User login
CASE REPORT: Altered Mental Status in an Elderly Woman
Case
A 100-year-old woman with a history of hypertension, hypothyroidism, and moderate Alzheimer dementia was brought to the ED by emergency medical services (EMS) for altered mental status after her home health aide (HHA) noted a change in the patient’s behavior. For the past few days, the patient’s appetite waned, and she became progressively more lethargic, not eating for over 24 hours. The aide activated 911 on the direction of the patient’s primary care physician. There were no reported changes to the patient’s medications which included aspirin, levothyroxine, and hydrochlorothiazide. She was unable to provide any meaningful history.
On arrival to the ED, the patient appeared comfortable in bed. She was sleepy, but easily aroused. Initial vital signs were: heart rate, 110 beats/minute; respiratory rate, 12 breaths/minute; blood pressure, 163/103 mm Hg; oral temperature, 98.2˚F. Oxygen (O2) saturation was 96% on room air. She was oriented to person only and responded appropriately to simple questions, intermittently following one-step commands. She was unable to attend and required redirection throughout the interview. (According to the aide, this behavior was different than her baseline.)
The patient’s head and neck examination were notable for some mild, boggy, periorbital edema and dry mucous membranes. Her thyroid examination was normal; her lungs were clear; and her cardiac examination revealed a 2/6 systolic ejection murmur over the second right intercostal space. Examination of the abdomen, extremities, and skin was unrevealing, and there were no gross focal neurological deficits. Her reflexes were normal throughout.
Initial assessment of this patient suggested a diagnosis of dementia and hypoactive delirium—the latter due to one or more of several possible etiologies.
Altered Mental Status
While altered mental status is a billable medical ICD-9-CM code1 used to specify a diagnosis on a reimbursement claim, it is not a disease state itself. Instead, it is a catchall phrase that incorporates any change in mental status, encompassing symptomatology that may have the largest differential diagnosis encountered in emergency medicine.
Delirium
An important category of altered mental status is delirium. The diagnostic criteria2 for delirium in DSM-V have remained essentially unchanged from DSM-IV; however, the prevalence of delirium as one of the key geriatric syndromes has grown as a result of increased research and education, particularly in the emergency medical setting. Distilled down, delirium can be defined as an acute change in mental status not caused by underlying dementia. Its cause is often multifactorial, and it is frequently an underappreciated consequence of both critical illness and the hospital environment.3
Delirium is an emergency unto itself, with an in-hospital mortality rate mirroring that of sepsis or acute myocardial infarction.4 The older-adult population is especially at risk of delirium and can present with one of three clinical subtypes: hyperactive (ie, agitated, etc), hypoactive (ie, somnolent, lethargic, stuporous, etc), and mixed type.5
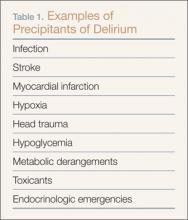
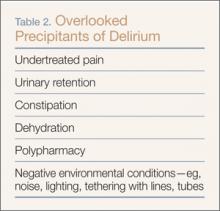
The composition of factors precipitating the onset of delirium includes age, dementia, alcohol use, depression, illness severity, and drug exposure—notably benzodiazepines, opiates, and medications with anticholinergic properties.8 While major precipitants or causes of delirium, traditionally considered as potentially life-threatening acute events, are well known (Table 1), others are often overlooked (Table 2). Yet, ironically, these more frequently bypassed causes are more readily reversible, once discovered, such as inadequate pain control, urinary retention, constipation, dehydration, polypharmacy, and negative environmental conditions in the patient’s immediate surroundings. These findings have recently been corroborated.9
The Confusion Assessment Method
Identifying delirium can be a particular challenge for emergency physicians (EPs), especially when the patient has an underlying diagnosis of dementia and the specific degree of cognitive impairment is not known. The Confusion Assessment Method (CAM)10 is the most commonly used tool in the critical care setting11 and is the only validated tool for the ED, with an 86% sensitivity and 100% specificity.12 It evaluates four elements: (1) acute onset and fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. A patient must demonstrate the first two elements in addition to either the third or fourth element to be considered to have delirium.10
The CAM intensive care unit scale has the potential to be even more applicable in the ED. Recent findings support its validation.9
Case Continued
With respect to the elderly patient in this case with dementia and multiple potential causes for hypoactive delirium, the life-saving measure was the New York City (NYC) mandate that all 911 responding EMS workers wear ambient carbon monoxide (CO) detectors. Though the value of these detectors is controversial due to their low sensitivity, the emergency medical technicians (EMTs) detected an elevated CO level of 300 ppm when they arrived at the patient’s home.
