User login
Online clinic saves time and money, researchers say
An online clinic launched by HealthPartners Health Plan in Minneapolis delivered savings of $88 per care episode – plus high patient satisfaction ratings – for simple conditions such as acute sinusitis and urinary tract infections, according to a study published Feb. 4 in the Health Affairs.
The study, which compared the cost of visits to HealthPartners virtual clinic – virtuwell – to non-virtuwell visits, showed that well-designed online care can save health costs and increase patients’ access to care.
Dr. Neil Calman, president and CEO for the New York City–based Institute for Family Health, responded to these findings in an interview: "Online visits are one of many electronic interactions that are becoming more prevalent every day.
"Technology, especially the almost ubiquitous evolution of handheld devices like smartphones, has facilitated interactions with supermarkets, airlines, major merchandisers, and now with health care providers as well. In the past, our offices were open at our convenience. But moving forward, we must make health care interactions convenient and accessible to our patients. This is part of a very important movement to increase patient engagement in care and improve access and quality while decreasing cost," he noted.
Dr. Jeffrey J. Cain, president of the American Academy of Family Physicians, noted that the AAFP applauds opportunities for patients to communicate with physicians on newer platforms, such as e-visits, but only when it occurs in the context of a patient-centered home and there is an existing face-to-face relationship between the patient and the primary care physician giving the advice.
Dr. Patrick T. Courneya, a family physician and medical director of HealthPartners Health Plan in Minneapolis, and his coauthors, noted that "Virtuwell’s early results suggest that online care has the potential to meet the ‘triple aim’ goals of a better health care experience for patients, improved population health, and more affordable health care – especially for conditions typically associated with primary care" (Health Aff. 2013; 32:385-92 [doi:10.1377/hlthaff.2012.1157]).
In an interview, Dr. Courneya said that he sees the scope of care provided by virtuwell as comparable to that provided by retail clinics. "We can’t remove a splinter virtually, but when you look at the list of services you can get at one of the retail clinics, it’s obvious that we can meet the lion’s share of visits that are common to them," he said.
About half of those patients who come to virtuwell wind up needing care at a different venue, and about half also do not have a primary care relationship, Dr. Courneya said.
And that is exactly what worried Dr. Cain: "The problem with a virtual clinic such as the one described in the study is that it may exist outside the context of the patient-centered medical home. When health care is as dysfunctional as it is in many parts of the United States, a patient may get one piece of care from a virtual clinic, another from a walk-in clinic, a third from the emergency department, and still another from a primary care provider. All these providers do not communicate with one another. The result may be the ordering of duplicate tests and medication.
And yes, the visit to the e-clinic may be inexpensive but in the end all that fragmented care delivered without coordination drives up health care costs for that patient and for the country, said Dr. Cain, a family physician in Denver.
In defense of such reservations, Dr. Courneya noted that about half of those patients who come to virtuwell wind up needing care at a different venue, and about half also do not have a primary care relationship. Because of this, HealthPartners has worked with clinics to ensure that patients can connect with a primary care office
As described in the study, the HealthPartners online clinic program, established in 2010, is accessible 24/7 and offers treatment for about 40 simple conditions. It uses sophisticated interview algorithms, plus reviews by nurse practitioners or physician assistants.
Patients visit the site (http://virtuwell.com) and answer questions about their conditions and symptoms, plus their medical histories, allergies, and other medications. A certified nurse practitioner then reviews the information and writes a treatment plan, which usually is ready within a half hour or less. If a prescription is needed, that scrip is sent electronically to a pharmacy chosen by the patient.
The patient may speak to a nurse practitioner at any time during or after the visit – in fact, virtuwell nurse practitioners call patients in about half of the cases, the researchers reported. The retail cost for the visit is $40, although about 85% of virtuwell’s more than 96,000 total customers have used insurance to cover at least some of the cost.
About 40,000 patients have received treatment plans from virtuwell, and another 56,000 patients with symptoms beyond the scope of the service have been referred to in-person providers, according to the researchers. More than three-quarters of those using the service have been female, and most have been aged 24-45.
When measuring total claims costs, the researchers found care provided through virtuwell cost an average of $113.13, compared with $201.16 for care provided through traditional channels. Virtuwell treatment for the three highest volume conditions – acute sinusitis, conjunctivitis, and lower genitourinary system infections – cost $20-$30 less than that of convenience clinics, $80-$142 less that of office visits, $82-$124 less than that of urgent care visits, and $159-$469 less than that of emergency department visits.
In addition, there was no evidence of increased patient demand for health care services, despite round-the-clock availability of the online service. Postvisit surveys indicated that at least 90% of virtuwell visits displaced in-person visits, and only about 6% displaced a "watch and wait" or home care approach.
Dr. Calman noted in an interview that the study offers one indication that "we are at the beginning of a revolution in health information technology."
The shortage of primary care providers nationally, predicted to worsen in the coming years, necessitates a major effort to provide information to people to help them determine when an acute office visit is needed, he said.
"This is not rationing care, but rationalizing care," Dr. Calman stated. "It will save time, save money, and save valuable physician time so that more patients who really need face-to-face care will have it available."
Even if patients opt not to engage in virtual clinics, the Internet gives patients the ability to investigate symptoms and determine if they need to seek care at no cost to the medical system, said Dr. Calman, who is also professor and chair of family medicine and community health at Icahn School of Medicine at Mount Sinai in New York.
Eventually, Dr. Calman said, it may be possible for patients to use algorithm-driven sites similar to virtuwell at no cost to determine whether they need care, potentially saving the price of many office visits. "The more people who do this, the more people will be able to care for themselves. We’re democratizing medical information – taking it out of the hands of the medical community," he said.
Dr. Courneya, Dr. Cain, and Dr. Calman reported that they had no relevant conflicts of interest.
An online clinic launched by HealthPartners Health Plan in Minneapolis delivered savings of $88 per care episode – plus high patient satisfaction ratings – for simple conditions such as acute sinusitis and urinary tract infections, according to a study published Feb. 4 in the Health Affairs.
The study, which compared the cost of visits to HealthPartners virtual clinic – virtuwell – to non-virtuwell visits, showed that well-designed online care can save health costs and increase patients’ access to care.
Dr. Neil Calman, president and CEO for the New York City–based Institute for Family Health, responded to these findings in an interview: "Online visits are one of many electronic interactions that are becoming more prevalent every day.
"Technology, especially the almost ubiquitous evolution of handheld devices like smartphones, has facilitated interactions with supermarkets, airlines, major merchandisers, and now with health care providers as well. In the past, our offices were open at our convenience. But moving forward, we must make health care interactions convenient and accessible to our patients. This is part of a very important movement to increase patient engagement in care and improve access and quality while decreasing cost," he noted.
Dr. Jeffrey J. Cain, president of the American Academy of Family Physicians, noted that the AAFP applauds opportunities for patients to communicate with physicians on newer platforms, such as e-visits, but only when it occurs in the context of a patient-centered home and there is an existing face-to-face relationship between the patient and the primary care physician giving the advice.
Dr. Patrick T. Courneya, a family physician and medical director of HealthPartners Health Plan in Minneapolis, and his coauthors, noted that "Virtuwell’s early results suggest that online care has the potential to meet the ‘triple aim’ goals of a better health care experience for patients, improved population health, and more affordable health care – especially for conditions typically associated with primary care" (Health Aff. 2013; 32:385-92 [doi:10.1377/hlthaff.2012.1157]).
In an interview, Dr. Courneya said that he sees the scope of care provided by virtuwell as comparable to that provided by retail clinics. "We can’t remove a splinter virtually, but when you look at the list of services you can get at one of the retail clinics, it’s obvious that we can meet the lion’s share of visits that are common to them," he said.
About half of those patients who come to virtuwell wind up needing care at a different venue, and about half also do not have a primary care relationship, Dr. Courneya said.
And that is exactly what worried Dr. Cain: "The problem with a virtual clinic such as the one described in the study is that it may exist outside the context of the patient-centered medical home. When health care is as dysfunctional as it is in many parts of the United States, a patient may get one piece of care from a virtual clinic, another from a walk-in clinic, a third from the emergency department, and still another from a primary care provider. All these providers do not communicate with one another. The result may be the ordering of duplicate tests and medication.
And yes, the visit to the e-clinic may be inexpensive but in the end all that fragmented care delivered without coordination drives up health care costs for that patient and for the country, said Dr. Cain, a family physician in Denver.
In defense of such reservations, Dr. Courneya noted that about half of those patients who come to virtuwell wind up needing care at a different venue, and about half also do not have a primary care relationship. Because of this, HealthPartners has worked with clinics to ensure that patients can connect with a primary care office
As described in the study, the HealthPartners online clinic program, established in 2010, is accessible 24/7 and offers treatment for about 40 simple conditions. It uses sophisticated interview algorithms, plus reviews by nurse practitioners or physician assistants.
Patients visit the site (http://virtuwell.com) and answer questions about their conditions and symptoms, plus their medical histories, allergies, and other medications. A certified nurse practitioner then reviews the information and writes a treatment plan, which usually is ready within a half hour or less. If a prescription is needed, that scrip is sent electronically to a pharmacy chosen by the patient.
The patient may speak to a nurse practitioner at any time during or after the visit – in fact, virtuwell nurse practitioners call patients in about half of the cases, the researchers reported. The retail cost for the visit is $40, although about 85% of virtuwell’s more than 96,000 total customers have used insurance to cover at least some of the cost.
About 40,000 patients have received treatment plans from virtuwell, and another 56,000 patients with symptoms beyond the scope of the service have been referred to in-person providers, according to the researchers. More than three-quarters of those using the service have been female, and most have been aged 24-45.
