User login
When should nutritional support be implemented in a hospitalized patient?
Case
A 60-year-old male with a history of head & neck cancer, treated with radical neck dissection and radiation 5 years prior is admitted with community-acquired pneumonia and anasarca. Prior to admission, he was on a soft dysphagia diet and reports increased difficulty with solid foods and weight loss from 70 kg to 55 kg over 2.5 years. Should nutritional support be initiated?
Background
Malnutrition is associated with increased hospital mortality, decreased functional status and quality of life, infections, longer length of stay, higher hospital costs, and more frequent nonelective readmissions.1,2
Identifying patients who are malnourished or at risk for malnutrition
An international consensus committee recommended the following criteria for the diagnosis of undernutrition if two of six are present3:
- Insufficient energy intake.
- Weight loss.
- Loss of muscle mass.
- Loss of subcutaneous fat.
- Localized or generalized fluid accumulation that may sometimes mask weight loss.
- Diminished functional status as measured by handgrip strength.
The joint commission requires that all patients admitted to acute care hospitals be screened for risk of malnutrition within 24 hours. The American College of Gastroenterologists recommends using a validated score to assess nutritional risk, such as the Nutritional Risk Score (NRS) 2002 or the NUTRIC (Nutrition Risk in the Critically Ill) Score, which use a combination of nutritional status and diet-related factors – weight loss, body mass index, and food intake – and also severity of illness measurements.4
- Starvation-related malnutrition, such as anorexia nervosa, presents with a deficiency in calories and protein without inflammation, .
- Chronic disease–related malnutrition, such as that caused chronic obstructive pulmonary disease, cancer, and obesity, presents with mild to moderate inflammation.
- Acute disease or injury–related malnutrition, such as that caused by sepsis, burns, and trauma, presents with acute and severe inflammation.
Laboratory indicators such as albumin, prealbumin, and transferrin are not recommended for the determination of nutritional status. Instead, as negative acute-phase reactants, they can be used as surrogate markers of nutritional risk and degree of inflammation.4
Overview of the data
What are the indications for initiating nutritional support, and what is the optimal timing for initiation?
Patients who are malnourished or at significant risk for becoming malnourished should receive specialized nutrition support. Early enteral nutrition should be initiated within 24-48 hours of admission in critically ill patients with high nutritional risk who are unable to maintain volitional intake.6 In the absence of preexisting malnutrition, nutritional support should be provided for patients with inadequate oral intake for 7-14 days or for those in whom inadequate oral intake is expected over the same time period.7
How should nutritional support be administered?
Dietary modification and supplementation
In patients who can tolerate an oral diet, dietary modifications may be made in order to facilitate the provision of essential nutrients in a well-tolerated form. Modifications may include adjusting the consistency of foods, energy value of foods, types of nutrients consumed, and number and frequency of meals.8 Commercial meal replacement beverages are widely used to support a standard oral diet, but there is no data to support their routine use.7
Enteral nutrition
Enteral nutrition (EN) is the method of choice for administering nutrition support. Contraindications to enteral feeding include diffuse peritonitis, intestinal obstruction, and gastrointestinal ischemia.9 The potential advantages of EN over parenteral nutrition (PN) include decreased infection rate, decreased total complications, and shorter length of stay, but there has been no observed difference in mortality. EN is also suggested to have nonnutritional benefits related to providing luminal nutrients – these include maintaining gut integrity, beneficial immune responses, and favorable metabolic responses that help maintain euglycemia and enhance more physiologic fuel utilization.4
Enteral feeding can be administered through the following routes of access:
- Nasogastric tubes: A nasogastric or orogastric tube with radiologic confirmation of positioning is the first line of enteral access. Gastric feeding is preferred because it is well tolerated in the majority of patients, is more physiological, requires a lower level of expertise, and minimizes any delay in initiation of feeding.
- Postpyloric tubes: Postpyloric feeding tubes are indicated if gastric feeding is poorly tolerated or if the patient is at high risk for aspiration because jejunal feedings decrease the incidence of reflux, regurgitation, and aspiration.
- Percutaneous access: When long-term enteral access is required – that is, for greater than 4 weeks – a percutaneous enteral access device should be placed. Prolonged use of a nasoenteric tube may be associated with erosion of the nares and an increase in the incidence of aspiration pneumonia, sinusitis, and esophageal ulceration or stricture. Patients who have had a stroke are the most likely to benefit from percutaneous endoscopic gastrostomy placement, as 40% of patients can have continued dysphagia as long as 1 year after.4,10 Absolute contraindications for PEG placement include serious coagulation disorders (international normalized ratio greater than 1.5; fewer than 50,000 platelets/mcL), sepsis, abdominal wall infections, marked peritoneal carcinomatosis, peritonitis, severe gastroparesis, gastric outlet obstruction, or a history of total gastrectomy. Risks often outweigh benefits in patients who have cirrhosis with ascites, patients undergoing peritoneal dialysis, and patients who have portal hypertension with gastric varices, but PEG can be considered on a case-by-case basis.11
Parenteral nutrition
Parenteral nutrition is reserved for patients in whom enteral feeding is contraindicated or who fail to meet their nutritional needs with enteral feedings. If EN is not feasible, then parenteral nutrition should be initiated as soon as possible in patients who had high nutritional risk on admission. Otherwise, PN should not be initiated during the first week of hospitalization because there is evidence to suggest net harm when initiated early. Supplemental PN may be considered for patients already on EN who are unable to meet more than 60% of their energy and protein requirements by the enteral route alone, but again, this should only be considered after 7-10 days on EN. PN is generally stopped when the patients achieve more than 60% of their energy and protein goals from EN.4
How should patients be monitored while receiving nutritional support?
