User login
FDA clears software for immunohematology labs
The US Food and Drug Administration (FDA) has granted 510(k) clearance for ORTHO CONNECT V2.0, a software system developed by Ortho Clinical Diagnostics.
ORTHO CONNECT V2.0 is middleware designed to keep large quantities of data accessible and consistent across multiple instruments and laboratory systems.
ORTHO CONNECT V2.0 works with other products Ortho Clinical Diagnostics has developed for immunohematology labs.
The software is now available for purchase in the US.
According to Ortho Clinical Diagnostics, ORTHO CONNECT V2.0 is comprehensive, integrated, and customizable middleware (software that acts as a bridge between an operating system or database and application).
ORTHO CONNECT V2.0 centralizes laboratory operations and workflow across hospitals and networks, allowing blood banks and their data to be managed through one central terminal. The software can link all Ortho Clinical Diagnostics instruments to lab information systems through a single interface.
Acting as an intermediary between instruments and lab information systems, ORTHO CONNECT V2.0 allows labs to exchange data, perform data management, and complete regulatory process tasks that are not easily performed alone. All test results on connected analyzers can be viewed and verified no matter the location.
ORTHO CONNECT V2.0 enables the ORTHO VISION® and ORTHO VISION® Max immunohematology analyzers, which test blood for transfusion compatibility, to integrate with a hospital’s laboratory information systems through a single validated connection to exchange data and simplify processes.
“Ortho [Clinical Diagnostics] is focused on diminishing the complexities of immunohematology testing while improving safety, speed, and efficiency throughout the blood bank,” said Robert Yates, the company’s chief operating officer.
“ORTHO CONNECT does just that, bringing improved functionality to laboratory information systems that are often relatively rigid and outdated. It’s the perfect complement to our ORTHO VISION platform of analyzers.”
The US Food and Drug Administration (FDA) has granted 510(k) clearance for ORTHO CONNECT V2.0, a software system developed by Ortho Clinical Diagnostics.
ORTHO CONNECT V2.0 is middleware designed to keep large quantities of data accessible and consistent across multiple instruments and laboratory systems.
ORTHO CONNECT V2.0 works with other products Ortho Clinical Diagnostics has developed for immunohematology labs.
The software is now available for purchase in the US.
According to Ortho Clinical Diagnostics, ORTHO CONNECT V2.0 is comprehensive, integrated, and customizable middleware (software that acts as a bridge between an operating system or database and application).
ORTHO CONNECT V2.0 centralizes laboratory operations and workflow across hospitals and networks, allowing blood banks and their data to be managed through one central terminal. The software can link all Ortho Clinical Diagnostics instruments to lab information systems through a single interface.
Acting as an intermediary between instruments and lab information systems, ORTHO CONNECT V2.0 allows labs to exchange data, perform data management, and complete regulatory process tasks that are not easily performed alone. All test results on connected analyzers can be viewed and verified no matter the location.
ORTHO CONNECT V2.0 enables the ORTHO VISION® and ORTHO VISION® Max immunohematology analyzers, which test blood for transfusion compatibility, to integrate with a hospital’s laboratory information systems through a single validated connection to exchange data and simplify processes.
“Ortho [Clinical Diagnostics] is focused on diminishing the complexities of immunohematology testing while improving safety, speed, and efficiency throughout the blood bank,” said Robert Yates, the company’s chief operating officer.
“ORTHO CONNECT does just that, bringing improved functionality to laboratory information systems that are often relatively rigid and outdated. It’s the perfect complement to our ORTHO VISION platform of analyzers.”
The US Food and Drug Administration (FDA) has granted 510(k) clearance for ORTHO CONNECT V2.0, a software system developed by Ortho Clinical Diagnostics.
ORTHO CONNECT V2.0 is middleware designed to keep large quantities of data accessible and consistent across multiple instruments and laboratory systems.
ORTHO CONNECT V2.0 works with other products Ortho Clinical Diagnostics has developed for immunohematology labs.
The software is now available for purchase in the US.
According to Ortho Clinical Diagnostics, ORTHO CONNECT V2.0 is comprehensive, integrated, and customizable middleware (software that acts as a bridge between an operating system or database and application).
ORTHO CONNECT V2.0 centralizes laboratory operations and workflow across hospitals and networks, allowing blood banks and their data to be managed through one central terminal. The software can link all Ortho Clinical Diagnostics instruments to lab information systems through a single interface.
Acting as an intermediary between instruments and lab information systems, ORTHO CONNECT V2.0 allows labs to exchange data, perform data management, and complete regulatory process tasks that are not easily performed alone. All test results on connected analyzers can be viewed and verified no matter the location.
ORTHO CONNECT V2.0 enables the ORTHO VISION® and ORTHO VISION® Max immunohematology analyzers, which test blood for transfusion compatibility, to integrate with a hospital’s laboratory information systems through a single validated connection to exchange data and simplify processes.
“Ortho [Clinical Diagnostics] is focused on diminishing the complexities of immunohematology testing while improving safety, speed, and efficiency throughout the blood bank,” said Robert Yates, the company’s chief operating officer.
“ORTHO CONNECT does just that, bringing improved functionality to laboratory information systems that are often relatively rigid and outdated. It’s the perfect complement to our ORTHO VISION platform of analyzers.”
CHMP recommends rejection for betrixaban
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has issued a negative opinion recommending refusal of marketing authorization for the factor Xa inhibitor betrixaban (Dexxience).
Portola Pharmaceuticals, Inc. is seeking approval of betrixaban for the prevention of venous thromboembolism (VTE) in adults hospitalized for an acute medical illness with risk factors for VTE, including VTE-related death.
The marketing authorization application for betrixaban was supported by data from the phase 3 APEX study. In this study, researchers compared oral betrixaban to injectable enoxaparin for the prevention of VTE in patients with acute medical illnesses.
The CHMP said APEX did not satisfactorily show that betrixaban’s benefits outweigh its risk in this patient population. The study results were not considered reliable because some test results for VTEs were not available.
In addition, patients treated with betrixaban had more episodes of bleeding than those treated with enoxaparin. This was considered an important concern given that betrixaban was expected to be used in patients with serious underlying conditions.
For these reasons, the CHMP recommended that betrixaban be refused marketing authorization.
Portola Pharmaceuticals said it intends to appeal the CHMP’s opinion and ask the committee for a re-examination.
“We believe we have generated substantial evidence which demonstrates the clinically meaningful benefit of betrixaban in reducing VTE and VTE-related deaths in this vulnerable patient population, and we remain confident in its potential to have a major public health impact,” said Jack Lawrence, MD, chief medical officer of Portola Pharmaceuticals.
“The re-examination process allows us the opportunity to address the CHMP’s questions and provide further clarification as needed, with the goal of making betrixaban available to acute medically ill patients in Europe who are at risk for VTE.”
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has issued a negative opinion recommending refusal of marketing authorization for the factor Xa inhibitor betrixaban (Dexxience).
Portola Pharmaceuticals, Inc. is seeking approval of betrixaban for the prevention of venous thromboembolism (VTE) in adults hospitalized for an acute medical illness with risk factors for VTE, including VTE-related death.
The marketing authorization application for betrixaban was supported by data from the phase 3 APEX study. In this study, researchers compared oral betrixaban to injectable enoxaparin for the prevention of VTE in patients with acute medical illnesses.
The CHMP said APEX did not satisfactorily show that betrixaban’s benefits outweigh its risk in this patient population. The study results were not considered reliable because some test results for VTEs were not available.
In addition, patients treated with betrixaban had more episodes of bleeding than those treated with enoxaparin. This was considered an important concern given that betrixaban was expected to be used in patients with serious underlying conditions.
For these reasons, the CHMP recommended that betrixaban be refused marketing authorization.
Portola Pharmaceuticals said it intends to appeal the CHMP’s opinion and ask the committee for a re-examination.
“We believe we have generated substantial evidence which demonstrates the clinically meaningful benefit of betrixaban in reducing VTE and VTE-related deaths in this vulnerable patient population, and we remain confident in its potential to have a major public health impact,” said Jack Lawrence, MD, chief medical officer of Portola Pharmaceuticals.
“The re-examination process allows us the opportunity to address the CHMP’s questions and provide further clarification as needed, with the goal of making betrixaban available to acute medically ill patients in Europe who are at risk for VTE.”
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has issued a negative opinion recommending refusal of marketing authorization for the factor Xa inhibitor betrixaban (Dexxience).
Portola Pharmaceuticals, Inc. is seeking approval of betrixaban for the prevention of venous thromboembolism (VTE) in adults hospitalized for an acute medical illness with risk factors for VTE, including VTE-related death.
The marketing authorization application for betrixaban was supported by data from the phase 3 APEX study. In this study, researchers compared oral betrixaban to injectable enoxaparin for the prevention of VTE in patients with acute medical illnesses.
The CHMP said APEX did not satisfactorily show that betrixaban’s benefits outweigh its risk in this patient population. The study results were not considered reliable because some test results for VTEs were not available.
In addition, patients treated with betrixaban had more episodes of bleeding than those treated with enoxaparin. This was considered an important concern given that betrixaban was expected to be used in patients with serious underlying conditions.
For these reasons, the CHMP recommended that betrixaban be refused marketing authorization.
Portola Pharmaceuticals said it intends to appeal the CHMP’s opinion and ask the committee for a re-examination.
