User login
Survey Time
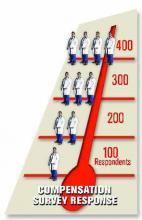
SHM has established an aggressive goal of getting 400 respondents for its biannual Productivity and Compensation Survey. This would mean a 33% increase over the 300 respondents to the 2003 survey. SHM is tracking the number of respondents on its Web site homepage (www.hospitalmedicine.org). All surveys must be completed and returned by Nov. 25.
By now hospital medicine group leaders should have received a copy of the survey with instructions. SHM prefers that you complete the survey online. The response process for the online survey is simplified with built-in edits and a streamlined flow. In addition, you can stop in the middle of the questionnaire and return to complete it later.
WHY SHOULD YOU PARTICIPATE?
- Information: The survey questions represent the metrics most critical in benchmarking your hospital medicine program. You’ll be able to compare the characteristics and performance of your group with other hospital medicine programs across the country.
- Financial Incentive: There is a financial incentive to participate. Only survey respondents will receive the full survey report and analysis on a CD at no additional charge. Nonrespondents will pay as much as $495 for the results. The results will be available at the SHM Annual Meeting in Washington D.C., May 3-5, 2006.
- Potential Awards: Participants will be eligible to participate in a drawing to receive complimentary registrations to an upcoming Leadership Academy (valued at $1,500) or to the 2006 SHM Annual Meeting (valued at $525). If your group submits its completed questionnaires by Oct. 25 it will have two entries in the drawing. After that date, you’ll receive only one entry.
- Confidentiality: Survey responses will be completely confidential and data will be reported only in the aggregate. International Communications Research, an experienced survey research firm, is conducting the survey. SHM is not involved in collecting or processing the data.
SURVEY CONTENT
This year’s survey builds on the success of the 2003 survey, which is viewed by SHM members as the most accurate and useful source of hospitalist benchmark information. The 2005 survey features the following improvements: better definitions and instructions, and additional questions covering such topics as night coverage, hospitalist services, and the use of nurse practitioners and physician assistants.
The group questionnaire poses questions intended to characterize your hospital medicine program at the group and hospital level. To answer these questions you will need specific information about your hospital (e.g., number of beds, teaching status), the number of fulltime employees (including nonclinical staff), staff turnover, additional revenue received from the hospital or other sources, and the program’s average length-of-stay and case-mix index.
The individual questionnaire poses questions at individual hospitalist level. To answer these you will need information about demographics (age, gender, fulltime employees, specialty, years as a hospitalist, years with group), billing information (encounters, relative value units, charges, collections), hours and shifts worked, and compensation/ benefits for each hospitalist in the group.
CALL TO ACTION
If your hospital medicine group has not received a survey and you would like to participate, e-mail the following information to Marie Francois at mfrancois@hospitalmedicine.org: the name of your group, leader’s name, mailing address, e-mail, and telephone number. If you are completing the survey and you need clarification about any of the questions, contact SHM Customer Service at CustomerService@hospitalmedicine.org or call (800) 843-3360.
As hospital medicine continues to grow and emerge, SHM seeks to provide vital data characterizing the specialty to hospitalists, hospital and healthcare leaders, and policymakers. The 2005 Productivity and Compensation Survey is the key vehicle for providing that data. Help us achieve our goal of 400 hospital medicine group respondents.
Joe Miller is senior vice president for SHM.
NPs and PAs Help Shape SHM Initiatives
By Kevin Whitford, MD
The Nonphysician-Provider Task Force met at SHM’s Annual Meeting in Chicago in April. The meeting marked a significant transition as Mitchell Wilson, MD, concluded his term as chair of the committee. Dr. Wilson’s excellent leadership and organization greatly benefited the task force during its inaugural year. The task force is fortunate to have Dr. Wilson remain as a member.
During the April meeting, the group reviewed the SHM charge to the task force: the responsibility to develop initiatives and programs to promote and define the role of nurse practitioners, physician assistants, and other hospitalist nonphysician providers in hospital medicine. The task force must recommend an SHM nonphysicianprovider agenda to the SHM Board. The task force is looking for opportunities to encourage nonphysician providers to become active SHM members.
The group prepared a document, “Top Five Roles/Functions for Nonphysician Providers” to present to the SHM Board as a framework for the future.
At the annual meeting the task force pursued strategic planning for 2005 and 2006. The Web-based “Resource Center” development was at the top of the list. The task force has collected job descriptions that include acute care nurse practitioner, hospitalist physician assistant, clinical care coordinator, clinical nurse manager, hospitalist case manager, hospitalist program manager, and medical director.
Competency forms are also posted on the SHM Web site; the forms may be used as models to evaluate hospitalist clinical coordinator, hospitalist physician assistant, hospitalist program manager, and advanced nurse practitioner in hospital medicine. The task force plans to expand this resource area to include staffing models, billing and documentation, frequently asked questions, and a document on the value added by nonphysician providers.
The Nonphysician-Provider Task Force also has a “Hub and Spoke” initiative to broaden the input for nonphysician providers by linking members to the task force with hospitalist nonphysician providers across a broad representation of practices.
Other covered areas include plans for publishing articles in The Hospitalist, membership initiatives, and promoting the development of external relationships with national organizations such as the American Academy of Physician Assistants and American Association of Nurse Practitioners.
Task force members helped lead the forum on nonphysician providers at the SHM Annual Meeting. Participants’ questions ranged from specifics regarding the roles of nonphysician providers to filling in documentation issues and included a broad spectrum of practice types from small private to large academic medical centers. The Nonphysician-Provider Task Force is making plans for the program for the 2006 Annual Meeting.
We’ve also sought involvement across the spectrum of task forces and committees in the SHM to increase the representation and raise the awareness of nonphysician providers.
The SHM Board approved the list of top five roles for nonphysician providers in SHM. These include:
- To foster hospital medicine nonphysician-provider educational and professional development;
- To network with other nonphysician providers to share ideas concerning the integration of nonphysician providers in hospital medicine;
- To provide input to SHM and SHM committees/task forces related to the role of the nonphysician provider on the hospital medicine team;
- To serve as “ambassadors” for SHM recruitment of nonphysician-provider members; and
- To share varied expertise in the educational offerings pertinent to nonphysician providers on the hospitalist team.
In the coming year, the task force will further refine this list and present a revised charge to the SHM Board. The original charge specifically mentions only nurse practitioners and physician assistants. We’ve been fortunate to have a clinical care coordinator and a health systems pharmacist join the task force. This broader perspective will benefit the task force and recognizes the broad range of professionals working with the hospitalist team.
If you’re interested in the issues being addressed by the Nonphysician-Provider Task Force, you have several avenues available to pursue those interests. The SHM listserv is an active forum for discussing issues and sharing solutions. If you’re interested in working with the Nonphysician Task Force directly, contact Jeanette Kalupa at kalupa.jeanette@cogenthealthcare.com or Scarlett Blue at sblue@firsthealth.org to be added to the Hub and Spoke initiative. You can also visit the resource center on the SHM Web site to view the nonphysician-provider resources, or you can submit documents for the task force to review for posting to the resource area.
Dr. Whitford is chair of SHM’s Nonphysician-Provider Task Force. Contact him at whitford.kevin@mayo.edu.
SHM’s Advocacy Efforts
Pay-for-performance legislation gains momentum on Capitol Hill
By Eric Siegal, MD
Washington policymakers are embracing a new approach to reforming the Medicare payment system: giving physicians and other providers financial incentives to meet certain quality standards. The so-called “pay-for-performance” or “value-based purchasing” model contained in various bills moving through Congress builds on recommendations made earlier this year by the Medicare Payment Advisory Commission (MedPAC) and mirrors initiatives that have proliferated in the private sector. In its March 2005 report to Congress, MedPAC officially recommended that Congress establish a pay-for-performance system for Medicare providers.
The Center for Medicare and Medicaid Services (CMS) is also developing and implementing a set of pay-for-performance initiatives to support quality improvement in the care of Medicare beneficiaries. CMS Administrator Mark McClellan, MD, an internist, has been a big proponent of this effort.