When measuring total claims costs, the researchers found care provided through virtuwell cost an average of $113.13, compared with $201.16 for care provided through traditional channels. Virtuwell treatment for the three highest volume conditions – acute sinusitis, conjunctivitis, and lower genitourinary system infections – cost $20-$30 less than that of convenience clinics, $80-$142 less that of office visits, $82-$124 less than that of urgent care visits, and $159-$469 less than that of emergency department visits.
In addition, there was no evidence of increased patient demand for health care services, despite round-the-clock availability of the online service. Postvisit surveys indicated that at least 90% of virtuwell visits displaced in-person visits, and only about 6% displaced a "watch and wait" or home care approach.
Dr. Calman noted in an interview that the study offers one indication that "we are at the beginning of a revolution in health information technology."
The shortage of primary care providers nationally, predicted to worsen in the coming years, necessitates a major effort to provide information to people to help them determine when an acute office visit is needed, he said.
"This is not rationing care, but rationalizing care," Dr. Calman stated. "It will save time, save money, and save valuable physician time so that more patients who really need face-to-face care will have it available."
Even if patients opt not to engage in virtual clinics, the Internet gives patients the ability to investigate symptoms and determine if they need to seek care at no cost to the medical system, said Dr. Calman, who is also professor and chair of family medicine and community health at Icahn School of Medicine at Mount Sinai in New York.
Eventually, Dr. Calman said, it may be possible for patients to use algorithm-driven sites similar to virtuwell at no cost to determine whether they need care, potentially saving the price of many office visits. "The more people who do this, the more people will be able to care for themselves. We’re democratizing medical information – taking it out of the hands of the medical community," he said.
Dr. Courneya, Dr. Cain, and Dr. Calman reported that they had no relevant conflicts of interest.
An online clinic launched by HealthPartners Health Plan in Minneapolis delivered savings of $88 per care episode – plus high patient satisfaction ratings – for simple conditions such as acute sinusitis and urinary tract infections, according to a study published Feb. 4 in the Health Affairs.
The study, which compared the cost of visits to HealthPartners virtual clinic – virtuwell – to non-virtuwell visits, showed that well-designed online care can save health costs and increase patients’ access to care.
Dr. Neil Calman, president and CEO for the New York City–based Institute for Family Health, responded to these findings in an interview: "Online visits are one of many electronic interactions that are becoming more prevalent every day.
"Technology, especially the almost ubiquitous evolution of handheld devices like smartphones, has facilitated interactions with supermarkets, airlines, major merchandisers, and now with health care providers as well. In the past, our offices were open at our convenience. But moving forward, we must make health care interactions convenient and accessible to our patients. This is part of a very important movement to increase patient engagement in care and improve access and quality while decreasing cost," he noted.
Dr. Jeffrey J. Cain, president of the American Academy of Family Physicians, noted that the AAFP applauds opportunities for patients to communicate with physicians on newer platforms, such as e-visits, but only when it occurs in the context of a patient-centered home and there is an existing face-to-face relationship between the patient and the primary care physician giving the advice.
Dr. Patrick T. Courneya, a family physician and medical director of HealthPartners Health Plan in Minneapolis, and his coauthors, noted that "Virtuwell’s early results suggest that online care has the potential to meet the ‘triple aim’ goals of a better health care experience for patients, improved population health, and more affordable health care – especially for conditions typically associated with primary care" (Health Aff. 2013; 32:385-92 [doi:10.1377/hlthaff.2012.1157]).
In an interview, Dr. Courneya said that he sees the scope of care provided by virtuwell as comparable to that provided by retail clinics. "We can’t remove a splinter virtually, but when you look at the list of services you can get at one of the retail clinics, it’s obvious that we can meet the lion’s share of visits that are common to them," he said.
About half of those patients who come to virtuwell wind up needing care at a different venue, and about half also do not have a primary care relationship, Dr. Courneya said.
And that is exactly what worried Dr. Cain: "The problem with a virtual clinic such as the one described in the study is that it may exist outside the context of the patient-centered medical home. When health care is as dysfunctional as it is in many parts of the United States, a patient may get one piece of care from a virtual clinic, another from a walk-in clinic, a third from the emergency department, and still another from a primary care provider. All these providers do not communicate with one another. The result may be the ordering of duplicate tests and medication.
And yes, the visit to the e-clinic may be inexpensive but in the end all that fragmented care delivered without coordination drives up health care costs for that patient and for the country, said Dr. Cain, a family physician in Denver.
In defense of such reservations, Dr. Courneya noted that about half of those patients who come to virtuwell wind up needing care at a different venue, and about half also do not have a primary care relationship. Because of this, HealthPartners has worked with clinics to ensure that patients can connect with a primary care office
As described in the study, the HealthPartners online clinic program, established in 2010, is accessible 24/7 and offers treatment for about 40 simple conditions. It uses sophisticated interview algorithms, plus reviews by nurse practitioners or physician assistants.
Patients visit the site (http://virtuwell.com) and answer questions about their conditions and symptoms, plus their medical histories, allergies, and other medications. A certified nurse practitioner then reviews the information and writes a treatment plan, which usually is ready within a half hour or less. If a prescription is needed, that scrip is sent electronically to a pharmacy chosen by the patient.
The patient may speak to a nurse practitioner at any time during or after the visit – in fact, virtuwell nurse practitioners call patients in about half of the cases, the researchers reported. The retail cost for the visit is $40, although about 85% of virtuwell’s more than 96,000 total customers have used insurance to cover at least some of the cost.
About 40,000 patients have received treatment plans from virtuwell, and another 56,000 patients with symptoms beyond the scope of the service have been referred to in-person providers, according to the researchers. More than three-quarters of those using the service have been female, and most have been aged 24-45.
When measuring total claims costs, the researchers found care provided through virtuwell cost an average of $113.13, compared with $201.16 for care provided through traditional channels. Virtuwell treatment for the three highest volume conditions – acute sinusitis, conjunctivitis, and lower genitourinary system infections – cost $20-$30 less than that of convenience clinics, $80-$142 less that of office visits, $82-$124 less than that of urgent care visits, and $159-$469 less than that of emergency department visits.
In addition, there was no evidence of increased patient demand for health care services, despite round-the-clock availability of the online service. Postvisit surveys indicated that at least 90% of virtuwell visits displaced in-person visits, and only about 6% displaced a "watch and wait" or home care approach.
Dr. Calman noted in an interview that the study offers one indication that "we are at the beginning of a revolution in health information technology."
The shortage of primary care providers nationally, predicted to worsen in the coming years, necessitates a major effort to provide information to people to help them determine when an acute office visit is needed, he said.
"This is not rationing care, but rationalizing care," Dr. Calman stated. "It will save time, save money, and save valuable physician time so that more patients who really need face-to-face care will have it available."
Even if patients opt not to engage in virtual clinics, the Internet gives patients the ability to investigate symptoms and determine if they need to seek care at no cost to the medical system, said Dr. Calman, who is also professor and chair of family medicine and community health at Icahn School of Medicine at Mount Sinai in New York.
Eventually, Dr. Calman said, it may be possible for patients to use algorithm-driven sites similar to virtuwell at no cost to determine whether they need care, potentially saving the price of many office visits. "The more people who do this, the more people will be able to care for themselves. We’re democratizing medical information – taking it out of the hands of the medical community," he said.
Dr. Courneya, Dr. Cain, and Dr. Calman reported that they had no relevant conflicts of interest.
FROM HEALTH AFFAIRS
Major finding: An online clinic led to savings of $88 per care episode.
Data source: Comparison of 4,008 online care episodes and 175,678 care episodes handled in traditional settings.
Disclosures: Dr. Courneya is medical director of HealthPartners, which conducted the study. There were no other disclosures.
School suspension, expulsion on pediatricians' radar
Out-of-school suspensions and expulsions broadly affect students, and pediatricians should stand ready to help children and their families affected by these disciplinary tactics while working to encourage alternatives, a policy statement from the American Academy of Pediatrics recommends.
The policy statement, published Feb. 25 in Pediatrics, notes that research has demonstrated not only that "zero-tolerance policies" can be ineffective deterrents, but also, in fact, they can be harmful to students.
The statement (doi:10.1542/peds.2012-3932) urges pediatricians to screen children early for behavioral problems so that they can be referred to Head Start or other community resources, and to communicate with school health officials about how to assist or support school-age students who have behavior problems before those problems result in suspension or expulsion.
Finally, the policy urges pediatricians to learn about their local school districts’ policies on disciplinary actions that remove students from school, and advocate for policies that focus on prevention and positive behavior change.
"Out-of-school suspension and expulsion can contribute to the risk of a student dropping out of high school," the authors wrote. "The costs of a person’s failure to complete his or her secondary education are significant and are borne by society as a whole."
Out-of-school suspensions and expulsions broadly affect students, and pediatricians should stand ready to help children and their families affected by these disciplinary tactics while working to encourage alternatives, a policy statement from the American Academy of Pediatrics recommends.
The policy statement, published Feb. 25 in Pediatrics, notes that research has demonstrated not only that "zero-tolerance policies" can be ineffective deterrents, but also, in fact, they can be harmful to students.
The statement (doi:10.1542/peds.2012-3932) urges pediatricians to screen children early for behavioral problems so that they can be referred to Head Start or other community resources, and to communicate with school health officials about how to assist or support school-age students who have behavior problems before those problems result in suspension or expulsion.
Finally, the policy urges pediatricians to learn about their local school districts’ policies on disciplinary actions that remove students from school, and advocate for policies that focus on prevention and positive behavior change.
"Out-of-school suspension and expulsion can contribute to the risk of a student dropping out of high school," the authors wrote. "The costs of a person’s failure to complete his or her secondary education are significant and are borne by society as a whole."
Out-of-school suspensions and expulsions broadly affect students, and pediatricians should stand ready to help children and their families affected by these disciplinary tactics while working to encourage alternatives, a policy statement from the American Academy of Pediatrics recommends.