“We believe we have generated substantial evidence which demonstrates the clinically meaningful benefit of betrixaban in reducing VTE and VTE-related deaths in this vulnerable patient population, and we remain confident in its potential to have a major public health impact,” said Jack Lawrence, MD, chief medical officer of Portola Pharmaceuticals.
“The re-examination process allows us the opportunity to address the CHMP’s questions and provide further clarification as needed, with the goal of making betrixaban available to acute medically ill patients in Europe who are at risk for VTE.”
Mortality in patients with PTLD
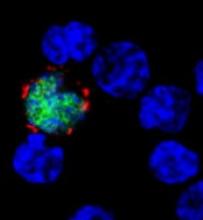
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
LISBON—A review of recent studies has revealed a “significant burden” of mortality related to post-transplant lymphoproliferative disorder (PTLD), according to researchers.
Of the 120 PTLD patients studied, 64% died and 42.5% died with PTLD.
The median time from hematopoietic stem cell transplant (HSCT) to the development of PTLD was about 9 weeks in children and 11 weeks in adults.
The median time from PTLD diagnosis to death was about 6 weeks in adults and 8 weeks in children.
These findings were presented at 44th Annual Meeting of the EBMT (abstract A219).
The research was funded by Atara Biotherapeutics, Inc., which is developing tabelecleucel (formerly ATA129), a T-cell immunotherapy intended to treat patients with Epstein-Barr virus-associated PTLD who have failed treatment with rituximab.
The review included 9 articles, published in 2005 and later, detailing studies of patients who developed PTLD after HSCT.
There were 120 patients. They had a mean age of 28.97, 67% were male, and 79% had received rituximab.
The 31 pediatric patients had a mean age of 9.84, 81% were male, and 74% had received rituximab. The 89 adult patients had a mean age of 35.63, 62% were male, and 81% had received rituximab.
Among the 16 pediatric patients with available data, the median time from HSCT to PTLD diagnosis was 65 days, and the mean was 138 days.
For the 59 adults with available data, the median time from HSCT to PTLD was 76 days, and the mean was 132 days.
The all-cause mortality rate was 64% in the entire population (77/120), 71% in children (22/31), and 62% in adults (55/89).
Overall, 42.5% of patients (51/120) died with PTLD—35.5% of children (11/31) and 44.9% of adults (40/89).
Among the patients who died with PTLD, the median time from PTLD diagnosis to death was 55 days for children and 40 days for adults. The mean time from PTLD to death was 71 days and 51 days, respectively.
There were 110 patients with available overall survival data. The median survival time from PTLD diagnosis was 116 days in the entire cohort, 153 days in children, and 92 days in adults.
“Patients with PTLD following [HSCT] experience high mortality rates under the current standard of care due to aggressive disease that often rapidly progresses to death after diagnosis,” said Chris Haqq, MD, PhD, of Atara Biotherapeutics.
“Children and relatively young adults in their prime working years are disproportionately affected. Atara is dedicated to progressing tab‑cel™ development in the ongoing phase 3 clinical studies to potentially address the compelling medical need for patients with this life-threatening condition.”
Amgen withdraws application for darbepoetin alfa
Amgen has withdrawn its application to expand the existing marketing authorization for darbepoetin alfa (Aranesp), according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The goal with this application was to extend the authorization for darbepoetin alfa to include the treatment of anemia in adults with low-risk or intermediate-1-risk myelodysplastic syndromes (MDS) who have low transfusion demand.
Darbepoetin alfa is currently approved in the European Union (EU) to treat anemia in adults and children with chronic renal failure and adults who are receiving chemotherapy for non-myeloid malignancies.
Amgen withdrew the application for darbepoetin alfa in MDS patients after the CHMP had evaluated initial documentation provided by the company and formulated a list of questions. Amgen had not yet responded to the questions when it notified the CHMP of the withdrawal.
At the time of the withdrawal, the CHMP was of the provisional opinion that darbepoetin alfa could not have been approved for the treatment of anemia in adults with MDS.
This opinion was based on concerns about the data supporting the application—results from the phase 3 ARCADE trial (NCT01362140) and a phase 2 trial (NCT00095264).
The CHMP said changes to the design of the phase 3 trial and the exclusion of a high number of patients from the analysis of the results raise questions about the validity of the data.
In addition, the phase 2 trial, which was conducted in the US, was not in line with EU recommendations for the treatment of MDS patients.
Therefore, at the time of the withdrawal, the CHMP had decided the marketing authorization could not be expanded based on the data provided.
In a letter to the CHMP, Amgen said its decision to withdraw the application is based on the CHMP’s negative opinion.
Amgen has withdrawn its application to expand the existing marketing authorization for darbepoetin alfa (Aranesp), according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The goal with this application was to extend the authorization for darbepoetin alfa to include the treatment of anemia in adults with low-risk or intermediate-1-risk myelodysplastic syndromes (MDS) who have low transfusion demand.
Darbepoetin alfa is currently approved in the European Union (EU) to treat anemia in adults and children with chronic renal failure and adults who are receiving chemotherapy for non-myeloid malignancies.
Amgen withdrew the application for darbepoetin alfa in MDS patients after the CHMP had evaluated initial documentation provided by the company and formulated a list of questions. Amgen had not yet responded to the questions when it notified the CHMP of the withdrawal.
At the time of the withdrawal, the CHMP was of the provisional opinion that darbepoetin alfa could not have been approved for the treatment of anemia in adults with MDS.
This opinion was based on concerns about the data supporting the application—results from the phase 3 ARCADE trial (NCT01362140) and a phase 2 trial (NCT00095264).
The CHMP said changes to the design of the phase 3 trial and the exclusion of a high number of patients from the analysis of the results raise questions about the validity of the data.
In addition, the phase 2 trial, which was conducted in the US, was not in line with EU recommendations for the treatment of MDS patients.
Therefore, at the time of the withdrawal, the CHMP had decided the marketing authorization could not be expanded based on the data provided.
In a letter to the CHMP, Amgen said its decision to withdraw the application is based on the CHMP’s negative opinion.
Amgen has withdrawn its application to expand the existing marketing authorization for darbepoetin alfa (Aranesp), according to the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP).
The goal with this application was to extend the authorization for darbepoetin alfa to include the treatment of anemia in adults with low-risk or intermediate-1-risk myelodysplastic syndromes (MDS) who have low transfusion demand.
Darbepoetin alfa is currently approved in the European Union (EU) to treat anemia in adults and children with chronic renal failure and adults who are receiving chemotherapy for non-myeloid malignancies.
Amgen withdrew the application for darbepoetin alfa in MDS patients after the CHMP had evaluated initial documentation provided by the company and formulated a list of questions. Amgen had not yet responded to the questions when it notified the CHMP of the withdrawal.
At the time of the withdrawal, the CHMP was of the provisional opinion that darbepoetin alfa could not have been approved for the treatment of anemia in adults with MDS.
This opinion was based on concerns about the data supporting the application—results from the phase 3 ARCADE trial (NCT01362140) and a phase 2 trial (NCT00095264).
The CHMP said changes to the design of the phase 3 trial and the exclusion of a high number of patients from the analysis of the results raise questions about the validity of the data.
In addition, the phase 2 trial, which was conducted in the US, was not in line with EU recommendations for the treatment of MDS patients.
Therefore, at the time of the withdrawal, the CHMP had decided the marketing authorization could not be expanded based on the data provided.
In a letter to the CHMP, Amgen said its decision to withdraw the application is based on the CHMP’s negative opinion.
FDA approves nilotinib for kids with CML
The US Food and Drug Administration (FDA) has expanded the approved indication for nilotinib (Tasigna®) to include the treatment of children.
The drug is now approved to treat patients age 1 and older who have newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in the chronic phase.
Nilotinib is also approved to treat pediatric patients age 1 and older who have chronic phase, Ph+ CML that is resistant or intolerant to prior tyrosine kinase inhibitor (TKI) therapy, as well as adults with Ph+ CML in chronic phase and accelerated phase that is resistant or intolerant to prior therapy including imatinib.
The new pediatric indications for nilotinib, granted under the FDA’s priority review designation, are based on results from 2 studies of the drug—a phase 1 and phase 2.
According to Novartis, the studies included 69 CML patients who ranged in age from 2 to 17. They had either newly diagnosed, chronic phase, Ph+ CML or chronic phase, Ph+ CML with resistance or intolerance to prior TKI therapy.
In the newly diagnosed patients, the major molecular response (MMR) rate was 60.0% at 12 cycles, with 15 patients achieving MMR.
In patients with resistance or intolerance to prior therapy, the MMR rate was 40.9% at 12 cycles, with 18 patients being in MMR.
In newly diagnosed patients, the cumulative MMR rate was 64.0% by cycle 12. In patients with resistance or intolerance to prior therapy, the cumulative MMR rate was 47.7% by cycle 12.
Adverse events were generally consistent with those observed in adults, with the exception of hyperbilirubinemia and transaminase elevation, which were reported at a higher frequency than in adults.
The rate of grade 3/4 hyperbilirubinemia was 13.0%, the rate of grade 3/4 AST elevation was 1.4%, and the rate of grade 3/4 ALT elevation was 8.7%.
There were no deaths on treatment or after treatment discontinuation.
