User login
Is expectant management a safe alternative to immediate delivery in patients with PPROM close to term?
Preterm premature rupture of membranes (PPROM) refers to rupture of membranes prior to the onset of labor before 37 weeks’ gestation. It accounts for one-third of all preterm births.1 Pregnancy complications associated with PPROM include intrauterine infection (chorioamnionitis), preterm labor, and placental abruption. Should such complications develop, immediate delivery is indicated. When to recommend elective delivery in the absence of complications, however, remains controversial.
The American College of Obstetricians and Gynecologists (ACOG) currently recommends elective delivery at or after 34 weeks’ gestation,2 because the prevailing evidence suggests that the risk of pregnancy-related complications (especially ascending infection) exceeds the risks of iatrogenic prematurity at this gestational age. However, ACOG acknowledges that this recommendation is based on “limited and inconsistent scientific evidence.”2 To address deficiencies in the literature, investigators designed the PPROMT (preterm prelabor rupture of the membranes close to term) trial to study women with ruptured membranes before the onset of labor between 34 and 37 weeks’ gestation.
PPROMT study designMorris and colleagues present results of their multicenter, international, randomized controlled trial (RCT) of expectant management versus planned delivery in pregnancies complicated by PPROM at 34 0/7 through 36 6/7 weeks’ gestation carried out in 65 centers across 11 countries. A total of 1,839 women not requiring urgent delivery were randomly assigned to either immediate delivery (n = 924) or expectant management (n = 915).
No difference was noted in the primary outcome of neonatal sepsis between the immediate birth (n = 23 [2%]) and expectant management groups (n = 29 [3%]; relative risk [RR], 0.8; 95% confidence interval [CI], 0.5–1.3). This also was true in the subgroup of women who were colonized with group B streptococcus (RR, 0.9; 95% CI, 0.2–4.5).
There also was no difference in the secondary outcome measure, a composite metric including sepsis, ventilation for 24 or more hours, or death (73 [8%] in the immediate delivery group vs 61 [7%] in the expectant management group; RR, 1.2; 95% CI, 0.9–1.6). However, infants born to women randomly assigned to immediate delivery, versus expectant management, had a significantly higher rate of respiratory distress syndrome (RR, 1.6; 95% CI, 1.1–2.3) and mechanical ventilation (RR, 1.4; 95% CI, 1.0–1.8). In addition, the immediate-delivery infants had a longer median stay in the special care nursery/neonatal intensive care unit (4.0 days, interquartile range [IQR], 0.0–10.0 vs 2.0 days, IQR, 0.0–7.0) and total hospital stay (6.0 days, IQR, 3.0–10.0 vs 4.0 days, IQR, 3.0–8.0). As expected, women in the expectant management group had a significantly longer hospital stay than women in the immediate delivery group, because 75% (688/912) were managed as inpatients. Interestingly, women in the immediate delivery group had a higher cesarean delivery rate than those in the expectant management group (239 [26%] vs 169 [19%], respectively; RR, 1.4; 95% CI, 1.2–1.7), although no explanation was offered.
Strengths and limitationsMajor strengths of this study include the large sample size and superior study design. It is by far the largest RCT to address this question. Because this was a pragmatic RCT, certain practices (such as the choice of latency antibiotic regimen) varied across centers, although randomization would be expected to minimize the effect of such variables on study outcome.
A major limitation is that participant recruitment occurred over a period of more than 10 years, during which time antenatal and neonatal intensive care unit practices likely would have changed.
What this evidence means for practiceFew clinical studies have the potential to significantly change obstetric management. This report by Morris and colleagues is one such study. It was well designed, well executed, and powered to look at the most clinically relevant outcome, namely, neonatal sepsis. While these study results do call into question the current American College of Obstetricians and Gynecologists recommendations to electively deliver patients with PPROM at or after 34 weeks’ gestation, additional discussion is needed at the national level before these recommendations can be changed.
—Denis A. Vaughan, MBBCh, BAO, MRCPI, and Errol R. Norwitz, MD, PhD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Goldenberg RL, Rouse DJ. Prevention of premature birth. N Engl J Med. 1998;339(5):313–320.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins–Obstetrics. ACOG Practice Bulletin No. 160: premature rupture of membranes. Obstet Gynecol. 2016;127(1):192–194.
Preterm premature rupture of membranes (PPROM) refers to rupture of membranes prior to the onset of labor before 37 weeks’ gestation. It accounts for one-third of all preterm births.1 Pregnancy complications associated with PPROM include intrauterine infection (chorioamnionitis), preterm labor, and placental abruption. Should such complications develop, immediate delivery is indicated. When to recommend elective delivery in the absence of complications, however, remains controversial.
The American College of Obstetricians and Gynecologists (ACOG) currently recommends elective delivery at or after 34 weeks’ gestation,2 because the prevailing evidence suggests that the risk of pregnancy-related complications (especially ascending infection) exceeds the risks of iatrogenic prematurity at this gestational age. However, ACOG acknowledges that this recommendation is based on “limited and inconsistent scientific evidence.”2 To address deficiencies in the literature, investigators designed the PPROMT (preterm prelabor rupture of the membranes close to term) trial to study women with ruptured membranes before the onset of labor between 34 and 37 weeks’ gestation.
PPROMT study designMorris and colleagues present results of their multicenter, international, randomized controlled trial (RCT) of expectant management versus planned delivery in pregnancies complicated by PPROM at 34 0/7 through 36 6/7 weeks’ gestation carried out in 65 centers across 11 countries. A total of 1,839 women not requiring urgent delivery were randomly assigned to either immediate delivery (n = 924) or expectant management (n = 915).
No difference was noted in the primary outcome of neonatal sepsis between the immediate birth (n = 23 [2%]) and expectant management groups (n = 29 [3%]; relative risk [RR], 0.8; 95% confidence interval [CI], 0.5–1.3). This also was true in the subgroup of women who were colonized with group B streptococcus (RR, 0.9; 95% CI, 0.2–4.5).
There also was no difference in the secondary outcome measure, a composite metric including sepsis, ventilation for 24 or more hours, or death (73 [8%] in the immediate delivery group vs 61 [7%] in the expectant management group; RR, 1.2; 95% CI, 0.9–1.6). However, infants born to women randomly assigned to immediate delivery, versus expectant management, had a significantly higher rate of respiratory distress syndrome (RR, 1.6; 95% CI, 1.1–2.3) and mechanical ventilation (RR, 1.4; 95% CI, 1.0–1.8). In addition, the immediate-delivery infants had a longer median stay in the special care nursery/neonatal intensive care unit (4.0 days, interquartile range [IQR], 0.0–10.0 vs 2.0 days, IQR, 0.0–7.0) and total hospital stay (6.0 days, IQR, 3.0–10.0 vs 4.0 days, IQR, 3.0–8.0). As expected, women in the expectant management group had a significantly longer hospital stay than women in the immediate delivery group, because 75% (688/912) were managed as inpatients. Interestingly, women in the immediate delivery group had a higher cesarean delivery rate than those in the expectant management group (239 [26%] vs 169 [19%], respectively; RR, 1.4; 95% CI, 1.2–1.7), although no explanation was offered.
Strengths and limitationsMajor strengths of this study include the large sample size and superior study design. It is by far the largest RCT to address this question. Because this was a pragmatic RCT, certain practices (such as the choice of latency antibiotic regimen) varied across centers, although randomization would be expected to minimize the effect of such variables on study outcome.
A major limitation is that participant recruitment occurred over a period of more than 10 years, during which time antenatal and neonatal intensive care unit practices likely would have changed.
What this evidence means for practiceFew clinical studies have the potential to significantly change obstetric management. This report by Morris and colleagues is one such study. It was well designed, well executed, and powered to look at the most clinically relevant outcome, namely, neonatal sepsis. While these study results do call into question the current American College of Obstetricians and Gynecologists recommendations to electively deliver patients with PPROM at or after 34 weeks’ gestation, additional discussion is needed at the national level before these recommendations can be changed.
—Denis A. Vaughan, MBBCh, BAO, MRCPI, and Errol R. Norwitz, MD, PhD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Preterm premature rupture of membranes (PPROM) refers to rupture of membranes prior to the onset of labor before 37 weeks’ gestation. It accounts for one-third of all preterm births.1 Pregnancy complications associated with PPROM include intrauterine infection (chorioamnionitis), preterm labor, and placental abruption. Should such complications develop, immediate delivery is indicated. When to recommend elective delivery in the absence of complications, however, remains controversial.
The American College of Obstetricians and Gynecologists (ACOG) currently recommends elective delivery at or after 34 weeks’ gestation,2 because the prevailing evidence suggests that the risk of pregnancy-related complications (especially ascending infection) exceeds the risks of iatrogenic prematurity at this gestational age. However, ACOG acknowledges that this recommendation is based on “limited and inconsistent scientific evidence.”2 To address deficiencies in the literature, investigators designed the PPROMT (preterm prelabor rupture of the membranes close to term) trial to study women with ruptured membranes before the onset of labor between 34 and 37 weeks’ gestation.
PPROMT study designMorris and colleagues present results of their multicenter, international, randomized controlled trial (RCT) of expectant management versus planned delivery in pregnancies complicated by PPROM at 34 0/7 through 36 6/7 weeks’ gestation carried out in 65 centers across 11 countries. A total of 1,839 women not requiring urgent delivery were randomly assigned to either immediate delivery (n = 924) or expectant management (n = 915).
No difference was noted in the primary outcome of neonatal sepsis between the immediate birth (n = 23 [2%]) and expectant management groups (n = 29 [3%]; relative risk [RR], 0.8; 95% confidence interval [CI], 0.5–1.3). This also was true in the subgroup of women who were colonized with group B streptococcus (RR, 0.9; 95% CI, 0.2–4.5).
There also was no difference in the secondary outcome measure, a composite metric including sepsis, ventilation for 24 or more hours, or death (73 [8%] in the immediate delivery group vs 61 [7%] in the expectant management group; RR, 1.2; 95% CI, 0.9–1.6). However, infants born to women randomly assigned to immediate delivery, versus expectant management, had a significantly higher rate of respiratory distress syndrome (RR, 1.6; 95% CI, 1.1–2.3) and mechanical ventilation (RR, 1.4; 95% CI, 1.0–1.8). In addition, the immediate-delivery infants had a longer median stay in the special care nursery/neonatal intensive care unit (4.0 days, interquartile range [IQR], 0.0–10.0 vs 2.0 days, IQR, 0.0–7.0) and total hospital stay (6.0 days, IQR, 3.0–10.0 vs 4.0 days, IQR, 3.0–8.0). As expected, women in the expectant management group had a significantly longer hospital stay than women in the immediate delivery group, because 75% (688/912) were managed as inpatients. Interestingly, women in the immediate delivery group had a higher cesarean delivery rate than those in the expectant management group (239 [26%] vs 169 [19%], respectively; RR, 1.4; 95% CI, 1.2–1.7), although no explanation was offered.
Strengths and limitationsMajor strengths of this study include the large sample size and superior study design. It is by far the largest RCT to address this question. Because this was a pragmatic RCT, certain practices (such as the choice of latency antibiotic regimen) varied across centers, although randomization would be expected to minimize the effect of such variables on study outcome.
A major limitation is that participant recruitment occurred over a period of more than 10 years, during which time antenatal and neonatal intensive care unit practices likely would have changed.
What this evidence means for practiceFew clinical studies have the potential to significantly change obstetric management. This report by Morris and colleagues is one such study. It was well designed, well executed, and powered to look at the most clinically relevant outcome, namely, neonatal sepsis. While these study results do call into question the current American College of Obstetricians and Gynecologists recommendations to electively deliver patients with PPROM at or after 34 weeks’ gestation, additional discussion is needed at the national level before these recommendations can be changed.
—Denis A. Vaughan, MBBCh, BAO, MRCPI, and Errol R. Norwitz, MD, PhD
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
- Goldenberg RL, Rouse DJ. Prevention of premature birth. N Engl J Med. 1998;339(5):313–320.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins–Obstetrics. ACOG Practice Bulletin No. 160: premature rupture of membranes. Obstet Gynecol. 2016;127(1):192–194.
- Goldenberg RL, Rouse DJ. Prevention of premature birth. N Engl J Med. 1998;339(5):313–320.
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins–Obstetrics. ACOG Practice Bulletin No. 160: premature rupture of membranes. Obstet Gynecol. 2016;127(1):192–194.
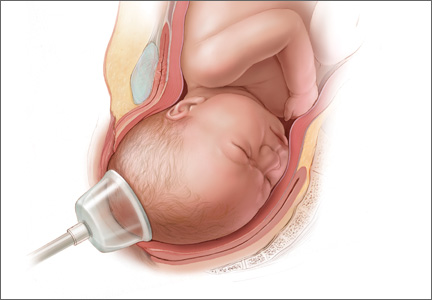
Does episiotomy at vacuum delivery increase maternal morbidity?
Episiotomy refers to an incision into the perineal body made during the second stage of labor to expedite delivery. It comes in 2 main flavors (midline and mediolateral), and neither one is particularly palatable. Routine use of episiotomy is strongly discouraged, for several reasons:
- There is little evidence of benefit
- It is associated with an increased risk of short- and long-term complications to both the mother and neonate, including postpartum hemorrhage, severe perineal injury, and pelvic floor dysfunction.1,2
Whether to perform an episiotomy at the time of operative vaginal delivery (forceps or vacuum), however, remains controversial.
Sagi-Dain and Sagi performed a meta- analysis of the existing literature in an effort to answer a single clinically relevant question: Should an episiotomy be performed at the time of vacuum delivery?
Details of the study
The primary endpoint was obstetric anal sphincter injuries (OASIS), which are more commonly referred to in the United States as severe perineal injury (3rd- and 4th-degree perineal laceration). Secondary endpoints were, among others, neonatal outcomes (including Apgar scores, neonatal trauma, shoulder dystocia, neonatal resuscitation, and admission to the neonatal intensive care unit) and maternal complications (including postpartum hemorrhage, perineal infection, urinary retention, urinary/fecal incontinence, prolonged hospital stay, and analgesia use).
Of 812 original research reports initially identified that examined the effect of episiotomy at vacuum delivery on any measure of maternal or neonatal outcome, 15 articles encompassing 350,764 deliveries were included in the final analysis. Of these, 14 were observational cohort studies (13 retrospective and 1 prospective) plus 1 case-control analysis; no randomized trials were identified.
Overall, episiotomy was performed in 64.3% (SD, 18.8%; range, 28.7%-86.0%) of vacuum deliveries and was more common in nulliparous (58.7%; SD, 17.8%) than in multiparous women (34.2%; SD, 14.6%; P = .035). The investigators found that US and Canadian studies reported using mainly median episiotomy, whereas European, Scandinavian, and Australian studies used mainly mediolateral episiotomy.
Overall, OASIS occurred in 8.5% (SD, 10.6%; range 1.0%-23.6%) of vacuum deliveries, with a higher rate occurring in nulliparous compared with multiparous women (9.6%; [SD, 6.2%] vs 1.7% [SD, 1.3%], respectively; P = .031).
Median (midline) episiotomy at the time of vacuum delivery was associated with a significant increase in OASIS in both nulliparous (odds ratio [OR], 5.11; 95% confidence interval [CI], 3.23-8.08) and multip- arous women (OR, 89.4; 95% CI, 11.8-677.1). A similar increase in OASIS was seen when a mediolateral episiotomy was performed at vacuum delivery in multiparous women (OR, 1.27; 95% CI, 1.05-1.53), although no statistically significant relationship was evident between mediolateral episiotomy at vacuum delivery and OASIS in nulliparous women (OR, 0.68; 95% CI, 0.43-1.07). Mediolateral episiotomy also was linked to increased rates of postpartum hemorrhage (OR, 1.82; 95% CI, 1.16-2.86) and analgesia use (OR, 2.10; 95% CI, 1.39-3.17).
Strengths and limitations
Meta-analysis (systematic review) is not synonymous with a review of the literature. It has a very specific methodology and should be treated as original research, albeit in silico. Meta-analyses use precise statistical methods to combine and contrast results from a number of independent original research reports. The current study is an exemplary illustration of just how such an analysis should be conducted. As prescribed by the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines,3 it included all study designs, both published and unpublished data, and was not limited to English language reports.
In addition, if results were unclear or data were missing, the investigators contacted the authors directly to verify the information. Prior published statistical analyses were disregarded, and the investigators conducted an independent evaluation of the pooled data using each patient as a separate data point. Data classification and coding were clearly described; the analysis was performed independently by 2 separate investigators; and a detailed assessment of data quality, heterogeneity, and sensitivity testing was included.
What this evidence means for practice
Episiotomy at the time of vacuum delivery does not appear to be of benefit, and it more likely than not increases maternal morbidity. This is especially true of median episiotomy (the type used most commonly in the United States), which increases the risk of OASIS at the time of vacuum delivery 5-fold in nulliparous and 89-fold in multiparous women.
Confidence in these conclusions is guarded. Based on the small number of reports, the lack of randomized trials, and the significant heterogeneity between the studies, the authors rated the overall quality of evidence as “low” to “very low” using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group criteria. Additional large prospective clinical trials are needed to definitively answer the question of whether episiotomy at vacuum delivery increases maternal morbidity.
Until such studies are available, however, it would be best if obstetric care providers avoid episiotomy at the time of vacuum delivery. On a personal note, I look forward to the day when a medical student turns to an attending and asks: “What is an episiotomy?” And the attending responds: “I don’t know. I’ve never seen one.” Only then will I be ready to retire.
>> Errol R. Norwitz, MD, PhD
1. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
2. Ali U, Norwitz ER. Vacuum-assisted vaginal delivery. Rev Obstet Gynecol. 2009;2(1):5-17.
3. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012.
Episiotomy refers to an incision into the perineal body made during the second stage of labor to expedite delivery. It comes in 2 main flavors (midline and mediolateral), and neither one is particularly palatable. Routine use of episiotomy is strongly discouraged, for several reasons:
- There is little evidence of benefit
- It is associated with an increased risk of short- and long-term complications to both the mother and neonate, including postpartum hemorrhage, severe perineal injury, and pelvic floor dysfunction.1,2
Whether to perform an episiotomy at the time of operative vaginal delivery (forceps or vacuum), however, remains controversial.
Sagi-Dain and Sagi performed a meta- analysis of the existing literature in an effort to answer a single clinically relevant question: Should an episiotomy be performed at the time of vacuum delivery?
Details of the study
The primary endpoint was obstetric anal sphincter injuries (OASIS), which are more commonly referred to in the United States as severe perineal injury (3rd- and 4th-degree perineal laceration). Secondary endpoints were, among others, neonatal outcomes (including Apgar scores, neonatal trauma, shoulder dystocia, neonatal resuscitation, and admission to the neonatal intensive care unit) and maternal complications (including postpartum hemorrhage, perineal infection, urinary retention, urinary/fecal incontinence, prolonged hospital stay, and analgesia use).
Of 812 original research reports initially identified that examined the effect of episiotomy at vacuum delivery on any measure of maternal or neonatal outcome, 15 articles encompassing 350,764 deliveries were included in the final analysis. Of these, 14 were observational cohort studies (13 retrospective and 1 prospective) plus 1 case-control analysis; no randomized trials were identified.
Overall, episiotomy was performed in 64.3% (SD, 18.8%; range, 28.7%-86.0%) of vacuum deliveries and was more common in nulliparous (58.7%; SD, 17.8%) than in multiparous women (34.2%; SD, 14.6%; P = .035). The investigators found that US and Canadian studies reported using mainly median episiotomy, whereas European, Scandinavian, and Australian studies used mainly mediolateral episiotomy.
Overall, OASIS occurred in 8.5% (SD, 10.6%; range 1.0%-23.6%) of vacuum deliveries, with a higher rate occurring in nulliparous compared with multiparous women (9.6%; [SD, 6.2%] vs 1.7% [SD, 1.3%], respectively; P = .031).
Median (midline) episiotomy at the time of vacuum delivery was associated with a significant increase in OASIS in both nulliparous (odds ratio [OR], 5.11; 95% confidence interval [CI], 3.23-8.08) and multip- arous women (OR, 89.4; 95% CI, 11.8-677.1). A similar increase in OASIS was seen when a mediolateral episiotomy was performed at vacuum delivery in multiparous women (OR, 1.27; 95% CI, 1.05-1.53), although no statistically significant relationship was evident between mediolateral episiotomy at vacuum delivery and OASIS in nulliparous women (OR, 0.68; 95% CI, 0.43-1.07). Mediolateral episiotomy also was linked to increased rates of postpartum hemorrhage (OR, 1.82; 95% CI, 1.16-2.86) and analgesia use (OR, 2.10; 95% CI, 1.39-3.17).
Strengths and limitations
Meta-analysis (systematic review) is not synonymous with a review of the literature. It has a very specific methodology and should be treated as original research, albeit in silico. Meta-analyses use precise statistical methods to combine and contrast results from a number of independent original research reports. The current study is an exemplary illustration of just how such an analysis should be conducted. As prescribed by the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines,3 it included all study designs, both published and unpublished data, and was not limited to English language reports.
In addition, if results were unclear or data were missing, the investigators contacted the authors directly to verify the information. Prior published statistical analyses were disregarded, and the investigators conducted an independent evaluation of the pooled data using each patient as a separate data point. Data classification and coding were clearly described; the analysis was performed independently by 2 separate investigators; and a detailed assessment of data quality, heterogeneity, and sensitivity testing was included.
What this evidence means for practice
Episiotomy at the time of vacuum delivery does not appear to be of benefit, and it more likely than not increases maternal morbidity. This is especially true of median episiotomy (the type used most commonly in the United States), which increases the risk of OASIS at the time of vacuum delivery 5-fold in nulliparous and 89-fold in multiparous women.
Confidence in these conclusions is guarded. Based on the small number of reports, the lack of randomized trials, and the significant heterogeneity between the studies, the authors rated the overall quality of evidence as “low” to “very low” using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group criteria. Additional large prospective clinical trials are needed to definitively answer the question of whether episiotomy at vacuum delivery increases maternal morbidity.
Until such studies are available, however, it would be best if obstetric care providers avoid episiotomy at the time of vacuum delivery. On a personal note, I look forward to the day when a medical student turns to an attending and asks: “What is an episiotomy?” And the attending responds: “I don’t know. I’ve never seen one.” Only then will I be ready to retire.
>> Errol R. Norwitz, MD, PhD
Episiotomy refers to an incision into the perineal body made during the second stage of labor to expedite delivery. It comes in 2 main flavors (midline and mediolateral), and neither one is particularly palatable. Routine use of episiotomy is strongly discouraged, for several reasons:
- There is little evidence of benefit
- It is associated with an increased risk of short- and long-term complications to both the mother and neonate, including postpartum hemorrhage, severe perineal injury, and pelvic floor dysfunction.1,2
Whether to perform an episiotomy at the time of operative vaginal delivery (forceps or vacuum), however, remains controversial.
Sagi-Dain and Sagi performed a meta- analysis of the existing literature in an effort to answer a single clinically relevant question: Should an episiotomy be performed at the time of vacuum delivery?
Details of the study
The primary endpoint was obstetric anal sphincter injuries (OASIS), which are more commonly referred to in the United States as severe perineal injury (3rd- and 4th-degree perineal laceration). Secondary endpoints were, among others, neonatal outcomes (including Apgar scores, neonatal trauma, shoulder dystocia, neonatal resuscitation, and admission to the neonatal intensive care unit) and maternal complications (including postpartum hemorrhage, perineal infection, urinary retention, urinary/fecal incontinence, prolonged hospital stay, and analgesia use).
Of 812 original research reports initially identified that examined the effect of episiotomy at vacuum delivery on any measure of maternal or neonatal outcome, 15 articles encompassing 350,764 deliveries were included in the final analysis. Of these, 14 were observational cohort studies (13 retrospective and 1 prospective) plus 1 case-control analysis; no randomized trials were identified.
Overall, episiotomy was performed in 64.3% (SD, 18.8%; range, 28.7%-86.0%) of vacuum deliveries and was more common in nulliparous (58.7%; SD, 17.8%) than in multiparous women (34.2%; SD, 14.6%; P = .035). The investigators found that US and Canadian studies reported using mainly median episiotomy, whereas European, Scandinavian, and Australian studies used mainly mediolateral episiotomy.
Overall, OASIS occurred in 8.5% (SD, 10.6%; range 1.0%-23.6%) of vacuum deliveries, with a higher rate occurring in nulliparous compared with multiparous women (9.6%; [SD, 6.2%] vs 1.7% [SD, 1.3%], respectively; P = .031).
Median (midline) episiotomy at the time of vacuum delivery was associated with a significant increase in OASIS in both nulliparous (odds ratio [OR], 5.11; 95% confidence interval [CI], 3.23-8.08) and multip- arous women (OR, 89.4; 95% CI, 11.8-677.1). A similar increase in OASIS was seen when a mediolateral episiotomy was performed at vacuum delivery in multiparous women (OR, 1.27; 95% CI, 1.05-1.53), although no statistically significant relationship was evident between mediolateral episiotomy at vacuum delivery and OASIS in nulliparous women (OR, 0.68; 95% CI, 0.43-1.07). Mediolateral episiotomy also was linked to increased rates of postpartum hemorrhage (OR, 1.82; 95% CI, 1.16-2.86) and analgesia use (OR, 2.10; 95% CI, 1.39-3.17).
Strengths and limitations
Meta-analysis (systematic review) is not synonymous with a review of the literature. It has a very specific methodology and should be treated as original research, albeit in silico. Meta-analyses use precise statistical methods to combine and contrast results from a number of independent original research reports. The current study is an exemplary illustration of just how such an analysis should be conducted. As prescribed by the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines,3 it included all study designs, both published and unpublished data, and was not limited to English language reports.
In addition, if results were unclear or data were missing, the investigators contacted the authors directly to verify the information. Prior published statistical analyses were disregarded, and the investigators conducted an independent evaluation of the pooled data using each patient as a separate data point. Data classification and coding were clearly described; the analysis was performed independently by 2 separate investigators; and a detailed assessment of data quality, heterogeneity, and sensitivity testing was included.
What this evidence means for practice
Episiotomy at the time of vacuum delivery does not appear to be of benefit, and it more likely than not increases maternal morbidity. This is especially true of median episiotomy (the type used most commonly in the United States), which increases the risk of OASIS at the time of vacuum delivery 5-fold in nulliparous and 89-fold in multiparous women.
Confidence in these conclusions is guarded. Based on the small number of reports, the lack of randomized trials, and the significant heterogeneity between the studies, the authors rated the overall quality of evidence as “low” to “very low” using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) working group criteria. Additional large prospective clinical trials are needed to definitively answer the question of whether episiotomy at vacuum delivery increases maternal morbidity.
Until such studies are available, however, it would be best if obstetric care providers avoid episiotomy at the time of vacuum delivery. On a personal note, I look forward to the day when a medical student turns to an attending and asks: “What is an episiotomy?” And the attending responds: “I don’t know. I’ve never seen one.” Only then will I be ready to retire.
>> Errol R. Norwitz, MD, PhD
1. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
2. Ali U, Norwitz ER. Vacuum-assisted vaginal delivery. Rev Obstet Gynecol. 2009;2(1):5-17.
3. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012.
1. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.
2. Ali U, Norwitz ER. Vacuum-assisted vaginal delivery. Rev Obstet Gynecol. 2009;2(1):5-17.
3. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008-2012.
10 evidence-based recommendations to prevent surgical site infection after cesarean delivery
Infection is the second leading cause of pregnancy-related mortality in the United States, responsible for 13.6% of all maternal deaths.1 Cesarean delivery is the single most important risk factor for puerperal infection, increasing its incidence approximately 5- to 20-fold.2
Given that cesarean deliveries represent 32.7% of all births in the United States,3 the overall health and socioeconomic burden of these infections is substantial. In addition, more than half of all pregnancies are complicated by maternal obesity, which is associated with an increased risk of cesarean delivery as well as subsequent wound complications.4
In this review, we offer 10 evidence-based strategies to prevent surgical site infection (SSI) after cesarean delivery.
1 Maintain strict glycemic control in women with diabetes
Perioperative hyperglycemia is associated with an increased risk of postoperative infection in patients with diabetes
Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591.
Hanazaki K, Maeda H, Okabayashi T. Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol. 2009;15(33):4122–4125.