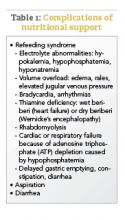
If a patient is severely malnourished and refeeding is initiated, serious complications can occur, which are summarized in Table 1; these complications can include severe electrolyte disorders, fluid shifts, and even death.12 Refeeding syndrome occurs in the first few days of initiating a diet in severely malnourished patients, and its severity is directly related to the severity of malnutrition prior to refeeding. The National Institute of Health and Clinical Excellence created criteria to identify patients at risk for refeeding syndrome; these criteria include having a BMI less than 18.5 kg/m2; unintentional weight loss of greater than 10% in the previous 3-6 months; little or no nutritional intake for more than 5 days; low levels of potassium, phosphorus, or magnesium before refeeding; and a history of alcohol misuse or taking certain drugs, such as insulin, chemotherapy, antacids, or diuretics.9
Aspiration is a risk with enteral feeding – the risk factors include being older than 70 years, altered mental status, supine position, and bolus rather than continuous infusion.4 Postpyloric feeding may reduce the risk of aspiration. Expert consensus suggests elevating the head of the bed by 30°-40° for all intubated patients receiving EN, as well as administering chlorhexidine mouthwash twice daily.6
Diarrhea is very common in patients receiving EN. After evaluating for other etiologies of diarrhea, tube feeding–associated diarrhea may be managed first by using a fiber-containing formulation. Fiber should be avoided in patients at risk for bowel ischemia or severe dysmotility. If diarrhea persists despite fiber, small peptide formulations, also known as elemental tube feeds, may be used.4,6
Gastric residual volume (GRV) is commonly monitored in patients receiving enteral nutrition. However, the American College of Gastroenterology does not recommend using GRVs to monitor EN feeding because it is a poor marker of clinically meaningful variables, such as gastric emptying, risk of aspiration, and risk of poor outcomes, and increases the risk of tube clogging and inadequate delivery of EN. If GRVs are being monitored, tube feedings should not be withheld because of high GRVs when there are no other signs of intolerance.4 Nausea may be managed by changing a patient from bolus to continuous feedings or by adding promotility agents such as metoclopramide or erythromycin.6
Special considerations in common conditions treated by hospitalists
The principles outlined above are general guidelines that are applicable to most patients requiring nutrition support. We have highlighted special considerations for common conditions in hospitalized patients who require nutritional support below.
Critical Illness
- Defer enteral nutrition until patient is fully resuscitated and hemodynamically stable.
- Severely malnourished or high nutritional-risk patients should be advanced toward goals as quickly as can be tolerated over 24-48 hours.
- Patients with acute respiratory distress syndrome or acute lung injury, or those expected to require mechanical ventilation for more than 72 hours, should receive trophic feeds or full nutrition by enteral route.6
Pancreatitis
- Oral feeding should be attempted as soon as abdominal pain is decreasing and inflammatory markers are improving.13
- A regular solid, low-fat diet should be initiated, rather than slowly advancing from a clear liquid diet.13
- In severe acute pancreatitis, initiation of enteral nutrition within 48 hours of presentation is associated with improved outcomes.13
- There is no difference in outcomes between gastric and postpyloric feeding.14
- Initiation of parenteral nutrition may be delayed for up to 5 days to allow for a trial of oral or enteral feeding.13
Surgical patients
- Consider postponing surgery to provide 7-10 days of preoperative nutrition supplementation in patients with risk of severe undernutrition.16
- Consider postoperative nutritional support if patients are at risk for severe undernutrition, are unable to eat for more than 7 days perioperatively, or are unable to maintain oral intake above 60% of recommended intake for more than 10 days.16
- Consider total parenteral nutrition in cases of impaired gastrointestinal function and absorption, high output enterocutaneous fistulae, obstructive lesions that do not allow enteral refeeding, or prolonged gastrointestinal failure.16
Prolonged Starvation
- Because of the high risk of refeeding syndrome, patients greater than 30% below ideal body weight should be hospitalized for close monitoring during refeeding.12
- Typical goal for weight gain is no greater than 2-3 pounds per week.10
- Total parenteral nutrition should be reserved for extreme cases, and if used, carbohydrate intake should not exceed 7 mg/kg/min.12
Stroke
- Enteral nutrition should be initiated within 24-48 hours of initial hospitalization if a patient is estimated to require feeding for more than 5 days and/or remain nil per os for 5-7 days.
- If a patient is intubated with increased intracranial pressure, this could delay gastric motility requiring a postpyloric tube placement.
- Initial placement of percutaneous endoscopic gastrostomy tubes can be considered if the hospitalized patient is expected to require nutritional support for greater than 30 days. Most patients will have improved dysphagia symptoms within 1 month of their acute stroke, although as many as 40% can have continued dysphagia up to 1 year.10
Back to the Case
The patient was admitted for a common general medical condition, but it is important to recognize that malnutrition was present on admission with weight loss and generalized fluid overload. Furthermore, he is at high nutritional risk because of his low body weight, poor oral intake, and dysphagia. Additionally, the acute inflammation from pneumonia places him in an increased catabolic state.
He was able to maintain some volitional oral intake, but after 7 days of close monitoring by a licensed dietician, it was determined that he was unable to meet his nutritional needs via the oral route. A percutaneous endoscopic gastrostomy tube was placed, and tube feeds were initiated, because his dysphagia – which was a significant factor contributing to his inability to meet his nutritional needs orally – was expected to persist for greater than 30 days.