The policy statement, published Feb. 25 in Pediatrics, notes that research has demonstrated not only that "zero-tolerance policies" can be ineffective deterrents, but also, in fact, they can be harmful to students.
The statement (doi:10.1542/peds.2012-3932) urges pediatricians to screen children early for behavioral problems so that they can be referred to Head Start or other community resources, and to communicate with school health officials about how to assist or support school-age students who have behavior problems before those problems result in suspension or expulsion.
Finally, the policy urges pediatricians to learn about their local school districts’ policies on disciplinary actions that remove students from school, and advocate for policies that focus on prevention and positive behavior change.
"Out-of-school suspension and expulsion can contribute to the risk of a student dropping out of high school," the authors wrote. "The costs of a person’s failure to complete his or her secondary education are significant and are borne by society as a whole."
FROM PEDIATRICS
Alcohol counseling often missed in teen visits
Just over half of 10th graders who saw a physician in the past year were asked about their use of alcohol and fewer were counseled about the dangers of alcohol abuse.
Ralph W. Hingson, Sc.D., and his colleagues at the National Institutes of Health surveyed 2,519 10th graders, and found that 36% reported drinking in the past month, 28% reported binge-drinking, and 23% reported drunkenness. More than 1 in 10 said they drank alcohol more than six times in the past month, and about 1 in 20 said they binge-drank in the past month, the researchers found. The study was published Jan. 31 in Pediatrics.
More than 80% of teen respondents said they had seen a doctor in the past year; of those, 54% reported that their physician had asked about drinking. A total of 40% were advised about potential harms from drinking, and 17% were advised to reduce or stop drinking, the study reported. Among those teens who reported frequent binge drinking, only 21% were advised to cut back or stop (Pediatrics 2013;131:249-57).
In comparison, physicians advised 36% of frequent smokers, 27% of frequent marijuana users, and 42% of those who said they used other drugs frequently to reduce or quit those behaviors.
Since it’s illegal to sell alcohol to minors, many physicians may not realize that drinking needs to be explored, Dr. Hingson and colleagues speculated. Even so, teen smoking and drug use also are illegal, and more physicians asked about those problems than asked about drinking.
"Per clinical practice recommendations, alcohol screening should be universal," they wrote. "Patients with unhealthy alcohol use patterns are less likely to be detected when screening is not routine."
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; and the Health Resources and Services Administration, with supplemental support from the National Institute on Drug Abuse. As federal employees, the authors have no commercial conflicts of interest.
Just over half of 10th graders who saw a physician in the past year were asked about their use of alcohol and fewer were counseled about the dangers of alcohol abuse.
Ralph W. Hingson, Sc.D., and his colleagues at the National Institutes of Health surveyed 2,519 10th graders, and found that 36% reported drinking in the past month, 28% reported binge-drinking, and 23% reported drunkenness. More than 1 in 10 said they drank alcohol more than six times in the past month, and about 1 in 20 said they binge-drank in the past month, the researchers found. The study was published Jan. 31 in Pediatrics.
More than 80% of teen respondents said they had seen a doctor in the past year; of those, 54% reported that their physician had asked about drinking. A total of 40% were advised about potential harms from drinking, and 17% were advised to reduce or stop drinking, the study reported. Among those teens who reported frequent binge drinking, only 21% were advised to cut back or stop (Pediatrics 2013;131:249-57).
In comparison, physicians advised 36% of frequent smokers, 27% of frequent marijuana users, and 42% of those who said they used other drugs frequently to reduce or quit those behaviors.
Since it’s illegal to sell alcohol to minors, many physicians may not realize that drinking needs to be explored, Dr. Hingson and colleagues speculated. Even so, teen smoking and drug use also are illegal, and more physicians asked about those problems than asked about drinking.
"Per clinical practice recommendations, alcohol screening should be universal," they wrote. "Patients with unhealthy alcohol use patterns are less likely to be detected when screening is not routine."
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; and the Health Resources and Services Administration, with supplemental support from the National Institute on Drug Abuse. As federal employees, the authors have no commercial conflicts of interest.
Just over half of 10th graders who saw a physician in the past year were asked about their use of alcohol and fewer were counseled about the dangers of alcohol abuse.
Ralph W. Hingson, Sc.D., and his colleagues at the National Institutes of Health surveyed 2,519 10th graders, and found that 36% reported drinking in the past month, 28% reported binge-drinking, and 23% reported drunkenness. More than 1 in 10 said they drank alcohol more than six times in the past month, and about 1 in 20 said they binge-drank in the past month, the researchers found. The study was published Jan. 31 in Pediatrics.
More than 80% of teen respondents said they had seen a doctor in the past year; of those, 54% reported that their physician had asked about drinking. A total of 40% were advised about potential harms from drinking, and 17% were advised to reduce or stop drinking, the study reported. Among those teens who reported frequent binge drinking, only 21% were advised to cut back or stop (Pediatrics 2013;131:249-57).
In comparison, physicians advised 36% of frequent smokers, 27% of frequent marijuana users, and 42% of those who said they used other drugs frequently to reduce or quit those behaviors.
Since it’s illegal to sell alcohol to minors, many physicians may not realize that drinking needs to be explored, Dr. Hingson and colleagues speculated. Even so, teen smoking and drug use also are illegal, and more physicians asked about those problems than asked about drinking.
"Per clinical practice recommendations, alcohol screening should be universal," they wrote. "Patients with unhealthy alcohol use patterns are less likely to be detected when screening is not routine."
The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; and the Health Resources and Services Administration, with supplemental support from the National Institute on Drug Abuse. As federal employees, the authors have no commercial conflicts of interest.
FROM PEDIATRICS
Major Finding: Counseling on harmful behaviors was inconsistent as 21% of teens were advised to reduce/stop binge drinking while 36% were advised to reduce/stop smoking.
Data Source: The NEXT Generation Health Study, an in-school study of 2,519 students in 10th grade.
Disclosures: The study was funded by several institutes of the National Institutes of Health. The authors, as federal employees, had no conflicts of interest to disclose.
Practice changes warrant residency reforms
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these." The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis ( Ann. Surg. 2012;256:553-9).
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekends, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The effects of this and various technology changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote. They laid out potential ways in which residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas..
• There should be earlier specialty focus in residency training for those residents who already know the specialty they would like to pursue.
• Residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area,
• Training should expand to include additional skills, such as the use of ultrasound and the use of interventional catheter techniques.
The authors reported no conflicts.
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these." The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis ( Ann. Surg. 2012;256:553-9).
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekends, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The effects of this and various technology changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote. They laid out potential ways in which residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas..
• There should be earlier specialty focus in residency training for those residents who already know the specialty they would like to pursue.
• Residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area,
• Training should expand to include additional skills, such as the use of ultrasound and the use of interventional catheter techniques.
The authors reported no conflicts.
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these." The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis ( Ann. Surg. 2012;256:553-9).
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekends, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The effects of this and various technology changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote. They laid out potential ways in which residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas..
• There should be earlier specialty focus in residency training for those residents who already know the specialty they would like to pursue.
• Residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area,
• Training should expand to include additional skills, such as the use of ultrasound and the use of interventional catheter techniques.
The authors reported no conflicts.
Changes Warrant Residency Reforms
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these," Dr. Frank Lewis and Dr. Mary Klingensmith wrote. "Evidence is now emerging of significant issues in the overall performance of recent graduates from at least three sources – the evaluation of external agents who incorporate these graduates into their practice or group, the opinions of the residents themselves, and the performance of graduates on the oral examination of the American Board of Surgery during the last 8 years" (Ann. Surg. 2012;256:553-59).
The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis.
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekend experience, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The most significant clinical change has been the development of laparoscopic surgery for intra-abdominal surgical management, which is replacing open surgery and the abdominal incision. Because surgeons in academic settings have been slower to adopt laparoscopy, resident training in the use of this technology has proceeded slowly, they explained.
"While the Residency Review Committee (RRC) for Surgery has been steadily increasing the requirements for surgical resident training, it is still the rule that the most complex laparoscopic surgery is reserved for fellows in postresidency fellowships and not for residents during surgical training, although there is no reason this should be the case," they noted.
In addition, operations performed by general surgeons, and the way in which they are done, have changed significantly in the past 20 years, according to the analysis. For example, the advent of better medical management for benign peptic ulcer disease – along with flexible endoscopy and endoscopic retrograde cholangiopancreatography – means that fewer surgical interventions for peptic ulcer complications and biliary tree stone disease are necessary.
Furthermore, technological innovations have allowed vascular surgeons, rather than general surgeons, to perform most abdominal vascular surgery. Finally, the two surgeons reported, abdominal trauma injuries – which require surgical intervention in 80%-90% of cases – have declined dramatically since 1992.
These types of changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote.
They laid out seven potential ways in which surgical residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas, such as laparoscopic surgery and endoscopic surgery.
• There should be an earlier specialty focus in residency training for those surgical residents who already know which specialty they would like to pursue.
• Surgical residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area, so "any discussion of extending residency only applies to the 20% of residents who currently complete only general surgical residency and do not seek subspecialty training," they said. "Extending residency by 1 year to obtain more extensive training in general surgery per se would not seem to be an insurmountable issue if the benefits clearly warranted it."
• Surgical training should expand to include additional skills, such as the use of ultrasound for better diagnosis of conditions in breast, endocrine, vascular, and trauma diseases and the use of interventional catheter techniques for the diagnosis or treatment of a variety of conditions.
It’s not possible to reverse the changes that have occurred over the past 2 decades, and in fact the workweek could see further shortening, as has happened in Europe, the investigators noted. "The most effective way in which to address the changes is therefore to look at the things which can be changed in resident training, the many areas in which improvements in resident teaching are possible, and the areas in which residents’ capabilities could be productively expanded."
The investigators did not report any conflicts of interest.
