User login
FDA aims to improve access to clinical trial info
The US Food and Drug Administration (FDA) says it is taking new steps to improve public access to clinical trial information.
The agency is launching a pilot program to evaluate whether releasing portions of clinical study reports (CSRs) will improve public access to drug approval information.
The FDA is also planning to add NCT numbers to FDA materials to make it easier to match listings on ClinicalTrials.gov to FDA communications.
FDA Commissioner Scott Gottlieb, MD, noted that, when a drug is approved, the FDA releases certain information the agency used when reviewing the new drug application (NDA).
This includes summaries written by medical reviewers that capture their assessment of the data, the proposed labeling or other requirements, and other data supporting safe and effective use. This information is included in the drug approvals database, Drugs@FDA.
Dr Gottlieb said these summaries are packaged in a format that can sometimes make it difficult for external audiences to extract all of the detailed clinical evidence that supported the FDA’s approval decisions.
Therefore, the agency is launching a pilot program to evaluate whether disclosing certain information included in CSRs will provide stakeholders with more details on the clinical evidence supporting a drug application and more transparency into the FDA’s decision-making process.
The FDA plans to select up to 9 recently approved NDAs whose sponsors will provide portions of CSRs from trials that were submitted to the FDA.
The CSRs will be posted on a new web page on the FDA’s website that describes the pilot program, in addition to appearing on Drugs@FDA along with the drug’s approval information.
The pilot will begin this month. The FDA will soon begin contacting sponsors to see if they are interested in participating in the pilot.
The agency will provide participating sponsors with additional information to ensure their understanding of the process. The FDA also promises to protect patient privacy, trade secret, and confidential commercial information in the CSRs it releases.
Once the pilot program is complete, the FDA will seek public feedback through a Federal Register notice and docket for public comments.
To augment the CSR pilot, the FDA is adding NCT numbers to materials for future drug approvals.
The agency believes this will make it easier to associate listings on ClinicalTrials.gov with FDA communications about specific drugs, including product labeling and advisory committee meeting materials. ![]()
The US Food and Drug Administration (FDA) says it is taking new steps to improve public access to clinical trial information.
The agency is launching a pilot program to evaluate whether releasing portions of clinical study reports (CSRs) will improve public access to drug approval information.
The FDA is also planning to add NCT numbers to FDA materials to make it easier to match listings on ClinicalTrials.gov to FDA communications.
FDA Commissioner Scott Gottlieb, MD, noted that, when a drug is approved, the FDA releases certain information the agency used when reviewing the new drug application (NDA).
This includes summaries written by medical reviewers that capture their assessment of the data, the proposed labeling or other requirements, and other data supporting safe and effective use. This information is included in the drug approvals database, Drugs@FDA.
Dr Gottlieb said these summaries are packaged in a format that can sometimes make it difficult for external audiences to extract all of the detailed clinical evidence that supported the FDA’s approval decisions.
Therefore, the agency is launching a pilot program to evaluate whether disclosing certain information included in CSRs will provide stakeholders with more details on the clinical evidence supporting a drug application and more transparency into the FDA’s decision-making process.
The FDA plans to select up to 9 recently approved NDAs whose sponsors will provide portions of CSRs from trials that were submitted to the FDA.
The CSRs will be posted on a new web page on the FDA’s website that describes the pilot program, in addition to appearing on Drugs@FDA along with the drug’s approval information.
The pilot will begin this month. The FDA will soon begin contacting sponsors to see if they are interested in participating in the pilot.
The agency will provide participating sponsors with additional information to ensure their understanding of the process. The FDA also promises to protect patient privacy, trade secret, and confidential commercial information in the CSRs it releases.
Once the pilot program is complete, the FDA will seek public feedback through a Federal Register notice and docket for public comments.
To augment the CSR pilot, the FDA is adding NCT numbers to materials for future drug approvals.
The agency believes this will make it easier to associate listings on ClinicalTrials.gov with FDA communications about specific drugs, including product labeling and advisory committee meeting materials. ![]()
The US Food and Drug Administration (FDA) says it is taking new steps to improve public access to clinical trial information.
The agency is launching a pilot program to evaluate whether releasing portions of clinical study reports (CSRs) will improve public access to drug approval information.
The FDA is also planning to add NCT numbers to FDA materials to make it easier to match listings on ClinicalTrials.gov to FDA communications.
FDA Commissioner Scott Gottlieb, MD, noted that, when a drug is approved, the FDA releases certain information the agency used when reviewing the new drug application (NDA).
This includes summaries written by medical reviewers that capture their assessment of the data, the proposed labeling or other requirements, and other data supporting safe and effective use. This information is included in the drug approvals database, Drugs@FDA.
Dr Gottlieb said these summaries are packaged in a format that can sometimes make it difficult for external audiences to extract all of the detailed clinical evidence that supported the FDA’s approval decisions.
Therefore, the agency is launching a pilot program to evaluate whether disclosing certain information included in CSRs will provide stakeholders with more details on the clinical evidence supporting a drug application and more transparency into the FDA’s decision-making process.
The FDA plans to select up to 9 recently approved NDAs whose sponsors will provide portions of CSRs from trials that were submitted to the FDA.
The CSRs will be posted on a new web page on the FDA’s website that describes the pilot program, in addition to appearing on Drugs@FDA along with the drug’s approval information.
The pilot will begin this month. The FDA will soon begin contacting sponsors to see if they are interested in participating in the pilot.
The agency will provide participating sponsors with additional information to ensure their understanding of the process. The FDA also promises to protect patient privacy, trade secret, and confidential commercial information in the CSRs it releases.
Once the pilot program is complete, the FDA will seek public feedback through a Federal Register notice and docket for public comments.
To augment the CSR pilot, the FDA is adding NCT numbers to materials for future drug approvals.
The agency believes this will make it easier to associate listings on ClinicalTrials.gov with FDA communications about specific drugs, including product labeling and advisory committee meeting materials. ![]()
Drug’s label updated to include risk of allergic reactions
The US Food and Drug Administration (FDA) and Tesaro, Inc., have updated the prescribing information for Varubi® (rolapitant) injectable emulsion to include a new warning about the risk of allergic reactions.
Varubi injectable emulsion is a substance P/neurokinin receptor antagonist approved to prevent delayed nausea and vomiting associated with chemotherapy in adults.
Since Varubi injectable emulsion gained FDA approval, there have been reports of anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions to the drug, some of which required hospitalization.
Now, the labeling for Varubi injectable emulsion has been changed to include information about these events. The changes include modifications to the CONTRAINDICATIONS, WARNINGS and PRECAUTIONS, and ADVERSE REACTIONS sections of the label.
Since Varubi injectable emulsion was introduced to the US market in late November 2017, at least 7000 doses of the drug have been administered to patients receiving emetogenic chemotherapy in the US, according to Tesaro.
Anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions have occurred during or soon after the infusion of Varubi. Most reactions have occurred within the first few minutes of administration.
The FDA has advised that patients who are hypersensitive to any component of Varubi injectable emulsion (including soybean oil) do not receive the drug. And patients with known allergies to legumes or other related allergens should be monitored closely.
The FDA said healthcare professionals should be vigilant for signs of hypersensitivity or anaphylaxis in all patients receiving Varubi injectable emulsion, both during administration and afterward.
Symptoms of anaphylaxis can include wheezing, difficulty breathing, swelling of the face or throat, hives, flushing, itching, abdominal cramping, abdominal pain, vomiting, back pain, chest pain, hypotension, and shock.
If anaphylaxis or any other serious hypersensitivity/infusion reaction occurs, Varubi injectable emulsion should be stopped immediately and permanently. The patient should receive appropriate medical management, including epinephrine and/or antihistamines.
To ensure patients and healthcare professionals are aware of the label update to Varubi injectable emulsion, Tesaro has issued a Dear Healthcare Professional letter. In addition, the updated prescribing information has been posted on the Varubi website.
For any questions about the use of Varubi injectable emulsion or to report adverse events related to the drug, contact Tesaro’s medical information department at 1-844-4-TESARO (1-844-483-7276).
Adverse events related to Varubi should also be reported to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) and Tesaro, Inc., have updated the prescribing information for Varubi® (rolapitant) injectable emulsion to include a new warning about the risk of allergic reactions.
Varubi injectable emulsion is a substance P/neurokinin receptor antagonist approved to prevent delayed nausea and vomiting associated with chemotherapy in adults.
Since Varubi injectable emulsion gained FDA approval, there have been reports of anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions to the drug, some of which required hospitalization.
Now, the labeling for Varubi injectable emulsion has been changed to include information about these events. The changes include modifications to the CONTRAINDICATIONS, WARNINGS and PRECAUTIONS, and ADVERSE REACTIONS sections of the label.
Since Varubi injectable emulsion was introduced to the US market in late November 2017, at least 7000 doses of the drug have been administered to patients receiving emetogenic chemotherapy in the US, according to Tesaro.
Anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions have occurred during or soon after the infusion of Varubi. Most reactions have occurred within the first few minutes of administration.
The FDA has advised that patients who are hypersensitive to any component of Varubi injectable emulsion (including soybean oil) do not receive the drug. And patients with known allergies to legumes or other related allergens should be monitored closely.
The FDA said healthcare professionals should be vigilant for signs of hypersensitivity or anaphylaxis in all patients receiving Varubi injectable emulsion, both during administration and afterward.
Symptoms of anaphylaxis can include wheezing, difficulty breathing, swelling of the face or throat, hives, flushing, itching, abdominal cramping, abdominal pain, vomiting, back pain, chest pain, hypotension, and shock.
If anaphylaxis or any other serious hypersensitivity/infusion reaction occurs, Varubi injectable emulsion should be stopped immediately and permanently. The patient should receive appropriate medical management, including epinephrine and/or antihistamines.
To ensure patients and healthcare professionals are aware of the label update to Varubi injectable emulsion, Tesaro has issued a Dear Healthcare Professional letter. In addition, the updated prescribing information has been posted on the Varubi website.
For any questions about the use of Varubi injectable emulsion or to report adverse events related to the drug, contact Tesaro’s medical information department at 1-844-4-TESARO (1-844-483-7276).
Adverse events related to Varubi should also be reported to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
The US Food and Drug Administration (FDA) and Tesaro, Inc., have updated the prescribing information for Varubi® (rolapitant) injectable emulsion to include a new warning about the risk of allergic reactions.
Varubi injectable emulsion is a substance P/neurokinin receptor antagonist approved to prevent delayed nausea and vomiting associated with chemotherapy in adults.
Since Varubi injectable emulsion gained FDA approval, there have been reports of anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions to the drug, some of which required hospitalization.
Now, the labeling for Varubi injectable emulsion has been changed to include information about these events. The changes include modifications to the CONTRAINDICATIONS, WARNINGS and PRECAUTIONS, and ADVERSE REACTIONS sections of the label.
Since Varubi injectable emulsion was introduced to the US market in late November 2017, at least 7000 doses of the drug have been administered to patients receiving emetogenic chemotherapy in the US, according to Tesaro.
Anaphylaxis, anaphylactic shock, and other serious hypersensitivity reactions have occurred during or soon after the infusion of Varubi. Most reactions have occurred within the first few minutes of administration.
The FDA has advised that patients who are hypersensitive to any component of Varubi injectable emulsion (including soybean oil) do not receive the drug. And patients with known allergies to legumes or other related allergens should be monitored closely.
The FDA said healthcare professionals should be vigilant for signs of hypersensitivity or anaphylaxis in all patients receiving Varubi injectable emulsion, both during administration and afterward.
Symptoms of anaphylaxis can include wheezing, difficulty breathing, swelling of the face or throat, hives, flushing, itching, abdominal cramping, abdominal pain, vomiting, back pain, chest pain, hypotension, and shock.
If anaphylaxis or any other serious hypersensitivity/infusion reaction occurs, Varubi injectable emulsion should be stopped immediately and permanently. The patient should receive appropriate medical management, including epinephrine and/or antihistamines.
To ensure patients and healthcare professionals are aware of the label update to Varubi injectable emulsion, Tesaro has issued a Dear Healthcare Professional letter. In addition, the updated prescribing information has been posted on the Varubi website.
For any questions about the use of Varubi injectable emulsion or to report adverse events related to the drug, contact Tesaro’s medical information department at 1-844-4-TESARO (1-844-483-7276).
Adverse events related to Varubi should also be reported to the FDA’s MedWatch Safety Information and Adverse Event Reporting Program. ![]()
FDA expands approval for arsenic trioxide
The US Food and Drug Administration (FDA) has expanded the approved use of arsenic trioxide (TRISENOX®) injection.
The drug is now approved for use in combination with all-trans retinoic acid (ATRA) for the treatment of adults with newly diagnosed, low-risk acute promyelocytic leukemia (APL) whose disease is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
Arsenic trioxide is also FDA-approved for induction of remission and consolidation in patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy and whose APL is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
“This label expansion represents an important benefit, as TRISENOX is now an FDA-approved, first-line treatment option for patients with acute promyelocytic leukemia,” said Paul Rittman, senior vice-president and general manager of Teva Oncology.
The expanded approval for arsenic trioxide was based on a priority review by the FDA of data from the scientific literature and a review of Teva’s global safety database for arsenic trioxide.
Data from this database were presented at the 2016 ASH Annual Meeting.
According to the presentation, the most common adverse events observed in patients receiving arsenic trioxide were QT prolongation, decrease in white blood cells, APL differentiation syndrome, febrile neutropenia, neutropenia, pyrexia, alanine aminotransferase increase, neutrophil decrease, platelet count decrease, aspartate aminotransferase increase, leukocytosis, and pancytopenia.
The combination of arsenic trioxide and ATRA was evaluated in a phase 3 trial of patients with APL. Results from this trial were published in the Journal of Clinical Oncology in February 2017.
The study included 276 adults (ages 18 to 71) with newly diagnosed, low- or intermediate-risk APL. Patients were randomized to receive ATRA plus arsenic trioxide or ATRA plus chemotherapy.
A total of 263 patients were evaluable for response to induction. One hundred percent of patients in the arsenic trioxide arm (127/127) achieved a complete response (CR), as did 97% (132/136) of patients in the chemotherapy arm (P=0.12).
After a median follow-up of 40.6 months, the event-free survival was 97.3% in the arsenic trioxide arm and 80% in the chemotherapy arm (P<0.001). The cumulative incidence of relapse was 1.9% and 13.9%, respectively (P=0.0013).
At 50 months, the overall survival was 99.2% in the arsenic trioxide arm and 92.6% in the chemotherapy arm (P=0.0073).
After induction, there were 2 relapses and 1 death in CR in the arsenic trioxide arm.
In the chemotherapy arm, there were 2 instances of molecular resistance after third consolidation, 15 relapses, 5 deaths in CR, and 2 patients who developed a therapy-related myeloid neoplasm. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of arsenic trioxide (TRISENOX®) injection.
The drug is now approved for use in combination with all-trans retinoic acid (ATRA) for the treatment of adults with newly diagnosed, low-risk acute promyelocytic leukemia (APL) whose disease is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
Arsenic trioxide is also FDA-approved for induction of remission and consolidation in patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy and whose APL is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
“This label expansion represents an important benefit, as TRISENOX is now an FDA-approved, first-line treatment option for patients with acute promyelocytic leukemia,” said Paul Rittman, senior vice-president and general manager of Teva Oncology.
The expanded approval for arsenic trioxide was based on a priority review by the FDA of data from the scientific literature and a review of Teva’s global safety database for arsenic trioxide.
Data from this database were presented at the 2016 ASH Annual Meeting.
According to the presentation, the most common adverse events observed in patients receiving arsenic trioxide were QT prolongation, decrease in white blood cells, APL differentiation syndrome, febrile neutropenia, neutropenia, pyrexia, alanine aminotransferase increase, neutrophil decrease, platelet count decrease, aspartate aminotransferase increase, leukocytosis, and pancytopenia.
The combination of arsenic trioxide and ATRA was evaluated in a phase 3 trial of patients with APL. Results from this trial were published in the Journal of Clinical Oncology in February 2017.
The study included 276 adults (ages 18 to 71) with newly diagnosed, low- or intermediate-risk APL. Patients were randomized to receive ATRA plus arsenic trioxide or ATRA plus chemotherapy.
A total of 263 patients were evaluable for response to induction. One hundred percent of patients in the arsenic trioxide arm (127/127) achieved a complete response (CR), as did 97% (132/136) of patients in the chemotherapy arm (P=0.12).
After a median follow-up of 40.6 months, the event-free survival was 97.3% in the arsenic trioxide arm and 80% in the chemotherapy arm (P<0.001). The cumulative incidence of relapse was 1.9% and 13.9%, respectively (P=0.0013).
At 50 months, the overall survival was 99.2% in the arsenic trioxide arm and 92.6% in the chemotherapy arm (P=0.0073).
After induction, there were 2 relapses and 1 death in CR in the arsenic trioxide arm.
In the chemotherapy arm, there were 2 instances of molecular resistance after third consolidation, 15 relapses, 5 deaths in CR, and 2 patients who developed a therapy-related myeloid neoplasm. ![]()
The US Food and Drug Administration (FDA) has expanded the approved use of arsenic trioxide (TRISENOX®) injection.
The drug is now approved for use in combination with all-trans retinoic acid (ATRA) for the treatment of adults with newly diagnosed, low-risk acute promyelocytic leukemia (APL) whose disease is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
Arsenic trioxide is also FDA-approved for induction of remission and consolidation in patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy and whose APL is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
“This label expansion represents an important benefit, as TRISENOX is now an FDA-approved, first-line treatment option for patients with acute promyelocytic leukemia,” said Paul Rittman, senior vice-president and general manager of Teva Oncology.
