User login
The New Opioid Epidemic: Prescriptions, Synthetics, and Street Drugs
Opioid misuse, which often is the result of a prescription written for a very painful condition, has created an epidemic of opioid abuse, addiction, and fatalities across the United States. To reduce the risks from prescribed opioids, regulators and public health authorities have implemented intensive risk mitigation programs, prescription-monitoring programs, and prescribing guidelines.
Clinicians have been encouraged to manage acute and chronic pain more comprehensively. Concurrently, pharmaceutical companies have introduced tamper-resistant formulations, also known as abuse-deterrent formulations, intended to limit manipulation of the contents for insufflation or injection. Although some of these formulations have made tampering difficult, overall they have not effectively reduced inappropriate use or abuse.
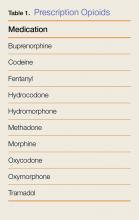
All of these interventions have resulted in a reduction in the availability of affordable, commercially available pharmaceutical opioids (Table 1). Simultaneously, other prescription opioid users have found that the analgesic or euphoric effects of their prescription opioids were no longer sufficient, due to opioid tolerance and hyperalgesia. Both of these forces are driving opioid users to seek more potent opioid products and higher doses to achieve the desired psychoactive and pain-relieving effects.
For these reasons, many opioid users turned to less expensive, readily available, illicitly produced heroin and potent synthetic opioids—mainly fentanyl derivatives. The increased use of heroin and synthetic opioids has resulted in a sharp rise in overdoses and deaths, which continue to be a daily presentation in EDs throughout the country.
This review describes the emergence of the new synthetic opioids, and the steps emergency physicians (EPs) can take to identify and manage ED patients who have been exposed to these agents.
Case
A 34-year-old woman with a history of opioid-use disorder was found unresponsive by a family member who immediately called emergency medical services (EMS). Upon arrival, the emergency medical technicians noted the patient’s agonal respiration and pinpoint pupils. They immediately provided assisted ventilations via a bag-valve-mask (BVM) and administered 2 mg of intranasal naloxone prior to transport. The patient remained unresponsive, with no improvement in her respiratory status.
Upon arrival at the ED, the patient was still comatose, and her pupils remained pinpoint. Vital signs at presentation were: heart rate, 48 beats/min; blood pressure, 70/40 mm Hg; agonal respiration; and temperature, 98.2°F. Oxygen saturation was 86% while receiving assisted ventilation through BVM. An intravenous (IV) line was established.
What is the differential diagnosis of this toxidrome in the current era of emerging drugs of abuse?
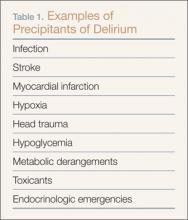
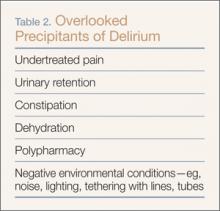
The differential diagnosis of a patient with pinpoint pupils and respiratory depression who does not respond to naloxone typically includes overdose with gamma-hydroxybutyrate, clonidine, or the combined use of sedative-hypnotic agents with ethanol (organophosphate exposure and pontine strokes are two other causes). Naloxone administration may help diagnose opioids as a cause, and, in the past, a lack of response to naloxone was used to help exclude opioids as a cause. However, opioid poisoning should no longer be excluded from consideration in the differential diagnosis when patients are nonresponsive to naloxone. Patients who combine the use of opioids with another sedative hypnotic or who develop hypoxic encephalopathy following opioid overdose may not respond to naloxone with arousal. Most important, the emergence of ultra-potent synthetic opioid use raises the possibility that a patient may appear to be resistant to naloxone due to the extreme potency of these drugs, but may respond to extremely large doses of naloxone. These new opioids pose a grave public health threat and have already resulted in hundreds, if not thousands, of deaths.1
What are novel synthetic opioids?
Unlike heroin, which requires harvesting of plant-derived opium, the novel synthetic opioids are synthesized in laboratories, primarily in China, and shipped to the United States through commercial channels (eg, US Postal Service).2,3 Over the past few years, novel synthetic opioids have been supplementing or replacing heroin sold on the illicit market.1 Most of these novel synthetic opioids are fentanyl analogs (Table 2) that are purchased in bulk on the “Darknet”—an area hidden deep in the Internet (not discoverable by the common major search engines) that allows users to engage in questionable, even illegal, activities utilizing nontraceable currencies such as Bitcoin.4
At the local level, dealers may seek to attract heroin users by adulterating, or even replacing, heroin with fentanyl or novel synthetic opioids, marketing it as a “high-quality” heroin offering more rapid, intense effects. These fentanyl analogs are often hundreds of times more potent than fentanyl, and therefore thousands of times more potent than heroin. Only a miniscule amount increases the perceived potency of the “heroin,” allowing dealers to increase their profit margins.
Selling and using novel synthetic opioids leave little room for error, and small dosing miscalculations have resulted in profound overdoses and deaths. Obviously, the quality control, contents, and dose uniformity of illicitly traded products are poor, adding to the risks of use. In some cases, the novel synthetic opioids are pressed into tablets and marketed as diverted prescription opioids or benzodiazepines. In many, if not most, circumstances, intermediary dealers, as well as users, may be unaware of the product’s contents.5,6 Carfentanil, used as a large-animal tranquilizer, is reportedly 10,000 times more potent than morphine and has recently been implicated in a cluster of deaths of opioid users in the Midwest.7,8 Other synthetic opioids coming to market were initially developed for laboratory research, including W18, which was identified in Canada; and U47700, an opioid identified on autopsy of the musician Prince3,9 (Table 2).
Novel synthetic opioids can be identified only by specific, specialized assays not available in clinical settings. Because their molecular structures differ substantially from morphine, these compounds skirt identification by standard urine “opiate” drug screens. With the exception of fentanyl, pharmacokinetic data for the use of the majority of these agents in humans is unknown.
How are patients who present to EDs with an opioid toxidrome managed in practice today?
Classic teaching for the management of opioid-induced respiratory depression in adults is to provide ventilatory support (ie, BVM or intubation) or administer a low dose of naloxone (0.04 mg IV every 2-5 minutes, up to 2 mg) until adequate respirations are restored. This approach is reasonable for patients exposed to heroin or fentanyl, and provides safer reversal in the ED than administration of a large bolus dose of 0.4 or 2 mg naloxone in opioid-dependent patients.
However, patients exposed to novel synthetic opioids may ultimately require higher than usual doses of naloxone to achieve reversal—reportedly IV doses as high as 6 to 10 mg or more.10 It is not yet fully understood if the need for high-dose naloxone is due to the binding affinity of the opioid or the relatively high dose of opioid administered.
Because the clinical effects of the novel synthetic opioids are generally indistinguishable from those of other opioids, providing respiratory support in the ED remains a critical intervention while awaiting the effect of titrated doses of naloxone. Of concern, though, is that these opioids are so potent that they may cause immediate respiratory arrest, resulting in a more rapid progression to cardiac arrest, limiting the ability to administer rescue breathing or antidote.
In the “bystander” setting, administration of a larger initial dose of naloxone may be reasonable, given the lack of advanced medical supportive care. However, the ability to provide larger doses in these settings is hampered by the accessibility of the antidote. In addition, prehospital-care providers need to consider the possibility of precipitating opioid withdrawal in patients with opioid dependence, which itself can carry significant consequences (eg, aspiration, agitated delirium), as well as the subsequent uncooperativeness of the victim, who may attempt to leave the scene and self-administer an additional dose of opioid or develop recurrent respiratory depression when the naloxone wanes. Since many patients with life-threatening opioid intoxication will suffer long-term consequences if reversal is delayed, the risk of administering high-dose naloxone in the bystander setting generally is worthwhile. However, the risks and benefits of naloxone must still be thoughtfully considered by prehospital-care providers who can provide alternative supportive therapies.
In the ED, the EP must decide whether to intubate the patient directly or first give a brief trial of low-dose naloxone. If a trial of naloxone is unsuccessful at reversing the respiratory depression, dose escalation can be tried while supporting oxygenation and ventilation noninvasively. Administration of naloxone postintubation is not usually necessary or even desired, since respiratory depression, the primary mechanism of death, has been addressed.
Are any special precautions required for health care workers?
Some of the ultra-potent synthetic opioids are available as powders or sprays that can be inadvertently absorbed through the skin (after dissolution in skin moisture) or inhaled.8 The safety of health care providers and law enforcement personnel who may be exposed to synthetic opioids in this manner is currently unknown, though some law enforcement and public health agencies have published warnings in an effort to be proactively cautious.8
While it is highly unlikely that the handling of body fluids of opioid-intoxicated patients poses any health threats, universal safety precautions of wearing disposable gloves should be utilized. As noted, contact with the actual substances may be more concerning, particularly when airborne; in such situations, a particulate mask should also be utilized. Although fentanyl in liquid formulation can slowly enter the skin transdermally (eg, fentanyl patch), there are very limited data to either support or refute the ability of the newer potent opioids to do so. Until more data on these opioid analogs become available, those entering grossly contaminated areas, in which dermal or inhalational exposure is high, should employ a higher level of personal safety precautions.11 In addition, naloxone should be readily available.
How can we detect novel opioid use?
As noted, there is no ability to specifically detect the use of novel potent opioids in the clinical setting (eg, hospital laboratory); therefore, clinicians must maintain a high level of suspicion and provide care empirically. The ability to make a specific diagnosis is further clouded because a patient who has used a synthetic opioid may have also used certain prescription opioids or heroin, which can be detected by standard testing.
Blood and urine samples obtained early in care and sent to specialized laboratories may provide specific identification. Such testing is typically only done by reference laboratories, health departments, or law enforcement agencies. The information obtained from these analyses may help to understand the epidemiology of novel opioid abuse, prevent others from succumbing to addiction, and determine the cause of related deaths.
Which patients can be safely discharged from the ED after an opioid overdose?
Patients who survive reversal of an opioid overdose, whether from a conventional or novel opioid, are at extremely high risk of subsequent death from continued use, as well as from the initial exposure to a long-acting opioid that outlasts the reversal effects of naloxone. Such patients should undergo a sufficient observation period after the last dose of naloxone has been administered to allow its effects to dissipate. This is likely at least 2 hours, but may be longer in certain individuals. Attempts at establishing a link for the patient to long-term treatment or (where available) providing a naloxone rescue kit and training to patients and their families are worthwhile. Although some data support releasing responsive patients after a short, but safe interval after naloxone administration, the changing landscape of opioid use should prompt reconsideration of such practices.12
To whom should suspected opioid overdose patients be reported?
While most EPs are familiar with the management of patients with opioid-induced respiratory depression, atypical cases (eg, patients less responsive to naloxone, those who suffer cardiac arrest) or clusters of suspected cases should always be reported to a regional poison control center (PCC) or health department. The PCC is typically engaged in surveillance and works cooperatively with area EDs and public health officials to track and notify physicians of emerging trends. The epidemiological data derived from reports from a variety of hospitals allow health officials to effectively engage resources for public warnings, facilitate forensic identification of circulating products, and determine any unique clinical information that can then be broadly disseminated.
Case Conclusion
The patient was supported with BVM ventilations. Despite additional titrated IV naloxone (up to a total of 4 mg) the patient was nonresponsive and unarousable. She was intubated, and awoke several hours later. She fully recovered and subsequently was referred to both a harm-reduction and an opioid detoxification program. Analysis of her blood and urine, available several weeks later, confirmed an exposure to U47700.
1. Centers for Disease Control and Prevention. Health Alert Network. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. https://emergency.cdc.gov/han/han00384.asp. Updated October 26, 2015. Accessed January 10, 2017.
2. MacQuarrie B. Synthetic opioids are getting into US by mail. Boston Globe. December 27, 2016. http://www.bostonglobe.com/metro/2016/12/26/synthetic-opioids-slipping-into-via-mail-security-experts-say/23TCEuIES8aEQYAWWHKCiI/story.html. Accessed January 10, 2017.
3. Lucyk SN, Nelson LS. Novel synthetic opioids: an opioid epidemic within an opioid epidemic. Ann Emerg Med. 2017;69(1):91-93. doi:10.1016/j.annemergmed.2016.08.445.
4. Mounteney J, Bo A, Oteo A; OteoEuropean Monitoring Centre for Drugs and Drug Addiction project group. The Internet and Drug Markets. Publications Office of the European Union, Luxembourg, Luxembourg; 2016:1-136. http://www.emcdda.europa.eu/system/files/publications/2155/TDXD16001ENN_FINAL. pdf. doi:10.2810/324608. Accessed January 17, 2017.