Bottom Line
Nutrition support should be initiated in this patient with malnutrition on admission and high nutritional risk.
Dr. Abalos is an assistant professor at Georgetown University Medical Center in Washington. Dr. Corbett is an assistant professor at the University of Oklahoma Health Sciences Center in Oklahoma City.
References
1. Correia MI et al. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003 Jun;22(3):235-9.
2. Felder S et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015 Nov-Dec;31(11-12):1385-93.
3. White JV et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012 May;112(5):730-8.
4. McClave SA et al. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
5. Mueller C et al. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enter Nutr. 2011 Jan;35(1):16-24.
6. McClave SA et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. JPEN J Parenter Enter Nutr. 2016 Feb;40(2):159-211.
7. August D et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enter Nutr. 2002 Jan-Feb:26(1):SUPPL:1SA-138SA.
8. Kirkland LL et al. Nutrition in the hospitalized patient. J Hosp Med. 2013 Jan;8(1):52-8.
9. National Collaborating Centre for Acute Care, February 2006. Nutrition support in adults Oral nutrition support, enteral tube feeding and parenteral nutrition. National Collaborating Centre for Acute Care, London. Available from www.rcseng.ac.uk.
10. Corrigan ML et al. Nutrition in the stroke patient. Nutr Clin Pract. 2011 Jun;26(3):242-52.
11. Loser C et al. ESPEN guidelines on artificial enteral nutrition – Percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005 Oct;24(5):848-61.
12. Mehler PS et al. Nutritional rehabilitation: Practical guidelines for refeeding the anorectic patient. J Nutr Metab. 2010. doi: 10.1155/2010/625782.
13. Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul-Aug;13(4 Suppl 2):e1-15.
14. Singh N et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: A noninferiority randomized controlled trial. Pancreas. 2012 Jan;41(1):153-9.
15. Braga M et al. ESPEN guidelines on parenteral nutrition: Surgery. Clin Nutr. 2009 Aug;28(4):378-86.
16. Weimann A et al. ESPEN Guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr. 2006 Apr;25(2):224-44.
Additional reading
- Kirkland LL et al. Nutrition in the Hospitalized Patient. J Hosp Med. 2013 Jan;8(1):52-8.
- McClave SA et al. ACG Clinical Guideline: Nutrition Therapy in the Adult Hospitalized Patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
Quiz: Recognizing Malnutrition
Which of the following is not a criteria for the diagnosis of malnutrition?
A. Weight loss
B. Insufficient energy intake
C. Prealbumin
D. Diminished handgrip strength
Answer: C. Prealbumin. Laboratory indicators of nutrition, such as albumin, prealbumin, and transferrin, and markers of infection or inflammation are not recommended for the determination of nutritional status. Because negative acute-phase reactants, they instead can be used as surrogate markers of nutritional risk and degree of inflammation
Key Points
- At the time of admission to the hospital, malnutrition is present in 20-50% of patients. All hospitalized patients should be screened for nutritional risk and nutritional support should be considered if patients are not expected to be able to meet nutritional needs for more than 7 days.
- Patients with severe malnutrition on admission, severe critical illness, or severe acute pancreatitis should be provided nutritional support within 24-48 hours.
- Use the gut! Nutritional support should be provided via the most physiologic route possible. Total parenteral nutrition (TPN) should be reserved for patients in whom adequate nutrition cannot be provided enterally.
- Consider a percutaneous endoscopic gastrostomy (PEG) tube if the patient is expected to require tube feedings for more than 30 days.
- Patients with severe malnutrition who are given nutritional support are at high risk of developing refeeding syndrome, which manifests as electrolyte depletions and heart failure or volume overload.
Case
A 60-year-old male with a history of head & neck cancer, treated with radical neck dissection and radiation 5 years prior is admitted with community-acquired pneumonia and anasarca. Prior to admission, he was on a soft dysphagia diet and reports increased difficulty with solid foods and weight loss from 70 kg to 55 kg over 2.5 years. Should nutritional support be initiated?
Background
Malnutrition is associated with increased hospital mortality, decreased functional status and quality of life, infections, longer length of stay, higher hospital costs, and more frequent nonelective readmissions.1,2
Identifying patients who are malnourished or at risk for malnutrition
An international consensus committee recommended the following criteria for the diagnosis of undernutrition if two of six are present3:
- Insufficient energy intake.
- Weight loss.
- Loss of muscle mass.
- Loss of subcutaneous fat.
- Localized or generalized fluid accumulation that may sometimes mask weight loss.
- Diminished functional status as measured by handgrip strength.
The joint commission requires that all patients admitted to acute care hospitals be screened for risk of malnutrition within 24 hours. The American College of Gastroenterologists recommends using a validated score to assess nutritional risk, such as the Nutritional Risk Score (NRS) 2002 or the NUTRIC (Nutrition Risk in the Critically Ill) Score, which use a combination of nutritional status and diet-related factors – weight loss, body mass index, and food intake – and also severity of illness measurements.4
- Starvation-related malnutrition, such as anorexia nervosa, presents with a deficiency in calories and protein without inflammation, .
- Chronic disease–related malnutrition, such as that caused chronic obstructive pulmonary disease, cancer, and obesity, presents with mild to moderate inflammation.
- Acute disease or injury–related malnutrition, such as that caused by sepsis, burns, and trauma, presents with acute and severe inflammation.
