User login
FDA grants drug orphan designation for PNH
The US Food and Drug Administration (FDA) has granted orphan drug designation to RA101495 for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
RA101495 is a synthetic, macrocyclic peptide being developed by Ra Pharmaceuticals.
The peptide binds complement component 5 (C5) with sub-nanomolar affinity and allosterically inhibits its cleavage into C5a and C5b upon activation of the classical, alternative, or lectin pathways.
By binding to a region of C5 corresponding to C5b, RA101495 also disrupts the interaction between C5b and C6 and prevents assembly of the membrane attack complex.
In phase 1 studies, dosing of RA101495 was well tolerated in healthy volunteers and demonstrated sustained and near complete suppression of hemolysis and complement activity.
The phase 1 results were presented at the 21st Congress of the European Hematology Association in June 2016 (abstracts LB2249 and P632).
RA101495 is currently under investigation in a phase 2 trial of patients with PNH.
“There is an urgent need for new treatment options for patients suffering from PNH,” said Doug Treco, PhD, president and chief executive officer of Ra Pharmaceuticals.
“The current standard of care requires biweekly intravenous infusions, a dosing regimen that imposes a severe burden on patients, providers, and caregivers. We have designed RA101495 for once-daily, subcutaneous self-administration, an approach which has the potential to ease this burden, improve convenience, and provide much-needed dosing flexibility.”
“We are encouraged by our initial phase 2 data in PNH patients, which showed near-complete inhibition of hemolysis and a favorable safety and tolerability profile. We look forward to advancing our PNH program and providing additional data updates around year-end.”
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to RA101495 for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
RA101495 is a synthetic, macrocyclic peptide being developed by Ra Pharmaceuticals.
The peptide binds complement component 5 (C5) with sub-nanomolar affinity and allosterically inhibits its cleavage into C5a and C5b upon activation of the classical, alternative, or lectin pathways.
By binding to a region of C5 corresponding to C5b, RA101495 also disrupts the interaction between C5b and C6 and prevents assembly of the membrane attack complex.
In phase 1 studies, dosing of RA101495 was well tolerated in healthy volunteers and demonstrated sustained and near complete suppression of hemolysis and complement activity.
The phase 1 results were presented at the 21st Congress of the European Hematology Association in June 2016 (abstracts LB2249 and P632).
RA101495 is currently under investigation in a phase 2 trial of patients with PNH.
“There is an urgent need for new treatment options for patients suffering from PNH,” said Doug Treco, PhD, president and chief executive officer of Ra Pharmaceuticals.
“The current standard of care requires biweekly intravenous infusions, a dosing regimen that imposes a severe burden on patients, providers, and caregivers. We have designed RA101495 for once-daily, subcutaneous self-administration, an approach which has the potential to ease this burden, improve convenience, and provide much-needed dosing flexibility.”
“We are encouraged by our initial phase 2 data in PNH patients, which showed near-complete inhibition of hemolysis and a favorable safety and tolerability profile. We look forward to advancing our PNH program and providing additional data updates around year-end.”
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
The US Food and Drug Administration (FDA) has granted orphan drug designation to RA101495 for the treatment of paroxysmal nocturnal hemoglobinuria (PNH).
RA101495 is a synthetic, macrocyclic peptide being developed by Ra Pharmaceuticals.
The peptide binds complement component 5 (C5) with sub-nanomolar affinity and allosterically inhibits its cleavage into C5a and C5b upon activation of the classical, alternative, or lectin pathways.
By binding to a region of C5 corresponding to C5b, RA101495 also disrupts the interaction between C5b and C6 and prevents assembly of the membrane attack complex.
In phase 1 studies, dosing of RA101495 was well tolerated in healthy volunteers and demonstrated sustained and near complete suppression of hemolysis and complement activity.
The phase 1 results were presented at the 21st Congress of the European Hematology Association in June 2016 (abstracts LB2249 and P632).
RA101495 is currently under investigation in a phase 2 trial of patients with PNH.
“There is an urgent need for new treatment options for patients suffering from PNH,” said Doug Treco, PhD, president and chief executive officer of Ra Pharmaceuticals.
“The current standard of care requires biweekly intravenous infusions, a dosing regimen that imposes a severe burden on patients, providers, and caregivers. We have designed RA101495 for once-daily, subcutaneous self-administration, an approach which has the potential to ease this burden, improve convenience, and provide much-needed dosing flexibility.”
“We are encouraged by our initial phase 2 data in PNH patients, which showed near-complete inhibition of hemolysis and a favorable safety and tolerability profile. We look forward to advancing our PNH program and providing additional data updates around year-end.”
About orphan designation
The FDA grants orphan designation to drugs and biologics intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the US.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved. ![]()
FDA approves enasidenib to treat relapsed/refractory AML
The US Food and Drug Administration (FDA) has approved marketing of the oral IDH2 inhibitor enasidenib (IDHIFA®).
The drug is now approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) and an IDH2 mutation, as detected by an FDA-approved test.
Enasidenib is available in 50 mg and 100 mg tablets. The recommended dose is 100 mg once daily until disease progression or unacceptable toxicity.
The prescribing information for enasidenib includes a boxed warning that the drug may cause differentiation syndrome, and this adverse event (AE) can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, and hepatic, renal, or multi-organ dysfunction. At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor patients closely until symptoms resolve.
Companion diagnostic
Enasidenib was approved concurrently with the Abbott RealTime™ IDH2 companion diagnostic test, which was approved as an aid in identifying AML patients for treatment with enasidenib.
The FDA granted approval of enasidenib to Celgene Corporation and approval of the RealTime IDH2 Assay to Abbott Laboratories.
Enasidenib is licensed from Agios Pharmaceuticals.
Trial results
The FDA’s approval of enasidenib and the companion diagnostic test was based on data from a phase 1/2 trial (Study AG221-C-001, NCT01915498).
Data from this trial were recently presented at the ASCO 2017 Annual Meeting. However, the definitive data are included in the prescribing information for enasidenib.
The prescribing information includes efficacy data for 199 adults with relapsed/refractory AML and an IDH2 mutation. IDH2 mutations were identified or confirmed by the Abbott RealTime™ IDH2 test.
The 199 patients received enasidenib at a starting dose of 100 mg daily until disease progression or unacceptable toxicity. Dose reductions were allowed to manage side effects.
The patients’ median age was 68 (range, 19 to 100). They received a median of 2 prior anticancer regimens (range, 1 to 6). More than half (52%) were refractory to previous therapy.