The expanded approval for arsenic trioxide was based on a priority review by the FDA of data from the scientific literature and a review of Teva’s global safety database for arsenic trioxide.
Data from this database were presented at the 2016 ASH Annual Meeting.
According to the presentation, the most common adverse events observed in patients receiving arsenic trioxide were QT prolongation, decrease in white blood cells, APL differentiation syndrome, febrile neutropenia, neutropenia, pyrexia, alanine aminotransferase increase, neutrophil decrease, platelet count decrease, aspartate aminotransferase increase, leukocytosis, and pancytopenia.
The combination of arsenic trioxide and ATRA was evaluated in a phase 3 trial of patients with APL. Results from this trial were published in the Journal of Clinical Oncology in February 2017.
The study included 276 adults (ages 18 to 71) with newly diagnosed, low- or intermediate-risk APL. Patients were randomized to receive ATRA plus arsenic trioxide or ATRA plus chemotherapy.
A total of 263 patients were evaluable for response to induction. One hundred percent of patients in the arsenic trioxide arm (127/127) achieved a complete response (CR), as did 97% (132/136) of patients in the chemotherapy arm (P=0.12).
After a median follow-up of 40.6 months, the event-free survival was 97.3% in the arsenic trioxide arm and 80% in the chemotherapy arm (P<0.001). The cumulative incidence of relapse was 1.9% and 13.9%, respectively (P=0.0013).
At 50 months, the overall survival was 99.2% in the arsenic trioxide arm and 92.6% in the chemotherapy arm (P=0.0073).
After induction, there were 2 relapses and 1 death in CR in the arsenic trioxide arm.
In the chemotherapy arm, there were 2 instances of molecular resistance after third consolidation, 15 relapses, 5 deaths in CR, and 2 patients who developed a therapy-related myeloid neoplasm. ![]()
How a malaria parasite is evading treatment
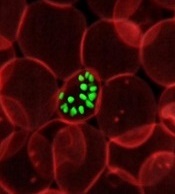
New research has revealed mutations that help the malaria parasite Plasmodium falciparum evade treatment.
Researchers used whole-genome analyses and chemogenetics to identify drug targets and resistance genes in cell lines of P falciparum that are resistant to antimalarial compounds.
The group’s work confirmed previously known mutations that contribute to the parasite’s resistance but also revealed new targets that may deepen our understanding of the parasite’s underlying biology.
“This exploration of the P falciparum resistome—the collection of antibiotic resistance genes—and its druggable genome will help guide new drug discovery efforts and advance our understanding of how the malaria parasite evolves to fight back,” said Elizabeth Winzeler, PhD, of the University of California San Diego School of Medicine.
She and her colleagues conducted this research and reported the results in Science.
“A single human [malaria] infection can result in a person containing upwards of a trillion asexual blood-stage parasites,” Dr Winzeler said. “Even with a relatively slow random mutation rate, these numbers confer extraordinary adaptability.”
“In just a few cycles of replication, the P falciparum genome can acquire a random genetic change that may render at least one parasite resistant to the activity of a drug or human-encoded antibody.”
Such rapid evolution can be exploited in vitro to document how the parasite evolves in the presence of antimalarials, and it can be used to reveal new drug targets.
With this in mind, Dr Winzeler and her colleagues performed a genome analysis of 262 P falciparum parasites resistant to 37 groups of compounds.
In 83 genes associated with drug resistance, the researchers identified hundreds of changes that could be mediating the resistance, including 159 gene amplifications and 148 nonsynonymous mutations.
The team then used clones of well-studied P falciparum parasites and exposed them to the compounds over time to induce resistance, monitoring the genetic changes that occurred as resistance developed.
The researchers were able to identify a likely target or resistance gene for every compound.
In addition, the team identified mutations that repeatedly occurred upon individual exposure to a variety of drugs, meaning these mutations are likely mediating resistance to numerous existing treatments.
“Our findings showed and underscored the challenging complexity of evolved drug resistance in P falciparum, but they also identified new drug targets or resistance genes for every compound for which resistant parasites were generated,” Dr Winzeler said.
“It revealed the complicated chemogenetic landscape of P falciparum but also provided a potential guide for designing new small-molecule inhibitors to fight this pathogen.” ![]()
New research has revealed mutations that help the malaria parasite Plasmodium falciparum evade treatment.
Researchers used whole-genome analyses and chemogenetics to identify drug targets and resistance genes in cell lines of P falciparum that are resistant to antimalarial compounds.
The group’s work confirmed previously known mutations that contribute to the parasite’s resistance but also revealed new targets that may deepen our understanding of the parasite’s underlying biology.
“This exploration of the P falciparum resistome—the collection of antibiotic resistance genes—and its druggable genome will help guide new drug discovery efforts and advance our understanding of how the malaria parasite evolves to fight back,” said Elizabeth Winzeler, PhD, of the University of California San Diego School of Medicine.
She and her colleagues conducted this research and reported the results in Science.
“A single human [malaria] infection can result in a person containing upwards of a trillion asexual blood-stage parasites,” Dr Winzeler said. “Even with a relatively slow random mutation rate, these numbers confer extraordinary adaptability.”
“In just a few cycles of replication, the P falciparum genome can acquire a random genetic change that may render at least one parasite resistant to the activity of a drug or human-encoded antibody.”
Such rapid evolution can be exploited in vitro to document how the parasite evolves in the presence of antimalarials, and it can be used to reveal new drug targets.
With this in mind, Dr Winzeler and her colleagues performed a genome analysis of 262 P falciparum parasites resistant to 37 groups of compounds.
In 83 genes associated with drug resistance, the researchers identified hundreds of changes that could be mediating the resistance, including 159 gene amplifications and 148 nonsynonymous mutations.
The team then used clones of well-studied P falciparum parasites and exposed them to the compounds over time to induce resistance, monitoring the genetic changes that occurred as resistance developed.
The researchers were able to identify a likely target or resistance gene for every compound.
In addition, the team identified mutations that repeatedly occurred upon individual exposure to a variety of drugs, meaning these mutations are likely mediating resistance to numerous existing treatments.
“Our findings showed and underscored the challenging complexity of evolved drug resistance in P falciparum, but they also identified new drug targets or resistance genes for every compound for which resistant parasites were generated,” Dr Winzeler said.
“It revealed the complicated chemogenetic landscape of P falciparum but also provided a potential guide for designing new small-molecule inhibitors to fight this pathogen.” ![]()
New research has revealed mutations that help the malaria parasite Plasmodium falciparum evade treatment.
Researchers used whole-genome analyses and chemogenetics to identify drug targets and resistance genes in cell lines of P falciparum that are resistant to antimalarial compounds.
The group’s work confirmed previously known mutations that contribute to the parasite’s resistance but also revealed new targets that may deepen our understanding of the parasite’s underlying biology.
“This exploration of the P falciparum resistome—the collection of antibiotic resistance genes—and its druggable genome will help guide new drug discovery efforts and advance our understanding of how the malaria parasite evolves to fight back,” said Elizabeth Winzeler, PhD, of the University of California San Diego School of Medicine.
She and her colleagues conducted this research and reported the results in Science.
“A single human [malaria] infection can result in a person containing upwards of a trillion asexual blood-stage parasites,” Dr Winzeler said. “Even with a relatively slow random mutation rate, these numbers confer extraordinary adaptability.”
“In just a few cycles of replication, the P falciparum genome can acquire a random genetic change that may render at least one parasite resistant to the activity of a drug or human-encoded antibody.”
Such rapid evolution can be exploited in vitro to document how the parasite evolves in the presence of antimalarials, and it can be used to reveal new drug targets.
With this in mind, Dr Winzeler and her colleagues performed a genome analysis of 262 P falciparum parasites resistant to 37 groups of compounds.
In 83 genes associated with drug resistance, the researchers identified hundreds of changes that could be mediating the resistance, including 159 gene amplifications and 148 nonsynonymous mutations.
The team then used clones of well-studied P falciparum parasites and exposed them to the compounds over time to induce resistance, monitoring the genetic changes that occurred as resistance developed.
The researchers were able to identify a likely target or resistance gene for every compound.
In addition, the team identified mutations that repeatedly occurred upon individual exposure to a variety of drugs, meaning these mutations are likely mediating resistance to numerous existing treatments.
“Our findings showed and underscored the challenging complexity of evolved drug resistance in P falciparum, but they also identified new drug targets or resistance genes for every compound for which resistant parasites were generated,” Dr Winzeler said.
“It revealed the complicated chemogenetic landscape of P falciparum but also provided a potential guide for designing new small-molecule inhibitors to fight this pathogen.” ![]()
Emicizumab still available despite legal issues
The Roche Group has issued a statement reassuring the US hemophilia community that legal issues are not affecting patient access to emicizumab (Hemlibra), at least for the time being.
Emicizumab is a bispecific factor IXa- and factor X-directed antibody approved in the US as routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults and children who have hemophilia A and factor VIII (FVIII) inhibitors.
