User login
Before you hit 'send': Will an e-mail to your patient put you at legal risk?
Dear Dr. Mossman,
Some of my patients e-mail me questions about their prescriptions, test results, treatment, appointments, etc. I’m often unsure about the best way to respond. If I use e-mail to communicate with patients, what step(s) should I take to minimize medicolegal risks?
Submitted by “Dr. V”
Medicine adopts new communication technologies cautiously. Calling patients seems unremarkable to us now, but it took decades after the invention of the telephone for doctors to feel comfortable talking to patients other than in face-to-face meetings.1,2
Patients want to communicate with their physicians via electronic mail,3 but concerns about security, confidentiality, and liability stop many physicians from using e-mail in their practice. Yet many medical organizations, including the Institute of Medicine,4 the American Medical Association,5 and the American Psychiatric Association,6 recognize that e-mail can facilitate care, if used properly.
Although e-mailing patients may feel awkward, a growing minority of clinicians regularly use e-mail for patient communication.2,7 In this article, we discuss ways to help safeguard your patients and their communications and to protect yourself from legal headaches.8
As you’re reading, please remember that we’re discussing communications to patients through standard e-mail, not secure portals (such as MyChart) that allow patients to contact physicians confidentially through their electronic medical records.
Privacy and security
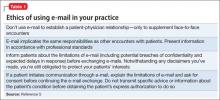
Doctor-patient e-mails implicate the same professional, ethical, and legal responsibilities that govern any communication with patients.2,9,10 If handled improperly, outside-the-office doctor-patient communication can breach traditional duties to protect confidentiality, or they can violate provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA).11 Confidentiality breaches can lead to malpractice litigation, and HIPAA infractions can result in civil and criminal penalties levied by federal agencies.12 Further, e-mails that breach ethical standards (Table 15) can generate complaints to your state’s medical licensure board.
E-mail appeals to many patients, if for no other reason than to save time or avoid the inconvenience of playing “phone tag” with the doctor’s office. But e-mail has drawbacks. Patients may think or behave as though online communications are intimate and confidential, but they usually aren’t. If e-mail programs are left open or aren’t password protected, friends and family members might look at messages and even act upon them. For this reason, doctors often cannot be sure whether they are communicating with the patient or with someone else who has gained access to the patient’s e-mail account.
Parties outside the treatment relationship could have access to e-mail data stored on servers.6 Also, it’s easy to misread or mistype an e-mail address and send confidential information to the wrong person. A truly “secure” e-mail exchange uses encryption software that protects messages during transmission and storage and requires users to authenticate who they are through actions that link their identity to the e-mail address.13 But some patients and physicians do not know about the availability of such security measures, and implementing them can feel cumbersome to those who are not computer savvy. Not surprisingly, then, recent studies have shown that such measures are used infrequently by physicians and patients.14
Topics for e-mail communication
One way to minimize potential privacy problems is to limit the topics and types of communication dealt with by e-mail. Several experts and organizations have published suggestions, recommendations, and resources for doing this with common practices (Table 2).6,7,15
Receiving e-mail permission
Many patients e-mail their physicians without the physicians’ prior agreement. But physicians who plan to use e-mail in their practice should get patients’ explicit consent. This can be done verbally, with the content of the discussion documented in the medical record. But it’s better to have patients authorize e-mail communications in writing by means of a permission form that also sets out your office’s e-mail policies, expected response times, and privacy limitations.
Commonly recommended contents of such forms5-7,9,15,16 include:
• discussing security mechanisms and limits of security
• e-mail encryption requirements (or waiving them, if the patient prefers)
• providing an expected response time
• indemnifying you or your institution for information loss caused by technical failure
• identifying who reads e-mails (eg, office staff members, a nurse, physician [only])
• asking patients to put their name and other identifying information in the body of the message, not the subject line
• asking patients to put the type of question in the subject line (eg, “prescription,” “appointment,” “billing”)
• asking patients to use the “auto reply” feature to acknowledge receipt of your messages.
In addition to using patient consent forms, other suggestions and recommendations for physicians include:
• Do not use e-mail to establish patient-physician relationships, only to supplement personal encounters.
• If you work for an agency or institution, know and follow its guidelines and policies.
• If a rule or “boundary” is breached (eg, a patient sends you a detailed e-mail on a topic beyond the scope of your previous agreement), address this directly in a treatment session.
• File e-mail correspondence, including your reply, in the patient’s medical record.
• Use encryption technology if it is available, practical, and user-friendly.
• Use a practice-dedicated e-mail address with an automatic response that explains when e-mail will be answered and reminds patients to seek immediate help for urgent matters.
Real legal risk
Earlier, we described conceivable legal risks that e-mail might create. But has e-mail caused legal problems for physicians? At least 3 recent published decisions answer: “Yes.” And, remember, only a fraction of legal cases lead to published decisions.
• Huffine v Department of Health17 concerns a psychiatrist who was censured by the Washington state medical quality assurance commission for several boundary crossings, including sending his adolescent patient overly intimate e-mails.
• Wheeler v Kron18 lists a variety of legal claims—intentional infliction of emotional distress, negligent infliction of emotional distress, general negligence, and medical malpractice—that arose from a psychiatrist’s e-mailed concerns about visitation arrangements in a divorcing couple’s custody dispute. Although the court dismissed the last 3 claims, it allowed the intentional infliction of emotional distress claim to proceed.
• Ortegoza v Kho19 includes excerpts of e-mails between a primary care physician and his married patient, with whom the physician had affair that led to a medical malpractice lawsuit.
Bottom Line
Most patients want to e-mail their physicians, and many psychiatrists find e-mail helpful in caring for patients. If you are using e-mail in your practice or are contemplating doing so, get the patient’s permission (preferably in writing), and follow the recommendations and guidelines cited in this article’s references.
Related Resources
• Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. http://jamia.oxfordjournals.org/content/5/1/104.long.
• Professional Risk Management Services, Inc. Sample email consent and guide to email use. www.psychprogram.com/currentpsychiatry.html.
1. Wieczorek SM. From telegraph to e-mail: preserving the doctor-patient relationship in a high-tech environment. ETC: A Review of General Semantics. 2010;67(3):311-327.
2. Spielberg AR. Online without a net: physician-patient communication by electronic mail. Am J Law Med. 1999;25(2-3):267-295.
3. Pelletier AL, Sutton GR, Walker RR. Are your patients ready for electronic communication? Fam Pract Manag. 2007;14(9):25-26.
4. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001.
5. American Medical Association. AMA Code of Medical Ethics. Opinion 5.026 - the use of electronic mail. http:// www.ama-assn.org/ama/pub/physician-resources/ medical-ethics/code-medical-ethics/opinion5026.page. Published June 2013. Accessed March 8, 2015.
6. American Psychiatric Association, Council on Psychiatry & Law. Resource document on telepsychiatry and related technologies in clinical psychiatry. http://www.psychiatry. org/learn/library--archives/resource-documents. Published January 2014. Accessed March 25, 2015.
7. Koh S, Cattell GM, Cochran DM, et al. Psychiatrists’ use of electronic communication and social media and a proposed framework for future guidelines. J Psychiatr Pract. 2013;19(3):254-263.
8. Sands DZ. Help for physicians contemplating use of e-mail with patients. J Am Med Inform Assoc. 2004;11(4):268-269.
9. Bovi AM; Council on Ethical and Judicial Affairs of the American Medical Association. Ethical guidelines for use of electronic mail between patients and physicians. Am J Bioeth. 2003;3(3):W-IF2.
10. Kuszler PC. A question of duty: common law legal issues resulting from physician response to unsolicited patient email inquiries. J Med Internet Res. 2000;2(3):E17.
11. 45 CFR Parts 160 and 164.
12. Vanderpool D. Hippa-should I be worried? Innov Clin Neurosci. 2012;9(11-12):51-55.
13. Tjora A, Tran T, Faxvaag A. Privacy vs. usability: a qualitative exploration of patients’ experiences with secure internet communication with their general practitioner. J Med Internet Res. 2005;7(2):e15.
14. Menachemi N, Prickett CT, Brooks RG. The use of physician-patient email: a follow-up examination of adoption and best-practice adherence 2005-2008. J Med Internet Res. 2011;13(1):e23.
15. Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. The AMIA Internet Working Group, Task Force on guidelines for the use of clinic-patient electronic mail. J Am Med Inform Assoc. 1998;5(1):104-111.
16. Car J, Sheikh A. Email consultations in health care: 2–acceptability and safe application. BMJ. 2004; 329(7463):439-442.
17. Huffine v Department of Health, 148 Wn App 1015 (Wash Ct App 2009).
18. Wheeler v Akron (NY Misc LEXIS 942, 2011) NY Slip Op 30530(U) (NY Misc 2011).
19. Ortegoza v Kho, 2013 U.S. Dist .LEXIS 69999 (SD Cal 2013).
Dear Dr. Mossman,
Some of my patients e-mail me questions about their prescriptions, test results, treatment, appointments, etc. I’m often unsure about the best way to respond. If I use e-mail to communicate with patients, what step(s) should I take to minimize medicolegal risks?
Submitted by “Dr. V”
Medicine adopts new communication technologies cautiously. Calling patients seems unremarkable to us now, but it took decades after the invention of the telephone for doctors to feel comfortable talking to patients other than in face-to-face meetings.1,2
Patients want to communicate with their physicians via electronic mail,3 but concerns about security, confidentiality, and liability stop many physicians from using e-mail in their practice. Yet many medical organizations, including the Institute of Medicine,4 the American Medical Association,5 and the American Psychiatric Association,6 recognize that e-mail can facilitate care, if used properly.
Although e-mailing patients may feel awkward, a growing minority of clinicians regularly use e-mail for patient communication.2,7 In this article, we discuss ways to help safeguard your patients and their communications and to protect yourself from legal headaches.8
As you’re reading, please remember that we’re discussing communications to patients through standard e-mail, not secure portals (such as MyChart) that allow patients to contact physicians confidentially through their electronic medical records.
Privacy and security
Doctor-patient e-mails implicate the same professional, ethical, and legal responsibilities that govern any communication with patients.2,9,10 If handled improperly, outside-the-office doctor-patient communication can breach traditional duties to protect confidentiality, or they can violate provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA).11 Confidentiality breaches can lead to malpractice litigation, and HIPAA infractions can result in civil and criminal penalties levied by federal agencies.12 Further, e-mails that breach ethical standards (Table 15) can generate complaints to your state’s medical licensure board.
E-mail appeals to many patients, if for no other reason than to save time or avoid the inconvenience of playing “phone tag” with the doctor’s office. But e-mail has drawbacks. Patients may think or behave as though online communications are intimate and confidential, but they usually aren’t. If e-mail programs are left open or aren’t password protected, friends and family members might look at messages and even act upon them. For this reason, doctors often cannot be sure whether they are communicating with the patient or with someone else who has gained access to the patient’s e-mail account.
Parties outside the treatment relationship could have access to e-mail data stored on servers.6 Also, it’s easy to misread or mistype an e-mail address and send confidential information to the wrong person. A truly “secure” e-mail exchange uses encryption software that protects messages during transmission and storage and requires users to authenticate who they are through actions that link their identity to the e-mail address.13 But some patients and physicians do not know about the availability of such security measures, and implementing them can feel cumbersome to those who are not computer savvy. Not surprisingly, then, recent studies have shown that such measures are used infrequently by physicians and patients.14
Topics for e-mail communication
One way to minimize potential privacy problems is to limit the topics and types of communication dealt with by e-mail. Several experts and organizations have published suggestions, recommendations, and resources for doing this with common practices (Table 2).6,7,15
Receiving e-mail permission
Many patients e-mail their physicians without the physicians’ prior agreement. But physicians who plan to use e-mail in their practice should get patients’ explicit consent. This can be done verbally, with the content of the discussion documented in the medical record. But it’s better to have patients authorize e-mail communications in writing by means of a permission form that also sets out your office’s e-mail policies, expected response times, and privacy limitations.
Commonly recommended contents of such forms5-7,9,15,16 include:
• discussing security mechanisms and limits of security
• e-mail encryption requirements (or waiving them, if the patient prefers)
• providing an expected response time
• indemnifying you or your institution for information loss caused by technical failure
• identifying who reads e-mails (eg, office staff members, a nurse, physician [only])
• asking patients to put their name and other identifying information in the body of the message, not the subject line
• asking patients to put the type of question in the subject line (eg, “prescription,” “appointment,” “billing”)
• asking patients to use the “auto reply” feature to acknowledge receipt of your messages.
In addition to using patient consent forms, other suggestions and recommendations for physicians include:
• Do not use e-mail to establish patient-physician relationships, only to supplement personal encounters.
• If you work for an agency or institution, know and follow its guidelines and policies.
• If a rule or “boundary” is breached (eg, a patient sends you a detailed e-mail on a topic beyond the scope of your previous agreement), address this directly in a treatment session.
• File e-mail correspondence, including your reply, in the patient’s medical record.
• Use encryption technology if it is available, practical, and user-friendly.
• Use a practice-dedicated e-mail address with an automatic response that explains when e-mail will be answered and reminds patients to seek immediate help for urgent matters.
Real legal risk
Earlier, we described conceivable legal risks that e-mail might create. But has e-mail caused legal problems for physicians? At least 3 recent published decisions answer: “Yes.” And, remember, only a fraction of legal cases lead to published decisions.
• Huffine v Department of Health17 concerns a psychiatrist who was censured by the Washington state medical quality assurance commission for several boundary crossings, including sending his adolescent patient overly intimate e-mails.
• Wheeler v Kron18 lists a variety of legal claims—intentional infliction of emotional distress, negligent infliction of emotional distress, general negligence, and medical malpractice—that arose from a psychiatrist’s e-mailed concerns about visitation arrangements in a divorcing couple’s custody dispute. Although the court dismissed the last 3 claims, it allowed the intentional infliction of emotional distress claim to proceed.
• Ortegoza v Kho19 includes excerpts of e-mails between a primary care physician and his married patient, with whom the physician had affair that led to a medical malpractice lawsuit.
Bottom Line
Most patients want to e-mail their physicians, and many psychiatrists find e-mail helpful in caring for patients. If you are using e-mail in your practice or are contemplating doing so, get the patient’s permission (preferably in writing), and follow the recommendations and guidelines cited in this article’s references.
Related Resources
• Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. http://jamia.oxfordjournals.org/content/5/1/104.long.
• Professional Risk Management Services, Inc. Sample email consent and guide to email use. www.psychprogram.com/currentpsychiatry.html.
Dear Dr. Mossman,
Some of my patients e-mail me questions about their prescriptions, test results, treatment, appointments, etc. I’m often unsure about the best way to respond. If I use e-mail to communicate with patients, what step(s) should I take to minimize medicolegal risks?
Submitted by “Dr. V”
Medicine adopts new communication technologies cautiously. Calling patients seems unremarkable to us now, but it took decades after the invention of the telephone for doctors to feel comfortable talking to patients other than in face-to-face meetings.1,2
Patients want to communicate with their physicians via electronic mail,3 but concerns about security, confidentiality, and liability stop many physicians from using e-mail in their practice. Yet many medical organizations, including the Institute of Medicine,4 the American Medical Association,5 and the American Psychiatric Association,6 recognize that e-mail can facilitate care, if used properly.
Although e-mailing patients may feel awkward, a growing minority of clinicians regularly use e-mail for patient communication.2,7 In this article, we discuss ways to help safeguard your patients and their communications and to protect yourself from legal headaches.8
As you’re reading, please remember that we’re discussing communications to patients through standard e-mail, not secure portals (such as MyChart) that allow patients to contact physicians confidentially through their electronic medical records.
Privacy and security
Doctor-patient e-mails implicate the same professional, ethical, and legal responsibilities that govern any communication with patients.2,9,10 If handled improperly, outside-the-office doctor-patient communication can breach traditional duties to protect confidentiality, or they can violate provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA).11 Confidentiality breaches can lead to malpractice litigation, and HIPAA infractions can result in civil and criminal penalties levied by federal agencies.12 Further, e-mails that breach ethical standards (Table 15) can generate complaints to your state’s medical licensure board.
E-mail appeals to many patients, if for no other reason than to save time or avoid the inconvenience of playing “phone tag” with the doctor’s office. But e-mail has drawbacks. Patients may think or behave as though online communications are intimate and confidential, but they usually aren’t. If e-mail programs are left open or aren’t password protected, friends and family members might look at messages and even act upon them. For this reason, doctors often cannot be sure whether they are communicating with the patient or with someone else who has gained access to the patient’s e-mail account.
Parties outside the treatment relationship could have access to e-mail data stored on servers.6 Also, it’s easy to misread or mistype an e-mail address and send confidential information to the wrong person. A truly “secure” e-mail exchange uses encryption software that protects messages during transmission and storage and requires users to authenticate who they are through actions that link their identity to the e-mail address.13 But some patients and physicians do not know about the availability of such security measures, and implementing them can feel cumbersome to those who are not computer savvy. Not surprisingly, then, recent studies have shown that such measures are used infrequently by physicians and patients.14
Topics for e-mail communication
One way to minimize potential privacy problems is to limit the topics and types of communication dealt with by e-mail. Several experts and organizations have published suggestions, recommendations, and resources for doing this with common practices (Table 2).6,7,15
Receiving e-mail permission
Many patients e-mail their physicians without the physicians’ prior agreement. But physicians who plan to use e-mail in their practice should get patients’ explicit consent. This can be done verbally, with the content of the discussion documented in the medical record. But it’s better to have patients authorize e-mail communications in writing by means of a permission form that also sets out your office’s e-mail policies, expected response times, and privacy limitations.
Commonly recommended contents of such forms5-7,9,15,16 include:
• discussing security mechanisms and limits of security
• e-mail encryption requirements (or waiving them, if the patient prefers)
• providing an expected response time
• indemnifying you or your institution for information loss caused by technical failure
• identifying who reads e-mails (eg, office staff members, a nurse, physician [only])
• asking patients to put their name and other identifying information in the body of the message, not the subject line
• asking patients to put the type of question in the subject line (eg, “prescription,” “appointment,” “billing”)
• asking patients to use the “auto reply” feature to acknowledge receipt of your messages.
In addition to using patient consent forms, other suggestions and recommendations for physicians include:
• Do not use e-mail to establish patient-physician relationships, only to supplement personal encounters.
• If you work for an agency or institution, know and follow its guidelines and policies.
• If a rule or “boundary” is breached (eg, a patient sends you a detailed e-mail on a topic beyond the scope of your previous agreement), address this directly in a treatment session.
• File e-mail correspondence, including your reply, in the patient’s medical record.
• Use encryption technology if it is available, practical, and user-friendly.
• Use a practice-dedicated e-mail address with an automatic response that explains when e-mail will be answered and reminds patients to seek immediate help for urgent matters.
Real legal risk
Earlier, we described conceivable legal risks that e-mail might create. But has e-mail caused legal problems for physicians? At least 3 recent published decisions answer: “Yes.” And, remember, only a fraction of legal cases lead to published decisions.
• Huffine v Department of Health17 concerns a psychiatrist who was censured by the Washington state medical quality assurance commission for several boundary crossings, including sending his adolescent patient overly intimate e-mails.
• Wheeler v Kron18 lists a variety of legal claims—intentional infliction of emotional distress, negligent infliction of emotional distress, general negligence, and medical malpractice—that arose from a psychiatrist’s e-mailed concerns about visitation arrangements in a divorcing couple’s custody dispute. Although the court dismissed the last 3 claims, it allowed the intentional infliction of emotional distress claim to proceed.
• Ortegoza v Kho19 includes excerpts of e-mails between a primary care physician and his married patient, with whom the physician had affair that led to a medical malpractice lawsuit.
Bottom Line
Most patients want to e-mail their physicians, and many psychiatrists find e-mail helpful in caring for patients. If you are using e-mail in your practice or are contemplating doing so, get the patient’s permission (preferably in writing), and follow the recommendations and guidelines cited in this article’s references.
Related Resources
• Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. http://jamia.oxfordjournals.org/content/5/1/104.long.
• Professional Risk Management Services, Inc. Sample email consent and guide to email use. www.psychprogram.com/currentpsychiatry.html.
1. Wieczorek SM. From telegraph to e-mail: preserving the doctor-patient relationship in a high-tech environment. ETC: A Review of General Semantics. 2010;67(3):311-327.
2. Spielberg AR. Online without a net: physician-patient communication by electronic mail. Am J Law Med. 1999;25(2-3):267-295.
3. Pelletier AL, Sutton GR, Walker RR. Are your patients ready for electronic communication? Fam Pract Manag. 2007;14(9):25-26.
4. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001.
5. American Medical Association. AMA Code of Medical Ethics. Opinion 5.026 - the use of electronic mail. http:// www.ama-assn.org/ama/pub/physician-resources/ medical-ethics/code-medical-ethics/opinion5026.page. Published June 2013. Accessed March 8, 2015.
6. American Psychiatric Association, Council on Psychiatry & Law. Resource document on telepsychiatry and related technologies in clinical psychiatry. http://www.psychiatry. org/learn/library--archives/resource-documents. Published January 2014. Accessed March 25, 2015.
7. Koh S, Cattell GM, Cochran DM, et al. Psychiatrists’ use of electronic communication and social media and a proposed framework for future guidelines. J Psychiatr Pract. 2013;19(3):254-263.
8. Sands DZ. Help for physicians contemplating use of e-mail with patients. J Am Med Inform Assoc. 2004;11(4):268-269.
9. Bovi AM; Council on Ethical and Judicial Affairs of the American Medical Association. Ethical guidelines for use of electronic mail between patients and physicians. Am J Bioeth. 2003;3(3):W-IF2.
10. Kuszler PC. A question of duty: common law legal issues resulting from physician response to unsolicited patient email inquiries. J Med Internet Res. 2000;2(3):E17.
11. 45 CFR Parts 160 and 164.
12. Vanderpool D. Hippa-should I be worried? Innov Clin Neurosci. 2012;9(11-12):51-55.
13. Tjora A, Tran T, Faxvaag A. Privacy vs. usability: a qualitative exploration of patients’ experiences with secure internet communication with their general practitioner. J Med Internet Res. 2005;7(2):e15.
14. Menachemi N, Prickett CT, Brooks RG. The use of physician-patient email: a follow-up examination of adoption and best-practice adherence 2005-2008. J Med Internet Res. 2011;13(1):e23.
15. Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. The AMIA Internet Working Group, Task Force on guidelines for the use of clinic-patient electronic mail. J Am Med Inform Assoc. 1998;5(1):104-111.
16. Car J, Sheikh A. Email consultations in health care: 2–acceptability and safe application. BMJ. 2004; 329(7463):439-442.
17. Huffine v Department of Health, 148 Wn App 1015 (Wash Ct App 2009).
18. Wheeler v Akron (NY Misc LEXIS 942, 2011) NY Slip Op 30530(U) (NY Misc 2011).
19. Ortegoza v Kho, 2013 U.S. Dist .LEXIS 69999 (SD Cal 2013).
1. Wieczorek SM. From telegraph to e-mail: preserving the doctor-patient relationship in a high-tech environment. ETC: A Review of General Semantics. 2010;67(3):311-327.
2. Spielberg AR. Online without a net: physician-patient communication by electronic mail. Am J Law Med. 1999;25(2-3):267-295.
3. Pelletier AL, Sutton GR, Walker RR. Are your patients ready for electronic communication? Fam Pract Manag. 2007;14(9):25-26.
4. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: National Academies Press; 2001.
5. American Medical Association. AMA Code of Medical Ethics. Opinion 5.026 - the use of electronic mail. http:// www.ama-assn.org/ama/pub/physician-resources/ medical-ethics/code-medical-ethics/opinion5026.page. Published June 2013. Accessed March 8, 2015.
6. American Psychiatric Association, Council on Psychiatry & Law. Resource document on telepsychiatry and related technologies in clinical psychiatry. http://www.psychiatry. org/learn/library--archives/resource-documents. Published January 2014. Accessed March 25, 2015.
7. Koh S, Cattell GM, Cochran DM, et al. Psychiatrists’ use of electronic communication and social media and a proposed framework for future guidelines. J Psychiatr Pract. 2013;19(3):254-263.
8. Sands DZ. Help for physicians contemplating use of e-mail with patients. J Am Med Inform Assoc. 2004;11(4):268-269.
9. Bovi AM; Council on Ethical and Judicial Affairs of the American Medical Association. Ethical guidelines for use of electronic mail between patients and physicians. Am J Bioeth. 2003;3(3):W-IF2.
10. Kuszler PC. A question of duty: common law legal issues resulting from physician response to unsolicited patient email inquiries. J Med Internet Res. 2000;2(3):E17.
11. 45 CFR Parts 160 and 164.
12. Vanderpool D. Hippa-should I be worried? Innov Clin Neurosci. 2012;9(11-12):51-55.
13. Tjora A, Tran T, Faxvaag A. Privacy vs. usability: a qualitative exploration of patients’ experiences with secure internet communication with their general practitioner. J Med Internet Res. 2005;7(2):e15.
14. Menachemi N, Prickett CT, Brooks RG. The use of physician-patient email: a follow-up examination of adoption and best-practice adherence 2005-2008. J Med Internet Res. 2011;13(1):e23.
15. Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. The AMIA Internet Working Group, Task Force on guidelines for the use of clinic-patient electronic mail. J Am Med Inform Assoc. 1998;5(1):104-111.
16. Car J, Sheikh A. Email consultations in health care: 2–acceptability and safe application. BMJ. 2004; 329(7463):439-442.
17. Huffine v Department of Health, 148 Wn App 1015 (Wash Ct App 2009).
18. Wheeler v Akron (NY Misc LEXIS 942, 2011) NY Slip Op 30530(U) (NY Misc 2011).
19. Ortegoza v Kho, 2013 U.S. Dist .LEXIS 69999 (SD Cal 2013).
Good, bad, and ugly: Prior authorization and medicolegal risk
Dear Dr. Mossman,
Where I practice, most health care plans won’t pay for certain medications without giving prior authorization (PA). Completing PA forms and making telephone calls take up time that could be better spent treating patients. I’m tempted to set a new policy of not doing PAs. If I do, might I face legal trouble?
Submitted by “Dr. A”
If you provide clinical care, you’ve probably dealt with third-party payers who require prior authorization (PA) before they will pay for certain treatments. Dr. A is not alone in feeling exasperated about the time it takes to complete a PA.1 After spending several hours each month waiting on hold and wading through stacks of paperwork, you may feel like Dr. A and consider refusing to do any more PAs.
But is Dr. A’s proposed solution a good idea? To address this question and the frustration that lies behind it, we’ll take a cue from Italian film director Sergio Leone and discuss:
• how PAs affect psychiatric care: the good, the bad, and the ugly
• potential exposure to professional liability and ethics complaints that might result from refusing or failing to seek PA
• strategies to reduce the burden of PAs while providing efficient, effective care.
The good
Recent decades have witnessed huge increases in spending on prescription medication. Psychotropics are no exception; state Medicaid spending for anti-psychotic medication grew from <$1 billion in 1995 to >$5.5 billion in 2005.2
Requiring a PA for expensive drugs is one way that third-party payers try to rein in costs and hold down insurance premiums. Imposing financial constraints often is just one aim of a pharmacy benefit management (PBM) program. Insurers also justify PBMs by pointing out that feedback to practitioners whose prescribing falls well outside the norm—in the form of mailed warnings, physician second opinions, or pharmacist consultation—can improve patient safety and encourage appropriate treatment options for enrolled patients.3,4 Examples of such benefits include reducing overuse of prescription opioids5 and antipsychotics among children,3 misuse of buprenorphine,6 and adverse effects from potentially inappropriate prescriptions.7
The bad
The bad news for doctors: Cost savings for payers come at the expense of providers and their practices, in the form of time spent doing paperwork and talking on the phone to complete PAs or contest PA decisions.8 Addressing PA requests costs an estimated $83,000 per physician per year. The total administrative burden for all 835,000 physicians who practice in the United States therefore is 868,000,000 hours, or $69 billion annually.9
To make matters worse, PA requirements may increase the overall cost of care. After Georgia Medicaid instituted PA requirements for second-generation antipsychotics (SGAs), average monthly per member drug costs fell $19.62, but average monthly outpatient treatment costs rose $31.59 per member.10 Pharmacy savings that result from requiring PAs for SGAs can be offset quickly by small increases in the hospitalization rate or emergency department visits.9,11
The ugly
Many physicians believe that the PA process undermines patient care by decreasing time devoted to direct patient contact, incentivizing suboptimal treatment, and limiting medication access.1,12,13 But do any data support this belief? Do PAs impede treatment for vulnerable persons with severe mental illnesses?
The answer, some studies suggest, is “Yes.” A Maine Medicaid PA policy slowed initiation of treatment for bipolar disorder by reducing the rate of starting non-preferred medications, although the same policy had no impact on patients already receiving treatment.14 Another study examined the effect of PA processes for inpatient psychiatry treatment and found that patients were less likely to be admitted on weekends, probably because PA review was not available on those days.15 A third study showed that PA requirements and resulting impediments to getting refills were correlated with medication discontinuation by patients with schizophrenia or bipolar disorder, which can increase the risk of decompensation, work-related problems, and hospitalization.16
Problems with PAs
Whether they are helpful or counterproductive, PAs are a practice reality. Dr. A’s proposed solution sounds appealing, but it might create ethical and legal problems.
