyak MJ. Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry. 2006;51(8):492-501.
47. DelMonte MT, Bostwick JR, Bess JD, et al. Evaluation of a computer-based intervention to enhance metabolic monitoring in psychiatry inpatients treated with second-generation antipsychotics. J Clin Pharm Ther. 2012;37(6):668-673.
48. Lai CL, Chan HY, Pan YJ, et al. The effectiveness of a computer reminder system for laboratory monitoring of metabolic syndrome in schizophrenic outpatients using second-generation antipsychotics. Pharmacopsychiatry. 2015;48(1):25-29.
49. Bailey RK, Adams JB, Unger DM. Atypical antipsychotics: a case study in new era risk management. J Psychiatr Pract. 2006;12(4):253-258.
Dear Dr. Mossman,
All the psychiatrists at our clinic agree: It is hard to remember when our patients who take an antipsychotic are due for metabolic monitoring, and it’s even harder to get many of them to follow through with timely blood tests. For many, stopping their medication would be a bad idea. If we keep a patient on an antipsychotic and a metabolic problem results, how serious is our malpractice liability risk?
Submitted by “Dr. V”
Antipsychotics, the mainstay of treatment for schizophrenia,1 put patients at risk of gaining weight and developing metabolic syndrome, including type 2 diabetes mellitus, hypertension, and dyslipidemia.2 Second-generation antipsychotics are the biggest offenders, but taking a first-generation antipsychotic also can lead to these adverse effects.3
Most psychiatrists are aware of these risks and prefer that their patients do not experience them. However, many psychiatrists neglect proper monitoring or, like Dr. V, find it hard to ensure it happens and thus worry about clinical deterioration if patients stop taking an antipsychotic.4 If you are in the same situation as Dr. V, what medicolegal risks are you facing?
To answer this question, we will:
- review the clinical guidelines and standards for monitoring metabolic effects of antipsychotics
- examine how well (or poorly) physicians adhere to these standards
- discuss what “standard of care” means and how a practice guideline affects the standard effects
- propose how psychiatrists can do better at policing the metabolic effects of antipsychotics.
I’ll be watching you: Following guidelines
Several medical specialty societies have published guidelines for monitoring the metabolic effects of antipsychotics.5-8 These guidelines instruct physicians to obtain a thorough personal and family history; consider metabolic risks when starting a medication; and monitor weight, waist circumference, blood pressure, glucose, hemoglobin A1c, and lipids at various intervals. They also advise referral for management of detected metabolic problems.
Although the recommendations seem clear, many physicians don’t follow them. A 2012 meta-analysis of 48 studies, covering >200,000 antipsychotic-treated patients, showed that baseline measurements of cholesterol, glucose, and weight occurred in <50% of cases.9 A more recent review found that, among adults with a serious mental illness, the rate of lipid testing varied from 6% to 85% and for glucose monitoring, between 18% and 75%.10 In the first years after antipsychotic monitoring guidelines were established, they had only a modest impact on practice,9,11 and some studies showed the guidelines made no difference at all.12-14
Monitoring compliance varies with the type of insurance coverage patients have but remains suboptimal among the commercially insured,11 Medicaid patients,14-16 and veterans.17,18 Studies on antipsychotic treatment in children, adolescents, patients with dementia, and patients with an intellectual disability show insufficient monitoring as well.9,14,17,19-21 The reasons for these gaps are manifold, but one commonly cited factor is uncertainty about whether the psychiatrist or primary care physician should handle monitoring.22
Every claim you stake: The ‘standard of care’
In a medical malpractice case, the party claiming injury must show that the accused physician failed to follow “the generally recognized practices and procedures which would be exercised by ordinary competent practitioners in a defendant doctor’s field of medicine under the same or similar circumstances.”23 In the studies mentioned above,9-14 a large fraction of psychiatrists—many of whom, we can presume, are “competent practitioners”—don’t follow the antipsychotic monitoring guidelines in actual practice. Could failing to follow those guidelines still be the basis for a successful lawsuit?
The answer seems to be ‘yes.’ Published legal decisions describe malpractice lawsuits alleging physicians’ failure to follow antipsychotic guidelines,24,25 and online advertisements show that attorneys believe such cases can generate a payout.26,27 This may seem odd, given what studies say about psychiatrists’ monitoring practices. But determining the “standard of care” in a malpractice case is not an empirical question; it is a legal matter that is decided based on the testimony of expert witnesses.28 Here, customary practice matters, but it’s not the whole story.
Although the standard of care against which courts measure a physician’s actions “is that of a reasonably prudent practitioner …, The degree of care actually practiced by members of the profession is only some evidence of what is reasonably prudent—it is not dispositive.”29 To support their opinion concerning the standard of care, testifying medical witnesses sometimes use practice guidelines. In this case, an explanation of why a particular guideline was chosen is crucial.30
Using guidelines to establish the standard is controversial. On one hand, using guidelines in malpractice litigation allows for some consistency about expectations of practitioners.31,32 Although guidelines are not identical to evidenced-based medicine, they generally reflect an evidence-based expert consensus about sound medical practice. If a hospital uses a guideline to train its employees, the guideline provides the courts with clear information on what should have happened.33,34 Laws in some states allow clinicians to invoke their adherence to a guideline in defense against malpractice claims.35
On the other hand, critics contend that guidelines may not set an accurate standard for the quality of care, nor do they necessarily reflect a proper balance of the conflicting interests of patients and the health care system.36 The American Psychiatric Association states that its practice guidelines “are not intended to serve or be construed as a ‘standard of medical care.’”37
Conformity is not the only measure of prudent practice, and following guidelines does not immunize a clinician from lawsuit if a particular clinical situation demands a different course of action.32 Guidelines can be costly to implement,36 compliance with guidelines generally is low,35 and national guidelines do not necessarily improve the quality of care.38 Last, relying on guidelines to determine the standard of care might stifle innovation or development of alternate approaches by silencing viewpoints.39,40 Table 133-35,39,41 (page 60)summarizes variables that make a guideline more indicative of the standard of care.
Every step you take: Better monitoring
Medical professionals often are slow to update their practice to reflect new knowledge about optimal treatment. But practice guidelines influence the court’s views about the standard of care, and Dr. V’s question shows that he and his colleagues agree that metabolic status needs to be better monitored when patients take antipsychotic drugs. The following discussion and Table 242-45 offer suggestions for how psychiatrists and their practice settings could better accomplish this.
Electronic health records (EHRs). Monitoring health indices often is the largest hurdle that health care professionals face.46 However, large health care systems with EHRs are in a good position to develop and implement automated computer routines that track which patients need monitoring and note due dates, abnormal results, and management interventions.42 Some studies suggest that monitoring rates in both inpatient47 and outpatient48 settings improve with built-in EHR reminders. However, if a system uses too many reminders, the resulting “alert fatigue” will limit their value.22 Providing individual feedback about monitoring practices may enhance physicians’ buy-in to reminder systems.48
Integrated care systems can improve patient outcomes, particularly antipsychotic monitoring. Advantages include shared funding streams, a unified medical record, coordinated scheduling of psychiatric and primary care appointments, and addressing blood-draw refusals.43 More frequent primary care visits make antipsychotic monitoring more likely.11 Ultimately, integrated care could resolve problems related to determining which clinicians are responsible for monitoring and managing adverse metabolic effects.
Third-party payers. Managed care interventions also could improve monitoring rates.44 Prior authorization often requires physicians to obtain appropriate lab work. Insurers might contact physicians with educational interventions, including free webinars, provider alerts, and letters about monitoring rates in their region. Some insurers also provide disease management programs for patients and their caregivers.
Individual and small group practices. Psychiatrists who practice outside a large health care system might designate 2 months each year as “physical health months.” In the “Let’s Get Physical” program,45 physicians were given longer appointment times during these months to address metabolic monitoring, provide education about managing side effects of medication, and encourage better diets and exercise.
Overall, the best techniques might be those implicit to good doctoring: clear and open communication with patients, effective patient education, respect of informed consent, and thorough follow-up.49
Dear Dr. Mossman,
All the psychiatrists at our clinic agree: It is hard to remember when our patients who take an antipsychotic are due for metabolic monitoring, and it’s even harder to get many of them to follow through with timely blood tests. For many, stopping their medication would be a bad idea. If we keep a patient on an antipsychotic and a metabolic problem results, how serious is our malpractice liability risk?
Submitted by “Dr. V”
Antipsychotics, the mainstay of treatment for schizophrenia,1 put patients at risk of gaining weight and developing metabolic syndrome, including type 2 diabetes mellitus, hypertension, and dyslipidemia.2 Second-generation antipsychotics are the biggest offenders, but taking a first-generation antipsychotic also can lead to these adverse effects.3
Most psychiatrists are aware of these risks and prefer that their patients do not experience them. However, many psychiatrists neglect proper monitoring or, like Dr. V, find it hard to ensure it happens and thus worry about clinical deterioration if patients stop taking an antipsychotic.4 If you are in the same situation as Dr. V, what medicolegal risks are you facing?
To answer this question, we will:
- review the clinical guidelines and standards for monitoring metabolic effects of antipsychotics
- examine how well (or poorly) physicians adhere to these standards
- discuss what “standard of care” means and how a practice guideline affects the standard effects
- propose how psychiatrists can do better at policing the metabolic effects of antipsychotics.
I’ll be watching you: Following guidelines
Several medical specialty societies have published guidelines for monitoring the metabolic effects of antipsychotics.5-8 These guidelines instruct physicians to obtain a thorough personal and family history; consider metabolic risks when starting a medication; and monitor weight, waist circumference, blood pressure, glucose, hemoglobin A1c, and lipids at various intervals. They also advise referral for management of detected metabolic problems.
Although the recommendations seem clear, many physicians don’t follow them. A 2012 meta-analysis of 48 studies, covering >200,000 antipsychotic-treated patients, showed that baseline measurements of cholesterol, glucose, and weight occurred in <50% of cases.9 A more recent review found that, among adults with a serious mental illness, the rate of lipid testing varied from 6% to 85% and for glucose monitoring, between 18% and 75%.10 In the first years after antipsychotic monitoring guidelines were established, they had only a modest impact on practice,9,11 and some studies showed the guidelines made no difference at all.12-14
Monitoring compliance varies with the type of insurance coverage patients have but remains suboptimal among the commercially insured,11 Medicaid patients,14-16 and veterans.17,18 Studies on antipsychotic treatment in children, adolescents, patients with dementia, and patients with an intellectual disability show insufficient monitoring as well.9,14,17,19-21 The reasons for these gaps are manifold, but one commonly cited factor is uncertainty about whether the psychiatrist or primary care physician should handle monitoring.22
Every claim you stake: The ‘standard of care’
In a medical malpractice case, the party claiming injury must show that the accused physician failed to follow “the generally recognized practices and procedures which would be exercised by ordinary competent practitioners in a defendant doctor’s field of medicine under the same or similar circumstances.”23 In the studies mentioned above,9-14 a large fraction of psychiatrists—many of whom, we can presume, are “competent practitioners”—don’t follow the antipsychotic monitoring guidelines in actual practice. Could failing to follow those guidelines still be the basis for a successful lawsuit?
The answer seems to be ‘yes.’ Published legal decisions describe malpractice lawsuits alleging physicians’ failure to follow antipsychotic guidelines,24,25 and online advertisements show that attorneys believe such cases can generate a payout.26,27 This may seem odd, given what studies say about psychiatrists’ monitoring practices. But determining the “standard of care” in a malpractice case is not an empirical question; it is a legal matter that is decided based on the testimony of expert witnesses.28 Here, customary practice matters, but it’s not the whole story.
Although the standard of care against which courts measure a physician’s actions “is that of a reasonably prudent practitioner …, The degree of care actually practiced by members of the profession is only some evidence of what is reasonably prudent—it is not dispositive.”29 To support their opinion concerning the standard of care, testifying medical witnesses sometimes use practice guidelines. In this case, an explanation of why a particular guideline was chosen is crucial.30
Using guidelines to establish the standard is controversial. On one hand, using guidelines in malpractice litigation allows for some consistency about expectations of practitioners.31,32 Although guidelines are not identical to evidenced-based medicine, they generally reflect an evidence-based expert consensus about sound medical practice. If a hospital uses a guideline to train its employees, the guideline provides the courts with clear information on what should have happened.33,34 Laws in some states allow clinicians to invoke their adherence to a guideline in defense against malpractice claims.35
On the other hand, critics contend that guidelines may not set an accurate standard for the quality of care, nor do they necessarily reflect a proper balance of the conflicting interests of patients and the health care system.36 The American Psychiatric Association states that its practice guidelines “are not intended to serve or be construed as a ‘standard of medical care.’”37
Conformity is not the only measure of prudent practice, and following guidelines does not immunize a clinician from lawsuit if a particular clinical situation demands a different course of action.32 Guidelines can be costly to implement,36 compliance with guidelines generally is low,35 and national guidelines do not necessarily improve the quality of care.38 Last, relying on guidelines to determine the standard of care might stifle innovation or development of alternate approaches by silencing viewpoints.39,40 Table 133-35,39,41 (page 60)summarizes variables that make a guideline more indicative of the standard of care.
Every step you take: Better monitoring
Medical professionals often are slow to update their practice to reflect new knowledge about optimal treatment. But practice guidelines influence the court’s views about the standard of care, and Dr. V’s question shows that he and his colleagues agree that metabolic status needs to be better monitored when patients take antipsychotic drugs. The following discussion and Table 242-45 offer suggestions for how psychiatrists and their practice settings could better accomplish this.
Electronic health records (EHRs). Monitoring health indices often is the largest hurdle that health care professionals face.46 However, large health care systems with EHRs are in a good position to develop and implement automated computer routines that track which patients need monitoring and note due dates, abnormal results, and management interventions.42 Some studies suggest that monitoring rates in both inpatient47 and outpatient48 settings improve with built-in EHR reminders. However, if a system uses too many reminders, the resulting “alert fatigue” will limit their value.22 Providing individual feedback about monitoring practices may enhance physicians’ buy-in to reminder systems.48
Integrated care systems can improve patient outcomes, particularly antipsychotic monitoring. Advantages include shared funding streams, a unified medical record, coordinated scheduling of psychiatric and primary care appointments, and addressing blood-draw refusals.43 More frequent primary care visits make antipsychotic monitoring more likely.11 Ultimately, integrated care could resolve problems related to determining which clinicians are responsible for monitoring and managing adverse metabolic effects.
Third-party payers. Managed care interventions also could improve monitoring rates.44 Prior authorization often requires physicians to obtain appropriate lab work. Insurers might contact physicians with educational interventions, including free webinars, provider alerts, and letters about monitoring rates in their region. Some insurers also provide disease management programs for patients and their caregivers.
Individual and small group practices. Psychiatrists who practice outside a large health care system might designate 2 months each year as “physical health months.” In the “Let’s Get Physical” program,45 physicians were given longer appointment times during these months to address metabolic monitoring, provide education about managing side effects of medication, and encourage better diets and exercise.
Overall, the best techniques might be those implicit to good doctoring: clear and open communication with patients, effective patient education, respect of informed consent, and thorough follow-up.49
1. Mossman D, Steinberg JL. Promoting, prescribing, and pushing pills: understanding the lessons of antipsychotic drug litigation. Michigan St U J Med & Law. 2009;13:263-334.
2. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation: evaluating the risk/benefit equation and improving the standard of care. J Clin Psychopharmacol. 2004;24(5 suppl 1):S7-S14.
3. De Hert M, Schreurs V, Sweers K, et al. Typical and atypical antipsychotics differentially affect long-term incidence rates of the metabolic syndrome in first-episode patients with schizophrenia: a retrospective chart review. Schizophr Res. 2008;101(1-3):295-303.
4. Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.
5. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65(2):267-272.
6. Pappadopulos E, Macintyre JC II, Crismon ML, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. J Am Acad Child Adolesc Psychiatry. 2003;42(2):145-161.
7. Pringsheim T, Panagiotopoulos C, Davidson J, et al; CAMESA guideline group. Evidence-based recommendations for monitoring safety of second generation antipsychotics in children and youth [Erratum in: J Can Acad Adolesc Psychiatry. 2011;20(3):1-2]. J Can Acad Child Adolesc Psychiatry. 2011;20(3):218-233.
8. Gleason MM, Egger HL, Emslie GJ, et al. Psychopharmacological treatment for very young children: contexts and guidelines. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1532-1572.
9. Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychol Med. 2012;42(1):125-147.
10. Baller JB, McGinty EE, Azrin ST, et al. Screening for cardiovascular risk factors in adults with serious mental illness: a review of the evidence. BMC Psychiatry. 2015;15:55.
11. Haupt DW, Rosenblatt LC, Kim E, et al. Prevalence and predictors of lipid monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166(3):345-353.
12. Dhamane AD, Martin BC, Brixner DI, et al. Metabolic monitoring of patients prescribed second-generation antipsychotics. J Psychiatr Pract. 2013;19(5):360-374.
13. Morrato EH, Newcomer JW, Kamat S, et al. Metabolic screening after the American Diabetes Association’s consensus statement on antipsychotic drugs and diabetes. Diabetes Care. 2009;32(6):1037-1042.
14. Morrato EH, Druss B, Hartung DM, et al. Metabolic testing rates in 3 state Medicaid programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Arch Gen Psychiatry. 2010;67(1):17-24.
15. Moeller KE, Rigler SK, Mayorga A, et al. Quality of monitoring for metabolic effects associated with second generation antipsychotics in patients with schizophrenia on public insurance. Schizophr Res. 2011;126(1-3):117-123.
16. Barnett M, VonMuenster S, Wehring H, et al. Assessment of monitoring for glucose and lipid dysregulation in adult Medi-Cal patients newly started on antipsychotics. Ann Clin Psychiatry. 2010;22(1):9-18.
17. Mittal D, Li C, Viverito K, et al. Monitoring for metabolic side effects among outpatients with dementia receiving antipsychotics. Psychiatr Serv. 2014;65(9):1147-1153.
18. Hsu C, Ried LD, Bengtson MA, et al. Metabolic monitoring in veterans with schizophrenia-related disorders and treated with second-generation antipsychotics: findings from a Veterans Affairs-based population. J Am Pharm Assoc. 2008;48(3):393-400.
19. Raebel MA, Penfold R, McMahon AW, et al. Adherence to guidelines for glucose assessment in starting second-generation antipsychotics. Pediatrics. 2014;134(5):e1308-e1314.
20. Connolly JG, Toomey TJ, Schneeweiss MC. Metabolic monitoring for youths initiating use of second-generation antipsychotics, 2003-2011. Psychiatr Serv. 2015;66(6):604-609.
21. Teeluckdharry S, Sharma S, O’Rourke E, et al. Monitoring metabolic side effects of atypical antipsychotics in people with an intellectual disability. J Intellect Disabil. 2013;17(3):223-235.
22. Lee J, Dalack GW, Casher MI, et al. Persistence of metabolic monitoring for psychiatry inpatients treated with second-generation antipsychotics utilizing a computer-based intervention. J Clin Pharm Ther. 2016;41(2):209-213.
23. McCourt v Abernathy, 457 SE2d 603 (SC 1995).
24. Schultz v AstraZeneca Pharma LP, LEXIS 94534, 2006 WL 3797932, (ND Cal 2006).
25. Redmond v AstraZeneca Pharma LP, 492 F Supp 2d 575 (SD Miss 2007).
26. Goguen D. Risperdal, Seroquel, Symbyax, Zyprexa, and other antipsychotic drugs. http://www.nolo.com/legal-encyclopedia/risperdal-seroquel-symbyax-zyprexa-antipsychotics-29866.html. Accessed April 4, 2016.
27. FreeAdvice staff. Risperdal medical malpractice lawsuits: Risperdal injury lawyer explains what you need to know. http://injury-law.freeadvice.com/injury-law/drug-toxic_chemicals/risperdal.htm. Accessed April 4, 2016.
28. Lewis MK, Gohagan JK, Merenstein DJ. The locality rule and the physician’s dilemma: local medical practices vs the national standard of care. JAMA. 2007;297(23):2633-2637.
29. Harris v Groth, 99 Wn2d 438, 663 P2d 113 (1983).
30. Moffett P, Moore G. The standard of care: legal history and definitions: the bad and good news. West J Emerg Med. 2011;12(1):109-112.
31. Taylor C. The use of clinical practice guidelines in determining standard of care. J Legal Med. 2014;35(2):273-290.
32. Bal BS, Brenner LH. Medicolegal sidebar: the law and social values: conformity to norms. Clin Orthop Relat Res. 2015;473(5):1555-1559.
33. Recupero PR. Clinical practice guidelines as learned treatises: understanding their use as evidence in the courtroom. J Am Acad Psychiatry Law. 2008;36(3):290-301.
34. Price v Cleveland Clinic Found, 515 NE2d 931 (Ohio Ct App 1986).
35. Zonana H. Commentary: when is a practice guideline only a guideline? J Am Acad Psychiatry Law. 2008;36(3):302-305.
36. Guillod O. Clinical guidelines and professional liability: a short comment from the legal side. ORL J Otorhinolaryngol Relat Spec. 2010;72(3):133-136; discussion 136-137.
37. American Psychiatric Association. Practice guidelines for the psychiatric evaluation of adults. 3rd ed. Arlington, VA: American Psychiatric Association; 2016.
38. Brouwers MC, Kho ME, Browman GP, et al; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839-E842.
39. Vermaas AM. Liability in relation to the use of professional medical guidelines. Med Law. 2003;22(2):233-238.
40. Strauss DC, Thomas JM. What does the medical profession mean by “standard of care?”. J Clin Oncol. 2009;27(32):e192-e193.
41. Kozlick D. Clinical practice guidelines and the legal standard of care: warnings, predictions, and interdisciplinary encounters. Health Law J. 2011;19:125-151.
42. Owen RR, Drummond KL, Viverito KM, et al. Monitoring and managing metabolic effects of antipsychotics: a cluster randomized trial of an intervention combining evidence-based quality improvement and external facilitation. Implement Sci. 2013;8:120.
43. Ruiz LM, Damron M, Jones KB, et al. Antipsychotic use and metabolic monitoring in individuals with developmental disabilities served in a Medicaid medical home [published online January 27, 2016]. J Autism Dev Disord. doi: 10.1007/s10803-016-2712-x.
44. Edelsohn GA, Parthasarathy M, Terhorst L, et al. Measurement of metabolic monitoring in youth and adult Medicaid recipients prescribed antipsychotics. J Manag Care Spec Pharm. 2015;21(9):769-77,777a-777cc.
45. Wilson E, Randall C, Patterson S, et al. Monitoring and management of metabolic abnormalities: mixed-method evaluation of a successful intervention. Australas Psychiatry. 2014;22(3):248-253.
46. Cohn TA, Sernyak MJ. Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry. 2006;51(8):492-501.
47. DelMonte MT, Bostwick JR, Bess JD, et al. Evaluation of a computer-based intervention to enhance metabolic monitoring in psychiatry inpatients treated with second-generation antipsychotics. J Clin Pharm Ther. 2012;37(6):668-673.
48. Lai CL, Chan HY, Pan YJ, et al. The effectiveness of a computer reminder system for laboratory monitoring of metabolic syndrome in schizophrenic outpatients using second-generation antipsychotics. Pharmacopsychiatry. 2015;48(1):25-29.
49. Bailey RK, Adams JB, Unger DM. Atypical antipsychotics: a case study in new era risk management. J Psychiatr Pract. 2006;12(4):253-258.
1. Mossman D, Steinberg JL. Promoting, prescribing, and pushing pills: understanding the lessons of antipsychotic drug litigation. Michigan St U J Med & Law. 2009;13:263-334.
2. Nasrallah HA, Newcomer JW. Atypical antipsychotics and metabolic dysregulation: evaluating the risk/benefit equation and improving the standard of care. J Clin Psychopharmacol. 2004;24(5 suppl 1):S7-S14.
3. De Hert M, Schreurs V, Sweers K, et al. Typical and atypical antipsychotics differentially affect long-term incidence rates of the metabolic syndrome in first-episode patients with schizophrenia: a retrospective chart review. Schizophr Res. 2008;101(1-3):295-303.
4. Appelbaum PS, Gutheil TG. Clinical handbook of psychiatry and the law. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007.
5. American Diabetes Association; American Psychiatric Association; American Association of Clinical Endocrinologists; North American Association for the Study of Obesity. Consensus development conference on antipsychotic drugs and obesity and diabetes. J Clin Psychiatry. 2004;65(2):267-272.
6. Pappadopulos E, Macintyre JC II, Crismon ML, et al. Treatment recommendations for the use of antipsychotics for aggressive youth (TRAAY). Part II. J Am Acad Child Adolesc Psychiatry. 2003;42(2):145-161.
7. Pringsheim T, Panagiotopoulos C, Davidson J, et al; CAMESA guideline group. Evidence-based recommendations for monitoring safety of second generation antipsychotics in children and youth [Erratum in: J Can Acad Adolesc Psychiatry. 2011;20(3):1-2]. J Can Acad Child Adolesc Psychiatry. 2011;20(3):218-233.
8. Gleason MM, Egger HL, Emslie GJ, et al. Psychopharmacological treatment for very young children: contexts and guidelines. J Am Acad Child Adolesc Psychiatry. 2007;46(12):1532-1572.
9. Mitchell AJ, Delaffon V, Vancampfort D, et al. Guideline concordant monitoring of metabolic risk in people treated with antipsychotic medication: systematic review and meta-analysis of screening practices. Psychol Med. 2012;42(1):125-147.
10. Baller JB, McGinty EE, Azrin ST, et al. Screening for cardiovascular risk factors in adults with serious mental illness: a review of the evidence. BMC Psychiatry. 2015;15:55.
11. Haupt DW, Rosenblatt LC, Kim E, et al. Prevalence and predictors of lipid monitoring in commercially insured patients treated with second-generation antipsychotic agents. Am J Psychiatry. 2009;166(3):345-353.
12. Dhamane AD, Martin BC, Brixner DI, et al. Metabolic monitoring of patients prescribed second-generation antipsychotics. J Psychiatr Pract. 2013;19(5):360-374.
13. Morrato EH, Newcomer JW, Kamat S, et al. Metabolic screening after the American Diabetes Association’s consensus statement on antipsychotic drugs and diabetes. Diabetes Care. 2009;32(6):1037-1042.
14. Morrato EH, Druss B, Hartung DM, et al. Metabolic testing rates in 3 state Medicaid programs after FDA warnings and ADA/APA recommendations for second-generation antipsychotic drugs. Arch Gen Psychiatry. 2010;67(1):17-24.
15. Moeller KE, Rigler SK, Mayorga A, et al. Quality of monitoring for metabolic effects associated with second generation antipsychotics in patients with schizophrenia on public insurance. Schizophr Res. 2011;126(1-3):117-123.
16. Barnett M, VonMuenster S, Wehring H, et al. Assessment of monitoring for glucose and lipid dysregulation in adult Medi-Cal patients newly started on antipsychotics. Ann Clin Psychiatry. 2010;22(1):9-18.
17. Mittal D, Li C, Viverito K, et al. Monitoring for metabolic side effects among outpatients with dementia receiving antipsychotics. Psychiatr Serv. 2014;65(9):1147-1153.
18. Hsu C, Ried LD, Bengtson MA, et al. Metabolic monitoring in veterans with schizophrenia-related disorders and treated with second-generation antipsychotics: findings from a Veterans Affairs-based population. J Am Pharm Assoc. 2008;48(3):393-400.
19. Raebel MA, Penfold R, McMahon AW, et al. Adherence to guidelines for glucose assessment in starting second-generation antipsychotics. Pediatrics. 2014;134(5):e1308-e1314.
20. Connolly JG, Toomey TJ, Schneeweiss MC. Metabolic monitoring for youths initiating use of second-generation antipsychotics, 2003-2011. Psychiatr Serv. 2015;66(6):604-609.
21. Teeluckdharry S, Sharma S, O’Rourke E, et al. Monitoring metabolic side effects of atypical antipsychotics in people with an intellectual disability. J Intellect Disabil. 2013;17(3):223-235.
22. Lee J, Dalack GW, Casher MI, et al. Persistence of metabolic monitoring for psychiatry inpatients treated with second-generation antipsychotics utilizing a computer-based intervention. J Clin Pharm Ther. 2016;41(2):209-213.
23. McCourt v Abernathy, 457 SE2d 603 (SC 1995).
24. Schultz v AstraZeneca Pharma LP, LEXIS 94534, 2006 WL 3797932, (ND Cal 2006).
25. Redmond v AstraZeneca Pharma LP, 492 F Supp 2d 575 (SD Miss 2007).
26. Goguen D. Risperdal, Seroquel, Symbyax, Zyprexa, and other antipsychotic drugs. http://www.nolo.com/legal-encyclopedia/risperdal-seroquel-symbyax-zyprexa-antipsychotics-29866.html. Accessed April 4, 2016.
27. FreeAdvice staff. Risperdal medical malpractice lawsuits: Risperdal injury lawyer explains what you need to know. http://injury-law.freeadvice.com/injury-law/drug-toxic_chemicals/risperdal.htm. Accessed April 4, 2016.
28. Lewis MK, Gohagan JK, Merenstein DJ. The locality rule and the physician’s dilemma: local medical practices vs the national standard of care. JAMA. 2007;297(23):2633-2637.
29. Harris v Groth, 99 Wn2d 438, 663 P2d 113 (1983).
30. Moffett P, Moore G. The standard of care: legal history and definitions: the bad and good news. West J Emerg Med. 2011;12(1):109-112.
31. Taylor C. The use of clinical practice guidelines in determining standard of care. J Legal Med. 2014;35(2):273-290.
32. Bal BS, Brenner LH. Medicolegal sidebar: the law and social values: conformity to norms. Clin Orthop Relat Res. 2015;473(5):1555-1559.
33. Recupero PR. Clinical practice guidelines as learned treatises: understanding their use as evidence in the courtroom. J Am Acad Psychiatry Law. 2008;36(3):290-301.
34. Price v Cleveland Clinic Found, 515 NE2d 931 (Ohio Ct App 1986).
35. Zonana H. Commentary: when is a practice guideline only a guideline? J Am Acad Psychiatry Law. 2008;36(3):302-305.
36. Guillod O. Clinical guidelines and professional liability: a short comment from the legal side. ORL J Otorhinolaryngol Relat Spec. 2010;72(3):133-136; discussion 136-137.
37. American Psychiatric Association. Practice guidelines for the psychiatric evaluation of adults. 3rd ed. Arlington, VA: American Psychiatric Association; 2016.
38. Brouwers MC, Kho ME, Browman GP, et al; AGREE Next Steps Consortium. AGREE II: advancing guideline development, reporting and evaluation in health care. CMAJ. 2010;182(18):E839-E842.
39. Vermaas AM. Liability in relation to the use of professional medical guidelines. Med Law. 2003;22(2):233-238.
40. Strauss DC, Thomas JM. What does the medical profession mean by “standard of care?”. J Clin Oncol. 2009;27(32):e192-e193.
