User login
Identifying Pediatric Skull Fracture Using Point-of-Care Ultrasound
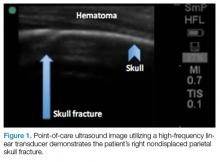
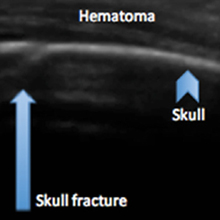
Evaluating pediatric patients presenting to the ED with head trauma can be a challenging task for emergency physicians (EPs). Specifically, identifying a nondisplaced skull fracture is not always possible through physical examination alone.1 However, point-of-care (POC) ultrasound permits rapid identification of skull fractures, which in turn assists the EP to determine if advanced imaging studies such as computed tomography (CT) are necessary.
Case
A previously healthy 10-month-old male infant presented to the ED with his mother for evaluation of rhinorrhea, cough, and fever, the onset of which began 24 hours prior to presentation. The patient’s mother reported that the infant continually tugged at his right ear throughout the previous evening and was increasingly irritable, but not inconsolable.
Initial vital signs at presentation were: blood pressure, 95/54 mm Hg; heart rate, 146 beats/min; respiratory rate, 36 beats/min, and temperature, 101.8°F. Oxygen saturation was 96% on room air. The physical examination was notable for an alert well-appearing infant who had a tender nonecchymotic scalp hematoma superior to the right pinna, clear tympanic membranes, crusted mucous bilaterally at the nares, nonlabored respirations, and wheezing throughout the lung fields.
Imaging Technique
To evaluate for skull fractures using POC ultrasound, the area of localized trauma must first be identified.2,3 Evidence of trauma includes an area of focal tenderness, abrasion, soft-tissue swelling, and hematoma.2,3 The presence of any depressed and open cranial injuries are contraindications to ultrasound. In which case, a physician should consult a neurosurgical specialist and obtain a CT scan of the head.
A high-frequency linear probe (5-10 MHz) is used to scan the area of localized trauma; this should be performed in two perpendicular planes using copious gel and light pressure (Figures 2a-2c).
Discussion
Closed head trauma is one of the most common pediatric injuries, accounting for roughly 1.4 million ED visits annually in the United States.5 Four to 12% percent of these minor traumas result in an intracranial injury,2 and the presence of a skull fracture is associated with a 4- to 20-fold increase in risk of underlying intracranial hemorrhage.3
Clinical assessment alone is not always reliable in predicting skull fracture and intracranial injury, especially in children younger than 2 years of age.2,3 Ultrasound is safe, noninvasive, expedient, cost-effective, and well tolerated in the pediatric population for identifying skull fractures,3 and can obviate the need for skull radiographs4 or procedural sedation. Moreover, POC ultrasound can serve as an adjunct to the Pediatric Emergency Care Applied Research Network head injury algorithm for head CT use decision rules if the fracture is not palpable on examination.
Several prospective studies and case reports have demonstrated the usefulness of POC ultrasound in diagnosing pediatric skull fractures in the ED.1-4 Two of the four cases published represented cases in which the EP identified an undisclosed nonaccidental trauma through POC ultrasound. Rabiner et al,3 estimates a combined sensitivity and specificity of 94% and 96%, respectively. It is important to remember that intracranial injury can still occur without an associated skull fracture. As our case demonstrates, POC ultrasound is a useful tool in risk-stratifying minor head trauma in children.
Case Conclusion
The head CT study confirmed a nondisplaced, oblique, and acute-appearing linear fracture of the right parietal bone extending from the squamosal to the lambdoid suture. There was no associated intracranial hemorrhage. The patient was admitted to the hospital for a nonaccidental trauma evaluation. The Department of Children and Family Services was contacted and the patient was discharged in the temporary custody of his maternal grandmother.
Summary
Point-of-care ultrasound is a useful diagnostic tool to rapidly evaluate for, and diagnose skull fractures in pediatric patients. Given its high sensitivity and specificity, ultrasound can help EPs identify occult nondisplaced skull fractures in children.
1. Riera A, Chen L. Ultrasound evaluation of skull fractures in children: a feasibility study. Pediatr Emerg Care. 2012;28(5):420-425. doi:10.1097/PEC.0b013e318252da3b.
