User login
Foster Ownership Culture
In my June column (“Follow the Money,” p. 61), I wrote about my concern that SHM’s “2007-2008 SHM Survey: State of the Hospital Medicine Movement” showed that more than one-third of hospitalist group leaders reported they did not know their groups’ annual professional fee revenues or expenses.
This is consistent with my experience working as a consultant with many other practices, and is one of many common findings in a struggling practice.
What about the opposite side of the coin? What are the common attributes of a healthy, successful practice? I talk about this all the time with my consulting colleague, Leslie Flores (director of practice management for SHM). We’ve become convinced that while the attributes to ensure success vary a little from one practice to the next, they can be rolled into the global heading of a “culture of ownership.” That is, the practices in which hospitalists think of themselves as owners of the practice (even if they are, in fact, employees of the hospital or some other organization) are most likely to be successful.
What is it?
Ownership culture is a mind-set, not a legal description of who has contractual ownership of the practice. I learned the hard way that not everyone knows what I mean when I talk about an ownership culture.
During the course of a conference a few years ago, I had several conversations with a sharp hospitalist practice leader about the problems his group faced. Apparently, many other doctors at the hospital treated them like residents. As I learned more it sounded as though this largely was the fault of the hospitalists themselves. It seemed clear to me the underlying theme was each doctor in the practice felt little connection to his/her hospitalist colleagues and the hospital in which they worked.
I began talking with the practice leader about how things could be different if the hospitalists would think of themselves as business owners and act accordingly. Yet, he couldn’t make sense of what I was saying since he thought I was suggesting that all the hospitalists resign from employment by the hospital (and presumably give up the financial support it provided) and form their own corporation. That isn’t necessary. It is possible to maintain an ownership culture even if the hospitalists are employees of a larger organization like a hospital (and not owners of their practice in the contractual sense).
Recognize it
A Web search on “ownership culture” returns a number of interesting sites. In fact, there is a National Center for Employee Ownership, which has an interesting Web site geared toward employees who own a significant portion of their company’s stock.
You also might want to look at their article titled “What Is an Ownership Culture?” (www.nceo.org/library/ownership_culture.html) and think about how your practice fits into that description.
Leslie and I have developed an informal quiz to help hospitalist practices think about whether they are supporting an ownership mindset. While we haven’t done research to validate these measures, we have considerable anecdotal experience supporting the idea that a high score on the questionnaire (i.e., lots of answers in the “pretty much” or “100%” columns) correlates well with an ownership mentality on the part of the doctors in the practice.
We’ve found such practices usually function more effectively and have happier hospitalists and customers (e.g., hospital personnel, other doctors, and patients). If you have an idea for valuable additions, deletions, or modifications to the questionnaire I’d love to hear from you.
Does it Matter?
While there are lots of other components to a good practice, I believe an ownership culture is one of the most important features leading to a successful and thriving practice. It is difficult to maintain a successful practice for very long without it.
You don’t have to take my word for it. Writing in The Baptist Health Care Journey to Excellence, Al Stubblefield says:
“Because it is so rare, an organization that is able to create this culture of ownership within its workforce has a high probability of creating a sustainable competitive advantage … The second advantage, which came as an unexpected bonus for us, is that creating a strong, attractive culture results in incredible recruiting power.” TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
In my June column (“Follow the Money,” p. 61), I wrote about my concern that SHM’s “2007-2008 SHM Survey: State of the Hospital Medicine Movement” showed that more than one-third of hospitalist group leaders reported they did not know their groups’ annual professional fee revenues or expenses.
This is consistent with my experience working as a consultant with many other practices, and is one of many common findings in a struggling practice.
What about the opposite side of the coin? What are the common attributes of a healthy, successful practice? I talk about this all the time with my consulting colleague, Leslie Flores (director of practice management for SHM). We’ve become convinced that while the attributes to ensure success vary a little from one practice to the next, they can be rolled into the global heading of a “culture of ownership.” That is, the practices in which hospitalists think of themselves as owners of the practice (even if they are, in fact, employees of the hospital or some other organization) are most likely to be successful.
What is it?
Ownership culture is a mind-set, not a legal description of who has contractual ownership of the practice. I learned the hard way that not everyone knows what I mean when I talk about an ownership culture.
During the course of a conference a few years ago, I had several conversations with a sharp hospitalist practice leader about the problems his group faced. Apparently, many other doctors at the hospital treated them like residents. As I learned more it sounded as though this largely was the fault of the hospitalists themselves. It seemed clear to me the underlying theme was each doctor in the practice felt little connection to his/her hospitalist colleagues and the hospital in which they worked.
I began talking with the practice leader about how things could be different if the hospitalists would think of themselves as business owners and act accordingly. Yet, he couldn’t make sense of what I was saying since he thought I was suggesting that all the hospitalists resign from employment by the hospital (and presumably give up the financial support it provided) and form their own corporation. That isn’t necessary. It is possible to maintain an ownership culture even if the hospitalists are employees of a larger organization like a hospital (and not owners of their practice in the contractual sense).
Recognize it
A Web search on “ownership culture” returns a number of interesting sites. In fact, there is a National Center for Employee Ownership, which has an interesting Web site geared toward employees who own a significant portion of their company’s stock.
You also might want to look at their article titled “What Is an Ownership Culture?” (www.nceo.org/library/ownership_culture.html) and think about how your practice fits into that description.
Leslie and I have developed an informal quiz to help hospitalist practices think about whether they are supporting an ownership mindset. While we haven’t done research to validate these measures, we have considerable anecdotal experience supporting the idea that a high score on the questionnaire (i.e., lots of answers in the “pretty much” or “100%” columns) correlates well with an ownership mentality on the part of the doctors in the practice.
We’ve found such practices usually function more effectively and have happier hospitalists and customers (e.g., hospital personnel, other doctors, and patients). If you have an idea for valuable additions, deletions, or modifications to the questionnaire I’d love to hear from you.
Does it Matter?
While there are lots of other components to a good practice, I believe an ownership culture is one of the most important features leading to a successful and thriving practice. It is difficult to maintain a successful practice for very long without it.
You don’t have to take my word for it. Writing in The Baptist Health Care Journey to Excellence, Al Stubblefield says:
“Because it is so rare, an organization that is able to create this culture of ownership within its workforce has a high probability of creating a sustainable competitive advantage … The second advantage, which came as an unexpected bonus for us, is that creating a strong, attractive culture results in incredible recruiting power.” TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
In my June column (“Follow the Money,” p. 61), I wrote about my concern that SHM’s “2007-2008 SHM Survey: State of the Hospital Medicine Movement” showed that more than one-third of hospitalist group leaders reported they did not know their groups’ annual professional fee revenues or expenses.
This is consistent with my experience working as a consultant with many other practices, and is one of many common findings in a struggling practice.
What about the opposite side of the coin? What are the common attributes of a healthy, successful practice? I talk about this all the time with my consulting colleague, Leslie Flores (director of practice management for SHM). We’ve become convinced that while the attributes to ensure success vary a little from one practice to the next, they can be rolled into the global heading of a “culture of ownership.” That is, the practices in which hospitalists think of themselves as owners of the practice (even if they are, in fact, employees of the hospital or some other organization) are most likely to be successful.
What is it?
Ownership culture is a mind-set, not a legal description of who has contractual ownership of the practice. I learned the hard way that not everyone knows what I mean when I talk about an ownership culture.
During the course of a conference a few years ago, I had several conversations with a sharp hospitalist practice leader about the problems his group faced. Apparently, many other doctors at the hospital treated them like residents. As I learned more it sounded as though this largely was the fault of the hospitalists themselves. It seemed clear to me the underlying theme was each doctor in the practice felt little connection to his/her hospitalist colleagues and the hospital in which they worked.
I began talking with the practice leader about how things could be different if the hospitalists would think of themselves as business owners and act accordingly. Yet, he couldn’t make sense of what I was saying since he thought I was suggesting that all the hospitalists resign from employment by the hospital (and presumably give up the financial support it provided) and form their own corporation. That isn’t necessary. It is possible to maintain an ownership culture even if the hospitalists are employees of a larger organization like a hospital (and not owners of their practice in the contractual sense).
Recognize it
A Web search on “ownership culture” returns a number of interesting sites. In fact, there is a National Center for Employee Ownership, which has an interesting Web site geared toward employees who own a significant portion of their company’s stock.
You also might want to look at their article titled “What Is an Ownership Culture?” (www.nceo.org/library/ownership_culture.html) and think about how your practice fits into that description.
Leslie and I have developed an informal quiz to help hospitalist practices think about whether they are supporting an ownership mindset. While we haven’t done research to validate these measures, we have considerable anecdotal experience supporting the idea that a high score on the questionnaire (i.e., lots of answers in the “pretty much” or “100%” columns) correlates well with an ownership mentality on the part of the doctors in the practice.
We’ve found such practices usually function more effectively and have happier hospitalists and customers (e.g., hospital personnel, other doctors, and patients). If you have an idea for valuable additions, deletions, or modifications to the questionnaire I’d love to hear from you.
Does it Matter?
While there are lots of other components to a good practice, I believe an ownership culture is one of the most important features leading to a successful and thriving practice. It is difficult to maintain a successful practice for very long without it.
You don’t have to take my word for it. Writing in The Baptist Health Care Journey to Excellence, Al Stubblefield says:
“Because it is so rare, an organization that is able to create this culture of ownership within its workforce has a high probability of creating a sustainable competitive advantage … The second advantage, which came as an unexpected bonus for us, is that creating a strong, attractive culture results in incredible recruiting power.” TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
We’re Hiring
At the 2008 SHM Annual Meeting in San Diego, I had the pleasure of serving as moderator for a panel commenting on the opportunities and challenges faced by hospitalists. I’m not sure how well our predictions will withstand the test of time, but two things came up that I’ll discuss here:
1) Nearly every group is recruiting, and many seem to think the hospitalist shortage will last throughout the careers of those in practice today.
2) Nearly all hospitalist groups are looking for more doctors. I asked the approximately 1,600 in attendance how many are recruiting for more hospitalists. Nearly every hand in the room shot up. It was impressive; one friend (Bob Reynolds) told me he was sitting in the back and could feel a breeze in the room from all the hands being raised. Only about three hands went up when I asked how many thought their staffing was adequate.
Bear in mind that based on the show of hands nearly every group in the country is recruiting. Many groups are looking to add three to six hospitalists this year alone. This is on top of the average group growing about 20% to 25% the past two years, based on my study of data from the “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement.” The survey showed the number of FTE doctors in the average hospitalist group grew from a median six to eight hospitalists (the average went from eight to 9.7).
Hospital medicine is the fastest-growing field in the history of American medicine, and it looks like the demand for hospitalists may be increasing even faster than the supply.
I was tempted to ask for a show of hands from doctors at the meeting who were looking for a hospitalist position, but feared it could disrupt the whole conference as those seeking new doctors pounced on the potential candidates in a piranha-like feeding frenzy. So there is good news for anyone interested in joining a hospitalist group: You should have a lot of choices. If you’re recruiting, you’d better get to work to make sure you have really good plan. Let me offer a few ideas.
Never stop recruiting. Dr. Greg Mappin, VPMA at Self Regional Hospital in Greenwood, S.C., told me his philosophy is to “recruit forever, and hire when necessary.” I agree.
You should build and maintain a robust candidate pipeline by ensuring your practice maintains a high level of visibility before your best source of new doctors. The best source for most groups is the closest residency training program, though other nearby hospitalist or outpatient practices might be a secondary source of new manpower.
I suggest you engage residents by hosting a dinner near their hospital once or twice a year and inviting all second- and third-year residents to attend regardless of their interest in becoming hospitalists. You might do this even in years you may not need to add hospitalists to ensure your dinner becomes a regular event for them and to ensure they’re very familiar with your program. Some hospitals develop night and weekend moonlighting programs that employ nearby residents, which increases the chance some will join the practice upon completion of their training.
Ensure all hospitalists—especially the group leader—actively participate in recruiting. Your hospital or medical group’s physician recruiter can be a terrific asset. He/she can provide advice regarding how to find candidates, arranging interviews, etc. Yet, it is critical for the hospitalist group leader to actively communicate with every candidate, including responding to every inquiry within a day or so.
Too many group leaders make a big mistake by waiting many days to respond to new inquiries, or letting the recruiter handle all communication in advance of an interview. During the interview, be sure the candidate spends time with many of the current group members and provides contact information for every group member in case the candidate would like to call any who weren’t available on the interview day. Consider providing the candidate with a copy of the group schedule, any orientation documents you have, and other such printed materials to review after the visit.
Recruit specifically for short-term members of your practice. Despite concerns about turnover, I think it is reasonable to actively pursue candidates who may have as little as two years to work in your practice. For example, they may plan to move to another town (e.g., when their spouse finishes training) or start fellowship training. In my experience, at least half of new doctors who plan to be a hospitalist for only a year or two will choose to stay on long term.
If you want your classified ad to stand out, think about writing one that specifically targets short-term hospitalists. It could say something like: “Do you have only two years to work as a hospitalist? Then this is the place for you.” You even could add benefits, such as tuition to attend conferences that would be of value for the doctor regardless of their future specialty or practice setting. If you desperately need additional doctors, get creative in recruiting those who plan to stay with you for only a couple years. I’m confident some will end up staying long term.
Continue “recruiting” the doctors in your practice. For a number of reasons, hospitalist turnover may be higher than most other specialties. So it is particularly important to take steps to minimize it. SHM’s white paper on hospitalist career satisfaction (“A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction”) offers observations and valuable suggestions for any practice. Find it under the “Publications” link on SHM’s Web site, www. hospitalmedicine.org.
No End to Shortage
Now back to that panel discussion at SHM’s Annual Meeting in April. I asked the panelists what things would be like if in 10 years the demand for hospitalists decreased, and the supply finally caught up with and ultimately exceeded demand.
I thought this could be a provocative question that would lead to a discussion about how much of our current situation, such as recent increases in hospital financial support provided per hospitalist, are due to the current hospitalist shortage. Will hospitals decrease their support if there is ever an excess of hospitalists?
No one was buying it. Everyone was convinced that despite the incredible growth in numbers of doctors practicing as hospitalists, the demand for hospitalists will continue to grow even faster than the supply. Panelist Ron Greeno, MD, FCCP, chief medical officer of Cogent Healthcare in Irvine, Calif., thought this hospitalist shortage would continue throughout our lifetime. I’m not sure how long Ron thinks he (or I) will live, but that’s a pretty bold prediction.