41. Kozlick D. Clinical practice guidelines and the legal standard of care: warnings, predictions, and interdisciplinary encounters. Health Law J. 2011;19:125-151.
42. Owen RR, Drummond KL, Viverito KM, et al. Monitoring and managing metabolic effects of antipsychotics: a cluster randomized trial of an intervention combining evidence-based quality improvement and external facilitation. Implement Sci. 2013;8:120.
43. Ruiz LM, Damron M, Jones KB, et al. Antipsychotic use and metabolic monitoring in individuals with developmental disabilities served in a Medicaid medical home [published online January 27, 2016]. J Autism Dev Disord. doi: 10.1007/s10803-016-2712-x.
44. Edelsohn GA, Parthasarathy M, Terhorst L, et al. Measurement of metabolic monitoring in youth and adult Medicaid recipients prescribed antipsychotics. J Manag Care Spec Pharm. 2015;21(9):769-77,777a-777cc.
45. Wilson E, Randall C, Patterson S, et al. Monitoring and management of metabolic abnormalities: mixed-method evaluation of a successful intervention. Australas Psychiatry. 2014;22(3):248-253.
46. Cohn TA, Sernyak MJ. Metabolic monitoring for patients treated with antipsychotic medications. Can J Psychiatry. 2006;51(8):492-501.
47. DelMonte MT, Bostwick JR, Bess JD, et al. Evaluation of a computer-based intervention to enhance metabolic monitoring in psychiatry inpatients treated with second-generation antipsychotics. J Clin Pharm Ther. 2012;37(6):668-673.
48. Lai CL, Chan HY, Pan YJ, et al. The effectiveness of a computer reminder system for laboratory monitoring of metabolic syndrome in schizophrenic outpatients using second-generation antipsychotics. Pharmacopsychiatry. 2015;48(1):25-29.
49. Bailey RK, Adams JB, Unger DM. Atypical antipsychotics: a case study in new era risk management. J Psychiatr Pract. 2006;12(4):253-258.
Imposing treatment on patients with eating disorders: What are the legal risks?
Dear Dr. Mossman,
At the general hospital where I perform consultations, the medical service asked me to fill out psychiatric “hold” documents to keep a severely malnourished young woman with anorexia nervosa from leaving the hospital. Ms. Q, whose body mass index (BMI) was 12 (yes, 12), came to the hospital to have her “electrolytes fixed.” She was willing to stay the night for electrolyte repletion, but insisted she could gain weight on her own at home.
I’m worried that she might die without prompt inpatient treatment; she needs to stay on the medical service. Should I fill out a psychiatric hold to keep her there? What legal risks could I face if Ms. Q is detained and force-fed against her will? What are the legal risks of letting her leave the hospital before she is medically stable?
Submitted by “Dr. F”
When a severely malnourished patient with an eating disorder arrives on a medical floor, treatment teams often ask psychiatric consultants to help them impose care the patient desperately needs but doesn’t want. This reaction is understandable. After all, an eating disorder is a psychiatric illness, and hospital-based psychiatrists have experience with treating involuntary patients. A psychiatric hold may seem like a sensible way to save the life of a hospitalized patient with a mental illness.
But filling out a psychiatric hold only scratches the surface of what a psychiatric consultant’s contribution should include; in Ms. Q’s case, initiating a psychiatric hold is probably the wrong thing to do.
Why would filling out a psychiatric hold be inappropriate for Ms. Q? What clinical factors and legal issues should a psychiatrist consider when helping medical colleagues provide unwanted treatment to a severely malnourished patient with an eating disorder? We’ll explore these matters as we consider the case of Ms. Q (Figure) and the following questions:
- What type of care is most appropriate for her now?
- Can she refuse medical treatment?
- What are the medicolegal risks of letting her leave the hospital?
- What are the medicolegal risks of detaining and force-feeding her against her will?
- When is a psychiatric “hold” appropriate?
What care is appropriate?
Given her state of self-starvation, Ms. Q’s treatment plan could require close monitoring of her electrolytes and cardiac status, as well as watching her for signs of “refeeding syndrome”—rapid, potentially fatal fluid shifts and metabolic derangements that malnourished patients could experience when they receive artificial refeeding.1
First, the physicians who are caring for Ms. Q should determine whether she needs more intensive medical supervision than is usually available on a psychiatric unit. If she does, but she won’t agree to stay on a medical unit for care, a psychiatric hold is the wrong step, for 2 reasons:
- Once a psychiatric hold has been executed, state statutes require the patient to be placed in a psychiatric facility—a state-approved psychiatric treatment setting, such as a psychiatric unit or free-standing psychiatric hospital—within a specified period.2,3 Most nonpsychiatric medical units would not meet state’s statutory definition for such a facility.
- A psychiatric hold only permits short-term detention. It does not provide legal authority to impose unwanted medical treatment.
Does Ms. Q have capacity?
In the United States, Ms. Q has a legal right to refuse medical care—even if she needs it urgently—provided that her refusal is made competently.4 As Appelbaum and Grisso5 explained in a now-classic 1988 article:
The legal standards for competence include the four related skills of communicating a choice, understanding relevant information, appreciating the current situation and its consequences, and manipulating information rationally.
The Table5 describes these abilities in more detail.
Only courts can make legal determinations of competence, so physicians refer to an evaluation of a patient’s competence-related abilities as a “capacity assessment.” The decision as to whether a patient has capacity ultimately rests with the primary treatment team; however, physicians in other specialties often enlist psychiatrists’ help with this matter because of their interviewing skills and knowledge of how mental illness can impair capacity.
No easy-to-use instrument for evaluating capacity is available. However, Appelbaum6 provides examples of questions that often prove useful in such assessments, and a review by Sessums et al7 on several capacity evaluation tools suggests that the Aid to Capacity Evaluation8 may be the best instrument for performing capacity assessments.
Patients with anorexia nervosa often differ substantially from healthy people in how they assign values to life and death,9 which can make it difficult to evaluate their capacity to refuse life-saving treatment. Malnutrition can alter patients’ ability to think clearly, a phenomenon that some patients with anorexia mention as a reason they are grateful (in retrospect) for the compulsory treatment they received.10 Yet, if an evaluation shows that the patient has the decision-making capacity to refuse care, then her (his) caregivers should carefully document this conclusion and the basis for it. Although caregivers might encourage her to accept the treatment they believe she needs, they should not provide treatment that conflicts with their patient’s wishes.
If evaluation shows that the patient lacks capacity, however, the findings that support this conclusion should be documented clearly. The team then should consult the hospital attorney to determine how to best proceed. The attorney might recommend that a physician on the primary treatment team initiate a “medical hold”—an order that the patient may not leave against medical advice (AMA)—and then seek an emergency guardianship to permit medical treatment, such as refeeding.
To treat or not to treat?
What are the legal risks of allowing Ms. Q to leave AMA before she reaches medical stability?
Powers and Cloak11 describe a case of a 26-year-old woman with anorexia nervosa who came to the hospital with dizziness, weakness, and a very low blood glucose level. She was discharged after 6 days without having received any feeding, only to return to the emergency department 2 days later. This time, she had a letter from her physician stating that she needed medical supervision to start refeeding, yet she was discharged from the emergency department within a few hours. She was re-admitted to the hospital the next day.
Powers and Cloak11 do not report this woman’s medical outcome. But what if she had suffered a fatal cardiac arrhythmia before her third presentation to the emergency department or suffered another injury attributable to her nutritional state: Could her physicians be found at fault?
On Cohen & Associates’ Web site, they essentially answer, “Yes.” They describe a case of “Miss McIntosh,” who had anorexia nervosa and was discharged home from a hospital despite “chronic metabolic problems and not eating properly.” She went into a “hypoglycemic encephalopathic coma” and “suffered irreversible brain damage.” A subsequent lawsuit against the hospital resulted in a 7-figure settlement,12 illustrating the potential for adverse medicolegal consequences if failure to treat a patient with anorexia nervosa could be linked to subsequent physical harm. On the other hand, could a patient with anorexia who is being force-fed take legal action against her providers? At least 3 recent British cases suggest that this is possible.13-15 A British medical student with anorexia, E, made an emergency application to the Court of Protection in London, claiming that being fed against her will was akin to reliving her past experience of sexual abuse. In E’s case, the judge ruled “that the balance tips slowly but unmistakably in the direction of life preserving treatment” and authorized feeding over her objection.6 In 2 other cases, however, British courts have ruled that force-feeding anorexic patients would be futile and disallowed the practice.14,15
Faced with possible legal action, no matter what course you take, how should you respond? Getting legal and ethical consultation is prudent if time allows. In many cases, hospital attorneys might prefer that physicians err on the side of preserving life(D. Vanderpool, MBA, JD, personal communication, February 3, 2016)—even if that means detaining a patient without clear legal authorization to do so—because attorneys would prefer to defend a doctor who acted to save someone’s life than to defend a doctor who knowingly allowed a patient to die.
When might persons with an eating disorder be civilly committed?
Suppose that Ms. Q does not need urgent nonpsychiatric medical care, or that her life-threatening physical problems now have been addressed. Her physicians strongly recommend that she undergo inpatient psychiatric treatment for her eating disorder, but she wants to leave. Would it now be appropriate to fill out paperwork to initiate a psychiatric hold?
All U.S. jurisdictions authorize “civil commitment” proceedings that can lead to involuntary psychiatric hospitalization of people who have a mental disorder and pose a risk to themselves or others because of the disorder.16
In general, to be subject to civil commitment, a person must have a substantial disorder of thought, mood, perception, orientation, or memory. In addition, that disorder must grossly impair her (his) judgment, behavior, reality testing, or ability to meet the demands of everyday life.17
People with psychosis, a severe mood disorder, or dementia often meet these criteria. However, psychiatrists do not usually consider anorexia nervosa to be a thought disorder, mood disorder, or memory disorder. Does this mean that people with anorexia nervosa cannot meet the “substantial” mental disorder criterion?
It does not. Courts interpret the words in statutes based on their “ordinary and natural meaning.”18 If Ms. Q perceived herself as fat, despite having a BMI that was far below the healthy range, most people would regard her thinking to be disordered. If, in addition, her mental disorder impaired her “judgment, behavior, and capacity to meet the ordinary demands of sustaining existence,” then her anorexia nervosa “would qualify as a mental disorder for commitment purposes.”19
To be subject to civil commitment, a person with a substantial mental disorder also must pose a risk of harm to herself or others because of the disorder. That risk can be evidenced via an action, attempt, or threat to do direct physical harm, or it might inhere in the potential for developing grave disability through neglect of one’s basic needs, such as failing to eat adequately. In Ms. Q’s case, if the evidence shows her eating-disordered behavior has placed her at imminent risk of permanent injury or death, she has satisfied the legal criteria that justify court-ordered psychiatric hospitalization.
Bottom Line
When a severely malnourished patient with anorexia nervosa does not agree to allow recommended care, an appropriate clinical response should include judgment about the urgency of the proposed treatment, what treatment setting is best suited to the patient’s condition, and whether the patient has the mental capacity to refuse potentially life-saving care.
1. Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008;336(7659):1495-1498.
2. Ohio Revised Code §5122.01(F).
3. Oregon Revised Statutes §426.005(c).
4. Schloendorff v Society of New York Hospital, 211 N.Y. 125, 105 N.E. 92 (N1914).
5. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
6. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
7. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-427.
8. Community tools: Aid to Capacity Evaluation (ACE). University of Toronto Joint Centre for Bioethics. http://www.jcb.utoronto.ca/tools/ace_download.shtml. Updated May 8, 2008. Accessed December 21, 2015.
9. Tan J, Hope T, Stewart A. Competence to refuse treatment in anorexia nervosa. Int J Law Psychiatry. 2003;26(6):697-707.
10. Elzakkers IF, Danner UN, Hoek HW, et al. Compulsory treatment in anorexia nervosa: a review. Int J Eat Disord. 2014;47(8):845-852.
11. Powers PS, Cloak NL. Failure to feed patients with anorexia nervosa and other perils and perplexities in the medical care of eating disorder patients. Eat Disord. 2013;21(1):81-89.
12. “Failure to properly treat anorexia nervosa.” Harry S. Cohen & Associates. http://medmal1.com/article/failure-to-properly-treat-anorexia-nervosa. Accessed February 1, 2016.
13. A Local Authority v E. and Others [2012] EWHC 1639 (COP).
14. A NHS Foundation Trust v Ms. X [2014] EWCOP 35.
15. NHS Trust v L [2012] EWHC 2741 (COP).
16. Pinals DA, Mossman D. Evaluation for civil commitment. New York, NY: Oxford University Press; 2011.
17. Castellano-Hoyt DW. Enhancing police response to persons in mental health crisis: providing strategies, communication techniques, and crisis intervention preparation in overcoming institutional challenges. Springfield, IL: Charles C. Thomas Publisher, Ltd; 2003.
18. FDIC v Meyer, 510 U.S. 471 (1994).
19. Appelbaum PS, Rumpf T. Civil commitment of the anorexic patient. Gen Hosp Psychiatry. 1998;20(4):225-230.
Dear Dr. Mossman,
At the general hospital where I perform consultations, the medical service asked me to fill out psychiatric “hold” documents to keep a severely malnourished young woman with anorexia nervosa from leaving the hospital. Ms. Q, whose body mass index (BMI) was 12 (yes, 12), came to the hospital to have her “electrolytes fixed.” She was willing to stay the night for electrolyte repletion, but insisted she could gain weight on her own at home.
I’m worried that she might die without prompt inpatient treatment; she needs to stay on the medical service. Should I fill out a psychiatric hold to keep her there? What legal risks could I face if Ms. Q is detained and force-fed against her will? What are the legal risks of letting her leave the hospital before she is medically stable?
Submitted by “Dr. F”
When a severely malnourished patient with an eating disorder arrives on a medical floor, treatment teams often ask psychiatric consultants to help them impose care the patient desperately needs but doesn’t want. This reaction is understandable. After all, an eating disorder is a psychiatric illness, and hospital-based psychiatrists have experience with treating involuntary patients. A psychiatric hold may seem like a sensible way to save the life of a hospitalized patient with a mental illness.
But filling out a psychiatric hold only scratches the surface of what a psychiatric consultant’s contribution should include; in Ms. Q’s case, initiating a psychiatric hold is probably the wrong thing to do.
Why would filling out a psychiatric hold be inappropriate for Ms. Q? What clinical factors and legal issues should a psychiatrist consider when helping medical colleagues provide unwanted treatment to a severely malnourished patient with an eating disorder? We’ll explore these matters as we consider the case of Ms. Q (Figure) and the following questions:
- What type of care is most appropriate for her now?
- Can she refuse medical treatment?
- What are the medicolegal risks of letting her leave the hospital?
- What are the medicolegal risks of detaining and force-feeding her against her will?
- When is a psychiatric “hold” appropriate?
What care is appropriate?
Given her state of self-starvation, Ms. Q’s treatment plan could require close monitoring of her electrolytes and cardiac status, as well as watching her for signs of “refeeding syndrome”—rapid, potentially fatal fluid shifts and metabolic derangements that malnourished patients could experience when they receive artificial refeeding.1
First, the physicians who are caring for Ms. Q should determine whether she needs more intensive medical supervision than is usually available on a psychiatric unit. If she does, but she won’t agree to stay on a medical unit for care, a psychiatric hold is the wrong step, for 2 reasons:
- Once a psychiatric hold has been executed, state statutes require the patient to be placed in a psychiatric facility—a state-approved psychiatric treatment setting, such as a psychiatric unit or free-standing psychiatric hospital—within a specified period.2,3 Most nonpsychiatric medical units would not meet state’s statutory definition for such a facility.