2. Parri N, Crosby BJ, Glass C, et al. Ability of emergency ultrasonography to detect pediatric skull fractures: a prospective, observational study. J Emerg Med. 2013;44(1)135-141.
3. Rabiner JE, Friedman LM, Khine H, Avner JR, Tsung JW. Accuracy of point-of-care ultrasound for diagnosis of skull fractures in children. Pediatrics. 2013;131(6):e1757-1764. doi:10.1542/peds.2012-3921.
4. Ramirez-Schrempp D, Vinci RJ, Liteplo AS. Bedside ultrasound in the diagnosis of skull fractures in the pediatric emergency department. Pediatr Emerg Care. 2011;27(4):312-314. doi:10.1097/PEC.0b013e3182131579.
5. Coronado VG, Xu L, Basavaraju SV, et al; Centers for Disease Control and Prevention (CDC). Surveillance for traumatic brain injury-related deaths--United States, 1997-2007. MMWR Surveill Summ. 2011;60(5):1-32.
Evaluating pediatric patients presenting to the ED with head trauma can be a challenging task for emergency physicians (EPs). Specifically, identifying a nondisplaced skull fracture is not always possible through physical examination alone.1 However, point-of-care (POC) ultrasound permits rapid identification of skull fractures, which in turn assists the EP to determine if advanced imaging studies such as computed tomography (CT) are necessary.
Case
A previously healthy 10-month-old male infant presented to the ED with his mother for evaluation of rhinorrhea, cough, and fever, the onset of which began 24 hours prior to presentation. The patient’s mother reported that the infant continually tugged at his right ear throughout the previous evening and was increasingly irritable, but not inconsolable.
Initial vital signs at presentation were: blood pressure, 95/54 mm Hg; heart rate, 146 beats/min; respiratory rate, 36 beats/min, and temperature, 101.8°F. Oxygen saturation was 96% on room air. The physical examination was notable for an alert well-appearing infant who had a tender nonecchymotic scalp hematoma superior to the right pinna, clear tympanic membranes, crusted mucous bilaterally at the nares, nonlabored respirations, and wheezing throughout the lung fields.
Imaging Technique
To evaluate for skull fractures using POC ultrasound, the area of localized trauma must first be identified.2,3 Evidence of trauma includes an area of focal tenderness, abrasion, soft-tissue swelling, and hematoma.2,3 The presence of any depressed and open cranial injuries are contraindications to ultrasound. In which case, a physician should consult a neurosurgical specialist and obtain a CT scan of the head.
A high-frequency linear probe (5-10 MHz) is used to scan the area of localized trauma; this should be performed in two perpendicular planes using copious gel and light pressure (Figures 2a-2c).
Discussion
Closed head trauma is one of the most common pediatric injuries, accounting for roughly 1.4 million ED visits annually in the United States.5 Four to 12% percent of these minor traumas result in an intracranial injury,2 and the presence of a skull fracture is associated with a 4- to 20-fold increase in risk of underlying intracranial hemorrhage.3
Clinical assessment alone is not always reliable in predicting skull fracture and intracranial injury, especially in children younger than 2 years of age.2,3 Ultrasound is safe, noninvasive, expedient, cost-effective, and well tolerated in the pediatric population for identifying skull fractures,3 and can obviate the need for skull radiographs4 or procedural sedation. Moreover, POC ultrasound can serve as an adjunct to the Pediatric Emergency Care Applied Research Network head injury algorithm for head CT use decision rules if the fracture is not palpable on examination.
Several prospective studies and case reports have demonstrated the usefulness of POC ultrasound in diagnosing pediatric skull fractures in the ED.1-4 Two of the four cases published represented cases in which the EP identified an undisclosed nonaccidental trauma through POC ultrasound. Rabiner et al,3 estimates a combined sensitivity and specificity of 94% and 96%, respectively. It is important to remember that intracranial injury can still occur without an associated skull fracture. As our case demonstrates, POC ultrasound is a useful tool in risk-stratifying minor head trauma in children.