It looks like the current intense recruiting environment is here to stay for a long time. Every practice should be thinking about how best to manage it. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
At the 2008 SHM Annual Meeting in San Diego, I had the pleasure of serving as moderator for a panel commenting on the opportunities and challenges faced by hospitalists. I’m not sure how well our predictions will withstand the test of time, but two things came up that I’ll discuss here:
1) Nearly every group is recruiting, and many seem to think the hospitalist shortage will last throughout the careers of those in practice today.
2) Nearly all hospitalist groups are looking for more doctors. I asked the approximately 1,600 in attendance how many are recruiting for more hospitalists. Nearly every hand in the room shot up. It was impressive; one friend (Bob Reynolds) told me he was sitting in the back and could feel a breeze in the room from all the hands being raised. Only about three hands went up when I asked how many thought their staffing was adequate.
Bear in mind that based on the show of hands nearly every group in the country is recruiting. Many groups are looking to add three to six hospitalists this year alone. This is on top of the average group growing about 20% to 25% the past two years, based on my study of data from the “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement.” The survey showed the number of FTE doctors in the average hospitalist group grew from a median six to eight hospitalists (the average went from eight to 9.7).
Hospital medicine is the fastest-growing field in the history of American medicine, and it looks like the demand for hospitalists may be increasing even faster than the supply.
I was tempted to ask for a show of hands from doctors at the meeting who were looking for a hospitalist position, but feared it could disrupt the whole conference as those seeking new doctors pounced on the potential candidates in a piranha-like feeding frenzy. So there is good news for anyone interested in joining a hospitalist group: You should have a lot of choices. If you’re recruiting, you’d better get to work to make sure you have really good plan. Let me offer a few ideas.
Never stop recruiting. Dr. Greg Mappin, VPMA at Self Regional Hospital in Greenwood, S.C., told me his philosophy is to “recruit forever, and hire when necessary.” I agree.
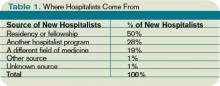
You should build and maintain a robust candidate pipeline by ensuring your practice maintains a high level of visibility before your best source of new doctors. The best source for most groups is the closest residency training program, though other nearby hospitalist or outpatient practices might be a secondary source of new manpower.
I suggest you engage residents by hosting a dinner near their hospital once or twice a year and inviting all second- and third-year residents to attend regardless of their interest in becoming hospitalists. You might do this even in years you may not need to add hospitalists to ensure your dinner becomes a regular event for them and to ensure they’re very familiar with your program. Some hospitals develop night and weekend moonlighting programs that employ nearby residents, which increases the chance some will join the practice upon completion of their training.
Ensure all hospitalists—especially the group leader—actively participate in recruiting. Your hospital or medical group’s physician recruiter can be a terrific asset. He/she can provide advice regarding how to find candidates, arranging interviews, etc. Yet, it is critical for the hospitalist group leader to actively communicate with every candidate, including responding to every inquiry within a day or so.
Too many group leaders make a big mistake by waiting many days to respond to new inquiries, or letting the recruiter handle all communication in advance of an interview. During the interview, be sure the candidate spends time with many of the current group members and provides contact information for every group member in case the candidate would like to call any who weren’t available on the interview day. Consider providing the candidate with a copy of the group schedule, any orientation documents you have, and other such printed materials to review after the visit.
Recruit specifically for short-term members of your practice. Despite concerns about turnover, I think it is reasonable to actively pursue candidates who may have as little as two years to work in your practice. For example, they may plan to move to another town (e.g., when their spouse finishes training) or start fellowship training. In my experience, at least half of new doctors who plan to be a hospitalist for only a year or two will choose to stay on long term.
If you want your classified ad to stand out, think about writing one that specifically targets short-term hospitalists. It could say something like: “Do you have only two years to work as a hospitalist? Then this is the place for you.” You even could add benefits, such as tuition to attend conferences that would be of value for the doctor regardless of their future specialty or practice setting. If you desperately need additional doctors, get creative in recruiting those who plan to stay with you for only a couple years. I’m confident some will end up staying long term.
Continue “recruiting” the doctors in your practice. For a number of reasons, hospitalist turnover may be higher than most other specialties. So it is particularly important to take steps to minimize it. SHM’s white paper on hospitalist career satisfaction (“A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction”) offers observations and valuable suggestions for any practice. Find it under the “Publications” link on SHM’s Web site, www. hospitalmedicine.org.
No End to Shortage
Now back to that panel discussion at SHM’s Annual Meeting in April. I asked the panelists what things would be like if in 10 years the demand for hospitalists decreased, and the supply finally caught up with and ultimately exceeded demand.
I thought this could be a provocative question that would lead to a discussion about how much of our current situation, such as recent increases in hospital financial support provided per hospitalist, are due to the current hospitalist shortage. Will hospitals decrease their support if there is ever an excess of hospitalists?
No one was buying it. Everyone was convinced that despite the incredible growth in numbers of doctors practicing as hospitalists, the demand for hospitalists will continue to grow even faster than the supply. Panelist Ron Greeno, MD, FCCP, chief medical officer of Cogent Healthcare in Irvine, Calif., thought this hospitalist shortage would continue throughout our lifetime. I’m not sure how long Ron thinks he (or I) will live, but that’s a pretty bold prediction.
It looks like the current intense recruiting environment is here to stay for a long time. Every practice should be thinking about how best to manage it. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
At the 2008 SHM Annual Meeting in San Diego, I had the pleasure of serving as moderator for a panel commenting on the opportunities and challenges faced by hospitalists. I’m not sure how well our predictions will withstand the test of time, but two things came up that I’ll discuss here:
1) Nearly every group is recruiting, and many seem to think the hospitalist shortage will last throughout the careers of those in practice today.
2) Nearly all hospitalist groups are looking for more doctors. I asked the approximately 1,600 in attendance how many are recruiting for more hospitalists. Nearly every hand in the room shot up. It was impressive; one friend (Bob Reynolds) told me he was sitting in the back and could feel a breeze in the room from all the hands being raised. Only about three hands went up when I asked how many thought their staffing was adequate.
Bear in mind that based on the show of hands nearly every group in the country is recruiting. Many groups are looking to add three to six hospitalists this year alone. This is on top of the average group growing about 20% to 25% the past two years, based on my study of data from the “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement.” The survey showed the number of FTE doctors in the average hospitalist group grew from a median six to eight hospitalists (the average went from eight to 9.7).
Hospital medicine is the fastest-growing field in the history of American medicine, and it looks like the demand for hospitalists may be increasing even faster than the supply.
I was tempted to ask for a show of hands from doctors at the meeting who were looking for a hospitalist position, but feared it could disrupt the whole conference as those seeking new doctors pounced on the potential candidates in a piranha-like feeding frenzy. So there is good news for anyone interested in joining a hospitalist group: You should have a lot of choices. If you’re recruiting, you’d better get to work to make sure you have really good plan. Let me offer a few ideas.
Never stop recruiting. Dr. Greg Mappin, VPMA at Self Regional Hospital in Greenwood, S.C., told me his philosophy is to “recruit forever, and hire when necessary.” I agree.
You should build and maintain a robust candidate pipeline by ensuring your practice maintains a high level of visibility before your best source of new doctors. The best source for most groups is the closest residency training program, though other nearby hospitalist or outpatient practices might be a secondary source of new manpower.
I suggest you engage residents by hosting a dinner near their hospital once or twice a year and inviting all second- and third-year residents to attend regardless of their interest in becoming hospitalists. You might do this even in years you may not need to add hospitalists to ensure your dinner becomes a regular event for them and to ensure they’re very familiar with your program. Some hospitals develop night and weekend moonlighting programs that employ nearby residents, which increases the chance some will join the practice upon completion of their training.
Ensure all hospitalists—especially the group leader—actively participate in recruiting. Your hospital or medical group’s physician recruiter can be a terrific asset. He/she can provide advice regarding how to find candidates, arranging interviews, etc. Yet, it is critical for the hospitalist group leader to actively communicate with every candidate, including responding to every inquiry within a day or so.
Too many group leaders make a big mistake by waiting many days to respond to new inquiries, or letting the recruiter handle all communication in advance of an interview. During the interview, be sure the candidate spends time with many of the current group members and provides contact information for every group member in case the candidate would like to call any who weren’t available on the interview day. Consider providing the candidate with a copy of the group schedule, any orientation documents you have, and other such printed materials to review after the visit.
Recruit specifically for short-term members of your practice. Despite concerns about turnover, I think it is reasonable to actively pursue candidates who may have as little as two years to work in your practice. For example, they may plan to move to another town (e.g., when their spouse finishes training) or start fellowship training. In my experience, at least half of new doctors who plan to be a hospitalist for only a year or two will choose to stay on long term.
If you want your classified ad to stand out, think about writing one that specifically targets short-term hospitalists. It could say something like: “Do you have only two years to work as a hospitalist? Then this is the place for you.” You even could add benefits, such as tuition to attend conferences that would be of value for the doctor regardless of their future specialty or practice setting. If you desperately need additional doctors, get creative in recruiting those who plan to stay with you for only a couple years. I’m confident some will end up staying long term.
Continue “recruiting” the doctors in your practice. For a number of reasons, hospitalist turnover may be higher than most other specialties. So it is particularly important to take steps to minimize it. SHM’s white paper on hospitalist career satisfaction (“A Challenge for a New Specialty: A White Paper on Hospitalist Career Satisfaction”) offers observations and valuable suggestions for any practice. Find it under the “Publications” link on SHM’s Web site, www. hospitalmedicine.org.
No End to Shortage
Now back to that panel discussion at SHM’s Annual Meeting in April. I asked the panelists what things would be like if in 10 years the demand for hospitalists decreased, and the supply finally caught up with and ultimately exceeded demand.
I thought this could be a provocative question that would lead to a discussion about how much of our current situation, such as recent increases in hospital financial support provided per hospitalist, are due to the current hospitalist shortage. Will hospitals decrease their support if there is ever an excess of hospitalists?
No one was buying it. Everyone was convinced that despite the incredible growth in numbers of doctors practicing as hospitalists, the demand for hospitalists will continue to grow even faster than the supply. Panelist Ron Greeno, MD, FCCP, chief medical officer of Cogent Healthcare in Irvine, Calif., thought this hospitalist shortage would continue throughout our lifetime. I’m not sure how long Ron thinks he (or I) will live, but that’s a pretty bold prediction.
It looks like the current intense recruiting environment is here to stay for a long time. Every practice should be thinking about how best to manage it. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Follow the Money
I eagerly await results from SHM’s survey of hospitalist productivity and compensation every two years. I’m most curious about whether a typical hospitalist has experienced an improvement in his/her “juice to squeeze ratio” (aka compensation per unit of work).
I was pleased to see in the recently released “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement” that average hospitalist salaries increased the most for any two-year interval since we began surveying in 1997. If you haven’t seen the survey results, go to SHM’s Web site www.hospitalmedicine.org. Production remained flat, while compensation increased to an average of $188,500. (The survey showed an adjusted mean annual compensation of $193,300, and a median salary of $183,900. See complete survey for explanation regarding the adjusted mean, which refers to data for hospitalists who care for adult patients only.)
The 2008 survey has a couple of findings even more compelling than the gratifying improvement in compensation:
- 37% of HMG leaders did not know their annual expenses; and
- 35% of HMG leaders did not know their annual professional fee revenues.
Think about this for a minute. One-third of hospitalist group leaders don’t know enough about their own practice’s financial picture to know high-level details related to income and expenses. We only can presume an even larger portion of non-leader hospitalists don’t know these things about their practice.
These numbers are disconcerting, and they’re even a little worse than the numbers reported two years ago. How can this be?
Behind the Numbers
My first inclination is to look for reasons the data are misleading. Maybe some leaders chose to respond by indicating they don’t know these numbers, when in fact they do have the numbers but were just too busy to look them up and complete that part of the survey. So they might be better informed than the survey suggests, but just too busy to demonstrate it.
Or, some group leaders in large organizations, like Kaiser, may track and account for productivity and financial health in ways that differ from a typical practice. They may know a lot about their practice, but the metrics the survey asks for aren’t relevant to them.
Maybe the survey results are misleading and group leaders know a lot more about their practice financials than these numbers suggest. Well, maybe.
Unfortunately, in my consulting work up close and personal with hundreds of practices, I regularly meet group leaders who don’t see financial accountability as one of their duties. I think the survey numbers may be a reasonably accurate reflection of reality.
I typically ask group leaders things like what portion of their practice budget is funded by professional fee collections vs. payment from the hospital (or other “sponsoring organization”) and what the pro fee collection rate is. As in the survey, a large portion don’t know. They often say it’s up to someone else to keep track of those numbers and worry about the practice budget. I worry that a leader with such a hands-off approach to the practice budget can’t be very effective.
I also ask leaders things like what is their most important duty as group leader. “Making the schedule” is too often the disappointing answer. Clearly the schedule is a critical part of operating a practice, but in many practices it is reasonable, even optimal, to have a clerical person manage the schedule, or rotate responsibility for creating it among all members of the group. This frees some time the leader can spend on other activities like managing the group’s financial performance, among other things.
What Leaders Do
The ideal hospitalist practice leader’s job description will vary from place to place. It includes many things in addition to ensuring the schedule gets created. There are a handful of things that should probably be on every leader’s list. For my money, this leader should:
- Understand where the money comes from, where it goes, and what portion comes from professional fee collections vs. other sources. Also, to ensure all members of the group are updated on financial parameters regularly;
- Put in place mechanisms to ensure the hospitalists provide high-quality care to patients;
- Facilitate communication among hospitalists, hospital personnel, and medical staff to foster effective working relationships and facilitate problem-solving and conflict resolution;
- Proactively identify opportunities for the practice to enhance the service it provides to its constituents and the organization in general, and negotiating a reasonable balance between such opportunities and the practice’s resources and clinical expertise;
- Serve as a point of contact for referring primary care physicians;
- Representing the group when working and negotiating with the hospital administration; and
- Take an active role in recruitment while addressing behavior and performance issues within the practice.
Whether the leader handles these issues alone, delegates responsibility but still provides oversight, or forms a committee with other hospitalists, will vary from place to place. In every case, though, the leader should make sure these things are happening effectively.
Our field is young, and I think tends to attract people who want to avoid managing a complex practice. Perhaps it is no surprise some leaders may not be handling their job optimally. Fortunately, help is available.
Any group leader who wants to function more effectively can do several things. First, start talking to other practice leaders in your hospital. You could ask the lead doctor in another group what he/she regards as the most important components of their leadership role, and strategies that person used to become an effective leader.
Additionally, SHM has a highly regarded Leadership Academy designed to provide group leaders with the skills and resources required to successfully lead and manage a hospital medicine program now and in the future.