Without this information, the patient’s age and clinical presentation would almost certainly have prompted an extensive evaluation to determine the etiology of her change in mental status and most likely would have missed the true cause of CO toxicity, which was confirmed by venous co-oximetry showing the patient to have a carboxyhemoglobin (HbCO) level of 19.5%.
Carbon Monoxide Toxicity
Carbon monoxide affects multiple cell types. It binds to myoglobin and in high concentrations depresses myocardial contractility. In platelets, CO displaces nitric oxide potentially resulting in vasodilation. Life-threatening CO poisoning causes hypotension, syncope, tachycardia, and an altered mental status. Delayed neuropsychiatric sequelae also may occur as the result of free radical injury to the brain.13
Symptoms
Patients with chronic CO poisoning who can adequately communicate may report nausea, headache, lightheadedness, and lethargy mimicking other seasonal illnesses. In debilitated or cognitively impaired patients who are unable to communicate, findings may include tachycardia, a mild change in mental status, and little else. Prolonged exposure and physiologic accumulation of CO may cause depressed mental status, coma, or death.
Although HbCO levels are confirmatory of exposure, venous levels do not necessarily reflect tissue concentrations or outcomes. Patients with a similar level to that of this patient (19.5%) may present with no symptoms, mild headache, or a deep coma depending on the duration of exposure to CO.
Definitive treatment is removal from the toxic environment and prompt administration of O2. In some cases, hyperbaric therapy may be beneficial.14
Diagnosis
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
It is rarely easy to diagnose the first case of an illness of which one is unfamiliar or not accustomed to treating. Likewise, it is very difficult to consider, diagnose and, as a result, effectively manage the first presentation of a known condition that is typically seasonal or linked to a different geographic location. Acute presentations of environmental exposures, illicit drug poisonings, and communicable infectious diseases are increasingly the purview of emergency medicine. Whether it is the first case of Ebola, of severe acute respiratory syndrome, the influenza virus, a new lethal street drug overdose, or CO poisoning prior to the onset of winter, maintaining a high index of suspicion for the “index case” is of paramount importance. The patient presented here, the first CO poisoning of the season at the authors’ institution, illustrates the responsibility the EP to consider, diagnose, and prevent a wide-range of deadly consequences—injury prevention as the result of vigilance. Moreover, the consequences of missing the diagnosis would have placed others at risk for continued poisoning and possibly death.
Portable and Ambient Carboxyhemoglobin Monitors
The NYC Department of Health (NYCDOH) requires that all EMTs and paramedics wear CO detectors and all residential housing contain CO monitors. The NYCDOH also mandates that all identified cases of CO poisoning be reported to the NYC Poison Control Center. This centralization of data on any and all patients exposed to CO can result in an investigation of the source of CO by the fire department and capture symptomatic patients who present for care outside of the 911 response system. The source of CO in this patient was ultimately traced to a faulty furnace that was repaired to prevent others in the building from becoming victims of CO poisoning.
