Article
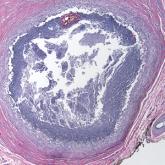
Recurrent Cutaneous Exophiala Phaeohyphomycosis in an Immunosuppressed Patient
- Author:
- Noel Turner, MD
- Nour Kibbi, MD
- Gauri Panse, MD
- Suguru Imaeda, MD
Phaeohyphomycosis is an infection with dematiaceous fungi that most commonly affects immunosuppressed patients.