Each group leader should periodically step back from the day-to-day work to think about whether his/her time and energy is optimally allocated. Is the mix of clinical and administrative work reasonable? Does the leader devote time to activities (e.g., making the schedule) that could be handed off to others?
The standards used to differentiate between an effective and ineffective leader are hard to pin down and will vary a lot depending on the characteristics of a practice. Still, a comprehensive understanding of the practice’s budget and financial performance should probably be on everyone’s list. I hope the next SHM survey in late 2009 shows a lot more group leaders know things like their group’s annual expenses and revenues. We’ll see. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
I eagerly await results from SHM’s survey of hospitalist productivity and compensation every two years. I’m most curious about whether a typical hospitalist has experienced an improvement in his/her “juice to squeeze ratio” (aka compensation per unit of work).
I was pleased to see in the recently released “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement” that average hospitalist salaries increased the most for any two-year interval since we began surveying in 1997. If you haven’t seen the survey results, go to SHM’s Web site www.hospitalmedicine.org. Production remained flat, while compensation increased to an average of $188,500. (The survey showed an adjusted mean annual compensation of $193,300, and a median salary of $183,900. See complete survey for explanation regarding the adjusted mean, which refers to data for hospitalists who care for adult patients only.)
The 2008 survey has a couple of findings even more compelling than the gratifying improvement in compensation:
- 37% of HMG leaders did not know their annual expenses; and
- 35% of HMG leaders did not know their annual professional fee revenues.
Think about this for a minute. One-third of hospitalist group leaders don’t know enough about their own practice’s financial picture to know high-level details related to income and expenses. We only can presume an even larger portion of non-leader hospitalists don’t know these things about their practice.
These numbers are disconcerting, and they’re even a little worse than the numbers reported two years ago. How can this be?
Behind the Numbers
My first inclination is to look for reasons the data are misleading. Maybe some leaders chose to respond by indicating they don’t know these numbers, when in fact they do have the numbers but were just too busy to look them up and complete that part of the survey. So they might be better informed than the survey suggests, but just too busy to demonstrate it.
Or, some group leaders in large organizations, like Kaiser, may track and account for productivity and financial health in ways that differ from a typical practice. They may know a lot about their practice, but the metrics the survey asks for aren’t relevant to them.
Maybe the survey results are misleading and group leaders know a lot more about their practice financials than these numbers suggest. Well, maybe.
Unfortunately, in my consulting work up close and personal with hundreds of practices, I regularly meet group leaders who don’t see financial accountability as one of their duties. I think the survey numbers may be a reasonably accurate reflection of reality.
I typically ask group leaders things like what portion of their practice budget is funded by professional fee collections vs. payment from the hospital (or other “sponsoring organization”) and what the pro fee collection rate is. As in the survey, a large portion don’t know. They often say it’s up to someone else to keep track of those numbers and worry about the practice budget. I worry that a leader with such a hands-off approach to the practice budget can’t be very effective.
I also ask leaders things like what is their most important duty as group leader. “Making the schedule” is too often the disappointing answer. Clearly the schedule is a critical part of operating a practice, but in many practices it is reasonable, even optimal, to have a clerical person manage the schedule, or rotate responsibility for creating it among all members of the group. This frees some time the leader can spend on other activities like managing the group’s financial performance, among other things.
What Leaders Do
The ideal hospitalist practice leader’s job description will vary from place to place. It includes many things in addition to ensuring the schedule gets created. There are a handful of things that should probably be on every leader’s list. For my money, this leader should:
- Understand where the money comes from, where it goes, and what portion comes from professional fee collections vs. other sources. Also, to ensure all members of the group are updated on financial parameters regularly;
- Put in place mechanisms to ensure the hospitalists provide high-quality care to patients;
- Facilitate communication among hospitalists, hospital personnel, and medical staff to foster effective working relationships and facilitate problem-solving and conflict resolution;
- Proactively identify opportunities for the practice to enhance the service it provides to its constituents and the organization in general, and negotiating a reasonable balance between such opportunities and the practice’s resources and clinical expertise;
- Serve as a point of contact for referring primary care physicians;
- Representing the group when working and negotiating with the hospital administration; and
- Take an active role in recruitment while addressing behavior and performance issues within the practice.
Whether the leader handles these issues alone, delegates responsibility but still provides oversight, or forms a committee with other hospitalists, will vary from place to place. In every case, though, the leader should make sure these things are happening effectively.
Our field is young, and I think tends to attract people who want to avoid managing a complex practice. Perhaps it is no surprise some leaders may not be handling their job optimally. Fortunately, help is available.
Any group leader who wants to function more effectively can do several things. First, start talking to other practice leaders in your hospital. You could ask the lead doctor in another group what he/she regards as the most important components of their leadership role, and strategies that person used to become an effective leader.
Additionally, SHM has a highly regarded Leadership Academy designed to provide group leaders with the skills and resources required to successfully lead and manage a hospital medicine program now and in the future.
Each group leader should periodically step back from the day-to-day work to think about whether his/her time and energy is optimally allocated. Is the mix of clinical and administrative work reasonable? Does the leader devote time to activities (e.g., making the schedule) that could be handed off to others?
The standards used to differentiate between an effective and ineffective leader are hard to pin down and will vary a lot depending on the characteristics of a practice. Still, a comprehensive understanding of the practice’s budget and financial performance should probably be on everyone’s list. I hope the next SHM survey in late 2009 shows a lot more group leaders know things like their group’s annual expenses and revenues. We’ll see. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
I eagerly await results from SHM’s survey of hospitalist productivity and compensation every two years. I’m most curious about whether a typical hospitalist has experienced an improvement in his/her “juice to squeeze ratio” (aka compensation per unit of work).
I was pleased to see in the recently released “Society of Hospital Medicine 2007-08 Survey: The Authoritative Source on the State of the Hospitalist Movement” that average hospitalist salaries increased the most for any two-year interval since we began surveying in 1997. If you haven’t seen the survey results, go to SHM’s Web site www.hospitalmedicine.org. Production remained flat, while compensation increased to an average of $188,500. (The survey showed an adjusted mean annual compensation of $193,300, and a median salary of $183,900. See complete survey for explanation regarding the adjusted mean, which refers to data for hospitalists who care for adult patients only.)
The 2008 survey has a couple of findings even more compelling than the gratifying improvement in compensation:
- 37% of HMG leaders did not know their annual expenses; and
- 35% of HMG leaders did not know their annual professional fee revenues.
Think about this for a minute. One-third of hospitalist group leaders don’t know enough about their own practice’s financial picture to know high-level details related to income and expenses. We only can presume an even larger portion of non-leader hospitalists don’t know these things about their practice.
These numbers are disconcerting, and they’re even a little worse than the numbers reported two years ago. How can this be?
Behind the Numbers
My first inclination is to look for reasons the data are misleading. Maybe some leaders chose to respond by indicating they don’t know these numbers, when in fact they do have the numbers but were just too busy to look them up and complete that part of the survey. So they might be better informed than the survey suggests, but just too busy to demonstrate it.
Or, some group leaders in large organizations, like Kaiser, may track and account for productivity and financial health in ways that differ from a typical practice. They may know a lot about their practice, but the metrics the survey asks for aren’t relevant to them.
Maybe the survey results are misleading and group leaders know a lot more about their practice financials than these numbers suggest. Well, maybe.
Unfortunately, in my consulting work up close and personal with hundreds of practices, I regularly meet group leaders who don’t see financial accountability as one of their duties. I think the survey numbers may be a reasonably accurate reflection of reality.
I typically ask group leaders things like what portion of their practice budget is funded by professional fee collections vs. payment from the hospital (or other “sponsoring organization”) and what the pro fee collection rate is. As in the survey, a large portion don’t know. They often say it’s up to someone else to keep track of those numbers and worry about the practice budget. I worry that a leader with such a hands-off approach to the practice budget can’t be very effective.
I also ask leaders things like what is their most important duty as group leader. “Making the schedule” is too often the disappointing answer. Clearly the schedule is a critical part of operating a practice, but in many practices it is reasonable, even optimal, to have a clerical person manage the schedule, or rotate responsibility for creating it among all members of the group. This frees some time the leader can spend on other activities like managing the group’s financial performance, among other things.
What Leaders Do
The ideal hospitalist practice leader’s job description will vary from place to place. It includes many things in addition to ensuring the schedule gets created. There are a handful of things that should probably be on every leader’s list. For my money, this leader should:
- Understand where the money comes from, where it goes, and what portion comes from professional fee collections vs. other sources. Also, to ensure all members of the group are updated on financial parameters regularly;
- Put in place mechanisms to ensure the hospitalists provide high-quality care to patients;
- Facilitate communication among hospitalists, hospital personnel, and medical staff to foster effective working relationships and facilitate problem-solving and conflict resolution;
- Proactively identify opportunities for the practice to enhance the service it provides to its constituents and the organization in general, and negotiating a reasonable balance between such opportunities and the practice’s resources and clinical expertise;
- Serve as a point of contact for referring primary care physicians;
- Representing the group when working and negotiating with the hospital administration; and
- Take an active role in recruitment while addressing behavior and performance issues within the practice.
Whether the leader handles these issues alone, delegates responsibility but still provides oversight, or forms a committee with other hospitalists, will vary from place to place. In every case, though, the leader should make sure these things are happening effectively.
Our field is young, and I think tends to attract people who want to avoid managing a complex practice. Perhaps it is no surprise some leaders may not be handling their job optimally. Fortunately, help is available.
Any group leader who wants to function more effectively can do several things. First, start talking to other practice leaders in your hospital. You could ask the lead doctor in another group what he/she regards as the most important components of their leadership role, and strategies that person used to become an effective leader.
Additionally, SHM has a highly regarded Leadership Academy designed to provide group leaders with the skills and resources required to successfully lead and manage a hospital medicine program now and in the future.
Each group leader should periodically step back from the day-to-day work to think about whether his/her time and energy is optimally allocated. Is the mix of clinical and administrative work reasonable? Does the leader devote time to activities (e.g., making the schedule) that could be handed off to others?
The standards used to differentiate between an effective and ineffective leader are hard to pin down and will vary a lot depending on the characteristics of a practice. Still, a comprehensive understanding of the practice’s budget and financial performance should probably be on everyone’s list. I hope the next SHM survey in late 2009 shows a lot more group leaders know things like their group’s annual expenses and revenues. We’ll see. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Value Your Practice
The issue of practice valuation is a sensitive one. Some hospitalist practices might have significant monetary value, which could make it reasonable to ask new doctors to buy in or enable selling the practice for a profit. Still, it’s risky to assume this is the case for your practice.
Let’s examine the issue using a pair of situations I encountered not long ago. I have changed some details of the practices to more clearly illustrate a point and conceal which practices I’m describing. Both situations would have gone smoother if it was clear what the hospitalist practice was worth. But how do you assess that value?
Case No. 1
During a couple of days in 2006, I consulted with a high-performing private practice hospitalist group on the East Coast. The group was led by one of the most energetic and thoughtful leaders I’ve encountered.
Like many other private practice groups, they divided physician members of the practice into partners and non-partners (sometimes referred to as shareholder and non-shareholders in the corporation). A hospitalist who had been a full-time member of the practice for a specified period of time (two years in this case) was eligible to become partner.
This entailed a “buy-in” requiring the doctor to pay money to the practice (usually the doctor would pay using a loan from the practice, which was repaid through deductions from his/her paycheck).
For this practice, the principal benefits of partner status were having a vote in group decisions (non-partners couldn’t vote) and receiving a portion of the distribution of all corporate profits each year. These profits came from two sources:
- Money remaining after all salaries and overhead were paid; and
- Buy-in money received by the practice.
Because the partners had this “upside potential” they agreed they would cover any staff shortages by working extra shifts instead of the non-partners.
Setting things up with a buy-in to achieve partner/shareholder status seemed to make a lot of sense. After all, it is the way nearly all private-practice medical groups in other specialties are structured.
Problems soon arose when they realized there wasn’t significant “profit” available unless there happened to be two or three doctors buying into the practice in a given year.
So, the partners became disenchanted because they shouldered the burden of covering any extra shifts but didn’t get a significant profit distribution in most years. Non-partners who became eligible for partnership were choosing not to buy in because it seemed like more responsibility without more income. The group’s system began breaking down.
Keep in mind they had a terrific practice. The docs liked each other and were pleased with the group leader, were highly regarded by hospital executives and other doctors, and had a growing patient volume.
Yet, the partners were unhappy they weren’t seeing extra compensation as a reward for buying into the practice with the money, time, and effort they invested.
Despite being a desirable practice in nearly every respect, new doctors were choosing to forgo partnership status. These things were creating significant morale issues that threatened the ongoing success of the group.
So why did these problems arise?
Case No. 2
Later in 2006, I worked with a different private-practice hospitalist group out West. Their practice had been started by, and was still owned by, a “parent” medical group. As the hospitalist practice grew, everyone (hospitalists and non-hospitalist doctors in the group) agreed it made sense to have the hospitalist practice separate into its own distinct corporation. Like the practice in the first case, all parties had high regard for one another.
The problem was the non-hospitalists who invested the time and energy to start the hospitalist practice wanted the departing hospitalists to compensate the larger group.
The hospitalists could understand why the other doctors proposed a buyout but wondered what the hospitalists would get in return for paying it. The answer seemed to be not much. They weren’t confident they could recoup their investment by having future hospitalists buy in to the practice (proposing this had scared off more than one recruit), or by selling the practice to another party.
Assess Your Value
The problems faced by both these practices are a result of uncertainty about what their practices are worth.
In the first case, doctors who had the opportunity to buy into the practice were choosing not to because they believed they weren’t going to get anything in return (and had the added burden of putting themselves on the schedule more often to cover open shifts).
Likewise, in the second case the hospitalists agreed it seemed reasonable to pay the other doctors in the parent group to go out on their own. But the hospitalists worried they would never be able to recoup that money by selling shares of the practice to new partner hospitalists or selling the whole group to another entity.
It’s tricky to value any medical practice. A common approach is to put a price on tangible assets owned by the practice (e.g., buildings and equipment like computers and lab apparatus, and the accounts receivable), and the patient base (or good will) the practice has developed.
It isn’t too difficult to come up with a value for tangible assets, and most hospitalist practices have little or nothing in this category (the only hard assets I can think of that I own are my pager, stethoscope, and a couple of lab coats I never wear). Patient lists and good will are particularly difficult to place a value on. Even for a primary care practice with thousands of patient charts, there is no guarantee patients will agree to transfer their care to a purchasing doctor.
