User login
Danielle Scheurer, MD, MSCR, SFHM, is a hospitalist and the chief quality officer at the Medical University of South Carolina (MUSC) in Charleston. She is former SHM physician advisor, an SHM blogger, and member of SHM's Education Committee. She also serves as faculty of SHM's annual meeting "ABIM Maintenance of Certification (MOC) Learning Session" pre-course. Dr. Scheurer earned her undergraduate degree at Emory University in Atlanta, graduated medical school from the University of Tennessee in Knoxville, and trained at Duke University in Durham, N.C. She has served as physician editor of The Hospitalist since 2012.
Why Hospitalists Should Focus on Patient-Care Basics
We all are too familiar with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, a standardized set of questions randomly deployed to recently discharged patients. More recently, hospitalists have noticed the introduction of the Clinician and Groups Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) survey, randomly deployed to recently evaluated ambulatory patients. HCAHPS has been publicly reported since 2008. CG-CAHPS will be in the near future. In addition to these, there are a variety of other types of CAHPS surveys, ranging from ambulatory surgery to patient-centered medical homes. For HCAHPS alone, there are more than 8,200 adult surveys completed every day from almost 4,000 different U.S. hospitals.1
In addition to these surveys being publicly reported and widely viewed online by patients, payors, and employers, the results now are tightly coupled to the reimbursement of hospitals and, in some cases, individual providers. As of October 2012, Medicare has relegated 30% of its hospital value-based purchasing (VBP) program to the results of hospitals’ HCAPHS survey results. For the foreseeable future, about one-third of the financial bonus—or penalty—of a hospital rests in the hands of how well our patients perceive their care. Many individual hospitals and practice groups have started coupling individual physicians’ compensation to their patients’ CAHPS scores. Within the (approximately) seven minutes it takes to complete the survey, our patients determine millions of dollars of physician and hospital reimbursement.1
With all of the financial and reputational emphasis on HCAHPS, it is vital that hospitalists understand what it is these surveys are actually measuring, and if they have any correlation with the quality of the care the patient receives. The questions currently address 11 different domains of hospital care:
- Communication with doctors;
- Communication with nurses;
- Responsiveness of hospital staff;
- Pain management;
- Communication about medicines;
- Discharge information;
- Cleanliness of hospital environment;
- Quietness of hospital environment;
- Transitions of care;
- Overall rating of the hospital; and
- Willingness to recommend the hospital.
As the domains of care are all very different, one can imagine a wide range of answers to the various questions; a patient can perceive that communication was excellent but the quietness and cleanliness was disgraceful. And, depending on what they consider the most important aspects of their stay, they therefore may rate their overall stay as excellent or disgraceful. Why? Because each of these rest in the eye of the beholder.
But to keep pace, hospitals and providers across the country have invested millions of hours dissecting the meaning of the results and trying to improve upon them. My hospital has struggled for years with the “cleanliness” question, trying to figure out what our patients are trying to tell us: that we need to sweep and mop more often, that hospital supplies are cluttering our patient rooms, that the trashcans are overflowing or within eyesight? When we ask focus groups, we often get all of the above—and then try to implement several solutions all at once.
The quietness question is much easier to interpret but certainly difficult to improve upon. We have implemented “yacker trackers,” “quiet time,” and soft-wheeled trash cans. And the results of the surveys take months to come back and get analyzed, so it is difficult to quickly know if your interventions are actually working. Given that so many hospitals and providers are back-flipping to “play to the test,” we really need some validation that care is truly improving based on this patient feedback.
A recent New York Times article calls to light a natural paradox in the medical field, in that patients who understand more about disease processes and medical information actually feel less, rather than more, informed. In other words, those who are actually the most well-informed may rate communication the lowest. The article also calls to light the natural paradox between providers being honest and providers being likable, especially considering they routinely have to deliver messages that patients do not want to hear:
- You need to quit smoking;
- Your weight is affecting your health; and
- Your disease is not curable.
Given these natural paradoxes, the article argues that it is difficult to reconcile why hospitals and providers should be held financially accountable for their patients’ perception of care, when that perception may not equate to “real” care quality.2
However, there is some evidence that patient satisfaction surveys may actually be good proxies for care quality. A large study found that hospitals with the highest quartile HCAHPS ratings also have about 2%-3% higher quality scores for acute MI, CHF, pneumonia, and surgery, compared to those in the lowest quartile. The highest scoring hospitals also have about 2%-3% lower readmission rates for acute MI, CHF, and pneumonia.3,4 And, similar to other quality metrics, there is evidence that the longer a hospital has been administering HCAHPS, the better are their scores. So maybe hospital systems and providers can improve not only the perception a patient has of the quality of the care they received, but improve the quality, as measured by the patient’s perception.
Although there are legitimate arguments on both sides as to whether a patient’s perception of care reflects “real” care quality, in the end these CAHPS surveys are, and have been publicly reported, and will be tightly coupled to reimbursement for hospitals and (likely) providers for the foreseeable future. So in the meantime, we should continue to focus on patient-centered care, take seriously any voiced concerns, and have a relentless pursuit of perfection for how patients perceive their care. Because in the end, you would do it for your family so we should do it for our patients.
References
- Centers for Medicare & Medicaid Services. Spring 2013 HCAHPS Executive Insight Letter. Available at: www.hcahpsonline.org/Executive_Insight. Accessed Aug. 15, 2013.
- Rosenbaum L. When doctors tell patients what they don’t want to hear. The New Yorker website. Available at: www.newyorker.com/online/blogs/elements/2013/07/when-doctors-tell-patients-what-they-dont-want-to-hear.html. Published July 23, 2013. Accessed Aug. 15, 2013.
- Jha AK, Orav EJ, Zheng J, Epstein AM. Patients' perception of hospital care in the US. New Eng J Med. 2008;359(18):1921-1931.
- Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
We all are too familiar with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, a standardized set of questions randomly deployed to recently discharged patients. More recently, hospitalists have noticed the introduction of the Clinician and Groups Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) survey, randomly deployed to recently evaluated ambulatory patients. HCAHPS has been publicly reported since 2008. CG-CAHPS will be in the near future. In addition to these, there are a variety of other types of CAHPS surveys, ranging from ambulatory surgery to patient-centered medical homes. For HCAHPS alone, there are more than 8,200 adult surveys completed every day from almost 4,000 different U.S. hospitals.1
In addition to these surveys being publicly reported and widely viewed online by patients, payors, and employers, the results now are tightly coupled to the reimbursement of hospitals and, in some cases, individual providers. As of October 2012, Medicare has relegated 30% of its hospital value-based purchasing (VBP) program to the results of hospitals’ HCAPHS survey results. For the foreseeable future, about one-third of the financial bonus—or penalty—of a hospital rests in the hands of how well our patients perceive their care. Many individual hospitals and practice groups have started coupling individual physicians’ compensation to their patients’ CAHPS scores. Within the (approximately) seven minutes it takes to complete the survey, our patients determine millions of dollars of physician and hospital reimbursement.1
With all of the financial and reputational emphasis on HCAHPS, it is vital that hospitalists understand what it is these surveys are actually measuring, and if they have any correlation with the quality of the care the patient receives. The questions currently address 11 different domains of hospital care:
- Communication with doctors;
- Communication with nurses;
- Responsiveness of hospital staff;
- Pain management;
- Communication about medicines;
- Discharge information;
- Cleanliness of hospital environment;
- Quietness of hospital environment;
- Transitions of care;
- Overall rating of the hospital; and
- Willingness to recommend the hospital.
As the domains of care are all very different, one can imagine a wide range of answers to the various questions; a patient can perceive that communication was excellent but the quietness and cleanliness was disgraceful. And, depending on what they consider the most important aspects of their stay, they therefore may rate their overall stay as excellent or disgraceful. Why? Because each of these rest in the eye of the beholder.
But to keep pace, hospitals and providers across the country have invested millions of hours dissecting the meaning of the results and trying to improve upon them. My hospital has struggled for years with the “cleanliness” question, trying to figure out what our patients are trying to tell us: that we need to sweep and mop more often, that hospital supplies are cluttering our patient rooms, that the trashcans are overflowing or within eyesight? When we ask focus groups, we often get all of the above—and then try to implement several solutions all at once.
The quietness question is much easier to interpret but certainly difficult to improve upon. We have implemented “yacker trackers,” “quiet time,” and soft-wheeled trash cans. And the results of the surveys take months to come back and get analyzed, so it is difficult to quickly know if your interventions are actually working. Given that so many hospitals and providers are back-flipping to “play to the test,” we really need some validation that care is truly improving based on this patient feedback.
A recent New York Times article calls to light a natural paradox in the medical field, in that patients who understand more about disease processes and medical information actually feel less, rather than more, informed. In other words, those who are actually the most well-informed may rate communication the lowest. The article also calls to light the natural paradox between providers being honest and providers being likable, especially considering they routinely have to deliver messages that patients do not want to hear:
- You need to quit smoking;
- Your weight is affecting your health; and
- Your disease is not curable.
Given these natural paradoxes, the article argues that it is difficult to reconcile why hospitals and providers should be held financially accountable for their patients’ perception of care, when that perception may not equate to “real” care quality.2
However, there is some evidence that patient satisfaction surveys may actually be good proxies for care quality. A large study found that hospitals with the highest quartile HCAHPS ratings also have about 2%-3% higher quality scores for acute MI, CHF, pneumonia, and surgery, compared to those in the lowest quartile. The highest scoring hospitals also have about 2%-3% lower readmission rates for acute MI, CHF, and pneumonia.3,4 And, similar to other quality metrics, there is evidence that the longer a hospital has been administering HCAHPS, the better are their scores. So maybe hospital systems and providers can improve not only the perception a patient has of the quality of the care they received, but improve the quality, as measured by the patient’s perception.
Although there are legitimate arguments on both sides as to whether a patient’s perception of care reflects “real” care quality, in the end these CAHPS surveys are, and have been publicly reported, and will be tightly coupled to reimbursement for hospitals and (likely) providers for the foreseeable future. So in the meantime, we should continue to focus on patient-centered care, take seriously any voiced concerns, and have a relentless pursuit of perfection for how patients perceive their care. Because in the end, you would do it for your family so we should do it for our patients.
References
- Centers for Medicare & Medicaid Services. Spring 2013 HCAHPS Executive Insight Letter. Available at: www.hcahpsonline.org/Executive_Insight. Accessed Aug. 15, 2013.
- Rosenbaum L. When doctors tell patients what they don’t want to hear. The New Yorker website. Available at: www.newyorker.com/online/blogs/elements/2013/07/when-doctors-tell-patients-what-they-dont-want-to-hear.html. Published July 23, 2013. Accessed Aug. 15, 2013.
- Jha AK, Orav EJ, Zheng J, Epstein AM. Patients' perception of hospital care in the US. New Eng J Med. 2008;359(18):1921-1931.
- Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
We all are too familiar with the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, a standardized set of questions randomly deployed to recently discharged patients. More recently, hospitalists have noticed the introduction of the Clinician and Groups Consumer Assessment of Healthcare Providers and Systems (CG-CAHPS) survey, randomly deployed to recently evaluated ambulatory patients. HCAHPS has been publicly reported since 2008. CG-CAHPS will be in the near future. In addition to these, there are a variety of other types of CAHPS surveys, ranging from ambulatory surgery to patient-centered medical homes. For HCAHPS alone, there are more than 8,200 adult surveys completed every day from almost 4,000 different U.S. hospitals.1
In addition to these surveys being publicly reported and widely viewed online by patients, payors, and employers, the results now are tightly coupled to the reimbursement of hospitals and, in some cases, individual providers. As of October 2012, Medicare has relegated 30% of its hospital value-based purchasing (VBP) program to the results of hospitals’ HCAPHS survey results. For the foreseeable future, about one-third of the financial bonus—or penalty—of a hospital rests in the hands of how well our patients perceive their care. Many individual hospitals and practice groups have started coupling individual physicians’ compensation to their patients’ CAHPS scores. Within the (approximately) seven minutes it takes to complete the survey, our patients determine millions of dollars of physician and hospital reimbursement.1
With all of the financial and reputational emphasis on HCAHPS, it is vital that hospitalists understand what it is these surveys are actually measuring, and if they have any correlation with the quality of the care the patient receives. The questions currently address 11 different domains of hospital care:
- Communication with doctors;
- Communication with nurses;
- Responsiveness of hospital staff;
- Pain management;
- Communication about medicines;
- Discharge information;
- Cleanliness of hospital environment;
- Quietness of hospital environment;
- Transitions of care;
- Overall rating of the hospital; and
- Willingness to recommend the hospital.
As the domains of care are all very different, one can imagine a wide range of answers to the various questions; a patient can perceive that communication was excellent but the quietness and cleanliness was disgraceful. And, depending on what they consider the most important aspects of their stay, they therefore may rate their overall stay as excellent or disgraceful. Why? Because each of these rest in the eye of the beholder.
But to keep pace, hospitals and providers across the country have invested millions of hours dissecting the meaning of the results and trying to improve upon them. My hospital has struggled for years with the “cleanliness” question, trying to figure out what our patients are trying to tell us: that we need to sweep and mop more often, that hospital supplies are cluttering our patient rooms, that the trashcans are overflowing or within eyesight? When we ask focus groups, we often get all of the above—and then try to implement several solutions all at once.
The quietness question is much easier to interpret but certainly difficult to improve upon. We have implemented “yacker trackers,” “quiet time,” and soft-wheeled trash cans. And the results of the surveys take months to come back and get analyzed, so it is difficult to quickly know if your interventions are actually working. Given that so many hospitals and providers are back-flipping to “play to the test,” we really need some validation that care is truly improving based on this patient feedback.
A recent New York Times article calls to light a natural paradox in the medical field, in that patients who understand more about disease processes and medical information actually feel less, rather than more, informed. In other words, those who are actually the most well-informed may rate communication the lowest. The article also calls to light the natural paradox between providers being honest and providers being likable, especially considering they routinely have to deliver messages that patients do not want to hear:
- You need to quit smoking;
- Your weight is affecting your health; and
- Your disease is not curable.
Given these natural paradoxes, the article argues that it is difficult to reconcile why hospitals and providers should be held financially accountable for their patients’ perception of care, when that perception may not equate to “real” care quality.2
However, there is some evidence that patient satisfaction surveys may actually be good proxies for care quality. A large study found that hospitals with the highest quartile HCAHPS ratings also have about 2%-3% higher quality scores for acute MI, CHF, pneumonia, and surgery, compared to those in the lowest quartile. The highest scoring hospitals also have about 2%-3% lower readmission rates for acute MI, CHF, and pneumonia.3,4 And, similar to other quality metrics, there is evidence that the longer a hospital has been administering HCAHPS, the better are their scores. So maybe hospital systems and providers can improve not only the perception a patient has of the quality of the care they received, but improve the quality, as measured by the patient’s perception.
Although there are legitimate arguments on both sides as to whether a patient’s perception of care reflects “real” care quality, in the end these CAHPS surveys are, and have been publicly reported, and will be tightly coupled to reimbursement for hospitals and (likely) providers for the foreseeable future. So in the meantime, we should continue to focus on patient-centered care, take seriously any voiced concerns, and have a relentless pursuit of perfection for how patients perceive their care. Because in the end, you would do it for your family so we should do it for our patients.
References
- Centers for Medicare & Medicaid Services. Spring 2013 HCAHPS Executive Insight Letter. Available at: www.hcahpsonline.org/Executive_Insight. Accessed Aug. 15, 2013.
- Rosenbaum L. When doctors tell patients what they don’t want to hear. The New Yorker website. Available at: www.newyorker.com/online/blogs/elements/2013/07/when-doctors-tell-patients-what-they-dont-want-to-hear.html. Published July 23, 2013. Accessed Aug. 15, 2013.
- Jha AK, Orav EJ, Zheng J, Epstein AM. Patients' perception of hospital care in the US. New Eng J Med. 2008;359(18):1921-1931.
- Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41-48.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Proactive Approaches Necessary to Offset Primary-Care Physician Shortage
As I was reading my departmental, end-of-the-academic-year newsletter, I was pondering my own group’s hospitalist pipeline. Each year, I earnestly read the list of internal-medicine-program graduates, focusing on what and where they are going to practice. I first selfishly scan the list for “hospital medicine, MUSC.” Then I go back and reread the list to see who I can now send my discharges to or who I can refer any new friends or relatives who move to town, scanning the list for “primary care, MUSC.”
This year, similar to recent years, the list for “primary care” is slim.
SHM has long been motivated to think about the pipeline, about how to get the best and the brightest interested in practicing HM, and practicing primary care, as they are vital partners in the spectrum of generalist care. We need to know and understand our pipeline: Where will they train, how will they be trained, will they be prepared to function and thrive in the medical industry of tomorrow? Regardless of how or where you practice, all of us should be thinking about our pipeline.
As such, all of us should be thinking about graduate medical education (GME), how it is funded, how much it is funded, and what regulations control the types of specialties that come out of U.S. training programs.1 This is especially true given the projected need for more hospitalists in all areas of the hospital of the future, the ever-expanding role of “specialty hospitalists,” and the need for hospitalists during the “peri-hospital” stay (from pre-operative clinics to post-discharge clinics). And this is especially true given the ongoing projected expanse of the primary-care shortage.