5. Associated Press. ‘Norco’ fentanyl overdose deaths rise to 14; problem spreads to Bay Area. Los Angeles Times. April 26, 2016. http://www.latimes.com/local/lanow/la-me-ln-norco-fentanyl-overdose-deaths-rise-to-14-problem-spreads-to-bay-area-20160426-story.html.
6. Centers for Disease Control and Prevention. Health Alert Network. Influx of fentanyl-laced counterfeit pills and toxic fentanyl-related compounds further increases risk of fentanyl-related overdose and fatalities. https://emergency.cdc.gov/han/han00395.asp. Accessed January 10, 2017.
7. Sandy E. Cleveland Scene. 236 heroin overdoses in Akron in 3 weeks; heroin being cut with elephant sedative. http://www.clevescene.com/scene-and-heard/archives/2016/07/14/akron-police-chief-heroin-being-cut-with-elephant-sedative-88-overdoses-since-july-5. Accessed January 10, 2017.
8. DEA issues carfentanil warning to police and public [news release]. Washington, DC: United States Drug Enforcement Administration; September 22, 2016. https://www.dea.gov/divisions/hq/2016/hq092216.shtml. Accessed January 10, 2017.
9. Armenian P, Olson A, Anaya A, Kurtz A, Ruegner R, Gerona RR. Fentanyl and a novel synthetic opioid U-47700 masquerading as street “Norco” in Central California: a case report. Ann Emerg Med. 2017;69(1):87-90. doi:10.1016/j.annemergmed.2016.06.014.
10. Schumann H, Erickson T, Thompson TM, Zautcke JL, Denton JS. Fentanyl epidemic in Chicago, Illinois and surrounding Cook County. Clin Toxicol (Phila). 2008;46(6):501-506. doi:10.1080/15563650701877374.
11. George AV, Lu JJ, Pisano MV, Metz J, Erickson TB. Carfentanil—an ultra potent opioid. Am J Emerg Med. 2010;28(4):530-532. doi:10.1016/j.ajem.2010.03.003.
12. Kolinsky D, Keim SM, Cohn BG, Schwarz ES, Yealy DM. Is a prehospital treat and release protocol for opioid overdose safe? J Emerg Med. 2017;52(1):52-58. doi:10.1016/j.jemermed.2016.09.015.
Opioid misuse, which often is the result of a prescription written for a very painful condition, has created an epidemic of opioid abuse, addiction, and fatalities across the United States. To reduce the risks from prescribed opioids, regulators and public health authorities have implemented intensive risk mitigation programs, prescription-monitoring programs, and prescribing guidelines.
Clinicians have been encouraged to manage acute and chronic pain more comprehensively. Concurrently, pharmaceutical companies have introduced tamper-resistant formulations, also known as abuse-deterrent formulations, intended to limit manipulation of the contents for insufflation or injection. Although some of these formulations have made tampering difficult, overall they have not effectively reduced inappropriate use or abuse.
All of these interventions have resulted in a reduction in the availability of affordable, commercially available pharmaceutical opioids (Table 1). Simultaneously, other prescription opioid users have found that the analgesic or euphoric effects of their prescription opioids were no longer sufficient, due to opioid tolerance and hyperalgesia. Both of these forces are driving opioid users to seek more potent opioid products and higher doses to achieve the desired psychoactive and pain-relieving effects.
For these reasons, many opioid users turned to less expensive, readily available, illicitly produced heroin and potent synthetic opioids—mainly fentanyl derivatives. The increased use of heroin and synthetic opioids has resulted in a sharp rise in overdoses and deaths, which continue to be a daily presentation in EDs throughout the country.
This review describes the emergence of the new synthetic opioids, and the steps emergency physicians (EPs) can take to identify and manage ED patients who have been exposed to these agents.
Case
A 34-year-old woman with a history of opioid-use disorder was found unresponsive by a family member who immediately called emergency medical services (EMS). Upon arrival, the emergency medical technicians noted the patient’s agonal respiration and pinpoint pupils. They immediately provided assisted ventilations via a bag-valve-mask (BVM) and administered 2 mg of intranasal naloxone prior to transport. The patient remained unresponsive, with no improvement in her respiratory status.
Upon arrival at the ED, the patient was still comatose, and her pupils remained pinpoint. Vital signs at presentation were: heart rate, 48 beats/min; blood pressure, 70/40 mm Hg; agonal respiration; and temperature, 98.2°F. Oxygen saturation was 86% while receiving assisted ventilation through BVM. An intravenous (IV) line was established.
What is the differential diagnosis of this toxidrome in the current era of emerging drugs of abuse?
The differential diagnosis of a patient with pinpoint pupils and respiratory depression who does not respond to naloxone typically includes overdose with gamma-hydroxybutyrate, clonidine, or the combined use of sedative-hypnotic agents with ethanol (organophosphate exposure and pontine strokes are two other causes). Naloxone administration may help diagnose opioids as a cause, and, in the past, a lack of response to naloxone was used to help exclude opioids as a cause. However, opioid poisoning should no longer be excluded from consideration in the differential diagnosis when patients are nonresponsive to naloxone. Patients who combine the use of opioids with another sedative hypnotic or who develop hypoxic encephalopathy following opioid overdose may not respond to naloxone with arousal. Most important, the emergence of ultra-potent synthetic opioid use raises the possibility that a patient may appear to be resistant to naloxone due to the extreme potency of these drugs, but may respond to extremely large doses of naloxone. These new opioids pose a grave public health threat and have already resulted in hundreds, if not thousands, of deaths.1
What are novel synthetic opioids?
Unlike heroin, which requires harvesting of plant-derived opium, the novel synthetic opioids are synthesized in laboratories, primarily in China, and shipped to the United States through commercial channels (eg, US Postal Service).2,3 Over the past few years, novel synthetic opioids have been supplementing or replacing heroin sold on the illicit market.1 Most of these novel synthetic opioids are fentanyl analogs (Table 2) that are purchased in bulk on the “Darknet”—an area hidden deep in the Internet (not discoverable by the common major search engines) that allows users to engage in questionable, even illegal, activities utilizing nontraceable currencies such as Bitcoin.4
At the local level, dealers may seek to attract heroin users by adulterating, or even replacing, heroin with fentanyl or novel synthetic opioids, marketing it as a “high-quality” heroin offering more rapid, intense effects. These fentanyl analogs are often hundreds of times more potent than fentanyl, and therefore thousands of times more potent than heroin. Only a miniscule amount increases the perceived potency of the “heroin,” allowing dealers to increase their profit margins.
Selling and using novel synthetic opioids leave little room for error, and small dosing miscalculations have resulted in profound overdoses and deaths. Obviously, the quality control, contents, and dose uniformity of illicitly traded products are poor, adding to the risks of use. In some cases, the novel synthetic opioids are pressed into tablets and marketed as diverted prescription opioids or benzodiazepines. In many, if not most, circumstances, intermediary dealers, as well as users, may be unaware of the product’s contents.5,6 Carfentanil, used as a large-animal tranquilizer, is reportedly 10,000 times more potent than morphine and has recently been implicated in a cluster of deaths of opioid users in the Midwest.7,8 Other synthetic opioids coming to market were initially developed for laboratory research, including W18, which was identified in Canada; and U47700, an opioid identified on autopsy of the musician Prince3,9 (Table 2).
Novel synthetic opioids can be identified only by specific, specialized assays not available in clinical settings. Because their molecular structures differ substantially from morphine, these compounds skirt identification by standard urine “opiate” drug screens. With the exception of fentanyl, pharmacokinetic data for the use of the majority of these agents in humans is unknown.
How are patients who present to EDs with an opioid toxidrome managed in practice today?
Classic teaching for the management of opioid-induced respiratory depression in adults is to provide ventilatory support (ie, BVM or intubation) or administer a low dose of naloxone (0.04 mg IV every 2-5 minutes, up to 2 mg) until adequate respirations are restored. This approach is reasonable for patients exposed to heroin or fentanyl, and provides safer reversal in the ED than administration of a large bolus dose of 0.4 or 2 mg naloxone in opioid-dependent patients.
However, patients exposed to novel synthetic opioids may ultimately require higher than usual doses of naloxone to achieve reversal—reportedly IV doses as high as 6 to 10 mg or more.10 It is not yet fully understood if the need for high-dose naloxone is due to the binding affinity of the opioid or the relatively high dose of opioid administered.
Because the clinical effects of the novel synthetic opioids are generally indistinguishable from those of other opioids, providing respiratory support in the ED remains a critical intervention while awaiting the effect of titrated doses of naloxone. Of concern, though, is that these opioids are so potent that they may cause immediate respiratory arrest, resulting in a more rapid progression to cardiac arrest, limiting the ability to administer rescue breathing or antidote.
In the “bystander” setting, administration of a larger initial dose of naloxone may be reasonable, given the lack of advanced medical supportive care. However, the ability to provide larger doses in these settings is hampered by the accessibility of the antidote. In addition, prehospital-care providers need to consider the possibility of precipitating opioid withdrawal in patients with opioid dependence, which itself can carry significant consequences (eg, aspiration, agitated delirium), as well as the subsequent uncooperativeness of the victim, who may attempt to leave the scene and self-administer an additional dose of opioid or develop recurrent respiratory depression when the naloxone wanes. Since many patients with life-threatening opioid intoxication will suffer long-term consequences if reversal is delayed, the risk of administering high-dose naloxone in the bystander setting generally is worthwhile. However, the risks and benefits of naloxone must still be thoughtfully considered by prehospital-care providers who can provide alternative supportive therapies.
In the ED, the EP must decide whether to intubate the patient directly or first give a brief trial of low-dose naloxone. If a trial of naloxone is unsuccessful at reversing the respiratory depression, dose escalation can be tried while supporting oxygenation and ventilation noninvasively. Administration of naloxone postintubation is not usually necessary or even desired, since respiratory depression, the primary mechanism of death, has been addressed.
Are any special precautions required for health care workers?
Some of the ultra-potent synthetic opioids are available as powders or sprays that can be inadvertently absorbed through the skin (after dissolution in skin moisture) or inhaled.8 The safety of health care providers and law enforcement personnel who may be exposed to synthetic opioids in this manner is currently unknown, though some law enforcement and public health agencies have published warnings in an effort to be proactively cautious.8
While it is highly unlikely that the handling of body fluids of opioid-intoxicated patients poses any health threats, universal safety precautions of wearing disposable gloves should be utilized. As noted, contact with the actual substances may be more concerning, particularly when airborne; in such situations, a particulate mask should also be utilized. Although fentanyl in liquid formulation can slowly enter the skin transdermally (eg, fentanyl patch), there are very limited data to either support or refute the ability of the newer potent opioids to do so. Until more data on these opioid analogs become available, those entering grossly contaminated areas, in which dermal or inhalational exposure is high, should employ a higher level of personal safety precautions.11 In addition, naloxone should be readily available.
How can we detect novel opioid use?
As noted, there is no ability to specifically detect the use of novel potent opioids in the clinical setting (eg, hospital laboratory); therefore, clinicians must maintain a high level of suspicion and provide care empirically. The ability to make a specific diagnosis is further clouded because a patient who has used a synthetic opioid may have also used certain prescription opioids or heroin, which can be detected by standard testing.
Blood and urine samples obtained early in care and sent to specialized laboratories may provide specific identification. Such testing is typically only done by reference laboratories, health departments, or law enforcement agencies. The information obtained from these analyses may help to understand the epidemiology of novel opioid abuse, prevent others from succumbing to addiction, and determine the cause of related deaths.
Which patients can be safely discharged from the ED after an opioid overdose?
Patients who survive reversal of an opioid overdose, whether from a conventional or novel opioid, are at extremely high risk of subsequent death from continued use, as well as from the initial exposure to a long-acting opioid that outlasts the reversal effects of naloxone. Such patients should undergo a sufficient observation period after the last dose of naloxone has been administered to allow its effects to dissipate. This is likely at least 2 hours, but may be longer in certain individuals. Attempts at establishing a link for the patient to long-term treatment or (where available) providing a naloxone rescue kit and training to patients and their families are worthwhile. Although some data support releasing responsive patients after a short, but safe interval after naloxone administration, the changing landscape of opioid use should prompt reconsideration of such practices.12
To whom should suspected opioid overdose patients be reported?