The Roche Group—which consists of Genentech in the US, Chugai in Japan, and Roche in the rest of the world—said emicizumab is still available for these patients, despite a legal battle with Baxalta, a wholly owned subsidiary of Shire.
In May 2017, Baxalta sued Genentech and Chugai for allegedly infringing upon US Patent No. 7,033,590.
The patent covers factor IX/factor IXa antibodies and antibody derivatives. It was issued to Baxter in April 2006 and assigned to Baxalta in March 2016. The patent is still active.
According to Baxalta, Genentech and Chugai are infringing on the patent by manufacturing, selling, or importing emicizumab. Therefore, Baxalta is seeking judgment in its favor and monetary damages.
The trial for this case is scheduled for September 2019.
However, in December 2017, Baxalta filed a motion for a preliminary injunction that would prevent the sale of emicizumab in the US. If granted, the injunction would prevent the following patients from receiving emicizumab:
- Hemophilia A patients with inhibitors (an inhibitor titer of greater than 5 Bethesda units) who cannot be treated effectively with FVIII replacement therapy, unless (i) they have already started emicizumab before the injunction is granted or (ii) they have previous experience with on-demand or prophylactic bypassing agents and their needs are not being met, as defined by Shire using criteria that include experiencing certain life- or limb-threatening bleeds or venous access issues.
- Hemophilia A patients who have an inhibitor titer less than or equal to 5 Bethesda units or who can be effectively treated with FVIII replacement therapy, regardless of whether they have already started emicizumab.
- Hemophilia A patients without inhibitors, regardless of whether they have already started emicizumab.
The Roche Group said it believes Baxalta’s claim is not valid, emicizumab does not infringe upon the patent, and the group will oppose the injunction.
The court’s decision on the injunction is expected this summer. In the meantime, emicizumab is still available for the aforementioned patients. ![]()
The Roche Group has issued a statement reassuring the US hemophilia community that legal issues are not affecting patient access to emicizumab (Hemlibra), at least for the time being.
Emicizumab is a bispecific factor IXa- and factor X-directed antibody approved in the US as routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults and children who have hemophilia A and factor VIII (FVIII) inhibitors.
The Roche Group—which consists of Genentech in the US, Chugai in Japan, and Roche in the rest of the world—said emicizumab is still available for these patients, despite a legal battle with Baxalta, a wholly owned subsidiary of Shire.
In May 2017, Baxalta sued Genentech and Chugai for allegedly infringing upon US Patent No. 7,033,590.
The patent covers factor IX/factor IXa antibodies and antibody derivatives. It was issued to Baxter in April 2006 and assigned to Baxalta in March 2016. The patent is still active.
According to Baxalta, Genentech and Chugai are infringing on the patent by manufacturing, selling, or importing emicizumab. Therefore, Baxalta is seeking judgment in its favor and monetary damages.
The trial for this case is scheduled for September 2019.
However, in December 2017, Baxalta filed a motion for a preliminary injunction that would prevent the sale of emicizumab in the US. If granted, the injunction would prevent the following patients from receiving emicizumab:
- Hemophilia A patients with inhibitors (an inhibitor titer of greater than 5 Bethesda units) who cannot be treated effectively with FVIII replacement therapy, unless (i) they have already started emicizumab before the injunction is granted or (ii) they have previous experience with on-demand or prophylactic bypassing agents and their needs are not being met, as defined by Shire using criteria that include experiencing certain life- or limb-threatening bleeds or venous access issues.
- Hemophilia A patients who have an inhibitor titer less than or equal to 5 Bethesda units or who can be effectively treated with FVIII replacement therapy, regardless of whether they have already started emicizumab.
- Hemophilia A patients without inhibitors, regardless of whether they have already started emicizumab.
The Roche Group said it believes Baxalta’s claim is not valid, emicizumab does not infringe upon the patent, and the group will oppose the injunction.
The court’s decision on the injunction is expected this summer. In the meantime, emicizumab is still available for the aforementioned patients. ![]()
The Roche Group has issued a statement reassuring the US hemophilia community that legal issues are not affecting patient access to emicizumab (Hemlibra), at least for the time being.
Emicizumab is a bispecific factor IXa- and factor X-directed antibody approved in the US as routine prophylaxis to prevent or reduce the frequency of bleeding episodes in adults and children who have hemophilia A and factor VIII (FVIII) inhibitors.
The Roche Group—which consists of Genentech in the US, Chugai in Japan, and Roche in the rest of the world—said emicizumab is still available for these patients, despite a legal battle with Baxalta, a wholly owned subsidiary of Shire.
In May 2017, Baxalta sued Genentech and Chugai for allegedly infringing upon US Patent No. 7,033,590.
The patent covers factor IX/factor IXa antibodies and antibody derivatives. It was issued to Baxter in April 2006 and assigned to Baxalta in March 2016. The patent is still active.
According to Baxalta, Genentech and Chugai are infringing on the patent by manufacturing, selling, or importing emicizumab. Therefore, Baxalta is seeking judgment in its favor and monetary damages.
The trial for this case is scheduled for September 2019.
However, in December 2017, Baxalta filed a motion for a preliminary injunction that would prevent the sale of emicizumab in the US. If granted, the injunction would prevent the following patients from receiving emicizumab:
- Hemophilia A patients with inhibitors (an inhibitor titer of greater than 5 Bethesda units) who cannot be treated effectively with FVIII replacement therapy, unless (i) they have already started emicizumab before the injunction is granted or (ii) they have previous experience with on-demand or prophylactic bypassing agents and their needs are not being met, as defined by Shire using criteria that include experiencing certain life- or limb-threatening bleeds or venous access issues.
- Hemophilia A patients who have an inhibitor titer less than or equal to 5 Bethesda units or who can be effectively treated with FVIII replacement therapy, regardless of whether they have already started emicizumab.
- Hemophilia A patients without inhibitors, regardless of whether they have already started emicizumab.
The Roche Group said it believes Baxalta’s claim is not valid, emicizumab does not infringe upon the patent, and the group will oppose the injunction.
The court’s decision on the injunction is expected this summer. In the meantime, emicizumab is still available for the aforementioned patients. ![]()
Generic bortezomib available in US
Fresenius Kabi has introduced its generic version of Velcade, Bortezomib for Injection, to the US market.
This is the first intravenous alternative to Velcade available in the US.
Bortezomib for Injection is available as a single dose vial containing 3.5 mg of lyophilized powder.
The product is approved to treat patients with multiple myeloma and patients with mantle cell lymphoma who have received at least 1 prior therapy.
For details, see the prescribing information for Bortezomib for Injection.
Velcade is a registered trademark of Millennium Pharmaceuticals, Inc. ![]()
Fresenius Kabi has introduced its generic version of Velcade, Bortezomib for Injection, to the US market.
This is the first intravenous alternative to Velcade available in the US.
Bortezomib for Injection is available as a single dose vial containing 3.5 mg of lyophilized powder.
The product is approved to treat patients with multiple myeloma and patients with mantle cell lymphoma who have received at least 1 prior therapy.
For details, see the prescribing information for Bortezomib for Injection.
Velcade is a registered trademark of Millennium Pharmaceuticals, Inc. ![]()
Fresenius Kabi has introduced its generic version of Velcade, Bortezomib for Injection, to the US market.
This is the first intravenous alternative to Velcade available in the US.
Bortezomib for Injection is available as a single dose vial containing 3.5 mg of lyophilized powder.
The product is approved to treat patients with multiple myeloma and patients with mantle cell lymphoma who have received at least 1 prior therapy.
For details, see the prescribing information for Bortezomib for Injection.
Velcade is a registered trademark of Millennium Pharmaceuticals, Inc. ![]()
Interventions can increase cord blood donations
Simple interventions can increase cord blood donations, according to research published in Scientific Reports.
Researchers saw a significant increase in cord blood donation when expectant mothers received information about the procedure and were asked to indicate their interest in donating at both early and late stages of their pregnancies.
“We more than doubled the number of cord blood units that were collected,” said study author Nicola Lacetera, PhD, of the University of Toronto Mississauga in Ontario, Canada.
“We learned a lot, and we did a little bit of good too, so that feels nice.”
Dr Lacetera and his colleagues conducted this study in Milan, Italy, where private cord blood banking is banned.
The team set out to determine if providing expectant mothers with information about cord blood donation and prompting them to consider the procedure would increase donations to a public cord blood bank.
Interventions
The researchers enrolled 850 expectant mothers and divided them into 6 treatment cohorts.
The T0 cohort included 217 control subjects who did not receive any information on cord blood donation.
The T1 cohort included 64 subjects who received information on cord blood donation during their first trimester.
The T2 cohort included 88 subjects who were given information on cord blood donation and asked about their intentions to donate in their first trimester.
The T3 cohort included 197 subjects who received information on cord blood donation in their third trimester.
The T4 cohort included 249 subjects who were given information on cord blood donation and asked about their intentions to donate during their third trimester.
