User login
Patchy hair loss on the scalp
A 12-year-old girl has a large, irregular area of hair loss over the central frontoparietal scalp. Physical examination reveals scattered short hairs of varying lengths and a few small crusts throughout the area of alopecia (Figure 1). The remainder of the scalp appears normal.
Q: Which diagnosis is most likely?
- Alopecia areata
- Lichen planopilaris
- Discoid lupus erythematosus
- Trichotillomania
- Follicular degeneration syndrome
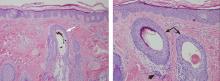
A: The correct answer is trichotillomania, the compulsive pulling out of one’s own hair. Irregularly shaped areas of alopecia containing short hairs of varied lengths and excoriation should raise clinical suspicion of trichotillomania. Biopsy can confirm the diagnosis when follicles devoid of hair shafts, hemorrhage, and misshapen fragments of scalp hair (pigment casts) are seen.
DIAGNOSTIC CLUES
Trichotillomania may present as striking hair loss (alopecia) with an irregular pattern, often with sharp angles or scalloped borders.1 Short and broken hairs within involved areas are typically seen because regenerating hairs are too short to be grasped and pulled out.2 Although hair loss on the scalp may be most evident, hair loss on any hair-bearing area of the body may be noted, including eyebrows and eyelashes.
Family members and the affected individual are often aware of compulsive manipulation of hair.
Depression, anxiety, and other grooming behaviors such as skin-picking and nail-biting may be associated with trichotillomania. Affected individuals often feel a sense of gratification from pulling out hairs. Although systemic complications are rare, some individuals ingest the removed hairs (trichophagy), and the hairs may be caught in the gastric folds and eventually form a trichobezoar.3
The diagnosis is usually based on clinical findings and by asking the patient about hair-pulling. Asking the patient if the habit is due to the feel of the hair, a need to calm himself or herself, or other factors may be revealing. The majority of cases can be diagnosed without biopsy. Biopsy from affected areas reveals changes related to trauma such as empty hair follicles, hemorrhage, and hair shaft fragments in the dermis2 (Figure 2). The number of catagen follicles is increased. Other causes of patchy alopecia are associated with different findings on biopsy.
Alopecia areata may be associated with an increased number of catagen hairs but is characterized by a peribulbar lymphocytic infiltrate.
Biopsy of lichen planopilaris typically reveals vacuolar changes along the dermal-follicular junction and necrotic keratinocytes.
Cutaneous lupus erythematosus is associated with thickening of the basement membrane zone, increased mucin in the dermis, follicular plugging by keratin, and vacuolar changes along the dermal-epidermal junction.
Biopsy of follicular degeneration syndrome exhibits premature desquamation of the internal root sheath as well as an increased number of fibrous tracts marking the sites of lost hairs.
The etiology of trichotillomania remains largely unknown, and the prognosis varies.4,5 There may be a family history, as there appears to be a genetic component to this disease. The disorder may also occur in the absence of external stressors.5
TREATMENT OPTIONS
Young children often develop trichotillomania that is transient in nature and most often does not require formal intervention. Older children may benefit from psychotherapy.5
Clomipramine (Anafranil) has been shown to be more effective than placebo.6 Selective serotonin reuptake inhibitors are no more effective than placebo.6,7 Pimozide (Orap), haloperidol (Haldol), and other agents have been reported to be of benefit in some instances. Although no large randomized clinical trials in children have been performed, N-acetylcysteine (Acetadote) seems to be a very promising form of therapy in adults.8 A multidisciplinary approach is usually helpful in finding the best treatment option for a particular patient.
- Shah KN, Fried RG. Factitial dermatoses in children. Curr Opin Pediatr 2006; 18:403–409.
- Hautmann G, Hercogova J, Lotti T. Trichotillomania. J Am Acad Dermatol 2002; 46:807–821.
- Lynch KA, Feola PG, Guenther E. Gastric trichobezoar: an important cause of abdominal pain presenting to the pediatric emergency department. Pediatr Emerg Care 2003; 19:343–347.
- Franklin ME, Tolin DF, editors. In: Treating Trichotillomania: Cognitive-Behavioral Therapy for Hairpulling and Related Problems. New York, NY: Springer; 2007.
- Duke DC, Keeley ML, Geffken GR, Storch EA. Trichotillomania: a current review. Clin Psychol Rev 2010; 30:181–193.
- Bloch MH, Landeros-Weisenberger A, Dombrowski P, et al. Systematic review: pharmacological and behavioral treatment for trichotillomania. Biol Psychiatry 2007; 62:839–846.
- Bloch MH. Trichotillomania across the life span. J Am Acad Child Adolesc Psychiatry 2009; 48:879–883.
- Grant JE, Odlaug BL, Kim SW. N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: a double-blind, placebo-controlled study. Arch Gen Psychiatry 2009; 66:756–763.