The rate of complete response (CR) or CR with partial hematologic improvement (CRh) was 23% (n=46). The median duration of CR/CRh was 8.2 months (range, 4.3 to 19.4).
For patients who achieved a CR/CRh, the median time to first response was 1.9 months (range, 0.5 to 7.5), and the median time to best response of CR/CRh was 3.7 months (range, 0.6 to 11.2).
Among the 157 patients who were dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 53 (34%) became independent of RBC and platelet transfusions during any 56-day period post-baseline.
Of the 42 patients who were independent of both RBC and platelet transfusions at baseline, 32 (76%) remained transfusion independent during any 56-day post-baseline period.
Researchers evaluated the safety of enasidenib in 214 patients. The median duration of exposure to enasidenib was 4.3 months (range, 0.3 to 23.6).
The most common AEs of any grade (≥20%) were nausea, vomiting, diarrhea, elevated bilirubin, and decreased appetite.
Serious AEs were reported in 77.1% of patients. The most frequent serious AEs (≥2%) were leukocytosis, diarrhea, nausea, vomiting, decreased appetite, tumor lysis syndrome, and differentiation syndrome.
The 30-day and 60-day mortality rates were 4.2% (9/214) and 11.7% (25/214), respectively. ![]()
The US Food and Drug Administration (FDA) has approved marketing of the oral IDH2 inhibitor enasidenib (IDHIFA®).
The drug is now approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) and an IDH2 mutation, as detected by an FDA-approved test.
Enasidenib is available in 50 mg and 100 mg tablets. The recommended dose is 100 mg once daily until disease progression or unacceptable toxicity.
The prescribing information for enasidenib includes a boxed warning that the drug may cause differentiation syndrome, and this adverse event (AE) can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, and hepatic, renal, or multi-organ dysfunction. At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor patients closely until symptoms resolve.
Companion diagnostic
Enasidenib was approved concurrently with the Abbott RealTime™ IDH2 companion diagnostic test, which was approved as an aid in identifying AML patients for treatment with enasidenib.
The FDA granted approval of enasidenib to Celgene Corporation and approval of the RealTime IDH2 Assay to Abbott Laboratories.
Enasidenib is licensed from Agios Pharmaceuticals.
Trial results
The FDA’s approval of enasidenib and the companion diagnostic test was based on data from a phase 1/2 trial (Study AG221-C-001, NCT01915498).
Data from this trial were recently presented at the ASCO 2017 Annual Meeting. However, the definitive data are included in the prescribing information for enasidenib.
The prescribing information includes efficacy data for 199 adults with relapsed/refractory AML and an IDH2 mutation. IDH2 mutations were identified or confirmed by the Abbott RealTime™ IDH2 test.
The 199 patients received enasidenib at a starting dose of 100 mg daily until disease progression or unacceptable toxicity. Dose reductions were allowed to manage side effects.
The patients’ median age was 68 (range, 19 to 100). They received a median of 2 prior anticancer regimens (range, 1 to 6). More than half (52%) were refractory to previous therapy.
The rate of complete response (CR) or CR with partial hematologic improvement (CRh) was 23% (n=46). The median duration of CR/CRh was 8.2 months (range, 4.3 to 19.4).
For patients who achieved a CR/CRh, the median time to first response was 1.9 months (range, 0.5 to 7.5), and the median time to best response of CR/CRh was 3.7 months (range, 0.6 to 11.2).
Among the 157 patients who were dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 53 (34%) became independent of RBC and platelet transfusions during any 56-day period post-baseline.
Of the 42 patients who were independent of both RBC and platelet transfusions at baseline, 32 (76%) remained transfusion independent during any 56-day post-baseline period.
Researchers evaluated the safety of enasidenib in 214 patients. The median duration of exposure to enasidenib was 4.3 months (range, 0.3 to 23.6).
The most common AEs of any grade (≥20%) were nausea, vomiting, diarrhea, elevated bilirubin, and decreased appetite.
Serious AEs were reported in 77.1% of patients. The most frequent serious AEs (≥2%) were leukocytosis, diarrhea, nausea, vomiting, decreased appetite, tumor lysis syndrome, and differentiation syndrome.
The 30-day and 60-day mortality rates were 4.2% (9/214) and 11.7% (25/214), respectively. ![]()
The US Food and Drug Administration (FDA) has approved marketing of the oral IDH2 inhibitor enasidenib (IDHIFA®).
The drug is now approved to treat adults with relapsed or refractory acute myeloid leukemia (AML) and an IDH2 mutation, as detected by an FDA-approved test.
Enasidenib is available in 50 mg and 100 mg tablets. The recommended dose is 100 mg once daily until disease progression or unacceptable toxicity.
The prescribing information for enasidenib includes a boxed warning that the drug may cause differentiation syndrome, and this adverse event (AE) can be fatal if not treated.
Signs and symptoms of differentiation syndrome may include fever, dyspnea, acute respiratory distress, radiographic pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain, peripheral edema, and hepatic, renal, or multi-organ dysfunction. At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor patients closely until symptoms resolve.
Companion diagnostic
Enasidenib was approved concurrently with the Abbott RealTime™ IDH2 companion diagnostic test, which was approved as an aid in identifying AML patients for treatment with enasidenib.
The FDA granted approval of enasidenib to Celgene Corporation and approval of the RealTime IDH2 Assay to Abbott Laboratories.
Enasidenib is licensed from Agios Pharmaceuticals.
Trial results
The FDA’s approval of enasidenib and the companion diagnostic test was based on data from a phase 1/2 trial (Study AG221-C-001, NCT01915498).
Data from this trial were recently presented at the ASCO 2017 Annual Meeting. However, the definitive data are included in the prescribing information for enasidenib.
The prescribing information includes efficacy data for 199 adults with relapsed/refractory AML and an IDH2 mutation. IDH2 mutations were identified or confirmed by the Abbott RealTime™ IDH2 test.
The 199 patients received enasidenib at a starting dose of 100 mg daily until disease progression or unacceptable toxicity. Dose reductions were allowed to manage side effects.
The patients’ median age was 68 (range, 19 to 100). They received a median of 2 prior anticancer regimens (range, 1 to 6). More than half (52%) were refractory to previous therapy.
The rate of complete response (CR) or CR with partial hematologic improvement (CRh) was 23% (n=46). The median duration of CR/CRh was 8.2 months (range, 4.3 to 19.4).
For patients who achieved a CR/CRh, the median time to first response was 1.9 months (range, 0.5 to 7.5), and the median time to best response of CR/CRh was 3.7 months (range, 0.6 to 11.2).
Among the 157 patients who were dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 53 (34%) became independent of RBC and platelet transfusions during any 56-day period post-baseline.
