User login
Parameters of Scratch Pleasurability in the Management of Pruritic Conditions
To the Editor:
The itch-scratch cycle refers to the sequence created when a pruritic skin condition leads to scratching and skin barrier disruption, ultimately facilitating secondary skin changes and neural activation that prolongs pruritus. In patients with pruritic conditions, the itch-scratch cycle often can run unrestrained, with patients unaware of their scratching habits. Understanding what drives a patient to scratch, such as the pleasure gained from scratching, may be beneficial for dermatologists combating a patient’s scratching habits. The earliest documented attempts to understand the mechanism of an itch were made in Greece around the fifth century, but the pathophysiology of this sensation still is not fully understood. The Latin term pruritus refers to itching, irritation, or sexual excitement, while the Greek term knêsmos and related words also denote itch in an irritating or pleasurable sense.1 This paradoxical duality of irritation and pleasure is a phenomenon all too well understood by those affected with pruritic symptoms.
Although there are many measured characteristics of an itch, the pleasure granted from scratching an itch rarely is addressed. Understanding the factors influencing the pleasurability of scratching could help improve management and outcomes of patients’ pruritic conditions.
Pruritus is associated with a wide array of etiologies including dermatologic, infectious, metabolic, and autoimmune, but unanimously it evokes a strong desire to scratch. Scratching an itch often yields temporary relief from the irritation by dispensing a complex sensory concoction between pleasure and pain.2 The neurobiology behind this pleasure phenomenon is inconclusive. Some hypotheses point to how scratching-induced pleasure may be derived from the deactivation or inhibition of the unpleasant sensation of an itch in the central nervous system, the stimulation of the reward signals in the C-fiber system in the peripheral nervous system, the release of pruritis-inhibiting prostaglandin D2, or a combination of these pathways. Levels of sensation and pleasure induced from itch attenuation by scratching even vary based on anatomic location. One study demonstrated that, when compared to the forearms, the ankles and back perceived baseline induced itch most intensely, but no significant difference in perceived itch intensity was found between the ankles and back. Additionally, scratching an itchy back or ankle notably induced more pleasure when compared to the forearms, but there was no significant difference in scratching pleasurability between the ankle and back.3
Although there are adequate questionnaires and scales (eg, ItchyQoL,4 Skindex-16, Skindex-29) to quantify the severity of pruritus and its effects on a patient’s quality of life, these measurements do not assess the pleasure yielded from scratching, the impact of scratch pleasure on the patient experience, or the effect of scratch pleasure on the disease state.4 It appears that there are inadequate assessment tools to define factors associated with the pleasurability of scratching. A PubMed search of articles indexed for MEDLINE using the terms scratching pleasure scale and pruritus pleasure questionnaire yielded scarce results measuring patient perspectives on scratching-associated pleasure. A pertinent study performed by O’Neill et al5 compared the differences in itch characteristics between patients with psoriasis and those with atopic dermatitis using a web-based questionnaire featuring a numerical pleasure scale (ranging from −5 [highly unpleasurable] to +5 [highly pleasurable]) on an 11-point Likert scale. The questionnaire sought to measure the effects of scratching during a typical episode of itch within the past 2 weeks. Scratching was found pleasurable in both groups of patients.5 Another web-based questionnaire that characterized pleasurability in scratching a typical episode of itch in individuals with atopic dermatitis using a −5 to +5 Likert scale (−5 [highly unpleasurable] to +5 [highly pleasurable]) found that most participants perceived scratching as pleasurable and that there was a positive correlation between itch intensity and scratch pleasurability.6 Both of these studies quantified that scratching an itch is pleasurable, a correlation that may not come as a surprise. This direct correlation suggests that a more detailed analysis of this scratch pleasure could be beneficial in the management of pruritic conditions.
Treating the underlying cause of an itch is key to inhibiting the sensation; in some cases, anti-itch medications must be used. Current medications have limited effects on itch relief, but an expanding understanding of itch pathophysiology through clinical and laboratory research in the fields of dermatology, immunology, and neurology is paving the way for promising new therapeutic medications.7-11 In a review of the literature, Sanders and Akiyama12 elucidated the influence of stress and anxiety in scratching an itch and the way in which both pharmacologic and nonpharmacologic (ie, psychological and educational interventions) may be used to help break the itch-scratch cycle. Possible techniques include habit-reversal training, relaxation therapy, and cognitive behavioral therapy.13 Understanding patient perspectives on the pleasure yielded from scratching an itch and the disease factors that influence this pleasure seeking are paramount to reducing patient scratching. In understanding the pleasurability of scratching in pruritic conditions, the itch-scratch cycle and its accompanying deleterious effects (eg, stress, anxiety, pain, infection, secondary skin changes) can be broken.