Case Conclusion
The head CT study confirmed a nondisplaced, oblique, and acute-appearing linear fracture of the right parietal bone extending from the squamosal to the lambdoid suture. There was no associated intracranial hemorrhage. The patient was admitted to the hospital for a nonaccidental trauma evaluation. The Department of Children and Family Services was contacted and the patient was discharged in the temporary custody of his maternal grandmother.
Summary
Point-of-care ultrasound is a useful diagnostic tool to rapidly evaluate for, and diagnose skull fractures in pediatric patients. Given its high sensitivity and specificity, ultrasound can help EPs identify occult nondisplaced skull fractures in children.
Evaluating pediatric patients presenting to the ED with head trauma can be a challenging task for emergency physicians (EPs). Specifically, identifying a nondisplaced skull fracture is not always possible through physical examination alone.1 However, point-of-care (POC) ultrasound permits rapid identification of skull fractures, which in turn assists the EP to determine if advanced imaging studies such as computed tomography (CT) are necessary.
Case
A previously healthy 10-month-old male infant presented to the ED with his mother for evaluation of rhinorrhea, cough, and fever, the onset of which began 24 hours prior to presentation. The patient’s mother reported that the infant continually tugged at his right ear throughout the previous evening and was increasingly irritable, but not inconsolable.
Initial vital signs at presentation were: blood pressure, 95/54 mm Hg; heart rate, 146 beats/min; respiratory rate, 36 beats/min, and temperature, 101.8°F. Oxygen saturation was 96% on room air. The physical examination was notable for an alert well-appearing infant who had a tender nonecchymotic scalp hematoma superior to the right pinna, clear tympanic membranes, crusted mucous bilaterally at the nares, nonlabored respirations, and wheezing throughout the lung fields.
Imaging Technique
To evaluate for skull fractures using POC ultrasound, the area of localized trauma must first be identified.2,3 Evidence of trauma includes an area of focal tenderness, abrasion, soft-tissue swelling, and hematoma.2,3 The presence of any depressed and open cranial injuries are contraindications to ultrasound. In which case, a physician should consult a neurosurgical specialist and obtain a CT scan of the head.
A high-frequency linear probe (5-10 MHz) is used to scan the area of localized trauma; this should be performed in two perpendicular planes using copious gel and light pressure (Figures 2a-2c).
Discussion
Closed head trauma is one of the most common pediatric injuries, accounting for roughly 1.4 million ED visits annually in the United States.5 Four to 12% percent of these minor traumas result in an intracranial injury,2 and the presence of a skull fracture is associated with a 4- to 20-fold increase in risk of underlying intracranial hemorrhage.3
Clinical assessment alone is not always reliable in predicting skull fracture and intracranial injury, especially in children younger than 2 years of age.2,3 Ultrasound is safe, noninvasive, expedient, cost-effective, and well tolerated in the pediatric population for identifying skull fractures,3 and can obviate the need for skull radiographs4 or procedural sedation. Moreover, POC ultrasound can serve as an adjunct to the Pediatric Emergency Care Applied Research Network head injury algorithm for head CT use decision rules if the fracture is not palpable on examination.
Several prospective studies and case reports have demonstrated the usefulness of POC ultrasound in diagnosing pediatric skull fractures in the ED.1-4 Two of the four cases published represented cases in which the EP identified an undisclosed nonaccidental trauma through POC ultrasound. Rabiner et al,3 estimates a combined sensitivity and specificity of 94% and 96%, respectively. It is important to remember that intracranial injury can still occur without an associated skull fracture. As our case demonstrates, POC ultrasound is a useful tool in risk-stratifying minor head trauma in children.
Case Conclusion
The head CT study confirmed a nondisplaced, oblique, and acute-appearing linear fracture of the right parietal bone extending from the squamosal to the lambdoid suture. There was no associated intracranial hemorrhage. The patient was admitted to the hospital for a nonaccidental trauma evaluation. The Department of Children and Family Services was contacted and the patient was discharged in the temporary custody of his maternal grandmother.
Summary
Point-of-care ultrasound is a useful diagnostic tool to rapidly evaluate for, and diagnose skull fractures in pediatric patients. Given its high sensitivity and specificity, ultrasound can help EPs identify occult nondisplaced skull fractures in children.