- A psychiatric hold only permits short-term detention. It does not provide legal authority to impose unwanted medical treatment.
Does Ms. Q have capacity?
In the United States, Ms. Q has a legal right to refuse medical care—even if she needs it urgently—provided that her refusal is made competently.4 As Appelbaum and Grisso5 explained in a now-classic 1988 article:
The legal standards for competence include the four related skills of communicating a choice, understanding relevant information, appreciating the current situation and its consequences, and manipulating information rationally.
The Table5 describes these abilities in more detail.
Only courts can make legal determinations of competence, so physicians refer to an evaluation of a patient’s competence-related abilities as a “capacity assessment.” The decision as to whether a patient has capacity ultimately rests with the primary treatment team; however, physicians in other specialties often enlist psychiatrists’ help with this matter because of their interviewing skills and knowledge of how mental illness can impair capacity.
No easy-to-use instrument for evaluating capacity is available. However, Appelbaum6 provides examples of questions that often prove useful in such assessments, and a review by Sessums et al7 on several capacity evaluation tools suggests that the Aid to Capacity Evaluation8 may be the best instrument for performing capacity assessments.
Patients with anorexia nervosa often differ substantially from healthy people in how they assign values to life and death,9 which can make it difficult to evaluate their capacity to refuse life-saving treatment. Malnutrition can alter patients’ ability to think clearly, a phenomenon that some patients with anorexia mention as a reason they are grateful (in retrospect) for the compulsory treatment they received.10 Yet, if an evaluation shows that the patient has the decision-making capacity to refuse care, then her (his) caregivers should carefully document this conclusion and the basis for it. Although caregivers might encourage her to accept the treatment they believe she needs, they should not provide treatment that conflicts with their patient’s wishes.
If evaluation shows that the patient lacks capacity, however, the findings that support this conclusion should be documented clearly. The team then should consult the hospital attorney to determine how to best proceed. The attorney might recommend that a physician on the primary treatment team initiate a “medical hold”—an order that the patient may not leave against medical advice (AMA)—and then seek an emergency guardianship to permit medical treatment, such as refeeding.
To treat or not to treat?
What are the legal risks of allowing Ms. Q to leave AMA before she reaches medical stability?
Powers and Cloak11 describe a case of a 26-year-old woman with anorexia nervosa who came to the hospital with dizziness, weakness, and a very low blood glucose level. She was discharged after 6 days without having received any feeding, only to return to the emergency department 2 days later. This time, she had a letter from her physician stating that she needed medical supervision to start refeeding, yet she was discharged from the emergency department within a few hours. She was re-admitted to the hospital the next day.
Powers and Cloak11 do not report this woman’s medical outcome. But what if she had suffered a fatal cardiac arrhythmia before her third presentation to the emergency department or suffered another injury attributable to her nutritional state: Could her physicians be found at fault?
On Cohen & Associates’ Web site, they essentially answer, “Yes.” They describe a case of “Miss McIntosh,” who had anorexia nervosa and was discharged home from a hospital despite “chronic metabolic problems and not eating properly.” She went into a “hypoglycemic encephalopathic coma” and “suffered irreversible brain damage.” A subsequent lawsuit against the hospital resulted in a 7-figure settlement,12 illustrating the potential for adverse medicolegal consequences if failure to treat a patient with anorexia nervosa could be linked to subsequent physical harm. On the other hand, could a patient with anorexia who is being force-fed take legal action against her providers? At least 3 recent British cases suggest that this is possible.13-15 A British medical student with anorexia, E, made an emergency application to the Court of Protection in London, claiming that being fed against her will was akin to reliving her past experience of sexual abuse. In E’s case, the judge ruled “that the balance tips slowly but unmistakably in the direction of life preserving treatment” and authorized feeding over her objection.6 In 2 other cases, however, British courts have ruled that force-feeding anorexic patients would be futile and disallowed the practice.14,15
Faced with possible legal action, no matter what course you take, how should you respond? Getting legal and ethical consultation is prudent if time allows. In many cases, hospital attorneys might prefer that physicians err on the side of preserving life(D. Vanderpool, MBA, JD, personal communication, February 3, 2016)—even if that means detaining a patient without clear legal authorization to do so—because attorneys would prefer to defend a doctor who acted to save someone’s life than to defend a doctor who knowingly allowed a patient to die.
When might persons with an eating disorder be civilly committed?
Suppose that Ms. Q does not need urgent nonpsychiatric medical care, or that her life-threatening physical problems now have been addressed. Her physicians strongly recommend that she undergo inpatient psychiatric treatment for her eating disorder, but she wants to leave. Would it now be appropriate to fill out paperwork to initiate a psychiatric hold?
All U.S. jurisdictions authorize “civil commitment” proceedings that can lead to involuntary psychiatric hospitalization of people who have a mental disorder and pose a risk to themselves or others because of the disorder.16
In general, to be subject to civil commitment, a person must have a substantial disorder of thought, mood, perception, orientation, or memory. In addition, that disorder must grossly impair her (his) judgment, behavior, reality testing, or ability to meet the demands of everyday life.17
People with psychosis, a severe mood disorder, or dementia often meet these criteria. However, psychiatrists do not usually consider anorexia nervosa to be a thought disorder, mood disorder, or memory disorder. Does this mean that people with anorexia nervosa cannot meet the “substantial” mental disorder criterion?
It does not. Courts interpret the words in statutes based on their “ordinary and natural meaning.”18 If Ms. Q perceived herself as fat, despite having a BMI that was far below the healthy range, most people would regard her thinking to be disordered. If, in addition, her mental disorder impaired her “judgment, behavior, and capacity to meet the ordinary demands of sustaining existence,” then her anorexia nervosa “would qualify as a mental disorder for commitment purposes.”19
To be subject to civil commitment, a person with a substantial mental disorder also must pose a risk of harm to herself or others because of the disorder. That risk can be evidenced via an action, attempt, or threat to do direct physical harm, or it might inhere in the potential for developing grave disability through neglect of one’s basic needs, such as failing to eat adequately. In Ms. Q’s case, if the evidence shows her eating-disordered behavior has placed her at imminent risk of permanent injury or death, she has satisfied the legal criteria that justify court-ordered psychiatric hospitalization.
Bottom Line
When a severely malnourished patient with anorexia nervosa does not agree to allow recommended care, an appropriate clinical response should include judgment about the urgency of the proposed treatment, what treatment setting is best suited to the patient’s condition, and whether the patient has the mental capacity to refuse potentially life-saving care.
Dear Dr. Mossman,
At the general hospital where I perform consultations, the medical service asked me to fill out psychiatric “hold” documents to keep a severely malnourished young woman with anorexia nervosa from leaving the hospital. Ms. Q, whose body mass index (BMI) was 12 (yes, 12), came to the hospital to have her “electrolytes fixed.” She was willing to stay the night for electrolyte repletion, but insisted she could gain weight on her own at home.
I’m worried that she might die without prompt inpatient treatment; she needs to stay on the medical service. Should I fill out a psychiatric hold to keep her there? What legal risks could I face if Ms. Q is detained and force-fed against her will? What are the legal risks of letting her leave the hospital before she is medically stable?
Submitted by “Dr. F”
When a severely malnourished patient with an eating disorder arrives on a medical floor, treatment teams often ask psychiatric consultants to help them impose care the patient desperately needs but doesn’t want. This reaction is understandable. After all, an eating disorder is a psychiatric illness, and hospital-based psychiatrists have experience with treating involuntary patients. A psychiatric hold may seem like a sensible way to save the life of a hospitalized patient with a mental illness.
But filling out a psychiatric hold only scratches the surface of what a psychiatric consultant’s contribution should include; in Ms. Q’s case, initiating a psychiatric hold is probably the wrong thing to do.
Why would filling out a psychiatric hold be inappropriate for Ms. Q? What clinical factors and legal issues should a psychiatrist consider when helping medical colleagues provide unwanted treatment to a severely malnourished patient with an eating disorder? We’ll explore these matters as we consider the case of Ms. Q (Figure) and the following questions:
- What type of care is most appropriate for her now?
- Can she refuse medical treatment?
- What are the medicolegal risks of letting her leave the hospital?
- What are the medicolegal risks of detaining and force-feeding her against her will?
- When is a psychiatric “hold” appropriate?
What care is appropriate?
Given her state of self-starvation, Ms. Q’s treatment plan could require close monitoring of her electrolytes and cardiac status, as well as watching her for signs of “refeeding syndrome”—rapid, potentially fatal fluid shifts and metabolic derangements that malnourished patients could experience when they receive artificial refeeding.1
First, the physicians who are caring for Ms. Q should determine whether she needs more intensive medical supervision than is usually available on a psychiatric unit. If she does, but she won’t agree to stay on a medical unit for care, a psychiatric hold is the wrong step, for 2 reasons:
- Once a psychiatric hold has been executed, state statutes require the patient to be placed in a psychiatric facility—a state-approved psychiatric treatment setting, such as a psychiatric unit or free-standing psychiatric hospital—within a specified period.2,3 Most nonpsychiatric medical units would not meet state’s statutory definition for such a facility.
- A psychiatric hold only permits short-term detention. It does not provide legal authority to impose unwanted medical treatment.
Does Ms. Q have capacity?
In the United States, Ms. Q has a legal right to refuse medical care—even if she needs it urgently—provided that her refusal is made competently.4 As Appelbaum and Grisso5 explained in a now-classic 1988 article:
The legal standards for competence include the four related skills of communicating a choice, understanding relevant information, appreciating the current situation and its consequences, and manipulating information rationally.
The Table5 describes these abilities in more detail.
Only courts can make legal determinations of competence, so physicians refer to an evaluation of a patient’s competence-related abilities as a “capacity assessment.” The decision as to whether a patient has capacity ultimately rests with the primary treatment team; however, physicians in other specialties often enlist psychiatrists’ help with this matter because of their interviewing skills and knowledge of how mental illness can impair capacity.
No easy-to-use instrument for evaluating capacity is available. However, Appelbaum6 provides examples of questions that often prove useful in such assessments, and a review by Sessums et al7 on several capacity evaluation tools suggests that the Aid to Capacity Evaluation8 may be the best instrument for performing capacity assessments.
Patients with anorexia nervosa often differ substantially from healthy people in how they assign values to life and death,9 which can make it difficult to evaluate their capacity to refuse life-saving treatment. Malnutrition can alter patients’ ability to think clearly, a phenomenon that some patients with anorexia mention as a reason they are grateful (in retrospect) for the compulsory treatment they received.10 Yet, if an evaluation shows that the patient has the decision-making capacity to refuse care, then her (his) caregivers should carefully document this conclusion and the basis for it. Although caregivers might encourage her to accept the treatment they believe she needs, they should not provide treatment that conflicts with their patient’s wishes.
If evaluation shows that the patient lacks capacity, however, the findings that support this conclusion should be documented clearly. The team then should consult the hospital attorney to determine how to best proceed. The attorney might recommend that a physician on the primary treatment team initiate a “medical hold”—an order that the patient may not leave against medical advice (AMA)—and then seek an emergency guardianship to permit medical treatment, such as refeeding.
To treat or not to treat?
What are the legal risks of allowing Ms. Q to leave AMA before she reaches medical stability?
Powers and Cloak11 describe a case of a 26-year-old woman with anorexia nervosa who came to the hospital with dizziness, weakness, and a very low blood glucose level. She was discharged after 6 days without having received any feeding, only to return to the emergency department 2 days later. This time, she had a letter from her physician stating that she needed medical supervision to start refeeding, yet she was discharged from the emergency department within a few hours. She was re-admitted to the hospital the next day.
Powers and Cloak11 do not report this woman’s medical outcome. But what if she had suffered a fatal cardiac arrhythmia before her third presentation to the emergency department or suffered another injury attributable to her nutritional state: Could her physicians be found at fault?
On Cohen & Associates’ Web site, they essentially answer, “Yes.” They describe a case of “Miss McIntosh,” who had anorexia nervosa and was discharged home from a hospital despite “chronic metabolic problems and not eating properly.” She went into a “hypoglycemic encephalopathic coma” and “suffered irreversible brain damage.” A subsequent lawsuit against the hospital resulted in a 7-figure settlement,12 illustrating the potential for adverse medicolegal consequences if failure to treat a patient with anorexia nervosa could be linked to subsequent physical harm. On the other hand, could a patient with anorexia who is being force-fed take legal action against her providers? At least 3 recent British cases suggest that this is possible.13-15 A British medical student with anorexia, E, made an emergency application to the Court of Protection in London, claiming that being fed against her will was akin to reliving her past experience of sexual abuse. In E’s case, the judge ruled “that the balance tips slowly but unmistakably in the direction of life preserving treatment” and authorized feeding over her objection.6 In 2 other cases, however, British courts have ruled that force-feeding anorexic patients would be futile and disallowed the practice.14,15
Faced with possible legal action, no matter what course you take, how should you respond? Getting legal and ethical consultation is prudent if time allows. In many cases, hospital attorneys might prefer that physicians err on the side of preserving life(D. Vanderpool, MBA, JD, personal communication, February 3, 2016)—even if that means detaining a patient without clear legal authorization to do so—because attorneys would prefer to defend a doctor who acted to save someone’s life than to defend a doctor who knowingly allowed a patient to die.
When might persons with an eating disorder be civilly committed?
Suppose that Ms. Q does not need urgent nonpsychiatric medical care, or that her life-threatening physical problems now have been addressed. Her physicians strongly recommend that she undergo inpatient psychiatric treatment for her eating disorder, but she wants to leave. Would it now be appropriate to fill out paperwork to initiate a psychiatric hold?
All U.S. jurisdictions authorize “civil commitment” proceedings that can lead to involuntary psychiatric hospitalization of people who have a mental disorder and pose a risk to themselves or others because of the disorder.16
In general, to be subject to civil commitment, a person must have a substantial disorder of thought, mood, perception, orientation, or memory. In addition, that disorder must grossly impair her (his) judgment, behavior, reality testing, or ability to meet the demands of everyday life.17
People with psychosis, a severe mood disorder, or dementia often meet these criteria. However, psychiatrists do not usually consider anorexia nervosa to be a thought disorder, mood disorder, or memory disorder. Does this mean that people with anorexia nervosa cannot meet the “substantial” mental disorder criterion?
It does not. Courts interpret the words in statutes based on their “ordinary and natural meaning.”18 If Ms. Q perceived herself as fat, despite having a BMI that was far below the healthy range, most people would regard her thinking to be disordered. If, in addition, her mental disorder impaired her “judgment, behavior, and capacity to meet the ordinary demands of sustaining existence,” then her anorexia nervosa “would qualify as a mental disorder for commitment purposes.”19
To be subject to civil commitment, a person with a substantial mental disorder also must pose a risk of harm to herself or others because of the disorder. That risk can be evidenced via an action, attempt, or threat to do direct physical harm, or it might inhere in the potential for developing grave disability through neglect of one’s basic needs, such as failing to eat adequately. In Ms. Q’s case, if the evidence shows her eating-disordered behavior has placed her at imminent risk of permanent injury or death, she has satisfied the legal criteria that justify court-ordered psychiatric hospitalization.
Bottom Line
When a severely malnourished patient with anorexia nervosa does not agree to allow recommended care, an appropriate clinical response should include judgment about the urgency of the proposed treatment, what treatment setting is best suited to the patient’s condition, and whether the patient has the mental capacity to refuse potentially life-saving care.
1. Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008;336(7659):1495-1498.