Among the fundamental elements of ethical medical practice is physicians’ obligation to give patients “guidance … as to the optimal course of action” and to “advocate for patients in dealing with third parties when appropriate.”17 It’s fine for psychiatrists to consider prescribing treatments that patients’ health care coverage favors, but we also have to help patients weigh and evaluate costs, particularly when patients’ circumstances and medical interests militate strongly for options that third-party payers balk at paying for. Patients’ interests—not what’s expedient—are always physicians’ foremost concern.18
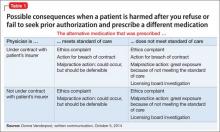
Beyond purely ethical considerations, you might face legal consequences if you refuse or fail to seek PAs for what you think is the proper medication. As Table 1 shows, one key factor is whether you are under contract with the patient’s insurance carrier; if you are, failure to seek a PA when appropriate may constitute a breach of the contract (Donna Vanderpool, written communication, October 5, 2014).
If the prescribed medication does not meet the standard of care and your patient suffers some harm, a licensing board complaint and investigation are possible. You also face exposure to a medical malpractice action. Although we do not know of any instances in which such an action has succeeded, 2 recent court decisions suggest that harm to a patient stemmed from failing to seek PA for a medication could constitute grounds for a lawsuit.19,20 Efforts to contain medical costs have been around for decades, and courts have held that physicians, third-party payers, and utilization review intermediaries are bound by “the standard of reasonable community practice”21 and should not let cost limitations “corrupt medical judgment.”22 Physicians who do not appeal limitations at odds with their medical judgment might bear responsibility for any injuries that occur.18,22
Managing PA requests
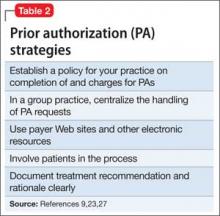
Given the inevitability of encountering PA requests and your ethical and professional obligations to help patients, what can you do (Table 29,23,27)?
Some practitioners charge patients for time spent completing PAs.23 Although physicians should “complete without charge the appropriate ‘simplified’ insurance claim form as a part of service to the patient;” they also may consider “a charge for more complex or multiple forms … in conformity with local custom.”24 Legally, physicians’ contracts with insurance panels may preclude charging such fees, but if a patient is being seen out of network, the physician does not have a contractual obligation and may charge.9 If your practice setting lets you choose which insurances you accept, the impact and burden of seeking PAs is a factor to consider when deciding whether to participate in a particular panel.23
In an interesting twist, an Ohio physician successfully sued a medical insurance administrator for the cost of his time responding to PA inquiries.25 Reasoning that the insurance administrator “should expect to pay for the reasonable value of” the doctor’s time because the PAs “were solely intended for the benefit of the insurance administrator” or parties whom the administrator served, the judge awarded the doctor $187.50 plus 8% interest.
Considerations that are more practical relate to how to triage and address the volume of PA requests. Some large medical practices centralize PAs and try to set up pre-approved plans of care or blanket approvals for frequently encountered conditions. Centralization also allows one key administrative assistant to develop skills in processing PA requests and to build relationships with payers.26
The administrative assistant also can compile lists of preferred alternative medications, PA forms, and payer Web sites. Using and submitting requests through payer Web sites can speed up PA processing, which saves time and money.27 As electronic health records improve, they may incorporate patients’ formularies and provide automatic alerts for required PAs.23
Patients should be involved, too. They can help to obtain relevant formulary information and to weigh alternative therapies. You can help them understand your role in the PA process, the reasoning behind your treatment recommendations, and the delays in picking up prescribed medications that waiting for PA approval can create.
It’s easy to get angry about PAs
Your best response, however, is to practice prudent and—within reason— cost-effective medicine. When generic or insurer-preferred medications are clinically appropriate and meet treatment guidelines, trying them first is sensible and defensible. If your patient fails the initial low-cost treatment, or if a low-cost choice isn’t appropriate, document this clearly and seek approval for a costlier treatment.9
BOTTOM LINE
Physicians have ethical and legal obligations to advocate for their patients’ needs and best interests. This sometimes includes completing prior authorization requests. Find strategies that minimize hassle and make sense in your practice, and seek efficient ways to document the medical necessity of requested tests, procedures, or therapies.
Acknowledgment
Drs. Marett and Mossman thanks Donna Vanderpool, MBA, JD, and Annette Reynolds, MD, for their helpful input in preparing this article.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brown CM, Richards K, Rascati KL, et al. Effects of a psychotherapeutic drug prior authorization (PA) requirement on patients and providers: a providers’ perspective. Adm Policy Ment Health. 2008;35(3):181-188.
2. Law MR, Ross-Degnan D, Soumerai SB. Effect of prior authorization of second-generation antipsychotic agents on pharmacy utilization and reimbursements. Psychiatr Serv. 2008;59(5):540-546.
3. Stein BD, Leckman-Westin E, Okeke E, et al. The effects of prior authorization policies on Medicaid-enrolled children’s use of antipsychotic medications: evidence from two Mid-Atlantic states. J Child Adolesc Psychopharmacol. 2014;24(7):374-381.
4. Adams KT. Prior authorization–still used, still an issue. Biotechnol Healthc. 2010;7(4):28.
5. Garcia MM, Angelini MC, Thomas T, et al. Implementation of an opioid management initiative by a state Medicaid program. J Manag Care Pharm. 2014;20(5):447-454.
6. Clark RE, Baxter JD, Barton BA, et al. The impact of prior authorization on buprenorphine dose, relapse rates, and cost for Massachusetts Medicaid beneficiaries with opioid dependence [published online July 9, 2014]. Health Serv Res. doi: 10.1111/1475-6773.12201.
7. Dunn RL, Harrison D, Ripley TL. The beers criteria as an outpatient screening tool for potentially inappropriate medications. Consult Pharm. 2011;26(10):754-763.
8. Lennertz MD, Wertheimer AI. Is prior authorization for prescribed drugs cost-effective? Drug Benefit Trends. 2008;20:136-139.
9. Bendix J. The prior authorization predicament. Med Econ. 2014;91(13)29-30,32,34-35.
10. Farley JF, Cline RR, Schommer JC, et al. Retrospective assessment of Medicaid step-therapy prior authorization policy for atypical antipsychotic medications. Clin Ther. 2008;30(8):1524-1539; discussion 1506-1507.
11. Abouzaid S, Jutkowitz E, Foley KA, et al. Economic impact of prior authorization policies for atypical antipsychotics in the treatment of schizophrenia. Popul Health Manag. 2010;13(5):247-254.
12. Brown CM, Nwokeji E, Rascati KL, et al. Development of the burden of prior authorization of psychotherapeutics (BoPAP) scale to assess the effects of prior authorization among Texas Medicaid providers. Adm Policy Ment Health. 2009;36(4):278-287.
13. Rascati KL, Brown CM. Prior authorization for antipsychotic medications—It’s not just about the money. Clin Ther. 2008;30(8):1506-1507.
14. Lu CY, Soumerai SB, Ross-Degnan D, et al. Unintended impacts of a Medicaid prior authorization policy on access to medications for bipolar disorder. Med Care. 2010;48(1):4-9.
15. Stephens RJ, White SE, Cudnik M, et al. Factors associated with longer lengths of stay for mental health emergency department patients. J Emerg Med. 2014; 47(4):412-419.
16. Brown JD, Barrett A, Caffery E, et al. Medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder. Psychiatr Serv. 2013;64(9):878-885.
17. American Medical Association. Opinion 10.01– Fundamental elements of the patient-physician relationship. http://www.ama-assn.org/ama/pub/ physician-resources/medical-ethics/code-medical-ethics/opinion1001.page?. Accessed October 11, 2014.
18. Hall RC. Ethical and legal implications of managed care. Gen Hosp Psychiatry. 1997;19(3):200-208.
19. Porter v Thadani, 2010 U.S. Dist. LEXIS 35145 (NH 2010).
20. NB ex rel Peacock v District of Columbia, 682 F3d 77 (DC Cir 2012).
21. Wilson v Blue Cross of Southern California, 222 Cal App 3d 660, 271 Cal Rptr 876 (1990).
22. Wickline v State of California, 192 Cal App 3d 1630, 239 Cal Rptr 810 (1986).
23. Terry K. Prior authorization made easier. Med Econ. 2007;84(20):34,38,40.
24. American Medical Association. Ethics Opinion 6.07– Insurance forms completion charges. http://www. ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion607.page? Updated June 1994. Accessed October 11, 2014.
25. Gibson v Medco Health Solutions, 06-CVF-106 (OH 2008).
26. Bendix J. Curing the prior authorization headache. Med Econ. 2013;90(19):24,26-27,29-31.
27. American Medical Association. Electronic prior authorization toolkit. Available at http://www.ama-assn.org/ama/pub/advocacy/topics/administrative-simplification-initiatives/electronic-transactions-toolkit/ prior-authorization.page. Accessed October 11, 2014.
Dear Dr. Mossman,
Where I practice, most health care plans won’t pay for certain medications without giving prior authorization (PA). Completing PA forms and making telephone calls take up time that could be better spent treating patients. I’m tempted to set a new policy of not doing PAs. If I do, might I face legal trouble?
Submitted by “Dr. A”
If you provide clinical care, you’ve probably dealt with third-party payers who require prior authorization (PA) before they will pay for certain treatments. Dr. A is not alone in feeling exasperated about the time it takes to complete a PA.1 After spending several hours each month waiting on hold and wading through stacks of paperwork, you may feel like Dr. A and consider refusing to do any more PAs.
But is Dr. A’s proposed solution a good idea? To address this question and the frustration that lies behind it, we’ll take a cue from Italian film director Sergio Leone and discuss:
• how PAs affect psychiatric care: the good, the bad, and the ugly
• potential exposure to professional liability and ethics complaints that might result from refusing or failing to seek PA
• strategies to reduce the burden of PAs while providing efficient, effective care.
The good
Recent decades have witnessed huge increases in spending on prescription medication. Psychotropics are no exception; state Medicaid spending for anti-psychotic medication grew from <$1 billion in 1995 to >$5.5 billion in 2005.2
Requiring a PA for expensive drugs is one way that third-party payers try to rein in costs and hold down insurance premiums. Imposing financial constraints often is just one aim of a pharmacy benefit management (PBM) program. Insurers also justify PBMs by pointing out that feedback to practitioners whose prescribing falls well outside the norm—in the form of mailed warnings, physician second opinions, or pharmacist consultation—can improve patient safety and encourage appropriate treatment options for enrolled patients.3,4 Examples of such benefits include reducing overuse of prescription opioids5 and antipsychotics among children,3 misuse of buprenorphine,6 and adverse effects from potentially inappropriate prescriptions.7
The bad
The bad news for doctors: Cost savings for payers come at the expense of providers and their practices, in the form of time spent doing paperwork and talking on the phone to complete PAs or contest PA decisions.8 Addressing PA requests costs an estimated $83,000 per physician per year. The total administrative burden for all 835,000 physicians who practice in the United States therefore is 868,000,000 hours, or $69 billion annually.9
To make matters worse, PA requirements may increase the overall cost of care. After Georgia Medicaid instituted PA requirements for second-generation antipsychotics (SGAs), average monthly per member drug costs fell $19.62, but average monthly outpatient treatment costs rose $31.59 per member.10 Pharmacy savings that result from requiring PAs for SGAs can be offset quickly by small increases in the hospitalization rate or emergency department visits.9,11
The ugly
Many physicians believe that the PA process undermines patient care by decreasing time devoted to direct patient contact, incentivizing suboptimal treatment, and limiting medication access.1,12,13 But do any data support this belief? Do PAs impede treatment for vulnerable persons with severe mental illnesses?
The answer, some studies suggest, is “Yes.” A Maine Medicaid PA policy slowed initiation of treatment for bipolar disorder by reducing the rate of starting non-preferred medications, although the same policy had no impact on patients already receiving treatment.14 Another study examined the effect of PA processes for inpatient psychiatry treatment and found that patients were less likely to be admitted on weekends, probably because PA review was not available on those days.15 A third study showed that PA requirements and resulting impediments to getting refills were correlated with medication discontinuation by patients with schizophrenia or bipolar disorder, which can increase the risk of decompensation, work-related problems, and hospitalization.16
Problems with PAs
Whether they are helpful or counterproductive, PAs are a practice reality. Dr. A’s proposed solution sounds appealing, but it might create ethical and legal problems.
Among the fundamental elements of ethical medical practice is physicians’ obligation to give patients “guidance … as to the optimal course of action” and to “advocate for patients in dealing with third parties when appropriate.”17 It’s fine for psychiatrists to consider prescribing treatments that patients’ health care coverage favors, but we also have to help patients weigh and evaluate costs, particularly when patients’ circumstances and medical interests militate strongly for options that third-party payers balk at paying for. Patients’ interests—not what’s expedient—are always physicians’ foremost concern.18
Beyond purely ethical considerations, you might face legal consequences if you refuse or fail to seek PAs for what you think is the proper medication. As Table 1 shows, one key factor is whether you are under contract with the patient’s insurance carrier; if you are, failure to seek a PA when appropriate may constitute a breach of the contract (Donna Vanderpool, written communication, October 5, 2014).
If the prescribed medication does not meet the standard of care and your patient suffers some harm, a licensing board complaint and investigation are possible. You also face exposure to a medical malpractice action. Although we do not know of any instances in which such an action has succeeded, 2 recent court decisions suggest that harm to a patient stemmed from failing to seek PA for a medication could constitute grounds for a lawsuit.19,20 Efforts to contain medical costs have been around for decades, and courts have held that physicians, third-party payers, and utilization review intermediaries are bound by “the standard of reasonable community practice”21 and should not let cost limitations “corrupt medical judgment.”22 Physicians who do not appeal limitations at odds with their medical judgment might bear responsibility for any injuries that occur.18,22
Managing PA requests
Given the inevitability of encountering PA requests and your ethical and professional obligations to help patients, what can you do (Table 29,23,27)?
Some practitioners charge patients for time spent completing PAs.23 Although physicians should “complete without charge the appropriate ‘simplified’ insurance claim form as a part of service to the patient;” they also may consider “a charge for more complex or multiple forms … in conformity with local custom.”24 Legally, physicians’ contracts with insurance panels may preclude charging such fees, but if a patient is being seen out of network, the physician does not have a contractual obligation and may charge.9 If your practice setting lets you choose which insurances you accept, the impact and burden of seeking PAs is a factor to consider when deciding whether to participate in a particular panel.23
In an interesting twist, an Ohio physician successfully sued a medical insurance administrator for the cost of his time responding to PA inquiries.25 Reasoning that the insurance administrator “should expect to pay for the reasonable value of” the doctor’s time because the PAs “were solely intended for the benefit of the insurance administrator” or parties whom the administrator served, the judge awarded the doctor $187.50 plus 8% interest.
Considerations that are more practical relate to how to triage and address the volume of PA requests. Some large medical practices centralize PAs and try to set up pre-approved plans of care or blanket approvals for frequently encountered conditions. Centralization also allows one key administrative assistant to develop skills in processing PA requests and to build relationships with payers.26
The administrative assistant also can compile lists of preferred alternative medications, PA forms, and payer Web sites. Using and submitting requests through payer Web sites can speed up PA processing, which saves time and money.27 As electronic health records improve, they may incorporate patients’ formularies and provide automatic alerts for required PAs.23
Patients should be involved, too. They can help to obtain relevant formulary information and to weigh alternative therapies. You can help them understand your role in the PA process, the reasoning behind your treatment recommendations, and the delays in picking up prescribed medications that waiting for PA approval can create.
It’s easy to get angry about PAs
Your best response, however, is to practice prudent and—within reason— cost-effective medicine. When generic or insurer-preferred medications are clinically appropriate and meet treatment guidelines, trying them first is sensible and defensible. If your patient fails the initial low-cost treatment, or if a low-cost choice isn’t appropriate, document this clearly and seek approval for a costlier treatment.9
BOTTOM LINE
Physicians have ethical and legal obligations to advocate for their patients’ needs and best interests. This sometimes includes completing prior authorization requests. Find strategies that minimize hassle and make sense in your practice, and seek efficient ways to document the medical necessity of requested tests, procedures, or therapies.
Acknowledgment
Drs. Marett and Mossman thanks Donna Vanderpool, MBA, JD, and Annette Reynolds, MD, for their helpful input in preparing this article.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
Where I practice, most health care plans won’t pay for certain medications without giving prior authorization (PA). Completing PA forms and making telephone calls take up time that could be better spent treating patients. I’m tempted to set a new policy of not doing PAs. If I do, might I face legal trouble?
Submitted by “Dr. A”
If you provide clinical care, you’ve probably dealt with third-party payers who require prior authorization (PA) before they will pay for certain treatments. Dr. A is not alone in feeling exasperated about the time it takes to complete a PA.1 After spending several hours each month waiting on hold and wading through stacks of paperwork, you may feel like Dr. A and consider refusing to do any more PAs.
But is Dr. A’s proposed solution a good idea? To address this question and the frustration that lies behind it, we’ll take a cue from Italian film director Sergio Leone and discuss:
• how PAs affect psychiatric care: the good, the bad, and the ugly
• potential exposure to professional liability and ethics complaints that might result from refusing or failing to seek PA
• strategies to reduce the burden of PAs while providing efficient, effective care.
The good
Recent decades have witnessed huge increases in spending on prescription medication. Psychotropics are no exception; state Medicaid spending for anti-psychotic medication grew from <$1 billion in 1995 to >$5.5 billion in 2005.2
Requiring a PA for expensive drugs is one way that third-party payers try to rein in costs and hold down insurance premiums. Imposing financial constraints often is just one aim of a pharmacy benefit management (PBM) program. Insurers also justify PBMs by pointing out that feedback to practitioners whose prescribing falls well outside the norm—in the form of mailed warnings, physician second opinions, or pharmacist consultation—can improve patient safety and encourage appropriate treatment options for enrolled patients.3,4 Examples of such benefits include reducing overuse of prescription opioids5 and antipsychotics among children,3 misuse of buprenorphine,6 and adverse effects from potentially inappropriate prescriptions.7
The bad
The bad news for doctors: Cost savings for payers come at the expense of providers and their practices, in the form of time spent doing paperwork and talking on the phone to complete PAs or contest PA decisions.8 Addressing PA requests costs an estimated $83,000 per physician per year. The total administrative burden for all 835,000 physicians who practice in the United States therefore is 868,000,000 hours, or $69 billion annually.9
To make matters worse, PA requirements may increase the overall cost of care. After Georgia Medicaid instituted PA requirements for second-generation antipsychotics (SGAs), average monthly per member drug costs fell $19.62, but average monthly outpatient treatment costs rose $31.59 per member.10 Pharmacy savings that result from requiring PAs for SGAs can be offset quickly by small increases in the hospitalization rate or emergency department visits.9,11
The ugly
Many physicians believe that the PA process undermines patient care by decreasing time devoted to direct patient contact, incentivizing suboptimal treatment, and limiting medication access.1,12,13 But do any data support this belief? Do PAs impede treatment for vulnerable persons with severe mental illnesses?
The answer, some studies suggest, is “Yes.” A Maine Medicaid PA policy slowed initiation of treatment for bipolar disorder by reducing the rate of starting non-preferred medications, although the same policy had no impact on patients already receiving treatment.14 Another study examined the effect of PA processes for inpatient psychiatry treatment and found that patients were less likely to be admitted on weekends, probably because PA review was not available on those days.15 A third study showed that PA requirements and resulting impediments to getting refills were correlated with medication discontinuation by patients with schizophrenia or bipolar disorder, which can increase the risk of decompensation, work-related problems, and hospitalization.16
Problems with PAs
Whether they are helpful or counterproductive, PAs are a practice reality. Dr. A’s proposed solution sounds appealing, but it might create ethical and legal problems.
Among the fundamental elements of ethical medical practice is physicians’ obligation to give patients “guidance … as to the optimal course of action” and to “advocate for patients in dealing with third parties when appropriate.”17 It’s fine for psychiatrists to consider prescribing treatments that patients’ health care coverage favors, but we also have to help patients weigh and evaluate costs, particularly when patients’ circumstances and medical interests militate strongly for options that third-party payers balk at paying for. Patients’ interests—not what’s expedient—are always physicians’ foremost concern.18
Beyond purely ethical considerations, you might face legal consequences if you refuse or fail to seek PAs for what you think is the proper medication. As Table 1 shows, one key factor is whether you are under contract with the patient’s insurance carrier; if you are, failure to seek a PA when appropriate may constitute a breach of the contract (Donna Vanderpool, written communication, October 5, 2014).
If the prescribed medication does not meet the standard of care and your patient suffers some harm, a licensing board complaint and investigation are possible. You also face exposure to a medical malpractice action. Although we do not know of any instances in which such an action has succeeded, 2 recent court decisions suggest that harm to a patient stemmed from failing to seek PA for a medication could constitute grounds for a lawsuit.19,20 Efforts to contain medical costs have been around for decades, and courts have held that physicians, third-party payers, and utilization review intermediaries are bound by “the standard of reasonable community practice”21 and should not let cost limitations “corrupt medical judgment.”22 Physicians who do not appeal limitations at odds with their medical judgment might bear responsibility for any injuries that occur.18,22
Managing PA requests
Given the inevitability of encountering PA requests and your ethical and professional obligations to help patients, what can you do (Table 29,23,27)?
Some practitioners charge patients for time spent completing PAs.23 Although physicians should “complete without charge the appropriate ‘simplified’ insurance claim form as a part of service to the patient;” they also may consider “a charge for more complex or multiple forms … in conformity with local custom.”24 Legally, physicians’ contracts with insurance panels may preclude charging such fees, but if a patient is being seen out of network, the physician does not have a contractual obligation and may charge.9 If your practice setting lets you choose which insurances you accept, the impact and burden of seeking PAs is a factor to consider when deciding whether to participate in a particular panel.23
In an interesting twist, an Ohio physician successfully sued a medical insurance administrator for the cost of his time responding to PA inquiries.25 Reasoning that the insurance administrator “should expect to pay for the reasonable value of” the doctor’s time because the PAs “were solely intended for the benefit of the insurance administrator” or parties whom the administrator served, the judge awarded the doctor $187.50 plus 8% interest.
Considerations that are more practical relate to how to triage and address the volume of PA requests. Some large medical practices centralize PAs and try to set up pre-approved plans of care or blanket approvals for frequently encountered conditions. Centralization also allows one key administrative assistant to develop skills in processing PA requests and to build relationships with payers.26
The administrative assistant also can compile lists of preferred alternative medications, PA forms, and payer Web sites. Using and submitting requests through payer Web sites can speed up PA processing, which saves time and money.27 As electronic health records improve, they may incorporate patients’ formularies and provide automatic alerts for required PAs.23
Patients should be involved, too. They can help to obtain relevant formulary information and to weigh alternative therapies. You can help them understand your role in the PA process, the reasoning behind your treatment recommendations, and the delays in picking up prescribed medications that waiting for PA approval can create.
It’s easy to get angry about PAs
Your best response, however, is to practice prudent and—within reason— cost-effective medicine. When generic or insurer-preferred medications are clinically appropriate and meet treatment guidelines, trying them first is sensible and defensible. If your patient fails the initial low-cost treatment, or if a low-cost choice isn’t appropriate, document this clearly and seek approval for a costlier treatment.9
BOTTOM LINE
Physicians have ethical and legal obligations to advocate for their patients’ needs and best interests. This sometimes includes completing prior authorization requests. Find strategies that minimize hassle and make sense in your practice, and seek efficient ways to document the medical necessity of requested tests, procedures, or therapies.
Acknowledgment
Drs. Marett and Mossman thanks Donna Vanderpool, MBA, JD, and Annette Reynolds, MD, for their helpful input in preparing this article.
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Brown CM, Richards K, Rascati KL, et al. Effects of a psychotherapeutic drug prior authorization (PA) requirement on patients and providers: a providers’ perspective. Adm Policy Ment Health. 2008;35(3):181-188.
2. Law MR, Ross-Degnan D, Soumerai SB. Effect of prior authorization of second-generation antipsychotic agents on pharmacy utilization and reimbursements. Psychiatr Serv. 2008;59(5):540-546.
3. Stein BD, Leckman-Westin E, Okeke E, et al. The effects of prior authorization policies on Medicaid-enrolled children’s use of antipsychotic medications: evidence from two Mid-Atlantic states. J Child Adolesc Psychopharmacol. 2014;24(7):374-381.
4. Adams KT. Prior authorization–still used, still an issue. Biotechnol Healthc. 2010;7(4):28.
5. Garcia MM, Angelini MC, Thomas T, et al. Implementation of an opioid management initiative by a state Medicaid program. J Manag Care Pharm. 2014;20(5):447-454.
6. Clark RE, Baxter JD, Barton BA, et al. The impact of prior authorization on buprenorphine dose, relapse rates, and cost for Massachusetts Medicaid beneficiaries with opioid dependence [published online July 9, 2014]. Health Serv Res. doi: 10.1111/1475-6773.12201.
7. Dunn RL, Harrison D, Ripley TL. The beers criteria as an outpatient screening tool for potentially inappropriate medications. Consult Pharm. 2011;26(10):754-763.
8. Lennertz MD, Wertheimer AI. Is prior authorization for prescribed drugs cost-effective? Drug Benefit Trends. 2008;20:136-139.
9. Bendix J. The prior authorization predicament. Med Econ. 2014;91(13)29-30,32,34-35.
10. Farley JF, Cline RR, Schommer JC, et al. Retrospective assessment of Medicaid step-therapy prior authorization policy for atypical antipsychotic medications. Clin Ther. 2008;30(8):1524-1539; discussion 1506-1507.
11. Abouzaid S, Jutkowitz E, Foley KA, et al. Economic impact of prior authorization policies for atypical antipsychotics in the treatment of schizophrenia. Popul Health Manag. 2010;13(5):247-254.
12. Brown CM, Nwokeji E, Rascati KL, et al. Development of the burden of prior authorization of psychotherapeutics (BoPAP) scale to assess the effects of prior authorization among Texas Medicaid providers. Adm Policy Ment Health. 2009;36(4):278-287.
13. Rascati KL, Brown CM. Prior authorization for antipsychotic medications—It’s not just about the money. Clin Ther. 2008;30(8):1506-1507.
14. Lu CY, Soumerai SB, Ross-Degnan D, et al. Unintended impacts of a Medicaid prior authorization policy on access to medications for bipolar disorder. Med Care. 2010;48(1):4-9.
15. Stephens RJ, White SE, Cudnik M, et al. Factors associated with longer lengths of stay for mental health emergency department patients. J Emerg Med. 2014; 47(4):412-419.
16. Brown JD, Barrett A, Caffery E, et al. Medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder. Psychiatr Serv. 2013;64(9):878-885.
17. American Medical Association. Opinion 10.01– Fundamental elements of the patient-physician relationship. http://www.ama-assn.org/ama/pub/ physician-resources/medical-ethics/code-medical-ethics/opinion1001.page?. Accessed October 11, 2014.
18. Hall RC. Ethical and legal implications of managed care. Gen Hosp Psychiatry. 1997;19(3):200-208.
19. Porter v Thadani, 2010 U.S. Dist. LEXIS 35145 (NH 2010).
20. NB ex rel Peacock v District of Columbia, 682 F3d 77 (DC Cir 2012).
21. Wilson v Blue Cross of Southern California, 222 Cal App 3d 660, 271 Cal Rptr 876 (1990).
22. Wickline v State of California, 192 Cal App 3d 1630, 239 Cal Rptr 810 (1986).
23. Terry K. Prior authorization made easier. Med Econ. 2007;84(20):34,38,40.
24. American Medical Association. Ethics Opinion 6.07– Insurance forms completion charges. http://www. ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion607.page? Updated June 1994. Accessed October 11, 2014.
25. Gibson v Medco Health Solutions, 06-CVF-106 (OH 2008).
26. Bendix J. Curing the prior authorization headache. Med Econ. 2013;90(19):24,26-27,29-31.
27. American Medical Association. Electronic prior authorization toolkit. Available at http://www.ama-assn.org/ama/pub/advocacy/topics/administrative-simplification-initiatives/electronic-transactions-toolkit/ prior-authorization.page. Accessed October 11, 2014.
1. Brown CM, Richards K, Rascati KL, et al. Effects of a psychotherapeutic drug prior authorization (PA) requirement on patients and providers: a providers’ perspective. Adm Policy Ment Health. 2008;35(3):181-188.
2. Law MR, Ross-Degnan D, Soumerai SB. Effect of prior authorization of second-generation antipsychotic agents on pharmacy utilization and reimbursements. Psychiatr Serv. 2008;59(5):540-546.
3. Stein BD, Leckman-Westin E, Okeke E, et al. The effects of prior authorization policies on Medicaid-enrolled children’s use of antipsychotic medications: evidence from two Mid-Atlantic states. J Child Adolesc Psychopharmacol. 2014;24(7):374-381.