Of the 42 patients who were independent of both RBC and platelet transfusions at baseline, 32 (76%) remained transfusion independent during any 56-day post-baseline period.
Researchers evaluated the safety of enasidenib in 214 patients. The median duration of exposure to enasidenib was 4.3 months (range, 0.3 to 23.6).
The most common AEs of any grade (≥20%) were nausea, vomiting, diarrhea, elevated bilirubin, and decreased appetite.
Serious AEs were reported in 77.1% of patients. The most frequent serious AEs (≥2%) were leukocytosis, diarrhea, nausea, vomiting, decreased appetite, tumor lysis syndrome, and differentiation syndrome.
The 30-day and 60-day mortality rates were 4.2% (9/214) and 11.7% (25/214), respectively. ![]()
Delirium linked to early death in advanced cancer patients
A diagnosis of delirium during a visit to the emergency department (ED) is a poor prognostic factor for patients with advanced cancer, according to research published in The Oncologist.
The study showed that patients with advanced cancer who were diagnosed with delirium during an ED visit were more likely to be admitted to the hospital or intensive care unit (ICU) and more likely to die earlier than patients without delirium.
This shows the importance of accurately diagnosing delirium in advanced cancer patients, said Ahmed Elsayem, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Previous studies have shown that delirium is associated with poor survival in advanced cancer patients being treated in ICUs or receiving palliative care in hospices, but no one had investigated whether the same was true for patients visiting EDs.
“To the best our knowledge, this is the first study to show the poor survival of advanced cancer patients in the emergency department setting,” Dr Elsayem said.
He and his colleagues previously conducted a study in which they assessed the frequency of delirium in advanced cancer patients visiting the ED at MD Anderson. The researchers tested for delirium using 2 questionnaires—the Confusion Assessment Method (CAM) and Memorial Delirium Assessment Scale (MDAS).
Questioning 243 patients in total, the team found that 44 patients, or 18%, were suffering with delirium according to at least 1 of the questionnaires.
In the current study, Dr Elsayem and his colleagues determined how many of these cancer patients, with and without delirium, were subsequently admitted to hospital and ICUs, as well as how long the patients lived after their visit to the ED.
Results
The rate of hospitalization was 82% among patients with delirium according to CAM and/or MDAS, 77% among patients with delirium according to MDAS only, and 49% among patients without delirium (P=0.0013). Rates of ICU admission were 18%, 14%, and 2%, respectively (P=0.0004).
The median overall survival was 1.23 months for patients with delirium according to CAM and/or MDAS, 4.70 months for patients with delirium according to MDAS only, and 10.45 months for patients without delirium. The difference between the patients with and without delirium was significant (P<0.0001).
Given the influence delirium appears to have on survival, Dr Elsayem said prompt diagnosis and management in hospital EDs is essential.
He noted that, in many cases, delirium in advanced cancer patients can be resolved by simply stopping or modifying their medication and treating any associated infections.
“Treating the triggers if known—such as stopping medications—is the main treatment for an episode of delirium,” Dr Elsayem said.
He also suggested that further research needs to be done on this topic, including conducting similar studies on delirium in advanced cancer patients in other EDs and with larger groups of patients. ![]()
A diagnosis of delirium during a visit to the emergency department (ED) is a poor prognostic factor for patients with advanced cancer, according to research published in The Oncologist.
The study showed that patients with advanced cancer who were diagnosed with delirium during an ED visit were more likely to be admitted to the hospital or intensive care unit (ICU) and more likely to die earlier than patients without delirium.
This shows the importance of accurately diagnosing delirium in advanced cancer patients, said Ahmed Elsayem, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Previous studies have shown that delirium is associated with poor survival in advanced cancer patients being treated in ICUs or receiving palliative care in hospices, but no one had investigated whether the same was true for patients visiting EDs.
“To the best our knowledge, this is the first study to show the poor survival of advanced cancer patients in the emergency department setting,” Dr Elsayem said.
He and his colleagues previously conducted a study in which they assessed the frequency of delirium in advanced cancer patients visiting the ED at MD Anderson. The researchers tested for delirium using 2 questionnaires—the Confusion Assessment Method (CAM) and Memorial Delirium Assessment Scale (MDAS).
Questioning 243 patients in total, the team found that 44 patients, or 18%, were suffering with delirium according to at least 1 of the questionnaires.
In the current study, Dr Elsayem and his colleagues determined how many of these cancer patients, with and without delirium, were subsequently admitted to hospital and ICUs, as well as how long the patients lived after their visit to the ED.
Results
The rate of hospitalization was 82% among patients with delirium according to CAM and/or MDAS, 77% among patients with delirium according to MDAS only, and 49% among patients without delirium (P=0.0013). Rates of ICU admission were 18%, 14%, and 2%, respectively (P=0.0004).
The median overall survival was 1.23 months for patients with delirium according to CAM and/or MDAS, 4.70 months for patients with delirium according to MDAS only, and 10.45 months for patients without delirium. The difference between the patients with and without delirium was significant (P<0.0001).
Given the influence delirium appears to have on survival, Dr Elsayem said prompt diagnosis and management in hospital EDs is essential.
He noted that, in many cases, delirium in advanced cancer patients can be resolved by simply stopping or modifying their medication and treating any associated infections.
“Treating the triggers if known—such as stopping medications—is the main treatment for an episode of delirium,” Dr Elsayem said.
He also suggested that further research needs to be done on this topic, including conducting similar studies on delirium in advanced cancer patients in other EDs and with larger groups of patients. ![]()
A diagnosis of delirium during a visit to the emergency department (ED) is a poor prognostic factor for patients with advanced cancer, according to research published in The Oncologist.
The study showed that patients with advanced cancer who were diagnosed with delirium during an ED visit were more likely to be admitted to the hospital or intensive care unit (ICU) and more likely to die earlier than patients without delirium.
This shows the importance of accurately diagnosing delirium in advanced cancer patients, said Ahmed Elsayem, MD, of the University of Texas MD Anderson Cancer Center in Houston.
Previous studies have shown that delirium is associated with poor survival in advanced cancer patients being treated in ICUs or receiving palliative care in hospices, but no one had investigated whether the same was true for patients visiting EDs.
“To the best our knowledge, this is the first study to show the poor survival of advanced cancer patients in the emergency department setting,” Dr Elsayem said.
He and his colleagues previously conducted a study in which they assessed the frequency of delirium in advanced cancer patients visiting the ED at MD Anderson. The researchers tested for delirium using 2 questionnaires—the Confusion Assessment Method (CAM) and Memorial Delirium Assessment Scale (MDAS).