2. Ohio Revised Code §5122.01(F).
3. Oregon Revised Statutes §426.005(c).
4. Schloendorff v Society of New York Hospital, 211 N.Y. 125, 105 N.E. 92 (N1914).
5. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
6. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
7. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-427.
8. Community tools: Aid to Capacity Evaluation (ACE). University of Toronto Joint Centre for Bioethics. http://www.jcb.utoronto.ca/tools/ace_download.shtml. Updated May 8, 2008. Accessed December 21, 2015.
9. Tan J, Hope T, Stewart A. Competence to refuse treatment in anorexia nervosa. Int J Law Psychiatry. 2003;26(6):697-707.
10. Elzakkers IF, Danner UN, Hoek HW, et al. Compulsory treatment in anorexia nervosa: a review. Int J Eat Disord. 2014;47(8):845-852.
11. Powers PS, Cloak NL. Failure to feed patients with anorexia nervosa and other perils and perplexities in the medical care of eating disorder patients. Eat Disord. 2013;21(1):81-89.
12. “Failure to properly treat anorexia nervosa.” Harry S. Cohen & Associates. http://medmal1.com/article/failure-to-properly-treat-anorexia-nervosa. Accessed February 1, 2016.
13. A Local Authority v E. and Others [2012] EWHC 1639 (COP).
14. A NHS Foundation Trust v Ms. X [2014] EWCOP 35.
15. NHS Trust v L [2012] EWHC 2741 (COP).
16. Pinals DA, Mossman D. Evaluation for civil commitment. New York, NY: Oxford University Press; 2011.
17. Castellano-Hoyt DW. Enhancing police response to persons in mental health crisis: providing strategies, communication techniques, and crisis intervention preparation in overcoming institutional challenges. Springfield, IL: Charles C. Thomas Publisher, Ltd; 2003.
18. FDIC v Meyer, 510 U.S. 471 (1994).
19. Appelbaum PS, Rumpf T. Civil commitment of the anorexic patient. Gen Hosp Psychiatry. 1998;20(4):225-230.
1. Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008;336(7659):1495-1498.
2. Ohio Revised Code §5122.01(F).
3. Oregon Revised Statutes §426.005(c).
4. Schloendorff v Society of New York Hospital, 211 N.Y. 125, 105 N.E. 92 (N1914).
5. Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med. 1988;319(25):1635-1638.
6. Appelbaum PS. Clinical practice. Assessment of patients’ competence to consent to treatment. N Engl J Med. 2007;357(18):1834-1840.
7. Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA. 2011;306(4):420-427.
8. Community tools: Aid to Capacity Evaluation (ACE). University of Toronto Joint Centre for Bioethics. http://www.jcb.utoronto.ca/tools/ace_download.shtml. Updated May 8, 2008. Accessed December 21, 2015.
9. Tan J, Hope T, Stewart A. Competence to refuse treatment in anorexia nervosa. Int J Law Psychiatry. 2003;26(6):697-707.
10. Elzakkers IF, Danner UN, Hoek HW, et al. Compulsory treatment in anorexia nervosa: a review. Int J Eat Disord. 2014;47(8):845-852.
11. Powers PS, Cloak NL. Failure to feed patients with anorexia nervosa and other perils and perplexities in the medical care of eating disorder patients. Eat Disord. 2013;21(1):81-89.
12. “Failure to properly treat anorexia nervosa.” Harry S. Cohen & Associates. http://medmal1.com/article/failure-to-properly-treat-anorexia-nervosa. Accessed February 1, 2016.
13. A Local Authority v E. and Others [2012] EWHC 1639 (COP).
14. A NHS Foundation Trust v Ms. X [2014] EWCOP 35.
15. NHS Trust v L [2012] EWHC 2741 (COP).
16. Pinals DA, Mossman D. Evaluation for civil commitment. New York, NY: Oxford University Press; 2011.
17. Castellano-Hoyt DW. Enhancing police response to persons in mental health crisis: providing strategies, communication techniques, and crisis intervention preparation in overcoming institutional challenges. Springfield, IL: Charles C. Thomas Publisher, Ltd; 2003.
18. FDIC v Meyer, 510 U.S. 471 (1994).
19. Appelbaum PS, Rumpf T. Civil commitment of the anorexic patient. Gen Hosp Psychiatry. 1998;20(4):225-230.
‘You’ve been served’: What to do if you receive a subpoena
Dear Dr. Mossman,
Psychiatrists should not reveal what their patients say except to avert a threat to health or safety or to report abuse. So, how can psychiatrists be subpoenaed to provide information for a trial? If I receive a subpoena, how can I comply without violating patient privacy? If I have to go to court, can I “plead the Fifth”?
Submitted by “Dr. S”
Physicians who are served with a subpoena feel upset for the reason Dr. S described: Complying with a subpoena seems to violate the obligation to protect patients’ privacy. But physicians can’t “plead the Fifth” under these circumstances, because the Fifth Amendment to the U.S. Constitution only bars forcing someone to give self-incriminating testimony.1
If you receive a subpoena for information gleaned during patient care, you should not ignore it. Failing to respond might place you in contempt of court and subject you to a fine or even jail time. Yet simply complying could have legal and professional implications, too.
Often, a psychiatrist who receives a subpoena should seek an attorney’s advice on how to best respond. But understanding what subpoenas are and how they work might let you feel less anxious as you go through the process of responding. With this goal in mind, this article covers:
• what a subpoena is and isn’t
• 2 types of privacy obligations
• legal options
• avoiding potential embarrassment (Box).2
What is a subpoena?
All citizens have a legal obligation to furnish courts with the information needed to decide legal issues.3 Statutes and legal rules dictate how such material comes to court.
Issuing a subpoena (from the Latin sub poena, “under penalty”) is one way of obtaining information needed for a legal proceeding. A subpoena ad testificandum directs the recipient to appear at a legal proceeding and provide testimony. A subpoena duces tecum (“you shall bring with you”) directs the recipient to produce specific records or to appear at a legal proceeding with the records.
Usually, subpoenas are issued by attorneys or court clerks, not by judges. As such, they are not court orders. If you receive a subpoena, you should make a timely response of some sort. But, ultimately, you might not have to release the information. Although physicians have to follow the same rules as other citizens, courts recognize that doctors also have professional obligations to their patients.
Confidentiality: Your reason to hesitate
Receiving a subpoena doesn’t change your obligation to protect your patient’s confidentiality. From the law’s standpoint, patient confidentiality is a function of the rules that govern use of information in legal proceedings.
The Privacy Rule4 that arose from the Health Insurance Portability and Accountability Act (HIPAA) of 19965 provides guidance on acceptable responses to subpoenas by “covered entities,” which includes most physicians’ practices. HIPAA permits disclosure of the minimum amount of personal information needed to fulfill the demands of a subpoena. The Table6,7 explains HIPAA’s rules about specific responses to subpoenas, depending on their source.
Many states have patient privacy laws that are stricter than HIPAA rules. If you practice in one of those states, you have to follow the more stringent rule.8 For example, Ohio law does not let subpoenaed providers tender medical records for use in a grand jury proceeding without a release signed by the patient, although HIPAA would allow this (Table).6,7 Out of concern that “giving law enforcement unbridled access to medical records could discourage patients from seeking medical treatment,” Ohio protects patient records more than HIPAA does.9 New York State’s privilege rules also are stricter than HIPAA10 and contain specific provisions about releasing certain types of information (eg, HIV status11). State courts expect physicians to follow their laws about patient privacy and to consult attorneys to make sure that releasing information is done properly.12
Releasing information improperly could become grounds for legal action against you, even if you released the information in response to a subpoena. Legal action could take the form of a lawsuit for breach of confidentiality, a HIPAA-based complaint, a complaint to the state medical board, or all 3 of these.
Must you turn over information?
Before you testify or turn over documents, you need to verify that the legal and ethical requirements for the disclosure are met—as you would for any release of patient information. You can do this by obtaining your patient’s formal, written consent for the disclosure. Before you accept the patient’s agreement, however, you might—and in most cases should— consider discussing how the disclosure could affect the patient’s well-being or your treatment relationship.
If the patient will not agree to the disclosure, the patient or the patient’s attorney can seek to have the subpoena modified or quashed (declared void). One tactic for doing this is by asserting doctor–patient privilege, a legal doctrine codified in most state’s laws. The privilege recognizes that, because privacy is important in medical care, stopping clinical information from automatically coming in court serves an important social purpose.13
The doctor–patient privilege belongs to the litigant—here, your patient—not to you, so your patient has to raise the objection to releasing information.14 Also, the privilege is not absolute. If having the clinical information is necessary, the judge may issue a court order denying the patient’s motion to quash. Unless the judge later modifies or vacates the order, you risk being found in contempt of court if you still refuse to turn over documents demanded by the subpoena.
Fact witness or expert witness?
If the subpoena demands your testimony, the issuing party might want you to serve as a fact witness or expert witness. Persons with relevant personal knowledge to a legal proceeding can serve as fact witnesses, and testify about things they did or perceived.15 For example, a psychiatrist serving as a fact witness could recount having heard or seen a patient talking aloud as if arguing with someone when no real interlocutor was present.
A witness whom the court deems an “expert” by virtue of special knowledge, skill, experience, training, or education may offer opinions based on specific sets of facts. Courts hear such testimony when the expert’s specialized knowledge will help the jury understand the evidence or reach a verdict in a case.16 To return to the example above: a psychiatric expert witness might tell jurors that the patient’s “arguing” was evidence that she was hallucinating and suffered from schizophrenia.
If you receive a subpoena to testify about someone you have treated, you should notify the issuing party that you will provide fact testimony if required to do so. You cannot be compelled to serve as an expert witness, however. In many situations, attempting to provide objective expert testimony about one’s own patient could create unresolvable conflicts between the obligation to tell the truth and your obligation to serve your patient’s interests.17
If the subpoena requests deposition testimony about a patient, you probably will be able to schedule the deposition at a time that is convenient for you and the attorneys involved. Yet you should not agree to be deposed unless (a) you have received the patient’s authorization, (b) a court has ordered you to testify despite the patient’s objection, or (c) your attorney (whom you have consulted about the situation) has advised you that providing testimony is appropriate.
If you are called as a fact witness for a trial, the attorney or court that has subpoenaed you often will try to schedule things to minimize the time taken away from your other duties. Once in court, you can ask the judge (on the record) whether you must answer if you are asked questions about a patient who has not previously authorized you to release treatment information. A judge’s explicit command to respond absolves you of any further ethical obligation to withhold confidential information about the patient’s care.
Bottom Line
If you receive a subpoena for records or testimony, obtaining the patient’s written authorization should allow you to release the information without violating confidentiality obligations. If your patient won’t agree to the release, if turning over information might adversely affect the patient, or if you’re not sure what to do, seek advice from an attorney who knows about medical privacy rules. That way, you can be sure you are meeting all legal and professional standards that apply.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with any manufacturers of competing products.
1. Kastigar v United States, 406 US 441 (1972).
2. Barsky AE. Clinicians in court, second edition: A guide to subpoenas, depositions, testifying, and everything else you need to know. New York, NY: Guilford Press; 2012.
3. United States v Bryan, 339 US 323 (1950).
4. 45 CFR §164.50.
5. 45 CFR Parts 160 and 164.
6. 45 CFR §164.512.
7. Stanger K. HIPAA: responding to subpoenas, orders, and administrative demands. http://www.hhhealthlawblog.com/2013/10/hipaa-responding-to-subpoenas-orders-and-administrative-demands.html. Published October 9, 2013. Accessed September 22, 2015.
8. Zwerling AL, de Harder WA, Tarpey CM. To disclose or not to disclose, that is the question: issues to consider before responding to a subpoena. J Am Coll Radiol. 2012;9(4):279-281.
9. Turk v Oilier, 732 F Supp 2d 758 (ND Ohio 2010).
10. In re Antonia E, 16 Misc 3d 637 (Fam Ct Queens County 2007).
11. NY PBH Law §2785.
12. Crescenzo v Crane, 796 A2d 283 (NJ Super Ct App Div 2002).
13. In re Bruendl’s Will, 102 Wis 45, 78 NW 169 (1899).
14. In re Lifschutz, 2 Cal 3d 415, 85 Cal Rptr 829, 467 P2d 557 (1970).
15. Broun KS, Dix GE, Imwinkelried EJ, et al. McCormick on evidence. 7th ed. St. Paul, MN: West Group; 2013.
16. Fed Evid R 702.
17. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154:448-456.
Dear Dr. Mossman,
Psychiatrists should not reveal what their patients say except to avert a threat to health or safety or to report abuse. So, how can psychiatrists be subpoenaed to provide information for a trial? If I receive a subpoena, how can I comply without violating patient privacy? If I have to go to court, can I “plead the Fifth”?
Submitted by “Dr. S”
Physicians who are served with a subpoena feel upset for the reason Dr. S described: Complying with a subpoena seems to violate the obligation to protect patients’ privacy. But physicians can’t “plead the Fifth” under these circumstances, because the Fifth Amendment to the U.S. Constitution only bars forcing someone to give self-incriminating testimony.1
If you receive a subpoena for information gleaned during patient care, you should not ignore it. Failing to respond might place you in contempt of court and subject you to a fine or even jail time. Yet simply complying could have legal and professional implications, too.
Often, a psychiatrist who receives a subpoena should seek an attorney’s advice on how to best respond. But understanding what subpoenas are and how they work might let you feel less anxious as you go through the process of responding. With this goal in mind, this article covers:
• what a subpoena is and isn’t
• 2 types of privacy obligations
• legal options
• avoiding potential embarrassment (Box).2
What is a subpoena?
All citizens have a legal obligation to furnish courts with the information needed to decide legal issues.3 Statutes and legal rules dictate how such material comes to court.
Issuing a subpoena (from the Latin sub poena, “under penalty”) is one way of obtaining information needed for a legal proceeding. A subpoena ad testificandum directs the recipient to appear at a legal proceeding and provide testimony. A subpoena duces tecum (“you shall bring with you”) directs the recipient to produce specific records or to appear at a legal proceeding with the records.
Usually, subpoenas are issued by attorneys or court clerks, not by judges. As such, they are not court orders. If you receive a subpoena, you should make a timely response of some sort. But, ultimately, you might not have to release the information. Although physicians have to follow the same rules as other citizens, courts recognize that doctors also have professional obligations to their patients.
Confidentiality: Your reason to hesitate
Receiving a subpoena doesn’t change your obligation to protect your patient’s confidentiality. From the law’s standpoint, patient confidentiality is a function of the rules that govern use of information in legal proceedings.
The Privacy Rule4 that arose from the Health Insurance Portability and Accountability Act (HIPAA) of 19965 provides guidance on acceptable responses to subpoenas by “covered entities,” which includes most physicians’ practices. HIPAA permits disclosure of the minimum amount of personal information needed to fulfill the demands of a subpoena. The Table6,7 explains HIPAA’s rules about specific responses to subpoenas, depending on their source.
Many states have patient privacy laws that are stricter than HIPAA rules. If you practice in one of those states, you have to follow the more stringent rule.8 For example, Ohio law does not let subpoenaed providers tender medical records for use in a grand jury proceeding without a release signed by the patient, although HIPAA would allow this (Table).6,7 Out of concern that “giving law enforcement unbridled access to medical records could discourage patients from seeking medical treatment,” Ohio protects patient records more than HIPAA does.9 New York State’s privilege rules also are stricter than HIPAA10 and contain specific provisions about releasing certain types of information (eg, HIV status11). State courts expect physicians to follow their laws about patient privacy and to consult attorneys to make sure that releasing information is done properly.12
Releasing information improperly could become grounds for legal action against you, even if you released the information in response to a subpoena. Legal action could take the form of a lawsuit for breach of confidentiality, a HIPAA-based complaint, a complaint to the state medical board, or all 3 of these.