The career path for physicians starts long before medical school and is heavily shaped by what types of physicians they are exposed to, when they are exposed to them, and what their experience was. The periods of medical school and graduate medical education training can have a profound impact on the “health” of the U.S. health-care system and whether it is equipped to care for the needs of its citizens.
American taxpayers have long been in the business of funding the physician pipeline. The federal government invests $13 billion annually on graduate medical education subsidies. The money flows directly to teaching hospitals to pay for the salaries of the trainees and the salaries of the attendings who supervise their work, as well as the hospital overhead that has to be invested to house these trainees during their tenure.
Federal subsidies for apprenticeships are relatively unheard of in other industries; this funding stream was initiated with the passage of Medicare almost 50 years ago, under the provision that additional training for medical students would result in better and safer medical care for all Americans. However, what was not set up as a tagline to these federal subsidies was any type of accountability on process or outcome measures, such as how exactly do teaching hospitals invest their GME money, and how will they produce the types and amounts of physicians that the U.S. needs?
Cold, Hard Facts
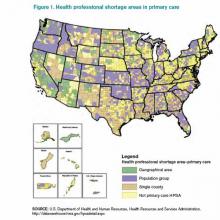
Source: U.S. Department of Health and Human Resources, Health Resources and Services Administration, http://datawarehouse.hrsa.gov/hpsadetail.aspx
So what do Americans get for that annual $13 billion investment? We get what we should expect out of the “free will” of graduating residents: We get an oversupply of specialists in areas of abundance and an undersupply of generalists in most areas. The system “produces” the most appealing specialties (those handsomely reimbursed and highly prestigious), leaving a dwindling number of generalists to be spread thinly. And the most prestigious and top-ranked academic medical centers are the least likely to produce generalists. In many of these highly ranked training programs, less than 10% of their graduates go on to work in primary care, and even fewer work in rural or public health facilities. More than 20% of all residency programs produce no primary-care physicians (PCPs) at all. Despite the $13 billion annual investment, the American Association of Medical Colleges (AAMC) predicts a shortage of 45,000 primary-care physicians by 2020.2
Because of this shortage, even fully insured Americans find the act of securing a generalist to be problematic: Almost 1 in 5 of us live in a federally designated primary-care-shortage area (see Figure 1).3 It is estimated that our current training programs will produce 40% fewer PCPs than will be needed to keep pace with the baby boomers and the insurance expansion of the Affordable Care Act. Attempts at using GME subsidies as a lever to increase the number of generalists have failed for decades. Almost 30 years ago, Dan Quayle petitioned Medicare to forgo any subsidies to training programs that did not commit to graduating at least 70% of trainees to primary-care careers, to no avail. Years later, the Institute of Medicine appealed to the federal government to reduce the training of specialists, and increase the training pool for generalists, to no avail. To reduce the financial burden of GME training, about 15 years ago, Congress threw in place a stop-gap measure, putting a freeze on the total number of residency slots that would be funded, but it did not put any measures in place to ensure that the allocation of slots would match what the U.S. health-care system needs. This has left us in a global shortage of physicians, the most grotesque of which is among generalists in regions of greatest need.
The Good News
So where does this leave hospitalists? Fortunately for our specialty, hospital medicine remains very appealing to new graduates and to the health-care system. For new graduates, it offers a competitive salary and work-life balance, without additional fellowship training. For the health-care system, we are generalists who can enhance the “value equation,” having proven to enhance quality while simultaneously reducing cost. As generalists, our specialty remains relatively undifferentiated and flexible to meet the needs of the system, including caring for patients at many stages of an acute or chronic illness; pre-operative care; post-discharge transitions of care; and assisting in some stages of “specialty care” (e.g. the medical care of the neurologic emergency, the pregnant patient, comanagement with a variety of surgical subspecialists).
As a progressive specialty, we should continue to focus on the pipeline, not only to ensure we recruit our “favorite picks” to hospital medicine, but also to support the reform needed to enhance the appeal of generalist practices and reduce the irresistible appeal of specialty care. In this way, we can add yet another meaningful contribution to meeting the needs of the U.S. health-care system.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Longman P. First teach no harm. The Washington Monthly website. Available at: http://www.washingtonmonthly.com/magazine/july_august_2013/features/first_teach_no_harm045361.php?page=all. Accessed Aug. 4, 2013.
- Association of American Medical Colleges. Physician shortages to worsen without increases in residency training. Association of American Medical Colleges website. Available at: https://www.aamc.org/download/150612/data/md-shortage.pdf. Accessed Aug. 4, 2013.
As I was reading my departmental, end-of-the-academic-year newsletter, I was pondering my own group’s hospitalist pipeline. Each year, I earnestly read the list of internal-medicine-program graduates, focusing on what and where they are going to practice. I first selfishly scan the list for “hospital medicine, MUSC.” Then I go back and reread the list to see who I can now send my discharges to or who I can refer any new friends or relatives who move to town, scanning the list for “primary care, MUSC.”
This year, similar to recent years, the list for “primary care” is slim.
SHM has long been motivated to think about the pipeline, about how to get the best and the brightest interested in practicing HM, and practicing primary care, as they are vital partners in the spectrum of generalist care. We need to know and understand our pipeline: Where will they train, how will they be trained, will they be prepared to function and thrive in the medical industry of tomorrow? Regardless of how or where you practice, all of us should be thinking about our pipeline.
As such, all of us should be thinking about graduate medical education (GME), how it is funded, how much it is funded, and what regulations control the types of specialties that come out of U.S. training programs.1 This is especially true given the projected need for more hospitalists in all areas of the hospital of the future, the ever-expanding role of “specialty hospitalists,” and the need for hospitalists during the “peri-hospital” stay (from pre-operative clinics to post-discharge clinics). And this is especially true given the ongoing projected expanse of the primary-care shortage.
The career path for physicians starts long before medical school and is heavily shaped by what types of physicians they are exposed to, when they are exposed to them, and what their experience was. The periods of medical school and graduate medical education training can have a profound impact on the “health” of the U.S. health-care system and whether it is equipped to care for the needs of its citizens.
American taxpayers have long been in the business of funding the physician pipeline. The federal government invests $13 billion annually on graduate medical education subsidies. The money flows directly to teaching hospitals to pay for the salaries of the trainees and the salaries of the attendings who supervise their work, as well as the hospital overhead that has to be invested to house these trainees during their tenure.
Federal subsidies for apprenticeships are relatively unheard of in other industries; this funding stream was initiated with the passage of Medicare almost 50 years ago, under the provision that additional training for medical students would result in better and safer medical care for all Americans. However, what was not set up as a tagline to these federal subsidies was any type of accountability on process or outcome measures, such as how exactly do teaching hospitals invest their GME money, and how will they produce the types and amounts of physicians that the U.S. needs?
Cold, Hard Facts
Source: U.S. Department of Health and Human Resources, Health Resources and Services Administration, http://datawarehouse.hrsa.gov/hpsadetail.aspx
So what do Americans get for that annual $13 billion investment? We get what we should expect out of the “free will” of graduating residents: We get an oversupply of specialists in areas of abundance and an undersupply of generalists in most areas. The system “produces” the most appealing specialties (those handsomely reimbursed and highly prestigious), leaving a dwindling number of generalists to be spread thinly. And the most prestigious and top-ranked academic medical centers are the least likely to produce generalists. In many of these highly ranked training programs, less than 10% of their graduates go on to work in primary care, and even fewer work in rural or public health facilities. More than 20% of all residency programs produce no primary-care physicians (PCPs) at all. Despite the $13 billion annual investment, the American Association of Medical Colleges (AAMC) predicts a shortage of 45,000 primary-care physicians by 2020.2
Because of this shortage, even fully insured Americans find the act of securing a generalist to be problematic: Almost 1 in 5 of us live in a federally designated primary-care-shortage area (see Figure 1).3 It is estimated that our current training programs will produce 40% fewer PCPs than will be needed to keep pace with the baby boomers and the insurance expansion of the Affordable Care Act. Attempts at using GME subsidies as a lever to increase the number of generalists have failed for decades. Almost 30 years ago, Dan Quayle petitioned Medicare to forgo any subsidies to training programs that did not commit to graduating at least 70% of trainees to primary-care careers, to no avail. Years later, the Institute of Medicine appealed to the federal government to reduce the training of specialists, and increase the training pool for generalists, to no avail. To reduce the financial burden of GME training, about 15 years ago, Congress threw in place a stop-gap measure, putting a freeze on the total number of residency slots that would be funded, but it did not put any measures in place to ensure that the allocation of slots would match what the U.S. health-care system needs. This has left us in a global shortage of physicians, the most grotesque of which is among generalists in regions of greatest need.
The Good News
So where does this leave hospitalists? Fortunately for our specialty, hospital medicine remains very appealing to new graduates and to the health-care system. For new graduates, it offers a competitive salary and work-life balance, without additional fellowship training. For the health-care system, we are generalists who can enhance the “value equation,” having proven to enhance quality while simultaneously reducing cost. As generalists, our specialty remains relatively undifferentiated and flexible to meet the needs of the system, including caring for patients at many stages of an acute or chronic illness; pre-operative care; post-discharge transitions of care; and assisting in some stages of “specialty care” (e.g. the medical care of the neurologic emergency, the pregnant patient, comanagement with a variety of surgical subspecialists).
As a progressive specialty, we should continue to focus on the pipeline, not only to ensure we recruit our “favorite picks” to hospital medicine, but also to support the reform needed to enhance the appeal of generalist practices and reduce the irresistible appeal of specialty care. In this way, we can add yet another meaningful contribution to meeting the needs of the U.S. health-care system.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Longman P. First teach no harm. The Washington Monthly website. Available at: http://www.washingtonmonthly.com/magazine/july_august_2013/features/first_teach_no_harm045361.php?page=all. Accessed Aug. 4, 2013.
- Association of American Medical Colleges. Physician shortages to worsen without increases in residency training. Association of American Medical Colleges website. Available at: https://www.aamc.org/download/150612/data/md-shortage.pdf. Accessed Aug. 4, 2013.
As I was reading my departmental, end-of-the-academic-year newsletter, I was pondering my own group’s hospitalist pipeline. Each year, I earnestly read the list of internal-medicine-program graduates, focusing on what and where they are going to practice. I first selfishly scan the list for “hospital medicine, MUSC.” Then I go back and reread the list to see who I can now send my discharges to or who I can refer any new friends or relatives who move to town, scanning the list for “primary care, MUSC.”
This year, similar to recent years, the list for “primary care” is slim.
SHM has long been motivated to think about the pipeline, about how to get the best and the brightest interested in practicing HM, and practicing primary care, as they are vital partners in the spectrum of generalist care. We need to know and understand our pipeline: Where will they train, how will they be trained, will they be prepared to function and thrive in the medical industry of tomorrow? Regardless of how or where you practice, all of us should be thinking about our pipeline.
As such, all of us should be thinking about graduate medical education (GME), how it is funded, how much it is funded, and what regulations control the types of specialties that come out of U.S. training programs.1 This is especially true given the projected need for more hospitalists in all areas of the hospital of the future, the ever-expanding role of “specialty hospitalists,” and the need for hospitalists during the “peri-hospital” stay (from pre-operative clinics to post-discharge clinics). And this is especially true given the ongoing projected expanse of the primary-care shortage.
The career path for physicians starts long before medical school and is heavily shaped by what types of physicians they are exposed to, when they are exposed to them, and what their experience was. The periods of medical school and graduate medical education training can have a profound impact on the “health” of the U.S. health-care system and whether it is equipped to care for the needs of its citizens.
American taxpayers have long been in the business of funding the physician pipeline. The federal government invests $13 billion annually on graduate medical education subsidies. The money flows directly to teaching hospitals to pay for the salaries of the trainees and the salaries of the attendings who supervise their work, as well as the hospital overhead that has to be invested to house these trainees during their tenure.
Federal subsidies for apprenticeships are relatively unheard of in other industries; this funding stream was initiated with the passage of Medicare almost 50 years ago, under the provision that additional training for medical students would result in better and safer medical care for all Americans. However, what was not set up as a tagline to these federal subsidies was any type of accountability on process or outcome measures, such as how exactly do teaching hospitals invest their GME money, and how will they produce the types and amounts of physicians that the U.S. needs?
Cold, Hard Facts
Source: U.S. Department of Health and Human Resources, Health Resources and Services Administration, http://datawarehouse.hrsa.gov/hpsadetail.aspx
So what do Americans get for that annual $13 billion investment? We get what we should expect out of the “free will” of graduating residents: We get an oversupply of specialists in areas of abundance and an undersupply of generalists in most areas. The system “produces” the most appealing specialties (those handsomely reimbursed and highly prestigious), leaving a dwindling number of generalists to be spread thinly. And the most prestigious and top-ranked academic medical centers are the least likely to produce generalists. In many of these highly ranked training programs, less than 10% of their graduates go on to work in primary care, and even fewer work in rural or public health facilities. More than 20% of all residency programs produce no primary-care physicians (PCPs) at all. Despite the $13 billion annual investment, the American Association of Medical Colleges (AAMC) predicts a shortage of 45,000 primary-care physicians by 2020.2
Because of this shortage, even fully insured Americans find the act of securing a generalist to be problematic: Almost 1 in 5 of us live in a federally designated primary-care-shortage area (see Figure 1).3 It is estimated that our current training programs will produce 40% fewer PCPs than will be needed to keep pace with the baby boomers and the insurance expansion of the Affordable Care Act. Attempts at using GME subsidies as a lever to increase the number of generalists have failed for decades. Almost 30 years ago, Dan Quayle petitioned Medicare to forgo any subsidies to training programs that did not commit to graduating at least 70% of trainees to primary-care careers, to no avail. Years later, the Institute of Medicine appealed to the federal government to reduce the training of specialists, and increase the training pool for generalists, to no avail. To reduce the financial burden of GME training, about 15 years ago, Congress threw in place a stop-gap measure, putting a freeze on the total number of residency slots that would be funded, but it did not put any measures in place to ensure that the allocation of slots would match what the U.S. health-care system needs. This has left us in a global shortage of physicians, the most grotesque of which is among generalists in regions of greatest need.
The Good News
So where does this leave hospitalists? Fortunately for our specialty, hospital medicine remains very appealing to new graduates and to the health-care system. For new graduates, it offers a competitive salary and work-life balance, without additional fellowship training. For the health-care system, we are generalists who can enhance the “value equation,” having proven to enhance quality while simultaneously reducing cost. As generalists, our specialty remains relatively undifferentiated and flexible to meet the needs of the system, including caring for patients at many stages of an acute or chronic illness; pre-operative care; post-discharge transitions of care; and assisting in some stages of “specialty care” (e.g. the medical care of the neurologic emergency, the pregnant patient, comanagement with a variety of surgical subspecialists).
As a progressive specialty, we should continue to focus on the pipeline, not only to ensure we recruit our “favorite picks” to hospital medicine, but also to support the reform needed to enhance the appeal of generalist practices and reduce the irresistible appeal of specialty care. In this way, we can add yet another meaningful contribution to meeting the needs of the U.S. health-care system.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Longman P. First teach no harm. The Washington Monthly website. Available at: http://www.washingtonmonthly.com/magazine/july_august_2013/features/first_teach_no_harm045361.php?page=all. Accessed Aug. 4, 2013.
- Association of American Medical Colleges. Physician shortages to worsen without increases in residency training. Association of American Medical Colleges website. Available at: https://www.aamc.org/download/150612/data/md-shortage.pdf. Accessed Aug. 4, 2013.
Consumer Reports' Hospital Quality Ratings Dubious
Who doesn’t know and love Consumer Reports? I personally have used this product to help me make a wide range of purchases, from child-care products to a new automobile. Consumer Reports has enjoyed a relatively unblemished reputation since its inception as an unbiased repository of invaluable information for consumers. This nonprofit advocacy organization advises consumers looking to purchase anything from small, menial items (e.g. blenders and toasters) to large, expensive ones (e.g. computers, lawn mowers, cars). It has been categorizing and publishing large-scale consumer feedback and in-house testing since 1936. According to Wikipedia, Consumer Reports has more than 7 million subscribers and runs a budget in excess of $21 million annually.
One of the reasons for its longstanding success is that it does not appear to have any hidden agenda. It does not have any partiality to a specific company or service, and therefore has maintained its impartial stance during testing and evaluation of any good or service. Its Consumer Reports magazine houses no advertisements in order to maintain its objectivity. Its only agenda is to reflect the interests and opinions of the consumers themselves, and its mission is to provide a “fair, just, and safe marketplace for all consumers and to empower consumers to protect themselves.”1 A perfect agent from which to seek advice.
And as a company, it has grown with the times, as it now hosts a variety of platforms from which consumers can seek advice. It has long hosted a website (ConsumerReports.org). Now it has Consumer Reports Television and The Consumerist blog, the latter of which accepts “tips” from anyone on what stories to cover, helpful tips for consumers, or interesting pictures. For a few years, there was also Consumer Reports WebWatch, which was aimed at improving the credibility of websites through rigorous investigative reporting.
So it seems that Consumer Reports could be a good avenue to seek advice on where to “consume” health care. And, in fact, it is now in the business of rating the health-care industry. Recent blog posts from Consumer Reports have entailed topics as wide-ranging as the number of uninsured in the U.S. to the number and types of recalls of food products.
