User login
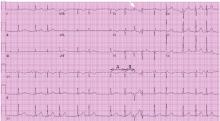
Presumed premature ventricular contractions
What is the diagnosis? Is a cardiology consult warranted?
AN ABERRANT CONDUCTION PATTERN
The finding seen in this electrocardiogram is known as the Ashman phenomenon, an aberrant conduction pattern seen in atrial dysrhythmias, mainly atrial fibrillation, atrial tachycardia, and atrial ectopy, when a relatively long cycle is followed by a relatively short cycle. The beat terminating the short cycle often has the morphology of right bundle branch block.
This pattern was first described by Gouaux and Ashman in 1947; however, the aberrant conduction of supraventricular impulses was first described by Lewis in 1910.1,2
Ashman phenomenon and right bundle branch block
The three criteria for the diagnosis of right bundle branch block in adults are:
- A QRS duration of 120 msec or more
- An rsr', rsR', or rSR' in leads V1 or V2 (the R' or r' deflection is usually wider than the initial R wave)
- The duration of the S wave in I and V6 is usually greater than that of the R wave or is greater than 40 msec.3
Variation in the heart rate (due to atrial fibrillation in this patient) affects the width of the QRS interval; the refractory period of a cycle is influenced by the RR interval of the previous cycle. Therefore, if after a long cycle with a consequent long refractory period, a shorter cycle follows, then the beat terminating the short cycle is likely to be aberrantly conducted because one of the bundle branches is still in the refractory period. Because the refractory period for the right bundle branch is longer than that of the left bundle branch, the right bundle branch block pattern is more common.4
In our patient’s tracing (Figure 1), the aberrantly conducted beat has the shortest coupling intervals of any of the conducted beats on the tracing. Although the RR interval preceding the short cycle is not the longest on this tracing, it is moderately long, and so the refractory period of the right bundle branch is moderately long.
The Ashman pattern vs ventricular premature beat
Atrial arrhythmias cause a variation in the refractory period of the bundle branches and the ventricular conduction system, and this explains why the Ashman phenomenon occurs more often in this setting. It is important to distinguish the aberrant conduction seen in the Ashman phenomenon, which electrophysiologically is restricted to the His-Purkinje system, from premature ventricular complexes and ventricular tachycardia.
The current criteria used to distinguish the Ashman phenomenon were described by Fisch5,6:
- A relatively long cycle immediately preceding the cycle terminated by the aberrant QRS complex: a short-long-short interval is even more likely to initiate aberration. The aberration can be left or right bundle branch block, or both, even in the same patient.
- Right bundle branch block morphology, with normal orientation of the initial QRS vector. Concealed perpetuation of the aberration is possible, and so a series of wide QRS supraventricular beats is possible.
- Irregular coupling of aberrant QRS complexes.
- Lack of a fully compensatory pause.
In Figure 1, the second aberrantly conducted beat is not as aberrant as the first, even though it is even more premature than the first. This can be explained because the refractory period of the right bundle branch has now shortened.
Also, the mechanism of aberrancy of the second beat may be partly the result of concealed perpetuation, ie, incomplete penetration of the His bundle depolarizations in either direction with secondary abnormalities of antegrade or retrograde conduction. This pattern is not directly reflected on the surface electrocardiogram but can be detected on intracardiac electrophysiologic studies.7 In concealed perpetuation, instead of inducing tachycardia, the extra stimuli are followed by pauses that exceed the tachycardia cycle length.8
Treated by managing the atrial arrhythmia
There is no specific treatment for the aberrant cycles. Rather, treatment is directed at the atrial arrhythmia.9 Adequate control of the underlying process and the atrial tachyarrhythmia itself is important. In our patient, control of the exacerbation of chronic obstructive pulmonary disease and of the heart rate improved the ventricular response to atrial fibrillation.
- Fisch C, Knoebel SB. Vagaries of acceleration dependent aberration. Br Heart J 1992; 67:16–24.
- Gouaux JL, Ashman R. Auricular fibrillation with aberration simulating ventricular paroxysmal tachycardia. Am Heart J 1947; 34:366–373.