Laboratory indicators such as albumin, prealbumin, and transferrin are not recommended for the determination of nutritional status. Instead, as negative acute-phase reactants, they can be used as surrogate markers of nutritional risk and degree of inflammation.4
Overview of the data
What are the indications for initiating nutritional support, and what is the optimal timing for initiation?
Patients who are malnourished or at significant risk for becoming malnourished should receive specialized nutrition support. Early enteral nutrition should be initiated within 24-48 hours of admission in critically ill patients with high nutritional risk who are unable to maintain volitional intake.6 In the absence of preexisting malnutrition, nutritional support should be provided for patients with inadequate oral intake for 7-14 days or for those in whom inadequate oral intake is expected over the same time period.7
How should nutritional support be administered?
Dietary modification and supplementation
In patients who can tolerate an oral diet, dietary modifications may be made in order to facilitate the provision of essential nutrients in a well-tolerated form. Modifications may include adjusting the consistency of foods, energy value of foods, types of nutrients consumed, and number and frequency of meals.8 Commercial meal replacement beverages are widely used to support a standard oral diet, but there is no data to support their routine use.7
Enteral nutrition
Enteral nutrition (EN) is the method of choice for administering nutrition support. Contraindications to enteral feeding include diffuse peritonitis, intestinal obstruction, and gastrointestinal ischemia.9 The potential advantages of EN over parenteral nutrition (PN) include decreased infection rate, decreased total complications, and shorter length of stay, but there has been no observed difference in mortality. EN is also suggested to have nonnutritional benefits related to providing luminal nutrients – these include maintaining gut integrity, beneficial immune responses, and favorable metabolic responses that help maintain euglycemia and enhance more physiologic fuel utilization.4
Enteral feeding can be administered through the following routes of access:
- Nasogastric tubes: A nasogastric or orogastric tube with radiologic confirmation of positioning is the first line of enteral access. Gastric feeding is preferred because it is well tolerated in the majority of patients, is more physiological, requires a lower level of expertise, and minimizes any delay in initiation of feeding.
- Postpyloric tubes: Postpyloric feeding tubes are indicated if gastric feeding is poorly tolerated or if the patient is at high risk for aspiration because jejunal feedings decrease the incidence of reflux, regurgitation, and aspiration.
- Percutaneous access: When long-term enteral access is required – that is, for greater than 4 weeks – a percutaneous enteral access device should be placed. Prolonged use of a nasoenteric tube may be associated with erosion of the nares and an increase in the incidence of aspiration pneumonia, sinusitis, and esophageal ulceration or stricture. Patients who have had a stroke are the most likely to benefit from percutaneous endoscopic gastrostomy placement, as 40% of patients can have continued dysphagia as long as 1 year after.4,10 Absolute contraindications for PEG placement include serious coagulation disorders (international normalized ratio greater than 1.5; fewer than 50,000 platelets/mcL), sepsis, abdominal wall infections, marked peritoneal carcinomatosis, peritonitis, severe gastroparesis, gastric outlet obstruction, or a history of total gastrectomy. Risks often outweigh benefits in patients who have cirrhosis with ascites, patients undergoing peritoneal dialysis, and patients who have portal hypertension with gastric varices, but PEG can be considered on a case-by-case basis.11
Parenteral nutrition
Parenteral nutrition is reserved for patients in whom enteral feeding is contraindicated or who fail to meet their nutritional needs with enteral feedings. If EN is not feasible, then parenteral nutrition should be initiated as soon as possible in patients who had high nutritional risk on admission. Otherwise, PN should not be initiated during the first week of hospitalization because there is evidence to suggest net harm when initiated early. Supplemental PN may be considered for patients already on EN who are unable to meet more than 60% of their energy and protein requirements by the enteral route alone, but again, this should only be considered after 7-10 days on EN. PN is generally stopped when the patients achieve more than 60% of their energy and protein goals from EN.4
How should patients be monitored while receiving nutritional support?
If a patient is severely malnourished and refeeding is initiated, serious complications can occur, which are summarized in Table 1; these complications can include severe electrolyte disorders, fluid shifts, and even death.12 Refeeding syndrome occurs in the first few days of initiating a diet in severely malnourished patients, and its severity is directly related to the severity of malnutrition prior to refeeding. The National Institute of Health and Clinical Excellence created criteria to identify patients at risk for refeeding syndrome; these criteria include having a BMI less than 18.5 kg/m2; unintentional weight loss of greater than 10% in the previous 3-6 months; little or no nutritional intake for more than 5 days; low levels of potassium, phosphorus, or magnesium before refeeding; and a history of alcohol misuse or taking certain drugs, such as insulin, chemotherapy, antacids, or diuretics.9
Aspiration is a risk with enteral feeding – the risk factors include being older than 70 years, altered mental status, supine position, and bolus rather than continuous infusion.4 Postpyloric feeding may reduce the risk of aspiration. Expert consensus suggests elevating the head of the bed by 30°-40° for all intubated patients receiving EN, as well as administering chlorhexidine mouthwash twice daily.6
Diarrhea is very common in patients receiving EN. After evaluating for other etiologies of diarrhea, tube feeding–associated diarrhea may be managed first by using a fiber-containing formulation. Fiber should be avoided in patients at risk for bowel ischemia or severe dysmotility. If diarrhea persists despite fiber, small peptide formulations, also known as elemental tube feeds, may be used.4,6
Gastric residual volume (GRV) is commonly monitored in patients receiving enteral nutrition. However, the American College of Gastroenterology does not recommend using GRVs to monitor EN feeding because it is a poor marker of clinically meaningful variables, such as gastric emptying, risk of aspiration, and risk of poor outcomes, and increases the risk of tube clogging and inadequate delivery of EN. If GRVs are being monitored, tube feedings should not be withheld because of high GRVs when there are no other signs of intolerance.4 Nausea may be managed by changing a patient from bolus to continuous feedings or by adding promotility agents such as metoclopramide or erythromycin.6
Special considerations in common conditions treated by hospitalists
The principles outlined above are general guidelines that are applicable to most patients requiring nutrition support. We have highlighted special considerations for common conditions in hospitalized patients who require nutritional support below.