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these," Dr. Frank Lewis and Dr. Mary Klingensmith wrote. "Evidence is now emerging of significant issues in the overall performance of recent graduates from at least three sources – the evaluation of external agents who incorporate these graduates into their practice or group, the opinions of the residents themselves, and the performance of graduates on the oral examination of the American Board of Surgery during the last 8 years" (Ann. Surg. 2012;256:553-59).
The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis.
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekend experience, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The most significant clinical change has been the development of laparoscopic surgery for intra-abdominal surgical management, which is replacing open surgery and the abdominal incision. Because surgeons in academic settings have been slower to adopt laparoscopy, resident training in the use of this technology has proceeded slowly, they explained.
"While the Residency Review Committee (RRC) for Surgery has been steadily increasing the requirements for surgical resident training, it is still the rule that the most complex laparoscopic surgery is reserved for fellows in postresidency fellowships and not for residents during surgical training, although there is no reason this should be the case," they noted.
In addition, operations performed by general surgeons, and the way in which they are done, have changed significantly in the past 20 years, according to the analysis. For example, the advent of better medical management for benign peptic ulcer disease – along with flexible endoscopy and endoscopic retrograde cholangiopancreatography – means that fewer surgical interventions for peptic ulcer complications and biliary tree stone disease are necessary.
Furthermore, technological innovations have allowed vascular surgeons, rather than general surgeons, to perform most abdominal vascular surgery. Finally, the two surgeons reported, abdominal trauma injuries – which require surgical intervention in 80%-90% of cases – have declined dramatically since 1992.
These types of changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote.
They laid out seven potential ways in which surgical residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas, such as laparoscopic surgery and endoscopic surgery.
• There should be an earlier specialty focus in residency training for those surgical residents who already know which specialty they would like to pursue.
• Surgical residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area, so "any discussion of extending residency only applies to the 20% of residents who currently complete only general surgical residency and do not seek subspecialty training," they said. "Extending residency by 1 year to obtain more extensive training in general surgery per se would not seem to be an insurmountable issue if the benefits clearly warranted it."
• Surgical training should expand to include additional skills, such as the use of ultrasound for better diagnosis of conditions in breast, endocrine, vascular, and trauma diseases and the use of interventional catheter techniques for the diagnosis or treatment of a variety of conditions.
It’s not possible to reverse the changes that have occurred over the past 2 decades, and in fact the workweek could see further shortening, as has happened in Europe, the investigators noted. "The most effective way in which to address the changes is therefore to look at the things which can be changed in resident training, the many areas in which improvements in resident teaching are possible, and the areas in which residents’ capabilities could be productively expanded."
The investigators did not report any conflicts of interest.
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these," Dr. Frank Lewis and Dr. Mary Klingensmith wrote. "Evidence is now emerging of significant issues in the overall performance of recent graduates from at least three sources – the evaluation of external agents who incorporate these graduates into their practice or group, the opinions of the residents themselves, and the performance of graduates on the oral examination of the American Board of Surgery during the last 8 years" (Ann. Surg. 2012;256:553-59).
The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis.
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekend experience, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The most significant clinical change has been the development of laparoscopic surgery for intra-abdominal surgical management, which is replacing open surgery and the abdominal incision. Because surgeons in academic settings have been slower to adopt laparoscopy, resident training in the use of this technology has proceeded slowly, they explained.
"While the Residency Review Committee (RRC) for Surgery has been steadily increasing the requirements for surgical resident training, it is still the rule that the most complex laparoscopic surgery is reserved for fellows in postresidency fellowships and not for residents during surgical training, although there is no reason this should be the case," they noted.
In addition, operations performed by general surgeons, and the way in which they are done, have changed significantly in the past 20 years, according to the analysis. For example, the advent of better medical management for benign peptic ulcer disease – along with flexible endoscopy and endoscopic retrograde cholangiopancreatography – means that fewer surgical interventions for peptic ulcer complications and biliary tree stone disease are necessary.
Furthermore, technological innovations have allowed vascular surgeons, rather than general surgeons, to perform most abdominal vascular surgery. Finally, the two surgeons reported, abdominal trauma injuries – which require surgical intervention in 80%-90% of cases – have declined dramatically since 1992.
These types of changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote.
They laid out seven potential ways in which surgical residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas, such as laparoscopic surgery and endoscopic surgery.
• There should be an earlier specialty focus in residency training for those surgical residents who already know which specialty they would like to pursue.
• Surgical residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area, so "any discussion of extending residency only applies to the 20% of residents who currently complete only general surgical residency and do not seek subspecialty training," they said. "Extending residency by 1 year to obtain more extensive training in general surgery per se would not seem to be an insurmountable issue if the benefits clearly warranted it."
• Surgical training should expand to include additional skills, such as the use of ultrasound for better diagnosis of conditions in breast, endocrine, vascular, and trauma diseases and the use of interventional catheter techniques for the diagnosis or treatment of a variety of conditions.
It’s not possible to reverse the changes that have occurred over the past 2 decades, and in fact the workweek could see further shortening, as has happened in Europe, the investigators noted. "The most effective way in which to address the changes is therefore to look at the things which can be changed in resident training, the many areas in which improvements in resident teaching are possible, and the areas in which residents’ capabilities could be productively expanded."
The investigators did not report any conflicts of interest.
EXPERT ANALYSIS FROM ANNALS OF SURGERY
ACP: Performance Measures for 'Low-Value' Services Needed
Performance measures targeting services that provide little value for patients have the potential to help control health care costs by changing physicians’ behavior through feedback and possible financial incentives, according to a policy paper from the American College of Physicians published Oct. 30 in Annals of Internal Medicine.
To date, performance measurement data mainly have been used to encourage physicians to provide more high-value services, such as immunizations and medications for chronic diseases. But measures for low-value services could prove equally valuable.
"The first step in addressing the high cost of health care should be decreasing use of interventions that provide no or very little benefit and are of low value," according to the policy paper. "For example, at the same time that we should be measuring the proportion of patients age 50 to 75 [years] who have been screened for colorectal cancer, we should be assessing the proportion of patients over the age of 75 who had colorectal cancer screening that was not indicated."
Diagnostic imaging for uncomplicated low back pain is another example of a low-value intervention, the paper noted, because the evidence indicates that the use of routine x-ray or advanced imaging methods does not improve outcomes for patients.
Low-value services include those for which the harms likely exceed the benefits and those that may provide benefits, but for which the tradeoff between benefits and costs is undesirable, the policy paper indicated. There’s no universally accepted "bright line" that defines the point where the tradeoff indicates a service isn’t cost-effective, the authors wrote, adding, "this will ultimately be a societal decision that depends on how much money we are willing to spend on health care, as well as societal priorities."
Measures that target low-value interventions likely will need to be applied at the level of the hospital or the multispecialty group practice because many individual physicians won’t see enough patients with the target conditions.
"In addition, primary care physicians and specialists are often involved in decision making, and both should be held accountable rather than just the person who ordered the test," the paper said.
The policy recommends that performance measures should be based on high-quality evidence that assesses the benefits, risks, and costs of interventions. Like other performance measures, those for low-value services could be used for feedback and public reporting, and to provide financial incentives to change physician behavior, according to the ACP.
Performance measures targeting services that provide little value for patients have the potential to help control health care costs by changing physicians’ behavior through feedback and possible financial incentives, according to a policy paper from the American College of Physicians published Oct. 30 in Annals of Internal Medicine.
To date, performance measurement data mainly have been used to encourage physicians to provide more high-value services, such as immunizations and medications for chronic diseases. But measures for low-value services could prove equally valuable.
"The first step in addressing the high cost of health care should be decreasing use of interventions that provide no or very little benefit and are of low value," according to the policy paper. "For example, at the same time that we should be measuring the proportion of patients age 50 to 75 [years] who have been screened for colorectal cancer, we should be assessing the proportion of patients over the age of 75 who had colorectal cancer screening that was not indicated."
Diagnostic imaging for uncomplicated low back pain is another example of a low-value intervention, the paper noted, because the evidence indicates that the use of routine x-ray or advanced imaging methods does not improve outcomes for patients.
Low-value services include those for which the harms likely exceed the benefits and those that may provide benefits, but for which the tradeoff between benefits and costs is undesirable, the policy paper indicated. There’s no universally accepted "bright line" that defines the point where the tradeoff indicates a service isn’t cost-effective, the authors wrote, adding, "this will ultimately be a societal decision that depends on how much money we are willing to spend on health care, as well as societal priorities."
Measures that target low-value interventions likely will need to be applied at the level of the hospital or the multispecialty group practice because many individual physicians won’t see enough patients with the target conditions.
"In addition, primary care physicians and specialists are often involved in decision making, and both should be held accountable rather than just the person who ordered the test," the paper said.
The policy recommends that performance measures should be based on high-quality evidence that assesses the benefits, risks, and costs of interventions. Like other performance measures, those for low-value services could be used for feedback and public reporting, and to provide financial incentives to change physician behavior, according to the ACP.
Performance measures targeting services that provide little value for patients have the potential to help control health care costs by changing physicians’ behavior through feedback and possible financial incentives, according to a policy paper from the American College of Physicians published Oct. 30 in Annals of Internal Medicine.
To date, performance measurement data mainly have been used to encourage physicians to provide more high-value services, such as immunizations and medications for chronic diseases. But measures for low-value services could prove equally valuable.
"The first step in addressing the high cost of health care should be decreasing use of interventions that provide no or very little benefit and are of low value," according to the policy paper. "For example, at the same time that we should be measuring the proportion of patients age 50 to 75 [years] who have been screened for colorectal cancer, we should be assessing the proportion of patients over the age of 75 who had colorectal cancer screening that was not indicated."
Diagnostic imaging for uncomplicated low back pain is another example of a low-value intervention, the paper noted, because the evidence indicates that the use of routine x-ray or advanced imaging methods does not improve outcomes for patients.