A 12-year-old girl has a large, irregular area of hair loss over the central frontoparietal scalp. Physical examination reveals scattered short hairs of varying lengths and a few small crusts throughout the area of alopecia (Figure 1). The remainder of the scalp appears normal.
Q: Which diagnosis is most likely?
- Alopecia areata
- Lichen planopilaris
- Discoid lupus erythematosus
- Trichotillomania
- Follicular degeneration syndrome
A: The correct answer is trichotillomania, the compulsive pulling out of one’s own hair. Irregularly shaped areas of alopecia containing short hairs of varied lengths and excoriation should raise clinical suspicion of trichotillomania. Biopsy can confirm the diagnosis when follicles devoid of hair shafts, hemorrhage, and misshapen fragments of scalp hair (pigment casts) are seen.
DIAGNOSTIC CLUES
Trichotillomania may present as striking hair loss (alopecia) with an irregular pattern, often with sharp angles or scalloped borders.1 Short and broken hairs within involved areas are typically seen because regenerating hairs are too short to be grasped and pulled out.2 Although hair loss on the scalp may be most evident, hair loss on any hair-bearing area of the body may be noted, including eyebrows and eyelashes.
Family members and the affected individual are often aware of compulsive manipulation of hair.
Depression, anxiety, and other grooming behaviors such as skin-picking and nail-biting may be associated with trichotillomania. Affected individuals often feel a sense of gratification from pulling out hairs. Although systemic complications are rare, some individuals ingest the removed hairs (trichophagy), and the hairs may be caught in the gastric folds and eventually form a trichobezoar.3
The diagnosis is usually based on clinical findings and by asking the patient about hair-pulling. Asking the patient if the habit is due to the feel of the hair, a need to calm himself or herself, or other factors may be revealing. The majority of cases can be diagnosed without biopsy. Biopsy from affected areas reveals changes related to trauma such as empty hair follicles, hemorrhage, and hair shaft fragments in the dermis2 (Figure 2). The number of catagen follicles is increased. Other causes of patchy alopecia are associated with different findings on biopsy.
Alopecia areata may be associated with an increased number of catagen hairs but is characterized by a peribulbar lymphocytic infiltrate.
Biopsy of lichen planopilaris typically reveals vacuolar changes along the dermal-follicular junction and necrotic keratinocytes.
Cutaneous lupus erythematosus is associated with thickening of the basement membrane zone, increased mucin in the dermis, follicular plugging by keratin, and vacuolar changes along the dermal-epidermal junction.
Biopsy of follicular degeneration syndrome exhibits premature desquamation of the internal root sheath as well as an increased number of fibrous tracts marking the sites of lost hairs.
The etiology of trichotillomania remains largely unknown, and the prognosis varies.4,5 There may be a family history, as there appears to be a genetic component to this disease. The disorder may also occur in the absence of external stressors.5
TREATMENT OPTIONS
Young children often develop trichotillomania that is transient in nature and most often does not require formal intervention. Older children may benefit from psychotherapy.5
Clomipramine (Anafranil) has been shown to be more effective than placebo.6 Selective serotonin reuptake inhibitors are no more effective than placebo.6,7 Pimozide (Orap), haloperidol (Haldol), and other agents have been reported to be of benefit in some instances. Although no large randomized clinical trials in children have been performed, N-acetylcysteine (Acetadote) seems to be a very promising form of therapy in adults.8 A multidisciplinary approach is usually helpful in finding the best treatment option for a particular patient.
A 12-year-old girl has a large, irregular area of hair loss over the central frontoparietal scalp. Physical examination reveals scattered short hairs of varying lengths and a few small crusts throughout the area of alopecia (Figure 1). The remainder of the scalp appears normal.
Q: Which diagnosis is most likely?
- Alopecia areata
- Lichen planopilaris
- Discoid lupus erythematosus
- Trichotillomania
- Follicular degeneration syndrome
A: The correct answer is trichotillomania, the compulsive pulling out of one’s own hair. Irregularly shaped areas of alopecia containing short hairs of varied lengths and excoriation should raise clinical suspicion of trichotillomania. Biopsy can confirm the diagnosis when follicles devoid of hair shafts, hemorrhage, and misshapen fragments of scalp hair (pigment casts) are seen.
DIAGNOSTIC CLUES
Trichotillomania may present as striking hair loss (alopecia) with an irregular pattern, often with sharp angles or scalloped borders.1 Short and broken hairs within involved areas are typically seen because regenerating hairs are too short to be grasped and pulled out.2 Although hair loss on the scalp may be most evident, hair loss on any hair-bearing area of the body may be noted, including eyebrows and eyelashes.
Family members and the affected individual are often aware of compulsive manipulation of hair.