4. Adams KT. Prior authorization–still used, still an issue. Biotechnol Healthc. 2010;7(4):28.
5. Garcia MM, Angelini MC, Thomas T, et al. Implementation of an opioid management initiative by a state Medicaid program. J Manag Care Pharm. 2014;20(5):447-454.
6. Clark RE, Baxter JD, Barton BA, et al. The impact of prior authorization on buprenorphine dose, relapse rates, and cost for Massachusetts Medicaid beneficiaries with opioid dependence [published online July 9, 2014]. Health Serv Res. doi: 10.1111/1475-6773.12201.
7. Dunn RL, Harrison D, Ripley TL. The beers criteria as an outpatient screening tool for potentially inappropriate medications. Consult Pharm. 2011;26(10):754-763.
8. Lennertz MD, Wertheimer AI. Is prior authorization for prescribed drugs cost-effective? Drug Benefit Trends. 2008;20:136-139.
9. Bendix J. The prior authorization predicament. Med Econ. 2014;91(13)29-30,32,34-35.
10. Farley JF, Cline RR, Schommer JC, et al. Retrospective assessment of Medicaid step-therapy prior authorization policy for atypical antipsychotic medications. Clin Ther. 2008;30(8):1524-1539; discussion 1506-1507.
11. Abouzaid S, Jutkowitz E, Foley KA, et al. Economic impact of prior authorization policies for atypical antipsychotics in the treatment of schizophrenia. Popul Health Manag. 2010;13(5):247-254.
12. Brown CM, Nwokeji E, Rascati KL, et al. Development of the burden of prior authorization of psychotherapeutics (BoPAP) scale to assess the effects of prior authorization among Texas Medicaid providers. Adm Policy Ment Health. 2009;36(4):278-287.
13. Rascati KL, Brown CM. Prior authorization for antipsychotic medications—It’s not just about the money. Clin Ther. 2008;30(8):1506-1507.
14. Lu CY, Soumerai SB, Ross-Degnan D, et al. Unintended impacts of a Medicaid prior authorization policy on access to medications for bipolar disorder. Med Care. 2010;48(1):4-9.
15. Stephens RJ, White SE, Cudnik M, et al. Factors associated with longer lengths of stay for mental health emergency department patients. J Emerg Med. 2014; 47(4):412-419.
16. Brown JD, Barrett A, Caffery E, et al. Medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder. Psychiatr Serv. 2013;64(9):878-885.
17. American Medical Association. Opinion 10.01– Fundamental elements of the patient-physician relationship. http://www.ama-assn.org/ama/pub/ physician-resources/medical-ethics/code-medical-ethics/opinion1001.page?. Accessed October 11, 2014.
18. Hall RC. Ethical and legal implications of managed care. Gen Hosp Psychiatry. 1997;19(3):200-208.
19. Porter v Thadani, 2010 U.S. Dist. LEXIS 35145 (NH 2010).
20. NB ex rel Peacock v District of Columbia, 682 F3d 77 (DC Cir 2012).
21. Wilson v Blue Cross of Southern California, 222 Cal App 3d 660, 271 Cal Rptr 876 (1990).
22. Wickline v State of California, 192 Cal App 3d 1630, 239 Cal Rptr 810 (1986).
23. Terry K. Prior authorization made easier. Med Econ. 2007;84(20):34,38,40.
24. American Medical Association. Ethics Opinion 6.07– Insurance forms completion charges. http://www. ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion607.page? Updated June 1994. Accessed October 11, 2014.
25. Gibson v Medco Health Solutions, 06-CVF-106 (OH 2008).
26. Bendix J. Curing the prior authorization headache. Med Econ. 2013;90(19):24,26-27,29-31.
27. American Medical Association. Electronic prior authorization toolkit. Available at http://www.ama-assn.org/ama/pub/advocacy/topics/administrative-simplification-initiatives/electronic-transactions-toolkit/ prior-authorization.page. Accessed October 11, 2014.
What makes you responsible during a screening call?
What are your responsibilities after a screening call?
Dear Dr. Mossman,
When I take a call from a treatment-seeker at our outpatient clinic, I ask brief screening questions to determine whether our services would be appropriate. Shortly after I screened one caller, Ms. C, she called back requesting a medication refill and asking about her diagnosis.
What obligation do I have to Ms. C? Is she my patient? Would I be liable if I didn’t help her out and something bad happened to her?
Submitted by “Dr. S”
Office and hospital Web sites, LinkedIn profiles, and Facebook pages are just a few of the ways that people find physicians and learn about their services. But most 21st century doctor-patient relationships still start with 19th century technology: a telephone call.
Talking with prospective patients before setting up an appointment makes sense. A short conversation can clarify whether you offer the services that a caller needs and increases the show-up rate for initial appointments.1
But if you ask for some personal history and information about symptoms in a screening interview, does that make the caller your patient? Ms. C seemed to have thought so. To find out whether Ms. C was right and to learn how Dr. S should handle initial telephone calls, we’ll look at:
• the rationale for screening callers before initiating treatment
• features of screening that can create a doctor-patient relationship
• how to fulfill duties that result from screening.
Why screen prospective patients?
Mental health treatment has become more diversified and specialized over the past 30 years. No psychiatrist nowadays has all the therapeutic skills that all potential patients might need.
Before speaking to you, a treatment-seeker often won’t know whether your practice style will fit his (her) needs. You might prefer not to provide medication management for another clinician’s psychotherapy patient or, if you’re like most psychiatrists, you might not offer psychotherapy.
In the absence of prior obligation (eg, agreeing to provide coverage for an emergency room), physicians may structure their practices and contract for their services as they see fit2—but this leaves you with some obligation to screen potential patients for appropriate mutual fit. In years past, some psychiatrists saw potential patients for an in-office evaluation to decide whether to provide treatment—a practicethat remains acceptable if the person is told, when the appointment is made, that the first meeting is “to meet each other and see if you want to establish a treatment relationship.”3
Good treatment plans take into account patients’ temperament, emotional state, cognitive capacity, culture, family circumstances, substance use, and medical history.4 Common mental conditions often can be identified in a telephone call.5,6 Although the diagnostic accuracy of such efforts is uncertain,7 such calls can help practitioners determine whether they offer the right services for callers. Good decisions about initiating care always take financial pressures and constraints into account,8 and a pre-appointment telephone call can address those issues, too.
For all these reasons, talking to a prospective patient before he comes to see you makes sense. Screening lets you decide:
• whether you’re the right clinician for his needs
• who the right clinician is if you are not
• whether he should seek emergency evaluation when the situation sounds urgent.
Do phone calls start treatment?
As Dr. S’s questions show, telephone screenings might leave some callers thinking that treatment has started, even before their first office appointment. Having a treatment relationship is a prerequisite to malpractice liability,9 and courts have concluded that, under the right circumstances, telephone assessments do create physician-patient relationships.
Creating a physician-patient relationship
How or when might telephone screening make someone your patient? This question doesn’t have a precise answer, but how courts decided similar questions has depended on the questions the physician asked and whether the physician offered what sounded like medical advice.10,11 A physician-patient relationship forms when the physician takes some implied or affirmative action to treat, see, examine, care for, or offer a diagnosis to the patient,9,12,13 such as:
• knowingly accepting someone as a patient14
• explicitly agreeing to treat a person
• “acting in some other way such that the patient might reasonably be led to assume a doctor-patient relationship has been established.”15
Also, the “fact that a physician does not deal directly with a patient does not necessarily preclude the existence of a physician-patient relationship,”12 so a telephone conversation can create such a relationship if it contains the right elements. Table 116 highlights actions that, during the course of screening, might constitute initiation of a physician-patient relationship. Table 2 offers suggestions for managing initial telephone contacts to reduce the chance of inadvertently creating a physician-patient relationship.
In the eyes of the law, whether a physician-patient relationship was formed depends on specific facts of the situation and may be decided by a jury.13,14 In the case of Ms. C, Dr. S might avoid premature creation of a physician-patient relationship by refraining from offering a diagnosis at the conclusion of the screening call.17
Prescribing
Although features of the original screening interview indicated that Ms. C was not yet Dr. S’s patient, prescribing certainly would commence a physician-patient relationship.18 But even if the screening had made Ms. C a patient, refilling her prescription now probably is a bad idea.
Assuming that a physician-patient relationship exists, it is unlikely that a short telephone interview gave Dr. S enough information about Ms. C’s medical history and present mental status to ensure that his diagnostic reasoning would not be faulty. It also is unlikely that telephone screening allowed Dr. S to meet the standard of care for prescribing—a process that involves choosing medications suitable to the patient’s clinical needs, checking the results of any necessary lab tests, and obtaining appropriate informed consent.19
Satisfying duties
Outpatient facilities can instruct telephone screeners to conduct interviews in ways that reduce inadvertent establishment of a treatment relationship, but establishing such a relationship cannot be avoided in all cases. If a caller is distraught or in crisis, for example, compassion dictates helping him, and some callers (eg, Ms. C) may feel they have a firmer treatment relationship than actually exists.
Once you have created a physician-patient relationship, you must continue that relationship until you end it appropriately.3 That does not mean you have to provide definitive treatment; you simply need to exercise “reasonable care according to the standards of the profession.”16,20 If a caller telephones in an emergency situation, for example, the screening clinician should take appropriate steps to ensure safety, which might include calling law enforcement or facilitating hospitalization.3
One way to fulfill the duties of a physician-patient relationship inadvertently established during initial screening is through explicit discharge (if medically appropriate) or transfer of care to another physician.15 A prudent clinic or practitioner will describe other mental health resources in the community and sometimes assist with referral if the inquiring potential patient needs services that the provider does not offer.
In many communities, finding appropriate mental health resources is difficult. Creative approaches to this problem include transitional psychiatry or crisis support clinics that serve as a “bridge” to longer-term services,21,22 preliminary process groups,23 and telepsychiatry transitional clinics.24 When a clinic does not accept a person as a patient, the clinic should clearly document 1) key features of the contact and 2) the rationale for that decision
Bottom Line
You have a right and a responsibility to screen prospective patients for good fit to your treatment services. In doing so, however, you might inadvertently create a physician-patient relationship. If this happens, you should fulfill your clinical responsibilities, as you would for any patient, by helping the patient get appropriate care from you or another provider.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Shoffner J, Staudt M, Marcus S, et al. Using telephone reminders to increase attendance at psychiatric appointments: findings of a pilot study in rural Appalachia. Psychiatr Serv. 2007;58(6):872-875.
2. Hiser v Randolph, 1980 617 P2d 774 (Ariz App).
3. American Psychiatric Association. Practice management for early career psychiatrists: a reference guide, 6th edition. http://www.psych.org/practice/managing-a-practice/ starting-a-practice. Published October 16, 2006. Accessed July 8, 2014.
4. Delgado SV, Strawn JR. Difficult psychiatric consultations: an integrated approach. New York, NY: Springer; 2014.
5. Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatric Pract. 2004;10(5): 307-313.
6. Michel C, Schimmelmann BG, Kupferschmid S, et al. Reliability of telephone assessments of at-risk criteria of psychosis: a comparison to face-to-face interviews. Schizophr Res. 2014;153(1-3):251-253.
7. Muskens EM, Lucassen P, Groenleer W, et al. Psychiatric diagnosis by telephone: is it an opportunity [published online March 15, 2014]? Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-014-0861-9.
8. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802.
9. Roberts v Sankey, 2004 813 NE2d 1195 (Ind App).
10. O’Neill v Montefiore Hospital, 1960 202 NYS 2d 436 (NY App).
11. McKinney v Schlatter, 1997 692 NE2d 1045 (Ohio App).
12. Dehn v Edgecombe, 865 A2d 603 (Md 2005).
13. Kelley v Middle Tennessee Emergency Physicians, 133 SW3d 587 (Tenn 2004).
14. Oliver v Brock, 342 So2d 1 (Ala 1976).
15. Appelbaum PS, Gutheil TG. Malpractice and other forms of liability. In: Appelbaum PS, Gutheil TG, eds. Clinical Handbook of Psychiatry and the Law, 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2007:115-116.
16. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
17. Torres A, Wagner R. Establishing the physician-patient relationship. J Dermatol Surg Oncol. 1993;19(2):147-149.
18. Aboff BM, Collier VU, Farber NJ, et al. Residents’ prescription writing for nonpatients. JAMA. 2002;288(3):381-385.
19. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
20. Brown v Koulizakis, 331 SE2d 440 (Va 1985).
21. University of Michigan Department of Psychiatry. Crisis support clinic. http://www.psych.med.umich.edu/patient-care/crisis-support-clinic. Accessed July 9, 2014.
22. UAB Department of Psychiatry. http://www.uab.edu/ medicine/psychiatry. Accessed July 9, 2014.
23. Stone WN, Klein EB. The waiting-list group. Int J Group Psychother. 1999;49(4):417-428.
24. Detweiler MB, Arif S, Candelario J, et al. A telepsychiatry transition clinic: the first 12 months experience. J Telemed Telecare. 2011;17(6):293-297.
Dear Dr. Mossman,
When I take a call from a treatment-seeker at our outpatient clinic, I ask brief screening questions to determine whether our services would be appropriate. Shortly after I screened one caller, Ms. C, she called back requesting a medication refill and asking about her diagnosis.
What obligation do I have to Ms. C? Is she my patient? Would I be liable if I didn’t help her out and something bad happened to her?
Submitted by “Dr. S”
Office and hospital Web sites, LinkedIn profiles, and Facebook pages are just a few of the ways that people find physicians and learn about their services. But most 21st century doctor-patient relationships still start with 19th century technology: a telephone call.
Talking with prospective patients before setting up an appointment makes sense. A short conversation can clarify whether you offer the services that a caller needs and increases the show-up rate for initial appointments.1
But if you ask for some personal history and information about symptoms in a screening interview, does that make the caller your patient? Ms. C seemed to have thought so. To find out whether Ms. C was right and to learn how Dr. S should handle initial telephone calls, we’ll look at:
• the rationale for screening callers before initiating treatment
• features of screening that can create a doctor-patient relationship
• how to fulfill duties that result from screening.
Why screen prospective patients?
Mental health treatment has become more diversified and specialized over the past 30 years. No psychiatrist nowadays has all the therapeutic skills that all potential patients might need.
Before speaking to you, a treatment-seeker often won’t know whether your practice style will fit his (her) needs. You might prefer not to provide medication management for another clinician’s psychotherapy patient or, if you’re like most psychiatrists, you might not offer psychotherapy.
In the absence of prior obligation (eg, agreeing to provide coverage for an emergency room), physicians may structure their practices and contract for their services as they see fit2—but this leaves you with some obligation to screen potential patients for appropriate mutual fit. In years past, some psychiatrists saw potential patients for an in-office evaluation to decide whether to provide treatment—a practicethat remains acceptable if the person is told, when the appointment is made, that the first meeting is “to meet each other and see if you want to establish a treatment relationship.”3
Good treatment plans take into account patients’ temperament, emotional state, cognitive capacity, culture, family circumstances, substance use, and medical history.4 Common mental conditions often can be identified in a telephone call.5,6 Although the diagnostic accuracy of such efforts is uncertain,7 such calls can help practitioners determine whether they offer the right services for callers. Good decisions about initiating care always take financial pressures and constraints into account,8 and a pre-appointment telephone call can address those issues, too.
For all these reasons, talking to a prospective patient before he comes to see you makes sense. Screening lets you decide:
• whether you’re the right clinician for his needs
• who the right clinician is if you are not
• whether he should seek emergency evaluation when the situation sounds urgent.
Do phone calls start treatment?
As Dr. S’s questions show, telephone screenings might leave some callers thinking that treatment has started, even before their first office appointment. Having a treatment relationship is a prerequisite to malpractice liability,9 and courts have concluded that, under the right circumstances, telephone assessments do create physician-patient relationships.
Creating a physician-patient relationship
How or when might telephone screening make someone your patient? This question doesn’t have a precise answer, but how courts decided similar questions has depended on the questions the physician asked and whether the physician offered what sounded like medical advice.10,11 A physician-patient relationship forms when the physician takes some implied or affirmative action to treat, see, examine, care for, or offer a diagnosis to the patient,9,12,13 such as:
• knowingly accepting someone as a patient14
• explicitly agreeing to treat a person
• “acting in some other way such that the patient might reasonably be led to assume a doctor-patient relationship has been established.”15
Also, the “fact that a physician does not deal directly with a patient does not necessarily preclude the existence of a physician-patient relationship,”12 so a telephone conversation can create such a relationship if it contains the right elements. Table 116 highlights actions that, during the course of screening, might constitute initiation of a physician-patient relationship. Table 2 offers suggestions for managing initial telephone contacts to reduce the chance of inadvertently creating a physician-patient relationship.
In the eyes of the law, whether a physician-patient relationship was formed depends on specific facts of the situation and may be decided by a jury.13,14 In the case of Ms. C, Dr. S might avoid premature creation of a physician-patient relationship by refraining from offering a diagnosis at the conclusion of the screening call.17
Prescribing
Although features of the original screening interview indicated that Ms. C was not yet Dr. S’s patient, prescribing certainly would commence a physician-patient relationship.18 But even if the screening had made Ms. C a patient, refilling her prescription now probably is a bad idea.
Assuming that a physician-patient relationship exists, it is unlikely that a short telephone interview gave Dr. S enough information about Ms. C’s medical history and present mental status to ensure that his diagnostic reasoning would not be faulty. It also is unlikely that telephone screening allowed Dr. S to meet the standard of care for prescribing—a process that involves choosing medications suitable to the patient’s clinical needs, checking the results of any necessary lab tests, and obtaining appropriate informed consent.19
Satisfying duties
Outpatient facilities can instruct telephone screeners to conduct interviews in ways that reduce inadvertent establishment of a treatment relationship, but establishing such a relationship cannot be avoided in all cases. If a caller is distraught or in crisis, for example, compassion dictates helping him, and some callers (eg, Ms. C) may feel they have a firmer treatment relationship than actually exists.
Once you have created a physician-patient relationship, you must continue that relationship until you end it appropriately.3 That does not mean you have to provide definitive treatment; you simply need to exercise “reasonable care according to the standards of the profession.”16,20 If a caller telephones in an emergency situation, for example, the screening clinician should take appropriate steps to ensure safety, which might include calling law enforcement or facilitating hospitalization.3
One way to fulfill the duties of a physician-patient relationship inadvertently established during initial screening is through explicit discharge (if medically appropriate) or transfer of care to another physician.15 A prudent clinic or practitioner will describe other mental health resources in the community and sometimes assist with referral if the inquiring potential patient needs services that the provider does not offer.
In many communities, finding appropriate mental health resources is difficult. Creative approaches to this problem include transitional psychiatry or crisis support clinics that serve as a “bridge” to longer-term services,21,22 preliminary process groups,23 and telepsychiatry transitional clinics.24 When a clinic does not accept a person as a patient, the clinic should clearly document 1) key features of the contact and 2) the rationale for that decision
Bottom Line
You have a right and a responsibility to screen prospective patients for good fit to your treatment services. In doing so, however, you might inadvertently create a physician-patient relationship. If this happens, you should fulfill your clinical responsibilities, as you would for any patient, by helping the patient get appropriate care from you or another provider.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
When I take a call from a treatment-seeker at our outpatient clinic, I ask brief screening questions to determine whether our services would be appropriate. Shortly after I screened one caller, Ms. C, she called back requesting a medication refill and asking about her diagnosis.
What obligation do I have to Ms. C? Is she my patient? Would I be liable if I didn’t help her out and something bad happened to her?
Submitted by “Dr. S”
Office and hospital Web sites, LinkedIn profiles, and Facebook pages are just a few of the ways that people find physicians and learn about their services. But most 21st century doctor-patient relationships still start with 19th century technology: a telephone call.
Talking with prospective patients before setting up an appointment makes sense. A short conversation can clarify whether you offer the services that a caller needs and increases the show-up rate for initial appointments.1
But if you ask for some personal history and information about symptoms in a screening interview, does that make the caller your patient? Ms. C seemed to have thought so. To find out whether Ms. C was right and to learn how Dr. S should handle initial telephone calls, we’ll look at:
• the rationale for screening callers before initiating treatment
• features of screening that can create a doctor-patient relationship
• how to fulfill duties that result from screening.
Why screen prospective patients?
Mental health treatment has become more diversified and specialized over the past 30 years. No psychiatrist nowadays has all the therapeutic skills that all potential patients might need.
Before speaking to you, a treatment-seeker often won’t know whether your practice style will fit his (her) needs. You might prefer not to provide medication management for another clinician’s psychotherapy patient or, if you’re like most psychiatrists, you might not offer psychotherapy.
In the absence of prior obligation (eg, agreeing to provide coverage for an emergency room), physicians may structure their practices and contract for their services as they see fit2—but this leaves you with some obligation to screen potential patients for appropriate mutual fit. In years past, some psychiatrists saw potential patients for an in-office evaluation to decide whether to provide treatment—a practicethat remains acceptable if the person is told, when the appointment is made, that the first meeting is “to meet each other and see if you want to establish a treatment relationship.”3
Good treatment plans take into account patients’ temperament, emotional state, cognitive capacity, culture, family circumstances, substance use, and medical history.4 Common mental conditions often can be identified in a telephone call.5,6 Although the diagnostic accuracy of such efforts is uncertain,7 such calls can help practitioners determine whether they offer the right services for callers. Good decisions about initiating care always take financial pressures and constraints into account,8 and a pre-appointment telephone call can address those issues, too.
For all these reasons, talking to a prospective patient before he comes to see you makes sense. Screening lets you decide:
• whether you’re the right clinician for his needs
• who the right clinician is if you are not
• whether he should seek emergency evaluation when the situation sounds urgent.
Do phone calls start treatment?
As Dr. S’s questions show, telephone screenings might leave some callers thinking that treatment has started, even before their first office appointment. Having a treatment relationship is a prerequisite to malpractice liability,9 and courts have concluded that, under the right circumstances, telephone assessments do create physician-patient relationships.
Creating a physician-patient relationship
How or when might telephone screening make someone your patient? This question doesn’t have a precise answer, but how courts decided similar questions has depended on the questions the physician asked and whether the physician offered what sounded like medical advice.10,11 A physician-patient relationship forms when the physician takes some implied or affirmative action to treat, see, examine, care for, or offer a diagnosis to the patient,9,12,13 such as:
• knowingly accepting someone as a patient14
• explicitly agreeing to treat a person
• “acting in some other way such that the patient might reasonably be led to assume a doctor-patient relationship has been established.”15
Also, the “fact that a physician does not deal directly with a patient does not necessarily preclude the existence of a physician-patient relationship,”12 so a telephone conversation can create such a relationship if it contains the right elements. Table 116 highlights actions that, during the course of screening, might constitute initiation of a physician-patient relationship. Table 2 offers suggestions for managing initial telephone contacts to reduce the chance of inadvertently creating a physician-patient relationship.
In the eyes of the law, whether a physician-patient relationship was formed depends on specific facts of the situation and may be decided by a jury.13,14 In the case of Ms. C, Dr. S might avoid premature creation of a physician-patient relationship by refraining from offering a diagnosis at the conclusion of the screening call.17
Prescribing
Although features of the original screening interview indicated that Ms. C was not yet Dr. S’s patient, prescribing certainly would commence a physician-patient relationship.18 But even if the screening had made Ms. C a patient, refilling her prescription now probably is a bad idea.
Assuming that a physician-patient relationship exists, it is unlikely that a short telephone interview gave Dr. S enough information about Ms. C’s medical history and present mental status to ensure that his diagnostic reasoning would not be faulty. It also is unlikely that telephone screening allowed Dr. S to meet the standard of care for prescribing—a process that involves choosing medications suitable to the patient’s clinical needs, checking the results of any necessary lab tests, and obtaining appropriate informed consent.19
Satisfying duties
Outpatient facilities can instruct telephone screeners to conduct interviews in ways that reduce inadvertent establishment of a treatment relationship, but establishing such a relationship cannot be avoided in all cases. If a caller is distraught or in crisis, for example, compassion dictates helping him, and some callers (eg, Ms. C) may feel they have a firmer treatment relationship than actually exists.
Once you have created a physician-patient relationship, you must continue that relationship until you end it appropriately.3 That does not mean you have to provide definitive treatment; you simply need to exercise “reasonable care according to the standards of the profession.”16,20 If a caller telephones in an emergency situation, for example, the screening clinician should take appropriate steps to ensure safety, which might include calling law enforcement or facilitating hospitalization.3
One way to fulfill the duties of a physician-patient relationship inadvertently established during initial screening is through explicit discharge (if medically appropriate) or transfer of care to another physician.15 A prudent clinic or practitioner will describe other mental health resources in the community and sometimes assist with referral if the inquiring potential patient needs services that the provider does not offer.
In many communities, finding appropriate mental health resources is difficult. Creative approaches to this problem include transitional psychiatry or crisis support clinics that serve as a “bridge” to longer-term services,21,22 preliminary process groups,23 and telepsychiatry transitional clinics.24 When a clinic does not accept a person as a patient, the clinic should clearly document 1) key features of the contact and 2) the rationale for that decision
Bottom Line
You have a right and a responsibility to screen prospective patients for good fit to your treatment services. In doing so, however, you might inadvertently create a physician-patient relationship. If this happens, you should fulfill your clinical responsibilities, as you would for any patient, by helping the patient get appropriate care from you or another provider.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Shoffner J, Staudt M, Marcus S, et al. Using telephone reminders to increase attendance at psychiatric appointments: findings of a pilot study in rural Appalachia. Psychiatr Serv. 2007;58(6):872-875.
2. Hiser v Randolph, 1980 617 P2d 774 (Ariz App).
3. American Psychiatric Association. Practice management for early career psychiatrists: a reference guide, 6th edition. http://www.psych.org/practice/managing-a-practice/ starting-a-practice. Published October 16, 2006. Accessed July 8, 2014.
4. Delgado SV, Strawn JR. Difficult psychiatric consultations: an integrated approach. New York, NY: Springer; 2014.
5. Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatric Pract. 2004;10(5): 307-313.
6. Michel C, Schimmelmann BG, Kupferschmid S, et al. Reliability of telephone assessments of at-risk criteria of psychosis: a comparison to face-to-face interviews. Schizophr Res. 2014;153(1-3):251-253.
7. Muskens EM, Lucassen P, Groenleer W, et al. Psychiatric diagnosis by telephone: is it an opportunity [published online March 15, 2014]? Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-014-0861-9.
8. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802.
9. Roberts v Sankey, 2004 813 NE2d 1195 (Ind App).
10. O’Neill v Montefiore Hospital, 1960 202 NYS 2d 436 (NY App).
11. McKinney v Schlatter, 1997 692 NE2d 1045 (Ohio App).
12. Dehn v Edgecombe, 865 A2d 603 (Md 2005).
13. Kelley v Middle Tennessee Emergency Physicians, 133 SW3d 587 (Tenn 2004).
14. Oliver v Brock, 342 So2d 1 (Ala 1976).
15. Appelbaum PS, Gutheil TG. Malpractice and other forms of liability. In: Appelbaum PS, Gutheil TG, eds. Clinical Handbook of Psychiatry and the Law, 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2007:115-116.
16. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
17. Torres A, Wagner R. Establishing the physician-patient relationship. J Dermatol Surg Oncol. 1993;19(2):147-149.
18. Aboff BM, Collier VU, Farber NJ, et al. Residents’ prescription writing for nonpatients. JAMA. 2002;288(3):381-385.
19. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
20. Brown v Koulizakis, 331 SE2d 440 (Va 1985).
21. University of Michigan Department of Psychiatry. Crisis support clinic. http://www.psych.med.umich.edu/patient-care/crisis-support-clinic. Accessed July 9, 2014.
22. UAB Department of Psychiatry. http://www.uab.edu/ medicine/psychiatry. Accessed July 9, 2014.
23. Stone WN, Klein EB. The waiting-list group. Int J Group Psychother. 1999;49(4):417-428.
24. Detweiler MB, Arif S, Candelario J, et al. A telepsychiatry transition clinic: the first 12 months experience. J Telemed Telecare. 2011;17(6):293-297.
1. Shoffner J, Staudt M, Marcus S, et al. Using telephone reminders to increase attendance at psychiatric appointments: findings of a pilot study in rural Appalachia. Psychiatr Serv. 2007;58(6):872-875.
2. Hiser v Randolph, 1980 617 P2d 774 (Ariz App).
3. American Psychiatric Association. Practice management for early career psychiatrists: a reference guide, 6th edition. http://www.psych.org/practice/managing-a-practice/ starting-a-practice. Published October 16, 2006. Accessed July 8, 2014.
4. Delgado SV, Strawn JR. Difficult psychiatric consultations: an integrated approach. New York, NY: Springer; 2014.
5. Aziz MA, Kenford S. Comparability of telephone and face-to-face interviews in assessing patients with posttraumatic stress disorder. J Psychiatric Pract. 2004;10(5): 307-313.
6. Michel C, Schimmelmann BG, Kupferschmid S, et al. Reliability of telephone assessments of at-risk criteria of psychosis: a comparison to face-to-face interviews. Schizophr Res. 2014;153(1-3):251-253.