While most EPs are familiar with the management of patients with opioid-induced respiratory depression, atypical cases (eg, patients less responsive to naloxone, those who suffer cardiac arrest) or clusters of suspected cases should always be reported to a regional poison control center (PCC) or health department. The PCC is typically engaged in surveillance and works cooperatively with area EDs and public health officials to track and notify physicians of emerging trends. The epidemiological data derived from reports from a variety of hospitals allow health officials to effectively engage resources for public warnings, facilitate forensic identification of circulating products, and determine any unique clinical information that can then be broadly disseminated.
Case Conclusion
The patient was supported with BVM ventilations. Despite additional titrated IV naloxone (up to a total of 4 mg) the patient was nonresponsive and unarousable. She was intubated, and awoke several hours later. She fully recovered and subsequently was referred to both a harm-reduction and an opioid detoxification program. Analysis of her blood and urine, available several weeks later, confirmed an exposure to U47700.
Opioid misuse, which often is the result of a prescription written for a very painful condition, has created an epidemic of opioid abuse, addiction, and fatalities across the United States. To reduce the risks from prescribed opioids, regulators and public health authorities have implemented intensive risk mitigation programs, prescription-monitoring programs, and prescribing guidelines.
Clinicians have been encouraged to manage acute and chronic pain more comprehensively. Concurrently, pharmaceutical companies have introduced tamper-resistant formulations, also known as abuse-deterrent formulations, intended to limit manipulation of the contents for insufflation or injection. Although some of these formulations have made tampering difficult, overall they have not effectively reduced inappropriate use or abuse.
All of these interventions have resulted in a reduction in the availability of affordable, commercially available pharmaceutical opioids (Table 1). Simultaneously, other prescription opioid users have found that the analgesic or euphoric effects of their prescription opioids were no longer sufficient, due to opioid tolerance and hyperalgesia. Both of these forces are driving opioid users to seek more potent opioid products and higher doses to achieve the desired psychoactive and pain-relieving effects.
For these reasons, many opioid users turned to less expensive, readily available, illicitly produced heroin and potent synthetic opioids—mainly fentanyl derivatives. The increased use of heroin and synthetic opioids has resulted in a sharp rise in overdoses and deaths, which continue to be a daily presentation in EDs throughout the country.
This review describes the emergence of the new synthetic opioids, and the steps emergency physicians (EPs) can take to identify and manage ED patients who have been exposed to these agents.
Case
A 34-year-old woman with a history of opioid-use disorder was found unresponsive by a family member who immediately called emergency medical services (EMS). Upon arrival, the emergency medical technicians noted the patient’s agonal respiration and pinpoint pupils. They immediately provided assisted ventilations via a bag-valve-mask (BVM) and administered 2 mg of intranasal naloxone prior to transport. The patient remained unresponsive, with no improvement in her respiratory status.
Upon arrival at the ED, the patient was still comatose, and her pupils remained pinpoint. Vital signs at presentation were: heart rate, 48 beats/min; blood pressure, 70/40 mm Hg; agonal respiration; and temperature, 98.2°F. Oxygen saturation was 86% while receiving assisted ventilation through BVM. An intravenous (IV) line was established.
What is the differential diagnosis of this toxidrome in the current era of emerging drugs of abuse?
The differential diagnosis of a patient with pinpoint pupils and respiratory depression who does not respond to naloxone typically includes overdose with gamma-hydroxybutyrate, clonidine, or the combined use of sedative-hypnotic agents with ethanol (organophosphate exposure and pontine strokes are two other causes). Naloxone administration may help diagnose opioids as a cause, and, in the past, a lack of response to naloxone was used to help exclude opioids as a cause. However, opioid poisoning should no longer be excluded from consideration in the differential diagnosis when patients are nonresponsive to naloxone. Patients who combine the use of opioids with another sedative hypnotic or who develop hypoxic encephalopathy following opioid overdose may not respond to naloxone with arousal. Most important, the emergence of ultra-potent synthetic opioid use raises the possibility that a patient may appear to be resistant to naloxone due to the extreme potency of these drugs, but may respond to extremely large doses of naloxone. These new opioids pose a grave public health threat and have already resulted in hundreds, if not thousands, of deaths.1
What are novel synthetic opioids?
Unlike heroin, which requires harvesting of plant-derived opium, the novel synthetic opioids are synthesized in laboratories, primarily in China, and shipped to the United States through commercial channels (eg, US Postal Service).2,3 Over the past few years, novel synthetic opioids have been supplementing or replacing heroin sold on the illicit market.1 Most of these novel synthetic opioids are fentanyl analogs (Table 2) that are purchased in bulk on the “Darknet”—an area hidden deep in the Internet (not discoverable by the common major search engines) that allows users to engage in questionable, even illegal, activities utilizing nontraceable currencies such as Bitcoin.4
At the local level, dealers may seek to attract heroin users by adulterating, or even replacing, heroin with fentanyl or novel synthetic opioids, marketing it as a “high-quality” heroin offering more rapid, intense effects. These fentanyl analogs are often hundreds of times more potent than fentanyl, and therefore thousands of times more potent than heroin. Only a miniscule amount increases the perceived potency of the “heroin,” allowing dealers to increase their profit margins.
Selling and using novel synthetic opioids leave little room for error, and small dosing miscalculations have resulted in profound overdoses and deaths. Obviously, the quality control, contents, and dose uniformity of illicitly traded products are poor, adding to the risks of use. In some cases, the novel synthetic opioids are pressed into tablets and marketed as diverted prescription opioids or benzodiazepines. In many, if not most, circumstances, intermediary dealers, as well as users, may be unaware of the product’s contents.5,6 Carfentanil, used as a large-animal tranquilizer, is reportedly 10,000 times more potent than morphine and has recently been implicated in a cluster of deaths of opioid users in the Midwest.7,8 Other synthetic opioids coming to market were initially developed for laboratory research, including W18, which was identified in Canada; and U47700, an opioid identified on autopsy of the musician Prince3,9 (Table 2).
Novel synthetic opioids can be identified only by specific, specialized assays not available in clinical settings. Because their molecular structures differ substantially from morphine, these compounds skirt identification by standard urine “opiate” drug screens. With the exception of fentanyl, pharmacokinetic data for the use of the majority of these agents in humans is unknown.
How are patients who present to EDs with an opioid toxidrome managed in practice today?
Classic teaching for the management of opioid-induced respiratory depression in adults is to provide ventilatory support (ie, BVM or intubation) or administer a low dose of naloxone (0.04 mg IV every 2-5 minutes, up to 2 mg) until adequate respirations are restored. This approach is reasonable for patients exposed to heroin or fentanyl, and provides safer reversal in the ED than administration of a large bolus dose of 0.4 or 2 mg naloxone in opioid-dependent patients.
However, patients exposed to novel synthetic opioids may ultimately require higher than usual doses of naloxone to achieve reversal—reportedly IV doses as high as 6 to 10 mg or more.10 It is not yet fully understood if the need for high-dose naloxone is due to the binding affinity of the opioid or the relatively high dose of opioid administered.
Because the clinical effects of the novel synthetic opioids are generally indistinguishable from those of other opioids, providing respiratory support in the ED remains a critical intervention while awaiting the effect of titrated doses of naloxone. Of concern, though, is that these opioids are so potent that they may cause immediate respiratory arrest, resulting in a more rapid progression to cardiac arrest, limiting the ability to administer rescue breathing or antidote.
In the “bystander” setting, administration of a larger initial dose of naloxone may be reasonable, given the lack of advanced medical supportive care. However, the ability to provide larger doses in these settings is hampered by the accessibility of the antidote. In addition, prehospital-care providers need to consider the possibility of precipitating opioid withdrawal in patients with opioid dependence, which itself can carry significant consequences (eg, aspiration, agitated delirium), as well as the subsequent uncooperativeness of the victim, who may attempt to leave the scene and self-administer an additional dose of opioid or develop recurrent respiratory depression when the naloxone wanes. Since many patients with life-threatening opioid intoxication will suffer long-term consequences if reversal is delayed, the risk of administering high-dose naloxone in the bystander setting generally is worthwhile. However, the risks and benefits of naloxone must still be thoughtfully considered by prehospital-care providers who can provide alternative supportive therapies.
In the ED, the EP must decide whether to intubate the patient directly or first give a brief trial of low-dose naloxone. If a trial of naloxone is unsuccessful at reversing the respiratory depression, dose escalation can be tried while supporting oxygenation and ventilation noninvasively. Administration of naloxone postintubation is not usually necessary or even desired, since respiratory depression, the primary mechanism of death, has been addressed.
Are any special precautions required for health care workers?
Some of the ultra-potent synthetic opioids are available as powders or sprays that can be inadvertently absorbed through the skin (after dissolution in skin moisture) or inhaled.8 The safety of health care providers and law enforcement personnel who may be exposed to synthetic opioids in this manner is currently unknown, though some law enforcement and public health agencies have published warnings in an effort to be proactively cautious.8
While it is highly unlikely that the handling of body fluids of opioid-intoxicated patients poses any health threats, universal safety precautions of wearing disposable gloves should be utilized. As noted, contact with the actual substances may be more concerning, particularly when airborne; in such situations, a particulate mask should also be utilized. Although fentanyl in liquid formulation can slowly enter the skin transdermally (eg, fentanyl patch), there are very limited data to either support or refute the ability of the newer potent opioids to do so. Until more data on these opioid analogs become available, those entering grossly contaminated areas, in which dermal or inhalational exposure is high, should employ a higher level of personal safety precautions.11 In addition, naloxone should be readily available.
How can we detect novel opioid use?
As noted, there is no ability to specifically detect the use of novel potent opioids in the clinical setting (eg, hospital laboratory); therefore, clinicians must maintain a high level of suspicion and provide care empirically. The ability to make a specific diagnosis is further clouded because a patient who has used a synthetic opioid may have also used certain prescription opioids or heroin, which can be detected by standard testing.
Blood and urine samples obtained early in care and sent to specialized laboratories may provide specific identification. Such testing is typically only done by reference laboratories, health departments, or law enforcement agencies. The information obtained from these analyses may help to understand the epidemiology of novel opioid abuse, prevent others from succumbing to addiction, and determine the cause of related deaths.
Which patients can be safely discharged from the ED after an opioid overdose?
Patients who survive reversal of an opioid overdose, whether from a conventional or novel opioid, are at extremely high risk of subsequent death from continued use, as well as from the initial exposure to a long-acting opioid that outlasts the reversal effects of naloxone. Such patients should undergo a sufficient observation period after the last dose of naloxone has been administered to allow its effects to dissipate. This is likely at least 2 hours, but may be longer in certain individuals. Attempts at establishing a link for the patient to long-term treatment or (where available) providing a naloxone rescue kit and training to patients and their families are worthwhile. Although some data support releasing responsive patients after a short, but safe interval after naloxone administration, the changing landscape of opioid use should prompt reconsideration of such practices.12
To whom should suspected opioid overdose patients be reported?
While most EPs are familiar with the management of patients with opioid-induced respiratory depression, atypical cases (eg, patients less responsive to naloxone, those who suffer cardiac arrest) or clusters of suspected cases should always be reported to a regional poison control center (PCC) or health department. The PCC is typically engaged in surveillance and works cooperatively with area EDs and public health officials to track and notify physicians of emerging trends. The epidemiological data derived from reports from a variety of hospitals allow health officials to effectively engage resources for public warnings, facilitate forensic identification of circulating products, and determine any unique clinical information that can then be broadly disseminated.
Case Conclusion
The patient was supported with BVM ventilations. Despite additional titrated IV naloxone (up to a total of 4 mg) the patient was nonresponsive and unarousable. She was intubated, and awoke several hours later. She fully recovered and subsequently was referred to both a harm-reduction and an opioid detoxification program. Analysis of her blood and urine, available several weeks later, confirmed an exposure to U47700.
1. Centers for Disease Control and Prevention. Health Alert Network. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. https://emergency.cdc.gov/han/han00384.asp. Updated October 26, 2015. Accessed January 10, 2017.
2. MacQuarrie B. Synthetic opioids are getting into US by mail. Boston Globe. December 27, 2016. http://www.bostonglobe.com/metro/2016/12/26/synthetic-opioids-slipping-into-via-mail-security-experts-say/23TCEuIES8aEQYAWWHKCiI/story.html. Accessed January 10, 2017.
