User login
Natriuretic Peptide Screening for Primary Prevention or Early Detection of Heart Failure: A Pharmacist-Driven Team-Based Approach
Heart failure (HF) is one of the leading causes of hospitalizations and the most expensive Medicare diagnosis. Its prevalence continues to rise with a projected increase of 46% from 2012 to 2030 resulting in > 8 million people aged ≥ 18 years with HF in the United States. Despite improvements in therapy, mortality remains unacceptably high with a 50% mortality rate within 5 years. Early detection strategies are needed to identify patients at risk of developing HF to delay the disease course and improve survival.1,2
Emerging data indicates that natriuretic peptide biomarker-based screening using B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP) and early intervention for patients at risk of HF could prevent development of left ventricular dysfunction or new-onset HF.3-5 The 2013 St. Vincent’s Screening to Prevent Heart Failure (STOP-HF) trial is the largest study to date to evaluate BNP as a screening tool for patients at risk for HF.4 Patients at risk of HF who did not have established left ventricular systolic dysfunction or symptomatic HF were assigned randomly to usual primary care or BNP screening. Patients with BNP levels ≥ 50 pg/mL underwent echocardiogram and were referred to a cardiovascular specialty service for management. The cardiovascular specialty clinic included a team of registered nurses, nurse practitioners, pharmacists, dieticians, palliative care specialists, and cardiologists. Individuals in the intervention group showed increased renin-angiotensin system (RAS) inhibitor use at follow-up (control, 49.6%; intervention, 59.6%; P = .01). All patients received coaching by a nurse who emphasized individual risk, importance of medication adherence, and healthy lifestyle behaviors. After a mean follow-up of 4.2 years, 59 of 677 participants (8.7%) in the control group and 37 of 697 (5.3%) in the intervention group (odds ratio [OR], 0.55; 95% CI, 0.37 to 0.82; P = .003) met the primary end point of left ventricular dysfunction with or without HF. BNP-based screening in conjunction with collaborative care reduced rates of left ventricular dysfunction and HF.
In the 2013 PONTIAC trial, patients with type 2 diabetes mellitus (T2DM) without cardiac disease but with NT-proBNP levels > 125 pg/mL were randomized to usual diabetes care or intensified care at a cardiac outpatient clinic for initiation and increase of RAS inhibitors and β blockers.5 After 2 years, patients randomized to the intensified care group showed a 65% risk reduction of the primary endpoint of hospitalization or death from cardiac disease (P = .04).
Based on this evidence, the 2017 focused update of the American College of Cardiology (ACC)/American Heart Association (AHA)/Heart Failure Society of America (HFSA) guideline for managing HF added a IIa recommendation for natriuretic peptide biomarker screening in those at risk of developing HF.6 The guideline recommends biomarker screening in conjunction with team-based care, including a cardiovascular specialist, and guideline-directed management and therapy to prevent development of left ventricular dysfunction or new-onset HF.
Although ordering a natriuretic peptide biomarker laboratory test is straightforward, the variability of team-based care across institutions and health systems makes it difficult to standardize screening and interventions for patients at risk for HF. We developed and piloted a process using clinical pharmacists in primary care for natriuretic peptide biomarker screening and risk factor reduction within the established patient aligned care team (PACT) framework at a US Department of Veterans Affairs (VA) medical center. In this paper, we describe our implementation process including descriptive preliminary outcomes.
Methods
The PACT team-based approach in primary care clinics is similar to the patient-centered medical home framework. A PACT includes the veteran patient and an interdisciplinary team of health professionals composed of their primary care practitioner (PCP), registered nurse care manager, clinical pharmacist, and other clinical and administrative staff. The PACT clinical pharmacist has prescriptive authority within a scope of practice to provide postdiagnostic chronic disease state management including management of T2DM, hypertension, HF, chronic obstructive pulmonary disease, anticoagulation, tobacco cessation, and atherosclerotic cardiovascular disease (ASCVD) risk reduction. Clinical pharmacists can prescribe and adjust medications and order laboratory tests.
Our institution, Clement J. Zablocki VA Medical Center (CJZVAMC) in Milwaukee, Wisconsin, has a specialty HF clinic that primarily manages ACC/AHA Stage C HF patients. The HF clinic uses a team-based approach to collaborate and coordinate care for the veteran. The HF team is comprised of cardiology specialists, registered nurses, clinical pharmacists, dietitians, and administrative staff. Two PACT clinical pharmacists also staff the HF clinic at CJZVAMC and work collaboratively to initiate, adjust, and optimize veterans’ HF medication regimens.
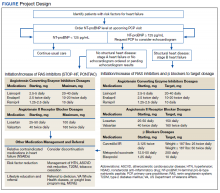
Two primary care PACT panels were selected for this project. Before implementation, a pharmacy resident and 3 PACT clinical pharmacists (2 of whom also staff the HF clinic) met with a HF cardiology specialist and 2 PACT PCPs to finalize the team-based process and workflow. PCPs were presented with the evidence-based background, purpose, and project design, which included patient identification, NT-proBNP laboratory test ordering, medication adjustment schedules, and protocol for ordering echocardiograms (Figure). Templated notes were created to allow for consistent documentation in patients’ electronic health record. A telephone script also was written for the initial telephone call to patients to explain in patient-friendly terms the implications of an elevated NT-proBNP level, the echocardiogram procedure, and recommendations for risk reduction.
Patient Selection
Patients aged ≥ 18 years with hypertension, taking antihypertensive medication for ≥ 1 month, or diagnosed with T2DM for ≥ 6 months were included. Using the parameters provided in the STOP-HF trial, patients with evidence or history of left ventricular dysfunction, defined as a left ventricular ejection fraction (EF) < 50% or an E/e’ ratio > 15 in the setting of normal EF, or symptomatic HF were excluded. Patients with a diagnosis causing life expectancy < 1 year were excluded, which was determined based on review of the patient’s chart or discussion with the PCP.
A clinical pharmacist screened patients with an upcoming PCP appointment between September 2019 and January 2020 for eligibility. For patients who met criteria, the clinical pharmacist ordered a NT-proBNP laboratory test to their already scheduled tests and entered a templated note into the patient’s chart to alert the PCP of the test. NT-proBNP was used rather than BNP because it was the natriuretic peptide laboratory test available at CJZVAMC during this time. Patients with NT-proBNP < 125 pg/mL received usual care from their PCPs. Patients with NT-proBNP ≥ 125 pg/mL received a follow-up phone call from a clinical pharmacist to discuss the laboratory test result with recommendations for initiation or increase of RAS inhibitors and an echocardiogram. If the patient agreed to an echocardiogram, the PCP was notified to order the test. For patients aged > 80 years with elevated NT-proBNP, risk vs benefit and patient-specific goals of care were discussed with the PCP. For patients whose echocardiograms revealed left ventricular dysfunction, initiation or adjustment of β blockers was considered. During RAS inhibitor increase, the clinical pharmacists provided a review of the patient’s risk factors and optimized management of hypertension, T2DM, ASCVD risk reduction, oral nonsteroidal anti-inflammatory drug (NSAID) reduction, and tobacco cessation.
Outcome Measures
Outcome measures included the percentage of patients who met inclusion/exclusion criteria and had an elevated NT-proBNP level, percent change in RAS inhibitor prescriptions and optimized dosing after intervention, frequency of left ventricular dysfunction visualized with echocardiograms, and quantification of pharmacist interventions in disease state management. Descriptive statistics were used to analyze demographic data, RAS inhibitors prescriptions before and after intervention, echocardiogram results, pharmacist recommendations, and acceptance rates of disease state management.
Results
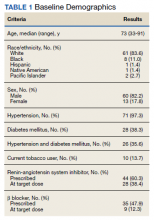
Between September 2019 and January 2020, 570 patients from 2 PACT teams were screened. Of the 570 patients, 246 met inclusion criteria with upcoming appointments. Of these, 24 were excluded, 10 for EF < 50%, 13 for E/e’ > 15 in setting of normal EF, and 1 for hypertension diagnosis without an antihypertensive regimen or elevated blood pressure. The remaining 222 patients had an NT-proBNP level ordered and drawn and 73 (32.9%) patients had an NT-proBNP ≥ 125 pg/mL. Baseline characteristics are described in Table 1.
Data was collected through March 2020 (due to COVID-19) found that among the 73 patients with elevated NT-proBNP: 14 had an echocardiogram within the past year without evidence of left ventricular dysfunction; 39 had echocardiograms ordered; and 19 had echocardiograms completed by March 2020. Among the 19 echocardiograms, 16 (84%) showed no evidence of left ventricular dysfunction, 2 (11%) revealed mildly reduced EF (40% to 50%), and 1 (5%) revealed a reduced EF (< 40%). These patients were identified early in the disease course before symptom onset and received intervention with RAS inhibitors and disease state management.
Patients prescribed RAS inhibitors increased from 44 to 50. The number of patients who were able to have their RAS inhibitor dosage adjusted increased from 28 to 31. For the 3 patients with mildly reduced or reduced EF, management with β blockers was based on RAS inhibitor adjustment toleration. One patient with mildly reduced EF was switched from metoprolol tartrate to metoprolol succinate.
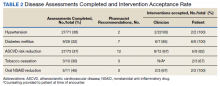
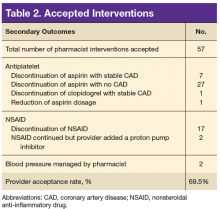
Clinical pharmacists completed disease state assessments to optimize management of hypertension, T2DM, ASCVD risk reduction, oral NSAID reduction, and tobacco cessation (Table 2). Interventions clinical pharmacists recommended for hypertension, in addition to RAS inhibitor management, included initiation and adjustment of amlodipine. For T2DM, interventions included initiation of metformin and initiation or adjustment of empagliflozin. For ASCVD risk reduction, interventions included starting a statin or adjusting statin therapies to appropriate intensities based on clinical ASCVD 10-year risk. Tobacco cessation interventions included pharmacotherapies, counseling, and education with written materials. Pharmacists counseled patients to minimize or eliminate NSAID use and, when appropriate, discontinued active oral NSAID prescriptions.
Discussion
We included patients diagnosed with T2DM and hypertension for several reasons. Most patients (62%) studied in the STOP-HF trial were diagnosed with hypertension. Also, T2DM represented the patient population enrolled in the PONTIAC trial. Guidance from the European Society of Cardiology recommends use of natriuretic peptides in high-risk populations, such as patients with DM and hypertension, to help target initiation of preventive measures.7 Lastly, T2DM and hypertension patients were easily identified using population management software available at the VA.
The percentage of patients in this project with risk factors for HF and an elevated NT-proBNP were similar to the elevated levels described in the STOP-HF trial. In our project, 32.9% of patients had elevated NT-proBNP levels, similar to the 41.6% of patients in STOP-HF. Among the completed echocardiograms, 16% revealed mildly reduced or reduced EF. These patients were identified early in the disease course before symptom onset and received intervention with RAS inhibitors and disease state management.
In addition to early identification of reduced EF, this project allowed a targeted approach to identifying patients for risk factor reduction. Between the 2 PACT teams, 246 patients with T2DM and/or hypertension were seen from September 2019 to January 2020. By using natriuretic peptide screening, the clinical pharmacists were able to prioritize and focus risk factor management on patients at higher risk. Pharmacists were then able to intervene for all risk factors assessed: hypertension, T2DM, ASCVD risk reduction, NSAID use reduction, and tobacco cessation.
During the implementation period, VA criteria of use of the angiotensin receptor-neprilysin inhibitor, sacubitril/valsartan, was restricted to VA cardiology. For patients with reduced EF, it was up to the PCP’s discretion to consult cardiology for further follow-up. In November 2020, the VA removed the restriction to cardiology and PCPs were able to order sacubitril/valsartan. Although not included in the Figure at the time of project implementation, the clinical pharmacist could now transition a patient with reduced EF from a RAS inhibitor to sacubitril/valsartan and adjust to target dosages.
Clinical pharmacists involved in this project had established working relationships with each of the PACT members before project initiation. The PACT employed the clinical pharmacists regularly for chronic disease state management. This facilitated adoption of the natriuretic peptide screening process and PCP buy-in and support. The PCPs agreed to discuss adding a NT-proBNP laboratory test with the patient, when possible, during their in-person appointment and informed the patient that a pharmacist would call if the result was elevated. This warm hand-off facilitated the patient’s reception to the clinical pharmacists’ recommendations after an elevated NT-proBNP result. We also reported PCPs’ high acceptance rate of pharmacist recommendations and interventions for disease state management. These high acceptance rates reflect the established working relationships between clinical pharmacists and the PACT.