The basic thrust of pay-for-performance is to use Medicare’s purchasing power to reward and promote quality. This effort is also tied to legislation to accelerate the development of electronic medical records and to expand the use of information technology in the healthcare delivery system. The Public Policy Committee is examining the pay-for-performance bills introduced in Congress and their implications for hospital medicine.
SENATE LEGISLATION
In late June, Senate Finance Committee Chair Charles Grassley (R-IA) and Ranking Member Max Baucus (D-MT) introduced the Medicare Value Purchasing Act of 2005, S. 1356. This legislation would apply to physicians, acute care hospitals, Medicare Advantage plans, end-stage renal disease providers, home health agencies, and (to some extent) skilled nursing facilities.
In the first phase of implementation, Medicare reimbursement rates would be tied directly to reporting data on quality measures, while the second phase ties a portion of payment to provider performance. The Senate bill doesn’t makes changes to the sustainable growth rate formula that determines Medicare payments to physicians. That will likely be handled in separate legislation.
S. 1356 directs the Secretary of Health and Human Services to select quality measures through a multistakeholder, consensus-building process. Those quality measures already developed and accepted by the healthcare community would be taken into account. Under the legislation, the Secretary has the ability to vary measures used within types of providers. For example, the Secretary could differentiate hospital measures by the hospital’s size and scope of services. Or, the Secretary could vary physician measures based on physician specialty, type of practitioner, or the volume of services delivered. The legislation also specifies criteria for the selection of quality measures. For example, the measures should be evidence-based, reliable, and valid; relevant to rural areas; and relevant to the frail elderly and those with chronic conditions. They should include measures of over- and under use and measures of health information technology infrastructure.
HOUSE ACTION
House Ways and Means Health Subcommittee Chair Nancy Johnson (R-CT) was expected to introduce legislation before the August Congressional recess that would add pay-for-performance programs for physicians under Medicare and repeal the sustainable growth rate formula.
On July 12, Ways and Means Committee Chairman William M. Thomas (R-CA) and Johnson asked McClellan to make regulatory changes that could avert a 4.3% cut in the Medicare physician update in 2006. In particular, the lawmakers said that CMS should remove prescription drug expenditures from the sustainable growth rate, which are used to calculate yearly changes in reimbursements. Legislation to permanently fix the sustainable growth rate “would be prohibitively expensive given current interpretations of the formula,” they said.
In testimony before the Ways and Means Committee July 21, McClellan said eliminating the sustainable growth rate system in favor of an update that is similar to the current Medicare Economic Index, which measures the weighted average price change for various inputs involved with producing physicians’ services, would cost $183 billion over 10 years. CMS is currently reviewing the legal arguments regarding whether it can remove prescription drugs from the services included in the sustainable growth rate under existing authorities, he told the subcommittee.
The notion of linking a portion of Medicare payments to valid measures of quality, or paying for performance, is clearly here to stay. The concept has broad support from the Administration, Congress, CMS, and several specialty societies, even though many questions about its implementation must still be answered. The Public Policy Committee will work to position SHM to influence this important debate.
In the first phase of the Medicare Value Purchasing Act of 2005 implementation, Medicare reimbursement rates would be tied directly to reporting data on quality measures, while the second phase ties a portion of payment to provider performance.
SHM Partners with Patient Safety Leadership Fellowship Program
Focus on interdisciplinary leadership and patient safety proves invaluable
By Jeanne M. Huddleston, MD, FACP
SHM is now a partner in the Patient Safety Leadership Fellowship (PSLF) program, an intensive learning experience that develops leadership competencies and advances patient safety in healthcare through a dynamic, highly participatory, structured learning community.
The Health Forum-American Hospital Association and the National Patient Safety Foundation created the fellowship and now has several program partners. SHM has joined the list as a program partner in this PSLF with the Health Research and Education Trust (HRET), the American Organization of Nurse Executives (AONE), and the American Society for Healthcare Risk Management (ASHRM).
The ultimate objective of the PSLF is to provide multidisciplinary teams and individual providers with the opportunity to develop the leadership competencies necessary to make meaningful changes in healthcare safety. Through a combination of expert leadership and patient safety faculty, a specially designed curriculum, and field-based projects, PSLF Health Forum Fellowships offer an intensive educational opportunity.
Each fellowship experience is highly participatory and interdisciplinary. Participants from past fellowship classes include physicians, pharmacists, nurses, lawyers, risk managers, educators, administrators, and patients. This environment encourages the creation of new knowledge to advance the patient safety science and enhances interpersonal and professional effectiveness. Each fellowship is a yearlong journey that blends face-to-face leadership retreats, self-study educational curriculum, online computer conferencing, and site visits.
The heart of the fellowship program is an Action Learning Project (ALP) that fellows design and implement in their own organization/community/region. This allows for direct application of each participant’s knowledge and experience gained through the other curricular venues to be immediately applied with the added benefit of being able to draw on the experience of the fellowship faculty and staff to advance the participant’s progress. Fellows are required to provide a midyear and final report to their respective executives and/or boards, in addition to their learning community of fellows during the face-to-face leadership retreats. Examples of ALPs can be found at www.healthforumfellowships.com/healthforumfellowships/html/project.htm.
Through the course of the one-year learning experience, fellows are exposed to the following curricular components:
- Knowledge of what creates safe healthcare systems;
- Leadership, collaboration, and complexity;
- The path to a culture of safety;
- Lessons from inside and outside healthcare;
- Disclosure, reporting, and transparency; and
- The business case for creating a culture of safety.
Given the alignment of interests in quality, patient safety, and leadership between this fellowship and the developing core curriculum in hospital medicine, SHM became a program partner in mid2004. During 2005, SHM will become more involved by serving on the Fellowship’s Advisory and Curriculum Committees to help with oversight of the program concept and curricular development. In addition, SHM will provide one day of educational content drawing from the vast experience of hospitalists in the fields of leadership and patient safety.
I participated in the 2002-2003 PSLF inaugural class. The interdisciplinary nature of the education experience was rewarding and, I believe, was one of the core reasons the curricula benefited my effectiveness specifically in participating in quality and patient safety initiatives. My fellow alumni continue to serve as a community of quality and patient safety champions and assist each other by being a sounding board and advisory group to ongoing local activities. TH
Dr. Huddleston can be contacted via e-mail at huddleston.jeanne@mayo.edu.
SHM has established an aggressive goal of getting 400 respondents for its biannual Productivity and Compensation Survey. This would mean a 33% increase over the 300 respondents to the 2003 survey. SHM is tracking the number of respondents on its Web site homepage (www.hospitalmedicine.org). All surveys must be completed and returned by Nov. 25.
By now hospital medicine group leaders should have received a copy of the survey with instructions. SHM prefers that you complete the survey online. The response process for the online survey is simplified with built-in edits and a streamlined flow. In addition, you can stop in the middle of the questionnaire and return to complete it later.
WHY SHOULD YOU PARTICIPATE?
- Information: The survey questions represent the metrics most critical in benchmarking your hospital medicine program. You’ll be able to compare the characteristics and performance of your group with other hospital medicine programs across the country.
- Financial Incentive: There is a financial incentive to participate. Only survey respondents will receive the full survey report and analysis on a CD at no additional charge. Nonrespondents will pay as much as $495 for the results. The results will be available at the SHM Annual Meeting in Washington D.C., May 3-5, 2006.
- Potential Awards: Participants will be eligible to participate in a drawing to receive complimentary registrations to an upcoming Leadership Academy (valued at $1,500) or to the 2006 SHM Annual Meeting (valued at $525). If your group submits its completed questionnaires by Oct. 25 it will have two entries in the drawing. After that date, you’ll receive only one entry.
- Confidentiality: Survey responses will be completely confidential and data will be reported only in the aggregate. International Communications Research, an experienced survey research firm, is conducting the survey. SHM is not involved in collecting or processing the data.
SURVEY CONTENT
This year’s survey builds on the success of the 2003 survey, which is viewed by SHM members as the most accurate and useful source of hospitalist benchmark information. The 2005 survey features the following improvements: better definitions and instructions, and additional questions covering such topics as night coverage, hospitalist services, and the use of nurse practitioners and physician assistants.