3. Lucyk SN, Nelson LS. Novel synthetic opioids: an opioid epidemic within an opioid epidemic. Ann Emerg Med. 2017;69(1):91-93. doi:10.1016/j.annemergmed.2016.08.445.
4. Mounteney J, Bo A, Oteo A; OteoEuropean Monitoring Centre for Drugs and Drug Addiction project group. The Internet and Drug Markets. Publications Office of the European Union, Luxembourg, Luxembourg; 2016:1-136. http://www.emcdda.europa.eu/system/files/publications/2155/TDXD16001ENN_FINAL. pdf. doi:10.2810/324608. Accessed January 17, 2017.
5. Associated Press. ‘Norco’ fentanyl overdose deaths rise to 14; problem spreads to Bay Area. Los Angeles Times. April 26, 2016. http://www.latimes.com/local/lanow/la-me-ln-norco-fentanyl-overdose-deaths-rise-to-14-problem-spreads-to-bay-area-20160426-story.html.
6. Centers for Disease Control and Prevention. Health Alert Network. Influx of fentanyl-laced counterfeit pills and toxic fentanyl-related compounds further increases risk of fentanyl-related overdose and fatalities. https://emergency.cdc.gov/han/han00395.asp. Accessed January 10, 2017.
7. Sandy E. Cleveland Scene. 236 heroin overdoses in Akron in 3 weeks; heroin being cut with elephant sedative. http://www.clevescene.com/scene-and-heard/archives/2016/07/14/akron-police-chief-heroin-being-cut-with-elephant-sedative-88-overdoses-since-july-5. Accessed January 10, 2017.
8. DEA issues carfentanil warning to police and public [news release]. Washington, DC: United States Drug Enforcement Administration; September 22, 2016. https://www.dea.gov/divisions/hq/2016/hq092216.shtml. Accessed January 10, 2017.
9. Armenian P, Olson A, Anaya A, Kurtz A, Ruegner R, Gerona RR. Fentanyl and a novel synthetic opioid U-47700 masquerading as street “Norco” in Central California: a case report. Ann Emerg Med. 2017;69(1):87-90. doi:10.1016/j.annemergmed.2016.06.014.
10. Schumann H, Erickson T, Thompson TM, Zautcke JL, Denton JS. Fentanyl epidemic in Chicago, Illinois and surrounding Cook County. Clin Toxicol (Phila). 2008;46(6):501-506. doi:10.1080/15563650701877374.
11. George AV, Lu JJ, Pisano MV, Metz J, Erickson TB. Carfentanil—an ultra potent opioid. Am J Emerg Med. 2010;28(4):530-532. doi:10.1016/j.ajem.2010.03.003.
12. Kolinsky D, Keim SM, Cohn BG, Schwarz ES, Yealy DM. Is a prehospital treat and release protocol for opioid overdose safe? J Emerg Med. 2017;52(1):52-58. doi:10.1016/j.jemermed.2016.09.015.
1. Centers for Disease Control and Prevention. Health Alert Network. Increases in fentanyl drug confiscations and fentanyl-related overdose fatalities. https://emergency.cdc.gov/han/han00384.asp. Updated October 26, 2015. Accessed January 10, 2017.
2. MacQuarrie B. Synthetic opioids are getting into US by mail. Boston Globe. December 27, 2016. http://www.bostonglobe.com/metro/2016/12/26/synthetic-opioids-slipping-into-via-mail-security-experts-say/23TCEuIES8aEQYAWWHKCiI/story.html. Accessed January 10, 2017.
3. Lucyk SN, Nelson LS. Novel synthetic opioids: an opioid epidemic within an opioid epidemic. Ann Emerg Med. 2017;69(1):91-93. doi:10.1016/j.annemergmed.2016.08.445.
4. Mounteney J, Bo A, Oteo A; OteoEuropean Monitoring Centre for Drugs and Drug Addiction project group. The Internet and Drug Markets. Publications Office of the European Union, Luxembourg, Luxembourg; 2016:1-136. http://www.emcdda.europa.eu/system/files/publications/2155/TDXD16001ENN_FINAL. pdf. doi:10.2810/324608. Accessed January 17, 2017.
5. Associated Press. ‘Norco’ fentanyl overdose deaths rise to 14; problem spreads to Bay Area. Los Angeles Times. April 26, 2016. http://www.latimes.com/local/lanow/la-me-ln-norco-fentanyl-overdose-deaths-rise-to-14-problem-spreads-to-bay-area-20160426-story.html.
6. Centers for Disease Control and Prevention. Health Alert Network. Influx of fentanyl-laced counterfeit pills and toxic fentanyl-related compounds further increases risk of fentanyl-related overdose and fatalities. https://emergency.cdc.gov/han/han00395.asp. Accessed January 10, 2017.
7. Sandy E. Cleveland Scene. 236 heroin overdoses in Akron in 3 weeks; heroin being cut with elephant sedative. http://www.clevescene.com/scene-and-heard/archives/2016/07/14/akron-police-chief-heroin-being-cut-with-elephant-sedative-88-overdoses-since-july-5. Accessed January 10, 2017.
8. DEA issues carfentanil warning to police and public [news release]. Washington, DC: United States Drug Enforcement Administration; September 22, 2016. https://www.dea.gov/divisions/hq/2016/hq092216.shtml. Accessed January 10, 2017.
9. Armenian P, Olson A, Anaya A, Kurtz A, Ruegner R, Gerona RR. Fentanyl and a novel synthetic opioid U-47700 masquerading as street “Norco” in Central California: a case report. Ann Emerg Med. 2017;69(1):87-90. doi:10.1016/j.annemergmed.2016.06.014.
10. Schumann H, Erickson T, Thompson TM, Zautcke JL, Denton JS. Fentanyl epidemic in Chicago, Illinois and surrounding Cook County. Clin Toxicol (Phila). 2008;46(6):501-506. doi:10.1080/15563650701877374.
11. George AV, Lu JJ, Pisano MV, Metz J, Erickson TB. Carfentanil—an ultra potent opioid. Am J Emerg Med. 2010;28(4):530-532. doi:10.1016/j.ajem.2010.03.003.
12. Kolinsky D, Keim SM, Cohn BG, Schwarz ES, Yealy DM. Is a prehospital treat and release protocol for opioid overdose safe? J Emerg Med. 2017;52(1):52-58. doi:10.1016/j.jemermed.2016.09.015.
Case Studies in Toxicology: Managing Missed Methadone
A 53-year-old woman presented to the ED after experiencing a fall. Her medical history was significant for chronic obstructive pulmonary disease, hepatitis, and a remote history of intravenous drug use, for which she had been maintained on methadone for the past 20 years. She reported that she had suffered several “fainting episodes” over the past month, and the morning prior to arrival, had sustained what she thought was a mechanical fall outside of the methadone program she attended. She complained of tenderness on her head but denied any other injuries.
The methadone program had referred the patient to the ED for evaluation, noting to the ED staff that her daily methadone dose of 185 mg had not been dispensed prior to transfer. During evaluation, the patient requested that the emergency physician (EP) provide the methadone dose since the clinic would close prior to her discharge from the ED.
How can requests for methadone be managed in the ED?
Methadone is a long-acting oral opioid that is used for both opioid replacement therapy and pain management. When used to reduce craving in opioid-dependent patients, methadone is administered daily through federally sanctioned methadone maintenance treatment (MMT) programs. Patients who consistently adhere to the required guidelines are given “take home” doses. When used for pain management, methadone is typically administered several times daily and may be prescribed by any provider with an appropriate DEA registration.
When given for MMT, methadone saturates the µ-opioid receptors and hinders their binding and agonism by other opioids such as heroin or oxycodone. Patients in MMT programs are started on a low initial dose and slowly titrated upward as tolerance to the adverse effects (eg, sedation) develop.
How are symptomatic patients with methadone withdrawal treated?
Most methadone programs have limited hours and require that patients who miss a dose wait until the following day to return to the program. This is typically without medical consequence because the high dose dispensed by these programs maintains a therapeutic blood concentration for far longer than the expected delay. Although the half-life of methadone exhibits wide interindividual variability, it generally ranges from 12 hours to more than 40 hours.1 Regardless, patients may feel anxious about potential opioid withdrawal, and this often leads them to access the ED for a missed dose.
The neuropsychiatric symptoms attending withdrawal may precede the objective signs of opioid withdrawal. Patients with objective signs of opioid withdrawal (eg, piloerection, vomiting, diarrhea, dilated pupils) may be sufficiently treated with supportive care alone, using antiemetics, hydration, and sometimes clonidine.
Administration of substitute opioids is problematic due to the patient’s underlying tolerance necessitating careful dose titration. Therefore, direct replacement of methadone in the ED remains controversial, and some EDs have strict policies prohibiting the administration of methadone to patients who have missed an MMT dose. Such policies, which are intended to discourage patients from using the ED as a convenience, may be appropriate given the generally benign—though uncomfortable—course of opioid withdrawal due to abstinence.
Other EDs provide replacement methadone for asymptomatic, treat-and-release patients confirmed to be enrolled in an MMT program when the time to the next dose is likely to be 24 hours or greater from the missed dose. Typically, a dose of no more than 10 mg orally or 10 mg intramuscularly (IM) is recommended, and patients should be advised that they will be receiving only a low dose to sufficient to prevent withdrawal—one that may not have the equivalent effects of the outpatient dose.
Whenever possible, a patient’s MMT program should be contacted and informed of the ED visit. For patients who display objective signs of withdrawal and who cannot be confirmed or who do not participate in an MMT program, 10 mg of methadone IM will prevent uncertainty of drug absorption in the setting of nausea or vomiting. All patients receiving oral methadone should be observed for 1 hour, and those receiving IM methadone should be observed for at least 90 minutes to assess for unexpected sedation.2
Patients encountering circumstances that prevent opioid access (eg, incarceration) and who are not in withdrawal but have gone without opioids for more than 5 days may have a loss of tolerance to their usual doses—whether the medication was obtained through an MMT program or illicitly. Harm-reduction strategies aimed at educating patients on the potential vulnerability to their familiar dosing regimens are warranted to avert inadvertent overdoses in chronic opioid users who are likely to resume illicit opoiod use.
Does this patient need syncope evaluation?
Further complicating the decision regarding ED dispensing of methadone are the effects of the drug on myocardial repolarization. Methadone affects conduction across the hERG potassium rectifier current and can prolong the QTc interval on the surface electrocardiogram (ECG), predisposing a patient to torsade de pointes (TdP). Although there is controversy regarding the role of ECG screening during the enrollment of patients in methadone maintenance clinics, doses above 60 mg, underlying myocardial disease, female sex, and electrolyte disturbances may increase the risk of QT prolongation and TdP.3
Whether there is value in obtaining a screening ECG in a patient receiving an initial dose of methadone in the ED is unclear, and this practice is controversial even among methadone clinics. However, some of the excess death in patients taking methadone may be explained by the dysrhythmogenic potential of methadone.4 An ECG therefore may elucidate a correctable cause in methadone patients presenting with syncope.
Administering methadone to patients with documented QT prolongation must weigh the risk of methadone’s conduction effects against the substantial risks of illicit opioid self-administration. For some patients at-risk for TdP, it may be preferable to use buprenorphine if possible, since it does not carry the same cardiac effects as methadone.1,5 Such therapy requires referral to a physician licensed to prescribe this medication.
How should admitted patients be managed?
While administration of methadone for withdrawal or maintenance therapy in the ED is acceptable, outpatient prescribing of methadone for these reasons is not legal, and only federally regulated clinics may engage in this practice. Hospitalized patients who are enrolled in an MMT program should have their daily methadone dose confirmed and continued—as long as the patient has not lost tolerance. Patients not participating in an MMT program can receive up to 3 days of methadone in the hospital, even if the practitioner is not registered to provide methadone.6 For these patients, it is recommended that the physician order a low dose of methadone and also consult with an addiction specialist to determine whether the patient should continue on MMT maintenance or undergo detoxification.
It is important to note that methadone may be prescribed for pain, but its use in the ED for this purpose is strongly discouraged, especially in patients who have never received methadone previously. For admitted patients requiring such potent opioid analgesia, consultation with a pain service or, when indicated, a palliative care/hospice specialist is warranted as the dosing intervals are different in each setting, and the risk of respiratory depression is high.
Case Conclusion
As requested by the MMT clinic, the patient was administered methadone 185 mg orally in the ED, though a dose of 10 mg would have been sufficient to prevent withdrawal. Unfortunately, the EP did not appreciate the relationship of the markedly prolonged QTc and the methadone, which should have prompted a dose reduction.