There was 1 patient with resistant/intolerant CML who progressed to advance phase/blast crisis after about 10 months on nilotinib.
The US Food and Drug Administration (FDA) has expanded the approved indication for nilotinib (Tasigna®) to include the treatment of children.
The drug is now approved to treat patients age 1 and older who have newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in the chronic phase.
Nilotinib is also approved to treat pediatric patients age 1 and older who have chronic phase, Ph+ CML that is resistant or intolerant to prior tyrosine kinase inhibitor (TKI) therapy, as well as adults with Ph+ CML in chronic phase and accelerated phase that is resistant or intolerant to prior therapy including imatinib.
The new pediatric indications for nilotinib, granted under the FDA’s priority review designation, are based on results from 2 studies of the drug—a phase 1 and phase 2.
According to Novartis, the studies included 69 CML patients who ranged in age from 2 to 17. They had either newly diagnosed, chronic phase, Ph+ CML or chronic phase, Ph+ CML with resistance or intolerance to prior TKI therapy.
In the newly diagnosed patients, the major molecular response (MMR) rate was 60.0% at 12 cycles, with 15 patients achieving MMR.
In patients with resistance or intolerance to prior therapy, the MMR rate was 40.9% at 12 cycles, with 18 patients being in MMR.
In newly diagnosed patients, the cumulative MMR rate was 64.0% by cycle 12. In patients with resistance or intolerance to prior therapy, the cumulative MMR rate was 47.7% by cycle 12.
Adverse events were generally consistent with those observed in adults, with the exception of hyperbilirubinemia and transaminase elevation, which were reported at a higher frequency than in adults.
The rate of grade 3/4 hyperbilirubinemia was 13.0%, the rate of grade 3/4 AST elevation was 1.4%, and the rate of grade 3/4 ALT elevation was 8.7%.
There were no deaths on treatment or after treatment discontinuation.
There was 1 patient with resistant/intolerant CML who progressed to advance phase/blast crisis after about 10 months on nilotinib.
The US Food and Drug Administration (FDA) has expanded the approved indication for nilotinib (Tasigna®) to include the treatment of children.
The drug is now approved to treat patients age 1 and older who have newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in the chronic phase.
Nilotinib is also approved to treat pediatric patients age 1 and older who have chronic phase, Ph+ CML that is resistant or intolerant to prior tyrosine kinase inhibitor (TKI) therapy, as well as adults with Ph+ CML in chronic phase and accelerated phase that is resistant or intolerant to prior therapy including imatinib.
The new pediatric indications for nilotinib, granted under the FDA’s priority review designation, are based on results from 2 studies of the drug—a phase 1 and phase 2.
According to Novartis, the studies included 69 CML patients who ranged in age from 2 to 17. They had either newly diagnosed, chronic phase, Ph+ CML or chronic phase, Ph+ CML with resistance or intolerance to prior TKI therapy.
In the newly diagnosed patients, the major molecular response (MMR) rate was 60.0% at 12 cycles, with 15 patients achieving MMR.
In patients with resistance or intolerance to prior therapy, the MMR rate was 40.9% at 12 cycles, with 18 patients being in MMR.
In newly diagnosed patients, the cumulative MMR rate was 64.0% by cycle 12. In patients with resistance or intolerance to prior therapy, the cumulative MMR rate was 47.7% by cycle 12.
Adverse events were generally consistent with those observed in adults, with the exception of hyperbilirubinemia and transaminase elevation, which were reported at a higher frequency than in adults.
The rate of grade 3/4 hyperbilirubinemia was 13.0%, the rate of grade 3/4 AST elevation was 1.4%, and the rate of grade 3/4 ALT elevation was 8.7%.
There were no deaths on treatment or after treatment discontinuation.
There was 1 patient with resistant/intolerant CML who progressed to advance phase/blast crisis after about 10 months on nilotinib.
Health Canada approves SC rituximab for CLL
Health Canada has approved a subcutaneous (SC) formulation of rituximab (Rituxan®) to treat patients with chronic lymphocytic leukemia (CLL).
The product is now approved for use in combination with fludarabine and cyclophosphamide to treat patients with previously treated or untreated CLL, Binet Stage B or C.
The SC formulation is intended to provide a more convenient delivery method than intravenous (IV) rituximab. The SC formulation enables administration of the drug in large volumes under the skin.
“The approval of Rituxan SC is exciting news and a meaningful advancement for those living with CLL, as intravenous treatments can take around 4 hours to receive, requiring patients to spend up to a half day sitting in the chemo suite,” said Robin Markowitz, chief executive officer of Lymphoma Canada.
“The administration of Rituxan SC only takes 7 minutes, giving patients valuable time back in their day.”
SAWYER study
Health Canada’s approval of SC rituximab is based on data from the phase 1b SAWYER study. This randomized study was conducted in patients with previously untreated CLL to investigate the pharmacokinetic profile, safety, and efficacy of SC rituximab in combination with chemotherapy.
Results from this study were published in The Lancet Haematology in March 2016.
The trial included 176 patients who were randomized to receive SC rituximab (1600 mg, n=88) or IV rituximab (500 mg/m2, n=88) on day 1 from cycles 2 to 6. In cycle 1, both groups received IV rituximab (375 mg/m2) on day 0.
All patients also received fludarabine (IV 25 mg/m2 on days 1-3 of all cycles or orally at either 25 mg/m2 on days 1-5 of all cycles or 30-40 mg/m2 on days 1-3 of all cycles) and cyclophosphamide (IV at 250 mg/m2 on days 1-3 of all cycles or orally at either 150 mg/m2 on days 1-5 of all cycles or 200-250 mg/m2 on days 1-3 of all cycles) every 4 weeks for up to 6 cycles.
The primary endpoint was pharmacokinetic noninferiority of SC to IV rituximab assessed at cycle 5. At that time, the geometric mean trough serum concentration in the SC rituximab arm was noninferior to that in the IV arm—97.5 µg/mL and 61.5 µg/mL, respectively—with an adjusted geometric mean ratio of 1.53 (90% CI, 1.27 to 1.85).
Safety was a secondary endpoint, and efficacy was an exploratory endpoint.
The overall response rate was 85% in the SC arm and 81% in the IV arm. Complete response rates were 26% and 33%, respectively.
Rates of adverse events (AEs) were 96% in the SC arm and 91% in the IV arm. Rates of grade 3 or higher AEs were 69% and 71%, respectively, and rates of serious AEs were 29% and 33%, respectively.
The most common serious AE overall was febrile neutropenia, which occurred in 11% of patients in the SC arm and 4% in the IV arm.
The most common AEs of any grade (occurring in >20% of patients in either arm) were:
- Neutropenia—65% with SC and 58% with IV
- Thrombocytopenia—24% with SC and 26% with IV
- Anemia—13% with SC and 24% with IV
- Nausea—38% with SC and 35% with IV
- Vomiting—21% with SC and 22% with IV
- Pyrexia—32% with SC and 25% with IV
- Injection-site erythema—26% with SC and 0% with IV.
Local cutaneous reactions were reported in 42% of patients in the SC arm. The most common of these were injection-site erythema (26%) and injection-site pain (16%).
Health Canada has approved a subcutaneous (SC) formulation of rituximab (Rituxan®) to treat patients with chronic lymphocytic leukemia (CLL).
The product is now approved for use in combination with fludarabine and cyclophosphamide to treat patients with previously treated or untreated CLL, Binet Stage B or C.
The SC formulation is intended to provide a more convenient delivery method than intravenous (IV) rituximab. The SC formulation enables administration of the drug in large volumes under the skin.
“The approval of Rituxan SC is exciting news and a meaningful advancement for those living with CLL, as intravenous treatments can take around 4 hours to receive, requiring patients to spend up to a half day sitting in the chemo suite,” said Robin Markowitz, chief executive officer of Lymphoma Canada.
“The administration of Rituxan SC only takes 7 minutes, giving patients valuable time back in their day.”
SAWYER study
Health Canada’s approval of SC rituximab is based on data from the phase 1b SAWYER study. This randomized study was conducted in patients with previously untreated CLL to investigate the pharmacokinetic profile, safety, and efficacy of SC rituximab in combination with chemotherapy.
Results from this study were published in The Lancet Haematology in March 2016.
The trial included 176 patients who were randomized to receive SC rituximab (1600 mg, n=88) or IV rituximab (500 mg/m2, n=88) on day 1 from cycles 2 to 6. In cycle 1, both groups received IV rituximab (375 mg/m2) on day 0.
All patients also received fludarabine (IV 25 mg/m2 on days 1-3 of all cycles or orally at either 25 mg/m2 on days 1-5 of all cycles or 30-40 mg/m2 on days 1-3 of all cycles) and cyclophosphamide (IV at 250 mg/m2 on days 1-3 of all cycles or orally at either 150 mg/m2 on days 1-5 of all cycles or 200-250 mg/m2 on days 1-3 of all cycles) every 4 weeks for up to 6 cycles.
The primary endpoint was pharmacokinetic noninferiority of SC to IV rituximab assessed at cycle 5. At that time, the geometric mean trough serum concentration in the SC rituximab arm was noninferior to that in the IV arm—97.5 µg/mL and 61.5 µg/mL, respectively—with an adjusted geometric mean ratio of 1.53 (90% CI, 1.27 to 1.85).