The group questionnaire poses questions intended to characterize your hospital medicine program at the group and hospital level. To answer these questions you will need specific information about your hospital (e.g., number of beds, teaching status), the number of fulltime employees (including nonclinical staff), staff turnover, additional revenue received from the hospital or other sources, and the program’s average length-of-stay and case-mix index.
The individual questionnaire poses questions at individual hospitalist level. To answer these you will need information about demographics (age, gender, fulltime employees, specialty, years as a hospitalist, years with group), billing information (encounters, relative value units, charges, collections), hours and shifts worked, and compensation/ benefits for each hospitalist in the group.
CALL TO ACTION
If your hospital medicine group has not received a survey and you would like to participate, e-mail the following information to Marie Francois at mfrancois@hospitalmedicine.org: the name of your group, leader’s name, mailing address, e-mail, and telephone number. If you are completing the survey and you need clarification about any of the questions, contact SHM Customer Service at CustomerService@hospitalmedicine.org or call (800) 843-3360.
As hospital medicine continues to grow and emerge, SHM seeks to provide vital data characterizing the specialty to hospitalists, hospital and healthcare leaders, and policymakers. The 2005 Productivity and Compensation Survey is the key vehicle for providing that data. Help us achieve our goal of 400 hospital medicine group respondents.
Joe Miller is senior vice president for SHM.
NPs and PAs Help Shape SHM Initiatives
By Kevin Whitford, MD
The Nonphysician-Provider Task Force met at SHM’s Annual Meeting in Chicago in April. The meeting marked a significant transition as Mitchell Wilson, MD, concluded his term as chair of the committee. Dr. Wilson’s excellent leadership and organization greatly benefited the task force during its inaugural year. The task force is fortunate to have Dr. Wilson remain as a member.
During the April meeting, the group reviewed the SHM charge to the task force: the responsibility to develop initiatives and programs to promote and define the role of nurse practitioners, physician assistants, and other hospitalist nonphysician providers in hospital medicine. The task force must recommend an SHM nonphysicianprovider agenda to the SHM Board. The task force is looking for opportunities to encourage nonphysician providers to become active SHM members.
The group prepared a document, “Top Five Roles/Functions for Nonphysician Providers” to present to the SHM Board as a framework for the future.
At the annual meeting the task force pursued strategic planning for 2005 and 2006. The Web-based “Resource Center” development was at the top of the list. The task force has collected job descriptions that include acute care nurse practitioner, hospitalist physician assistant, clinical care coordinator, clinical nurse manager, hospitalist case manager, hospitalist program manager, and medical director.
Competency forms are also posted on the SHM Web site; the forms may be used as models to evaluate hospitalist clinical coordinator, hospitalist physician assistant, hospitalist program manager, and advanced nurse practitioner in hospital medicine. The task force plans to expand this resource area to include staffing models, billing and documentation, frequently asked questions, and a document on the value added by nonphysician providers.
The Nonphysician-Provider Task Force also has a “Hub and Spoke” initiative to broaden the input for nonphysician providers by linking members to the task force with hospitalist nonphysician providers across a broad representation of practices.
Other covered areas include plans for publishing articles in The Hospitalist, membership initiatives, and promoting the development of external relationships with national organizations such as the American Academy of Physician Assistants and American Association of Nurse Practitioners.
Task force members helped lead the forum on nonphysician providers at the SHM Annual Meeting. Participants’ questions ranged from specifics regarding the roles of nonphysician providers to filling in documentation issues and included a broad spectrum of practice types from small private to large academic medical centers. The Nonphysician-Provider Task Force is making plans for the program for the 2006 Annual Meeting.
We’ve also sought involvement across the spectrum of task forces and committees in the SHM to increase the representation and raise the awareness of nonphysician providers.
The SHM Board approved the list of top five roles for nonphysician providers in SHM. These include:
- To foster hospital medicine nonphysician-provider educational and professional development;
- To network with other nonphysician providers to share ideas concerning the integration of nonphysician providers in hospital medicine;
- To provide input to SHM and SHM committees/task forces related to the role of the nonphysician provider on the hospital medicine team;
- To serve as “ambassadors” for SHM recruitment of nonphysician-provider members; and
- To share varied expertise in the educational offerings pertinent to nonphysician providers on the hospitalist team.
In the coming year, the task force will further refine this list and present a revised charge to the SHM Board. The original charge specifically mentions only nurse practitioners and physician assistants. We’ve been fortunate to have a clinical care coordinator and a health systems pharmacist join the task force. This broader perspective will benefit the task force and recognizes the broad range of professionals working with the hospitalist team.
If you’re interested in the issues being addressed by the Nonphysician-Provider Task Force, you have several avenues available to pursue those interests. The SHM listserv is an active forum for discussing issues and sharing solutions. If you’re interested in working with the Nonphysician Task Force directly, contact Jeanette Kalupa at kalupa.jeanette@cogenthealthcare.com or Scarlett Blue at sblue@firsthealth.org to be added to the Hub and Spoke initiative. You can also visit the resource center on the SHM Web site to view the nonphysician-provider resources, or you can submit documents for the task force to review for posting to the resource area.
Dr. Whitford is chair of SHM’s Nonphysician-Provider Task Force. Contact him at whitford.kevin@mayo.edu.
SHM’s Advocacy Efforts
Pay-for-performance legislation gains momentum on Capitol Hill
By Eric Siegal, MD
Washington policymakers are embracing a new approach to reforming the Medicare payment system: giving physicians and other providers financial incentives to meet certain quality standards. The so-called “pay-for-performance” or “value-based purchasing” model contained in various bills moving through Congress builds on recommendations made earlier this year by the Medicare Payment Advisory Commission (MedPAC) and mirrors initiatives that have proliferated in the private sector. In its March 2005 report to Congress, MedPAC officially recommended that Congress establish a pay-for-performance system for Medicare providers.
The Center for Medicare and Medicaid Services (CMS) is also developing and implementing a set of pay-for-performance initiatives to support quality improvement in the care of Medicare beneficiaries. CMS Administrator Mark McClellan, MD, an internist, has been a big proponent of this effort.
The basic thrust of pay-for-performance is to use Medicare’s purchasing power to reward and promote quality. This effort is also tied to legislation to accelerate the development of electronic medical records and to expand the use of information technology in the healthcare delivery system. The Public Policy Committee is examining the pay-for-performance bills introduced in Congress and their implications for hospital medicine.
SENATE LEGISLATION
In late June, Senate Finance Committee Chair Charles Grassley (R-IA) and Ranking Member Max Baucus (D-MT) introduced the Medicare Value Purchasing Act of 2005, S. 1356. This legislation would apply to physicians, acute care hospitals, Medicare Advantage plans, end-stage renal disease providers, home health agencies, and (to some extent) skilled nursing facilities.
In the first phase of implementation, Medicare reimbursement rates would be tied directly to reporting data on quality measures, while the second phase ties a portion of payment to provider performance. The Senate bill doesn’t makes changes to the sustainable growth rate formula that determines Medicare payments to physicians. That will likely be handled in separate legislation.
S. 1356 directs the Secretary of Health and Human Services to select quality measures through a multistakeholder, consensus-building process. Those quality measures already developed and accepted by the healthcare community would be taken into account. Under the legislation, the Secretary has the ability to vary measures used within types of providers. For example, the Secretary could differentiate hospital measures by the hospital’s size and scope of services. Or, the Secretary could vary physician measures based on physician specialty, type of practitioner, or the volume of services delivered. The legislation also specifies criteria for the selection of quality measures. For example, the measures should be evidence-based, reliable, and valid; relevant to rural areas; and relevant to the frail elderly and those with chronic conditions. They should include measures of over- and under use and measures of health information technology infrastructure.
HOUSE ACTION
House Ways and Means Health Subcommittee Chair Nancy Johnson (R-CT) was expected to introduce legislation before the August Congressional recess that would add pay-for-performance programs for physicians under Medicare and repeal the sustainable growth rate formula.