- Surawicz B, Childers R, Deal BJ, et al; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009; 53:976–981.
- Antunes E, Brugada J, Steurer G, Andries E, Brugada P. The differential diagnosis of a regular tachycardia with a wide QRS complex on the 12-lead ECG: ventricular tachycardia, supraventricular tachycardia with aberrant intraventricular conduction, and supraventricular tachycardia with anterograde conduction over an accessory pathway. Pacing Clin Electrophysiol 1994; 17:1515–1524.
- Fisch C, Knoebel SB, eds. Clinical Electrocardiography of Arrhythmias. Armonk, NY: Futura Publishing Company, 2000:407.
- Gulamhusein S, Yee R, Ko PT, Klein GJ. Electrocardiographic criteria for differentiating aberrancy and ventricular extrasystole in chronic atrial fibrillation: validation by intracardiac recordings. J Electrocardiol 1985; 18:41–50.
- Josephson ME. Miscellaneous phenomena related to atrioventricular conduction. In: Clinical Cardiac Electrophysiology: Techniques and Interpretations. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2002:140–154.
- Josephson ME. Recurrent ventricular tachycardia. In: Clinical Cardiac Electrophysiology: Techniques and Interpretations. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2002:425–610.
- Hope RR, Lazzara R, Scherlag BJ. The induction of ventricular arrhythmias in acute myocardial ischemia by atrial pacing with long-short cycle sequences. Chest 1977; 71:651–658.
What is the diagnosis? Is a cardiology consult warranted?
AN ABERRANT CONDUCTION PATTERN
The finding seen in this electrocardiogram is known as the Ashman phenomenon, an aberrant conduction pattern seen in atrial dysrhythmias, mainly atrial fibrillation, atrial tachycardia, and atrial ectopy, when a relatively long cycle is followed by a relatively short cycle. The beat terminating the short cycle often has the morphology of right bundle branch block.
This pattern was first described by Gouaux and Ashman in 1947; however, the aberrant conduction of supraventricular impulses was first described by Lewis in 1910.1,2
Ashman phenomenon and right bundle branch block
The three criteria for the diagnosis of right bundle branch block in adults are:
- A QRS duration of 120 msec or more
- An rsr', rsR', or rSR' in leads V1 or V2 (the R' or r' deflection is usually wider than the initial R wave)
- The duration of the S wave in I and V6 is usually greater than that of the R wave or is greater than 40 msec.3
Variation in the heart rate (due to atrial fibrillation in this patient) affects the width of the QRS interval; the refractory period of a cycle is influenced by the RR interval of the previous cycle. Therefore, if after a long cycle with a consequent long refractory period, a shorter cycle follows, then the beat terminating the short cycle is likely to be aberrantly conducted because one of the bundle branches is still in the refractory period. Because the refractory period for the right bundle branch is longer than that of the left bundle branch, the right bundle branch block pattern is more common.4
In our patient’s tracing (Figure 1), the aberrantly conducted beat has the shortest coupling intervals of any of the conducted beats on the tracing. Although the RR interval preceding the short cycle is not the longest on this tracing, it is moderately long, and so the refractory period of the right bundle branch is moderately long.
The Ashman pattern vs ventricular premature beat
Atrial arrhythmias cause a variation in the refractory period of the bundle branches and the ventricular conduction system, and this explains why the Ashman phenomenon occurs more often in this setting. It is important to distinguish the aberrant conduction seen in the Ashman phenomenon, which electrophysiologically is restricted to the His-Purkinje system, from premature ventricular complexes and ventricular tachycardia.
The current criteria used to distinguish the Ashman phenomenon were described by Fisch5,6:
- A relatively long cycle immediately preceding the cycle terminated by the aberrant QRS complex: a short-long-short interval is even more likely to initiate aberration. The aberration can be left or right bundle branch block, or both, even in the same patient.
- Right bundle branch block morphology, with normal orientation of the initial QRS vector. Concealed perpetuation of the aberration is possible, and so a series of wide QRS supraventricular beats is possible.
- Irregular coupling of aberrant QRS complexes.