Questioning 243 patients in total, the team found that 44 patients, or 18%, were suffering with delirium according to at least 1 of the questionnaires.
In the current study, Dr Elsayem and his colleagues determined how many of these cancer patients, with and without delirium, were subsequently admitted to hospital and ICUs, as well as how long the patients lived after their visit to the ED.
Results
The rate of hospitalization was 82% among patients with delirium according to CAM and/or MDAS, 77% among patients with delirium according to MDAS only, and 49% among patients without delirium (P=0.0013). Rates of ICU admission were 18%, 14%, and 2%, respectively (P=0.0004).
The median overall survival was 1.23 months for patients with delirium according to CAM and/or MDAS, 4.70 months for patients with delirium according to MDAS only, and 10.45 months for patients without delirium. The difference between the patients with and without delirium was significant (P<0.0001).
Given the influence delirium appears to have on survival, Dr Elsayem said prompt diagnosis and management in hospital EDs is essential.
He noted that, in many cases, delirium in advanced cancer patients can be resolved by simply stopping or modifying their medication and treating any associated infections.
“Treating the triggers if known—such as stopping medications—is the main treatment for an episode of delirium,” Dr Elsayem said.
He also suggested that further research needs to be done on this topic, including conducting similar studies on delirium in advanced cancer patients in other EDs and with larger groups of patients. ![]()
FDA grants acalabrutinib breakthrough designation
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to acalabrutinib, a BTK inhibitor being developed to treat multiple B-cell malignancies.
The breakthrough designation applies to acalabrutinib as a treatment for patients with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The FDA granted acalabrutinib breakthrough designation based on data from the drug’s development program, which includes data from the phase 2 ACE-LY-004 trial in patients with relapsed or refractory MCL.
Data from this trial have not yet been released to the public but are expected to be presented at an upcoming medical meeting. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to acalabrutinib, a BTK inhibitor being developed to treat multiple B-cell malignancies.
The breakthrough designation applies to acalabrutinib as a treatment for patients with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The FDA granted acalabrutinib breakthrough designation based on data from the drug’s development program, which includes data from the phase 2 ACE-LY-004 trial in patients with relapsed or refractory MCL.
Data from this trial have not yet been released to the public but are expected to be presented at an upcoming medical meeting. ![]()
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to acalabrutinib, a BTK inhibitor being developed to treat multiple B-cell malignancies.
The breakthrough designation applies to acalabrutinib as a treatment for patients with mantle cell lymphoma (MCL) who have received at least 1 prior therapy.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
The designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
The FDA granted acalabrutinib breakthrough designation based on data from the drug’s development program, which includes data from the phase 2 ACE-LY-004 trial in patients with relapsed or refractory MCL.
Data from this trial have not yet been released to the public but are expected to be presented at an upcoming medical meeting. ![]()
Understanding childhood cancer in sub-Saharan Africa
Researchers say they have published the most extensive data ever collected on childhood cancer in sub-Saharan Africa.
On the African continent, only South Africa operates a childhood cancer registry on the national level.
Researchers brought together data from 16 of the smaller, local registries, collecting this information for the first time and presenting it in an accessible format.
The data were published in ecancermedicalscience.
Examining the data in context allowed the researchers to notice trends in cancer incidence. For example, they found that, in Blantyre, Malawi’s second-largest city, the cumulative risk of a child developing Burkitt lymphoma is 2 in every thousand.
The researchers called this incidence “remarkable” and noted that the global research community is largely unaware of this.
“Everything starts with awareness,” said study author Cristina Stefan, global clinical leader of oncology for Roche Diagnostics International Ltd of Switzerland and director of the African Medical Research and Innovation Institute.
“It is highly necessary to publicize these data, which, at the moment, represent the best image of the malignant disease in children in the respective regions.”
The researchers also noted that factors such as the prevalence of malaria and the Epstein-Barr virus contribute to the unique epidemiology of childhood cancer in Africa.
“Our colleagues can learn that the patterns and distribution of cancers in Africa are totally different from Europe, and there is a need for further research into the roles of factors such as genetic predispositions and the influence of infections and other comorbidities in the evolution of cancer,” Dr Stefan said.
“We have learned many universal lessons about data collection as we prepared this work. Our hope is that the publication of this monograph will open the forums for future discussions and that the work will be referenced for the better understanding of cancer in children in Africa and used to improve outcomes for children affected there.” ![]()
Researchers say they have published the most extensive data ever collected on childhood cancer in sub-Saharan Africa.
On the African continent, only South Africa operates a childhood cancer registry on the national level.
Researchers brought together data from 16 of the smaller, local registries, collecting this information for the first time and presenting it in an accessible format.
The data were published in ecancermedicalscience.
Examining the data in context allowed the researchers to notice trends in cancer incidence. For example, they found that, in Blantyre, Malawi’s second-largest city, the cumulative risk of a child developing Burkitt lymphoma is 2 in every thousand.
The researchers called this incidence “remarkable” and noted that the global research community is largely unaware of this.
“Everything starts with awareness,” said study author Cristina Stefan, global clinical leader of oncology for Roche Diagnostics International Ltd of Switzerland and director of the African Medical Research and Innovation Institute.
“It is highly necessary to publicize these data, which, at the moment, represent the best image of the malignant disease in children in the respective regions.”
The researchers also noted that factors such as the prevalence of malaria and the Epstein-Barr virus contribute to the unique epidemiology of childhood cancer in Africa.
“Our colleagues can learn that the patterns and distribution of cancers in Africa are totally different from Europe, and there is a need for further research into the roles of factors such as genetic predispositions and the influence of infections and other comorbidities in the evolution of cancer,” Dr Stefan said.
“We have learned many universal lessons about data collection as we prepared this work. Our hope is that the publication of this monograph will open the forums for future discussions and that the work will be referenced for the better understanding of cancer in children in Africa and used to improve outcomes for children affected there.” ![]()
Researchers say they have published the most extensive data ever collected on childhood cancer in sub-Saharan Africa.
On the African continent, only South Africa operates a childhood cancer registry on the national level.
Researchers brought together data from 16 of the smaller, local registries, collecting this information for the first time and presenting it in an accessible format.
The data were published in ecancermedicalscience.
Examining the data in context allowed the researchers to notice trends in cancer incidence. For example, they found that, in Blantyre, Malawi’s second-largest city, the cumulative risk of a child developing Burkitt lymphoma is 2 in every thousand.
The researchers called this incidence “remarkable” and noted that the global research community is largely unaware of this.