On July 12, Ways and Means Committee Chairman William M. Thomas (R-CA) and Johnson asked McClellan to make regulatory changes that could avert a 4.3% cut in the Medicare physician update in 2006. In particular, the lawmakers said that CMS should remove prescription drug expenditures from the sustainable growth rate, which are used to calculate yearly changes in reimbursements. Legislation to permanently fix the sustainable growth rate “would be prohibitively expensive given current interpretations of the formula,” they said.
In testimony before the Ways and Means Committee July 21, McClellan said eliminating the sustainable growth rate system in favor of an update that is similar to the current Medicare Economic Index, which measures the weighted average price change for various inputs involved with producing physicians’ services, would cost $183 billion over 10 years. CMS is currently reviewing the legal arguments regarding whether it can remove prescription drugs from the services included in the sustainable growth rate under existing authorities, he told the subcommittee.
The notion of linking a portion of Medicare payments to valid measures of quality, or paying for performance, is clearly here to stay. The concept has broad support from the Administration, Congress, CMS, and several specialty societies, even though many questions about its implementation must still be answered. The Public Policy Committee will work to position SHM to influence this important debate.
In the first phase of the Medicare Value Purchasing Act of 2005 implementation, Medicare reimbursement rates would be tied directly to reporting data on quality measures, while the second phase ties a portion of payment to provider performance.
SHM Partners with Patient Safety Leadership Fellowship Program
Focus on interdisciplinary leadership and patient safety proves invaluable
By Jeanne M. Huddleston, MD, FACP
SHM is now a partner in the Patient Safety Leadership Fellowship (PSLF) program, an intensive learning experience that develops leadership competencies and advances patient safety in healthcare through a dynamic, highly participatory, structured learning community.
The Health Forum-American Hospital Association and the National Patient Safety Foundation created the fellowship and now has several program partners. SHM has joined the list as a program partner in this PSLF with the Health Research and Education Trust (HRET), the American Organization of Nurse Executives (AONE), and the American Society for Healthcare Risk Management (ASHRM).
The ultimate objective of the PSLF is to provide multidisciplinary teams and individual providers with the opportunity to develop the leadership competencies necessary to make meaningful changes in healthcare safety. Through a combination of expert leadership and patient safety faculty, a specially designed curriculum, and field-based projects, PSLF Health Forum Fellowships offer an intensive educational opportunity.
Each fellowship experience is highly participatory and interdisciplinary. Participants from past fellowship classes include physicians, pharmacists, nurses, lawyers, risk managers, educators, administrators, and patients. This environment encourages the creation of new knowledge to advance the patient safety science and enhances interpersonal and professional effectiveness. Each fellowship is a yearlong journey that blends face-to-face leadership retreats, self-study educational curriculum, online computer conferencing, and site visits.
The heart of the fellowship program is an Action Learning Project (ALP) that fellows design and implement in their own organization/community/region. This allows for direct application of each participant’s knowledge and experience gained through the other curricular venues to be immediately applied with the added benefit of being able to draw on the experience of the fellowship faculty and staff to advance the participant’s progress. Fellows are required to provide a midyear and final report to their respective executives and/or boards, in addition to their learning community of fellows during the face-to-face leadership retreats. Examples of ALPs can be found at www.healthforumfellowships.com/healthforumfellowships/html/project.htm.
Through the course of the one-year learning experience, fellows are exposed to the following curricular components:
- Knowledge of what creates safe healthcare systems;
- Leadership, collaboration, and complexity;
- The path to a culture of safety;
- Lessons from inside and outside healthcare;
- Disclosure, reporting, and transparency; and
- The business case for creating a culture of safety.
Given the alignment of interests in quality, patient safety, and leadership between this fellowship and the developing core curriculum in hospital medicine, SHM became a program partner in mid2004. During 2005, SHM will become more involved by serving on the Fellowship’s Advisory and Curriculum Committees to help with oversight of the program concept and curricular development. In addition, SHM will provide one day of educational content drawing from the vast experience of hospitalists in the fields of leadership and patient safety.
I participated in the 2002-2003 PSLF inaugural class. The interdisciplinary nature of the education experience was rewarding and, I believe, was one of the core reasons the curricula benefited my effectiveness specifically in participating in quality and patient safety initiatives. My fellow alumni continue to serve as a community of quality and patient safety champions and assist each other by being a sounding board and advisory group to ongoing local activities. TH
Dr. Huddleston can be contacted via e-mail at huddleston.jeanne@mayo.edu.
SHM has established an aggressive goal of getting 400 respondents for its biannual Productivity and Compensation Survey. This would mean a 33% increase over the 300 respondents to the 2003 survey. SHM is tracking the number of respondents on its Web site homepage (www.hospitalmedicine.org). All surveys must be completed and returned by Nov. 25.
By now hospital medicine group leaders should have received a copy of the survey with instructions. SHM prefers that you complete the survey online. The response process for the online survey is simplified with built-in edits and a streamlined flow. In addition, you can stop in the middle of the questionnaire and return to complete it later.
WHY SHOULD YOU PARTICIPATE?
- Information: The survey questions represent the metrics most critical in benchmarking your hospital medicine program. You’ll be able to compare the characteristics and performance of your group with other hospital medicine programs across the country.
- Financial Incentive: There is a financial incentive to participate. Only survey respondents will receive the full survey report and analysis on a CD at no additional charge. Nonrespondents will pay as much as $495 for the results. The results will be available at the SHM Annual Meeting in Washington D.C., May 3-5, 2006.
- Potential Awards: Participants will be eligible to participate in a drawing to receive complimentary registrations to an upcoming Leadership Academy (valued at $1,500) or to the 2006 SHM Annual Meeting (valued at $525). If your group submits its completed questionnaires by Oct. 25 it will have two entries in the drawing. After that date, you’ll receive only one entry.
- Confidentiality: Survey responses will be completely confidential and data will be reported only in the aggregate. International Communications Research, an experienced survey research firm, is conducting the survey. SHM is not involved in collecting or processing the data.
SURVEY CONTENT
This year’s survey builds on the success of the 2003 survey, which is viewed by SHM members as the most accurate and useful source of hospitalist benchmark information. The 2005 survey features the following improvements: better definitions and instructions, and additional questions covering such topics as night coverage, hospitalist services, and the use of nurse practitioners and physician assistants.
The group questionnaire poses questions intended to characterize your hospital medicine program at the group and hospital level. To answer these questions you will need specific information about your hospital (e.g., number of beds, teaching status), the number of fulltime employees (including nonclinical staff), staff turnover, additional revenue received from the hospital or other sources, and the program’s average length-of-stay and case-mix index.
The individual questionnaire poses questions at individual hospitalist level. To answer these you will need information about demographics (age, gender, fulltime employees, specialty, years as a hospitalist, years with group), billing information (encounters, relative value units, charges, collections), hours and shifts worked, and compensation/ benefits for each hospitalist in the group.
CALL TO ACTION
If your hospital medicine group has not received a survey and you would like to participate, e-mail the following information to Marie Francois at mfrancois@hospitalmedicine.org: the name of your group, leader’s name, mailing address, e-mail, and telephone number. If you are completing the survey and you need clarification about any of the questions, contact SHM Customer Service at CustomerService@hospitalmedicine.org or call (800) 843-3360.
As hospital medicine continues to grow and emerge, SHM seeks to provide vital data characterizing the specialty to hospitalists, hospital and healthcare leaders, and policymakers. The 2005 Productivity and Compensation Survey is the key vehicle for providing that data. Help us achieve our goal of 400 hospital medicine group respondents.
Joe Miller is senior vice president for SHM.
NPs and PAs Help Shape SHM Initiatives
By Kevin Whitford, MD
The Nonphysician-Provider Task Force met at SHM’s Annual Meeting in Chicago in April. The meeting marked a significant transition as Mitchell Wilson, MD, concluded his term as chair of the committee. Dr. Wilson’s excellent leadership and organization greatly benefited the task force during its inaugural year. The task force is fortunate to have Dr. Wilson remain as a member.
During the April meeting, the group reviewed the SHM charge to the task force: the responsibility to develop initiatives and programs to promote and define the role of nurse practitioners, physician assistants, and other hospitalist nonphysician providers in hospital medicine. The task force must recommend an SHM nonphysicianprovider agenda to the SHM Board. The task force is looking for opportunities to encourage nonphysician providers to become active SHM members.