- Lack of a fully compensatory pause.
In Figure 1, the second aberrantly conducted beat is not as aberrant as the first, even though it is even more premature than the first. This can be explained because the refractory period of the right bundle branch has now shortened.
Also, the mechanism of aberrancy of the second beat may be partly the result of concealed perpetuation, ie, incomplete penetration of the His bundle depolarizations in either direction with secondary abnormalities of antegrade or retrograde conduction. This pattern is not directly reflected on the surface electrocardiogram but can be detected on intracardiac electrophysiologic studies.7 In concealed perpetuation, instead of inducing tachycardia, the extra stimuli are followed by pauses that exceed the tachycardia cycle length.8
Treated by managing the atrial arrhythmia
There is no specific treatment for the aberrant cycles. Rather, treatment is directed at the atrial arrhythmia.9 Adequate control of the underlying process and the atrial tachyarrhythmia itself is important. In our patient, control of the exacerbation of chronic obstructive pulmonary disease and of the heart rate improved the ventricular response to atrial fibrillation.
What is the diagnosis? Is a cardiology consult warranted?
AN ABERRANT CONDUCTION PATTERN
The finding seen in this electrocardiogram is known as the Ashman phenomenon, an aberrant conduction pattern seen in atrial dysrhythmias, mainly atrial fibrillation, atrial tachycardia, and atrial ectopy, when a relatively long cycle is followed by a relatively short cycle. The beat terminating the short cycle often has the morphology of right bundle branch block.
This pattern was first described by Gouaux and Ashman in 1947; however, the aberrant conduction of supraventricular impulses was first described by Lewis in 1910.1,2
Ashman phenomenon and right bundle branch block
The three criteria for the diagnosis of right bundle branch block in adults are:
- A QRS duration of 120 msec or more
- An rsr', rsR', or rSR' in leads V1 or V2 (the R' or r' deflection is usually wider than the initial R wave)
- The duration of the S wave in I and V6 is usually greater than that of the R wave or is greater than 40 msec.3
Variation in the heart rate (due to atrial fibrillation in this patient) affects the width of the QRS interval; the refractory period of a cycle is influenced by the RR interval of the previous cycle. Therefore, if after a long cycle with a consequent long refractory period, a shorter cycle follows, then the beat terminating the short cycle is likely to be aberrantly conducted because one of the bundle branches is still in the refractory period. Because the refractory period for the right bundle branch is longer than that of the left bundle branch, the right bundle branch block pattern is more common.4
In our patient’s tracing (Figure 1), the aberrantly conducted beat has the shortest coupling intervals of any of the conducted beats on the tracing. Although the RR interval preceding the short cycle is not the longest on this tracing, it is moderately long, and so the refractory period of the right bundle branch is moderately long.
The Ashman pattern vs ventricular premature beat
Atrial arrhythmias cause a variation in the refractory period of the bundle branches and the ventricular conduction system, and this explains why the Ashman phenomenon occurs more often in this setting. It is important to distinguish the aberrant conduction seen in the Ashman phenomenon, which electrophysiologically is restricted to the His-Purkinje system, from premature ventricular complexes and ventricular tachycardia.
The current criteria used to distinguish the Ashman phenomenon were described by Fisch5,6:
- A relatively long cycle immediately preceding the cycle terminated by the aberrant QRS complex: a short-long-short interval is even more likely to initiate aberration. The aberration can be left or right bundle branch block, or both, even in the same patient.
- Right bundle branch block morphology, with normal orientation of the initial QRS vector. Concealed perpetuation of the aberration is possible, and so a series of wide QRS supraventricular beats is possible.
- Irregular coupling of aberrant QRS complexes.
- Lack of a fully compensatory pause.
In Figure 1, the second aberrantly conducted beat is not as aberrant as the first, even though it is even more premature than the first. This can be explained because the refractory period of the right bundle branch has now shortened.