Safety was a secondary endpoint, and efficacy was an exploratory endpoint.
The overall response rate was 85% in the SC arm and 81% in the IV arm. Complete response rates were 26% and 33%, respectively.
Rates of adverse events (AEs) were 96% in the SC arm and 91% in the IV arm. Rates of grade 3 or higher AEs were 69% and 71%, respectively, and rates of serious AEs were 29% and 33%, respectively.
The most common serious AE overall was febrile neutropenia, which occurred in 11% of patients in the SC arm and 4% in the IV arm.
The most common AEs of any grade (occurring in >20% of patients in either arm) were:
- Neutropenia—65% with SC and 58% with IV
- Thrombocytopenia—24% with SC and 26% with IV
- Anemia—13% with SC and 24% with IV
- Nausea—38% with SC and 35% with IV
- Vomiting—21% with SC and 22% with IV
- Pyrexia—32% with SC and 25% with IV
- Injection-site erythema—26% with SC and 0% with IV.
Local cutaneous reactions were reported in 42% of patients in the SC arm. The most common of these were injection-site erythema (26%) and injection-site pain (16%).
Health Canada has approved a subcutaneous (SC) formulation of rituximab (Rituxan®) to treat patients with chronic lymphocytic leukemia (CLL).
The product is now approved for use in combination with fludarabine and cyclophosphamide to treat patients with previously treated or untreated CLL, Binet Stage B or C.
The SC formulation is intended to provide a more convenient delivery method than intravenous (IV) rituximab. The SC formulation enables administration of the drug in large volumes under the skin.
“The approval of Rituxan SC is exciting news and a meaningful advancement for those living with CLL, as intravenous treatments can take around 4 hours to receive, requiring patients to spend up to a half day sitting in the chemo suite,” said Robin Markowitz, chief executive officer of Lymphoma Canada.
“The administration of Rituxan SC only takes 7 minutes, giving patients valuable time back in their day.”
SAWYER study
Health Canada’s approval of SC rituximab is based on data from the phase 1b SAWYER study. This randomized study was conducted in patients with previously untreated CLL to investigate the pharmacokinetic profile, safety, and efficacy of SC rituximab in combination with chemotherapy.
Results from this study were published in The Lancet Haematology in March 2016.
The trial included 176 patients who were randomized to receive SC rituximab (1600 mg, n=88) or IV rituximab (500 mg/m2, n=88) on day 1 from cycles 2 to 6. In cycle 1, both groups received IV rituximab (375 mg/m2) on day 0.
All patients also received fludarabine (IV 25 mg/m2 on days 1-3 of all cycles or orally at either 25 mg/m2 on days 1-5 of all cycles or 30-40 mg/m2 on days 1-3 of all cycles) and cyclophosphamide (IV at 250 mg/m2 on days 1-3 of all cycles or orally at either 150 mg/m2 on days 1-5 of all cycles or 200-250 mg/m2 on days 1-3 of all cycles) every 4 weeks for up to 6 cycles.
The primary endpoint was pharmacokinetic noninferiority of SC to IV rituximab assessed at cycle 5. At that time, the geometric mean trough serum concentration in the SC rituximab arm was noninferior to that in the IV arm—97.5 µg/mL and 61.5 µg/mL, respectively—with an adjusted geometric mean ratio of 1.53 (90% CI, 1.27 to 1.85).
Safety was a secondary endpoint, and efficacy was an exploratory endpoint.
The overall response rate was 85% in the SC arm and 81% in the IV arm. Complete response rates were 26% and 33%, respectively.
Rates of adverse events (AEs) were 96% in the SC arm and 91% in the IV arm. Rates of grade 3 or higher AEs were 69% and 71%, respectively, and rates of serious AEs were 29% and 33%, respectively.
The most common serious AE overall was febrile neutropenia, which occurred in 11% of patients in the SC arm and 4% in the IV arm.
The most common AEs of any grade (occurring in >20% of patients in either arm) were:
- Neutropenia—65% with SC and 58% with IV
- Thrombocytopenia—24% with SC and 26% with IV
- Anemia—13% with SC and 24% with IV
- Nausea—38% with SC and 35% with IV
- Vomiting—21% with SC and 22% with IV
- Pyrexia—32% with SC and 25% with IV
- Injection-site erythema—26% with SC and 0% with IV.
Local cutaneous reactions were reported in 42% of patients in the SC arm. The most common of these were injection-site erythema (26%) and injection-site pain (16%).
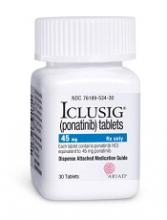
Ponatinib efficacy maintained despite dose reductions
Final results from the phase 2 PACE trial suggest dose reductions did not have an effect on the efficacy of ponatinib in patients with chronic phase (CP) chronic myeloid leukemia (CML).
Trial investigators began reducing ponatinib doses after the drug was linked to arterial occlusive events (AOEs).
Most patients who achieved a major molecular response (MMR) or major cytogenetic response (MCyR) on higher doses of ponatinib maintained those responses after dose reductions.
These results were published in Blood. The trial was sponsored by Ariad Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Earlier results from the PACE trial indicated that ponatinib increased a patient’s risk of vascular occlusive events (VOEs), including AOEs.
Therefore, in October 2013, a phase 3 trial of ponatinib was discontinued, and all other ponatinib trials were put on partial clinical hold. Trial enrollment was halted temporarily, and investigators began reducing ponatinib doses.
Then, the US Food and Drug Administration suspended sales and marketing of ponatinib, pending results of a safety evaluation.
However, in December 2013, the agency decided ponatinib could return to the market if new safety measures were implemented. In January 2014, the drug was back on the market.
Patients
The PACE trial included 449 patients with CML or acute lymphoblastic leukemia, but the results published in Blood focused only on patients with CP-CML. All of these patients were resistant or intolerant to dasatinib or nilotinib, or they had the BCR-ABLT315I mutation.
There were 270 patients with CP-CML. They had a median age of 60 (range, 18-94), and 47% were female.
Ninety-three percent had received at least 2 prior approved tyrosine kinase inhibitors (TKIs), and 57% had received at least 3. The median duration of prior TKI treatment was 5.4 years (range, 0.4-13.3).
Eighty percent of patients were resistant to dasatinib or nilotinib, 14% were intolerant to either drug, and 19% were both resistant and intolerant. Twenty-four percent of patients had the T315I mutation.
Treatment
The starting dose of ponatinib was 45 mg once daily. Doses were reduced to 30 mg or 15 mg once daily to manage adverse events (AEs), or reductions were implemented proactively (starting on October 10, 2013) due to concerns about VOEs.
Unless a benefit-risk analysis justified use of a higher dose, the recommendation for CP-CML patients was a 15 mg daily dose for those with an MCyR and a 30 mg daily dose for those without an MCyR.
Patients received ponatinib until disease progression, intolerance, or the patient or investigator decided to stop treatment.
The median duration of treatment was 32.1 months (range, 0.1-73.0), and the median follow-up was 56.8 months (range, 0.1-73.1).
Efficacy
Of the 267 evaluable patients, 60% achieved an MCyR at any time, with 54% achieving a complete cytogenetic response. Forty-eight percent of patients were still in MCyR at the last response assessment, and 82% of patients who achieved an MCyR were estimated to remain in MCyR at 5 years.
There were 69 patients in MCyR as of October 10, 2013, when pre-emptive dose reduction began, who had their dose reduced. Ninety-six percent of these patients (n=66) maintained MCyR after dose reduction. Of the 34 patients in MCyR who did not have pre-emptive dose reductions, 94% (n=32) maintained MCyR.
Forty percent of patients attained a major molecular response (MMR) at any time during the study, with 30% achieving MR4 and 24% achieving MR4.5. Thirty percent of patients were in MMR at the last response assessment, and 59% of patients who achieved MMR were estimated to remain in MMR at 5 years.
There were 52 patients in MMR as of October 10, 2013, who had their dose reduced. Ninety percent (n=47) of these patients maintained MMR following dose reduction. Of the 19 patients in MMR who did not have pre-emptive dose reductions, 95% (n=18) maintained MMR.
“The PACE trial is among the longest and largest studies of patients with CP-CML who have received 2 or 3 prior TKIs, and the findings provide treating physicians with important updated information . . . ,” said study author Jorge Eduardo Cortes, MD, of MD Anderson Cancer Center in Houston, Texas.
“These final PACE results demonstrate that [ponatinib] provides lasting clinically meaningful responses, irrespective of dose reductions, in this population.”
At 5 years, the progression-free survival rate was 53%, and the overall survival rate was 73%.
AOEs
The incidence of AOEs was 31%, and the incidence of serious AOEs was 26%. This included cardiovascular AOEs (16%, 12% serious), cerebrovascular (13%, 10% serious), and peripheral vascular AOEs (14%, 11% serious). The exposure-adjusted incidence of AOEs was 14.1 per 100 patient-years.
Among patients without AOEs prior to October 2013 when pre-emptive dose reductions began, the incidence of AOEs was 19% in patients who had dose reductions and 18% in patients who did not.
The cumulative incidence of AOEs increased over time, but the exposure-adjusted incidence of new AOEs did not. It was 15.8 per 100 patient-years in year 1 and 4.9 per 100 patient-years in year 5.