The T5 cohort included 35 subjects who were given information on cord blood donation and asked about their intentions to donate during the first trimester and the third trimester.
Results
The researchers found that T5 subjects had the highest donation rate.
In the entire study sample, the donation rate was 2.3% (5/217) in controls, 6.3% (4/64) in T1 subjects, 1.1% (1/88) in T2, 8.1% (16/197) in T3, 10.0% (25/249) in T4, and 17.1% in T5 (6/35).
These results may not be entirely accurate, however, because the researchers could only confirm patients’ donation status if mothers delivered their babies at the study hospital, Ospedale dei Bambini Vittore Buzzi (also known as Buzzi Hospital, BH).
Among women who delivered at BH, donation rates were 2.7% (5/183) in controls, 11.7% (4/34) in T1, 2.2% (1/45) in T2, 8.9% (16/179) in T3, 11.4% (25/42) in T4, and 21.4% (6/28) in T5.
Though these data suggest the various interventions tested can increase cord blood donations, donation rates in this study could have been even higher, according to the researchers.
There were 197 women who submitted consent forms to donate cord blood, were medically eligible to donate, and delivered their babies at BH. However, only 57 of these women successfully donated cord blood.
There were 62 women (56.9%) who could not donate because of medical complications during delivery.
Thirty-three women (30.3%) failed to donate because of organizational reasons, including overcrowding of the delivery room and the absence of obstetric nurses certified to collect and process cord blood at the time of delivery.
There were 14 women (7.1%) who did not donate for institution-related reasons. For example, the women gave birth when the Milan Cord Blood Bank was closed.
There were no details on the remaining 31 women who failed to donate. ![]()
Simple interventions can increase cord blood donations, according to research published in Scientific Reports.
Researchers saw a significant increase in cord blood donation when expectant mothers received information about the procedure and were asked to indicate their interest in donating at both early and late stages of their pregnancies.
“We more than doubled the number of cord blood units that were collected,” said study author Nicola Lacetera, PhD, of the University of Toronto Mississauga in Ontario, Canada.
“We learned a lot, and we did a little bit of good too, so that feels nice.”
Dr Lacetera and his colleagues conducted this study in Milan, Italy, where private cord blood banking is banned.
The team set out to determine if providing expectant mothers with information about cord blood donation and prompting them to consider the procedure would increase donations to a public cord blood bank.
Interventions
The researchers enrolled 850 expectant mothers and divided them into 6 treatment cohorts.
The T0 cohort included 217 control subjects who did not receive any information on cord blood donation.
The T1 cohort included 64 subjects who received information on cord blood donation during their first trimester.
The T2 cohort included 88 subjects who were given information on cord blood donation and asked about their intentions to donate in their first trimester.
The T3 cohort included 197 subjects who received information on cord blood donation in their third trimester.
The T4 cohort included 249 subjects who were given information on cord blood donation and asked about their intentions to donate during their third trimester.
The T5 cohort included 35 subjects who were given information on cord blood donation and asked about their intentions to donate during the first trimester and the third trimester.
Results
The researchers found that T5 subjects had the highest donation rate.
In the entire study sample, the donation rate was 2.3% (5/217) in controls, 6.3% (4/64) in T1 subjects, 1.1% (1/88) in T2, 8.1% (16/197) in T3, 10.0% (25/249) in T4, and 17.1% in T5 (6/35).
These results may not be entirely accurate, however, because the researchers could only confirm patients’ donation status if mothers delivered their babies at the study hospital, Ospedale dei Bambini Vittore Buzzi (also known as Buzzi Hospital, BH).
Among women who delivered at BH, donation rates were 2.7% (5/183) in controls, 11.7% (4/34) in T1, 2.2% (1/45) in T2, 8.9% (16/179) in T3, 11.4% (25/42) in T4, and 21.4% (6/28) in T5.
Though these data suggest the various interventions tested can increase cord blood donations, donation rates in this study could have been even higher, according to the researchers.
There were 197 women who submitted consent forms to donate cord blood, were medically eligible to donate, and delivered their babies at BH. However, only 57 of these women successfully donated cord blood.
There were 62 women (56.9%) who could not donate because of medical complications during delivery.
Thirty-three women (30.3%) failed to donate because of organizational reasons, including overcrowding of the delivery room and the absence of obstetric nurses certified to collect and process cord blood at the time of delivery.
There were 14 women (7.1%) who did not donate for institution-related reasons. For example, the women gave birth when the Milan Cord Blood Bank was closed.
There were no details on the remaining 31 women who failed to donate. ![]()
Simple interventions can increase cord blood donations, according to research published in Scientific Reports.
Researchers saw a significant increase in cord blood donation when expectant mothers received information about the procedure and were asked to indicate their interest in donating at both early and late stages of their pregnancies.
“We more than doubled the number of cord blood units that were collected,” said study author Nicola Lacetera, PhD, of the University of Toronto Mississauga in Ontario, Canada.
“We learned a lot, and we did a little bit of good too, so that feels nice.”
Dr Lacetera and his colleagues conducted this study in Milan, Italy, where private cord blood banking is banned.
The team set out to determine if providing expectant mothers with information about cord blood donation and prompting them to consider the procedure would increase donations to a public cord blood bank.
Interventions
The researchers enrolled 850 expectant mothers and divided them into 6 treatment cohorts.
The T0 cohort included 217 control subjects who did not receive any information on cord blood donation.
The T1 cohort included 64 subjects who received information on cord blood donation during their first trimester.
The T2 cohort included 88 subjects who were given information on cord blood donation and asked about their intentions to donate in their first trimester.
The T3 cohort included 197 subjects who received information on cord blood donation in their third trimester.
The T4 cohort included 249 subjects who were given information on cord blood donation and asked about their intentions to donate during their third trimester.
The T5 cohort included 35 subjects who were given information on cord blood donation and asked about their intentions to donate during the first trimester and the third trimester.
Results
The researchers found that T5 subjects had the highest donation rate.
In the entire study sample, the donation rate was 2.3% (5/217) in controls, 6.3% (4/64) in T1 subjects, 1.1% (1/88) in T2, 8.1% (16/197) in T3, 10.0% (25/249) in T4, and 17.1% in T5 (6/35).
These results may not be entirely accurate, however, because the researchers could only confirm patients’ donation status if mothers delivered their babies at the study hospital, Ospedale dei Bambini Vittore Buzzi (also known as Buzzi Hospital, BH).
Among women who delivered at BH, donation rates were 2.7% (5/183) in controls, 11.7% (4/34) in T1, 2.2% (1/45) in T2, 8.9% (16/179) in T3, 11.4% (25/42) in T4, and 21.4% (6/28) in T5.
Though these data suggest the various interventions tested can increase cord blood donations, donation rates in this study could have been even higher, according to the researchers.
There were 197 women who submitted consent forms to donate cord blood, were medically eligible to donate, and delivered their babies at BH. However, only 57 of these women successfully donated cord blood.
There were 62 women (56.9%) who could not donate because of medical complications during delivery.
Thirty-three women (30.3%) failed to donate because of organizational reasons, including overcrowding of the delivery room and the absence of obstetric nurses certified to collect and process cord blood at the time of delivery.
There were 14 women (7.1%) who did not donate for institution-related reasons. For example, the women gave birth when the Milan Cord Blood Bank was closed.
There were no details on the remaining 31 women who failed to donate.
EMA recommends orphan designation for pracinostat
The European Medicines Agency (EMA) has recommended that pracinostat receive orphan drug designation.
Pracinostat is an oral histone deacetylase inhibitor currently under investigation in a phase 3 study in combination with azacitidine for the treatment of acute myeloid leukemia (AML) in adult patients unfit to receive induction chemotherapy.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure. The designation also provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Phase 2 study
The EMA’s recommendation that pracinostat receive orphan drug designation is based on results of a phase 2 study, which were presented at the 2016 ASH Annual Meeting.
The study included 50 patients who had a median age of 75 (range, 66-84). Sixty-six percent of patients had de novo AML, and 34% had secondary AML.
The patients received pracinostat at 60 mg orally on days 1, 3, and 5 of each week for 21 days of each 28-day cycle. They received azacitidine at 75 mg/m2 subcutaneously or intravenously on days 1-7 or days 1-5 and 8-9 (per site preference) of each 28-day cycle.
As of October 15, 2016, 90% of patients had discontinued treatment, 42% due to progressive disease, 28% due to adverse events (AEs), 14% due to patient decision, and 6% due to investigator decision.
Fifty-two percent of patients (n=26) achieved the primary endpoint of complete response (CR) plus CR with incomplete count recovery (CRi) plus morphologic leukemia-free state (MLFS).
Forty-two percent of patients had a CR, 4% had a CRi, and 6% achieved MLFS. The median duration of CR/CRi/MLFS was 13.2 months. The median duration of CR/CRi was 17.2 months.
The median overall survival was 19.1 months. The 1-year survival rate was 62%, and the 2-year survival rate was 41%.