Evaluation of the patient’s electrolyte levels, which included magnesium and potassium, were normal. An ECG was repeated 24 hours later and revealed a persistent, but improved, QT interval at 505 ms. The remainder of the syncope workup was negative. Because the patient had no additional symptoms or events during her stay, she was discharged. At discharge, the EP followed up with the MMT clinic to discuss lowering the patient’s daily methadone dose, as well as close cardiology follow-up.
Dr Rao is the chief of the division of medical toxicology at New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at the New York University School of Medicine and the New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board.
- Chou R, Weimer MB, Dana T. Methadone overdose and cardiac arrhythmia potential: findings from a review of the evidence for an American Pain Society and College on Problems of Drug Dependence clinical practice guideline. J Pain. 2014;15(4):338-365.
- National Highway Traffic Safety Administration Web site. Methadone. http://www.nhtsa.gov/people/injury/research/job185drugs/methadone.htm. Accessed August 3, 2015.
- Martin JA, Campbell A, Killip T, et al; Substance Abuse and Mental Health Services Administration. QT interval screening in methadone maintenance treatment: report of a SAMHSA expert panel. J Addict Dis. 2011;30(4):283-306. Erratum in: J Addict Dis. 2012;31(1):91.
- Ray WA, Chung CP, Murray KT, Cooper WO, Hall K, Stein CM. Out-of-hospital mortality among patients receiving methadone for noncancer pain. JAMA Intern Med. 2015;175(3):420-427.
- Davis MP. Twelve reasons for considering buprenorphine as a frontline analgesic in the management of pain. J Support Oncol. 2012;10(6):209-219.
- US Government Printing Office. Federal Digital System. Administering or dispensing of narcotic drugs. Code of Federal Regulations. Title 21 CFR §1306.07. http://www.gpo.gov/fdsys/pkg/CFR-1998-title21-vol9/pdf/CFR-1998-title21-vol9-sec1306-07.pdf. Accessed August 4, 2015.
A 53-year-old woman presented to the ED after experiencing a fall. Her medical history was significant for chronic obstructive pulmonary disease, hepatitis, and a remote history of intravenous drug use, for which she had been maintained on methadone for the past 20 years. She reported that she had suffered several “fainting episodes” over the past month, and the morning prior to arrival, had sustained what she thought was a mechanical fall outside of the methadone program she attended. She complained of tenderness on her head but denied any other injuries.
The methadone program had referred the patient to the ED for evaluation, noting to the ED staff that her daily methadone dose of 185 mg had not been dispensed prior to transfer. During evaluation, the patient requested that the emergency physician (EP) provide the methadone dose since the clinic would close prior to her discharge from the ED.
How can requests for methadone be managed in the ED?
Methadone is a long-acting oral opioid that is used for both opioid replacement therapy and pain management. When used to reduce craving in opioid-dependent patients, methadone is administered daily through federally sanctioned methadone maintenance treatment (MMT) programs. Patients who consistently adhere to the required guidelines are given “take home” doses. When used for pain management, methadone is typically administered several times daily and may be prescribed by any provider with an appropriate DEA registration.
When given for MMT, methadone saturates the µ-opioid receptors and hinders their binding and agonism by other opioids such as heroin or oxycodone. Patients in MMT programs are started on a low initial dose and slowly titrated upward as tolerance to the adverse effects (eg, sedation) develop.
How are symptomatic patients with methadone withdrawal treated?
Most methadone programs have limited hours and require that patients who miss a dose wait until the following day to return to the program. This is typically without medical consequence because the high dose dispensed by these programs maintains a therapeutic blood concentration for far longer than the expected delay. Although the half-life of methadone exhibits wide interindividual variability, it generally ranges from 12 hours to more than 40 hours.1 Regardless, patients may feel anxious about potential opioid withdrawal, and this often leads them to access the ED for a missed dose.
The neuropsychiatric symptoms attending withdrawal may precede the objective signs of opioid withdrawal. Patients with objective signs of opioid withdrawal (eg, piloerection, vomiting, diarrhea, dilated pupils) may be sufficiently treated with supportive care alone, using antiemetics, hydration, and sometimes clonidine.
Administration of substitute opioids is problematic due to the patient’s underlying tolerance necessitating careful dose titration. Therefore, direct replacement of methadone in the ED remains controversial, and some EDs have strict policies prohibiting the administration of methadone to patients who have missed an MMT dose. Such policies, which are intended to discourage patients from using the ED as a convenience, may be appropriate given the generally benign—though uncomfortable—course of opioid withdrawal due to abstinence.
Other EDs provide replacement methadone for asymptomatic, treat-and-release patients confirmed to be enrolled in an MMT program when the time to the next dose is likely to be 24 hours or greater from the missed dose. Typically, a dose of no more than 10 mg orally or 10 mg intramuscularly (IM) is recommended, and patients should be advised that they will be receiving only a low dose to sufficient to prevent withdrawal—one that may not have the equivalent effects of the outpatient dose.
Whenever possible, a patient’s MMT program should be contacted and informed of the ED visit. For patients who display objective signs of withdrawal and who cannot be confirmed or who do not participate in an MMT program, 10 mg of methadone IM will prevent uncertainty of drug absorption in the setting of nausea or vomiting. All patients receiving oral methadone should be observed for 1 hour, and those receiving IM methadone should be observed for at least 90 minutes to assess for unexpected sedation.2
Patients encountering circumstances that prevent opioid access (eg, incarceration) and who are not in withdrawal but have gone without opioids for more than 5 days may have a loss of tolerance to their usual doses—whether the medication was obtained through an MMT program or illicitly. Harm-reduction strategies aimed at educating patients on the potential vulnerability to their familiar dosing regimens are warranted to avert inadvertent overdoses in chronic opioid users who are likely to resume illicit opoiod use.
Does this patient need syncope evaluation?
Further complicating the decision regarding ED dispensing of methadone are the effects of the drug on myocardial repolarization. Methadone affects conduction across the hERG potassium rectifier current and can prolong the QTc interval on the surface electrocardiogram (ECG), predisposing a patient to torsade de pointes (TdP). Although there is controversy regarding the role of ECG screening during the enrollment of patients in methadone maintenance clinics, doses above 60 mg, underlying myocardial disease, female sex, and electrolyte disturbances may increase the risk of QT prolongation and TdP.3
Whether there is value in obtaining a screening ECG in a patient receiving an initial dose of methadone in the ED is unclear, and this practice is controversial even among methadone clinics. However, some of the excess death in patients taking methadone may be explained by the dysrhythmogenic potential of methadone.4 An ECG therefore may elucidate a correctable cause in methadone patients presenting with syncope.
Administering methadone to patients with documented QT prolongation must weigh the risk of methadone’s conduction effects against the substantial risks of illicit opioid self-administration. For some patients at-risk for TdP, it may be preferable to use buprenorphine if possible, since it does not carry the same cardiac effects as methadone.1,5 Such therapy requires referral to a physician licensed to prescribe this medication.
How should admitted patients be managed?
While administration of methadone for withdrawal or maintenance therapy in the ED is acceptable, outpatient prescribing of methadone for these reasons is not legal, and only federally regulated clinics may engage in this practice. Hospitalized patients who are enrolled in an MMT program should have their daily methadone dose confirmed and continued—as long as the patient has not lost tolerance. Patients not participating in an MMT program can receive up to 3 days of methadone in the hospital, even if the practitioner is not registered to provide methadone.6 For these patients, it is recommended that the physician order a low dose of methadone and also consult with an addiction specialist to determine whether the patient should continue on MMT maintenance or undergo detoxification.
It is important to note that methadone may be prescribed for pain, but its use in the ED for this purpose is strongly discouraged, especially in patients who have never received methadone previously. For admitted patients requiring such potent opioid analgesia, consultation with a pain service or, when indicated, a palliative care/hospice specialist is warranted as the dosing intervals are different in each setting, and the risk of respiratory depression is high.
Case Conclusion
As requested by the MMT clinic, the patient was administered methadone 185 mg orally in the ED, though a dose of 10 mg would have been sufficient to prevent withdrawal. Unfortunately, the EP did not appreciate the relationship of the markedly prolonged QTc and the methadone, which should have prompted a dose reduction.
Evaluation of the patient’s electrolyte levels, which included magnesium and potassium, were normal. An ECG was repeated 24 hours later and revealed a persistent, but improved, QT interval at 505 ms. The remainder of the syncope workup was negative. Because the patient had no additional symptoms or events during her stay, she was discharged. At discharge, the EP followed up with the MMT clinic to discuss lowering the patient’s daily methadone dose, as well as close cardiology follow-up.
Dr Rao is the chief of the division of medical toxicology at New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at the New York University School of Medicine and the New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board.
A 53-year-old woman presented to the ED after experiencing a fall. Her medical history was significant for chronic obstructive pulmonary disease, hepatitis, and a remote history of intravenous drug use, for which she had been maintained on methadone for the past 20 years. She reported that she had suffered several “fainting episodes” over the past month, and the morning prior to arrival, had sustained what she thought was a mechanical fall outside of the methadone program she attended. She complained of tenderness on her head but denied any other injuries.
The methadone program had referred the patient to the ED for evaluation, noting to the ED staff that her daily methadone dose of 185 mg had not been dispensed prior to transfer. During evaluation, the patient requested that the emergency physician (EP) provide the methadone dose since the clinic would close prior to her discharge from the ED.
How can requests for methadone be managed in the ED?
Methadone is a long-acting oral opioid that is used for both opioid replacement therapy and pain management. When used to reduce craving in opioid-dependent patients, methadone is administered daily through federally sanctioned methadone maintenance treatment (MMT) programs. Patients who consistently adhere to the required guidelines are given “take home” doses. When used for pain management, methadone is typically administered several times daily and may be prescribed by any provider with an appropriate DEA registration.
When given for MMT, methadone saturates the µ-opioid receptors and hinders their binding and agonism by other opioids such as heroin or oxycodone. Patients in MMT programs are started on a low initial dose and slowly titrated upward as tolerance to the adverse effects (eg, sedation) develop.
How are symptomatic patients with methadone withdrawal treated?
Most methadone programs have limited hours and require that patients who miss a dose wait until the following day to return to the program. This is typically without medical consequence because the high dose dispensed by these programs maintains a therapeutic blood concentration for far longer than the expected delay. Although the half-life of methadone exhibits wide interindividual variability, it generally ranges from 12 hours to more than 40 hours.1 Regardless, patients may feel anxious about potential opioid withdrawal, and this often leads them to access the ED for a missed dose.
The neuropsychiatric symptoms attending withdrawal may precede the objective signs of opioid withdrawal. Patients with objective signs of opioid withdrawal (eg, piloerection, vomiting, diarrhea, dilated pupils) may be sufficiently treated with supportive care alone, using antiemetics, hydration, and sometimes clonidine.
Administration of substitute opioids is problematic due to the patient’s underlying tolerance necessitating careful dose titration. Therefore, direct replacement of methadone in the ED remains controversial, and some EDs have strict policies prohibiting the administration of methadone to patients who have missed an MMT dose. Such policies, which are intended to discourage patients from using the ED as a convenience, may be appropriate given the generally benign—though uncomfortable—course of opioid withdrawal due to abstinence.
Other EDs provide replacement methadone for asymptomatic, treat-and-release patients confirmed to be enrolled in an MMT program when the time to the next dose is likely to be 24 hours or greater from the missed dose. Typically, a dose of no more than 10 mg orally or 10 mg intramuscularly (IM) is recommended, and patients should be advised that they will be receiving only a low dose to sufficient to prevent withdrawal—one that may not have the equivalent effects of the outpatient dose.
Whenever possible, a patient’s MMT program should be contacted and informed of the ED visit. For patients who display objective signs of withdrawal and who cannot be confirmed or who do not participate in an MMT program, 10 mg of methadone IM will prevent uncertainty of drug absorption in the setting of nausea or vomiting. All patients receiving oral methadone should be observed for 1 hour, and those receiving IM methadone should be observed for at least 90 minutes to assess for unexpected sedation.2
Patients encountering circumstances that prevent opioid access (eg, incarceration) and who are not in withdrawal but have gone without opioids for more than 5 days may have a loss of tolerance to their usual doses—whether the medication was obtained through an MMT program or illicitly. Harm-reduction strategies aimed at educating patients on the potential vulnerability to their familiar dosing regimens are warranted to avert inadvertent overdoses in chronic opioid users who are likely to resume illicit opoiod use.