1. Riera A, Chen L. Ultrasound evaluation of skull fractures in children: a feasibility study. Pediatr Emerg Care. 2012;28(5):420-425. doi:10.1097/PEC.0b013e318252da3b.
2. Parri N, Crosby BJ, Glass C, et al. Ability of emergency ultrasonography to detect pediatric skull fractures: a prospective, observational study. J Emerg Med. 2013;44(1)135-141.
3. Rabiner JE, Friedman LM, Khine H, Avner JR, Tsung JW. Accuracy of point-of-care ultrasound for diagnosis of skull fractures in children. Pediatrics. 2013;131(6):e1757-1764. doi:10.1542/peds.2012-3921.
4. Ramirez-Schrempp D, Vinci RJ, Liteplo AS. Bedside ultrasound in the diagnosis of skull fractures in the pediatric emergency department. Pediatr Emerg Care. 2011;27(4):312-314. doi:10.1097/PEC.0b013e3182131579.
5. Coronado VG, Xu L, Basavaraju SV, et al; Centers for Disease Control and Prevention (CDC). Surveillance for traumatic brain injury-related deaths--United States, 1997-2007. MMWR Surveill Summ. 2011;60(5):1-32.
1. Riera A, Chen L. Ultrasound evaluation of skull fractures in children: a feasibility study. Pediatr Emerg Care. 2012;28(5):420-425. doi:10.1097/PEC.0b013e318252da3b.
2. Parri N, Crosby BJ, Glass C, et al. Ability of emergency ultrasonography to detect pediatric skull fractures: a prospective, observational study. J Emerg Med. 2013;44(1)135-141.
3. Rabiner JE, Friedman LM, Khine H, Avner JR, Tsung JW. Accuracy of point-of-care ultrasound for diagnosis of skull fractures in children. Pediatrics. 2013;131(6):e1757-1764. doi:10.1542/peds.2012-3921.
4. Ramirez-Schrempp D, Vinci RJ, Liteplo AS. Bedside ultrasound in the diagnosis of skull fractures in the pediatric emergency department. Pediatr Emerg Care. 2011;27(4):312-314. doi:10.1097/PEC.0b013e3182131579.
5. Coronado VG, Xu L, Basavaraju SV, et al; Centers for Disease Control and Prevention (CDC). Surveillance for traumatic brain injury-related deaths--United States, 1997-2007. MMWR Surveill Summ. 2011;60(5):1-32.
Emergency Ultrasound: Ultrasound-Guided Hip Arthrocentesis
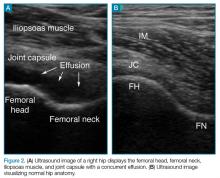
Hip ultrasound has long been considered an effective diagnostic and interventional tool to identify hip effusions and perform guided arthrocentesis in patients with suspected septic arthritis. Although imaging and interventional techniques are typically performed by interventional radiologists, several case reports support the use of these techniques by the emergency physician (EP) in both pediatric and adult patients presenting with hip pain.1,2
Hip ultrasound permits rapid visualization of the joint space to assess the presence of a hip effusion, and provides the opportunity for the clinician to quickly perform hip arthrocentesis and to obtain synovial fluid for analysis—the current gold standard of diagnosis. The current literature shows treatment of effusion in the adult hip via ultrasound-guided interventional methods to be more convenient and less painful than traditional fluoroscopic-guided techniques, and to have the same procedural success rate.3 With the increasing utilization of point-of-care (POC) ultrasound in the ED, ultrasound-guided hip arthrocentesis has become a powerful tool in the EP’s armamentarium to aid in evaluating and treating patients in the ED presenting with hip pain.
Imaging Technique
To perform an ultrasound-guided arthrocentesis, the patient should be placed in the supine position, with both knees bent and the hips externally rotated in the frog leg position (Figure 1).
Arthrocentesis
When an effusion is present, arthrocentesis is warranted. To perform this procedure, the femoral vessels should be identified inferior to the inguinal ligament and avoided laterally. The hip should be prepared in a sterile fashion and a lubricated probe should be placed in a sterile dressing with a cord cover. The effusion should be visualized again, and the area should be anesthetized superficially and deeply with local anesthetic, aspirating prior to infusing at the deeper levels. An 18-gauge spinal needle affixed to a 20-mL syringe should be introduced and advanced while aspirating under direct visualization through the capsule of the hip into the effusion. The fluid is then aspirated and sent for laboratory analysis.