Must you turn over information?
Before you testify or turn over documents, you need to verify that the legal and ethical requirements for the disclosure are met—as you would for any release of patient information. You can do this by obtaining your patient’s formal, written consent for the disclosure. Before you accept the patient’s agreement, however, you might—and in most cases should— consider discussing how the disclosure could affect the patient’s well-being or your treatment relationship.
If the patient will not agree to the disclosure, the patient or the patient’s attorney can seek to have the subpoena modified or quashed (declared void). One tactic for doing this is by asserting doctor–patient privilege, a legal doctrine codified in most state’s laws. The privilege recognizes that, because privacy is important in medical care, stopping clinical information from automatically coming in court serves an important social purpose.13
The doctor–patient privilege belongs to the litigant—here, your patient—not to you, so your patient has to raise the objection to releasing information.14 Also, the privilege is not absolute. If having the clinical information is necessary, the judge may issue a court order denying the patient’s motion to quash. Unless the judge later modifies or vacates the order, you risk being found in contempt of court if you still refuse to turn over documents demanded by the subpoena.
Fact witness or expert witness?
If the subpoena demands your testimony, the issuing party might want you to serve as a fact witness or expert witness. Persons with relevant personal knowledge to a legal proceeding can serve as fact witnesses, and testify about things they did or perceived.15 For example, a psychiatrist serving as a fact witness could recount having heard or seen a patient talking aloud as if arguing with someone when no real interlocutor was present.
A witness whom the court deems an “expert” by virtue of special knowledge, skill, experience, training, or education may offer opinions based on specific sets of facts. Courts hear such testimony when the expert’s specialized knowledge will help the jury understand the evidence or reach a verdict in a case.16 To return to the example above: a psychiatric expert witness might tell jurors that the patient’s “arguing” was evidence that she was hallucinating and suffered from schizophrenia.
If you receive a subpoena to testify about someone you have treated, you should notify the issuing party that you will provide fact testimony if required to do so. You cannot be compelled to serve as an expert witness, however. In many situations, attempting to provide objective expert testimony about one’s own patient could create unresolvable conflicts between the obligation to tell the truth and your obligation to serve your patient’s interests.17
If the subpoena requests deposition testimony about a patient, you probably will be able to schedule the deposition at a time that is convenient for you and the attorneys involved. Yet you should not agree to be deposed unless (a) you have received the patient’s authorization, (b) a court has ordered you to testify despite the patient’s objection, or (c) your attorney (whom you have consulted about the situation) has advised you that providing testimony is appropriate.
If you are called as a fact witness for a trial, the attorney or court that has subpoenaed you often will try to schedule things to minimize the time taken away from your other duties. Once in court, you can ask the judge (on the record) whether you must answer if you are asked questions about a patient who has not previously authorized you to release treatment information. A judge’s explicit command to respond absolves you of any further ethical obligation to withhold confidential information about the patient’s care.
Bottom Line
If you receive a subpoena for records or testimony, obtaining the patient’s written authorization should allow you to release the information without violating confidentiality obligations. If your patient won’t agree to the release, if turning over information might adversely affect the patient, or if you’re not sure what to do, seek advice from an attorney who knows about medical privacy rules. That way, you can be sure you are meeting all legal and professional standards that apply.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with any manufacturers of competing products.
Dear Dr. Mossman,
Psychiatrists should not reveal what their patients say except to avert a threat to health or safety or to report abuse. So, how can psychiatrists be subpoenaed to provide information for a trial? If I receive a subpoena, how can I comply without violating patient privacy? If I have to go to court, can I “plead the Fifth”?
Submitted by “Dr. S”
Physicians who are served with a subpoena feel upset for the reason Dr. S described: Complying with a subpoena seems to violate the obligation to protect patients’ privacy. But physicians can’t “plead the Fifth” under these circumstances, because the Fifth Amendment to the U.S. Constitution only bars forcing someone to give self-incriminating testimony.1
If you receive a subpoena for information gleaned during patient care, you should not ignore it. Failing to respond might place you in contempt of court and subject you to a fine or even jail time. Yet simply complying could have legal and professional implications, too.
Often, a psychiatrist who receives a subpoena should seek an attorney’s advice on how to best respond. But understanding what subpoenas are and how they work might let you feel less anxious as you go through the process of responding. With this goal in mind, this article covers:
• what a subpoena is and isn’t
• 2 types of privacy obligations
• legal options
• avoiding potential embarrassment (Box).2
What is a subpoena?
All citizens have a legal obligation to furnish courts with the information needed to decide legal issues.3 Statutes and legal rules dictate how such material comes to court.
Issuing a subpoena (from the Latin sub poena, “under penalty”) is one way of obtaining information needed for a legal proceeding. A subpoena ad testificandum directs the recipient to appear at a legal proceeding and provide testimony. A subpoena duces tecum (“you shall bring with you”) directs the recipient to produce specific records or to appear at a legal proceeding with the records.
Usually, subpoenas are issued by attorneys or court clerks, not by judges. As such, they are not court orders. If you receive a subpoena, you should make a timely response of some sort. But, ultimately, you might not have to release the information. Although physicians have to follow the same rules as other citizens, courts recognize that doctors also have professional obligations to their patients.
Confidentiality: Your reason to hesitate
Receiving a subpoena doesn’t change your obligation to protect your patient’s confidentiality. From the law’s standpoint, patient confidentiality is a function of the rules that govern use of information in legal proceedings.
The Privacy Rule4 that arose from the Health Insurance Portability and Accountability Act (HIPAA) of 19965 provides guidance on acceptable responses to subpoenas by “covered entities,” which includes most physicians’ practices. HIPAA permits disclosure of the minimum amount of personal information needed to fulfill the demands of a subpoena. The Table6,7 explains HIPAA’s rules about specific responses to subpoenas, depending on their source.
Many states have patient privacy laws that are stricter than HIPAA rules. If you practice in one of those states, you have to follow the more stringent rule.8 For example, Ohio law does not let subpoenaed providers tender medical records for use in a grand jury proceeding without a release signed by the patient, although HIPAA would allow this (Table).6,7 Out of concern that “giving law enforcement unbridled access to medical records could discourage patients from seeking medical treatment,” Ohio protects patient records more than HIPAA does.9 New York State’s privilege rules also are stricter than HIPAA10 and contain specific provisions about releasing certain types of information (eg, HIV status11). State courts expect physicians to follow their laws about patient privacy and to consult attorneys to make sure that releasing information is done properly.12
Releasing information improperly could become grounds for legal action against you, even if you released the information in response to a subpoena. Legal action could take the form of a lawsuit for breach of confidentiality, a HIPAA-based complaint, a complaint to the state medical board, or all 3 of these.
Must you turn over information?
Before you testify or turn over documents, you need to verify that the legal and ethical requirements for the disclosure are met—as you would for any release of patient information. You can do this by obtaining your patient’s formal, written consent for the disclosure. Before you accept the patient’s agreement, however, you might—and in most cases should— consider discussing how the disclosure could affect the patient’s well-being or your treatment relationship.
If the patient will not agree to the disclosure, the patient or the patient’s attorney can seek to have the subpoena modified or quashed (declared void). One tactic for doing this is by asserting doctor–patient privilege, a legal doctrine codified in most state’s laws. The privilege recognizes that, because privacy is important in medical care, stopping clinical information from automatically coming in court serves an important social purpose.13
The doctor–patient privilege belongs to the litigant—here, your patient—not to you, so your patient has to raise the objection to releasing information.14 Also, the privilege is not absolute. If having the clinical information is necessary, the judge may issue a court order denying the patient’s motion to quash. Unless the judge later modifies or vacates the order, you risk being found in contempt of court if you still refuse to turn over documents demanded by the subpoena.
Fact witness or expert witness?
If the subpoena demands your testimony, the issuing party might want you to serve as a fact witness or expert witness. Persons with relevant personal knowledge to a legal proceeding can serve as fact witnesses, and testify about things they did or perceived.15 For example, a psychiatrist serving as a fact witness could recount having heard or seen a patient talking aloud as if arguing with someone when no real interlocutor was present.
A witness whom the court deems an “expert” by virtue of special knowledge, skill, experience, training, or education may offer opinions based on specific sets of facts. Courts hear such testimony when the expert’s specialized knowledge will help the jury understand the evidence or reach a verdict in a case.16 To return to the example above: a psychiatric expert witness might tell jurors that the patient’s “arguing” was evidence that she was hallucinating and suffered from schizophrenia.
If you receive a subpoena to testify about someone you have treated, you should notify the issuing party that you will provide fact testimony if required to do so. You cannot be compelled to serve as an expert witness, however. In many situations, attempting to provide objective expert testimony about one’s own patient could create unresolvable conflicts between the obligation to tell the truth and your obligation to serve your patient’s interests.17
If the subpoena requests deposition testimony about a patient, you probably will be able to schedule the deposition at a time that is convenient for you and the attorneys involved. Yet you should not agree to be deposed unless (a) you have received the patient’s authorization, (b) a court has ordered you to testify despite the patient’s objection, or (c) your attorney (whom you have consulted about the situation) has advised you that providing testimony is appropriate.
If you are called as a fact witness for a trial, the attorney or court that has subpoenaed you often will try to schedule things to minimize the time taken away from your other duties. Once in court, you can ask the judge (on the record) whether you must answer if you are asked questions about a patient who has not previously authorized you to release treatment information. A judge’s explicit command to respond absolves you of any further ethical obligation to withhold confidential information about the patient’s care.
Bottom Line
If you receive a subpoena for records or testimony, obtaining the patient’s written authorization should allow you to release the information without violating confidentiality obligations. If your patient won’t agree to the release, if turning over information might adversely affect the patient, or if you’re not sure what to do, seek advice from an attorney who knows about medical privacy rules. That way, you can be sure you are meeting all legal and professional standards that apply.
Disclosure
The author reports no financial relationship with any company whose products are mentioned in this article or with any manufacturers of competing products.
1. Kastigar v United States, 406 US 441 (1972).
2. Barsky AE. Clinicians in court, second edition: A guide to subpoenas, depositions, testifying, and everything else you need to know. New York, NY: Guilford Press; 2012.
3. United States v Bryan, 339 US 323 (1950).
4. 45 CFR §164.50.
5. 45 CFR Parts 160 and 164.
6. 45 CFR §164.512.
7. Stanger K. HIPAA: responding to subpoenas, orders, and administrative demands. http://www.hhhealthlawblog.com/2013/10/hipaa-responding-to-subpoenas-orders-and-administrative-demands.html. Published October 9, 2013. Accessed September 22, 2015.
8. Zwerling AL, de Harder WA, Tarpey CM. To disclose or not to disclose, that is the question: issues to consider before responding to a subpoena. J Am Coll Radiol. 2012;9(4):279-281.
9. Turk v Oilier, 732 F Supp 2d 758 (ND Ohio 2010).
10. In re Antonia E, 16 Misc 3d 637 (Fam Ct Queens County 2007).
11. NY PBH Law §2785.
12. Crescenzo v Crane, 796 A2d 283 (NJ Super Ct App Div 2002).
13. In re Bruendl’s Will, 102 Wis 45, 78 NW 169 (1899).
14. In re Lifschutz, 2 Cal 3d 415, 85 Cal Rptr 829, 467 P2d 557 (1970).
15. Broun KS, Dix GE, Imwinkelried EJ, et al. McCormick on evidence. 7th ed. St. Paul, MN: West Group; 2013.
16. Fed Evid R 702.
17. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154:448-456.
1. Kastigar v United States, 406 US 441 (1972).
2. Barsky AE. Clinicians in court, second edition: A guide to subpoenas, depositions, testifying, and everything else you need to know. New York, NY: Guilford Press; 2012.
3. United States v Bryan, 339 US 323 (1950).
4. 45 CFR §164.50.
5. 45 CFR Parts 160 and 164.
6. 45 CFR §164.512.
7. Stanger K. HIPAA: responding to subpoenas, orders, and administrative demands. http://www.hhhealthlawblog.com/2013/10/hipaa-responding-to-subpoenas-orders-and-administrative-demands.html. Published October 9, 2013. Accessed September 22, 2015.
8. Zwerling AL, de Harder WA, Tarpey CM. To disclose or not to disclose, that is the question: issues to consider before responding to a subpoena. J Am Coll Radiol. 2012;9(4):279-281.
9. Turk v Oilier, 732 F Supp 2d 758 (ND Ohio 2010).
10. In re Antonia E, 16 Misc 3d 637 (Fam Ct Queens County 2007).
11. NY PBH Law §2785.
12. Crescenzo v Crane, 796 A2d 283 (NJ Super Ct App Div 2002).
13. In re Bruendl’s Will, 102 Wis 45, 78 NW 169 (1899).
14. In re Lifschutz, 2 Cal 3d 415, 85 Cal Rptr 829, 467 P2d 557 (1970).
15. Broun KS, Dix GE, Imwinkelried EJ, et al. McCormick on evidence. 7th ed. St. Paul, MN: West Group; 2013.
16. Fed Evid R 702.
17. Strasburger LH, Gutheil TG, Brodsky A. On wearing two hats: role conflict in serving as both psychotherapist and expert witness. Am J Psychiatry. 1997;154:448-456.
Peaceful feeling, or up in smoke? Medical marijuana in medicolegal context
Dear Dr. Mossman,
I practice in a state that allows medical marijuana use. A few of my patients have asked me to help them obtain marijuana for their conditions. How risky would it be to oblige?
Submitted by “Dr. J”
In recent years, public debate about marijuana has acquired 2 new dimensions: (1) the wishes and medical needs of people who seek marijuana for its purported health benefits, and (2) the role of physicians who practice where “medical marijuana” is legal. This article, the authors’ joint effort to address Dr. J’s concerns, hits 3 topics:
• the intersection of marijuana policy and health care in the United States
• the risks and possible benefits of marijuana use
• the medicolegal problems faced by physicians who might advise patients to use marijuana.
Legal haze
Two cannabinoids—dronabinol and nabilone—have received FDA approval as appetite enhancers and anti-nausea agents. Third-party payors usually cover these types of medications, but no insurer pays for medical marijuana.1 The Controlled Substances Act of 19702 classified marijuana as a Schedule I drug because of its abuse potential, lack of accepted medical applications, and uncertain safety. The FDA has not approved marijuana use for any medical condition.
Although people commonly speak of “prescribing” marijuana, physicians cannot legally do this in the United States. What physicians may do, in the 23 states that allow medical marijuana, is recommend or certify a patient’s marijuana use—an action that has constitutional protection under the First Amendment’s freedom of speech clause.3,4
A physician may complete documentation that a patient has one of the qualifying medical conditions for which the jurisdiction has legalized medical marijuana. Either the patient or the physician then submits that documentation to the appropriate government agency (eg, the state’s department of health).
If the documentation receives approval, the agency will issue the patient a registration card that allows possession of medical marijuana, with which the patient can obtain or grow a small amount of marijuana. The cannabinoid content of marijuana products varies considerably,5 and physicians who certify marijuana typically defer dosage recommendations to the patient or the dispensary.1
In states that allow medical marijuana, users may assert an affirmative defense of medical necessity if they face criminal prosecution.3,6 Possession of marijuana remains illegal under federal law, however, regardless of one’s reason for having it.7,8 Since October 2009, the Attorney General’s office has discouraged federal prosecutions of persons “whose actions are in clear and unambiguous compliance with existing state laws providing for the medical use of marijuana.”9 But given the remaining conflicts between state and federal laws, “the legal implications of certifying patients for medical marijuana remain unclear.”10
Physicians have few resources to instruct them on the legal risks of certifying medical marijuana. When Canada legalized medical marijuana, the organization that provides malpractice insurance to Canadian physicians told its members that “prescribing medical marijuana cannot be compared to prescribing prescription drugs” and recommended that physicians obtain signed release forms documenting that they have discussed the risks of medical marijuana with patients.11 For some risky approved drugs, the FDA has established a risk evaluation and mitigation strategy, but no such guidance is available for marijuana.