Critical Illness
- Defer enteral nutrition until patient is fully resuscitated and hemodynamically stable.
- Severely malnourished or high nutritional-risk patients should be advanced toward goals as quickly as can be tolerated over 24-48 hours.
- Patients with acute respiratory distress syndrome or acute lung injury, or those expected to require mechanical ventilation for more than 72 hours, should receive trophic feeds or full nutrition by enteral route.6
Pancreatitis
- Oral feeding should be attempted as soon as abdominal pain is decreasing and inflammatory markers are improving.13
- A regular solid, low-fat diet should be initiated, rather than slowly advancing from a clear liquid diet.13
- In severe acute pancreatitis, initiation of enteral nutrition within 48 hours of presentation is associated with improved outcomes.13
- There is no difference in outcomes between gastric and postpyloric feeding.14
- Initiation of parenteral nutrition may be delayed for up to 5 days to allow for a trial of oral or enteral feeding.13
Surgical patients
- Consider postponing surgery to provide 7-10 days of preoperative nutrition supplementation in patients with risk of severe undernutrition.16
- Consider postoperative nutritional support if patients are at risk for severe undernutrition, are unable to eat for more than 7 days perioperatively, or are unable to maintain oral intake above 60% of recommended intake for more than 10 days.16
- Consider total parenteral nutrition in cases of impaired gastrointestinal function and absorption, high output enterocutaneous fistulae, obstructive lesions that do not allow enteral refeeding, or prolonged gastrointestinal failure.16
Prolonged Starvation
- Because of the high risk of refeeding syndrome, patients greater than 30% below ideal body weight should be hospitalized for close monitoring during refeeding.12
- Typical goal for weight gain is no greater than 2-3 pounds per week.10
- Total parenteral nutrition should be reserved for extreme cases, and if used, carbohydrate intake should not exceed 7 mg/kg/min.12
Stroke
- Enteral nutrition should be initiated within 24-48 hours of initial hospitalization if a patient is estimated to require feeding for more than 5 days and/or remain nil per os for 5-7 days.
- If a patient is intubated with increased intracranial pressure, this could delay gastric motility requiring a postpyloric tube placement.
- Initial placement of percutaneous endoscopic gastrostomy tubes can be considered if the hospitalized patient is expected to require nutritional support for greater than 30 days. Most patients will have improved dysphagia symptoms within 1 month of their acute stroke, although as many as 40% can have continued dysphagia up to 1 year.10
Back to the Case
The patient was admitted for a common general medical condition, but it is important to recognize that malnutrition was present on admission with weight loss and generalized fluid overload. Furthermore, he is at high nutritional risk because of his low body weight, poor oral intake, and dysphagia. Additionally, the acute inflammation from pneumonia places him in an increased catabolic state.
He was able to maintain some volitional oral intake, but after 7 days of close monitoring by a licensed dietician, it was determined that he was unable to meet his nutritional needs via the oral route. A percutaneous endoscopic gastrostomy tube was placed, and tube feeds were initiated, because his dysphagia – which was a significant factor contributing to his inability to meet his nutritional needs orally – was expected to persist for greater than 30 days.
Bottom Line
Nutrition support should be initiated in this patient with malnutrition on admission and high nutritional risk.
Dr. Abalos is an assistant professor at Georgetown University Medical Center in Washington. Dr. Corbett is an assistant professor at the University of Oklahoma Health Sciences Center in Oklahoma City.
References
1. Correia MI et al. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003 Jun;22(3):235-9.
2. Felder S et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015 Nov-Dec;31(11-12):1385-93.
3. White JV et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012 May;112(5):730-8.
4. McClave SA et al. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
5. Mueller C et al. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enter Nutr. 2011 Jan;35(1):16-24.
6. McClave SA et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. JPEN J Parenter Enter Nutr. 2016 Feb;40(2):159-211.
7. August D et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enter Nutr. 2002 Jan-Feb:26(1):SUPPL:1SA-138SA.
8. Kirkland LL et al. Nutrition in the hospitalized patient. J Hosp Med. 2013 Jan;8(1):52-8.
9. National Collaborating Centre for Acute Care, February 2006. Nutrition support in adults Oral nutrition support, enteral tube feeding and parenteral nutrition. National Collaborating Centre for Acute Care, London. Available from www.rcseng.ac.uk.
10. Corrigan ML et al. Nutrition in the stroke patient. Nutr Clin Pract. 2011 Jun;26(3):242-52.
11. Loser C et al. ESPEN guidelines on artificial enteral nutrition – Percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005 Oct;24(5):848-61.
12. Mehler PS et al. Nutritional rehabilitation: Practical guidelines for refeeding the anorectic patient. J Nutr Metab. 2010. doi: 10.1155/2010/625782.
13. Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul-Aug;13(4 Suppl 2):e1-15.