The health part of the website covers beauty and personal care (sunscreens and anti-wrinkle serums), exercise and fitness (bikes and diet plans), foods (coffee to frozen meals), home medical supplies (heart rate and blood pressure monitors), vitamins, supplements, and, last but not least, health services. This last section rates health insurance, heart surgeons, heart screening tests, and hospitals.
It even goes so far as to “rate” medications; its Best Buy Drugs compares the cost and effectiveness of a variety of prescription drugs ranging from anti-hypertensives to diabetic agents.
In Focus: Hospitals
Consumer Reports’ latest foray into the health-care industry now includes reporting on the quality of hospitals. The current ratings evaluated more than 2,000 acute-care hospitals in the U.S. and came up with several rankings.
The first rating includes “patient outcomes,” which is a conglomerate of hospital-acquired central-line-associated bloodstream infection (CLABSI) rates, select surgical-site-infection [SSI] rates, 30-day readmission rates (for acute MI [AMI], congestive heart failure [CHF], and pneumonia), and eight “Patient Safety Indicators” (derived from definitions from the Agency for Healthcare Research & Quality [AHRQ], and includes pressure ulcers, pneumothorax, CLABSI, accidental puncture injury during surgery, and four postoperative complications, including VTE, sepsis, hip fracture, and wound dehiscence).
It also includes ratings of the patient experience (from a subset of HCAHPS questions) and two measures of hospital practices, including the use of electronic health records (from the American Hospital Association) and the use of “double scans” (simultaneous thoracic and abdominal CT scans).
From all of these ratings, Consumer Reports combined some of the metrics to arrive at a “Safety Score,” which ranges from 0 to 100 (100 being the safest), based on five categories, including infections (CLABSI and SSI), readmission rates (for AMI, CHF, and pneumonia), patient ratings of communication about their medications and about their discharge process, rate of double scans, and avoidance of the aforementioned AHRQ Patient Safety Indicators.
As to how potential patients are supposed to use this information, Consumer Reports gives the following advice to those wanting to know how the ratings can help a patient get better care: “They can help you compare hospitals in your area so you can choose the one that’s best for you. Even if you don’t have a choice of hospitals, our ratings can alert you to particular concerns so you can take steps to prevent problems no matter which hospital you go to. For example, if a hospital scores low in communicating with patients about what to do when they’re discharged, you should ask about discharge planning at the hospital you choose and make sure you know what to do when you leave.”
Overall, the average Safety Score for included hospitals was a 49, with a range from 14 to 74 across the U.S. Teaching hospitals were among the lowest scorers, with two-thirds of them rated below average.
At first blush, the numbers seem humbling, even startling, but it is not clear if they reflect bad care or bad metrics. Consumer Reports, similar to many other rating scales, has glued together a hodge-podge of different metrics and converted them into a summary score that may or may not line up with other organizational ratings (e.g. U.S. News and World Report, Leapfrog Group, Healthgrades, etc). Consumer Reports does acknowledge that none of the information for their rankings is actually collected from Consumer Reports but from other sources, such as the Centers for Medicare & Medicaid Services (CMS) and the American Hospital Association (AHA).
The Bottom Line
Despite all this attention from Consumer Reports and others, online ratings are only used by about 14% of consumers to review hospitals or health-care facilities and by about 17% of consumers to review physicians or other health-care providers.2 Although the uptick is relatively low for use of online ratings to seek health care, that likely will change as the measurements get better and are more reflective of true care quality.
The bottom line for consumers is: Where do I want to be hospitalized when I get sick, and can I tell at the front end in which aspects a hospital is going to do well?
I think the answer for consumers should be to stay informed, always have an advocate at your side, and never stop asking questions.And for now, relegate Consumer Reports to purchases, not health care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Consumer Reports. How we rate hospitals. Consumer Reports website. Available at: http://www.consumerreports.org/cro/2012/10/how-we-rate-hospitals/index.htm. Accessed May 12, 2013.
- Pew Internet & American Life Project. Peer-to-peer health care. Pew Internet website. Available at: http://www.pewinternet.org/Reports/2013/Health-online/Part-Two/Section-2.aspx. Accessed May 12, 2013.
Who doesn’t know and love Consumer Reports? I personally have used this product to help me make a wide range of purchases, from child-care products to a new automobile. Consumer Reports has enjoyed a relatively unblemished reputation since its inception as an unbiased repository of invaluable information for consumers. This nonprofit advocacy organization advises consumers looking to purchase anything from small, menial items (e.g. blenders and toasters) to large, expensive ones (e.g. computers, lawn mowers, cars). It has been categorizing and publishing large-scale consumer feedback and in-house testing since 1936. According to Wikipedia, Consumer Reports has more than 7 million subscribers and runs a budget in excess of $21 million annually.
One of the reasons for its longstanding success is that it does not appear to have any hidden agenda. It does not have any partiality to a specific company or service, and therefore has maintained its impartial stance during testing and evaluation of any good or service. Its Consumer Reports magazine houses no advertisements in order to maintain its objectivity. Its only agenda is to reflect the interests and opinions of the consumers themselves, and its mission is to provide a “fair, just, and safe marketplace for all consumers and to empower consumers to protect themselves.”1 A perfect agent from which to seek advice.
And as a company, it has grown with the times, as it now hosts a variety of platforms from which consumers can seek advice. It has long hosted a website (ConsumerReports.org). Now it has Consumer Reports Television and The Consumerist blog, the latter of which accepts “tips” from anyone on what stories to cover, helpful tips for consumers, or interesting pictures. For a few years, there was also Consumer Reports WebWatch, which was aimed at improving the credibility of websites through rigorous investigative reporting.
So it seems that Consumer Reports could be a good avenue to seek advice on where to “consume” health care. And, in fact, it is now in the business of rating the health-care industry. Recent blog posts from Consumer Reports have entailed topics as wide-ranging as the number of uninsured in the U.S. to the number and types of recalls of food products.
The health part of the website covers beauty and personal care (sunscreens and anti-wrinkle serums), exercise and fitness (bikes and diet plans), foods (coffee to frozen meals), home medical supplies (heart rate and blood pressure monitors), vitamins, supplements, and, last but not least, health services. This last section rates health insurance, heart surgeons, heart screening tests, and hospitals.
It even goes so far as to “rate” medications; its Best Buy Drugs compares the cost and effectiveness of a variety of prescription drugs ranging from anti-hypertensives to diabetic agents.
In Focus: Hospitals
Consumer Reports’ latest foray into the health-care industry now includes reporting on the quality of hospitals. The current ratings evaluated more than 2,000 acute-care hospitals in the U.S. and came up with several rankings.
The first rating includes “patient outcomes,” which is a conglomerate of hospital-acquired central-line-associated bloodstream infection (CLABSI) rates, select surgical-site-infection [SSI] rates, 30-day readmission rates (for acute MI [AMI], congestive heart failure [CHF], and pneumonia), and eight “Patient Safety Indicators” (derived from definitions from the Agency for Healthcare Research & Quality [AHRQ], and includes pressure ulcers, pneumothorax, CLABSI, accidental puncture injury during surgery, and four postoperative complications, including VTE, sepsis, hip fracture, and wound dehiscence).
It also includes ratings of the patient experience (from a subset of HCAHPS questions) and two measures of hospital practices, including the use of electronic health records (from the American Hospital Association) and the use of “double scans” (simultaneous thoracic and abdominal CT scans).
From all of these ratings, Consumer Reports combined some of the metrics to arrive at a “Safety Score,” which ranges from 0 to 100 (100 being the safest), based on five categories, including infections (CLABSI and SSI), readmission rates (for AMI, CHF, and pneumonia), patient ratings of communication about their medications and about their discharge process, rate of double scans, and avoidance of the aforementioned AHRQ Patient Safety Indicators.
As to how potential patients are supposed to use this information, Consumer Reports gives the following advice to those wanting to know how the ratings can help a patient get better care: “They can help you compare hospitals in your area so you can choose the one that’s best for you. Even if you don’t have a choice of hospitals, our ratings can alert you to particular concerns so you can take steps to prevent problems no matter which hospital you go to. For example, if a hospital scores low in communicating with patients about what to do when they’re discharged, you should ask about discharge planning at the hospital you choose and make sure you know what to do when you leave.”
Overall, the average Safety Score for included hospitals was a 49, with a range from 14 to 74 across the U.S. Teaching hospitals were among the lowest scorers, with two-thirds of them rated below average.
At first blush, the numbers seem humbling, even startling, but it is not clear if they reflect bad care or bad metrics. Consumer Reports, similar to many other rating scales, has glued together a hodge-podge of different metrics and converted them into a summary score that may or may not line up with other organizational ratings (e.g. U.S. News and World Report, Leapfrog Group, Healthgrades, etc). Consumer Reports does acknowledge that none of the information for their rankings is actually collected from Consumer Reports but from other sources, such as the Centers for Medicare & Medicaid Services (CMS) and the American Hospital Association (AHA).
The Bottom Line
Despite all this attention from Consumer Reports and others, online ratings are only used by about 14% of consumers to review hospitals or health-care facilities and by about 17% of consumers to review physicians or other health-care providers.2 Although the uptick is relatively low for use of online ratings to seek health care, that likely will change as the measurements get better and are more reflective of true care quality.
The bottom line for consumers is: Where do I want to be hospitalized when I get sick, and can I tell at the front end in which aspects a hospital is going to do well?
I think the answer for consumers should be to stay informed, always have an advocate at your side, and never stop asking questions.And for now, relegate Consumer Reports to purchases, not health care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Consumer Reports. How we rate hospitals. Consumer Reports website. Available at: http://www.consumerreports.org/cro/2012/10/how-we-rate-hospitals/index.htm. Accessed May 12, 2013.
- Pew Internet & American Life Project. Peer-to-peer health care. Pew Internet website. Available at: http://www.pewinternet.org/Reports/2013/Health-online/Part-Two/Section-2.aspx. Accessed May 12, 2013.
Who doesn’t know and love Consumer Reports? I personally have used this product to help me make a wide range of purchases, from child-care products to a new automobile. Consumer Reports has enjoyed a relatively unblemished reputation since its inception as an unbiased repository of invaluable information for consumers. This nonprofit advocacy organization advises consumers looking to purchase anything from small, menial items (e.g. blenders and toasters) to large, expensive ones (e.g. computers, lawn mowers, cars). It has been categorizing and publishing large-scale consumer feedback and in-house testing since 1936. According to Wikipedia, Consumer Reports has more than 7 million subscribers and runs a budget in excess of $21 million annually.
One of the reasons for its longstanding success is that it does not appear to have any hidden agenda. It does not have any partiality to a specific company or service, and therefore has maintained its impartial stance during testing and evaluation of any good or service. Its Consumer Reports magazine houses no advertisements in order to maintain its objectivity. Its only agenda is to reflect the interests and opinions of the consumers themselves, and its mission is to provide a “fair, just, and safe marketplace for all consumers and to empower consumers to protect themselves.”1 A perfect agent from which to seek advice.
And as a company, it has grown with the times, as it now hosts a variety of platforms from which consumers can seek advice. It has long hosted a website (ConsumerReports.org). Now it has Consumer Reports Television and The Consumerist blog, the latter of which accepts “tips” from anyone on what stories to cover, helpful tips for consumers, or interesting pictures. For a few years, there was also Consumer Reports WebWatch, which was aimed at improving the credibility of websites through rigorous investigative reporting.
So it seems that Consumer Reports could be a good avenue to seek advice on where to “consume” health care. And, in fact, it is now in the business of rating the health-care industry. Recent blog posts from Consumer Reports have entailed topics as wide-ranging as the number of uninsured in the U.S. to the number and types of recalls of food products.
The health part of the website covers beauty and personal care (sunscreens and anti-wrinkle serums), exercise and fitness (bikes and diet plans), foods (coffee to frozen meals), home medical supplies (heart rate and blood pressure monitors), vitamins, supplements, and, last but not least, health services. This last section rates health insurance, heart surgeons, heart screening tests, and hospitals.
It even goes so far as to “rate” medications; its Best Buy Drugs compares the cost and effectiveness of a variety of prescription drugs ranging from anti-hypertensives to diabetic agents.
In Focus: Hospitals
Consumer Reports’ latest foray into the health-care industry now includes reporting on the quality of hospitals. The current ratings evaluated more than 2,000 acute-care hospitals in the U.S. and came up with several rankings.
The first rating includes “patient outcomes,” which is a conglomerate of hospital-acquired central-line-associated bloodstream infection (CLABSI) rates, select surgical-site-infection [SSI] rates, 30-day readmission rates (for acute MI [AMI], congestive heart failure [CHF], and pneumonia), and eight “Patient Safety Indicators” (derived from definitions from the Agency for Healthcare Research & Quality [AHRQ], and includes pressure ulcers, pneumothorax, CLABSI, accidental puncture injury during surgery, and four postoperative complications, including VTE, sepsis, hip fracture, and wound dehiscence).
It also includes ratings of the patient experience (from a subset of HCAHPS questions) and two measures of hospital practices, including the use of electronic health records (from the American Hospital Association) and the use of “double scans” (simultaneous thoracic and abdominal CT scans).
From all of these ratings, Consumer Reports combined some of the metrics to arrive at a “Safety Score,” which ranges from 0 to 100 (100 being the safest), based on five categories, including infections (CLABSI and SSI), readmission rates (for AMI, CHF, and pneumonia), patient ratings of communication about their medications and about their discharge process, rate of double scans, and avoidance of the aforementioned AHRQ Patient Safety Indicators.
As to how potential patients are supposed to use this information, Consumer Reports gives the following advice to those wanting to know how the ratings can help a patient get better care: “They can help you compare hospitals in your area so you can choose the one that’s best for you. Even if you don’t have a choice of hospitals, our ratings can alert you to particular concerns so you can take steps to prevent problems no matter which hospital you go to. For example, if a hospital scores low in communicating with patients about what to do when they’re discharged, you should ask about discharge planning at the hospital you choose and make sure you know what to do when you leave.”
Overall, the average Safety Score for included hospitals was a 49, with a range from 14 to 74 across the U.S. Teaching hospitals were among the lowest scorers, with two-thirds of them rated below average.
At first blush, the numbers seem humbling, even startling, but it is not clear if they reflect bad care or bad metrics. Consumer Reports, similar to many other rating scales, has glued together a hodge-podge of different metrics and converted them into a summary score that may or may not line up with other organizational ratings (e.g. U.S. News and World Report, Leapfrog Group, Healthgrades, etc). Consumer Reports does acknowledge that none of the information for their rankings is actually collected from Consumer Reports but from other sources, such as the Centers for Medicare & Medicaid Services (CMS) and the American Hospital Association (AHA).
The Bottom Line
Despite all this attention from Consumer Reports and others, online ratings are only used by about 14% of consumers to review hospitals or health-care facilities and by about 17% of consumers to review physicians or other health-care providers.2 Although the uptick is relatively low for use of online ratings to seek health care, that likely will change as the measurements get better and are more reflective of true care quality.
The bottom line for consumers is: Where do I want to be hospitalized when I get sick, and can I tell at the front end in which aspects a hospital is going to do well?
I think the answer for consumers should be to stay informed, always have an advocate at your side, and never stop asking questions.And for now, relegate Consumer Reports to purchases, not health care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Consumer Reports. How we rate hospitals. Consumer Reports website. Available at: http://www.consumerreports.org/cro/2012/10/how-we-rate-hospitals/index.htm. Accessed May 12, 2013.
- Pew Internet & American Life Project. Peer-to-peer health care. Pew Internet website. Available at: http://www.pewinternet.org/Reports/2013/Health-online/Part-Two/Section-2.aspx. Accessed May 12, 2013.
Medicare Outlines Anticipated Funding Changes Under Affordable Care Act
The Centers for Medicare & Medicaid Services (CMS) recently released a few Fact Sheets on how they anticipate funding changes on a few of their programs that were implemented (or sustained) under the Affordable Care Act. As a background, CMS pays most acute-care hospitals by prospectively determining payment based on a patient’s diagnosis and the severity of illness within that diagnosis (e.g. “MS-DRG”). These payment amounts are updated annually after evaluating several factors, including the costs associated with the delivery of care.
One of the most major changes described in the Fact Sheet that will affect hospitalists is how CMS will review inpatient stays based on the number of nights in the hospital. CMS has proposed that any patient who stays in the hospital for two or more “midnights” should be appropriate for payment under Medicare Part A. For those who stay in the hospital for only one (or zero) midnights, payment under Medicare Part A will only be appropriate if:
- There is sufficient documentation at the time of admission that the anticipated length of stay is two or more nights; and.
- Further documentation that circumstances changed, and the hospital stay ended prematurely because of those changes.
Overall for hospitalists, this should substantially simplify the admitting process, whereby most inpatients being admitted with the anticipation of two or more nights should qualify for an inpatient stay. This also reduces the administrative burden of correcting the “inpatient” versus “observation” designation, which keeps many hospital staffs entirely too busy. This change also should relieve a significant burden from the patients and their families, who if kept in observation for a period of time, may have to pay substantially out of pocket to make up for the difference between the cost of the stay and the reimbursement from CMS for observation status. So this is one of the moves that CMS is making to simplify (and not complicate) an already too-complicated payment system. This should go into effect October 2013 and will be a sigh of much relief from many of us.