Development of templated notes, medication adjustment schedules, and telephone script allowed for consistent implementation into the PACT panels. This process could be duplicated and adopted into other PACTs who want to use a clinical pharmacist to facilitate natriuretic peptide screening and risk factor reduction. The findings from this project can be extrapolated to other team-based care such as the patient-centered medical home model because these programs exhibit many similarities. Both health care models centralize patient care and use interdisciplinary care teams to promote continuity, care coordination, and access to achieve optimized patient outcomes.
Cost was an important factor to consider when implementing this project. With an increase in prescriptions and elective, outpatient echocardiograms, higher outpatient cost is expected. A cost-effectiveness analysis in the STOP-HF trial found an overall cost benefit by reducing the number of patients diagnosed with left ventricular dysfunction or HF and emergency hospitalizations for cardiac events in those who received collaborative care after natriuretic peptide testing.8 These cost savings offset increased outpatient costs.
Limitations
Participants were identified initially through a computer-generated list of patients with hypertension or T2DM without a HF diagnosis documented in their problem list. This problem list is manually updated by PCPs. Although we reviewed records for exclusion criteria, eligible patients might have been excluded. The use and interpretation of an NT-proBNP level is not specific to cardiac disease. Elevations can be seen with increased age, kidney dysfunction, and pulmonary disease. Additionally, an NT-proBNP level might be falsely low in patients who are overweight or obese. Because of the relatively short period of time, we could not analyze associations with HF diagnosis or progression, hospitalizations due to HF, or mortality. Regarding external validity, because of the pre-established interdisciplinary clinic settings and VA pharmacists’ scope of practice with prescriptive authority, implementing this project might have been better received by PCPs and allowed for higher acceptance rates of pharmacist interventions at the VA compared with a community setting.
Conclusions
The ACC/AHA/HFSA guidelines recommended use of natriuretic peptide biomarker screening in conjunction with team-based care for those at risk of developing HF. We describe our process for implementing team-based care using clinical pharmacists in primary care. Our process provides a targeted approach to identifying patients for risk factor reduction through comprehensive medication management and could be replicated by other primary care clinics using a patient-centered medical home model.
Acknowledgments
We would like to acknowledge Dr. Sara Hariman, Dr. Payal Sanghani, and Dr. Cecilia Scholcoff for their support and collaboration with the project.
1. Braunwald E. Heart failure. J Am Coll Cardiol HF. 2013;1(1):1-20. doi: 10.1016/j.jchf.2012.10.002
2. Heidenreich PA, Albert NM, Allen LA, et al; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606-619. doi:10.1161/HHF.0b013e318291329a
3. Doust J, Lehman R, Glasziou P. The role of BNP testing in heart failure. Am Fam Physician. 2006;74(11):1893-1900.
4. Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA. 2013;310(1):66-74. doi:10.1001/jama.2013.7588
5. Huelsmann M, Neuhold S, Resl M, et al. PONTIAC (NT-proBNP selected prevention of cardiac events in a population of diabetic patients without a history of cardiac disease): a prospective randomized controlled trial. J Am Coll Cardiol. 2013;62(15):1365-1372. doi:10.1016/j.jacc.2013.05.069
6. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70(6):776-803. doi:10.1016/j.jacc.2017.04.025
7. Mueller C, McDonald K, de Boer RA, et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eu J Heart Fail. 2019;21:715-731. doi:10.1002/ejhf.1494
8. Ledwidge MT, O’Connell E, Gallagher J, et al; Heart Failure Association of the European Society of Cardiology. Cost-effectiveness of natriuretic peptide-based screening and collaborative care: a report from the STOP-HF (St. Vincent’s Screening to Prevent Heart Failure) study. Eur J Heart Fail. 2015;17(7):672-679.
Heart failure (HF) is one of the leading causes of hospitalizations and the most expensive Medicare diagnosis. Its prevalence continues to rise with a projected increase of 46% from 2012 to 2030 resulting in > 8 million people aged ≥ 18 years with HF in the United States. Despite improvements in therapy, mortality remains unacceptably high with a 50% mortality rate within 5 years. Early detection strategies are needed to identify patients at risk of developing HF to delay the disease course and improve survival.1,2
Emerging data indicates that natriuretic peptide biomarker-based screening using B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP) and early intervention for patients at risk of HF could prevent development of left ventricular dysfunction or new-onset HF.3-5 The 2013 St. Vincent’s Screening to Prevent Heart Failure (STOP-HF) trial is the largest study to date to evaluate BNP as a screening tool for patients at risk for HF.4 Patients at risk of HF who did not have established left ventricular systolic dysfunction or symptomatic HF were assigned randomly to usual primary care or BNP screening. Patients with BNP levels ≥ 50 pg/mL underwent echocardiogram and were referred to a cardiovascular specialty service for management. The cardiovascular specialty clinic included a team of registered nurses, nurse practitioners, pharmacists, dieticians, palliative care specialists, and cardiologists. Individuals in the intervention group showed increased renin-angiotensin system (RAS) inhibitor use at follow-up (control, 49.6%; intervention, 59.6%; P = .01). All patients received coaching by a nurse who emphasized individual risk, importance of medication adherence, and healthy lifestyle behaviors. After a mean follow-up of 4.2 years, 59 of 677 participants (8.7%) in the control group and 37 of 697 (5.3%) in the intervention group (odds ratio [OR], 0.55; 95% CI, 0.37 to 0.82; P = .003) met the primary end point of left ventricular dysfunction with or without HF. BNP-based screening in conjunction with collaborative care reduced rates of left ventricular dysfunction and HF.
In the 2013 PONTIAC trial, patients with type 2 diabetes mellitus (T2DM) without cardiac disease but with NT-proBNP levels > 125 pg/mL were randomized to usual diabetes care or intensified care at a cardiac outpatient clinic for initiation and increase of RAS inhibitors and β blockers.5 After 2 years, patients randomized to the intensified care group showed a 65% risk reduction of the primary endpoint of hospitalization or death from cardiac disease (P = .04).
Based on this evidence, the 2017 focused update of the American College of Cardiology (ACC)/American Heart Association (AHA)/Heart Failure Society of America (HFSA) guideline for managing HF added a IIa recommendation for natriuretic peptide biomarker screening in those at risk of developing HF.6 The guideline recommends biomarker screening in conjunction with team-based care, including a cardiovascular specialist, and guideline-directed management and therapy to prevent development of left ventricular dysfunction or new-onset HF.
Although ordering a natriuretic peptide biomarker laboratory test is straightforward, the variability of team-based care across institutions and health systems makes it difficult to standardize screening and interventions for patients at risk for HF. We developed and piloted a process using clinical pharmacists in primary care for natriuretic peptide biomarker screening and risk factor reduction within the established patient aligned care team (PACT) framework at a US Department of Veterans Affairs (VA) medical center. In this paper, we describe our implementation process including descriptive preliminary outcomes.
Methods
The PACT team-based approach in primary care clinics is similar to the patient-centered medical home framework. A PACT includes the veteran patient and an interdisciplinary team of health professionals composed of their primary care practitioner (PCP), registered nurse care manager, clinical pharmacist, and other clinical and administrative staff. The PACT clinical pharmacist has prescriptive authority within a scope of practice to provide postdiagnostic chronic disease state management including management of T2DM, hypertension, HF, chronic obstructive pulmonary disease, anticoagulation, tobacco cessation, and atherosclerotic cardiovascular disease (ASCVD) risk reduction. Clinical pharmacists can prescribe and adjust medications and order laboratory tests.
Our institution, Clement J. Zablocki VA Medical Center (CJZVAMC) in Milwaukee, Wisconsin, has a specialty HF clinic that primarily manages ACC/AHA Stage C HF patients. The HF clinic uses a team-based approach to collaborate and coordinate care for the veteran. The HF team is comprised of cardiology specialists, registered nurses, clinical pharmacists, dietitians, and administrative staff. Two PACT clinical pharmacists also staff the HF clinic at CJZVAMC and work collaboratively to initiate, adjust, and optimize veterans’ HF medication regimens.
Two primary care PACT panels were selected for this project. Before implementation, a pharmacy resident and 3 PACT clinical pharmacists (2 of whom also staff the HF clinic) met with a HF cardiology specialist and 2 PACT PCPs to finalize the team-based process and workflow. PCPs were presented with the evidence-based background, purpose, and project design, which included patient identification, NT-proBNP laboratory test ordering, medication adjustment schedules, and protocol for ordering echocardiograms (Figure). Templated notes were created to allow for consistent documentation in patients’ electronic health record. A telephone script also was written for the initial telephone call to patients to explain in patient-friendly terms the implications of an elevated NT-proBNP level, the echocardiogram procedure, and recommendations for risk reduction.
Patient Selection
Patients aged ≥ 18 years with hypertension, taking antihypertensive medication for ≥ 1 month, or diagnosed with T2DM for ≥ 6 months were included. Using the parameters provided in the STOP-HF trial, patients with evidence or history of left ventricular dysfunction, defined as a left ventricular ejection fraction (EF) < 50% or an E/e’ ratio > 15 in the setting of normal EF, or symptomatic HF were excluded. Patients with a diagnosis causing life expectancy < 1 year were excluded, which was determined based on review of the patient’s chart or discussion with the PCP.
A clinical pharmacist screened patients with an upcoming PCP appointment between September 2019 and January 2020 for eligibility. For patients who met criteria, the clinical pharmacist ordered a NT-proBNP laboratory test to their already scheduled tests and entered a templated note into the patient’s chart to alert the PCP of the test. NT-proBNP was used rather than BNP because it was the natriuretic peptide laboratory test available at CJZVAMC during this time. Patients with NT-proBNP < 125 pg/mL received usual care from their PCPs. Patients with NT-proBNP ≥ 125 pg/mL received a follow-up phone call from a clinical pharmacist to discuss the laboratory test result with recommendations for initiation or increase of RAS inhibitors and an echocardiogram. If the patient agreed to an echocardiogram, the PCP was notified to order the test. For patients aged > 80 years with elevated NT-proBNP, risk vs benefit and patient-specific goals of care were discussed with the PCP. For patients whose echocardiograms revealed left ventricular dysfunction, initiation or adjustment of β blockers was considered. During RAS inhibitor increase, the clinical pharmacists provided a review of the patient’s risk factors and optimized management of hypertension, T2DM, ASCVD risk reduction, oral nonsteroidal anti-inflammatory drug (NSAID) reduction, and tobacco cessation.
Outcome Measures
Outcome measures included the percentage of patients who met inclusion/exclusion criteria and had an elevated NT-proBNP level, percent change in RAS inhibitor prescriptions and optimized dosing after intervention, frequency of left ventricular dysfunction visualized with echocardiograms, and quantification of pharmacist interventions in disease state management. Descriptive statistics were used to analyze demographic data, RAS inhibitors prescriptions before and after intervention, echocardiogram results, pharmacist recommendations, and acceptance rates of disease state management.
Results
Between September 2019 and January 2020, 570 patients from 2 PACT teams were screened. Of the 570 patients, 246 met inclusion criteria with upcoming appointments. Of these, 24 were excluded, 10 for EF < 50%, 13 for E/e’ > 15 in setting of normal EF, and 1 for hypertension diagnosis without an antihypertensive regimen or elevated blood pressure. The remaining 222 patients had an NT-proBNP level ordered and drawn and 73 (32.9%) patients had an NT-proBNP ≥ 125 pg/mL. Baseline characteristics are described in Table 1.
Data was collected through March 2020 (due to COVID-19) found that among the 73 patients with elevated NT-proBNP: 14 had an echocardiogram within the past year without evidence of left ventricular dysfunction; 39 had echocardiograms ordered; and 19 had echocardiograms completed by March 2020. Among the 19 echocardiograms, 16 (84%) showed no evidence of left ventricular dysfunction, 2 (11%) revealed mildly reduced EF (40% to 50%), and 1 (5%) revealed a reduced EF (< 40%). These patients were identified early in the disease course before symptom onset and received intervention with RAS inhibitors and disease state management.