It should be noted that portable noninvasive HbCO monitors may be inadequate to rule out CO poisoning as the sensitivity of such devices can be as low as 48%.15 Carbon monoxide poisoning can result from brief exposure to a high ambient concentration, such as a fire in which environmental concentrations may exceed 500 ppm or more insidiously, in a setting of a chronic exposure. Faulty furnaces—a common seasonal cause of CO poisoning—may continue to produce adequate heat and fail to prompt any concerns.
Since CO is colorless and odorless, ambient CO detectors stationed in the home are the best means of alerting one to exposure. In this case, though mandated by NYCDOH, a CO detector was not present in the patient’s home.
Case Conclusion
Through the rapid identification of CO poisoning in this elderly patient with altered mental status, EMS was able to evacuate the building while bringing the elderly tenant and her home attendant to the ED.
Based on the elderly patient’s elevated HbCO level, she was treated with O2 and discharged from the hospital the following day feeling well. In addition to the patient’s symptoms, when the aide was interviewed, she reported that she had been experiencing daily headaches, which she said soon resolved on departure from her client’s house. Her symptoms had been bothersome, but not so severe as to prompt her to seek medical attention. The aide was found to have an HbCO level of 12.5% and was discharged from the ED after 6 hours of observation and O2 therapy. The third occupant of the building, a tenant, was also brought to the ED and found to have an HbCO level of 12%. The tenant was treated with O2 therapy and discharged to home.
Dr Caldwell is an assistant professor of medicine in the department of emergency medicine, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Rao is an assistant professor of emergency medicine; and the chief in the division of medical Toxicology, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Stern is an assistant professor of medicine, department of emergency medicine; chief of geriatric emergency medicine; and codirector of geriatric emergency medicine fellowship at New York Presbyterian Hospital/Weill Cornell Medical Center, New York.
- ICD-9Data.com Web site. 2014 ICD-9-CM Diagnosis Codes. http://www.icd9data.com/2014/Volume1/default.htm. Accessed December 4, 2014.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
- Han JH, Wilson A, Ely EW. Delirium in the older emergency department patient: a quiet epidemic. Emerg Med Clin North Am. 2010;28(3):611-631.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
- Mulcare MR, Halpern A, Stern ME. The geriatric patient. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:741-753.
- Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193-200.
- Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
- Han JH, Vasilevskis EE, Ely EW. Sedation and delirium. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:704-717.
- Rosen T, Connors S, Halpern A, et al. Improving emergency department identification and management of agitated delirium in older adults: Implementation and impact assessment of a comprehensive clinical protocol using an A-B-C-D-E-F mnemonic. Ann Emerg Med. 2013;62(4)(Supp 4):S53-54.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
- Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
- Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23(1):20-25.
- Weaver LK. Carbon monoxide poisoning. New Engl J Med. 2009;360(12):1217-1225.
- Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric therapy for acute carbon monoxide poisoning. New Engl J Med. 2002;347(14):1057-1067.
- Touger M, Birnbaum A, Wang J, Chou K, Pearson D, Bijur P. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):382-388.
Case
A 100-year-old woman with a history of hypertension, hypothyroidism, and moderate Alzheimer dementia was brought to the ED by emergency medical services (EMS) for altered mental status after her home health aide (HHA) noted a change in the patient’s behavior. For the past few days, the patient’s appetite waned, and she became progressively more lethargic, not eating for over 24 hours. The aide activated 911 on the direction of the patient’s primary care physician. There were no reported changes to the patient’s medications which included aspirin, levothyroxine, and hydrochlorothiazide. She was unable to provide any meaningful history.
On arrival to the ED, the patient appeared comfortable in bed. She was sleepy, but easily aroused. Initial vital signs were: heart rate, 110 beats/minute; respiratory rate, 12 breaths/minute; blood pressure, 163/103 mm Hg; oral temperature, 98.2˚F. Oxygen (O2) saturation was 96% on room air. She was oriented to person only and responded appropriately to simple questions, intermittently following one-step commands. She was unable to attend and required redirection throughout the interview. (According to the aide, this behavior was different than her baseline.)