The group prepared a document, “Top Five Roles/Functions for Nonphysician Providers” to present to the SHM Board as a framework for the future.
At the annual meeting the task force pursued strategic planning for 2005 and 2006. The Web-based “Resource Center” development was at the top of the list. The task force has collected job descriptions that include acute care nurse practitioner, hospitalist physician assistant, clinical care coordinator, clinical nurse manager, hospitalist case manager, hospitalist program manager, and medical director.
Competency forms are also posted on the SHM Web site; the forms may be used as models to evaluate hospitalist clinical coordinator, hospitalist physician assistant, hospitalist program manager, and advanced nurse practitioner in hospital medicine. The task force plans to expand this resource area to include staffing models, billing and documentation, frequently asked questions, and a document on the value added by nonphysician providers.
The Nonphysician-Provider Task Force also has a “Hub and Spoke” initiative to broaden the input for nonphysician providers by linking members to the task force with hospitalist nonphysician providers across a broad representation of practices.
Other covered areas include plans for publishing articles in The Hospitalist, membership initiatives, and promoting the development of external relationships with national organizations such as the American Academy of Physician Assistants and American Association of Nurse Practitioners.
Task force members helped lead the forum on nonphysician providers at the SHM Annual Meeting. Participants’ questions ranged from specifics regarding the roles of nonphysician providers to filling in documentation issues and included a broad spectrum of practice types from small private to large academic medical centers. The Nonphysician-Provider Task Force is making plans for the program for the 2006 Annual Meeting.
We’ve also sought involvement across the spectrum of task forces and committees in the SHM to increase the representation and raise the awareness of nonphysician providers.
The SHM Board approved the list of top five roles for nonphysician providers in SHM. These include:
- To foster hospital medicine nonphysician-provider educational and professional development;
- To network with other nonphysician providers to share ideas concerning the integration of nonphysician providers in hospital medicine;
- To provide input to SHM and SHM committees/task forces related to the role of the nonphysician provider on the hospital medicine team;
- To serve as “ambassadors” for SHM recruitment of nonphysician-provider members; and
- To share varied expertise in the educational offerings pertinent to nonphysician providers on the hospitalist team.
In the coming year, the task force will further refine this list and present a revised charge to the SHM Board. The original charge specifically mentions only nurse practitioners and physician assistants. We’ve been fortunate to have a clinical care coordinator and a health systems pharmacist join the task force. This broader perspective will benefit the task force and recognizes the broad range of professionals working with the hospitalist team.
If you’re interested in the issues being addressed by the Nonphysician-Provider Task Force, you have several avenues available to pursue those interests. The SHM listserv is an active forum for discussing issues and sharing solutions. If you’re interested in working with the Nonphysician Task Force directly, contact Jeanette Kalupa at kalupa.jeanette@cogenthealthcare.com or Scarlett Blue at sblue@firsthealth.org to be added to the Hub and Spoke initiative. You can also visit the resource center on the SHM Web site to view the nonphysician-provider resources, or you can submit documents for the task force to review for posting to the resource area.
Dr. Whitford is chair of SHM’s Nonphysician-Provider Task Force. Contact him at whitford.kevin@mayo.edu.
SHM’s Advocacy Efforts
Pay-for-performance legislation gains momentum on Capitol Hill
By Eric Siegal, MD
Washington policymakers are embracing a new approach to reforming the Medicare payment system: giving physicians and other providers financial incentives to meet certain quality standards. The so-called “pay-for-performance” or “value-based purchasing” model contained in various bills moving through Congress builds on recommendations made earlier this year by the Medicare Payment Advisory Commission (MedPAC) and mirrors initiatives that have proliferated in the private sector. In its March 2005 report to Congress, MedPAC officially recommended that Congress establish a pay-for-performance system for Medicare providers.
The Center for Medicare and Medicaid Services (CMS) is also developing and implementing a set of pay-for-performance initiatives to support quality improvement in the care of Medicare beneficiaries. CMS Administrator Mark McClellan, MD, an internist, has been a big proponent of this effort.
The basic thrust of pay-for-performance is to use Medicare’s purchasing power to reward and promote quality. This effort is also tied to legislation to accelerate the development of electronic medical records and to expand the use of information technology in the healthcare delivery system. The Public Policy Committee is examining the pay-for-performance bills introduced in Congress and their implications for hospital medicine.
SENATE LEGISLATION
In late June, Senate Finance Committee Chair Charles Grassley (R-IA) and Ranking Member Max Baucus (D-MT) introduced the Medicare Value Purchasing Act of 2005, S. 1356. This legislation would apply to physicians, acute care hospitals, Medicare Advantage plans, end-stage renal disease providers, home health agencies, and (to some extent) skilled nursing facilities.
In the first phase of implementation, Medicare reimbursement rates would be tied directly to reporting data on quality measures, while the second phase ties a portion of payment to provider performance. The Senate bill doesn’t makes changes to the sustainable growth rate formula that determines Medicare payments to physicians. That will likely be handled in separate legislation.
S. 1356 directs the Secretary of Health and Human Services to select quality measures through a multistakeholder, consensus-building process. Those quality measures already developed and accepted by the healthcare community would be taken into account. Under the legislation, the Secretary has the ability to vary measures used within types of providers. For example, the Secretary could differentiate hospital measures by the hospital’s size and scope of services. Or, the Secretary could vary physician measures based on physician specialty, type of practitioner, or the volume of services delivered. The legislation also specifies criteria for the selection of quality measures. For example, the measures should be evidence-based, reliable, and valid; relevant to rural areas; and relevant to the frail elderly and those with chronic conditions. They should include measures of over- and under use and measures of health information technology infrastructure.
HOUSE ACTION
House Ways and Means Health Subcommittee Chair Nancy Johnson (R-CT) was expected to introduce legislation before the August Congressional recess that would add pay-for-performance programs for physicians under Medicare and repeal the sustainable growth rate formula.
On July 12, Ways and Means Committee Chairman William M. Thomas (R-CA) and Johnson asked McClellan to make regulatory changes that could avert a 4.3% cut in the Medicare physician update in 2006. In particular, the lawmakers said that CMS should remove prescription drug expenditures from the sustainable growth rate, which are used to calculate yearly changes in reimbursements. Legislation to permanently fix the sustainable growth rate “would be prohibitively expensive given current interpretations of the formula,” they said.
In testimony before the Ways and Means Committee July 21, McClellan said eliminating the sustainable growth rate system in favor of an update that is similar to the current Medicare Economic Index, which measures the weighted average price change for various inputs involved with producing physicians’ services, would cost $183 billion over 10 years. CMS is currently reviewing the legal arguments regarding whether it can remove prescription drugs from the services included in the sustainable growth rate under existing authorities, he told the subcommittee.
The notion of linking a portion of Medicare payments to valid measures of quality, or paying for performance, is clearly here to stay. The concept has broad support from the Administration, Congress, CMS, and several specialty societies, even though many questions about its implementation must still be answered. The Public Policy Committee will work to position SHM to influence this important debate.
In the first phase of the Medicare Value Purchasing Act of 2005 implementation, Medicare reimbursement rates would be tied directly to reporting data on quality measures, while the second phase ties a portion of payment to provider performance.
SHM Partners with Patient Safety Leadership Fellowship Program
Focus on interdisciplinary leadership and patient safety proves invaluable
By Jeanne M. Huddleston, MD, FACP
SHM is now a partner in the Patient Safety Leadership Fellowship (PSLF) program, an intensive learning experience that develops leadership competencies and advances patient safety in healthcare through a dynamic, highly participatory, structured learning community.
The Health Forum-American Hospital Association and the National Patient Safety Foundation created the fellowship and now has several program partners. SHM has joined the list as a program partner in this PSLF with the Health Research and Education Trust (HRET), the American Organization of Nurse Executives (AONE), and the American Society for Healthcare Risk Management (ASHRM).