The investigators said the lack of increase in exposure-adjusted AOE incidence could be due to the natural history or etiology of AOEs, dose reductions, or a change in the patient population (ie, an enrichment of patients who may have a lower risk of vascular events).
Therefore, it is unclear whether lower doses of ponatinib reduce the risk of AOEs in patients with risk factors. However, AOEs appear to be dose-related and modified by pre-existing cardiovascular disease and other risk factors.
Venous thromboembolism (VTE), on the other hand, does not seem to be dose-related. The investigators said the rate of VTE in this study was consistent with rates typically observed in cancer patients.
The incidence of VTE was 6%, and 5% of patients had serious VTEs. The exposure-adjusted incidence of VTEs was 2.1 per 100 patient-years.
Other AEs
The most common any-grade treatment-emergent AEs (≥40%) were rash (47%), abdominal pain (46%), thrombocytopenia (46%), headache (43%), dry skin (42%), and constipation (41%).
The most common grade 3/4 treatment-emergent AEs (≥10%) were thrombocytopenia (35%), neutropenia (17%), hypertension (14%), increased lipase (13%), abdominal pain (10%), and anemia (10%).
Serious AEs (≥5%) included pancreatitis (7%), atrial fibrillation (6%), pneumonia (6%), and angina pectoris (5%).
There were 12 deaths (4%) that occurred on study or within 30 days of the end of study treatment. Two deaths were considered possibly or probably related to ponatinib, 1 due to pneumonia and 1 due to acute myocardial infarction.
Final results from the phase 2 PACE trial suggest dose reductions did not have an effect on the efficacy of ponatinib in patients with chronic phase (CP) chronic myeloid leukemia (CML).
Trial investigators began reducing ponatinib doses after the drug was linked to arterial occlusive events (AOEs).
Most patients who achieved a major molecular response (MMR) or major cytogenetic response (MCyR) on higher doses of ponatinib maintained those responses after dose reductions.
These results were published in Blood. The trial was sponsored by Ariad Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Earlier results from the PACE trial indicated that ponatinib increased a patient’s risk of vascular occlusive events (VOEs), including AOEs.
Therefore, in October 2013, a phase 3 trial of ponatinib was discontinued, and all other ponatinib trials were put on partial clinical hold. Trial enrollment was halted temporarily, and investigators began reducing ponatinib doses.
Then, the US Food and Drug Administration suspended sales and marketing of ponatinib, pending results of a safety evaluation.
However, in December 2013, the agency decided ponatinib could return to the market if new safety measures were implemented. In January 2014, the drug was back on the market.
Patients
The PACE trial included 449 patients with CML or acute lymphoblastic leukemia, but the results published in Blood focused only on patients with CP-CML. All of these patients were resistant or intolerant to dasatinib or nilotinib, or they had the BCR-ABLT315I mutation.
There were 270 patients with CP-CML. They had a median age of 60 (range, 18-94), and 47% were female.
Ninety-three percent had received at least 2 prior approved tyrosine kinase inhibitors (TKIs), and 57% had received at least 3. The median duration of prior TKI treatment was 5.4 years (range, 0.4-13.3).
Eighty percent of patients were resistant to dasatinib or nilotinib, 14% were intolerant to either drug, and 19% were both resistant and intolerant. Twenty-four percent of patients had the T315I mutation.
Treatment
The starting dose of ponatinib was 45 mg once daily. Doses were reduced to 30 mg or 15 mg once daily to manage adverse events (AEs), or reductions were implemented proactively (starting on October 10, 2013) due to concerns about VOEs.
Unless a benefit-risk analysis justified use of a higher dose, the recommendation for CP-CML patients was a 15 mg daily dose for those with an MCyR and a 30 mg daily dose for those without an MCyR.
Patients received ponatinib until disease progression, intolerance, or the patient or investigator decided to stop treatment.
The median duration of treatment was 32.1 months (range, 0.1-73.0), and the median follow-up was 56.8 months (range, 0.1-73.1).
Efficacy
Of the 267 evaluable patients, 60% achieved an MCyR at any time, with 54% achieving a complete cytogenetic response. Forty-eight percent of patients were still in MCyR at the last response assessment, and 82% of patients who achieved an MCyR were estimated to remain in MCyR at 5 years.
There were 69 patients in MCyR as of October 10, 2013, when pre-emptive dose reduction began, who had their dose reduced. Ninety-six percent of these patients (n=66) maintained MCyR after dose reduction. Of the 34 patients in MCyR who did not have pre-emptive dose reductions, 94% (n=32) maintained MCyR.
Forty percent of patients attained a major molecular response (MMR) at any time during the study, with 30% achieving MR4 and 24% achieving MR4.5. Thirty percent of patients were in MMR at the last response assessment, and 59% of patients who achieved MMR were estimated to remain in MMR at 5 years.
There were 52 patients in MMR as of October 10, 2013, who had their dose reduced. Ninety percent (n=47) of these patients maintained MMR following dose reduction. Of the 19 patients in MMR who did not have pre-emptive dose reductions, 95% (n=18) maintained MMR.
“The PACE trial is among the longest and largest studies of patients with CP-CML who have received 2 or 3 prior TKIs, and the findings provide treating physicians with important updated information . . . ,” said study author Jorge Eduardo Cortes, MD, of MD Anderson Cancer Center in Houston, Texas.
“These final PACE results demonstrate that [ponatinib] provides lasting clinically meaningful responses, irrespective of dose reductions, in this population.”
At 5 years, the progression-free survival rate was 53%, and the overall survival rate was 73%.
AOEs
The incidence of AOEs was 31%, and the incidence of serious AOEs was 26%. This included cardiovascular AOEs (16%, 12% serious), cerebrovascular (13%, 10% serious), and peripheral vascular AOEs (14%, 11% serious). The exposure-adjusted incidence of AOEs was 14.1 per 100 patient-years.
Among patients without AOEs prior to October 2013 when pre-emptive dose reductions began, the incidence of AOEs was 19% in patients who had dose reductions and 18% in patients who did not.
The cumulative incidence of AOEs increased over time, but the exposure-adjusted incidence of new AOEs did not. It was 15.8 per 100 patient-years in year 1 and 4.9 per 100 patient-years in year 5.
The investigators said the lack of increase in exposure-adjusted AOE incidence could be due to the natural history or etiology of AOEs, dose reductions, or a change in the patient population (ie, an enrichment of patients who may have a lower risk of vascular events).
Therefore, it is unclear whether lower doses of ponatinib reduce the risk of AOEs in patients with risk factors. However, AOEs appear to be dose-related and modified by pre-existing cardiovascular disease and other risk factors.
Venous thromboembolism (VTE), on the other hand, does not seem to be dose-related. The investigators said the rate of VTE in this study was consistent with rates typically observed in cancer patients.
The incidence of VTE was 6%, and 5% of patients had serious VTEs. The exposure-adjusted incidence of VTEs was 2.1 per 100 patient-years.
Other AEs
The most common any-grade treatment-emergent AEs (≥40%) were rash (47%), abdominal pain (46%), thrombocytopenia (46%), headache (43%), dry skin (42%), and constipation (41%).
The most common grade 3/4 treatment-emergent AEs (≥10%) were thrombocytopenia (35%), neutropenia (17%), hypertension (14%), increased lipase (13%), abdominal pain (10%), and anemia (10%).
Serious AEs (≥5%) included pancreatitis (7%), atrial fibrillation (6%), pneumonia (6%), and angina pectoris (5%).
There were 12 deaths (4%) that occurred on study or within 30 days of the end of study treatment. Two deaths were considered possibly or probably related to ponatinib, 1 due to pneumonia and 1 due to acute myocardial infarction.
Final results from the phase 2 PACE trial suggest dose reductions did not have an effect on the efficacy of ponatinib in patients with chronic phase (CP) chronic myeloid leukemia (CML).
Trial investigators began reducing ponatinib doses after the drug was linked to arterial occlusive events (AOEs).
Most patients who achieved a major molecular response (MMR) or major cytogenetic response (MCyR) on higher doses of ponatinib maintained those responses after dose reductions.
These results were published in Blood. The trial was sponsored by Ariad Pharmaceuticals, Inc., a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Earlier results from the PACE trial indicated that ponatinib increased a patient’s risk of vascular occlusive events (VOEs), including AOEs.
Therefore, in October 2013, a phase 3 trial of ponatinib was discontinued, and all other ponatinib trials were put on partial clinical hold. Trial enrollment was halted temporarily, and investigators began reducing ponatinib doses.
Then, the US Food and Drug Administration suspended sales and marketing of ponatinib, pending results of a safety evaluation.
However, in December 2013, the agency decided ponatinib could return to the market if new safety measures were implemented. In January 2014, the drug was back on the market.
Patients
The PACE trial included 449 patients with CML or acute lymphoblastic leukemia, but the results published in Blood focused only on patients with CP-CML. All of these patients were resistant or intolerant to dasatinib or nilotinib, or they had the BCR-ABLT315I mutation.
There were 270 patients with CP-CML. They had a median age of 60 (range, 18-94), and 47% were female.
Ninety-three percent had received at least 2 prior approved tyrosine kinase inhibitors (TKIs), and 57% had received at least 3. The median duration of prior TKI treatment was 5.4 years (range, 0.4-13.3).