A few other anticipated changes that will affect hospitalists include:
Payments for Unfunded Care
Another major change that will go into affect October 2013 is the amount of monies received by hospitals that care for unfunded patients. These payments historically have been made to “Disproportionate Share Hospitals” (DSH), which are hospitals that care for a higher percentage of unfunded patients. Under the Affordable Care Act, only 25% of these payments will be distributed to DSH hospitals; the remaining 75% will be reduced based on the number of uninsured in the U.S., then redistributed to DSH hospitals based on their portion of uninsured care delivered.
Most DSH hospitals should expect a decrease in DSH payments, the amount of which will depend on their share of unfunded patients.
Any reduction in the “bottom line” to the hospital can affect hospitalists, especially those who are directly employed by the hospital.
Hospital-Acquired Conditions
CMS has long had the Hospital-Acquired Condition (HAC) program in effect, which has the ability to reduce the amount of payment for inpatients who acquire a HAC during their hospital stay. Starting in October 2014, CMS will impose additional financial penalties for hospitals with high HAC rates.
Specifically, those hospitals in the highest 25th percentile of HAC rates will be penalized 1% of their overall CMS payments. Another proposed change is that the following be included in the HAC reduction plan (two “domains” of measures):
- Domain No. 1: Six of the AHRQ Patient Safety Indicators (PSIs), including pressure ulcers, foreign bodies left in after surgery, iatrogenic pneumothorax, postoperative physiologic or metabolic derangements, postoperative VTE, and accidental puncture/laceration.
- Domain No. 2: Central-line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTIs).
The domains will be weighted equally, and an average score will determine the total score. There will be some methodology for risk adjustment, and hospitals will be given a review and comment period to validate their own scores.
Most hospitalists have at least indirect control over many of these HACs,and all need to pay very close attention to their hospital’s rates of these now and in the future.
Readmissions
As we all know, the Hospital Readmission Reduction program went into effect October 2012; it placed 1% of CMS payments at risk. This will increase to 2% of payments as of October 2013. CMS will continue to use AMI, CHF, and pneumonia as the three conditions under which the readmissions are measured but will put in some methodology to account for planned readmissions.
In addition, in October 2014, they plan to add readmission rates for COPD and for hip/knee arthroplasty.
Hospitalists will continue to need to progress their transitions of care programs, at least for these five patients conditions but more likely (and more effectively) for all hospital discharges.
Quality Measures
Currently more than 99% of acute-care hospitals participate in the pay-for-reporting quality program through CMS, the results of which have been displayed on the Hospital Compare website (www.hospitalcompare.hhs.gov) for years. The program started in 2004 with 10 quality metrics and now includes 57 metrics. These include process and outcome measures for AMI, CHF, and pneumonia, as well as process measures for surgical care, HACs, and patient-satisfaction surveys, among others.
This program will continue to expand over time, including hospital-acquired MRSA and Clostridium difficile rates. The few hospitals not participating will have their CMS annual payments reduced by 2%.
EHR Incentives
CMS is evaluating ways to reduce the burden of reporting by aligning EHR incentives with the Inpatient Quality Reporting program.
Summary
After an open commentary period, the Final Rule will be published Aug. 1, and will become effective for discharges on or after Oct. 1. Although CMS will continue to expand the total number of measures that need to be reported, and the penalties for non-reporting or low performance will continue to escalate, CMS is at least attempting to reduce the overall burden of reporting by combining measures and programs over time and using EHRs to facilitate the bulk of reporting over time.
The global message to hospitalists is: Continue to focus on reducing the burden of HACs, enhance throughput, and carefully and thoughtfully transition patients to the next provider after their hospital discharge. All in all, although at times this can feel overwhelming, these changes represent the right direction to move for high-quality and safe patient care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
The Centers for Medicare & Medicaid Services (CMS) recently released a few Fact Sheets on how they anticipate funding changes on a few of their programs that were implemented (or sustained) under the Affordable Care Act. As a background, CMS pays most acute-care hospitals by prospectively determining payment based on a patient’s diagnosis and the severity of illness within that diagnosis (e.g. “MS-DRG”). These payment amounts are updated annually after evaluating several factors, including the costs associated with the delivery of care.
One of the most major changes described in the Fact Sheet that will affect hospitalists is how CMS will review inpatient stays based on the number of nights in the hospital. CMS has proposed that any patient who stays in the hospital for two or more “midnights” should be appropriate for payment under Medicare Part A. For those who stay in the hospital for only one (or zero) midnights, payment under Medicare Part A will only be appropriate if:
- There is sufficient documentation at the time of admission that the anticipated length of stay is two or more nights; and.
- Further documentation that circumstances changed, and the hospital stay ended prematurely because of those changes.
Overall for hospitalists, this should substantially simplify the admitting process, whereby most inpatients being admitted with the anticipation of two or more nights should qualify for an inpatient stay. This also reduces the administrative burden of correcting the “inpatient” versus “observation” designation, which keeps many hospital staffs entirely too busy. This change also should relieve a significant burden from the patients and their families, who if kept in observation for a period of time, may have to pay substantially out of pocket to make up for the difference between the cost of the stay and the reimbursement from CMS for observation status. So this is one of the moves that CMS is making to simplify (and not complicate) an already too-complicated payment system. This should go into effect October 2013 and will be a sigh of much relief from many of us.
A few other anticipated changes that will affect hospitalists include:
Payments for Unfunded Care
Another major change that will go into affect October 2013 is the amount of monies received by hospitals that care for unfunded patients. These payments historically have been made to “Disproportionate Share Hospitals” (DSH), which are hospitals that care for a higher percentage of unfunded patients. Under the Affordable Care Act, only 25% of these payments will be distributed to DSH hospitals; the remaining 75% will be reduced based on the number of uninsured in the U.S., then redistributed to DSH hospitals based on their portion of uninsured care delivered.
Most DSH hospitals should expect a decrease in DSH payments, the amount of which will depend on their share of unfunded patients.
Any reduction in the “bottom line” to the hospital can affect hospitalists, especially those who are directly employed by the hospital.
Hospital-Acquired Conditions
CMS has long had the Hospital-Acquired Condition (HAC) program in effect, which has the ability to reduce the amount of payment for inpatients who acquire a HAC during their hospital stay. Starting in October 2014, CMS will impose additional financial penalties for hospitals with high HAC rates.
Specifically, those hospitals in the highest 25th percentile of HAC rates will be penalized 1% of their overall CMS payments. Another proposed change is that the following be included in the HAC reduction plan (two “domains” of measures):
- Domain No. 1: Six of the AHRQ Patient Safety Indicators (PSIs), including pressure ulcers, foreign bodies left in after surgery, iatrogenic pneumothorax, postoperative physiologic or metabolic derangements, postoperative VTE, and accidental puncture/laceration.
- Domain No. 2: Central-line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTIs).
The domains will be weighted equally, and an average score will determine the total score. There will be some methodology for risk adjustment, and hospitals will be given a review and comment period to validate their own scores.
Most hospitalists have at least indirect control over many of these HACs,and all need to pay very close attention to their hospital’s rates of these now and in the future.
Readmissions
As we all know, the Hospital Readmission Reduction program went into effect October 2012; it placed 1% of CMS payments at risk. This will increase to 2% of payments as of October 2013. CMS will continue to use AMI, CHF, and pneumonia as the three conditions under which the readmissions are measured but will put in some methodology to account for planned readmissions.
In addition, in October 2014, they plan to add readmission rates for COPD and for hip/knee arthroplasty.
Hospitalists will continue to need to progress their transitions of care programs, at least for these five patients conditions but more likely (and more effectively) for all hospital discharges.
Quality Measures
Currently more than 99% of acute-care hospitals participate in the pay-for-reporting quality program through CMS, the results of which have been displayed on the Hospital Compare website (www.hospitalcompare.hhs.gov) for years. The program started in 2004 with 10 quality metrics and now includes 57 metrics. These include process and outcome measures for AMI, CHF, and pneumonia, as well as process measures for surgical care, HACs, and patient-satisfaction surveys, among others.
This program will continue to expand over time, including hospital-acquired MRSA and Clostridium difficile rates. The few hospitals not participating will have their CMS annual payments reduced by 2%.
EHR Incentives
CMS is evaluating ways to reduce the burden of reporting by aligning EHR incentives with the Inpatient Quality Reporting program.
Summary
After an open commentary period, the Final Rule will be published Aug. 1, and will become effective for discharges on or after Oct. 1. Although CMS will continue to expand the total number of measures that need to be reported, and the penalties for non-reporting or low performance will continue to escalate, CMS is at least attempting to reduce the overall burden of reporting by combining measures and programs over time and using EHRs to facilitate the bulk of reporting over time.
The global message to hospitalists is: Continue to focus on reducing the burden of HACs, enhance throughput, and carefully and thoughtfully transition patients to the next provider after their hospital discharge. All in all, although at times this can feel overwhelming, these changes represent the right direction to move for high-quality and safe patient care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
The Centers for Medicare & Medicaid Services (CMS) recently released a few Fact Sheets on how they anticipate funding changes on a few of their programs that were implemented (or sustained) under the Affordable Care Act. As a background, CMS pays most acute-care hospitals by prospectively determining payment based on a patient’s diagnosis and the severity of illness within that diagnosis (e.g. “MS-DRG”). These payment amounts are updated annually after evaluating several factors, including the costs associated with the delivery of care.
One of the most major changes described in the Fact Sheet that will affect hospitalists is how CMS will review inpatient stays based on the number of nights in the hospital. CMS has proposed that any patient who stays in the hospital for two or more “midnights” should be appropriate for payment under Medicare Part A. For those who stay in the hospital for only one (or zero) midnights, payment under Medicare Part A will only be appropriate if:
- There is sufficient documentation at the time of admission that the anticipated length of stay is two or more nights; and.
- Further documentation that circumstances changed, and the hospital stay ended prematurely because of those changes.
Overall for hospitalists, this should substantially simplify the admitting process, whereby most inpatients being admitted with the anticipation of two or more nights should qualify for an inpatient stay. This also reduces the administrative burden of correcting the “inpatient” versus “observation” designation, which keeps many hospital staffs entirely too busy. This change also should relieve a significant burden from the patients and their families, who if kept in observation for a period of time, may have to pay substantially out of pocket to make up for the difference between the cost of the stay and the reimbursement from CMS for observation status. So this is one of the moves that CMS is making to simplify (and not complicate) an already too-complicated payment system. This should go into effect October 2013 and will be a sigh of much relief from many of us.
A few other anticipated changes that will affect hospitalists include:
Payments for Unfunded Care
Another major change that will go into affect October 2013 is the amount of monies received by hospitals that care for unfunded patients. These payments historically have been made to “Disproportionate Share Hospitals” (DSH), which are hospitals that care for a higher percentage of unfunded patients. Under the Affordable Care Act, only 25% of these payments will be distributed to DSH hospitals; the remaining 75% will be reduced based on the number of uninsured in the U.S., then redistributed to DSH hospitals based on their portion of uninsured care delivered.
Most DSH hospitals should expect a decrease in DSH payments, the amount of which will depend on their share of unfunded patients.
Any reduction in the “bottom line” to the hospital can affect hospitalists, especially those who are directly employed by the hospital.
Hospital-Acquired Conditions
CMS has long had the Hospital-Acquired Condition (HAC) program in effect, which has the ability to reduce the amount of payment for inpatients who acquire a HAC during their hospital stay. Starting in October 2014, CMS will impose additional financial penalties for hospitals with high HAC rates.
Specifically, those hospitals in the highest 25th percentile of HAC rates will be penalized 1% of their overall CMS payments. Another proposed change is that the following be included in the HAC reduction plan (two “domains” of measures):
- Domain No. 1: Six of the AHRQ Patient Safety Indicators (PSIs), including pressure ulcers, foreign bodies left in after surgery, iatrogenic pneumothorax, postoperative physiologic or metabolic derangements, postoperative VTE, and accidental puncture/laceration.
- Domain No. 2: Central-line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTIs).
The domains will be weighted equally, and an average score will determine the total score. There will be some methodology for risk adjustment, and hospitals will be given a review and comment period to validate their own scores.
Most hospitalists have at least indirect control over many of these HACs,and all need to pay very close attention to their hospital’s rates of these now and in the future.
Readmissions
As we all know, the Hospital Readmission Reduction program went into effect October 2012; it placed 1% of CMS payments at risk. This will increase to 2% of payments as of October 2013. CMS will continue to use AMI, CHF, and pneumonia as the three conditions under which the readmissions are measured but will put in some methodology to account for planned readmissions.
In addition, in October 2014, they plan to add readmission rates for COPD and for hip/knee arthroplasty.
Hospitalists will continue to need to progress their transitions of care programs, at least for these five patients conditions but more likely (and more effectively) for all hospital discharges.
Quality Measures
Currently more than 99% of acute-care hospitals participate in the pay-for-reporting quality program through CMS, the results of which have been displayed on the Hospital Compare website (www.hospitalcompare.hhs.gov) for years. The program started in 2004 with 10 quality metrics and now includes 57 metrics. These include process and outcome measures for AMI, CHF, and pneumonia, as well as process measures for surgical care, HACs, and patient-satisfaction surveys, among others.
This program will continue to expand over time, including hospital-acquired MRSA and Clostridium difficile rates. The few hospitals not participating will have their CMS annual payments reduced by 2%.
EHR Incentives
CMS is evaluating ways to reduce the burden of reporting by aligning EHR incentives with the Inpatient Quality Reporting program.
Summary
After an open commentary period, the Final Rule will be published Aug. 1, and will become effective for discharges on or after Oct. 1. Although CMS will continue to expand the total number of measures that need to be reported, and the penalties for non-reporting or low performance will continue to escalate, CMS is at least attempting to reduce the overall burden of reporting by combining measures and programs over time and using EHRs to facilitate the bulk of reporting over time.
The global message to hospitalists is: Continue to focus on reducing the burden of HACs, enhance throughput, and carefully and thoughtfully transition patients to the next provider after their hospital discharge. All in all, although at times this can feel overwhelming, these changes represent the right direction to move for high-quality and safe patient care.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
Strong Leadership Evident at HM13
After wrapping up the SHM annual meeting, I was left with a sense of security about hospital medicine’s future. This security I can summarize in a single word: leadership. SHM has long had a strong set of leaders, which are needed now more than ever. With explosive expansion in volume and scope, hospitalist practice is going to require tireless leadership in the coming years and decades to ensure our trajectory is strategic and viable.
The Science
Wikipedia describes leadership as “a process of social influence in which one person can enlist the aid and support of others in the accomplishment of a common task.” Notice a few key words in that definition? “Process,” which implies that it takes time, patience, and tenacity. It is not something that automatically happens without any time or effort. Also notice the word “influence,” which does not include “power” or “authority” or “pay grade”—all terms that are entirely overused and misused in the medical industry.
There is a wealth of literature describing what leadership is and what it takes to be a leader. There are an abundance of theories on what traits and characteristics make up a good leader, and an equal abundance of theories on how great leaders evolve. Some subscribe to the inherited theory, in which genetic makeup will at least partially dictate whether you will be a “natural-born” a leader. Others subscribe to the belief that leadership is more situational, whereby leaders are effective in some situations but ineffective in others. Still others believe leaders emerge as a mixture of nature and nurture, that most good leaders can lead in a variety of climates and situations, but that a perfect leadership situation might not emerge for any one leader. For other leaders, a perfect situational opportunity might emerge that suits their leadership style, and transformational change can occur under their direction.
The science of leadership has found that some personal traits are more commonly associated with leaders than nonleaders, including extraversion, self-efficacy, conscientiousness, intelligence, and openness to experience. However, absence of these characteristics does not guarantee a hopeless leadership void; equally true, the presence of them does not guarantee good leadership.
The Art
So one can go on for the length of an encyclopedia about the science of leadership, but what about the art of leadership? The ability of a leader to “read the audience,” to “take the pulse” of their staff, to strategize their next foray into new territory, or to say no to a new (seemingly exciting) opportunity. It is the art of leadership that is much more intriguing. I have had the good fortune of seeing a variety of incredible leaders at work, both within and outside of SHM, including their artful mastery of difficult situations.
There were plenty of these artful masters exemplified over the course of the three-day meeting worthy of mention. Three outgoing board members have long led the society down many strategic pathways with brilliance and ease. Lakshmi Halasyamani is wise, kind, and even-keeled. Eric Siegal is sharp-minded, sharp-witted, and sharp-tongued. Joe Li is authentic, energetic, and conscientious. Three oncoming members will bring vast experience and collective wisdom to the SHM board—Brad Sharpe, Patrick Torcson, and Howard Epstein.
In the brief session celebrating the past presidents, I was struck by the number of impressive names and faces who all have gone on to do an array of other jobs. Together, they represent a collective footprint of impressive magnitude. As past president Shaun Frost gave his thoughtful exit speech, and new president Eric Howell gave his lively, energetic, and humorous entry speech, I was reassured that we indeed are in good hands, with a foothold of grounded past leaders, and a wealth of talent on the launching board. Moreover, the introduction of three new Masters in Hospital Medicine—Scott Flanders, Jeff Wiese, and David Meltzer—adds to the collective wisdom and talent of SHM.