Although data are limited on the impact of perioperative glycemic control on postcesarean infection rates, the association has been well documented in the general surgery literature. Results of a retrospective cohort study of 995 patients undergoing general or vascular surgery demonstrated that postoperative hyperglycemia increased the risk of infection by 30% for every 40-point increase in serum glucose levels from normoglycemia (defined as <110 mg/dL) (odds ratio, 1.3; 95% confidence interval [CI], 1.03–1.64).5 Hyperglycemia causes abnormalities of leukocyte function, including impaired granulocyte adherence, impaired phagocytosis, delayed chemotaxis, and depressed bactericidal capacity. And all of these abnormalities in leukocyte function appear to improve with strict glycemic control, although the target range for blood glucose remains uncertain.6
2 Recommend preoperative antiseptic showering
Ask patients to shower with 4% chlorhexidine gluconate the night before surgery to reduce the presence of bacterial skin flora
Mangram AJ, Horan TC, Pearson ML, et al; Hospital Infection Control Practices Advisory Committee. Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):247–278.
Chlebicki MP, Safdar N, O’Horo JC, Maki DG. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–173.
According to the Centers for Disease Control and Prevention, preoperative showering with chlorhexidine reduces the presence of bacterial skin flora. A study of more than 700 patients showed that preoperative showers with chlorhexidine reduced bacterial colony counts 9-fold, compared with only 1.3-fold for povidone-iodine.7 Whether this translates into a reduction in SSI remains controversial, in large part because of poor quality of the existing prospective trials, which used different agents, concentrations, and methods of skin preparation.8
Small clinical trials have found a benefit to chlorhexidine treatment the day before surgery.9,10 However, a recent meta-analysis of 16 randomized trials failed to show a significant reduction in the rate of SSI with chlorhexidine compared with soap, placebo, or no washing (relative risk [RR], 0.90; 95% CI, 0.77–1.05).11
3 Administer intravenous antibiotic prophylaxis
All patients who undergo cesarean delivery should be given appropriate antibiotic prophylaxis within 60 minutes before the skin incision
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472–1483.
Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a meta-analysis. Am J Obstet Gynecol. 2008;199(3):301.e1–e6.
The American College of Obstetricians and Gynecologists (ACOG) recommends the use of a single dose of a narrow-spectrum, first-generation cephalosporin (or a single dose of clindamycin with an aminoglycoside for those with a significant penicillin allergy) as SSI chemoprophylaxis for cesarean delivery.12 Due to concerns about fetal antibiotic exposure, such prophylaxis traditionally has been given after clamping of the umbilical cord. However, results of a recent meta-analysis of 5 randomized controlled trials demonstrated that antibiotic prophylaxis significantly reduced infectious morbidity (RR, 0.50; 95% CI, 0.33–0.78) when it was given 60 minutes before the skin incision, with no significant effect on neonatal outcome.13
4 Give a higher dose of preoperative antibiotics in obese women
Given the increased volume of distribution and the increased risk of postcesarean infection in the obese population, a higher dose of preoperative antibiotic prophylaxis is recommended
Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106(6):1357–1364.
Pevzner L, Swank M, Krepel C, et al. Effects of maternal obesity on tissue concentrations of prophylactic cefazolin during cesarean delivery. Obstet Gynecol. 2011;117(4):877–882.
The impact of maternal obesity on the risk of SSI after cesarean delivery was illustrated in a 2005 retrospective cohort study of 10,134 obese women. Moderately obese women with a prepregnancy weight of 90 to 100 kg were 1.6 times (95% CI, 1.31–1.95) more likely to have a wound infection, and severely obese women (>120 kg) were 4.45 times (95% CI, 3.00–6.61) more likely to have a wound infection after cesarean delivery, compared with women of normal weight.14
Moreover, a study of tissue concentrations of prophylactic cefazolin in obese women demonstrated that concentrations within adipose tissue at the site of the skin incision were inversely proportional to maternal body mass index (BMI).15 Given these findings, consideration should be given to using a higher dose of preoperative antibiotic prophylaxis in obese women, specifically 3 g of intravenous (IV) cefazolin for women with a BMI greater than 30 kg/m2 or an absolute weight of more than 100 kg.12
5 Use clippers for preoperative hair removal
If hair removal is necessary to perform the skin incision for cesarean delivery, the use of clippers is preferred
Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
In a Cochrane review of 3 randomized clinical trials comparing preoperative hair-removal techniques, shaving was associated with an increased risk of SSI, compared with clipping (RR, 2.09; 95% CI, 1.15–3.80).15 Shaving is thought to result in microscopic skin abrasions that can serve as foci for bacterial growth.
Interestingly, in this same Cochrane review, a separate analysis of 6 studies failed to show a benefit of preoperative hair removal by any means, compared with no hair removal,15 suggesting that routine hair removal may not be indicated for all patients.
6 Use chlorhexidine-alcohol for skin prep
Prepare the skin with chlorhexidine-alcohol immediately before surgery
Darouiche RO, Wall MJ Jr, Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2014;18:1–5.
Data from a randomized multicenter trial of 849 patients showed that the use of a chlorhexidine-alcohol skin preparation immediately before surgery lowered the rate of SSI after clean-contaminated surgery, compared with povidone-iodine (RR, 0.59; 95% CI, 0.41–0.85).16 Studies focusing on cesarean delivery alone are limited, although 1 small randomized trial found that chlorhexidine treatment significantly reduced bacterial growth at 18 hours after cesarean, compared with povidone-iodine (RR, 0.23; 95% CI, 0.07–0.70).17
7 Consider an alcohol-based hand rub for preoperative antisepsis
Alcohol-based hand rubs may be more effective than conventional surgical scrub
Shen NJ, Pan SC, Sheng WH, et al. Comparative antimicrobial efficacy of alcohol-based hand rub and conventional surgical scrub in a medical center [published online ahead of print September 21, 2013]. J Microbiol Immunol Infect. pii:S1684–1182(13)00150–3.
Tanner J, Swarbrook S, Stuart J. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev. 2008;1:CD004288.
Several agents are available for preoperative surgical hand antisepsis, including newer alcohol-based rubs and conventional aqueous scrubs that contain either chlorhexidine gluconate or povidone-iodine. In a prospective cohort study of 128 health care providers, use of an alcohol-based rub for surgical hand antisepsis was associated with a lower rate of positive bacterial culture (6.2%), compared with a chlorhexidine-based conventional scrub (47.6%; P<.001).18 However, if an aqueous-based scrub is the only option available for surgical hand antisepsis, a Cochrane review found that chlorhexidine gluconate scrubs were more effective than povidone-iodine scrubs in 3 trials, resulting in fewer colony-forming units of bacteria on the hands of the surgical team.19
8 Close the skin with subcuticular sutures
Use of subcuticular sutures for skin closure is associated with a lower risk of wound complications, compared with staples
Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a meta-analysis [published online ahead of print December 19, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.12.020.
A meta-analysis of 12 randomized controlled trials including 3,112 women demonstrated that subcuticular closure is associated with a decreased risk of wound complications, compared with staple closure (RR, 0.49; 95% CI, 0.28–0.87). The reduced risk remained significant even when stratified by obesity. Both closure techniques were shown to be equivalent with regard to postoperative pain, cosmetic outcome, and patient satisfaction.20
9 Close the subcutaneous tissue
Closure of the subcutaneous fat is associated with a decreased risk of wound disruption for women with a tissue thickness of more than 2 cm
Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103(5 pt 1):974–980.
Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
A meta-analysis of 5 randomized controlled trials demonstrated that suture closure of subcutaneous fat is associated with a 34% decrease in the risk of wound disruption in women with fat thickness greater than 2 cm (RR, 0.66; 95% CI, 0.48–0.91).21
A recent systematic review of evidence-based guidelines for surgical decisions during cesarean delivery also recommended this practice based on results of 9 published studies.22 In this review, however, subcutaneous drain placement did not offer any additional benefit, regardless of tissue thickness.22
10 Avoid unproven techniques
Several commonly performed techniques have not been associated with a decreased risk of SSI after cesarean delivery
Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
CORONIS Trial Collaborative Group. The CORONIS Trial. International study of caesarean section surgical techniques: a randomised fractional, factorial trial. BMC Pregnancy Childbirth. 2007;7:24. doi:10.1186/1471-2393-7-24.
Familiarity with the obstetric literature will help providers determine which interventions prevent SSI and which do not. Well-designed clinical studies have demonstrated no significant difference in the rate of postcesarean infectious morbidity with the administration of high concentrations of perioperative oxygen,22 saline wound irrigation,22 placement of subcutaneous drains,22 blunt versus sharp abdominal entry,23 and exteriorization of the uterus for repair.23
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125(1):5–12.
2. Leth RA, Moller JK, Thomsen RW, Uldbjerg N, Norgaard M. Risk of selected postpartum infections after cesarean section compared with vaginal birth: a five-year cohort study of 32,468 women. Acta Obstet Gynecol Scand. 2009;88(9):976–983.
3. Martin JA, Hamilton BE, Osterman JK, et al. Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–65.
4. American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 549: Obesity in pregnancy. Obstet Gynecol. 2013;121(1):213–217.
5. Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
6. Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591.
7. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Hospital Infection Control Practices Advisory Committee: Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):250–278.
8. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9:CD004985.
9. Hayek LJ, Emerson JM, Gardner AM. A placebo-controlled trial of the effect of two preoperative baths or showers with chlorhexidine detergent on post-operative wound infection rates. J Hosp Infect. 1987;10(2):165–172.
10. Wihlborg O. The effect of washing with chlorhexidine soap on wound infection rate in general surgery: a controlled clinical study. Ann Chir Gynaecol. 1987;76(5):263–265.
11. Chlebicki MP, Safdar N, O’Horo JC, Maki DG. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–173.
12. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472–1483.
13. Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a meta-analysis. Am J Obstet Gynecol. 2008;199(3):301.e1–e6.
14. Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106(6):1357–1364.
15. Pevzner L, Swank M, Krepel C, et al. Effects of maternal obesity on tissue concentrations of prophylactic cefazolin during cesarean delivery. Obstet Gynecol. 2011;117(4):877–882.
16. Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
17. Darouiche RO, Wall MJ Jr, Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
18. Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2014;18:1–5.
19. Shen NJ, Pan SC, Sheng WH, et al. Comparative antimicrobial efficacy of alcohol-based hand rub and conventional surgical scrub in a medical center [published online ahead of print September 21, 2013]. J Microbiol Immunol Infect. pii:S1684–1182(13)00150–3.
20. Tanner J, Swarbrook S, Stuart J. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev. 2008;1:CD004288.
21. Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a meta-analysis [published online ahead of print December 19, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.12.020.
22. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103(5 Pt 1):974–980.
23. Hanazaki K, Maeda H, Okabayashi T. Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol. 2009;15(33):4122–4125.
Infection is the second leading cause of pregnancy-related mortality in the United States, responsible for 13.6% of all maternal deaths.1 Cesarean delivery is the single most important risk factor for puerperal infection, increasing its incidence approximately 5- to 20-fold.2
Given that cesarean deliveries represent 32.7% of all births in the United States,3 the overall health and socioeconomic burden of these infections is substantial. In addition, more than half of all pregnancies are complicated by maternal obesity, which is associated with an increased risk of cesarean delivery as well as subsequent wound complications.4
In this review, we offer 10 evidence-based strategies to prevent surgical site infection (SSI) after cesarean delivery.
1 Maintain strict glycemic control in women with diabetes
Perioperative hyperglycemia is associated with an increased risk of postoperative infection in patients with diabetes
Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591.
Hanazaki K, Maeda H, Okabayashi T. Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol. 2009;15(33):4122–4125.
Although data are limited on the impact of perioperative glycemic control on postcesarean infection rates, the association has been well documented in the general surgery literature. Results of a retrospective cohort study of 995 patients undergoing general or vascular surgery demonstrated that postoperative hyperglycemia increased the risk of infection by 30% for every 40-point increase in serum glucose levels from normoglycemia (defined as <110 mg/dL) (odds ratio, 1.3; 95% confidence interval [CI], 1.03–1.64).5 Hyperglycemia causes abnormalities of leukocyte function, including impaired granulocyte adherence, impaired phagocytosis, delayed chemotaxis, and depressed bactericidal capacity. And all of these abnormalities in leukocyte function appear to improve with strict glycemic control, although the target range for blood glucose remains uncertain.6
2 Recommend preoperative antiseptic showering
Ask patients to shower with 4% chlorhexidine gluconate the night before surgery to reduce the presence of bacterial skin flora
Mangram AJ, Horan TC, Pearson ML, et al; Hospital Infection Control Practices Advisory Committee. Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):247–278.
Chlebicki MP, Safdar N, O’Horo JC, Maki DG. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–173.
According to the Centers for Disease Control and Prevention, preoperative showering with chlorhexidine reduces the presence of bacterial skin flora. A study of more than 700 patients showed that preoperative showers with chlorhexidine reduced bacterial colony counts 9-fold, compared with only 1.3-fold for povidone-iodine.7 Whether this translates into a reduction in SSI remains controversial, in large part because of poor quality of the existing prospective trials, which used different agents, concentrations, and methods of skin preparation.8
Small clinical trials have found a benefit to chlorhexidine treatment the day before surgery.9,10 However, a recent meta-analysis of 16 randomized trials failed to show a significant reduction in the rate of SSI with chlorhexidine compared with soap, placebo, or no washing (relative risk [RR], 0.90; 95% CI, 0.77–1.05).11
3 Administer intravenous antibiotic prophylaxis
All patients who undergo cesarean delivery should be given appropriate antibiotic prophylaxis within 60 minutes before the skin incision
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472–1483.
Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a meta-analysis. Am J Obstet Gynecol. 2008;199(3):301.e1–e6.
The American College of Obstetricians and Gynecologists (ACOG) recommends the use of a single dose of a narrow-spectrum, first-generation cephalosporin (or a single dose of clindamycin with an aminoglycoside for those with a significant penicillin allergy) as SSI chemoprophylaxis for cesarean delivery.12 Due to concerns about fetal antibiotic exposure, such prophylaxis traditionally has been given after clamping of the umbilical cord. However, results of a recent meta-analysis of 5 randomized controlled trials demonstrated that antibiotic prophylaxis significantly reduced infectious morbidity (RR, 0.50; 95% CI, 0.33–0.78) when it was given 60 minutes before the skin incision, with no significant effect on neonatal outcome.13
4 Give a higher dose of preoperative antibiotics in obese women
Given the increased volume of distribution and the increased risk of postcesarean infection in the obese population, a higher dose of preoperative antibiotic prophylaxis is recommended
Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106(6):1357–1364.
Pevzner L, Swank M, Krepel C, et al. Effects of maternal obesity on tissue concentrations of prophylactic cefazolin during cesarean delivery. Obstet Gynecol. 2011;117(4):877–882.
The impact of maternal obesity on the risk of SSI after cesarean delivery was illustrated in a 2005 retrospective cohort study of 10,134 obese women. Moderately obese women with a prepregnancy weight of 90 to 100 kg were 1.6 times (95% CI, 1.31–1.95) more likely to have a wound infection, and severely obese women (>120 kg) were 4.45 times (95% CI, 3.00–6.61) more likely to have a wound infection after cesarean delivery, compared with women of normal weight.14
Moreover, a study of tissue concentrations of prophylactic cefazolin in obese women demonstrated that concentrations within adipose tissue at the site of the skin incision were inversely proportional to maternal body mass index (BMI).15 Given these findings, consideration should be given to using a higher dose of preoperative antibiotic prophylaxis in obese women, specifically 3 g of intravenous (IV) cefazolin for women with a BMI greater than 30 kg/m2 or an absolute weight of more than 100 kg.12
5 Use clippers for preoperative hair removal
If hair removal is necessary to perform the skin incision for cesarean delivery, the use of clippers is preferred
Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
In a Cochrane review of 3 randomized clinical trials comparing preoperative hair-removal techniques, shaving was associated with an increased risk of SSI, compared with clipping (RR, 2.09; 95% CI, 1.15–3.80).15 Shaving is thought to result in microscopic skin abrasions that can serve as foci for bacterial growth.
Interestingly, in this same Cochrane review, a separate analysis of 6 studies failed to show a benefit of preoperative hair removal by any means, compared with no hair removal,15 suggesting that routine hair removal may not be indicated for all patients.
6 Use chlorhexidine-alcohol for skin prep
Prepare the skin with chlorhexidine-alcohol immediately before surgery
Darouiche RO, Wall MJ Jr, Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2014;18:1–5.
Data from a randomized multicenter trial of 849 patients showed that the use of a chlorhexidine-alcohol skin preparation immediately before surgery lowered the rate of SSI after clean-contaminated surgery, compared with povidone-iodine (RR, 0.59; 95% CI, 0.41–0.85).16 Studies focusing on cesarean delivery alone are limited, although 1 small randomized trial found that chlorhexidine treatment significantly reduced bacterial growth at 18 hours after cesarean, compared with povidone-iodine (RR, 0.23; 95% CI, 0.07–0.70).17
7 Consider an alcohol-based hand rub for preoperative antisepsis
Alcohol-based hand rubs may be more effective than conventional surgical scrub
Shen NJ, Pan SC, Sheng WH, et al. Comparative antimicrobial efficacy of alcohol-based hand rub and conventional surgical scrub in a medical center [published online ahead of print September 21, 2013]. J Microbiol Immunol Infect. pii:S1684–1182(13)00150–3.
Tanner J, Swarbrook S, Stuart J. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev. 2008;1:CD004288.
Several agents are available for preoperative surgical hand antisepsis, including newer alcohol-based rubs and conventional aqueous scrubs that contain either chlorhexidine gluconate or povidone-iodine. In a prospective cohort study of 128 health care providers, use of an alcohol-based rub for surgical hand antisepsis was associated with a lower rate of positive bacterial culture (6.2%), compared with a chlorhexidine-based conventional scrub (47.6%; P<.001).18 However, if an aqueous-based scrub is the only option available for surgical hand antisepsis, a Cochrane review found that chlorhexidine gluconate scrubs were more effective than povidone-iodine scrubs in 3 trials, resulting in fewer colony-forming units of bacteria on the hands of the surgical team.19
8 Close the skin with subcuticular sutures
Use of subcuticular sutures for skin closure is associated with a lower risk of wound complications, compared with staples
Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a meta-analysis [published online ahead of print December 19, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.12.020.
A meta-analysis of 12 randomized controlled trials including 3,112 women demonstrated that subcuticular closure is associated with a decreased risk of wound complications, compared with staple closure (RR, 0.49; 95% CI, 0.28–0.87). The reduced risk remained significant even when stratified by obesity. Both closure techniques were shown to be equivalent with regard to postoperative pain, cosmetic outcome, and patient satisfaction.20
9 Close the subcutaneous tissue
Closure of the subcutaneous fat is associated with a decreased risk of wound disruption for women with a tissue thickness of more than 2 cm
Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103(5 pt 1):974–980.
Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
A meta-analysis of 5 randomized controlled trials demonstrated that suture closure of subcutaneous fat is associated with a 34% decrease in the risk of wound disruption in women with fat thickness greater than 2 cm (RR, 0.66; 95% CI, 0.48–0.91).21
A recent systematic review of evidence-based guidelines for surgical decisions during cesarean delivery also recommended this practice based on results of 9 published studies.22 In this review, however, subcutaneous drain placement did not offer any additional benefit, regardless of tissue thickness.22
10 Avoid unproven techniques
Several commonly performed techniques have not been associated with a decreased risk of SSI after cesarean delivery
Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
CORONIS Trial Collaborative Group. The CORONIS Trial. International study of caesarean section surgical techniques: a randomised fractional, factorial trial. BMC Pregnancy Childbirth. 2007;7:24. doi:10.1186/1471-2393-7-24.
Familiarity with the obstetric literature will help providers determine which interventions prevent SSI and which do not. Well-designed clinical studies have demonstrated no significant difference in the rate of postcesarean infectious morbidity with the administration of high concentrations of perioperative oxygen,22 saline wound irrigation,22 placement of subcutaneous drains,22 blunt versus sharp abdominal entry,23 and exteriorization of the uterus for repair.23
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Infection is the second leading cause of pregnancy-related mortality in the United States, responsible for 13.6% of all maternal deaths.1 Cesarean delivery is the single most important risk factor for puerperal infection, increasing its incidence approximately 5- to 20-fold.2
Given that cesarean deliveries represent 32.7% of all births in the United States,3 the overall health and socioeconomic burden of these infections is substantial. In addition, more than half of all pregnancies are complicated by maternal obesity, which is associated with an increased risk of cesarean delivery as well as subsequent wound complications.4
In this review, we offer 10 evidence-based strategies to prevent surgical site infection (SSI) after cesarean delivery.
1 Maintain strict glycemic control in women with diabetes
Perioperative hyperglycemia is associated with an increased risk of postoperative infection in patients with diabetes
Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591.
Hanazaki K, Maeda H, Okabayashi T. Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol. 2009;15(33):4122–4125.
Although data are limited on the impact of perioperative glycemic control on postcesarean infection rates, the association has been well documented in the general surgery literature. Results of a retrospective cohort study of 995 patients undergoing general or vascular surgery demonstrated that postoperative hyperglycemia increased the risk of infection by 30% for every 40-point increase in serum glucose levels from normoglycemia (defined as <110 mg/dL) (odds ratio, 1.3; 95% confidence interval [CI], 1.03–1.64).5 Hyperglycemia causes abnormalities of leukocyte function, including impaired granulocyte adherence, impaired phagocytosis, delayed chemotaxis, and depressed bactericidal capacity. And all of these abnormalities in leukocyte function appear to improve with strict glycemic control, although the target range for blood glucose remains uncertain.6
2 Recommend preoperative antiseptic showering
Ask patients to shower with 4% chlorhexidine gluconate the night before surgery to reduce the presence of bacterial skin flora
Mangram AJ, Horan TC, Pearson ML, et al; Hospital Infection Control Practices Advisory Committee. Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):247–278.
Chlebicki MP, Safdar N, O’Horo JC, Maki DG. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–173.
According to the Centers for Disease Control and Prevention, preoperative showering with chlorhexidine reduces the presence of bacterial skin flora. A study of more than 700 patients showed that preoperative showers with chlorhexidine reduced bacterial colony counts 9-fold, compared with only 1.3-fold for povidone-iodine.7 Whether this translates into a reduction in SSI remains controversial, in large part because of poor quality of the existing prospective trials, which used different agents, concentrations, and methods of skin preparation.8
Small clinical trials have found a benefit to chlorhexidine treatment the day before surgery.9,10 However, a recent meta-analysis of 16 randomized trials failed to show a significant reduction in the rate of SSI with chlorhexidine compared with soap, placebo, or no washing (relative risk [RR], 0.90; 95% CI, 0.77–1.05).11
3 Administer intravenous antibiotic prophylaxis
All patients who undergo cesarean delivery should be given appropriate antibiotic prophylaxis within 60 minutes before the skin incision
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472–1483.
Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a meta-analysis. Am J Obstet Gynecol. 2008;199(3):301.e1–e6.
The American College of Obstetricians and Gynecologists (ACOG) recommends the use of a single dose of a narrow-spectrum, first-generation cephalosporin (or a single dose of clindamycin with an aminoglycoside for those with a significant penicillin allergy) as SSI chemoprophylaxis for cesarean delivery.12 Due to concerns about fetal antibiotic exposure, such prophylaxis traditionally has been given after clamping of the umbilical cord. However, results of a recent meta-analysis of 5 randomized controlled trials demonstrated that antibiotic prophylaxis significantly reduced infectious morbidity (RR, 0.50; 95% CI, 0.33–0.78) when it was given 60 minutes before the skin incision, with no significant effect on neonatal outcome.13
4 Give a higher dose of preoperative antibiotics in obese women
Given the increased volume of distribution and the increased risk of postcesarean infection in the obese population, a higher dose of preoperative antibiotic prophylaxis is recommended
Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106(6):1357–1364.
Pevzner L, Swank M, Krepel C, et al. Effects of maternal obesity on tissue concentrations of prophylactic cefazolin during cesarean delivery. Obstet Gynecol. 2011;117(4):877–882.
The impact of maternal obesity on the risk of SSI after cesarean delivery was illustrated in a 2005 retrospective cohort study of 10,134 obese women. Moderately obese women with a prepregnancy weight of 90 to 100 kg were 1.6 times (95% CI, 1.31–1.95) more likely to have a wound infection, and severely obese women (>120 kg) were 4.45 times (95% CI, 3.00–6.61) more likely to have a wound infection after cesarean delivery, compared with women of normal weight.14
Moreover, a study of tissue concentrations of prophylactic cefazolin in obese women demonstrated that concentrations within adipose tissue at the site of the skin incision were inversely proportional to maternal body mass index (BMI).15 Given these findings, consideration should be given to using a higher dose of preoperative antibiotic prophylaxis in obese women, specifically 3 g of intravenous (IV) cefazolin for women with a BMI greater than 30 kg/m2 or an absolute weight of more than 100 kg.12
5 Use clippers for preoperative hair removal
If hair removal is necessary to perform the skin incision for cesarean delivery, the use of clippers is preferred
Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
In a Cochrane review of 3 randomized clinical trials comparing preoperative hair-removal techniques, shaving was associated with an increased risk of SSI, compared with clipping (RR, 2.09; 95% CI, 1.15–3.80).15 Shaving is thought to result in microscopic skin abrasions that can serve as foci for bacterial growth.
Interestingly, in this same Cochrane review, a separate analysis of 6 studies failed to show a benefit of preoperative hair removal by any means, compared with no hair removal,15 suggesting that routine hair removal may not be indicated for all patients.
6 Use chlorhexidine-alcohol for skin prep
Prepare the skin with chlorhexidine-alcohol immediately before surgery
Darouiche RO, Wall MJ Jr, Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2014;18:1–5.
Data from a randomized multicenter trial of 849 patients showed that the use of a chlorhexidine-alcohol skin preparation immediately before surgery lowered the rate of SSI after clean-contaminated surgery, compared with povidone-iodine (RR, 0.59; 95% CI, 0.41–0.85).16 Studies focusing on cesarean delivery alone are limited, although 1 small randomized trial found that chlorhexidine treatment significantly reduced bacterial growth at 18 hours after cesarean, compared with povidone-iodine (RR, 0.23; 95% CI, 0.07–0.70).17
7 Consider an alcohol-based hand rub for preoperative antisepsis
Alcohol-based hand rubs may be more effective than conventional surgical scrub
Shen NJ, Pan SC, Sheng WH, et al. Comparative antimicrobial efficacy of alcohol-based hand rub and conventional surgical scrub in a medical center [published online ahead of print September 21, 2013]. J Microbiol Immunol Infect. pii:S1684–1182(13)00150–3.
Tanner J, Swarbrook S, Stuart J. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev. 2008;1:CD004288.
Several agents are available for preoperative surgical hand antisepsis, including newer alcohol-based rubs and conventional aqueous scrubs that contain either chlorhexidine gluconate or povidone-iodine. In a prospective cohort study of 128 health care providers, use of an alcohol-based rub for surgical hand antisepsis was associated with a lower rate of positive bacterial culture (6.2%), compared with a chlorhexidine-based conventional scrub (47.6%; P<.001).18 However, if an aqueous-based scrub is the only option available for surgical hand antisepsis, a Cochrane review found that chlorhexidine gluconate scrubs were more effective than povidone-iodine scrubs in 3 trials, resulting in fewer colony-forming units of bacteria on the hands of the surgical team.19
8 Close the skin with subcuticular sutures
Use of subcuticular sutures for skin closure is associated with a lower risk of wound complications, compared with staples
Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a meta-analysis [published online ahead of print December 19, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.12.020.
A meta-analysis of 12 randomized controlled trials including 3,112 women demonstrated that subcuticular closure is associated with a decreased risk of wound complications, compared with staple closure (RR, 0.49; 95% CI, 0.28–0.87). The reduced risk remained significant even when stratified by obesity. Both closure techniques were shown to be equivalent with regard to postoperative pain, cosmetic outcome, and patient satisfaction.20
9 Close the subcutaneous tissue
Closure of the subcutaneous fat is associated with a decreased risk of wound disruption for women with a tissue thickness of more than 2 cm
Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103(5 pt 1):974–980.
Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
A meta-analysis of 5 randomized controlled trials demonstrated that suture closure of subcutaneous fat is associated with a 34% decrease in the risk of wound disruption in women with fat thickness greater than 2 cm (RR, 0.66; 95% CI, 0.48–0.91).21
A recent systematic review of evidence-based guidelines for surgical decisions during cesarean delivery also recommended this practice based on results of 9 published studies.22 In this review, however, subcutaneous drain placement did not offer any additional benefit, regardless of tissue thickness.22
10 Avoid unproven techniques
Several commonly performed techniques have not been associated with a decreased risk of SSI after cesarean delivery
Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
CORONIS Trial Collaborative Group. The CORONIS Trial. International study of caesarean section surgical techniques: a randomised fractional, factorial trial. BMC Pregnancy Childbirth. 2007;7:24. doi:10.1186/1471-2393-7-24.