Does this patient need syncope evaluation?
Further complicating the decision regarding ED dispensing of methadone are the effects of the drug on myocardial repolarization. Methadone affects conduction across the hERG potassium rectifier current and can prolong the QTc interval on the surface electrocardiogram (ECG), predisposing a patient to torsade de pointes (TdP). Although there is controversy regarding the role of ECG screening during the enrollment of patients in methadone maintenance clinics, doses above 60 mg, underlying myocardial disease, female sex, and electrolyte disturbances may increase the risk of QT prolongation and TdP.3
Whether there is value in obtaining a screening ECG in a patient receiving an initial dose of methadone in the ED is unclear, and this practice is controversial even among methadone clinics. However, some of the excess death in patients taking methadone may be explained by the dysrhythmogenic potential of methadone.4 An ECG therefore may elucidate a correctable cause in methadone patients presenting with syncope.
Administering methadone to patients with documented QT prolongation must weigh the risk of methadone’s conduction effects against the substantial risks of illicit opioid self-administration. For some patients at-risk for TdP, it may be preferable to use buprenorphine if possible, since it does not carry the same cardiac effects as methadone.1,5 Such therapy requires referral to a physician licensed to prescribe this medication.
How should admitted patients be managed?
While administration of methadone for withdrawal or maintenance therapy in the ED is acceptable, outpatient prescribing of methadone for these reasons is not legal, and only federally regulated clinics may engage in this practice. Hospitalized patients who are enrolled in an MMT program should have their daily methadone dose confirmed and continued—as long as the patient has not lost tolerance. Patients not participating in an MMT program can receive up to 3 days of methadone in the hospital, even if the practitioner is not registered to provide methadone.6 For these patients, it is recommended that the physician order a low dose of methadone and also consult with an addiction specialist to determine whether the patient should continue on MMT maintenance or undergo detoxification.
It is important to note that methadone may be prescribed for pain, but its use in the ED for this purpose is strongly discouraged, especially in patients who have never received methadone previously. For admitted patients requiring such potent opioid analgesia, consultation with a pain service or, when indicated, a palliative care/hospice specialist is warranted as the dosing intervals are different in each setting, and the risk of respiratory depression is high.
Case Conclusion
As requested by the MMT clinic, the patient was administered methadone 185 mg orally in the ED, though a dose of 10 mg would have been sufficient to prevent withdrawal. Unfortunately, the EP did not appreciate the relationship of the markedly prolonged QTc and the methadone, which should have prompted a dose reduction.
Evaluation of the patient’s electrolyte levels, which included magnesium and potassium, were normal. An ECG was repeated 24 hours later and revealed a persistent, but improved, QT interval at 505 ms. The remainder of the syncope workup was negative. Because the patient had no additional symptoms or events during her stay, she was discharged. At discharge, the EP followed up with the MMT clinic to discuss lowering the patient’s daily methadone dose, as well as close cardiology follow-up.
Dr Rao is the chief of the division of medical toxicology at New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Nelson, editor of “Case Studies in Toxicology,” is a professor in the department of emergency medicine and director of the medical toxicology fellowship program at the New York University School of Medicine and the New York City Poison Control Center. He is also associate editor, toxicology, of the EMERGENCY MEDICINE editorial board.
- Chou R, Weimer MB, Dana T. Methadone overdose and cardiac arrhythmia potential: findings from a review of the evidence for an American Pain Society and College on Problems of Drug Dependence clinical practice guideline. J Pain. 2014;15(4):338-365.
- National Highway Traffic Safety Administration Web site. Methadone. http://www.nhtsa.gov/people/injury/research/job185drugs/methadone.htm. Accessed August 3, 2015.
- Martin JA, Campbell A, Killip T, et al; Substance Abuse and Mental Health Services Administration. QT interval screening in methadone maintenance treatment: report of a SAMHSA expert panel. J Addict Dis. 2011;30(4):283-306. Erratum in: J Addict Dis. 2012;31(1):91.
- Ray WA, Chung CP, Murray KT, Cooper WO, Hall K, Stein CM. Out-of-hospital mortality among patients receiving methadone for noncancer pain. JAMA Intern Med. 2015;175(3):420-427.
- Davis MP. Twelve reasons for considering buprenorphine as a frontline analgesic in the management of pain. J Support Oncol. 2012;10(6):209-219.
- US Government Printing Office. Federal Digital System. Administering or dispensing of narcotic drugs. Code of Federal Regulations. Title 21 CFR §1306.07. http://www.gpo.gov/fdsys/pkg/CFR-1998-title21-vol9/pdf/CFR-1998-title21-vol9-sec1306-07.pdf. Accessed August 4, 2015.
- Chou R, Weimer MB, Dana T. Methadone overdose and cardiac arrhythmia potential: findings from a review of the evidence for an American Pain Society and College on Problems of Drug Dependence clinical practice guideline. J Pain. 2014;15(4):338-365.
- National Highway Traffic Safety Administration Web site. Methadone. http://www.nhtsa.gov/people/injury/research/job185drugs/methadone.htm. Accessed August 3, 2015.
- Martin JA, Campbell A, Killip T, et al; Substance Abuse and Mental Health Services Administration. QT interval screening in methadone maintenance treatment: report of a SAMHSA expert panel. J Addict Dis. 2011;30(4):283-306. Erratum in: J Addict Dis. 2012;31(1):91.
- Ray WA, Chung CP, Murray KT, Cooper WO, Hall K, Stein CM. Out-of-hospital mortality among patients receiving methadone for noncancer pain. JAMA Intern Med. 2015;175(3):420-427.
- Davis MP. Twelve reasons for considering buprenorphine as a frontline analgesic in the management of pain. J Support Oncol. 2012;10(6):209-219.
- US Government Printing Office. Federal Digital System. Administering or dispensing of narcotic drugs. Code of Federal Regulations. Title 21 CFR §1306.07. http://www.gpo.gov/fdsys/pkg/CFR-1998-title21-vol9/pdf/CFR-1998-title21-vol9-sec1306-07.pdf. Accessed August 4, 2015.
CASE REPORT: Altered Mental Status in an Elderly Woman
Case
A 100-year-old woman with a history of hypertension, hypothyroidism, and moderate Alzheimer dementia was brought to the ED by emergency medical services (EMS) for altered mental status after her home health aide (HHA) noted a change in the patient’s behavior. For the past few days, the patient’s appetite waned, and she became progressively more lethargic, not eating for over 24 hours. The aide activated 911 on the direction of the patient’s primary care physician. There were no reported changes to the patient’s medications which included aspirin, levothyroxine, and hydrochlorothiazide. She was unable to provide any meaningful history.
On arrival to the ED, the patient appeared comfortable in bed. She was sleepy, but easily aroused. Initial vital signs were: heart rate, 110 beats/minute; respiratory rate, 12 breaths/minute; blood pressure, 163/103 mm Hg; oral temperature, 98.2˚F. Oxygen (O2) saturation was 96% on room air. She was oriented to person only and responded appropriately to simple questions, intermittently following one-step commands. She was unable to attend and required redirection throughout the interview. (According to the aide, this behavior was different than her baseline.)
The patient’s head and neck examination were notable for some mild, boggy, periorbital edema and dry mucous membranes. Her thyroid examination was normal; her lungs were clear; and her cardiac examination revealed a 2/6 systolic ejection murmur over the second right intercostal space. Examination of the abdomen, extremities, and skin was unrevealing, and there were no gross focal neurological deficits. Her reflexes were normal throughout.
Initial assessment of this patient suggested a diagnosis of dementia and hypoactive delirium—the latter due to one or more of several possible etiologies.
Altered Mental Status
While altered mental status is a billable medical ICD-9-CM code1 used to specify a diagnosis on a reimbursement claim, it is not a disease state itself. Instead, it is a catchall phrase that incorporates any change in mental status, encompassing symptomatology that may have the largest differential diagnosis encountered in emergency medicine.
Delirium
An important category of altered mental status is delirium. The diagnostic criteria2 for delirium in DSM-V have remained essentially unchanged from DSM-IV; however, the prevalence of delirium as one of the key geriatric syndromes has grown as a result of increased research and education, particularly in the emergency medical setting. Distilled down, delirium can be defined as an acute change in mental status not caused by underlying dementia. Its cause is often multifactorial, and it is frequently an underappreciated consequence of both critical illness and the hospital environment.3
Delirium is an emergency unto itself, with an in-hospital mortality rate mirroring that of sepsis or acute myocardial infarction.4 The older-adult population is especially at risk of delirium and can present with one of three clinical subtypes: hyperactive (ie, agitated, etc), hypoactive (ie, somnolent, lethargic, stuporous, etc), and mixed type.5
The composition of factors precipitating the onset of delirium includes age, dementia, alcohol use, depression, illness severity, and drug exposure—notably benzodiazepines, opiates, and medications with anticholinergic properties.8 While major precipitants or causes of delirium, traditionally considered as potentially life-threatening acute events, are well known (Table 1), others are often overlooked (Table 2). Yet, ironically, these more frequently bypassed causes are more readily reversible, once discovered, such as inadequate pain control, urinary retention, constipation, dehydration, polypharmacy, and negative environmental conditions in the patient’s immediate surroundings. These findings have recently been corroborated.9
The Confusion Assessment Method
Identifying delirium can be a particular challenge for emergency physicians (EPs), especially when the patient has an underlying diagnosis of dementia and the specific degree of cognitive impairment is not known. The Confusion Assessment Method (CAM)10 is the most commonly used tool in the critical care setting11 and is the only validated tool for the ED, with an 86% sensitivity and 100% specificity.12 It evaluates four elements: (1) acute onset and fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. A patient must demonstrate the first two elements in addition to either the third or fourth element to be considered to have delirium.10
The CAM intensive care unit scale has the potential to be even more applicable in the ED. Recent findings support its validation.9
Case Continued
With respect to the elderly patient in this case with dementia and multiple potential causes for hypoactive delirium, the life-saving measure was the New York City (NYC) mandate that all 911 responding EMS workers wear ambient carbon monoxide (CO) detectors. Though the value of these detectors is controversial due to their low sensitivity, the emergency medical technicians (EMTs) detected an elevated CO level of 300 ppm when they arrived at the patient’s home.
Without this information, the patient’s age and clinical presentation would almost certainly have prompted an extensive evaluation to determine the etiology of her change in mental status and most likely would have missed the true cause of CO toxicity, which was confirmed by venous co-oximetry showing the patient to have a carboxyhemoglobin (HbCO) level of 19.5%.
Carbon Monoxide Toxicity
Carbon monoxide affects multiple cell types. It binds to myoglobin and in high concentrations depresses myocardial contractility. In platelets, CO displaces nitric oxide potentially resulting in vasodilation. Life-threatening CO poisoning causes hypotension, syncope, tachycardia, and an altered mental status. Delayed neuropsychiatric sequelae also may occur as the result of free radical injury to the brain.13
Symptoms
Patients with chronic CO poisoning who can adequately communicate may report nausea, headache, lightheadedness, and lethargy mimicking other seasonal illnesses. In debilitated or cognitively impaired patients who are unable to communicate, findings may include tachycardia, a mild change in mental status, and little else. Prolonged exposure and physiologic accumulation of CO may cause depressed mental status, coma, or death.
Although HbCO levels are confirmatory of exposure, venous levels do not necessarily reflect tissue concentrations or outcomes. Patients with a similar level to that of this patient (19.5%) may present with no symptoms, mild headache, or a deep coma depending on the duration of exposure to CO.
Definitive treatment is removal from the toxic environment and prompt administration of O2. In some cases, hyperbaric therapy may be beneficial.14
Diagnosis
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
It is rarely easy to diagnose the first case of an illness of which one is unfamiliar or not accustomed to treating. Likewise, it is very difficult to consider, diagnose and, as a result, effectively manage the first presentation of a known condition that is typically seasonal or linked to a different geographic location. Acute presentations of environmental exposures, illicit drug poisonings, and communicable infectious diseases are increasingly the purview of emergency medicine. Whether it is the first case of Ebola, of severe acute respiratory syndrome, the influenza virus, a new lethal street drug overdose, or CO poisoning prior to the onset of winter, maintaining a high index of suspicion for the “index case” is of paramount importance. The patient presented here, the first CO poisoning of the season at the authors’ institution, illustrates the responsibility the EP to consider, diagnose, and prevent a wide-range of deadly consequences—injury prevention as the result of vigilance. Moreover, the consequences of missing the diagnosis would have placed others at risk for continued poisoning and possibly death.