We were blessed at the meeting by the presence of other incredible leaders in health care, including Patrick Conway and David Feinberg. Dr. Conway, the CMO of Medicare, is a service-minded colleague determined to make CMS more transparent, easier to traverse, and more aligned with what its recipients really need. Dr. Feinberg is a genuinely compassionate physician who has transformed UCLA medical center from a Motel 6 to a Ritz-Carlton in customer service. I have seen him speak before and had quite a bit of respect for him to begin with, but to watch how he handled a flock of unwieldy and uninvited guests on the stage was more than what anyone could expect from a great leader.
The Art of the Science
As we continue this unwieldy and unpredictable journey that we call health care and hospital medicine, the need for effective leadership within the industry will continue to increase. And there is little need to argue about whether leaders are naturally born, because there are more leaders needed than there are natural-born. So either way, many of us have to figure out how to be leaders, whether of a small program, a newly formed group, or a large conglomerate. And whether your contribution is large or small, it will be a contribution nonetheless.
Just as Mother Teresa was once presented with a statement from a reporter about how her care for the poor and neglected was just a “drop in the bucket” on combating poverty and dispassion. She paused and agreed: “Yes, it is just a drop in the bucket but it’s my drop.”
Just as Dr. Feinberg recounted when he was first offered the CEO position at UCLA, as an interim and unlikely candidate, he didn’t know what to do, so he just started doing what he knew how to do best. He just started walking around the hospital seeing patients, listening, visiting, saying “hello,” and giving out his business cards (his drop in the bucket). He wasn’t trying to do anything terribly innovative or strategic at the time—at least, not that he admits to. And anyone who watches Larry Wellikson work a boardroom or a ballroom can learn something about the art of leadership.
So think of leadership not as a secret sauce, or set of skills that can only be relegated to those enshrined with the DNA of a Kennedy or an MBA from an Ivy League school. It is a willingness to try to get some drops in some buckets, and lead people in a common direction. It is about being unambiguously committed and completely authentic, with a little science, and a lot of art.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
After wrapping up the SHM annual meeting, I was left with a sense of security about hospital medicine’s future. This security I can summarize in a single word: leadership. SHM has long had a strong set of leaders, which are needed now more than ever. With explosive expansion in volume and scope, hospitalist practice is going to require tireless leadership in the coming years and decades to ensure our trajectory is strategic and viable.
The Science
Wikipedia describes leadership as “a process of social influence in which one person can enlist the aid and support of others in the accomplishment of a common task.” Notice a few key words in that definition? “Process,” which implies that it takes time, patience, and tenacity. It is not something that automatically happens without any time or effort. Also notice the word “influence,” which does not include “power” or “authority” or “pay grade”—all terms that are entirely overused and misused in the medical industry.
There is a wealth of literature describing what leadership is and what it takes to be a leader. There are an abundance of theories on what traits and characteristics make up a good leader, and an equal abundance of theories on how great leaders evolve. Some subscribe to the inherited theory, in which genetic makeup will at least partially dictate whether you will be a “natural-born” a leader. Others subscribe to the belief that leadership is more situational, whereby leaders are effective in some situations but ineffective in others. Still others believe leaders emerge as a mixture of nature and nurture, that most good leaders can lead in a variety of climates and situations, but that a perfect leadership situation might not emerge for any one leader. For other leaders, a perfect situational opportunity might emerge that suits their leadership style, and transformational change can occur under their direction.
The science of leadership has found that some personal traits are more commonly associated with leaders than nonleaders, including extraversion, self-efficacy, conscientiousness, intelligence, and openness to experience. However, absence of these characteristics does not guarantee a hopeless leadership void; equally true, the presence of them does not guarantee good leadership.
The Art
So one can go on for the length of an encyclopedia about the science of leadership, but what about the art of leadership? The ability of a leader to “read the audience,” to “take the pulse” of their staff, to strategize their next foray into new territory, or to say no to a new (seemingly exciting) opportunity. It is the art of leadership that is much more intriguing. I have had the good fortune of seeing a variety of incredible leaders at work, both within and outside of SHM, including their artful mastery of difficult situations.
There were plenty of these artful masters exemplified over the course of the three-day meeting worthy of mention. Three outgoing board members have long led the society down many strategic pathways with brilliance and ease. Lakshmi Halasyamani is wise, kind, and even-keeled. Eric Siegal is sharp-minded, sharp-witted, and sharp-tongued. Joe Li is authentic, energetic, and conscientious. Three oncoming members will bring vast experience and collective wisdom to the SHM board—Brad Sharpe, Patrick Torcson, and Howard Epstein.
In the brief session celebrating the past presidents, I was struck by the number of impressive names and faces who all have gone on to do an array of other jobs. Together, they represent a collective footprint of impressive magnitude. As past president Shaun Frost gave his thoughtful exit speech, and new president Eric Howell gave his lively, energetic, and humorous entry speech, I was reassured that we indeed are in good hands, with a foothold of grounded past leaders, and a wealth of talent on the launching board. Moreover, the introduction of three new Masters in Hospital Medicine—Scott Flanders, Jeff Wiese, and David Meltzer—adds to the collective wisdom and talent of SHM.
We were blessed at the meeting by the presence of other incredible leaders in health care, including Patrick Conway and David Feinberg. Dr. Conway, the CMO of Medicare, is a service-minded colleague determined to make CMS more transparent, easier to traverse, and more aligned with what its recipients really need. Dr. Feinberg is a genuinely compassionate physician who has transformed UCLA medical center from a Motel 6 to a Ritz-Carlton in customer service. I have seen him speak before and had quite a bit of respect for him to begin with, but to watch how he handled a flock of unwieldy and uninvited guests on the stage was more than what anyone could expect from a great leader.
The Art of the Science
As we continue this unwieldy and unpredictable journey that we call health care and hospital medicine, the need for effective leadership within the industry will continue to increase. And there is little need to argue about whether leaders are naturally born, because there are more leaders needed than there are natural-born. So either way, many of us have to figure out how to be leaders, whether of a small program, a newly formed group, or a large conglomerate. And whether your contribution is large or small, it will be a contribution nonetheless.
Just as Mother Teresa was once presented with a statement from a reporter about how her care for the poor and neglected was just a “drop in the bucket” on combating poverty and dispassion. She paused and agreed: “Yes, it is just a drop in the bucket but it’s my drop.”
Just as Dr. Feinberg recounted when he was first offered the CEO position at UCLA, as an interim and unlikely candidate, he didn’t know what to do, so he just started doing what he knew how to do best. He just started walking around the hospital seeing patients, listening, visiting, saying “hello,” and giving out his business cards (his drop in the bucket). He wasn’t trying to do anything terribly innovative or strategic at the time—at least, not that he admits to. And anyone who watches Larry Wellikson work a boardroom or a ballroom can learn something about the art of leadership.
So think of leadership not as a secret sauce, or set of skills that can only be relegated to those enshrined with the DNA of a Kennedy or an MBA from an Ivy League school. It is a willingness to try to get some drops in some buckets, and lead people in a common direction. It is about being unambiguously committed and completely authentic, with a little science, and a lot of art.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
After wrapping up the SHM annual meeting, I was left with a sense of security about hospital medicine’s future. This security I can summarize in a single word: leadership. SHM has long had a strong set of leaders, which are needed now more than ever. With explosive expansion in volume and scope, hospitalist practice is going to require tireless leadership in the coming years and decades to ensure our trajectory is strategic and viable.
The Science
Wikipedia describes leadership as “a process of social influence in which one person can enlist the aid and support of others in the accomplishment of a common task.” Notice a few key words in that definition? “Process,” which implies that it takes time, patience, and tenacity. It is not something that automatically happens without any time or effort. Also notice the word “influence,” which does not include “power” or “authority” or “pay grade”—all terms that are entirely overused and misused in the medical industry.
There is a wealth of literature describing what leadership is and what it takes to be a leader. There are an abundance of theories on what traits and characteristics make up a good leader, and an equal abundance of theories on how great leaders evolve. Some subscribe to the inherited theory, in which genetic makeup will at least partially dictate whether you will be a “natural-born” a leader. Others subscribe to the belief that leadership is more situational, whereby leaders are effective in some situations but ineffective in others. Still others believe leaders emerge as a mixture of nature and nurture, that most good leaders can lead in a variety of climates and situations, but that a perfect leadership situation might not emerge for any one leader. For other leaders, a perfect situational opportunity might emerge that suits their leadership style, and transformational change can occur under their direction.
The science of leadership has found that some personal traits are more commonly associated with leaders than nonleaders, including extraversion, self-efficacy, conscientiousness, intelligence, and openness to experience. However, absence of these characteristics does not guarantee a hopeless leadership void; equally true, the presence of them does not guarantee good leadership.
The Art
So one can go on for the length of an encyclopedia about the science of leadership, but what about the art of leadership? The ability of a leader to “read the audience,” to “take the pulse” of their staff, to strategize their next foray into new territory, or to say no to a new (seemingly exciting) opportunity. It is the art of leadership that is much more intriguing. I have had the good fortune of seeing a variety of incredible leaders at work, both within and outside of SHM, including their artful mastery of difficult situations.
There were plenty of these artful masters exemplified over the course of the three-day meeting worthy of mention. Three outgoing board members have long led the society down many strategic pathways with brilliance and ease. Lakshmi Halasyamani is wise, kind, and even-keeled. Eric Siegal is sharp-minded, sharp-witted, and sharp-tongued. Joe Li is authentic, energetic, and conscientious. Three oncoming members will bring vast experience and collective wisdom to the SHM board—Brad Sharpe, Patrick Torcson, and Howard Epstein.
In the brief session celebrating the past presidents, I was struck by the number of impressive names and faces who all have gone on to do an array of other jobs. Together, they represent a collective footprint of impressive magnitude. As past president Shaun Frost gave his thoughtful exit speech, and new president Eric Howell gave his lively, energetic, and humorous entry speech, I was reassured that we indeed are in good hands, with a foothold of grounded past leaders, and a wealth of talent on the launching board. Moreover, the introduction of three new Masters in Hospital Medicine—Scott Flanders, Jeff Wiese, and David Meltzer—adds to the collective wisdom and talent of SHM.
We were blessed at the meeting by the presence of other incredible leaders in health care, including Patrick Conway and David Feinberg. Dr. Conway, the CMO of Medicare, is a service-minded colleague determined to make CMS more transparent, easier to traverse, and more aligned with what its recipients really need. Dr. Feinberg is a genuinely compassionate physician who has transformed UCLA medical center from a Motel 6 to a Ritz-Carlton in customer service. I have seen him speak before and had quite a bit of respect for him to begin with, but to watch how he handled a flock of unwieldy and uninvited guests on the stage was more than what anyone could expect from a great leader.
The Art of the Science
As we continue this unwieldy and unpredictable journey that we call health care and hospital medicine, the need for effective leadership within the industry will continue to increase. And there is little need to argue about whether leaders are naturally born, because there are more leaders needed than there are natural-born. So either way, many of us have to figure out how to be leaders, whether of a small program, a newly formed group, or a large conglomerate. And whether your contribution is large or small, it will be a contribution nonetheless.
Just as Mother Teresa was once presented with a statement from a reporter about how her care for the poor and neglected was just a “drop in the bucket” on combating poverty and dispassion. She paused and agreed: “Yes, it is just a drop in the bucket but it’s my drop.”
Just as Dr. Feinberg recounted when he was first offered the CEO position at UCLA, as an interim and unlikely candidate, he didn’t know what to do, so he just started doing what he knew how to do best. He just started walking around the hospital seeing patients, listening, visiting, saying “hello,” and giving out his business cards (his drop in the bucket). He wasn’t trying to do anything terribly innovative or strategic at the time—at least, not that he admits to. And anyone who watches Larry Wellikson work a boardroom or a ballroom can learn something about the art of leadership.
So think of leadership not as a secret sauce, or set of skills that can only be relegated to those enshrined with the DNA of a Kennedy or an MBA from an Ivy League school. It is a willingness to try to get some drops in some buckets, and lead people in a common direction. It is about being unambiguously committed and completely authentic, with a little science, and a lot of art.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Lack of Transparency Plagues U.S. Health Care System
Everything has a price, and we all have become accustomed to knowing how much something is going to cost before we buy it. Generally, we start with thinking about how much we are willing to pay, then finding what we need within the range of what we expect to pay. Whether it is shopping on Amazon.com, negotiating the price with a landscaper, or going out to eat, we get to weigh the options in advance of acquiring the goods or services. And, generally ahead of the purchase of big-ticket items, we get an itemized list of what is available.
I recently had to buy a car. Some of the many decisions that went into the purchase were whether to include some of the offered amenities, including:
- “Surround sound”;
- Seat heaters;
- Blind-spot indicator system;
- Premium floor mat package; and
- Built-in GPS.
My husband and I thought about the price of each of these line items relative to what we were going to “get out of it”—e.g., the value. Seat heaters in South Carolina? No, thanks. Surround sound? We had to flip a coin on that one. Safety features? Absolutely. Premium floor mat package? Only if they were guaranteed to be Fruit Roll-Ups-resistant.
Over the course of several negotiations, we picked and chose options that were highly likely to add value (safety, comfort, convenience) and omitted the rest. Then we settled on a total price, paid the negotiated price, and drove away fairly content.
Now, this doesn’t mean that we actually knew the cost of adding each of those amenities into our new car; would anyone actually be able to tell us exactly how much each of those features cost to innovate, create, and install? Probably not, but they might be able to give us a pretty good estimate, as well as an estimate of how much had been added in to ship it to the dealer, to pay the overhead for the dealership, and to pay the dealership staff (from the front desk to the CEO). And we could feel pretty certain that most buyers would be presented with similar prices, regardless of their personal characteristics.
So all in all, there was a reasonable amount of transparency around the cost and the price of the car and all of its amenities, as there would be in most industries. Except in health care.
A Ton of Money, for What?
There was a fascinating article in the March 4 edition of Time titled “Bitter Pill” that discussed the cost and the price of health-care services.1 It certainly is a worthy topic, as the U.S. spends about 20% of our gross domestic product on health care, whereas most other developed countries spend half of that. In fact, according to the article, the U.S. spends more on health care annually ($2.8 trillion) than the top 10 countries combined—Japan, Germany, France, China, United Kingdom, Italy, Canada, Brazil, Spain, and Australia.
About $800 billion of our health care is paid out annually by the Centers for Medicare & Medicaid Services (CMS). CMS is an ongoing and substantial driver to the depth of the federal deficit. When Medicare was enacted in 1965, they expected the cost in 1990 to be about $12 billion per year, which was miscalculated by more than a factor of 10.
And the federal deficit, while insurmountably important, pales in comparison to the sobering statistic that 60% of personal bankruptcies are filed due to health-care bills.
Equally disappointing, the U.S. does not appear to get great value out of this exorbitant price tag, as our health-care outcomes certainly are not any better, and are sometimes worse, than other industrialized countries.
Elephants in the Room
The Time article talks extensively about the lack of transparency and drivers for cost in the industry. But there are two major, unreconciled questions the article fails to answer that are at the core of the issue:
- Is health care in the U.S. a right or a luxury?
- Can the U.S. health-care system be compassionate and restrictive at the same time?
You really don’t encounter the first question with any other industry. If I am hungry and do not have any money, I would not march into a restaurant and say, “I am hungry; therefore, you must feed me.” But we all feel like we can—and should—march into an emergency room and say, “I am sick; therefore, you must treat me,” no matter our financial situation. For all other industries, we rely on community resources, nonprofit agencies, and some state/federal funding to bridge gaps in basic necessities (food, housing, clothing, and transportation). And when those run short, people do without.
Car dealerships and Jiffy Lube do not have to follow any Emergency Medicine Treatment and Active Labor Act rules. If health care is a right, then we should not make individuals figure out how to get it, and we should not accept huge disparities in the provision of care based on personal characteristics.
My hospital, like most others in the U.S., is trying to figure out how to cut costs and do more with less. In a series of town-hall-style meetings, our leadership has been telling all of our hospital staff about planned cost-cutting and revenue-generating strategies. One of the tactics is to be more proactive and consistent with collecting copays in outpatient settings (before the delivery of any visit, test, or procedure) and to have parity with our local market on setting the price of those copays. But several employees were wrestling with the thought of collecting copays before the delivery of service. Some voiced a particular concern: “But what if they don’t have the money?” Again, not a conversation heard too often at car dealerships or Jiffy Lube.
The U.S. has a long way to go in reconciling these questions. Addressing them might be easier if there were more transparency in pricing. When you walk into Jiffy Lube, you are presented with all the things you might need for your car, based on make, model, and mileage; you get a listing of the cost of all the items, then you make decisions about what you do and do not need as you factor in what you are willing to spend. But when you go for your annual primary-care check-up, you are not presented a list of all the things you need (based on age, comorbidities, family history, etc.); you are not given a listing of the cost of those available services (check-up, eye exam, colonoscopy, pneumococcal vaccination); and rarely is there ever a discussion of what you are willing to spend. You just assume you need what is recommended, then get a bill later. There is almost no incentive for providers to discuss or present those prices to patients in advance. There is even less incentive to reduce the utilization of those offered services. And the price on the bill variably reflects the actual cost of the products/services provided.