Also, the mechanism of aberrancy of the second beat may be partly the result of concealed perpetuation, ie, incomplete penetration of the His bundle depolarizations in either direction with secondary abnormalities of antegrade or retrograde conduction. This pattern is not directly reflected on the surface electrocardiogram but can be detected on intracardiac electrophysiologic studies.7 In concealed perpetuation, instead of inducing tachycardia, the extra stimuli are followed by pauses that exceed the tachycardia cycle length.8
Treated by managing the atrial arrhythmia
There is no specific treatment for the aberrant cycles. Rather, treatment is directed at the atrial arrhythmia.9 Adequate control of the underlying process and the atrial tachyarrhythmia itself is important. In our patient, control of the exacerbation of chronic obstructive pulmonary disease and of the heart rate improved the ventricular response to atrial fibrillation.
- Fisch C, Knoebel SB. Vagaries of acceleration dependent aberration. Br Heart J 1992; 67:16–24.
- Gouaux JL, Ashman R. Auricular fibrillation with aberration simulating ventricular paroxysmal tachycardia. Am Heart J 1947; 34:366–373.
- Surawicz B, Childers R, Deal BJ, et al; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009; 53:976–981.
- Antunes E, Brugada J, Steurer G, Andries E, Brugada P. The differential diagnosis of a regular tachycardia with a wide QRS complex on the 12-lead ECG: ventricular tachycardia, supraventricular tachycardia with aberrant intraventricular conduction, and supraventricular tachycardia with anterograde conduction over an accessory pathway. Pacing Clin Electrophysiol 1994; 17:1515–1524.
- Fisch C, Knoebel SB, eds. Clinical Electrocardiography of Arrhythmias. Armonk, NY: Futura Publishing Company, 2000:407.
- Gulamhusein S, Yee R, Ko PT, Klein GJ. Electrocardiographic criteria for differentiating aberrancy and ventricular extrasystole in chronic atrial fibrillation: validation by intracardiac recordings. J Electrocardiol 1985; 18:41–50.
- Josephson ME. Miscellaneous phenomena related to atrioventricular conduction. In: Clinical Cardiac Electrophysiology: Techniques and Interpretations. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2002:140–154.
- Josephson ME. Recurrent ventricular tachycardia. In: Clinical Cardiac Electrophysiology: Techniques and Interpretations. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2002:425–610.
- Hope RR, Lazzara R, Scherlag BJ. The induction of ventricular arrhythmias in acute myocardial ischemia by atrial pacing with long-short cycle sequences. Chest 1977; 71:651–658.
- Fisch C, Knoebel SB. Vagaries of acceleration dependent aberration. Br Heart J 1992; 67:16–24.
- Gouaux JL, Ashman R. Auricular fibrillation with aberration simulating ventricular paroxysmal tachycardia. Am Heart J 1947; 34:366–373.
- Surawicz B, Childers R, Deal BJ, et al; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009; 53:976–981.
- Antunes E, Brugada J, Steurer G, Andries E, Brugada P. The differential diagnosis of a regular tachycardia with a wide QRS complex on the 12-lead ECG: ventricular tachycardia, supraventricular tachycardia with aberrant intraventricular conduction, and supraventricular tachycardia with anterograde conduction over an accessory pathway. Pacing Clin Electrophysiol 1994; 17:1515–1524.
- Fisch C, Knoebel SB, eds. Clinical Electrocardiography of Arrhythmias. Armonk, NY: Futura Publishing Company, 2000:407.
- Gulamhusein S, Yee R, Ko PT, Klein GJ. Electrocardiographic criteria for differentiating aberrancy and ventricular extrasystole in chronic atrial fibrillation: validation by intracardiac recordings. J Electrocardiol 1985; 18:41–50.
- Josephson ME. Miscellaneous phenomena related to atrioventricular conduction. In: Clinical Cardiac Electrophysiology: Techniques and Interpretations. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2002:140–154.
- Josephson ME. Recurrent ventricular tachycardia. In: Clinical Cardiac Electrophysiology: Techniques and Interpretations. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2002:425–610.
- Hope RR, Lazzara R, Scherlag BJ. The induction of ventricular arrhythmias in acute myocardial ischemia by atrial pacing with long-short cycle sequences. Chest 1977; 71:651–658.