7. Muskens EM, Lucassen P, Groenleer W, et al. Psychiatric diagnosis by telephone: is it an opportunity [published online March 15, 2014]? Soc Psychiatry Psychiatr Epidemiol. doi: 10.1007/s00127-014-0861-9.
8. Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307(17):1801-1802.
9. Roberts v Sankey, 2004 813 NE2d 1195 (Ind App).
10. O’Neill v Montefiore Hospital, 1960 202 NYS 2d 436 (NY App).
11. McKinney v Schlatter, 1997 692 NE2d 1045 (Ohio App).
12. Dehn v Edgecombe, 865 A2d 603 (Md 2005).
13. Kelley v Middle Tennessee Emergency Physicians, 133 SW3d 587 (Tenn 2004).
14. Oliver v Brock, 342 So2d 1 (Ala 1976).
15. Appelbaum PS, Gutheil TG. Malpractice and other forms of liability. In: Appelbaum PS, Gutheil TG, eds. Clinical Handbook of Psychiatry and the Law, 4th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2007:115-116.
16. Simon RI, Shuman DW. The doctor-patient relationship. Focus. 2007;5(4):423-431.
17. Torres A, Wagner R. Establishing the physician-patient relationship. J Dermatol Surg Oncol. 1993;19(2):147-149.
18. Aboff BM, Collier VU, Farber NJ, et al. Residents’ prescription writing for nonpatients. JAMA. 2002;288(3):381-385.
19. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115-119.
20. Brown v Koulizakis, 331 SE2d 440 (Va 1985).
21. University of Michigan Department of Psychiatry. Crisis support clinic. http://www.psych.med.umich.edu/patient-care/crisis-support-clinic. Accessed July 9, 2014.
22. UAB Department of Psychiatry. http://www.uab.edu/ medicine/psychiatry. Accessed July 9, 2014.
23. Stone WN, Klein EB. The waiting-list group. Int J Group Psychother. 1999;49(4):417-428.
24. Detweiler MB, Arif S, Candelario J, et al. A telepsychiatry transition clinic: the first 12 months experience. J Telemed Telecare. 2011;17(6):293-297.
Could ‘Rx: Pet therapy’ come back to bite you?
Dear Dr. Mossman,
My patient, Ms. A, asked me to write a letter to her landlord (who has a “no pets” policy) stating that she needed to keep her dog in her apartment for “therapeutic” purposes—to provide comfort and reduce her posttraumatic stress (PTSD) and anxiety. I hesitated. Could my written statement make me liable if her dog bit someone?
Submitted by “Dr. B”
Studies showing that animals can help outpatients manage psychiatric conditions have received a lot of publicity lately. As a result, more patients are asking physicians to provide documentation to support having pets in their apartments or letting their pets accompany them on planes and buses and at restaurants and shopping malls.
But sometimes, animals hurt people. The Centers for Disease Control and Prevention reports that dogs bite 4.5 million Americans each year and that one-fifth of dog bites cause injury that requires medical attention; in 2012, more than 27,000 dog-bite victims needed reconstructive surgery.1 If Dr. B writes a letter to support letting Ms. A keep a dog in her apartment, how likely is Dr. B to incur professional liability?
To answer this question, let’s examine:
• the history and background of “pet therapy”
• types of assistance animals
• potential liability for owners, landlords, and clinicians.
History and background
Using animals to improve hospitalized patients’ mental well-being dates back to the 18th century.2 In the late 1980s, medical publications began to document systematically how service dogs whose primary role was to help physically disabled individuals to navigate independently also provided social and emotional benefits.3-7 Since the 1990s, accessibility mandates in Title III of the Americans with Disabilities Act (ADA) (Table 18) have led to the gradual acceptance of service animals in public places where their presence was previously frowned upon or prohibited.9,10
If service dogs help people with physical problems feel better, it only makes sense that dogs and other animals might lessen emotional ailments, too.11-13 Florence Nightingale and Sigmund Freud both recognized that involving pets in treatment reduced patients’ depression and anxiety,14 but credit for formally introducing animals into therapy usually goes to psychologist Boris Levinson, whose 1969 book described how his dog Jingles helped troubled children communicate.15 Over the past decade, using animals— trained and untrained—for psychological assistance has become an increasingly popular therapeutic maneuver for diverse mental disorders, including autism, anxiety, schizophrenia, and PTSD.16-19
Terminology
Because animals can provide many types of assistance and support, a variety of terms are used to refer to them: service animals, companion animals, therapy pets, and so on. In certain situations (including the one described by Dr. B), carefully delineating animals’ roles and functions can reduce confusion and misinterpretation by patients, health care professionals, policy makers, and regulators.
Parenti et al20 have proposed a “taxonomy” for assistance dogs based on variables that include:
• performing task related to a disability
• the skill level required of the dog
• who uses the dog
• applicable training standards
• legal protections for the dog and its handler.
Table 220 summarizes this classification system and key variables that differentiate types of assistance dogs.
Certification
Health care facilities often require that visiting dogs have some form of “certification” that they are well behaved, and the ADA and many state statutes require that service dogs and some other animals be “certified” to perform their roles. Yet no federal or state statutes lay out explicit training standards or requirements for certification. Therapy Dogs International21 and Pet Partners22 are 2 organizations that provide certifications accepted by many agencies and organizations.
Assistance Dogs International, an assistance animal advocacy group, has proposed “minimum standards” for training and deployment of service dogs. These include responding to basic obedience commands from the client in public and at home, being able to perform at least 3 tasks to mitigate the client’s disability, teaching the client about dog training and health care, and scheduled follow-ups for skill maintenance. Dogs also should be spayed or neutered, properly vaccinated, nonaggressive, clean, and continent in public places.23
Liability laws
Most U.S. jurisdictions make owners liable for animal-caused injuries, including injuries caused by service dogs.24 In many states (eg, Minnesota25), an owner can be liable for dog-bite injury even if the owner did nothing wrong and had no reason to suspect from prior behavior that the dog might bite someone. Other jurisdictions require evidence of owner negligence, or they allow liability only when bites occur off the owner’s premises26 or if the owner let the dog run loose.27 Many homeowners’ insurance policies include liability coverage for dog bites, and a few companies offer a special canine liability policy.
Landlords often try to bar tenants from having a dog, partly to avoid liability for dog bites. Most states have case law stating that, if a tenant’s apparently friendly dog bites someone, the landlord is not liable for the injury28,29; landlords can be liable only if they know about a dangerous dog and do nothing about it.30 In a recent decision, however, the Kentucky Supreme Court made landlords statutory owners with potential liability for dog bites if they give tenants permission to have dogs “on or about” the rental premises.31
Clinicians and liability
Asking tenants to provide documentation about their need for therapeutic pets has become standard operating procedure for landlords in many states, so Ms. A’s request to Dr. B sounds reasonable. But could Dr. B’s written statement lead to liability if Ms. A’s dog bit and injured someone else?
The best answer is, “It’s conceivable, but really unlikely.” Donna Vanderpool, MBA, JD, an author and attorney who develops and implements risk management services for psychiatrists, has not seen any claims or case reports on litigation blaming mental health clinicians for injury caused by emotional support pets after the clinicians had written a letter for housing purposes (oral and written communications, April 7-13, 2014).
Dr. B might wonder whether writing a letter for Ms. A would imply that he had evaluated the dog and Ms. A’s ability to control it. Psychiatrists don’t usually discuss—let alone evaluate—the temperament or behavior of their patients’ pets; even if they did they aren’t experts on pet training. Recognizing this, Dr. B’s letter could include a statement to the effect that he was not vouching for the dog’s behavior, but only for how the dog would help Ms. A.
Dr. B also might talk with Ms. A about her need for the dog and whether she had obtained appropriate certification, as discussed above. The ADA provisions pertaining to use and presence of service animals do not apply to dogs that are merely patients’ pets, notwithstanding the genuine emotional benefits that a dog’s companionship might provide. Stating that a patient needs an animal to treat an illness might be fraud if the doctor knew the pet was just a buddy.
Bottom Line
Psychiatrists can expect that more and more patients will ask them for letters to support having pets accompany them at home or in public. Although liability seems unlikely, cautious psychiatrists can state in such letters that they have not evaluated the animal in question, only the potential benefits that the patient might derive from it.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing articles.
1. Dog Bites. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/homeandrecreationalsafety/ dog-bites/index.html. Updated October 25, 2013. Accessed April 22, 2014.
2. Serpell JA. Animal-assisted interventions in historical perspective. In Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010:17-32.
3. Eddy J, Hart LA, Boltz RP. The effects of service dogs on social acknowledgments of people in wheelchairs. J Psychol. 1988;122(1):39-45.
4. Mader B, Hart LA, Bergin B. Social acknowledgments for children with disabilities: effects of service dogs. Child Dev. 1989;60(6):1529-1534.
5. Allen K, Blascovich J. The value of service dogs for people with severe ambulatory disabilities. A randomized controlled trial. JAMA. 1996;275(13):1001-1006.
6. Camp MM. The use of service dogs as an adaptive strategy: a qualitative study. Am J Occup Ther. 2001;55(5):509-517.
7. Allen K, Shykoff BE, Izzo JL Jr. Pet ownership, but not ace inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38(4):815-820.
8. ADA requirements: service animals. United States Department of Justice Civil Rights Division, Disability Rights Section Web site. http://www.ada.gov/service_ animals_2010.htm. Published September 15, 2010. Accessed April 22, 2014.
9. Eames E, Eames T. Interpreting legal mandates. Assistance dogs in medical facilities. Nurs Manage. 1997;28(6):49-51.
10. Houghtalen RP, Doody J. After the ADA: service dogs on inpatient psychiatric units. Bull Am Acad Psychiatry Law. 1995;23(2):211-217.
11. Wenthold N, Savage TA. Ethical issues with service animals. Top Stroke Rehabil. 2007;14(2):68-74.
12. DiSalvo H, Haiduven D, Johnson N, et al. Who let the dogs out? Infection control did: utility of dogs in health care settings and infection control aspects. Am J Infect Control. 2006;34:301-307.
13. Collins DM, Fitzgerald SG, Sachs-Ericsson N, et al. Psychosocial well-being and community participation of service dog partners. Disabil Rehabil Assist Technol. 2006;1(1-2):41-48.
14. Coren S. Foreward. In: Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010: xv-xviii.
15. Levinson BM, Mallon GP. Pet-oriented child psychotherapy. 2nd ed. Springfield IL: Charles C Thomas Publisher, Ltd; 1997.
16. Esnayra J. Help from man’s best friend. Psychiatric service dogs are helping consumers deal with the symptoms of mental illness. Behav Healthc. 2007;27(7):30-32.
17. Barak Y, Savorai O, Mavashev S, et al. Animal-assisted therapy for elderly schizophrenic patients: a one year controlled trial. Am J Geriatr Psychiatry. 2001;9(4):439-442.
18. Burrows KE, Adams CL, Millman ST. Factors affecting behavior and welfare of service dogs for children with autism spectrum disorder. J Appl Anim Welf Sci. 2008;11(1):42-62.
19. Yount RA, Olmert MD, Lee MR. Service dog training program for treatment of posttraumatic stress in service members. US Army Med Dep J. 2012:63-69.
20. Parenti L, Foreman A, Meade BJ, et al. A revised taxonomy of assistance animals. J Rehabil Res Dev. 2013;50(6):745-756.
21. Testing Requirements. Therapy Dogs International. http:// www.tdi-dog.org/images/TestingBrochure.pdf. Accessed April 22, 2014.
22. How to become a registered therapy animal team. Pet Partners. http://www.petpartners.org/TAPinfo. Accessed April 22, 2014.
23. ADI Guide to Assistance Dog Laws. Assistance Dogs International. http://www.assistancedogsinternational. org/access-and-laws/adi-guide-to-assistance-dog-laws. Accessed April 22, 2014.
24. Id Stat §56-704.
25. Seim v Garavalia, 306 NW2d 806 (Minn 1981).
26. ME Rev Stat title 7, §3961.
27. Chadbourne v Kappaz, 2001 779 A2d 293 (DC App).
28. Stokes v Lyddy, 2002 75 (Conn App 252).
29. Georgianna v Gizzy, 483 NYS2d 892 (NY 1984).
30. Linebaugh v Hyndman, 516 A2d 638 (NJ 1986).
31. Benningfield v Zinsmeister, 367 SW3d 561 (Ky 2012).
Dear Dr. Mossman,
My patient, Ms. A, asked me to write a letter to her landlord (who has a “no pets” policy) stating that she needed to keep her dog in her apartment for “therapeutic” purposes—to provide comfort and reduce her posttraumatic stress (PTSD) and anxiety. I hesitated. Could my written statement make me liable if her dog bit someone?
Submitted by “Dr. B”
Studies showing that animals can help outpatients manage psychiatric conditions have received a lot of publicity lately. As a result, more patients are asking physicians to provide documentation to support having pets in their apartments or letting their pets accompany them on planes and buses and at restaurants and shopping malls.
But sometimes, animals hurt people. The Centers for Disease Control and Prevention reports that dogs bite 4.5 million Americans each year and that one-fifth of dog bites cause injury that requires medical attention; in 2012, more than 27,000 dog-bite victims needed reconstructive surgery.1 If Dr. B writes a letter to support letting Ms. A keep a dog in her apartment, how likely is Dr. B to incur professional liability?
To answer this question, let’s examine:
• the history and background of “pet therapy”
• types of assistance animals
• potential liability for owners, landlords, and clinicians.
History and background
Using animals to improve hospitalized patients’ mental well-being dates back to the 18th century.2 In the late 1980s, medical publications began to document systematically how service dogs whose primary role was to help physically disabled individuals to navigate independently also provided social and emotional benefits.3-7 Since the 1990s, accessibility mandates in Title III of the Americans with Disabilities Act (ADA) (Table 18) have led to the gradual acceptance of service animals in public places where their presence was previously frowned upon or prohibited.9,10
If service dogs help people with physical problems feel better, it only makes sense that dogs and other animals might lessen emotional ailments, too.11-13 Florence Nightingale and Sigmund Freud both recognized that involving pets in treatment reduced patients’ depression and anxiety,14 but credit for formally introducing animals into therapy usually goes to psychologist Boris Levinson, whose 1969 book described how his dog Jingles helped troubled children communicate.15 Over the past decade, using animals— trained and untrained—for psychological assistance has become an increasingly popular therapeutic maneuver for diverse mental disorders, including autism, anxiety, schizophrenia, and PTSD.16-19
Terminology
Because animals can provide many types of assistance and support, a variety of terms are used to refer to them: service animals, companion animals, therapy pets, and so on. In certain situations (including the one described by Dr. B), carefully delineating animals’ roles and functions can reduce confusion and misinterpretation by patients, health care professionals, policy makers, and regulators.
Parenti et al20 have proposed a “taxonomy” for assistance dogs based on variables that include:
• performing task related to a disability
• the skill level required of the dog
• who uses the dog
• applicable training standards
• legal protections for the dog and its handler.
Table 220 summarizes this classification system and key variables that differentiate types of assistance dogs.
Certification
Health care facilities often require that visiting dogs have some form of “certification” that they are well behaved, and the ADA and many state statutes require that service dogs and some other animals be “certified” to perform their roles. Yet no federal or state statutes lay out explicit training standards or requirements for certification. Therapy Dogs International21 and Pet Partners22 are 2 organizations that provide certifications accepted by many agencies and organizations.
Assistance Dogs International, an assistance animal advocacy group, has proposed “minimum standards” for training and deployment of service dogs. These include responding to basic obedience commands from the client in public and at home, being able to perform at least 3 tasks to mitigate the client’s disability, teaching the client about dog training and health care, and scheduled follow-ups for skill maintenance. Dogs also should be spayed or neutered, properly vaccinated, nonaggressive, clean, and continent in public places.23
Liability laws
Most U.S. jurisdictions make owners liable for animal-caused injuries, including injuries caused by service dogs.24 In many states (eg, Minnesota25), an owner can be liable for dog-bite injury even if the owner did nothing wrong and had no reason to suspect from prior behavior that the dog might bite someone. Other jurisdictions require evidence of owner negligence, or they allow liability only when bites occur off the owner’s premises26 or if the owner let the dog run loose.27 Many homeowners’ insurance policies include liability coverage for dog bites, and a few companies offer a special canine liability policy.
Landlords often try to bar tenants from having a dog, partly to avoid liability for dog bites. Most states have case law stating that, if a tenant’s apparently friendly dog bites someone, the landlord is not liable for the injury28,29; landlords can be liable only if they know about a dangerous dog and do nothing about it.30 In a recent decision, however, the Kentucky Supreme Court made landlords statutory owners with potential liability for dog bites if they give tenants permission to have dogs “on or about” the rental premises.31
Clinicians and liability
Asking tenants to provide documentation about their need for therapeutic pets has become standard operating procedure for landlords in many states, so Ms. A’s request to Dr. B sounds reasonable. But could Dr. B’s written statement lead to liability if Ms. A’s dog bit and injured someone else?
The best answer is, “It’s conceivable, but really unlikely.” Donna Vanderpool, MBA, JD, an author and attorney who develops and implements risk management services for psychiatrists, has not seen any claims or case reports on litigation blaming mental health clinicians for injury caused by emotional support pets after the clinicians had written a letter for housing purposes (oral and written communications, April 7-13, 2014).
Dr. B might wonder whether writing a letter for Ms. A would imply that he had evaluated the dog and Ms. A’s ability to control it. Psychiatrists don’t usually discuss—let alone evaluate—the temperament or behavior of their patients’ pets; even if they did they aren’t experts on pet training. Recognizing this, Dr. B’s letter could include a statement to the effect that he was not vouching for the dog’s behavior, but only for how the dog would help Ms. A.
Dr. B also might talk with Ms. A about her need for the dog and whether she had obtained appropriate certification, as discussed above. The ADA provisions pertaining to use and presence of service animals do not apply to dogs that are merely patients’ pets, notwithstanding the genuine emotional benefits that a dog’s companionship might provide. Stating that a patient needs an animal to treat an illness might be fraud if the doctor knew the pet was just a buddy.
Bottom Line
Psychiatrists can expect that more and more patients will ask them for letters to support having pets accompany them at home or in public. Although liability seems unlikely, cautious psychiatrists can state in such letters that they have not evaluated the animal in question, only the potential benefits that the patient might derive from it.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing articles.
Dear Dr. Mossman,
My patient, Ms. A, asked me to write a letter to her landlord (who has a “no pets” policy) stating that she needed to keep her dog in her apartment for “therapeutic” purposes—to provide comfort and reduce her posttraumatic stress (PTSD) and anxiety. I hesitated. Could my written statement make me liable if her dog bit someone?
Submitted by “Dr. B”
Studies showing that animals can help outpatients manage psychiatric conditions have received a lot of publicity lately. As a result, more patients are asking physicians to provide documentation to support having pets in their apartments or letting their pets accompany them on planes and buses and at restaurants and shopping malls.
But sometimes, animals hurt people. The Centers for Disease Control and Prevention reports that dogs bite 4.5 million Americans each year and that one-fifth of dog bites cause injury that requires medical attention; in 2012, more than 27,000 dog-bite victims needed reconstructive surgery.1 If Dr. B writes a letter to support letting Ms. A keep a dog in her apartment, how likely is Dr. B to incur professional liability?
To answer this question, let’s examine:
• the history and background of “pet therapy”
• types of assistance animals
• potential liability for owners, landlords, and clinicians.
History and background
Using animals to improve hospitalized patients’ mental well-being dates back to the 18th century.2 In the late 1980s, medical publications began to document systematically how service dogs whose primary role was to help physically disabled individuals to navigate independently also provided social and emotional benefits.3-7 Since the 1990s, accessibility mandates in Title III of the Americans with Disabilities Act (ADA) (Table 18) have led to the gradual acceptance of service animals in public places where their presence was previously frowned upon or prohibited.9,10
If service dogs help people with physical problems feel better, it only makes sense that dogs and other animals might lessen emotional ailments, too.11-13 Florence Nightingale and Sigmund Freud both recognized that involving pets in treatment reduced patients’ depression and anxiety,14 but credit for formally introducing animals into therapy usually goes to psychologist Boris Levinson, whose 1969 book described how his dog Jingles helped troubled children communicate.15 Over the past decade, using animals— trained and untrained—for psychological assistance has become an increasingly popular therapeutic maneuver for diverse mental disorders, including autism, anxiety, schizophrenia, and PTSD.16-19
Terminology
Because animals can provide many types of assistance and support, a variety of terms are used to refer to them: service animals, companion animals, therapy pets, and so on. In certain situations (including the one described by Dr. B), carefully delineating animals’ roles and functions can reduce confusion and misinterpretation by patients, health care professionals, policy makers, and regulators.
Parenti et al20 have proposed a “taxonomy” for assistance dogs based on variables that include:
• performing task related to a disability
• the skill level required of the dog
• who uses the dog
• applicable training standards
• legal protections for the dog and its handler.
Table 220 summarizes this classification system and key variables that differentiate types of assistance dogs.
Certification
Health care facilities often require that visiting dogs have some form of “certification” that they are well behaved, and the ADA and many state statutes require that service dogs and some other animals be “certified” to perform their roles. Yet no federal or state statutes lay out explicit training standards or requirements for certification. Therapy Dogs International21 and Pet Partners22 are 2 organizations that provide certifications accepted by many agencies and organizations.
Assistance Dogs International, an assistance animal advocacy group, has proposed “minimum standards” for training and deployment of service dogs. These include responding to basic obedience commands from the client in public and at home, being able to perform at least 3 tasks to mitigate the client’s disability, teaching the client about dog training and health care, and scheduled follow-ups for skill maintenance. Dogs also should be spayed or neutered, properly vaccinated, nonaggressive, clean, and continent in public places.23
Liability laws
Most U.S. jurisdictions make owners liable for animal-caused injuries, including injuries caused by service dogs.24 In many states (eg, Minnesota25), an owner can be liable for dog-bite injury even if the owner did nothing wrong and had no reason to suspect from prior behavior that the dog might bite someone. Other jurisdictions require evidence of owner negligence, or they allow liability only when bites occur off the owner’s premises26 or if the owner let the dog run loose.27 Many homeowners’ insurance policies include liability coverage for dog bites, and a few companies offer a special canine liability policy.
Landlords often try to bar tenants from having a dog, partly to avoid liability for dog bites. Most states have case law stating that, if a tenant’s apparently friendly dog bites someone, the landlord is not liable for the injury28,29; landlords can be liable only if they know about a dangerous dog and do nothing about it.30 In a recent decision, however, the Kentucky Supreme Court made landlords statutory owners with potential liability for dog bites if they give tenants permission to have dogs “on or about” the rental premises.31
Clinicians and liability
Asking tenants to provide documentation about their need for therapeutic pets has become standard operating procedure for landlords in many states, so Ms. A’s request to Dr. B sounds reasonable. But could Dr. B’s written statement lead to liability if Ms. A’s dog bit and injured someone else?
The best answer is, “It’s conceivable, but really unlikely.” Donna Vanderpool, MBA, JD, an author and attorney who develops and implements risk management services for psychiatrists, has not seen any claims or case reports on litigation blaming mental health clinicians for injury caused by emotional support pets after the clinicians had written a letter for housing purposes (oral and written communications, April 7-13, 2014).
Dr. B might wonder whether writing a letter for Ms. A would imply that he had evaluated the dog and Ms. A’s ability to control it. Psychiatrists don’t usually discuss—let alone evaluate—the temperament or behavior of their patients’ pets; even if they did they aren’t experts on pet training. Recognizing this, Dr. B’s letter could include a statement to the effect that he was not vouching for the dog’s behavior, but only for how the dog would help Ms. A.
Dr. B also might talk with Ms. A about her need for the dog and whether she had obtained appropriate certification, as discussed above. The ADA provisions pertaining to use and presence of service animals do not apply to dogs that are merely patients’ pets, notwithstanding the genuine emotional benefits that a dog’s companionship might provide. Stating that a patient needs an animal to treat an illness might be fraud if the doctor knew the pet was just a buddy.
Bottom Line
Psychiatrists can expect that more and more patients will ask them for letters to support having pets accompany them at home or in public. Although liability seems unlikely, cautious psychiatrists can state in such letters that they have not evaluated the animal in question, only the potential benefits that the patient might derive from it.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing articles.
1. Dog Bites. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/homeandrecreationalsafety/ dog-bites/index.html. Updated October 25, 2013. Accessed April 22, 2014.
2. Serpell JA. Animal-assisted interventions in historical perspective. In Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010:17-32.
3. Eddy J, Hart LA, Boltz RP. The effects of service dogs on social acknowledgments of people in wheelchairs. J Psychol. 1988;122(1):39-45.
4. Mader B, Hart LA, Bergin B. Social acknowledgments for children with disabilities: effects of service dogs. Child Dev. 1989;60(6):1529-1534.
5. Allen K, Blascovich J. The value of service dogs for people with severe ambulatory disabilities. A randomized controlled trial. JAMA. 1996;275(13):1001-1006.
6. Camp MM. The use of service dogs as an adaptive strategy: a qualitative study. Am J Occup Ther. 2001;55(5):509-517.
7. Allen K, Shykoff BE, Izzo JL Jr. Pet ownership, but not ace inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38(4):815-820.
8. ADA requirements: service animals. United States Department of Justice Civil Rights Division, Disability Rights Section Web site. http://www.ada.gov/service_ animals_2010.htm. Published September 15, 2010. Accessed April 22, 2014.
9. Eames E, Eames T. Interpreting legal mandates. Assistance dogs in medical facilities. Nurs Manage. 1997;28(6):49-51.
10. Houghtalen RP, Doody J. After the ADA: service dogs on inpatient psychiatric units. Bull Am Acad Psychiatry Law. 1995;23(2):211-217.
11. Wenthold N, Savage TA. Ethical issues with service animals. Top Stroke Rehabil. 2007;14(2):68-74.
12. DiSalvo H, Haiduven D, Johnson N, et al. Who let the dogs out? Infection control did: utility of dogs in health care settings and infection control aspects. Am J Infect Control. 2006;34:301-307.
13. Collins DM, Fitzgerald SG, Sachs-Ericsson N, et al. Psychosocial well-being and community participation of service dog partners. Disabil Rehabil Assist Technol. 2006;1(1-2):41-48.
14. Coren S. Foreward. In: Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010: xv-xviii.
15. Levinson BM, Mallon GP. Pet-oriented child psychotherapy. 2nd ed. Springfield IL: Charles C Thomas Publisher, Ltd; 1997.
16. Esnayra J. Help from man’s best friend. Psychiatric service dogs are helping consumers deal with the symptoms of mental illness. Behav Healthc. 2007;27(7):30-32.
17. Barak Y, Savorai O, Mavashev S, et al. Animal-assisted therapy for elderly schizophrenic patients: a one year controlled trial. Am J Geriatr Psychiatry. 2001;9(4):439-442.
18. Burrows KE, Adams CL, Millman ST. Factors affecting behavior and welfare of service dogs for children with autism spectrum disorder. J Appl Anim Welf Sci. 2008;11(1):42-62.
19. Yount RA, Olmert MD, Lee MR. Service dog training program for treatment of posttraumatic stress in service members. US Army Med Dep J. 2012:63-69.
20. Parenti L, Foreman A, Meade BJ, et al. A revised taxonomy of assistance animals. J Rehabil Res Dev. 2013;50(6):745-756.
21. Testing Requirements. Therapy Dogs International. http:// www.tdi-dog.org/images/TestingBrochure.pdf. Accessed April 22, 2014.
22. How to become a registered therapy animal team. Pet Partners. http://www.petpartners.org/TAPinfo. Accessed April 22, 2014.
23. ADI Guide to Assistance Dog Laws. Assistance Dogs International. http://www.assistancedogsinternational. org/access-and-laws/adi-guide-to-assistance-dog-laws. Accessed April 22, 2014.
24. Id Stat §56-704.
25. Seim v Garavalia, 306 NW2d 806 (Minn 1981).
26. ME Rev Stat title 7, §3961.
27. Chadbourne v Kappaz, 2001 779 A2d 293 (DC App).
28. Stokes v Lyddy, 2002 75 (Conn App 252).
29. Georgianna v Gizzy, 483 NYS2d 892 (NY 1984).
30. Linebaugh v Hyndman, 516 A2d 638 (NJ 1986).
31. Benningfield v Zinsmeister, 367 SW3d 561 (Ky 2012).
1. Dog Bites. Centers for Disease Control and Prevention Web site. http://www.cdc.gov/homeandrecreationalsafety/ dog-bites/index.html. Updated October 25, 2013. Accessed April 22, 2014.
2. Serpell JA. Animal-assisted interventions in historical perspective. In Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010:17-32.
3. Eddy J, Hart LA, Boltz RP. The effects of service dogs on social acknowledgments of people in wheelchairs. J Psychol. 1988;122(1):39-45.
4. Mader B, Hart LA, Bergin B. Social acknowledgments for children with disabilities: effects of service dogs. Child Dev. 1989;60(6):1529-1534.
5. Allen K, Blascovich J. The value of service dogs for people with severe ambulatory disabilities. A randomized controlled trial. JAMA. 1996;275(13):1001-1006.