Patients prescribed RAS inhibitors increased from 44 to 50. The number of patients who were able to have their RAS inhibitor dosage adjusted increased from 28 to 31. For the 3 patients with mildly reduced or reduced EF, management with β blockers was based on RAS inhibitor adjustment toleration. One patient with mildly reduced EF was switched from metoprolol tartrate to metoprolol succinate.
Clinical pharmacists completed disease state assessments to optimize management of hypertension, T2DM, ASCVD risk reduction, oral NSAID reduction, and tobacco cessation (Table 2). Interventions clinical pharmacists recommended for hypertension, in addition to RAS inhibitor management, included initiation and adjustment of amlodipine. For T2DM, interventions included initiation of metformin and initiation or adjustment of empagliflozin. For ASCVD risk reduction, interventions included starting a statin or adjusting statin therapies to appropriate intensities based on clinical ASCVD 10-year risk. Tobacco cessation interventions included pharmacotherapies, counseling, and education with written materials. Pharmacists counseled patients to minimize or eliminate NSAID use and, when appropriate, discontinued active oral NSAID prescriptions.
Discussion
We included patients diagnosed with T2DM and hypertension for several reasons. Most patients (62%) studied in the STOP-HF trial were diagnosed with hypertension. Also, T2DM represented the patient population enrolled in the PONTIAC trial. Guidance from the European Society of Cardiology recommends use of natriuretic peptides in high-risk populations, such as patients with DM and hypertension, to help target initiation of preventive measures.7 Lastly, T2DM and hypertension patients were easily identified using population management software available at the VA.
The percentage of patients in this project with risk factors for HF and an elevated NT-proBNP were similar to the elevated levels described in the STOP-HF trial. In our project, 32.9% of patients had elevated NT-proBNP levels, similar to the 41.6% of patients in STOP-HF. Among the completed echocardiograms, 16% revealed mildly reduced or reduced EF. These patients were identified early in the disease course before symptom onset and received intervention with RAS inhibitors and disease state management.
In addition to early identification of reduced EF, this project allowed a targeted approach to identifying patients for risk factor reduction. Between the 2 PACT teams, 246 patients with T2DM and/or hypertension were seen from September 2019 to January 2020. By using natriuretic peptide screening, the clinical pharmacists were able to prioritize and focus risk factor management on patients at higher risk. Pharmacists were then able to intervene for all risk factors assessed: hypertension, T2DM, ASCVD risk reduction, NSAID use reduction, and tobacco cessation.
During the implementation period, VA criteria of use of the angiotensin receptor-neprilysin inhibitor, sacubitril/valsartan, was restricted to VA cardiology. For patients with reduced EF, it was up to the PCP’s discretion to consult cardiology for further follow-up. In November 2020, the VA removed the restriction to cardiology and PCPs were able to order sacubitril/valsartan. Although not included in the Figure at the time of project implementation, the clinical pharmacist could now transition a patient with reduced EF from a RAS inhibitor to sacubitril/valsartan and adjust to target dosages.
Clinical pharmacists involved in this project had established working relationships with each of the PACT members before project initiation. The PACT employed the clinical pharmacists regularly for chronic disease state management. This facilitated adoption of the natriuretic peptide screening process and PCP buy-in and support. The PCPs agreed to discuss adding a NT-proBNP laboratory test with the patient, when possible, during their in-person appointment and informed the patient that a pharmacist would call if the result was elevated. This warm hand-off facilitated the patient’s reception to the clinical pharmacists’ recommendations after an elevated NT-proBNP result. We also reported PCPs’ high acceptance rate of pharmacist recommendations and interventions for disease state management. These high acceptance rates reflect the established working relationships between clinical pharmacists and the PACT.
Development of templated notes, medication adjustment schedules, and telephone script allowed for consistent implementation into the PACT panels. This process could be duplicated and adopted into other PACTs who want to use a clinical pharmacist to facilitate natriuretic peptide screening and risk factor reduction. The findings from this project can be extrapolated to other team-based care such as the patient-centered medical home model because these programs exhibit many similarities. Both health care models centralize patient care and use interdisciplinary care teams to promote continuity, care coordination, and access to achieve optimized patient outcomes.
Cost was an important factor to consider when implementing this project. With an increase in prescriptions and elective, outpatient echocardiograms, higher outpatient cost is expected. A cost-effectiveness analysis in the STOP-HF trial found an overall cost benefit by reducing the number of patients diagnosed with left ventricular dysfunction or HF and emergency hospitalizations for cardiac events in those who received collaborative care after natriuretic peptide testing.8 These cost savings offset increased outpatient costs.
Limitations
Participants were identified initially through a computer-generated list of patients with hypertension or T2DM without a HF diagnosis documented in their problem list. This problem list is manually updated by PCPs. Although we reviewed records for exclusion criteria, eligible patients might have been excluded. The use and interpretation of an NT-proBNP level is not specific to cardiac disease. Elevations can be seen with increased age, kidney dysfunction, and pulmonary disease. Additionally, an NT-proBNP level might be falsely low in patients who are overweight or obese. Because of the relatively short period of time, we could not analyze associations with HF diagnosis or progression, hospitalizations due to HF, or mortality. Regarding external validity, because of the pre-established interdisciplinary clinic settings and VA pharmacists’ scope of practice with prescriptive authority, implementing this project might have been better received by PCPs and allowed for higher acceptance rates of pharmacist interventions at the VA compared with a community setting.
Conclusions
The ACC/AHA/HFSA guidelines recommended use of natriuretic peptide biomarker screening in conjunction with team-based care for those at risk of developing HF. We describe our process for implementing team-based care using clinical pharmacists in primary care. Our process provides a targeted approach to identifying patients for risk factor reduction through comprehensive medication management and could be replicated by other primary care clinics using a patient-centered medical home model.
Acknowledgments
We would like to acknowledge Dr. Sara Hariman, Dr. Payal Sanghani, and Dr. Cecilia Scholcoff for their support and collaboration with the project.
Heart failure (HF) is one of the leading causes of hospitalizations and the most expensive Medicare diagnosis. Its prevalence continues to rise with a projected increase of 46% from 2012 to 2030 resulting in > 8 million people aged ≥ 18 years with HF in the United States. Despite improvements in therapy, mortality remains unacceptably high with a 50% mortality rate within 5 years. Early detection strategies are needed to identify patients at risk of developing HF to delay the disease course and improve survival.1,2
Emerging data indicates that natriuretic peptide biomarker-based screening using B-type natriuretic peptide (BNP) or N-terminal pro-B-type natriuretic peptide (NT-proBNP) and early intervention for patients at risk of HF could prevent development of left ventricular dysfunction or new-onset HF.3-5 The 2013 St. Vincent’s Screening to Prevent Heart Failure (STOP-HF) trial is the largest study to date to evaluate BNP as a screening tool for patients at risk for HF.4 Patients at risk of HF who did not have established left ventricular systolic dysfunction or symptomatic HF were assigned randomly to usual primary care or BNP screening. Patients with BNP levels ≥ 50 pg/mL underwent echocardiogram and were referred to a cardiovascular specialty service for management. The cardiovascular specialty clinic included a team of registered nurses, nurse practitioners, pharmacists, dieticians, palliative care specialists, and cardiologists. Individuals in the intervention group showed increased renin-angiotensin system (RAS) inhibitor use at follow-up (control, 49.6%; intervention, 59.6%; P = .01). All patients received coaching by a nurse who emphasized individual risk, importance of medication adherence, and healthy lifestyle behaviors. After a mean follow-up of 4.2 years, 59 of 677 participants (8.7%) in the control group and 37 of 697 (5.3%) in the intervention group (odds ratio [OR], 0.55; 95% CI, 0.37 to 0.82; P = .003) met the primary end point of left ventricular dysfunction with or without HF. BNP-based screening in conjunction with collaborative care reduced rates of left ventricular dysfunction and HF.
In the 2013 PONTIAC trial, patients with type 2 diabetes mellitus (T2DM) without cardiac disease but with NT-proBNP levels > 125 pg/mL were randomized to usual diabetes care or intensified care at a cardiac outpatient clinic for initiation and increase of RAS inhibitors and β blockers.5 After 2 years, patients randomized to the intensified care group showed a 65% risk reduction of the primary endpoint of hospitalization or death from cardiac disease (P = .04).
Based on this evidence, the 2017 focused update of the American College of Cardiology (ACC)/American Heart Association (AHA)/Heart Failure Society of America (HFSA) guideline for managing HF added a IIa recommendation for natriuretic peptide biomarker screening in those at risk of developing HF.6 The guideline recommends biomarker screening in conjunction with team-based care, including a cardiovascular specialist, and guideline-directed management and therapy to prevent development of left ventricular dysfunction or new-onset HF.
Although ordering a natriuretic peptide biomarker laboratory test is straightforward, the variability of team-based care across institutions and health systems makes it difficult to standardize screening and interventions for patients at risk for HF. We developed and piloted a process using clinical pharmacists in primary care for natriuretic peptide biomarker screening and risk factor reduction within the established patient aligned care team (PACT) framework at a US Department of Veterans Affairs (VA) medical center. In this paper, we describe our implementation process including descriptive preliminary outcomes.
Methods
The PACT team-based approach in primary care clinics is similar to the patient-centered medical home framework. A PACT includes the veteran patient and an interdisciplinary team of health professionals composed of their primary care practitioner (PCP), registered nurse care manager, clinical pharmacist, and other clinical and administrative staff. The PACT clinical pharmacist has prescriptive authority within a scope of practice to provide postdiagnostic chronic disease state management including management of T2DM, hypertension, HF, chronic obstructive pulmonary disease, anticoagulation, tobacco cessation, and atherosclerotic cardiovascular disease (ASCVD) risk reduction. Clinical pharmacists can prescribe and adjust medications and order laboratory tests.
Our institution, Clement J. Zablocki VA Medical Center (CJZVAMC) in Milwaukee, Wisconsin, has a specialty HF clinic that primarily manages ACC/AHA Stage C HF patients. The HF clinic uses a team-based approach to collaborate and coordinate care for the veteran. The HF team is comprised of cardiology specialists, registered nurses, clinical pharmacists, dietitians, and administrative staff. Two PACT clinical pharmacists also staff the HF clinic at CJZVAMC and work collaboratively to initiate, adjust, and optimize veterans’ HF medication regimens.
Two primary care PACT panels were selected for this project. Before implementation, a pharmacy resident and 3 PACT clinical pharmacists (2 of whom also staff the HF clinic) met with a HF cardiology specialist and 2 PACT PCPs to finalize the team-based process and workflow. PCPs were presented with the evidence-based background, purpose, and project design, which included patient identification, NT-proBNP laboratory test ordering, medication adjustment schedules, and protocol for ordering echocardiograms (Figure). Templated notes were created to allow for consistent documentation in patients’ electronic health record. A telephone script also was written for the initial telephone call to patients to explain in patient-friendly terms the implications of an elevated NT-proBNP level, the echocardiogram procedure, and recommendations for risk reduction.
Patient Selection
Patients aged ≥ 18 years with hypertension, taking antihypertensive medication for ≥ 1 month, or diagnosed with T2DM for ≥ 6 months were included. Using the parameters provided in the STOP-HF trial, patients with evidence or history of left ventricular dysfunction, defined as a left ventricular ejection fraction (EF) < 50% or an E/e’ ratio > 15 in the setting of normal EF, or symptomatic HF were excluded. Patients with a diagnosis causing life expectancy < 1 year were excluded, which was determined based on review of the patient’s chart or discussion with the PCP.
A clinical pharmacist screened patients with an upcoming PCP appointment between September 2019 and January 2020 for eligibility. For patients who met criteria, the clinical pharmacist ordered a NT-proBNP laboratory test to their already scheduled tests and entered a templated note into the patient’s chart to alert the PCP of the test. NT-proBNP was used rather than BNP because it was the natriuretic peptide laboratory test available at CJZVAMC during this time. Patients with NT-proBNP < 125 pg/mL received usual care from their PCPs. Patients with NT-proBNP ≥ 125 pg/mL received a follow-up phone call from a clinical pharmacist to discuss the laboratory test result with recommendations for initiation or increase of RAS inhibitors and an echocardiogram. If the patient agreed to an echocardiogram, the PCP was notified to order the test. For patients aged > 80 years with elevated NT-proBNP, risk vs benefit and patient-specific goals of care were discussed with the PCP. For patients whose echocardiograms revealed left ventricular dysfunction, initiation or adjustment of β blockers was considered. During RAS inhibitor increase, the clinical pharmacists provided a review of the patient’s risk factors and optimized management of hypertension, T2DM, ASCVD risk reduction, oral nonsteroidal anti-inflammatory drug (NSAID) reduction, and tobacco cessation.