The ultimate objective of the PSLF is to provide multidisciplinary teams and individual providers with the opportunity to develop the leadership competencies necessary to make meaningful changes in healthcare safety. Through a combination of expert leadership and patient safety faculty, a specially designed curriculum, and field-based projects, PSLF Health Forum Fellowships offer an intensive educational opportunity.
Each fellowship experience is highly participatory and interdisciplinary. Participants from past fellowship classes include physicians, pharmacists, nurses, lawyers, risk managers, educators, administrators, and patients. This environment encourages the creation of new knowledge to advance the patient safety science and enhances interpersonal and professional effectiveness. Each fellowship is a yearlong journey that blends face-to-face leadership retreats, self-study educational curriculum, online computer conferencing, and site visits.
The heart of the fellowship program is an Action Learning Project (ALP) that fellows design and implement in their own organization/community/region. This allows for direct application of each participant’s knowledge and experience gained through the other curricular venues to be immediately applied with the added benefit of being able to draw on the experience of the fellowship faculty and staff to advance the participant’s progress. Fellows are required to provide a midyear and final report to their respective executives and/or boards, in addition to their learning community of fellows during the face-to-face leadership retreats. Examples of ALPs can be found at www.healthforumfellowships.com/healthforumfellowships/html/project.htm.
Through the course of the one-year learning experience, fellows are exposed to the following curricular components:
- Knowledge of what creates safe healthcare systems;
- Leadership, collaboration, and complexity;
- The path to a culture of safety;
- Lessons from inside and outside healthcare;
- Disclosure, reporting, and transparency; and
- The business case for creating a culture of safety.
Given the alignment of interests in quality, patient safety, and leadership between this fellowship and the developing core curriculum in hospital medicine, SHM became a program partner in mid2004. During 2005, SHM will become more involved by serving on the Fellowship’s Advisory and Curriculum Committees to help with oversight of the program concept and curricular development. In addition, SHM will provide one day of educational content drawing from the vast experience of hospitalists in the fields of leadership and patient safety.
I participated in the 2002-2003 PSLF inaugural class. The interdisciplinary nature of the education experience was rewarding and, I believe, was one of the core reasons the curricula benefited my effectiveness specifically in participating in quality and patient safety initiatives. My fellow alumni continue to serve as a community of quality and patient safety champions and assist each other by being a sounding board and advisory group to ongoing local activities. TH
Dr. Huddleston can be contacted via e-mail at huddleston.jeanne@mayo.edu.
A View of the SHM Annual Meeting in Chicago
Editor’s Note:
Having returned from the 8th SHM Annual Meeting at the time of this writing, it is clear that this was not only the biggest but also the best Annual Meeting to date. As Larry Wellikson and Joe Miller describe more fully in this issue, the lectures, workshops and networking activities available far outstripped the ability of attendees to take part in all of them. In fact, it was common to feel that there were 2, 3, or even more “must attend” sessions taking place simultaneously and if this was sometimes frustrating, it also spoke to the fact that the meeting’s quality was strikingly high. With the realization that a collection of articles is unable to fully convey the vibrancy of the meeting, we have assembled in the following section a “Big Picture” from imbedded reporter Joe Miller, overviews of 2 of the plenary lectures, and recaps of several outstanding breakout sessions. A separate monograph that will include other highlights of the Annual Meeting is under development and will be mailed in August.―JP
I was invited to write a short piece for The Hospitalist summarizing SHM’s 8th Annual Meeting on Thursday, April 28 through Saturday, April 30 in Chicago. As I sat on the airplane on my return flight to Boston, I reflected on what would define a “successful” annual meeting for the professional society representing hospitalists. I concluded that three criteria would define success. Specifically that the conference would:
- Demonstrate the strength and resiliency of the hospital medicine movement
- Provide quality content and learning opportunities to a diverse group of attendees
- Demonstrate that SHM is a competent and effective organization meeting the needs of its members.
I believe the meeting measured up extremely well on all three criteria.
With regard to demonstrating the vibrancy of the hospital medicine movement:
- At the conference, there was recognition by three significant stakeholders in the healthcare industry (hospitals, employers, and regulators) of the critical role of hospitalists. In the opening keynote address, Rick Wade, Senior Vice President of the American Hospital Association, described the growing pressure on hospitals to be “transparent,” sharing information with patients and the public on their performance. Mr. Wade’s address was followed by a presentation by Arnold Milstein, MD, Medical Director of the Pacific Business Group on Health and cofounder of the Leapfrog Group. Dr. Milstein used the metaphor of a shark’s jaws to describe the threat of the continued escalation of healthcare costs, and he indicated that the key to addressing this crisis is to “re-engineer” clinical processes to make them more efficient. On Saturday, Dennis O’Leary, CEO of JCAHO, described the challenge of evaluating the performance of hospitals in the era of patient safety. All three speakers indicated that hospitalists will be critical resources to healthcare leaders faced with these challenges. Another measure of the recognition of hospitalists as a force in the healthcare industry was the fact that over 90 exhibitors wanted the opportunity to get the ear of the conference attendees. The exhibit floor was teeming with hospitalists interested in learning about programs, products, and services.
- The growth of the hospital medicine movement was clearly evident to attendees of the conference. This year’s conference had over 1000 attendees,a growth of 15% over the 2004 annual meeting. When Alpesh Amin, MD, co-director of the course, opened the meeting, the attendees responded to a series of questions through the audience response system. For over 50% of the attendees, this was their first SHM Annual Meeting, indicating that the specialty of hospital medicine has a constant influx of “new blood.” And at the President’s Luncheon, the presentation by Larry Wellikson, MD, CEO of SHM, conveyed a broad array of statistics on the status of the hospital medicine movement, including the fact that the 12,000+ hospitalists in the U.S. makes the specialty bigger than gastroenterology and neurology. Approximately 30% of all U.S. Hospitals have hospital medicine programs; for hospitals with over 200 beds, 55% have hospitalists.
- The excellence of the hospital medicine movement was evident through the quality of the 120+ research, innovation, and clinical vignette posters presented on Friday. Furthermore, the accomplishments of the SHM award winners announced at the President’s Luncheon were quite impressive. Joseph Li, MD, won the award for Outstanding Service in Hospital Medicine, Sunil Kripalani, MD, was named the Outstanding Young Investigator, Shaun Frost, MD, won the Clinical Excellence award, and Jeff Wiese, MD, won the award for Excellence in Teaching. Hospitalists are demonstrating their ability to be innovative, high impact physicians.
With regard to providing learning opportunities for a diverse audience:
- The pre-courses on Thursday allowed attendees to gain in-depth knowledge on practice management, perioperative medicine, and critical care medicine.
- There were 35 separate presentations in 7 tracks over the 2 days of the main meeting. The clinical, adult clinical, and pediatric clinical tracks covered a wide array of topics, from maternal fetal medicine to acquired pediatric heart disease to addiction medicine. Tracks on quality and patient safety were very well attended, and the academic track included an important update on the hospitalist core curriculum being developed by SHM.
- There were 10 special interest forums allowing attendees interested in the following subjects to exchange ideas: community based hospitalists, research, education, medical directors, women hospitalists, pediatric hospitalists, family practice hospitalists, geriatric hospitalists, early career hospitalists, and nurse practitioners and physician assistants.
- The plenary sessions on updates in hospital medicine and pediatric hospital medicine provided excellent reviews of recent research relevant to hospitalists. Bob Wachter’s annual presentation, this year entitled “Hospital Medicine: Still Crazy After All These Years” laid out some important challenges for the hospital medicine movement as it moves into adolescence.
Finally, with regard to demonstrating SHM’s competence and its ability to meet the needs of its members:
- At the President’s Luncheon, the depth of SHM leadership was evident. Jeanne Huddleston, MD, reported on the significant accomplishments of the past year and handed the torch to SHM’s new President, Steve Pantilat, MD. Steve described his two goals for the upcoming year, the development ofan SHM Research Foundation and an emphasis on the role of hospitalists in palliative care. And Larry Wellikson, MD, SHM’s CEO, displayed energy and charisma throughout the meeting.
- The power of SHM volunteerism was unmistakable throughout the meeting. Preetha Basaviah, MD, the overall course director, harnessed group of SHM members participating in a planning committee to decide on the topics and choose the speakers for the meeting. A broad cross-section of SHM members participated in over 15 committee meetings in Chicago, as they donated their time to improving the field of hospital medicine.