For most any kind of medical practice, including a hospitalist group, good will mainly is a function of the referral relationships doctors have developed that ensure a steady flow of patients. Since a steady flow of patients is not a problem for most hospitalist practices (too many patients is more common than too few) the value of that referral stream may not be much.
Another asset many hospitalist practices own is their contract(s) with sponsoring organizations (usually hospitals, but sometimes health plans). They provide for supplemental payments over and above professional fees the practice collects.
This is often a hospitalist practice’s most valuable asset, and it may be worth investing money to acquire. It’s the primary reason large hospitalist staffing companies are willing to pay to acquire local hospitalist practices.
Usually these contracts cannot automatically be assigned to another party without the hospital’s consent. Most hospitals’ loyalty lies with the hospitalists who provide their coverage, not with the company that may hold the contract. For example, with the hospitalists in the second case, their hospital would have been willing to immediately sign a new contract with their spin-off group to maintain their existing hospitalist coverage. The parent group’s hospital contract wasn’t worth acquiring.
All this suggests hospitalist practices may not have much monetary value. That is, an outside party probably wouldn’t pay much to buy your practice. I think this is true for the two practices I describe above. For practices like these, it is probably best to avoid having a buy-in to achieve partner status, and not diverting some practice revenue that would otherwise be used to pay salaries into a “profit” pool from which distributions are made to partners/owners periodically.
Practices Worth A Lot
I’m aware my comments might seem insulting to a group of hospitalists who have worked long and hard for several years to build what they think is a great practice. Surely it’s worth something.
Maybe your practice really does have significant value over and above the salaries the doctors earn. Perhaps you have developed proprietary operational processes that are particularly valuable and would be difficult for others to replicate without knowing your “trade secrets.” These could include things such as particularly effective ways to document, code, and collect professional fees; methods to enhance hospitalist efficiency and/or quality; unusually effective recruitment strategies; or even the ability to negotiate highly favorable contracts with payers.
Even if your practice does have remarkably effective proprietary components, you still would have to convince a buyer these valuable assets would persist after the change in ownership and the departure of key individuals. For example, you might have the best practice in the country because you’ve been able to recruit the best doctors. If I buy your practice and those excellent doctors leave, I’ve lost the unique asset that was key to the practice’s value.
Clearly there is room for a lot of debate about hospitalist practice valuation. (Search the Internet for “medical practice valuation” for a number of good articles about this.) There are many practice management companies that rely on the notion that their ideas and operations provide greater value than other practices. One such company, IPC, had a successful initial public offering of stock that found a marketplace willing to pay for its perceived value. But keep in mind that this company has many practices in many states, and much of the value may lie in the fact that the value of the whole is greater than the sum of its parts. So, unless your practice is huge and has sites in many states, I don’t think you can assume IPC’s public offering means your practice might have a similar value.
Think critically about your practice. Challenge yourself to think about what you would pay for your practice and what you would get in return. If you have a hard time coming up with clear reasons your practice has significant intangible value, you should probably avoid structuring a buy-in for new doctors or a buy-out for departing doctors. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
The issue of practice valuation is a sensitive one. Some hospitalist practices might have significant monetary value, which could make it reasonable to ask new doctors to buy in or enable selling the practice for a profit. Still, it’s risky to assume this is the case for your practice.
Let’s examine the issue using a pair of situations I encountered not long ago. I have changed some details of the practices to more clearly illustrate a point and conceal which practices I’m describing. Both situations would have gone smoother if it was clear what the hospitalist practice was worth. But how do you assess that value?
Case No. 1
During a couple of days in 2006, I consulted with a high-performing private practice hospitalist group on the East Coast. The group was led by one of the most energetic and thoughtful leaders I’ve encountered.
Like many other private practice groups, they divided physician members of the practice into partners and non-partners (sometimes referred to as shareholder and non-shareholders in the corporation). A hospitalist who had been a full-time member of the practice for a specified period of time (two years in this case) was eligible to become partner.
This entailed a “buy-in” requiring the doctor to pay money to the practice (usually the doctor would pay using a loan from the practice, which was repaid through deductions from his/her paycheck).
For this practice, the principal benefits of partner status were having a vote in group decisions (non-partners couldn’t vote) and receiving a portion of the distribution of all corporate profits each year. These profits came from two sources:
- Money remaining after all salaries and overhead were paid; and
- Buy-in money received by the practice.
Because the partners had this “upside potential” they agreed they would cover any staff shortages by working extra shifts instead of the non-partners.
Setting things up with a buy-in to achieve partner/shareholder status seemed to make a lot of sense. After all, it is the way nearly all private-practice medical groups in other specialties are structured.
Problems soon arose when they realized there wasn’t significant “profit” available unless there happened to be two or three doctors buying into the practice in a given year.
So, the partners became disenchanted because they shouldered the burden of covering any extra shifts but didn’t get a significant profit distribution in most years. Non-partners who became eligible for partnership were choosing not to buy in because it seemed like more responsibility without more income. The group’s system began breaking down.
Keep in mind they had a terrific practice. The docs liked each other and were pleased with the group leader, were highly regarded by hospital executives and other doctors, and had a growing patient volume.
Yet, the partners were unhappy they weren’t seeing extra compensation as a reward for buying into the practice with the money, time, and effort they invested.
Despite being a desirable practice in nearly every respect, new doctors were choosing to forgo partnership status. These things were creating significant morale issues that threatened the ongoing success of the group.
So why did these problems arise?
Case No. 2
Later in 2006, I worked with a different private-practice hospitalist group out West. Their practice had been started by, and was still owned by, a “parent” medical group. As the hospitalist practice grew, everyone (hospitalists and non-hospitalist doctors in the group) agreed it made sense to have the hospitalist practice separate into its own distinct corporation. Like the practice in the first case, all parties had high regard for one another.
The problem was the non-hospitalists who invested the time and energy to start the hospitalist practice wanted the departing hospitalists to compensate the larger group.
The hospitalists could understand why the other doctors proposed a buyout but wondered what the hospitalists would get in return for paying it. The answer seemed to be not much. They weren’t confident they could recoup their investment by having future hospitalists buy in to the practice (proposing this had scared off more than one recruit), or by selling the practice to another party.
Assess Your Value
The problems faced by both these practices are a result of uncertainty about what their practices are worth.
In the first case, doctors who had the opportunity to buy into the practice were choosing not to because they believed they weren’t going to get anything in return (and had the added burden of putting themselves on the schedule more often to cover open shifts).
Likewise, in the second case the hospitalists agreed it seemed reasonable to pay the other doctors in the parent group to go out on their own. But the hospitalists worried they would never be able to recoup that money by selling shares of the practice to new partner hospitalists or selling the whole group to another entity.
It’s tricky to value any medical practice. A common approach is to put a price on tangible assets owned by the practice (e.g., buildings and equipment like computers and lab apparatus, and the accounts receivable), and the patient base (or good will) the practice has developed.
It isn’t too difficult to come up with a value for tangible assets, and most hospitalist practices have little or nothing in this category (the only hard assets I can think of that I own are my pager, stethoscope, and a couple of lab coats I never wear). Patient lists and good will are particularly difficult to place a value on. Even for a primary care practice with thousands of patient charts, there is no guarantee patients will agree to transfer their care to a purchasing doctor.
For most any kind of medical practice, including a hospitalist group, good will mainly is a function of the referral relationships doctors have developed that ensure a steady flow of patients. Since a steady flow of patients is not a problem for most hospitalist practices (too many patients is more common than too few) the value of that referral stream may not be much.
Another asset many hospitalist practices own is their contract(s) with sponsoring organizations (usually hospitals, but sometimes health plans). They provide for supplemental payments over and above professional fees the practice collects.
This is often a hospitalist practice’s most valuable asset, and it may be worth investing money to acquire. It’s the primary reason large hospitalist staffing companies are willing to pay to acquire local hospitalist practices.
Usually these contracts cannot automatically be assigned to another party without the hospital’s consent. Most hospitals’ loyalty lies with the hospitalists who provide their coverage, not with the company that may hold the contract. For example, with the hospitalists in the second case, their hospital would have been willing to immediately sign a new contract with their spin-off group to maintain their existing hospitalist coverage. The parent group’s hospital contract wasn’t worth acquiring.
All this suggests hospitalist practices may not have much monetary value. That is, an outside party probably wouldn’t pay much to buy your practice. I think this is true for the two practices I describe above. For practices like these, it is probably best to avoid having a buy-in to achieve partner status, and not diverting some practice revenue that would otherwise be used to pay salaries into a “profit” pool from which distributions are made to partners/owners periodically.
Practices Worth A Lot
I’m aware my comments might seem insulting to a group of hospitalists who have worked long and hard for several years to build what they think is a great practice. Surely it’s worth something.
Maybe your practice really does have significant value over and above the salaries the doctors earn. Perhaps you have developed proprietary operational processes that are particularly valuable and would be difficult for others to replicate without knowing your “trade secrets.” These could include things such as particularly effective ways to document, code, and collect professional fees; methods to enhance hospitalist efficiency and/or quality; unusually effective recruitment strategies; or even the ability to negotiate highly favorable contracts with payers.
Even if your practice does have remarkably effective proprietary components, you still would have to convince a buyer these valuable assets would persist after the change in ownership and the departure of key individuals. For example, you might have the best practice in the country because you’ve been able to recruit the best doctors. If I buy your practice and those excellent doctors leave, I’ve lost the unique asset that was key to the practice’s value.
Clearly there is room for a lot of debate about hospitalist practice valuation. (Search the Internet for “medical practice valuation” for a number of good articles about this.) There are many practice management companies that rely on the notion that their ideas and operations provide greater value than other practices. One such company, IPC, had a successful initial public offering of stock that found a marketplace willing to pay for its perceived value. But keep in mind that this company has many practices in many states, and much of the value may lie in the fact that the value of the whole is greater than the sum of its parts. So, unless your practice is huge and has sites in many states, I don’t think you can assume IPC’s public offering means your practice might have a similar value.
Think critically about your practice. Challenge yourself to think about what you would pay for your practice and what you would get in return. If you have a hard time coming up with clear reasons your practice has significant intangible value, you should probably avoid structuring a buy-in for new doctors or a buy-out for departing doctors. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
The issue of practice valuation is a sensitive one. Some hospitalist practices might have significant monetary value, which could make it reasonable to ask new doctors to buy in or enable selling the practice for a profit. Still, it’s risky to assume this is the case for your practice.
Let’s examine the issue using a pair of situations I encountered not long ago. I have changed some details of the practices to more clearly illustrate a point and conceal which practices I’m describing. Both situations would have gone smoother if it was clear what the hospitalist practice was worth. But how do you assess that value?
Case No. 1
During a couple of days in 2006, I consulted with a high-performing private practice hospitalist group on the East Coast. The group was led by one of the most energetic and thoughtful leaders I’ve encountered.
Like many other private practice groups, they divided physician members of the practice into partners and non-partners (sometimes referred to as shareholder and non-shareholders in the corporation). A hospitalist who had been a full-time member of the practice for a specified period of time (two years in this case) was eligible to become partner.
This entailed a “buy-in” requiring the doctor to pay money to the practice (usually the doctor would pay using a loan from the practice, which was repaid through deductions from his/her paycheck).
For this practice, the principal benefits of partner status were having a vote in group decisions (non-partners couldn’t vote) and receiving a portion of the distribution of all corporate profits each year. These profits came from two sources:
- Money remaining after all salaries and overhead were paid; and
- Buy-in money received by the practice.
Because the partners had this “upside potential” they agreed they would cover any staff shortages by working extra shifts instead of the non-partners.
Setting things up with a buy-in to achieve partner/shareholder status seemed to make a lot of sense. After all, it is the way nearly all private-practice medical groups in other specialties are structured.
Problems soon arose when they realized there wasn’t significant “profit” available unless there happened to be two or three doctors buying into the practice in a given year.
So, the partners became disenchanted because they shouldered the burden of covering any extra shifts but didn’t get a significant profit distribution in most years. Non-partners who became eligible for partnership were choosing not to buy in because it seemed like more responsibility without more income. The group’s system began breaking down.
Keep in mind they had a terrific practice. The docs liked each other and were pleased with the group leader, were highly regarded by hospital executives and other doctors, and had a growing patient volume.
Yet, the partners were unhappy they weren’t seeing extra compensation as a reward for buying into the practice with the money, time, and effort they invested.
Despite being a desirable practice in nearly every respect, new doctors were choosing to forgo partnership status. These things were creating significant morale issues that threatened the ongoing success of the group.
So why did these problems arise?
Case No. 2
Later in 2006, I worked with a different private-practice hospitalist group out West. Their practice had been started by, and was still owned by, a “parent” medical group. As the hospitalist practice grew, everyone (hospitalists and non-hospitalist doctors in the group) agreed it made sense to have the hospitalist practice separate into its own distinct corporation. Like the practice in the first case, all parties had high regard for one another.
The problem was the non-hospitalists who invested the time and energy to start the hospitalist practice wanted the departing hospitalists to compensate the larger group.
The hospitalists could understand why the other doctors proposed a buyout but wondered what the hospitalists would get in return for paying it. The answer seemed to be not much. They weren’t confident they could recoup their investment by having future hospitalists buy in to the practice (proposing this had scared off more than one recruit), or by selling the practice to another party.
Assess Your Value
The problems faced by both these practices are a result of uncertainty about what their practices are worth.
In the first case, doctors who had the opportunity to buy into the practice were choosing not to because they believed they weren’t going to get anything in return (and had the added burden of putting themselves on the schedule more often to cover open shifts).
Likewise, in the second case the hospitalists agreed it seemed reasonable to pay the other doctors in the parent group to go out on their own. But the hospitalists worried they would never be able to recoup that money by selling shares of the practice to new partner hospitalists or selling the whole group to another entity.
It’s tricky to value any medical practice. A common approach is to put a price on tangible assets owned by the practice (e.g., buildings and equipment like computers and lab apparatus, and the accounts receivable), and the patient base (or good will) the practice has developed.
It isn’t too difficult to come up with a value for tangible assets, and most hospitalist practices have little or nothing in this category (the only hard assets I can think of that I own are my pager, stethoscope, and a couple of lab coats I never wear). Patient lists and good will are particularly difficult to place a value on. Even for a primary care practice with thousands of patient charts, there is no guarantee patients will agree to transfer their care to a purchasing doctor.
For most any kind of medical practice, including a hospitalist group, good will mainly is a function of the referral relationships doctors have developed that ensure a steady flow of patients. Since a steady flow of patients is not a problem for most hospitalist practices (too many patients is more common than too few) the value of that referral stream may not be much.