The pleasure yielded from scratching an itch is a component of patient scratching habits that should be analyzed and quantified to reduce itch in pruritic conditions, mitigate damaging consequences of scratching, and improve the quality of life of patients with pruritic conditions. Furthermore, this understanding may help guide clinicians in management, such as counseling patients on the itch-scratch cycle and deciding which forthcoming medications could ameliorate a patient’s pruritic symptoms.
- Weisshaar E, Grüll V, König A, et al. The symptom of itch in medical history: highlights through the centuries. Int J Dermatol. 2009;48:1385-1394.
- Lavery MJ, Kinney MO, Mochizuki H, et al. Pruritus: an overview. what drives people to scratch an itch? Ulster Med J. 2016;85:164-173.
- Bin Saif GA, Papoiu ADP, Banari L, et al. The pleasurability of scratching an itch: a psychophysical and topographical assessment. Br J Dermatol. 2012;166:981-985.
- Desai NS, Poindexter GB, Monthrope YM, et al. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59:234-244.
- O’Neill JL, Chan YH, Rapp SR, et al. Differences in itch characteristics between psoriasis and atopic dermatitis patients: results of a web-based questionnaire. Acta Derm Venereol. 2011;91:537-540.
- Dawn A, Papoiu ADP, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160:642-644.
- Yosipovitch G, Rosen JD, Hashimoto T. Itch: from mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol. 2018;142:1375-1390.
- Yosipovitch G, Misery L, Proksch E, et al. Skin barrier damage and itch: review of mechanisms, topical management and future directions. Acta Derm Venereol. 2019;99:1201-1209.
- Dong X, Dong X. Peripheral and central mechanisms of itch. Neuron. 2018;98:482-494.
- Lerner EA. Pathophysiology of itch. Dermatol Clin. 2018;36:175-177.
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982.
- Sanders KM, Akiyama T. The vicious cycle of itch and anxiety. Neurosci Biobehav Rev. 2018;87:17-26.
- Sanders KM, Nattkemper LA, Yosipovitch G. Advances in understanding itching and scratching: a new era of targeted treatments [published online August 22, 2016]. F1000Res. doi:10.12688/f1000research.8659.
To the Editor:
The itch-scratch cycle refers to the sequence created when a pruritic skin condition leads to scratching and skin barrier disruption, ultimately facilitating secondary skin changes and neural activation that prolongs pruritus. In patients with pruritic conditions, the itch-scratch cycle often can run unrestrained, with patients unaware of their scratching habits. Understanding what drives a patient to scratch, such as the pleasure gained from scratching, may be beneficial for dermatologists combating a patient’s scratching habits. The earliest documented attempts to understand the mechanism of an itch were made in Greece around the fifth century, but the pathophysiology of this sensation still is not fully understood. The Latin term pruritus refers to itching, irritation, or sexual excitement, while the Greek term knêsmos and related words also denote itch in an irritating or pleasurable sense.1 This paradoxical duality of irritation and pleasure is a phenomenon all too well understood by those affected with pruritic symptoms.
Although there are many measured characteristics of an itch, the pleasure granted from scratching an itch rarely is addressed. Understanding the factors influencing the pleasurability of scratching could help improve management and outcomes of patients’ pruritic conditions.