Outcome Measures
Outcome measures included the percentage of patients who met inclusion/exclusion criteria and had an elevated NT-proBNP level, percent change in RAS inhibitor prescriptions and optimized dosing after intervention, frequency of left ventricular dysfunction visualized with echocardiograms, and quantification of pharmacist interventions in disease state management. Descriptive statistics were used to analyze demographic data, RAS inhibitors prescriptions before and after intervention, echocardiogram results, pharmacist recommendations, and acceptance rates of disease state management.
Results
Between September 2019 and January 2020, 570 patients from 2 PACT teams were screened. Of the 570 patients, 246 met inclusion criteria with upcoming appointments. Of these, 24 were excluded, 10 for EF < 50%, 13 for E/e’ > 15 in setting of normal EF, and 1 for hypertension diagnosis without an antihypertensive regimen or elevated blood pressure. The remaining 222 patients had an NT-proBNP level ordered and drawn and 73 (32.9%) patients had an NT-proBNP ≥ 125 pg/mL. Baseline characteristics are described in Table 1.
Data was collected through March 2020 (due to COVID-19) found that among the 73 patients with elevated NT-proBNP: 14 had an echocardiogram within the past year without evidence of left ventricular dysfunction; 39 had echocardiograms ordered; and 19 had echocardiograms completed by March 2020. Among the 19 echocardiograms, 16 (84%) showed no evidence of left ventricular dysfunction, 2 (11%) revealed mildly reduced EF (40% to 50%), and 1 (5%) revealed a reduced EF (< 40%). These patients were identified early in the disease course before symptom onset and received intervention with RAS inhibitors and disease state management.
Patients prescribed RAS inhibitors increased from 44 to 50. The number of patients who were able to have their RAS inhibitor dosage adjusted increased from 28 to 31. For the 3 patients with mildly reduced or reduced EF, management with β blockers was based on RAS inhibitor adjustment toleration. One patient with mildly reduced EF was switched from metoprolol tartrate to metoprolol succinate.
Clinical pharmacists completed disease state assessments to optimize management of hypertension, T2DM, ASCVD risk reduction, oral NSAID reduction, and tobacco cessation (Table 2). Interventions clinical pharmacists recommended for hypertension, in addition to RAS inhibitor management, included initiation and adjustment of amlodipine. For T2DM, interventions included initiation of metformin and initiation or adjustment of empagliflozin. For ASCVD risk reduction, interventions included starting a statin or adjusting statin therapies to appropriate intensities based on clinical ASCVD 10-year risk. Tobacco cessation interventions included pharmacotherapies, counseling, and education with written materials. Pharmacists counseled patients to minimize or eliminate NSAID use and, when appropriate, discontinued active oral NSAID prescriptions.
Discussion
We included patients diagnosed with T2DM and hypertension for several reasons. Most patients (62%) studied in the STOP-HF trial were diagnosed with hypertension. Also, T2DM represented the patient population enrolled in the PONTIAC trial. Guidance from the European Society of Cardiology recommends use of natriuretic peptides in high-risk populations, such as patients with DM and hypertension, to help target initiation of preventive measures.7 Lastly, T2DM and hypertension patients were easily identified using population management software available at the VA.
The percentage of patients in this project with risk factors for HF and an elevated NT-proBNP were similar to the elevated levels described in the STOP-HF trial. In our project, 32.9% of patients had elevated NT-proBNP levels, similar to the 41.6% of patients in STOP-HF. Among the completed echocardiograms, 16% revealed mildly reduced or reduced EF. These patients were identified early in the disease course before symptom onset and received intervention with RAS inhibitors and disease state management.
In addition to early identification of reduced EF, this project allowed a targeted approach to identifying patients for risk factor reduction. Between the 2 PACT teams, 246 patients with T2DM and/or hypertension were seen from September 2019 to January 2020. By using natriuretic peptide screening, the clinical pharmacists were able to prioritize and focus risk factor management on patients at higher risk. Pharmacists were then able to intervene for all risk factors assessed: hypertension, T2DM, ASCVD risk reduction, NSAID use reduction, and tobacco cessation.
During the implementation period, VA criteria of use of the angiotensin receptor-neprilysin inhibitor, sacubitril/valsartan, was restricted to VA cardiology. For patients with reduced EF, it was up to the PCP’s discretion to consult cardiology for further follow-up. In November 2020, the VA removed the restriction to cardiology and PCPs were able to order sacubitril/valsartan. Although not included in the Figure at the time of project implementation, the clinical pharmacist could now transition a patient with reduced EF from a RAS inhibitor to sacubitril/valsartan and adjust to target dosages.
Clinical pharmacists involved in this project had established working relationships with each of the PACT members before project initiation. The PACT employed the clinical pharmacists regularly for chronic disease state management. This facilitated adoption of the natriuretic peptide screening process and PCP buy-in and support. The PCPs agreed to discuss adding a NT-proBNP laboratory test with the patient, when possible, during their in-person appointment and informed the patient that a pharmacist would call if the result was elevated. This warm hand-off facilitated the patient’s reception to the clinical pharmacists’ recommendations after an elevated NT-proBNP result. We also reported PCPs’ high acceptance rate of pharmacist recommendations and interventions for disease state management. These high acceptance rates reflect the established working relationships between clinical pharmacists and the PACT.
Development of templated notes, medication adjustment schedules, and telephone script allowed for consistent implementation into the PACT panels. This process could be duplicated and adopted into other PACTs who want to use a clinical pharmacist to facilitate natriuretic peptide screening and risk factor reduction. The findings from this project can be extrapolated to other team-based care such as the patient-centered medical home model because these programs exhibit many similarities. Both health care models centralize patient care and use interdisciplinary care teams to promote continuity, care coordination, and access to achieve optimized patient outcomes.
Cost was an important factor to consider when implementing this project. With an increase in prescriptions and elective, outpatient echocardiograms, higher outpatient cost is expected. A cost-effectiveness analysis in the STOP-HF trial found an overall cost benefit by reducing the number of patients diagnosed with left ventricular dysfunction or HF and emergency hospitalizations for cardiac events in those who received collaborative care after natriuretic peptide testing.8 These cost savings offset increased outpatient costs.
Limitations
Participants were identified initially through a computer-generated list of patients with hypertension or T2DM without a HF diagnosis documented in their problem list. This problem list is manually updated by PCPs. Although we reviewed records for exclusion criteria, eligible patients might have been excluded. The use and interpretation of an NT-proBNP level is not specific to cardiac disease. Elevations can be seen with increased age, kidney dysfunction, and pulmonary disease. Additionally, an NT-proBNP level might be falsely low in patients who are overweight or obese. Because of the relatively short period of time, we could not analyze associations with HF diagnosis or progression, hospitalizations due to HF, or mortality. Regarding external validity, because of the pre-established interdisciplinary clinic settings and VA pharmacists’ scope of practice with prescriptive authority, implementing this project might have been better received by PCPs and allowed for higher acceptance rates of pharmacist interventions at the VA compared with a community setting.
Conclusions
The ACC/AHA/HFSA guidelines recommended use of natriuretic peptide biomarker screening in conjunction with team-based care for those at risk of developing HF. We describe our process for implementing team-based care using clinical pharmacists in primary care. Our process provides a targeted approach to identifying patients for risk factor reduction through comprehensive medication management and could be replicated by other primary care clinics using a patient-centered medical home model.
Acknowledgments
We would like to acknowledge Dr. Sara Hariman, Dr. Payal Sanghani, and Dr. Cecilia Scholcoff for their support and collaboration with the project.
1. Braunwald E. Heart failure. J Am Coll Cardiol HF. 2013;1(1):1-20. doi: 10.1016/j.jchf.2012.10.002
2. Heidenreich PA, Albert NM, Allen LA, et al; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606-619. doi:10.1161/HHF.0b013e318291329a
3. Doust J, Lehman R, Glasziou P. The role of BNP testing in heart failure. Am Fam Physician. 2006;74(11):1893-1900.
4. Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA. 2013;310(1):66-74. doi:10.1001/jama.2013.7588
5. Huelsmann M, Neuhold S, Resl M, et al. PONTIAC (NT-proBNP selected prevention of cardiac events in a population of diabetic patients without a history of cardiac disease): a prospective randomized controlled trial. J Am Coll Cardiol. 2013;62(15):1365-1372. doi:10.1016/j.jacc.2013.05.069
6. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70(6):776-803. doi:10.1016/j.jacc.2017.04.025
7. Mueller C, McDonald K, de Boer RA, et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eu J Heart Fail. 2019;21:715-731. doi:10.1002/ejhf.1494
8. Ledwidge MT, O’Connell E, Gallagher J, et al; Heart Failure Association of the European Society of Cardiology. Cost-effectiveness of natriuretic peptide-based screening and collaborative care: a report from the STOP-HF (St. Vincent’s Screening to Prevent Heart Failure) study. Eur J Heart Fail. 2015;17(7):672-679.
1. Braunwald E. Heart failure. J Am Coll Cardiol HF. 2013;1(1):1-20. doi: 10.1016/j.jchf.2012.10.002
2. Heidenreich PA, Albert NM, Allen LA, et al; American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6(3):606-619. doi:10.1161/HHF.0b013e318291329a
3. Doust J, Lehman R, Glasziou P. The role of BNP testing in heart failure. Am Fam Physician. 2006;74(11):1893-1900.
4. Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA. 2013;310(1):66-74. doi:10.1001/jama.2013.7588
5. Huelsmann M, Neuhold S, Resl M, et al. PONTIAC (NT-proBNP selected prevention of cardiac events in a population of diabetic patients without a history of cardiac disease): a prospective randomized controlled trial. J Am Coll Cardiol. 2013;62(15):1365-1372. doi:10.1016/j.jacc.2013.05.069
6. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70(6):776-803. doi:10.1016/j.jacc.2017.04.025
7. Mueller C, McDonald K, de Boer RA, et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eu J Heart Fail. 2019;21:715-731. doi:10.1002/ejhf.1494
8. Ledwidge MT, O’Connell E, Gallagher J, et al; Heart Failure Association of the European Society of Cardiology. Cost-effectiveness of natriuretic peptide-based screening and collaborative care: a report from the STOP-HF (St. Vincent’s Screening to Prevent Heart Failure) study. Eur J Heart Fail. 2015;17(7):672-679.
Pharmacist Interventions to Reduce Modifiable Bleeding Risk Factors Using HAS-BLED in Patients Taking Warfarin (FULL)
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is associated with a 5-fold increase in the risk of ischemic stroke and the risk increases with age.1-3 Oral anticoagulation (OAC) therapy effectively reduces the risk of ischemic stroke in patients with nonvalvular AF. However, OAC therapy carries a bleeding risk.4
Several bleeding risk scores have been developed and validated for patients with AF who are taking warfarin: HEMORR2HAGES (Hepatic or renal disease, Ethanol abuse, Malignancy, Older age, Reduced platelet count or function, Re-bleeding, Hypertension, Anemia, Genetic factors, Excessive fall risk, Stroke), ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation), and HAS-BLED (Hypertension, Abnormal renal and/or liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio [INR], Elderly, and Drugs and/or alcohol excess concomitantly).4,5 All 3 bleeding risk scores demonstrate only modest ability to predict clinically relevant bleeding in patients taking warfarin. The HAS-BLED score was superior to HEMORR2HAGES and ATRIA for predicting any clinically relevant bleeding and was the only bleeding risk score that demonstrated significant predictive performance for intracranial hemorrhage.5 Compared with HEMORR2HAGES, the HAS-BLED score is simpler to use and to assess risk factors that can be gathered from medical history or routinely tested in patients with AF.4 Unlike HAS-BLED, HEMORR2HAGES and ATRIA do not consider medications that could increase the risk of bleeding.