14. Singh N et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: A noninferiority randomized controlled trial. Pancreas. 2012 Jan;41(1):153-9.
15. Braga M et al. ESPEN guidelines on parenteral nutrition: Surgery. Clin Nutr. 2009 Aug;28(4):378-86.
16. Weimann A et al. ESPEN Guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr. 2006 Apr;25(2):224-44.
Additional reading
- Kirkland LL et al. Nutrition in the Hospitalized Patient. J Hosp Med. 2013 Jan;8(1):52-8.
- McClave SA et al. ACG Clinical Guideline: Nutrition Therapy in the Adult Hospitalized Patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
Quiz: Recognizing Malnutrition
Which of the following is not a criteria for the diagnosis of malnutrition?
A. Weight loss
B. Insufficient energy intake
C. Prealbumin
D. Diminished handgrip strength
Answer: C. Prealbumin. Laboratory indicators of nutrition, such as albumin, prealbumin, and transferrin, and markers of infection or inflammation are not recommended for the determination of nutritional status. Because negative acute-phase reactants, they instead can be used as surrogate markers of nutritional risk and degree of inflammation
Key Points
- At the time of admission to the hospital, malnutrition is present in 20-50% of patients. All hospitalized patients should be screened for nutritional risk and nutritional support should be considered if patients are not expected to be able to meet nutritional needs for more than 7 days.
- Patients with severe malnutrition on admission, severe critical illness, or severe acute pancreatitis should be provided nutritional support within 24-48 hours.
- Use the gut! Nutritional support should be provided via the most physiologic route possible. Total parenteral nutrition (TPN) should be reserved for patients in whom adequate nutrition cannot be provided enterally.
- Consider a percutaneous endoscopic gastrostomy (PEG) tube if the patient is expected to require tube feedings for more than 30 days.
- Patients with severe malnutrition who are given nutritional support are at high risk of developing refeeding syndrome, which manifests as electrolyte depletions and heart failure or volume overload.
Case
A 60-year-old male with a history of head & neck cancer, treated with radical neck dissection and radiation 5 years prior is admitted with community-acquired pneumonia and anasarca. Prior to admission, he was on a soft dysphagia diet and reports increased difficulty with solid foods and weight loss from 70 kg to 55 kg over 2.5 years. Should nutritional support be initiated?
Background
Malnutrition is associated with increased hospital mortality, decreased functional status and quality of life, infections, longer length of stay, higher hospital costs, and more frequent nonelective readmissions.1,2
Identifying patients who are malnourished or at risk for malnutrition
An international consensus committee recommended the following criteria for the diagnosis of undernutrition if two of six are present3:
- Insufficient energy intake.
- Weight loss.
- Loss of muscle mass.
- Loss of subcutaneous fat.
- Localized or generalized fluid accumulation that may sometimes mask weight loss.
- Diminished functional status as measured by handgrip strength.
The joint commission requires that all patients admitted to acute care hospitals be screened for risk of malnutrition within 24 hours. The American College of Gastroenterologists recommends using a validated score to assess nutritional risk, such as the Nutritional Risk Score (NRS) 2002 or the NUTRIC (Nutrition Risk in the Critically Ill) Score, which use a combination of nutritional status and diet-related factors – weight loss, body mass index, and food intake – and also severity of illness measurements.4
- Starvation-related malnutrition, such as anorexia nervosa, presents with a deficiency in calories and protein without inflammation, .
- Chronic disease–related malnutrition, such as that caused chronic obstructive pulmonary disease, cancer, and obesity, presents with mild to moderate inflammation.
- Acute disease or injury–related malnutrition, such as that caused by sepsis, burns, and trauma, presents with acute and severe inflammation.
Laboratory indicators such as albumin, prealbumin, and transferrin are not recommended for the determination of nutritional status. Instead, as negative acute-phase reactants, they can be used as surrogate markers of nutritional risk and degree of inflammation.4
Overview of the data
What are the indications for initiating nutritional support, and what is the optimal timing for initiation?
Patients who are malnourished or at significant risk for becoming malnourished should receive specialized nutrition support. Early enteral nutrition should be initiated within 24-48 hours of admission in critically ill patients with high nutritional risk who are unable to maintain volitional intake.6 In the absence of preexisting malnutrition, nutritional support should be provided for patients with inadequate oral intake for 7-14 days or for those in whom inadequate oral intake is expected over the same time period.7
How should nutritional support be administered?
Dietary modification and supplementation
In patients who can tolerate an oral diet, dietary modifications may be made in order to facilitate the provision of essential nutrients in a well-tolerated form. Modifications may include adjusting the consistency of foods, energy value of foods, types of nutrients consumed, and number and frequency of meals.8 Commercial meal replacement beverages are widely used to support a standard oral diet, but there is no data to support their routine use.7
Enteral nutrition
Enteral nutrition (EN) is the method of choice for administering nutrition support. Contraindications to enteral feeding include diffuse peritonitis, intestinal obstruction, and gastrointestinal ischemia.9 The potential advantages of EN over parenteral nutrition (PN) include decreased infection rate, decreased total complications, and shorter length of stay, but there has been no observed difference in mortality. EN is also suggested to have nonnutritional benefits related to providing luminal nutrients – these include maintaining gut integrity, beneficial immune responses, and favorable metabolic responses that help maintain euglycemia and enhance more physiologic fuel utilization.4
Enteral feeding can be administered through the following routes of access:
- Nasogastric tubes: A nasogastric or orogastric tube with radiologic confirmation of positioning is the first line of enteral access. Gastric feeding is preferred because it is well tolerated in the majority of patients, is more physiological, requires a lower level of expertise, and minimizes any delay in initiation of feeding.
