Opinion

Gynecologic Oncology Consult: Update on Endometrial Cancer Treatment
- Author:
- Jennifer Haag, MD, PhD
- Katherine Tucker, MD
Checkpoint inhibitors improve outcomes in women with advanced endometrial cancer and an immunotherapy and antivascular endothelial growth factor...
Opinion

Molecular Classification of Endometrial Carcinomas
- Author:
- Jennifer Haag, MD, MPH
- Katherine Tucker, MD
When The Cancer Genome Atlas performed genomic, transcriptomic, and proteomic characterization of endometrial carcinomas, they identified four...
Opinion

Surgical management of borderline ovarian tumors, part 1
- Author:
- Katherine Tucker, MD
Ovarian-sparing procedures should be offered to patients in the setting of borderline ovarian tumors, with the understanding that they are...
Opinion

Update on secondary cytoreduction in recurrent ovarian cancer
- Author:
- Catherine John, MD
- Katherine Tucker, MD
Secondary debulking surgery has been studied since the 1980s with mixed results; these data have shown that the largest barrier to care has been...
Opinion

Update on high-grade vulvar interepithelial neoplasia
- Author:
- Lisa Jackson-Moore, MD
- Katherine Tucker, MD
Treatment of high-grade vulvar intraepithelial neoplasia should be driven by the clinical characteristics of the vulvar lesions, patients’...
Opinion
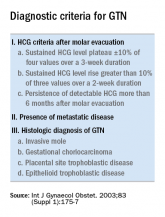
The role of repeat uterine curettage in postmolar gestational trophoblastic neoplasia
- Author:
- Katherine Tucker, MD
Second uterine evacuation for treatment of nonmetastatic, low-risk postmolar GTN is a reasonable treatment option and one that should be...
Opinion

Estrogen replacement therapy in endometrial cancer survivors
- Author:
- Katherine Tucker, MD
Given the data we have, ERT does not appear to significantly affect oncologic outcomes in low-risk, early-stage endometrial cancer survivors.
Opinion

The perils of CA-125 as a diagnostic tool in patients with adnexal masses
- Author:
- Katherine Tucker, MD
It is important to have conversations with patients before ordering a CA-125 (or other serum biomarkers) about potential results and their effect...