The patient’s head and neck examination were notable for some mild, boggy, periorbital edema and dry mucous membranes. Her thyroid examination was normal; her lungs were clear; and her cardiac examination revealed a 2/6 systolic ejection murmur over the second right intercostal space. Examination of the abdomen, extremities, and skin was unrevealing, and there were no gross focal neurological deficits. Her reflexes were normal throughout.
Initial assessment of this patient suggested a diagnosis of dementia and hypoactive delirium—the latter due to one or more of several possible etiologies.
Altered Mental Status
While altered mental status is a billable medical ICD-9-CM code1 used to specify a diagnosis on a reimbursement claim, it is not a disease state itself. Instead, it is a catchall phrase that incorporates any change in mental status, encompassing symptomatology that may have the largest differential diagnosis encountered in emergency medicine.
Delirium
An important category of altered mental status is delirium. The diagnostic criteria2 for delirium in DSM-V have remained essentially unchanged from DSM-IV; however, the prevalence of delirium as one of the key geriatric syndromes has grown as a result of increased research and education, particularly in the emergency medical setting. Distilled down, delirium can be defined as an acute change in mental status not caused by underlying dementia. Its cause is often multifactorial, and it is frequently an underappreciated consequence of both critical illness and the hospital environment.3
Delirium is an emergency unto itself, with an in-hospital mortality rate mirroring that of sepsis or acute myocardial infarction.4 The older-adult population is especially at risk of delirium and can present with one of three clinical subtypes: hyperactive (ie, agitated, etc), hypoactive (ie, somnolent, lethargic, stuporous, etc), and mixed type.5
The composition of factors precipitating the onset of delirium includes age, dementia, alcohol use, depression, illness severity, and drug exposure—notably benzodiazepines, opiates, and medications with anticholinergic properties.8 While major precipitants or causes of delirium, traditionally considered as potentially life-threatening acute events, are well known (Table 1), others are often overlooked (Table 2). Yet, ironically, these more frequently bypassed causes are more readily reversible, once discovered, such as inadequate pain control, urinary retention, constipation, dehydration, polypharmacy, and negative environmental conditions in the patient’s immediate surroundings. These findings have recently been corroborated.9
The Confusion Assessment Method
Identifying delirium can be a particular challenge for emergency physicians (EPs), especially when the patient has an underlying diagnosis of dementia and the specific degree of cognitive impairment is not known. The Confusion Assessment Method (CAM)10 is the most commonly used tool in the critical care setting11 and is the only validated tool for the ED, with an 86% sensitivity and 100% specificity.12 It evaluates four elements: (1) acute onset and fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. A patient must demonstrate the first two elements in addition to either the third or fourth element to be considered to have delirium.10
The CAM intensive care unit scale has the potential to be even more applicable in the ED. Recent findings support its validation.9
Case Continued
With respect to the elderly patient in this case with dementia and multiple potential causes for hypoactive delirium, the life-saving measure was the New York City (NYC) mandate that all 911 responding EMS workers wear ambient carbon monoxide (CO) detectors. Though the value of these detectors is controversial due to their low sensitivity, the emergency medical technicians (EMTs) detected an elevated CO level of 300 ppm when they arrived at the patient’s home.
Without this information, the patient’s age and clinical presentation would almost certainly have prompted an extensive evaluation to determine the etiology of her change in mental status and most likely would have missed the true cause of CO toxicity, which was confirmed by venous co-oximetry showing the patient to have a carboxyhemoglobin (HbCO) level of 19.5%.