Eighty percent of patients were resistant to dasatinib or nilotinib, 14% were intolerant to either drug, and 19% were both resistant and intolerant. Twenty-four percent of patients had the T315I mutation.
Treatment
The starting dose of ponatinib was 45 mg once daily. Doses were reduced to 30 mg or 15 mg once daily to manage adverse events (AEs), or reductions were implemented proactively (starting on October 10, 2013) due to concerns about VOEs.
Unless a benefit-risk analysis justified use of a higher dose, the recommendation for CP-CML patients was a 15 mg daily dose for those with an MCyR and a 30 mg daily dose for those without an MCyR.
Patients received ponatinib until disease progression, intolerance, or the patient or investigator decided to stop treatment.
The median duration of treatment was 32.1 months (range, 0.1-73.0), and the median follow-up was 56.8 months (range, 0.1-73.1).
Efficacy
Of the 267 evaluable patients, 60% achieved an MCyR at any time, with 54% achieving a complete cytogenetic response. Forty-eight percent of patients were still in MCyR at the last response assessment, and 82% of patients who achieved an MCyR were estimated to remain in MCyR at 5 years.
There were 69 patients in MCyR as of October 10, 2013, when pre-emptive dose reduction began, who had their dose reduced. Ninety-six percent of these patients (n=66) maintained MCyR after dose reduction. Of the 34 patients in MCyR who did not have pre-emptive dose reductions, 94% (n=32) maintained MCyR.
Forty percent of patients attained a major molecular response (MMR) at any time during the study, with 30% achieving MR4 and 24% achieving MR4.5. Thirty percent of patients were in MMR at the last response assessment, and 59% of patients who achieved MMR were estimated to remain in MMR at 5 years.
There were 52 patients in MMR as of October 10, 2013, who had their dose reduced. Ninety percent (n=47) of these patients maintained MMR following dose reduction. Of the 19 patients in MMR who did not have pre-emptive dose reductions, 95% (n=18) maintained MMR.
“The PACE trial is among the longest and largest studies of patients with CP-CML who have received 2 or 3 prior TKIs, and the findings provide treating physicians with important updated information . . . ,” said study author Jorge Eduardo Cortes, MD, of MD Anderson Cancer Center in Houston, Texas.
“These final PACE results demonstrate that [ponatinib] provides lasting clinically meaningful responses, irrespective of dose reductions, in this population.”
At 5 years, the progression-free survival rate was 53%, and the overall survival rate was 73%.
AOEs
The incidence of AOEs was 31%, and the incidence of serious AOEs was 26%. This included cardiovascular AOEs (16%, 12% serious), cerebrovascular (13%, 10% serious), and peripheral vascular AOEs (14%, 11% serious). The exposure-adjusted incidence of AOEs was 14.1 per 100 patient-years.
Among patients without AOEs prior to October 2013 when pre-emptive dose reductions began, the incidence of AOEs was 19% in patients who had dose reductions and 18% in patients who did not.
The cumulative incidence of AOEs increased over time, but the exposure-adjusted incidence of new AOEs did not. It was 15.8 per 100 patient-years in year 1 and 4.9 per 100 patient-years in year 5.
The investigators said the lack of increase in exposure-adjusted AOE incidence could be due to the natural history or etiology of AOEs, dose reductions, or a change in the patient population (ie, an enrichment of patients who may have a lower risk of vascular events).
Therefore, it is unclear whether lower doses of ponatinib reduce the risk of AOEs in patients with risk factors. However, AOEs appear to be dose-related and modified by pre-existing cardiovascular disease and other risk factors.
Venous thromboembolism (VTE), on the other hand, does not seem to be dose-related. The investigators said the rate of VTE in this study was consistent with rates typically observed in cancer patients.
The incidence of VTE was 6%, and 5% of patients had serious VTEs. The exposure-adjusted incidence of VTEs was 2.1 per 100 patient-years.
Other AEs
The most common any-grade treatment-emergent AEs (≥40%) were rash (47%), abdominal pain (46%), thrombocytopenia (46%), headache (43%), dry skin (42%), and constipation (41%).
The most common grade 3/4 treatment-emergent AEs (≥10%) were thrombocytopenia (35%), neutropenia (17%), hypertension (14%), increased lipase (13%), abdominal pain (10%), and anemia (10%).
Serious AEs (≥5%) included pancreatitis (7%), atrial fibrillation (6%), pneumonia (6%), and angina pectoris (5%).
There were 12 deaths (4%) that occurred on study or within 30 days of the end of study treatment. Two deaths were considered possibly or probably related to ponatinib, 1 due to pneumonia and 1 due to acute myocardial infarction.
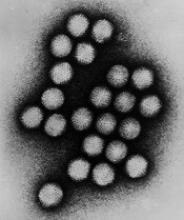
Kids may have higher rate of AdV infection after HSCT
LISBON—Results of a large study revealed a higher incidence of adenovirus (AdV) infection after allogeneic hematopoietic stem cell transplant (allo-HSCT) in children than adults.
The rate of AdV infection in the 6 months after allo-HSCT was 32% in children and 6% in adults.
However, researchers believe this data may be influenced by a lack of routine AdV screening in adults.
These findings—from the AdVance study—were reported at the 44th Annual Meeting of the EBMT as abstracts OS9-7 and B043.*
Other results from AdVance were also presented at the meeting, with mortality data reported as abstract OS9-8 and hospitalization data reported as abstract B073. The AdVance study was sponsored by Chimerix, Inc.
“The robust findings of the AdVance study are extremely important for transplant clinicians, as we seek to better understand the rates and clinical outcomes of adenovirus infection and assess ways to evaluate antiviral therapies,” said study investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients—1738 pediatric patients and 2538 adults. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Abstract OS9-7: Incidence
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT, and 23% (n=395) developed detectable AdV viremia. Fourteen percent (n=241) had AdV viremia ≥ 1000 copies/mL, a level previously associated with negative clinical outcomes.
Meanwhile, 6% (n=141) of adults had an AdV infection in the 6 months after transplant, 3% (n=77) developed AdV viremia, and 2% (n=39) had ≥ 1000 copies /mL.
Further analysis revealed that age, donor type, and use of T-cell depletion were independent predictors of AdV viremia ≥ 1000 copies/mL.
Older age was associated with a lower risk of AdV viremia ≥ 1000 copies/mL. There was a stepwise reduction in risk with increasing age (compared to ages 0-2, P=0.104 for ages 2-12, P=0.001 for ages 13-17, and P<0.0001 for ages 18-65+).
T-cell depletion was associated with an increased risk of AdV viremia ≥ 1000 copies/mL. Compared to no T-cell depletion, there was an increased risk for depletion with antithymocyte globulin (P=0.036) or alemtuzumab (P<0.0001) and for ex vivo depletion (P=0.002).
Compared to patients who received a matched related transplant, recipients of other transplants had an increased risk of AdV viremia ≥ 1000 copies/mL. This includes matched unrelated (P=0.016), cord blood (P=0.011), haploidentical (P=0.007), and mismatched (P<0.001) transplants.
Abstract B043: Screening
Dr Zecca and his colleagues believe the difference in AdV incidence between children and adults may have been affected by a lack of routine screening in adults.
To assess the use of screening, the investigators analyzed practice surveys from physicians at centers included in the AdVance study. There were 28 survey respondents who treat pediatric patients and 14 who treat adults.
All 28 physicians treating pediatric patients said there is routine AdV screening at their center. Ninety-three percent of these doctors said they routinely screen all pediatric allo-HSCT recipients for AdV infection. The remaining 7% said they screen patients considered to be at high-risk of AdV infection.
Thirty-six percent of the physicians treating adults (5/14) said they routinely screen for AdV, and 21% (3/14) said they routinely screen all of their adult allo-HSCT recipients for AdV infection.
Of the 11 doctors who said they did not routinely screen adult allo-HSCT recipients, some said they would screen recipients with a high-risk of AdV infection, such as those with graft-versus-host disease (4/11) or those who received haploidentical, mismatched, or cord blood transplants (3/11).
*Data in the abstracts differ from the presentations.
LISBON—Results of a large study revealed a higher incidence of adenovirus (AdV) infection after allogeneic hematopoietic stem cell transplant (allo-HSCT) in children than adults.
The rate of AdV infection in the 6 months after allo-HSCT was 32% in children and 6% in adults.
However, researchers believe this data may be influenced by a lack of routine AdV screening in adults.
These findings—from the AdVance study—were reported at the 44th Annual Meeting of the EBMT as abstracts OS9-7 and B043.*
Other results from AdVance were also presented at the meeting, with mortality data reported as abstract OS9-8 and hospitalization data reported as abstract B073. The AdVance study was sponsored by Chimerix, Inc.
“The robust findings of the AdVance study are extremely important for transplant clinicians, as we seek to better understand the rates and clinical outcomes of adenovirus infection and assess ways to evaluate antiviral therapies,” said study investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients—1738 pediatric patients and 2538 adults. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Abstract OS9-7: Incidence
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT, and 23% (n=395) developed detectable AdV viremia. Fourteen percent (n=241) had AdV viremia ≥ 1000 copies/mL, a level previously associated with negative clinical outcomes.
Meanwhile, 6% (n=141) of adults had an AdV infection in the 6 months after transplant, 3% (n=77) developed AdV viremia, and 2% (n=39) had ≥ 1000 copies /mL.