Depression, anxiety, and other grooming behaviors such as skin-picking and nail-biting may be associated with trichotillomania. Affected individuals often feel a sense of gratification from pulling out hairs. Although systemic complications are rare, some individuals ingest the removed hairs (trichophagy), and the hairs may be caught in the gastric folds and eventually form a trichobezoar.3
The diagnosis is usually based on clinical findings and by asking the patient about hair-pulling. Asking the patient if the habit is due to the feel of the hair, a need to calm himself or herself, or other factors may be revealing. The majority of cases can be diagnosed without biopsy. Biopsy from affected areas reveals changes related to trauma such as empty hair follicles, hemorrhage, and hair shaft fragments in the dermis2 (Figure 2). The number of catagen follicles is increased. Other causes of patchy alopecia are associated with different findings on biopsy.
Alopecia areata may be associated with an increased number of catagen hairs but is characterized by a peribulbar lymphocytic infiltrate.
Biopsy of lichen planopilaris typically reveals vacuolar changes along the dermal-follicular junction and necrotic keratinocytes.
Cutaneous lupus erythematosus is associated with thickening of the basement membrane zone, increased mucin in the dermis, follicular plugging by keratin, and vacuolar changes along the dermal-epidermal junction.
Biopsy of follicular degeneration syndrome exhibits premature desquamation of the internal root sheath as well as an increased number of fibrous tracts marking the sites of lost hairs.
The etiology of trichotillomania remains largely unknown, and the prognosis varies.4,5 There may be a family history, as there appears to be a genetic component to this disease. The disorder may also occur in the absence of external stressors.5
TREATMENT OPTIONS
Young children often develop trichotillomania that is transient in nature and most often does not require formal intervention. Older children may benefit from psychotherapy.5
Clomipramine (Anafranil) has been shown to be more effective than placebo.6 Selective serotonin reuptake inhibitors are no more effective than placebo.6,7 Pimozide (Orap), haloperidol (Haldol), and other agents have been reported to be of benefit in some instances. Although no large randomized clinical trials in children have been performed, N-acetylcysteine (Acetadote) seems to be a very promising form of therapy in adults.8 A multidisciplinary approach is usually helpful in finding the best treatment option for a particular patient.
- Shah KN, Fried RG. Factitial dermatoses in children. Curr Opin Pediatr 2006; 18:403–409.
- Hautmann G, Hercogova J, Lotti T. Trichotillomania. J Am Acad Dermatol 2002; 46:807–821.
- Lynch KA, Feola PG, Guenther E. Gastric trichobezoar: an important cause of abdominal pain presenting to the pediatric emergency department. Pediatr Emerg Care 2003; 19:343–347.
- Franklin ME, Tolin DF, editors. In: Treating Trichotillomania: Cognitive-Behavioral Therapy for Hairpulling and Related Problems. New York, NY: Springer; 2007.
- Duke DC, Keeley ML, Geffken GR, Storch EA. Trichotillomania: a current review. Clin Psychol Rev 2010; 30:181–193.
- Bloch MH, Landeros-Weisenberger A, Dombrowski P, et al. Systematic review: pharmacological and behavioral treatment for trichotillomania. Biol Psychiatry 2007; 62:839–846.
- Bloch MH. Trichotillomania across the life span. J Am Acad Child Adolesc Psychiatry 2009; 48:879–883.
- Grant JE, Odlaug BL, Kim SW. N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: a double-blind, placebo-controlled study. Arch Gen Psychiatry 2009; 66:756–763.
- Shah KN, Fried RG. Factitial dermatoses in children. Curr Opin Pediatr 2006; 18:403–409.
- Hautmann G, Hercogova J, Lotti T. Trichotillomania. J Am Acad Dermatol 2002; 46:807–821.
- Lynch KA, Feola PG, Guenther E. Gastric trichobezoar: an important cause of abdominal pain presenting to the pediatric emergency department. Pediatr Emerg Care 2003; 19:343–347.
- Franklin ME, Tolin DF, editors. In: Treating Trichotillomania: Cognitive-Behavioral Therapy for Hairpulling and Related Problems. New York, NY: Springer; 2007.
- Duke DC, Keeley ML, Geffken GR, Storch EA. Trichotillomania: a current review. Clin Psychol Rev 2010; 30:181–193.
- Bloch MH, Landeros-Weisenberger A, Dombrowski P, et al. Systematic review: pharmacological and behavioral treatment for trichotillomania. Biol Psychiatry 2007; 62:839–846.
- Bloch MH. Trichotillomania across the life span. J Am Acad Child Adolesc Psychiatry 2009; 48:879–883.
- Grant JE, Odlaug BL, Kim SW. N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: a double-blind, placebo-controlled study. Arch Gen Psychiatry 2009; 66:756–763.