Article
A Crisis in Scope: Recruitment and Retention Challenges Reported by VA Gastroenterology Section Chiefs
- Author:
- Erik C. von Rosenvinge, MD
- Stacie A. Vela, MD
- Elizabeth R. Paine, MD
- Michael F. Chang, MD
- Brian J. Hanson, MD
- Tamar Taddei, MD
- Walter E. Smalley, MD
- Kerry B. Dunbar, MD, PhD
- Nabeel H. Khan, MD
- Lyn Sue Kahng, MD
- Jennifer Anwar, MHA
- Robert Zing, RN
- Andrew Gawron, MD
- Jason A. Dominitz, MD
- Gyorgy Baffy, MD, PhD
Having a sufficient number of gastroenterologists is important to protect the digestive health of veterans; however, gastroenterology is among the...
Article
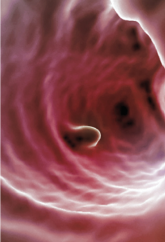
A Nationwide Survey and Needs Assessment of Colonoscopy Quality Assurance Programs
- Author:
- Andrew J. Gawron, MD, PhD, MS
- Phillip Lawrence, PharmD
- Morgan M. Millar, PhD
- Jason A. Dominitz, MD
- Samir Gupta, MD
- Mary Whooley, MD
- Tonya Kaltenbach, MD
Variability exists in quality documentation, measurement, and reporting practices of colonoscopy screening in VA facilities, and most do not have...
News

Colon section: C. diff and colorectal screening
- Author:
- Jason A. Dominitz, MD
Publish date: September 24, 2013