Familiarity with the obstetric literature will help providers determine which interventions prevent SSI and which do not. Well-designed clinical studies have demonstrated no significant difference in the rate of postcesarean infectious morbidity with the administration of high concentrations of perioperative oxygen,22 saline wound irrigation,22 placement of subcutaneous drains,22 blunt versus sharp abdominal entry,23 and exteriorization of the uterus for repair.23
Share your thoughts! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125(1):5–12.
2. Leth RA, Moller JK, Thomsen RW, Uldbjerg N, Norgaard M. Risk of selected postpartum infections after cesarean section compared with vaginal birth: a five-year cohort study of 32,468 women. Acta Obstet Gynecol Scand. 2009;88(9):976–983.
3. Martin JA, Hamilton BE, Osterman JK, et al. Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–65.
4. American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 549: Obesity in pregnancy. Obstet Gynecol. 2013;121(1):213–217.
5. Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
6. Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591.
7. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Hospital Infection Control Practices Advisory Committee: Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):250–278.
8. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9:CD004985.
9. Hayek LJ, Emerson JM, Gardner AM. A placebo-controlled trial of the effect of two preoperative baths or showers with chlorhexidine detergent on post-operative wound infection rates. J Hosp Infect. 1987;10(2):165–172.
10. Wihlborg O. The effect of washing with chlorhexidine soap on wound infection rate in general surgery: a controlled clinical study. Ann Chir Gynaecol. 1987;76(5):263–265.
11. Chlebicki MP, Safdar N, O’Horo JC, Maki DG. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–173.
12. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472–1483.
13. Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a meta-analysis. Am J Obstet Gynecol. 2008;199(3):301.e1–e6.
14. Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106(6):1357–1364.
15. Pevzner L, Swank M, Krepel C, et al. Effects of maternal obesity on tissue concentrations of prophylactic cefazolin during cesarean delivery. Obstet Gynecol. 2011;117(4):877–882.
16. Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
17. Darouiche RO, Wall MJ Jr, Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
18. Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2014;18:1–5.
19. Shen NJ, Pan SC, Sheng WH, et al. Comparative antimicrobial efficacy of alcohol-based hand rub and conventional surgical scrub in a medical center [published online ahead of print September 21, 2013]. J Microbiol Immunol Infect. pii:S1684–1182(13)00150–3.
20. Tanner J, Swarbrook S, Stuart J. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev. 2008;1:CD004288.
21. Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a meta-analysis [published online ahead of print December 19, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.12.020.
22. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103(5 Pt 1):974–980.
23. Hanazaki K, Maeda H, Okabayashi T. Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol. 2009;15(33):4122–4125.
1. Creanga AA, Berg CJ, Syverson C, Seed K, Bruce FC, Callaghan WM. Pregnancy-related mortality in the United States, 2006–2010. Obstet Gynecol. 2015;125(1):5–12.
2. Leth RA, Moller JK, Thomsen RW, Uldbjerg N, Norgaard M. Risk of selected postpartum infections after cesarean section compared with vaginal birth: a five-year cohort study of 32,468 women. Acta Obstet Gynecol Scand. 2009;88(9):976–983.
3. Martin JA, Hamilton BE, Osterman JK, et al. Births: final data for 2013. Natl Vital Stat Rep. 2015;64(1):1–65.
4. American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 549: Obesity in pregnancy. Obstet Gynecol. 2013;121(1):213–217.
5. Dahlke JD, Mendez-Figueroa H, Rouse DJ, Berghella V, Baxter JK, Chauhan SP. Evidence-based surgery for cesarean delivery: an updated systematic review. Am J Obstet Gynecol. 2013;209(4):294–306.
6. Ramos M, Khalpey Z, Lipsitz S, et al. Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg. 2008;248(4):585–591.
7. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Hospital Infection Control Practices Advisory Committee: Guideline for prevention of surgical site infection, 1999. Infect Control Hosp Epidemiol. 1999;20(4):250–278.
8. Webster J, Osborne S. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev. 2012;9:CD004985.
9. Hayek LJ, Emerson JM, Gardner AM. A placebo-controlled trial of the effect of two preoperative baths or showers with chlorhexidine detergent on post-operative wound infection rates. J Hosp Infect. 1987;10(2):165–172.
10. Wihlborg O. The effect of washing with chlorhexidine soap on wound infection rate in general surgery: a controlled clinical study. Ann Chir Gynaecol. 1987;76(5):263–265.
11. Chlebicki MP, Safdar N, O’Horo JC, Maki DG. Preoperative chlorhexidine shower or bath for prevention of surgical site infection: a meta-analysis. Am J Infect Control. 2013;41(2):167–173.
12. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 120: Use of prophylactic antibiotics in labor and delivery. Obstet Gynecol. 2011;117(6):1472–1483.
13. Costantine MM, Rahman M, Ghulmiyah L, et al. Timing of perioperative antibiotics for cesarean delivery: a meta-analysis. Am J Obstet Gynecol. 2008;199(3):301.e1–e6.
14. Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106(6):1357–1364.
15. Pevzner L, Swank M, Krepel C, et al. Effects of maternal obesity on tissue concentrations of prophylactic cefazolin during cesarean delivery. Obstet Gynecol. 2011;117(4):877–882.
16. Tanner J, Norrie P, Melen K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev. 2011;11:CD004122.
17. Darouiche RO, Wall MJ Jr, Itani KM, et al. Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med. 2010;362(1):18–26.
18. Kunkle CM, Marchan J, Safadi S, Whitman S, Chmait RH. Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med. 2014;18:1–5.
19. Shen NJ, Pan SC, Sheng WH, et al. Comparative antimicrobial efficacy of alcohol-based hand rub and conventional surgical scrub in a medical center [published online ahead of print September 21, 2013]. J Microbiol Immunol Infect. pii:S1684–1182(13)00150–3.
20. Tanner J, Swarbrook S, Stuart J. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev. 2008;1:CD004288.
21. Mackeen AD, Schuster M, Berghella V. Suture versus staples for skin closure after cesarean: a meta-analysis [published online ahead of print December 19, 2014]. Am J Obstet Gynecol. doi:10.1016/j.ajog.2014.12.020.
22. Chelmow D, Rodriguez EJ, Sabatini MM. Suture closure of subcutaneous fat and wound disruption after cesarean delivery: a meta-analysis. Obstet Gynecol. 2004;103(5 Pt 1):974–980.
23. Hanazaki K, Maeda H, Okabayashi T. Relationship between perioperative glycemic control and postoperative infections. World J Gastroenterol. 2009;15(33):4122–4125.
Does stage of labor at time of cesarean affect the risk of subsequent preterm birth?
Recent policy changes in the United States have led to a modest reduction in the incidence of late PTB (34–37 weeks), but the rate of PTB before 34 weeks’ gestation has changed little over the past 40 years. One reason: It has taken us more than 30 years to recognize that uterine contractions are a downstream consequence—not a cause—of preterm labor. By the time a woman presents to labor and delivery with regular phasic uterine contractions and cervical change, it is too late to alter the course of events; the pathogenic processes leading to this clinical presentation have been active for weeks—probably months. Efforts to suppress myometrial contractility at this point using standard tocolytic medications have little or no effect. At best, they delay delivery for 24 to 48 hours, just time enough to transfer the patient to a tertiary care center, administer antenatal corticosteroids, and, possibly, administer magnesium sulfate for neuroprotection.
There is mounting evidence that the cervix plays a central role in spontaneous PTB pathogenesis. The task of the cervix is to remain functionally intact (long and closed) throughout gestation even as the fetus grows and the uterus expands, and then to efface and dilate in the days and hours before labor. PTB ensues if this process of cervical remodeling occurs prematurely.
In support of this hypothesis, cervical shortening on transvaginal ultrasound in the mid second trimester is a major risk factor for spontaneous PTB that is independent of parity and obstetric history.1 This risk can be abrogated by interventions that artificially “strengthen” the cervix (such as placement of a cervical cerclage or pessary) or interfere with the biochemical changes within the cervical stroma that promote cervical effacement (by progesterone supplementation). This analysis by Levine and colleagues provides additional evidence in support of the role of the cervix in spontaneous PTB.
As the investigators themselves hypothesize: “… there may be an inherent biologic risk in achieving complete dilation, regardless of mode of delivery, or perhaps something protective about not achieving complete dilation. This could be attributed to changes in cervical stroma that occur with complete dilation that causes the cervix to be more susceptible to premature dilation in a future pregnancy.”
Although compelling, the “cervical trauma” hypothesis remains to be confirmed. Additional studies are needed to confirm these observations, and it would be preferable to limit these studies to the risk of subsequent spontaneous PTB with intact membranes only, rather than including women with preterm premature rupture of membranes, as in the current study.
What this evidence means for practice
This study suggests that the attainment of full dilation during the course of labor may damage the fibrous tissues that make up the cervical stroma, leading to a persistent functional defect that manifests as spontaneous PTB in a future pregnancy. If that is true, could it also be true that a normal vaginal delivery at term is a “risk factor” for spontaneous PTB in a future pregnancy? There is one clinical variable that could account for this apparent contradiction—the interpregnancy interval. It is well known that a short interval (<6 months) is a risk factor for adverse pregnancy outcomes, including PTB. It is possible that, having been injured at the time of delivery, the cervical stroma needs time to heal. Similar observations have been made when investigating the association between cervical conization and PTB.2 This is a testable hypothesis that I hope these investigators will pursue. In the meantime, we should continue to advise our patients to allow for an appropriate interval between pregnancies.
Errol R. Norwitz, MD, PHD
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996;334(9):567–572.
2.Himes KP, Simhan HN. Time from cervical conization to pregnancy and preterm birth. Obstet Gynecol. 2007;109(2 pt 1):314–319.
Recent policy changes in the United States have led to a modest reduction in the incidence of late PTB (34–37 weeks), but the rate of PTB before 34 weeks’ gestation has changed little over the past 40 years. One reason: It has taken us more than 30 years to recognize that uterine contractions are a downstream consequence—not a cause—of preterm labor. By the time a woman presents to labor and delivery with regular phasic uterine contractions and cervical change, it is too late to alter the course of events; the pathogenic processes leading to this clinical presentation have been active for weeks—probably months. Efforts to suppress myometrial contractility at this point using standard tocolytic medications have little or no effect. At best, they delay delivery for 24 to 48 hours, just time enough to transfer the patient to a tertiary care center, administer antenatal corticosteroids, and, possibly, administer magnesium sulfate for neuroprotection.
There is mounting evidence that the cervix plays a central role in spontaneous PTB pathogenesis. The task of the cervix is to remain functionally intact (long and closed) throughout gestation even as the fetus grows and the uterus expands, and then to efface and dilate in the days and hours before labor. PTB ensues if this process of cervical remodeling occurs prematurely.
In support of this hypothesis, cervical shortening on transvaginal ultrasound in the mid second trimester is a major risk factor for spontaneous PTB that is independent of parity and obstetric history.1 This risk can be abrogated by interventions that artificially “strengthen” the cervix (such as placement of a cervical cerclage or pessary) or interfere with the biochemical changes within the cervical stroma that promote cervical effacement (by progesterone supplementation). This analysis by Levine and colleagues provides additional evidence in support of the role of the cervix in spontaneous PTB.
As the investigators themselves hypothesize: “… there may be an inherent biologic risk in achieving complete dilation, regardless of mode of delivery, or perhaps something protective about not achieving complete dilation. This could be attributed to changes in cervical stroma that occur with complete dilation that causes the cervix to be more susceptible to premature dilation in a future pregnancy.”
Although compelling, the “cervical trauma” hypothesis remains to be confirmed. Additional studies are needed to confirm these observations, and it would be preferable to limit these studies to the risk of subsequent spontaneous PTB with intact membranes only, rather than including women with preterm premature rupture of membranes, as in the current study.
What this evidence means for practice
This study suggests that the attainment of full dilation during the course of labor may damage the fibrous tissues that make up the cervical stroma, leading to a persistent functional defect that manifests as spontaneous PTB in a future pregnancy. If that is true, could it also be true that a normal vaginal delivery at term is a “risk factor” for spontaneous PTB in a future pregnancy? There is one clinical variable that could account for this apparent contradiction—the interpregnancy interval. It is well known that a short interval (<6 months) is a risk factor for adverse pregnancy outcomes, including PTB. It is possible that, having been injured at the time of delivery, the cervical stroma needs time to heal. Similar observations have been made when investigating the association between cervical conization and PTB.2 This is a testable hypothesis that I hope these investigators will pursue. In the meantime, we should continue to advise our patients to allow for an appropriate interval between pregnancies.
Errol R. Norwitz, MD, PHD
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
Recent policy changes in the United States have led to a modest reduction in the incidence of late PTB (34–37 weeks), but the rate of PTB before 34 weeks’ gestation has changed little over the past 40 years. One reason: It has taken us more than 30 years to recognize that uterine contractions are a downstream consequence—not a cause—of preterm labor. By the time a woman presents to labor and delivery with regular phasic uterine contractions and cervical change, it is too late to alter the course of events; the pathogenic processes leading to this clinical presentation have been active for weeks—probably months. Efforts to suppress myometrial contractility at this point using standard tocolytic medications have little or no effect. At best, they delay delivery for 24 to 48 hours, just time enough to transfer the patient to a tertiary care center, administer antenatal corticosteroids, and, possibly, administer magnesium sulfate for neuroprotection.
There is mounting evidence that the cervix plays a central role in spontaneous PTB pathogenesis. The task of the cervix is to remain functionally intact (long and closed) throughout gestation even as the fetus grows and the uterus expands, and then to efface and dilate in the days and hours before labor. PTB ensues if this process of cervical remodeling occurs prematurely.
In support of this hypothesis, cervical shortening on transvaginal ultrasound in the mid second trimester is a major risk factor for spontaneous PTB that is independent of parity and obstetric history.1 This risk can be abrogated by interventions that artificially “strengthen” the cervix (such as placement of a cervical cerclage or pessary) or interfere with the biochemical changes within the cervical stroma that promote cervical effacement (by progesterone supplementation). This analysis by Levine and colleagues provides additional evidence in support of the role of the cervix in spontaneous PTB.
As the investigators themselves hypothesize: “… there may be an inherent biologic risk in achieving complete dilation, regardless of mode of delivery, or perhaps something protective about not achieving complete dilation. This could be attributed to changes in cervical stroma that occur with complete dilation that causes the cervix to be more susceptible to premature dilation in a future pregnancy.”
Although compelling, the “cervical trauma” hypothesis remains to be confirmed. Additional studies are needed to confirm these observations, and it would be preferable to limit these studies to the risk of subsequent spontaneous PTB with intact membranes only, rather than including women with preterm premature rupture of membranes, as in the current study.
What this evidence means for practice
This study suggests that the attainment of full dilation during the course of labor may damage the fibrous tissues that make up the cervical stroma, leading to a persistent functional defect that manifests as spontaneous PTB in a future pregnancy. If that is true, could it also be true that a normal vaginal delivery at term is a “risk factor” for spontaneous PTB in a future pregnancy? There is one clinical variable that could account for this apparent contradiction—the interpregnancy interval. It is well known that a short interval (<6 months) is a risk factor for adverse pregnancy outcomes, including PTB. It is possible that, having been injured at the time of delivery, the cervical stroma needs time to heal. Similar observations have been made when investigating the association between cervical conization and PTB.2 This is a testable hypothesis that I hope these investigators will pursue. In the meantime, we should continue to advise our patients to allow for an appropriate interval between pregnancies.
Errol R. Norwitz, MD, PHD
Share your thoughts on this article! Send your Letter to the Editor to rbarbieri@frontlinemedcom.com. Please include your name and the city and state in which you practice.
1. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996;334(9):567–572.
2.Himes KP, Simhan HN. Time from cervical conization to pregnancy and preterm birth. Obstet Gynecol. 2007;109(2 pt 1):314–319.
1. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996;334(9):567–572.
2.Himes KP, Simhan HN. Time from cervical conization to pregnancy and preterm birth. Obstet Gynecol. 2007;109(2 pt 1):314–319.
Hypertension and pregnancy and preventing the first cesarean delivery
This peer to peer discussion focuses on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines1 and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.2
In this 20-minute audiocast, listen to these experts discuss:
Changing diagnostic tools for preeclampsia
- The 24-hour urinary protein estimation: When is it necessary?
- Use of magnesium sulfate for seizure prophylaxis
Preventing the first cesarean delivery
- Redefining the stages of labor: When is the second-stage too long?
- The lost skill of forceps delivery
- Is cesarean delivery rate the optimal metric for measuring neonatal outcome?
John T. Repke, MD, is University Professor and Chairman of the Department of Obstetrics and Gynecology at Penn State University College of Medicine, and Obstetrician-Gynecologist-in-Chief at the Milton S. Hershey Medical Center in Hershey, Pennsylvania. Dr. Repke is a member of the Board of Editors of OBG Management and is author of the June 2014 Guest Editorial on hypertension and pregnancy.
Errol R. Norwitz, MD, PhD, is the Louis E. Phaneuf Professor and Chairman of the Department of Obstetrics and Gynecology at Tufts Medical Center and Tufts University School of Medicine in Boston, Massachusetts. Dr. Norwitz is a member of the Board of Editors of OBG Management and is author of the June 2014 Update on operative vaginal delivery.
The speakers report no financial relationships relevant to this audiocast.
Click here for a downloadable transcript
TRANSCRIPT
ACOG guidelines on hypertension and pregnancy raise some questions
John T. Repke, MD: So, Errol, I was impressed over the first couple of days of being at the meeting. As you know, we had a postgraduate course, and one of the items that we talked about was the new hypertension and pregnancy document that was released by the Task Force on Hypertension and Pregnancy1 charged by the American College of Obstetricians and Gynecologists. I’ve got to say that while the goal of the document was to provide some standardization and clarification, there still seems to be a lot of confusion in my audience about how to interpret some of the guidelines. Have you found that?
Errol R. Norwitz, MD, PhD: Yes, I have. I found it interesting that it was put out as an executive summary, and not as a practice bulletin, which will probably follow in months. That document, which came out in November 2013, helped to address many of the issues we’ve had over the years of preeclampsia, in terms of its definition and some of the management issues. But, it also raised a number of questions that still need to be resolved.
Dr. Repke: Yes. I think one of the things to keep in mind, and I’ve tabulated all of the recommendations, is that about 60 recommendations came out of that document and only six of the 60 were accompanied by a strong quality of evidence, or rather, a high quality of evidence, and a strong recommendation. And a lot of those things were addressing issues that I think most practitioners already did, in so far as using antenatal steroids for maturation; using magnesium sulfate for patients with preeclampsia with severe features; and using magnesium sulfate as a treatment of eclampsia. But a lot of the other recommendations really were based on either moderate- or low-quality evidence, and had qualified recommendations. And, I think that’s what has led to some of the confusion.
Changing diagnostic tools for preeclampsia
Dr. Repke: What sort of specific things are your practitioners asking you about as far as, “Is this gestational hypertension or is this preeclampsia?” The guidelines say proteinuria is not required anymore. How are you dealing with that?
Should we still do the 24-hour urinary protein estimation?
Dr. Norwitz: The biggest change, in my mind, is the statement that you no longer require significant proteinuria to make the diagnosis of preeclampsia, and, indeed, of severe preeclampsia. So, if you do have significant proteinuria, then that would confirm the diagnosis. But, you can also have preeclampsia in the presence of other endorgan injuries, such as kidney injury and liver injury in the absence of significant proteinuria.
So, one of the questions that comes up is, “Should we actually do the 24-hour urinary protein estimation?”
And, my answer is, “yes.” If you have significant proteinuria, then that would confirm the diagnosis. If you don’t, you can still make the diagnosis in the setting of low platelets, elevated liver enzymes, or abnormal renal function. So, the issue is, and I’d be curious to hear your answer, if you have someone with platelets of, let’s say, 78, a new onset of sustained elevation of blood pressure, would you do the 24-hour urine estimation or just defer it?
Dr. Repke: We wouldn’t perform the 24-hour urine test under those circumstances. And, we would consider that nuance of hypertension with a severe feature that is now preeclampsia with severe feature, and the management would be based on gestational age. With a platelet count that low, the management would be stabilization and delivery. Although, if stabilized, I think that’s the type of patient that potentially could have delivery delayed until you could get an effective antenatal steroid if she was less that 34 weeks’ gestation.
Dr. Norwitz: So, that’s one issue I think needs to be clarified. If there’s other evidence of endorgan damage, then you can defer the 24-hour urinary protein. That’s another question that comes up. I’m pleased they could resolve the issue of repeated 24-hour urinary estimations. Once you have your 300 mg suggestive of the diagnosis of preeclampsia, there’s no reason to then repeat it looking for elevation and increased leakage of protein into the urine, because it doesn’t correlate with adverse outcome for the mother or fetus. So, that issue was clarified.
Dr. Repke: I think that two questions that came up in our course, and I think they were very legitimate, are, “Do we even need to do urine protein at all?” Because if you look at the guidelines for management, the only difference between preeclampsia management without severe features and gestational hypertension is frequency of antenatal testing until you decide to begin delivery. Now, in the old days, one would say, “Well, another difference would be that the preeclamptic would get magnesium sulfate.” But the current Hypertension in Pregnancy Guidelines1 suggest that preeclampsia without severe features doesn’t necessarily have to be managed with magnesium sulfate. So, I’m still wrestling with whether, other than the fact that it might be for study purposes or for categorization or research, whether proteinuria adds anything to the equation.
And, then the second question is, “How do you resolve the issue of disagreement?” So, the example is protein:creatinine ratio allows for a more rapid diagnosis of significant proteinuria. If that patient doesn’t have to deliver immediately and a 24-hour urine sample is obtained, which do you believe if you have a protein:creatinine ratio greater than 0.3, but now your 24-hour urine is 212 mg/dL? And, I don’t have the answer to that, but that’s another area of confusion.
Dr. Norwitz: And, I think that confusion will persist. I don’t think this document is going to resolve it.
New terminology: Preeclampsia with or without severe features
Dr. Norwitz: I do like the difference in terminology between preeclampsia with severe features and preeclampsia without severe features. I think the old terminology of severe and mild preeclampsia was somewhat confusing. I certainly appreciate that alteration in terminology, although it may take a while for it to catch on. I’m still seeing the term “mild preeclampsia” used quite widely.
Use of magnesium sulfate for seizure prophylaxis
Dr. Norwitz: You did raise the issue of magnesium sulfate for seizure prophylaxis in the setting of severe preeclampsia without severe features. And I was struck by the statement. Not only is it not necessary to give it, but in the Executive Summary, as you suggest, it is not indicated and you recommended against starting it. Is that how you interpret it as the well?
Dr. Repke: Well, I might have interpreted the statement the way I wanted to interpret it. And, as you know, in our institution, because we feel we are a teaching program, people can progress very quickly intrapartum from not having severe features to having severe features, and we don’t want to miss that window of opportunity. Our practice in that regard does not follow the guidelines. We use intrapartum magnesium prophylaxis for all patients with the diagnosis of preeclampsia, and continue it for 24 hours postpartum.
Dr. Norwitz: And I would have to say we decided do the same. So, once a diagnosis of preeclampsia is made, we would give intrapartum, and then postpartum magnesium seizure prophylaxis for 24 hours, regardless of whether there’s evidence of severe features or no severe features.
Dr. Repke: And there again, I think it’s why, for you and I, it will still be important to assess the proteinuria because that diagnostic difference between preeclampsia and gestational hypertension is going to alter management. But if you follow the document word for word, if you’re not going to use magnesium without severe features, I’m not really sure what proteinuria adds. I guess, at the end of the day, you’ve got to be a good doctor. And, you’ve got to be physically assessing your patient on a very regular basis.
Preventing the first cesarean delivery. Will cesarean rates decline?
Dr. Repke: So, speaking of guidelines, the Society for Maternal Fetal Medicine (SMFM) just came out with a document trying to address this issue of the cesarean-section rate in the United States and are there things that we can be doing to lower the primary C-section rate.2 My feeling is probably disseminated from the recognition that vaginal birth after C-section never got to the levels of acceptance that anybody hoped back when Healthy People 2010 was first written. And, we could eliminate that issue or, at least significantly reduce that issue, if the first C-section never took place.
And, I guess I’d like some of your thoughts about some of the things in that document, some of the things we need to be reconsidering in terms of how we define labor and so on.
Dr. Norwitz: It is true, I think, that there’s been an epidemic of cesarean deliveries in the last decade in the US, but also throughout the world, I think, even in countries that have traditionally had very low cesarean delivery rates, the classic one being Ireland and the UK countries. Their rates are now increasing significantly.
And there are a number of different reasons as to why this may be. I think, certainly the obesity epidemic has contributed to this. You want to deliver patients who have an elevated BMI prior to the postterm period. But, it’s often difficult to monitor these patients, and the cesarean-delivery rate overall is much higher in that population. So, that might be one reason why cesarean-delivery rates overall are going up. But, certainly there are many others.
Dr. Repke: Yes, I think you’re absolutely right: the demographics of change. Childbearing is being delayed. We know that uterine contractility dynamics alter with advanced maternal age. We’ve got a higher incidence of multiple gestations with advanced maternal age. We have more patients that require induction because of supervening medical complications of pregnancy, whether that be Class A2 gestational diabetes, or whether that be pregnancy-induced hypertension.
Redefining the stages of labor
Dr. Repke: I think some of the intriguing data, to me, is a willingness to re-look at how we define the stages of labor. And what are acceptable norms? And, while I have some concerns about how that may be interpreted in the rank and file, I think it’s at least heightened the awareness of my faculty that we just can’t tolerate the C-section at 4 cm, or whether the latent phase of labor should be allowed to go to 6 cm. I don’t think we really have the data for that. But I’d be happy if I could just start to see a reduction in “failure to progress at 4 cm.”
And then the issue of second stage, I think, is also important. What do you think about the guidelines’ recommendation that there may not really be an upper limit of allowability for second-stage labors?
Dr. Norwitz: Well, certainly I think it’s important to think back to the historical context of where the labor curves developed. The original labor curves were actually developed in Zimbabwe (at that time it was Rhodesia) by an obstetrician working in the community called Philpott. And he was trying to determine when it was appropriate to send patients into the tertiary care center. So he designed the labor curve and said if patients failed to progress over a certain number of hours, those are patients that are likely to need an operative delivery, and he would then send them into the tertiary care center.
And, then Dr. Freidman picked up on that idea and developed the Freidman Curve in Boston. But that was an era, again, many years ago when the population demographics were very different, when not many patients received regional anesthesia. I think if you look at the current guidelines, there is a huge discrepancy between women who get epidural anesthesia and those that don’t in terms of the progress of labor, both the first stage and the second stage.
Is it anesthesia?
Dr. Repke: One of the things that, you know, I haven’t looked at this paper in a long time, but you remember at Brigham and Women’s Hospital, probably 20 years ago, we were winding down the Active Management of Labor Study3 that was designed to try to replicate what had gone on at the Dublin Maternity Hospital,4 and if I’m remembering correctly, one of the remarkable things about that is that in Dublin, there were virtually no C-sections in the second stage. And so people assumed that while they were more aggressive with forceps, the operative vaginal delivery rate was no different between Brigham and Women’s Hospital and the Dublin Maternity Hospital. And so there needed to be another explanation.
And, I know I’m going to incur some of the ire of our anesthesia colleagues, but I really wonder whether there is a contribution of regional anesthesia to some of the labor dystocias that we see, and whether that’s a new demographic that we haven’t really adequately assessed. Even though I recognize some of the anesthesia literature5 seems to suggest very strongly that it has no effect. You know, if you were to plot a graph of regional anesthesia rates and cesarean section rates, they would probably parallel each other.
Dr. Norwitz: I think they do. I think we’ve long known that epidural anesthesia slows down the second stage of labor. These analyses suggest that it also has a significant effect on the first stage. And, I think that needs to be taken into account.
The lost skill of forceps delivery
Dr. Norwitz: I personally think that the skill set, in terms of operative vaginal delivery with forceps and vacuum, has really been lost. And I do feel that’s one of the factors contributing to the increase in cesarean delivery rates. I certainly see that in my practice: that I’m comfortable doing rotational forceps and mid-cavity forceps deliveries, where many of my colleagues have lost that skill, and rely now on the vacuum, which in certain circumstances is a less-than-ideal instrument. So, I believe that’s part of the reason why the cesarean delivery rates have gone up.