Another asset many hospitalist practices own is their contract(s) with sponsoring organizations (usually hospitals, but sometimes health plans). They provide for supplemental payments over and above professional fees the practice collects.
This is often a hospitalist practice’s most valuable asset, and it may be worth investing money to acquire. It’s the primary reason large hospitalist staffing companies are willing to pay to acquire local hospitalist practices.
Usually these contracts cannot automatically be assigned to another party without the hospital’s consent. Most hospitals’ loyalty lies with the hospitalists who provide their coverage, not with the company that may hold the contract. For example, with the hospitalists in the second case, their hospital would have been willing to immediately sign a new contract with their spin-off group to maintain their existing hospitalist coverage. The parent group’s hospital contract wasn’t worth acquiring.
All this suggests hospitalist practices may not have much monetary value. That is, an outside party probably wouldn’t pay much to buy your practice. I think this is true for the two practices I describe above. For practices like these, it is probably best to avoid having a buy-in to achieve partner status, and not diverting some practice revenue that would otherwise be used to pay salaries into a “profit” pool from which distributions are made to partners/owners periodically.
Practices Worth A Lot
I’m aware my comments might seem insulting to a group of hospitalists who have worked long and hard for several years to build what they think is a great practice. Surely it’s worth something.
Maybe your practice really does have significant value over and above the salaries the doctors earn. Perhaps you have developed proprietary operational processes that are particularly valuable and would be difficult for others to replicate without knowing your “trade secrets.” These could include things such as particularly effective ways to document, code, and collect professional fees; methods to enhance hospitalist efficiency and/or quality; unusually effective recruitment strategies; or even the ability to negotiate highly favorable contracts with payers.
Even if your practice does have remarkably effective proprietary components, you still would have to convince a buyer these valuable assets would persist after the change in ownership and the departure of key individuals. For example, you might have the best practice in the country because you’ve been able to recruit the best doctors. If I buy your practice and those excellent doctors leave, I’ve lost the unique asset that was key to the practice’s value.
Clearly there is room for a lot of debate about hospitalist practice valuation. (Search the Internet for “medical practice valuation” for a number of good articles about this.) There are many practice management companies that rely on the notion that their ideas and operations provide greater value than other practices. One such company, IPC, had a successful initial public offering of stock that found a marketplace willing to pay for its perceived value. But keep in mind that this company has many practices in many states, and much of the value may lie in the fact that the value of the whole is greater than the sum of its parts. So, unless your practice is huge and has sites in many states, I don’t think you can assume IPC’s public offering means your practice might have a similar value.
Think critically about your practice. Challenge yourself to think about what you would pay for your practice and what you would get in return. If you have a hard time coming up with clear reasons your practice has significant intangible value, you should probably avoid structuring a buy-in for new doctors or a buy-out for departing doctors. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Data Daze
As I write this column, our nation’s economy is looking pretty shaky. In early January, the labor market report showed a significant uptick in the unemployment rate. This led worried investors to sell stocks, and the Federal Reserve lowered the interest rate dramatically in response to the sudden fall in the stock market. Or at least that’s the version of events we’re being fed by most of the press.
Do investors overreact to job numbers? There is a lot of debate about the accuracy of job and unemployment statistics. Clearly they are valuable, but there are all kinds of problems with the way the labor surveys are conducted and the resulting data analyzed.
There may not be a better way to collect the data, so despite their flaws surveys may provide the best information on the labor market that we can get.
The real problem arises when investors—sort of like you and me but a lot richer—look at these data and fail to keep in mind all its strengths and weaknesses. There is a risk people will focus on a single number and overestimate its precision. This has been called the “salience bias.” Writing in The New Yorker, James Surowiecki says this salience bias can lead to “a hard-to-break feedback loop: The fact that traders act as if the jobs report were definitive makes it so. A little information can be a dangerous thing.”1
I discuss hospitalist survey data with people all the time. I’m struck by how often they seem misled by salience bias, among other things. With SHM’s release this month of its latest biannual survey of hospitalist productivity and compensation, now seems like a good time to discuss the strengths and weaknesses in the data—and cautions when interpreting it.
Understand the strengths and limitations of the survey. SHM’s “Bi-Annual Survey on the State of the Hospital Medicine Movement” is a self-reporting survey in which each practice leader (or his/her designee) completes the survey. The responses aren’t verified or audited, so some respondents might submit shoddy data. Perhaps a busy group leader might complete the survey from memory and estimate things like each doctor’s production of work-only relative value units (wRVUs). When I’ve looked at the raw data, I’ve wondered if some respondents are trying to “spin” their numbers higher or lower for a variety of reasons (e.g., to look unusually good or show how hard their doctors can work). And there may be a response bias: Those who think their practice is atypical might not respond to the survey.
This year, SHM worked to “scrub” the data. Outlier metrics were established for each question, and SHM staff followed up with the respondent to ensure he/she understood the question and provided accurate data. In fact, I completed the survey for the group I’m part of and got a call from a survey staffer questioning the productivity I reported for some members of the group (our nocturnists have lower wRVU productivity than others in the group—that is one reason they’re willing to work at night).
Remember that data are historical and should be “aged” to the time period you’re using it. The data in the 2008 SHM survey were collected from October through December.
Review the original questions asked in the survey. To make sense of the survey responses, you will need to clearly understand the question asked. Review the survey instrument and form your own conclusions about ways the questions were posed that might influence the responses. And don’t assume you understand what a particular term means—verify it by looking at the survey instrument. For example, I encounter a wide variety of opinions regarding what constitutes base salary, incentive pay, productivity compensation, bonus, and total compensation. The survey instrument spells these things out clearly.
It can be valuable to trend some data over successive surveys. For example, you may want to know the trend in the average hospitalist’s wRVU productivity over the past two surveys. You should look at the questions asked in both surveys to make sure there hasn’t been a change that could influence the responses. In the case of wRVUs you will need to understand how the January 2007 change in wRVUs values for many services provided by hospitalists was handled by the survey.
Pay attention to how data are lumped or split. Some data are appropriate for analysis of hospitalist groups, other data for individual hospitalists. If half of hospitalist groups use a shift-based schedule, that doesn’t mean half of individual hospitalists work such a schedule. Shift-based schedules are more common in larger groups, so even if half the groups in the country schedule by shifts, there may be 80% of individual hospitalists who use this schedule.
Salary incentives illustrate another way responses are lumped or split. As of the last survey (reported in 2006), most hospitalists had a variable component to their compensation—most often based on productivity or quality. There are relatively few ways hospitalists are paid on productivity (basing it on wRVUs is most common). But there are myriad quality incentives, based on things like Centers for Medicare and Medicaid Services core measures, and patient and referring physician satisfaction. Depending on how you aggregated these different categories in the 2006 survey, you might reach different conclusions about whether more hospitalists have productivity-based incentives or quality-based incentives (productivity was more common in the 2006 survey).
Drill down to respondent populations that most closely match your group. There is a real temptation to overemphasize the “headline” numbers in the survey like the average total salary for a hospitalist. Yet in many cases, it may be more useful to drill down to a population that matches your group. You might be most interested in compensation for hospital-employed hospitalists in non-teaching hospitals in the South (thereby excluding academicians and pediatric hospitalists from your comparison group). Just make sure to look at the resultant sample size (the “n”) reported for that subset of the data to make sure it is large enough to be meaningful.
Remember that the survey is not telling you what is right for your group. The survey simply describes a number of metrics relevant to hospitalist practice. It is not SHM’s position on the right compensation or productivity for a particular practice. It is the best source of national data regarding hospitalists. (See my column “Comp Close-Up” for a comparison between the SHM and Medical Group Management Association surveys [July 2007, p.73]). Things like the two other hospitalist practices in your town probably will have a lot more to do with influencing your group’s productivity and compensation metrics than any national data set.
While it’s tempting to reduce things to a single number (e.g., how much is the average hospitalist paid?) this is falling prey to salience bias. Try to grasp the stories behind the numbers by understanding the survey methods and looking at responses for different subsets of the survey population. And realize that the right or optimal compensation and productivity for a group might be quite different from the survey means and medians. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Surowiecki J. Running numbers. The New Yorker. January 21, 2008. Available online at www.newyorker.com/talk/financial/2008/01/21/080121ta_talk_surowiecki. Last accessed Feb. 7, 2008.
As I write this column, our nation’s economy is looking pretty shaky. In early January, the labor market report showed a significant uptick in the unemployment rate. This led worried investors to sell stocks, and the Federal Reserve lowered the interest rate dramatically in response to the sudden fall in the stock market. Or at least that’s the version of events we’re being fed by most of the press.
Do investors overreact to job numbers? There is a lot of debate about the accuracy of job and unemployment statistics. Clearly they are valuable, but there are all kinds of problems with the way the labor surveys are conducted and the resulting data analyzed.
There may not be a better way to collect the data, so despite their flaws surveys may provide the best information on the labor market that we can get.
The real problem arises when investors—sort of like you and me but a lot richer—look at these data and fail to keep in mind all its strengths and weaknesses. There is a risk people will focus on a single number and overestimate its precision. This has been called the “salience bias.” Writing in The New Yorker, James Surowiecki says this salience bias can lead to “a hard-to-break feedback loop: The fact that traders act as if the jobs report were definitive makes it so. A little information can be a dangerous thing.”1
I discuss hospitalist survey data with people all the time. I’m struck by how often they seem misled by salience bias, among other things. With SHM’s release this month of its latest biannual survey of hospitalist productivity and compensation, now seems like a good time to discuss the strengths and weaknesses in the data—and cautions when interpreting it.
Understand the strengths and limitations of the survey. SHM’s “Bi-Annual Survey on the State of the Hospital Medicine Movement” is a self-reporting survey in which each practice leader (or his/her designee) completes the survey. The responses aren’t verified or audited, so some respondents might submit shoddy data. Perhaps a busy group leader might complete the survey from memory and estimate things like each doctor’s production of work-only relative value units (wRVUs). When I’ve looked at the raw data, I’ve wondered if some respondents are trying to “spin” their numbers higher or lower for a variety of reasons (e.g., to look unusually good or show how hard their doctors can work). And there may be a response bias: Those who think their practice is atypical might not respond to the survey.
This year, SHM worked to “scrub” the data. Outlier metrics were established for each question, and SHM staff followed up with the respondent to ensure he/she understood the question and provided accurate data. In fact, I completed the survey for the group I’m part of and got a call from a survey staffer questioning the productivity I reported for some members of the group (our nocturnists have lower wRVU productivity than others in the group—that is one reason they’re willing to work at night).
Remember that data are historical and should be “aged” to the time period you’re using it. The data in the 2008 SHM survey were collected from October through December.
Review the original questions asked in the survey. To make sense of the survey responses, you will need to clearly understand the question asked. Review the survey instrument and form your own conclusions about ways the questions were posed that might influence the responses. And don’t assume you understand what a particular term means—verify it by looking at the survey instrument. For example, I encounter a wide variety of opinions regarding what constitutes base salary, incentive pay, productivity compensation, bonus, and total compensation. The survey instrument spells these things out clearly.
It can be valuable to trend some data over successive surveys. For example, you may want to know the trend in the average hospitalist’s wRVU productivity over the past two surveys. You should look at the questions asked in both surveys to make sure there hasn’t been a change that could influence the responses. In the case of wRVUs you will need to understand how the January 2007 change in wRVUs values for many services provided by hospitalists was handled by the survey.
Pay attention to how data are lumped or split. Some data are appropriate for analysis of hospitalist groups, other data for individual hospitalists. If half of hospitalist groups use a shift-based schedule, that doesn’t mean half of individual hospitalists work such a schedule. Shift-based schedules are more common in larger groups, so even if half the groups in the country schedule by shifts, there may be 80% of individual hospitalists who use this schedule.
Salary incentives illustrate another way responses are lumped or split. As of the last survey (reported in 2006), most hospitalists had a variable component to their compensation—most often based on productivity or quality. There are relatively few ways hospitalists are paid on productivity (basing it on wRVUs is most common). But there are myriad quality incentives, based on things like Centers for Medicare and Medicaid Services core measures, and patient and referring physician satisfaction. Depending on how you aggregated these different categories in the 2006 survey, you might reach different conclusions about whether more hospitalists have productivity-based incentives or quality-based incentives (productivity was more common in the 2006 survey).
Drill down to respondent populations that most closely match your group. There is a real temptation to overemphasize the “headline” numbers in the survey like the average total salary for a hospitalist. Yet in many cases, it may be more useful to drill down to a population that matches your group. You might be most interested in compensation for hospital-employed hospitalists in non-teaching hospitals in the South (thereby excluding academicians and pediatric hospitalists from your comparison group). Just make sure to look at the resultant sample size (the “n”) reported for that subset of the data to make sure it is large enough to be meaningful.
Remember that the survey is not telling you what is right for your group. The survey simply describes a number of metrics relevant to hospitalist practice. It is not SHM’s position on the right compensation or productivity for a particular practice. It is the best source of national data regarding hospitalists. (See my column “Comp Close-Up” for a comparison between the SHM and Medical Group Management Association surveys [July 2007, p.73]). Things like the two other hospitalist practices in your town probably will have a lot more to do with influencing your group’s productivity and compensation metrics than any national data set.
While it’s tempting to reduce things to a single number (e.g., how much is the average hospitalist paid?) this is falling prey to salience bias. Try to grasp the stories behind the numbers by understanding the survey methods and looking at responses for different subsets of the survey population. And realize that the right or optimal compensation and productivity for a group might be quite different from the survey means and medians. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Surowiecki J. Running numbers. The New Yorker. January 21, 2008. Available online at www.newyorker.com/talk/financial/2008/01/21/080121ta_talk_surowiecki. Last accessed Feb. 7, 2008.
As I write this column, our nation’s economy is looking pretty shaky. In early January, the labor market report showed a significant uptick in the unemployment rate. This led worried investors to sell stocks, and the Federal Reserve lowered the interest rate dramatically in response to the sudden fall in the stock market. Or at least that’s the version of events we’re being fed by most of the press.
Do investors overreact to job numbers? There is a lot of debate about the accuracy of job and unemployment statistics. Clearly they are valuable, but there are all kinds of problems with the way the labor surveys are conducted and the resulting data analyzed.
There may not be a better way to collect the data, so despite their flaws surveys may provide the best information on the labor market that we can get.
The real problem arises when investors—sort of like you and me but a lot richer—look at these data and fail to keep in mind all its strengths and weaknesses. There is a risk people will focus on a single number and overestimate its precision. This has been called the “salience bias.” Writing in The New Yorker, James Surowiecki says this salience bias can lead to “a hard-to-break feedback loop: The fact that traders act as if the jobs report were definitive makes it so. A little information can be a dangerous thing.”1
I discuss hospitalist survey data with people all the time. I’m struck by how often they seem misled by salience bias, among other things. With SHM’s release this month of its latest biannual survey of hospitalist productivity and compensation, now seems like a good time to discuss the strengths and weaknesses in the data—and cautions when interpreting it.
