Article
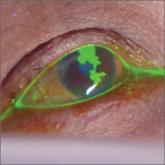
Painful facial blisters, fever, and conjunctivitis
- Author:
- Melissa Neuman, MD
- Jack Spittler, MD
Following Tx for facial blisters, our patient returned with what appeared to be viral conjunctivitis. Further evaluation revealed a missed tip-off...
Article

How do hyaluronic acid and corticosteroid injections compare for knee OA relief?
- Author:
- Corey Lyon, DO
- Emily Spencer, MD
- Jack Spittler, MD
- Kristen Desanto, MSLS, MS, RD, AHIP
EVIDENCE-BASED ANSWER: Inconsistent evidence shows a small amount of pain relief early (one week to 3 months) with corticosteroid (CS) injections...