Lengthy second stage
Dr. Norwitz: But, certainly, I think, epidural anesthesia has made a difference, and I think we need to be cognizant of the fact that there is no “hard stop” now, in terms of the length of the second stage. If you get to 3 hours, even 4 hours, I would say, and there’s continued descent with pushing and fetal heart-rate tracing is reassuring, it’s reasonable to continue beyond those cutoffs.
Dr. Repke: I agree. I also have a concern about that, and I’m going to use a little bit of a parallel example of, you know, 7 or 8 years ago, there was a big push, and I think it was an appropriate push, to try to avoid elective deliveries prior to 39 weeks.6,7 What ended up happening was that people forgot about the term “elective,” and all they heard was 39 weeks. And what we would see on Board Examinations was, “Why do you have this placenta previa delivering at 39 weeks?”
“Well, that’s our hospital policy. We can’t deliver before 39 weeks.”
And, I think, the complications started to arise, and that’s what led to SMFM and ACOG coming out with guidelines for when it is acceptable to deliver prior to 39 weeks.2,6–8
So, the analogy is: I’m afraid that people are only going to see there is no upper limit for latent phase, there is no upper limit for second stage; that clinical judgment may not get its due in making these decisions. And we’ve all been in situations where, when you are trying to extract the head out of the pelvis, a cesarean section after a 5- or 6-hour second stage has its own set of complications. So my concern is that I hope we will recognize that we have to still use some clinical judgment, what I term the so-called “art of obstetrics,” into managing these patients.
Are you optimistic that we’re going to the lower C-section rate?
Dr. Norwitz: No, I think, it’s going to continue to go up. I think, with the increasing number of multiple pregnancies, obesity, maternal age getting further and further along, I think this is only going to continue to rise. And to be honest, I don’t know the correct cesarean delivery rate, or even if that is the metric that we should be measuring.
What is the right metric to measure neonatal outcome?
Dr. Norwitz: Maybe we should be looking at perinatal outcome. If perinatal outcome is improved, then maybe the cesarean rate is less important. Obviously, the first cesarean does have implications for subsequent pregnancy outcomes, and if we do continue to see this rise in cesarean deliveries, we are going to end up with many more placental accretas and hemorrhages in women in years to come.
So, careful counseling is important. If patients plan to have one or two kids only, maybe a cesarean delivery is very reasonable. If they are planning on having six or seven kids, then maybe you have to have a more careful discussion.
Dr. Repke: Yes, I think, that’s a very good point: the number of cesareans and the potential risks for abnormal placentation. I think societal expectations have changed in terms of what they want. Most mothers are willing to sacrifice maternal risk for presumed benefits to the fetus.
I think, where we’ve gotten into trouble as a specialty, though, is that we’ve had a hard time proving that neonatal outcome, in fact, has improved—despite an almost tripling of the cesarean section rate since, probably, the early 1970s. Although, anecdotally, what my pediatric and neonatal colleagues will tell me is they don’t get the kind of damaged babies they used to get. So the neonatologists that are closer to my age that have been doing this for a long time, they’re not seeing the really severe meconium aspiration syndromes; they’re not seeing really severe forceps-related injuries, or vacuum-related injuries that they used to see. So, those may be data that we’re going to need to accumulate with a little bit more rigor, and see if that’s true.
But I tend to agree with you. I don’t know what the right cesarean section rate is. I often tell people, I have yet to meet a patient who doesn’t think her cesarean section was indicated. And that’s where I think we hit the crossroads of individual patient-care management. So, we know across all other disciplines in medicine we’re entering the era of personalized medicine, yet we want to make broad public health policy that may not apply to individuals, and run with that. So, that’s also a concern. But, as they say, a story we will follow with interest.
Dr. Norwitz: I think so. I think the other part of that equation is the stillbirth rate, and the fact that there’s a push now to avoid elective inductions before 39 weeks, which I think is very reasonable, with a focus there again on elective inductions.
There’s also a push to induce patients before 42 weeks. And that bar has been pushed back, and in most practices around the country now, deliveries are being affected and recommended at 41 weeks. And clearly, if you take a nulliparous patient with an unfavorable cervix and induce at 41 weeks, you are going to increase the cesarean rate. I would argue that you are also decreasing the chance that there will be a stillbirth. But that data has not been forthcoming.
So this issue is by no means resolved. I think there are going to be many more years of data and studies and consensus opinions before we have a much better sense of what the right cesarean
rate is.
Dr. Repke: Yes, I think that’s a great point. And, one thing that I think people aren’t maybe that familiar with is when this push came, and again, it is an appropriate push to minimize elective deliveries before 39 weeks. When they looked at neonatal outcomes, all they looked at were the group that delivered at 37 weeks, and the group that delivered at 39 weeks. And they didn’t look at what happened with the other ones.9
So, they did look at the stillbirths of fetal distress or the other complications that happened between 37 and 1, and 38 and 6. They just looked at neonates that were born at 37 weeks and compared them to neonates that were born at 39 weeks, and found reduced instances of things like transient tachypnea of the newborn, hyperbilirubinemia, and thermoregulation issues, and those sorts of things. But, never looked at the neonates in that window, so no question 39 is better than 37, but, 37 is better than not making it to 39. So that, as you said, we’ve got a lot more information we’ve got to gather.
Errol, good talking with you.
Dr. Norwitz: Thank you.
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus: Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Frigoletto FD, Lieberman E, Lang J, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333(12):745–750.
- O’Driscoll K, Meagher D, Boylan P. Active Management of Labor. 3rd ed. London: Mosby- Yearbook; 1993.
- Chestnut DH, McGrath JM, Vincent RD, et al. Does early administration of epidural analgesia effect obstetric outcome in nulliparous women who are in spontaneous labor? Anesthesiology. 1994;80(6):1201–1208.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 560: Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915.
- Spong CY, Mercer BM, D’Alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):323–333.
- Tita ATN, Landon MB, Spong CY, et al; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat Cesarean Delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
This peer to peer discussion focuses on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines1 and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.2
In this 20-minute audiocast, listen to these experts discuss:
Changing diagnostic tools for preeclampsia
- The 24-hour urinary protein estimation: When is it necessary?
- Use of magnesium sulfate for seizure prophylaxis
Preventing the first cesarean delivery
- Redefining the stages of labor: When is the second-stage too long?
- The lost skill of forceps delivery
- Is cesarean delivery rate the optimal metric for measuring neonatal outcome?
John T. Repke, MD, is University Professor and Chairman of the Department of Obstetrics and Gynecology at Penn State University College of Medicine, and Obstetrician-Gynecologist-in-Chief at the Milton S. Hershey Medical Center in Hershey, Pennsylvania. Dr. Repke is a member of the Board of Editors of OBG Management and is author of the June 2014 Guest Editorial on hypertension and pregnancy.
Errol R. Norwitz, MD, PhD, is the Louis E. Phaneuf Professor and Chairman of the Department of Obstetrics and Gynecology at Tufts Medical Center and Tufts University School of Medicine in Boston, Massachusetts. Dr. Norwitz is a member of the Board of Editors of OBG Management and is author of the June 2014 Update on operative vaginal delivery.
The speakers report no financial relationships relevant to this audiocast.
Click here for a downloadable transcript
TRANSCRIPT
ACOG guidelines on hypertension and pregnancy raise some questions
John T. Repke, MD: So, Errol, I was impressed over the first couple of days of being at the meeting. As you know, we had a postgraduate course, and one of the items that we talked about was the new hypertension and pregnancy document that was released by the Task Force on Hypertension and Pregnancy1 charged by the American College of Obstetricians and Gynecologists. I’ve got to say that while the goal of the document was to provide some standardization and clarification, there still seems to be a lot of confusion in my audience about how to interpret some of the guidelines. Have you found that?
Errol R. Norwitz, MD, PhD: Yes, I have. I found it interesting that it was put out as an executive summary, and not as a practice bulletin, which will probably follow in months. That document, which came out in November 2013, helped to address many of the issues we’ve had over the years of preeclampsia, in terms of its definition and some of the management issues. But, it also raised a number of questions that still need to be resolved.
Dr. Repke: Yes. I think one of the things to keep in mind, and I’ve tabulated all of the recommendations, is that about 60 recommendations came out of that document and only six of the 60 were accompanied by a strong quality of evidence, or rather, a high quality of evidence, and a strong recommendation. And a lot of those things were addressing issues that I think most practitioners already did, in so far as using antenatal steroids for maturation; using magnesium sulfate for patients with preeclampsia with severe features; and using magnesium sulfate as a treatment of eclampsia. But a lot of the other recommendations really were based on either moderate- or low-quality evidence, and had qualified recommendations. And, I think that’s what has led to some of the confusion.
Changing diagnostic tools for preeclampsia
Dr. Repke: What sort of specific things are your practitioners asking you about as far as, “Is this gestational hypertension or is this preeclampsia?” The guidelines say proteinuria is not required anymore. How are you dealing with that?
Should we still do the 24-hour urinary protein estimation?
Dr. Norwitz: The biggest change, in my mind, is the statement that you no longer require significant proteinuria to make the diagnosis of preeclampsia, and, indeed, of severe preeclampsia. So, if you do have significant proteinuria, then that would confirm the diagnosis. But, you can also have preeclampsia in the presence of other endorgan injuries, such as kidney injury and liver injury in the absence of significant proteinuria.
So, one of the questions that comes up is, “Should we actually do the 24-hour urinary protein estimation?”
And, my answer is, “yes.” If you have significant proteinuria, then that would confirm the diagnosis. If you don’t, you can still make the diagnosis in the setting of low platelets, elevated liver enzymes, or abnormal renal function. So, the issue is, and I’d be curious to hear your answer, if you have someone with platelets of, let’s say, 78, a new onset of sustained elevation of blood pressure, would you do the 24-hour urine estimation or just defer it?
Dr. Repke: We wouldn’t perform the 24-hour urine test under those circumstances. And, we would consider that nuance of hypertension with a severe feature that is now preeclampsia with severe feature, and the management would be based on gestational age. With a platelet count that low, the management would be stabilization and delivery. Although, if stabilized, I think that’s the type of patient that potentially could have delivery delayed until you could get an effective antenatal steroid if she was less that 34 weeks’ gestation.
Dr. Norwitz: So, that’s one issue I think needs to be clarified. If there’s other evidence of endorgan damage, then you can defer the 24-hour urinary protein. That’s another question that comes up. I’m pleased they could resolve the issue of repeated 24-hour urinary estimations. Once you have your 300 mg suggestive of the diagnosis of preeclampsia, there’s no reason to then repeat it looking for elevation and increased leakage of protein into the urine, because it doesn’t correlate with adverse outcome for the mother or fetus. So, that issue was clarified.
Dr. Repke: I think that two questions that came up in our course, and I think they were very legitimate, are, “Do we even need to do urine protein at all?” Because if you look at the guidelines for management, the only difference between preeclampsia management without severe features and gestational hypertension is frequency of antenatal testing until you decide to begin delivery. Now, in the old days, one would say, “Well, another difference would be that the preeclamptic would get magnesium sulfate.” But the current Hypertension in Pregnancy Guidelines1 suggest that preeclampsia without severe features doesn’t necessarily have to be managed with magnesium sulfate. So, I’m still wrestling with whether, other than the fact that it might be for study purposes or for categorization or research, whether proteinuria adds anything to the equation.
And, then the second question is, “How do you resolve the issue of disagreement?” So, the example is protein:creatinine ratio allows for a more rapid diagnosis of significant proteinuria. If that patient doesn’t have to deliver immediately and a 24-hour urine sample is obtained, which do you believe if you have a protein:creatinine ratio greater than 0.3, but now your 24-hour urine is 212 mg/dL? And, I don’t have the answer to that, but that’s another area of confusion.
Dr. Norwitz: And, I think that confusion will persist. I don’t think this document is going to resolve it.
New terminology: Preeclampsia with or without severe features
Dr. Norwitz: I do like the difference in terminology between preeclampsia with severe features and preeclampsia without severe features. I think the old terminology of severe and mild preeclampsia was somewhat confusing. I certainly appreciate that alteration in terminology, although it may take a while for it to catch on. I’m still seeing the term “mild preeclampsia” used quite widely.
Use of magnesium sulfate for seizure prophylaxis
Dr. Norwitz: You did raise the issue of magnesium sulfate for seizure prophylaxis in the setting of severe preeclampsia without severe features. And I was struck by the statement. Not only is it not necessary to give it, but in the Executive Summary, as you suggest, it is not indicated and you recommended against starting it. Is that how you interpret it as the well?
Dr. Repke: Well, I might have interpreted the statement the way I wanted to interpret it. And, as you know, in our institution, because we feel we are a teaching program, people can progress very quickly intrapartum from not having severe features to having severe features, and we don’t want to miss that window of opportunity. Our practice in that regard does not follow the guidelines. We use intrapartum magnesium prophylaxis for all patients with the diagnosis of preeclampsia, and continue it for 24 hours postpartum.
Dr. Norwitz: And I would have to say we decided do the same. So, once a diagnosis of preeclampsia is made, we would give intrapartum, and then postpartum magnesium seizure prophylaxis for 24 hours, regardless of whether there’s evidence of severe features or no severe features.
Dr. Repke: And there again, I think it’s why, for you and I, it will still be important to assess the proteinuria because that diagnostic difference between preeclampsia and gestational hypertension is going to alter management. But if you follow the document word for word, if you’re not going to use magnesium without severe features, I’m not really sure what proteinuria adds. I guess, at the end of the day, you’ve got to be a good doctor. And, you’ve got to be physically assessing your patient on a very regular basis.
Preventing the first cesarean delivery. Will cesarean rates decline?
Dr. Repke: So, speaking of guidelines, the Society for Maternal Fetal Medicine (SMFM) just came out with a document trying to address this issue of the cesarean-section rate in the United States and are there things that we can be doing to lower the primary C-section rate.2 My feeling is probably disseminated from the recognition that vaginal birth after C-section never got to the levels of acceptance that anybody hoped back when Healthy People 2010 was first written. And, we could eliminate that issue or, at least significantly reduce that issue, if the first C-section never took place.
And, I guess I’d like some of your thoughts about some of the things in that document, some of the things we need to be reconsidering in terms of how we define labor and so on.
Dr. Norwitz: It is true, I think, that there’s been an epidemic of cesarean deliveries in the last decade in the US, but also throughout the world, I think, even in countries that have traditionally had very low cesarean delivery rates, the classic one being Ireland and the UK countries. Their rates are now increasing significantly.
And there are a number of different reasons as to why this may be. I think, certainly the obesity epidemic has contributed to this. You want to deliver patients who have an elevated BMI prior to the postterm period. But, it’s often difficult to monitor these patients, and the cesarean-delivery rate overall is much higher in that population. So, that might be one reason why cesarean-delivery rates overall are going up. But, certainly there are many others.
Dr. Repke: Yes, I think you’re absolutely right: the demographics of change. Childbearing is being delayed. We know that uterine contractility dynamics alter with advanced maternal age. We’ve got a higher incidence of multiple gestations with advanced maternal age. We have more patients that require induction because of supervening medical complications of pregnancy, whether that be Class A2 gestational diabetes, or whether that be pregnancy-induced hypertension.
Redefining the stages of labor
Dr. Repke: I think some of the intriguing data, to me, is a willingness to re-look at how we define the stages of labor. And what are acceptable norms? And, while I have some concerns about how that may be interpreted in the rank and file, I think it’s at least heightened the awareness of my faculty that we just can’t tolerate the C-section at 4 cm, or whether the latent phase of labor should be allowed to go to 6 cm. I don’t think we really have the data for that. But I’d be happy if I could just start to see a reduction in “failure to progress at 4 cm.”
And then the issue of second stage, I think, is also important. What do you think about the guidelines’ recommendation that there may not really be an upper limit of allowability for second-stage labors?
Dr. Norwitz: Well, certainly I think it’s important to think back to the historical context of where the labor curves developed. The original labor curves were actually developed in Zimbabwe (at that time it was Rhodesia) by an obstetrician working in the community called Philpott. And he was trying to determine when it was appropriate to send patients into the tertiary care center. So he designed the labor curve and said if patients failed to progress over a certain number of hours, those are patients that are likely to need an operative delivery, and he would then send them into the tertiary care center.
And, then Dr. Freidman picked up on that idea and developed the Freidman Curve in Boston. But that was an era, again, many years ago when the population demographics were very different, when not many patients received regional anesthesia. I think if you look at the current guidelines, there is a huge discrepancy between women who get epidural anesthesia and those that don’t in terms of the progress of labor, both the first stage and the second stage.
Is it anesthesia?
Dr. Repke: One of the things that, you know, I haven’t looked at this paper in a long time, but you remember at Brigham and Women’s Hospital, probably 20 years ago, we were winding down the Active Management of Labor Study3 that was designed to try to replicate what had gone on at the Dublin Maternity Hospital,4 and if I’m remembering correctly, one of the remarkable things about that is that in Dublin, there were virtually no C-sections in the second stage. And so people assumed that while they were more aggressive with forceps, the operative vaginal delivery rate was no different between Brigham and Women’s Hospital and the Dublin Maternity Hospital. And so there needed to be another explanation.
And, I know I’m going to incur some of the ire of our anesthesia colleagues, but I really wonder whether there is a contribution of regional anesthesia to some of the labor dystocias that we see, and whether that’s a new demographic that we haven’t really adequately assessed. Even though I recognize some of the anesthesia literature5 seems to suggest very strongly that it has no effect. You know, if you were to plot a graph of regional anesthesia rates and cesarean section rates, they would probably parallel each other.
Dr. Norwitz: I think they do. I think we’ve long known that epidural anesthesia slows down the second stage of labor. These analyses suggest that it also has a significant effect on the first stage. And, I think that needs to be taken into account.
The lost skill of forceps delivery
Dr. Norwitz: I personally think that the skill set, in terms of operative vaginal delivery with forceps and vacuum, has really been lost. And I do feel that’s one of the factors contributing to the increase in cesarean delivery rates. I certainly see that in my practice: that I’m comfortable doing rotational forceps and mid-cavity forceps deliveries, where many of my colleagues have lost that skill, and rely now on the vacuum, which in certain circumstances is a less-than-ideal instrument. So, I believe that’s part of the reason why the cesarean delivery rates have gone up.
Lengthy second stage
Dr. Norwitz: But, certainly, I think, epidural anesthesia has made a difference, and I think we need to be cognizant of the fact that there is no “hard stop” now, in terms of the length of the second stage. If you get to 3 hours, even 4 hours, I would say, and there’s continued descent with pushing and fetal heart-rate tracing is reassuring, it’s reasonable to continue beyond those cutoffs.
Dr. Repke: I agree. I also have a concern about that, and I’m going to use a little bit of a parallel example of, you know, 7 or 8 years ago, there was a big push, and I think it was an appropriate push, to try to avoid elective deliveries prior to 39 weeks.6,7 What ended up happening was that people forgot about the term “elective,” and all they heard was 39 weeks. And what we would see on Board Examinations was, “Why do you have this placenta previa delivering at 39 weeks?”
“Well, that’s our hospital policy. We can’t deliver before 39 weeks.”
And, I think, the complications started to arise, and that’s what led to SMFM and ACOG coming out with guidelines for when it is acceptable to deliver prior to 39 weeks.2,6–8
So, the analogy is: I’m afraid that people are only going to see there is no upper limit for latent phase, there is no upper limit for second stage; that clinical judgment may not get its due in making these decisions. And we’ve all been in situations where, when you are trying to extract the head out of the pelvis, a cesarean section after a 5- or 6-hour second stage has its own set of complications. So my concern is that I hope we will recognize that we have to still use some clinical judgment, what I term the so-called “art of obstetrics,” into managing these patients.
Are you optimistic that we’re going to the lower C-section rate?
Dr. Norwitz: No, I think, it’s going to continue to go up. I think, with the increasing number of multiple pregnancies, obesity, maternal age getting further and further along, I think this is only going to continue to rise. And to be honest, I don’t know the correct cesarean delivery rate, or even if that is the metric that we should be measuring.
What is the right metric to measure neonatal outcome?
Dr. Norwitz: Maybe we should be looking at perinatal outcome. If perinatal outcome is improved, then maybe the cesarean rate is less important. Obviously, the first cesarean does have implications for subsequent pregnancy outcomes, and if we do continue to see this rise in cesarean deliveries, we are going to end up with many more placental accretas and hemorrhages in women in years to come.
So, careful counseling is important. If patients plan to have one or two kids only, maybe a cesarean delivery is very reasonable. If they are planning on having six or seven kids, then maybe you have to have a more careful discussion.
Dr. Repke: Yes, I think, that’s a very good point: the number of cesareans and the potential risks for abnormal placentation. I think societal expectations have changed in terms of what they want. Most mothers are willing to sacrifice maternal risk for presumed benefits to the fetus.
I think, where we’ve gotten into trouble as a specialty, though, is that we’ve had a hard time proving that neonatal outcome, in fact, has improved—despite an almost tripling of the cesarean section rate since, probably, the early 1970s. Although, anecdotally, what my pediatric and neonatal colleagues will tell me is they don’t get the kind of damaged babies they used to get. So the neonatologists that are closer to my age that have been doing this for a long time, they’re not seeing the really severe meconium aspiration syndromes; they’re not seeing really severe forceps-related injuries, or vacuum-related injuries that they used to see. So, those may be data that we’re going to need to accumulate with a little bit more rigor, and see if that’s true.
But I tend to agree with you. I don’t know what the right cesarean section rate is. I often tell people, I have yet to meet a patient who doesn’t think her cesarean section was indicated. And that’s where I think we hit the crossroads of individual patient-care management. So, we know across all other disciplines in medicine we’re entering the era of personalized medicine, yet we want to make broad public health policy that may not apply to individuals, and run with that. So, that’s also a concern. But, as they say, a story we will follow with interest.
Dr. Norwitz: I think so. I think the other part of that equation is the stillbirth rate, and the fact that there’s a push now to avoid elective inductions before 39 weeks, which I think is very reasonable, with a focus there again on elective inductions.
There’s also a push to induce patients before 42 weeks. And that bar has been pushed back, and in most practices around the country now, deliveries are being affected and recommended at 41 weeks. And clearly, if you take a nulliparous patient with an unfavorable cervix and induce at 41 weeks, you are going to increase the cesarean rate. I would argue that you are also decreasing the chance that there will be a stillbirth. But that data has not been forthcoming.
So this issue is by no means resolved. I think there are going to be many more years of data and studies and consensus opinions before we have a much better sense of what the right cesarean
rate is.
Dr. Repke: Yes, I think that’s a great point. And, one thing that I think people aren’t maybe that familiar with is when this push came, and again, it is an appropriate push to minimize elective deliveries before 39 weeks. When they looked at neonatal outcomes, all they looked at were the group that delivered at 37 weeks, and the group that delivered at 39 weeks. And they didn’t look at what happened with the other ones.9
So, they did look at the stillbirths of fetal distress or the other complications that happened between 37 and 1, and 38 and 6. They just looked at neonates that were born at 37 weeks and compared them to neonates that were born at 39 weeks, and found reduced instances of things like transient tachypnea of the newborn, hyperbilirubinemia, and thermoregulation issues, and those sorts of things. But, never looked at the neonates in that window, so no question 39 is better than 37, but, 37 is better than not making it to 39. So that, as you said, we’ve got a lot more information we’ve got to gather.
Errol, good talking with you.
Dr. Norwitz: Thank you.
This peer to peer discussion focuses on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines1 and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.2
In this 20-minute audiocast, listen to these experts discuss:
Changing diagnostic tools for preeclampsia
- The 24-hour urinary protein estimation: When is it necessary?
- Use of magnesium sulfate for seizure prophylaxis
Preventing the first cesarean delivery
- Redefining the stages of labor: When is the second-stage too long?
- The lost skill of forceps delivery
- Is cesarean delivery rate the optimal metric for measuring neonatal outcome?
John T. Repke, MD, is University Professor and Chairman of the Department of Obstetrics and Gynecology at Penn State University College of Medicine, and Obstetrician-Gynecologist-in-Chief at the Milton S. Hershey Medical Center in Hershey, Pennsylvania. Dr. Repke is a member of the Board of Editors of OBG Management and is author of the June 2014 Guest Editorial on hypertension and pregnancy.
Errol R. Norwitz, MD, PhD, is the Louis E. Phaneuf Professor and Chairman of the Department of Obstetrics and Gynecology at Tufts Medical Center and Tufts University School of Medicine in Boston, Massachusetts. Dr. Norwitz is a member of the Board of Editors of OBG Management and is author of the June 2014 Update on operative vaginal delivery.
The speakers report no financial relationships relevant to this audiocast.
Click here for a downloadable transcript
TRANSCRIPT
ACOG guidelines on hypertension and pregnancy raise some questions
John T. Repke, MD: So, Errol, I was impressed over the first couple of days of being at the meeting. As you know, we had a postgraduate course, and one of the items that we talked about was the new hypertension and pregnancy document that was released by the Task Force on Hypertension and Pregnancy1 charged by the American College of Obstetricians and Gynecologists. I’ve got to say that while the goal of the document was to provide some standardization and clarification, there still seems to be a lot of confusion in my audience about how to interpret some of the guidelines. Have you found that?
Errol R. Norwitz, MD, PhD: Yes, I have. I found it interesting that it was put out as an executive summary, and not as a practice bulletin, which will probably follow in months. That document, which came out in November 2013, helped to address many of the issues we’ve had over the years of preeclampsia, in terms of its definition and some of the management issues. But, it also raised a number of questions that still need to be resolved.
Dr. Repke: Yes. I think one of the things to keep in mind, and I’ve tabulated all of the recommendations, is that about 60 recommendations came out of that document and only six of the 60 were accompanied by a strong quality of evidence, or rather, a high quality of evidence, and a strong recommendation. And a lot of those things were addressing issues that I think most practitioners already did, in so far as using antenatal steroids for maturation; using magnesium sulfate for patients with preeclampsia with severe features; and using magnesium sulfate as a treatment of eclampsia. But a lot of the other recommendations really were based on either moderate- or low-quality evidence, and had qualified recommendations. And, I think that’s what has led to some of the confusion.
Changing diagnostic tools for preeclampsia
Dr. Repke: What sort of specific things are your practitioners asking you about as far as, “Is this gestational hypertension or is this preeclampsia?” The guidelines say proteinuria is not required anymore. How are you dealing with that?
Should we still do the 24-hour urinary protein estimation?
Dr. Norwitz: The biggest change, in my mind, is the statement that you no longer require significant proteinuria to make the diagnosis of preeclampsia, and, indeed, of severe preeclampsia. So, if you do have significant proteinuria, then that would confirm the diagnosis. But, you can also have preeclampsia in the presence of other endorgan injuries, such as kidney injury and liver injury in the absence of significant proteinuria.
So, one of the questions that comes up is, “Should we actually do the 24-hour urinary protein estimation?”
And, my answer is, “yes.” If you have significant proteinuria, then that would confirm the diagnosis. If you don’t, you can still make the diagnosis in the setting of low platelets, elevated liver enzymes, or abnormal renal function. So, the issue is, and I’d be curious to hear your answer, if you have someone with platelets of, let’s say, 78, a new onset of sustained elevation of blood pressure, would you do the 24-hour urine estimation or just defer it?
Dr. Repke: We wouldn’t perform the 24-hour urine test under those circumstances. And, we would consider that nuance of hypertension with a severe feature that is now preeclampsia with severe feature, and the management would be based on gestational age. With a platelet count that low, the management would be stabilization and delivery. Although, if stabilized, I think that’s the type of patient that potentially could have delivery delayed until you could get an effective antenatal steroid if she was less that 34 weeks’ gestation.
Dr. Norwitz: So, that’s one issue I think needs to be clarified. If there’s other evidence of endorgan damage, then you can defer the 24-hour urinary protein. That’s another question that comes up. I’m pleased they could resolve the issue of repeated 24-hour urinary estimations. Once you have your 300 mg suggestive of the diagnosis of preeclampsia, there’s no reason to then repeat it looking for elevation and increased leakage of protein into the urine, because it doesn’t correlate with adverse outcome for the mother or fetus. So, that issue was clarified.
Dr. Repke: I think that two questions that came up in our course, and I think they were very legitimate, are, “Do we even need to do urine protein at all?” Because if you look at the guidelines for management, the only difference between preeclampsia management without severe features and gestational hypertension is frequency of antenatal testing until you decide to begin delivery. Now, in the old days, one would say, “Well, another difference would be that the preeclamptic would get magnesium sulfate.” But the current Hypertension in Pregnancy Guidelines1 suggest that preeclampsia without severe features doesn’t necessarily have to be managed with magnesium sulfate. So, I’m still wrestling with whether, other than the fact that it might be for study purposes or for categorization or research, whether proteinuria adds anything to the equation.