6. Camp MM. The use of service dogs as an adaptive strategy: a qualitative study. Am J Occup Ther. 2001;55(5):509-517.
7. Allen K, Shykoff BE, Izzo JL Jr. Pet ownership, but not ace inhibitor therapy, blunts home blood pressure responses to mental stress. Hypertension. 2001;38(4):815-820.
8. ADA requirements: service animals. United States Department of Justice Civil Rights Division, Disability Rights Section Web site. http://www.ada.gov/service_ animals_2010.htm. Published September 15, 2010. Accessed April 22, 2014.
9. Eames E, Eames T. Interpreting legal mandates. Assistance dogs in medical facilities. Nurs Manage. 1997;28(6):49-51.
10. Houghtalen RP, Doody J. After the ADA: service dogs on inpatient psychiatric units. Bull Am Acad Psychiatry Law. 1995;23(2):211-217.
11. Wenthold N, Savage TA. Ethical issues with service animals. Top Stroke Rehabil. 2007;14(2):68-74.
12. DiSalvo H, Haiduven D, Johnson N, et al. Who let the dogs out? Infection control did: utility of dogs in health care settings and infection control aspects. Am J Infect Control. 2006;34:301-307.
13. Collins DM, Fitzgerald SG, Sachs-Ericsson N, et al. Psychosocial well-being and community participation of service dog partners. Disabil Rehabil Assist Technol. 2006;1(1-2):41-48.
14. Coren S. Foreward. In: Fine AH, ed. Handbook on animal-assisted therapy: theoretical foundations and guidelines for practice. 3rd ed. Burlington, MA: Academic Press; 2010: xv-xviii.
15. Levinson BM, Mallon GP. Pet-oriented child psychotherapy. 2nd ed. Springfield IL: Charles C Thomas Publisher, Ltd; 1997.
16. Esnayra J. Help from man’s best friend. Psychiatric service dogs are helping consumers deal with the symptoms of mental illness. Behav Healthc. 2007;27(7):30-32.
17. Barak Y, Savorai O, Mavashev S, et al. Animal-assisted therapy for elderly schizophrenic patients: a one year controlled trial. Am J Geriatr Psychiatry. 2001;9(4):439-442.
18. Burrows KE, Adams CL, Millman ST. Factors affecting behavior and welfare of service dogs for children with autism spectrum disorder. J Appl Anim Welf Sci. 2008;11(1):42-62.
19. Yount RA, Olmert MD, Lee MR. Service dog training program for treatment of posttraumatic stress in service members. US Army Med Dep J. 2012:63-69.
20. Parenti L, Foreman A, Meade BJ, et al. A revised taxonomy of assistance animals. J Rehabil Res Dev. 2013;50(6):745-756.
21. Testing Requirements. Therapy Dogs International. http:// www.tdi-dog.org/images/TestingBrochure.pdf. Accessed April 22, 2014.
22. How to become a registered therapy animal team. Pet Partners. http://www.petpartners.org/TAPinfo. Accessed April 22, 2014.
23. ADI Guide to Assistance Dog Laws. Assistance Dogs International. http://www.assistancedogsinternational. org/access-and-laws/adi-guide-to-assistance-dog-laws. Accessed April 22, 2014.
24. Id Stat §56-704.
25. Seim v Garavalia, 306 NW2d 806 (Minn 1981).
26. ME Rev Stat title 7, §3961.
27. Chadbourne v Kappaz, 2001 779 A2d 293 (DC App).
28. Stokes v Lyddy, 2002 75 (Conn App 252).
29. Georgianna v Gizzy, 483 NYS2d 892 (NY 1984).
30. Linebaugh v Hyndman, 516 A2d 638 (NJ 1986).
31. Benningfield v Zinsmeister, 367 SW3d 561 (Ky 2012).
Are the people we serve ‘patients’ or ‘customers’?
Dear Dr. Mossman,
At the multispecialty hospital where I work, administrators refer to patients as “customers” and tell us that, by improving “the customer experience,” we can reduce complaints and avoid malpractice suits. This business lingo offends me. Doesn’t providing good care do more to prevent malpractice claims than calling sick patients “customers”?
Submitted by “Dr. H”
“All words are pegs to hang ideas on.” As was true when Reverend Henry Ward Beecher uttered this phrase in the 19th century,1 names affect how we relate to and feel about people. Many doctors don’t think of themselves as “selling” services, and they find calling patients “customers” distasteful.
But for at least 4 decades, mental health professionals themselves have used a “customer approach” to think about certain aspects of psychiatrist–patient encounters.2 More pertinent to Dr. H’s questions, many attorneys who advise physicians are convinced that giving patients a satisfying “customer experience” is a sound strategy for reducing the risk of malpractice litigation.3
If the attorneys are right, taking a customer service perspective can lower the likelihood that psychiatrists will be sued. To understand why, this article looks at:
• terms for referring to health care recipients
• the feelings those terms generate
• how the “customer service” perspective has become a malpractice prevention
strategy.
Off-putting connotations
All the currently used ways of referring to persons served by doctors have off-putting features.
The word “patient” dates back to the 14th century and comes from Latin present
participles of pati, “to suffer.” Although Alpha Omega Alpha’s motto—“be worthy
to serve the suffering”4—expresses doctors’ commitment to help others, “patient”
carries emotional baggage. A “patient” is “a sick individual” who seeks treatment
from a physician,5 a circumstance that most people (including doctors) find unpleasant and hope is only temporary. The adjective “patient” means “bearing pains or trials calmly or without complaint” and “manifesting forbearance under provocation or strain,”5 phrases associated with passivity, deference, and a long wait to see the doctor.
Because “patient” evokes notions of helplessness and need for direction, non-medical psychotherapists often use “client” to designate care recipients. “Client” has the same Latin root as “to lean” and refers to someone “under the protection of another.” More pertinent to discussions of mental health care, a “client” also is “a person who pays a professional person or organization for services” or “a customer.”5 The latter definition explains what makes “client” feel wrong to medical practitioners, who regard those they treat as deserving more compassion and sacrifice than someone who simply purchases professional services.
“Consumer,” a word of French origin derived from the Latin consumere (“to take
up”), refers to “a person who buys goods and services.”5 If “consumers” are buyers, then those from whom they make purchases are merchants or sellers. Western marketplace concepts often regard consumers as sovereign judges of their needs, and the role of commodity producers is to try to satisfy those needs.6
The problem with viewing health care recipients this way is that sellers don’t caution customers about buying things when only principles of supply-and-demand govern exchange relationships.7 Quite the contrary: producers sometimes promote their products through “advertising [that] distorts reality and creates artificial needs to make profit for a firm.”8 If physicians behave this way, however, they get criticism and deserve it.
A “customer” in 15th-century Middle English was a tax collector, but in modern
usage, a customer is someone who, like a consumer, “purchases some commodity or service.”5 By the early 20th century, “customer” became associated with notions of empowerment embodied in the merchants’ credo, “The customer is always right.”9 Chronic illnesses often require self-management and collaboration with those labeled the “givers” and “recipients” of medical care. Research shows that “patients are more trusting of, and committed to, physicians who adopt an empowering communication style with them,” which suggests “that empowering
patients presents a means to improve the patient–physician relationship.”10
Feelings about names
People have strong feelings about what they are called. In opposing calling patients “consumers,” Nobel Prize-winning economist Paul Krugman explains: “Medical care is an area in which crucial decisions—life and death decisions—must be made; yet making those decisions intelligently requires a vast amount of specialized knowledge; and often those decisions must also be made under conditions in which the patient …needs action immediately, with no time for discussion, let alone comparison shopping. …That’s why doctors have traditionally…been expected to behave according to higher standards than the average professional…The idea that all this can be reduced to money—that doctors are just people selling services to consumers of health care—is, well, sickening.”11
Less famous recipients of nonpsychiatric medical services also prefer being called
“patients” over “clients” or “consumers.”12-14 Recipients of mental health services have a different view, however. In some surveys, “patient” gets a plurality or majority of service recipients’ votes,15,16 but in others, recipients prefer to be called “clients” or other terms.17,18 Of note, people who prefer being called “patients” tend to strongly dislike being called “clients.”19 On the professional
side, psychiatrists—along with other physicians—prefer to speak of treating “patients” and to criticize letting economic phrases infect medical discourse.20-22
Names: A practical difference?
Does what psychiatrists call those they serve make any practical difference? Perhaps not, but evidence suggests that the attitudes that doctors take toward patients affects economic success and malpractice risk.
When they have choices about where they can seek health care, medical patients value physicians’ competence, but they also consider nonclinical factors such as family members’ opinions and convenience.23 Knowing this, the federal government’s Centers for Medicare & Medicaid Services publishes results from its Hospital Consumer Assessment of Healthcare Providers and Systems to “create incentives for hospitals to improve their quality of care.”24
Nonclinical factors play a big part in patients’ decisions about suing their doctors, too. Many malpractice claims turn out to be groundless in the sense that they do not involve medical errors,25 and most errors that result in injury do not lead to malpractice suits.26
What explains this disparity? Often when a lawsuit is filed, whatever injury may have occurred is coupled with an aggravating factor, such as a communication gaffe,27 a physician’s domineering tone of voice,28 or failure to acknowledge error.29 The lower a physician’s patient satisfaction ratings, the higher the physician’s likelihood of receiving complaints and getting sued for malpractice.30,31
These kinds of considerations probably lie behind the recommendation of one hospital manager to doctors: “Continue to call them patients but treat them like
customers.”32 More insights into this view come from responses solicited from Yale
students, staff members, and alumni about whether it seems preferable to be a “patient” or a “customer” (Box).33
Bottom Line
When patients get injured during medical care, evidence suggests that how they feel about their doctors makes a big difference in whether they decide to file suit. If you’re like most psychiatrists, you prefer to call persons whom you treat “patients.” But watching and improving the things that affect your patients’ “customer experience” may help you avoid malpractice litigation.
Related Resource
• Goldhill D. To fix healthcare, turn patients into customers. Bloomberg Personal Finance. www.bloomberg.com/news/2013-01-03/to-fix-health-care-turn-patients-intocustomers.html.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Beecher HW, Drysdale W. Proverbs from Plymouth pulpit. New York, NY: D. Appleton & Co.;1887.
2. Lazare A, Eisenthal S, Wasserman L. The customer approach to patienthood: attending to patient requests in a walk-in clinic. Arch Gen Psychiatry. 1975;32:553-558.
3. Schleiter KE. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
4. Alpha Omega Alpha Honor Medical Society. Alpha Omega Alpha constitution. http://www.alphaomegaalpha.org/constitution.html. Accessed December 13, 2013. Accessed December 13, 2013.
5. Merriam-Webster. Dictionary. http://www.merriamwebster.com. Accessed December 9, 2013.
6. Kotler P, Burton S, Deans K, et al. Marketing, 9th ed. Frenchs Forest, Australia: Pearson Education Australia; 2013.
7. Deber RB. Getting what we pay for: myths and realities about financing Canada’s health care system. Health Law Can. 2000;21(2):9-56.
8. Takala T, Uusitalo O. An alternative view of relationship marketing: a framework for ethical analysis. Eur J Mark. 1996;30:45-60.
9. Van Vuren FS. The Yankee who taught Britishers that ‘the customer is always right.’ Milwaukee Journal. http://www.wisconsinhistory.org/wlhba/articleView.
asp?pg=1&id=11176. Published September 9, 1932. Accessed December 20, 2013.
10. Ouschan T, Sweeney J, Johnson L. Customer empowerment and relationship outcomes in healthcare consultations. Eur J Mark. 2006;40:1068-1086.
11. Krugman P. Patients are not consumers. The New York Times. http://krugman.blogs.nytimes.com/2011/04/20/patients-are-not-consumers. Published April 20, 2011. Accessed December 13, 2013.
12. Nair BR. Patient, client or customer? Med J Aust. 1998;169:593.
13. Wing PC. Patient or client? If in doubt, ask. CMAJ. 1997;157:287-289.
14. Deber RB, Kraetschmer N, Urowitz S, et al. Patient, consumer, client, or customer: what do people want to be called? Health Expect. 2005;8(4):345-351.
15. Sharma V, Whitney D, Kazarian SS, et al. Preferred terms for users of mental health services among service providers and recipients. Psychiatr Serv. 2000;51(2): 203-209.
16. Simmons P, Hawley CJ, Gale TM, et al. Service user, patient, client, user or survivor: describing recipients of mental health services. Psychiatrist. 2010;34:20-23.
17. Lloyd C, King R, Bassett H, et al. Patient, client or consumer? A survey of preferred terms. Australas Psychiatry. 2001; 9(4):321-324.
18. Covell NH, McCorkle BH, Weissman EM, et al. What’s in a name? Terms preferred by service recipients. Adm Policy Ment Health. 2007;34(5):443-447.
19. Ritchie CW, Hayes D, Ames DJ. Patient or client? The opinions of people attending a psychiatric clinic. Psychiatrist. 2000;24(12):447-450.
20. Andreasen NC. Clients, consumers, providers, and products: where will it all end? Am J Psychiatry. 1995;152:1107-1109.
21. Editorial. What’s in a name? Lancet. 2000;356(9248):2111.
22. Torrey EF. Patients, clients, consumers, survivors et al: what’s in a name? Schizophr Bull. 2011;37(3):466-468.
23. Wilson CT, Woloshin S, Schwartz L. Choosing where to have major surgery: who makes the decision? Arch Surg. 2007;142(3):242-246.
24. Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems. http://www.hcahpsonline.org. Accessed
January 26, 2014.
25. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354:2024-2033.
26. Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence—results of the Harvard Medical Practice Study III. N Engl J Med. 1991;325:245-251.
27. Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Bayl Univ Med Cent. 2003;16(2):157-161.
28. Ambady N, Laplante D, Nguyen T, et al. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132(1):5-9.
29. Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156(22):2565-2569.
30. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):
1126-1133.
31. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951-2957.
32. Bain W. Do we need a new word for patients? Continue to call them patients but treat them like customers. BMJ. 1999;319(7222):1436.
33. Johnson R, Moskowitz E, Thomas J, et al. Would you rather be treated as a patient or a customer? Yale Insights. http://insights.som.yale.edu/insights/would-you-rather-betreated-patient-or-customer. Accessed December 13, 2013.
Dear Dr. Mossman,
At the multispecialty hospital where I work, administrators refer to patients as “customers” and tell us that, by improving “the customer experience,” we can reduce complaints and avoid malpractice suits. This business lingo offends me. Doesn’t providing good care do more to prevent malpractice claims than calling sick patients “customers”?
Submitted by “Dr. H”
“All words are pegs to hang ideas on.” As was true when Reverend Henry Ward Beecher uttered this phrase in the 19th century,1 names affect how we relate to and feel about people. Many doctors don’t think of themselves as “selling” services, and they find calling patients “customers” distasteful.
But for at least 4 decades, mental health professionals themselves have used a “customer approach” to think about certain aspects of psychiatrist–patient encounters.2 More pertinent to Dr. H’s questions, many attorneys who advise physicians are convinced that giving patients a satisfying “customer experience” is a sound strategy for reducing the risk of malpractice litigation.3
If the attorneys are right, taking a customer service perspective can lower the likelihood that psychiatrists will be sued. To understand why, this article looks at:
• terms for referring to health care recipients
• the feelings those terms generate
• how the “customer service” perspective has become a malpractice prevention
strategy.
Off-putting connotations
All the currently used ways of referring to persons served by doctors have off-putting features.
The word “patient” dates back to the 14th century and comes from Latin present
participles of pati, “to suffer.” Although Alpha Omega Alpha’s motto—“be worthy
to serve the suffering”4—expresses doctors’ commitment to help others, “patient”
carries emotional baggage. A “patient” is “a sick individual” who seeks treatment
from a physician,5 a circumstance that most people (including doctors) find unpleasant and hope is only temporary. The adjective “patient” means “bearing pains or trials calmly or without complaint” and “manifesting forbearance under provocation or strain,”5 phrases associated with passivity, deference, and a long wait to see the doctor.
Because “patient” evokes notions of helplessness and need for direction, non-medical psychotherapists often use “client” to designate care recipients. “Client” has the same Latin root as “to lean” and refers to someone “under the protection of another.” More pertinent to discussions of mental health care, a “client” also is “a person who pays a professional person or organization for services” or “a customer.”5 The latter definition explains what makes “client” feel wrong to medical practitioners, who regard those they treat as deserving more compassion and sacrifice than someone who simply purchases professional services.
“Consumer,” a word of French origin derived from the Latin consumere (“to take
up”), refers to “a person who buys goods and services.”5 If “consumers” are buyers, then those from whom they make purchases are merchants or sellers. Western marketplace concepts often regard consumers as sovereign judges of their needs, and the role of commodity producers is to try to satisfy those needs.6
The problem with viewing health care recipients this way is that sellers don’t caution customers about buying things when only principles of supply-and-demand govern exchange relationships.7 Quite the contrary: producers sometimes promote their products through “advertising [that] distorts reality and creates artificial needs to make profit for a firm.”8 If physicians behave this way, however, they get criticism and deserve it.
A “customer” in 15th-century Middle English was a tax collector, but in modern
usage, a customer is someone who, like a consumer, “purchases some commodity or service.”5 By the early 20th century, “customer” became associated with notions of empowerment embodied in the merchants’ credo, “The customer is always right.”9 Chronic illnesses often require self-management and collaboration with those labeled the “givers” and “recipients” of medical care. Research shows that “patients are more trusting of, and committed to, physicians who adopt an empowering communication style with them,” which suggests “that empowering
patients presents a means to improve the patient–physician relationship.”10
Feelings about names
People have strong feelings about what they are called. In opposing calling patients “consumers,” Nobel Prize-winning economist Paul Krugman explains: “Medical care is an area in which crucial decisions—life and death decisions—must be made; yet making those decisions intelligently requires a vast amount of specialized knowledge; and often those decisions must also be made under conditions in which the patient …needs action immediately, with no time for discussion, let alone comparison shopping. …That’s why doctors have traditionally…been expected to behave according to higher standards than the average professional…The idea that all this can be reduced to money—that doctors are just people selling services to consumers of health care—is, well, sickening.”11
Less famous recipients of nonpsychiatric medical services also prefer being called
“patients” over “clients” or “consumers.”12-14 Recipients of mental health services have a different view, however. In some surveys, “patient” gets a plurality or majority of service recipients’ votes,15,16 but in others, recipients prefer to be called “clients” or other terms.17,18 Of note, people who prefer being called “patients” tend to strongly dislike being called “clients.”19 On the professional
side, psychiatrists—along with other physicians—prefer to speak of treating “patients” and to criticize letting economic phrases infect medical discourse.20-22
Names: A practical difference?
Does what psychiatrists call those they serve make any practical difference? Perhaps not, but evidence suggests that the attitudes that doctors take toward patients affects economic success and malpractice risk.
When they have choices about where they can seek health care, medical patients value physicians’ competence, but they also consider nonclinical factors such as family members’ opinions and convenience.23 Knowing this, the federal government’s Centers for Medicare & Medicaid Services publishes results from its Hospital Consumer Assessment of Healthcare Providers and Systems to “create incentives for hospitals to improve their quality of care.”24
Nonclinical factors play a big part in patients’ decisions about suing their doctors, too. Many malpractice claims turn out to be groundless in the sense that they do not involve medical errors,25 and most errors that result in injury do not lead to malpractice suits.26
What explains this disparity? Often when a lawsuit is filed, whatever injury may have occurred is coupled with an aggravating factor, such as a communication gaffe,27 a physician’s domineering tone of voice,28 or failure to acknowledge error.29 The lower a physician’s patient satisfaction ratings, the higher the physician’s likelihood of receiving complaints and getting sued for malpractice.30,31
These kinds of considerations probably lie behind the recommendation of one hospital manager to doctors: “Continue to call them patients but treat them like
customers.”32 More insights into this view come from responses solicited from Yale
students, staff members, and alumni about whether it seems preferable to be a “patient” or a “customer” (Box).33
Bottom Line
When patients get injured during medical care, evidence suggests that how they feel about their doctors makes a big difference in whether they decide to file suit. If you’re like most psychiatrists, you prefer to call persons whom you treat “patients.” But watching and improving the things that affect your patients’ “customer experience” may help you avoid malpractice litigation.
Related Resource
• Goldhill D. To fix healthcare, turn patients into customers. Bloomberg Personal Finance. www.bloomberg.com/news/2013-01-03/to-fix-health-care-turn-patients-intocustomers.html.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
At the multispecialty hospital where I work, administrators refer to patients as “customers” and tell us that, by improving “the customer experience,” we can reduce complaints and avoid malpractice suits. This business lingo offends me. Doesn’t providing good care do more to prevent malpractice claims than calling sick patients “customers”?
Submitted by “Dr. H”
“All words are pegs to hang ideas on.” As was true when Reverend Henry Ward Beecher uttered this phrase in the 19th century,1 names affect how we relate to and feel about people. Many doctors don’t think of themselves as “selling” services, and they find calling patients “customers” distasteful.
But for at least 4 decades, mental health professionals themselves have used a “customer approach” to think about certain aspects of psychiatrist–patient encounters.2 More pertinent to Dr. H’s questions, many attorneys who advise physicians are convinced that giving patients a satisfying “customer experience” is a sound strategy for reducing the risk of malpractice litigation.3
If the attorneys are right, taking a customer service perspective can lower the likelihood that psychiatrists will be sued. To understand why, this article looks at:
• terms for referring to health care recipients
• the feelings those terms generate
• how the “customer service” perspective has become a malpractice prevention
strategy.
Off-putting connotations
All the currently used ways of referring to persons served by doctors have off-putting features.
The word “patient” dates back to the 14th century and comes from Latin present
participles of pati, “to suffer.” Although Alpha Omega Alpha’s motto—“be worthy
to serve the suffering”4—expresses doctors’ commitment to help others, “patient”
carries emotional baggage. A “patient” is “a sick individual” who seeks treatment
from a physician,5 a circumstance that most people (including doctors) find unpleasant and hope is only temporary. The adjective “patient” means “bearing pains or trials calmly or without complaint” and “manifesting forbearance under provocation or strain,”5 phrases associated with passivity, deference, and a long wait to see the doctor.
Because “patient” evokes notions of helplessness and need for direction, non-medical psychotherapists often use “client” to designate care recipients. “Client” has the same Latin root as “to lean” and refers to someone “under the protection of another.” More pertinent to discussions of mental health care, a “client” also is “a person who pays a professional person or organization for services” or “a customer.”5 The latter definition explains what makes “client” feel wrong to medical practitioners, who regard those they treat as deserving more compassion and sacrifice than someone who simply purchases professional services.
“Consumer,” a word of French origin derived from the Latin consumere (“to take
up”), refers to “a person who buys goods and services.”5 If “consumers” are buyers, then those from whom they make purchases are merchants or sellers. Western marketplace concepts often regard consumers as sovereign judges of their needs, and the role of commodity producers is to try to satisfy those needs.6
The problem with viewing health care recipients this way is that sellers don’t caution customers about buying things when only principles of supply-and-demand govern exchange relationships.7 Quite the contrary: producers sometimes promote their products through “advertising [that] distorts reality and creates artificial needs to make profit for a firm.”8 If physicians behave this way, however, they get criticism and deserve it.
A “customer” in 15th-century Middle English was a tax collector, but in modern
usage, a customer is someone who, like a consumer, “purchases some commodity or service.”5 By the early 20th century, “customer” became associated with notions of empowerment embodied in the merchants’ credo, “The customer is always right.”9 Chronic illnesses often require self-management and collaboration with those labeled the “givers” and “recipients” of medical care. Research shows that “patients are more trusting of, and committed to, physicians who adopt an empowering communication style with them,” which suggests “that empowering
patients presents a means to improve the patient–physician relationship.”10
Feelings about names
People have strong feelings about what they are called. In opposing calling patients “consumers,” Nobel Prize-winning economist Paul Krugman explains: “Medical care is an area in which crucial decisions—life and death decisions—must be made; yet making those decisions intelligently requires a vast amount of specialized knowledge; and often those decisions must also be made under conditions in which the patient …needs action immediately, with no time for discussion, let alone comparison shopping. …That’s why doctors have traditionally…been expected to behave according to higher standards than the average professional…The idea that all this can be reduced to money—that doctors are just people selling services to consumers of health care—is, well, sickening.”11
Less famous recipients of nonpsychiatric medical services also prefer being called
“patients” over “clients” or “consumers.”12-14 Recipients of mental health services have a different view, however. In some surveys, “patient” gets a plurality or majority of service recipients’ votes,15,16 but in others, recipients prefer to be called “clients” or other terms.17,18 Of note, people who prefer being called “patients” tend to strongly dislike being called “clients.”19 On the professional
side, psychiatrists—along with other physicians—prefer to speak of treating “patients” and to criticize letting economic phrases infect medical discourse.20-22
Names: A practical difference?
Does what psychiatrists call those they serve make any practical difference? Perhaps not, but evidence suggests that the attitudes that doctors take toward patients affects economic success and malpractice risk.
When they have choices about where they can seek health care, medical patients value physicians’ competence, but they also consider nonclinical factors such as family members’ opinions and convenience.23 Knowing this, the federal government’s Centers for Medicare & Medicaid Services publishes results from its Hospital Consumer Assessment of Healthcare Providers and Systems to “create incentives for hospitals to improve their quality of care.”24
Nonclinical factors play a big part in patients’ decisions about suing their doctors, too. Many malpractice claims turn out to be groundless in the sense that they do not involve medical errors,25 and most errors that result in injury do not lead to malpractice suits.26
What explains this disparity? Often when a lawsuit is filed, whatever injury may have occurred is coupled with an aggravating factor, such as a communication gaffe,27 a physician’s domineering tone of voice,28 or failure to acknowledge error.29 The lower a physician’s patient satisfaction ratings, the higher the physician’s likelihood of receiving complaints and getting sued for malpractice.30,31
These kinds of considerations probably lie behind the recommendation of one hospital manager to doctors: “Continue to call them patients but treat them like
customers.”32 More insights into this view come from responses solicited from Yale
students, staff members, and alumni about whether it seems preferable to be a “patient” or a “customer” (Box).33
Bottom Line
When patients get injured during medical care, evidence suggests that how they feel about their doctors makes a big difference in whether they decide to file suit. If you’re like most psychiatrists, you prefer to call persons whom you treat “patients.” But watching and improving the things that affect your patients’ “customer experience” may help you avoid malpractice litigation.
Related Resource
• Goldhill D. To fix healthcare, turn patients into customers. Bloomberg Personal Finance. www.bloomberg.com/news/2013-01-03/to-fix-health-care-turn-patients-intocustomers.html.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Beecher HW, Drysdale W. Proverbs from Plymouth pulpit. New York, NY: D. Appleton & Co.;1887.
2. Lazare A, Eisenthal S, Wasserman L. The customer approach to patienthood: attending to patient requests in a walk-in clinic. Arch Gen Psychiatry. 1975;32:553-558.
3. Schleiter KE. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
4. Alpha Omega Alpha Honor Medical Society. Alpha Omega Alpha constitution. http://www.alphaomegaalpha.org/constitution.html. Accessed December 13, 2013. Accessed December 13, 2013.
5. Merriam-Webster. Dictionary. http://www.merriamwebster.com. Accessed December 9, 2013.
6. Kotler P, Burton S, Deans K, et al. Marketing, 9th ed. Frenchs Forest, Australia: Pearson Education Australia; 2013.
7. Deber RB. Getting what we pay for: myths and realities about financing Canada’s health care system. Health Law Can. 2000;21(2):9-56.
8. Takala T, Uusitalo O. An alternative view of relationship marketing: a framework for ethical analysis. Eur J Mark. 1996;30:45-60.
9. Van Vuren FS. The Yankee who taught Britishers that ‘the customer is always right.’ Milwaukee Journal. http://www.wisconsinhistory.org/wlhba/articleView.
asp?pg=1&id=11176. Published September 9, 1932. Accessed December 20, 2013.
10. Ouschan T, Sweeney J, Johnson L. Customer empowerment and relationship outcomes in healthcare consultations. Eur J Mark. 2006;40:1068-1086.
11. Krugman P. Patients are not consumers. The New York Times. http://krugman.blogs.nytimes.com/2011/04/20/patients-are-not-consumers. Published April 20, 2011. Accessed December 13, 2013.
12. Nair BR. Patient, client or customer? Med J Aust. 1998;169:593.
13. Wing PC. Patient or client? If in doubt, ask. CMAJ. 1997;157:287-289.
14. Deber RB, Kraetschmer N, Urowitz S, et al. Patient, consumer, client, or customer: what do people want to be called? Health Expect. 2005;8(4):345-351.
15. Sharma V, Whitney D, Kazarian SS, et al. Preferred terms for users of mental health services among service providers and recipients. Psychiatr Serv. 2000;51(2): 203-209.
16. Simmons P, Hawley CJ, Gale TM, et al. Service user, patient, client, user or survivor: describing recipients of mental health services. Psychiatrist. 2010;34:20-23.