Understand the strengths and limitations of the survey. SHM’s “Bi-Annual Survey on the State of the Hospital Medicine Movement” is a self-reporting survey in which each practice leader (or his/her designee) completes the survey. The responses aren’t verified or audited, so some respondents might submit shoddy data. Perhaps a busy group leader might complete the survey from memory and estimate things like each doctor’s production of work-only relative value units (wRVUs). When I’ve looked at the raw data, I’ve wondered if some respondents are trying to “spin” their numbers higher or lower for a variety of reasons (e.g., to look unusually good or show how hard their doctors can work). And there may be a response bias: Those who think their practice is atypical might not respond to the survey.
This year, SHM worked to “scrub” the data. Outlier metrics were established for each question, and SHM staff followed up with the respondent to ensure he/she understood the question and provided accurate data. In fact, I completed the survey for the group I’m part of and got a call from a survey staffer questioning the productivity I reported for some members of the group (our nocturnists have lower wRVU productivity than others in the group—that is one reason they’re willing to work at night).
Remember that data are historical and should be “aged” to the time period you’re using it. The data in the 2008 SHM survey were collected from October through December.
Review the original questions asked in the survey. To make sense of the survey responses, you will need to clearly understand the question asked. Review the survey instrument and form your own conclusions about ways the questions were posed that might influence the responses. And don’t assume you understand what a particular term means—verify it by looking at the survey instrument. For example, I encounter a wide variety of opinions regarding what constitutes base salary, incentive pay, productivity compensation, bonus, and total compensation. The survey instrument spells these things out clearly.
It can be valuable to trend some data over successive surveys. For example, you may want to know the trend in the average hospitalist’s wRVU productivity over the past two surveys. You should look at the questions asked in both surveys to make sure there hasn’t been a change that could influence the responses. In the case of wRVUs you will need to understand how the January 2007 change in wRVUs values for many services provided by hospitalists was handled by the survey.
Pay attention to how data are lumped or split. Some data are appropriate for analysis of hospitalist groups, other data for individual hospitalists. If half of hospitalist groups use a shift-based schedule, that doesn’t mean half of individual hospitalists work such a schedule. Shift-based schedules are more common in larger groups, so even if half the groups in the country schedule by shifts, there may be 80% of individual hospitalists who use this schedule.
Salary incentives illustrate another way responses are lumped or split. As of the last survey (reported in 2006), most hospitalists had a variable component to their compensation—most often based on productivity or quality. There are relatively few ways hospitalists are paid on productivity (basing it on wRVUs is most common). But there are myriad quality incentives, based on things like Centers for Medicare and Medicaid Services core measures, and patient and referring physician satisfaction. Depending on how you aggregated these different categories in the 2006 survey, you might reach different conclusions about whether more hospitalists have productivity-based incentives or quality-based incentives (productivity was more common in the 2006 survey).
Drill down to respondent populations that most closely match your group. There is a real temptation to overemphasize the “headline” numbers in the survey like the average total salary for a hospitalist. Yet in many cases, it may be more useful to drill down to a population that matches your group. You might be most interested in compensation for hospital-employed hospitalists in non-teaching hospitals in the South (thereby excluding academicians and pediatric hospitalists from your comparison group). Just make sure to look at the resultant sample size (the “n”) reported for that subset of the data to make sure it is large enough to be meaningful.
Remember that the survey is not telling you what is right for your group. The survey simply describes a number of metrics relevant to hospitalist practice. It is not SHM’s position on the right compensation or productivity for a particular practice. It is the best source of national data regarding hospitalists. (See my column “Comp Close-Up” for a comparison between the SHM and Medical Group Management Association surveys [July 2007, p.73]). Things like the two other hospitalist practices in your town probably will have a lot more to do with influencing your group’s productivity and compensation metrics than any national data set.
While it’s tempting to reduce things to a single number (e.g., how much is the average hospitalist paid?) this is falling prey to salience bias. Try to grasp the stories behind the numbers by understanding the survey methods and looking at responses for different subsets of the survey population. And realize that the right or optimal compensation and productivity for a group might be quite different from the survey means and medians. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Surowiecki J. Running numbers. The New Yorker. January 21, 2008. Available online at www.newyorker.com/talk/financial/2008/01/21/080121ta_talk_surowiecki. Last accessed Feb. 7, 2008.
Nocturnal Economics
In my previous column, I reviewed different strategies for providing hospitalist practice night coverage based on the size of the group (February 2008, p. 61). I suggested that dedicated nocturnists are a valuable though expensive asset that any practice larger than about six to eight full-time equivalents (FTE) should consider.
This month, I offer additional thoughts about compensation for nocturnists. I’ll demonstrate why adding dedicated night coverage—in which the doctor working at night doesn’t work during the daytime hours the day before or after the night shift—may not increase practice workload significantly.
What follows is adapted from a new book I co-wrote with Joe Miller, senior vice president of SHM, and Win Whitcomb, MD, a hospitalist at Mercy Medical Center in Springfield, Mass., and co-founder of SHM.1
Compensation
If all hospitalists provide an equal amount of night coverage in rotation (e.g., each member of a four-person group works 61 nights annually), it’s not necessary to adjust the compensation scheme to reflect night work. A night-shift differential in this situation will not influence a doctor’s annual income relative to that of his partner hospitalists.
However, if the hospitalist program seeks more flexibility, it may be advisable to pay more for a night of work than a day of work. Under this scheme, hospitalists may trade day and night work among themselves, leading to enhanced satisfaction. For example, Dr. McCartney is willing to work some of Dr. Lennon’s nights because of the income benefit. Dr. Lennon may or may not work some of Dr. McCartney’s days in return.
If the practice has one or more dedicated nocturnists, they will need to realize some benefit to working only nights. This benefit can take many forms:
- The night hospitalist works less often than day doctors (e.g., day doctors work 220 days annually, night doctors work 182);
- The night hospitalist has a lighter patient load (e.g., a night hospitalist in a small practice typically sleeps three to six hours per night shift while the day doctors typically work a busy eight-to-12-hour shift);
- The night doctor earns more than the day doctors; or
- The night doctor has a higher priority in time-off scheduling.
It is common to combine these benefits. For example a night hospitalist might work less often than day doctors, have a lighter patient load, and earn the same annual income. Anecdotal experience shows that having more income or fewer workdays than day doctors is valued more than a reduced patient load.
For most practices, compensating hospitalists based significantly or entirely on their production can be a good idea but might be problematic for a night doctor. It could lead the night doctor to encourage marginal admissions, some of whom would need to be discharged by the daytime hospitalists hours later. In effect, the night hospitalist could say: “I’ll admit anyone I can get my hands on because my income will increase. I’ll leave it for the day doctors to sort out what to do with all these patients tomorrow.”
An Example
A traditional system of night call (such as pager call from home while also working days) is usually cheaper than dedicated night shifts. And while there are many benefits to having dedicated night shifts, increased patient capacity may not be one of them. Consider the following example:
- On any given day, a five-FTE hospitalist practice has three doctors working, one of whom will be on-call that night by pager;
- That will mean 219 worked days per year for each doctor, one-third of which (73) will be on-call. Each hospitalist gets 146 days off per year;
- The practice decides to switch to dedicated night shifts in which the doctors do not work the day before or after a night shift. The practice wants to retain the 146 days off for each hospitalist. This new coverage arrangement is equivalent to adding 365 shifts annually (one for each night); and
- This will require an additional 1.67 FTE hospitalists (1.67 hospitalists at 219 shifts/year=365).
In this example, by switching from on-call coverage to on-site coverage, the practice increased from five FTEs to 6.67 FTEs. If the daytime work was already enough to keep all three doctors busy, adding 1.67 FTEs for dedicated night shifts may not increase practice productivity or revenue significantly. The practice looks much less productive per FTE (6.67 FTEs are now seeing the volume previously handled by five FTEs) and much costlier.
Changing from traditional night call to dedicated night coverage can be expensive because it may require adding staff yet doesn’t usually increase practice capacity significantly. But it offers other benefits such as those listed in Table 1 (see p. TK). Some practices find they must provide dedicated night coverage to recruit hospitalists. Other institutions choose to support it believing it leads to more timely, efficient, higher-quality care. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Miller J, Nelson J, Whitcomb W. Hospitalists: A Guide to Building and Sustaining a Successful Program. Chicago:Health Administration Press;2007:149-150.
In my previous column, I reviewed different strategies for providing hospitalist practice night coverage based on the size of the group (February 2008, p. 61). I suggested that dedicated nocturnists are a valuable though expensive asset that any practice larger than about six to eight full-time equivalents (FTE) should consider.
This month, I offer additional thoughts about compensation for nocturnists. I’ll demonstrate why adding dedicated night coverage—in which the doctor working at night doesn’t work during the daytime hours the day before or after the night shift—may not increase practice workload significantly.
What follows is adapted from a new book I co-wrote with Joe Miller, senior vice president of SHM, and Win Whitcomb, MD, a hospitalist at Mercy Medical Center in Springfield, Mass., and co-founder of SHM.1
Compensation
If all hospitalists provide an equal amount of night coverage in rotation (e.g., each member of a four-person group works 61 nights annually), it’s not necessary to adjust the compensation scheme to reflect night work. A night-shift differential in this situation will not influence a doctor’s annual income relative to that of his partner hospitalists.
However, if the hospitalist program seeks more flexibility, it may be advisable to pay more for a night of work than a day of work. Under this scheme, hospitalists may trade day and night work among themselves, leading to enhanced satisfaction. For example, Dr. McCartney is willing to work some of Dr. Lennon’s nights because of the income benefit. Dr. Lennon may or may not work some of Dr. McCartney’s days in return.
If the practice has one or more dedicated nocturnists, they will need to realize some benefit to working only nights. This benefit can take many forms:
- The night hospitalist works less often than day doctors (e.g., day doctors work 220 days annually, night doctors work 182);
- The night hospitalist has a lighter patient load (e.g., a night hospitalist in a small practice typically sleeps three to six hours per night shift while the day doctors typically work a busy eight-to-12-hour shift);
- The night doctor earns more than the day doctors; or
- The night doctor has a higher priority in time-off scheduling.
It is common to combine these benefits. For example a night hospitalist might work less often than day doctors, have a lighter patient load, and earn the same annual income. Anecdotal experience shows that having more income or fewer workdays than day doctors is valued more than a reduced patient load.
For most practices, compensating hospitalists based significantly or entirely on their production can be a good idea but might be problematic for a night doctor. It could lead the night doctor to encourage marginal admissions, some of whom would need to be discharged by the daytime hospitalists hours later. In effect, the night hospitalist could say: “I’ll admit anyone I can get my hands on because my income will increase. I’ll leave it for the day doctors to sort out what to do with all these patients tomorrow.”
An Example
A traditional system of night call (such as pager call from home while also working days) is usually cheaper than dedicated night shifts. And while there are many benefits to having dedicated night shifts, increased patient capacity may not be one of them. Consider the following example:
- On any given day, a five-FTE hospitalist practice has three doctors working, one of whom will be on-call that night by pager;
- That will mean 219 worked days per year for each doctor, one-third of which (73) will be on-call. Each hospitalist gets 146 days off per year;
- The practice decides to switch to dedicated night shifts in which the doctors do not work the day before or after a night shift. The practice wants to retain the 146 days off for each hospitalist. This new coverage arrangement is equivalent to adding 365 shifts annually (one for each night); and
- This will require an additional 1.67 FTE hospitalists (1.67 hospitalists at 219 shifts/year=365).
In this example, by switching from on-call coverage to on-site coverage, the practice increased from five FTEs to 6.67 FTEs. If the daytime work was already enough to keep all three doctors busy, adding 1.67 FTEs for dedicated night shifts may not increase practice productivity or revenue significantly. The practice looks much less productive per FTE (6.67 FTEs are now seeing the volume previously handled by five FTEs) and much costlier.
Changing from traditional night call to dedicated night coverage can be expensive because it may require adding staff yet doesn’t usually increase practice capacity significantly. But it offers other benefits such as those listed in Table 1 (see p. TK). Some practices find they must provide dedicated night coverage to recruit hospitalists. Other institutions choose to support it believing it leads to more timely, efficient, higher-quality care. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Miller J, Nelson J, Whitcomb W. Hospitalists: A Guide to Building and Sustaining a Successful Program. Chicago:Health Administration Press;2007:149-150.
In my previous column, I reviewed different strategies for providing hospitalist practice night coverage based on the size of the group (February 2008, p. 61). I suggested that dedicated nocturnists are a valuable though expensive asset that any practice larger than about six to eight full-time equivalents (FTE) should consider.
This month, I offer additional thoughts about compensation for nocturnists. I’ll demonstrate why adding dedicated night coverage—in which the doctor working at night doesn’t work during the daytime hours the day before or after the night shift—may not increase practice workload significantly.
What follows is adapted from a new book I co-wrote with Joe Miller, senior vice president of SHM, and Win Whitcomb, MD, a hospitalist at Mercy Medical Center in Springfield, Mass., and co-founder of SHM.1
Compensation
If all hospitalists provide an equal amount of night coverage in rotation (e.g., each member of a four-person group works 61 nights annually), it’s not necessary to adjust the compensation scheme to reflect night work. A night-shift differential in this situation will not influence a doctor’s annual income relative to that of his partner hospitalists.
However, if the hospitalist program seeks more flexibility, it may be advisable to pay more for a night of work than a day of work. Under this scheme, hospitalists may trade day and night work among themselves, leading to enhanced satisfaction. For example, Dr. McCartney is willing to work some of Dr. Lennon’s nights because of the income benefit. Dr. Lennon may or may not work some of Dr. McCartney’s days in return.
If the practice has one or more dedicated nocturnists, they will need to realize some benefit to working only nights. This benefit can take many forms:
- The night hospitalist works less often than day doctors (e.g., day doctors work 220 days annually, night doctors work 182);
- The night hospitalist has a lighter patient load (e.g., a night hospitalist in a small practice typically sleeps three to six hours per night shift while the day doctors typically work a busy eight-to-12-hour shift);
- The night doctor earns more than the day doctors; or
- The night doctor has a higher priority in time-off scheduling.
It is common to combine these benefits. For example a night hospitalist might work less often than day doctors, have a lighter patient load, and earn the same annual income. Anecdotal experience shows that having more income or fewer workdays than day doctors is valued more than a reduced patient load.