Further analysis revealed that age, donor type, and use of T-cell depletion were independent predictors of AdV viremia ≥ 1000 copies/mL.
Older age was associated with a lower risk of AdV viremia ≥ 1000 copies/mL. There was a stepwise reduction in risk with increasing age (compared to ages 0-2, P=0.104 for ages 2-12, P=0.001 for ages 13-17, and P<0.0001 for ages 18-65+).
T-cell depletion was associated with an increased risk of AdV viremia ≥ 1000 copies/mL. Compared to no T-cell depletion, there was an increased risk for depletion with antithymocyte globulin (P=0.036) or alemtuzumab (P<0.0001) and for ex vivo depletion (P=0.002).
Compared to patients who received a matched related transplant, recipients of other transplants had an increased risk of AdV viremia ≥ 1000 copies/mL. This includes matched unrelated (P=0.016), cord blood (P=0.011), haploidentical (P=0.007), and mismatched (P<0.001) transplants.
Abstract B043: Screening
Dr Zecca and his colleagues believe the difference in AdV incidence between children and adults may have been affected by a lack of routine screening in adults.
To assess the use of screening, the investigators analyzed practice surveys from physicians at centers included in the AdVance study. There were 28 survey respondents who treat pediatric patients and 14 who treat adults.
All 28 physicians treating pediatric patients said there is routine AdV screening at their center. Ninety-three percent of these doctors said they routinely screen all pediatric allo-HSCT recipients for AdV infection. The remaining 7% said they screen patients considered to be at high-risk of AdV infection.
Thirty-six percent of the physicians treating adults (5/14) said they routinely screen for AdV, and 21% (3/14) said they routinely screen all of their adult allo-HSCT recipients for AdV infection.
Of the 11 doctors who said they did not routinely screen adult allo-HSCT recipients, some said they would screen recipients with a high-risk of AdV infection, such as those with graft-versus-host disease (4/11) or those who received haploidentical, mismatched, or cord blood transplants (3/11).
*Data in the abstracts differ from the presentations.
LISBON—Results of a large study revealed a higher incidence of adenovirus (AdV) infection after allogeneic hematopoietic stem cell transplant (allo-HSCT) in children than adults.
The rate of AdV infection in the 6 months after allo-HSCT was 32% in children and 6% in adults.
However, researchers believe this data may be influenced by a lack of routine AdV screening in adults.
These findings—from the AdVance study—were reported at the 44th Annual Meeting of the EBMT as abstracts OS9-7 and B043.*
Other results from AdVance were also presented at the meeting, with mortality data reported as abstract OS9-8 and hospitalization data reported as abstract B073. The AdVance study was sponsored by Chimerix, Inc.
“The robust findings of the AdVance study are extremely important for transplant clinicians, as we seek to better understand the rates and clinical outcomes of adenovirus infection and assess ways to evaluate antiviral therapies,” said study investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients—1738 pediatric patients and 2538 adults. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Abstract OS9-7: Incidence
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT, and 23% (n=395) developed detectable AdV viremia. Fourteen percent (n=241) had AdV viremia ≥ 1000 copies/mL, a level previously associated with negative clinical outcomes.
Meanwhile, 6% (n=141) of adults had an AdV infection in the 6 months after transplant, 3% (n=77) developed AdV viremia, and 2% (n=39) had ≥ 1000 copies /mL.
Further analysis revealed that age, donor type, and use of T-cell depletion were independent predictors of AdV viremia ≥ 1000 copies/mL.
Older age was associated with a lower risk of AdV viremia ≥ 1000 copies/mL. There was a stepwise reduction in risk with increasing age (compared to ages 0-2, P=0.104 for ages 2-12, P=0.001 for ages 13-17, and P<0.0001 for ages 18-65+).
T-cell depletion was associated with an increased risk of AdV viremia ≥ 1000 copies/mL. Compared to no T-cell depletion, there was an increased risk for depletion with antithymocyte globulin (P=0.036) or alemtuzumab (P<0.0001) and for ex vivo depletion (P=0.002).
Compared to patients who received a matched related transplant, recipients of other transplants had an increased risk of AdV viremia ≥ 1000 copies/mL. This includes matched unrelated (P=0.016), cord blood (P=0.011), haploidentical (P=0.007), and mismatched (P<0.001) transplants.
Abstract B043: Screening
Dr Zecca and his colleagues believe the difference in AdV incidence between children and adults may have been affected by a lack of routine screening in adults.
To assess the use of screening, the investigators analyzed practice surveys from physicians at centers included in the AdVance study. There were 28 survey respondents who treat pediatric patients and 14 who treat adults.
All 28 physicians treating pediatric patients said there is routine AdV screening at their center. Ninety-three percent of these doctors said they routinely screen all pediatric allo-HSCT recipients for AdV infection. The remaining 7% said they screen patients considered to be at high-risk of AdV infection.
Thirty-six percent of the physicians treating adults (5/14) said they routinely screen for AdV, and 21% (3/14) said they routinely screen all of their adult allo-HSCT recipients for AdV infection.
Of the 11 doctors who said they did not routinely screen adult allo-HSCT recipients, some said they would screen recipients with a high-risk of AdV infection, such as those with graft-versus-host disease (4/11) or those who received haploidentical, mismatched, or cord blood transplants (3/11).
*Data in the abstracts differ from the presentations.
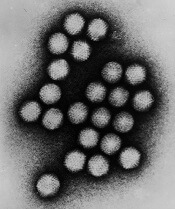
AdV viral burden linked to mortality in kids
LISBON—Data from the AdVance study revealed a “strong correlation” between adenovirus (AdV) viral load and mortality in pediatric recipients of allogeneic hematopoietic stem cell transplant (allo-HSCT), according to researchers.
The team found that patients with the highest AdV viral burden had roughly 12 times the risk of all-cause mortality as patients with the lowest viral burden.
These findings were presented at the 44th Annual Meeting of the EBMT (abstract OS9-8).*
Other findings from AdVance were also reported at the meeting (abstracts OS9-7 and B043 as well as B073). The study was sponsored by Chimerix, Inc.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients, including 1738 pediatric patients. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT. Twenty-three percent (n=395) developed detectable AdV viremia, and 14% (n=241) had AdV viremia ≥ 1000 copies/mL.
The researchers assessed AdV plasma viral burden, measured by time-averaged area under the curve (AAUC) over 16 weeks from the time of viremia ≥ 1000 copies/mL, and its correlation with all-cause mortality.
“[T]he highest mortality was observed in those with the greatest adenovirus burden,” said AdVance investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
He and his colleagues divided patients into 4 quartiles according to AdV AAUC, with the third and fourth quartiles reflecting higher, more prolonged AdV viremia.
Rates of all-cause mortality at 6 months (from the first viremia ≥ 1000 copies/mL) were 52% in the fourth quartile, 10% in the third, 7% in the second, and 3% in the first quartile.
Forty percent of patients in the fourth quartile died within 2 months of transplant.
The hazard ratio for mortality was 11.7 in the fourth quartile, 2.7 in the third, and 1.5 in the second, with the first quartile as the reference.
“These data suggest that AdV AAUC is an appropriate endpoint to assess the potential benefits of antiviral therapies for the treatment of adenovirus,” Dr Zecca concluded.
*Data in the abstract differ from the presentation.
LISBON—Data from the AdVance study revealed a “strong correlation” between adenovirus (AdV) viral load and mortality in pediatric recipients of allogeneic hematopoietic stem cell transplant (allo-HSCT), according to researchers.
The team found that patients with the highest AdV viral burden had roughly 12 times the risk of all-cause mortality as patients with the lowest viral burden.
These findings were presented at the 44th Annual Meeting of the EBMT (abstract OS9-8).*
Other findings from AdVance were also reported at the meeting (abstracts OS9-7 and B043 as well as B073). The study was sponsored by Chimerix, Inc.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients, including 1738 pediatric patients. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT. Twenty-three percent (n=395) developed detectable AdV viremia, and 14% (n=241) had AdV viremia ≥ 1000 copies/mL.
The researchers assessed AdV plasma viral burden, measured by time-averaged area under the curve (AAUC) over 16 weeks from the time of viremia ≥ 1000 copies/mL, and its correlation with all-cause mortality.
“[T]he highest mortality was observed in those with the greatest adenovirus burden,” said AdVance investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
He and his colleagues divided patients into 4 quartiles according to AdV AAUC, with the third and fourth quartiles reflecting higher, more prolonged AdV viremia.
Rates of all-cause mortality at 6 months (from the first viremia ≥ 1000 copies/mL) were 52% in the fourth quartile, 10% in the third, 7% in the second, and 3% in the first quartile.
Forty percent of patients in the fourth quartile died within 2 months of transplant.
The hazard ratio for mortality was 11.7 in the fourth quartile, 2.7 in the third, and 1.5 in the second, with the first quartile as the reference.
“These data suggest that AdV AAUC is an appropriate endpoint to assess the potential benefits of antiviral therapies for the treatment of adenovirus,” Dr Zecca concluded.
*Data in the abstract differ from the presentation.
LISBON—Data from the AdVance study revealed a “strong correlation” between adenovirus (AdV) viral load and mortality in pediatric recipients of allogeneic hematopoietic stem cell transplant (allo-HSCT), according to researchers.