“Everything starts with awareness,” said study author Cristina Stefan, global clinical leader of oncology for Roche Diagnostics International Ltd of Switzerland and director of the African Medical Research and Innovation Institute.
“It is highly necessary to publicize these data, which, at the moment, represent the best image of the malignant disease in children in the respective regions.”
The researchers also noted that factors such as the prevalence of malaria and the Epstein-Barr virus contribute to the unique epidemiology of childhood cancer in Africa.
“Our colleagues can learn that the patterns and distribution of cancers in Africa are totally different from Europe, and there is a need for further research into the roles of factors such as genetic predispositions and the influence of infections and other comorbidities in the evolution of cancer,” Dr Stefan said.
“We have learned many universal lessons about data collection as we prepared this work. Our hope is that the publication of this monograph will open the forums for future discussions and that the work will be referenced for the better understanding of cancer in children in Africa and used to improve outcomes for children affected there.” ![]()
Thalassemia case provides insight into history of malaria
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
The earliest documented case of β-thalassemia in Sardinia suggests malaria was widespread on the island long before the Middle Ages, according to researchers.
The team noted that Sardinia has one of the highest incidence rates of β-thalassemia in Europe due to its long history of endemic malaria.
However, it has been assumed that malaria was only endemic on the island since the Middle Ages (500-1500 CE).
New research, published in the American Journal of Physical Anthropology, suggests malaria was probably already endemic on Sardinia during the Roman period.
Since ancient DNA of malaria is difficult to extract, the researchers studied thalassemia and other genetic adaptations in its place.
The team studied a thalassemia allele called cod39 β-thalassemia, which is dominant on Sardinia. They were able to confirm the presence of the cod39 allele in the 2000-year-old (approximately 300 BCE to 100 CE) remains of a Roman man.
“This is the very first documented case of the genetic adaptation to malaria on Sardinia,” said study author Claudia Vigano, of the Institute for Evolutionary Medicine of the University of Zurich in Switzerland.
“We also discovered that the person was genetically a Sardinian in all probability and not an immigrant from another area.”
“Our study shows the importance of a multidisciplinary approach to history,” said Abigail Bouwman, also of the Institute for Evolutionary Medicine of the University of Zurich.
“We are researching the evolution of today’s diseases, such as malaria, to explain why the human body becomes sick at all and how adaptations occur.” ![]()
ASCO updates guidelines on antiemetic use in cancer patients
The American Society of Clinical Oncology (ASCO) has updated its clinical practice guidelines on the use of antiemetics in cancer patients.
The update, published in the Journal of Clinical Oncology, provides new evidence-based information on the appropriate use of olanzapine, NK1 receptor antagonists, and dexamethasone.
“The adverse impact of inadequately controlled nausea and vomiting on patients’ quality of life is well documented,” said Paul J. Hesketh, MD, co-chair of the ASCO expert panel that updated the guidelines.
“By following the ASCO antiemetics guideline, clinicians have the opportunity to improve patients’ quality of life by minimizing treatment-induced emesis.”
To update ASCO’s guidelines on antiemetics, the expert panel conducted a systematic review of the medical literature published between November 2009 and June 2016. The panel included members with expertise in medical oncology, radiation oncology, nursing, pharmacy, and health services research, as well as a patient representative.
“Tremendous progress has been realized over the last 25 years in the prevention of chemotherapy-induced nausea and vomiting with the introduction of new classes of antiemetic agents,” said Mark G. Kris, MD, co-chair of the expert panel that updated the guidelines.
“The full benefit of these treatment advances will only be realized, however, if evidence-based guidelines are fully implemented.”
Key recommendations in the updated guidelines include:
For adults receiving chemotherapy with a high risk for nausea and vomiting (eg, cisplatin or the combination of cyclophosphamide and an anthracycline), olanzapine should be added to standard antiemetic regimens (the combination of a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and dexamethasone). Olanzapine also helps individuals who experience symptoms despite receiving medicines to prevent vomiting before chemotherapy is given.
For adults receiving carboplatin-based chemotherapy or high-dose chemotherapy and children receiving chemotherapy with a high risk for nausea and vomiting, an NK1 receptor antagonist should be added to the standard antiemetic regimen (the combination of 5-HT3 receptor antagonist and dexamethasone).
Dexamethasone treatment can be limited to the day of chemotherapy administration in patients receiving an anthracycline and cyclophosphamide.
Dronabinol and nabilone, cannabinoids approved by the US Food and Drug Administration, can be used to treat nausea and vomiting that is resistant to standard antiemetic therapies. Evidence remains insufficient to recommend medical marijuana for either prevention or treatment of nausea and vomiting in patients with cancer receiving chemotherapy or radiation therapy. ![]()
The American Society of Clinical Oncology (ASCO) has updated its clinical practice guidelines on the use of antiemetics in cancer patients.
The update, published in the Journal of Clinical Oncology, provides new evidence-based information on the appropriate use of olanzapine, NK1 receptor antagonists, and dexamethasone.
“The adverse impact of inadequately controlled nausea and vomiting on patients’ quality of life is well documented,” said Paul J. Hesketh, MD, co-chair of the ASCO expert panel that updated the guidelines.
“By following the ASCO antiemetics guideline, clinicians have the opportunity to improve patients’ quality of life by minimizing treatment-induced emesis.”
To update ASCO’s guidelines on antiemetics, the expert panel conducted a systematic review of the medical literature published between November 2009 and June 2016. The panel included members with expertise in medical oncology, radiation oncology, nursing, pharmacy, and health services research, as well as a patient representative.
“Tremendous progress has been realized over the last 25 years in the prevention of chemotherapy-induced nausea and vomiting with the introduction of new classes of antiemetic agents,” said Mark G. Kris, MD, co-chair of the expert panel that updated the guidelines.
“The full benefit of these treatment advances will only be realized, however, if evidence-based guidelines are fully implemented.”
Key recommendations in the updated guidelines include:
For adults receiving chemotherapy with a high risk for nausea and vomiting (eg, cisplatin or the combination of cyclophosphamide and an anthracycline), olanzapine should be added to standard antiemetic regimens (the combination of a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and dexamethasone). Olanzapine also helps individuals who experience symptoms despite receiving medicines to prevent vomiting before chemotherapy is given.
For adults receiving carboplatin-based chemotherapy or high-dose chemotherapy and children receiving chemotherapy with a high risk for nausea and vomiting, an NK1 receptor antagonist should be added to the standard antiemetic regimen (the combination of 5-HT3 receptor antagonist and dexamethasone).