Pruritus is associated with a wide array of etiologies including dermatologic, infectious, metabolic, and autoimmune, but unanimously it evokes a strong desire to scratch. Scratching an itch often yields temporary relief from the irritation by dispensing a complex sensory concoction between pleasure and pain.2 The neurobiology behind this pleasure phenomenon is inconclusive. Some hypotheses point to how scratching-induced pleasure may be derived from the deactivation or inhibition of the unpleasant sensation of an itch in the central nervous system, the stimulation of the reward signals in the C-fiber system in the peripheral nervous system, the release of pruritis-inhibiting prostaglandin D2, or a combination of these pathways. Levels of sensation and pleasure induced from itch attenuation by scratching even vary based on anatomic location. One study demonstrated that, when compared to the forearms, the ankles and back perceived baseline induced itch most intensely, but no significant difference in perceived itch intensity was found between the ankles and back. Additionally, scratching an itchy back or ankle notably induced more pleasure when compared to the forearms, but there was no significant difference in scratching pleasurability between the ankle and back.3
Although there are adequate questionnaires and scales (eg, ItchyQoL,4 Skindex-16, Skindex-29) to quantify the severity of pruritus and its effects on a patient’s quality of life, these measurements do not assess the pleasure yielded from scratching, the impact of scratch pleasure on the patient experience, or the effect of scratch pleasure on the disease state.4 It appears that there are inadequate assessment tools to define factors associated with the pleasurability of scratching. A PubMed search of articles indexed for MEDLINE using the terms scratching pleasure scale and pruritus pleasure questionnaire yielded scarce results measuring patient perspectives on scratching-associated pleasure. A pertinent study performed by O’Neill et al5 compared the differences in itch characteristics between patients with psoriasis and those with atopic dermatitis using a web-based questionnaire featuring a numerical pleasure scale (ranging from −5 [highly unpleasurable] to +5 [highly pleasurable]) on an 11-point Likert scale. The questionnaire sought to measure the effects of scratching during a typical episode of itch within the past 2 weeks. Scratching was found pleasurable in both groups of patients.5 Another web-based questionnaire that characterized pleasurability in scratching a typical episode of itch in individuals with atopic dermatitis using a −5 to +5 Likert scale (−5 [highly unpleasurable] to +5 [highly pleasurable]) found that most participants perceived scratching as pleasurable and that there was a positive correlation between itch intensity and scratch pleasurability.6 Both of these studies quantified that scratching an itch is pleasurable, a correlation that may not come as a surprise. This direct correlation suggests that a more detailed analysis of this scratch pleasure could be beneficial in the management of pruritic conditions.
Treating the underlying cause of an itch is key to inhibiting the sensation; in some cases, anti-itch medications must be used. Current medications have limited effects on itch relief, but an expanding understanding of itch pathophysiology through clinical and laboratory research in the fields of dermatology, immunology, and neurology is paving the way for promising new therapeutic medications.7-11 In a review of the literature, Sanders and Akiyama12 elucidated the influence of stress and anxiety in scratching an itch and the way in which both pharmacologic and nonpharmacologic (ie, psychological and educational interventions) may be used to help break the itch-scratch cycle. Possible techniques include habit-reversal training, relaxation therapy, and cognitive behavioral therapy.13 Understanding patient perspectives on the pleasure yielded from scratching an itch and the disease factors that influence this pleasure seeking are paramount to reducing patient scratching. In understanding the pleasurability of scratching in pruritic conditions, the itch-scratch cycle and its accompanying deleterious effects (eg, stress, anxiety, pain, infection, secondary skin changes) can be broken.
The pleasure yielded from scratching an itch is a component of patient scratching habits that should be analyzed and quantified to reduce itch in pruritic conditions, mitigate damaging consequences of scratching, and improve the quality of life of patients with pruritic conditions. Furthermore, this understanding may help guide clinicians in management, such as counseling patients on the itch-scratch cycle and deciding which forthcoming medications could ameliorate a patient’s pruritic symptoms.
To the Editor:
The itch-scratch cycle refers to the sequence created when a pruritic skin condition leads to scratching and skin barrier disruption, ultimately facilitating secondary skin changes and neural activation that prolongs pruritus. In patients with pruritic conditions, the itch-scratch cycle often can run unrestrained, with patients unaware of their scratching habits. Understanding what drives a patient to scratch, such as the pleasure gained from scratching, may be beneficial for dermatologists combating a patient’s scratching habits. The earliest documented attempts to understand the mechanism of an itch were made in Greece around the fifth century, but the pathophysiology of this sensation still is not fully understood. The Latin term pruritus refers to itching, irritation, or sexual excitement, while the Greek term knêsmos and related words also denote itch in an irritating or pleasurable sense.1 This paradoxical duality of irritation and pleasure is a phenomenon all too well understood by those affected with pruritic symptoms.
Although there are many measured characteristics of an itch, the pleasure granted from scratching an itch rarely is addressed. Understanding the factors influencing the pleasurability of scratching could help improve management and outcomes of patients’ pruritic conditions.