Portable and Ambient Carboxyhemoglobin Monitors
The NYC Department of Health (NYCDOH) requires that all EMTs and paramedics wear CO detectors and all residential housing contain CO monitors. The NYCDOH also mandates that all identified cases of CO poisoning be reported to the NYC Poison Control Center. This centralization of data on any and all patients exposed to CO can result in an investigation of the source of CO by the fire department and capture symptomatic patients who present for care outside of the 911 response system. The source of CO in this patient was ultimately traced to a faulty furnace that was repaired to prevent others in the building from becoming victims of CO poisoning.
It should be noted that portable noninvasive HbCO monitors may be inadequate to rule out CO poisoning as the sensitivity of such devices can be as low as 48%.15 Carbon monoxide poisoning can result from brief exposure to a high ambient concentration, such as a fire in which environmental concentrations may exceed 500 ppm or more insidiously, in a setting of a chronic exposure. Faulty furnaces—a common seasonal cause of CO poisoning—may continue to produce adequate heat and fail to prompt any concerns.
Since CO is colorless and odorless, ambient CO detectors stationed in the home are the best means of alerting one to exposure. In this case, though mandated by NYCDOH, a CO detector was not present in the patient’s home.
Case Conclusion
Through the rapid identification of CO poisoning in this elderly patient with altered mental status, EMS was able to evacuate the building while bringing the elderly tenant and her home attendant to the ED.
Based on the elderly patient’s elevated HbCO level, she was treated with O2 and discharged from the hospital the following day feeling well. In addition to the patient’s symptoms, when the aide was interviewed, she reported that she had been experiencing daily headaches, which she said soon resolved on departure from her client’s house. Her symptoms had been bothersome, but not so severe as to prompt her to seek medical attention. The aide was found to have an HbCO level of 12.5% and was discharged from the ED after 6 hours of observation and O2 therapy. The third occupant of the building, a tenant, was also brought to the ED and found to have an HbCO level of 12%. The tenant was treated with O2 therapy and discharged to home.
Dr Caldwell is an assistant professor of medicine in the department of emergency medicine, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Rao is an assistant professor of emergency medicine; and the chief in the division of medical Toxicology, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Stern is an assistant professor of medicine, department of emergency medicine; chief of geriatric emergency medicine; and codirector of geriatric emergency medicine fellowship at New York Presbyterian Hospital/Weill Cornell Medical Center, New York.
- ICD-9Data.com Web site. 2014 ICD-9-CM Diagnosis Codes. http://www.icd9data.com/2014/Volume1/default.htm. Accessed December 4, 2014.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
- Han JH, Wilson A, Ely EW. Delirium in the older emergency department patient: a quiet epidemic. Emerg Med Clin North Am. 2010;28(3):611-631.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
- Mulcare MR, Halpern A, Stern ME. The geriatric patient. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:741-753.
- Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193-200.
- Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
- Han JH, Vasilevskis EE, Ely EW. Sedation and delirium. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:704-717.
- Rosen T, Connors S, Halpern A, et al. Improving emergency department identification and management of agitated delirium in older adults: Implementation and impact assessment of a comprehensive clinical protocol using an A-B-C-D-E-F mnemonic. Ann Emerg Med. 2013;62(4)(Supp 4):S53-54.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
- Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
- Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23(1):20-25.
- Weaver LK. Carbon monoxide poisoning. New Engl J Med. 2009;360(12):1217-1225.
- Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric therapy for acute carbon monoxide poisoning. New Engl J Med. 2002;347(14):1057-1067.
- Touger M, Birnbaum A, Wang J, Chou K, Pearson D, Bijur P. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):382-388.
Case
A 100-year-old woman with a history of hypertension, hypothyroidism, and moderate Alzheimer dementia was brought to the ED by emergency medical services (EMS) for altered mental status after her home health aide (HHA) noted a change in the patient’s behavior. For the past few days, the patient’s appetite waned, and she became progressively more lethargic, not eating for over 24 hours. The aide activated 911 on the direction of the patient’s primary care physician. There were no reported changes to the patient’s medications which included aspirin, levothyroxine, and hydrochlorothiazide. She was unable to provide any meaningful history.
On arrival to the ED, the patient appeared comfortable in bed. She was sleepy, but easily aroused. Initial vital signs were: heart rate, 110 beats/minute; respiratory rate, 12 breaths/minute; blood pressure, 163/103 mm Hg; oral temperature, 98.2˚F. Oxygen (O2) saturation was 96% on room air. She was oriented to person only and responded appropriately to simple questions, intermittently following one-step commands. She was unable to attend and required redirection throughout the interview. (According to the aide, this behavior was different than her baseline.)
The patient’s head and neck examination were notable for some mild, boggy, periorbital edema and dry mucous membranes. Her thyroid examination was normal; her lungs were clear; and her cardiac examination revealed a 2/6 systolic ejection murmur over the second right intercostal space. Examination of the abdomen, extremities, and skin was unrevealing, and there were no gross focal neurological deficits. Her reflexes were normal throughout.
Initial assessment of this patient suggested a diagnosis of dementia and hypoactive delirium—the latter due to one or more of several possible etiologies.
Altered Mental Status
While altered mental status is a billable medical ICD-9-CM code1 used to specify a diagnosis on a reimbursement claim, it is not a disease state itself. Instead, it is a catchall phrase that incorporates any change in mental status, encompassing symptomatology that may have the largest differential diagnosis encountered in emergency medicine.
Delirium
An important category of altered mental status is delirium. The diagnostic criteria2 for delirium in DSM-V have remained essentially unchanged from DSM-IV; however, the prevalence of delirium as one of the key geriatric syndromes has grown as a result of increased research and education, particularly in the emergency medical setting. Distilled down, delirium can be defined as an acute change in mental status not caused by underlying dementia. Its cause is often multifactorial, and it is frequently an underappreciated consequence of both critical illness and the hospital environment.3
Delirium is an emergency unto itself, with an in-hospital mortality rate mirroring that of sepsis or acute myocardial infarction.4 The older-adult population is especially at risk of delirium and can present with one of three clinical subtypes: hyperactive (ie, agitated, etc), hypoactive (ie, somnolent, lethargic, stuporous, etc), and mixed type.5
The composition of factors precipitating the onset of delirium includes age, dementia, alcohol use, depression, illness severity, and drug exposure—notably benzodiazepines, opiates, and medications with anticholinergic properties.8 While major precipitants or causes of delirium, traditionally considered as potentially life-threatening acute events, are well known (Table 1), others are often overlooked (Table 2). Yet, ironically, these more frequently bypassed causes are more readily reversible, once discovered, such as inadequate pain control, urinary retention, constipation, dehydration, polypharmacy, and negative environmental conditions in the patient’s immediate surroundings. These findings have recently been corroborated.9
The Confusion Assessment Method
Identifying delirium can be a particular challenge for emergency physicians (EPs), especially when the patient has an underlying diagnosis of dementia and the specific degree of cognitive impairment is not known. The Confusion Assessment Method (CAM)10 is the most commonly used tool in the critical care setting11 and is the only validated tool for the ED, with an 86% sensitivity and 100% specificity.12 It evaluates four elements: (1) acute onset and fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. A patient must demonstrate the first two elements in addition to either the third or fourth element to be considered to have delirium.10
The CAM intensive care unit scale has the potential to be even more applicable in the ED. Recent findings support its validation.9
Case Continued
With respect to the elderly patient in this case with dementia and multiple potential causes for hypoactive delirium, the life-saving measure was the New York City (NYC) mandate that all 911 responding EMS workers wear ambient carbon monoxide (CO) detectors. Though the value of these detectors is controversial due to their low sensitivity, the emergency medical technicians (EMTs) detected an elevated CO level of 300 ppm when they arrived at the patient’s home.
Without this information, the patient’s age and clinical presentation would almost certainly have prompted an extensive evaluation to determine the etiology of her change in mental status and most likely would have missed the true cause of CO toxicity, which was confirmed by venous co-oximetry showing the patient to have a carboxyhemoglobin (HbCO) level of 19.5%.
Carbon Monoxide Toxicity
Carbon monoxide affects multiple cell types. It binds to myoglobin and in high concentrations depresses myocardial contractility. In platelets, CO displaces nitric oxide potentially resulting in vasodilation. Life-threatening CO poisoning causes hypotension, syncope, tachycardia, and an altered mental status. Delayed neuropsychiatric sequelae also may occur as the result of free radical injury to the brain.13
Symptoms
Patients with chronic CO poisoning who can adequately communicate may report nausea, headache, lightheadedness, and lethargy mimicking other seasonal illnesses. In debilitated or cognitively impaired patients who are unable to communicate, findings may include tachycardia, a mild change in mental status, and little else. Prolonged exposure and physiologic accumulation of CO may cause depressed mental status, coma, or death.
Although HbCO levels are confirmatory of exposure, venous levels do not necessarily reflect tissue concentrations or outcomes. Patients with a similar level to that of this patient (19.5%) may present with no symptoms, mild headache, or a deep coma depending on the duration of exposure to CO.
Definitive treatment is removal from the toxic environment and prompt administration of O2. In some cases, hyperbaric therapy may be beneficial.14
Diagnosis
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
It is rarely easy to diagnose the first case of an illness of which one is unfamiliar or not accustomed to treating. Likewise, it is very difficult to consider, diagnose and, as a result, effectively manage the first presentation of a known condition that is typically seasonal or linked to a different geographic location. Acute presentations of environmental exposures, illicit drug poisonings, and communicable infectious diseases are increasingly the purview of emergency medicine. Whether it is the first case of Ebola, of severe acute respiratory syndrome, the influenza virus, a new lethal street drug overdose, or CO poisoning prior to the onset of winter, maintaining a high index of suspicion for the “index case” is of paramount importance. The patient presented here, the first CO poisoning of the season at the authors’ institution, illustrates the responsibility the EP to consider, diagnose, and prevent a wide-range of deadly consequences—injury prevention as the result of vigilance. Moreover, the consequences of missing the diagnosis would have placed others at risk for continued poisoning and possibly death.
Portable and Ambient Carboxyhemoglobin Monitors
The NYC Department of Health (NYCDOH) requires that all EMTs and paramedics wear CO detectors and all residential housing contain CO monitors. The NYCDOH also mandates that all identified cases of CO poisoning be reported to the NYC Poison Control Center. This centralization of data on any and all patients exposed to CO can result in an investigation of the source of CO by the fire department and capture symptomatic patients who present for care outside of the 911 response system. The source of CO in this patient was ultimately traced to a faulty furnace that was repaired to prevent others in the building from becoming victims of CO poisoning.
It should be noted that portable noninvasive HbCO monitors may be inadequate to rule out CO poisoning as the sensitivity of such devices can be as low as 48%.15 Carbon monoxide poisoning can result from brief exposure to a high ambient concentration, such as a fire in which environmental concentrations may exceed 500 ppm or more insidiously, in a setting of a chronic exposure. Faulty furnaces—a common seasonal cause of CO poisoning—may continue to produce adequate heat and fail to prompt any concerns.
Since CO is colorless and odorless, ambient CO detectors stationed in the home are the best means of alerting one to exposure. In this case, though mandated by NYCDOH, a CO detector was not present in the patient’s home.
Case Conclusion
Through the rapid identification of CO poisoning in this elderly patient with altered mental status, EMS was able to evacuate the building while bringing the elderly tenant and her home attendant to the ED.
Based on the elderly patient’s elevated HbCO level, she was treated with O2 and discharged from the hospital the following day feeling well. In addition to the patient’s symptoms, when the aide was interviewed, she reported that she had been experiencing daily headaches, which she said soon resolved on departure from her client’s house. Her symptoms had been bothersome, but not so severe as to prompt her to seek medical attention. The aide was found to have an HbCO level of 12.5% and was discharged from the ED after 6 hours of observation and O2 therapy. The third occupant of the building, a tenant, was also brought to the ED and found to have an HbCO level of 12%. The tenant was treated with O2 therapy and discharged to home.
Dr Caldwell is an assistant professor of medicine in the department of emergency medicine, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Rao is an assistant professor of emergency medicine; and the chief in the division of medical Toxicology, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Stern is an assistant professor of medicine, department of emergency medicine; chief of geriatric emergency medicine; and codirector of geriatric emergency medicine fellowship at New York Presbyterian Hospital/Weill Cornell Medical Center, New York.