In the hospital setting, the price of most products/services are based on the “chargemaster,” which is a fictional line listing of prices, which, according to the Time article, “gives them a big number to put in front of rich, uninsured patients” to make up for the losses in revenue from all other patients.
For the most part, health-care reform efforts have done little to address the two unanswered questions. And although reform efforts have triggered plenty of discussions about changing the rules on who pays for what and when, these efforts have done little to change the price or the cost of care, or make them more transparent.
The author of “Bitter Pill” makes an attempt to call out the “bad actors” in the industry, those who drive up the cost of health care—health-care leaders with generous salaries, pharmaceutical companies, device/product companies, trial lawyers, and profitable laboratory and radiology departments. But the article does not come close to capturing the other elephants in the room. Without confronting those issues, we will continue to fail to distinguish between the cost and the price, and any value within.
Reference
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Everything has a price, and we all have become accustomed to knowing how much something is going to cost before we buy it. Generally, we start with thinking about how much we are willing to pay, then finding what we need within the range of what we expect to pay. Whether it is shopping on Amazon.com, negotiating the price with a landscaper, or going out to eat, we get to weigh the options in advance of acquiring the goods or services. And, generally ahead of the purchase of big-ticket items, we get an itemized list of what is available.
I recently had to buy a car. Some of the many decisions that went into the purchase were whether to include some of the offered amenities, including:
- “Surround sound”;
- Seat heaters;
- Blind-spot indicator system;
- Premium floor mat package; and
- Built-in GPS.
My husband and I thought about the price of each of these line items relative to what we were going to “get out of it”—e.g., the value. Seat heaters in South Carolina? No, thanks. Surround sound? We had to flip a coin on that one. Safety features? Absolutely. Premium floor mat package? Only if they were guaranteed to be Fruit Roll-Ups-resistant.
Over the course of several negotiations, we picked and chose options that were highly likely to add value (safety, comfort, convenience) and omitted the rest. Then we settled on a total price, paid the negotiated price, and drove away fairly content.
Now, this doesn’t mean that we actually knew the cost of adding each of those amenities into our new car; would anyone actually be able to tell us exactly how much each of those features cost to innovate, create, and install? Probably not, but they might be able to give us a pretty good estimate, as well as an estimate of how much had been added in to ship it to the dealer, to pay the overhead for the dealership, and to pay the dealership staff (from the front desk to the CEO). And we could feel pretty certain that most buyers would be presented with similar prices, regardless of their personal characteristics.
So all in all, there was a reasonable amount of transparency around the cost and the price of the car and all of its amenities, as there would be in most industries. Except in health care.
A Ton of Money, for What?
There was a fascinating article in the March 4 edition of Time titled “Bitter Pill” that discussed the cost and the price of health-care services.1 It certainly is a worthy topic, as the U.S. spends about 20% of our gross domestic product on health care, whereas most other developed countries spend half of that. In fact, according to the article, the U.S. spends more on health care annually ($2.8 trillion) than the top 10 countries combined—Japan, Germany, France, China, United Kingdom, Italy, Canada, Brazil, Spain, and Australia.
About $800 billion of our health care is paid out annually by the Centers for Medicare & Medicaid Services (CMS). CMS is an ongoing and substantial driver to the depth of the federal deficit. When Medicare was enacted in 1965, they expected the cost in 1990 to be about $12 billion per year, which was miscalculated by more than a factor of 10.
And the federal deficit, while insurmountably important, pales in comparison to the sobering statistic that 60% of personal bankruptcies are filed due to health-care bills.
Equally disappointing, the U.S. does not appear to get great value out of this exorbitant price tag, as our health-care outcomes certainly are not any better, and are sometimes worse, than other industrialized countries.
Elephants in the Room
The Time article talks extensively about the lack of transparency and drivers for cost in the industry. But there are two major, unreconciled questions the article fails to answer that are at the core of the issue:
- Is health care in the U.S. a right or a luxury?
- Can the U.S. health-care system be compassionate and restrictive at the same time?
You really don’t encounter the first question with any other industry. If I am hungry and do not have any money, I would not march into a restaurant and say, “I am hungry; therefore, you must feed me.” But we all feel like we can—and should—march into an emergency room and say, “I am sick; therefore, you must treat me,” no matter our financial situation. For all other industries, we rely on community resources, nonprofit agencies, and some state/federal funding to bridge gaps in basic necessities (food, housing, clothing, and transportation). And when those run short, people do without.
Car dealerships and Jiffy Lube do not have to follow any Emergency Medicine Treatment and Active Labor Act rules. If health care is a right, then we should not make individuals figure out how to get it, and we should not accept huge disparities in the provision of care based on personal characteristics.
My hospital, like most others in the U.S., is trying to figure out how to cut costs and do more with less. In a series of town-hall-style meetings, our leadership has been telling all of our hospital staff about planned cost-cutting and revenue-generating strategies. One of the tactics is to be more proactive and consistent with collecting copays in outpatient settings (before the delivery of any visit, test, or procedure) and to have parity with our local market on setting the price of those copays. But several employees were wrestling with the thought of collecting copays before the delivery of service. Some voiced a particular concern: “But what if they don’t have the money?” Again, not a conversation heard too often at car dealerships or Jiffy Lube.
The U.S. has a long way to go in reconciling these questions. Addressing them might be easier if there were more transparency in pricing. When you walk into Jiffy Lube, you are presented with all the things you might need for your car, based on make, model, and mileage; you get a listing of the cost of all the items, then you make decisions about what you do and do not need as you factor in what you are willing to spend. But when you go for your annual primary-care check-up, you are not presented a list of all the things you need (based on age, comorbidities, family history, etc.); you are not given a listing of the cost of those available services (check-up, eye exam, colonoscopy, pneumococcal vaccination); and rarely is there ever a discussion of what you are willing to spend. You just assume you need what is recommended, then get a bill later. There is almost no incentive for providers to discuss or present those prices to patients in advance. There is even less incentive to reduce the utilization of those offered services. And the price on the bill variably reflects the actual cost of the products/services provided.
In the hospital setting, the price of most products/services are based on the “chargemaster,” which is a fictional line listing of prices, which, according to the Time article, “gives them a big number to put in front of rich, uninsured patients” to make up for the losses in revenue from all other patients.
For the most part, health-care reform efforts have done little to address the two unanswered questions. And although reform efforts have triggered plenty of discussions about changing the rules on who pays for what and when, these efforts have done little to change the price or the cost of care, or make them more transparent.
The author of “Bitter Pill” makes an attempt to call out the “bad actors” in the industry, those who drive up the cost of health care—health-care leaders with generous salaries, pharmaceutical companies, device/product companies, trial lawyers, and profitable laboratory and radiology departments. But the article does not come close to capturing the other elephants in the room. Without confronting those issues, we will continue to fail to distinguish between the cost and the price, and any value within.
Reference
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Everything has a price, and we all have become accustomed to knowing how much something is going to cost before we buy it. Generally, we start with thinking about how much we are willing to pay, then finding what we need within the range of what we expect to pay. Whether it is shopping on Amazon.com, negotiating the price with a landscaper, or going out to eat, we get to weigh the options in advance of acquiring the goods or services. And, generally ahead of the purchase of big-ticket items, we get an itemized list of what is available.
I recently had to buy a car. Some of the many decisions that went into the purchase were whether to include some of the offered amenities, including:
- “Surround sound”;
- Seat heaters;
- Blind-spot indicator system;
- Premium floor mat package; and
- Built-in GPS.
My husband and I thought about the price of each of these line items relative to what we were going to “get out of it”—e.g., the value. Seat heaters in South Carolina? No, thanks. Surround sound? We had to flip a coin on that one. Safety features? Absolutely. Premium floor mat package? Only if they were guaranteed to be Fruit Roll-Ups-resistant.
Over the course of several negotiations, we picked and chose options that were highly likely to add value (safety, comfort, convenience) and omitted the rest. Then we settled on a total price, paid the negotiated price, and drove away fairly content.
Now, this doesn’t mean that we actually knew the cost of adding each of those amenities into our new car; would anyone actually be able to tell us exactly how much each of those features cost to innovate, create, and install? Probably not, but they might be able to give us a pretty good estimate, as well as an estimate of how much had been added in to ship it to the dealer, to pay the overhead for the dealership, and to pay the dealership staff (from the front desk to the CEO). And we could feel pretty certain that most buyers would be presented with similar prices, regardless of their personal characteristics.
So all in all, there was a reasonable amount of transparency around the cost and the price of the car and all of its amenities, as there would be in most industries. Except in health care.
A Ton of Money, for What?
There was a fascinating article in the March 4 edition of Time titled “Bitter Pill” that discussed the cost and the price of health-care services.1 It certainly is a worthy topic, as the U.S. spends about 20% of our gross domestic product on health care, whereas most other developed countries spend half of that. In fact, according to the article, the U.S. spends more on health care annually ($2.8 trillion) than the top 10 countries combined—Japan, Germany, France, China, United Kingdom, Italy, Canada, Brazil, Spain, and Australia.
About $800 billion of our health care is paid out annually by the Centers for Medicare & Medicaid Services (CMS). CMS is an ongoing and substantial driver to the depth of the federal deficit. When Medicare was enacted in 1965, they expected the cost in 1990 to be about $12 billion per year, which was miscalculated by more than a factor of 10.
And the federal deficit, while insurmountably important, pales in comparison to the sobering statistic that 60% of personal bankruptcies are filed due to health-care bills.
Equally disappointing, the U.S. does not appear to get great value out of this exorbitant price tag, as our health-care outcomes certainly are not any better, and are sometimes worse, than other industrialized countries.
Elephants in the Room
The Time article talks extensively about the lack of transparency and drivers for cost in the industry. But there are two major, unreconciled questions the article fails to answer that are at the core of the issue:
- Is health care in the U.S. a right or a luxury?
- Can the U.S. health-care system be compassionate and restrictive at the same time?
You really don’t encounter the first question with any other industry. If I am hungry and do not have any money, I would not march into a restaurant and say, “I am hungry; therefore, you must feed me.” But we all feel like we can—and should—march into an emergency room and say, “I am sick; therefore, you must treat me,” no matter our financial situation. For all other industries, we rely on community resources, nonprofit agencies, and some state/federal funding to bridge gaps in basic necessities (food, housing, clothing, and transportation). And when those run short, people do without.
Car dealerships and Jiffy Lube do not have to follow any Emergency Medicine Treatment and Active Labor Act rules. If health care is a right, then we should not make individuals figure out how to get it, and we should not accept huge disparities in the provision of care based on personal characteristics.
My hospital, like most others in the U.S., is trying to figure out how to cut costs and do more with less. In a series of town-hall-style meetings, our leadership has been telling all of our hospital staff about planned cost-cutting and revenue-generating strategies. One of the tactics is to be more proactive and consistent with collecting copays in outpatient settings (before the delivery of any visit, test, or procedure) and to have parity with our local market on setting the price of those copays. But several employees were wrestling with the thought of collecting copays before the delivery of service. Some voiced a particular concern: “But what if they don’t have the money?” Again, not a conversation heard too often at car dealerships or Jiffy Lube.
The U.S. has a long way to go in reconciling these questions. Addressing them might be easier if there were more transparency in pricing. When you walk into Jiffy Lube, you are presented with all the things you might need for your car, based on make, model, and mileage; you get a listing of the cost of all the items, then you make decisions about what you do and do not need as you factor in what you are willing to spend. But when you go for your annual primary-care check-up, you are not presented a list of all the things you need (based on age, comorbidities, family history, etc.); you are not given a listing of the cost of those available services (check-up, eye exam, colonoscopy, pneumococcal vaccination); and rarely is there ever a discussion of what you are willing to spend. You just assume you need what is recommended, then get a bill later. There is almost no incentive for providers to discuss or present those prices to patients in advance. There is even less incentive to reduce the utilization of those offered services. And the price on the bill variably reflects the actual cost of the products/services provided.
In the hospital setting, the price of most products/services are based on the “chargemaster,” which is a fictional line listing of prices, which, according to the Time article, “gives them a big number to put in front of rich, uninsured patients” to make up for the losses in revenue from all other patients.
For the most part, health-care reform efforts have done little to address the two unanswered questions. And although reform efforts have triggered plenty of discussions about changing the rules on who pays for what and when, these efforts have done little to change the price or the cost of care, or make them more transparent.
The author of “Bitter Pill” makes an attempt to call out the “bad actors” in the industry, those who drive up the cost of health care—health-care leaders with generous salaries, pharmaceutical companies, device/product companies, trial lawyers, and profitable laboratory and radiology departments. But the article does not come close to capturing the other elephants in the room. Without confronting those issues, we will continue to fail to distinguish between the cost and the price, and any value within.
Reference
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Hospitals Seek Ways to Defuse Angry Doctors
Everyone is prone to an angry outburst from time to time, and doctors are no exception. With well-documented, negative effects on morale, nurse retention, and patient safety, it's safe to say anger issues crop up from time to time among the nearly 40,000 practicing hospitalists throughout the U.S.
A recent article in Kaiser Health News describes efforts by hospitals to deal with physicians' tirades, such as a three-day counseling program developed at Vanderbilt University in Nashville, Tenn.
"All physicians need to be aware that there should be a 'zero tolerance' attitude for disruptive behavior, hospitalists included, and that disruptive behavior undermines a culture of safety, and therefore can put patients in danger," says Danielle Scheurer, MD, MSCR, SFHM, hospitalist and chief quality officer at Medical University of South Carolina in Charleston and physician editor of The Hospitalist.
In 2009, The Joint Commission issued a sentinel alert about intimidating and disruptive behaviors by physicians and the ways in which hospitals can address the issue.
The problem is not unique to any physician specialty, including hospitalists, says Alan Rosenstein, MD, an internist and disruptive behavior researcher based in San Francisco. A physician's training or personality might contribute to angry outbursts, but excessive workloads will cause pressure, stress, and burnout, which can lead to poor behavior.
"Hospitals can no longer afford to look the other way," Dr. Rosenstein says. "I look at physicians as a precious resource. The organizations they're affiliated with need to be more proactive and empathetic, intervening before the problem reaches the stage of requiring discipline through techniques such as coaching and stress management." TH
Visit our website for more information about the impact of workloads on hospitalists.
Everyone is prone to an angry outburst from time to time, and doctors are no exception. With well-documented, negative effects on morale, nurse retention, and patient safety, it's safe to say anger issues crop up from time to time among the nearly 40,000 practicing hospitalists throughout the U.S.
A recent article in Kaiser Health News describes efforts by hospitals to deal with physicians' tirades, such as a three-day counseling program developed at Vanderbilt University in Nashville, Tenn.
"All physicians need to be aware that there should be a 'zero tolerance' attitude for disruptive behavior, hospitalists included, and that disruptive behavior undermines a culture of safety, and therefore can put patients in danger," says Danielle Scheurer, MD, MSCR, SFHM, hospitalist and chief quality officer at Medical University of South Carolina in Charleston and physician editor of The Hospitalist.
In 2009, The Joint Commission issued a sentinel alert about intimidating and disruptive behaviors by physicians and the ways in which hospitals can address the issue.
The problem is not unique to any physician specialty, including hospitalists, says Alan Rosenstein, MD, an internist and disruptive behavior researcher based in San Francisco. A physician's training or personality might contribute to angry outbursts, but excessive workloads will cause pressure, stress, and burnout, which can lead to poor behavior.
"Hospitals can no longer afford to look the other way," Dr. Rosenstein says. "I look at physicians as a precious resource. The organizations they're affiliated with need to be more proactive and empathetic, intervening before the problem reaches the stage of requiring discipline through techniques such as coaching and stress management." TH
Visit our website for more information about the impact of workloads on hospitalists.
Everyone is prone to an angry outburst from time to time, and doctors are no exception. With well-documented, negative effects on morale, nurse retention, and patient safety, it's safe to say anger issues crop up from time to time among the nearly 40,000 practicing hospitalists throughout the U.S.
A recent article in Kaiser Health News describes efforts by hospitals to deal with physicians' tirades, such as a three-day counseling program developed at Vanderbilt University in Nashville, Tenn.
"All physicians need to be aware that there should be a 'zero tolerance' attitude for disruptive behavior, hospitalists included, and that disruptive behavior undermines a culture of safety, and therefore can put patients in danger," says Danielle Scheurer, MD, MSCR, SFHM, hospitalist and chief quality officer at Medical University of South Carolina in Charleston and physician editor of The Hospitalist.
In 2009, The Joint Commission issued a sentinel alert about intimidating and disruptive behaviors by physicians and the ways in which hospitals can address the issue.
The problem is not unique to any physician specialty, including hospitalists, says Alan Rosenstein, MD, an internist and disruptive behavior researcher based in San Francisco. A physician's training or personality might contribute to angry outbursts, but excessive workloads will cause pressure, stress, and burnout, which can lead to poor behavior.
"Hospitals can no longer afford to look the other way," Dr. Rosenstein says. "I look at physicians as a precious resource. The organizations they're affiliated with need to be more proactive and empathetic, intervening before the problem reaches the stage of requiring discipline through techniques such as coaching and stress management." TH
Visit our website for more information about the impact of workloads on hospitalists.
Danielle Scheurer: Thousands of Hospitalists Set Their Sights on HM13
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
SHM’s annual meeting—or annui conventus, for you Latin lovers—is right around the corner, so be sure to cement your intentions and prepare to go if you have not already.