Pruritus is associated with a wide array of etiologies including dermatologic, infectious, metabolic, and autoimmune, but unanimously it evokes a strong desire to scratch. Scratching an itch often yields temporary relief from the irritation by dispensing a complex sensory concoction between pleasure and pain.2 The neurobiology behind this pleasure phenomenon is inconclusive. Some hypotheses point to how scratching-induced pleasure may be derived from the deactivation or inhibition of the unpleasant sensation of an itch in the central nervous system, the stimulation of the reward signals in the C-fiber system in the peripheral nervous system, the release of pruritis-inhibiting prostaglandin D2, or a combination of these pathways. Levels of sensation and pleasure induced from itch attenuation by scratching even vary based on anatomic location. One study demonstrated that, when compared to the forearms, the ankles and back perceived baseline induced itch most intensely, but no significant difference in perceived itch intensity was found between the ankles and back. Additionally, scratching an itchy back or ankle notably induced more pleasure when compared to the forearms, but there was no significant difference in scratching pleasurability between the ankle and back.3
Although there are adequate questionnaires and scales (eg, ItchyQoL,4 Skindex-16, Skindex-29) to quantify the severity of pruritus and its effects on a patient’s quality of life, these measurements do not assess the pleasure yielded from scratching, the impact of scratch pleasure on the patient experience, or the effect of scratch pleasure on the disease state.4 It appears that there are inadequate assessment tools to define factors associated with the pleasurability of scratching. A PubMed search of articles indexed for MEDLINE using the terms scratching pleasure scale and pruritus pleasure questionnaire yielded scarce results measuring patient perspectives on scratching-associated pleasure. A pertinent study performed by O’Neill et al5 compared the differences in itch characteristics between patients with psoriasis and those with atopic dermatitis using a web-based questionnaire featuring a numerical pleasure scale (ranging from −5 [highly unpleasurable] to +5 [highly pleasurable]) on an 11-point Likert scale. The questionnaire sought to measure the effects of scratching during a typical episode of itch within the past 2 weeks. Scratching was found pleasurable in both groups of patients.5 Another web-based questionnaire that characterized pleasurability in scratching a typical episode of itch in individuals with atopic dermatitis using a −5 to +5 Likert scale (−5 [highly unpleasurable] to +5 [highly pleasurable]) found that most participants perceived scratching as pleasurable and that there was a positive correlation between itch intensity and scratch pleasurability.6 Both of these studies quantified that scratching an itch is pleasurable, a correlation that may not come as a surprise. This direct correlation suggests that a more detailed analysis of this scratch pleasure could be beneficial in the management of pruritic conditions.
Treating the underlying cause of an itch is key to inhibiting the sensation; in some cases, anti-itch medications must be used. Current medications have limited effects on itch relief, but an expanding understanding of itch pathophysiology through clinical and laboratory research in the fields of dermatology, immunology, and neurology is paving the way for promising new therapeutic medications.7-11 In a review of the literature, Sanders and Akiyama12 elucidated the influence of stress and anxiety in scratching an itch and the way in which both pharmacologic and nonpharmacologic (ie, psychological and educational interventions) may be used to help break the itch-scratch cycle. Possible techniques include habit-reversal training, relaxation therapy, and cognitive behavioral therapy.13 Understanding patient perspectives on the pleasure yielded from scratching an itch and the disease factors that influence this pleasure seeking are paramount to reducing patient scratching. In understanding the pleasurability of scratching in pruritic conditions, the itch-scratch cycle and its accompanying deleterious effects (eg, stress, anxiety, pain, infection, secondary skin changes) can be broken.
The pleasure yielded from scratching an itch is a component of patient scratching habits that should be analyzed and quantified to reduce itch in pruritic conditions, mitigate damaging consequences of scratching, and improve the quality of life of patients with pruritic conditions. Furthermore, this understanding may help guide clinicians in management, such as counseling patients on the itch-scratch cycle and deciding which forthcoming medications could ameliorate a patient’s pruritic symptoms.
- Weisshaar E, Grüll V, König A, et al. The symptom of itch in medical history: highlights through the centuries. Int J Dermatol. 2009;48:1385-1394.
- Lavery MJ, Kinney MO, Mochizuki H, et al. Pruritus: an overview. what drives people to scratch an itch? Ulster Med J. 2016;85:164-173.
- Bin Saif GA, Papoiu ADP, Banari L, et al. The pleasurability of scratching an itch: a psychophysical and topographical assessment. Br J Dermatol. 2012;166:981-985.
- Desai NS, Poindexter GB, Monthrope YM, et al. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59:234-244.
- O’Neill JL, Chan YH, Rapp SR, et al. Differences in itch characteristics between psoriasis and atopic dermatitis patients: results of a web-based questionnaire. Acta Derm Venereol. 2011;91:537-540.
- Dawn A, Papoiu ADP, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160:642-644.
- Yosipovitch G, Rosen JD, Hashimoto T. Itch: from mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol. 2018;142:1375-1390.
- Yosipovitch G, Misery L, Proksch E, et al. Skin barrier damage and itch: review of mechanisms, topical management and future directions. Acta Derm Venereol. 2019;99:1201-1209.
- Dong X, Dong X. Peripheral and central mechanisms of itch. Neuron. 2018;98:482-494.
- Lerner EA. Pathophysiology of itch. Dermatol Clin. 2018;36:175-177.
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982.
- Sanders KM, Akiyama T. The vicious cycle of itch and anxiety. Neurosci Biobehav Rev. 2018;87:17-26.