Carbon Monoxide Toxicity
Carbon monoxide affects multiple cell types. It binds to myoglobin and in high concentrations depresses myocardial contractility. In platelets, CO displaces nitric oxide potentially resulting in vasodilation. Life-threatening CO poisoning causes hypotension, syncope, tachycardia, and an altered mental status. Delayed neuropsychiatric sequelae also may occur as the result of free radical injury to the brain.13
Symptoms
Patients with chronic CO poisoning who can adequately communicate may report nausea, headache, lightheadedness, and lethargy mimicking other seasonal illnesses. In debilitated or cognitively impaired patients who are unable to communicate, findings may include tachycardia, a mild change in mental status, and little else. Prolonged exposure and physiologic accumulation of CO may cause depressed mental status, coma, or death.
Although HbCO levels are confirmatory of exposure, venous levels do not necessarily reflect tissue concentrations or outcomes. Patients with a similar level to that of this patient (19.5%) may present with no symptoms, mild headache, or a deep coma depending on the duration of exposure to CO.
Definitive treatment is removal from the toxic environment and prompt administration of O2. In some cases, hyperbaric therapy may be beneficial.14
Diagnosis
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
It is rarely easy to diagnose the first case of an illness of which one is unfamiliar or not accustomed to treating. Likewise, it is very difficult to consider, diagnose and, as a result, effectively manage the first presentation of a known condition that is typically seasonal or linked to a different geographic location. Acute presentations of environmental exposures, illicit drug poisonings, and communicable infectious diseases are increasingly the purview of emergency medicine. Whether it is the first case of Ebola, of severe acute respiratory syndrome, the influenza virus, a new lethal street drug overdose, or CO poisoning prior to the onset of winter, maintaining a high index of suspicion for the “index case” is of paramount importance. The patient presented here, the first CO poisoning of the season at the authors’ institution, illustrates the responsibility the EP to consider, diagnose, and prevent a wide-range of deadly consequences—injury prevention as the result of vigilance. Moreover, the consequences of missing the diagnosis would have placed others at risk for continued poisoning and possibly death.
Portable and Ambient Carboxyhemoglobin Monitors
The NYC Department of Health (NYCDOH) requires that all EMTs and paramedics wear CO detectors and all residential housing contain CO monitors. The NYCDOH also mandates that all identified cases of CO poisoning be reported to the NYC Poison Control Center. This centralization of data on any and all patients exposed to CO can result in an investigation of the source of CO by the fire department and capture symptomatic patients who present for care outside of the 911 response system. The source of CO in this patient was ultimately traced to a faulty furnace that was repaired to prevent others in the building from becoming victims of CO poisoning.
It should be noted that portable noninvasive HbCO monitors may be inadequate to rule out CO poisoning as the sensitivity of such devices can be as low as 48%.15 Carbon monoxide poisoning can result from brief exposure to a high ambient concentration, such as a fire in which environmental concentrations may exceed 500 ppm or more insidiously, in a setting of a chronic exposure. Faulty furnaces—a common seasonal cause of CO poisoning—may continue to produce adequate heat and fail to prompt any concerns.
Since CO is colorless and odorless, ambient CO detectors stationed in the home are the best means of alerting one to exposure. In this case, though mandated by NYCDOH, a CO detector was not present in the patient’s home.
Case Conclusion
Through the rapid identification of CO poisoning in this elderly patient with altered mental status, EMS was able to evacuate the building while bringing the elderly tenant and her home attendant to the ED.
Based on the elderly patient’s elevated HbCO level, she was treated with O2 and discharged from the hospital the following day feeling well. In addition to the patient’s symptoms, when the aide was interviewed, she reported that she had been experiencing daily headaches, which she said soon resolved on departure from her client’s house. Her symptoms had been bothersome, but not so severe as to prompt her to seek medical attention. The aide was found to have an HbCO level of 12.5% and was discharged from the ED after 6 hours of observation and O2 therapy. The third occupant of the building, a tenant, was also brought to the ED and found to have an HbCO level of 12%. The tenant was treated with O2 therapy and discharged to home.
Dr Caldwell is an assistant professor of medicine in the department of emergency medicine, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Rao is an assistant professor of emergency medicine; and the chief in the division of medical Toxicology, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Stern is an assistant professor of medicine, department of emergency medicine; chief of geriatric emergency medicine; and codirector of geriatric emergency medicine fellowship at New York Presbyterian Hospital/Weill Cornell Medical Center, New York.