And, then the second question is, “How do you resolve the issue of disagreement?” So, the example is protein:creatinine ratio allows for a more rapid diagnosis of significant proteinuria. If that patient doesn’t have to deliver immediately and a 24-hour urine sample is obtained, which do you believe if you have a protein:creatinine ratio greater than 0.3, but now your 24-hour urine is 212 mg/dL? And, I don’t have the answer to that, but that’s another area of confusion.
Dr. Norwitz: And, I think that confusion will persist. I don’t think this document is going to resolve it.
New terminology: Preeclampsia with or without severe features
Dr. Norwitz: I do like the difference in terminology between preeclampsia with severe features and preeclampsia without severe features. I think the old terminology of severe and mild preeclampsia was somewhat confusing. I certainly appreciate that alteration in terminology, although it may take a while for it to catch on. I’m still seeing the term “mild preeclampsia” used quite widely.
Use of magnesium sulfate for seizure prophylaxis
Dr. Norwitz: You did raise the issue of magnesium sulfate for seizure prophylaxis in the setting of severe preeclampsia without severe features. And I was struck by the statement. Not only is it not necessary to give it, but in the Executive Summary, as you suggest, it is not indicated and you recommended against starting it. Is that how you interpret it as the well?
Dr. Repke: Well, I might have interpreted the statement the way I wanted to interpret it. And, as you know, in our institution, because we feel we are a teaching program, people can progress very quickly intrapartum from not having severe features to having severe features, and we don’t want to miss that window of opportunity. Our practice in that regard does not follow the guidelines. We use intrapartum magnesium prophylaxis for all patients with the diagnosis of preeclampsia, and continue it for 24 hours postpartum.
Dr. Norwitz: And I would have to say we decided do the same. So, once a diagnosis of preeclampsia is made, we would give intrapartum, and then postpartum magnesium seizure prophylaxis for 24 hours, regardless of whether there’s evidence of severe features or no severe features.
Dr. Repke: And there again, I think it’s why, for you and I, it will still be important to assess the proteinuria because that diagnostic difference between preeclampsia and gestational hypertension is going to alter management. But if you follow the document word for word, if you’re not going to use magnesium without severe features, I’m not really sure what proteinuria adds. I guess, at the end of the day, you’ve got to be a good doctor. And, you’ve got to be physically assessing your patient on a very regular basis.
Preventing the first cesarean delivery. Will cesarean rates decline?
Dr. Repke: So, speaking of guidelines, the Society for Maternal Fetal Medicine (SMFM) just came out with a document trying to address this issue of the cesarean-section rate in the United States and are there things that we can be doing to lower the primary C-section rate.2 My feeling is probably disseminated from the recognition that vaginal birth after C-section never got to the levels of acceptance that anybody hoped back when Healthy People 2010 was first written. And, we could eliminate that issue or, at least significantly reduce that issue, if the first C-section never took place.
And, I guess I’d like some of your thoughts about some of the things in that document, some of the things we need to be reconsidering in terms of how we define labor and so on.
Dr. Norwitz: It is true, I think, that there’s been an epidemic of cesarean deliveries in the last decade in the US, but also throughout the world, I think, even in countries that have traditionally had very low cesarean delivery rates, the classic one being Ireland and the UK countries. Their rates are now increasing significantly.
And there are a number of different reasons as to why this may be. I think, certainly the obesity epidemic has contributed to this. You want to deliver patients who have an elevated BMI prior to the postterm period. But, it’s often difficult to monitor these patients, and the cesarean-delivery rate overall is much higher in that population. So, that might be one reason why cesarean-delivery rates overall are going up. But, certainly there are many others.
Dr. Repke: Yes, I think you’re absolutely right: the demographics of change. Childbearing is being delayed. We know that uterine contractility dynamics alter with advanced maternal age. We’ve got a higher incidence of multiple gestations with advanced maternal age. We have more patients that require induction because of supervening medical complications of pregnancy, whether that be Class A2 gestational diabetes, or whether that be pregnancy-induced hypertension.
Redefining the stages of labor
Dr. Repke: I think some of the intriguing data, to me, is a willingness to re-look at how we define the stages of labor. And what are acceptable norms? And, while I have some concerns about how that may be interpreted in the rank and file, I think it’s at least heightened the awareness of my faculty that we just can’t tolerate the C-section at 4 cm, or whether the latent phase of labor should be allowed to go to 6 cm. I don’t think we really have the data for that. But I’d be happy if I could just start to see a reduction in “failure to progress at 4 cm.”
And then the issue of second stage, I think, is also important. What do you think about the guidelines’ recommendation that there may not really be an upper limit of allowability for second-stage labors?
Dr. Norwitz: Well, certainly I think it’s important to think back to the historical context of where the labor curves developed. The original labor curves were actually developed in Zimbabwe (at that time it was Rhodesia) by an obstetrician working in the community called Philpott. And he was trying to determine when it was appropriate to send patients into the tertiary care center. So he designed the labor curve and said if patients failed to progress over a certain number of hours, those are patients that are likely to need an operative delivery, and he would then send them into the tertiary care center.
And, then Dr. Freidman picked up on that idea and developed the Freidman Curve in Boston. But that was an era, again, many years ago when the population demographics were very different, when not many patients received regional anesthesia. I think if you look at the current guidelines, there is a huge discrepancy between women who get epidural anesthesia and those that don’t in terms of the progress of labor, both the first stage and the second stage.
Is it anesthesia?
Dr. Repke: One of the things that, you know, I haven’t looked at this paper in a long time, but you remember at Brigham and Women’s Hospital, probably 20 years ago, we were winding down the Active Management of Labor Study3 that was designed to try to replicate what had gone on at the Dublin Maternity Hospital,4 and if I’m remembering correctly, one of the remarkable things about that is that in Dublin, there were virtually no C-sections in the second stage. And so people assumed that while they were more aggressive with forceps, the operative vaginal delivery rate was no different between Brigham and Women’s Hospital and the Dublin Maternity Hospital. And so there needed to be another explanation.
And, I know I’m going to incur some of the ire of our anesthesia colleagues, but I really wonder whether there is a contribution of regional anesthesia to some of the labor dystocias that we see, and whether that’s a new demographic that we haven’t really adequately assessed. Even though I recognize some of the anesthesia literature5 seems to suggest very strongly that it has no effect. You know, if you were to plot a graph of regional anesthesia rates and cesarean section rates, they would probably parallel each other.
Dr. Norwitz: I think they do. I think we’ve long known that epidural anesthesia slows down the second stage of labor. These analyses suggest that it also has a significant effect on the first stage. And, I think that needs to be taken into account.
The lost skill of forceps delivery
Dr. Norwitz: I personally think that the skill set, in terms of operative vaginal delivery with forceps and vacuum, has really been lost. And I do feel that’s one of the factors contributing to the increase in cesarean delivery rates. I certainly see that in my practice: that I’m comfortable doing rotational forceps and mid-cavity forceps deliveries, where many of my colleagues have lost that skill, and rely now on the vacuum, which in certain circumstances is a less-than-ideal instrument. So, I believe that’s part of the reason why the cesarean delivery rates have gone up.
Lengthy second stage
Dr. Norwitz: But, certainly, I think, epidural anesthesia has made a difference, and I think we need to be cognizant of the fact that there is no “hard stop” now, in terms of the length of the second stage. If you get to 3 hours, even 4 hours, I would say, and there’s continued descent with pushing and fetal heart-rate tracing is reassuring, it’s reasonable to continue beyond those cutoffs.
Dr. Repke: I agree. I also have a concern about that, and I’m going to use a little bit of a parallel example of, you know, 7 or 8 years ago, there was a big push, and I think it was an appropriate push, to try to avoid elective deliveries prior to 39 weeks.6,7 What ended up happening was that people forgot about the term “elective,” and all they heard was 39 weeks. And what we would see on Board Examinations was, “Why do you have this placenta previa delivering at 39 weeks?”
“Well, that’s our hospital policy. We can’t deliver before 39 weeks.”
And, I think, the complications started to arise, and that’s what led to SMFM and ACOG coming out with guidelines for when it is acceptable to deliver prior to 39 weeks.2,6–8
So, the analogy is: I’m afraid that people are only going to see there is no upper limit for latent phase, there is no upper limit for second stage; that clinical judgment may not get its due in making these decisions. And we’ve all been in situations where, when you are trying to extract the head out of the pelvis, a cesarean section after a 5- or 6-hour second stage has its own set of complications. So my concern is that I hope we will recognize that we have to still use some clinical judgment, what I term the so-called “art of obstetrics,” into managing these patients.
Are you optimistic that we’re going to the lower C-section rate?
Dr. Norwitz: No, I think, it’s going to continue to go up. I think, with the increasing number of multiple pregnancies, obesity, maternal age getting further and further along, I think this is only going to continue to rise. And to be honest, I don’t know the correct cesarean delivery rate, or even if that is the metric that we should be measuring.
What is the right metric to measure neonatal outcome?
Dr. Norwitz: Maybe we should be looking at perinatal outcome. If perinatal outcome is improved, then maybe the cesarean rate is less important. Obviously, the first cesarean does have implications for subsequent pregnancy outcomes, and if we do continue to see this rise in cesarean deliveries, we are going to end up with many more placental accretas and hemorrhages in women in years to come.
So, careful counseling is important. If patients plan to have one or two kids only, maybe a cesarean delivery is very reasonable. If they are planning on having six or seven kids, then maybe you have to have a more careful discussion.
Dr. Repke: Yes, I think, that’s a very good point: the number of cesareans and the potential risks for abnormal placentation. I think societal expectations have changed in terms of what they want. Most mothers are willing to sacrifice maternal risk for presumed benefits to the fetus.
I think, where we’ve gotten into trouble as a specialty, though, is that we’ve had a hard time proving that neonatal outcome, in fact, has improved—despite an almost tripling of the cesarean section rate since, probably, the early 1970s. Although, anecdotally, what my pediatric and neonatal colleagues will tell me is they don’t get the kind of damaged babies they used to get. So the neonatologists that are closer to my age that have been doing this for a long time, they’re not seeing the really severe meconium aspiration syndromes; they’re not seeing really severe forceps-related injuries, or vacuum-related injuries that they used to see. So, those may be data that we’re going to need to accumulate with a little bit more rigor, and see if that’s true.
But I tend to agree with you. I don’t know what the right cesarean section rate is. I often tell people, I have yet to meet a patient who doesn’t think her cesarean section was indicated. And that’s where I think we hit the crossroads of individual patient-care management. So, we know across all other disciplines in medicine we’re entering the era of personalized medicine, yet we want to make broad public health policy that may not apply to individuals, and run with that. So, that’s also a concern. But, as they say, a story we will follow with interest.
Dr. Norwitz: I think so. I think the other part of that equation is the stillbirth rate, and the fact that there’s a push now to avoid elective inductions before 39 weeks, which I think is very reasonable, with a focus there again on elective inductions.
There’s also a push to induce patients before 42 weeks. And that bar has been pushed back, and in most practices around the country now, deliveries are being affected and recommended at 41 weeks. And clearly, if you take a nulliparous patient with an unfavorable cervix and induce at 41 weeks, you are going to increase the cesarean rate. I would argue that you are also decreasing the chance that there will be a stillbirth. But that data has not been forthcoming.
So this issue is by no means resolved. I think there are going to be many more years of data and studies and consensus opinions before we have a much better sense of what the right cesarean
rate is.
Dr. Repke: Yes, I think that’s a great point. And, one thing that I think people aren’t maybe that familiar with is when this push came, and again, it is an appropriate push to minimize elective deliveries before 39 weeks. When they looked at neonatal outcomes, all they looked at were the group that delivered at 37 weeks, and the group that delivered at 39 weeks. And they didn’t look at what happened with the other ones.9
So, they did look at the stillbirths of fetal distress or the other complications that happened between 37 and 1, and 38 and 6. They just looked at neonates that were born at 37 weeks and compared them to neonates that were born at 39 weeks, and found reduced instances of things like transient tachypnea of the newborn, hyperbilirubinemia, and thermoregulation issues, and those sorts of things. But, never looked at the neonates in that window, so no question 39 is better than 37, but, 37 is better than not making it to 39. So that, as you said, we’ve got a lot more information we’ve got to gather.
Errol, good talking with you.
Dr. Norwitz: Thank you.
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus: Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Frigoletto FD, Lieberman E, Lang J, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333(12):745–750.
- O’Driscoll K, Meagher D, Boylan P. Active Management of Labor. 3rd ed. London: Mosby- Yearbook; 1993.
- Chestnut DH, McGrath JM, Vincent RD, et al. Does early administration of epidural analgesia effect obstetric outcome in nulliparous women who are in spontaneous labor? Anesthesiology. 1994;80(6):1201–1208.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 560: Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915.
- Spong CY, Mercer BM, D’Alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):323–333.
- Tita ATN, Landon MB, Spong CY, et al; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat Cesarean Delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
- American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–1131.
- Caughey AB, Cahill AG, Guise JM, Rouse DJ; American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus: Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–193.
- Frigoletto FD, Lieberman E, Lang J, et al. A clinical trial of active management of labor. N Engl J Med. 1995;333(12):745–750.
- O’Driscoll K, Meagher D, Boylan P. Active Management of Labor. 3rd ed. London: Mosby- Yearbook; 1993.
- Chestnut DH, McGrath JM, Vincent RD, et al. Does early administration of epidural analgesia effect obstetric outcome in nulliparous women who are in spontaneous labor? Anesthesiology. 1994;80(6):1201–1208.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 560: Medically indicated late-preterm and early-term deliveries. Obstet Gynecol. 2013;121(4):908–910.
- American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 561: Nonmedically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915.
- Spong CY, Mercer BM, D’Alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):323–333.
- Tita ATN, Landon MB, Spong CY, et al; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat Cesarean Delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120.
2014 Update on operative vaginal delivery
The past year has seen the publication of four studies with relevance for clinicians:
- a retrospective cohort study that examined the maternal risks of operative vaginal delivery using forceps, vacuum extraction (FIGURE 1), or a combination of forceps and vacuum
- a prospective cohort study that investigated the efficacy and safety of three different techniques for midcavity rotational delivery in the setting of transverse arrest, namely manual rotation, vacuum rotation, and rotational forceps
- another retrospective cohort study that compared maternal morbidity among operative vaginal deliveries performed by midwives and physician providers in the United Kingdom
- a description of a new technique for instrumental vaginal delivery that is low-cost, simple, and easy to perform.
FIGURE 1. In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery when nonreassuring fetal
testing is noted during the second stage of labor.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery
John T. Repke, MD, author of the June Guest Editorial titled "Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a 're-run' or as a 'new series'?" recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
DO NOT SWITCH INSTRUMENTS
Fong A, Wu E, Pan D, Chung HJ, Ogunyemi DA. Temporal trends and morbidities of vacuum, forceps, and combined use of both [published online ahead of print April 9, 2014]. J Matern Fetal Neonatal Med. doi:10.3109/14767058.2014.904282.
In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery in the setting of nonreassuring fetal testing (“fetal distress”) in the second stage of labor. It takes just a few minutes to perform and can avert a frantic dash to the operating room for an emergent cesarean delivery. What to do then in a situation where the vacuum extractor keeps popping off, the vertex is at +3/+5 station, and the fetal heart rate has been at 80 bpm for 8 minutes? It is extremely tempting to discard the ventouse and grab the forceps. But would that be the right decision?
Related article: Is the rate of progress the same for induced and spontaneous labors? William F. Rayburn, MD, MBA (Examining the Evidence; November 2012)
Details of the study
Earlier studies suggested that the combination of vacuum and forceps is associated with an increased risk of fetal injury. Whether this is also true of injury to the mother was not known. To address this issue, Fong and colleagues performed a retrospective cohort study of all successful operative vaginal deliveries identified using ICD-9 procedure codes in the California Health Discharge Dataset from 2001 through 2007. Maternal outcomes were compared between the 202,439 fetuses delivered by vacuum extraction (reference group), 13,555 fetuses delivered by forceps, and 710 fetuses delivered using a combination of the two methods.
Using multivariate analysis modeling, Fong and colleagues demonstrated that, when compared with the vacuum alone, the combined use of vacuum and forceps was associated with significantly higher odds of:
- third- and fourth-degree perineal lacerations (adjusted odds ratio [aOR], 2.86; 95% confidence interval [CI], 2.43–3.36)
- postpartum hemorrhage (aOR, 1.81; 95% CI, 1.33–2.46)
- operative delivery failure (aOR, 2.81; 95% CI, 2.27–3.48).
Related articles:
• Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. Robert L. Barbieri, MD (Editorial; August 2013)
• Postpartum hemorrhage: 11 critical questions, answered by an expert. Q&A with Haywood L. Brown, MD (January 2011)
Fortunately, combined vacuum/forceps deliveries are uncommon, comprising only 0.33% of operative deliveries in this cohort.
Despite the large dataset used, the study was underpowered to examine the effect of combined vacuum/forceps on the incidence of rare events, such as pelvic hematoma, cervical laceration, thromboembolism, and maternal death.
What this EVIDENCE means for practice
The message is clear: Avoid combined vacuum/forceps deliveries. Choose your initial instrument with care because a failed operative vaginal delivery means a cesarean. You don’t get to choose again. The American College of Obstetricians and Gynecologists also recommends against using multiple instruments “unless there is a compelling and justifiable reason.”1
LEARN TO PERFORM MIDCAVITY ROTATIONAL DELIVERIES
Bahl R, Van de Venne M, Macleod M, Strachan B, Murphy DJ. Maternal and neonatal morbidity in relation to the instrument used for midcavity rotational operative vaginal delivery: A prospective cohort study. BJOG. 2013;120(12):1526–1532.
Cesarean delivery during the second stage of labor used to be an uncommon event. It was said that if labor progressed adequately to achieve full cervical dilatation, a vaginal delivery should be achieved. Over the past few decades, however, the rate of cesarean delivery at full cervical dilatation has increased substantially, thereby contributing to the well-documented cesarean epidemic.
The most common indication for cesarean delivery during the second stage of labor is arrest of descent due to malposition of the fetal head, typically a transverse arrest. A number of alternatives to cesarean are available, all of which involve assisted rotation of the fetal head. Historical case series reporting increased neonatal morbidity have led to a reduction in the use of rotational forceps to facilitate this rotation. Attempted manual rotation and “rotational vacuum extraction” are now preferred, particularly by less experienced providers. Which of these three approaches is most effective is unknown.
Related article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; July 2011)
Details of the study
A prospective cohort study was carried out at two university hospitals in Scotland and England to compare maternal and neonatal morbidity associated with alternative techniques for midcavity rotational delivery. The choice of instrument was left to the provider.
Of the 381 nulliparous women who had an attempted midcavity rotational operative vaginal delivery, 163 (42.8%) underwent manual rotation followed by nonrotational forceps delivery, 73 (19.1%) had a rotational vacuum delivery, and 145 (38.1%) delivered with the assistance of rotational (Kielland) forceps.
Regardless of the instrument used, successful rotation and vaginal delivery were achieved in more than 90% of cases, with a cesarean rate of 4.2%, 6.8%, and 9.6% for manual rotation, vacuum, and rotational forceps, respectively (aOR, 0.39; 95% CI, 0.14–1.06). There were no significant differences in maternal complications (postpartum hemorrhage, third- and fourth-degree perineal lacerations) and neonatal morbidity (low cord pH, neonatal trauma, and neonatal intensive care unit admission) between the three instruments.
What this EVIDENCE means for practice
Midcavity rotational delivery can be achieved with a high degree of success and few adverse events in women who develop transverse arrest in the second stage of labor. Maternal and perinatal outcomes are comparable with rotational forceps, vacuum extraction, and manual rotation. With appropriate training, midcavity rotational delivery can be practiced safely, including the use of Kielland forceps.
SHOULD MIDWIVES PERFORM OPERATIVE VAGINAL DELIVERIES?
Black M, Mitchell E, Danielian P. Instrumental vaginal deliveries; are midwives safer practitioners? A retrospective cohort study. Acta Obstet Gynecol Scand. 2013;92(12):1383–1387.
In the United States, instrumental vaginal deliveries are performed only by physicians. In the United Kingdom, the opportunity to perform such deliveries has recently become available to midwives as well. Because midwives have less experience in performing surgical procedures, the question has arisen as to whether their complication rate is higher than that of physicians. Alternatively, because midwives typically are more patient than physicians and more reluctant to resort to obstetric interventions, it is possible that their complication rate may be lower.
Details of the study
To address this issue, Black and colleagues performed a retrospective cohort study of consecutive women who had a successful nonrotational instrumental vaginal delivery of a liveborn singleton infant outside of the operating room between June 2005 and June 2010 at Aberdeen Maternity Hospital in the United Kingdom.
Of the 2,540 women included in the final analysis, 330 (13%) were delivered by midwives and the remaining 2,210 (87%) by physicians—1,049 (41%) by junior doctors and 1,161 (46%) by more senior doctors. All midwives had undergone formal training at the University of Bradford. There were no differences between groups in demographic characteristics (maternal age, gestational age, parity, body mass index, or birth weight) or in the indications for instrumental delivery.
Major findings were that midwives were significantly less likely than junior and senior physicians to use forceps as the instrument of choice for delivery (OR, 0.6; 95% CI, 0.4–0.7). Mean blood loss was significantly lower in the midwife group (57 mL), although it is unlikely that this finding was clinically significant. There were no differences in severe perineal injury (third- or fourth-degree perineal lacerations), arterial cord pH, or postpartum hemorrhage.
A secondary analysis comparing the outcome of operative vaginal deliveries by trained midwives with the outcome by junior physicians alone produced almost identical results.
Strengths of the study include the fact that it was conducted at a single center and had a large sample number. Weaknesses include its retrospective design and the fact that one major outcome (namely, failed operative vaginal delivery leading to cesarean) was not examined. This study was not designed or powered to examine neonatal outcomes.
What this EVIDENCE means for practice
These data demonstrate that midwives can perform operative vaginal deliveries using either forceps or vacuum with a rate of maternal morbidity equivalent to those performed by physicians.
Are these findings truly revolutionary? Although midwives do not perform cesarean deliveries, they do perform and repair episiotomies when indicated. Restricting instrumental vaginal deliveries to physicians alone may be motivated more by tradition and logistics than concerns over patient safety. Indeed, the ability of a midwife working in a remote area to perform an instrumental vaginal delivery in an emergency situation may be highly beneficial to perinatal outcome, although it should be stressed that such an approach ought to be limited to practitioners who have undergone rigorous formal training.
Other benefits of midwives performing operative vaginal deliveries may include increased autonomy for the midwifery providers, improvements in physician-midwife interactions, and enhanced continuity of care for women.
IN THE PIPELINE: THE ODÓN DEVICE FOR OPERATIVE VAGINAL DELIVERY
World Health Organization Odón Device Research Group. Feasibility and safety study of a new device (Odón device) for assisted vaginal deliveries: Study protocol. Reprod Health. 2013;10:33.
Childbirth remains a risky venture. According to the World Health Organization (WHO), approximately 2.6 million babies are stillborn and 260,000 women die in childbirth each year, with developing countries disproportionately affected. Many of these adverse events result from complications at the time of delivery. Instrumental vaginal delivery is used to shorten the second stage of labor and improve perinatal and maternal outcomes.
Operative vaginal delivery likely does reduce the rate of stillbirth and early neonatal death and lower the cesarean delivery rate, but the instruments themselves do occasionally cause maternal and fetal injury, including cephalohematoma, retinal hemorrhage, facial nerve palsy, and skull fractures. Although numerous modifications to the design of forceps and the vacuum extractor have been made over the years, no new technology has been introduced for centuries.
In 2005, Mr. Jorge Odón, a car mechanic from Argentina with no formal training in medicine or obstetrics (aside from being the father of five), came up with an idea for a novel technique to assist in delivery. He was inspired by a simple trick he used to entertain his friends. It involved removing a loose cork from the inside of an empty bottle using a plastic bag. It occurred to him one day that this same scientific principle could be used to expedite delivery of the fetal head from the birth canal, and so he built the first prototype. The device has since been named in his honor.
Description of the Odón device
The Odón device consists of a tube containing a polyethylene bag. The tube is inserted into the birth canal and the bag is deployed and inflated to create a plastic sleeve that hugs the baby’s head. The applicator tube is then discarded and traction is applied to the plastic bag to move the head (and the entire fetus) down the birth canal (FIGURE 2).
![]()
The advantages of the Odón device are that it is:
- low-cost
- simple to use
- compact, easy to transport and store
- designed to minimize trauma to the mother and fetus.
Current stage of development
The Odón device already has been piloted in the United States and South America. The WHO plans to introduce it into the obstetric armamentarium in a three-phase clinical trial outlined in the Odón Device Research Project report. The first phase is under way and involves testing the device under normal delivery conditions in tertiary hospitals in Argentina and South Africa. The next two phases will 1) assess its efficacy in women with a prolonged second stage of labor but no “fetal distress” and 2) compare its performance head-to-head against the vacuum extractor and forceps.
What this EVIDENCE means for practice
Enthusiasm for the Odón device is fueled by its simplicity and the likelihood that midlevel providers working in remote obstetric units can be trained in its use, thereby increasing access to an important modality of emergency obstetric care. This is particularly important in centers that lack immediate access to cesarean delivery capabilities. Whether the device can be used in developing countries to more effectively manage the second stage of labor and thereby reduce infectious morbidity and pelvic floor injuries has yet to be confirmed but is a testable hypothesis.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
Reference
- American College of Obstetricians and Gynecologists. ACOG practice bulletin #17: Operative vaginal delivery. Washington, DC: ACOG; 2000.
The past year has seen the publication of four studies with relevance for clinicians:
- a retrospective cohort study that examined the maternal risks of operative vaginal delivery using forceps, vacuum extraction (FIGURE 1), or a combination of forceps and vacuum
- a prospective cohort study that investigated the efficacy and safety of three different techniques for midcavity rotational delivery in the setting of transverse arrest, namely manual rotation, vacuum rotation, and rotational forceps
- another retrospective cohort study that compared maternal morbidity among operative vaginal deliveries performed by midwives and physician providers in the United Kingdom
- a description of a new technique for instrumental vaginal delivery that is low-cost, simple, and easy to perform.
FIGURE 1. In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery when nonreassuring fetal
testing is noted during the second stage of labor.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery
John T. Repke, MD, author of the June Guest Editorial titled "Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a 're-run' or as a 'new series'?" recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
DO NOT SWITCH INSTRUMENTS
Fong A, Wu E, Pan D, Chung HJ, Ogunyemi DA. Temporal trends and morbidities of vacuum, forceps, and combined use of both [published online ahead of print April 9, 2014]. J Matern Fetal Neonatal Med. doi:10.3109/14767058.2014.904282.
In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery in the setting of nonreassuring fetal testing (“fetal distress”) in the second stage of labor. It takes just a few minutes to perform and can avert a frantic dash to the operating room for an emergent cesarean delivery. What to do then in a situation where the vacuum extractor keeps popping off, the vertex is at +3/+5 station, and the fetal heart rate has been at 80 bpm for 8 minutes? It is extremely tempting to discard the ventouse and grab the forceps. But would that be the right decision?
Related article: Is the rate of progress the same for induced and spontaneous labors? William F. Rayburn, MD, MBA (Examining the Evidence; November 2012)
Details of the study
Earlier studies suggested that the combination of vacuum and forceps is associated with an increased risk of fetal injury. Whether this is also true of injury to the mother was not known. To address this issue, Fong and colleagues performed a retrospective cohort study of all successful operative vaginal deliveries identified using ICD-9 procedure codes in the California Health Discharge Dataset from 2001 through 2007. Maternal outcomes were compared between the 202,439 fetuses delivered by vacuum extraction (reference group), 13,555 fetuses delivered by forceps, and 710 fetuses delivered using a combination of the two methods.
Using multivariate analysis modeling, Fong and colleagues demonstrated that, when compared with the vacuum alone, the combined use of vacuum and forceps was associated with significantly higher odds of:
- third- and fourth-degree perineal lacerations (adjusted odds ratio [aOR], 2.86; 95% confidence interval [CI], 2.43–3.36)
- postpartum hemorrhage (aOR, 1.81; 95% CI, 1.33–2.46)
- operative delivery failure (aOR, 2.81; 95% CI, 2.27–3.48).