Despite the availability of validated bleeding risk scores, clinical application of these measures should not be used to exclude a patient from OAC therapy for patients who reach a threshold score. Rather, current guideline and expert consensus agree with the recommendation to use bleeding risk scores to identify risk factors and address those factors that are modifiable to reduce the risk of anticoagulant-associated major bleeding.6-8
The authors identified modifiable bleeding risk factors using the HAS-BLED score and evaluated pharmacist interventions to correct these factors in patients with nonvalvular AF who are taking warfarin. To the authors’ knowledge, there have been no published studies evaluating interventions to reduce modifiable bleeding risk factors identified by the HAS-BLED score.
Methods
Clinical pharmacy specialists (CPSs) in the primary care (PC) clinics at the Clement J. Zablocki VAMC (CJZVAMC) in Milwaukee, Wisconsin, have prescriptive authority within their scope of practice to manage smoking cessation and diseases, including anticoagulation, diabetes mellitus, heart failure, hypertension, and dyslipidemia. Patients who are on OAC therapy, including warfarin, receive comprehensive anticoagulation management from PC CPSs, including prescribing OAC therapy, education, dosage adjustments, and laboratory monitoring.
Patients were included in the HAS-BLED risk scoring and intervention if their warfarin therapy was managed by a PC CPS, had an active warfarin prescription with a diagnosis of nonvalvular AF in their problem list, and had ≥ 1 modifiable risk factor(s) from the HAS-BLED risk score. Modifiable risk factors evaluated were systolic blood pressure (SBP) > 160 mm Hg, an active prescription for VA or non-VA (which generally indicates over-the-counter [OTC] medication use) aspirin, clopidogrel, or a nonsteroidal anti-inflammatory drug (NSAID). Excess alcohol consumption was not listed as a modifiable risk factor in this assessment because nearly all the anticoagulation patients already receive regular recommendations to minimize alcohol use from the PC CPSs.
Patients were excluded from analysis if they had an indication for warfarin use other than nonvalvular AF, such as atrial flutter, acute/chronic deep vein thrombosis or pulmonary embolism, history of venous thromboembolism, peripheral vascular disease, or aortic or mitral mechanical valve. Patients also were excluded if they were on antiplatelet therapy for unstable coronary artery disease (CAD), experienced acute coronary syndrome within the past 1 year, history of stent placement, carotid endarterectomy, carotid stenosis, or noncardioembolic stroke and no other modifiable risk factors. Last, patients were excluded if clinic SBP readings were > 160 mm Hg but there was documented white coat hypertension or home SBP readings < 160 mm Hg.
The following definitions or measurements were used for assessing the HAS-BLED bleeding risk score4:
- Uncontrolled hypertension: most recently charted SBP > 160 mm Hg;
- Abnormal renal function: dialysis, renal transplant, serum creatinine > 2.26 mg/dL;
- Abnormal liver function: chronic hepatic disease, biochemical evidence of significant hepatic derangement (bilirubin > 2 × upper limit of normal and/or AST/ALT/alkaline phosphatase > 3 × upper limit of normal);
- Stroke: including history of transient ischemic attack;
- Bleeding history or predisposition: history of major bleeding (intracranial and/or any bleeding requiring hospitalization and/or causing a decrease in hemoglobin (Hgb) level of > 2 g/dL and/or requiring blood transfusion), anemia (males: Hgb < 13 g/dL; females: Hgb < 12 g/dL);
- Labile INR: percentage of INRs in therapeutic range < 60% (using the CJZVAMC anticoagulation management tool, which calculates percentage of INRs in goal reported since the first visit);
- Geriatric: age > 65 years at initial assessment;
- Concomitant drug use (VA prescription or non-VA medication list): aspirin, clopidogrel, or NSAID; and
- Alcohol in excess: > 8 alcohol servings per week from chart documentation of the patient’s self-report.
In the HAS-BLED bleeding risk score, patients receive 1 point for each component for a maximum score of 9 points. The score is stratified into low (0 points), intermediate (1 to 2 points), and high (≥ 3 points) bleeding risk.4
The HAS-BLED risk factors were obtained from patient chart review, including problem list, laboratory results, and PC CPS anticoagulation notes. Interventions included primary care provider (PCP) notification of elevated BP and offer of BP management by a PC CPS, patient education and/or PCP contact to discontinue concurrent NSAID or addition of a proton pump inhibitor (PPI) based on bleeding risk factor if the NSAID was deemed necessary, and discontinuation of concomitant antiplatelet drug(s) or reduction in aspirin dosage in consultation with patient’s PCP and cardiologist.9 In order to complete the initial HAS-BLED assessment and implement interventions, a note template was developed and entered into the electronic health record (EHR) that identified the patient’s modifiable risk factors.
Once the PCP and cardiologist (if applicable) responded to the note, by either accepting or declining the PC CPS recommendation(s), the HAS-BLED score was recalculated and recorded. If the provider did not respond to the initial note, an attempt was made to follow up at 3 months and at 6 months if necessary. If the provider did not respond at 6 months, the nonresponse was documented. For patients whose PCP requested PC CPS management of BP, the HAS-BLED score was recalculated 6 months after response from the PCP.
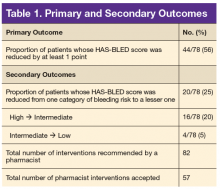
The primary outcome was the proportion of patients whose HAS-BLED score was reduced by at least 1 point. Secondary outcomes included the proportion of patients whose HAS-BLED score was reduced from one category of bleeding risk to a lesser one, total number of pharmacist interventions completed, number of pharmacist interventions made of each type (BP management, NSAID use, or antiplatelet drug use), and PCP acceptance rate.
Results
A total of 897 patients taking warfarin received anticoagulation management by a PC CPS at CJZVAMC in 2015. Of these, 819 patients were excluded based on the exclusion criteria (eFigure).
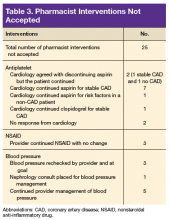
Seventy-eight patients were included in the assessment. Baseline HAS-BLED scores were calculated, and recommendations were made via an EHR progress note to the PCP and cardiologist (if applicable). Recommended interventions in the 78 patients resulted in 44 patients (56%) who experienced reduction in their HAS-BLED score by at least 1 point (Table 1). Twenty patients (25%) saw their HAS-BLED category reduced from a higher level of bleeding risk to a lower risk. The average HAS-BLED score in the 44 patients was 2.38 before intervention and 1.55 after the intervention.
In 10 patients, the HAS-BLED score did not decrease despite accepted PC CPS intervention. Specifically, 7 patients were on both an antiplatelet agent and NSAID. As a result of the pharmacist intervention, the NSAID was discontinued, but the antiplatelet remained because of stent placement or carotid stenosis. In 1 patient, the aspirin dosage was decreased from 325 to 81 mg/d. In 2 patients where NSAID use was deemed necessary—meloxicam in both cases—a PPI was ordered based on bleeding risk.9
A total of 82 interventions were recommended; 57 interventions were accepted, resulting in a provider acceptance rate of 69.5% (Tables 2 and 3). Thirty-five of the accepted interventions (61%) involved discontinuing an antiplatelet (aspirin or clopidogrel) in consultation with the patient’s PCP and cardiologist. Twenty-seven of these patients had no documented CAD, and 8 of the patients had stable CAD. Seventeen (30%) of the accepted recommendations were for discontinuing NSAID therapy, 2 (4%) were for BP management by a PC CPS, 2 (4%) for addition of PPI with continued NSAID use (meloxicam), and 1 (1%) for decreasing aspirin dosage from 325 to 81 mg/d. The NSAIDs that were discontinued included ibuprofen, indomethacin, meloxicam, and naproxen.
Discussion
This project is the first, to the authors’ knowledge, to evaluate pharmacist interventions to reduce modifiable bleeding risk factors identified by the HAS-BLED bleeding risk score. Most of the patients with nonvalvular AF in the PC clinics did not have modifiable bleeding risk factors. However, of the patients who received a recommendation to reduce a specific modifiable risk factor, most of the interventions were accepted by PCPs and
Most of the interventions recommended evaluating the use of antiplatelet agents, particularly aspirin. The benefits of antiplatelet therapy for secondary prevention of cardiovascular disease are well established. However, for AF patients on OAC therapy, the concomitant use of antiplatelet therapy significantly increases the risk of bleeding and should be reserved for high-risk patients.10 The 2012 American College of Chest Physicians guidelines support the use of OAC monotherapy in patients with AF with stable CAD, including patients with a myocardial infarction or percutaneous coronary intervention more than 1 year previously, which has been corroborated with guideline and expert consensus recommendations released in 2016.7,8,10,11
For patients taking warfarin for AF without CAD, the possible benefit of concomitant aspirin therapy for primary prevention is outweighed by the increased risk of major bleeding.12 Furthermore, warfarin monotherapy has been shown to be effective in primary prevention of CAD and seems to have cardiovascular benefit for secondary prevention but with increased bleeding.13,14 As a result, through the exclusion criteria this project aimed to evaluate warfarin patients with AF at low risk of cardiovascular events who might be taking unnecessary concurrent antiplatelet therapy.
More than one-half of the interventions involved discontinuing antiplatelet therapy. Chart reviews revealed a lack of documentation for the indication and intended duration of antiplatelet therapy. In many patients, it is likely that aspirin use predated AF diagnosis and warfarin initiation. In some of these cases, it would have been appropriate to discontinue aspirin when starting warfarin use. Although there is guidance to support the use of OAC monotherapy in patients with AF with stable CAD, the patient’s provider and cardiologist made the decision to discontinue an antiplatelet agent after weighing benefits and risks. Regardless of the outcome, this analysis revealed the importance and need for routine review of antiplatelet therapy and documenting the rationale for antiplatelet use in addition to anticoagulation.
The second largest category of interventions accepted was for evaluation of NSAID use. A 2014 study by Lamberts and colleagues found that concomitant use of oral anticoagulants and NSAIDs conferred an independent risk for major bleeding and thromboembolism in patients with AF.15 The increase in serious bleeding (absolute risk difference of 2.5 events per 1,000 patients) was observed even with short-term NSAID exposure of 14 days across all NSAID types (selective COX-2 inhibitors or nonselective NSAIDs). In addition, there was an incremental increase in bleeding risk with high NSAID dosages. The risk of serious bleeding was even greater when an NSAID is added to OAC therapy and aspirin. Seven out of 17 warfarin patients (41%) who were taking an NSAID also were on an antiplatelet agent. As a result of the pharmacist interventions, NSAIDs were discontinued in all of these patients, but the antiplatelet remained because of stent placement or carotid stenosis.
This analysis captured only those patients with a documented active prescription or self-reported OTC use of an NSAID. It is unknown how many patients might take OTC NSAIDs occasionally but not report this use to a provider or pharmacist. Primary care CPSs educate patients to not use NSAIDs while taking warfarin during their initial visit and periodically thereafter; however, with the number of different NSAIDs available without a prescription and the various brand and generic names offered, it can be difficult for patients to understand what they should or should not take for minor pain or fever. Therefore, it is imperative that NSAID use is reviewed regularly at anticoagulant follow-up visits and patients are educated about alternative OTC agents for pain relief (eg, acetaminophen, topical agents, heating pad) when necessary. It also is equally important for PCPs to weigh the benefit vs risk for each patient before prescribing an NSAID if alternatives have been exhausted especially if the patient also is taking an OAC and antiplatelet agent.
The smallest number of interventions completed was for BP management. According to the HAS-BLED bleeding risk score, BP management was recommended only if the most recent clinic SBP was > 160 mm Hg, excluding patients with documented white-coat syndrome or home SBP readings < 160 mm Hg. One potential explanation for the small number of patients with SBP > 160 mm Hg is that for many of the patients taking warfarin, the PC CPSs at CJZVAMC have been involved in their BP management through earlier consultation by providers.
Limitations
A limitation of the BP component of the HAS-BLED score was that the assessment of BP for this project was only one point in time. In 3 cases, the SBP was > 160 mm Hg only during the most recent measurement, and these patients had normal BP readings on return to the clinic for follow-up. This category of recommendation also took more time for follow-up because a PC CPS would need to evaluate the patient in clinic, implement changes to BP medications, and follow-up at subsequent visits. Although some PCPs felt that the patient did not need pharmacist intervention, the elevated SBPs were brought to the provider’s attention, and some patients received further monitoring by the PCP or through a specialty clinic (eg, nephrology).