Low-value services include those for which the harms likely exceed the benefits and those that may provide benefits, but for which the tradeoff between benefits and costs is undesirable, the policy paper indicated. There’s no universally accepted "bright line" that defines the point where the tradeoff indicates a service isn’t cost-effective, the authors wrote, adding, "this will ultimately be a societal decision that depends on how much money we are willing to spend on health care, as well as societal priorities."
Measures that target low-value interventions likely will need to be applied at the level of the hospital or the multispecialty group practice because many individual physicians won’t see enough patients with the target conditions.
"In addition, primary care physicians and specialists are often involved in decision making, and both should be held accountable rather than just the person who ordered the test," the paper said.
The policy recommends that performance measures should be based on high-quality evidence that assesses the benefits, risks, and costs of interventions. Like other performance measures, those for low-value services could be used for feedback and public reporting, and to provide financial incentives to change physician behavior, according to the ACP.
FROM ANNALS OF INTERNAL MEDICINE
Analysis: Surgical Practice Changes Warrant Residency Reforms
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these," Dr. Frank Lewis and Dr. Mary Klingensmith wrote. "Evidence is now emerging of significant issues in the overall performance of recent graduates from at least three sources – the evaluation of external agents who incorporate these graduates into their practice or group, the opinions of the residents themselves, and the performance of graduates on the oral examination of the American Board of Surgery during the last 8 years" (Ann. Surg. 2012;256:553-59).
The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis.
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekend experience, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The most significant clinical change has been the development of laparoscopic surgery for intra-abdominal surgical management, which is replacing open surgery and the abdominal incision. Because surgeons in academic settings have been slower to adopt laparoscopy, resident training in the use of this technology has proceeded slowly, they explained.
"While the Residency Review Committee (RRC) for Surgery has been steadily increasing the requirements for surgical resident training, it is still the rule that the most complex laparoscopic surgery is reserved for fellows in postresidency fellowships and not for residents during surgical training, although there is no reason this should be the case," they noted.
In addition, operations performed by general surgeons, and the way in which they are done, have changed significantly in the past 20 years, according to the analysis. For example, the advent of better medical management for benign peptic ulcer disease – along with flexible endoscopy and endoscopic retrograde cholangiopancreatography – means that fewer surgical interventions for peptic ulcer complications and biliary tree stone disease are necessary.
Furthermore, technological innovations have allowed vascular surgeons, rather than general surgeons, to perform most abdominal vascular surgery. Finally, the two surgeons reported, abdominal trauma injuries – which require surgical intervention in 80%-90% of cases – have declined dramatically since 1992.
These types of changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote.
They laid out seven potential ways in which surgical residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas, such as laparoscopic surgery and endoscopic surgery.
• There should be an earlier specialty focus in residency training for those surgical residents who already know which specialty they would like to pursue.
• Surgical residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area, so "any discussion of extending residency only applies to the 20% of residents who currently complete only general surgical residency and do not seek subspecialty training," they said. "Extending residency by 1 year to obtain more extensive training in general surgery per se would not seem to be an insurmountable issue if the benefits clearly warranted it."
• Surgical training should expand to include additional skills, such as the use of ultrasound for better diagnosis of conditions in breast, endocrine, vascular, and trauma diseases and the use of interventional catheter techniques for the diagnosis or treatment of a variety of conditions.
It’s not possible to reverse the changes that have occurred over the past 2 decades, and in fact the workweek could see further shortening, as has happened in Europe, the investigators noted. "The most effective way in which to address the changes is therefore to look at the things which can be changed in resident training, the many areas in which improvements in resident teaching are possible, and the areas in which residents’ capabilities could be productively expanded."
The investigators did not report any conflicts of interest.
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these," Dr. Frank Lewis and Dr. Mary Klingensmith wrote. "Evidence is now emerging of significant issues in the overall performance of recent graduates from at least three sources – the evaluation of external agents who incorporate these graduates into their practice or group, the opinions of the residents themselves, and the performance of graduates on the oral examination of the American Board of Surgery during the last 8 years" (Ann. Surg. 2012;256:553-59).
The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis.
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekend experience, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The most significant clinical change has been the development of laparoscopic surgery for intra-abdominal surgical management, which is replacing open surgery and the abdominal incision. Because surgeons in academic settings have been slower to adopt laparoscopy, resident training in the use of this technology has proceeded slowly, they explained.
"While the Residency Review Committee (RRC) for Surgery has been steadily increasing the requirements for surgical resident training, it is still the rule that the most complex laparoscopic surgery is reserved for fellows in postresidency fellowships and not for residents during surgical training, although there is no reason this should be the case," they noted.
In addition, operations performed by general surgeons, and the way in which they are done, have changed significantly in the past 20 years, according to the analysis. For example, the advent of better medical management for benign peptic ulcer disease – along with flexible endoscopy and endoscopic retrograde cholangiopancreatography – means that fewer surgical interventions for peptic ulcer complications and biliary tree stone disease are necessary.
Furthermore, technological innovations have allowed vascular surgeons, rather than general surgeons, to perform most abdominal vascular surgery. Finally, the two surgeons reported, abdominal trauma injuries – which require surgical intervention in 80%-90% of cases – have declined dramatically since 1992.
These types of changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote.
They laid out seven potential ways in which surgical residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas, such as laparoscopic surgery and endoscopic surgery.
• There should be an earlier specialty focus in residency training for those surgical residents who already know which specialty they would like to pursue.
• Surgical residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area, so "any discussion of extending residency only applies to the 20% of residents who currently complete only general surgical residency and do not seek subspecialty training," they said. "Extending residency by 1 year to obtain more extensive training in general surgery per se would not seem to be an insurmountable issue if the benefits clearly warranted it."
• Surgical training should expand to include additional skills, such as the use of ultrasound for better diagnosis of conditions in breast, endocrine, vascular, and trauma diseases and the use of interventional catheter techniques for the diagnosis or treatment of a variety of conditions.
It’s not possible to reverse the changes that have occurred over the past 2 decades, and in fact the workweek could see further shortening, as has happened in Europe, the investigators noted. "The most effective way in which to address the changes is therefore to look at the things which can be changed in resident training, the many areas in which improvements in resident teaching are possible, and the areas in which residents’ capabilities could be productively expanded."
The investigators did not report any conflicts of interest.
Surgical residency programs have not kept up with radical changes in the practice of surgery over the past two decades, but innovations ranging from curriculum reform to increasing the length of residency could help to improve the overall performance of recent surgical residency graduates, according to an analysis in Annals of Surgery.
"The changes that have occurred have been disruptive to residency training, and to date there has been minimal compensation for these," Dr. Frank Lewis and Dr. Mary Klingensmith wrote. "Evidence is now emerging of significant issues in the overall performance of recent graduates from at least three sources – the evaluation of external agents who incorporate these graduates into their practice or group, the opinions of the residents themselves, and the performance of graduates on the oral examination of the American Board of Surgery during the last 8 years" (Ann. Surg. 2012;256:553-59).
The changes include not only the 80-hour workweek for surgical residents, but also clinical areas, according to Dr. Lewis, executive director of the American Board of Surgery, and Dr. Klingensmith, residency program director at Washington University in St. Louis.
The effect of the 80-hour workweek has been a reduction by 6 months to a year of in-hospital experience during 5 years of residency. Most of that reduced time corresponds to night and weekend experience, when residents would be more likely to see urgent and emergent conditions, and to have a greater degree of independent functioning, autonomy, and indirect supervision, they said.
The most significant clinical change has been the development of laparoscopic surgery for intra-abdominal surgical management, which is replacing open surgery and the abdominal incision. Because surgeons in academic settings have been slower to adopt laparoscopy, resident training in the use of this technology has proceeded slowly, they explained.
"While the Residency Review Committee (RRC) for Surgery has been steadily increasing the requirements for surgical resident training, it is still the rule that the most complex laparoscopic surgery is reserved for fellows in postresidency fellowships and not for residents during surgical training, although there is no reason this should be the case," they noted.
In addition, operations performed by general surgeons, and the way in which they are done, have changed significantly in the past 20 years, according to the analysis. For example, the advent of better medical management for benign peptic ulcer disease – along with flexible endoscopy and endoscopic retrograde cholangiopancreatography – means that fewer surgical interventions for peptic ulcer complications and biliary tree stone disease are necessary.
Furthermore, technological innovations have allowed vascular surgeons, rather than general surgeons, to perform most abdominal vascular surgery. Finally, the two surgeons reported, abdominal trauma injuries – which require surgical intervention in 80%-90% of cases – have declined dramatically since 1992.
These types of changes "will undoubtedly continue, and the directions in which surgery will evolve in the future are not predictable," Dr. Lewis and Dr. Klingensmith wrote.
They laid out seven potential ways in which surgical residency programs can address the changes:
• There should be a continuous process to define and continually update the surgical residency curriculum, which needs to keep pace with the fast-changing surgical practice landscape, and to "prune" information related to diseases that no longer are seen frequently in practice.
"The starting point for making changes in residency is to recognize that much of what is being taught is obsolete, and addresses diseases that are no longer a significant problem, or those for which surgical treatment is rarely needed," they said.
• Residency programs should improve the efficacy of resident learning by reducing clerical functions for residents, using physician extenders where appropriate, and utilizing mobile computing technology to deliver "a more defined and comprehensive curriculum to residents at an individual level."
• Educators could make better use of simulators in certain areas, such as laparoscopic surgery and endoscopic surgery.
• There should be an earlier specialty focus in residency training for those surgical residents who already know which specialty they would like to pursue.
• Surgical residency should include expanded laparoscopic surgery training.