Summary
A delayed diagnosis of hip effusion and failure to initiate prompt treatment are the most common causes of late complications of septic arthritis.4 Point-of-care diagnostic and interventional ultrasound of the hip permit instant visualization and implementation of immediate diagnostic and therapeutic measures, which decrease morbidity in adult patients with septic arthritis. Hip arthrocentesis with subsequent synovial fluid analysis, the gold standard of diagnosis, has traditionally been performed by radiology services. Recent literature, however, has shown performance of these ultrasound-guided techniques by EPs to be safe and efficient, facilitating time to treatment.
1. Freeman K, Dewitz A, Baker WE. Ultrasound-guided hip arthrocentesis in the ED. Am J Emerg Med. 2007;25(1):80-86. doi:10.1016/j.ajem.2006.08.002.
2. Minardi JJ, Lander OM. Septic hip arthritis: diagnosis and arthrocentesis using bedside ultrasound. J Emerg Med. 2012;43(2):316-318. doi:10.1016/j.jemermed.2011.09.029.
3. Byrd JW, Potts EA, Allison RK, Jones KS. Ultrasound-guided hip injections: a comparative study with fluoroscopy-guided injections. Arthroscopy. 2014;30(1):42-46. doi:10.1016/j.arthro.2013.09.083.
4. Mascioli AA, Park AL. Infectious arthritis. In: Canale ST, Beaty JH eds. Campbell’s Operative Orthopaedics. Vol 1. 13th ed. Philadelphia, PA: Elsevier Mosby; 2013:749-772.
Hip ultrasound has long been considered an effective diagnostic and interventional tool to identify hip effusions and perform guided arthrocentesis in patients with suspected septic arthritis. Although imaging and interventional techniques are typically performed by interventional radiologists, several case reports support the use of these techniques by the emergency physician (EP) in both pediatric and adult patients presenting with hip pain.1,2
Hip ultrasound permits rapid visualization of the joint space to assess the presence of a hip effusion, and provides the opportunity for the clinician to quickly perform hip arthrocentesis and to obtain synovial fluid for analysis—the current gold standard of diagnosis. The current literature shows treatment of effusion in the adult hip via ultrasound-guided interventional methods to be more convenient and less painful than traditional fluoroscopic-guided techniques, and to have the same procedural success rate.3 With the increasing utilization of point-of-care (POC) ultrasound in the ED, ultrasound-guided hip arthrocentesis has become a powerful tool in the EP’s armamentarium to aid in evaluating and treating patients in the ED presenting with hip pain.
Imaging Technique
To perform an ultrasound-guided arthrocentesis, the patient should be placed in the supine position, with both knees bent and the hips externally rotated in the frog leg position (Figure 1).
Arthrocentesis
When an effusion is present, arthrocentesis is warranted. To perform this procedure, the femoral vessels should be identified inferior to the inguinal ligament and avoided laterally. The hip should be prepared in a sterile fashion and a lubricated probe should be placed in a sterile dressing with a cord cover. The effusion should be visualized again, and the area should be anesthetized superficially and deeply with local anesthetic, aspirating prior to infusing at the deeper levels. An 18-gauge spinal needle affixed to a 20-mL syringe should be introduced and advanced while aspirating under direct visualization through the capsule of the hip into the effusion. The fluid is then aspirated and sent for laboratory analysis.
Summary
A delayed diagnosis of hip effusion and failure to initiate prompt treatment are the most common causes of late complications of septic arthritis.4 Point-of-care diagnostic and interventional ultrasound of the hip permit instant visualization and implementation of immediate diagnostic and therapeutic measures, which decrease morbidity in adult patients with septic arthritis. Hip arthrocentesis with subsequent synovial fluid analysis, the gold standard of diagnosis, has traditionally been performed by radiology services. Recent literature, however, has shown performance of these ultrasound-guided techniques by EPs to be safe and efficient, facilitating time to treatment.