17. Lloyd C, King R, Bassett H, et al. Patient, client or consumer? A survey of preferred terms. Australas Psychiatry. 2001; 9(4):321-324.
18. Covell NH, McCorkle BH, Weissman EM, et al. What’s in a name? Terms preferred by service recipients. Adm Policy Ment Health. 2007;34(5):443-447.
19. Ritchie CW, Hayes D, Ames DJ. Patient or client? The opinions of people attending a psychiatric clinic. Psychiatrist. 2000;24(12):447-450.
20. Andreasen NC. Clients, consumers, providers, and products: where will it all end? Am J Psychiatry. 1995;152:1107-1109.
21. Editorial. What’s in a name? Lancet. 2000;356(9248):2111.
22. Torrey EF. Patients, clients, consumers, survivors et al: what’s in a name? Schizophr Bull. 2011;37(3):466-468.
23. Wilson CT, Woloshin S, Schwartz L. Choosing where to have major surgery: who makes the decision? Arch Surg. 2007;142(3):242-246.
24. Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems. http://www.hcahpsonline.org. Accessed
January 26, 2014.
25. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354:2024-2033.
26. Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence—results of the Harvard Medical Practice Study III. N Engl J Med. 1991;325:245-251.
27. Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Bayl Univ Med Cent. 2003;16(2):157-161.
28. Ambady N, Laplante D, Nguyen T, et al. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132(1):5-9.
29. Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156(22):2565-2569.
30. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):
1126-1133.
31. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951-2957.
32. Bain W. Do we need a new word for patients? Continue to call them patients but treat them like customers. BMJ. 1999;319(7222):1436.
33. Johnson R, Moskowitz E, Thomas J, et al. Would you rather be treated as a patient or a customer? Yale Insights. http://insights.som.yale.edu/insights/would-you-rather-betreated-patient-or-customer. Accessed December 13, 2013.
1. Beecher HW, Drysdale W. Proverbs from Plymouth pulpit. New York, NY: D. Appleton & Co.;1887.
2. Lazare A, Eisenthal S, Wasserman L. The customer approach to patienthood: attending to patient requests in a walk-in clinic. Arch Gen Psychiatry. 1975;32:553-558.
3. Schleiter KE. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
4. Alpha Omega Alpha Honor Medical Society. Alpha Omega Alpha constitution. http://www.alphaomegaalpha.org/constitution.html. Accessed December 13, 2013. Accessed December 13, 2013.
5. Merriam-Webster. Dictionary. http://www.merriamwebster.com. Accessed December 9, 2013.
6. Kotler P, Burton S, Deans K, et al. Marketing, 9th ed. Frenchs Forest, Australia: Pearson Education Australia; 2013.
7. Deber RB. Getting what we pay for: myths and realities about financing Canada’s health care system. Health Law Can. 2000;21(2):9-56.
8. Takala T, Uusitalo O. An alternative view of relationship marketing: a framework for ethical analysis. Eur J Mark. 1996;30:45-60.
9. Van Vuren FS. The Yankee who taught Britishers that ‘the customer is always right.’ Milwaukee Journal. http://www.wisconsinhistory.org/wlhba/articleView.
asp?pg=1&id=11176. Published September 9, 1932. Accessed December 20, 2013.
10. Ouschan T, Sweeney J, Johnson L. Customer empowerment and relationship outcomes in healthcare consultations. Eur J Mark. 2006;40:1068-1086.
11. Krugman P. Patients are not consumers. The New York Times. http://krugman.blogs.nytimes.com/2011/04/20/patients-are-not-consumers. Published April 20, 2011. Accessed December 13, 2013.
12. Nair BR. Patient, client or customer? Med J Aust. 1998;169:593.
13. Wing PC. Patient or client? If in doubt, ask. CMAJ. 1997;157:287-289.
14. Deber RB, Kraetschmer N, Urowitz S, et al. Patient, consumer, client, or customer: what do people want to be called? Health Expect. 2005;8(4):345-351.
15. Sharma V, Whitney D, Kazarian SS, et al. Preferred terms for users of mental health services among service providers and recipients. Psychiatr Serv. 2000;51(2): 203-209.
16. Simmons P, Hawley CJ, Gale TM, et al. Service user, patient, client, user or survivor: describing recipients of mental health services. Psychiatrist. 2010;34:20-23.
17. Lloyd C, King R, Bassett H, et al. Patient, client or consumer? A survey of preferred terms. Australas Psychiatry. 2001; 9(4):321-324.
18. Covell NH, McCorkle BH, Weissman EM, et al. What’s in a name? Terms preferred by service recipients. Adm Policy Ment Health. 2007;34(5):443-447.
19. Ritchie CW, Hayes D, Ames DJ. Patient or client? The opinions of people attending a psychiatric clinic. Psychiatrist. 2000;24(12):447-450.
20. Andreasen NC. Clients, consumers, providers, and products: where will it all end? Am J Psychiatry. 1995;152:1107-1109.
21. Editorial. What’s in a name? Lancet. 2000;356(9248):2111.
22. Torrey EF. Patients, clients, consumers, survivors et al: what’s in a name? Schizophr Bull. 2011;37(3):466-468.
23. Wilson CT, Woloshin S, Schwartz L. Choosing where to have major surgery: who makes the decision? Arch Surg. 2007;142(3):242-246.
24. Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems. http://www.hcahpsonline.org. Accessed
January 26, 2014.
25. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354:2024-2033.
26. Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence—results of the Harvard Medical Practice Study III. N Engl J Med. 1991;325:245-251.
27. Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Bayl Univ Med Cent. 2003;16(2):157-161.
28. Ambady N, Laplante D, Nguyen T, et al. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132(1):5-9.
29. Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156(22):2565-2569.
30. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):
1126-1133.
31. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951-2957.
32. Bain W. Do we need a new word for patients? Continue to call them patients but treat them like customers. BMJ. 1999;319(7222):1436.
33. Johnson R, Moskowitz E, Thomas J, et al. Would you rather be treated as a patient or a customer? Yale Insights. http://insights.som.yale.edu/insights/would-you-rather-betreated-patient-or-customer. Accessed December 13, 2013.
Are you admitting malpractice if you apologize to a patient?
Dear Dr. Mossman:
Recently, my prescribing error caused a patient to get very sick. I feel terrible. I want to tell my patient I’m sorry, but I’ve heard that a lawyer could use my “confession” to prove I’ve committed malpractice. If I apologize, could my words come back to haunt me if a lawsuit is filed?
Submitted by “Dr. E”
As several faiths have long recognized, apologies are important social acts that express our awareness of and obligations to each other. In recent years, psychologists have established how apologies confer emotional benefits on those who give and receive them.1 Offering a sincere apology can be the right thing to do and a beneficial act for both the apologizing and the injured parties.
Traditionally, physicians have avoided apologizing for errors that harmed patients. Part of the reluctance stemmed from pride or wanting to avoid shame. But as Dr. E’s question suggests, doctors also have feared—and lawyers have advised—that apologizing might compromise a malpractice defense.2
Attitudes have changed in recent years, however. Increasingly, practitioners, medical organizations, and risk management entities are telling physicians they should apologize for errors, and many states have laws that mitigate adverse legal consequences of saying “I’m sorry.”
In response to Dr. E’s questions, I’ll examine:
• ethical and professional obligations following unexpected outcomes
• physicians’ reasons for being reluctant to apologize
• the benefits of apologizing
• legal protections for apologies.
Owning up: Ethical and professional expectations
Current codes of medical ethics say that physicians should tell patients when mistakes and misjudgments have caused harm. “It is a fundamental ethical requirement that a physician should at all times deal honestly and openly with patients,” states the American Medical Association’s Code of Ethics. When a patient suffers because of a medical error, “the physician is ethically required to inform the patient of all the facts necessary to ensure” the patient can “make informed decisions regarding future medical care.”3
The National Patient Safety Foundation,4 the American College of Physicians,5 and the Joint Commission (the agency that provides official accreditation of thousands of healthcare organizations) have voiced similar positions for years. Since 2001, the Joint Commission has required that practitioners and medical facilities tell patients and families “about the outcomes of care, treatment, and services ... including unanticipated outcomes.”6
Reluctance is understandable
Although these recommendations and policies suggest that telling patients about medical errors is an established professional expectation, physicians remain reluctant to apologize to patients for emotional and legal reasons that are easy to understand.
Apologizing is hard. On one hand, research shows that refusing to apologize sometimes increases feelings of empowerment and control, and can boost self-esteem more than apologizing does.7 On the other, apologizing often requires one to acknowledge a failure or betrayal of trust and to experience guilt, shame, embarrassment, or fear that one’s apology will be met with anger or rejection.8
Physicians historically have treated errors as personal failures. Apologizing in a medical context can feel like saying, “I am incompetent.”9,10 The law has reinforced this attitude. As the Mississippi Supreme Court put it, “Medical malpractice is legal fault by a physician or surgeon. It arises from the failure of a physician to provide the quality of care required by law” (emphasis added).11
Some lawyers continue to advise physicians not to make admissions that could be used in a malpractice case. Their reasoning: If a doctor does something that adversely affects a malpractice insurer’s ability to defend the case, the insurer might not provide liability coverage for the adverse event.12
Emotional and legal benefits
Against this no-apology stance is a growing body of theoretical, empirical, and practical arguments favoring apologies for medical errors. Case studies suggest that anger is behind much medical malpractice litigation and that physicians’ apologies—which reduce anger and increase communication—might reduce patients’ motivations to sue.13 Apologies sometimes lead to forgiveness, an emotional state that “can provide victims and offenders with many important benefits, including enhanced psychological well-being ... and greater physiological health.”14 Apologies do this by mitigating the injured party’s negative emotional states and diminishing rumination about the transgression and perceived harm severity.
The practical argument favoring apologizing is that it may defuse feelings that lead to lawsuits and reduce the size of payouts. Experimental studies suggest that apologizing leads to earlier satisfaction and closure, faster settlements, and lower damage payments. When apologies include admissions of fault, injured parties feel greater respect for and less need to punish those who have harmed them, are more willing to forgive, and are more likely to accept settlement offers.15
Hospitals in Pennsylvania, Kentucky, and Michigan have found that sincere apologies and effective error disclosure programs reduce malpractice payouts and lead to faster settlements.16 As some plaintiffs’ lawyers point out, being honest and forthright and fixing the injured parties’ problems can quickly defuse a lawsuit. One attorney explained things this way: “We never sue the nice, contrite doctors. Their patients never call our offices. But the doctors who are poor communicators and abandon their patients get sued all the time. Their patients come to our offices looking for answers.”17
Apology laws: Protection from your own words
The belief that apologies by physicians can help patients emotionally and reduce malpractice litigation has led state legislatures to enact so-called apology laws in many jurisdictions in the United States.18 The general point of these rules and statutes is to prevent later use of doctors’ words in litigation. States differ substantially in the scope and type of protection that their laws offer. Some states prohibit doctors’ apologies for adverse outcomes from being used in litigation to prove negligence, while others only exclude expressions of sympathy or offers to pay for corrective treatment. Selected language from several states’ apology laws appears in the Table.19-23
Do apology laws work? Recent research by economists Ho and Liu indicates that they do. Comparing payouts in states with and without apology laws, they conclude that “apology laws have the greatest reduction in average payment size and settlement time in cases involving more severe patient outcomes,”13 such as obstetrics and anesthesia cases, cases that involve infants, and cases in which physicians improperly manage or fail to properly diagnose an illness.24
The practical impact of apologizing for psychiatric malpractice cases is unclear, but forensic psychiatrists Marilyn Price and Patricia Recupero believe that, following some unexpected outcomes, thoughtful expressions of sympathy, regret, and—if the outcome resulted from an error—apologies may be appropriate. Price and Recupero caution that such conversations should occur as part of broader programs that investigate unanticipated adverse events and provide education and coaching about appropriate ways to make disclosures. Clinicians also should consult with legal counsel, risk management officers, and liability insurance carriers before initiating such disclosures.25
Bottom Line
Apologizing for medical errors may mitigate malpractice liability and can help injured parties and physicians feel better. Whether plaintiffs can use apologies as evidence of malpractice depends on state laws and rules of evidence. Before you apologize for an unanticipated outcome, discuss the situation with your legal counsel, risk management officers, and insurers.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
Douglas Mossman, MD, talks about who you should consult before apologizing to a patient for a bad outcome. Dr. Mossman is Professor of Clinical Psychiatry and Director, Division of Forensic Psychiatry, University of Cincinnati College of Medicine, Cincinnati, Ohio.
1. McCullough ME, Sandage SJ, Brown SW, et al. Interpersonal forgiving in close relationships: II. Theoretical elaboration and measurement. J Pers Soc Psychol. 1998;75:1586-1603.
2. O’Reilly KB. “I’m sorry”: why is that so hard for doctors to say? http://www.amednews.com/article/20100201/profession/302019937/4. Published February 1, 2010. Accessed September 30, 2013.
3. American Medical Association. AMA Code of Medical Ethics, Opinion 8.12 – Patient information. http://www.ama-assn.org//ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion812.page. Published June 1994. Accessed September 30, 2013.
4. Hickson GB, Pichert JW. Disclosure and apology. http://www.npsf.org/wp-content/uploads/2011/10/RG_SUPS_After_Mod1_Hickson.pdf. Accessed October 4, 2013.
5. Snyder L, American College of Physicians Ethics, Professionalism, and Human Rights Committee. American College of Physicians ethics manual: sixth edition. Ann Intern Med. 2012;156(1, pt 2):73-104.
6. ECRI Institute. Disclosure of unanticipated outcomes. In: Healthcare risk control Supplement A, Risk analysis. Plymouth Meeting, PA: ECRI; 2002.
7. Okimoto TG, Wenzel M, Hedrick K. Refusing to apologize can have psychological benefits (and we issue no mea culpa for this research finding). Eur J Soc Psychol. 2013;43:22-31.
8. Lazare A. On apology. New York, NY: Oxford University Press; 2004.
9. Hilfiker D. Facing our mistakes. N Engl J Med. 1984;310:
118-122.
10. Leape LL. Error in medicine. JAMA. 1994;272:1851-1857.
11. Hall v. Hilbun, 466 So.2d 856 (Miss. 1985).
12. Kern SI. You continue to face exposure if you apologize. http://medicaleconomics.modernmedicine.com/medical-economics/news/modernmedicine/modern-medicine-now/you-continue-face-exposure-if-you-apologiz. Published September 24, 2010. Accessed October 1, 2013.
13. Ho B, Liu E. Does sorry work? The impact of apology laws on medical malpractice. J Risk Uncertain. 2011;43(2):141-167.
14. Fehr R, Gelfand MJ, Nag M. The road to forgiveness: a meta-analytic synthesis of its situational and dispositional correlates. Psychol Bull. 2010;136:894-914.
15. Robbennolt JK. Apologies and settlement. Court Review. 2009;45:90-97.
16. Saitta N, Hodge SD. Efficacy of a physician’s words of empathy: an overview of state apology laws. J Am Osteopath Assoc. 2012;112(5):302-306.
17. Wojcieszak D, Banja J, Houk C. The sorry works! coalition: making the case for full disclosure. Jt Comm J Qual Patient Saf. 2006;32(6):344-350.
18. National Conference of State Legislatures. Medical liability/Medical malpractice laws. http://www.ncsl.org/issues-research/banking/medical-liability-medical-malpractice-laws.aspx. Published August 15, 2011. Accessed October 4, 2013.
19. Conn Gen Stat Ann §52-184d(b).
20. Fla Stat §90.4026(2).
21. Ill Comp Stat §5/8-1901.
22. NC Gen Stat §8C-1, Rule 413.
23. Tex. Civ. Prac. & Rem. Code §18.061.
24. Ho B, Liu E. What’s an apology worth? Decomposing the effect of apologies on medical malpractice payments using state apology laws. J Empir Leg Stud. 2011;8:179-199.
25. Price M, Recupero PR. Risk management. In: Sharfstein SS, Dickerson FB, Oldham JM, eds. Textbook of hospital psychiatry. Arlington, VA: American Psychiatric Publishing, Inc.; 2009:411-412.
Dear Dr. Mossman:
Recently, my prescribing error caused a patient to get very sick. I feel terrible. I want to tell my patient I’m sorry, but I’ve heard that a lawyer could use my “confession” to prove I’ve committed malpractice. If I apologize, could my words come back to haunt me if a lawsuit is filed?
Submitted by “Dr. E”
As several faiths have long recognized, apologies are important social acts that express our awareness of and obligations to each other. In recent years, psychologists have established how apologies confer emotional benefits on those who give and receive them.1 Offering a sincere apology can be the right thing to do and a beneficial act for both the apologizing and the injured parties.
Traditionally, physicians have avoided apologizing for errors that harmed patients. Part of the reluctance stemmed from pride or wanting to avoid shame. But as Dr. E’s question suggests, doctors also have feared—and lawyers have advised—that apologizing might compromise a malpractice defense.2
Attitudes have changed in recent years, however. Increasingly, practitioners, medical organizations, and risk management entities are telling physicians they should apologize for errors, and many states have laws that mitigate adverse legal consequences of saying “I’m sorry.”
In response to Dr. E’s questions, I’ll examine:
• ethical and professional obligations following unexpected outcomes
• physicians’ reasons for being reluctant to apologize
• the benefits of apologizing
• legal protections for apologies.
Owning up: Ethical and professional expectations
Current codes of medical ethics say that physicians should tell patients when mistakes and misjudgments have caused harm. “It is a fundamental ethical requirement that a physician should at all times deal honestly and openly with patients,” states the American Medical Association’s Code of Ethics. When a patient suffers because of a medical error, “the physician is ethically required to inform the patient of all the facts necessary to ensure” the patient can “make informed decisions regarding future medical care.”3
The National Patient Safety Foundation,4 the American College of Physicians,5 and the Joint Commission (the agency that provides official accreditation of thousands of healthcare organizations) have voiced similar positions for years. Since 2001, the Joint Commission has required that practitioners and medical facilities tell patients and families “about the outcomes of care, treatment, and services ... including unanticipated outcomes.”6
Reluctance is understandable
Although these recommendations and policies suggest that telling patients about medical errors is an established professional expectation, physicians remain reluctant to apologize to patients for emotional and legal reasons that are easy to understand.
Apologizing is hard. On one hand, research shows that refusing to apologize sometimes increases feelings of empowerment and control, and can boost self-esteem more than apologizing does.7 On the other, apologizing often requires one to acknowledge a failure or betrayal of trust and to experience guilt, shame, embarrassment, or fear that one’s apology will be met with anger or rejection.8
Physicians historically have treated errors as personal failures. Apologizing in a medical context can feel like saying, “I am incompetent.”9,10 The law has reinforced this attitude. As the Mississippi Supreme Court put it, “Medical malpractice is legal fault by a physician or surgeon. It arises from the failure of a physician to provide the quality of care required by law” (emphasis added).11
Some lawyers continue to advise physicians not to make admissions that could be used in a malpractice case. Their reasoning: If a doctor does something that adversely affects a malpractice insurer’s ability to defend the case, the insurer might not provide liability coverage for the adverse event.12
Emotional and legal benefits
Against this no-apology stance is a growing body of theoretical, empirical, and practical arguments favoring apologies for medical errors. Case studies suggest that anger is behind much medical malpractice litigation and that physicians’ apologies—which reduce anger and increase communication—might reduce patients’ motivations to sue.13 Apologies sometimes lead to forgiveness, an emotional state that “can provide victims and offenders with many important benefits, including enhanced psychological well-being ... and greater physiological health.”14 Apologies do this by mitigating the injured party’s negative emotional states and diminishing rumination about the transgression and perceived harm severity.
The practical argument favoring apologizing is that it may defuse feelings that lead to lawsuits and reduce the size of payouts. Experimental studies suggest that apologizing leads to earlier satisfaction and closure, faster settlements, and lower damage payments. When apologies include admissions of fault, injured parties feel greater respect for and less need to punish those who have harmed them, are more willing to forgive, and are more likely to accept settlement offers.15
Hospitals in Pennsylvania, Kentucky, and Michigan have found that sincere apologies and effective error disclosure programs reduce malpractice payouts and lead to faster settlements.16 As some plaintiffs’ lawyers point out, being honest and forthright and fixing the injured parties’ problems can quickly defuse a lawsuit. One attorney explained things this way: “We never sue the nice, contrite doctors. Their patients never call our offices. But the doctors who are poor communicators and abandon their patients get sued all the time. Their patients come to our offices looking for answers.”17
Apology laws: Protection from your own words
The belief that apologies by physicians can help patients emotionally and reduce malpractice litigation has led state legislatures to enact so-called apology laws in many jurisdictions in the United States.18 The general point of these rules and statutes is to prevent later use of doctors’ words in litigation. States differ substantially in the scope and type of protection that their laws offer. Some states prohibit doctors’ apologies for adverse outcomes from being used in litigation to prove negligence, while others only exclude expressions of sympathy or offers to pay for corrective treatment. Selected language from several states’ apology laws appears in the Table.19-23
Do apology laws work? Recent research by economists Ho and Liu indicates that they do. Comparing payouts in states with and without apology laws, they conclude that “apology laws have the greatest reduction in average payment size and settlement time in cases involving more severe patient outcomes,”13 such as obstetrics and anesthesia cases, cases that involve infants, and cases in which physicians improperly manage or fail to properly diagnose an illness.24
The practical impact of apologizing for psychiatric malpractice cases is unclear, but forensic psychiatrists Marilyn Price and Patricia Recupero believe that, following some unexpected outcomes, thoughtful expressions of sympathy, regret, and—if the outcome resulted from an error—apologies may be appropriate. Price and Recupero caution that such conversations should occur as part of broader programs that investigate unanticipated adverse events and provide education and coaching about appropriate ways to make disclosures. Clinicians also should consult with legal counsel, risk management officers, and liability insurance carriers before initiating such disclosures.25
Bottom Line
Apologizing for medical errors may mitigate malpractice liability and can help injured parties and physicians feel better. Whether plaintiffs can use apologies as evidence of malpractice depends on state laws and rules of evidence. Before you apologize for an unanticipated outcome, discuss the situation with your legal counsel, risk management officers, and insurers.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
Douglas Mossman, MD, talks about who you should consult before apologizing to a patient for a bad outcome. Dr. Mossman is Professor of Clinical Psychiatry and Director, Division of Forensic Psychiatry, University of Cincinnati College of Medicine, Cincinnati, Ohio.
Dear Dr. Mossman:
Recently, my prescribing error caused a patient to get very sick. I feel terrible. I want to tell my patient I’m sorry, but I’ve heard that a lawyer could use my “confession” to prove I’ve committed malpractice. If I apologize, could my words come back to haunt me if a lawsuit is filed?
Submitted by “Dr. E”
As several faiths have long recognized, apologies are important social acts that express our awareness of and obligations to each other. In recent years, psychologists have established how apologies confer emotional benefits on those who give and receive them.1 Offering a sincere apology can be the right thing to do and a beneficial act for both the apologizing and the injured parties.
Traditionally, physicians have avoided apologizing for errors that harmed patients. Part of the reluctance stemmed from pride or wanting to avoid shame. But as Dr. E’s question suggests, doctors also have feared—and lawyers have advised—that apologizing might compromise a malpractice defense.2
Attitudes have changed in recent years, however. Increasingly, practitioners, medical organizations, and risk management entities are telling physicians they should apologize for errors, and many states have laws that mitigate adverse legal consequences of saying “I’m sorry.”
In response to Dr. E’s questions, I’ll examine:
• ethical and professional obligations following unexpected outcomes
• physicians’ reasons for being reluctant to apologize
• the benefits of apologizing
• legal protections for apologies.
Owning up: Ethical and professional expectations
Current codes of medical ethics say that physicians should tell patients when mistakes and misjudgments have caused harm. “It is a fundamental ethical requirement that a physician should at all times deal honestly and openly with patients,” states the American Medical Association’s Code of Ethics. When a patient suffers because of a medical error, “the physician is ethically required to inform the patient of all the facts necessary to ensure” the patient can “make informed decisions regarding future medical care.”3
The National Patient Safety Foundation,4 the American College of Physicians,5 and the Joint Commission (the agency that provides official accreditation of thousands of healthcare organizations) have voiced similar positions for years. Since 2001, the Joint Commission has required that practitioners and medical facilities tell patients and families “about the outcomes of care, treatment, and services ... including unanticipated outcomes.”6
Reluctance is understandable
Although these recommendations and policies suggest that telling patients about medical errors is an established professional expectation, physicians remain reluctant to apologize to patients for emotional and legal reasons that are easy to understand.
Apologizing is hard. On one hand, research shows that refusing to apologize sometimes increases feelings of empowerment and control, and can boost self-esteem more than apologizing does.7 On the other, apologizing often requires one to acknowledge a failure or betrayal of trust and to experience guilt, shame, embarrassment, or fear that one’s apology will be met with anger or rejection.8
Physicians historically have treated errors as personal failures. Apologizing in a medical context can feel like saying, “I am incompetent.”9,10 The law has reinforced this attitude. As the Mississippi Supreme Court put it, “Medical malpractice is legal fault by a physician or surgeon. It arises from the failure of a physician to provide the quality of care required by law” (emphasis added).11
Some lawyers continue to advise physicians not to make admissions that could be used in a malpractice case. Their reasoning: If a doctor does something that adversely affects a malpractice insurer’s ability to defend the case, the insurer might not provide liability coverage for the adverse event.12
Emotional and legal benefits
Against this no-apology stance is a growing body of theoretical, empirical, and practical arguments favoring apologies for medical errors. Case studies suggest that anger is behind much medical malpractice litigation and that physicians’ apologies—which reduce anger and increase communication—might reduce patients’ motivations to sue.13 Apologies sometimes lead to forgiveness, an emotional state that “can provide victims and offenders with many important benefits, including enhanced psychological well-being ... and greater physiological health.”14 Apologies do this by mitigating the injured party’s negative emotional states and diminishing rumination about the transgression and perceived harm severity.
The practical argument favoring apologizing is that it may defuse feelings that lead to lawsuits and reduce the size of payouts. Experimental studies suggest that apologizing leads to earlier satisfaction and closure, faster settlements, and lower damage payments. When apologies include admissions of fault, injured parties feel greater respect for and less need to punish those who have harmed them, are more willing to forgive, and are more likely to accept settlement offers.15
Hospitals in Pennsylvania, Kentucky, and Michigan have found that sincere apologies and effective error disclosure programs reduce malpractice payouts and lead to faster settlements.16 As some plaintiffs’ lawyers point out, being honest and forthright and fixing the injured parties’ problems can quickly defuse a lawsuit. One attorney explained things this way: “We never sue the nice, contrite doctors. Their patients never call our offices. But the doctors who are poor communicators and abandon their patients get sued all the time. Their patients come to our offices looking for answers.”17
Apology laws: Protection from your own words
The belief that apologies by physicians can help patients emotionally and reduce malpractice litigation has led state legislatures to enact so-called apology laws in many jurisdictions in the United States.18 The general point of these rules and statutes is to prevent later use of doctors’ words in litigation. States differ substantially in the scope and type of protection that their laws offer. Some states prohibit doctors’ apologies for adverse outcomes from being used in litigation to prove negligence, while others only exclude expressions of sympathy or offers to pay for corrective treatment. Selected language from several states’ apology laws appears in the Table.19-23
Do apology laws work? Recent research by economists Ho and Liu indicates that they do. Comparing payouts in states with and without apology laws, they conclude that “apology laws have the greatest reduction in average payment size and settlement time in cases involving more severe patient outcomes,”13 such as obstetrics and anesthesia cases, cases that involve infants, and cases in which physicians improperly manage or fail to properly diagnose an illness.24
The practical impact of apologizing for psychiatric malpractice cases is unclear, but forensic psychiatrists Marilyn Price and Patricia Recupero believe that, following some unexpected outcomes, thoughtful expressions of sympathy, regret, and—if the outcome resulted from an error—apologies may be appropriate. Price and Recupero caution that such conversations should occur as part of broader programs that investigate unanticipated adverse events and provide education and coaching about appropriate ways to make disclosures. Clinicians also should consult with legal counsel, risk management officers, and liability insurance carriers before initiating such disclosures.25
Bottom Line
Apologizing for medical errors may mitigate malpractice liability and can help injured parties and physicians feel better. Whether plaintiffs can use apologies as evidence of malpractice depends on state laws and rules of evidence. Before you apologize for an unanticipated outcome, discuss the situation with your legal counsel, risk management officers, and insurers.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Featured Audio
Douglas Mossman, MD, talks about who you should consult before apologizing to a patient for a bad outcome. Dr. Mossman is Professor of Clinical Psychiatry and Director, Division of Forensic Psychiatry, University of Cincinnati College of Medicine, Cincinnati, Ohio.
1. McCullough ME, Sandage SJ, Brown SW, et al. Interpersonal forgiving in close relationships: II. Theoretical elaboration and measurement. J Pers Soc Psychol. 1998;75:1586-1603.
2. O’Reilly KB. “I’m sorry”: why is that so hard for doctors to say? http://www.amednews.com/article/20100201/profession/302019937/4. Published February 1, 2010. Accessed September 30, 2013.