Another limitation of this project was that the bleeding risk evaluation occurred at only 1 visit. Patients’ medications and medical issues often change with time. Therefore, it is important to implement a process to regularly review (eg, annually) patients’ bleeding risk factors and to identify and act on modifiable risk factors. Another limitation was a lack of a comparator group and the time frame of the evaluation. As a result, the authors were unable to evaluate bleeding outcomes because of the small sample size and limited time frame. Future studies could consider evaluating bleeding events as an outcome, including additional modifiable risk factors, such as excess alcohol and labile INR, expanding the review to patients taking warfarin for indications other than AF, and review of patients on direct-acting oral anticoagulants (DOACs) with AF; keeping in mind that currently available bleeding risk calculators were developed for patients taking warfarin, not DOACs with AF. Patients could be counselled on reducing alcohol intake or switching to a DOAC if INR is labile despite adherence.
Conclusion
This quality improvement project successfully implemented use of the HAS-BLED bleeding risk score to identify and reduce modifiable bleeding risk factors in patients with AF taking warfarin. Pharmacist intervention resulted in a reduction of HAS-BLED scores and bleeding risk categories.
Click here to read the digital edition.
1. Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110(9):1042-1046.
2. Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014;129(23):2371-2379.
3. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983-988.
4. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093-1100.
5. Apostolakis S, Lane DA, Guo Y, Buller H, Lip GY. Performance of the HEMORR2HAGES, ATRIA, and HAS-BLED bleeding risk-prediction scores in patients with atrial fibrillation undergoing anticoagulation: the AMADEUS (evaluating the use of SR34006 compared to warfarin or acenocoumarol in patients with atrial fibrillation) study. J Am Coll Cardiol. 2012;60(9):861-867.
6. Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-865.
7. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893-2962.
8. Ruff CT, Ansell JE, Becker RC, et al. North American thrombosis forum, AF action initiative consensus document. Am J Med. 2016;129(suppl 5):S1-S29.
9. Lanza FL, Chan FK, Quigley EM; Practice Parameters Committee of the American College of Gastroenterology. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104(3):728-738.
10. You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation. Antithrombotic therapy and prevention of thrombosis, 9th ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(suppl 2):e531S-e575S.
11. Macle L, Cairns J, Leblanc K, et al; CCS Atrial Fibrillation Guidelines Committee. 2016 focused update of the Canadian Cardiovascular Society guidelines for the management of atrial fibrillation. Can J Cardiol. 2016;32(10):1170-1185.
12. Dentali F, Douketis JD, Lim W, Crowther M. Combined aspirin-oral anticoagulant therapy compared with oral anticoagulant therapy alone among patients at risk for cardiovascular disease: a meta-analysis of randomized trials. Arch Intern Med. 2007;167(2):117-124.
13. The Medical Research Council’s General Practice Research Framework. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet. 1998;351(9098):233-241.
14. Hurlen M, Abdelnoor M, Smith P, Erikssen J, Arnesen H. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002;347(13):969-974.
15. Lamberts M, Lip GY, Hansen ML, et al. Relation of nonsteroidal anti-inflammatory drugs to serious bleeding and thromboembolism risk in patients with atrial fibrillation receiving antithrombotic therapy: a nationwide cohort study. Ann Intern Med. 2014;161(10):690-698.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is associated with a 5-fold increase in the risk of ischemic stroke and the risk increases with age.1-3 Oral anticoagulation (OAC) therapy effectively reduces the risk of ischemic stroke in patients with nonvalvular AF. However, OAC therapy carries a bleeding risk.4
Several bleeding risk scores have been developed and validated for patients with AF who are taking warfarin: HEMORR2HAGES (Hepatic or renal disease, Ethanol abuse, Malignancy, Older age, Reduced platelet count or function, Re-bleeding, Hypertension, Anemia, Genetic factors, Excessive fall risk, Stroke), ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation), and HAS-BLED (Hypertension, Abnormal renal and/or liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio [INR], Elderly, and Drugs and/or alcohol excess concomitantly).4,5 All 3 bleeding risk scores demonstrate only modest ability to predict clinically relevant bleeding in patients taking warfarin. The HAS-BLED score was superior to HEMORR2HAGES and ATRIA for predicting any clinically relevant bleeding and was the only bleeding risk score that demonstrated significant predictive performance for intracranial hemorrhage.5 Compared with HEMORR2HAGES, the HAS-BLED score is simpler to use and to assess risk factors that can be gathered from medical history or routinely tested in patients with AF.4 Unlike HAS-BLED, HEMORR2HAGES and ATRIA do not consider medications that could increase the risk of bleeding.
Despite the availability of validated bleeding risk scores, clinical application of these measures should not be used to exclude a patient from OAC therapy for patients who reach a threshold score. Rather, current guideline and expert consensus agree with the recommendation to use bleeding risk scores to identify risk factors and address those factors that are modifiable to reduce the risk of anticoagulant-associated major bleeding.6-8
The authors identified modifiable bleeding risk factors using the HAS-BLED score and evaluated pharmacist interventions to correct these factors in patients with nonvalvular AF who are taking warfarin. To the authors’ knowledge, there have been no published studies evaluating interventions to reduce modifiable bleeding risk factors identified by the HAS-BLED score.
Methods
Clinical pharmacy specialists (CPSs) in the primary care (PC) clinics at the Clement J. Zablocki VAMC (CJZVAMC) in Milwaukee, Wisconsin, have prescriptive authority within their scope of practice to manage smoking cessation and diseases, including anticoagulation, diabetes mellitus, heart failure, hypertension, and dyslipidemia. Patients who are on OAC therapy, including warfarin, receive comprehensive anticoagulation management from PC CPSs, including prescribing OAC therapy, education, dosage adjustments, and laboratory monitoring.
Patients were included in the HAS-BLED risk scoring and intervention if their warfarin therapy was managed by a PC CPS, had an active warfarin prescription with a diagnosis of nonvalvular AF in their problem list, and had ≥ 1 modifiable risk factor(s) from the HAS-BLED risk score. Modifiable risk factors evaluated were systolic blood pressure (SBP) > 160 mm Hg, an active prescription for VA or non-VA (which generally indicates over-the-counter [OTC] medication use) aspirin, clopidogrel, or a nonsteroidal anti-inflammatory drug (NSAID). Excess alcohol consumption was not listed as a modifiable risk factor in this assessment because nearly all the anticoagulation patients already receive regular recommendations to minimize alcohol use from the PC CPSs.
Patients were excluded from analysis if they had an indication for warfarin use other than nonvalvular AF, such as atrial flutter, acute/chronic deep vein thrombosis or pulmonary embolism, history of venous thromboembolism, peripheral vascular disease, or aortic or mitral mechanical valve. Patients also were excluded if they were on antiplatelet therapy for unstable coronary artery disease (CAD), experienced acute coronary syndrome within the past 1 year, history of stent placement, carotid endarterectomy, carotid stenosis, or noncardioembolic stroke and no other modifiable risk factors. Last, patients were excluded if clinic SBP readings were > 160 mm Hg but there was documented white coat hypertension or home SBP readings < 160 mm Hg.
The following definitions or measurements were used for assessing the HAS-BLED bleeding risk score4:
- Uncontrolled hypertension: most recently charted SBP > 160 mm Hg;
- Abnormal renal function: dialysis, renal transplant, serum creatinine > 2.26 mg/dL;
- Abnormal liver function: chronic hepatic disease, biochemical evidence of significant hepatic derangement (bilirubin > 2 × upper limit of normal and/or AST/ALT/alkaline phosphatase > 3 × upper limit of normal);
- Stroke: including history of transient ischemic attack;
- Bleeding history or predisposition: history of major bleeding (intracranial and/or any bleeding requiring hospitalization and/or causing a decrease in hemoglobin (Hgb) level of > 2 g/dL and/or requiring blood transfusion), anemia (males: Hgb < 13 g/dL; females: Hgb < 12 g/dL);
- Labile INR: percentage of INRs in therapeutic range < 60% (using the CJZVAMC anticoagulation management tool, which calculates percentage of INRs in goal reported since the first visit);
- Geriatric: age > 65 years at initial assessment;
- Concomitant drug use (VA prescription or non-VA medication list): aspirin, clopidogrel, or NSAID; and
- Alcohol in excess: > 8 alcohol servings per week from chart documentation of the patient’s self-report.
In the HAS-BLED bleeding risk score, patients receive 1 point for each component for a maximum score of 9 points. The score is stratified into low (0 points), intermediate (1 to 2 points), and high (≥ 3 points) bleeding risk.4
The HAS-BLED risk factors were obtained from patient chart review, including problem list, laboratory results, and PC CPS anticoagulation notes. Interventions included primary care provider (PCP) notification of elevated BP and offer of BP management by a PC CPS, patient education and/or PCP contact to discontinue concurrent NSAID or addition of a proton pump inhibitor (PPI) based on bleeding risk factor if the NSAID was deemed necessary, and discontinuation of concomitant antiplatelet drug(s) or reduction in aspirin dosage in consultation with patient’s PCP and cardiologist.9 In order to complete the initial HAS-BLED assessment and implement interventions, a note template was developed and entered into the electronic health record (EHR) that identified the patient’s modifiable risk factors.
Once the PCP and cardiologist (if applicable) responded to the note, by either accepting or declining the PC CPS recommendation(s), the HAS-BLED score was recalculated and recorded. If the provider did not respond to the initial note, an attempt was made to follow up at 3 months and at 6 months if necessary. If the provider did not respond at 6 months, the nonresponse was documented. For patients whose PCP requested PC CPS management of BP, the HAS-BLED score was recalculated 6 months after response from the PCP.
The primary outcome was the proportion of patients whose HAS-BLED score was reduced by at least 1 point. Secondary outcomes included the proportion of patients whose HAS-BLED score was reduced from one category of bleeding risk to a lesser one, total number of pharmacist interventions completed, number of pharmacist interventions made of each type (BP management, NSAID use, or antiplatelet drug use), and PCP acceptance rate.
Results
A total of 897 patients taking warfarin received anticoagulation management by a PC CPS at CJZVAMC in 2015. Of these, 819 patients were excluded based on the exclusion criteria (eFigure).
Seventy-eight patients were included in the assessment. Baseline HAS-BLED scores were calculated, and recommendations were made via an EHR progress note to the PCP and cardiologist (if applicable). Recommended interventions in the 78 patients resulted in 44 patients (56%) who experienced reduction in their HAS-BLED score by at least 1 point (Table 1). Twenty patients (25%) saw their HAS-BLED category reduced from a higher level of bleeding risk to a lower risk. The average HAS-BLED score in the 44 patients was 2.38 before intervention and 1.55 after the intervention.
In 10 patients, the HAS-BLED score did not decrease despite accepted PC CPS intervention. Specifically, 7 patients were on both an antiplatelet agent and NSAID. As a result of the pharmacist intervention, the NSAID was discontinued, but the antiplatelet remained because of stent placement or carotid stenosis. In 1 patient, the aspirin dosage was decreased from 325 to 81 mg/d. In 2 patients where NSAID use was deemed necessary—meloxicam in both cases—a PPI was ordered based on bleeding risk.9
A total of 82 interventions were recommended; 57 interventions were accepted, resulting in a provider acceptance rate of 69.5% (Tables 2 and 3). Thirty-five of the accepted interventions (61%) involved discontinuing an antiplatelet (aspirin or clopidogrel) in consultation with the patient’s PCP and cardiologist. Twenty-seven of these patients had no documented CAD, and 8 of the patients had stable CAD. Seventeen (30%) of the accepted recommendations were for discontinuing NSAID therapy, 2 (4%) were for BP management by a PC CPS, 2 (4%) for addition of PPI with continued NSAID use (meloxicam), and 1 (1%) for decreasing aspirin dosage from 325 to 81 mg/d. The NSAIDs that were discontinued included ibuprofen, indomethacin, meloxicam, and naproxen.