Case
A 100-year-old woman with a history of hypertension, hypothyroidism, and moderate Alzheimer dementia was brought to the ED by emergency medical services (EMS) for altered mental status after her home health aide (HHA) noted a change in the patient’s behavior. For the past few days, the patient’s appetite waned, and she became progressively more lethargic, not eating for over 24 hours. The aide activated 911 on the direction of the patient’s primary care physician. There were no reported changes to the patient’s medications which included aspirin, levothyroxine, and hydrochlorothiazide. She was unable to provide any meaningful history.
On arrival to the ED, the patient appeared comfortable in bed. She was sleepy, but easily aroused. Initial vital signs were: heart rate, 110 beats/minute; respiratory rate, 12 breaths/minute; blood pressure, 163/103 mm Hg; oral temperature, 98.2˚F. Oxygen (O2) saturation was 96% on room air. She was oriented to person only and responded appropriately to simple questions, intermittently following one-step commands. She was unable to attend and required redirection throughout the interview. (According to the aide, this behavior was different than her baseline.)
The patient’s head and neck examination were notable for some mild, boggy, periorbital edema and dry mucous membranes. Her thyroid examination was normal; her lungs were clear; and her cardiac examination revealed a 2/6 systolic ejection murmur over the second right intercostal space. Examination of the abdomen, extremities, and skin was unrevealing, and there were no gross focal neurological deficits. Her reflexes were normal throughout.
Initial assessment of this patient suggested a diagnosis of dementia and hypoactive delirium—the latter due to one or more of several possible etiologies.
Altered Mental Status
While altered mental status is a billable medical ICD-9-CM code1 used to specify a diagnosis on a reimbursement claim, it is not a disease state itself. Instead, it is a catchall phrase that incorporates any change in mental status, encompassing symptomatology that may have the largest differential diagnosis encountered in emergency medicine.
Delirium
An important category of altered mental status is delirium. The diagnostic criteria2 for delirium in DSM-V have remained essentially unchanged from DSM-IV; however, the prevalence of delirium as one of the key geriatric syndromes has grown as a result of increased research and education, particularly in the emergency medical setting. Distilled down, delirium can be defined as an acute change in mental status not caused by underlying dementia. Its cause is often multifactorial, and it is frequently an underappreciated consequence of both critical illness and the hospital environment.3
Delirium is an emergency unto itself, with an in-hospital mortality rate mirroring that of sepsis or acute myocardial infarction.4 The older-adult population is especially at risk of delirium and can present with one of three clinical subtypes: hyperactive (ie, agitated, etc), hypoactive (ie, somnolent, lethargic, stuporous, etc), and mixed type.5
The composition of factors precipitating the onset of delirium includes age, dementia, alcohol use, depression, illness severity, and drug exposure—notably benzodiazepines, opiates, and medications with anticholinergic properties.8 While major precipitants or causes of delirium, traditionally considered as potentially life-threatening acute events, are well known (Table 1), others are often overlooked (Table 2). Yet, ironically, these more frequently bypassed causes are more readily reversible, once discovered, such as inadequate pain control, urinary retention, constipation, dehydration, polypharmacy, and negative environmental conditions in the patient’s immediate surroundings. These findings have recently been corroborated.9
The Confusion Assessment Method
Identifying delirium can be a particular challenge for emergency physicians (EPs), especially when the patient has an underlying diagnosis of dementia and the specific degree of cognitive impairment is not known. The Confusion Assessment Method (CAM)10 is the most commonly used tool in the critical care setting11 and is the only validated tool for the ED, with an 86% sensitivity and 100% specificity.12 It evaluates four elements: (1) acute onset and fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. A patient must demonstrate the first two elements in addition to either the third or fourth element to be considered to have delirium.10
The CAM intensive care unit scale has the potential to be even more applicable in the ED. Recent findings support its validation.9
Case Continued
With respect to the elderly patient in this case with dementia and multiple potential causes for hypoactive delirium, the life-saving measure was the New York City (NYC) mandate that all 911 responding EMS workers wear ambient carbon monoxide (CO) detectors. Though the value of these detectors is controversial due to their low sensitivity, the emergency medical technicians (EMTs) detected an elevated CO level of 300 ppm when they arrived at the patient’s home.