For most practices, compensating hospitalists based significantly or entirely on their production can be a good idea but might be problematic for a night doctor. It could lead the night doctor to encourage marginal admissions, some of whom would need to be discharged by the daytime hospitalists hours later. In effect, the night hospitalist could say: “I’ll admit anyone I can get my hands on because my income will increase. I’ll leave it for the day doctors to sort out what to do with all these patients tomorrow.”
An Example
A traditional system of night call (such as pager call from home while also working days) is usually cheaper than dedicated night shifts. And while there are many benefits to having dedicated night shifts, increased patient capacity may not be one of them. Consider the following example:
- On any given day, a five-FTE hospitalist practice has three doctors working, one of whom will be on-call that night by pager;
- That will mean 219 worked days per year for each doctor, one-third of which (73) will be on-call. Each hospitalist gets 146 days off per year;
- The practice decides to switch to dedicated night shifts in which the doctors do not work the day before or after a night shift. The practice wants to retain the 146 days off for each hospitalist. This new coverage arrangement is equivalent to adding 365 shifts annually (one for each night); and
- This will require an additional 1.67 FTE hospitalists (1.67 hospitalists at 219 shifts/year=365).
In this example, by switching from on-call coverage to on-site coverage, the practice increased from five FTEs to 6.67 FTEs. If the daytime work was already enough to keep all three doctors busy, adding 1.67 FTEs for dedicated night shifts may not increase practice productivity or revenue significantly. The practice looks much less productive per FTE (6.67 FTEs are now seeing the volume previously handled by five FTEs) and much costlier.
Changing from traditional night call to dedicated night coverage can be expensive because it may require adding staff yet doesn’t usually increase practice capacity significantly. But it offers other benefits such as those listed in Table 1 (see p. TK). Some practices find they must provide dedicated night coverage to recruit hospitalists. Other institutions choose to support it believing it leads to more timely, efficient, higher-quality care. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program” course. This column represents his views and is not intended to reflect an official position of SHM.
Reference
- Miller J, Nelson J, Whitcomb W. Hospitalists: A Guide to Building and Sustaining a Successful Program. Chicago:Health Administration Press;2007:149-150.
Duty after Dark
A colleague once told me his theory that we are all born with the capacity to work a predetermined number of night shifts.
Think of this as a physiologic parameter similar to women being born with a fixed number of ova that can’t be replenished or increased after birth. While there seems to be significant variation in the number of night shifts each of us has to offer at the start of our career, it seems nearly everyone has a maximum number that is almost genetically determined. The only control we have is how quickly we use them up.
After careful consideration, I’ve realized I’ve used up all—or nearly all—my night shifts. And I have to admit it appears I was born with a fairly small number of night shifts in my genetic code.
The way a hospitalist practice addresses night work can be critical to whether it offers a sustainable career for hospitalists and good care for patients. Night coverage for many non-teaching practices usually evolves based on the size of the practice. For example:
Small practices (on-call from home):
- Fewer than six providers: Moonlighters (often local primary care physicians) are paid to help hospitalists with night coverage; or
- Six to eight providers: Hospitalists handle call from home with minimal or no help from non-hospitalist moonlighters.
Medium to large practices (in-house coverage):
- Eight to 10 providers: A hospitalist stays in-house all night. All members of the practice usually rotate responsibility for this coverage. The nocturnist on duty doesn’t work the day before or after a night shift; or
- More than 10 providers: Dedicated nocturnists might work only, or almost exclusively, at night.
There are many reasonable approaches to night coverage, and I don’t intend to suggest a given practice evolve through the above steps as it grows. It would be reasonable to skip some steps or use different size thresholds when moving from one system to another. In my experience, small practices nearly always provide night coverage on-call from home because of low night-shift productivity. As the night shift gets busier, they usually switch to in-house coverage.
I think every practice of more than about eight providers should seriously consider adding dedicated nocturnists. Most or all night shifts could be covered by the nocturnists, and the other docs in the practice wouldn’t have to rotate between day and night work. This can provide a substantial recruiting advantage and enhance career sustainability for the daytime hospitalists.
Where to Find Them
People often tell me they’d love to add nocturnists to their practice but can’t imagine where they could find people willing to do the work.
There are many potential nocturnists who might be available, including hospitalists in your practice. You just have to ensure they have a better “juice-to-squeeze ratio” than others in the practice. Usually this means offering them some combination of more pay and/or less work than others in your practice. Many people are attracted to hospitalist work because they want an interesting job that provides a lot of time off. By having nocturnists work less than others in the practice, they can have more time to pursue other interests.
There is no perfect way to gauge the appropriate adjustments in workload and compensation that will attract people to a nocturnist position in your practice. Estimate what seems equitable and see if any of your doctors would be willing to become a dedicated nocturnist. If none find the deal attractive enough to consider seriously, the chances are a new doctor you try to recruit will come to the same conclusion.
While a good “juice-to-squeeze ratio” is most important in attracting nocturnists, you could also consider a nocturnist recruitment ad that screams at the top “Never work another day in your life!” That might attract a lot of attention amid competing ads that describe the wonderful schools, quality of life, and proximity to shopping, lakes, and recreation other positions offer.
How to Pay Them
Where can you find the money to pay the nocturnist well for doing less work than his or her daytime counterparts? Most practices can appeal to their “sponsoring” hospital for more money to support this valuable component of the practice. If doctors in the practice want to be relieved of night work badly enough, they might give up some salary that can be put toward the nocturnist position.
Ask your hospital to match the contribution the doctors make. For example, each of the eight doctors in the practice might accept a $5,000 reduction in annual compensation to be relieved of all night shifts. That $40,000 could be matched 100% by the hospital for a total of $80,000. Each of two nocturnists hired by the group could split that $80,000 so they could be paid the same salary as the day doctors plus $40,000.
The Long View
Nearly everyone tires of working the night shift eventually—even if it does mean less work and more pay. Two to five years of working solely as a nocturnist might be as long as most people can do it, so plan for relatively frequent turnover. But I know of several hospitalists who have worked only at night for more than 10 years, provide excellent patient care, and seem quite happy to continue working nights. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
A colleague once told me his theory that we are all born with the capacity to work a predetermined number of night shifts.
Think of this as a physiologic parameter similar to women being born with a fixed number of ova that can’t be replenished or increased after birth. While there seems to be significant variation in the number of night shifts each of us has to offer at the start of our career, it seems nearly everyone has a maximum number that is almost genetically determined. The only control we have is how quickly we use them up.
After careful consideration, I’ve realized I’ve used up all—or nearly all—my night shifts. And I have to admit it appears I was born with a fairly small number of night shifts in my genetic code.
The way a hospitalist practice addresses night work can be critical to whether it offers a sustainable career for hospitalists and good care for patients. Night coverage for many non-teaching practices usually evolves based on the size of the practice. For example:
Small practices (on-call from home):
- Fewer than six providers: Moonlighters (often local primary care physicians) are paid to help hospitalists with night coverage; or
- Six to eight providers: Hospitalists handle call from home with minimal or no help from non-hospitalist moonlighters.
Medium to large practices (in-house coverage):
- Eight to 10 providers: A hospitalist stays in-house all night. All members of the practice usually rotate responsibility for this coverage. The nocturnist on duty doesn’t work the day before or after a night shift; or
- More than 10 providers: Dedicated nocturnists might work only, or almost exclusively, at night.
There are many reasonable approaches to night coverage, and I don’t intend to suggest a given practice evolve through the above steps as it grows. It would be reasonable to skip some steps or use different size thresholds when moving from one system to another. In my experience, small practices nearly always provide night coverage on-call from home because of low night-shift productivity. As the night shift gets busier, they usually switch to in-house coverage.
I think every practice of more than about eight providers should seriously consider adding dedicated nocturnists. Most or all night shifts could be covered by the nocturnists, and the other docs in the practice wouldn’t have to rotate between day and night work. This can provide a substantial recruiting advantage and enhance career sustainability for the daytime hospitalists.
Where to Find Them
People often tell me they’d love to add nocturnists to their practice but can’t imagine where they could find people willing to do the work.
There are many potential nocturnists who might be available, including hospitalists in your practice. You just have to ensure they have a better “juice-to-squeeze ratio” than others in the practice. Usually this means offering them some combination of more pay and/or less work than others in your practice. Many people are attracted to hospitalist work because they want an interesting job that provides a lot of time off. By having nocturnists work less than others in the practice, they can have more time to pursue other interests.
There is no perfect way to gauge the appropriate adjustments in workload and compensation that will attract people to a nocturnist position in your practice. Estimate what seems equitable and see if any of your doctors would be willing to become a dedicated nocturnist. If none find the deal attractive enough to consider seriously, the chances are a new doctor you try to recruit will come to the same conclusion.
While a good “juice-to-squeeze ratio” is most important in attracting nocturnists, you could also consider a nocturnist recruitment ad that screams at the top “Never work another day in your life!” That might attract a lot of attention amid competing ads that describe the wonderful schools, quality of life, and proximity to shopping, lakes, and recreation other positions offer.
How to Pay Them
Where can you find the money to pay the nocturnist well for doing less work than his or her daytime counterparts? Most practices can appeal to their “sponsoring” hospital for more money to support this valuable component of the practice. If doctors in the practice want to be relieved of night work badly enough, they might give up some salary that can be put toward the nocturnist position.
Ask your hospital to match the contribution the doctors make. For example, each of the eight doctors in the practice might accept a $5,000 reduction in annual compensation to be relieved of all night shifts. That $40,000 could be matched 100% by the hospital for a total of $80,000. Each of two nocturnists hired by the group could split that $80,000 so they could be paid the same salary as the day doctors plus $40,000.
The Long View
Nearly everyone tires of working the night shift eventually—even if it does mean less work and more pay. Two to five years of working solely as a nocturnist might be as long as most people can do it, so plan for relatively frequent turnover. But I know of several hospitalists who have worked only at night for more than 10 years, provide excellent patient care, and seem quite happy to continue working nights. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
A colleague once told me his theory that we are all born with the capacity to work a predetermined number of night shifts.
Think of this as a physiologic parameter similar to women being born with a fixed number of ova that can’t be replenished or increased after birth. While there seems to be significant variation in the number of night shifts each of us has to offer at the start of our career, it seems nearly everyone has a maximum number that is almost genetically determined. The only control we have is how quickly we use them up.
After careful consideration, I’ve realized I’ve used up all—or nearly all—my night shifts. And I have to admit it appears I was born with a fairly small number of night shifts in my genetic code.
The way a hospitalist practice addresses night work can be critical to whether it offers a sustainable career for hospitalists and good care for patients. Night coverage for many non-teaching practices usually evolves based on the size of the practice. For example:
Small practices (on-call from home):
- Fewer than six providers: Moonlighters (often local primary care physicians) are paid to help hospitalists with night coverage; or
- Six to eight providers: Hospitalists handle call from home with minimal or no help from non-hospitalist moonlighters.
Medium to large practices (in-house coverage):
- Eight to 10 providers: A hospitalist stays in-house all night. All members of the practice usually rotate responsibility for this coverage. The nocturnist on duty doesn’t work the day before or after a night shift; or
- More than 10 providers: Dedicated nocturnists might work only, or almost exclusively, at night.
There are many reasonable approaches to night coverage, and I don’t intend to suggest a given practice evolve through the above steps as it grows. It would be reasonable to skip some steps or use different size thresholds when moving from one system to another. In my experience, small practices nearly always provide night coverage on-call from home because of low night-shift productivity. As the night shift gets busier, they usually switch to in-house coverage.
I think every practice of more than about eight providers should seriously consider adding dedicated nocturnists. Most or all night shifts could be covered by the nocturnists, and the other docs in the practice wouldn’t have to rotate between day and night work. This can provide a substantial recruiting advantage and enhance career sustainability for the daytime hospitalists.
Where to Find Them
People often tell me they’d love to add nocturnists to their practice but can’t imagine where they could find people willing to do the work.
There are many potential nocturnists who might be available, including hospitalists in your practice. You just have to ensure they have a better “juice-to-squeeze ratio” than others in the practice. Usually this means offering them some combination of more pay and/or less work than others in your practice. Many people are attracted to hospitalist work because they want an interesting job that provides a lot of time off. By having nocturnists work less than others in the practice, they can have more time to pursue other interests.
There is no perfect way to gauge the appropriate adjustments in workload and compensation that will attract people to a nocturnist position in your practice. Estimate what seems equitable and see if any of your doctors would be willing to become a dedicated nocturnist. If none find the deal attractive enough to consider seriously, the chances are a new doctor you try to recruit will come to the same conclusion.
While a good “juice-to-squeeze ratio” is most important in attracting nocturnists, you could also consider a nocturnist recruitment ad that screams at the top “Never work another day in your life!” That might attract a lot of attention amid competing ads that describe the wonderful schools, quality of life, and proximity to shopping, lakes, and recreation other positions offer.
How to Pay Them
Where can you find the money to pay the nocturnist well for doing less work than his or her daytime counterparts? Most practices can appeal to their “sponsoring” hospital for more money to support this valuable component of the practice. If doctors in the practice want to be relieved of night work badly enough, they might give up some salary that can be put toward the nocturnist position.
Ask your hospital to match the contribution the doctors make. For example, each of the eight doctors in the practice might accept a $5,000 reduction in annual compensation to be relieved of all night shifts. That $40,000 could be matched 100% by the hospital for a total of $80,000. Each of two nocturnists hired by the group could split that $80,000 so they could be paid the same salary as the day doctors plus $40,000.
The Long View
Nearly everyone tires of working the night shift eventually—even if it does mean less work and more pay. Two to five years of working solely as a nocturnist might be as long as most people can do it, so plan for relatively frequent turnover. But I know of several hospitalists who have worked only at night for more than 10 years, provide excellent patient care, and seem quite happy to continue working nights. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
Avoid Bottlenecks
I enjoy hearing about the value hospitalists provide our healthcare system. These stories come from peer-reviewed research, magazine articles, local newspapers, and even the occasional blog. When I talk to hospitalists from around the country, they are often eager to tell of their success and how they made it happen.
Not as often, I also hear about problems that may be a result of the hospitalist model. I think any successful practice, and our field as a whole, must remain open to the weaknesses in the hospitalist model and work continuously to address them. Issues like disruptions in care and poor communication between hospitalists and outpatient providers get a reasonable amount of attention and seem to be on most groups’ radar screens. But there are some potential problems I don’t hear discussed often, and I’m not aware of any significant research that has been published or presented to analyze them. I’ll review two such potential problems here.