Dexamethasone treatment can be limited to the day of chemotherapy administration in patients receiving an anthracycline and cyclophosphamide.
Dronabinol and nabilone, cannabinoids approved by the US Food and Drug Administration, can be used to treat nausea and vomiting that is resistant to standard antiemetic therapies. Evidence remains insufficient to recommend medical marijuana for either prevention or treatment of nausea and vomiting in patients with cancer receiving chemotherapy or radiation therapy. ![]()
The American Society of Clinical Oncology (ASCO) has updated its clinical practice guidelines on the use of antiemetics in cancer patients.
The update, published in the Journal of Clinical Oncology, provides new evidence-based information on the appropriate use of olanzapine, NK1 receptor antagonists, and dexamethasone.
“The adverse impact of inadequately controlled nausea and vomiting on patients’ quality of life is well documented,” said Paul J. Hesketh, MD, co-chair of the ASCO expert panel that updated the guidelines.
“By following the ASCO antiemetics guideline, clinicians have the opportunity to improve patients’ quality of life by minimizing treatment-induced emesis.”
To update ASCO’s guidelines on antiemetics, the expert panel conducted a systematic review of the medical literature published between November 2009 and June 2016. The panel included members with expertise in medical oncology, radiation oncology, nursing, pharmacy, and health services research, as well as a patient representative.
“Tremendous progress has been realized over the last 25 years in the prevention of chemotherapy-induced nausea and vomiting with the introduction of new classes of antiemetic agents,” said Mark G. Kris, MD, co-chair of the expert panel that updated the guidelines.
“The full benefit of these treatment advances will only be realized, however, if evidence-based guidelines are fully implemented.”
Key recommendations in the updated guidelines include:
For adults receiving chemotherapy with a high risk for nausea and vomiting (eg, cisplatin or the combination of cyclophosphamide and an anthracycline), olanzapine should be added to standard antiemetic regimens (the combination of a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and dexamethasone). Olanzapine also helps individuals who experience symptoms despite receiving medicines to prevent vomiting before chemotherapy is given.
For adults receiving carboplatin-based chemotherapy or high-dose chemotherapy and children receiving chemotherapy with a high risk for nausea and vomiting, an NK1 receptor antagonist should be added to the standard antiemetic regimen (the combination of 5-HT3 receptor antagonist and dexamethasone).
Dexamethasone treatment can be limited to the day of chemotherapy administration in patients receiving an anthracycline and cyclophosphamide.
Dronabinol and nabilone, cannabinoids approved by the US Food and Drug Administration, can be used to treat nausea and vomiting that is resistant to standard antiemetic therapies. Evidence remains insufficient to recommend medical marijuana for either prevention or treatment of nausea and vomiting in patients with cancer receiving chemotherapy or radiation therapy.
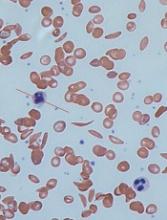
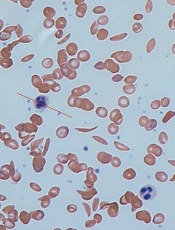
Models provide new understanding of sickle cell disease
Computer models have revealed new details of what happens inside a red blood cell affected by sickle cell disease (SCD), according to research published in Biophysical Journal.
In patients with SCD, mutated hemoglobin can polymerize, assembling into long fibers that push against the membranes of red blood cells and force them out of shape.
“The goal of our work is to model both how these sickle hemoglobin fibers form as well as the mechanical properties of those fibers,” said study author Lu Lu, a PhD student at Brown University in Providence, Rhode Island.
“There had been separate models for each of these things individually developed by us, but this brings those together into one comprehensive model.”
The model uses detailed biomechanical data on how sickle hemoglobin molecules behave and bind with each other to simulate the assembly of a polymer fiber.
Prior to this work, the problem had been that, as the fiber grows, so does the amount of data the model must crunch. Modeling an entire polymer fiber at a cellular scale using the details of each molecule was simply too computationally expensive.
“Even the world’s fastest supercomputers wouldn’t be able to handle it,” said study author George Karniadakis, PhD, of Brown University.
“There’s just too much happening and no way to capture it all computationally. That’s what we were able to overcome with this work.”
The researchers’ solution was to apply what they call a mesoscopic adaptive resolution scheme (MARS).
The MARS model calculates the detailed dynamics of each individual hemoglobin molecule only at the end of polymer fibers, where new molecules are being recruited into the fiber.
Once 4 layers of a fiber have been established, the model automatically dials back the resolution at which it represents that section. The model retains the important information about how the fiber behaves mechanically but glosses over the fine details of each constituent molecule.
“By eliminating the fine details where we don’t need them, we develop a model that can simulate this whole process and its effects on a red blood cell,” Dr Karniadakis said.
Using the new MARS simulations, the researchers were able to show how different configurations of growing polymer fibers are able to produce cells with different shapes.
“We are able to produce a polymerization profile for each of the cell types associated with the disease,” Dr Karniadakis said. “Now, the goal is to use these models to look for ways of preventing the disease onset.”
Using these new models, Dr Karniadakis and his colleagues can run simulations that include fetal hemoglobin. Those simulations could be used to confirm the theory that fetal hemoglobin disrupts polymerization, as well as determine how much fetal hemoglobin is necessary.
That could help in establishing better dosage guidelines for hydroxyurea or in developing new and more effective drugs for SCD, according to the researchers.
“The models give us a way to do preliminary testing on new approaches to stopping this disease,” Dr Karniadakis said. “Now that we can simulate the entire polymerization process, we think the models will be much more useful.”
Computer models have revealed new details of what happens inside a red blood cell affected by sickle cell disease (SCD), according to research published in Biophysical Journal.
In patients with SCD, mutated hemoglobin can polymerize, assembling into long fibers that push against the membranes of red blood cells and force them out of shape.
“The goal of our work is to model both how these sickle hemoglobin fibers form as well as the mechanical properties of those fibers,” said study author Lu Lu, a PhD student at Brown University in Providence, Rhode Island.
“There had been separate models for each of these things individually developed by us, but this brings those together into one comprehensive model.”
The model uses detailed biomechanical data on how sickle hemoglobin molecules behave and bind with each other to simulate the assembly of a polymer fiber.
Prior to this work, the problem had been that, as the fiber grows, so does the amount of data the model must crunch. Modeling an entire polymer fiber at a cellular scale using the details of each molecule was simply too computationally expensive.
“Even the world’s fastest supercomputers wouldn’t be able to handle it,” said study author George Karniadakis, PhD, of Brown University.
“There’s just too much happening and no way to capture it all computationally. That’s what we were able to overcome with this work.”