3. American Medical Association. AMA Code of Medical Ethics, Opinion 8.12 – Patient information. http://www.ama-assn.org//ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion812.page. Published June 1994. Accessed September 30, 2013.
4. Hickson GB, Pichert JW. Disclosure and apology. http://www.npsf.org/wp-content/uploads/2011/10/RG_SUPS_After_Mod1_Hickson.pdf. Accessed October 4, 2013.
5. Snyder L, American College of Physicians Ethics, Professionalism, and Human Rights Committee. American College of Physicians ethics manual: sixth edition. Ann Intern Med. 2012;156(1, pt 2):73-104.
6. ECRI Institute. Disclosure of unanticipated outcomes. In: Healthcare risk control Supplement A, Risk analysis. Plymouth Meeting, PA: ECRI; 2002.
7. Okimoto TG, Wenzel M, Hedrick K. Refusing to apologize can have psychological benefits (and we issue no mea culpa for this research finding). Eur J Soc Psychol. 2013;43:22-31.
8. Lazare A. On apology. New York, NY: Oxford University Press; 2004.
9. Hilfiker D. Facing our mistakes. N Engl J Med. 1984;310:
118-122.
10. Leape LL. Error in medicine. JAMA. 1994;272:1851-1857.
11. Hall v. Hilbun, 466 So.2d 856 (Miss. 1985).
12. Kern SI. You continue to face exposure if you apologize. http://medicaleconomics.modernmedicine.com/medical-economics/news/modernmedicine/modern-medicine-now/you-continue-face-exposure-if-you-apologiz. Published September 24, 2010. Accessed October 1, 2013.
13. Ho B, Liu E. Does sorry work? The impact of apology laws on medical malpractice. J Risk Uncertain. 2011;43(2):141-167.
14. Fehr R, Gelfand MJ, Nag M. The road to forgiveness: a meta-analytic synthesis of its situational and dispositional correlates. Psychol Bull. 2010;136:894-914.
15. Robbennolt JK. Apologies and settlement. Court Review. 2009;45:90-97.
16. Saitta N, Hodge SD. Efficacy of a physician’s words of empathy: an overview of state apology laws. J Am Osteopath Assoc. 2012;112(5):302-306.
17. Wojcieszak D, Banja J, Houk C. The sorry works! coalition: making the case for full disclosure. Jt Comm J Qual Patient Saf. 2006;32(6):344-350.
18. National Conference of State Legislatures. Medical liability/Medical malpractice laws. http://www.ncsl.org/issues-research/banking/medical-liability-medical-malpractice-laws.aspx. Published August 15, 2011. Accessed October 4, 2013.
19. Conn Gen Stat Ann §52-184d(b).
20. Fla Stat §90.4026(2).
21. Ill Comp Stat §5/8-1901.
22. NC Gen Stat §8C-1, Rule 413.
23. Tex. Civ. Prac. & Rem. Code §18.061.
24. Ho B, Liu E. What’s an apology worth? Decomposing the effect of apologies on medical malpractice payments using state apology laws. J Empir Leg Stud. 2011;8:179-199.
25. Price M, Recupero PR. Risk management. In: Sharfstein SS, Dickerson FB, Oldham JM, eds. Textbook of hospital psychiatry. Arlington, VA: American Psychiatric Publishing, Inc.; 2009:411-412.
1. McCullough ME, Sandage SJ, Brown SW, et al. Interpersonal forgiving in close relationships: II. Theoretical elaboration and measurement. J Pers Soc Psychol. 1998;75:1586-1603.
2. O’Reilly KB. “I’m sorry”: why is that so hard for doctors to say? http://www.amednews.com/article/20100201/profession/302019937/4. Published February 1, 2010. Accessed September 30, 2013.
3. American Medical Association. AMA Code of Medical Ethics, Opinion 8.12 – Patient information. http://www.ama-assn.org//ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion812.page. Published June 1994. Accessed September 30, 2013.
4. Hickson GB, Pichert JW. Disclosure and apology. http://www.npsf.org/wp-content/uploads/2011/10/RG_SUPS_After_Mod1_Hickson.pdf. Accessed October 4, 2013.
5. Snyder L, American College of Physicians Ethics, Professionalism, and Human Rights Committee. American College of Physicians ethics manual: sixth edition. Ann Intern Med. 2012;156(1, pt 2):73-104.
6. ECRI Institute. Disclosure of unanticipated outcomes. In: Healthcare risk control Supplement A, Risk analysis. Plymouth Meeting, PA: ECRI; 2002.
7. Okimoto TG, Wenzel M, Hedrick K. Refusing to apologize can have psychological benefits (and we issue no mea culpa for this research finding). Eur J Soc Psychol. 2013;43:22-31.
8. Lazare A. On apology. New York, NY: Oxford University Press; 2004.
9. Hilfiker D. Facing our mistakes. N Engl J Med. 1984;310:
118-122.
10. Leape LL. Error in medicine. JAMA. 1994;272:1851-1857.
11. Hall v. Hilbun, 466 So.2d 856 (Miss. 1985).
12. Kern SI. You continue to face exposure if you apologize. http://medicaleconomics.modernmedicine.com/medical-economics/news/modernmedicine/modern-medicine-now/you-continue-face-exposure-if-you-apologiz. Published September 24, 2010. Accessed October 1, 2013.
13. Ho B, Liu E. Does sorry work? The impact of apology laws on medical malpractice. J Risk Uncertain. 2011;43(2):141-167.
14. Fehr R, Gelfand MJ, Nag M. The road to forgiveness: a meta-analytic synthesis of its situational and dispositional correlates. Psychol Bull. 2010;136:894-914.
15. Robbennolt JK. Apologies and settlement. Court Review. 2009;45:90-97.
16. Saitta N, Hodge SD. Efficacy of a physician’s words of empathy: an overview of state apology laws. J Am Osteopath Assoc. 2012;112(5):302-306.
17. Wojcieszak D, Banja J, Houk C. The sorry works! coalition: making the case for full disclosure. Jt Comm J Qual Patient Saf. 2006;32(6):344-350.
18. National Conference of State Legislatures. Medical liability/Medical malpractice laws. http://www.ncsl.org/issues-research/banking/medical-liability-medical-malpractice-laws.aspx. Published August 15, 2011. Accessed October 4, 2013.
19. Conn Gen Stat Ann §52-184d(b).
20. Fla Stat §90.4026(2).
21. Ill Comp Stat §5/8-1901.
22. NC Gen Stat §8C-1, Rule 413.
23. Tex. Civ. Prac. & Rem. Code §18.061.
24. Ho B, Liu E. What’s an apology worth? Decomposing the effect of apologies on medical malpractice payments using state apology laws. J Empir Leg Stud. 2011;8:179-199.
25. Price M, Recupero PR. Risk management. In: Sharfstein SS, Dickerson FB, Oldham JM, eds. Textbook of hospital psychiatry. Arlington, VA: American Psychiatric Publishing, Inc.; 2009:411-412.
Pre-apology consultation
Should you report a patient who misuses a prescription?
Dear Dr. Mossman:
My patient, Ms. X, returned to see me after she had spent 3 months in jail. When I accessed her medication history in our state’s prescription registry, I discovered that, during her incarceration, a local pharmacy continued to fill her prescription for clonazepam. After anxiously explaining that her roommate had filled the prescriptions, Ms. X pleaded with me not to tell anyone. Do I have to report this to legal authorities? If I do, will I be breaching confidentiality?
Submitted by Dr. L
Preserving the confidentiality of patient encounters is an ethical responsibility as old as the Hippocratic Oath,1 but protecting privacy is not an absolute duty. As psychiatrists familiar with the Tarasoff case2 know, clinical events sometimes create moral and legal obligations that outweigh our confidentiality obligations.
What Dr. L should do may hinge on specific details of Ms. X’s previous and current treatment, but in this article, we’ll examine some general issues that affect Dr. L’s choices. These include:
• reporting a past crime
• liability risks associated with violating confidentiality.
Monitoring controlled substances
Dr. L’s clinical situation probably would not have arisen 10 years ago because until recently, she would have had no easy way to learn that Ms. X’s prescription had been filled. In 2002, Congress responded to increasing concern about “epidemic” abuse of controlled substances—especially opioids—by authorizing state grants for prescription drug monitoring programs (PDMPs).3
PDMPs are internet-based registries that let physicians quickly find out when and where their patients have filled prescriptions for controlled substances (defined in the Table).4,5 As the rate of opioid-related deaths has risen,6 at least 43 states have initiated PDMPs; soon, all U.S. jurisdictions likely will have such programs.7 Data about the impact of PDMPs, although limited, suggest that PDMPs reduce “doctor shopping” and prescription drug abuse.8
The U.S. Department of Health and Human Services is promoting the development of electronic architecture standards to facilitate information exchange across jurisdictions,9 but states currently run their own PDMPs independently and have varying regulations about how physicians should use PDMPs.10 Excerpts from the rules used in Ohio’s prescription reporting system appear in the Box.11
Reporting past crimes
What Ms. X told Dr. L implies that someone—the patient, her roommate, or both—misused a prescription to obtain a controlled substance. Simple improper possession of a scheduled drug is a federal misdemeanor offense,12 and deception and conspiracy to obtain a scheduled drug are federal-level felonies.13 Such actions also violate state laws. Dr. L therefore knows that a crime has occurred.
Are doctors obligated or legally required to breach confidentiality and tell authorities about a patient’s past criminal acts? Writing several years ago, Appelbaum and Meisel14 and Goldman and Gutheil15 said the answer, in general, is “no.”
In recent years, state legislatures have modified criminal codes to encourage people to disclose their knowledge of certain crimes to police. For example, failures to report environmental offenses and financial misdealings have become criminal acts.16 A minority of states now punish failure to report other kinds of illegal behavior, but these laws focus mainly on violent crimes (often involving harm to vulnerable persons).17 Although Ohio has a law that obligates everyone to report knowledge of any felony, it makes exceptions when the information is learned during a customarily confidential relationship—including a physician’s treatment of a patient.18 Unless Dr. L herself has aided or concealed a crime (both illegal acts19), concerns about possible prosecution should not affect her decision to report what she has learned thus far.14
Deciding how to proceed
If Dr. L still feels inclined to do something about the misused prescription, what are her options? What clinical, legal, and moral obligations to act should she consider?
Obtain the facts. First, Dr. L should try to learn more about what happened. Jails are reluctant to give inmates benzodiazepines20; did Ms. X receive clonazepam while in jail? When and how did Ms. X learn about her roommate’s actions? Did Ms. X obtain previous prescriptions from Dr. L with the intention of letting her roommate use them? Answers to these questions can help Dr. L determine whether her patient participated in prescription misuse, an important factor in deciding what clinical or legal actions to take.
Should the patient take the lead? Learning more about the situation might suggest that Ms. X should report what has happened herself. If, for example, the roommate has coerced Ms. X to engage in illegal conduct, Dr. L might help Ms. X figure out how to tell police what has happened—preferably after Ms. X has obtained legal advice.14
Consider implications for treatment. Last, what Ms. X reveals might significantly alter her future interactions with Dr. L. This is particularly true if Dr. L concluded that Ms. X would likely divert drugs in the future, or that the patient had established her relationship with Dr. L for purposes of improperly obtaining drugs. Federal regulations require that doctors prescribe drugs only for “legitimate medical purposes,” and issuing prescriptions to a patient who is known to be delivering the drugs to others violates this law.22
Bottom Line
Growing concern about prescription drug misuse has led to nationwide implementation of systems for monitoring patients’ access to, and receipt of, controlled substances. Psychiatrists are expected to be more vigilant about patients’ use of scheduled drugs and, when they believe that a prescription has been misused, to take appropriate clinical or legal action.
Related Resources
- Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. www.whitehouse.gov/sites/default/files/ondcp/issues-content/ prescription-drugs/rx_abuse_plan.pdf.
- California Department of Alcohol and Drug Misuse. Preventing prescription drug misuse. www.prescriptiondrugmisuse.org.
- U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm.
Drug Brand Names
Clonazepam • Klonopin Hydrocodone/acetaminophen • Vicodin
Methylphenidate • Ritalin Hydromorphone • Dilaudid
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
2. Tarasoff v Regents of the University of California, 17 Cal.3d 425, 551 P.2d 334, 131 Cal Rptr 14 (Cal 1976).
3. PubLNo.107-177,115Stat748.
4. ControlledSubstancesAct,21USC§812(b)(2007).
5. Schedules of Controlled Substances, 21 CFR. § 1308.11– 1308.15 (2013).
6. Dowell D, Kunins HV, Farley TA. Opioid analgesics— risky drugs, not risky patients. JAMA. 2013;309: 2219-2220.
7. US Department of Justice. Harold Rogers Prescription Drug Monitoring Program FY 2013 Competitive Grant Announcement. Washington, DC: Bureau of Justice Assistance, Office of Justice Programs; 2013. OMB No. 1121-0329.
8. Worley J. Prescription drug monitoring programs, a response to doctor shopping: purpose, effectiveness, and directions for future research. Issues Ment Health Nurs. 2012;33:319-328.
9. PubLNo.112-144,126Stat993.
10. Finklea KM, Bagalman E, Sacco L. Prescription Drug Monitoring Programs. Washington, DC: Library of Congress, Congressional Research Service; 2013. Report No. R42593.
11. Ohio State Medical Association. 4731-11-11 Standards and procedures for review of Ohio Automated Rx Reporting System (OARRS). http://www.osma.org/files/pdf/sept- 2011-draft-4731-11-11-ph-of-n-ru-20110520-1541.pdf. Accessed August 5, 2013.
12. Prohibited Acts C, 21 USC §843(a)(3) (2007).
13. PenaltyforSimplePossession,21USC§844(a)(2007).
14. Appelbaum PS, Meisel A. Therapists’ obligations to report their patients’ criminal acts. Bull Am Acad Psychiatry Law. 1986;14(3):221-230.
15. Goldman MJ, Gutheil TG. The misperceived duty to report patients’ past crimes. Bull Am Acad Psychiatry Law. 1994; 22(3):407-410.
16. Thompson SG. The white-collar police force: “duty to report” statutes in criminal law theory. William Mary Bill Rights J. 2002;11(1):3-65.
17. Trombley B. No stitches for snitches: the need for a duty-to-report law in Arkansas. Univ Ark Little Rock Law J. 2012; 34:813-832.
18. OhioRevisedCode§2921.22.
19. Section2:Principals,18USC§2(a).
20. Reeves R. Guideline, education, and peer comparison to reduce prescriptions of benzodiazepines and low-dose quetiapine in prison. J Correct Health Care. 2012;18(1): 45-52.
21. Appelbaum PS. Suits against clinicians for warning of patients’ violence. Psychiatr Serv. 1996;47(7):683-684.
22. UnitedStatesvRosen,582F2d1032(5thCir1978).
23. State Medical Board of Ohio. Regarding the duty of a physician to report criminal behavior to law enforcement. http://www.med.ohio.gov/pdf/NEWS/Duty%20to%20Report_March%202013.pdf. Adopted March 2013. Accessed July 1, 2013.
24. Missouri Department of Health & Senior Services. Preventing Prescription Fraud. http://health.mo.gov/ safety/bndd/publications.php. Accessed July 1, 2013.
Dear Dr. Mossman:
My patient, Ms. X, returned to see me after she had spent 3 months in jail. When I accessed her medication history in our state’s prescription registry, I discovered that, during her incarceration, a local pharmacy continued to fill her prescription for clonazepam. After anxiously explaining that her roommate had filled the prescriptions, Ms. X pleaded with me not to tell anyone. Do I have to report this to legal authorities? If I do, will I be breaching confidentiality?
Submitted by Dr. L
Preserving the confidentiality of patient encounters is an ethical responsibility as old as the Hippocratic Oath,1 but protecting privacy is not an absolute duty. As psychiatrists familiar with the Tarasoff case2 know, clinical events sometimes create moral and legal obligations that outweigh our confidentiality obligations.
What Dr. L should do may hinge on specific details of Ms. X’s previous and current treatment, but in this article, we’ll examine some general issues that affect Dr. L’s choices. These include:
• reporting a past crime
• liability risks associated with violating confidentiality.
Monitoring controlled substances
Dr. L’s clinical situation probably would not have arisen 10 years ago because until recently, she would have had no easy way to learn that Ms. X’s prescription had been filled. In 2002, Congress responded to increasing concern about “epidemic” abuse of controlled substances—especially opioids—by authorizing state grants for prescription drug monitoring programs (PDMPs).3
PDMPs are internet-based registries that let physicians quickly find out when and where their patients have filled prescriptions for controlled substances (defined in the Table).4,5 As the rate of opioid-related deaths has risen,6 at least 43 states have initiated PDMPs; soon, all U.S. jurisdictions likely will have such programs.7 Data about the impact of PDMPs, although limited, suggest that PDMPs reduce “doctor shopping” and prescription drug abuse.8
The U.S. Department of Health and Human Services is promoting the development of electronic architecture standards to facilitate information exchange across jurisdictions,9 but states currently run their own PDMPs independently and have varying regulations about how physicians should use PDMPs.10 Excerpts from the rules used in Ohio’s prescription reporting system appear in the Box.11
Reporting past crimes
What Ms. X told Dr. L implies that someone—the patient, her roommate, or both—misused a prescription to obtain a controlled substance. Simple improper possession of a scheduled drug is a federal misdemeanor offense,12 and deception and conspiracy to obtain a scheduled drug are federal-level felonies.13 Such actions also violate state laws. Dr. L therefore knows that a crime has occurred.
Are doctors obligated or legally required to breach confidentiality and tell authorities about a patient’s past criminal acts? Writing several years ago, Appelbaum and Meisel14 and Goldman and Gutheil15 said the answer, in general, is “no.”
In recent years, state legislatures have modified criminal codes to encourage people to disclose their knowledge of certain crimes to police. For example, failures to report environmental offenses and financial misdealings have become criminal acts.16 A minority of states now punish failure to report other kinds of illegal behavior, but these laws focus mainly on violent crimes (often involving harm to vulnerable persons).17 Although Ohio has a law that obligates everyone to report knowledge of any felony, it makes exceptions when the information is learned during a customarily confidential relationship—including a physician’s treatment of a patient.18 Unless Dr. L herself has aided or concealed a crime (both illegal acts19), concerns about possible prosecution should not affect her decision to report what she has learned thus far.14
Deciding how to proceed
If Dr. L still feels inclined to do something about the misused prescription, what are her options? What clinical, legal, and moral obligations to act should she consider?
Obtain the facts. First, Dr. L should try to learn more about what happened. Jails are reluctant to give inmates benzodiazepines20; did Ms. X receive clonazepam while in jail? When and how did Ms. X learn about her roommate’s actions? Did Ms. X obtain previous prescriptions from Dr. L with the intention of letting her roommate use them? Answers to these questions can help Dr. L determine whether her patient participated in prescription misuse, an important factor in deciding what clinical or legal actions to take.
Should the patient take the lead? Learning more about the situation might suggest that Ms. X should report what has happened herself. If, for example, the roommate has coerced Ms. X to engage in illegal conduct, Dr. L might help Ms. X figure out how to tell police what has happened—preferably after Ms. X has obtained legal advice.14
Consider implications for treatment. Last, what Ms. X reveals might significantly alter her future interactions with Dr. L. This is particularly true if Dr. L concluded that Ms. X would likely divert drugs in the future, or that the patient had established her relationship with Dr. L for purposes of improperly obtaining drugs. Federal regulations require that doctors prescribe drugs only for “legitimate medical purposes,” and issuing prescriptions to a patient who is known to be delivering the drugs to others violates this law.22
Bottom Line
Growing concern about prescription drug misuse has led to nationwide implementation of systems for monitoring patients’ access to, and receipt of, controlled substances. Psychiatrists are expected to be more vigilant about patients’ use of scheduled drugs and, when they believe that a prescription has been misused, to take appropriate clinical or legal action.
Related Resources
- Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. www.whitehouse.gov/sites/default/files/ondcp/issues-content/ prescription-drugs/rx_abuse_plan.pdf.
- California Department of Alcohol and Drug Misuse. Preventing prescription drug misuse. www.prescriptiondrugmisuse.org.
- U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm.
Drug Brand Names
Clonazepam • Klonopin Hydrocodone/acetaminophen • Vicodin
Methylphenidate • Ritalin Hydromorphone • Dilaudid
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman:
My patient, Ms. X, returned to see me after she had spent 3 months in jail. When I accessed her medication history in our state’s prescription registry, I discovered that, during her incarceration, a local pharmacy continued to fill her prescription for clonazepam. After anxiously explaining that her roommate had filled the prescriptions, Ms. X pleaded with me not to tell anyone. Do I have to report this to legal authorities? If I do, will I be breaching confidentiality?
Submitted by Dr. L
Preserving the confidentiality of patient encounters is an ethical responsibility as old as the Hippocratic Oath,1 but protecting privacy is not an absolute duty. As psychiatrists familiar with the Tarasoff case2 know, clinical events sometimes create moral and legal obligations that outweigh our confidentiality obligations.
What Dr. L should do may hinge on specific details of Ms. X’s previous and current treatment, but in this article, we’ll examine some general issues that affect Dr. L’s choices. These include:
• reporting a past crime
• liability risks associated with violating confidentiality.
Monitoring controlled substances
Dr. L’s clinical situation probably would not have arisen 10 years ago because until recently, she would have had no easy way to learn that Ms. X’s prescription had been filled. In 2002, Congress responded to increasing concern about “epidemic” abuse of controlled substances—especially opioids—by authorizing state grants for prescription drug monitoring programs (PDMPs).3
PDMPs are internet-based registries that let physicians quickly find out when and where their patients have filled prescriptions for controlled substances (defined in the Table).4,5 As the rate of opioid-related deaths has risen,6 at least 43 states have initiated PDMPs; soon, all U.S. jurisdictions likely will have such programs.7 Data about the impact of PDMPs, although limited, suggest that PDMPs reduce “doctor shopping” and prescription drug abuse.8
The U.S. Department of Health and Human Services is promoting the development of electronic architecture standards to facilitate information exchange across jurisdictions,9 but states currently run their own PDMPs independently and have varying regulations about how physicians should use PDMPs.10 Excerpts from the rules used in Ohio’s prescription reporting system appear in the Box.11
Reporting past crimes
What Ms. X told Dr. L implies that someone—the patient, her roommate, or both—misused a prescription to obtain a controlled substance. Simple improper possession of a scheduled drug is a federal misdemeanor offense,12 and deception and conspiracy to obtain a scheduled drug are federal-level felonies.13 Such actions also violate state laws. Dr. L therefore knows that a crime has occurred.
Are doctors obligated or legally required to breach confidentiality and tell authorities about a patient’s past criminal acts? Writing several years ago, Appelbaum and Meisel14 and Goldman and Gutheil15 said the answer, in general, is “no.”
In recent years, state legislatures have modified criminal codes to encourage people to disclose their knowledge of certain crimes to police. For example, failures to report environmental offenses and financial misdealings have become criminal acts.16 A minority of states now punish failure to report other kinds of illegal behavior, but these laws focus mainly on violent crimes (often involving harm to vulnerable persons).17 Although Ohio has a law that obligates everyone to report knowledge of any felony, it makes exceptions when the information is learned during a customarily confidential relationship—including a physician’s treatment of a patient.18 Unless Dr. L herself has aided or concealed a crime (both illegal acts19), concerns about possible prosecution should not affect her decision to report what she has learned thus far.14
Deciding how to proceed
If Dr. L still feels inclined to do something about the misused prescription, what are her options? What clinical, legal, and moral obligations to act should she consider?
Obtain the facts. First, Dr. L should try to learn more about what happened. Jails are reluctant to give inmates benzodiazepines20; did Ms. X receive clonazepam while in jail? When and how did Ms. X learn about her roommate’s actions? Did Ms. X obtain previous prescriptions from Dr. L with the intention of letting her roommate use them? Answers to these questions can help Dr. L determine whether her patient participated in prescription misuse, an important factor in deciding what clinical or legal actions to take.
Should the patient take the lead? Learning more about the situation might suggest that Ms. X should report what has happened herself. If, for example, the roommate has coerced Ms. X to engage in illegal conduct, Dr. L might help Ms. X figure out how to tell police what has happened—preferably after Ms. X has obtained legal advice.14
Consider implications for treatment. Last, what Ms. X reveals might significantly alter her future interactions with Dr. L. This is particularly true if Dr. L concluded that Ms. X would likely divert drugs in the future, or that the patient had established her relationship with Dr. L for purposes of improperly obtaining drugs. Federal regulations require that doctors prescribe drugs only for “legitimate medical purposes,” and issuing prescriptions to a patient who is known to be delivering the drugs to others violates this law.22
Bottom Line
Growing concern about prescription drug misuse has led to nationwide implementation of systems for monitoring patients’ access to, and receipt of, controlled substances. Psychiatrists are expected to be more vigilant about patients’ use of scheduled drugs and, when they believe that a prescription has been misused, to take appropriate clinical or legal action.
Related Resources
- Office of National Drug Control Policy. Epidemic: responding to America’s prescription drug abuse crisis. www.whitehouse.gov/sites/default/files/ondcp/issues-content/ prescription-drugs/rx_abuse_plan.pdf.
- California Department of Alcohol and Drug Misuse. Preventing prescription drug misuse. www.prescriptiondrugmisuse.org.
- U.S. Food and Drug Administration. Combating misuse and abuse of prescription drugs: Q&A with Michael Klein, PhD. www.fda.gov/ForConsumers/ConsumerUpdates/ ucm220112.htm.
Drug Brand Names
Clonazepam • Klonopin Hydrocodone/acetaminophen • Vicodin
Methylphenidate • Ritalin Hydromorphone • Dilaudid
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
2. Tarasoff v Regents of the University of California, 17 Cal.3d 425, 551 P.2d 334, 131 Cal Rptr 14 (Cal 1976).
3. PubLNo.107-177,115Stat748.
4. ControlledSubstancesAct,21USC§812(b)(2007).
5. Schedules of Controlled Substances, 21 CFR. § 1308.11– 1308.15 (2013).
6. Dowell D, Kunins HV, Farley TA. Opioid analgesics— risky drugs, not risky patients. JAMA. 2013;309: 2219-2220.
7. US Department of Justice. Harold Rogers Prescription Drug Monitoring Program FY 2013 Competitive Grant Announcement. Washington, DC: Bureau of Justice Assistance, Office of Justice Programs; 2013. OMB No. 1121-0329.
8. Worley J. Prescription drug monitoring programs, a response to doctor shopping: purpose, effectiveness, and directions for future research. Issues Ment Health Nurs. 2012;33:319-328.
9. PubLNo.112-144,126Stat993.
10. Finklea KM, Bagalman E, Sacco L. Prescription Drug Monitoring Programs. Washington, DC: Library of Congress, Congressional Research Service; 2013. Report No. R42593.
11. Ohio State Medical Association. 4731-11-11 Standards and procedures for review of Ohio Automated Rx Reporting System (OARRS). http://www.osma.org/files/pdf/sept- 2011-draft-4731-11-11-ph-of-n-ru-20110520-1541.pdf. Accessed August 5, 2013.
12. Prohibited Acts C, 21 USC §843(a)(3) (2007).
13. PenaltyforSimplePossession,21USC§844(a)(2007).
14. Appelbaum PS, Meisel A. Therapists’ obligations to report their patients’ criminal acts. Bull Am Acad Psychiatry Law. 1986;14(3):221-230.
15. Goldman MJ, Gutheil TG. The misperceived duty to report patients’ past crimes. Bull Am Acad Psychiatry Law. 1994; 22(3):407-410.
16. Thompson SG. The white-collar police force: “duty to report” statutes in criminal law theory. William Mary Bill Rights J. 2002;11(1):3-65.
17. Trombley B. No stitches for snitches: the need for a duty-to-report law in Arkansas. Univ Ark Little Rock Law J. 2012; 34:813-832.
18. OhioRevisedCode§2921.22.
19. Section2:Principals,18USC§2(a).
20. Reeves R. Guideline, education, and peer comparison to reduce prescriptions of benzodiazepines and low-dose quetiapine in prison. J Correct Health Care. 2012;18(1): 45-52.
21. Appelbaum PS. Suits against clinicians for warning of patients’ violence. Psychiatr Serv. 1996;47(7):683-684.
22. UnitedStatesvRosen,582F2d1032(5thCir1978).
23. State Medical Board of Ohio. Regarding the duty of a physician to report criminal behavior to law enforcement. http://www.med.ohio.gov/pdf/NEWS/Duty%20to%20Report_March%202013.pdf. Adopted March 2013. Accessed July 1, 2013.
24. Missouri Department of Health & Senior Services. Preventing Prescription Fraud. http://health.mo.gov/ safety/bndd/publications.php. Accessed July 1, 2013.
1. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
2. Tarasoff v Regents of the University of California, 17 Cal.3d 425, 551 P.2d 334, 131 Cal Rptr 14 (Cal 1976).
3. PubLNo.107-177,115Stat748.
4. ControlledSubstancesAct,21USC§812(b)(2007).
5. Schedules of Controlled Substances, 21 CFR. § 1308.11– 1308.15 (2013).
6. Dowell D, Kunins HV, Farley TA. Opioid analgesics— risky drugs, not risky patients. JAMA. 2013;309: 2219-2220.
7. US Department of Justice. Harold Rogers Prescription Drug Monitoring Program FY 2013 Competitive Grant Announcement. Washington, DC: Bureau of Justice Assistance, Office of Justice Programs; 2013. OMB No. 1121-0329.
8. Worley J. Prescription drug monitoring programs, a response to doctor shopping: purpose, effectiveness, and directions for future research. Issues Ment Health Nurs. 2012;33:319-328.
9. PubLNo.112-144,126Stat993.
10. Finklea KM, Bagalman E, Sacco L. Prescription Drug Monitoring Programs. Washington, DC: Library of Congress, Congressional Research Service; 2013. Report No. R42593.
11. Ohio State Medical Association. 4731-11-11 Standards and procedures for review of Ohio Automated Rx Reporting System (OARRS). http://www.osma.org/files/pdf/sept- 2011-draft-4731-11-11-ph-of-n-ru-20110520-1541.pdf. Accessed August 5, 2013.
12. Prohibited Acts C, 21 USC §843(a)(3) (2007).
13. PenaltyforSimplePossession,21USC§844(a)(2007).
14. Appelbaum PS, Meisel A. Therapists’ obligations to report their patients’ criminal acts. Bull Am Acad Psychiatry Law. 1986;14(3):221-230.
15. Goldman MJ, Gutheil TG. The misperceived duty to report patients’ past crimes. Bull Am Acad Psychiatry Law. 1994; 22(3):407-410.
16. Thompson SG. The white-collar police force: “duty to report” statutes in criminal law theory. William Mary Bill Rights J. 2002;11(1):3-65.
17. Trombley B. No stitches for snitches: the need for a duty-to-report law in Arkansas. Univ Ark Little Rock Law J. 2012; 34:813-832.
18. OhioRevisedCode§2921.22.
19. Section2:Principals,18USC§2(a).
20. Reeves R. Guideline, education, and peer comparison to reduce prescriptions of benzodiazepines and low-dose quetiapine in prison. J Correct Health Care. 2012;18(1): 45-52.
21. Appelbaum PS. Suits against clinicians for warning of patients’ violence. Psychiatr Serv. 1996;47(7):683-684.
22. UnitedStatesvRosen,582F2d1032(5thCir1978).
23. State Medical Board of Ohio. Regarding the duty of a physician to report criminal behavior to law enforcement. http://www.med.ohio.gov/pdf/NEWS/Duty%20to%20Report_March%202013.pdf. Adopted March 2013. Accessed July 1, 2013.
24. Missouri Department of Health & Senior Services. Preventing Prescription Fraud. http://health.mo.gov/ safety/bndd/publications.php. Accessed July 1, 2013.
Respondeat superior: What are your responsibilities?
Dear Dr. Mossman:
In my residency program, we cover the psychiatric emergency room (ER) overnight, and we admit, discharge, and make treatment recommendations without calling the attending psychiatrists about every decision. But if something goes wrong—eg, a discharged patient later commits suicide—I’ve heard that the faculty psychiatrist may be held liable despite never having met the patient. Should we awaken our attendings to discuss every major treatment decision?
Submitted by “Dr. R”
Postgraduate medical training programs in all specialties let interns and residents make judgments and decisions outside the direct supervision of board-certified faculty members. Medical education cannot occur unless doctors learn to take independent responsibility for patients. But if poor decisions by physicians-in-training lead to bad outcomes, might their teachers and training institutions share the blame—and the legal liability for damages?
The answer is “yes.” To understand why, and to learn about how Dr. R’s residency program should address this possibility, we’ll cover:
• the theory of respondeat superior
• factors affecting potential vicarious liability
• how postgraduate training balances supervision needs with letting residents get real-world treatment experience.
Vicarious liability
In general, if Person A injures Person B, Person B may initiate a tort action against Person A to seek monetary compensation. If the injury occurred while Person A was working for Person C, then under a legal doctrine called respondeat superior (Latin for “let the master answer”), courts may allow Person B to sue Person C, too, even if Person C wasn’t present when the injury occurred and did nothing that harmed Person B directly.
Respondeat superior imposes vicarious liability on an employer for negligent acts by employees who are “performing work assigned by the employer or engaging in a course of conduct subject to the employer’s control.”1 The doctrine extends back to 17th-century English courts and originated under the theory that, during a servant’s employment, one may presume that the servant acted by his master’s authority.2
Modern authors state that the justification for imposing vicarious liability “is largely one of public or social policy under which it has been determined that, irrespective of fault, a party should be held to respond for the acts of another.”3 Employers usually have more resources to pay damages than their employees do,4 and “in hard fact, the reason for the employers’ liability is the damages are taken from a deep pocket.”5
Determining potential responsibility
In Dr. R’s scenario, an adverse event follows the actions of a psychiatry resident who is performing a training activity at a hospital ER. Whether an attorney acting on behalf of an injured client can bring a claim of respondeat superior against the hospital, the resident’s academic institution, or the attending psychiatrist will depend on the nature of the relationships among these parties. This often becomes a complex legal matter that involves examining the residency program’s educational arrangements, official training documents (eg, affiliation agreements between a university and a hospital), employment contracts, and supervisory policies. In addition, statutes and legal precedents governing vicarious liability vary from state to state. Although an initial malpractice filing may name several individuals and institutions as defendants, courts eventually must apply their jurisdictions’ rules governing vicarious liability to determine which parties can lawfully bear potential liability.
Some courts have held that a private hospital generally is not responsible for negligent actions by attending physicians because the hospital does not control patient care decisions and physicians are not the hospital’s employees.6-8 Physicians in training, however, usually are employees of hospitals or their training institutions. Residents and attending physicians in many psychiatry training programs work at hospitals where patients reasonably believe that the doctors function as part of the hospital’s larger service enterprise. In some jurisdictions, this makes the hospitals potentially liable for their doctors’ acts,9 even when the doctors, as public employees, may have statutory immunity from being sued as individuals.10
Reuter11 has suggested that other agency theories may allow a resident’s error to create liability for an attending physician or medical school. The resident may be viewed as a “borrowed servant” such that, although a hospital was the resident’s general employer, the attending physician still exercised sufficient control with respect to the faulty act in question. A medical school faculty physician also may be liable along with the hospital under a joint employment theory based upon the faculty member’s “right to control” how the resident cares for the attending’s patient.11
Taking into account recent cases and trends in public expectations, Kachalia and Studdert12 suggest that potential liability of attending physicians rests on 2 factors: whether the treatment context and structure of supervisory obligations establishes a patient-physician relationship between the attending physician and the injured patient, and whether the attending physician has provided adequate supervision. Details of these 2 factors appear in Table 1.12-14
Independence vs oversight
Potential malpractice liability is one of many factors that postgraduate psychiatry programs consider when titrating the amount and intensity of supervision against letting residents make independent decisions and take on clinical responsibility for patients. Patients deserve good care and protection from mistakes that inexperienced physicians may make. At the same time, society recognizes that educating future physicians requires allowing residents to get real-world experiences in evaluating and treating patients.
These ideas are expressed in the “Program Requirements” for psychiatry residencies promulgated by the Accreditation Council for Graduate Medical Education (ACGME).15 According to the ACGME, the “essential learning activity” that teaches physicians how to provide medical care is “interaction with patients under the guidance and supervision of faculty members” who let residents “exercise those skills with greater independence.”15
Psychiatry residencies must fashion learning experiences and supervisory schemes that give residents “graded and progressive responsibility” for providing care. Although each patient should have “an identifiable, appropriately-credentialed and privileged attending physician,” residents may provide substantial services under various levels of supervision described in Table 2.16
Deciding when and what kinds of patient care may be delegated to residents is the responsibility of residency program directors, who should base their judgments on explicit, prespecified criteria using information provided by supervising faculty members. Before letting first-year residents see patients on their own, psychiatry programs must determine that the residents can:
• take a history accurately
• do emergency psychiatric assessments
• present findings and data accurately to supervisors.
Physicians at all levels need to recognize when they should ask for help. The most important ACGME criterion for allowing a psychiatry resident to work under less stringent supervision is that the resident has demonstrated an “ability and willingness to ask for help when indicated.”16
Getting specifics
One way to respond Dr. R’s questions is to ask, “Do you know when you need help, and will you ask for it?” But her concerns deserve a more detailed (and more thoughtful) response that inquires about details of her training program and its specific educational experiences. Although it would be impossible to list everything to consider, some possible topics include:
• At what level of experience and training do residents assume this coverage responsibility?
• What kind of preparation do residents receive?
• What range of problems and conditions do the patients present?
• What level of clinical support is available on site—eg, experienced psychiatric nurses, other mental health staff, or other medical specialists?
• What has the program’s experience shown about residents’ actual readiness to handle these coverage duties?
• What guidelines have faculty members provided about when to call an attending physician or request a faculty member’s presence? Do these guidelines seem sound, given the above considerations?
Bottom Line
Psychiatry residents have supervisee relationships that create potential vicarious liability for institutions and faculty members. Residency training programs address these concerns by implementing adequate preparation for advanced responsibility, developing evaluative criteria and supervisory guidelines, and making sure that residents will ask for help when they need it.
Related Resources
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. South Med J. 2002;95(5):545-548.
- Winrow B, Winrow AR. Personal protection: vicarious liability as applied to the various business structures. J Midwifery Womens Health. 2008;53(2):146-149.
- Pozgar GD. Legal aspects of health care administration. 11th edition. Sudbury, MA: Jones & Bartlett Learning, LLC; 2012.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Restatement of the law of agency. 3rd ed. §7.07(2). Philadelphia, PA: American Law Institute; 2006.
2. Baty T. Vicarious liability: a short history of the liability of employers, principals, partners, associations and trade-union members. Oxford, England: Clarendon Press; 1916.
3. Dessauer v Memorial General Hosp, 628 P.2d 337 (N.M. 1981).
4. Firestone MH. Agency. In: Sandbar SS, Firestone MH, eds. Legal medicine. 7th ed. Philadelphia, PA: Mosby Elsevier; 2007:43-47.
5. Dobbs D, Keeton RE, Owen DG. Prosser and Keaton on torts. 5th ed. St. Paul, MN: West Publishing Co; 1984.
6. Austin v Litvak, 682 P.2d 41 (Colo. 1984).
7. Kirk v Michael Reese Hospital and Medical Center, 513 N.E.2d 387 (Ill. 1987).
8. Gregg v National Medical Health Care Services, Inc., 499 P.2d 925 (Ariz. App. 1985).
9. Adamski v Tacoma General Hospital, 579 P.2d 970 (Wash. App. 1978).
10. Johnson v LeBonheur Children’s Medical Center, 74 S.W.3d 338 (Tenn. 2002).
11. Reuter SR. Professional liability in postgraduate medical education. Who is liable for resident negligence? J Leg Med. 1994;15(4):485-531.
12. Kachalia A, Studdert DM. Professional liability issues in graduate medical education. JAMA. 2004;292(9):1051-1056.
13. Lownsbury v VanBuren, 762 N.E.2d 354 (Ohio 2002).
14. Sterling v Johns Hopkins Hospital, 802 A.2d 440 (Md Ct Spec App 2002).
15. Accreditation Council for Graduate Medical Education. Program and institutional guidelines. https://www.acgme.org/acgmeweb/tabid/147/ProgramandInstitutional Guidelines/MedicalAccreditation/Psychiatry.aspx. Accessed April 8, 2013.
16. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in psychiatry. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_07012007_u04122008.pdf. Published July 1, 2007. Accessed April 8, 2013.
Dear Dr. Mossman:
In my residency program, we cover the psychiatric emergency room (ER) overnight, and we admit, discharge, and make treatment recommendations without calling the attending psychiatrists about every decision. But if something goes wrong—eg, a discharged patient later commits suicide—I’ve heard that the faculty psychiatrist may be held liable despite never having met the patient. Should we awaken our attendings to discuss every major treatment decision?
Submitted by “Dr. R”
Postgraduate medical training programs in all specialties let interns and residents make judgments and decisions outside the direct supervision of board-certified faculty members. Medical education cannot occur unless doctors learn to take independent responsibility for patients. But if poor decisions by physicians-in-training lead to bad outcomes, might their teachers and training institutions share the blame—and the legal liability for damages?
The answer is “yes.” To understand why, and to learn about how Dr. R’s residency program should address this possibility, we’ll cover:
• the theory of respondeat superior
• factors affecting potential vicarious liability
• how postgraduate training balances supervision needs with letting residents get real-world treatment experience.
Vicarious liability
In general, if Person A injures Person B, Person B may initiate a tort action against Person A to seek monetary compensation. If the injury occurred while Person A was working for Person C, then under a legal doctrine called respondeat superior (Latin for “let the master answer”), courts may allow Person B to sue Person C, too, even if Person C wasn’t present when the injury occurred and did nothing that harmed Person B directly.
Respondeat superior imposes vicarious liability on an employer for negligent acts by employees who are “performing work assigned by the employer or engaging in a course of conduct subject to the employer’s control.”1 The doctrine extends back to 17th-century English courts and originated under the theory that, during a servant’s employment, one may presume that the servant acted by his master’s authority.2
Modern authors state that the justification for imposing vicarious liability “is largely one of public or social policy under which it has been determined that, irrespective of fault, a party should be held to respond for the acts of another.”3 Employers usually have more resources to pay damages than their employees do,4 and “in hard fact, the reason for the employers’ liability is the damages are taken from a deep pocket.”5
Determining potential responsibility
In Dr. R’s scenario, an adverse event follows the actions of a psychiatry resident who is performing a training activity at a hospital ER. Whether an attorney acting on behalf of an injured client can bring a claim of respondeat superior against the hospital, the resident’s academic institution, or the attending psychiatrist will depend on the nature of the relationships among these parties. This often becomes a complex legal matter that involves examining the residency program’s educational arrangements, official training documents (eg, affiliation agreements between a university and a hospital), employment contracts, and supervisory policies. In addition, statutes and legal precedents governing vicarious liability vary from state to state. Although an initial malpractice filing may name several individuals and institutions as defendants, courts eventually must apply their jurisdictions’ rules governing vicarious liability to determine which parties can lawfully bear potential liability.
Some courts have held that a private hospital generally is not responsible for negligent actions by attending physicians because the hospital does not control patient care decisions and physicians are not the hospital’s employees.6-8 Physicians in training, however, usually are employees of hospitals or their training institutions. Residents and attending physicians in many psychiatry training programs work at hospitals where patients reasonably believe that the doctors function as part of the hospital’s larger service enterprise. In some jurisdictions, this makes the hospitals potentially liable for their doctors’ acts,9 even when the doctors, as public employees, may have statutory immunity from being sued as individuals.10
Reuter11 has suggested that other agency theories may allow a resident’s error to create liability for an attending physician or medical school. The resident may be viewed as a “borrowed servant” such that, although a hospital was the resident’s general employer, the attending physician still exercised sufficient control with respect to the faulty act in question. A medical school faculty physician also may be liable along with the hospital under a joint employment theory based upon the faculty member’s “right to control” how the resident cares for the attending’s patient.11
Taking into account recent cases and trends in public expectations, Kachalia and Studdert12 suggest that potential liability of attending physicians rests on 2 factors: whether the treatment context and structure of supervisory obligations establishes a patient-physician relationship between the attending physician and the injured patient, and whether the attending physician has provided adequate supervision. Details of these 2 factors appear in Table 1.12-14
Independence vs oversight
Potential malpractice liability is one of many factors that postgraduate psychiatry programs consider when titrating the amount and intensity of supervision against letting residents make independent decisions and take on clinical responsibility for patients. Patients deserve good care and protection from mistakes that inexperienced physicians may make. At the same time, society recognizes that educating future physicians requires allowing residents to get real-world experiences in evaluating and treating patients.
These ideas are expressed in the “Program Requirements” for psychiatry residencies promulgated by the Accreditation Council for Graduate Medical Education (ACGME).15 According to the ACGME, the “essential learning activity” that teaches physicians how to provide medical care is “interaction with patients under the guidance and supervision of faculty members” who let residents “exercise those skills with greater independence.”15
Psychiatry residencies must fashion learning experiences and supervisory schemes that give residents “graded and progressive responsibility” for providing care. Although each patient should have “an identifiable, appropriately-credentialed and privileged attending physician,” residents may provide substantial services under various levels of supervision described in Table 2.16
Deciding when and what kinds of patient care may be delegated to residents is the responsibility of residency program directors, who should base their judgments on explicit, prespecified criteria using information provided by supervising faculty members. Before letting first-year residents see patients on their own, psychiatry programs must determine that the residents can:
• take a history accurately
• do emergency psychiatric assessments
• present findings and data accurately to supervisors.
Physicians at all levels need to recognize when they should ask for help. The most important ACGME criterion for allowing a psychiatry resident to work under less stringent supervision is that the resident has demonstrated an “ability and willingness to ask for help when indicated.”16
Getting specifics
One way to respond Dr. R’s questions is to ask, “Do you know when you need help, and will you ask for it?” But her concerns deserve a more detailed (and more thoughtful) response that inquires about details of her training program and its specific educational experiences. Although it would be impossible to list everything to consider, some possible topics include:
• At what level of experience and training do residents assume this coverage responsibility?
• What kind of preparation do residents receive?
• What range of problems and conditions do the patients present?
• What level of clinical support is available on site—eg, experienced psychiatric nurses, other mental health staff, or other medical specialists?
• What has the program’s experience shown about residents’ actual readiness to handle these coverage duties?
• What guidelines have faculty members provided about when to call an attending physician or request a faculty member’s presence? Do these guidelines seem sound, given the above considerations?
Bottom Line
Psychiatry residents have supervisee relationships that create potential vicarious liability for institutions and faculty members. Residency training programs address these concerns by implementing adequate preparation for advanced responsibility, developing evaluative criteria and supervisory guidelines, and making sure that residents will ask for help when they need it.
Related Resources
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. South Med J. 2002;95(5):545-548.
- Winrow B, Winrow AR. Personal protection: vicarious liability as applied to the various business structures. J Midwifery Womens Health. 2008;53(2):146-149.
- Pozgar GD. Legal aspects of health care administration. 11th edition. Sudbury, MA: Jones & Bartlett Learning, LLC; 2012.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Restatement of the law of agency. 3rd ed. §7.07(2). Philadelphia, PA: American Law Institute; 2006.
2. Baty T. Vicarious liability: a short history of the liability of employers, principals, partners, associations and trade-union members. Oxford, England: Clarendon Press; 1916.
3. Dessauer v Memorial General Hosp, 628 P.2d 337 (N.M. 1981).
4. Firestone MH. Agency. In: Sandbar SS, Firestone MH, eds. Legal medicine. 7th ed. Philadelphia, PA: Mosby Elsevier; 2007:43-47.
5. Dobbs D, Keeton RE, Owen DG. Prosser and Keaton on torts. 5th ed. St. Paul, MN: West Publishing Co; 1984.
6. Austin v Litvak, 682 P.2d 41 (Colo. 1984).
7. Kirk v Michael Reese Hospital and Medical Center, 513 N.E.2d 387 (Ill. 1987).
8. Gregg v National Medical Health Care Services, Inc., 499 P.2d 925 (Ariz. App. 1985).
9. Adamski v Tacoma General Hospital, 579 P.2d 970 (Wash. App. 1978).
10. Johnson v LeBonheur Children’s Medical Center, 74 S.W.3d 338 (Tenn. 2002).
11. Reuter SR. Professional liability in postgraduate medical education. Who is liable for resident negligence? J Leg Med. 1994;15(4):485-531.
12. Kachalia A, Studdert DM. Professional liability issues in graduate medical education. JAMA. 2004;292(9):1051-1056.
13. Lownsbury v VanBuren, 762 N.E.2d 354 (Ohio 2002).
14. Sterling v Johns Hopkins Hospital, 802 A.2d 440 (Md Ct Spec App 2002).
15. Accreditation Council for Graduate Medical Education. Program and institutional guidelines. https://www.acgme.org/acgmeweb/tabid/147/ProgramandInstitutional Guidelines/MedicalAccreditation/Psychiatry.aspx. Accessed April 8, 2013.
16. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in psychiatry. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_07012007_u04122008.pdf. Published July 1, 2007. Accessed April 8, 2013.
Dear Dr. Mossman:
In my residency program, we cover the psychiatric emergency room (ER) overnight, and we admit, discharge, and make treatment recommendations without calling the attending psychiatrists about every decision. But if something goes wrong—eg, a discharged patient later commits suicide—I’ve heard that the faculty psychiatrist may be held liable despite never having met the patient. Should we awaken our attendings to discuss every major treatment decision?
Submitted by “Dr. R”
Postgraduate medical training programs in all specialties let interns and residents make judgments and decisions outside the direct supervision of board-certified faculty members. Medical education cannot occur unless doctors learn to take independent responsibility for patients. But if poor decisions by physicians-in-training lead to bad outcomes, might their teachers and training institutions share the blame—and the legal liability for damages?
The answer is “yes.” To understand why, and to learn about how Dr. R’s residency program should address this possibility, we’ll cover:
• the theory of respondeat superior
• factors affecting potential vicarious liability
• how postgraduate training balances supervision needs with letting residents get real-world treatment experience.
Vicarious liability
In general, if Person A injures Person B, Person B may initiate a tort action against Person A to seek monetary compensation. If the injury occurred while Person A was working for Person C, then under a legal doctrine called respondeat superior (Latin for “let the master answer”), courts may allow Person B to sue Person C, too, even if Person C wasn’t present when the injury occurred and did nothing that harmed Person B directly.
Respondeat superior imposes vicarious liability on an employer for negligent acts by employees who are “performing work assigned by the employer or engaging in a course of conduct subject to the employer’s control.”1 The doctrine extends back to 17th-century English courts and originated under the theory that, during a servant’s employment, one may presume that the servant acted by his master’s authority.2
Modern authors state that the justification for imposing vicarious liability “is largely one of public or social policy under which it has been determined that, irrespective of fault, a party should be held to respond for the acts of another.”3 Employers usually have more resources to pay damages than their employees do,4 and “in hard fact, the reason for the employers’ liability is the damages are taken from a deep pocket.”5
Determining potential responsibility
In Dr. R’s scenario, an adverse event follows the actions of a psychiatry resident who is performing a training activity at a hospital ER. Whether an attorney acting on behalf of an injured client can bring a claim of respondeat superior against the hospital, the resident’s academic institution, or the attending psychiatrist will depend on the nature of the relationships among these parties. This often becomes a complex legal matter that involves examining the residency program’s educational arrangements, official training documents (eg, affiliation agreements between a university and a hospital), employment contracts, and supervisory policies. In addition, statutes and legal precedents governing vicarious liability vary from state to state. Although an initial malpractice filing may name several individuals and institutions as defendants, courts eventually must apply their jurisdictions’ rules governing vicarious liability to determine which parties can lawfully bear potential liability.
Some courts have held that a private hospital generally is not responsible for negligent actions by attending physicians because the hospital does not control patient care decisions and physicians are not the hospital’s employees.6-8 Physicians in training, however, usually are employees of hospitals or their training institutions. Residents and attending physicians in many psychiatry training programs work at hospitals where patients reasonably believe that the doctors function as part of the hospital’s larger service enterprise. In some jurisdictions, this makes the hospitals potentially liable for their doctors’ acts,9 even when the doctors, as public employees, may have statutory immunity from being sued as individuals.10
Reuter11 has suggested that other agency theories may allow a resident’s error to create liability for an attending physician or medical school. The resident may be viewed as a “borrowed servant” such that, although a hospital was the resident’s general employer, the attending physician still exercised sufficient control with respect to the faulty act in question. A medical school faculty physician also may be liable along with the hospital under a joint employment theory based upon the faculty member’s “right to control” how the resident cares for the attending’s patient.11
Taking into account recent cases and trends in public expectations, Kachalia and Studdert12 suggest that potential liability of attending physicians rests on 2 factors: whether the treatment context and structure of supervisory obligations establishes a patient-physician relationship between the attending physician and the injured patient, and whether the attending physician has provided adequate supervision. Details of these 2 factors appear in Table 1.12-14
Independence vs oversight
Potential malpractice liability is one of many factors that postgraduate psychiatry programs consider when titrating the amount and intensity of supervision against letting residents make independent decisions and take on clinical responsibility for patients. Patients deserve good care and protection from mistakes that inexperienced physicians may make. At the same time, society recognizes that educating future physicians requires allowing residents to get real-world experiences in evaluating and treating patients.
These ideas are expressed in the “Program Requirements” for psychiatry residencies promulgated by the Accreditation Council for Graduate Medical Education (ACGME).15 According to the ACGME, the “essential learning activity” that teaches physicians how to provide medical care is “interaction with patients under the guidance and supervision of faculty members” who let residents “exercise those skills with greater independence.”15
Psychiatry residencies must fashion learning experiences and supervisory schemes that give residents “graded and progressive responsibility” for providing care. Although each patient should have “an identifiable, appropriately-credentialed and privileged attending physician,” residents may provide substantial services under various levels of supervision described in Table 2.16
Deciding when and what kinds of patient care may be delegated to residents is the responsibility of residency program directors, who should base their judgments on explicit, prespecified criteria using information provided by supervising faculty members. Before letting first-year residents see patients on their own, psychiatry programs must determine that the residents can:
• take a history accurately
• do emergency psychiatric assessments
• present findings and data accurately to supervisors.
Physicians at all levels need to recognize when they should ask for help. The most important ACGME criterion for allowing a psychiatry resident to work under less stringent supervision is that the resident has demonstrated an “ability and willingness to ask for help when indicated.”16
Getting specifics
One way to respond Dr. R’s questions is to ask, “Do you know when you need help, and will you ask for it?” But her concerns deserve a more detailed (and more thoughtful) response that inquires about details of her training program and its specific educational experiences. Although it would be impossible to list everything to consider, some possible topics include:
• At what level of experience and training do residents assume this coverage responsibility?
• What kind of preparation do residents receive?
• What range of problems and conditions do the patients present?
• What level of clinical support is available on site—eg, experienced psychiatric nurses, other mental health staff, or other medical specialists?
• What has the program’s experience shown about residents’ actual readiness to handle these coverage duties?
• What guidelines have faculty members provided about when to call an attending physician or request a faculty member’s presence? Do these guidelines seem sound, given the above considerations?
Bottom Line
Psychiatry residents have supervisee relationships that create potential vicarious liability for institutions and faculty members. Residency training programs address these concerns by implementing adequate preparation for advanced responsibility, developing evaluative criteria and supervisory guidelines, and making sure that residents will ask for help when they need it.
Related Resources
- Regan JJ, Regan WM. Medical malpractice and respondeat superior. South Med J. 2002;95(5):545-548.
- Winrow B, Winrow AR. Personal protection: vicarious liability as applied to the various business structures. J Midwifery Womens Health. 2008;53(2):146-149.
- Pozgar GD. Legal aspects of health care administration. 11th edition. Sudbury, MA: Jones & Bartlett Learning, LLC; 2012.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
References
1. Restatement of the law of agency. 3rd ed. §7.07(2). Philadelphia, PA: American Law Institute; 2006.
2. Baty T. Vicarious liability: a short history of the liability of employers, principals, partners, associations and trade-union members. Oxford, England: Clarendon Press; 1916.
3. Dessauer v Memorial General Hosp, 628 P.2d 337 (N.M. 1981).
4. Firestone MH. Agency. In: Sandbar SS, Firestone MH, eds. Legal medicine. 7th ed. Philadelphia, PA: Mosby Elsevier; 2007:43-47.
5. Dobbs D, Keeton RE, Owen DG. Prosser and Keaton on torts. 5th ed. St. Paul, MN: West Publishing Co; 1984.
6. Austin v Litvak, 682 P.2d 41 (Colo. 1984).
7. Kirk v Michael Reese Hospital and Medical Center, 513 N.E.2d 387 (Ill. 1987).
8. Gregg v National Medical Health Care Services, Inc., 499 P.2d 925 (Ariz. App. 1985).
9. Adamski v Tacoma General Hospital, 579 P.2d 970 (Wash. App. 1978).
10. Johnson v LeBonheur Children’s Medical Center, 74 S.W.3d 338 (Tenn. 2002).
11. Reuter SR. Professional liability in postgraduate medical education. Who is liable for resident negligence? J Leg Med. 1994;15(4):485-531.
12. Kachalia A, Studdert DM. Professional liability issues in graduate medical education. JAMA. 2004;292(9):1051-1056.
13. Lownsbury v VanBuren, 762 N.E.2d 354 (Ohio 2002).
14. Sterling v Johns Hopkins Hospital, 802 A.2d 440 (Md Ct Spec App 2002).
15. Accreditation Council for Graduate Medical Education. Program and institutional guidelines. https://www.acgme.org/acgmeweb/tabid/147/ProgramandInstitutional Guidelines/MedicalAccreditation/Psychiatry.aspx. Accessed April 8, 2013.
16. Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in psychiatry. https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/400_psychiatry_07012007_u04122008.pdf. Published July 1, 2007. Accessed April 8, 2013.