Hip ultrasound has long been considered an effective diagnostic and interventional tool to identify hip effusions and perform guided arthrocentesis in patients with suspected septic arthritis. Although imaging and interventional techniques are typically performed by interventional radiologists, several case reports support the use of these techniques by the emergency physician (EP) in both pediatric and adult patients presenting with hip pain.1,2
Hip ultrasound permits rapid visualization of the joint space to assess the presence of a hip effusion, and provides the opportunity for the clinician to quickly perform hip arthrocentesis and to obtain synovial fluid for analysis—the current gold standard of diagnosis. The current literature shows treatment of effusion in the adult hip via ultrasound-guided interventional methods to be more convenient and less painful than traditional fluoroscopic-guided techniques, and to have the same procedural success rate.3 With the increasing utilization of point-of-care (POC) ultrasound in the ED, ultrasound-guided hip arthrocentesis has become a powerful tool in the EP’s armamentarium to aid in evaluating and treating patients in the ED presenting with hip pain.
Imaging Technique
To perform an ultrasound-guided arthrocentesis, the patient should be placed in the supine position, with both knees bent and the hips externally rotated in the frog leg position (Figure 1).
Arthrocentesis
When an effusion is present, arthrocentesis is warranted. To perform this procedure, the femoral vessels should be identified inferior to the inguinal ligament and avoided laterally. The hip should be prepared in a sterile fashion and a lubricated probe should be placed in a sterile dressing with a cord cover. The effusion should be visualized again, and the area should be anesthetized superficially and deeply with local anesthetic, aspirating prior to infusing at the deeper levels. An 18-gauge spinal needle affixed to a 20-mL syringe should be introduced and advanced while aspirating under direct visualization through the capsule of the hip into the effusion. The fluid is then aspirated and sent for laboratory analysis.
Summary
A delayed diagnosis of hip effusion and failure to initiate prompt treatment are the most common causes of late complications of septic arthritis.4 Point-of-care diagnostic and interventional ultrasound of the hip permit instant visualization and implementation of immediate diagnostic and therapeutic measures, which decrease morbidity in adult patients with septic arthritis. Hip arthrocentesis with subsequent synovial fluid analysis, the gold standard of diagnosis, has traditionally been performed by radiology services. Recent literature, however, has shown performance of these ultrasound-guided techniques by EPs to be safe and efficient, facilitating time to treatment.
1. Freeman K, Dewitz A, Baker WE. Ultrasound-guided hip arthrocentesis in the ED. Am J Emerg Med. 2007;25(1):80-86. doi:10.1016/j.ajem.2006.08.002.
2. Minardi JJ, Lander OM. Septic hip arthritis: diagnosis and arthrocentesis using bedside ultrasound. J Emerg Med. 2012;43(2):316-318. doi:10.1016/j.jemermed.2011.09.029.
3. Byrd JW, Potts EA, Allison RK, Jones KS. Ultrasound-guided hip injections: a comparative study with fluoroscopy-guided injections. Arthroscopy. 2014;30(1):42-46. doi:10.1016/j.arthro.2013.09.083.
4. Mascioli AA, Park AL. Infectious arthritis. In: Canale ST, Beaty JH eds. Campbell’s Operative Orthopaedics. Vol 1. 13th ed. Philadelphia, PA: Elsevier Mosby; 2013:749-772.
1. Freeman K, Dewitz A, Baker WE. Ultrasound-guided hip arthrocentesis in the ED. Am J Emerg Med. 2007;25(1):80-86. doi:10.1016/j.ajem.2006.08.002.
2. Minardi JJ, Lander OM. Septic hip arthritis: diagnosis and arthrocentesis using bedside ultrasound. J Emerg Med. 2012;43(2):316-318. doi:10.1016/j.jemermed.2011.09.029.
3. Byrd JW, Potts EA, Allison RK, Jones KS. Ultrasound-guided hip injections: a comparative study with fluoroscopy-guided injections. Arthroscopy. 2014;30(1):42-46. doi:10.1016/j.arthro.2013.09.083.
4. Mascioli AA, Park AL. Infectious arthritis. In: Canale ST, Beaty JH eds. Campbell’s Operative Orthopaedics. Vol 1. 13th ed. Philadelphia, PA: Elsevier Mosby; 2013:749-772.