The researchers’ solution was to apply what they call a mesoscopic adaptive resolution scheme (MARS).
The MARS model calculates the detailed dynamics of each individual hemoglobin molecule only at the end of polymer fibers, where new molecules are being recruited into the fiber.
Once 4 layers of a fiber have been established, the model automatically dials back the resolution at which it represents that section. The model retains the important information about how the fiber behaves mechanically but glosses over the fine details of each constituent molecule.
“By eliminating the fine details where we don’t need them, we develop a model that can simulate this whole process and its effects on a red blood cell,” Dr Karniadakis said.
Using the new MARS simulations, the researchers were able to show how different configurations of growing polymer fibers are able to produce cells with different shapes.
“We are able to produce a polymerization profile for each of the cell types associated with the disease,” Dr Karniadakis said. “Now, the goal is to use these models to look for ways of preventing the disease onset.”
Using these new models, Dr Karniadakis and his colleagues can run simulations that include fetal hemoglobin. Those simulations could be used to confirm the theory that fetal hemoglobin disrupts polymerization, as well as determine how much fetal hemoglobin is necessary.
That could help in establishing better dosage guidelines for hydroxyurea or in developing new and more effective drugs for SCD, according to the researchers.
“The models give us a way to do preliminary testing on new approaches to stopping this disease,” Dr Karniadakis said. “Now that we can simulate the entire polymerization process, we think the models will be much more useful.”
Computer models have revealed new details of what happens inside a red blood cell affected by sickle cell disease (SCD), according to research published in Biophysical Journal.
In patients with SCD, mutated hemoglobin can polymerize, assembling into long fibers that push against the membranes of red blood cells and force them out of shape.
“The goal of our work is to model both how these sickle hemoglobin fibers form as well as the mechanical properties of those fibers,” said study author Lu Lu, a PhD student at Brown University in Providence, Rhode Island.
“There had been separate models for each of these things individually developed by us, but this brings those together into one comprehensive model.”
The model uses detailed biomechanical data on how sickle hemoglobin molecules behave and bind with each other to simulate the assembly of a polymer fiber.
Prior to this work, the problem had been that, as the fiber grows, so does the amount of data the model must crunch. Modeling an entire polymer fiber at a cellular scale using the details of each molecule was simply too computationally expensive.
“Even the world’s fastest supercomputers wouldn’t be able to handle it,” said study author George Karniadakis, PhD, of Brown University.
“There’s just too much happening and no way to capture it all computationally. That’s what we were able to overcome with this work.”
The researchers’ solution was to apply what they call a mesoscopic adaptive resolution scheme (MARS).
The MARS model calculates the detailed dynamics of each individual hemoglobin molecule only at the end of polymer fibers, where new molecules are being recruited into the fiber.
Once 4 layers of a fiber have been established, the model automatically dials back the resolution at which it represents that section. The model retains the important information about how the fiber behaves mechanically but glosses over the fine details of each constituent molecule.
“By eliminating the fine details where we don’t need them, we develop a model that can simulate this whole process and its effects on a red blood cell,” Dr Karniadakis said.
Using the new MARS simulations, the researchers were able to show how different configurations of growing polymer fibers are able to produce cells with different shapes.
“We are able to produce a polymerization profile for each of the cell types associated with the disease,” Dr Karniadakis said. “Now, the goal is to use these models to look for ways of preventing the disease onset.”
Using these new models, Dr Karniadakis and his colleagues can run simulations that include fetal hemoglobin. Those simulations could be used to confirm the theory that fetal hemoglobin disrupts polymerization, as well as determine how much fetal hemoglobin is necessary.
That could help in establishing better dosage guidelines for hydroxyurea or in developing new and more effective drugs for SCD, according to the researchers.
“The models give us a way to do preliminary testing on new approaches to stopping this disease,” Dr Karniadakis said. “Now that we can simulate the entire polymerization process, we think the models will be much more useful.”
FDA grants drug breakthrough designation for AML
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to venetoclax (Venclexta®).
The designation is for venetoclax in combination with low-dose cytarabine to treat elderly patients with previously untreated acute myeloid leukemia (AML) who are ineligible for intensive chemotherapy.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
About venetoclax
Venetoclax is a small molecule designed to selectively bind and inhibit the BCL-2 protein. The drug is being developed by AbbVie and Roche.
Last year, the FDA granted venetoclax accelerated approval to treat patients with chronic lymphocytic leukemia who have 17p deletion and have received at least one prior therapy. Continued approval of venetoclax for this indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA granted venetoclax breakthrough therapy designation for the AML indication based on data from an ongoing phase 1/2 study. Preliminary data from the study were presented at the 22nd European Hematology Association (EHA) Annual Congress.
The presentation included data on 61 elderly patients (older than 65) with previously untreated AML who were ineligible for intensive chemotherapy.
They received venetoclax in combination with low-dose cytarabine (as well as prophylaxis for tumor lysis syndrome). The patients’ median time on treatment was 6 months (range, <1 to 19 months), and 72% of patients discontinued treatment.
The overall response rate was 65%. Twenty-five percent of patients achieved a complete response, 38% had a complete response with incomplete blood count recovery, and 2% had a partial response.
The 30-day death rate was 3%, the 60-day death rate was 15%, and the median overall survival was approximately 12 months.
The most common adverse events of any grade (occurring in at least 30% of patients) were nausea (74%), hypokalemia (46%), diarrhea (46%), fatigue (44%), decreased appetite (41%), constipation (34%), hypomagnesemia (34%), vomiting (31%), thrombocytopenia (44%), febrile neutropenia (38%), and neutropenia (33%).
Grade 3/4 adverse events (occurring in at least 10% of patients) included thrombocytopenia (44%), febrile neutropenia (36%), neutropenia (33%), anemia (28%), hypokalemia (16%), hypophosphatemia (13%), and hypertension (12%).
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to venetoclax (Venclexta®).
The designation is for venetoclax in combination with low-dose cytarabine to treat elderly patients with previously untreated acute myeloid leukemia (AML) who are ineligible for intensive chemotherapy.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
About venetoclax
Venetoclax is a small molecule designed to selectively bind and inhibit the BCL-2 protein. The drug is being developed by AbbVie and Roche.
Last year, the FDA granted venetoclax accelerated approval to treat patients with chronic lymphocytic leukemia who have 17p deletion and have received at least one prior therapy. Continued approval of venetoclax for this indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA granted venetoclax breakthrough therapy designation for the AML indication based on data from an ongoing phase 1/2 study. Preliminary data from the study were presented at the 22nd European Hematology Association (EHA) Annual Congress.