- Sanders KM, Nattkemper LA, Yosipovitch G. Advances in understanding itching and scratching: a new era of targeted treatments [published online August 22, 2016]. F1000Res. doi:10.12688/f1000research.8659.
- Weisshaar E, Grüll V, König A, et al. The symptom of itch in medical history: highlights through the centuries. Int J Dermatol. 2009;48:1385-1394.
- Lavery MJ, Kinney MO, Mochizuki H, et al. Pruritus: an overview. what drives people to scratch an itch? Ulster Med J. 2016;85:164-173.
- Bin Saif GA, Papoiu ADP, Banari L, et al. The pleasurability of scratching an itch: a psychophysical and topographical assessment. Br J Dermatol. 2012;166:981-985.
- Desai NS, Poindexter GB, Monthrope YM, et al. A pilot quality-of-life instrument for pruritus. J Am Acad Dermatol. 2008;59:234-244.
- O’Neill JL, Chan YH, Rapp SR, et al. Differences in itch characteristics between psoriasis and atopic dermatitis patients: results of a web-based questionnaire. Acta Derm Venereol. 2011;91:537-540.
- Dawn A, Papoiu ADP, Chan YH, et al. Itch characteristics in atopic dermatitis: results of a web-based questionnaire. Br J Dermatol. 2009;160:642-644.
- Yosipovitch G, Rosen JD, Hashimoto T. Itch: from mechanism to (novel) therapeutic approaches. J Allergy Clin Immunol. 2018;142:1375-1390.
- Yosipovitch G, Misery L, Proksch E, et al. Skin barrier damage and itch: review of mechanisms, topical management and future directions. Acta Derm Venereol. 2019;99:1201-1209.
- Dong X, Dong X. Peripheral and central mechanisms of itch. Neuron. 2018;98:482-494.
- Lerner EA. Pathophysiology of itch. Dermatol Clin. 2018;36:175-177.
- Cevikbas F, Lerner EA. Physiology and pathophysiology of itch. Physiol Rev. 2020;100:945-982.
- Sanders KM, Akiyama T. The vicious cycle of itch and anxiety. Neurosci Biobehav Rev. 2018;87:17-26.
- Sanders KM, Nattkemper LA, Yosipovitch G. Advances in understanding itching and scratching: a new era of targeted treatments [published online August 22, 2016]. F1000Res. doi:10.12688/f1000research.8659.
Practice Points
- In individuals with pruritic skin conditions, the itch-scratch cycle can have damaging consequences such as anxiety, infection, and secondary skin changes.
- Understanding the pleasurability of scratching in pruritic skin conditions allows providers to help patients break the itch-scratch cycle and improve quality of life.
Postinflammatory Hyperpigmentation Following Treatment of Hyperkeratosis Lenticularis Perstans With Tazarotene Cream 0.1%
To the Editor:
Hyperkeratosis lenticularis perstans (HLP), or Flegel disease, is a rare keratinization disorder characterized by asymptomatic, red-brown, 1- to 5-mm papules with irregular horny scales commonly seen on the dorsal feet and lower legs.1 Hyperkeratosis lenticularis perstans is notorious for being difficult to treat. Various treatment options, including 5-fluorouracil, topical and oral retinoids, vitamin D3 derivatives, psoralen plus UVA therapy, and dermabrasion, have been explored but none have proven to be consistently effective.