Highlighting the benefits and risks
Proponents of medical marijuana claim that Cannabis can help patients, and dispassionate experts acknowledge that at least modest evidence supports the benefits of using “marijuana for nausea and vomiting related to chemotherapy, specific pain syndromes, and spasticity from multiple sclerosis.”10 For several other conditions— HIV/AIDS, depression, anxiety disorders, sleep disorders, psychosis, Tourette syndrome—evidence of benefit is poor.12 Rigorous evaluation of medical marijuana is difficult because the plant contains hundreds of active chemical compounds. The chemical content of marijuana is highly variable, depending on its preparation and administration,10,13—one reason why only a few good randomized controlled trials of marijuana have been conducted.
Marijuana has several side effects and carries many health risks (Table 1).4,14-20
On the highway: Marijuana and driving
Marijuana use impairs driving ability.14 Following enactment of more lenient marijuana laws, several states have reported higher numbers of fatally injured drivers who tested positive for Cannabis21-23 and had a positive screen of tetrahydrocannabinol (THC) in driving under the influence cases.24,25 One study showed that a blood THC concentration >5 ng/mL (comparable to a blood alcohol concentration of 0.15%) increased the crash odds ratio to 6.6.25,26
Marijuana impairs reaction time, information processing, motor performance, attention, and visual processing.14,16,27,28 Drivers who are under the influence of marijuana make more driving errors, despite being cautious about how they react to traffic.29 Even after weeks of abstinence, previous daily users of marijuana display some cognitive processing and driving-related impairments.30,31
Courts have found physicians negligent if their patients’ treatment-induced driving impairments injured others when the risk of driving-related injury was foreseeable.32 The Massachusetts case of Coombes v Florio33 likened the physician’s duty to that of a liquor store that sells alcohol to a minor who subsequently crashes, or to a father who did not lock his firearms away from his violent adult son.
Three variables influence a court’s judgment about whether risk is “foreseeable”: “the relative knowledge of the risk as between lay persons and physicians, whether the patient has previously used the medication and/or experienced the adverse effect, and whether a warning would otherwise have been futile.”34 A physician who certified a patient to use marijuana without adequately explaining the risks of driving might be vulnerable to a lawsuit if the patient’s driving accident occurred while the patient was under the influence of the drug. Recommending marijuana as a treatment also could lead to a malpractice action if a patient experienced and was harmed by the drug’s adverse effects.
Other drags
Another malpractice risk stems from marijuana’s addiction potential. Although many people think Cannabis isn’t addictive, nearly 10% of all marijuana users develop dependence.10,17 Regular Cannabis users are more likely to use alcohol, tobacco, and “recreational” drugs,17,35 and using alcohol and marijuana together greatly heightens the risk of driving accidents.14,15 Although we know of no case that relates directly to marijuana, physicians have faced lawsuits for injuries stemming from a patient’s addiction to prescription drugs,36 particularly when the patient’s behavior should have led the physician to suspect abuse or overuse.37
When certifying marijuana use, physicians have the same obligations that apply to more conventional medical treatment:
• establishing a proper physician–patient relationship
• taking an appropriate history
• conducting a proper examination
• reviewing records
• developing a comprehensive treatment plan
• weighing risks and alternatives
• providing follow-up care.
Neglecting these steps could lead to medical board sanctions and suspension or revocation of a medical license.13
The blunt reality
We advise against recommending marijuana for your patients. But if you have exhausted the alternatives, see marijuana as the last resort, and believe that taking the risk is worth the potential benefit, you can take some steps to reduce your legal risk (Table 2,1,32,37,38 and Table 313).
Bottom LinE
Medical marijuana is a controversial topic that demands more rigorous research and regulatory consideration. In the present climate, cautious physicians will avoid recommending marijuana to their patients. If you think that a patient has a medical indication, with no treatment option better than medical marijuana, be sure to understand the medical and legal ramifications before you authorize its use.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474-2483.
2. Controlled Substances Act title 21, §801.
3. Frezza C. Medical marijuana: a drug without a medical model. Georgetown Law J. 2013;101:1117-1145.
4. Conant v Walters, 309 F3d 629, 637 (9th Cir 2002).
5. Vandrey R, Raber JC, Raber ME, et al. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313(24):2491-2493.
6. Thompson AE. JAMA patient page. Medical marijuana. JAMA. 2015;313(24):2508.
7. United States v Oakland Cannabis Buyers’ Cooperative, 532 U.S. 483 (2001).
8. Gonzales v Raich, 545 U.S. 1 (2005).
9. Ogden DW. Memorandum for selected United States Attorneys on investigations and prosecutions in states authorizing the medical use of marijuana. http://www. justice.gov/opa/blog/memorandum-selected-united-state-attorneys-investigations-and-prosecutions-states. Published October 19, 2009. Accessed July 11, 2015.
10. D’Souza DC, Ranganathan M. Medical marijuana: is the cart before the horse? JAMA. 2015;313(24):2431-2432.
11. Picard A. Pot-prescribing doctors warned. The Globe and Mail. http://www.theglobeandmail.com/news/national/ pot-prescribing-doctors-warned/article22506373. Published October 19, 2005. Accessed July 21, 2015.
12. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
13. Barthwell AG, Baxter LE, Cermak T, et al. The role of the physician in “medical” marijuana: American Society of Addiction Medicine. http://www.aoaam.org/usr/ ASAM_Med_Marijuana_White_Paper_Final.pdf. Published September 2010. Accessed July 11, 2015.
14. Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109-119.
15. Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478-492.
16. Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52-60.
17. Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19-35.
18. Huang YH, Zhang ZF, Tashkin DP, et al. An epidemiologic review of marijuana and cancer: an update. Cancer Epidemiol Biomarkers Prev. 2015;24(1):15-31.
19. Delforterie MJ, Lynskey MT, Huizink AC, et al. The relationship between cannabis involvement and suicidal thoughts and behaviors. Drug Alcohol Depend. 2015;150:98-104.
20. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot-a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54.
21. Masten SV, Guenzburger GV. Changes in driver cannabinoid prevalence in 12 U.S. states after implementing medical marijuana laws. J Safety Res. 2014;50:35-52.
22. Pollini RA, Romano E, Johnson MB, et al. The impact of marijuana decriminalization on California drivers. Drug Alcohol Depend. 2015;150:135-140.
23. Salomonsen-Sautel S, Min SJ, Sakai JT, et al. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144.
24. Urfer S, Morton J, Beall V, et al. Analysis of Δ9- tetrahydrocannabinol driving under the influence of drug cases in Colorado from January 2011 to February 2014. J Anal Toxicol. 2014;38(8):575-581.
25. Couper FJ, Peterson BL. The prevalence of marijuana in suspected impaired driving cases in Washington state. J Anal Toxicol. 2014;38(8):569-574.
26. Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239-248.
27. Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101-106.
28. Schwitzer T, Schwan R, Angioi-Duprez K, et al. The cannabinoid system and visual processing: a review on experimental findings and clinical presumptions. Eur Neuropsychopharmacol. 2015;25(1):100-112.
29. Neavyn MJ, Blohm E, Babu KM, et al. Medical marijuana and driving: a review. J Med Toxicol. 2014;10(3):269-279.
30. Bosker WM, Karschner EL, Lee D, et al. Sustained abstinence improves psychomotor function in chronic daily cannabis smokers. Paper presented at: SOFT 2012: Society of Forensic Toxicologists 2012 Annual Meeting; July 1-6, 2012; Boston, MA.
31. Fabritius M, Augsburger M, Chtioui H, et al. Fitness to drive and cannabis: validation of two blood THCCOOH thresholds to distinguish occasional users from heavy users. Forensic Sci Int. 2014;242:1-8.
32. Annas GJ. Doctors, drugs, and driving—tort liability for patient-caused accidents. New Engl J Med. 2008;359(5):521-525.
33. Coombes v Florio, 877 NE2d 567 (Mass 2007).
34. McKenzie v Hawaii Permanente Medical Group, Inc. 47 P3d 209 (Haw 2002).
35. Ilgen MA, Bohnert K, Kleinberg F, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 2013;132(3):654-659.
36. Osborne v United States, 166 F Supp 2d 479 (SDW Va 2001).
37. Conrad-Hutsell v Colturi, 2002 Ohio App. LEXIS 2740 (2002).
38. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
Dear Dr. Mossman,
I practice in a state that allows medical marijuana use. A few of my patients have asked me to help them obtain marijuana for their conditions. How risky would it be to oblige?
Submitted by “Dr. J”
In recent years, public debate about marijuana has acquired 2 new dimensions: (1) the wishes and medical needs of people who seek marijuana for its purported health benefits, and (2) the role of physicians who practice where “medical marijuana” is legal. This article, the authors’ joint effort to address Dr. J’s concerns, hits 3 topics:
• the intersection of marijuana policy and health care in the United States
• the risks and possible benefits of marijuana use
• the medicolegal problems faced by physicians who might advise patients to use marijuana.
Legal haze
Two cannabinoids—dronabinol and nabilone—have received FDA approval as appetite enhancers and anti-nausea agents. Third-party payors usually cover these types of medications, but no insurer pays for medical marijuana.1 The Controlled Substances Act of 19702 classified marijuana as a Schedule I drug because of its abuse potential, lack of accepted medical applications, and uncertain safety. The FDA has not approved marijuana use for any medical condition.
Although people commonly speak of “prescribing” marijuana, physicians cannot legally do this in the United States. What physicians may do, in the 23 states that allow medical marijuana, is recommend or certify a patient’s marijuana use—an action that has constitutional protection under the First Amendment’s freedom of speech clause.3,4
A physician may complete documentation that a patient has one of the qualifying medical conditions for which the jurisdiction has legalized medical marijuana. Either the patient or the physician then submits that documentation to the appropriate government agency (eg, the state’s department of health).
If the documentation receives approval, the agency will issue the patient a registration card that allows possession of medical marijuana, with which the patient can obtain or grow a small amount of marijuana. The cannabinoid content of marijuana products varies considerably,5 and physicians who certify marijuana typically defer dosage recommendations to the patient or the dispensary.1
In states that allow medical marijuana, users may assert an affirmative defense of medical necessity if they face criminal prosecution.3,6 Possession of marijuana remains illegal under federal law, however, regardless of one’s reason for having it.7,8 Since October 2009, the Attorney General’s office has discouraged federal prosecutions of persons “whose actions are in clear and unambiguous compliance with existing state laws providing for the medical use of marijuana.”9 But given the remaining conflicts between state and federal laws, “the legal implications of certifying patients for medical marijuana remain unclear.”10
Physicians have few resources to instruct them on the legal risks of certifying medical marijuana. When Canada legalized medical marijuana, the organization that provides malpractice insurance to Canadian physicians told its members that “prescribing medical marijuana cannot be compared to prescribing prescription drugs” and recommended that physicians obtain signed release forms documenting that they have discussed the risks of medical marijuana with patients.11 For some risky approved drugs, the FDA has established a risk evaluation and mitigation strategy, but no such guidance is available for marijuana.
Highlighting the benefits and risks
Proponents of medical marijuana claim that Cannabis can help patients, and dispassionate experts acknowledge that at least modest evidence supports the benefits of using “marijuana for nausea and vomiting related to chemotherapy, specific pain syndromes, and spasticity from multiple sclerosis.”10 For several other conditions— HIV/AIDS, depression, anxiety disorders, sleep disorders, psychosis, Tourette syndrome—evidence of benefit is poor.12 Rigorous evaluation of medical marijuana is difficult because the plant contains hundreds of active chemical compounds. The chemical content of marijuana is highly variable, depending on its preparation and administration,10,13—one reason why only a few good randomized controlled trials of marijuana have been conducted.
Marijuana has several side effects and carries many health risks (Table 1).4,14-20
On the highway: Marijuana and driving
Marijuana use impairs driving ability.14 Following enactment of more lenient marijuana laws, several states have reported higher numbers of fatally injured drivers who tested positive for Cannabis21-23 and had a positive screen of tetrahydrocannabinol (THC) in driving under the influence cases.24,25 One study showed that a blood THC concentration >5 ng/mL (comparable to a blood alcohol concentration of 0.15%) increased the crash odds ratio to 6.6.25,26
Marijuana impairs reaction time, information processing, motor performance, attention, and visual processing.14,16,27,28 Drivers who are under the influence of marijuana make more driving errors, despite being cautious about how they react to traffic.29 Even after weeks of abstinence, previous daily users of marijuana display some cognitive processing and driving-related impairments.30,31
Courts have found physicians negligent if their patients’ treatment-induced driving impairments injured others when the risk of driving-related injury was foreseeable.32 The Massachusetts case of Coombes v Florio33 likened the physician’s duty to that of a liquor store that sells alcohol to a minor who subsequently crashes, or to a father who did not lock his firearms away from his violent adult son.
Three variables influence a court’s judgment about whether risk is “foreseeable”: “the relative knowledge of the risk as between lay persons and physicians, whether the patient has previously used the medication and/or experienced the adverse effect, and whether a warning would otherwise have been futile.”34 A physician who certified a patient to use marijuana without adequately explaining the risks of driving might be vulnerable to a lawsuit if the patient’s driving accident occurred while the patient was under the influence of the drug. Recommending marijuana as a treatment also could lead to a malpractice action if a patient experienced and was harmed by the drug’s adverse effects.
Other drags
Another malpractice risk stems from marijuana’s addiction potential. Although many people think Cannabis isn’t addictive, nearly 10% of all marijuana users develop dependence.10,17 Regular Cannabis users are more likely to use alcohol, tobacco, and “recreational” drugs,17,35 and using alcohol and marijuana together greatly heightens the risk of driving accidents.14,15 Although we know of no case that relates directly to marijuana, physicians have faced lawsuits for injuries stemming from a patient’s addiction to prescription drugs,36 particularly when the patient’s behavior should have led the physician to suspect abuse or overuse.37
When certifying marijuana use, physicians have the same obligations that apply to more conventional medical treatment:
• establishing a proper physician–patient relationship
• taking an appropriate history
• conducting a proper examination
• reviewing records
• developing a comprehensive treatment plan
• weighing risks and alternatives
• providing follow-up care.
Neglecting these steps could lead to medical board sanctions and suspension or revocation of a medical license.13
The blunt reality
We advise against recommending marijuana for your patients. But if you have exhausted the alternatives, see marijuana as the last resort, and believe that taking the risk is worth the potential benefit, you can take some steps to reduce your legal risk (Table 2,1,32,37,38 and Table 313).
Bottom LinE
Medical marijuana is a controversial topic that demands more rigorous research and regulatory consideration. In the present climate, cautious physicians will avoid recommending marijuana to their patients. If you think that a patient has a medical indication, with no treatment option better than medical marijuana, be sure to understand the medical and legal ramifications before you authorize its use.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
I practice in a state that allows medical marijuana use. A few of my patients have asked me to help them obtain marijuana for their conditions. How risky would it be to oblige?