Related articles:
• Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. Robert L. Barbieri, MD (Editorial; August 2013)
• Postpartum hemorrhage: 11 critical questions, answered by an expert. Q&A with Haywood L. Brown, MD (January 2011)
Fortunately, combined vacuum/forceps deliveries are uncommon, comprising only 0.33% of operative deliveries in this cohort.
Despite the large dataset used, the study was underpowered to examine the effect of combined vacuum/forceps on the incidence of rare events, such as pelvic hematoma, cervical laceration, thromboembolism, and maternal death.
What this EVIDENCE means for practice
The message is clear: Avoid combined vacuum/forceps deliveries. Choose your initial instrument with care because a failed operative vaginal delivery means a cesarean. You don’t get to choose again. The American College of Obstetricians and Gynecologists also recommends against using multiple instruments “unless there is a compelling and justifiable reason.”1
LEARN TO PERFORM MIDCAVITY ROTATIONAL DELIVERIES
Bahl R, Van de Venne M, Macleod M, Strachan B, Murphy DJ. Maternal and neonatal morbidity in relation to the instrument used for midcavity rotational operative vaginal delivery: A prospective cohort study. BJOG. 2013;120(12):1526–1532.
Cesarean delivery during the second stage of labor used to be an uncommon event. It was said that if labor progressed adequately to achieve full cervical dilatation, a vaginal delivery should be achieved. Over the past few decades, however, the rate of cesarean delivery at full cervical dilatation has increased substantially, thereby contributing to the well-documented cesarean epidemic.
The most common indication for cesarean delivery during the second stage of labor is arrest of descent due to malposition of the fetal head, typically a transverse arrest. A number of alternatives to cesarean are available, all of which involve assisted rotation of the fetal head. Historical case series reporting increased neonatal morbidity have led to a reduction in the use of rotational forceps to facilitate this rotation. Attempted manual rotation and “rotational vacuum extraction” are now preferred, particularly by less experienced providers. Which of these three approaches is most effective is unknown.
Related article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; July 2011)
Details of the study
A prospective cohort study was carried out at two university hospitals in Scotland and England to compare maternal and neonatal morbidity associated with alternative techniques for midcavity rotational delivery. The choice of instrument was left to the provider.
Of the 381 nulliparous women who had an attempted midcavity rotational operative vaginal delivery, 163 (42.8%) underwent manual rotation followed by nonrotational forceps delivery, 73 (19.1%) had a rotational vacuum delivery, and 145 (38.1%) delivered with the assistance of rotational (Kielland) forceps.
Regardless of the instrument used, successful rotation and vaginal delivery were achieved in more than 90% of cases, with a cesarean rate of 4.2%, 6.8%, and 9.6% for manual rotation, vacuum, and rotational forceps, respectively (aOR, 0.39; 95% CI, 0.14–1.06). There were no significant differences in maternal complications (postpartum hemorrhage, third- and fourth-degree perineal lacerations) and neonatal morbidity (low cord pH, neonatal trauma, and neonatal intensive care unit admission) between the three instruments.
What this EVIDENCE means for practice
Midcavity rotational delivery can be achieved with a high degree of success and few adverse events in women who develop transverse arrest in the second stage of labor. Maternal and perinatal outcomes are comparable with rotational forceps, vacuum extraction, and manual rotation. With appropriate training, midcavity rotational delivery can be practiced safely, including the use of Kielland forceps.
SHOULD MIDWIVES PERFORM OPERATIVE VAGINAL DELIVERIES?
Black M, Mitchell E, Danielian P. Instrumental vaginal deliveries; are midwives safer practitioners? A retrospective cohort study. Acta Obstet Gynecol Scand. 2013;92(12):1383–1387.
In the United States, instrumental vaginal deliveries are performed only by physicians. In the United Kingdom, the opportunity to perform such deliveries has recently become available to midwives as well. Because midwives have less experience in performing surgical procedures, the question has arisen as to whether their complication rate is higher than that of physicians. Alternatively, because midwives typically are more patient than physicians and more reluctant to resort to obstetric interventions, it is possible that their complication rate may be lower.
Details of the study
To address this issue, Black and colleagues performed a retrospective cohort study of consecutive women who had a successful nonrotational instrumental vaginal delivery of a liveborn singleton infant outside of the operating room between June 2005 and June 2010 at Aberdeen Maternity Hospital in the United Kingdom.
Of the 2,540 women included in the final analysis, 330 (13%) were delivered by midwives and the remaining 2,210 (87%) by physicians—1,049 (41%) by junior doctors and 1,161 (46%) by more senior doctors. All midwives had undergone formal training at the University of Bradford. There were no differences between groups in demographic characteristics (maternal age, gestational age, parity, body mass index, or birth weight) or in the indications for instrumental delivery.
Major findings were that midwives were significantly less likely than junior and senior physicians to use forceps as the instrument of choice for delivery (OR, 0.6; 95% CI, 0.4–0.7). Mean blood loss was significantly lower in the midwife group (57 mL), although it is unlikely that this finding was clinically significant. There were no differences in severe perineal injury (third- or fourth-degree perineal lacerations), arterial cord pH, or postpartum hemorrhage.
A secondary analysis comparing the outcome of operative vaginal deliveries by trained midwives with the outcome by junior physicians alone produced almost identical results.
Strengths of the study include the fact that it was conducted at a single center and had a large sample number. Weaknesses include its retrospective design and the fact that one major outcome (namely, failed operative vaginal delivery leading to cesarean) was not examined. This study was not designed or powered to examine neonatal outcomes.
What this EVIDENCE means for practice
These data demonstrate that midwives can perform operative vaginal deliveries using either forceps or vacuum with a rate of maternal morbidity equivalent to those performed by physicians.
Are these findings truly revolutionary? Although midwives do not perform cesarean deliveries, they do perform and repair episiotomies when indicated. Restricting instrumental vaginal deliveries to physicians alone may be motivated more by tradition and logistics than concerns over patient safety. Indeed, the ability of a midwife working in a remote area to perform an instrumental vaginal delivery in an emergency situation may be highly beneficial to perinatal outcome, although it should be stressed that such an approach ought to be limited to practitioners who have undergone rigorous formal training.
Other benefits of midwives performing operative vaginal deliveries may include increased autonomy for the midwifery providers, improvements in physician-midwife interactions, and enhanced continuity of care for women.
IN THE PIPELINE: THE ODÓN DEVICE FOR OPERATIVE VAGINAL DELIVERY
World Health Organization Odón Device Research Group. Feasibility and safety study of a new device (Odón device) for assisted vaginal deliveries: Study protocol. Reprod Health. 2013;10:33.
Childbirth remains a risky venture. According to the World Health Organization (WHO), approximately 2.6 million babies are stillborn and 260,000 women die in childbirth each year, with developing countries disproportionately affected. Many of these adverse events result from complications at the time of delivery. Instrumental vaginal delivery is used to shorten the second stage of labor and improve perinatal and maternal outcomes.
Operative vaginal delivery likely does reduce the rate of stillbirth and early neonatal death and lower the cesarean delivery rate, but the instruments themselves do occasionally cause maternal and fetal injury, including cephalohematoma, retinal hemorrhage, facial nerve palsy, and skull fractures. Although numerous modifications to the design of forceps and the vacuum extractor have been made over the years, no new technology has been introduced for centuries.
In 2005, Mr. Jorge Odón, a car mechanic from Argentina with no formal training in medicine or obstetrics (aside from being the father of five), came up with an idea for a novel technique to assist in delivery. He was inspired by a simple trick he used to entertain his friends. It involved removing a loose cork from the inside of an empty bottle using a plastic bag. It occurred to him one day that this same scientific principle could be used to expedite delivery of the fetal head from the birth canal, and so he built the first prototype. The device has since been named in his honor.
Description of the Odón device
The Odón device consists of a tube containing a polyethylene bag. The tube is inserted into the birth canal and the bag is deployed and inflated to create a plastic sleeve that hugs the baby’s head. The applicator tube is then discarded and traction is applied to the plastic bag to move the head (and the entire fetus) down the birth canal (FIGURE 2).
![]()
The advantages of the Odón device are that it is:
- low-cost
- simple to use
- compact, easy to transport and store
- designed to minimize trauma to the mother and fetus.
Current stage of development
The Odón device already has been piloted in the United States and South America. The WHO plans to introduce it into the obstetric armamentarium in a three-phase clinical trial outlined in the Odón Device Research Project report. The first phase is under way and involves testing the device under normal delivery conditions in tertiary hospitals in Argentina and South Africa. The next two phases will 1) assess its efficacy in women with a prolonged second stage of labor but no “fetal distress” and 2) compare its performance head-to-head against the vacuum extractor and forceps.
What this EVIDENCE means for practice
Enthusiasm for the Odón device is fueled by its simplicity and the likelihood that midlevel providers working in remote obstetric units can be trained in its use, thereby increasing access to an important modality of emergency obstetric care. This is particularly important in centers that lack immediate access to cesarean delivery capabilities. Whether the device can be used in developing countries to more effectively manage the second stage of labor and thereby reduce infectious morbidity and pelvic floor injuries has yet to be confirmed but is a testable hypothesis.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
The past year has seen the publication of four studies with relevance for clinicians:
- a retrospective cohort study that examined the maternal risks of operative vaginal delivery using forceps, vacuum extraction (FIGURE 1), or a combination of forceps and vacuum
- a prospective cohort study that investigated the efficacy and safety of three different techniques for midcavity rotational delivery in the setting of transverse arrest, namely manual rotation, vacuum rotation, and rotational forceps
- another retrospective cohort study that compared maternal morbidity among operative vaginal deliveries performed by midwives and physician providers in the United Kingdom
- a description of a new technique for instrumental vaginal delivery that is low-cost, simple, and easy to perform.
FIGURE 1. In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery when nonreassuring fetal
testing is noted during the second stage of labor.
OBSTETRIC PRACTICE CHANGERS 2014
Hypertension and pregnancy and preventing the first cesarean delivery
John T. Repke, MD, author of the June Guest Editorial titled "Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a 're-run' or as a 'new series'?" recently sat down with Errol R. Norwitz, MD, PhD, fellow OBG Management Board of Editors Member and author of this month’s "Update on Operative Vaginal Delivery." Their discussion focused on individual takeaways from ACOG’s Hypertension in Pregnancy guidelines and the recent joint ACOG−Society of Maternal-Fetal Medicine report on emerging clinical and scientific advances in safe prevention of the primary cesarean delivery.
From their conversation:
Dr. Repke: About 60 recommendations came out of ACOG’s Hypertension in Pregnancy document; only six had high-quality supporting evidence, and I think most practitioners already did them. Many really were based on either moderate- or low-quality evidence, with qualified recommendations. I think this has led to confusion.
Dr. Norwitz, how do you answer when a clinician asks you, “Is this gestational hypertension or is this preeclampsia?”
Click here to access the audiocast with full transcript.
DO NOT SWITCH INSTRUMENTS
Fong A, Wu E, Pan D, Chung HJ, Ogunyemi DA. Temporal trends and morbidities of vacuum, forceps, and combined use of both [published online ahead of print April 9, 2014]. J Matern Fetal Neonatal Med. doi:10.3109/14767058.2014.904282.
In trained hands, operative vaginal delivery can be an extremely effective intervention to expedite delivery in the setting of nonreassuring fetal testing (“fetal distress”) in the second stage of labor. It takes just a few minutes to perform and can avert a frantic dash to the operating room for an emergent cesarean delivery. What to do then in a situation where the vacuum extractor keeps popping off, the vertex is at +3/+5 station, and the fetal heart rate has been at 80 bpm for 8 minutes? It is extremely tempting to discard the ventouse and grab the forceps. But would that be the right decision?
Related article: Is the rate of progress the same for induced and spontaneous labors? William F. Rayburn, MD, MBA (Examining the Evidence; November 2012)
Details of the study
Earlier studies suggested that the combination of vacuum and forceps is associated with an increased risk of fetal injury. Whether this is also true of injury to the mother was not known. To address this issue, Fong and colleagues performed a retrospective cohort study of all successful operative vaginal deliveries identified using ICD-9 procedure codes in the California Health Discharge Dataset from 2001 through 2007. Maternal outcomes were compared between the 202,439 fetuses delivered by vacuum extraction (reference group), 13,555 fetuses delivered by forceps, and 710 fetuses delivered using a combination of the two methods.
Using multivariate analysis modeling, Fong and colleagues demonstrated that, when compared with the vacuum alone, the combined use of vacuum and forceps was associated with significantly higher odds of:
- third- and fourth-degree perineal lacerations (adjusted odds ratio [aOR], 2.86; 95% confidence interval [CI], 2.43–3.36)
- postpartum hemorrhage (aOR, 1.81; 95% CI, 1.33–2.46)
- operative delivery failure (aOR, 2.81; 95% CI, 2.27–3.48).
Related articles:
• Develop and use a checklist for 3rd- and 4th-degree perineal lacerations. Robert L. Barbieri, MD (Editorial; August 2013)
• Postpartum hemorrhage: 11 critical questions, answered by an expert. Q&A with Haywood L. Brown, MD (January 2011)
Fortunately, combined vacuum/forceps deliveries are uncommon, comprising only 0.33% of operative deliveries in this cohort.
Despite the large dataset used, the study was underpowered to examine the effect of combined vacuum/forceps on the incidence of rare events, such as pelvic hematoma, cervical laceration, thromboembolism, and maternal death.
What this EVIDENCE means for practice
The message is clear: Avoid combined vacuum/forceps deliveries. Choose your initial instrument with care because a failed operative vaginal delivery means a cesarean. You don’t get to choose again. The American College of Obstetricians and Gynecologists also recommends against using multiple instruments “unless there is a compelling and justifiable reason.”1
LEARN TO PERFORM MIDCAVITY ROTATIONAL DELIVERIES
Bahl R, Van de Venne M, Macleod M, Strachan B, Murphy DJ. Maternal and neonatal morbidity in relation to the instrument used for midcavity rotational operative vaginal delivery: A prospective cohort study. BJOG. 2013;120(12):1526–1532.
Cesarean delivery during the second stage of labor used to be an uncommon event. It was said that if labor progressed adequately to achieve full cervical dilatation, a vaginal delivery should be achieved. Over the past few decades, however, the rate of cesarean delivery at full cervical dilatation has increased substantially, thereby contributing to the well-documented cesarean epidemic.
The most common indication for cesarean delivery during the second stage of labor is arrest of descent due to malposition of the fetal head, typically a transverse arrest. A number of alternatives to cesarean are available, all of which involve assisted rotation of the fetal head. Historical case series reporting increased neonatal morbidity have led to a reduction in the use of rotational forceps to facilitate this rotation. Attempted manual rotation and “rotational vacuum extraction” are now preferred, particularly by less experienced providers. Which of these three approaches is most effective is unknown.
Related article: You are the second responder to a shoulder dystocia emergency. What do you do first? Robert L. Barbieri, MD (Editorial; July 2011)
Details of the study
A prospective cohort study was carried out at two university hospitals in Scotland and England to compare maternal and neonatal morbidity associated with alternative techniques for midcavity rotational delivery. The choice of instrument was left to the provider.
Of the 381 nulliparous women who had an attempted midcavity rotational operative vaginal delivery, 163 (42.8%) underwent manual rotation followed by nonrotational forceps delivery, 73 (19.1%) had a rotational vacuum delivery, and 145 (38.1%) delivered with the assistance of rotational (Kielland) forceps.
Regardless of the instrument used, successful rotation and vaginal delivery were achieved in more than 90% of cases, with a cesarean rate of 4.2%, 6.8%, and 9.6% for manual rotation, vacuum, and rotational forceps, respectively (aOR, 0.39; 95% CI, 0.14–1.06). There were no significant differences in maternal complications (postpartum hemorrhage, third- and fourth-degree perineal lacerations) and neonatal morbidity (low cord pH, neonatal trauma, and neonatal intensive care unit admission) between the three instruments.
What this EVIDENCE means for practice
Midcavity rotational delivery can be achieved with a high degree of success and few adverse events in women who develop transverse arrest in the second stage of labor. Maternal and perinatal outcomes are comparable with rotational forceps, vacuum extraction, and manual rotation. With appropriate training, midcavity rotational delivery can be practiced safely, including the use of Kielland forceps.
SHOULD MIDWIVES PERFORM OPERATIVE VAGINAL DELIVERIES?
Black M, Mitchell E, Danielian P. Instrumental vaginal deliveries; are midwives safer practitioners? A retrospective cohort study. Acta Obstet Gynecol Scand. 2013;92(12):1383–1387.
In the United States, instrumental vaginal deliveries are performed only by physicians. In the United Kingdom, the opportunity to perform such deliveries has recently become available to midwives as well. Because midwives have less experience in performing surgical procedures, the question has arisen as to whether their complication rate is higher than that of physicians. Alternatively, because midwives typically are more patient than physicians and more reluctant to resort to obstetric interventions, it is possible that their complication rate may be lower.
Details of the study
To address this issue, Black and colleagues performed a retrospective cohort study of consecutive women who had a successful nonrotational instrumental vaginal delivery of a liveborn singleton infant outside of the operating room between June 2005 and June 2010 at Aberdeen Maternity Hospital in the United Kingdom.
Of the 2,540 women included in the final analysis, 330 (13%) were delivered by midwives and the remaining 2,210 (87%) by physicians—1,049 (41%) by junior doctors and 1,161 (46%) by more senior doctors. All midwives had undergone formal training at the University of Bradford. There were no differences between groups in demographic characteristics (maternal age, gestational age, parity, body mass index, or birth weight) or in the indications for instrumental delivery.
Major findings were that midwives were significantly less likely than junior and senior physicians to use forceps as the instrument of choice for delivery (OR, 0.6; 95% CI, 0.4–0.7). Mean blood loss was significantly lower in the midwife group (57 mL), although it is unlikely that this finding was clinically significant. There were no differences in severe perineal injury (third- or fourth-degree perineal lacerations), arterial cord pH, or postpartum hemorrhage.
A secondary analysis comparing the outcome of operative vaginal deliveries by trained midwives with the outcome by junior physicians alone produced almost identical results.
Strengths of the study include the fact that it was conducted at a single center and had a large sample number. Weaknesses include its retrospective design and the fact that one major outcome (namely, failed operative vaginal delivery leading to cesarean) was not examined. This study was not designed or powered to examine neonatal outcomes.
What this EVIDENCE means for practice
These data demonstrate that midwives can perform operative vaginal deliveries using either forceps or vacuum with a rate of maternal morbidity equivalent to those performed by physicians.
Are these findings truly revolutionary? Although midwives do not perform cesarean deliveries, they do perform and repair episiotomies when indicated. Restricting instrumental vaginal deliveries to physicians alone may be motivated more by tradition and logistics than concerns over patient safety. Indeed, the ability of a midwife working in a remote area to perform an instrumental vaginal delivery in an emergency situation may be highly beneficial to perinatal outcome, although it should be stressed that such an approach ought to be limited to practitioners who have undergone rigorous formal training.
Other benefits of midwives performing operative vaginal deliveries may include increased autonomy for the midwifery providers, improvements in physician-midwife interactions, and enhanced continuity of care for women.
IN THE PIPELINE: THE ODÓN DEVICE FOR OPERATIVE VAGINAL DELIVERY
World Health Organization Odón Device Research Group. Feasibility and safety study of a new device (Odón device) for assisted vaginal deliveries: Study protocol. Reprod Health. 2013;10:33.
Childbirth remains a risky venture. According to the World Health Organization (WHO), approximately 2.6 million babies are stillborn and 260,000 women die in childbirth each year, with developing countries disproportionately affected. Many of these adverse events result from complications at the time of delivery. Instrumental vaginal delivery is used to shorten the second stage of labor and improve perinatal and maternal outcomes.
Operative vaginal delivery likely does reduce the rate of stillbirth and early neonatal death and lower the cesarean delivery rate, but the instruments themselves do occasionally cause maternal and fetal injury, including cephalohematoma, retinal hemorrhage, facial nerve palsy, and skull fractures. Although numerous modifications to the design of forceps and the vacuum extractor have been made over the years, no new technology has been introduced for centuries.
In 2005, Mr. Jorge Odón, a car mechanic from Argentina with no formal training in medicine or obstetrics (aside from being the father of five), came up with an idea for a novel technique to assist in delivery. He was inspired by a simple trick he used to entertain his friends. It involved removing a loose cork from the inside of an empty bottle using a plastic bag. It occurred to him one day that this same scientific principle could be used to expedite delivery of the fetal head from the birth canal, and so he built the first prototype. The device has since been named in his honor.
Description of the Odón device
The Odón device consists of a tube containing a polyethylene bag. The tube is inserted into the birth canal and the bag is deployed and inflated to create a plastic sleeve that hugs the baby’s head. The applicator tube is then discarded and traction is applied to the plastic bag to move the head (and the entire fetus) down the birth canal (FIGURE 2).
![]()
The advantages of the Odón device are that it is:
- low-cost
- simple to use
- compact, easy to transport and store
- designed to minimize trauma to the mother and fetus.
Current stage of development
The Odón device already has been piloted in the United States and South America. The WHO plans to introduce it into the obstetric armamentarium in a three-phase clinical trial outlined in the Odón Device Research Project report. The first phase is under way and involves testing the device under normal delivery conditions in tertiary hospitals in Argentina and South Africa. The next two phases will 1) assess its efficacy in women with a prolonged second stage of labor but no “fetal distress” and 2) compare its performance head-to-head against the vacuum extractor and forceps.
What this EVIDENCE means for practice
Enthusiasm for the Odón device is fueled by its simplicity and the likelihood that midlevel providers working in remote obstetric units can be trained in its use, thereby increasing access to an important modality of emergency obstetric care. This is particularly important in centers that lack immediate access to cesarean delivery capabilities. Whether the device can be used in developing countries to more effectively manage the second stage of labor and thereby reduce infectious morbidity and pelvic floor injuries has yet to be confirmed but is a testable hypothesis.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
Reference
- American College of Obstetricians and Gynecologists. ACOG practice bulletin #17: Operative vaginal delivery. Washington, DC: ACOG; 2000.
Reference
- American College of Obstetricians and Gynecologists. ACOG practice bulletin #17: Operative vaginal delivery. Washington, DC: ACOG; 2000.
Have you read the June Guest Editorial? Click here to access Dr. John T. Repke's Low-dose aspirin and preeclampsia prevention: Ready for prime time, but as a “re-run” or as a “new series”?
Why are well-educated women more likely to choose home birth?
In this audiocast, Dr. Norwitz discusses:
- His unique training and education, including his connection as an MD, PhD, to midwifery practice
- The increased number of women delivering at home in the United States
- Why older, well-educated, married, multiparous women are more likely to deliver at home
- What structure would support safe home care delivery
Dr. Norwitz is the author of What do the latest data reveal about the safety of home birth in the United States? (Examining the Evidence, November 2013).
In this audiocast, Dr. Norwitz discusses:
- His unique training and education, including his connection as an MD, PhD, to midwifery practice
- The increased number of women delivering at home in the United States
- Why older, well-educated, married, multiparous women are more likely to deliver at home
- What structure would support safe home care delivery
Dr. Norwitz is the author of What do the latest data reveal about the safety of home birth in the United States? (Examining the Evidence, November 2013).
In this audiocast, Dr. Norwitz discusses:
- His unique training and education, including his connection as an MD, PhD, to midwifery practice
- The increased number of women delivering at home in the United States
- Why older, well-educated, married, multiparous women are more likely to deliver at home
- What structure would support safe home care delivery
Dr. Norwitz is the author of What do the latest data reveal about the safety of home birth in the United States? (Examining the Evidence, November 2013).
What do the latest data reveal about the safety of home birth in the United States?
Every morning before I leave for work, I kiss my three children goodbye and tell them, “I love you. Make good choices today.”
This has become my mantra—so much so that, on her way out the door to join her friends at the movies recently, my daughter turned to me and said, “I know, Dad. I know. I’ll make good decisions tonight.”
And what decision is more important than where to deliver your child and who to have in attendance at the birth?
It is said that the passage from the uterus to the outside world that each one of us was forced to negotiate at birth is the most treacherous journey we will ever undertake. Any unnecessary delay or complication can have profound, lifelong consequences.
There is no question that the past few centuries have seen a significant “medicalization” of childbirth, including the relocation of deliveries from the community to a hospital setting, the introduction of male obstetricians, the unfortunate marginalization of midwives and support personnel (doulas), the development of uterotonic drugs, and the evolution of operative vaginal (forceps, vacuum) and cesarean deliveries.
Many of the practices initially introduced by obstetric care providers (including multiple vaginal examinations in labor, induction of labor for a large baby, and active management of labor protocols) have since been shown to be unhelpful in improving pregnancy outcomes, and some practices (such as episiotomy) have even been shown to be harmful.
Related article: Difficult fetal extraction at cesarean delivery: What should you do? Robert L. Barbieri, MD (Editorial, January 2012)
In the midst of this confusion, the one voice that has been lost is that of the patient herself.
Whose birth is it anyway?
The American College of Obstetricians and Gynecologists (ACOG), the American Academy of Pediatrics (AAP), and the American College of Nurse-Midwives (ACNM) all agree that patient autonomy is paramount, and that the final decision of where to deliver and who to have in attendance should be made by the patient herself, ideally in conjunction with her family and her obstetric care provider.1–3 But an informed decision is only as good as the available data. Regrettably, the literature on how planned home birth compares with hospital delivery in terms of pregnancy outcomes in the United States are sparse.
Related article: Lay midwives the the ObGyn: Is collaboration risky? Lucia DiVenere, MA (May 2012)
How safe is home birth in the United States?
Cheng and colleagues attempt to answer this question by reviewing newborn and maternal outcomes among planned home births versus hospital deliveries in a contemporary low-risk birth cohort. Their retrospective study included low-risk women at term with a singleton vertex live birth in 2008 in 27 of the 50 states using information from the Vital Statistics Natality Data provided by the Centers for Disease Control and Prevention.
Of these 2,081,753 women, 0.58% (n = 12,039) had planned home births, and the remainder delivered in a hospital setting. Women who had an “accidental” (unintended) home birth or who delivered in a freestanding birthing center were excluded. The primary outcome was the risk of a 5-minute Apgar score less than 4. Secondary outcomes included the risk of a 5-minute Apgar score less than 7, assisted ventilation for more than 6 hours, neonatal seizures, admission to the NICU, and a series of maternal outcome measures.
Besides the outcomes listed previously (top of page 24), women with a planned home birth had fewer obstetric interventions, including operative vaginal delivery and labor induction or augmentation. They also were less likely to be given antibiotics during labor (although the authors did not distinguish between antibiotics administered for prophylaxis against group B strep or surgical-site infection versus antibiotics to treat infections such as urinary tract infections or chorioamnionitis).
Of special interest is the fact that neither a prior vaginal delivery (multiparity) nor the absence of a prior cesarean delivery was protective against these adverse events.
The women at highest risk of an adverse event were those who delivered at home under the supervision of “other midwives.” Although these providers were not well defined, this term typically refers to community-based lay midwives whose only “training” consists of an unofficial apprenticeship of variable length. Despite the absence of formal training, the lack of certification and standardization of care, and the existence of legislation in many states banning their activity, such lay midwives continue to encourage and support home birth for both low- and high-risk women in the United States.
Related article: Update on Obstetrics John T. Repke, MD, and Jaimey M. Pauli, MD (January 2012)
Limitations of the study design
Although this dataset contains more than 2 million births, it includes only low-risk women at term and, therefore, is underpowered to measure outcomes such as fetal or neonatal death or birth injuries.
No data were presented on a number of important variables and outcome measures, such as the rate of or indications for cesarean delivery, the mode and frequency of intrapartum fetal monitoring, birth weight, intrapartum complications (uterine rupture, postpartum hemorrhage), blood transfusions, and infectious morbidity. The study also lacks long-term follow-up data on the infants.
That said, the study was well designed and very well written, and many of the limitations listed above are inherent in all retrospective cohort studies.
Putting these findings in context
These data are not novel, but they are remarkably consistent with other publications that have explored pregnancy outcomes in planned home birth versus hospital delivery from the Netherlands, the United Kingdom, Australia, and the United States, all of which show a higher rate of neonatal complications with planned home birth [see Reference 4 for review].4
Moreover, it is likely that the data in the current report significantly underestimate the risks of planned home birth for two reasons:
- Attempted home births that ended in transfer and, ultimately, delivery in a hospital setting (presumably for some unforeseen event such as excessive hemorrhage or uterine rupture or cord prolapse or nonreassuring fetal testing) were classified as hospital births.