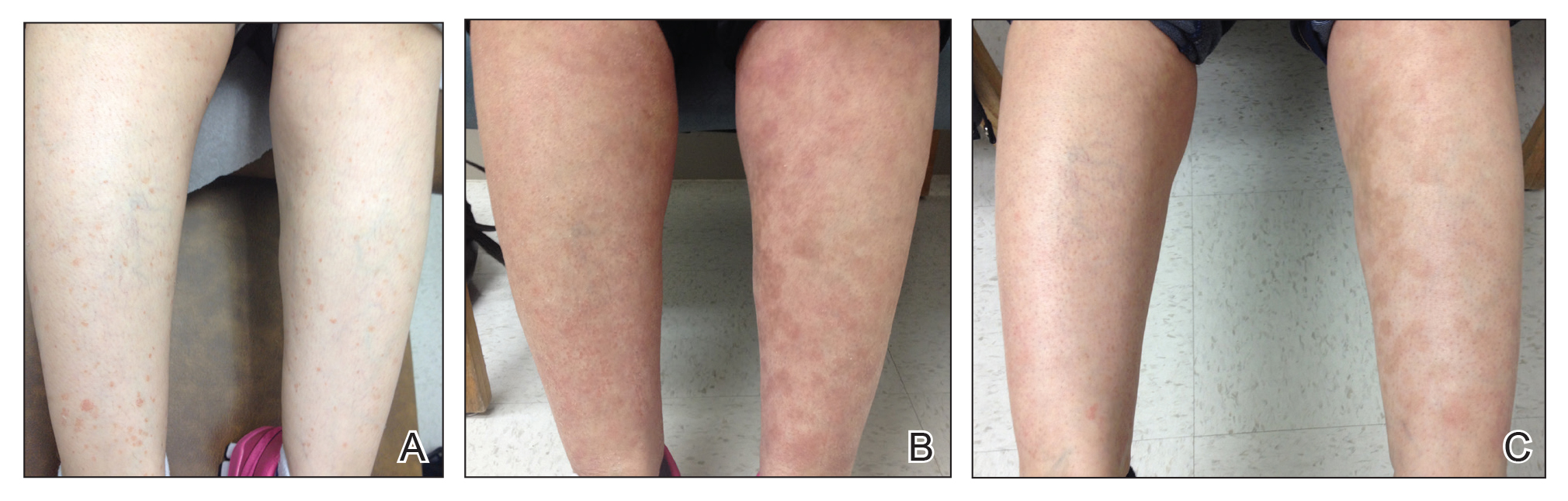
A woman in her 50s presented with an asymptomatic eruption on the legs and thighs that had been present for the last 20 years. She had been misdiagnosed by multiple outside providers with atopic dermatitis and was treated with topical steroids without considerable improvement. Upon initial presentation to our clinic , physical examination revealed a woman with Fitzpatrick skin type II with multiple hyperpigmented, red-brown, 2- to 6-mm papules on the extensor surfaces of the lower legs and upper thighs (Figure, A). A 3-mm punch biopsy of a lesion on the right upper thigh revealed hyperkeratosis and parakeratosis with basal layer degeneration and a perivascular lymphocytic infiltrate. The clinical and histopathologic findings were consistent with HLP.
The patient was started on treatment with 5-fluorouracil cream on the right leg and tazarotene cream 0.1% on the left leg to determine which agent would work best. After 9 weeks of treatment, slight improvement was observed on both legs, but the lesions were still erythematous (Figure, B). Treatment was continued, and after 14 weeks complete resolution of the lesions was noted on both legs; however, postinflammatory hyperpigmentation (PIH) was observed on the left leg, which had been treated with tazarotene (Figure, C). The patient was lost to follow-up prior to treatment of the PIH.
Postinflammatory hyperpigmentation is an acquired excess of pigment due to a prior disease process such as an infection, allergic reaction, trauma, inflammatory disease, or drug reaction. In our patient, this finding was unusual because tazarotene has been shown to be an effective treatment of PIH.2,3
In PIH, there is either abnormal production or distribution of melanin pigment in the epidermis and/or dermis. Several mechanisms for PIH have been suggested. One potential mechanism is disruption of the basal cell layer due to dermal lymphocytic inflammation, causing melanin to be released and trapped by macrophages present in the dermal papillae. Another possible mechanism is epidermal hypermelanosis, in which the release and oxidation of arachidonic acid to prostaglandins and leukotrienes alters immune cells and melanocytes, causing an increase in melanin and increased transfer of melanin to keratinocytes in the surrounding epidermis.4
Treatment of PIH can be a difficult and prolonged process, especially when a dermal rather than epidermal melanosis is observed. Topical retinoids, topical hydroquinone, azelaic acid, corticosteroids, tretinoin cream, glycolic acid, and trichloroacetic acid have been shown to be effective in treating epidermal PIH. Tazarotene is a synthetic retinoid that has been proven to be an effective treatment of PIH3; however, in our patient the PIH progressed with treatment. One plausible explanation is that irritation caused by the medication led to further PIH.2,5
It is uncommon for tazarotene to cause PIH. Hyperpigmentation is listed as an adverse effect observed during the postmarketing experience according to one manufacturer6 and the US Food and Drug Administration; however, details about prior incidents of hyperpigmentation have not been reported in the literature. Our case is unique because both treatments showed considerable improvement in HLP, but more PIH was observed on the tazarotene-treated leg.
- Bean SF. Hyperkeratosis lenticularis perstans. a clinical, histopathologic, and genetic study. Arch Dermatol. 1969;99:705-709.
- Callender V, St. Surin-Lord S, Davis E, et al. Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. Am J Clin Dermatol. 2011;12:87-99.
- McEvoy G. Tazarotene (topical). In: AHFS Drug Information. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2014:84-92.