The team found that patients with the highest AdV viral burden had roughly 12 times the risk of all-cause mortality as patients with the lowest viral burden.
These findings were presented at the 44th Annual Meeting of the EBMT (abstract OS9-8).*
Other findings from AdVance were also reported at the meeting (abstracts OS9-7 and B043 as well as B073). The study was sponsored by Chimerix, Inc.
AdVance is a multi-center, retrospective study of 4276 allo-HSCT recipients, including 1738 pediatric patients. The patients underwent transplants at 50 centers in Europe from January 2013 to September 2015.
Thirty-two percent (n=558) of pediatric patients developed an AdV infection in the first 6 months after allo-HSCT. Twenty-three percent (n=395) developed detectable AdV viremia, and 14% (n=241) had AdV viremia ≥ 1000 copies/mL.
The researchers assessed AdV plasma viral burden, measured by time-averaged area under the curve (AAUC) over 16 weeks from the time of viremia ≥ 1000 copies/mL, and its correlation with all-cause mortality.
“[T]he highest mortality was observed in those with the greatest adenovirus burden,” said AdVance investigator Marco Zecca, MD, of Fondazione IRCCS Policlinico San Matteo in Pavia, Italy.
He and his colleagues divided patients into 4 quartiles according to AdV AAUC, with the third and fourth quartiles reflecting higher, more prolonged AdV viremia.
Rates of all-cause mortality at 6 months (from the first viremia ≥ 1000 copies/mL) were 52% in the fourth quartile, 10% in the third, 7% in the second, and 3% in the first quartile.
Forty percent of patients in the fourth quartile died within 2 months of transplant.
The hazard ratio for mortality was 11.7 in the fourth quartile, 2.7 in the third, and 1.5 in the second, with the first quartile as the reference.
“These data suggest that AdV AAUC is an appropriate endpoint to assess the potential benefits of antiviral therapies for the treatment of adenovirus,” Dr Zecca concluded.
*Data in the abstract differ from the presentation.
FDA releases updates on BIA-ALCL
The US Food and Drug Administration (FDA) has released new information on breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The agency said it is now aware of 414 cases of BIA-ALCL, which includes 9 patients who died.
In addition, the medical literature suggests that patients with textured breast implants have a lifetime risk of developing BIA-ALCL that ranges from 1 in 3817 to 1 in 30,000.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health.
“We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants. As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
Reports to FDA
Most of the BIA-ALCL cases reported to the FDA occurred in patients with textured implants (n=242), but 30 occurred in patients with smooth implants. In the remaining 173 cases, the implant surface was not specified.
There were more silicone implants (n=234) than saline implants (n=179), and there was 1 case in which the implant filling was not specified.
The patients’ median age was 53 (range, 24-90), and the median time from last implant to BIA-ALCL diagnosis was 8 years (range, 0-44).
Cases of BIA-ALCL were ALK-negative (n=124) or did not have ALK status specified (n=290). And they were CD30-positive (n=126) or did not have CD30 status specified (n=288).
The most common clinical presentation was seroma (n=203), followed by breast swelling/pain (n=101), peri-implant mass/lump (n=45), and capsular contracture (n=42). In some cases, more than one clinical presentation was listed, and there were 141 cases where clinical presentation was unspecified/uncertain.
Medical literature
The FDA said a “significant body of medical literature” on BIA-ALCL has been published since the agency’s 2011 report on this malignancy.
For the aforementioned lifetime risk estimates—1 case of BIA-ALCL in 3817 to 30,000 individuals with textured implants—the FDA cited 3 sources:
- BIA-ALCL Resources : By the numbers, and what they mean
- Breast Implant–Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk
- Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast.
Recommendations, more updates
The FDA said this updated information does not change its recommendations regarding breast implants. The agency said the decision to obtain breast implants should be made based on individual needs and with the most complete information about risks and benefits.
“We hope that this information prompts providers and patients to have important, informed conversations about breast implants and the risk of BIA-ALCL,” Dr Ashar said. “At the same time, we remain committed to working in partnership with all stakeholders to continue to study, understand, and provide updates about this important public health issue.”
The FDA is also updating the content and format of the webpage for the agency’s breast implant post-approval studies to make current information about these studies easier for patients to read and understand.
The US Food and Drug Administration (FDA) has released new information on breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The agency said it is now aware of 414 cases of BIA-ALCL, which includes 9 patients who died.
In addition, the medical literature suggests that patients with textured breast implants have a lifetime risk of developing BIA-ALCL that ranges from 1 in 3817 to 1 in 30,000.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health.
“We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants. As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
Reports to FDA
Most of the BIA-ALCL cases reported to the FDA occurred in patients with textured implants (n=242), but 30 occurred in patients with smooth implants. In the remaining 173 cases, the implant surface was not specified.
There were more silicone implants (n=234) than saline implants (n=179), and there was 1 case in which the implant filling was not specified.
The patients’ median age was 53 (range, 24-90), and the median time from last implant to BIA-ALCL diagnosis was 8 years (range, 0-44).
Cases of BIA-ALCL were ALK-negative (n=124) or did not have ALK status specified (n=290). And they were CD30-positive (n=126) or did not have CD30 status specified (n=288).
The most common clinical presentation was seroma (n=203), followed by breast swelling/pain (n=101), peri-implant mass/lump (n=45), and capsular contracture (n=42). In some cases, more than one clinical presentation was listed, and there were 141 cases where clinical presentation was unspecified/uncertain.
Medical literature
The FDA said a “significant body of medical literature” on BIA-ALCL has been published since the agency’s 2011 report on this malignancy.
For the aforementioned lifetime risk estimates—1 case of BIA-ALCL in 3817 to 30,000 individuals with textured implants—the FDA cited 3 sources:
- BIA-ALCL Resources : By the numbers, and what they mean
- Breast Implant–Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk
- Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast.
Recommendations, more updates
The FDA said this updated information does not change its recommendations regarding breast implants. The agency said the decision to obtain breast implants should be made based on individual needs and with the most complete information about risks and benefits.
“We hope that this information prompts providers and patients to have important, informed conversations about breast implants and the risk of BIA-ALCL,” Dr Ashar said. “At the same time, we remain committed to working in partnership with all stakeholders to continue to study, understand, and provide updates about this important public health issue.”
The FDA is also updating the content and format of the webpage for the agency’s breast implant post-approval studies to make current information about these studies easier for patients to read and understand.
The US Food and Drug Administration (FDA) has released new information on breast implant-associated anaplastic large-cell lymphoma (BIA-ALCL).
The agency said it is now aware of 414 cases of BIA-ALCL, which includes 9 patients who died.
In addition, the medical literature suggests that patients with textured breast implants have a lifetime risk of developing BIA-ALCL that ranges from 1 in 3817 to 1 in 30,000.
“The FDA has been closely tracking the relationship between breast implants and a rare type of non-Hodgkin’s lymphoma since we first identified this possible association,” said Binita Ashar, MD, director of the division of surgical devices in the FDA’s Center for Devices and Radiological Health.
“We’ve been working to gather additional information to better characterize and quantify the risk so that patients and providers can have more informed discussions about breast implants. As part of that effort, we are working to update and enhance the information we have on this association, including updating the total number of known cases of BIA-ALCL and the lifetime risk of developing BIA-ALCL as reported in medical literature.”
Reports to FDA
Most of the BIA-ALCL cases reported to the FDA occurred in patients with textured implants (n=242), but 30 occurred in patients with smooth implants. In the remaining 173 cases, the implant surface was not specified.
There were more silicone implants (n=234) than saline implants (n=179), and there was 1 case in which the implant filling was not specified.
The patients’ median age was 53 (range, 24-90), and the median time from last implant to BIA-ALCL diagnosis was 8 years (range, 0-44).
Cases of BIA-ALCL were ALK-negative (n=124) or did not have ALK status specified (n=290). And they were CD30-positive (n=126) or did not have CD30 status specified (n=288).
The most common clinical presentation was seroma (n=203), followed by breast swelling/pain (n=101), peri-implant mass/lump (n=45), and capsular contracture (n=42). In some cases, more than one clinical presentation was listed, and there were 141 cases where clinical presentation was unspecified/uncertain.
Medical literature
The FDA said a “significant body of medical literature” on BIA-ALCL has been published since the agency’s 2011 report on this malignancy.
For the aforementioned lifetime risk estimates—1 case of BIA-ALCL in 3817 to 30,000 individuals with textured implants—the FDA cited 3 sources:
- BIA-ALCL Resources : By the numbers, and what they mean
- Breast Implant–Associated Anaplastic Large Cell Lymphoma in Australia and New Zealand: High-Surface-Area Textured Implants Are Associated with Increased Risk
- Breast Implants and the Risk of Anaplastic Large-Cell Lymphoma in the Breast.
Recommendations, more updates
The FDA said this updated information does not change its recommendations regarding breast implants. The agency said the decision to obtain breast implants should be made based on individual needs and with the most complete information about risks and benefits.
“We hope that this information prompts providers and patients to have important, informed conversations about breast implants and the risk of BIA-ALCL,” Dr Ashar said. “At the same time, we remain committed to working in partnership with all stakeholders to continue to study, understand, and provide updates about this important public health issue.”
The FDA is also updating the content and format of the webpage for the agency’s breast implant post-approval studies to make current information about these studies easier for patients to read and understand.