Submitted by “Dr. J”
In recent years, public debate about marijuana has acquired 2 new dimensions: (1) the wishes and medical needs of people who seek marijuana for its purported health benefits, and (2) the role of physicians who practice where “medical marijuana” is legal. This article, the authors’ joint effort to address Dr. J’s concerns, hits 3 topics:
• the intersection of marijuana policy and health care in the United States
• the risks and possible benefits of marijuana use
• the medicolegal problems faced by physicians who might advise patients to use marijuana.
Legal haze
Two cannabinoids—dronabinol and nabilone—have received FDA approval as appetite enhancers and anti-nausea agents. Third-party payors usually cover these types of medications, but no insurer pays for medical marijuana.1 The Controlled Substances Act of 19702 classified marijuana as a Schedule I drug because of its abuse potential, lack of accepted medical applications, and uncertain safety. The FDA has not approved marijuana use for any medical condition.
Although people commonly speak of “prescribing” marijuana, physicians cannot legally do this in the United States. What physicians may do, in the 23 states that allow medical marijuana, is recommend or certify a patient’s marijuana use—an action that has constitutional protection under the First Amendment’s freedom of speech clause.3,4
A physician may complete documentation that a patient has one of the qualifying medical conditions for which the jurisdiction has legalized medical marijuana. Either the patient or the physician then submits that documentation to the appropriate government agency (eg, the state’s department of health).
If the documentation receives approval, the agency will issue the patient a registration card that allows possession of medical marijuana, with which the patient can obtain or grow a small amount of marijuana. The cannabinoid content of marijuana products varies considerably,5 and physicians who certify marijuana typically defer dosage recommendations to the patient or the dispensary.1
In states that allow medical marijuana, users may assert an affirmative defense of medical necessity if they face criminal prosecution.3,6 Possession of marijuana remains illegal under federal law, however, regardless of one’s reason for having it.7,8 Since October 2009, the Attorney General’s office has discouraged federal prosecutions of persons “whose actions are in clear and unambiguous compliance with existing state laws providing for the medical use of marijuana.”9 But given the remaining conflicts between state and federal laws, “the legal implications of certifying patients for medical marijuana remain unclear.”10
Physicians have few resources to instruct them on the legal risks of certifying medical marijuana. When Canada legalized medical marijuana, the organization that provides malpractice insurance to Canadian physicians told its members that “prescribing medical marijuana cannot be compared to prescribing prescription drugs” and recommended that physicians obtain signed release forms documenting that they have discussed the risks of medical marijuana with patients.11 For some risky approved drugs, the FDA has established a risk evaluation and mitigation strategy, but no such guidance is available for marijuana.
Highlighting the benefits and risks
Proponents of medical marijuana claim that Cannabis can help patients, and dispassionate experts acknowledge that at least modest evidence supports the benefits of using “marijuana for nausea and vomiting related to chemotherapy, specific pain syndromes, and spasticity from multiple sclerosis.”10 For several other conditions— HIV/AIDS, depression, anxiety disorders, sleep disorders, psychosis, Tourette syndrome—evidence of benefit is poor.12 Rigorous evaluation of medical marijuana is difficult because the plant contains hundreds of active chemical compounds. The chemical content of marijuana is highly variable, depending on its preparation and administration,10,13—one reason why only a few good randomized controlled trials of marijuana have been conducted.
Marijuana has several side effects and carries many health risks (Table 1).4,14-20
On the highway: Marijuana and driving
Marijuana use impairs driving ability.14 Following enactment of more lenient marijuana laws, several states have reported higher numbers of fatally injured drivers who tested positive for Cannabis21-23 and had a positive screen of tetrahydrocannabinol (THC) in driving under the influence cases.24,25 One study showed that a blood THC concentration >5 ng/mL (comparable to a blood alcohol concentration of 0.15%) increased the crash odds ratio to 6.6.25,26
Marijuana impairs reaction time, information processing, motor performance, attention, and visual processing.14,16,27,28 Drivers who are under the influence of marijuana make more driving errors, despite being cautious about how they react to traffic.29 Even after weeks of abstinence, previous daily users of marijuana display some cognitive processing and driving-related impairments.30,31
Courts have found physicians negligent if their patients’ treatment-induced driving impairments injured others when the risk of driving-related injury was foreseeable.32 The Massachusetts case of Coombes v Florio33 likened the physician’s duty to that of a liquor store that sells alcohol to a minor who subsequently crashes, or to a father who did not lock his firearms away from his violent adult son.
Three variables influence a court’s judgment about whether risk is “foreseeable”: “the relative knowledge of the risk as between lay persons and physicians, whether the patient has previously used the medication and/or experienced the adverse effect, and whether a warning would otherwise have been futile.”34 A physician who certified a patient to use marijuana without adequately explaining the risks of driving might be vulnerable to a lawsuit if the patient’s driving accident occurred while the patient was under the influence of the drug. Recommending marijuana as a treatment also could lead to a malpractice action if a patient experienced and was harmed by the drug’s adverse effects.
Other drags
Another malpractice risk stems from marijuana’s addiction potential. Although many people think Cannabis isn’t addictive, nearly 10% of all marijuana users develop dependence.10,17 Regular Cannabis users are more likely to use alcohol, tobacco, and “recreational” drugs,17,35 and using alcohol and marijuana together greatly heightens the risk of driving accidents.14,15 Although we know of no case that relates directly to marijuana, physicians have faced lawsuits for injuries stemming from a patient’s addiction to prescription drugs,36 particularly when the patient’s behavior should have led the physician to suspect abuse or overuse.37
When certifying marijuana use, physicians have the same obligations that apply to more conventional medical treatment:
• establishing a proper physician–patient relationship
• taking an appropriate history
• conducting a proper examination
• reviewing records
• developing a comprehensive treatment plan
• weighing risks and alternatives
• providing follow-up care.
Neglecting these steps could lead to medical board sanctions and suspension or revocation of a medical license.13
The blunt reality
We advise against recommending marijuana for your patients. But if you have exhausted the alternatives, see marijuana as the last resort, and believe that taking the risk is worth the potential benefit, you can take some steps to reduce your legal risk (Table 2,1,32,37,38 and Table 313).
Bottom LinE
Medical marijuana is a controversial topic that demands more rigorous research and regulatory consideration. In the present climate, cautious physicians will avoid recommending marijuana to their patients. If you think that a patient has a medical indication, with no treatment option better than medical marijuana, be sure to understand the medical and legal ramifications before you authorize its use.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474-2483.
2. Controlled Substances Act title 21, §801.
3. Frezza C. Medical marijuana: a drug without a medical model. Georgetown Law J. 2013;101:1117-1145.
4. Conant v Walters, 309 F3d 629, 637 (9th Cir 2002).
5. Vandrey R, Raber JC, Raber ME, et al. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313(24):2491-2493.
6. Thompson AE. JAMA patient page. Medical marijuana. JAMA. 2015;313(24):2508.
7. United States v Oakland Cannabis Buyers’ Cooperative, 532 U.S. 483 (2001).
8. Gonzales v Raich, 545 U.S. 1 (2005).
9. Ogden DW. Memorandum for selected United States Attorneys on investigations and prosecutions in states authorizing the medical use of marijuana. http://www. justice.gov/opa/blog/memorandum-selected-united-state-attorneys-investigations-and-prosecutions-states. Published October 19, 2009. Accessed July 11, 2015.
10. D’Souza DC, Ranganathan M. Medical marijuana: is the cart before the horse? JAMA. 2015;313(24):2431-2432.
11. Picard A. Pot-prescribing doctors warned. The Globe and Mail. http://www.theglobeandmail.com/news/national/ pot-prescribing-doctors-warned/article22506373. Published October 19, 2005. Accessed July 21, 2015.
12. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
13. Barthwell AG, Baxter LE, Cermak T, et al. The role of the physician in “medical” marijuana: American Society of Addiction Medicine. http://www.aoaam.org/usr/ ASAM_Med_Marijuana_White_Paper_Final.pdf. Published September 2010. Accessed July 11, 2015.
14. Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109-119.
15. Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478-492.
16. Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52-60.
17. Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19-35.
18. Huang YH, Zhang ZF, Tashkin DP, et al. An epidemiologic review of marijuana and cancer: an update. Cancer Epidemiol Biomarkers Prev. 2015;24(1):15-31.
19. Delforterie MJ, Lynskey MT, Huizink AC, et al. The relationship between cannabis involvement and suicidal thoughts and behaviors. Drug Alcohol Depend. 2015;150:98-104.
20. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot-a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54.
21. Masten SV, Guenzburger GV. Changes in driver cannabinoid prevalence in 12 U.S. states after implementing medical marijuana laws. J Safety Res. 2014;50:35-52.
22. Pollini RA, Romano E, Johnson MB, et al. The impact of marijuana decriminalization on California drivers. Drug Alcohol Depend. 2015;150:135-140.
23. Salomonsen-Sautel S, Min SJ, Sakai JT, et al. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144.
24. Urfer S, Morton J, Beall V, et al. Analysis of Δ9- tetrahydrocannabinol driving under the influence of drug cases in Colorado from January 2011 to February 2014. J Anal Toxicol. 2014;38(8):575-581.
25. Couper FJ, Peterson BL. The prevalence of marijuana in suspected impaired driving cases in Washington state. J Anal Toxicol. 2014;38(8):569-574.
26. Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239-248.
27. Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101-106.
28. Schwitzer T, Schwan R, Angioi-Duprez K, et al. The cannabinoid system and visual processing: a review on experimental findings and clinical presumptions. Eur Neuropsychopharmacol. 2015;25(1):100-112.
29. Neavyn MJ, Blohm E, Babu KM, et al. Medical marijuana and driving: a review. J Med Toxicol. 2014;10(3):269-279.
30. Bosker WM, Karschner EL, Lee D, et al. Sustained abstinence improves psychomotor function in chronic daily cannabis smokers. Paper presented at: SOFT 2012: Society of Forensic Toxicologists 2012 Annual Meeting; July 1-6, 2012; Boston, MA.
31. Fabritius M, Augsburger M, Chtioui H, et al. Fitness to drive and cannabis: validation of two blood THCCOOH thresholds to distinguish occasional users from heavy users. Forensic Sci Int. 2014;242:1-8.
32. Annas GJ. Doctors, drugs, and driving—tort liability for patient-caused accidents. New Engl J Med. 2008;359(5):521-525.
33. Coombes v Florio, 877 NE2d 567 (Mass 2007).
34. McKenzie v Hawaii Permanente Medical Group, Inc. 47 P3d 209 (Haw 2002).
35. Ilgen MA, Bohnert K, Kleinberg F, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 2013;132(3):654-659.
36. Osborne v United States, 166 F Supp 2d 479 (SDW Va 2001).
37. Conrad-Hutsell v Colturi, 2002 Ohio App. LEXIS 2740 (2002).
38. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
1. Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474-2483.
2. Controlled Substances Act title 21, §801.
3. Frezza C. Medical marijuana: a drug without a medical model. Georgetown Law J. 2013;101:1117-1145.
4. Conant v Walters, 309 F3d 629, 637 (9th Cir 2002).
5. Vandrey R, Raber JC, Raber ME, et al. Cannabinoid dose and label accuracy in edible medical cannabis products. JAMA. 2015;313(24):2491-2493.
6. Thompson AE. JAMA patient page. Medical marijuana. JAMA. 2015;313(24):2508.
7. United States v Oakland Cannabis Buyers’ Cooperative, 532 U.S. 483 (2001).
8. Gonzales v Raich, 545 U.S. 1 (2005).
9. Ogden DW. Memorandum for selected United States Attorneys on investigations and prosecutions in states authorizing the medical use of marijuana. http://www. justice.gov/opa/blog/memorandum-selected-united-state-attorneys-investigations-and-prosecutions-states. Published October 19, 2009. Accessed July 11, 2015.
10. D’Souza DC, Ranganathan M. Medical marijuana: is the cart before the horse? JAMA. 2015;313(24):2431-2432.
11. Picard A. Pot-prescribing doctors warned. The Globe and Mail. http://www.theglobeandmail.com/news/national/ pot-prescribing-doctors-warned/article22506373. Published October 19, 2005. Accessed July 21, 2015.
12. Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
13. Barthwell AG, Baxter LE, Cermak T, et al. The role of the physician in “medical” marijuana: American Society of Addiction Medicine. http://www.aoaam.org/usr/ ASAM_Med_Marijuana_White_Paper_Final.pdf. Published September 2010. Accessed July 11, 2015.
14. Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109-119.
15. Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013;59(3):478-492.
16. Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52-60.
17. Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19-35.
18. Huang YH, Zhang ZF, Tashkin DP, et al. An epidemiologic review of marijuana and cancer: an update. Cancer Epidemiol Biomarkers Prev. 2015;24(1):15-31.
19. Delforterie MJ, Lynskey MT, Huizink AC, et al. The relationship between cannabis involvement and suicidal thoughts and behaviors. Drug Alcohol Depend. 2015;150:98-104.
20. Radhakrishnan R, Wilkinson ST, D’Souza DC. Gone to pot-a review of the association between cannabis and psychosis. Front Psychiatry. 2014;5:54.
21. Masten SV, Guenzburger GV. Changes in driver cannabinoid prevalence in 12 U.S. states after implementing medical marijuana laws. J Safety Res. 2014;50:35-52.
22. Pollini RA, Romano E, Johnson MB, et al. The impact of marijuana decriminalization on California drivers. Drug Alcohol Depend. 2015;150:135-140.
23. Salomonsen-Sautel S, Min SJ, Sakai JT, et al. Trends in fatal motor vehicle crashes before and after marijuana commercialization in Colorado. Drug Alcohol Depend. 2014;140:137-144.
24. Urfer S, Morton J, Beall V, et al. Analysis of Δ9- tetrahydrocannabinol driving under the influence of drug cases in Colorado from January 2011 to February 2014. J Anal Toxicol. 2014;38(8):575-581.
25. Couper FJ, Peterson BL. The prevalence of marijuana in suspected impaired driving cases in Washington state. J Anal Toxicol. 2014;38(8):569-574.
26. Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239-248.
27. Ashton CH. Pharmacology and effects of cannabis: a brief review. Br J Psychiatry. 2001;178:101-106.
28. Schwitzer T, Schwan R, Angioi-Duprez K, et al. The cannabinoid system and visual processing: a review on experimental findings and clinical presumptions. Eur Neuropsychopharmacol. 2015;25(1):100-112.
29. Neavyn MJ, Blohm E, Babu KM, et al. Medical marijuana and driving: a review. J Med Toxicol. 2014;10(3):269-279.
30. Bosker WM, Karschner EL, Lee D, et al. Sustained abstinence improves psychomotor function in chronic daily cannabis smokers. Paper presented at: SOFT 2012: Society of Forensic Toxicologists 2012 Annual Meeting; July 1-6, 2012; Boston, MA.
31. Fabritius M, Augsburger M, Chtioui H, et al. Fitness to drive and cannabis: validation of two blood THCCOOH thresholds to distinguish occasional users from heavy users. Forensic Sci Int. 2014;242:1-8.
32. Annas GJ. Doctors, drugs, and driving—tort liability for patient-caused accidents. New Engl J Med. 2008;359(5):521-525.
33. Coombes v Florio, 877 NE2d 567 (Mass 2007).
34. McKenzie v Hawaii Permanente Medical Group, Inc. 47 P3d 209 (Haw 2002).
35. Ilgen MA, Bohnert K, Kleinberg F, et al. Characteristics of adults seeking medical marijuana certification. Drug Alcohol Depend. 2013;132(3):654-659.
36. Osborne v United States, 166 F Supp 2d 479 (SDW Va 2001).
37. Conrad-Hutsell v Colturi, 2002 Ohio App. LEXIS 2740 (2002).
38. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.