ED Throughput
Are hospitalists sometimes the cause of a bottleneck in the emergency department (ED)? Hospitalist practice is nearly always credited with improving throughput at a hospital, including in the ED. But many hospitalist practices could impede throughput by delaying patients from leaving the ED when there are multiple simultaneous admissions. Consider the following scenarios:
The pre-hospitalist era: It is 7:30 p.m. and the ED has four patients ready for hand-off to an admitting doctor. There are several primary care groups at the hospital, and each has a doctor on call. Of the four patients needing admission, two go to Dr. Emerson from group A, one goes to Dr. Lake from group B, and one to Dr. Palmer from group C. Because the on-call doctor for these groups is home, he/she provides admitting orders by phone and may or may not see the patient that night. Of course, waiting until the next day to see the patient can be risky. In many cases the ED would have admitting orders on all four patients quickly, say within 30 minutes, and can send the patients up to the floor as soon as the bed is ready.
The hospitalist era: Things can happen differently when hospitalists are at this hospital. All daytime hospitalists are typically signed out to a single night hospitalist (nocturnist) at 7:30 p.m. when the ED has four patients to admit. This solo nocturnist might show up almost immediately after being notified about the admissions by the ED doctor and promptly start seeing the first of the four admissions. But it might take him/her three or four hours or more to finish admitting all four patients. By that time there are probably additional admissions waiting. The ED might end up keeping each patient much longer than in the first scenario.
The difference in these two scenarios is the availability of several doctors to admit patients simultaneously in the pre-hospitalist era. These doctors may be replaced by a single hospitalist who admits patients one at a time.
A clear benefit of the hospitalist system described in this example is that patients are seen in person by the hospitalist at the time of admission, rather than admitted over the phone by the primary care physician (PCP) and perhaps not seen in person by the PCP until the next day. Yet this may come at a cost of creating a bottleneck that didn’t exist in the pre-hospitalist era.
Think about whether this is a common problem in your practice. Several strategies might help minimize this bottleneck. The most common approach in a practice of more than about 10 hospitalists is to ensure that there is more than one hospitalist available to admit patients until 10 or 11 p.m. when admission volume typically subsides. This has led some groups to develop an evening “swing shift” from late afternoon until about 10 or 11 p.m.
Large groups may decide to dedicate one hospitalist entirely to the ED from sometime in the morning (e.g., 11 a.m.) until near midnight. This person is available to respond quickly to ED admissions and consult with ED doctors regarding management and disposition of borderline cases. While ED staff are usually thrilled to have a hospitalist for the day, that hospitalist often will need to get help from other hospitalists when several patients must be admitted at the same time. And hospitalist-patient continuity suffers because the patient will nearly always need to be handed off to a different hospitalist for follow-up visits.
Marginal Admissions
Do hospitalists increase the number of marginal or potentially avoidable admissions?
The pre-hospitalist era: The ED physician sees a patient of Dr. Bernstein’s at 1 a.m. and is having trouble deciding whether admission is the best approach. The ED doctor gets Dr. Bernstein or his on-call partner, Dr. Copeland, on the phone and learns this patient is well known to the practice and can be seen in the outpatient office early the next morning. Admission is unnecessary.
The hospitalist era: The ED physician sees the same patient at 1 a.m. Because there is a reasonable chance admission is the best approach, he decides to call the hospitalist first rather than the patient’s PCP. Neither the ED doctor nor the hospitalist knows the patient well, and they are unaware outpatient follow-up with the PCP next morning is an option. After all, most PCPs are already “booked up” and probably unable to work someone in on such short notice. And, it’s tough to be sure the PCP would have all the relevant records regarding the data gathered and decisions made during the ED visit. So the hospitalist and ED doctor agree the best approach is to admit this patient to observation status, when in the pre-hospitalist era the patient might have been safely discharged from the ED for outpatient follow-up.
I fear this is a reasonably common scenario for many hospitalist practices. And yet these marginal admissions are often discharged the next day, lowering the overall length of stay (LOS) for hospitalist patients. By admitting marginal patients, some of whom might have been safely discharged from the ED in the pre-hospitalist era, a hospitalist practice can improve its overall LOS. The hospitalists might be patting themselves on the back for such good performance on LOS by admitting patients who could be discharged.
These two problems are difficult to quantify. If you’re confident these aren’t an issue for your practice, you deserve lots of credit. But I think most practices should think carefully about both issues and work to minimize how often they occur. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
I enjoy hearing about the value hospitalists provide our healthcare system. These stories come from peer-reviewed research, magazine articles, local newspapers, and even the occasional blog. When I talk to hospitalists from around the country, they are often eager to tell of their success and how they made it happen.
Not as often, I also hear about problems that may be a result of the hospitalist model. I think any successful practice, and our field as a whole, must remain open to the weaknesses in the hospitalist model and work continuously to address them. Issues like disruptions in care and poor communication between hospitalists and outpatient providers get a reasonable amount of attention and seem to be on most groups’ radar screens. But there are some potential problems I don’t hear discussed often, and I’m not aware of any significant research that has been published or presented to analyze them. I’ll review two such potential problems here.
ED Throughput
Are hospitalists sometimes the cause of a bottleneck in the emergency department (ED)? Hospitalist practice is nearly always credited with improving throughput at a hospital, including in the ED. But many hospitalist practices could impede throughput by delaying patients from leaving the ED when there are multiple simultaneous admissions. Consider the following scenarios:
The pre-hospitalist era: It is 7:30 p.m. and the ED has four patients ready for hand-off to an admitting doctor. There are several primary care groups at the hospital, and each has a doctor on call. Of the four patients needing admission, two go to Dr. Emerson from group A, one goes to Dr. Lake from group B, and one to Dr. Palmer from group C. Because the on-call doctor for these groups is home, he/she provides admitting orders by phone and may or may not see the patient that night. Of course, waiting until the next day to see the patient can be risky. In many cases the ED would have admitting orders on all four patients quickly, say within 30 minutes, and can send the patients up to the floor as soon as the bed is ready.
The hospitalist era: Things can happen differently when hospitalists are at this hospital. All daytime hospitalists are typically signed out to a single night hospitalist (nocturnist) at 7:30 p.m. when the ED has four patients to admit. This solo nocturnist might show up almost immediately after being notified about the admissions by the ED doctor and promptly start seeing the first of the four admissions. But it might take him/her three or four hours or more to finish admitting all four patients. By that time there are probably additional admissions waiting. The ED might end up keeping each patient much longer than in the first scenario.
The difference in these two scenarios is the availability of several doctors to admit patients simultaneously in the pre-hospitalist era. These doctors may be replaced by a single hospitalist who admits patients one at a time.
A clear benefit of the hospitalist system described in this example is that patients are seen in person by the hospitalist at the time of admission, rather than admitted over the phone by the primary care physician (PCP) and perhaps not seen in person by the PCP until the next day. Yet this may come at a cost of creating a bottleneck that didn’t exist in the pre-hospitalist era.
Think about whether this is a common problem in your practice. Several strategies might help minimize this bottleneck. The most common approach in a practice of more than about 10 hospitalists is to ensure that there is more than one hospitalist available to admit patients until 10 or 11 p.m. when admission volume typically subsides. This has led some groups to develop an evening “swing shift” from late afternoon until about 10 or 11 p.m.
Large groups may decide to dedicate one hospitalist entirely to the ED from sometime in the morning (e.g., 11 a.m.) until near midnight. This person is available to respond quickly to ED admissions and consult with ED doctors regarding management and disposition of borderline cases. While ED staff are usually thrilled to have a hospitalist for the day, that hospitalist often will need to get help from other hospitalists when several patients must be admitted at the same time. And hospitalist-patient continuity suffers because the patient will nearly always need to be handed off to a different hospitalist for follow-up visits.
Marginal Admissions
Do hospitalists increase the number of marginal or potentially avoidable admissions?
The pre-hospitalist era: The ED physician sees a patient of Dr. Bernstein’s at 1 a.m. and is having trouble deciding whether admission is the best approach. The ED doctor gets Dr. Bernstein or his on-call partner, Dr. Copeland, on the phone and learns this patient is well known to the practice and can be seen in the outpatient office early the next morning. Admission is unnecessary.
The hospitalist era: The ED physician sees the same patient at 1 a.m. Because there is a reasonable chance admission is the best approach, he decides to call the hospitalist first rather than the patient’s PCP. Neither the ED doctor nor the hospitalist knows the patient well, and they are unaware outpatient follow-up with the PCP next morning is an option. After all, most PCPs are already “booked up” and probably unable to work someone in on such short notice. And, it’s tough to be sure the PCP would have all the relevant records regarding the data gathered and decisions made during the ED visit. So the hospitalist and ED doctor agree the best approach is to admit this patient to observation status, when in the pre-hospitalist era the patient might have been safely discharged from the ED for outpatient follow-up.
I fear this is a reasonably common scenario for many hospitalist practices. And yet these marginal admissions are often discharged the next day, lowering the overall length of stay (LOS) for hospitalist patients. By admitting marginal patients, some of whom might have been safely discharged from the ED in the pre-hospitalist era, a hospitalist practice can improve its overall LOS. The hospitalists might be patting themselves on the back for such good performance on LOS by admitting patients who could be discharged.
These two problems are difficult to quantify. If you’re confident these aren’t an issue for your practice, you deserve lots of credit. But I think most practices should think carefully about both issues and work to minimize how often they occur. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.
I enjoy hearing about the value hospitalists provide our healthcare system. These stories come from peer-reviewed research, magazine articles, local newspapers, and even the occasional blog. When I talk to hospitalists from around the country, they are often eager to tell of their success and how they made it happen.
Not as often, I also hear about problems that may be a result of the hospitalist model. I think any successful practice, and our field as a whole, must remain open to the weaknesses in the hospitalist model and work continuously to address them. Issues like disruptions in care and poor communication between hospitalists and outpatient providers get a reasonable amount of attention and seem to be on most groups’ radar screens. But there are some potential problems I don’t hear discussed often, and I’m not aware of any significant research that has been published or presented to analyze them. I’ll review two such potential problems here.
ED Throughput
Are hospitalists sometimes the cause of a bottleneck in the emergency department (ED)? Hospitalist practice is nearly always credited with improving throughput at a hospital, including in the ED. But many hospitalist practices could impede throughput by delaying patients from leaving the ED when there are multiple simultaneous admissions. Consider the following scenarios:
The pre-hospitalist era: It is 7:30 p.m. and the ED has four patients ready for hand-off to an admitting doctor. There are several primary care groups at the hospital, and each has a doctor on call. Of the four patients needing admission, two go to Dr. Emerson from group A, one goes to Dr. Lake from group B, and one to Dr. Palmer from group C. Because the on-call doctor for these groups is home, he/she provides admitting orders by phone and may or may not see the patient that night. Of course, waiting until the next day to see the patient can be risky. In many cases the ED would have admitting orders on all four patients quickly, say within 30 minutes, and can send the patients up to the floor as soon as the bed is ready.
The hospitalist era: Things can happen differently when hospitalists are at this hospital. All daytime hospitalists are typically signed out to a single night hospitalist (nocturnist) at 7:30 p.m. when the ED has four patients to admit. This solo nocturnist might show up almost immediately after being notified about the admissions by the ED doctor and promptly start seeing the first of the four admissions. But it might take him/her three or four hours or more to finish admitting all four patients. By that time there are probably additional admissions waiting. The ED might end up keeping each patient much longer than in the first scenario.
The difference in these two scenarios is the availability of several doctors to admit patients simultaneously in the pre-hospitalist era. These doctors may be replaced by a single hospitalist who admits patients one at a time.
A clear benefit of the hospitalist system described in this example is that patients are seen in person by the hospitalist at the time of admission, rather than admitted over the phone by the primary care physician (PCP) and perhaps not seen in person by the PCP until the next day. Yet this may come at a cost of creating a bottleneck that didn’t exist in the pre-hospitalist era.
Think about whether this is a common problem in your practice. Several strategies might help minimize this bottleneck. The most common approach in a practice of more than about 10 hospitalists is to ensure that there is more than one hospitalist available to admit patients until 10 or 11 p.m. when admission volume typically subsides. This has led some groups to develop an evening “swing shift” from late afternoon until about 10 or 11 p.m.
Large groups may decide to dedicate one hospitalist entirely to the ED from sometime in the morning (e.g., 11 a.m.) until near midnight. This person is available to respond quickly to ED admissions and consult with ED doctors regarding management and disposition of borderline cases. While ED staff are usually thrilled to have a hospitalist for the day, that hospitalist often will need to get help from other hospitalists when several patients must be admitted at the same time. And hospitalist-patient continuity suffers because the patient will nearly always need to be handed off to a different hospitalist for follow-up visits.
Marginal Admissions
Do hospitalists increase the number of marginal or potentially avoidable admissions?
The pre-hospitalist era: The ED physician sees a patient of Dr. Bernstein’s at 1 a.m. and is having trouble deciding whether admission is the best approach. The ED doctor gets Dr. Bernstein or his on-call partner, Dr. Copeland, on the phone and learns this patient is well known to the practice and can be seen in the outpatient office early the next morning. Admission is unnecessary.
The hospitalist era: The ED physician sees the same patient at 1 a.m. Because there is a reasonable chance admission is the best approach, he decides to call the hospitalist first rather than the patient’s PCP. Neither the ED doctor nor the hospitalist knows the patient well, and they are unaware outpatient follow-up with the PCP next morning is an option. After all, most PCPs are already “booked up” and probably unable to work someone in on such short notice. And, it’s tough to be sure the PCP would have all the relevant records regarding the data gathered and decisions made during the ED visit. So the hospitalist and ED doctor agree the best approach is to admit this patient to observation status, when in the pre-hospitalist era the patient might have been safely discharged from the ED for outpatient follow-up.
I fear this is a reasonably common scenario for many hospitalist practices. And yet these marginal admissions are often discharged the next day, lowering the overall length of stay (LOS) for hospitalist patients. By admitting marginal patients, some of whom might have been safely discharged from the ED in the pre-hospitalist era, a hospitalist practice can improve its overall LOS. The hospitalists might be patting themselves on the back for such good performance on LOS by admitting patients who could be discharged.
These two problems are difficult to quantify. If you’re confident these aren’t an issue for your practice, you deserve lots of credit. But I think most practices should think carefully about both issues and work to minimize how often they occur. TH
Dr. Nelson has been a practicing hospitalist since 1988 and is co-founder and past president of SHM. He is a principal in Nelson/Flores Associates, a national hospitalist practice management consulting firm. He is also part of the faculty for SHM’s “Best Practices in Managing a Hospital Medicine Program.” This column represents his views and is not intended to reflect an official position of SHM.