- Lacz N, Vafaie J, Kihiczak N, et al. Postinflammatory hyperpigmentation: a common but troubling condition. Int J Dermatol. 2004;43:362-365.
- Tazorac (tazarotene) cream [package insert]. Irvine, CA: Allergan, Inc; 2013.
- Tazorac (tazarotene) gel [package insert]. Irvine, CA: Allergan, Inc; 2014.
To the Editor:
Hyperkeratosis lenticularis perstans (HLP), or Flegel disease, is a rare keratinization disorder characterized by asymptomatic, red-brown, 1- to 5-mm papules with irregular horny scales commonly seen on the dorsal feet and lower legs.1 Hyperkeratosis lenticularis perstans is notorious for being difficult to treat. Various treatment options, including 5-fluorouracil, topical and oral retinoids, vitamin D3 derivatives, psoralen plus UVA therapy, and dermabrasion, have been explored but none have proven to be consistently effective.
A woman in her 50s presented with an asymptomatic eruption on the legs and thighs that had been present for the last 20 years. She had been misdiagnosed by multiple outside providers with atopic dermatitis and was treated with topical steroids without considerable improvement. Upon initial presentation to our clinic , physical examination revealed a woman with Fitzpatrick skin type II with multiple hyperpigmented, red-brown, 2- to 6-mm papules on the extensor surfaces of the lower legs and upper thighs (Figure, A). A 3-mm punch biopsy of a lesion on the right upper thigh revealed hyperkeratosis and parakeratosis with basal layer degeneration and a perivascular lymphocytic infiltrate. The clinical and histopathologic findings were consistent with HLP.
The patient was started on treatment with 5-fluorouracil cream on the right leg and tazarotene cream 0.1% on the left leg to determine which agent would work best. After 9 weeks of treatment, slight improvement was observed on both legs, but the lesions were still erythematous (Figure, B). Treatment was continued, and after 14 weeks complete resolution of the lesions was noted on both legs; however, postinflammatory hyperpigmentation (PIH) was observed on the left leg, which had been treated with tazarotene (Figure, C). The patient was lost to follow-up prior to treatment of the PIH.
Postinflammatory hyperpigmentation is an acquired excess of pigment due to a prior disease process such as an infection, allergic reaction, trauma, inflammatory disease, or drug reaction. In our patient, this finding was unusual because tazarotene has been shown to be an effective treatment of PIH.2,3
In PIH, there is either abnormal production or distribution of melanin pigment in the epidermis and/or dermis. Several mechanisms for PIH have been suggested. One potential mechanism is disruption of the basal cell layer due to dermal lymphocytic inflammation, causing melanin to be released and trapped by macrophages present in the dermal papillae. Another possible mechanism is epidermal hypermelanosis, in which the release and oxidation of arachidonic acid to prostaglandins and leukotrienes alters immune cells and melanocytes, causing an increase in melanin and increased transfer of melanin to keratinocytes in the surrounding epidermis.4
Treatment of PIH can be a difficult and prolonged process, especially when a dermal rather than epidermal melanosis is observed. Topical retinoids, topical hydroquinone, azelaic acid, corticosteroids, tretinoin cream, glycolic acid, and trichloroacetic acid have been shown to be effective in treating epidermal PIH. Tazarotene is a synthetic retinoid that has been proven to be an effective treatment of PIH3; however, in our patient the PIH progressed with treatment. One plausible explanation is that irritation caused by the medication led to further PIH.2,5
It is uncommon for tazarotene to cause PIH. Hyperpigmentation is listed as an adverse effect observed during the postmarketing experience according to one manufacturer6 and the US Food and Drug Administration; however, details about prior incidents of hyperpigmentation have not been reported in the literature. Our case is unique because both treatments showed considerable improvement in HLP, but more PIH was observed on the tazarotene-treated leg.
To the Editor:
Hyperkeratosis lenticularis perstans (HLP), or Flegel disease, is a rare keratinization disorder characterized by asymptomatic, red-brown, 1- to 5-mm papules with irregular horny scales commonly seen on the dorsal feet and lower legs.1 Hyperkeratosis lenticularis perstans is notorious for being difficult to treat. Various treatment options, including 5-fluorouracil, topical and oral retinoids, vitamin D3 derivatives, psoralen plus UVA therapy, and dermabrasion, have been explored but none have proven to be consistently effective.
A woman in her 50s presented with an asymptomatic eruption on the legs and thighs that had been present for the last 20 years. She had been misdiagnosed by multiple outside providers with atopic dermatitis and was treated with topical steroids without considerable improvement. Upon initial presentation to our clinic , physical examination revealed a woman with Fitzpatrick skin type II with multiple hyperpigmented, red-brown, 2- to 6-mm papules on the extensor surfaces of the lower legs and upper thighs (Figure, A). A 3-mm punch biopsy of a lesion on the right upper thigh revealed hyperkeratosis and parakeratosis with basal layer degeneration and a perivascular lymphocytic infiltrate. The clinical and histopathologic findings were consistent with HLP.