- Postpyloric tubes: Postpyloric feeding tubes are indicated if gastric feeding is poorly tolerated or if the patient is at high risk for aspiration because jejunal feedings decrease the incidence of reflux, regurgitation, and aspiration.
- Percutaneous access: When long-term enteral access is required – that is, for greater than 4 weeks – a percutaneous enteral access device should be placed. Prolonged use of a nasoenteric tube may be associated with erosion of the nares and an increase in the incidence of aspiration pneumonia, sinusitis, and esophageal ulceration or stricture. Patients who have had a stroke are the most likely to benefit from percutaneous endoscopic gastrostomy placement, as 40% of patients can have continued dysphagia as long as 1 year after.4,10 Absolute contraindications for PEG placement include serious coagulation disorders (international normalized ratio greater than 1.5; fewer than 50,000 platelets/mcL), sepsis, abdominal wall infections, marked peritoneal carcinomatosis, peritonitis, severe gastroparesis, gastric outlet obstruction, or a history of total gastrectomy. Risks often outweigh benefits in patients who have cirrhosis with ascites, patients undergoing peritoneal dialysis, and patients who have portal hypertension with gastric varices, but PEG can be considered on a case-by-case basis.11
Parenteral nutrition
Parenteral nutrition is reserved for patients in whom enteral feeding is contraindicated or who fail to meet their nutritional needs with enteral feedings. If EN is not feasible, then parenteral nutrition should be initiated as soon as possible in patients who had high nutritional risk on admission. Otherwise, PN should not be initiated during the first week of hospitalization because there is evidence to suggest net harm when initiated early. Supplemental PN may be considered for patients already on EN who are unable to meet more than 60% of their energy and protein requirements by the enteral route alone, but again, this should only be considered after 7-10 days on EN. PN is generally stopped when the patients achieve more than 60% of their energy and protein goals from EN.4
How should patients be monitored while receiving nutritional support?
If a patient is severely malnourished and refeeding is initiated, serious complications can occur, which are summarized in Table 1; these complications can include severe electrolyte disorders, fluid shifts, and even death.12 Refeeding syndrome occurs in the first few days of initiating a diet in severely malnourished patients, and its severity is directly related to the severity of malnutrition prior to refeeding. The National Institute of Health and Clinical Excellence created criteria to identify patients at risk for refeeding syndrome; these criteria include having a BMI less than 18.5 kg/m2; unintentional weight loss of greater than 10% in the previous 3-6 months; little or no nutritional intake for more than 5 days; low levels of potassium, phosphorus, or magnesium before refeeding; and a history of alcohol misuse or taking certain drugs, such as insulin, chemotherapy, antacids, or diuretics.9
Aspiration is a risk with enteral feeding – the risk factors include being older than 70 years, altered mental status, supine position, and bolus rather than continuous infusion.4 Postpyloric feeding may reduce the risk of aspiration. Expert consensus suggests elevating the head of the bed by 30°-40° for all intubated patients receiving EN, as well as administering chlorhexidine mouthwash twice daily.6
Diarrhea is very common in patients receiving EN. After evaluating for other etiologies of diarrhea, tube feeding–associated diarrhea may be managed first by using a fiber-containing formulation. Fiber should be avoided in patients at risk for bowel ischemia or severe dysmotility. If diarrhea persists despite fiber, small peptide formulations, also known as elemental tube feeds, may be used.4,6
Gastric residual volume (GRV) is commonly monitored in patients receiving enteral nutrition. However, the American College of Gastroenterology does not recommend using GRVs to monitor EN feeding because it is a poor marker of clinically meaningful variables, such as gastric emptying, risk of aspiration, and risk of poor outcomes, and increases the risk of tube clogging and inadequate delivery of EN. If GRVs are being monitored, tube feedings should not be withheld because of high GRVs when there are no other signs of intolerance.4 Nausea may be managed by changing a patient from bolus to continuous feedings or by adding promotility agents such as metoclopramide or erythromycin.6
Special considerations in common conditions treated by hospitalists
The principles outlined above are general guidelines that are applicable to most patients requiring nutrition support. We have highlighted special considerations for common conditions in hospitalized patients who require nutritional support below.
Critical Illness
- Defer enteral nutrition until patient is fully resuscitated and hemodynamically stable.
- Severely malnourished or high nutritional-risk patients should be advanced toward goals as quickly as can be tolerated over 24-48 hours.
- Patients with acute respiratory distress syndrome or acute lung injury, or those expected to require mechanical ventilation for more than 72 hours, should receive trophic feeds or full nutrition by enteral route.6
Pancreatitis
- Oral feeding should be attempted as soon as abdominal pain is decreasing and inflammatory markers are improving.13
- A regular solid, low-fat diet should be initiated, rather than slowly advancing from a clear liquid diet.13
- In severe acute pancreatitis, initiation of enteral nutrition within 48 hours of presentation is associated with improved outcomes.13
- There is no difference in outcomes between gastric and postpyloric feeding.14
- Initiation of parenteral nutrition may be delayed for up to 5 days to allow for a trial of oral or enteral feeding.13
Surgical patients
- Consider postponing surgery to provide 7-10 days of preoperative nutrition supplementation in patients with risk of severe undernutrition.16
- Consider postoperative nutritional support if patients are at risk for severe undernutrition, are unable to eat for more than 7 days perioperatively, or are unable to maintain oral intake above 60% of recommended intake for more than 10 days.16
- Consider total parenteral nutrition in cases of impaired gastrointestinal function and absorption, high output enterocutaneous fistulae, obstructive lesions that do not allow enteral refeeding, or prolonged gastrointestinal failure.16
Prolonged Starvation
- Because of the high risk of refeeding syndrome, patients greater than 30% below ideal body weight should be hospitalized for close monitoring during refeeding.12
- Typical goal for weight gain is no greater than 2-3 pounds per week.10
- Total parenteral nutrition should be reserved for extreme cases, and if used, carbohydrate intake should not exceed 7 mg/kg/min.12
Stroke
- Enteral nutrition should be initiated within 24-48 hours of initial hospitalization if a patient is estimated to require feeding for more than 5 days and/or remain nil per os for 5-7 days.