Case
A 100-year-old woman with a history of hypertension, hypothyroidism, and moderate Alzheimer dementia was brought to the ED by emergency medical services (EMS) for altered mental status after her home health aide (HHA) noted a change in the patient’s behavior. For the past few days, the patient’s appetite waned, and she became progressively more lethargic, not eating for over 24 hours. The aide activated 911 on the direction of the patient’s primary care physician. There were no reported changes to the patient’s medications which included aspirin, levothyroxine, and hydrochlorothiazide. She was unable to provide any meaningful history.
On arrival to the ED, the patient appeared comfortable in bed. She was sleepy, but easily aroused. Initial vital signs were: heart rate, 110 beats/minute; respiratory rate, 12 breaths/minute; blood pressure, 163/103 mm Hg; oral temperature, 98.2˚F. Oxygen (O2) saturation was 96% on room air. She was oriented to person only and responded appropriately to simple questions, intermittently following one-step commands. She was unable to attend and required redirection throughout the interview. (According to the aide, this behavior was different than her baseline.)
The patient’s head and neck examination were notable for some mild, boggy, periorbital edema and dry mucous membranes. Her thyroid examination was normal; her lungs were clear; and her cardiac examination revealed a 2/6 systolic ejection murmur over the second right intercostal space. Examination of the abdomen, extremities, and skin was unrevealing, and there were no gross focal neurological deficits. Her reflexes were normal throughout.
Initial assessment of this patient suggested a diagnosis of dementia and hypoactive delirium—the latter due to one or more of several possible etiologies.
Altered Mental Status
While altered mental status is a billable medical ICD-9-CM code1 used to specify a diagnosis on a reimbursement claim, it is not a disease state itself. Instead, it is a catchall phrase that incorporates any change in mental status, encompassing symptomatology that may have the largest differential diagnosis encountered in emergency medicine.
Delirium
An important category of altered mental status is delirium. The diagnostic criteria2 for delirium in DSM-V have remained essentially unchanged from DSM-IV; however, the prevalence of delirium as one of the key geriatric syndromes has grown as a result of increased research and education, particularly in the emergency medical setting. Distilled down, delirium can be defined as an acute change in mental status not caused by underlying dementia. Its cause is often multifactorial, and it is frequently an underappreciated consequence of both critical illness and the hospital environment.3
Delirium is an emergency unto itself, with an in-hospital mortality rate mirroring that of sepsis or acute myocardial infarction.4 The older-adult population is especially at risk of delirium and can present with one of three clinical subtypes: hyperactive (ie, agitated, etc), hypoactive (ie, somnolent, lethargic, stuporous, etc), and mixed type.5
The composition of factors precipitating the onset of delirium includes age, dementia, alcohol use, depression, illness severity, and drug exposure—notably benzodiazepines, opiates, and medications with anticholinergic properties.8 While major precipitants or causes of delirium, traditionally considered as potentially life-threatening acute events, are well known (Table 1), others are often overlooked (Table 2). Yet, ironically, these more frequently bypassed causes are more readily reversible, once discovered, such as inadequate pain control, urinary retention, constipation, dehydration, polypharmacy, and negative environmental conditions in the patient’s immediate surroundings. These findings have recently been corroborated.9
The Confusion Assessment Method
Identifying delirium can be a particular challenge for emergency physicians (EPs), especially when the patient has an underlying diagnosis of dementia and the specific degree of cognitive impairment is not known. The Confusion Assessment Method (CAM)10 is the most commonly used tool in the critical care setting11 and is the only validated tool for the ED, with an 86% sensitivity and 100% specificity.12 It evaluates four elements: (1) acute onset and fluctuating course; (2) inattention; (3) disorganized thinking; and (4) altered level of consciousness. A patient must demonstrate the first two elements in addition to either the third or fourth element to be considered to have delirium.10
The CAM intensive care unit scale has the potential to be even more applicable in the ED. Recent findings support its validation.9
Case Continued
With respect to the elderly patient in this case with dementia and multiple potential causes for hypoactive delirium, the life-saving measure was the New York City (NYC) mandate that all 911 responding EMS workers wear ambient carbon monoxide (CO) detectors. Though the value of these detectors is controversial due to their low sensitivity, the emergency medical technicians (EMTs) detected an elevated CO level of 300 ppm when they arrived at the patient’s home.
Without this information, the patient’s age and clinical presentation would almost certainly have prompted an extensive evaluation to determine the etiology of her change in mental status and most likely would have missed the true cause of CO toxicity, which was confirmed by venous co-oximetry showing the patient to have a carboxyhemoglobin (HbCO) level of 19.5%.
Carbon Monoxide Toxicity
Carbon monoxide affects multiple cell types. It binds to myoglobin and in high concentrations depresses myocardial contractility. In platelets, CO displaces nitric oxide potentially resulting in vasodilation. Life-threatening CO poisoning causes hypotension, syncope, tachycardia, and an altered mental status. Delayed neuropsychiatric sequelae also may occur as the result of free radical injury to the brain.13
Symptoms
Patients with chronic CO poisoning who can adequately communicate may report nausea, headache, lightheadedness, and lethargy mimicking other seasonal illnesses. In debilitated or cognitively impaired patients who are unable to communicate, findings may include tachycardia, a mild change in mental status, and little else. Prolonged exposure and physiologic accumulation of CO may cause depressed mental status, coma, or death.
Although HbCO levels are confirmatory of exposure, venous levels do not necessarily reflect tissue concentrations or outcomes. Patients with a similar level to that of this patient (19.5%) may present with no symptoms, mild headache, or a deep coma depending on the duration of exposure to CO.
Definitive treatment is removal from the toxic environment and prompt administration of O2. In some cases, hyperbaric therapy may be beneficial.14
Diagnosis
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
Although CO exposure is the most common cause of poisoning death worldwide, its detection requires a high index of suspicion, especially in areas where public-health protection measures are absent.
It is rarely easy to diagnose the first case of an illness of which one is unfamiliar or not accustomed to treating. Likewise, it is very difficult to consider, diagnose and, as a result, effectively manage the first presentation of a known condition that is typically seasonal or linked to a different geographic location. Acute presentations of environmental exposures, illicit drug poisonings, and communicable infectious diseases are increasingly the purview of emergency medicine. Whether it is the first case of Ebola, of severe acute respiratory syndrome, the influenza virus, a new lethal street drug overdose, or CO poisoning prior to the onset of winter, maintaining a high index of suspicion for the “index case” is of paramount importance. The patient presented here, the first CO poisoning of the season at the authors’ institution, illustrates the responsibility the EP to consider, diagnose, and prevent a wide-range of deadly consequences—injury prevention as the result of vigilance. Moreover, the consequences of missing the diagnosis would have placed others at risk for continued poisoning and possibly death.
Portable and Ambient Carboxyhemoglobin Monitors
The NYC Department of Health (NYCDOH) requires that all EMTs and paramedics wear CO detectors and all residential housing contain CO monitors. The NYCDOH also mandates that all identified cases of CO poisoning be reported to the NYC Poison Control Center. This centralization of data on any and all patients exposed to CO can result in an investigation of the source of CO by the fire department and capture symptomatic patients who present for care outside of the 911 response system. The source of CO in this patient was ultimately traced to a faulty furnace that was repaired to prevent others in the building from becoming victims of CO poisoning.
It should be noted that portable noninvasive HbCO monitors may be inadequate to rule out CO poisoning as the sensitivity of such devices can be as low as 48%.15 Carbon monoxide poisoning can result from brief exposure to a high ambient concentration, such as a fire in which environmental concentrations may exceed 500 ppm or more insidiously, in a setting of a chronic exposure. Faulty furnaces—a common seasonal cause of CO poisoning—may continue to produce adequate heat and fail to prompt any concerns.
Since CO is colorless and odorless, ambient CO detectors stationed in the home are the best means of alerting one to exposure. In this case, though mandated by NYCDOH, a CO detector was not present in the patient’s home.
Case Conclusion
Through the rapid identification of CO poisoning in this elderly patient with altered mental status, EMS was able to evacuate the building while bringing the elderly tenant and her home attendant to the ED.
Based on the elderly patient’s elevated HbCO level, she was treated with O2 and discharged from the hospital the following day feeling well. In addition to the patient’s symptoms, when the aide was interviewed, she reported that she had been experiencing daily headaches, which she said soon resolved on departure from her client’s house. Her symptoms had been bothersome, but not so severe as to prompt her to seek medical attention. The aide was found to have an HbCO level of 12.5% and was discharged from the ED after 6 hours of observation and O2 therapy. The third occupant of the building, a tenant, was also brought to the ED and found to have an HbCO level of 12%. The tenant was treated with O2 therapy and discharged to home.
Dr Caldwell is an assistant professor of medicine in the department of emergency medicine, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Rao is an assistant professor of emergency medicine; and the chief in the division of medical Toxicology, New York Presbyterian Hospital/Weill Cornell Medical Center, New York. Dr Stern is an assistant professor of medicine, department of emergency medicine; chief of geriatric emergency medicine; and codirector of geriatric emergency medicine fellowship at New York Presbyterian Hospital/Weill Cornell Medical Center, New York.
- ICD-9Data.com Web site. 2014 ICD-9-CM Diagnosis Codes. http://www.icd9data.com/2014/Volume1/default.htm. Accessed December 4, 2014.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
- Han JH, Wilson A, Ely EW. Delirium in the older emergency department patient: a quiet epidemic. Emerg Med Clin North Am. 2010;28(3):611-631.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
- Mulcare MR, Halpern A, Stern ME. The geriatric patient. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:741-753.
- Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193-200.
- Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
- Han JH, Vasilevskis EE, Ely EW. Sedation and delirium. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:704-717.
- Rosen T, Connors S, Halpern A, et al. Improving emergency department identification and management of agitated delirium in older adults: Implementation and impact assessment of a comprehensive clinical protocol using an A-B-C-D-E-F mnemonic. Ann Emerg Med. 2013;62(4)(Supp 4):S53-54.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
- Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
- Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23(1):20-25.
- Weaver LK. Carbon monoxide poisoning. New Engl J Med. 2009;360(12):1217-1225.
- Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric therapy for acute carbon monoxide poisoning. New Engl J Med. 2002;347(14):1057-1067.
- Touger M, Birnbaum A, Wang J, Chou K, Pearson D, Bijur P. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):382-388.
- ICD-9Data.com Web site. 2014 ICD-9-CM Diagnosis Codes. http://www.icd9data.com/2014/Volume1/default.htm. Accessed December 4, 2014.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
- Han JH, Wilson A, Ely EW. Delirium in the older emergency department patient: a quiet epidemic. Emerg Med Clin North Am. 2010;28(3):611-631.
- Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157-1165.
- Mulcare MR, Halpern A, Stern ME. The geriatric patient. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:741-753.
- Han JH, Zimmerman EE, Cutler N, et al. Delirium in older emergency department patients: recognition, risk factors, and psychomotor subtypes. Acad Emerg Med. 2009;16(3):193-200.
- Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA. 1996;275(11):852-857.
- Han JH, Vasilevskis EE, Ely EW. Sedation and delirium. In: Arbo JE, Ruoss SJ, Lighthall GK, Jones MP, eds. Decision Making in Emergency Critical Care: An Evidence-Based Handbook. Philadelphia, PA: Wolters Kluwer; 2015:704-717.
- Rosen T, Connors S, Halpern A, et al. Improving emergency department identification and management of agitated delirium in older adults: Implementation and impact assessment of a comprehensive clinical protocol using an A-B-C-D-E-F mnemonic. Ann Emerg Med. 2013;62(4)(Supp 4):S53-54.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941-948.
- Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc. 2008;56(5):823-830.
- Monette J, Galbaud du Fort G, Fung SH, et al. Evaluation of the Confusion Assessment Method (CAM) as a screening tool for delirium in the emergency room. Gen Hosp Psychiatry. 2001;23(1):20-25.
- Weaver LK. Carbon monoxide poisoning. New Engl J Med. 2009;360(12):1217-1225.
- Weaver LK, Hopkins RO, Chan KJ, et al. Hyperbaric therapy for acute carbon monoxide poisoning. New Engl J Med. 2002;347(14):1057-1067.
- Touger M, Birnbaum A, Wang J, Chou K, Pearson D, Bijur P. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglobin measurement. Ann Emerg Med. 2010;56(4):382-388.