The most common treatment-emergent AEs were nausea (78%), constipation (70%), fatigue (62%), decreased appetite (56%), diarrhea (50%), vomiting (40%), cough (36%), dyspnea (34%), hypokalemia (34%), peripheral edema (34%), pyrexia (34%), dizziness (32%), back pain (28%), insomnia (28%), febrile neutropenia (48%), thrombocytopenia (46%), anemia (38%), and neutropenia (38%).
Treatment-emergent AEs led to discontinuation in 14 patients. Three of these patients developed sepsis that proved fatal.
The other AEs leading to discontinuation included grade 3 acute axonal neuropathy, grade 3 parainfluenza, grade 3 prolonged QTc/atrial fibrillation, grade 1 acute kidney injury, grade 3 diverticulitis, grade 3 supraglottic ulcer, grade 2 upper respiratory infection, grade 3 fatigue (n=2), and grades 1 and 3 intermittent fatigue (n=2).
The European Medicines Agency (EMA) has recommended that pracinostat receive orphan drug designation.
Pracinostat is an oral histone deacetylase inhibitor currently under investigation in a phase 3 study in combination with azacitidine for the treatment of acute myeloid leukemia (AML) in adult patients unfit to receive induction chemotherapy.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure. The designation also provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Phase 2 study
The EMA’s recommendation that pracinostat receive orphan drug designation is based on results of a phase 2 study, which were presented at the 2016 ASH Annual Meeting.
The study included 50 patients who had a median age of 75 (range, 66-84). Sixty-six percent of patients had de novo AML, and 34% had secondary AML.
The patients received pracinostat at 60 mg orally on days 1, 3, and 5 of each week for 21 days of each 28-day cycle. They received azacitidine at 75 mg/m2 subcutaneously or intravenously on days 1-7 or days 1-5 and 8-9 (per site preference) of each 28-day cycle.
As of October 15, 2016, 90% of patients had discontinued treatment, 42% due to progressive disease, 28% due to adverse events (AEs), 14% due to patient decision, and 6% due to investigator decision.
Fifty-two percent of patients (n=26) achieved the primary endpoint of complete response (CR) plus CR with incomplete count recovery (CRi) plus morphologic leukemia-free state (MLFS).
Forty-two percent of patients had a CR, 4% had a CRi, and 6% achieved MLFS. The median duration of CR/CRi/MLFS was 13.2 months. The median duration of CR/CRi was 17.2 months.
The median overall survival was 19.1 months. The 1-year survival rate was 62%, and the 2-year survival rate was 41%.
The most common treatment-emergent AEs were nausea (78%), constipation (70%), fatigue (62%), decreased appetite (56%), diarrhea (50%), vomiting (40%), cough (36%), dyspnea (34%), hypokalemia (34%), peripheral edema (34%), pyrexia (34%), dizziness (32%), back pain (28%), insomnia (28%), febrile neutropenia (48%), thrombocytopenia (46%), anemia (38%), and neutropenia (38%).
Treatment-emergent AEs led to discontinuation in 14 patients. Three of these patients developed sepsis that proved fatal.
The other AEs leading to discontinuation included grade 3 acute axonal neuropathy, grade 3 parainfluenza, grade 3 prolonged QTc/atrial fibrillation, grade 1 acute kidney injury, grade 3 diverticulitis, grade 3 supraglottic ulcer, grade 2 upper respiratory infection, grade 3 fatigue (n=2), and grades 1 and 3 intermittent fatigue (n=2).
The European Medicines Agency (EMA) has recommended that pracinostat receive orphan drug designation.
Pracinostat is an oral histone deacetylase inhibitor currently under investigation in a phase 3 study in combination with azacitidine for the treatment of acute myeloid leukemia (AML) in adult patients unfit to receive induction chemotherapy.
Orphan designation provides regulatory and financial incentives for companies to develop and market therapies that treat life-threatening or chronically debilitating conditions affecting no more than 5 in 10,000 people in the European Union, and where no satisfactory treatment is available.
Orphan designation provides incentives for companies seeking protocol assistance from the EMA during the product development phase and direct access to the centralized authorization procedure. The designation also provides a 10-year period of marketing exclusivity if a therapy receives regulatory approval.
The EMA’s Committee for Orphan Medicinal Products adopts an opinion on the granting of orphan drug designation, and that opinion is submitted to the European Commission for a final decision.
Phase 2 study
The EMA’s recommendation that pracinostat receive orphan drug designation is based on results of a phase 2 study, which were presented at the 2016 ASH Annual Meeting.
The study included 50 patients who had a median age of 75 (range, 66-84). Sixty-six percent of patients had de novo AML, and 34% had secondary AML.
The patients received pracinostat at 60 mg orally on days 1, 3, and 5 of each week for 21 days of each 28-day cycle. They received azacitidine at 75 mg/m2 subcutaneously or intravenously on days 1-7 or days 1-5 and 8-9 (per site preference) of each 28-day cycle.
As of October 15, 2016, 90% of patients had discontinued treatment, 42% due to progressive disease, 28% due to adverse events (AEs), 14% due to patient decision, and 6% due to investigator decision.
Fifty-two percent of patients (n=26) achieved the primary endpoint of complete response (CR) plus CR with incomplete count recovery (CRi) plus morphologic leukemia-free state (MLFS).
Forty-two percent of patients had a CR, 4% had a CRi, and 6% achieved MLFS. The median duration of CR/CRi/MLFS was 13.2 months. The median duration of CR/CRi was 17.2 months.
The median overall survival was 19.1 months. The 1-year survival rate was 62%, and the 2-year survival rate was 41%.
The most common treatment-emergent AEs were nausea (78%), constipation (70%), fatigue (62%), decreased appetite (56%), diarrhea (50%), vomiting (40%), cough (36%), dyspnea (34%), hypokalemia (34%), peripheral edema (34%), pyrexia (34%), dizziness (32%), back pain (28%), insomnia (28%), febrile neutropenia (48%), thrombocytopenia (46%), anemia (38%), and neutropenia (38%).
Treatment-emergent AEs led to discontinuation in 14 patients. Three of these patients developed sepsis that proved fatal.
The other AEs leading to discontinuation included grade 3 acute axonal neuropathy, grade 3 parainfluenza, grade 3 prolonged QTc/atrial fibrillation, grade 1 acute kidney injury, grade 3 diverticulitis, grade 3 supraglottic ulcer, grade 2 upper respiratory infection, grade 3 fatigue (n=2), and grades 1 and 3 intermittent fatigue (n=2).
Survival differences among AYAs with blood cancers
A new report has revealed differences in survival among adolescents and young adults (AYAs) with hematologic malignancies.
The report includes information on AYAs—ages 15 to 39—living in Los Angeles County who were diagnosed with common cancers between 1988 and 2014.
The data showed differences in 5-year survival rates according to sex, race, age, and socioeconomic status (SES).
For example, lymphoma survival rates were lower for males, African Americans (AAs), older AYAs, and patients with low socioeconomic status (SES).
For AYAs with leukemias, there was no survival difference according to sex, but AAs had worse survival than patients of other races. And the impact of age and SES varied according to leukemia type.
“Cancer survival data are poorly understood for 15- to 39-year-olds,” noted Amie Hwang, PhD, of the University of Southern California Keck School of Medicine in Los Angeles.
That is why she and her colleagues created the report, “Cancer in Los Angeles County: Survival Among Adolescents and Young Adults 1988-2014.”
According to the authors, this is the first report to break down cancer survival rates for AYAs into segments on race/ethnicity, sex, age group, SES, and cancer stage.
Survival data for patients with hematologic malignancies were as follows.
Acute lymphoblastic leukemia
There were 1137 cases of acute lymphoblastic leukemia in the AYA population in Los Angeles County during the period studied. This included 752 males and 385 females.
Five-year survival was similar between males (43%) and females (41%).
Younger AYAs had better survival than older AYAs (48% for ages 15-24, 35% for ages 25-34, and 32% for ages 35-39).
Survival was highest among non-Latino whites (NLWs, 56%), followed by Asian/Pacific Islanders (APIs, 52%), patients of other/unknown races (51%), Latino whites (LWs, 38%), and AAs (29%).
Survival declined with SES (55% for high, 42% for middle, and 36% for low SES).
Acute myeloid leukemia
There were 1195 cases of acute myeloid leukemia—641 males and 554 females.
Five-year survival was similar for males (40%) and females (43%) as well as for the different age groups (45% for ages 15-24 vs 40% for the older age groups).
Survival was highest among NLWs (44%), followed by LWs (43%), APIs (40%), other/unknown (33%), and AAs (25%).
Survival declined somewhat with SES (49% for high, 39% for middle, and 41% for low SES).
Chronic myeloid leukemia
There were 655 cases of chronic myeloid leukemia—408 males and 247 females.
Five-year survival was similar for males (70%) and females (71%), but it was slightly higher for older AYAs (69% for ages 15-24, 68% for ages 25-34, and 76% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (76%), followed by LWs (73%), NLWs/APIs (both 72%), and AAs (57%).