Without this information, the patient’s age and clinical presentation would almost certainly have prompted an extensive evaluation to determine the etiology of her change in mental status and most likely would have missed the true cause of CO toxicity, which was confirmed by venous co-oximetry showing the patient to have a carboxyhemoglobin (HbCO) level of 19.5%.
Carbon Monoxide Toxicity
Carbon monoxide affects multiple cell types. It binds to myoglobin and in high concentrations depresses myocardial contractility. In platelets, CO displaces nitric oxide potentially resulting in vasodilation. Life-threatening CO poisoning causes hypotension, syncope, tachycardia, and an altered mental status. Delayed neuropsychiatric sequelae also may occur as the result of free radical injury to the brain.13
Symptoms
Patients with chronic CO poisoning who can adequately communicate may report nausea, headache, lightheadedness, and lethargy mimicking other seasonal illnesses. In debilitated or cognitively impaired patients who are unable to communicate, findings may include tachycardia, a mild change in mental status, and little else. Prolonged exposure and physiologic accumulation of CO may cause depressed mental status, coma, or death.
Although HbCO levels are confirmatory of exposure, venous levels do not necessarily reflect tissue concentrations or outcomes. Patients with a similar level to that of this patient (19.5%) may present with no symptoms, mild headache, or a deep coma depending on the duration of exposure to CO.
Definitive treatment is removal from the toxic environment and prompt administration of O2. In some cases, hyperbaric therapy may be beneficial.14
Diagnosis
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
It is rarely easy to diagnose the first case of an illness of which one is unfamiliar or not accustomed to treating. Likewise, it is very difficult to consider, diagnose and, as a result, effectively manage the first presentation of a known condition that is typically seasonal or linked to a different geographic location. Acute presentations of environmental exposures, illicit drug poisonings, and communicable infectious diseases are increasingly the purview of emergency medicine. Whether it is the first case of Ebola, of severe acute respiratory syndrome, the influenza virus, a new lethal street drug overdose, or CO poisoning prior to the onset of winter, maintaining a high index of suspicion for the “index case” is of paramount importance. The patient presented here, the first CO poisoning of the season at the authors’ institution, illustrates the responsibility the EP to consider, diagnose, and prevent a wide-range of deadly consequences—injury prevention as the result of vigilance. Moreover, the consequences of missing the diagnosis would have placed others at risk for continued poisoning and possibly death.
Portable and Ambient Carboxyhemoglobin Monitors
The NYC Department of Health (NYCDOH) requires that all EMTs and paramedics wear CO detectors and all residential housing contain CO monitors. The NYCDOH also mandates that all identified cases of CO poisoning be reported to the NYC Poison Control Center. This centralization of data on any and all patients exposed to CO can result in an investigation of the source of CO by the fire department and capture symptomatic patients who present for care outside of the 911 response system. The source of CO in this patient was ultimately traced to a faulty furnace that was repaired to prevent others in the building from becoming victims of CO poisoning.
It should be noted that portable noninvasive HbCO monitors may be inadequate to rule out CO poisoning as the sensitivity of such devices can be as low as 48%.15 Carbon monoxide poisoning can result from brief exposure to a high ambient concentration, such as a fire in which environmental concentrations may exceed 500 ppm or more insidiously, in a setting of a chronic exposure. Faulty furnaces—a common seasonal cause of CO poisoning—may continue to produce adequate heat and fail to prompt any concerns.