Now a “longstanding” tradition, the annual meeting serves many purposes, one of which is to act as a reservoir of time for individual hospitalists and for hospitalist groups to reflect on where they have been, where they are now, and where they are (or would like to be) going. A brief history of the SHM annual meeting makes us quickly realize how far we have come, and how far we have to go.
Where We’ve Been
The annual meeting’s history dates back to 1998, when a rogue gathering of about 100 self-proclaimed hospitalists gathered at the National Association of Inpatient Physicians (NAIP) meeting in San Diego. From the year before the first annual meeting to the year after the first annual meeting, membership in NAIP had grown from about 20 hospitalists to about 800 hospitalists. That rapidity of growth had never been seen by another specialty in the history of modern medicine. By the 2003 annual meeting in San Diego, the name had officially changed to the Society of Hospital Medicine, and membership had grown to more than 3,000; less than 10 years later, when the meeting returned to San Diego, membership had grown to more than 10,000. These continued steady increases in both membership size and attendance at the meeting serves as a testimony to the strength of the field and the leadership of the society.
Check out our 6-minute feature video: "Five Reasons You Should Attend HM13"
Where We Are Now
Growth: SHM’s annual meeting now has a track record to be reckoned with. The number of attendees expected for 2013 is a staggering 3,000, which is only a portion of the more than 11,000 SHM members who can actually take time away from their busy practices to attend. The event has now expanded to more than three and a half days, including eight pre-courses and more than 100 workshops/breakout sessions to meet the needs of most any hospitalist. The number of submissions for the Research, Innovations, and Clinical Vignettes competition has steadily risen over the years, topping an all-time record of 800 submissions in 2013. This is a testimony to the curiosity and productivity of so many hospitalists and HM groups.
Advocacy: SHM has been a longstanding and considerable advocate for healthcare reform for more than a decade. With the annual meeting in Washington, D.C., this year, and in lieu of the pre-courses, more than 100 hospitalists and SHM staff will be making a field trip to Capitol Hill to advocate for changes in the structure and payment within the medical industry, to promote good patient care for those we serve, and to promote continued research for better ways of delivering care in the future. Over the course of 2012, SHM submitted more than 20 influential advocacy letters to a variety of stakeholders on topics ranging from sustainable growth rate (SGR) repeal to Agency for Healthcare Research and Quality (AHRQ) funding.
Impact: The annual meeting is not just bigger and longer; it is better. The quality and reputation of the plenary, breakout, and workshop speakers is tremendous, with this year’s plenary speakers including Patrick Conway, chief medical officer of CMS, and David Feinberg, president of UCLA Health System and CEO of UCLA Hospital System. The annual award ceremony will recognize a highly qualified repertoire of dedicated hospitalists and teams and reflect the number and quality of those involved in HM in the areas of clinical excellence, teaching, research, service, and teamwork. The annual Fellows in Hospital Medicine induction will include more than 300 additional fellows and senior fellows, which is a testimony to the level of involvement so many hospitalists have within our specialty.
Where We Are Going
Growth: I suspect the annual meeting will continue to grow in size, and it will expand to better serve the needs of other types of hospital-based physicians (neurologists, obstetricians, etc.), other types of practitioners (NPs, PAs, other specialty nurses), and other types of professionals (administrators and executives). It likely will attract an international community of hospitalists as other nations identify and execute better models of care for hospitalized patients.
Advocacy: SHM and the annual meeting will continue to serve as a nidus for directing the best pathways toward a better healthcare system. It will continue to serve as an avenue by which we partner with and/or influence impactful organizations, such as federal, state, and local governments, the Centers for Medicare & Medicaid Services (CMS), the Joint Commission, and the American Hospital Association, to name a few.
Impact: SHM and the annual meeting will expand its role as the focus for learning and sharing new research and innovations within the field. It will serve as a platform for initiating and spreading standardized evidence-based implementation of best practices through a repertoire of mentored implementation programs. And it will continue to serve as proof of the strength of our hospital medicine community as we spread into every U.S. hospital system and beyond.
Reputation: The future of our annual meeting and reputation will be dependent on how fast and how carefully we craft the pathway for HM. Currently, about half of all the nation’s hospitalists have been in practice for five years or less. We will need to carefully focus on how to be compassionate providers and system advocates—not just shift workers and billing specialists. We will have to be the mentors by which other countries define best practice for inpatient care, including what ideal training for a hospitalist should look like, and what their scope of practice should entail.
If you ask one of the attendees of the first annui conventus what it was like, they will say it was a small mom-and-pop gathering of disparate physicians, with a pie-in-the-sky idea of the future of hospitalist practice. And someday, when our current generation of hospitalists attends an international conference of hospitalists, in Prague, in 2033, we can say, “Remember when we met in that tiny hotel in D.C. in 2013?”
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Better Thinking by Hospitalists Key to Improving Healthcare Industry
Old habits are hard to break. We all get used to doing things in certain ways, and the longer we do it, it becomes increasingly difficult to do them differently. We clearly are clinging to old habits in the healthcare industry, despite compelling evidence that we need to figure out better ways of doing business. Our industry has been in a crisis for a very long time—rising costs, drastic reimbursement reductions from payors, and continually escalating risks and medical errors.
Clearly, something is not working.
This is a time when hospitalists should start thinking about dropping some of our Pulaskis.
Handy, Useful, Versatile, Reliable
A Pulaski is a versatile tool that combines an axe and an adze; it’s most commonly used in firefighting, but it is also used in trail-blazing, gardening, and woodworking (see right). The Pulaski was invented by Ed Pulaski, a forest ranger in the 1910s who almost died in a forest fire after being trapped in an old mine tunnel. After he barely survived, he invented the Pulaski as a means to reduce the risk of future firefighters being trapped in his same situation. For more than 100 years, this tool has come in handy in countless situations. It is versatile, irreplaceable, reliable—a must-have. Unless you don’t need it. And then it becomes a 22-pound handicap.
Donald Berwick, MD, MPP, spoke about the Pulaski 13 years ago in a powerful speech to the National Forum on Quality Improvement in Health Care; his presentation was titled “Escape Fire.”1 He described the Mann Gulch fire of 1949, which took the lives of 13 young men when the fire did not behave as expected. The men were forced to outrun this fire, up a hill at a 76% slope, with the fire racing at them at 7 miles per hour, at an air temperature of 100 degrees. Only two firefighters survived. Those who perished tried to run up the hill with all of their gear, including their Pulaski, which served, at the time, only to slow them down. One survivor was lucky; he managed to get to the top of hill before the fire engulfed him. The other survivor, Wagner Dodge, was heroic. He realized the situation was hopeless and created a radical, innovative, and immediate solution to the problem at hand: He not only dropped his 22-pound handicap, but he also stopped running up the hill, stood still, and lit his own escape fire to avoid the larger fire at hand. The rest of the pack clung to the only option they could conceive of, which was outrunning the beast, despite the fact that it was traveling twice as fast as they were.
During his speech, Dr. Berwick also spoke of some of his personal experiences within U.S. hospitals that were filled with fear, uncertainty, and at times downright outrage; of misunderstandings, despicable care transitions, and daily medical errors or near misses. About how he and his wife struggled for security, appropriate treatments, and more answers than questions. He spoke of being in some of the best hospitals in the nation, and of being more organized and informed than most patients. Most patients would not possibly fare as well as the Berwicks, being under- or uninsured, of low health literacy, undereducated, or uninformed. It is incomprehensible that we have created a system that is so complicated and difficult to navigate that even the best and the brightest cannot traverse it unscathed. So it seems that sometimes the key to doing something better (or surviving, in the case of the Mann Gulch fire) is not knowing what new tools to adopt, but instead knowing what tools to get rid of.
Seize the Day
There is a dog park near my house that we take our dog to whenever we get a chance. There is a dog that frequents the park, a brown Labrador by the name of Gracie. Gracie’s favorite activity is fetching tennis balls; she dutifully catches the ball (usually in midair) and brings it back to her owner. When she gets back to her owner, she stands in front of him waiting for her order: “Drop it, Gracie.” As soon as Gracie hears the order, she drops the ball immediately. But she won’t drop the ball until ordered to do so—even though, by keeping the ball, she is that much further away from her next favorite activity. It seems like, to do the best for herself, she should come back and drop the ball, which would bring her that much closer to the one thing she loves best.
But she doesn’t. She waits dutifully for someone else to tell her when to drop the ball.
And interestingly, Gracie will not just drop it for anyone. When others at the park want to play with Gracie, and follow the lead of Gracie’s owner, and say “Drop it, Gracie,” she will look at the visitor, and then at her owner, looking for the approval that it really is in fact OK for her to drop it. Even after an approving look, she will hesitatingly drop the ball, and only after the stranger is a safe distance away, in case she needs to retrieve it sooner than later.
Many of us in the healthcare industry often wait for someone else to tell us when to start doing new things, but rarely do we expect, do we hear, or do we initiate the order to stop doing something. We need to think deeply about all the things we do that are useless Pulaskis, and about how to radically change the industry in which we work. Because this inching along is not going fast enough, and there is little evidence that we have made much progress in the last decade. So if you find yourself lugging around a Pulaski (or two), don’t just think about how to drop it, or when to drop it, or whether to drop it on certain days of the week. Just drop it, Gracie.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
Old habits are hard to break. We all get used to doing things in certain ways, and the longer we do it, it becomes increasingly difficult to do them differently. We clearly are clinging to old habits in the healthcare industry, despite compelling evidence that we need to figure out better ways of doing business. Our industry has been in a crisis for a very long time—rising costs, drastic reimbursement reductions from payors, and continually escalating risks and medical errors.
Clearly, something is not working.
This is a time when hospitalists should start thinking about dropping some of our Pulaskis.
Handy, Useful, Versatile, Reliable
A Pulaski is a versatile tool that combines an axe and an adze; it’s most commonly used in firefighting, but it is also used in trail-blazing, gardening, and woodworking (see right). The Pulaski was invented by Ed Pulaski, a forest ranger in the 1910s who almost died in a forest fire after being trapped in an old mine tunnel. After he barely survived, he invented the Pulaski as a means to reduce the risk of future firefighters being trapped in his same situation. For more than 100 years, this tool has come in handy in countless situations. It is versatile, irreplaceable, reliable—a must-have. Unless you don’t need it. And then it becomes a 22-pound handicap.
Donald Berwick, MD, MPP, spoke about the Pulaski 13 years ago in a powerful speech to the National Forum on Quality Improvement in Health Care; his presentation was titled “Escape Fire.”1 He described the Mann Gulch fire of 1949, which took the lives of 13 young men when the fire did not behave as expected. The men were forced to outrun this fire, up a hill at a 76% slope, with the fire racing at them at 7 miles per hour, at an air temperature of 100 degrees. Only two firefighters survived. Those who perished tried to run up the hill with all of their gear, including their Pulaski, which served, at the time, only to slow them down. One survivor was lucky; he managed to get to the top of hill before the fire engulfed him. The other survivor, Wagner Dodge, was heroic. He realized the situation was hopeless and created a radical, innovative, and immediate solution to the problem at hand: He not only dropped his 22-pound handicap, but he also stopped running up the hill, stood still, and lit his own escape fire to avoid the larger fire at hand. The rest of the pack clung to the only option they could conceive of, which was outrunning the beast, despite the fact that it was traveling twice as fast as they were.
During his speech, Dr. Berwick also spoke of some of his personal experiences within U.S. hospitals that were filled with fear, uncertainty, and at times downright outrage; of misunderstandings, despicable care transitions, and daily medical errors or near misses. About how he and his wife struggled for security, appropriate treatments, and more answers than questions. He spoke of being in some of the best hospitals in the nation, and of being more organized and informed than most patients. Most patients would not possibly fare as well as the Berwicks, being under- or uninsured, of low health literacy, undereducated, or uninformed. It is incomprehensible that we have created a system that is so complicated and difficult to navigate that even the best and the brightest cannot traverse it unscathed. So it seems that sometimes the key to doing something better (or surviving, in the case of the Mann Gulch fire) is not knowing what new tools to adopt, but instead knowing what tools to get rid of.
Seize the Day
There is a dog park near my house that we take our dog to whenever we get a chance. There is a dog that frequents the park, a brown Labrador by the name of Gracie. Gracie’s favorite activity is fetching tennis balls; she dutifully catches the ball (usually in midair) and brings it back to her owner. When she gets back to her owner, she stands in front of him waiting for her order: “Drop it, Gracie.” As soon as Gracie hears the order, she drops the ball immediately. But she won’t drop the ball until ordered to do so—even though, by keeping the ball, she is that much further away from her next favorite activity. It seems like, to do the best for herself, she should come back and drop the ball, which would bring her that much closer to the one thing she loves best.
But she doesn’t. She waits dutifully for someone else to tell her when to drop the ball.
And interestingly, Gracie will not just drop it for anyone. When others at the park want to play with Gracie, and follow the lead of Gracie’s owner, and say “Drop it, Gracie,” she will look at the visitor, and then at her owner, looking for the approval that it really is in fact OK for her to drop it. Even after an approving look, she will hesitatingly drop the ball, and only after the stranger is a safe distance away, in case she needs to retrieve it sooner than later.
Many of us in the healthcare industry often wait for someone else to tell us when to start doing new things, but rarely do we expect, do we hear, or do we initiate the order to stop doing something. We need to think deeply about all the things we do that are useless Pulaskis, and about how to radically change the industry in which we work. Because this inching along is not going fast enough, and there is little evidence that we have made much progress in the last decade. So if you find yourself lugging around a Pulaski (or two), don’t just think about how to drop it, or when to drop it, or whether to drop it on certain days of the week. Just drop it, Gracie.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
Old habits are hard to break. We all get used to doing things in certain ways, and the longer we do it, it becomes increasingly difficult to do them differently. We clearly are clinging to old habits in the healthcare industry, despite compelling evidence that we need to figure out better ways of doing business. Our industry has been in a crisis for a very long time—rising costs, drastic reimbursement reductions from payors, and continually escalating risks and medical errors.
Clearly, something is not working.
This is a time when hospitalists should start thinking about dropping some of our Pulaskis.
Handy, Useful, Versatile, Reliable
A Pulaski is a versatile tool that combines an axe and an adze; it’s most commonly used in firefighting, but it is also used in trail-blazing, gardening, and woodworking (see right). The Pulaski was invented by Ed Pulaski, a forest ranger in the 1910s who almost died in a forest fire after being trapped in an old mine tunnel. After he barely survived, he invented the Pulaski as a means to reduce the risk of future firefighters being trapped in his same situation. For more than 100 years, this tool has come in handy in countless situations. It is versatile, irreplaceable, reliable—a must-have. Unless you don’t need it. And then it becomes a 22-pound handicap.
Donald Berwick, MD, MPP, spoke about the Pulaski 13 years ago in a powerful speech to the National Forum on Quality Improvement in Health Care; his presentation was titled “Escape Fire.”1 He described the Mann Gulch fire of 1949, which took the lives of 13 young men when the fire did not behave as expected. The men were forced to outrun this fire, up a hill at a 76% slope, with the fire racing at them at 7 miles per hour, at an air temperature of 100 degrees. Only two firefighters survived. Those who perished tried to run up the hill with all of their gear, including their Pulaski, which served, at the time, only to slow them down. One survivor was lucky; he managed to get to the top of hill before the fire engulfed him. The other survivor, Wagner Dodge, was heroic. He realized the situation was hopeless and created a radical, innovative, and immediate solution to the problem at hand: He not only dropped his 22-pound handicap, but he also stopped running up the hill, stood still, and lit his own escape fire to avoid the larger fire at hand. The rest of the pack clung to the only option they could conceive of, which was outrunning the beast, despite the fact that it was traveling twice as fast as they were.
During his speech, Dr. Berwick also spoke of some of his personal experiences within U.S. hospitals that were filled with fear, uncertainty, and at times downright outrage; of misunderstandings, despicable care transitions, and daily medical errors or near misses. About how he and his wife struggled for security, appropriate treatments, and more answers than questions. He spoke of being in some of the best hospitals in the nation, and of being more organized and informed than most patients. Most patients would not possibly fare as well as the Berwicks, being under- or uninsured, of low health literacy, undereducated, or uninformed. It is incomprehensible that we have created a system that is so complicated and difficult to navigate that even the best and the brightest cannot traverse it unscathed. So it seems that sometimes the key to doing something better (or surviving, in the case of the Mann Gulch fire) is not knowing what new tools to adopt, but instead knowing what tools to get rid of.
Seize the Day
There is a dog park near my house that we take our dog to whenever we get a chance. There is a dog that frequents the park, a brown Labrador by the name of Gracie. Gracie’s favorite activity is fetching tennis balls; she dutifully catches the ball (usually in midair) and brings it back to her owner. When she gets back to her owner, she stands in front of him waiting for her order: “Drop it, Gracie.” As soon as Gracie hears the order, she drops the ball immediately. But she won’t drop the ball until ordered to do so—even though, by keeping the ball, she is that much further away from her next favorite activity. It seems like, to do the best for herself, she should come back and drop the ball, which would bring her that much closer to the one thing she loves best.
But she doesn’t. She waits dutifully for someone else to tell her when to drop the ball.