Survival declined somewhat with SES (76% for high, 67% for middle, and 68% for low SES).
Hodgkin lymphoma
There were 2993 AYAs diagnosed with Hodgkin lymphoma—1553 males and 1440 females.
The 5-year survival rate was higher in females (93%) than males (86%) and in younger AYAs (93% for ages 15-24, 89% for ages 25-34, and 85% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (96%), followed by APIs/NLWs (both 91%), LWs (88%), and AAs (83%).
Survival declined with SES (95% for high, 89% for middle, and 83% for low SES).
And survival was lower for patients with advanced-stage disease (93% localized, 94% regional, and 83% distant).
Non-Hodkgin lymphoma
There were 4485 AYAs diagnosed with non-Hodgkin lymphoma during the study period—3064 males and 1421 females.
The 5-year survival rate was higher in females (75%) than males (46%) and in younger AYAs (69% for ages 15-24, 51% for ages 25-34, and 52% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (88%), followed by APIs (68%), LWs/NLWs (both 53%), and AAs (50%).
Survival declined with SES (68% for high, 54% for middle, and 45% for low SES).
And survival was lower for patients with advanced-stage disease (61% localized, 66% regional, and 46% distant).
“Adolescents and young adults go to the doctor less often because they have this superhero mentality, like they’re invincible,” said author Dennis Deapen, DrPH, of the University of Southern California Keck School of Medicine.
“Once they do go to a health professional, their cancer diagnosis can be delayed because cancer isn’t the first concern doctors have for this age group. It comes as no surprise that patients diagnosed with late-stage cancer have reduced survival rates.”
A new report has revealed differences in survival among adolescents and young adults (AYAs) with hematologic malignancies.
The report includes information on AYAs—ages 15 to 39—living in Los Angeles County who were diagnosed with common cancers between 1988 and 2014.
The data showed differences in 5-year survival rates according to sex, race, age, and socioeconomic status (SES).
For example, lymphoma survival rates were lower for males, African Americans (AAs), older AYAs, and patients with low socioeconomic status (SES).
For AYAs with leukemias, there was no survival difference according to sex, but AAs had worse survival than patients of other races. And the impact of age and SES varied according to leukemia type.
“Cancer survival data are poorly understood for 15- to 39-year-olds,” noted Amie Hwang, PhD, of the University of Southern California Keck School of Medicine in Los Angeles.
That is why she and her colleagues created the report, “Cancer in Los Angeles County: Survival Among Adolescents and Young Adults 1988-2014.”
According to the authors, this is the first report to break down cancer survival rates for AYAs into segments on race/ethnicity, sex, age group, SES, and cancer stage.
Survival data for patients with hematologic malignancies were as follows.
Acute lymphoblastic leukemia
There were 1137 cases of acute lymphoblastic leukemia in the AYA population in Los Angeles County during the period studied. This included 752 males and 385 females.
Five-year survival was similar between males (43%) and females (41%).
Younger AYAs had better survival than older AYAs (48% for ages 15-24, 35% for ages 25-34, and 32% for ages 35-39).
Survival was highest among non-Latino whites (NLWs, 56%), followed by Asian/Pacific Islanders (APIs, 52%), patients of other/unknown races (51%), Latino whites (LWs, 38%), and AAs (29%).
Survival declined with SES (55% for high, 42% for middle, and 36% for low SES).
Acute myeloid leukemia
There were 1195 cases of acute myeloid leukemia—641 males and 554 females.
Five-year survival was similar for males (40%) and females (43%) as well as for the different age groups (45% for ages 15-24 vs 40% for the older age groups).
Survival was highest among NLWs (44%), followed by LWs (43%), APIs (40%), other/unknown (33%), and AAs (25%).
Survival declined somewhat with SES (49% for high, 39% for middle, and 41% for low SES).
Chronic myeloid leukemia
There were 655 cases of chronic myeloid leukemia—408 males and 247 females.
Five-year survival was similar for males (70%) and females (71%), but it was slightly higher for older AYAs (69% for ages 15-24, 68% for ages 25-34, and 76% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (76%), followed by LWs (73%), NLWs/APIs (both 72%), and AAs (57%).
Survival declined somewhat with SES (76% for high, 67% for middle, and 68% for low SES).
Hodgkin lymphoma
There were 2993 AYAs diagnosed with Hodgkin lymphoma—1553 males and 1440 females.
The 5-year survival rate was higher in females (93%) than males (86%) and in younger AYAs (93% for ages 15-24, 89% for ages 25-34, and 85% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (96%), followed by APIs/NLWs (both 91%), LWs (88%), and AAs (83%).
Survival declined with SES (95% for high, 89% for middle, and 83% for low SES).
And survival was lower for patients with advanced-stage disease (93% localized, 94% regional, and 83% distant).
Non-Hodkgin lymphoma
There were 4485 AYAs diagnosed with non-Hodgkin lymphoma during the study period—3064 males and 1421 females.
The 5-year survival rate was higher in females (75%) than males (46%) and in younger AYAs (69% for ages 15-24, 51% for ages 25-34, and 52% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (88%), followed by APIs (68%), LWs/NLWs (both 53%), and AAs (50%).
Survival declined with SES (68% for high, 54% for middle, and 45% for low SES).
And survival was lower for patients with advanced-stage disease (61% localized, 66% regional, and 46% distant).
“Adolescents and young adults go to the doctor less often because they have this superhero mentality, like they’re invincible,” said author Dennis Deapen, DrPH, of the University of Southern California Keck School of Medicine.
“Once they do go to a health professional, their cancer diagnosis can be delayed because cancer isn’t the first concern doctors have for this age group. It comes as no surprise that patients diagnosed with late-stage cancer have reduced survival rates.”
A new report has revealed differences in survival among adolescents and young adults (AYAs) with hematologic malignancies.
The report includes information on AYAs—ages 15 to 39—living in Los Angeles County who were diagnosed with common cancers between 1988 and 2014.
The data showed differences in 5-year survival rates according to sex, race, age, and socioeconomic status (SES).
For example, lymphoma survival rates were lower for males, African Americans (AAs), older AYAs, and patients with low socioeconomic status (SES).
For AYAs with leukemias, there was no survival difference according to sex, but AAs had worse survival than patients of other races. And the impact of age and SES varied according to leukemia type.
“Cancer survival data are poorly understood for 15- to 39-year-olds,” noted Amie Hwang, PhD, of the University of Southern California Keck School of Medicine in Los Angeles.
That is why she and her colleagues created the report, “Cancer in Los Angeles County: Survival Among Adolescents and Young Adults 1988-2014.”
According to the authors, this is the first report to break down cancer survival rates for AYAs into segments on race/ethnicity, sex, age group, SES, and cancer stage.
Survival data for patients with hematologic malignancies were as follows.
Acute lymphoblastic leukemia
There were 1137 cases of acute lymphoblastic leukemia in the AYA population in Los Angeles County during the period studied. This included 752 males and 385 females.
Five-year survival was similar between males (43%) and females (41%).
Younger AYAs had better survival than older AYAs (48% for ages 15-24, 35% for ages 25-34, and 32% for ages 35-39).
Survival was highest among non-Latino whites (NLWs, 56%), followed by Asian/Pacific Islanders (APIs, 52%), patients of other/unknown races (51%), Latino whites (LWs, 38%), and AAs (29%).
Survival declined with SES (55% for high, 42% for middle, and 36% for low SES).
Acute myeloid leukemia
There were 1195 cases of acute myeloid leukemia—641 males and 554 females.
Five-year survival was similar for males (40%) and females (43%) as well as for the different age groups (45% for ages 15-24 vs 40% for the older age groups).
Survival was highest among NLWs (44%), followed by LWs (43%), APIs (40%), other/unknown (33%), and AAs (25%).
Survival declined somewhat with SES (49% for high, 39% for middle, and 41% for low SES).
Chronic myeloid leukemia
There were 655 cases of chronic myeloid leukemia—408 males and 247 females.
Five-year survival was similar for males (70%) and females (71%), but it was slightly higher for older AYAs (69% for ages 15-24, 68% for ages 25-34, and 76% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (76%), followed by LWs (73%), NLWs/APIs (both 72%), and AAs (57%).
Survival declined somewhat with SES (76% for high, 67% for middle, and 68% for low SES).
Hodgkin lymphoma
There were 2993 AYAs diagnosed with Hodgkin lymphoma—1553 males and 1440 females.
The 5-year survival rate was higher in females (93%) than males (86%) and in younger AYAs (93% for ages 15-24, 89% for ages 25-34, and 85% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (96%), followed by APIs/NLWs (both 91%), LWs (88%), and AAs (83%).
Survival declined with SES (95% for high, 89% for middle, and 83% for low SES).
And survival was lower for patients with advanced-stage disease (93% localized, 94% regional, and 83% distant).