- If a patient is intubated with increased intracranial pressure, this could delay gastric motility requiring a postpyloric tube placement.
- Initial placement of percutaneous endoscopic gastrostomy tubes can be considered if the hospitalized patient is expected to require nutritional support for greater than 30 days. Most patients will have improved dysphagia symptoms within 1 month of their acute stroke, although as many as 40% can have continued dysphagia up to 1 year.10
Back to the Case
The patient was admitted for a common general medical condition, but it is important to recognize that malnutrition was present on admission with weight loss and generalized fluid overload. Furthermore, he is at high nutritional risk because of his low body weight, poor oral intake, and dysphagia. Additionally, the acute inflammation from pneumonia places him in an increased catabolic state.
He was able to maintain some volitional oral intake, but after 7 days of close monitoring by a licensed dietician, it was determined that he was unable to meet his nutritional needs via the oral route. A percutaneous endoscopic gastrostomy tube was placed, and tube feeds were initiated, because his dysphagia – which was a significant factor contributing to his inability to meet his nutritional needs orally – was expected to persist for greater than 30 days.
Bottom Line
Nutrition support should be initiated in this patient with malnutrition on admission and high nutritional risk.
Dr. Abalos is an assistant professor at Georgetown University Medical Center in Washington. Dr. Corbett is an assistant professor at the University of Oklahoma Health Sciences Center in Oklahoma City.
References
1. Correia MI et al. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003 Jun;22(3):235-9.
2. Felder S et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015 Nov-Dec;31(11-12):1385-93.
3. White JV et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012 May;112(5):730-8.
4. McClave SA et al. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
5. Mueller C et al. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enter Nutr. 2011 Jan;35(1):16-24.
6. McClave SA et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. JPEN J Parenter Enter Nutr. 2016 Feb;40(2):159-211.
7. August D et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enter Nutr. 2002 Jan-Feb:26(1):SUPPL:1SA-138SA.
8. Kirkland LL et al. Nutrition in the hospitalized patient. J Hosp Med. 2013 Jan;8(1):52-8.
9. National Collaborating Centre for Acute Care, February 2006. Nutrition support in adults Oral nutrition support, enteral tube feeding and parenteral nutrition. National Collaborating Centre for Acute Care, London. Available from www.rcseng.ac.uk.
10. Corrigan ML et al. Nutrition in the stroke patient. Nutr Clin Pract. 2011 Jun;26(3):242-52.
11. Loser C et al. ESPEN guidelines on artificial enteral nutrition – Percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005 Oct;24(5):848-61.
12. Mehler PS et al. Nutritional rehabilitation: Practical guidelines for refeeding the anorectic patient. J Nutr Metab. 2010. doi: 10.1155/2010/625782.
13. Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul-Aug;13(4 Suppl 2):e1-15.
14. Singh N et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: A noninferiority randomized controlled trial. Pancreas. 2012 Jan;41(1):153-9.
15. Braga M et al. ESPEN guidelines on parenteral nutrition: Surgery. Clin Nutr. 2009 Aug;28(4):378-86.
16. Weimann A et al. ESPEN Guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr. 2006 Apr;25(2):224-44.
Additional reading
- Kirkland LL et al. Nutrition in the Hospitalized Patient. J Hosp Med. 2013 Jan;8(1):52-8.
- McClave SA et al. ACG Clinical Guideline: Nutrition Therapy in the Adult Hospitalized Patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
Quiz: Recognizing Malnutrition
Which of the following is not a criteria for the diagnosis of malnutrition?
A. Weight loss
B. Insufficient energy intake
C. Prealbumin
D. Diminished handgrip strength
Answer: C. Prealbumin. Laboratory indicators of nutrition, such as albumin, prealbumin, and transferrin, and markers of infection or inflammation are not recommended for the determination of nutritional status. Because negative acute-phase reactants, they instead can be used as surrogate markers of nutritional risk and degree of inflammation
Key Points
- At the time of admission to the hospital, malnutrition is present in 20-50% of patients. All hospitalized patients should be screened for nutritional risk and nutritional support should be considered if patients are not expected to be able to meet nutritional needs for more than 7 days.
- Patients with severe malnutrition on admission, severe critical illness, or severe acute pancreatitis should be provided nutritional support within 24-48 hours.
- Use the gut! Nutritional support should be provided via the most physiologic route possible. Total parenteral nutrition (TPN) should be reserved for patients in whom adequate nutrition cannot be provided enterally.
- Consider a percutaneous endoscopic gastrostomy (PEG) tube if the patient is expected to require tube feedings for more than 30 days.
- Patients with severe malnutrition who are given nutritional support are at high risk of developing refeeding syndrome, which manifests as electrolyte depletions and heart failure or volume overload.