- The conference was a vehicle to display the public relations capabilities of SHM. Melanie Bloom, wife of NBC newscaster David Bloom who died in Iraq of DVT complications, described the awareness campaign that SHM led. The attendees then viewed a short video of the television appearances by hospitalists in the last year, as hospital medicine has received increasing attention in the media. Larry Wellikson announced that every SHM member will receive a DVD with these video news segments.
- The strength of SHM staff and organization was on display in Chicago. Larry Wellikson reported that the staff has more than doubled and he cited a litany of accomplishments, including a new improved website, electronic registration for meetings, a broad range of educational offerings, and a healthy financial outlook. Furthermore, SHM has continued to experience significant membership growth, as the number of members now exceeds 4700, an increase of more than 40% in the past 12 months.
- Finally, and perhaps most importantly, Wellikson described a wide variety of initiatives that are being pursued to meet the needs of SHM members. These initiatives include a long range plan for the formal certification of hospitalists, strategic partnerships with key organizations, public policy initiatives, and the continued strengthening of historical efforts regarding education, leadership, and surveys.
In summary, the SHM conference was greater than the sum of the parts. It was successfully executed on multiple fronts. However I have not yet discussed perhaps the most important achievement of this meeting. It served as an opportunity for hospitalists to meet new friends and to reconnect with old colleagues. The Annual Meeting in Chicago created a positive energy that will carry SHM members until we have the opportunity to meet again next year in Washington, DC.
Editor’s Note:
Having returned from the 8th SHM Annual Meeting at the time of this writing, it is clear that this was not only the biggest but also the best Annual Meeting to date. As Larry Wellikson and Joe Miller describe more fully in this issue, the lectures, workshops and networking activities available far outstripped the ability of attendees to take part in all of them. In fact, it was common to feel that there were 2, 3, or even more “must attend” sessions taking place simultaneously and if this was sometimes frustrating, it also spoke to the fact that the meeting’s quality was strikingly high. With the realization that a collection of articles is unable to fully convey the vibrancy of the meeting, we have assembled in the following section a “Big Picture” from imbedded reporter Joe Miller, overviews of 2 of the plenary lectures, and recaps of several outstanding breakout sessions. A separate monograph that will include other highlights of the Annual Meeting is under development and will be mailed in August.―JP
I was invited to write a short piece for The Hospitalist summarizing SHM’s 8th Annual Meeting on Thursday, April 28 through Saturday, April 30 in Chicago. As I sat on the airplane on my return flight to Boston, I reflected on what would define a “successful” annual meeting for the professional society representing hospitalists. I concluded that three criteria would define success. Specifically that the conference would:
- Demonstrate the strength and resiliency of the hospital medicine movement
- Provide quality content and learning opportunities to a diverse group of attendees
- Demonstrate that SHM is a competent and effective organization meeting the needs of its members.
I believe the meeting measured up extremely well on all three criteria.
With regard to demonstrating the vibrancy of the hospital medicine movement:
- At the conference, there was recognition by three significant stakeholders in the healthcare industry (hospitals, employers, and regulators) of the critical role of hospitalists. In the opening keynote address, Rick Wade, Senior Vice President of the American Hospital Association, described the growing pressure on hospitals to be “transparent,” sharing information with patients and the public on their performance. Mr. Wade’s address was followed by a presentation by Arnold Milstein, MD, Medical Director of the Pacific Business Group on Health and cofounder of the Leapfrog Group. Dr. Milstein used the metaphor of a shark’s jaws to describe the threat of the continued escalation of healthcare costs, and he indicated that the key to addressing this crisis is to “re-engineer” clinical processes to make them more efficient. On Saturday, Dennis O’Leary, CEO of JCAHO, described the challenge of evaluating the performance of hospitals in the era of patient safety. All three speakers indicated that hospitalists will be critical resources to healthcare leaders faced with these challenges. Another measure of the recognition of hospitalists as a force in the healthcare industry was the fact that over 90 exhibitors wanted the opportunity to get the ear of the conference attendees. The exhibit floor was teeming with hospitalists interested in learning about programs, products, and services.
- The growth of the hospital medicine movement was clearly evident to attendees of the conference. This year’s conference had over 1000 attendees,a growth of 15% over the 2004 annual meeting. When Alpesh Amin, MD, co-director of the course, opened the meeting, the attendees responded to a series of questions through the audience response system. For over 50% of the attendees, this was their first SHM Annual Meeting, indicating that the specialty of hospital medicine has a constant influx of “new blood.” And at the President’s Luncheon, the presentation by Larry Wellikson, MD, CEO of SHM, conveyed a broad array of statistics on the status of the hospital medicine movement, including the fact that the 12,000+ hospitalists in the U.S. makes the specialty bigger than gastroenterology and neurology. Approximately 30% of all U.S. Hospitals have hospital medicine programs; for hospitals with over 200 beds, 55% have hospitalists.
- The excellence of the hospital medicine movement was evident through the quality of the 120+ research, innovation, and clinical vignette posters presented on Friday. Furthermore, the accomplishments of the SHM award winners announced at the President’s Luncheon were quite impressive. Joseph Li, MD, won the award for Outstanding Service in Hospital Medicine, Sunil Kripalani, MD, was named the Outstanding Young Investigator, Shaun Frost, MD, won the Clinical Excellence award, and Jeff Wiese, MD, won the award for Excellence in Teaching. Hospitalists are demonstrating their ability to be innovative, high impact physicians.
With regard to providing learning opportunities for a diverse audience:
- The pre-courses on Thursday allowed attendees to gain in-depth knowledge on practice management, perioperative medicine, and critical care medicine.
- There were 35 separate presentations in 7 tracks over the 2 days of the main meeting. The clinical, adult clinical, and pediatric clinical tracks covered a wide array of topics, from maternal fetal medicine to acquired pediatric heart disease to addiction medicine. Tracks on quality and patient safety were very well attended, and the academic track included an important update on the hospitalist core curriculum being developed by SHM.
- There were 10 special interest forums allowing attendees interested in the following subjects to exchange ideas: community based hospitalists, research, education, medical directors, women hospitalists, pediatric hospitalists, family practice hospitalists, geriatric hospitalists, early career hospitalists, and nurse practitioners and physician assistants.
- The plenary sessions on updates in hospital medicine and pediatric hospital medicine provided excellent reviews of recent research relevant to hospitalists. Bob Wachter’s annual presentation, this year entitled “Hospital Medicine: Still Crazy After All These Years” laid out some important challenges for the hospital medicine movement as it moves into adolescence.
Finally, with regard to demonstrating SHM’s competence and its ability to meet the needs of its members:
- At the President’s Luncheon, the depth of SHM leadership was evident. Jeanne Huddleston, MD, reported on the significant accomplishments of the past year and handed the torch to SHM’s new President, Steve Pantilat, MD. Steve described his two goals for the upcoming year, the development ofan SHM Research Foundation and an emphasis on the role of hospitalists in palliative care. And Larry Wellikson, MD, SHM’s CEO, displayed energy and charisma throughout the meeting.
- The power of SHM volunteerism was unmistakable throughout the meeting. Preetha Basaviah, MD, the overall course director, harnessed group of SHM members participating in a planning committee to decide on the topics and choose the speakers for the meeting. A broad cross-section of SHM members participated in over 15 committee meetings in Chicago, as they donated their time to improving the field of hospital medicine.
- The conference was a vehicle to display the public relations capabilities of SHM. Melanie Bloom, wife of NBC newscaster David Bloom who died in Iraq of DVT complications, described the awareness campaign that SHM led. The attendees then viewed a short video of the television appearances by hospitalists in the last year, as hospital medicine has received increasing attention in the media. Larry Wellikson announced that every SHM member will receive a DVD with these video news segments.
- The strength of SHM staff and organization was on display in Chicago. Larry Wellikson reported that the staff has more than doubled and he cited a litany of accomplishments, including a new improved website, electronic registration for meetings, a broad range of educational offerings, and a healthy financial outlook. Furthermore, SHM has continued to experience significant membership growth, as the number of members now exceeds 4700, an increase of more than 40% in the past 12 months.