• Residency programs could increase in length to make up for the time lost to the 80-hour workweek rule. Four-fifths of surgical residents already elect to take a postresidency fellowship in a specialty or subspecialty area, so "any discussion of extending residency only applies to the 20% of residents who currently complete only general surgical residency and do not seek subspecialty training," they said. "Extending residency by 1 year to obtain more extensive training in general surgery per se would not seem to be an insurmountable issue if the benefits clearly warranted it."
• Surgical training should expand to include additional skills, such as the use of ultrasound for better diagnosis of conditions in breast, endocrine, vascular, and trauma diseases and the use of interventional catheter techniques for the diagnosis or treatment of a variety of conditions.
It’s not possible to reverse the changes that have occurred over the past 2 decades, and in fact the workweek could see further shortening, as has happened in Europe, the investigators noted. "The most effective way in which to address the changes is therefore to look at the things which can be changed in resident training, the many areas in which improvements in resident teaching are possible, and the areas in which residents’ capabilities could be productively expanded."
The investigators did not report any conflicts of interest.
EXPERT ANALYSIS FROM ANNALS OF SURGERY
AAP President-Elect Outlines Goals
Dr. James Perrin, who will take office as the American Academy of Pediatrics’ president in January, said he has three main goals for his term: Make sure health reform works for children and pediatricians; continue pediatric practice transformation efforts; and capitalize on diversity in the pediatric workforce.
Dr. Perrin, professor of pediatrics at Harvard Medical School and head of the division of general pediatrics at the Massachusetts General Hospital, both in Boston, was chosen as AAP president-elect in October. He said in an interview that these efforts all can help pediatricians care for children, especially children with chronic conditions such as asthma, mental health conditions, developmental disorders, and obesity.
"There’s a belief that chronic disease isn’t all that common in children, but we have lots and lots of children in practices that have chronic health conditions," he said. Moving toward a team care approach, as is advocated in both the Affordable Care Act and in practice transformation efforts championed by the AAP, can help take care of those children.
"To take care of the child with autism takes two times the amount of time of a child without autism," he said, adding that for practices to care appropriately for children with complex needs requires changes in the current payment system. In addition, Dr. Perrin noted that the pediatric workforce has become substantially more diverse, both in terms of race and in terms of gender. He said one of his goals is to enable mentoring programs, especially among women and minorities, that can help bring those pediatricians into leadership roles.
Dr. James Perrin, who will take office as the American Academy of Pediatrics’ president in January, said he has three main goals for his term: Make sure health reform works for children and pediatricians; continue pediatric practice transformation efforts; and capitalize on diversity in the pediatric workforce.
Dr. Perrin, professor of pediatrics at Harvard Medical School and head of the division of general pediatrics at the Massachusetts General Hospital, both in Boston, was chosen as AAP president-elect in October. He said in an interview that these efforts all can help pediatricians care for children, especially children with chronic conditions such as asthma, mental health conditions, developmental disorders, and obesity.
"There’s a belief that chronic disease isn’t all that common in children, but we have lots and lots of children in practices that have chronic health conditions," he said. Moving toward a team care approach, as is advocated in both the Affordable Care Act and in practice transformation efforts championed by the AAP, can help take care of those children.
"To take care of the child with autism takes two times the amount of time of a child without autism," he said, adding that for practices to care appropriately for children with complex needs requires changes in the current payment system. In addition, Dr. Perrin noted that the pediatric workforce has become substantially more diverse, both in terms of race and in terms of gender. He said one of his goals is to enable mentoring programs, especially among women and minorities, that can help bring those pediatricians into leadership roles.
Dr. James Perrin, who will take office as the American Academy of Pediatrics’ president in January, said he has three main goals for his term: Make sure health reform works for children and pediatricians; continue pediatric practice transformation efforts; and capitalize on diversity in the pediatric workforce.
Dr. Perrin, professor of pediatrics at Harvard Medical School and head of the division of general pediatrics at the Massachusetts General Hospital, both in Boston, was chosen as AAP president-elect in October. He said in an interview that these efforts all can help pediatricians care for children, especially children with chronic conditions such as asthma, mental health conditions, developmental disorders, and obesity.
"There’s a belief that chronic disease isn’t all that common in children, but we have lots and lots of children in practices that have chronic health conditions," he said. Moving toward a team care approach, as is advocated in both the Affordable Care Act and in practice transformation efforts championed by the AAP, can help take care of those children.
"To take care of the child with autism takes two times the amount of time of a child without autism," he said, adding that for practices to care appropriately for children with complex needs requires changes in the current payment system. In addition, Dr. Perrin noted that the pediatric workforce has become substantially more diverse, both in terms of race and in terms of gender. He said one of his goals is to enable mentoring programs, especially among women and minorities, that can help bring those pediatricians into leadership roles.
Americans Making Fewer Doctor Visits, Census Says
People aged 18-64 years are visiting the doctor less frequently than they did a decade ago: Average annual medical provider visits dropped about 19%, from 4.8 per year in 2001 to 3.9 per year in 2010, according to a report from the U.S. Census Bureau.
While the government did not delve into why, factors such as increasing insurance and copayment costs, declining middle-class income, and growing numbers of uninsured likely are behind the numbers, according to Dr. James Fasules, senior vice president for advocacy for the American College of Cardiology.
"For the middle class, disposable income has dropped," Dr. Fasules said in an interview. "People might make the decision that it would be better to have food on the table than to do a [preventive or elective] procedure."
But putting off necessary care ultimately costs the system more, Dr. Fasules pointed out. "If someone is not addressing their hypertension, is not taking care of their diabetes, by the time they present [for care], they’re much sicker and it costs more."
The report, "Health Status, Health Insurance, and Medical Services Utilization: 2010," looked at the number of visits to medical providers and dentists, the number of nights spent in the hospital, and the number of people who used prescription drugs per year. The report found that the average number of medical provider visits decreased among all groups, including those in poor health and those with insurance, between 2001 and 2010.
Among those people reporting at least one medical provider visit per year, the average number of medical provider visits fell from 6.4 per year in 2001 to 5.4 in 2010, the report said. For people who said they were in fair or poor health, the average number of visits fell from 12.9 per year to 11.6 per year.
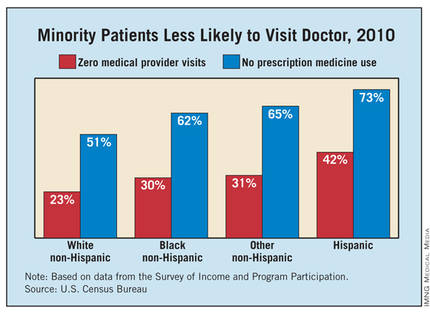
Less than a quarter (24%) of uninsured individuals reported at least one yearly medical visit in 2010, compared with 28% in 2001, the Census found. Additionally, the percentage of uninsured individuals who received routine checkups decreased from 14% in 2001 to 12% in 2010.
"Here’s glaring data that a lot of people don’t have access to care," said Dr. Glen Stream, president of the American Academy of Family Physicians.
Dr. Stream also cited several potential factors in the decrease in visits: the rise in insurance premiums and out-of-pocket costs, the poor economy, the shortage of physicians, and the difficulty in getting timely appointments.
The decline in medical visits hasn’t affected individual family doctors, Dr. Stream said in an interview, since most already are working as much as they can. "When you don’t have an adequate supply of family physicians, they’re all working at or above capacity. It’s not typical that practices are seeing an inadequate number of patients coming to the door."
The census report also looked at health status. It found that close to one-third of all people aged 18-64 years reported excellent health in 2010, while another 57% reported "very good" or "good" health. Almost 8% said their health was just "fair," and a little more than 2% called their health "poor." More men than women called their health "excellent," and non-Hispanic blacks were both least likely to report excellent health and most likely to report fair or poor health.
Health status and medical services utilization were linked in the report, with people who reported excellent health less likely to use services than people in poor health. Among those reporting excellent health in 2010, 68% visited a medical provider at least once in the previous 12 months, 4% reported one or more overnight stays in a hospital, and 30% said they took prescription medication in the previous 12 months.
Meanwhile, among those who reported poor health in 2010, 94.3% said they visited a medical provider at least once, 40.5% said they had at least one overnight stay in a hospital, and 91.5% took at least one prescription medication, the report found.
People aged 18-64 years are visiting the doctor less frequently than they did a decade ago: Average annual medical provider visits dropped about 19%, from 4.8 per year in 2001 to 3.9 per year in 2010, according to a report from the U.S. Census Bureau.
While the government did not delve into why, factors such as increasing insurance and copayment costs, declining middle-class income, and growing numbers of uninsured likely are behind the numbers, according to Dr. James Fasules, senior vice president for advocacy for the American College of Cardiology.
"For the middle class, disposable income has dropped," Dr. Fasules said in an interview. "People might make the decision that it would be better to have food on the table than to do a [preventive or elective] procedure."
But putting off necessary care ultimately costs the system more, Dr. Fasules pointed out. "If someone is not addressing their hypertension, is not taking care of their diabetes, by the time they present [for care], they’re much sicker and it costs more."
The report, "Health Status, Health Insurance, and Medical Services Utilization: 2010," looked at the number of visits to medical providers and dentists, the number of nights spent in the hospital, and the number of people who used prescription drugs per year. The report found that the average number of medical provider visits decreased among all groups, including those in poor health and those with insurance, between 2001 and 2010.
Among those people reporting at least one medical provider visit per year, the average number of medical provider visits fell from 6.4 per year in 2001 to 5.4 in 2010, the report said. For people who said they were in fair or poor health, the average number of visits fell from 12.9 per year to 11.6 per year.
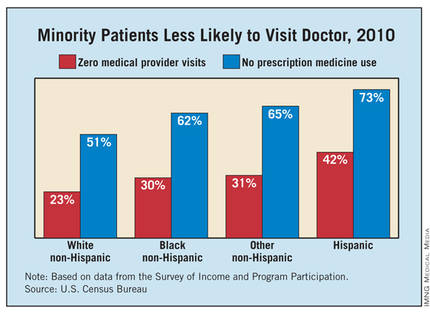
Less than a quarter (24%) of uninsured individuals reported at least one yearly medical visit in 2010, compared with 28% in 2001, the Census found. Additionally, the percentage of uninsured individuals who received routine checkups decreased from 14% in 2001 to 12% in 2010.