Discussion
This project is the first, to the authors’ knowledge, to evaluate pharmacist interventions to reduce modifiable bleeding risk factors identified by the HAS-BLED bleeding risk score. Most of the patients with nonvalvular AF in the PC clinics did not have modifiable bleeding risk factors. However, of the patients who received a recommendation to reduce a specific modifiable risk factor, most of the interventions were accepted by PCPs and
Most of the interventions recommended evaluating the use of antiplatelet agents, particularly aspirin. The benefits of antiplatelet therapy for secondary prevention of cardiovascular disease are well established. However, for AF patients on OAC therapy, the concomitant use of antiplatelet therapy significantly increases the risk of bleeding and should be reserved for high-risk patients.10 The 2012 American College of Chest Physicians guidelines support the use of OAC monotherapy in patients with AF with stable CAD, including patients with a myocardial infarction or percutaneous coronary intervention more than 1 year previously, which has been corroborated with guideline and expert consensus recommendations released in 2016.7,8,10,11
For patients taking warfarin for AF without CAD, the possible benefit of concomitant aspirin therapy for primary prevention is outweighed by the increased risk of major bleeding.12 Furthermore, warfarin monotherapy has been shown to be effective in primary prevention of CAD and seems to have cardiovascular benefit for secondary prevention but with increased bleeding.13,14 As a result, through the exclusion criteria this project aimed to evaluate warfarin patients with AF at low risk of cardiovascular events who might be taking unnecessary concurrent antiplatelet therapy.
More than one-half of the interventions involved discontinuing antiplatelet therapy. Chart reviews revealed a lack of documentation for the indication and intended duration of antiplatelet therapy. In many patients, it is likely that aspirin use predated AF diagnosis and warfarin initiation. In some of these cases, it would have been appropriate to discontinue aspirin when starting warfarin use. Although there is guidance to support the use of OAC monotherapy in patients with AF with stable CAD, the patient’s provider and cardiologist made the decision to discontinue an antiplatelet agent after weighing benefits and risks. Regardless of the outcome, this analysis revealed the importance and need for routine review of antiplatelet therapy and documenting the rationale for antiplatelet use in addition to anticoagulation.
The second largest category of interventions accepted was for evaluation of NSAID use. A 2014 study by Lamberts and colleagues found that concomitant use of oral anticoagulants and NSAIDs conferred an independent risk for major bleeding and thromboembolism in patients with AF.15 The increase in serious bleeding (absolute risk difference of 2.5 events per 1,000 patients) was observed even with short-term NSAID exposure of 14 days across all NSAID types (selective COX-2 inhibitors or nonselective NSAIDs). In addition, there was an incremental increase in bleeding risk with high NSAID dosages. The risk of serious bleeding was even greater when an NSAID is added to OAC therapy and aspirin. Seven out of 17 warfarin patients (41%) who were taking an NSAID also were on an antiplatelet agent. As a result of the pharmacist interventions, NSAIDs were discontinued in all of these patients, but the antiplatelet remained because of stent placement or carotid stenosis.
This analysis captured only those patients with a documented active prescription or self-reported OTC use of an NSAID. It is unknown how many patients might take OTC NSAIDs occasionally but not report this use to a provider or pharmacist. Primary care CPSs educate patients to not use NSAIDs while taking warfarin during their initial visit and periodically thereafter; however, with the number of different NSAIDs available without a prescription and the various brand and generic names offered, it can be difficult for patients to understand what they should or should not take for minor pain or fever. Therefore, it is imperative that NSAID use is reviewed regularly at anticoagulant follow-up visits and patients are educated about alternative OTC agents for pain relief (eg, acetaminophen, topical agents, heating pad) when necessary. It also is equally important for PCPs to weigh the benefit vs risk for each patient before prescribing an NSAID if alternatives have been exhausted especially if the patient also is taking an OAC and antiplatelet agent.
The smallest number of interventions completed was for BP management. According to the HAS-BLED bleeding risk score, BP management was recommended only if the most recent clinic SBP was > 160 mm Hg, excluding patients with documented white-coat syndrome or home SBP readings < 160 mm Hg. One potential explanation for the small number of patients with SBP > 160 mm Hg is that for many of the patients taking warfarin, the PC CPSs at CJZVAMC have been involved in their BP management through earlier consultation by providers.
Limitations
A limitation of the BP component of the HAS-BLED score was that the assessment of BP for this project was only one point in time. In 3 cases, the SBP was > 160 mm Hg only during the most recent measurement, and these patients had normal BP readings on return to the clinic for follow-up. This category of recommendation also took more time for follow-up because a PC CPS would need to evaluate the patient in clinic, implement changes to BP medications, and follow-up at subsequent visits. Although some PCPs felt that the patient did not need pharmacist intervention, the elevated SBPs were brought to the provider’s attention, and some patients received further monitoring by the PCP or through a specialty clinic (eg, nephrology).
Another limitation of this project was that the bleeding risk evaluation occurred at only 1 visit. Patients’ medications and medical issues often change with time. Therefore, it is important to implement a process to regularly review (eg, annually) patients’ bleeding risk factors and to identify and act on modifiable risk factors. Another limitation was a lack of a comparator group and the time frame of the evaluation. As a result, the authors were unable to evaluate bleeding outcomes because of the small sample size and limited time frame. Future studies could consider evaluating bleeding events as an outcome, including additional modifiable risk factors, such as excess alcohol and labile INR, expanding the review to patients taking warfarin for indications other than AF, and review of patients on direct-acting oral anticoagulants (DOACs) with AF; keeping in mind that currently available bleeding risk calculators were developed for patients taking warfarin, not DOACs with AF. Patients could be counselled on reducing alcohol intake or switching to a DOAC if INR is labile despite adherence.
Conclusion
This quality improvement project successfully implemented use of the HAS-BLED bleeding risk score to identify and reduce modifiable bleeding risk factors in patients with AF taking warfarin. Pharmacist intervention resulted in a reduction of HAS-BLED scores and bleeding risk categories.
Click here to read the digital edition.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is associated with a 5-fold increase in the risk of ischemic stroke and the risk increases with age.1-3 Oral anticoagulation (OAC) therapy effectively reduces the risk of ischemic stroke in patients with nonvalvular AF. However, OAC therapy carries a bleeding risk.4
Several bleeding risk scores have been developed and validated for patients with AF who are taking warfarin: HEMORR2HAGES (Hepatic or renal disease, Ethanol abuse, Malignancy, Older age, Reduced platelet count or function, Re-bleeding, Hypertension, Anemia, Genetic factors, Excessive fall risk, Stroke), ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation), and HAS-BLED (Hypertension, Abnormal renal and/or liver function, Stroke, Bleeding history or predisposition, Labile international normalized ratio [INR], Elderly, and Drugs and/or alcohol excess concomitantly).4,5 All 3 bleeding risk scores demonstrate only modest ability to predict clinically relevant bleeding in patients taking warfarin. The HAS-BLED score was superior to HEMORR2HAGES and ATRIA for predicting any clinically relevant bleeding and was the only bleeding risk score that demonstrated significant predictive performance for intracranial hemorrhage.5 Compared with HEMORR2HAGES, the HAS-BLED score is simpler to use and to assess risk factors that can be gathered from medical history or routinely tested in patients with AF.4 Unlike HAS-BLED, HEMORR2HAGES and ATRIA do not consider medications that could increase the risk of bleeding.
Despite the availability of validated bleeding risk scores, clinical application of these measures should not be used to exclude a patient from OAC therapy for patients who reach a threshold score. Rather, current guideline and expert consensus agree with the recommendation to use bleeding risk scores to identify risk factors and address those factors that are modifiable to reduce the risk of anticoagulant-associated major bleeding.6-8
The authors identified modifiable bleeding risk factors using the HAS-BLED score and evaluated pharmacist interventions to correct these factors in patients with nonvalvular AF who are taking warfarin. To the authors’ knowledge, there have been no published studies evaluating interventions to reduce modifiable bleeding risk factors identified by the HAS-BLED score.
Methods
Clinical pharmacy specialists (CPSs) in the primary care (PC) clinics at the Clement J. Zablocki VAMC (CJZVAMC) in Milwaukee, Wisconsin, have prescriptive authority within their scope of practice to manage smoking cessation and diseases, including anticoagulation, diabetes mellitus, heart failure, hypertension, and dyslipidemia. Patients who are on OAC therapy, including warfarin, receive comprehensive anticoagulation management from PC CPSs, including prescribing OAC therapy, education, dosage adjustments, and laboratory monitoring.
Patients were included in the HAS-BLED risk scoring and intervention if their warfarin therapy was managed by a PC CPS, had an active warfarin prescription with a diagnosis of nonvalvular AF in their problem list, and had ≥ 1 modifiable risk factor(s) from the HAS-BLED risk score. Modifiable risk factors evaluated were systolic blood pressure (SBP) > 160 mm Hg, an active prescription for VA or non-VA (which generally indicates over-the-counter [OTC] medication use) aspirin, clopidogrel, or a nonsteroidal anti-inflammatory drug (NSAID). Excess alcohol consumption was not listed as a modifiable risk factor in this assessment because nearly all the anticoagulation patients already receive regular recommendations to minimize alcohol use from the PC CPSs.
Patients were excluded from analysis if they had an indication for warfarin use other than nonvalvular AF, such as atrial flutter, acute/chronic deep vein thrombosis or pulmonary embolism, history of venous thromboembolism, peripheral vascular disease, or aortic or mitral mechanical valve. Patients also were excluded if they were on antiplatelet therapy for unstable coronary artery disease (CAD), experienced acute coronary syndrome within the past 1 year, history of stent placement, carotid endarterectomy, carotid stenosis, or noncardioembolic stroke and no other modifiable risk factors. Last, patients were excluded if clinic SBP readings were > 160 mm Hg but there was documented white coat hypertension or home SBP readings < 160 mm Hg.
The following definitions or measurements were used for assessing the HAS-BLED bleeding risk score4:
- Uncontrolled hypertension: most recently charted SBP > 160 mm Hg;
- Abnormal renal function: dialysis, renal transplant, serum creatinine > 2.26 mg/dL;
- Abnormal liver function: chronic hepatic disease, biochemical evidence of significant hepatic derangement (bilirubin > 2 × upper limit of normal and/or AST/ALT/alkaline phosphatase > 3 × upper limit of normal);
- Stroke: including history of transient ischemic attack;
- Bleeding history or predisposition: history of major bleeding (intracranial and/or any bleeding requiring hospitalization and/or causing a decrease in hemoglobin (Hgb) level of > 2 g/dL and/or requiring blood transfusion), anemia (males: Hgb < 13 g/dL; females: Hgb < 12 g/dL);
- Labile INR: percentage of INRs in therapeutic range < 60% (using the CJZVAMC anticoagulation management tool, which calculates percentage of INRs in goal reported since the first visit);
- Geriatric: age > 65 years at initial assessment;
- Concomitant drug use (VA prescription or non-VA medication list): aspirin, clopidogrel, or NSAID; and
- Alcohol in excess: > 8 alcohol servings per week from chart documentation of the patient’s self-report.
In the HAS-BLED bleeding risk score, patients receive 1 point for each component for a maximum score of 9 points. The score is stratified into low (0 points), intermediate (1 to 2 points), and high (≥ 3 points) bleeding risk.4
The HAS-BLED risk factors were obtained from patient chart review, including problem list, laboratory results, and PC CPS anticoagulation notes. Interventions included primary care provider (PCP) notification of elevated BP and offer of BP management by a PC CPS, patient education and/or PCP contact to discontinue concurrent NSAID or addition of a proton pump inhibitor (PPI) based on bleeding risk factor if the NSAID was deemed necessary, and discontinuation of concomitant antiplatelet drug(s) or reduction in aspirin dosage in consultation with patient’s PCP and cardiologist.9 In order to complete the initial HAS-BLED assessment and implement interventions, a note template was developed and entered into the electronic health record (EHR) that identified the patient’s modifiable risk factors.
Once the PCP and cardiologist (if applicable) responded to the note, by either accepting or declining the PC CPS recommendation(s), the HAS-BLED score was recalculated and recorded. If the provider did not respond to the initial note, an attempt was made to follow up at 3 months and at 6 months if necessary. If the provider did not respond at 6 months, the nonresponse was documented. For patients whose PCP requested PC CPS management of BP, the HAS-BLED score was recalculated 6 months after response from the PCP.
The primary outcome was the proportion of patients whose HAS-BLED score was reduced by at least 1 point. Secondary outcomes included the proportion of patients whose HAS-BLED score was reduced from one category of bleeding risk to a lesser one, total number of pharmacist interventions completed, number of pharmacist interventions made of each type (BP management, NSAID use, or antiplatelet drug use), and PCP acceptance rate.
Results
A total of 897 patients taking warfarin received anticoagulation management by a PC CPS at CJZVAMC in 2015. Of these, 819 patients were excluded based on the exclusion criteria (eFigure).