Since CO is colorless and odorless, ambient CO detectors stationed in the home are the best means of alerting one to exposure. In this case, though mandated by NYCDOH, a CO detector was not present in the patient’s home.
Case Conclusion
Through the rapid identification of CO poisoning in this elderly patient with altered mental status, EMS was able to evacuate the building while bringing the elderly tenant and her home attendant to the ED.
Based on the elderly patient’s elevated HbCO level, she was treated with O2 and discharged from the hospital the following day feeling well. In addition to the patient’s symptoms, when the aide was interviewed, she reported that she had been experiencing daily headaches, which she said soon resolved on departure from her client’s house. Her symptoms had been bothersome, but not so severe as to prompt her to seek medical attention. The aide was found to have an HbCO level of 12.5% and was discharged from the ED after 6 hours of observation and O2 therapy. The third occupant of the building, a tenant, was also brought to the ED and found to have an HbCO level of 12%. The tenant was treated with O2 therapy and discharged to home.
Dr Caldwell is an assistant professor of medicine in the department of emergency medicine, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Rao is an assistant professor of emergency medicine; and the chief in the division of medical Toxicology, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Stern is an assistant professor of medicine, department of emergency medicine; chief of geriatric emergency medicine; and codirector of geriatric emergency medicine fellowship at New York Presbyterian Hospital/Weill Cornell Medical Center, New York.
- ICD-9Data.com Web site. 2014 ICD-9-CM Diagnosis Codes. http://www.icd9data.com/2014/Volume1/default.htm. Accessed December 4, 2014.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
- Han JH, Wilson A, Ely EW. Delirium in the older emergency department patient: a quiet epidemic. Emerg Med Clin North Am. 2010;28(3):611-631.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
- Mulcare MR, Halpern A, Stern ME. The geriatric patient. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:741-753.
- Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193-200.
- Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
- Han JH, Vasilevskis EE, Ely EW. Sedation and delirium. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:704-717.
- Rosen T, Connors S, Halpern A, et al. Improving emergency department identification and management of agitated delirium in older adults: Implementation and impact assessment of a comprehensive clinical protocol using an A-B-C-D-E-F mnemonic. Ann Emerg Med. 2013;62(4)(Supp 4):S53-54.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
- Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
- Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23(1):20-25.
- Weaver LK. Carbon monoxide poisoning. New Engl J Med. 2009;360(12):1217-1225.
- Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric therapy for acute carbon monoxide poisoning. New Engl J Med. 2002;347(14):1057-1067.
- Touger M, Birnbaum A, Wang J, Chou K, Pearson D, Bijur P. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):382-388.
- ICD-9Data.com Web site. 2014 ICD-9-CM Diagnosis Codes. http://www.icd9data.com/2014/Volume1/default.htm. Accessed December 4, 2014.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
- Han JH, Wilson A, Ely EW. Delirium in the older emergency department patient: a quiet epidemic. Emerg Med Clin North Am. 2010;28(3):611-631.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
- Mulcare MR, Halpern A, Stern ME. The geriatric patient. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:741-753.
- Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193-200.
- Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
- Han JH, Vasilevskis EE, Ely EW. Sedation and delirium. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:704-717.
- Rosen T, Connors S, Halpern A, et al. Improving emergency department identification and management of agitated delirium in older adults: Implementation and impact assessment of a comprehensive clinical protocol using an A-B-C-D-E-F mnemonic. Ann Emerg Med. 2013;62(4)(Supp 4):S53-54.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
- Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
- Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23(1):20-25.
- Weaver LK. Carbon monoxide poisoning. New Engl J Med. 2009;360(12):1217-1225.
- Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric therapy for acute carbon monoxide poisoning. New Engl J Med. 2002;347(14):1057-1067.
- Touger M, Birnbaum A, Wang J, Chou K, Pearson D, Bijur P. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):382-388.