"Here’s glaring data that a lot of people don’t have access to care," said Dr. Glen Stream, president of the American Academy of Family Physicians.
Dr. Stream also cited several potential factors in the decrease in visits: the rise in insurance premiums and out-of-pocket costs, the poor economy, the shortage of physicians, and the difficulty in getting timely appointments.
The decline in medical visits hasn’t affected individual family doctors, Dr. Stream said in an interview, since most already are working as much as they can. "When you don’t have an adequate supply of family physicians, they’re all working at or above capacity. It’s not typical that practices are seeing an inadequate number of patients coming to the door."
The census report also looked at health status. It found that close to one-third of all people aged 18-64 years reported excellent health in 2010, while another 57% reported "very good" or "good" health. Almost 8% said their health was just "fair," and a little more than 2% called their health "poor." More men than women called their health "excellent," and non-Hispanic blacks were both least likely to report excellent health and most likely to report fair or poor health.
Health status and medical services utilization were linked in the report, with people who reported excellent health less likely to use services than people in poor health. Among those reporting excellent health in 2010, 68% visited a medical provider at least once in the previous 12 months, 4% reported one or more overnight stays in a hospital, and 30% said they took prescription medication in the previous 12 months.
Meanwhile, among those who reported poor health in 2010, 94.3% said they visited a medical provider at least once, 40.5% said they had at least one overnight stay in a hospital, and 91.5% took at least one prescription medication, the report found.
People aged 18-64 years are visiting the doctor less frequently than they did a decade ago: Average annual medical provider visits dropped about 19%, from 4.8 per year in 2001 to 3.9 per year in 2010, according to a report from the U.S. Census Bureau.
While the government did not delve into why, factors such as increasing insurance and copayment costs, declining middle-class income, and growing numbers of uninsured likely are behind the numbers, according to Dr. James Fasules, senior vice president for advocacy for the American College of Cardiology.
"For the middle class, disposable income has dropped," Dr. Fasules said in an interview. "People might make the decision that it would be better to have food on the table than to do a [preventive or elective] procedure."
But putting off necessary care ultimately costs the system more, Dr. Fasules pointed out. "If someone is not addressing their hypertension, is not taking care of their diabetes, by the time they present [for care], they’re much sicker and it costs more."
The report, "Health Status, Health Insurance, and Medical Services Utilization: 2010," looked at the number of visits to medical providers and dentists, the number of nights spent in the hospital, and the number of people who used prescription drugs per year. The report found that the average number of medical provider visits decreased among all groups, including those in poor health and those with insurance, between 2001 and 2010.
Among those people reporting at least one medical provider visit per year, the average number of medical provider visits fell from 6.4 per year in 2001 to 5.4 in 2010, the report said. For people who said they were in fair or poor health, the average number of visits fell from 12.9 per year to 11.6 per year.
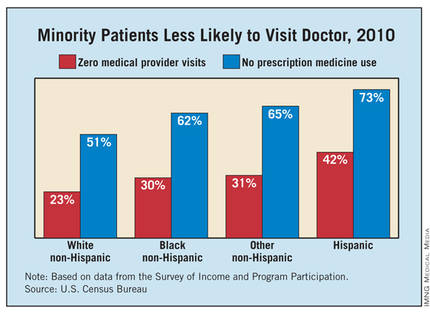
Less than a quarter (24%) of uninsured individuals reported at least one yearly medical visit in 2010, compared with 28% in 2001, the Census found. Additionally, the percentage of uninsured individuals who received routine checkups decreased from 14% in 2001 to 12% in 2010.
"Here’s glaring data that a lot of people don’t have access to care," said Dr. Glen Stream, president of the American Academy of Family Physicians.
Dr. Stream also cited several potential factors in the decrease in visits: the rise in insurance premiums and out-of-pocket costs, the poor economy, the shortage of physicians, and the difficulty in getting timely appointments.
The decline in medical visits hasn’t affected individual family doctors, Dr. Stream said in an interview, since most already are working as much as they can. "When you don’t have an adequate supply of family physicians, they’re all working at or above capacity. It’s not typical that practices are seeing an inadequate number of patients coming to the door."
The census report also looked at health status. It found that close to one-third of all people aged 18-64 years reported excellent health in 2010, while another 57% reported "very good" or "good" health. Almost 8% said their health was just "fair," and a little more than 2% called their health "poor." More men than women called their health "excellent," and non-Hispanic blacks were both least likely to report excellent health and most likely to report fair or poor health.
Health status and medical services utilization were linked in the report, with people who reported excellent health less likely to use services than people in poor health. Among those reporting excellent health in 2010, 68% visited a medical provider at least once in the previous 12 months, 4% reported one or more overnight stays in a hospital, and 30% said they took prescription medication in the previous 12 months.
Meanwhile, among those who reported poor health in 2010, 94.3% said they visited a medical provider at least once, 40.5% said they had at least one overnight stay in a hospital, and 91.5% took at least one prescription medication, the report found.
Open Surgery Tied to Small-Bowel Obstruction Risk
The risk of developing a small-bowel obstruction after open surgery is about fourfold higher when compared with laparoscopic surgery in nine commonly performed abdominal and pelvic procedures, including cholecystectomy, hysterectomy, and appendectomy, investigators reported.
Other factors such as patient age, , prior abdominal surgery, and comorbidities also contributed to the risk of SBO, the study showed. However, laparoscopy "exceeded other risk factors in reduction of the risk of SBO for most of the surgical procedures," wrote Dr. Eva Angenete and her colleagues (Arch. Surg. 2012;147:359-65).
"This study shows that, beyond important factors such as age, previous abdominal surgery, and comorbidity, the surgical technique is the most important factor related to SBO," the authors wrote. "Compared with laparoscopic surgery, open surgery seems to increase the risk of SBO at least four times."
It’s likely that the study results will hold up to further scrutiny because the study was population based and the sample size – 108,141 patients – is large, the authors said.
Still, laparoscopic surgery did not seem to reduce the incidence of SBO in some groups, including hysterectomy patients. "One hypothesis is that this result may be related to a limited dissection in the pelvis," but the small number of laparoscopic hysterectomy patients included in the study could have affected the study’s results, the authors wrote. In addition, there were no clear risk factors for SBO in patients undergoing bariatric surgery, they wrote.
The investigators used the Inpatient Register of the Swedish National Board of Health and Welfare to analyze the risk of SBO in nine procedures, including cholecystectomy, hysterectomy, salpingo-oophorectomy, bowel resection, anterior resection, abdominoperineal resection, rectopexy, appendectomy, and bariatric surgery performed from 2002 to 2004. The database included information on demographic characteristics, comorbidities, previous abdominal surgery, and deaths.
The rate of SBO was lowest after cholecystectomy, occurring in just 0.4% of all cases, and was highest, at 13.9%, in abdominoperineal resection patients. For most surgical procedures, patients who had SBO were older on average. SBO was also more common in patients with previous abdominal surgery.
In those who underwent cholecystectomy, bowel resection, or appendectomy, a higher level of comorbidity was associated with a greater incidence of SBO, the authors said. In the group of complicated cholecystectomy patients as well as the group of anterior resection patients, SBO was more common among men.
SBO was linked with an increased risk of death within 5 years, the study found.
"The aim of this study was to identify the incidence and risk factors for mechanical SBO after a number of common abdominal and pelvic procedures," the authors wrote. "Small-bowel obstruction is a substantial health care challenge, and correctly identified risk factors can provide improved tools to reduce the risk of SBO after an abdominal surgical procedure."
"The safety and the short-term benefits of laparoscopy are already known, and it is possible that laparoscopy should be regarded as the preferred technique in an attempt to further reduce the complications of surgery," the authors concluded.
The project was supported by grants from the Swedish Cancer Foundation, the Swedish Medical Association, the Gothenburg Medical Association, the Assar Gabrielsson Foundation, the Magn Berwall’s Foundation, and the Swedish Research Council. None of the funding sources had any role in the study or the preparation of the manuscript. The authors reported no financial conflicts of interest.
Replacing open abdominal surgery with laparoscopy when possible may offer an opportunity for improved quality of life and decreased morbidity for many patients, along with health care system cost savings, said Dr. Luke M. Funk and Dr. Stanley W. Ashley in an invited critique accompanying the study on small-bowel obstruction (SBO) risk (Arch Surg. 2012;147:365 [doi:10.1001/archsurg.2012.157]).
The finding that SBO risk was lower with laparoscopy even after accounting for patient factors such as age, comorbidities, and previous surgery, has important implications for both the quality and cost of surgical care, Dr. Funk and Dr. Ashley said in their commentary.
"For surgeons, it highlights another potential benefit of minimally invasive surgery and challenges us to continue to offer less invasive procedures whenever they are feasible," they wrote. "For payers and health care policy leaders, it suggests that substantial cost savings could be achieved if open surgery [were] replaced with laparoscopic surgery more often."
Inpatient expenses on adhesiolysis-related complications exceed $2 billion in the United States, they added.
However, to fully realize the benefits of laparoscopy, newer payment models such as bundled or episode-based payments would need to account for the higher initial cost of laparoscopy but lower long-term costs related to shorter hospitalizations, lower complication rates, fewer readmissions, and fewer reoperations, the two surgeons said.
Still, the study’s authors "have provided strong evidence that minimal invasion often results in maximal benefit," Dr. Funk and Dr. Ashley wrote.
Dr. Funk is a general surgeon at Brigham and Women’s Hospital in Boston. Dr. Ashley is vice chairman of the department of surgery at Brigham and Women’s.