Non-Hodkgin lymphoma
There were 4485 AYAs diagnosed with non-Hodgkin lymphoma during the study period—3064 males and 1421 females.
The 5-year survival rate was higher in females (75%) than males (46%) and in younger AYAs (69% for ages 15-24, 51% for ages 25-34, and 52% for ages 35-39).
Survival was highest among patients in the “other/unknown” race category (88%), followed by APIs (68%), LWs/NLWs (both 53%), and AAs (50%).
Survival declined with SES (68% for high, 54% for middle, and 45% for low SES).
And survival was lower for patients with advanced-stage disease (61% localized, 66% regional, and 46% distant).
“Adolescents and young adults go to the doctor less often because they have this superhero mentality, like they’re invincible,” said author Dennis Deapen, DrPH, of the University of Southern California Keck School of Medicine.
“Once they do go to a health professional, their cancer diagnosis can be delayed because cancer isn’t the first concern doctors have for this age group. It comes as no surprise that patients diagnosed with late-stage cancer have reduced survival rates.”
Marine animals aid development of cytotoxicity assay
Researchers have looked to deep-sea creatures with the goal of creating a better cytotoxicity assay.
The team harnessed the power of enzymes responsible for marine animal bioluminescence to create the “Matador assay,” which can be used to determine whether cellular and immune-therapeutic agents are actually killing target cells.
The researchers said the Matador assay is quick and simple as well as “highly sensitive,” with the ability to detect cytotoxicity induced by several types of therapies.
Preet M. Chaudhary, MD, PhD, of the University of Southern California Keck School of Medicine in Los Angeles, and his colleagues described the assay in Scientific Reports.
“One of the most promising areas in cancer research is immunotherapy. . .,” Dr Chaudhary said. “It is also one of the most difficult because the methods for testing immunotherapies are not ideal.”
“Radioactive chromium release assay is the gold standard for testing whether an immunotherapy kills cancer cells. This method is expensive, complicated, and requires special disposal practices. Other available methods also suffer from limitations and don’t allow scientists to rapidly screen immunotherapeutic agents to find the best candidates.”
Dr Chaudhary and his colleagues set out to develop a simple, precise, and inexpensive cytotoxicity assay based on marine animal luciferases, the enzymes responsible for bioluminescence.
The team used a group of small crustaceans and deep-sea shrimp, which were selected for their bright bioluminescence. Their luciferases became the basis of the Matador assay.
Engineered to get trapped inside cells, the luciferases leak out of cells when they die, causing a visible glow. The level of luminescence can then be measured with a luminometer.
To test the Matador assay’s effectiveness at measuring cell death, the researchers used several types of cancer cells, including chronic myelogenous leukemia, acute myelogenous leukemia, Burkitt lymphoma, and solid tumor cells.
The team treated these cells with a variety of therapies, including chimeric antigen receptor (CAR) T cells, bispecific T-cell engagers, monoclonal antibodies, and natural killer cells.
Results showed the Matador assay could detect the death of a single cell, a level of sensitivity superior to that of existing cytotoxicity assays.
The researchers also pointed out that the Matador assay is fast, inexpensive, and can be performed in a 384-well plate format, saving time and reagents.
“In our hands, the Matador assay can detect cell death in as little as 30 minutes, which can ultimately translate to more expedient treatments for patients getting cellular immunotherapies such as CAR T cells,” Dr Chaudhary said.
In fact, Dr Chaudhary’s lab has developed more than 75 cancer cell lines expressing the marine luciferases and used them with the Matador assay to develop next-generation CAR T cells.
Dr Chaudhary believes the Matador assay has many potential applications in biomedical research and cellular therapy manufacturing.
“It could potentially play a role in screening other types of anticancer agents or even measuring environmental toxins,” he said.
Researchers have looked to deep-sea creatures with the goal of creating a better cytotoxicity assay.
The team harnessed the power of enzymes responsible for marine animal bioluminescence to create the “Matador assay,” which can be used to determine whether cellular and immune-therapeutic agents are actually killing target cells.
The researchers said the Matador assay is quick and simple as well as “highly sensitive,” with the ability to detect cytotoxicity induced by several types of therapies.
Preet M. Chaudhary, MD, PhD, of the University of Southern California Keck School of Medicine in Los Angeles, and his colleagues described the assay in Scientific Reports.
“One of the most promising areas in cancer research is immunotherapy. . .,” Dr Chaudhary said. “It is also one of the most difficult because the methods for testing immunotherapies are not ideal.”
“Radioactive chromium release assay is the gold standard for testing whether an immunotherapy kills cancer cells. This method is expensive, complicated, and requires special disposal practices. Other available methods also suffer from limitations and don’t allow scientists to rapidly screen immunotherapeutic agents to find the best candidates.”
Dr Chaudhary and his colleagues set out to develop a simple, precise, and inexpensive cytotoxicity assay based on marine animal luciferases, the enzymes responsible for bioluminescence.
The team used a group of small crustaceans and deep-sea shrimp, which were selected for their bright bioluminescence. Their luciferases became the basis of the Matador assay.
Engineered to get trapped inside cells, the luciferases leak out of cells when they die, causing a visible glow. The level of luminescence can then be measured with a luminometer.
To test the Matador assay’s effectiveness at measuring cell death, the researchers used several types of cancer cells, including chronic myelogenous leukemia, acute myelogenous leukemia, Burkitt lymphoma, and solid tumor cells.
The team treated these cells with a variety of therapies, including chimeric antigen receptor (CAR) T cells, bispecific T-cell engagers, monoclonal antibodies, and natural killer cells.
Results showed the Matador assay could detect the death of a single cell, a level of sensitivity superior to that of existing cytotoxicity assays.
The researchers also pointed out that the Matador assay is fast, inexpensive, and can be performed in a 384-well plate format, saving time and reagents.
“In our hands, the Matador assay can detect cell death in as little as 30 minutes, which can ultimately translate to more expedient treatments for patients getting cellular immunotherapies such as CAR T cells,” Dr Chaudhary said.
In fact, Dr Chaudhary’s lab has developed more than 75 cancer cell lines expressing the marine luciferases and used them with the Matador assay to develop next-generation CAR T cells.
Dr Chaudhary believes the Matador assay has many potential applications in biomedical research and cellular therapy manufacturing.
“It could potentially play a role in screening other types of anticancer agents or even measuring environmental toxins,” he said.
Researchers have looked to deep-sea creatures with the goal of creating a better cytotoxicity assay.
The team harnessed the power of enzymes responsible for marine animal bioluminescence to create the “Matador assay,” which can be used to determine whether cellular and immune-therapeutic agents are actually killing target cells.
The researchers said the Matador assay is quick and simple as well as “highly sensitive,” with the ability to detect cytotoxicity induced by several types of therapies.
Preet M. Chaudhary, MD, PhD, of the University of Southern California Keck School of Medicine in Los Angeles, and his colleagues described the assay in Scientific Reports.
“One of the most promising areas in cancer research is immunotherapy. . .,” Dr Chaudhary said. “It is also one of the most difficult because the methods for testing immunotherapies are not ideal.”
“Radioactive chromium release assay is the gold standard for testing whether an immunotherapy kills cancer cells. This method is expensive, complicated, and requires special disposal practices. Other available methods also suffer from limitations and don’t allow scientists to rapidly screen immunotherapeutic agents to find the best candidates.”
Dr Chaudhary and his colleagues set out to develop a simple, precise, and inexpensive cytotoxicity assay based on marine animal luciferases, the enzymes responsible for bioluminescence.
The team used a group of small crustaceans and deep-sea shrimp, which were selected for their bright bioluminescence. Their luciferases became the basis of the Matador assay.
Engineered to get trapped inside cells, the luciferases leak out of cells when they die, causing a visible glow. The level of luminescence can then be measured with a luminometer.
To test the Matador assay’s effectiveness at measuring cell death, the researchers used several types of cancer cells, including chronic myelogenous leukemia, acute myelogenous leukemia, Burkitt lymphoma, and solid tumor cells.
The team treated these cells with a variety of therapies, including chimeric antigen receptor (CAR) T cells, bispecific T-cell engagers, monoclonal antibodies, and natural killer cells.
Results showed the Matador assay could detect the death of a single cell, a level of sensitivity superior to that of existing cytotoxicity assays.
The researchers also pointed out that the Matador assay is fast, inexpensive, and can be performed in a 384-well plate format, saving time and reagents.
“In our hands, the Matador assay can detect cell death in as little as 30 minutes, which can ultimately translate to more expedient treatments for patients getting cellular immunotherapies such as CAR T cells,” Dr Chaudhary said.
In fact, Dr Chaudhary’s lab has developed more than 75 cancer cell lines expressing the marine luciferases and used them with the Matador assay to develop next-generation CAR T cells.
Dr Chaudhary believes the Matador assay has many potential applications in biomedical research and cellular therapy manufacturing.
“It could potentially play a role in screening other types of anticancer agents or even measuring environmental toxins,” he said.