- Apgar scores at 5 minutes are assigned by the attending care provider, and there is no way to independently verify their accuracy. Because of their limited training and/or concern about efforts to limit the scope of their practice, “other midwives” may be inclined to assign more favorable Apgar scores.
Who is choosing to deliver at home?
The proportion of US women who delivered outside the hospital setting increased by 29% between 2004 and 2009,5 although home births still constitute a minority of low-risk births (0.58% in the current study).
Related Article: Why are well-educated women more likely to choose home birth? Errol R. Norwitz, MD, PhD (Audiocast, November 2013)
One of the more interesting questions raised by this publication is the issue of who is choosing to deliver at home. In this cohort, women who planned home birth were more likely to be older, married, multiparous, white, and well educated. These aren’t exactly the women you would expect to gamble with the lives of their unborn offspring. So why are they choosing to deliver at home?
It could be that they are not well informed about the risks. Alternatively, they may have concluded that, although the relative risk of an adverse event is significantly higher with home birth, the absolute risk is low and acceptable to them. Or it could be that they are frustrated by the lack of autonomy afforded to them in the decisions surrounding antenatal care and the birthing process.
In recent years, more women are asking for minimally invasive births that are physically, emotionally, and socially supported. As hospital-based obstetric care providers, we do not always respect or meet these expectations. We can and should do better.
Women should not have to choose between a good birth experience and medical safety, between social support and hospital resources, between a sense of autonomy and access to life-saving interventions. Although every effort should be taken to make the birthing experience a positive one for the mother and her family as a whole, it should not be done at the expense of safety. I have yet to hear an asphyxiated and brain-damaged child thank his mother’s obstetric care provider for allowing a wonderful birth experience.
What this evidence means for practice
Even in countries where home births are integrated fully into the medical care system and attended by trained and certified nurse-midwives, they are associated with increased risks, including a twofold to threefold increase in the odds of neonatal death.4 In the US, where no such integration exists, home births are dangerous.
Maternity care has come a long way since the 17th Century, when a woman had a 1 in 6 chance of dying in childbirth and only one of every five children lived to enjoy a first birthday. It is appropriate in this era of Obamacare and cost containment that we explore alternative methods. The option of a safe home delivery may well be part of the solution, as it is for many European countries--but until we can be assured that such an approach is safe for both mothers and infants, let's keep home delivery where it belongs...for pizza!
--Errol R. Norwitz, MD, PHD
We want to hear from you! Tell us what you think.
- Committee on Obstetric Practice; American College of Obstetricians and Gynecologists. Committee Opinion #476: Planned home birth. Obstet Gynecol. 2011;117(2 Pt 1):425–428.
- American Academy of Pediatrics. Committee on Fetus and Newborn. Planned home birth. Pediatrics. 2013;131(5):1016–1020.
- American College of Nurse-Midwives. Division of Standards and Practice. Position statement: Home birth. Approved by the ACNM Board of Directors, May 2011. http://midwife.org/ACNM/files/ACNMLibraryData/UPLOADFILENAME/000000000251/Home%20Birth%20Aug%202011.pdf. Accessed October 21, 2013
- Wax JR, Lucas FL, Lamont M, et al. Maternal and newborn outcomes in planned home birth vs planned hospital births: A meta-analysis. Am J Obstet Gynecol. 2012;203(3):243.e1–e8.
- Martin JA, Hamilton BE, Ventura SJ, et al; Division of Vital Statistics. Births: Final data for 2009. Natl Vital Stat Rep. 2011;60(1):1–70.
Every morning before I leave for work, I kiss my three children goodbye and tell them, “I love you. Make good choices today.”
This has become my mantra—so much so that, on her way out the door to join her friends at the movies recently, my daughter turned to me and said, “I know, Dad. I know. I’ll make good decisions tonight.”
And what decision is more important than where to deliver your child and who to have in attendance at the birth?
It is said that the passage from the uterus to the outside world that each one of us was forced to negotiate at birth is the most treacherous journey we will ever undertake. Any unnecessary delay or complication can have profound, lifelong consequences.
There is no question that the past few centuries have seen a significant “medicalization” of childbirth, including the relocation of deliveries from the community to a hospital setting, the introduction of male obstetricians, the unfortunate marginalization of midwives and support personnel (doulas), the development of uterotonic drugs, and the evolution of operative vaginal (forceps, vacuum) and cesarean deliveries.
Many of the practices initially introduced by obstetric care providers (including multiple vaginal examinations in labor, induction of labor for a large baby, and active management of labor protocols) have since been shown to be unhelpful in improving pregnancy outcomes, and some practices (such as episiotomy) have even been shown to be harmful.
Related article: Difficult fetal extraction at cesarean delivery: What should you do? Robert L. Barbieri, MD (Editorial, January 2012)
In the midst of this confusion, the one voice that has been lost is that of the patient herself.
Whose birth is it anyway?
The American College of Obstetricians and Gynecologists (ACOG), the American Academy of Pediatrics (AAP), and the American College of Nurse-Midwives (ACNM) all agree that patient autonomy is paramount, and that the final decision of where to deliver and who to have in attendance should be made by the patient herself, ideally in conjunction with her family and her obstetric care provider.1–3 But an informed decision is only as good as the available data. Regrettably, the literature on how planned home birth compares with hospital delivery in terms of pregnancy outcomes in the United States are sparse.
Related article: Lay midwives the the ObGyn: Is collaboration risky? Lucia DiVenere, MA (May 2012)
How safe is home birth in the United States?
Cheng and colleagues attempt to answer this question by reviewing newborn and maternal outcomes among planned home births versus hospital deliveries in a contemporary low-risk birth cohort. Their retrospective study included low-risk women at term with a singleton vertex live birth in 2008 in 27 of the 50 states using information from the Vital Statistics Natality Data provided by the Centers for Disease Control and Prevention.
Of these 2,081,753 women, 0.58% (n = 12,039) had planned home births, and the remainder delivered in a hospital setting. Women who had an “accidental” (unintended) home birth or who delivered in a freestanding birthing center were excluded. The primary outcome was the risk of a 5-minute Apgar score less than 4. Secondary outcomes included the risk of a 5-minute Apgar score less than 7, assisted ventilation for more than 6 hours, neonatal seizures, admission to the NICU, and a series of maternal outcome measures.
Besides the outcomes listed previously (top of page 24), women with a planned home birth had fewer obstetric interventions, including operative vaginal delivery and labor induction or augmentation. They also were less likely to be given antibiotics during labor (although the authors did not distinguish between antibiotics administered for prophylaxis against group B strep or surgical-site infection versus antibiotics to treat infections such as urinary tract infections or chorioamnionitis).
Of special interest is the fact that neither a prior vaginal delivery (multiparity) nor the absence of a prior cesarean delivery was protective against these adverse events.
The women at highest risk of an adverse event were those who delivered at home under the supervision of “other midwives.” Although these providers were not well defined, this term typically refers to community-based lay midwives whose only “training” consists of an unofficial apprenticeship of variable length. Despite the absence of formal training, the lack of certification and standardization of care, and the existence of legislation in many states banning their activity, such lay midwives continue to encourage and support home birth for both low- and high-risk women in the United States.
Related article: Update on Obstetrics John T. Repke, MD, and Jaimey M. Pauli, MD (January 2012)
Limitations of the study design
Although this dataset contains more than 2 million births, it includes only low-risk women at term and, therefore, is underpowered to measure outcomes such as fetal or neonatal death or birth injuries.
No data were presented on a number of important variables and outcome measures, such as the rate of or indications for cesarean delivery, the mode and frequency of intrapartum fetal monitoring, birth weight, intrapartum complications (uterine rupture, postpartum hemorrhage), blood transfusions, and infectious morbidity. The study also lacks long-term follow-up data on the infants.
That said, the study was well designed and very well written, and many of the limitations listed above are inherent in all retrospective cohort studies.
Putting these findings in context
These data are not novel, but they are remarkably consistent with other publications that have explored pregnancy outcomes in planned home birth versus hospital delivery from the Netherlands, the United Kingdom, Australia, and the United States, all of which show a higher rate of neonatal complications with planned home birth [see Reference 4 for review].4
Moreover, it is likely that the data in the current report significantly underestimate the risks of planned home birth for two reasons:
- Attempted home births that ended in transfer and, ultimately, delivery in a hospital setting (presumably for some unforeseen event such as excessive hemorrhage or uterine rupture or cord prolapse or nonreassuring fetal testing) were classified as hospital births.
- Apgar scores at 5 minutes are assigned by the attending care provider, and there is no way to independently verify their accuracy. Because of their limited training and/or concern about efforts to limit the scope of their practice, “other midwives” may be inclined to assign more favorable Apgar scores.
Who is choosing to deliver at home?
The proportion of US women who delivered outside the hospital setting increased by 29% between 2004 and 2009,5 although home births still constitute a minority of low-risk births (0.58% in the current study).
Related Article: Why are well-educated women more likely to choose home birth? Errol R. Norwitz, MD, PhD (Audiocast, November 2013)
One of the more interesting questions raised by this publication is the issue of who is choosing to deliver at home. In this cohort, women who planned home birth were more likely to be older, married, multiparous, white, and well educated. These aren’t exactly the women you would expect to gamble with the lives of their unborn offspring. So why are they choosing to deliver at home?
It could be that they are not well informed about the risks. Alternatively, they may have concluded that, although the relative risk of an adverse event is significantly higher with home birth, the absolute risk is low and acceptable to them. Or it could be that they are frustrated by the lack of autonomy afforded to them in the decisions surrounding antenatal care and the birthing process.
In recent years, more women are asking for minimally invasive births that are physically, emotionally, and socially supported. As hospital-based obstetric care providers, we do not always respect or meet these expectations. We can and should do better.
Women should not have to choose between a good birth experience and medical safety, between social support and hospital resources, between a sense of autonomy and access to life-saving interventions. Although every effort should be taken to make the birthing experience a positive one for the mother and her family as a whole, it should not be done at the expense of safety. I have yet to hear an asphyxiated and brain-damaged child thank his mother’s obstetric care provider for allowing a wonderful birth experience.
What this evidence means for practice
Even in countries where home births are integrated fully into the medical care system and attended by trained and certified nurse-midwives, they are associated with increased risks, including a twofold to threefold increase in the odds of neonatal death.4 In the US, where no such integration exists, home births are dangerous.
Maternity care has come a long way since the 17th Century, when a woman had a 1 in 6 chance of dying in childbirth and only one of every five children lived to enjoy a first birthday. It is appropriate in this era of Obamacare and cost containment that we explore alternative methods. The option of a safe home delivery may well be part of the solution, as it is for many European countries--but until we can be assured that such an approach is safe for both mothers and infants, let's keep home delivery where it belongs...for pizza!
--Errol R. Norwitz, MD, PHD
We want to hear from you! Tell us what you think.
Every morning before I leave for work, I kiss my three children goodbye and tell them, “I love you. Make good choices today.”
This has become my mantra—so much so that, on her way out the door to join her friends at the movies recently, my daughter turned to me and said, “I know, Dad. I know. I’ll make good decisions tonight.”
And what decision is more important than where to deliver your child and who to have in attendance at the birth?
It is said that the passage from the uterus to the outside world that each one of us was forced to negotiate at birth is the most treacherous journey we will ever undertake. Any unnecessary delay or complication can have profound, lifelong consequences.
There is no question that the past few centuries have seen a significant “medicalization” of childbirth, including the relocation of deliveries from the community to a hospital setting, the introduction of male obstetricians, the unfortunate marginalization of midwives and support personnel (doulas), the development of uterotonic drugs, and the evolution of operative vaginal (forceps, vacuum) and cesarean deliveries.
Many of the practices initially introduced by obstetric care providers (including multiple vaginal examinations in labor, induction of labor for a large baby, and active management of labor protocols) have since been shown to be unhelpful in improving pregnancy outcomes, and some practices (such as episiotomy) have even been shown to be harmful.
Related article: Difficult fetal extraction at cesarean delivery: What should you do? Robert L. Barbieri, MD (Editorial, January 2012)
In the midst of this confusion, the one voice that has been lost is that of the patient herself.
Whose birth is it anyway?
The American College of Obstetricians and Gynecologists (ACOG), the American Academy of Pediatrics (AAP), and the American College of Nurse-Midwives (ACNM) all agree that patient autonomy is paramount, and that the final decision of where to deliver and who to have in attendance should be made by the patient herself, ideally in conjunction with her family and her obstetric care provider.1–3 But an informed decision is only as good as the available data. Regrettably, the literature on how planned home birth compares with hospital delivery in terms of pregnancy outcomes in the United States are sparse.
Related article: Lay midwives the the ObGyn: Is collaboration risky? Lucia DiVenere, MA (May 2012)
How safe is home birth in the United States?
Cheng and colleagues attempt to answer this question by reviewing newborn and maternal outcomes among planned home births versus hospital deliveries in a contemporary low-risk birth cohort. Their retrospective study included low-risk women at term with a singleton vertex live birth in 2008 in 27 of the 50 states using information from the Vital Statistics Natality Data provided by the Centers for Disease Control and Prevention.
Of these 2,081,753 women, 0.58% (n = 12,039) had planned home births, and the remainder delivered in a hospital setting. Women who had an “accidental” (unintended) home birth or who delivered in a freestanding birthing center were excluded. The primary outcome was the risk of a 5-minute Apgar score less than 4. Secondary outcomes included the risk of a 5-minute Apgar score less than 7, assisted ventilation for more than 6 hours, neonatal seizures, admission to the NICU, and a series of maternal outcome measures.
Besides the outcomes listed previously (top of page 24), women with a planned home birth had fewer obstetric interventions, including operative vaginal delivery and labor induction or augmentation. They also were less likely to be given antibiotics during labor (although the authors did not distinguish between antibiotics administered for prophylaxis against group B strep or surgical-site infection versus antibiotics to treat infections such as urinary tract infections or chorioamnionitis).
Of special interest is the fact that neither a prior vaginal delivery (multiparity) nor the absence of a prior cesarean delivery was protective against these adverse events.
The women at highest risk of an adverse event were those who delivered at home under the supervision of “other midwives.” Although these providers were not well defined, this term typically refers to community-based lay midwives whose only “training” consists of an unofficial apprenticeship of variable length. Despite the absence of formal training, the lack of certification and standardization of care, and the existence of legislation in many states banning their activity, such lay midwives continue to encourage and support home birth for both low- and high-risk women in the United States.
Related article: Update on Obstetrics John T. Repke, MD, and Jaimey M. Pauli, MD (January 2012)
Limitations of the study design
Although this dataset contains more than 2 million births, it includes only low-risk women at term and, therefore, is underpowered to measure outcomes such as fetal or neonatal death or birth injuries.
No data were presented on a number of important variables and outcome measures, such as the rate of or indications for cesarean delivery, the mode and frequency of intrapartum fetal monitoring, birth weight, intrapartum complications (uterine rupture, postpartum hemorrhage), blood transfusions, and infectious morbidity. The study also lacks long-term follow-up data on the infants.
That said, the study was well designed and very well written, and many of the limitations listed above are inherent in all retrospective cohort studies.
Putting these findings in context
These data are not novel, but they are remarkably consistent with other publications that have explored pregnancy outcomes in planned home birth versus hospital delivery from the Netherlands, the United Kingdom, Australia, and the United States, all of which show a higher rate of neonatal complications with planned home birth [see Reference 4 for review].4
Moreover, it is likely that the data in the current report significantly underestimate the risks of planned home birth for two reasons:
- Attempted home births that ended in transfer and, ultimately, delivery in a hospital setting (presumably for some unforeseen event such as excessive hemorrhage or uterine rupture or cord prolapse or nonreassuring fetal testing) were classified as hospital births.
- Apgar scores at 5 minutes are assigned by the attending care provider, and there is no way to independently verify their accuracy. Because of their limited training and/or concern about efforts to limit the scope of their practice, “other midwives” may be inclined to assign more favorable Apgar scores.
Who is choosing to deliver at home?
The proportion of US women who delivered outside the hospital setting increased by 29% between 2004 and 2009,5 although home births still constitute a minority of low-risk births (0.58% in the current study).
Related Article: Why are well-educated women more likely to choose home birth? Errol R. Norwitz, MD, PhD (Audiocast, November 2013)
One of the more interesting questions raised by this publication is the issue of who is choosing to deliver at home. In this cohort, women who planned home birth were more likely to be older, married, multiparous, white, and well educated. These aren’t exactly the women you would expect to gamble with the lives of their unborn offspring. So why are they choosing to deliver at home?
It could be that they are not well informed about the risks. Alternatively, they may have concluded that, although the relative risk of an adverse event is significantly higher with home birth, the absolute risk is low and acceptable to them. Or it could be that they are frustrated by the lack of autonomy afforded to them in the decisions surrounding antenatal care and the birthing process.
In recent years, more women are asking for minimally invasive births that are physically, emotionally, and socially supported. As hospital-based obstetric care providers, we do not always respect or meet these expectations. We can and should do better.
Women should not have to choose between a good birth experience and medical safety, between social support and hospital resources, between a sense of autonomy and access to life-saving interventions. Although every effort should be taken to make the birthing experience a positive one for the mother and her family as a whole, it should not be done at the expense of safety. I have yet to hear an asphyxiated and brain-damaged child thank his mother’s obstetric care provider for allowing a wonderful birth experience.
What this evidence means for practice
Even in countries where home births are integrated fully into the medical care system and attended by trained and certified nurse-midwives, they are associated with increased risks, including a twofold to threefold increase in the odds of neonatal death.4 In the US, where no such integration exists, home births are dangerous.
Maternity care has come a long way since the 17th Century, when a woman had a 1 in 6 chance of dying in childbirth and only one of every five children lived to enjoy a first birthday. It is appropriate in this era of Obamacare and cost containment that we explore alternative methods. The option of a safe home delivery may well be part of the solution, as it is for many European countries--but until we can be assured that such an approach is safe for both mothers and infants, let's keep home delivery where it belongs...for pizza!
--Errol R. Norwitz, MD, PHD
We want to hear from you! Tell us what you think.
- Committee on Obstetric Practice; American College of Obstetricians and Gynecologists. Committee Opinion #476: Planned home birth. Obstet Gynecol. 2011;117(2 Pt 1):425–428.
- American Academy of Pediatrics. Committee on Fetus and Newborn. Planned home birth. Pediatrics. 2013;131(5):1016–1020.
- American College of Nurse-Midwives. Division of Standards and Practice. Position statement: Home birth. Approved by the ACNM Board of Directors, May 2011. http://midwife.org/ACNM/files/ACNMLibraryData/UPLOADFILENAME/000000000251/Home%20Birth%20Aug%202011.pdf. Accessed October 21, 2013
- Wax JR, Lucas FL, Lamont M, et al. Maternal and newborn outcomes in planned home birth vs planned hospital births: A meta-analysis. Am J Obstet Gynecol. 2012;203(3):243.e1–e8.
- Martin JA, Hamilton BE, Ventura SJ, et al; Division of Vital Statistics. Births: Final data for 2009. Natl Vital Stat Rep. 2011;60(1):1–70.
- Committee on Obstetric Practice; American College of Obstetricians and Gynecologists. Committee Opinion #476: Planned home birth. Obstet Gynecol. 2011;117(2 Pt 1):425–428.
- American Academy of Pediatrics. Committee on Fetus and Newborn. Planned home birth. Pediatrics. 2013;131(5):1016–1020.
- American College of Nurse-Midwives. Division of Standards and Practice. Position statement: Home birth. Approved by the ACNM Board of Directors, May 2011. http://midwife.org/ACNM/files/ACNMLibraryData/UPLOADFILENAME/000000000251/Home%20Birth%20Aug%202011.pdf. Accessed October 21, 2013
- Wax JR, Lucas FL, Lamont M, et al. Maternal and newborn outcomes in planned home birth vs planned hospital births: A meta-analysis. Am J Obstet Gynecol. 2012;203(3):243.e1–e8.
- Martin JA, Hamilton BE, Ventura SJ, et al; Division of Vital Statistics. Births: Final data for 2009. Natl Vital Stat Rep. 2011;60(1):1–70.

Errol R. Norwitz, MD, PhD (November 2013)
STOP using antiembolism stockings to prevent DVT
PREVENTING VTE?
- VTE risk from hormone therapy varies by formulation
(Web News, October 2012) - Does the risk of unplanned pregnancy outweigh the risk of VTE from hormonal contraception?
Jennifer Gunter, MD (Guest Editorial, October 2012) - Contraception
Tami Rowen, MD, MS; Mitchell D. Creinin, MD (Update, August 2012) - Menopause
Andrew M. Kaunitz, MD (Update, May 2012)
The author reports no financial relationships relevant to this article.
Venous thromboembolism (VTE)—deep vein thrombosis (DVT) and pulmonary embolism (PE)—remains a major cause of morbidity and mortality in the United States, resulting in an estimated 200,000 deaths each year.1 VTE is especially common among inpatients; hospitalization increases the risk of VTE eightfold,2 and VTE is the most common preventable cause of hospital-associated deaths.2,3 Most general medical and surgical inpatients have risk factors for VTE and, without prophylaxis, between 10% and 40% will develop DVT or PE.3 VTE is estimated to cost the US economy $4 billion annually in direct costs and substantially more in indirect costs, including lost productivity and subsequent medical expenses.4
There is no doubt that thromboprophylaxis is effective in preventing VTE in high-risk patients.2,3,5-7 For this reason, the Agency for Healthcare Research and Quality ranks VTE prophylaxis as the single most important patient safety initiative deserving of more widespread implementation.8 The importance of this intervention has also been acknowledged by the Joint Commission,9 and by the Centers for Medicare & Medicaid Services, which include VTE prophylaxis in their Surgical Care Improvement Project (SCIP) quality measures that guide hospital reimbursement.10
All patients undergoing surgery (including cesarean delivery) should be considered at high risk for VTE. Additional risk factors include, among others:
- personal or family history of VTE
- known inherited or acquired thrombophilia
- obesity
- advancing age
- prolonged immobility or bed rest
- cancer.2,3,5-7
Although there is general consensus that high-risk patients require thromboprophylaxis, exactly what form of prophylaxis to recommend remains controversial.
Graduated compression stockings may cause harm
Graduated compression stockings (also known as TED stockings) are commonly regarded as a safe and noninvasive method for preventing VTE. However, evidence in support of their efficacy is lacking. A recent consensus statement from the American College of Physicians recommended “against the use of mechanical prophylaxis with graduated compression stockings for prevention of venous thromboembolism (Grade: strong recommendation, moderate-quality evidence)” in medical and stroke patients.5 In support of their recommendation, the authors of this consensus statement cite a lack of evidence of benefit and significant evidence of patient harm related to skin breakdown from compression stockings. This recommendation is likely relevant also for obstetric and gynecologic patients. For this reason, I propose that the use of graduated compression stockings for DVT prophylaxis be abandoned.
Chemoprophylaxis should be routine in high-risk inpatients
VTE chemoprophylaxis with low molecular weight heparin (LMWH; eg, dalteparin or enoxaparin) or low-dose unfractionated heparin remains the most effective prophylactic measure and should be routine in all high-risk obstetric and gynecologic inpatients.2,3,5-7 Pneumatic compression devices and chemoprophylaxis may provide synergistic protection against VTE.5
Cesarean delivery affects need for prophylaxis
Although pregnancy is an independent risk factor for VTE, the absolute risk of VTE in an otherwise healthy patient is only about 0.05% in both the antepartum and postpartum periods.11 For this reason, routine VTE prophylaxis in pregnant patients would certainly cause more harm than good, and is not recommended. However, cesarean delivery doubles the risk of VTE, with an absolute risk in low-risk parturients of approximately 1 in 1,000 patients.12 And 85% of fatal PE cases in pregnancy follow cesarean delivery. For these reasons, placement of pneumatic compression devices and/or administration of LMWH is recommended before cesarean delivery for all women not already receiving chemoprophylaxis.7
One clarification. Although the use of graduated compression stockings to prevent VTE should be abandoned entirely, there is some evidence that compression stockings with an ankle pressure of 30 to 40 mm Hg may help reduce the risk of long-term phlebitis syndrome in patients with established DVT in pregnancy.13 Therefore, use of compression stockings may be considered in this setting.
We want to hear from you! Tell us what you think.
1. Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States 1979-1998: an analysis using multiple-cause mortality data. Arch Intern Med. 2003;163(14):1711-1717.
2. Michota F. Bridging the gap between evidence and practice in venous thromboembolism prophylaxis: quality improvement process. J Gen Intern Med. 2007;22(12):1762-1770.
3. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th ed. Chest. 2008;133(suppl 6):381S-453S.
4. Shorr A. The pharmacoeconomics of deep venous thrombosis treatment. Am J Med. 2007;120(10 Suppl 2):35S-41S.
5. Qaseem A, Chou R, Humphrey LL, et al. Clinical Guidelines Committee of the American College of Physicians. Venous thromboembolism prophylaxis in hospitalized patients: a clinical practice guideline from the American College of Physicians. Ann Int Med. 2011;155(9):625-632.
6. Committee on Practice Bulletins—Gynecology, American College of Obstetricians and Gynecologists. Practice Bulletin No. 84: Prevention of deep vein thrombosis and pulmonary embolism. Obstet Gynecol. 2007;110(2 Pt 1):429-440.
7. Committee on Practice Bulletins—Obstetrics, American College of Obstetricians and Gynecologists. Practice Bulletin No. 123: Thromboembolism in pregnancy. Obstet Gynecol. 2011;118(3):718-729.
8. Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ. Making health care safer: a critical analysis of patient safety practices. Evid Rep Technol Assessment (Summ). 2001;(43):l-x, 1-668.
9. The Joint Commission. 2011 Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oak Brook IL: Joint Commission Resources; 2010.
10. Centers for Medicare & Medicaid Services (CMS). Medicare Program—Revisions to Hospital Outpatient Prospective Payment System and Calendar Year 2007 Payment Rates; Final Rule. Baltimore Maryland: CMS; November 24, 2006.
11. Bourjeily G, Paidas M, Khalil H, Rosene-Montella K, Rodger M. Pulmonary embolism in pregnancy. Lancet. 2010;375(9713):500-512.
12. Macklon NS, Greer IA. Venous thromboembolic disease in obstetrics and gynaecology: the Scottish experience. Scott Med J. 1996;41(3):83-86.
13. Brandjes DPM, Buller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349(9054):759-762.
PREVENTING VTE?
- VTE risk from hormone therapy varies by formulation
(Web News, October 2012) - Does the risk of unplanned pregnancy outweigh the risk of VTE from hormonal contraception?
Jennifer Gunter, MD (Guest Editorial, October 2012) - Contraception
Tami Rowen, MD, MS; Mitchell D. Creinin, MD (Update, August 2012) - Menopause
Andrew M. Kaunitz, MD (Update, May 2012)
The author reports no financial relationships relevant to this article.
Venous thromboembolism (VTE)—deep vein thrombosis (DVT) and pulmonary embolism (PE)—remains a major cause of morbidity and mortality in the United States, resulting in an estimated 200,000 deaths each year.1 VTE is especially common among inpatients; hospitalization increases the risk of VTE eightfold,2 and VTE is the most common preventable cause of hospital-associated deaths.2,3 Most general medical and surgical inpatients have risk factors for VTE and, without prophylaxis, between 10% and 40% will develop DVT or PE.3 VTE is estimated to cost the US economy $4 billion annually in direct costs and substantially more in indirect costs, including lost productivity and subsequent medical expenses.4
There is no doubt that thromboprophylaxis is effective in preventing VTE in high-risk patients.2,3,5-7 For this reason, the Agency for Healthcare Research and Quality ranks VTE prophylaxis as the single most important patient safety initiative deserving of more widespread implementation.8 The importance of this intervention has also been acknowledged by the Joint Commission,9 and by the Centers for Medicare & Medicaid Services, which include VTE prophylaxis in their Surgical Care Improvement Project (SCIP) quality measures that guide hospital reimbursement.10
All patients undergoing surgery (including cesarean delivery) should be considered at high risk for VTE. Additional risk factors include, among others:
- personal or family history of VTE
- known inherited or acquired thrombophilia
- obesity
- advancing age
- prolonged immobility or bed rest
- cancer.2,3,5-7
Although there is general consensus that high-risk patients require thromboprophylaxis, exactly what form of prophylaxis to recommend remains controversial.