Replacing open abdominal surgery with laparoscopy when possible may offer an opportunity for improved quality of life and decreased morbidity for many patients, along with health care system cost savings, said Dr. Luke M. Funk and Dr. Stanley W. Ashley in an invited critique accompanying the study on small-bowel obstruction (SBO) risk (Arch Surg. 2012;147:365 [doi:10.1001/archsurg.2012.157]).
The finding that SBO risk was lower with laparoscopy even after accounting for patient factors such as age, comorbidities, and previous surgery, has important implications for both the quality and cost of surgical care, Dr. Funk and Dr. Ashley said in their commentary.
"For surgeons, it highlights another potential benefit of minimally invasive surgery and challenges us to continue to offer less invasive procedures whenever they are feasible," they wrote. "For payers and health care policy leaders, it suggests that substantial cost savings could be achieved if open surgery [were] replaced with laparoscopic surgery more often."
Inpatient expenses on adhesiolysis-related complications exceed $2 billion in the United States, they added.
However, to fully realize the benefits of laparoscopy, newer payment models such as bundled or episode-based payments would need to account for the higher initial cost of laparoscopy but lower long-term costs related to shorter hospitalizations, lower complication rates, fewer readmissions, and fewer reoperations, the two surgeons said.
Still, the study’s authors "have provided strong evidence that minimal invasion often results in maximal benefit," Dr. Funk and Dr. Ashley wrote.
Dr. Funk is a general surgeon at Brigham and Women’s Hospital in Boston. Dr. Ashley is vice chairman of the department of surgery at Brigham and Women’s.
Replacing open abdominal surgery with laparoscopy when possible may offer an opportunity for improved quality of life and decreased morbidity for many patients, along with health care system cost savings, said Dr. Luke M. Funk and Dr. Stanley W. Ashley in an invited critique accompanying the study on small-bowel obstruction (SBO) risk (Arch Surg. 2012;147:365 [doi:10.1001/archsurg.2012.157]).
The finding that SBO risk was lower with laparoscopy even after accounting for patient factors such as age, comorbidities, and previous surgery, has important implications for both the quality and cost of surgical care, Dr. Funk and Dr. Ashley said in their commentary.
"For surgeons, it highlights another potential benefit of minimally invasive surgery and challenges us to continue to offer less invasive procedures whenever they are feasible," they wrote. "For payers and health care policy leaders, it suggests that substantial cost savings could be achieved if open surgery [were] replaced with laparoscopic surgery more often."
Inpatient expenses on adhesiolysis-related complications exceed $2 billion in the United States, they added.
However, to fully realize the benefits of laparoscopy, newer payment models such as bundled or episode-based payments would need to account for the higher initial cost of laparoscopy but lower long-term costs related to shorter hospitalizations, lower complication rates, fewer readmissions, and fewer reoperations, the two surgeons said.
Still, the study’s authors "have provided strong evidence that minimal invasion often results in maximal benefit," Dr. Funk and Dr. Ashley wrote.
Dr. Funk is a general surgeon at Brigham and Women’s Hospital in Boston. Dr. Ashley is vice chairman of the department of surgery at Brigham and Women’s.
The risk of developing a small-bowel obstruction after open surgery is about fourfold higher when compared with laparoscopic surgery in nine commonly performed abdominal and pelvic procedures, including cholecystectomy, hysterectomy, and appendectomy, investigators reported.
Other factors such as patient age, , prior abdominal surgery, and comorbidities also contributed to the risk of SBO, the study showed. However, laparoscopy "exceeded other risk factors in reduction of the risk of SBO for most of the surgical procedures," wrote Dr. Eva Angenete and her colleagues (Arch. Surg. 2012;147:359-65).
"This study shows that, beyond important factors such as age, previous abdominal surgery, and comorbidity, the surgical technique is the most important factor related to SBO," the authors wrote. "Compared with laparoscopic surgery, open surgery seems to increase the risk of SBO at least four times."
It’s likely that the study results will hold up to further scrutiny because the study was population based and the sample size – 108,141 patients – is large, the authors said.
Still, laparoscopic surgery did not seem to reduce the incidence of SBO in some groups, including hysterectomy patients. "One hypothesis is that this result may be related to a limited dissection in the pelvis," but the small number of laparoscopic hysterectomy patients included in the study could have affected the study’s results, the authors wrote. In addition, there were no clear risk factors for SBO in patients undergoing bariatric surgery, they wrote.
The investigators used the Inpatient Register of the Swedish National Board of Health and Welfare to analyze the risk of SBO in nine procedures, including cholecystectomy, hysterectomy, salpingo-oophorectomy, bowel resection, anterior resection, abdominoperineal resection, rectopexy, appendectomy, and bariatric surgery performed from 2002 to 2004. The database included information on demographic characteristics, comorbidities, previous abdominal surgery, and deaths.
The rate of SBO was lowest after cholecystectomy, occurring in just 0.4% of all cases, and was highest, at 13.9%, in abdominoperineal resection patients. For most surgical procedures, patients who had SBO were older on average. SBO was also more common in patients with previous abdominal surgery.
In those who underwent cholecystectomy, bowel resection, or appendectomy, a higher level of comorbidity was associated with a greater incidence of SBO, the authors said. In the group of complicated cholecystectomy patients as well as the group of anterior resection patients, SBO was more common among men.
SBO was linked with an increased risk of death within 5 years, the study found.
"The aim of this study was to identify the incidence and risk factors for mechanical SBO after a number of common abdominal and pelvic procedures," the authors wrote. "Small-bowel obstruction is a substantial health care challenge, and correctly identified risk factors can provide improved tools to reduce the risk of SBO after an abdominal surgical procedure."
"The safety and the short-term benefits of laparoscopy are already known, and it is possible that laparoscopy should be regarded as the preferred technique in an attempt to further reduce the complications of surgery," the authors concluded.
The project was supported by grants from the Swedish Cancer Foundation, the Swedish Medical Association, the Gothenburg Medical Association, the Assar Gabrielsson Foundation, the Magn Berwall’s Foundation, and the Swedish Research Council. None of the funding sources had any role in the study or the preparation of the manuscript. The authors reported no financial conflicts of interest.
The risk of developing a small-bowel obstruction after open surgery is about fourfold higher when compared with laparoscopic surgery in nine commonly performed abdominal and pelvic procedures, including cholecystectomy, hysterectomy, and appendectomy, investigators reported.
Other factors such as patient age, , prior abdominal surgery, and comorbidities also contributed to the risk of SBO, the study showed. However, laparoscopy "exceeded other risk factors in reduction of the risk of SBO for most of the surgical procedures," wrote Dr. Eva Angenete and her colleagues (Arch. Surg. 2012;147:359-65).
"This study shows that, beyond important factors such as age, previous abdominal surgery, and comorbidity, the surgical technique is the most important factor related to SBO," the authors wrote. "Compared with laparoscopic surgery, open surgery seems to increase the risk of SBO at least four times."
It’s likely that the study results will hold up to further scrutiny because the study was population based and the sample size – 108,141 patients – is large, the authors said.
Still, laparoscopic surgery did not seem to reduce the incidence of SBO in some groups, including hysterectomy patients. "One hypothesis is that this result may be related to a limited dissection in the pelvis," but the small number of laparoscopic hysterectomy patients included in the study could have affected the study’s results, the authors wrote. In addition, there were no clear risk factors for SBO in patients undergoing bariatric surgery, they wrote.
The investigators used the Inpatient Register of the Swedish National Board of Health and Welfare to analyze the risk of SBO in nine procedures, including cholecystectomy, hysterectomy, salpingo-oophorectomy, bowel resection, anterior resection, abdominoperineal resection, rectopexy, appendectomy, and bariatric surgery performed from 2002 to 2004. The database included information on demographic characteristics, comorbidities, previous abdominal surgery, and deaths.
The rate of SBO was lowest after cholecystectomy, occurring in just 0.4% of all cases, and was highest, at 13.9%, in abdominoperineal resection patients. For most surgical procedures, patients who had SBO were older on average. SBO was also more common in patients with previous abdominal surgery.
In those who underwent cholecystectomy, bowel resection, or appendectomy, a higher level of comorbidity was associated with a greater incidence of SBO, the authors said. In the group of complicated cholecystectomy patients as well as the group of anterior resection patients, SBO was more common among men.
SBO was linked with an increased risk of death within 5 years, the study found.
"The aim of this study was to identify the incidence and risk factors for mechanical SBO after a number of common abdominal and pelvic procedures," the authors wrote. "Small-bowel obstruction is a substantial health care challenge, and correctly identified risk factors can provide improved tools to reduce the risk of SBO after an abdominal surgical procedure."
"The safety and the short-term benefits of laparoscopy are already known, and it is possible that laparoscopy should be regarded as the preferred technique in an attempt to further reduce the complications of surgery," the authors concluded.
The project was supported by grants from the Swedish Cancer Foundation, the Swedish Medical Association, the Gothenburg Medical Association, the Assar Gabrielsson Foundation, the Magn Berwall’s Foundation, and the Swedish Research Council. None of the funding sources had any role in the study or the preparation of the manuscript. The authors reported no financial conflicts of interest.
Major Finding: The risk of small-bowel obstruction is four times higher in patients who undergo open surgery than in patients who undergo laparoscopy for nine commonly performed procedures.
Data Source: Data were analyzed from 108,141 cases between 2002 and 2004 from the Inpatient Register of the Swedish National Board of Health and Welfare.
Disclosures: The project was supported by grants from the Swedish Cancer Foundation, the Swedish Medical Association, the Gothenburg Medical Association, the Assar Gabrielsson Foundation, the Magn Berwall’s Foundation, and the Swedish Research Council. None of the funding sources had any role in the study or the preparation of the manuscript. The authors reported no financial conflicts of interest.