And interestingly, Gracie will not just drop it for anyone. When others at the park want to play with Gracie, and follow the lead of Gracie’s owner, and say “Drop it, Gracie,” she will look at the visitor, and then at her owner, looking for the approval that it really is in fact OK for her to drop it. Even after an approving look, she will hesitatingly drop the ball, and only after the stranger is a safe distance away, in case she needs to retrieve it sooner than later.
Many of us in the healthcare industry often wait for someone else to tell us when to start doing new things, but rarely do we expect, do we hear, or do we initiate the order to stop doing something. We need to think deeply about all the things we do that are useless Pulaskis, and about how to radically change the industry in which we work. Because this inching along is not going fast enough, and there is little evidence that we have made much progress in the last decade. So if you find yourself lugging around a Pulaski (or two), don’t just think about how to drop it, or when to drop it, or whether to drop it on certain days of the week. Just drop it, Gracie.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
Reference
Fundamentals of Highly Reliable Organizations Could Benefit Hospitalists
Reliability. This sounds like a decent trait. Who wouldn’t want to be described as “reliable”? It sounds reputable whether you’re a person, a car, or a dishwasher. So how does one become or emulate the trait of being reliable, one who is predictable, punctua—“reproducible,” if you will?
Organizational reliability has received a fair bit of press these days. The industries that have come to embrace reliability concepts are those in which failure is easy to come by, and those in which failure is likely to be catastrophic if it occurs. In the medical industry, failure occurs to people, not widgets or machines, so by definition it tends to be catastrophic. These failures generally come in three flavors:
- The expected fails to occur (i.e. a patient with pneumonia does not receive their antibiotics on time);
- The unexpected occurs (i.e. a patient falls and breaks their hip); or
- The unexpected was not previously thought of (i.e. low-risk patient has a PEA arrest).
A fair bit of research has been done on how organizations can become more reliable. In their book “Managing the Unexpected: Assuring High Performance in an Age of Complexity,”1 Karl Weick and Kathleen Sutcliffe studied firefighting, workers on aircraft carriers, and nuclear power plant employees. They all have in common the fundamental similarity that failure in their workplace is catastrophically dangerous, and that they must continuously strive to reduce the risk and/or mitigate effectively. The Agency for Healthcare Research and Quality (AHRQ) specifically studied, through case studies and site visits, how some healthcare organizations have achieved some success in the different domains of reliability.2
What both studies found is that there are five prerequisites that, if done well, lead to an organizational “state of mindfulness.” What they and others have found in their research of highly reliable organizations (HROs) is not that they have failure-free operations, but that they continuously and “mindfully” think about how to be failure-free. Inattention and complacency are the biggest threats to reliability.
The Fundamentals
The first prerequisite is sensitivity to operations. This refers to actively seeking information on how things actually are working, instead of how they are supposed to be working. It is being acutely aware of all operations, including the smallest details: Does the patient have an armband on? Is the nurse washing their hands? Is the whiteboard information correct? Is the bed alarm enabled? It is the state of mind when everyone knows how things should work, look, feel, sound, and can recognize when something is out of bounds.
The next prerequisite is a preoccupation with failure. This refers to a system in which failure and near-misses are completely transparent, and openly and honestly discussed (without inciting individual blame or punitive action), and learned from communally. This “group thought” continually reaffirms the fact that systems, and everyone in them, are completely fallible to errors. It is the complete opposite of inattention and complacency. It is continuously asking “What can go wrong, how can it go wrong, when will it go wrong, and how can I stop it?”
The next prerequisite is reluctance to oversimplify. This does not imply that simplicity is bad, but that oversimplicity is lethal. It forces people and organizations to avoid shortcuts and to not rely on simplistic explanations for situations that need to be complicated. Think of this as making a complicated soufflé; if you leave out a step or an ingredient, the product will be far from a soufflé.
The next prerequisite is deference to expertise. This principle recognizes that authority and/or rank are not equivalent to expertise. This assumes that people and organizations are willing and able to defer decision-making to the person who will make the best decision, not to who ranks highest in the organizational chart. A junior hospitalist might be much more likely to make a good decision on building a new order set than the hospitalist director is.
The last prerequisite is resilience. Webster’s defines resilience as “the capability of a strained body to recover its size and shape after deformation caused especially by compressive stress … an ability to recover from or adjust easily to misfortune or change.” The “compressive stresses” and “misfortune or change” can present in a number of different ways, including bad patient outcomes, bad national press, or bad hospital rankings. A good HRO is not one that does not experience unexpected events, but is one that is not disabled by them. They routinely train and practice for worst-case scenarios. It is easy to “audit” resilience by looking at the organizational response to unexpected events. Are they handled with grace, ease, and speed, or with panic, anxiety, and ongoing uncertainty? Resilience involves adequately functioning despite adversity, recovering well, and learning from the experience.
Take-Home Message
The first three principles relate to how organizations can anticipate and reduce the risk of failure; the last two principles relate to how organizations mitigate the extent or severity of failure when it occurs. Together, they create the state of mindfulness, in which all senses are open and alert for signs of aberrations in the system, and where there is continuous learning of how to make the system function better.
What does this mean for a hospitalist to function in an HRO? Most hospitalists are on the front lines, where they routinely see where and how things can fail. They need to resist the urge to become complacent and remain continuously alert to signals that the system is not functioning for the safety of the patient. And when things do go awry, they need to be part of the resilience plan, to work with their teams to swiftly and effectively mitigate ongoing risks, and defer decision to expertise and not necessarily authority.
It also requires that each of us work within multidisciplinary teams in which all members add to the “state of mindfulness,” including the patient and their families (who very often note “aberrancies” before anyone else does). Think of your hospital as ascribed by Gordon Bethune, the former CEO of Continental Airlines. When asked why all employees received a bonus for on-time departure (instead of only employees on the front line), he held up his wristwatch and said, “What part of this watch don’t you think we need?”
Hospitalists can be powerful motivators for a culture change that empowers all hospital employees to be engaged in anticipating and managing failures—just by being mindful. This is a great place to start.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Weick KE, Sutcliffe KM. Managing the unexpected: Resilient performance in an age of uncertainty, 2nd ed. 2007: Hoboken, NJ: John Wiley & Sons Inc.
- Agency for Healthcare Research and Quality. Becoming a high reliability organization: operational advice for hospital leaders. Agency for Healthcare Research and Quality website. Available at: http://www.ahrq.gov/qual/hroadvice/. Accessed Dec. 10, 2012.
Reliability. This sounds like a decent trait. Who wouldn’t want to be described as “reliable”? It sounds reputable whether you’re a person, a car, or a dishwasher. So how does one become or emulate the trait of being reliable, one who is predictable, punctua—“reproducible,” if you will?
Organizational reliability has received a fair bit of press these days. The industries that have come to embrace reliability concepts are those in which failure is easy to come by, and those in which failure is likely to be catastrophic if it occurs. In the medical industry, failure occurs to people, not widgets or machines, so by definition it tends to be catastrophic. These failures generally come in three flavors:
- The expected fails to occur (i.e. a patient with pneumonia does not receive their antibiotics on time);
- The unexpected occurs (i.e. a patient falls and breaks their hip); or
- The unexpected was not previously thought of (i.e. low-risk patient has a PEA arrest).
A fair bit of research has been done on how organizations can become more reliable. In their book “Managing the Unexpected: Assuring High Performance in an Age of Complexity,”1 Karl Weick and Kathleen Sutcliffe studied firefighting, workers on aircraft carriers, and nuclear power plant employees. They all have in common the fundamental similarity that failure in their workplace is catastrophically dangerous, and that they must continuously strive to reduce the risk and/or mitigate effectively. The Agency for Healthcare Research and Quality (AHRQ) specifically studied, through case studies and site visits, how some healthcare organizations have achieved some success in the different domains of reliability.2
What both studies found is that there are five prerequisites that, if done well, lead to an organizational “state of mindfulness.” What they and others have found in their research of highly reliable organizations (HROs) is not that they have failure-free operations, but that they continuously and “mindfully” think about how to be failure-free. Inattention and complacency are the biggest threats to reliability.
The Fundamentals
The first prerequisite is sensitivity to operations. This refers to actively seeking information on how things actually are working, instead of how they are supposed to be working. It is being acutely aware of all operations, including the smallest details: Does the patient have an armband on? Is the nurse washing their hands? Is the whiteboard information correct? Is the bed alarm enabled? It is the state of mind when everyone knows how things should work, look, feel, sound, and can recognize when something is out of bounds.
The next prerequisite is a preoccupation with failure. This refers to a system in which failure and near-misses are completely transparent, and openly and honestly discussed (without inciting individual blame or punitive action), and learned from communally. This “group thought” continually reaffirms the fact that systems, and everyone in them, are completely fallible to errors. It is the complete opposite of inattention and complacency. It is continuously asking “What can go wrong, how can it go wrong, when will it go wrong, and how can I stop it?”
The next prerequisite is reluctance to oversimplify. This does not imply that simplicity is bad, but that oversimplicity is lethal. It forces people and organizations to avoid shortcuts and to not rely on simplistic explanations for situations that need to be complicated. Think of this as making a complicated soufflé; if you leave out a step or an ingredient, the product will be far from a soufflé.
The next prerequisite is deference to expertise. This principle recognizes that authority and/or rank are not equivalent to expertise. This assumes that people and organizations are willing and able to defer decision-making to the person who will make the best decision, not to who ranks highest in the organizational chart. A junior hospitalist might be much more likely to make a good decision on building a new order set than the hospitalist director is.
The last prerequisite is resilience. Webster’s defines resilience as “the capability of a strained body to recover its size and shape after deformation caused especially by compressive stress … an ability to recover from or adjust easily to misfortune or change.” The “compressive stresses” and “misfortune or change” can present in a number of different ways, including bad patient outcomes, bad national press, or bad hospital rankings. A good HRO is not one that does not experience unexpected events, but is one that is not disabled by them. They routinely train and practice for worst-case scenarios. It is easy to “audit” resilience by looking at the organizational response to unexpected events. Are they handled with grace, ease, and speed, or with panic, anxiety, and ongoing uncertainty? Resilience involves adequately functioning despite adversity, recovering well, and learning from the experience.
Take-Home Message
The first three principles relate to how organizations can anticipate and reduce the risk of failure; the last two principles relate to how organizations mitigate the extent or severity of failure when it occurs. Together, they create the state of mindfulness, in which all senses are open and alert for signs of aberrations in the system, and where there is continuous learning of how to make the system function better.
What does this mean for a hospitalist to function in an HRO? Most hospitalists are on the front lines, where they routinely see where and how things can fail. They need to resist the urge to become complacent and remain continuously alert to signals that the system is not functioning for the safety of the patient. And when things do go awry, they need to be part of the resilience plan, to work with their teams to swiftly and effectively mitigate ongoing risks, and defer decision to expertise and not necessarily authority.
It also requires that each of us work within multidisciplinary teams in which all members add to the “state of mindfulness,” including the patient and their families (who very often note “aberrancies” before anyone else does). Think of your hospital as ascribed by Gordon Bethune, the former CEO of Continental Airlines. When asked why all employees received a bonus for on-time departure (instead of only employees on the front line), he held up his wristwatch and said, “What part of this watch don’t you think we need?”
Hospitalists can be powerful motivators for a culture change that empowers all hospital employees to be engaged in anticipating and managing failures—just by being mindful. This is a great place to start.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Weick KE, Sutcliffe KM. Managing the unexpected: Resilient performance in an age of uncertainty, 2nd ed. 2007: Hoboken, NJ: John Wiley & Sons Inc.
- Agency for Healthcare Research and Quality. Becoming a high reliability organization: operational advice for hospital leaders. Agency for Healthcare Research and Quality website. Available at: http://www.ahrq.gov/qual/hroadvice/. Accessed Dec. 10, 2012.
Reliability. This sounds like a decent trait. Who wouldn’t want to be described as “reliable”? It sounds reputable whether you’re a person, a car, or a dishwasher. So how does one become or emulate the trait of being reliable, one who is predictable, punctua—“reproducible,” if you will?
Organizational reliability has received a fair bit of press these days. The industries that have come to embrace reliability concepts are those in which failure is easy to come by, and those in which failure is likely to be catastrophic if it occurs. In the medical industry, failure occurs to people, not widgets or machines, so by definition it tends to be catastrophic. These failures generally come in three flavors:
- The expected fails to occur (i.e. a patient with pneumonia does not receive their antibiotics on time);
- The unexpected occurs (i.e. a patient falls and breaks their hip); or
- The unexpected was not previously thought of (i.e. low-risk patient has a PEA arrest).
A fair bit of research has been done on how organizations can become more reliable. In their book “Managing the Unexpected: Assuring High Performance in an Age of Complexity,”1 Karl Weick and Kathleen Sutcliffe studied firefighting, workers on aircraft carriers, and nuclear power plant employees. They all have in common the fundamental similarity that failure in their workplace is catastrophically dangerous, and that they must continuously strive to reduce the risk and/or mitigate effectively. The Agency for Healthcare Research and Quality (AHRQ) specifically studied, through case studies and site visits, how some healthcare organizations have achieved some success in the different domains of reliability.2
What both studies found is that there are five prerequisites that, if done well, lead to an organizational “state of mindfulness.” What they and others have found in their research of highly reliable organizations (HROs) is not that they have failure-free operations, but that they continuously and “mindfully” think about how to be failure-free. Inattention and complacency are the biggest threats to reliability.
The Fundamentals
The first prerequisite is sensitivity to operations. This refers to actively seeking information on how things actually are working, instead of how they are supposed to be working. It is being acutely aware of all operations, including the smallest details: Does the patient have an armband on? Is the nurse washing their hands? Is the whiteboard information correct? Is the bed alarm enabled? It is the state of mind when everyone knows how things should work, look, feel, sound, and can recognize when something is out of bounds.
The next prerequisite is a preoccupation with failure. This refers to a system in which failure and near-misses are completely transparent, and openly and honestly discussed (without inciting individual blame or punitive action), and learned from communally. This “group thought” continually reaffirms the fact that systems, and everyone in them, are completely fallible to errors. It is the complete opposite of inattention and complacency. It is continuously asking “What can go wrong, how can it go wrong, when will it go wrong, and how can I stop it?”
The next prerequisite is reluctance to oversimplify. This does not imply that simplicity is bad, but that oversimplicity is lethal. It forces people and organizations to avoid shortcuts and to not rely on simplistic explanations for situations that need to be complicated. Think of this as making a complicated soufflé; if you leave out a step or an ingredient, the product will be far from a soufflé.
The next prerequisite is deference to expertise. This principle recognizes that authority and/or rank are not equivalent to expertise. This assumes that people and organizations are willing and able to defer decision-making to the person who will make the best decision, not to who ranks highest in the organizational chart. A junior hospitalist might be much more likely to make a good decision on building a new order set than the hospitalist director is.
The last prerequisite is resilience. Webster’s defines resilience as “the capability of a strained body to recover its size and shape after deformation caused especially by compressive stress … an ability to recover from or adjust easily to misfortune or change.” The “compressive stresses” and “misfortune or change” can present in a number of different ways, including bad patient outcomes, bad national press, or bad hospital rankings. A good HRO is not one that does not experience unexpected events, but is one that is not disabled by them. They routinely train and practice for worst-case scenarios. It is easy to “audit” resilience by looking at the organizational response to unexpected events. Are they handled with grace, ease, and speed, or with panic, anxiety, and ongoing uncertainty? Resilience involves adequately functioning despite adversity, recovering well, and learning from the experience.
Take-Home Message
The first three principles relate to how organizations can anticipate and reduce the risk of failure; the last two principles relate to how organizations mitigate the extent or severity of failure when it occurs. Together, they create the state of mindfulness, in which all senses are open and alert for signs of aberrations in the system, and where there is continuous learning of how to make the system function better.
What does this mean for a hospitalist to function in an HRO? Most hospitalists are on the front lines, where they routinely see where and how things can fail. They need to resist the urge to become complacent and remain continuously alert to signals that the system is not functioning for the safety of the patient. And when things do go awry, they need to be part of the resilience plan, to work with their teams to swiftly and effectively mitigate ongoing risks, and defer decision to expertise and not necessarily authority.
It also requires that each of us work within multidisciplinary teams in which all members add to the “state of mindfulness,” including the patient and their families (who very often note “aberrancies” before anyone else does). Think of your hospital as ascribed by Gordon Bethune, the former CEO of Continental Airlines. When asked why all employees received a bonus for on-time departure (instead of only employees on the front line), he held up his wristwatch and said, “What part of this watch don’t you think we need?”
Hospitalists can be powerful motivators for a culture change that empowers all hospital employees to be engaged in anticipating and managing failures—just by being mindful. This is a great place to start.
Dr. Scheurer is a hospitalist and chief quality officer at the Medical University of South Carolina in Charleston. She is physician editor of The Hospitalist. Email her at scheured@musc.edu.
References
- Weick KE, Sutcliffe KM. Managing the unexpected: Resilient performance in an age of uncertainty, 2nd ed. 2007: Hoboken, NJ: John Wiley & Sons Inc.
- Agency for Healthcare Research and Quality. Becoming a high reliability organization: operational advice for hospital leaders. Agency for Healthcare Research and Quality website. Available at: http://www.ahrq.gov/qual/hroadvice/. Accessed Dec. 10, 2012.