Seventy-eight patients were included in the assessment. Baseline HAS-BLED scores were calculated, and recommendations were made via an EHR progress note to the PCP and cardiologist (if applicable). Recommended interventions in the 78 patients resulted in 44 patients (56%) who experienced reduction in their HAS-BLED score by at least 1 point (Table 1). Twenty patients (25%) saw their HAS-BLED category reduced from a higher level of bleeding risk to a lower risk. The average HAS-BLED score in the 44 patients was 2.38 before intervention and 1.55 after the intervention.
In 10 patients, the HAS-BLED score did not decrease despite accepted PC CPS intervention. Specifically, 7 patients were on both an antiplatelet agent and NSAID. As a result of the pharmacist intervention, the NSAID was discontinued, but the antiplatelet remained because of stent placement or carotid stenosis. In 1 patient, the aspirin dosage was decreased from 325 to 81 mg/d. In 2 patients where NSAID use was deemed necessary—meloxicam in both cases—a PPI was ordered based on bleeding risk.9
A total of 82 interventions were recommended; 57 interventions were accepted, resulting in a provider acceptance rate of 69.5% (Tables 2 and 3). Thirty-five of the accepted interventions (61%) involved discontinuing an antiplatelet (aspirin or clopidogrel) in consultation with the patient’s PCP and cardiologist. Twenty-seven of these patients had no documented CAD, and 8 of the patients had stable CAD. Seventeen (30%) of the accepted recommendations were for discontinuing NSAID therapy, 2 (4%) were for BP management by a PC CPS, 2 (4%) for addition of PPI with continued NSAID use (meloxicam), and 1 (1%) for decreasing aspirin dosage from 325 to 81 mg/d. The NSAIDs that were discontinued included ibuprofen, indomethacin, meloxicam, and naproxen.
Discussion
This project is the first, to the authors’ knowledge, to evaluate pharmacist interventions to reduce modifiable bleeding risk factors identified by the HAS-BLED bleeding risk score. Most of the patients with nonvalvular AF in the PC clinics did not have modifiable bleeding risk factors. However, of the patients who received a recommendation to reduce a specific modifiable risk factor, most of the interventions were accepted by PCPs and
Most of the interventions recommended evaluating the use of antiplatelet agents, particularly aspirin. The benefits of antiplatelet therapy for secondary prevention of cardiovascular disease are well established. However, for AF patients on OAC therapy, the concomitant use of antiplatelet therapy significantly increases the risk of bleeding and should be reserved for high-risk patients.10 The 2012 American College of Chest Physicians guidelines support the use of OAC monotherapy in patients with AF with stable CAD, including patients with a myocardial infarction or percutaneous coronary intervention more than 1 year previously, which has been corroborated with guideline and expert consensus recommendations released in 2016.7,8,10,11
For patients taking warfarin for AF without CAD, the possible benefit of concomitant aspirin therapy for primary prevention is outweighed by the increased risk of major bleeding.12 Furthermore, warfarin monotherapy has been shown to be effective in primary prevention of CAD and seems to have cardiovascular benefit for secondary prevention but with increased bleeding.13,14 As a result, through the exclusion criteria this project aimed to evaluate warfarin patients with AF at low risk of cardiovascular events who might be taking unnecessary concurrent antiplatelet therapy.
More than one-half of the interventions involved discontinuing antiplatelet therapy. Chart reviews revealed a lack of documentation for the indication and intended duration of antiplatelet therapy. In many patients, it is likely that aspirin use predated AF diagnosis and warfarin initiation. In some of these cases, it would have been appropriate to discontinue aspirin when starting warfarin use. Although there is guidance to support the use of OAC monotherapy in patients with AF with stable CAD, the patient’s provider and cardiologist made the decision to discontinue an antiplatelet agent after weighing benefits and risks. Regardless of the outcome, this analysis revealed the importance and need for routine review of antiplatelet therapy and documenting the rationale for antiplatelet use in addition to anticoagulation.
The second largest category of interventions accepted was for evaluation of NSAID use. A 2014 study by Lamberts and colleagues found that concomitant use of oral anticoagulants and NSAIDs conferred an independent risk for major bleeding and thromboembolism in patients with AF.15 The increase in serious bleeding (absolute risk difference of 2.5 events per 1,000 patients) was observed even with short-term NSAID exposure of 14 days across all NSAID types (selective COX-2 inhibitors or nonselective NSAIDs). In addition, there was an incremental increase in bleeding risk with high NSAID dosages. The risk of serious bleeding was even greater when an NSAID is added to OAC therapy and aspirin. Seven out of 17 warfarin patients (41%) who were taking an NSAID also were on an antiplatelet agent. As a result of the pharmacist interventions, NSAIDs were discontinued in all of these patients, but the antiplatelet remained because of stent placement or carotid stenosis.
This analysis captured only those patients with a documented active prescription or self-reported OTC use of an NSAID. It is unknown how many patients might take OTC NSAIDs occasionally but not report this use to a provider or pharmacist. Primary care CPSs educate patients to not use NSAIDs while taking warfarin during their initial visit and periodically thereafter; however, with the number of different NSAIDs available without a prescription and the various brand and generic names offered, it can be difficult for patients to understand what they should or should not take for minor pain or fever. Therefore, it is imperative that NSAID use is reviewed regularly at anticoagulant follow-up visits and patients are educated about alternative OTC agents for pain relief (eg, acetaminophen, topical agents, heating pad) when necessary. It also is equally important for PCPs to weigh the benefit vs risk for each patient before prescribing an NSAID if alternatives have been exhausted especially if the patient also is taking an OAC and antiplatelet agent.
The smallest number of interventions completed was for BP management. According to the HAS-BLED bleeding risk score, BP management was recommended only if the most recent clinic SBP was > 160 mm Hg, excluding patients with documented white-coat syndrome or home SBP readings < 160 mm Hg. One potential explanation for the small number of patients with SBP > 160 mm Hg is that for many of the patients taking warfarin, the PC CPSs at CJZVAMC have been involved in their BP management through earlier consultation by providers.
Limitations
A limitation of the BP component of the HAS-BLED score was that the assessment of BP for this project was only one point in time. In 3 cases, the SBP was > 160 mm Hg only during the most recent measurement, and these patients had normal BP readings on return to the clinic for follow-up. This category of recommendation also took more time for follow-up because a PC CPS would need to evaluate the patient in clinic, implement changes to BP medications, and follow-up at subsequent visits. Although some PCPs felt that the patient did not need pharmacist intervention, the elevated SBPs were brought to the provider’s attention, and some patients received further monitoring by the PCP or through a specialty clinic (eg, nephrology).
Another limitation of this project was that the bleeding risk evaluation occurred at only 1 visit. Patients’ medications and medical issues often change with time. Therefore, it is important to implement a process to regularly review (eg, annually) patients’ bleeding risk factors and to identify and act on modifiable risk factors. Another limitation was a lack of a comparator group and the time frame of the evaluation. As a result, the authors were unable to evaluate bleeding outcomes because of the small sample size and limited time frame. Future studies could consider evaluating bleeding events as an outcome, including additional modifiable risk factors, such as excess alcohol and labile INR, expanding the review to patients taking warfarin for indications other than AF, and review of patients on direct-acting oral anticoagulants (DOACs) with AF; keeping in mind that currently available bleeding risk calculators were developed for patients taking warfarin, not DOACs with AF. Patients could be counselled on reducing alcohol intake or switching to a DOAC if INR is labile despite adherence.
Conclusion
This quality improvement project successfully implemented use of the HAS-BLED bleeding risk score to identify and reduce modifiable bleeding risk factors in patients with AF taking warfarin. Pharmacist intervention resulted in a reduction of HAS-BLED scores and bleeding risk categories.
Click here to read the digital edition.
1. Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110(9):1042-1046.
2. Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014;129(23):2371-2379.
3. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983-988.
4. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093-1100.
5. Apostolakis S, Lane DA, Guo Y, Buller H, Lip GY. Performance of the HEMORR2HAGES, ATRIA, and HAS-BLED bleeding risk-prediction scores in patients with atrial fibrillation undergoing anticoagulation: the AMADEUS (evaluating the use of SR34006 compared to warfarin or acenocoumarol in patients with atrial fibrillation) study. J Am Coll Cardiol. 2012;60(9):861-867.
6. Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-865.
7. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893-2962.
8. Ruff CT, Ansell JE, Becker RC, et al. North American thrombosis forum, AF action initiative consensus document. Am J Med. 2016;129(suppl 5):S1-S29.
9. Lanza FL, Chan FK, Quigley EM; Practice Parameters Committee of the American College of Gastroenterology. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104(3):728-738.
10. You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation. Antithrombotic therapy and prevention of thrombosis, 9th ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(suppl 2):e531S-e575S.
11. Macle L, Cairns J, Leblanc K, et al; CCS Atrial Fibrillation Guidelines Committee. 2016 focused update of the Canadian Cardiovascular Society guidelines for the management of atrial fibrillation. Can J Cardiol. 2016;32(10):1170-1185.
12. Dentali F, Douketis JD, Lim W, Crowther M. Combined aspirin-oral anticoagulant therapy compared with oral anticoagulant therapy alone among patients at risk for cardiovascular disease: a meta-analysis of randomized trials. Arch Intern Med. 2007;167(2):117-124.
13. The Medical Research Council’s General Practice Research Framework. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet. 1998;351(9098):233-241.
14. Hurlen M, Abdelnoor M, Smith P, Erikssen J, Arnesen H. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002;347(13):969-974.
15. Lamberts M, Lip GY, Hansen ML, et al. Relation of nonsteroidal anti-inflammatory drugs to serious bleeding and thromboembolism risk in patients with atrial fibrillation receiving antithrombotic therapy: a nationwide cohort study. Ann Intern Med. 2014;161(10):690-698.
1. Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development of atrial fibrillation: the Framingham Heart Study. Circulation. 2004;110(9):1042-1046.
2. Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010: implications for healthcare planning. Circulation. 2014;129(23):2371-2379.
3. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22(8):983-988.
4. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093-1100.
5. Apostolakis S, Lane DA, Guo Y, Buller H, Lip GY. Performance of the HEMORR2HAGES, ATRIA, and HAS-BLED bleeding risk-prediction scores in patients with atrial fibrillation undergoing anticoagulation: the AMADEUS (evaluating the use of SR34006 compared to warfarin or acenocoumarol in patients with atrial fibrillation) study. J Am Coll Cardiol. 2012;60(9):861-867.
6. Lane DA, Lip GY. Use of the CHA(2)DS(2)-VASc and HAS-BLED scores to aid decision making for thromboprophylaxis in nonvalvular atrial fibrillation. Circulation. 2012;126(7):860-865.
7. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893-2962.
8. Ruff CT, Ansell JE, Becker RC, et al. North American thrombosis forum, AF action initiative consensus document. Am J Med. 2016;129(suppl 5):S1-S29.
9. Lanza FL, Chan FK, Quigley EM; Practice Parameters Committee of the American College of Gastroenterology. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104(3):728-738.
10. You JJ, Singer DE, Howard PA, et al. Antithrombotic therapy for atrial fibrillation. Antithrombotic therapy and prevention of thrombosis, 9th ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(suppl 2):e531S-e575S.
11. Macle L, Cairns J, Leblanc K, et al; CCS Atrial Fibrillation Guidelines Committee. 2016 focused update of the Canadian Cardiovascular Society guidelines for the management of atrial fibrillation. Can J Cardiol. 2016;32(10):1170-1185.
12. Dentali F, Douketis JD, Lim W, Crowther M. Combined aspirin-oral anticoagulant therapy compared with oral anticoagulant therapy alone among patients at risk for cardiovascular disease: a meta-analysis of randomized trials. Arch Intern Med. 2007;167(2):117-124.
13. The Medical Research Council’s General Practice Research Framework. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet. 1998;351(9098):233-241.
14. Hurlen M, Abdelnoor M, Smith P, Erikssen J, Arnesen H. Warfarin, aspirin, or both after myocardial infarction. N Engl J Med. 2002;347(13):969-974.
15. Lamberts M, Lip GY, Hansen ML, et al. Relation of nonsteroidal anti-inflammatory drugs to serious bleeding and thromboembolism risk in patients with atrial fibrillation receiving antithrombotic therapy: a nationwide cohort study. Ann Intern Med. 2014;161(10):690-698.