- Finally, and perhaps most importantly, Wellikson described a wide variety of initiatives that are being pursued to meet the needs of SHM members. These initiatives include a long range plan for the formal certification of hospitalists, strategic partnerships with key organizations, public policy initiatives, and the continued strengthening of historical efforts regarding education, leadership, and surveys.
In summary, the SHM conference was greater than the sum of the parts. It was successfully executed on multiple fronts. However I have not yet discussed perhaps the most important achievement of this meeting. It served as an opportunity for hospitalists to meet new friends and to reconnect with old colleagues. The Annual Meeting in Chicago created a positive energy that will carry SHM members until we have the opportunity to meet again next year in Washington, DC.
Editor’s Note:
Having returned from the 8th SHM Annual Meeting at the time of this writing, it is clear that this was not only the biggest but also the best Annual Meeting to date. As Larry Wellikson and Joe Miller describe more fully in this issue, the lectures, workshops and networking activities available far outstripped the ability of attendees to take part in all of them. In fact, it was common to feel that there were 2, 3, or even more “must attend” sessions taking place simultaneously and if this was sometimes frustrating, it also spoke to the fact that the meeting’s quality was strikingly high. With the realization that a collection of articles is unable to fully convey the vibrancy of the meeting, we have assembled in the following section a “Big Picture” from imbedded reporter Joe Miller, overviews of 2 of the plenary lectures, and recaps of several outstanding breakout sessions. A separate monograph that will include other highlights of the Annual Meeting is under development and will be mailed in August.―JP
I was invited to write a short piece for The Hospitalist summarizing SHM’s 8th Annual Meeting on Thursday, April 28 through Saturday, April 30 in Chicago. As I sat on the airplane on my return flight to Boston, I reflected on what would define a “successful” annual meeting for the professional society representing hospitalists. I concluded that three criteria would define success. Specifically that the conference would:
- Demonstrate the strength and resiliency of the hospital medicine movement
- Provide quality content and learning opportunities to a diverse group of attendees
- Demonstrate that SHM is a competent and effective organization meeting the needs of its members.
I believe the meeting measured up extremely well on all three criteria.
With regard to demonstrating the vibrancy of the hospital medicine movement:
- At the conference, there was recognition by three significant stakeholders in the healthcare industry (hospitals, employers, and regulators) of the critical role of hospitalists. In the opening keynote address, Rick Wade, Senior Vice President of the American Hospital Association, described the growing pressure on hospitals to be “transparent,” sharing information with patients and the public on their performance. Mr. Wade’s address was followed by a presentation by Arnold Milstein, MD, Medical Director of the Pacific Business Group on Health and cofounder of the Leapfrog Group. Dr. Milstein used the metaphor of a shark’s jaws to describe the threat of the continued escalation of healthcare costs, and he indicated that the key to addressing this crisis is to “re-engineer” clinical processes to make them more efficient. On Saturday, Dennis O’Leary, CEO of JCAHO, described the challenge of evaluating the performance of hospitals in the era of patient safety. All three speakers indicated that hospitalists will be critical resources to healthcare leaders faced with these challenges. Another measure of the recognition of hospitalists as a force in the healthcare industry was the fact that over 90 exhibitors wanted the opportunity to get the ear of the conference attendees. The exhibit floor was teeming with hospitalists interested in learning about programs, products, and services.
- The growth of the hospital medicine movement was clearly evident to attendees of the conference. This year’s conference had over 1000 attendees,a growth of 15% over the 2004 annual meeting. When Alpesh Amin, MD, co-director of the course, opened the meeting, the attendees responded to a series of questions through the audience response system. For over 50% of the attendees, this was their first SHM Annual Meeting, indicating that the specialty of hospital medicine has a constant influx of “new blood.” And at the President’s Luncheon, the presentation by Larry Wellikson, MD, CEO of SHM, conveyed a broad array of statistics on the status of the hospital medicine movement, including the fact that the 12,000+ hospitalists in the U.S. makes the specialty bigger than gastroenterology and neurology. Approximately 30% of all U.S. Hospitals have hospital medicine programs; for hospitals with over 200 beds, 55% have hospitalists.
- The excellence of the hospital medicine movement was evident through the quality of the 120+ research, innovation, and clinical vignette posters presented on Friday. Furthermore, the accomplishments of the SHM award winners announced at the President’s Luncheon were quite impressive. Joseph Li, MD, won the award for Outstanding Service in Hospital Medicine, Sunil Kripalani, MD, was named the Outstanding Young Investigator, Shaun Frost, MD, won the Clinical Excellence award, and Jeff Wiese, MD, won the award for Excellence in Teaching. Hospitalists are demonstrating their ability to be innovative, high impact physicians.
With regard to providing learning opportunities for a diverse audience:
- The pre-courses on Thursday allowed attendees to gain in-depth knowledge on practice management, perioperative medicine, and critical care medicine.
- There were 35 separate presentations in 7 tracks over the 2 days of the main meeting. The clinical, adult clinical, and pediatric clinical tracks covered a wide array of topics, from maternal fetal medicine to acquired pediatric heart disease to addiction medicine. Tracks on quality and patient safety were very well attended, and the academic track included an important update on the hospitalist core curriculum being developed by SHM.
- There were 10 special interest forums allowing attendees interested in the following subjects to exchange ideas: community based hospitalists, research, education, medical directors, women hospitalists, pediatric hospitalists, family practice hospitalists, geriatric hospitalists, early career hospitalists, and nurse practitioners and physician assistants.
- The plenary sessions on updates in hospital medicine and pediatric hospital medicine provided excellent reviews of recent research relevant to hospitalists. Bob Wachter’s annual presentation, this year entitled “Hospital Medicine: Still Crazy After All These Years” laid out some important challenges for the hospital medicine movement as it moves into adolescence.
Finally, with regard to demonstrating SHM’s competence and its ability to meet the needs of its members:
- At the President’s Luncheon, the depth of SHM leadership was evident. Jeanne Huddleston, MD, reported on the significant accomplishments of the past year and handed the torch to SHM’s new President, Steve Pantilat, MD. Steve described his two goals for the upcoming year, the development ofan SHM Research Foundation and an emphasis on the role of hospitalists in palliative care. And Larry Wellikson, MD, SHM’s CEO, displayed energy and charisma throughout the meeting.
- The power of SHM volunteerism was unmistakable throughout the meeting. Preetha Basaviah, MD, the overall course director, harnessed group of SHM members participating in a planning committee to decide on the topics and choose the speakers for the meeting. A broad cross-section of SHM members participated in over 15 committee meetings in Chicago, as they donated their time to improving the field of hospital medicine.
- The conference was a vehicle to display the public relations capabilities of SHM. Melanie Bloom, wife of NBC newscaster David Bloom who died in Iraq of DVT complications, described the awareness campaign that SHM led. The attendees then viewed a short video of the television appearances by hospitalists in the last year, as hospital medicine has received increasing attention in the media. Larry Wellikson announced that every SHM member will receive a DVD with these video news segments.
- The strength of SHM staff and organization was on display in Chicago. Larry Wellikson reported that the staff has more than doubled and he cited a litany of accomplishments, including a new improved website, electronic registration for meetings, a broad range of educational offerings, and a healthy financial outlook. Furthermore, SHM has continued to experience significant membership growth, as the number of members now exceeds 4700, an increase of more than 40% in the past 12 months.
- Finally, and perhaps most importantly, Wellikson described a wide variety of initiatives that are being pursued to meet the needs of SHM members. These initiatives include a long range plan for the formal certification of hospitalists, strategic partnerships with key organizations, public policy initiatives, and the continued strengthening of historical efforts regarding education, leadership, and surveys.
In summary, the SHM conference was greater than the sum of the parts. It was successfully executed on multiple fronts. However I have not yet discussed perhaps the most important achievement of this meeting. It served as an opportunity for hospitalists to meet new friends and to reconnect with old colleagues. The Annual Meeting in Chicago created a positive energy that will carry SHM members until we have the opportunity to meet again next year in Washington, DC.