Graduated compression stockings may cause harm
Graduated compression stockings (also known as TED stockings) are commonly regarded as a safe and noninvasive method for preventing VTE. However, evidence in support of their efficacy is lacking. A recent consensus statement from the American College of Physicians recommended “against the use of mechanical prophylaxis with graduated compression stockings for prevention of venous thromboembolism (Grade: strong recommendation, moderate-quality evidence)” in medical and stroke patients.5 In support of their recommendation, the authors of this consensus statement cite a lack of evidence of benefit and significant evidence of patient harm related to skin breakdown from compression stockings. This recommendation is likely relevant also for obstetric and gynecologic patients. For this reason, I propose that the use of graduated compression stockings for DVT prophylaxis be abandoned.
Chemoprophylaxis should be routine in high-risk inpatients
VTE chemoprophylaxis with low molecular weight heparin (LMWH; eg, dalteparin or enoxaparin) or low-dose unfractionated heparin remains the most effective prophylactic measure and should be routine in all high-risk obstetric and gynecologic inpatients.2,3,5-7 Pneumatic compression devices and chemoprophylaxis may provide synergistic protection against VTE.5
Cesarean delivery affects need for prophylaxis
Although pregnancy is an independent risk factor for VTE, the absolute risk of VTE in an otherwise healthy patient is only about 0.05% in both the antepartum and postpartum periods.11 For this reason, routine VTE prophylaxis in pregnant patients would certainly cause more harm than good, and is not recommended. However, cesarean delivery doubles the risk of VTE, with an absolute risk in low-risk parturients of approximately 1 in 1,000 patients.12 And 85% of fatal PE cases in pregnancy follow cesarean delivery. For these reasons, placement of pneumatic compression devices and/or administration of LMWH is recommended before cesarean delivery for all women not already receiving chemoprophylaxis.7
One clarification. Although the use of graduated compression stockings to prevent VTE should be abandoned entirely, there is some evidence that compression stockings with an ankle pressure of 30 to 40 mm Hg may help reduce the risk of long-term phlebitis syndrome in patients with established DVT in pregnancy.13 Therefore, use of compression stockings may be considered in this setting.
We want to hear from you! Tell us what you think.
PREVENTING VTE?
- VTE risk from hormone therapy varies by formulation
(Web News, October 2012) - Does the risk of unplanned pregnancy outweigh the risk of VTE from hormonal contraception?
Jennifer Gunter, MD (Guest Editorial, October 2012) - Contraception
Tami Rowen, MD, MS; Mitchell D. Creinin, MD (Update, August 2012) - Menopause
Andrew M. Kaunitz, MD (Update, May 2012)
The author reports no financial relationships relevant to this article.
Venous thromboembolism (VTE)—deep vein thrombosis (DVT) and pulmonary embolism (PE)—remains a major cause of morbidity and mortality in the United States, resulting in an estimated 200,000 deaths each year.1 VTE is especially common among inpatients; hospitalization increases the risk of VTE eightfold,2 and VTE is the most common preventable cause of hospital-associated deaths.2,3 Most general medical and surgical inpatients have risk factors for VTE and, without prophylaxis, between 10% and 40% will develop DVT or PE.3 VTE is estimated to cost the US economy $4 billion annually in direct costs and substantially more in indirect costs, including lost productivity and subsequent medical expenses.4
There is no doubt that thromboprophylaxis is effective in preventing VTE in high-risk patients.2,3,5-7 For this reason, the Agency for Healthcare Research and Quality ranks VTE prophylaxis as the single most important patient safety initiative deserving of more widespread implementation.8 The importance of this intervention has also been acknowledged by the Joint Commission,9 and by the Centers for Medicare & Medicaid Services, which include VTE prophylaxis in their Surgical Care Improvement Project (SCIP) quality measures that guide hospital reimbursement.10
All patients undergoing surgery (including cesarean delivery) should be considered at high risk for VTE. Additional risk factors include, among others:
- personal or family history of VTE
- known inherited or acquired thrombophilia
- obesity
- advancing age
- prolonged immobility or bed rest
- cancer.2,3,5-7
Although there is general consensus that high-risk patients require thromboprophylaxis, exactly what form of prophylaxis to recommend remains controversial.
Graduated compression stockings may cause harm
Graduated compression stockings (also known as TED stockings) are commonly regarded as a safe and noninvasive method for preventing VTE. However, evidence in support of their efficacy is lacking. A recent consensus statement from the American College of Physicians recommended “against the use of mechanical prophylaxis with graduated compression stockings for prevention of venous thromboembolism (Grade: strong recommendation, moderate-quality evidence)” in medical and stroke patients.5 In support of their recommendation, the authors of this consensus statement cite a lack of evidence of benefit and significant evidence of patient harm related to skin breakdown from compression stockings. This recommendation is likely relevant also for obstetric and gynecologic patients. For this reason, I propose that the use of graduated compression stockings for DVT prophylaxis be abandoned.
Chemoprophylaxis should be routine in high-risk inpatients
VTE chemoprophylaxis with low molecular weight heparin (LMWH; eg, dalteparin or enoxaparin) or low-dose unfractionated heparin remains the most effective prophylactic measure and should be routine in all high-risk obstetric and gynecologic inpatients.2,3,5-7 Pneumatic compression devices and chemoprophylaxis may provide synergistic protection against VTE.5
Cesarean delivery affects need for prophylaxis
Although pregnancy is an independent risk factor for VTE, the absolute risk of VTE in an otherwise healthy patient is only about 0.05% in both the antepartum and postpartum periods.11 For this reason, routine VTE prophylaxis in pregnant patients would certainly cause more harm than good, and is not recommended. However, cesarean delivery doubles the risk of VTE, with an absolute risk in low-risk parturients of approximately 1 in 1,000 patients.12 And 85% of fatal PE cases in pregnancy follow cesarean delivery. For these reasons, placement of pneumatic compression devices and/or administration of LMWH is recommended before cesarean delivery for all women not already receiving chemoprophylaxis.7
One clarification. Although the use of graduated compression stockings to prevent VTE should be abandoned entirely, there is some evidence that compression stockings with an ankle pressure of 30 to 40 mm Hg may help reduce the risk of long-term phlebitis syndrome in patients with established DVT in pregnancy.13 Therefore, use of compression stockings may be considered in this setting.
We want to hear from you! Tell us what you think.
1. Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States 1979-1998: an analysis using multiple-cause mortality data. Arch Intern Med. 2003;163(14):1711-1717.
2. Michota F. Bridging the gap between evidence and practice in venous thromboembolism prophylaxis: quality improvement process. J Gen Intern Med. 2007;22(12):1762-1770.
3. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th ed. Chest. 2008;133(suppl 6):381S-453S.
4. Shorr A. The pharmacoeconomics of deep venous thrombosis treatment. Am J Med. 2007;120(10 Suppl 2):35S-41S.
5. Qaseem A, Chou R, Humphrey LL, et al. Clinical Guidelines Committee of the American College of Physicians. Venous thromboembolism prophylaxis in hospitalized patients: a clinical practice guideline from the American College of Physicians. Ann Int Med. 2011;155(9):625-632.
6. Committee on Practice Bulletins—Gynecology, American College of Obstetricians and Gynecologists. Practice Bulletin No. 84: Prevention of deep vein thrombosis and pulmonary embolism. Obstet Gynecol. 2007;110(2 Pt 1):429-440.
7. Committee on Practice Bulletins—Obstetrics, American College of Obstetricians and Gynecologists. Practice Bulletin No. 123: Thromboembolism in pregnancy. Obstet Gynecol. 2011;118(3):718-729.
8. Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ. Making health care safer: a critical analysis of patient safety practices. Evid Rep Technol Assessment (Summ). 2001;(43):l-x, 1-668.
9. The Joint Commission. 2011 Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oak Brook IL: Joint Commission Resources; 2010.
10. Centers for Medicare & Medicaid Services (CMS). Medicare Program—Revisions to Hospital Outpatient Prospective Payment System and Calendar Year 2007 Payment Rates; Final Rule. Baltimore Maryland: CMS; November 24, 2006.
11. Bourjeily G, Paidas M, Khalil H, Rosene-Montella K, Rodger M. Pulmonary embolism in pregnancy. Lancet. 2010;375(9713):500-512.
12. Macklon NS, Greer IA. Venous thromboembolic disease in obstetrics and gynaecology: the Scottish experience. Scott Med J. 1996;41(3):83-86.
13. Brandjes DPM, Buller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349(9054):759-762.
1. Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States 1979-1998: an analysis using multiple-cause mortality data. Arch Intern Med. 2003;163(14):1711-1717.
2. Michota F. Bridging the gap between evidence and practice in venous thromboembolism prophylaxis: quality improvement process. J Gen Intern Med. 2007;22(12):1762-1770.
3. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. 8th ed. Chest. 2008;133(suppl 6):381S-453S.
4. Shorr A. The pharmacoeconomics of deep venous thrombosis treatment. Am J Med. 2007;120(10 Suppl 2):35S-41S.
5. Qaseem A, Chou R, Humphrey LL, et al. Clinical Guidelines Committee of the American College of Physicians. Venous thromboembolism prophylaxis in hospitalized patients: a clinical practice guideline from the American College of Physicians. Ann Int Med. 2011;155(9):625-632.
6. Committee on Practice Bulletins—Gynecology, American College of Obstetricians and Gynecologists. Practice Bulletin No. 84: Prevention of deep vein thrombosis and pulmonary embolism. Obstet Gynecol. 2007;110(2 Pt 1):429-440.
7. Committee on Practice Bulletins—Obstetrics, American College of Obstetricians and Gynecologists. Practice Bulletin No. 123: Thromboembolism in pregnancy. Obstet Gynecol. 2011;118(3):718-729.
8. Shojania KG, Duncan BW, McDonald KM, Wachter RM, Markowitz AJ. Making health care safer: a critical analysis of patient safety practices. Evid Rep Technol Assessment (Summ). 2001;(43):l-x, 1-668.
9. The Joint Commission. 2011 Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oak Brook IL: Joint Commission Resources; 2010.
10. Centers for Medicare & Medicaid Services (CMS). Medicare Program—Revisions to Hospital Outpatient Prospective Payment System and Calendar Year 2007 Payment Rates; Final Rule. Baltimore Maryland: CMS; November 24, 2006.
11. Bourjeily G, Paidas M, Khalil H, Rosene-Montella K, Rodger M. Pulmonary embolism in pregnancy. Lancet. 2010;375(9713):500-512.
12. Macklon NS, Greer IA. Venous thromboembolic disease in obstetrics and gynaecology: the Scottish experience. Scott Med J. 1996;41(3):83-86.
13. Brandjes DPM, Buller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349(9054):759-762.
Does mediolateral episiotomy reduce the risk of anal sphincter injury in operative vaginal delivery?
Stop performing median episiotomy!
Robert L. Barbieri, MD (Editorial, April 2012)
Episiotomy is an incision into the perineal body that is made during the second stage of labor to expedite delivery. Despite guidelines recommending restrictions on its use, episiotomy is still performed in more than 25% of vaginal deliveries in the United States. Suggested benefits include a shortened second stage of labor, the substitution of a straight surgical incision for a ragged spontaneous tear, and a reduced incidence of severe perineal injury and resultant pelvic floor dysfunction. Few data support these assertions, however.
Episiotomy is no OASIS
Absolute indications for episiotomy have yet to be established. Although there is general agreement that episiotomy may be indicated in select circumstances (such as to expedite delivery in the setting of nonreassuring fetal testing in the second stage of labor, shoulder dystocia, or at the time of operative vaginal delivery), routine use is discouraged.1,2 Besides the lack of data showing its benefit, episiotomy is associated with several potential complications, including increased blood loss, fetal injury, and localized pain. In contrast to the stated goal of reducing perineal trauma, episiotomy is associated with an increased incidence of third- or fourth-degree perineal lacerations,3,4 referred to in this study as obstetric anal sphincter injuries (OASIS).
Third- or fourth-degree tears are identified clinically at the time of vaginal delivery in 0.6% to 9% of patients.4 Studies using two-dimensional endoanal ultrasonography suggest that the true incidence of rectal injury is probably closer to 11%.5 Such injuries are associated with an increased risk of subsequent urinary or fecal incontinence (or both) and pelvic organ prolapse.
If episiotomy is indicated, how should it be performed?
There are two main types of episiotomy: median (favored in the United States) and mediolateral episiotomy. Complications—especially OASIS—are more common with median episiotomy,3,6,7 which involves a vertical midline incision from the posterior fourchette toward the rectum. Mediolateral episiotomy (favored in Europe), refers to an incision performed at a 45° angle from the posterior fourchette. OASIS is more common after median episiotomy, compared with the mediolateral approach.4,6 What is not yet clear is whether mediolateral episiotomy actually protects against OASIS.
Details of the study
de Vogel and colleagues evaluated the frequency of OASIS in women at high risk—specifically, those undergoing operative vaginal delivery; they also sought to determine whether mediolateral episiotomy is protective against OASIS. To this end, they performed a retrospective analysis of 2,861 consecutive women who delivered a singleton liveborn infant at term by vacuum, forceps, or both, from 2001–2009. Women were identified through the Netherlands Perinatal Registry, a voluntary reporting national database that includes approximately 96% of the 190,000 births that occur after 16 weeks’ gestation each year in the Netherlands. Exclusion criteria included multiple gestation, breech presentation, and use of median episiotomy.
The overall frequency of OASIS was 5.7% (162 cases among 2,861 deliveries). After logistic-regression modeling, a number of variables were significantly associated with OASIS, all of which have been identified previously: forceps delivery, occiput posterior position, primiparity, and epidural anesthesia. Women with a mediolateral episiotomy were at a significantly lower risk for OASIS, compared with women without mediolateral episiotomy (3.5% vs 15.6%, respectively; P<.001). Further analysis suggested that 8.6 mediolateral episiotomies would be needed to prevent one OASIS during vacuum extraction, whereas 5.2 procedures would be necessary to prevent one OASIS during forceps delivery. de Vogel and colleagues concluded that mediolateral episiotomy should be performed during all operative vaginal deliveries to reduce the incidence of OASIS.
Although this study included a large sample from a well-established and validated dataset (collected prospectively), it was, by design, retrospective. There was no standardization of when or how to cut the mediolateral episiotomy. However, many of these uncontrolled variables (such as cutting an episiotomy that is more median than mediolateral or cutting an episiotomy only in women who appear to be at imminent risk of sustaining a perineal laceration) would increase—not decrease—the risk of severe perineal injury. This fact suggests that the protective effect of mediolateral episiotomy may be even more dramatic than the sixfold protection reported in this study.
This study focused on women who underwent operative vaginal delivery. It remains controversial whether mediolateral episiotomy is protective in women who have a spontaneous (noninstrumental) vaginal delivery.
The study also lacks follow-up data on how many women with OASIS went on to develop fecal or urinary incontinence or pelvic organ prolapse. However, a third- or fourth-degree perineal laceration is serious enough that it can serve as an acceptable primary outcome measure even in the absence of long-term functional data.
In this study, use of median episiotomy was an exclusion, mostly likely because it is rarely performed in Europe.
While the battle over “to cut or not to cut” continues to rage, one fact is clear: median episiotomy should be abandoned. If you are going to perform episiotomy, make it mediolateral. According to this report, accoucheurs should consider cutting a mediolateral episiotomy for perineal protection each time they perform operative vaginal delivery.
ERROL R. NORWITZ, MD, PHD
After reading this article, and Dr. Barbieri’s April Editorial, we want to know if these articles have changed your practice. If you were faced with a difficult vaginal delivery, would you use a median or mediolateral episiotomy incision? Why?
We want to hear from you! Tell us what you think.
1. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr KN. Outcomes of routine episiotomy: a systematic review. JAMA. 2005;293(17):2141-2148.
2. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.-
3. Helwig JT, Thorp JM, Jr, Bowes WA, Jr. Does midline episiotomy increase the risk of third- and fourth-degree lacerations in operative vaginal deliveries? Obstet Gynecol. 1993;82(2):276-279.
4. Dudding TC, Vaizey C, Kamm MA. Obstetric anal sphincter injury: incidence, risk factors, and management. Ann Surg. 2008;247(2):224-237.
5. Williams AB, Bartram CI, Halligan S, Spencer JA, Nicholls RJ, Kmiot WA. Anal sphincter damage after vaginal delivery using three-dimensional endosonography. Obstet Gynecol. 2001;97(5 Pt 1):770-775.
6. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87(5):408-412.
7. Kudish B, Blackwell S, McNeeley SG, et al. Operative vaginal delivery and midline episiotomy: a bad combination for the perineum. Am J Obstet Gynecol. 2006;195(3):749-754.
Stop performing median episiotomy!
Robert L. Barbieri, MD (Editorial, April 2012)
Episiotomy is an incision into the perineal body that is made during the second stage of labor to expedite delivery. Despite guidelines recommending restrictions on its use, episiotomy is still performed in more than 25% of vaginal deliveries in the United States. Suggested benefits include a shortened second stage of labor, the substitution of a straight surgical incision for a ragged spontaneous tear, and a reduced incidence of severe perineal injury and resultant pelvic floor dysfunction. Few data support these assertions, however.
Episiotomy is no OASIS
Absolute indications for episiotomy have yet to be established. Although there is general agreement that episiotomy may be indicated in select circumstances (such as to expedite delivery in the setting of nonreassuring fetal testing in the second stage of labor, shoulder dystocia, or at the time of operative vaginal delivery), routine use is discouraged.1,2 Besides the lack of data showing its benefit, episiotomy is associated with several potential complications, including increased blood loss, fetal injury, and localized pain. In contrast to the stated goal of reducing perineal trauma, episiotomy is associated with an increased incidence of third- or fourth-degree perineal lacerations,3,4 referred to in this study as obstetric anal sphincter injuries (OASIS).
Third- or fourth-degree tears are identified clinically at the time of vaginal delivery in 0.6% to 9% of patients.4 Studies using two-dimensional endoanal ultrasonography suggest that the true incidence of rectal injury is probably closer to 11%.5 Such injuries are associated with an increased risk of subsequent urinary or fecal incontinence (or both) and pelvic organ prolapse.
If episiotomy is indicated, how should it be performed?
There are two main types of episiotomy: median (favored in the United States) and mediolateral episiotomy. Complications—especially OASIS—are more common with median episiotomy,3,6,7 which involves a vertical midline incision from the posterior fourchette toward the rectum. Mediolateral episiotomy (favored in Europe), refers to an incision performed at a 45° angle from the posterior fourchette. OASIS is more common after median episiotomy, compared with the mediolateral approach.4,6 What is not yet clear is whether mediolateral episiotomy actually protects against OASIS.
Details of the study
de Vogel and colleagues evaluated the frequency of OASIS in women at high risk—specifically, those undergoing operative vaginal delivery; they also sought to determine whether mediolateral episiotomy is protective against OASIS. To this end, they performed a retrospective analysis of 2,861 consecutive women who delivered a singleton liveborn infant at term by vacuum, forceps, or both, from 2001–2009. Women were identified through the Netherlands Perinatal Registry, a voluntary reporting national database that includes approximately 96% of the 190,000 births that occur after 16 weeks’ gestation each year in the Netherlands. Exclusion criteria included multiple gestation, breech presentation, and use of median episiotomy.
The overall frequency of OASIS was 5.7% (162 cases among 2,861 deliveries). After logistic-regression modeling, a number of variables were significantly associated with OASIS, all of which have been identified previously: forceps delivery, occiput posterior position, primiparity, and epidural anesthesia. Women with a mediolateral episiotomy were at a significantly lower risk for OASIS, compared with women without mediolateral episiotomy (3.5% vs 15.6%, respectively; P<.001). Further analysis suggested that 8.6 mediolateral episiotomies would be needed to prevent one OASIS during vacuum extraction, whereas 5.2 procedures would be necessary to prevent one OASIS during forceps delivery. de Vogel and colleagues concluded that mediolateral episiotomy should be performed during all operative vaginal deliveries to reduce the incidence of OASIS.
Although this study included a large sample from a well-established and validated dataset (collected prospectively), it was, by design, retrospective. There was no standardization of when or how to cut the mediolateral episiotomy. However, many of these uncontrolled variables (such as cutting an episiotomy that is more median than mediolateral or cutting an episiotomy only in women who appear to be at imminent risk of sustaining a perineal laceration) would increase—not decrease—the risk of severe perineal injury. This fact suggests that the protective effect of mediolateral episiotomy may be even more dramatic than the sixfold protection reported in this study.
This study focused on women who underwent operative vaginal delivery. It remains controversial whether mediolateral episiotomy is protective in women who have a spontaneous (noninstrumental) vaginal delivery.
The study also lacks follow-up data on how many women with OASIS went on to develop fecal or urinary incontinence or pelvic organ prolapse. However, a third- or fourth-degree perineal laceration is serious enough that it can serve as an acceptable primary outcome measure even in the absence of long-term functional data.
In this study, use of median episiotomy was an exclusion, mostly likely because it is rarely performed in Europe.
While the battle over “to cut or not to cut” continues to rage, one fact is clear: median episiotomy should be abandoned. If you are going to perform episiotomy, make it mediolateral. According to this report, accoucheurs should consider cutting a mediolateral episiotomy for perineal protection each time they perform operative vaginal delivery.
ERROL R. NORWITZ, MD, PHD
After reading this article, and Dr. Barbieri’s April Editorial, we want to know if these articles have changed your practice. If you were faced with a difficult vaginal delivery, would you use a median or mediolateral episiotomy incision? Why?
We want to hear from you! Tell us what you think.
Stop performing median episiotomy!
Robert L. Barbieri, MD (Editorial, April 2012)
Episiotomy is an incision into the perineal body that is made during the second stage of labor to expedite delivery. Despite guidelines recommending restrictions on its use, episiotomy is still performed in more than 25% of vaginal deliveries in the United States. Suggested benefits include a shortened second stage of labor, the substitution of a straight surgical incision for a ragged spontaneous tear, and a reduced incidence of severe perineal injury and resultant pelvic floor dysfunction. Few data support these assertions, however.
Episiotomy is no OASIS
Absolute indications for episiotomy have yet to be established. Although there is general agreement that episiotomy may be indicated in select circumstances (such as to expedite delivery in the setting of nonreassuring fetal testing in the second stage of labor, shoulder dystocia, or at the time of operative vaginal delivery), routine use is discouraged.1,2 Besides the lack of data showing its benefit, episiotomy is associated with several potential complications, including increased blood loss, fetal injury, and localized pain. In contrast to the stated goal of reducing perineal trauma, episiotomy is associated with an increased incidence of third- or fourth-degree perineal lacerations,3,4 referred to in this study as obstetric anal sphincter injuries (OASIS).
Third- or fourth-degree tears are identified clinically at the time of vaginal delivery in 0.6% to 9% of patients.4 Studies using two-dimensional endoanal ultrasonography suggest that the true incidence of rectal injury is probably closer to 11%.5 Such injuries are associated with an increased risk of subsequent urinary or fecal incontinence (or both) and pelvic organ prolapse.
If episiotomy is indicated, how should it be performed?
There are two main types of episiotomy: median (favored in the United States) and mediolateral episiotomy. Complications—especially OASIS—are more common with median episiotomy,3,6,7 which involves a vertical midline incision from the posterior fourchette toward the rectum. Mediolateral episiotomy (favored in Europe), refers to an incision performed at a 45° angle from the posterior fourchette. OASIS is more common after median episiotomy, compared with the mediolateral approach.4,6 What is not yet clear is whether mediolateral episiotomy actually protects against OASIS.
Details of the study
de Vogel and colleagues evaluated the frequency of OASIS in women at high risk—specifically, those undergoing operative vaginal delivery; they also sought to determine whether mediolateral episiotomy is protective against OASIS. To this end, they performed a retrospective analysis of 2,861 consecutive women who delivered a singleton liveborn infant at term by vacuum, forceps, or both, from 2001–2009. Women were identified through the Netherlands Perinatal Registry, a voluntary reporting national database that includes approximately 96% of the 190,000 births that occur after 16 weeks’ gestation each year in the Netherlands. Exclusion criteria included multiple gestation, breech presentation, and use of median episiotomy.
The overall frequency of OASIS was 5.7% (162 cases among 2,861 deliveries). After logistic-regression modeling, a number of variables were significantly associated with OASIS, all of which have been identified previously: forceps delivery, occiput posterior position, primiparity, and epidural anesthesia. Women with a mediolateral episiotomy were at a significantly lower risk for OASIS, compared with women without mediolateral episiotomy (3.5% vs 15.6%, respectively; P<.001). Further analysis suggested that 8.6 mediolateral episiotomies would be needed to prevent one OASIS during vacuum extraction, whereas 5.2 procedures would be necessary to prevent one OASIS during forceps delivery. de Vogel and colleagues concluded that mediolateral episiotomy should be performed during all operative vaginal deliveries to reduce the incidence of OASIS.
Although this study included a large sample from a well-established and validated dataset (collected prospectively), it was, by design, retrospective. There was no standardization of when or how to cut the mediolateral episiotomy. However, many of these uncontrolled variables (such as cutting an episiotomy that is more median than mediolateral or cutting an episiotomy only in women who appear to be at imminent risk of sustaining a perineal laceration) would increase—not decrease—the risk of severe perineal injury. This fact suggests that the protective effect of mediolateral episiotomy may be even more dramatic than the sixfold protection reported in this study.
This study focused on women who underwent operative vaginal delivery. It remains controversial whether mediolateral episiotomy is protective in women who have a spontaneous (noninstrumental) vaginal delivery.
The study also lacks follow-up data on how many women with OASIS went on to develop fecal or urinary incontinence or pelvic organ prolapse. However, a third- or fourth-degree perineal laceration is serious enough that it can serve as an acceptable primary outcome measure even in the absence of long-term functional data.
In this study, use of median episiotomy was an exclusion, mostly likely because it is rarely performed in Europe.
While the battle over “to cut or not to cut” continues to rage, one fact is clear: median episiotomy should be abandoned. If you are going to perform episiotomy, make it mediolateral. According to this report, accoucheurs should consider cutting a mediolateral episiotomy for perineal protection each time they perform operative vaginal delivery.
ERROL R. NORWITZ, MD, PHD
After reading this article, and Dr. Barbieri’s April Editorial, we want to know if these articles have changed your practice. If you were faced with a difficult vaginal delivery, would you use a median or mediolateral episiotomy incision? Why?
We want to hear from you! Tell us what you think.
1. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr KN. Outcomes of routine episiotomy: a systematic review. JAMA. 2005;293(17):2141-2148.
2. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.-
3. Helwig JT, Thorp JM, Jr, Bowes WA, Jr. Does midline episiotomy increase the risk of third- and fourth-degree lacerations in operative vaginal deliveries? Obstet Gynecol. 1993;82(2):276-279.
4. Dudding TC, Vaizey C, Kamm MA. Obstetric anal sphincter injury: incidence, risk factors, and management. Ann Surg. 2008;247(2):224-237.
5. Williams AB, Bartram CI, Halligan S, Spencer JA, Nicholls RJ, Kmiot WA. Anal sphincter damage after vaginal delivery using three-dimensional endosonography. Obstet Gynecol. 2001;97(5 Pt 1):770-775.
6. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87(5):408-412.
7. Kudish B, Blackwell S, McNeeley SG, et al. Operative vaginal delivery and midline episiotomy: a bad combination for the perineum. Am J Obstet Gynecol. 2006;195(3):749-754.
1. Hartmann K, Viswanathan M, Palmieri R, Gartlehner G, Thorp J, Lohr KN. Outcomes of routine episiotomy: a systematic review. JAMA. 2005;293(17):2141-2148.
2. Carroli G, Mignini L. Episiotomy for vaginal birth. Cochrane Database Syst Rev. 2009;(1):CD000081.-
3. Helwig JT, Thorp JM, Jr, Bowes WA, Jr. Does midline episiotomy increase the risk of third- and fourth-degree lacerations in operative vaginal deliveries? Obstet Gynecol. 1993;82(2):276-279.
4. Dudding TC, Vaizey C, Kamm MA. Obstetric anal sphincter injury: incidence, risk factors, and management. Ann Surg. 2008;247(2):224-237.
5. Williams AB, Bartram CI, Halligan S, Spencer JA, Nicholls RJ, Kmiot WA. Anal sphincter damage after vaginal delivery using three-dimensional endosonography. Obstet Gynecol. 2001;97(5 Pt 1):770-775.
6. Coats PM, Chan KK, Wilkins M, Beard RJ. A comparison between midline and mediolateral episiotomies. Br J Obstet Gynaecol. 1980;87(5):408-412.
7. Kudish B, Blackwell S, McNeeley SG, et al. Operative vaginal delivery and midline episiotomy: a bad combination for the perineum. Am J Obstet Gynecol. 2006;195(3):749-754.