Opinion
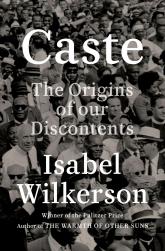
Understanding the enduring power of caste
- Author:
- Constance E. Dunlap, MD
- Ebony Dennis, PsyD
Publish date: September 24, 2020
Reading “Caste” is akin to the experience of gaining relief after struggling for years with a chronic malady, say Dr. Constance E. Dunlap and Dr....
Opinion

Management of race in psychotherapy and supervision
- Author:
- Constance E. Dunlap, MD
- Ebony Dennis, PsyD
- Flavia Desouza, MD, MHS
- Jessica Isom, MD, MPH
- And Myra Mathis, MD
Publish date: June 22, 2020
There is reason to believe that change can occur, say Dr. Constance E. Dunlap, Dr. Ebony Dennis, Dr. Flavia DeSouza, Dr. Jessica Isom, and Dr....