The patient was started on treatment with 5-fluorouracil cream on the right leg and tazarotene cream 0.1% on the left leg to determine which agent would work best. After 9 weeks of treatment, slight improvement was observed on both legs, but the lesions were still erythematous (Figure, B). Treatment was continued, and after 14 weeks complete resolution of the lesions was noted on both legs; however, postinflammatory hyperpigmentation (PIH) was observed on the left leg, which had been treated with tazarotene (Figure, C). The patient was lost to follow-up prior to treatment of the PIH.
Postinflammatory hyperpigmentation is an acquired excess of pigment due to a prior disease process such as an infection, allergic reaction, trauma, inflammatory disease, or drug reaction. In our patient, this finding was unusual because tazarotene has been shown to be an effective treatment of PIH.2,3
In PIH, there is either abnormal production or distribution of melanin pigment in the epidermis and/or dermis. Several mechanisms for PIH have been suggested. One potential mechanism is disruption of the basal cell layer due to dermal lymphocytic inflammation, causing melanin to be released and trapped by macrophages present in the dermal papillae. Another possible mechanism is epidermal hypermelanosis, in which the release and oxidation of arachidonic acid to prostaglandins and leukotrienes alters immune cells and melanocytes, causing an increase in melanin and increased transfer of melanin to keratinocytes in the surrounding epidermis.4
Treatment of PIH can be a difficult and prolonged process, especially when a dermal rather than epidermal melanosis is observed. Topical retinoids, topical hydroquinone, azelaic acid, corticosteroids, tretinoin cream, glycolic acid, and trichloroacetic acid have been shown to be effective in treating epidermal PIH. Tazarotene is a synthetic retinoid that has been proven to be an effective treatment of PIH3; however, in our patient the PIH progressed with treatment. One plausible explanation is that irritation caused by the medication led to further PIH.2,5
It is uncommon for tazarotene to cause PIH. Hyperpigmentation is listed as an adverse effect observed during the postmarketing experience according to one manufacturer6 and the US Food and Drug Administration; however, details about prior incidents of hyperpigmentation have not been reported in the literature. Our case is unique because both treatments showed considerable improvement in HLP, but more PIH was observed on the tazarotene-treated leg.
- Bean SF. Hyperkeratosis lenticularis perstans. a clinical, histopathologic, and genetic study. Arch Dermatol. 1969;99:705-709.
- Callender V, St. Surin-Lord S, Davis E, et al. Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. Am J Clin Dermatol. 2011;12:87-99.
- McEvoy G. Tazarotene (topical). In: AHFS Drug Information. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2014:84-92.
- Lacz N, Vafaie J, Kihiczak N, et al. Postinflammatory hyperpigmentation: a common but troubling condition. Int J Dermatol. 2004;43:362-365.
- Tazorac (tazarotene) cream [package insert]. Irvine, CA: Allergan, Inc; 2013.
- Tazorac (tazarotene) gel [package insert]. Irvine, CA: Allergan, Inc; 2014.
- Bean SF. Hyperkeratosis lenticularis perstans. a clinical, histopathologic, and genetic study. Arch Dermatol. 1969;99:705-709.
- Callender V, St. Surin-Lord S, Davis E, et al. Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. Am J Clin Dermatol. 2011;12:87-99.
- McEvoy G. Tazarotene (topical). In: AHFS Drug Information. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2014:84-92.
- Lacz N, Vafaie J, Kihiczak N, et al. Postinflammatory hyperpigmentation: a common but troubling condition. Int J Dermatol. 2004;43:362-365.
- Tazorac (tazarotene) cream [package insert]. Irvine, CA: Allergan, Inc; 2013.
- Tazorac (tazarotene) gel [package insert]. Irvine, CA: Allergan, Inc; 2014.
Practice Points
- Hyperkeratosis lenticularis perstans is a rare keratinization disorder that presents with asymptomatic red-brown papules with irregular horny scales on the lower extremities.
- Hyperkeratosis lenticularis perstans can be difficult to diagnose and treat. Hematoxylin and eosin staining generally will show hyperkeratosis and parakeratosis with basal layer degeneration and a perivascular lymphocytic infiltrate.
- Tazarotene cream 0.1% is a synthetic retinoid sometimes used for treatment of hyperpigmentation, but it also can cause postinflammatory hyperpigmentation.