The presentation included data on 61 elderly patients (older than 65) with previously untreated AML who were ineligible for intensive chemotherapy.
They received venetoclax in combination with low-dose cytarabine (as well as prophylaxis for tumor lysis syndrome). The patients’ median time on treatment was 6 months (range, <1 to 19 months), and 72% of patients discontinued treatment.
The overall response rate was 65%. Twenty-five percent of patients achieved a complete response, 38% had a complete response with incomplete blood count recovery, and 2% had a partial response.
The 30-day death rate was 3%, the 60-day death rate was 15%, and the median overall survival was approximately 12 months.
The most common adverse events of any grade (occurring in at least 30% of patients) were nausea (74%), hypokalemia (46%), diarrhea (46%), fatigue (44%), decreased appetite (41%), constipation (34%), hypomagnesemia (34%), vomiting (31%), thrombocytopenia (44%), febrile neutropenia (38%), and neutropenia (33%).
Grade 3/4 adverse events (occurring in at least 10% of patients) included thrombocytopenia (44%), febrile neutropenia (36%), neutropenia (33%), anemia (28%), hypokalemia (16%), hypophosphatemia (13%), and hypertension (12%).
The US Food and Drug Administration (FDA) has granted breakthrough therapy designation to venetoclax (Venclexta®).
The designation is for venetoclax in combination with low-dose cytarabine to treat elderly patients with previously untreated acute myeloid leukemia (AML) who are ineligible for intensive chemotherapy.
The FDA’s breakthrough designation is intended to expedite the development and review of new treatments for serious or life-threatening conditions.
Breakthrough designation entitles the company developing a therapy to more intensive FDA guidance on an efficient and accelerated development program, as well as eligibility for other actions to expedite FDA review, such as a rolling submission and priority review.
To earn breakthrough designation, a treatment must show encouraging early clinical results demonstrating substantial improvement over available therapies with regard to a clinically significant endpoint, or it must fulfill an unmet need.
About venetoclax
Venetoclax is a small molecule designed to selectively bind and inhibit the BCL-2 protein. The drug is being developed by AbbVie and Roche.
Last year, the FDA granted venetoclax accelerated approval to treat patients with chronic lymphocytic leukemia who have 17p deletion and have received at least one prior therapy. Continued approval of venetoclax for this indication may be contingent upon verification of clinical benefit in confirmatory trials.
The FDA granted venetoclax breakthrough therapy designation for the AML indication based on data from an ongoing phase 1/2 study. Preliminary data from the study were presented at the 22nd European Hematology Association (EHA) Annual Congress.
The presentation included data on 61 elderly patients (older than 65) with previously untreated AML who were ineligible for intensive chemotherapy.
They received venetoclax in combination with low-dose cytarabine (as well as prophylaxis for tumor lysis syndrome). The patients’ median time on treatment was 6 months (range, <1 to 19 months), and 72% of patients discontinued treatment.
The overall response rate was 65%. Twenty-five percent of patients achieved a complete response, 38% had a complete response with incomplete blood count recovery, and 2% had a partial response.
The 30-day death rate was 3%, the 60-day death rate was 15%, and the median overall survival was approximately 12 months.
The most common adverse events of any grade (occurring in at least 30% of patients) were nausea (74%), hypokalemia (46%), diarrhea (46%), fatigue (44%), decreased appetite (41%), constipation (34%), hypomagnesemia (34%), vomiting (31%), thrombocytopenia (44%), febrile neutropenia (38%), and neutropenia (33%).
Grade 3/4 adverse events (occurring in at least 10% of patients) included thrombocytopenia (44%), febrile neutropenia (36%), neutropenia (33%), anemia (28%), hypokalemia (16%), hypophosphatemia (13%), and hypertension (12%).
FDA clears new plasmapheresis system
The US Food and Drug Administration (FDA) has granted 510(k) clearance for Haemonetics Corporation’s NexSys PCS™ plasmapheresis system.
The open architecture of NexSys PCS facilitates bi-directional connectivity to donor management systems, enabling automated collection procedure programming and automated end-of-procedure documentation.
The guided operation, large touch screen, and on-screen troubleshooting assistance on NexSys PCS are designed to improve plasma center efficiency. The goal is to reduce donors’ time in centers and improve the centers’ collection capacity.
“NexSys PCS is designed to increase productivity and improve quality and compliance in plasma collection centers,” said Christopher Simon, CEO of Haemonetics.
“Each of these benefits is noteworthy and, when combined, we believe will unlock meaningful value for our customers.”
Haemonetics plans to begin limited production of NexSys PCS devices immediately and to pursue further regulatory clearances for additional enhancements to the overall product offering.
NexSys PCS was previously referred to as PCS 300.
The US Food and Drug Administration (FDA) has granted 510(k) clearance for Haemonetics Corporation’s NexSys PCS™ plasmapheresis system.
The open architecture of NexSys PCS facilitates bi-directional connectivity to donor management systems, enabling automated collection procedure programming and automated end-of-procedure documentation.
The guided operation, large touch screen, and on-screen troubleshooting assistance on NexSys PCS are designed to improve plasma center efficiency. The goal is to reduce donors’ time in centers and improve the centers’ collection capacity.
“NexSys PCS is designed to increase productivity and improve quality and compliance in plasma collection centers,” said Christopher Simon, CEO of Haemonetics.
“Each of these benefits is noteworthy and, when combined, we believe will unlock meaningful value for our customers.”
Haemonetics plans to begin limited production of NexSys PCS devices immediately and to pursue further regulatory clearances for additional enhancements to the overall product offering.
NexSys PCS was previously referred to as PCS 300.
The US Food and Drug Administration (FDA) has granted 510(k) clearance for Haemonetics Corporation’s NexSys PCS™ plasmapheresis system.
The open architecture of NexSys PCS facilitates bi-directional connectivity to donor management systems, enabling automated collection procedure programming and automated end-of-procedure documentation.
The guided operation, large touch screen, and on-screen troubleshooting assistance on NexSys PCS are designed to improve plasma center efficiency. The goal is to reduce donors’ time in centers and improve the centers’ collection capacity.
“NexSys PCS is designed to increase productivity and improve quality and compliance in plasma collection centers,” said Christopher Simon, CEO of Haemonetics.
“Each of these benefits is noteworthy and, when combined, we believe will unlock meaningful value for our customers.”
Haemonetics plans to begin limited production of NexSys PCS devices immediately and to pursue further regulatory clearances for additional enhancements to the overall product offering.
NexSys PCS was previously referred to as PCS 300.