User login
Unplanned Exubations in the ICU: Risk Factors and Strategies for Reducing Adverse Events
From the MetroHealth System, Cleveland, OH.
Abstract
- Objective: To describe risk factors for unplanned extubation (UE) among critically ill adults requiring mechanical ventilation and to identify strategies to reduce the occurrence of this adverse event.
- Methods: Review of the literature.
- Results: Inadvertent removal of an endotracheal tube, or a UE, occurs in 7% to 22.5% of mechanically ventilated adult patients and is often due to deliberate patient removal. Despite the multitude of research examining risk factors and predictors of UE, rates have remained unchanged for the past 2 decades. Risk factors can be classified by intensive care unit (ICU) type, including medical ICUs, surgical ICUs, and mixed medical-surgical ICUs. The majority of risk factors for UEs across ICUs may be amenable to changes in unit processes, such as programs for agitation management, use of weaning protocols, increased surveillance of patients, and ongoing education for patients and health care staff.
- Conclusion: Prevention of UE remains an elusive target. Changes in unit processes that target identified risk factors may be an effective method to decrease prevalence of UE.
Unplanned extubation (UE) is the inadvertent removal of an endotracheal tube, either by a patient (deliberate self-extubation), or by a member of the health care team providing routine care such as repositioning, suctioning, or procedures (accidental extubation). Approximately 7% to 22.5% of mechanically ventilated patients in the intensive care unit (ICU) experience UE [1–7]. Estimates are likely higher, as current regulatory and accreditation standards do not include mandatory reporting of this event. Despite numerous studies investigating risk factors associated with UE, it remains a prevalent problem with adverse outcomes for patients and hospitals. The purpose of this review is to provide a summary of the literature on risk factors for UE, review effects on patient and organizational outcomes, and identify evidence-based strategies for reducing occurrence of UE among mechanically ventilated patients.
Prevalence of Unplanned Exubation
There is substantial heterogeneity in how UE is calculated and reported in the research literature. UE is calculated as the number of UE events per 100 or 1000 patient days, or the number of UE per total ventilator days. Rates of UE are also reported as the proportion of patients who experience UE out of all intubated patients over a set time period [8]. Despite efforts aimed at mitigating risk factors for UE, rates have remained static over the past 2 decades. Reported UE rates from 1994–2002 were 2.6% to 14% [3,6,9–11], while rates from 2004–2014 ranged from 1% to 22% [3–5,8,12–15]. Interventions utilizing a multidisciplinary approach have been implemented with the aim of decreasing UE, yet few have proven successful on improving rates nationally.
Unplanned self-extubation by the patient (deliberate self-extubation) is the most common type of UE [3,10,12,16–18]. A multicenter trial of 426 patients from 11 medical centers indicates that 46 patients experienced UE, with 36 of these (78.2%) caused by patient self-extubation [6]. Prospective single-site studies report similar or higher estimates of patient self-extubation, ranging from 75.8% to 91.7% [3,5], while a multisite study of 10,112 patients revealed 32 of 35 UE (91.4%) were due to patient self-extubation [12]. Similarly, a 4-year analysis of 85 UEs reported 82 incidences (96.5%) were a result of deliberate patient removal [13]. Patients either physically pull out the endotracheal tube or use their tongue or coughing/gagging maneuvers to displace or intentionally remove the endotracheal tube [5]. Only 3% to 8% of UEs are caused by inadvertent removal by health care staff [3,5,12,13].
Effects on Patient and Organizational Outcomes
Regardless of the cause of the UE, there are adverse consequences for both patients and hospitals. Some patients who experience UE have higher rates of in-hospital mortality; however, this is often due to contributing factors associated with severity of injury, the need for reintubation, and underlying chronic diseases [13]. Patients who experience accidental UE have higher incidence of nosocomial pneumonia (27.6% vs. 138%, P = 0.002) [11], longer duration of mechanical ventilation, and increased length of stay (LOS) [7,13]. While some studies report UE can result in serious consequences such as respiratory distress, hypoxia [13], and even death [6,12], others report lower mortality and length of stay when UE occurs, likely due to the fact that many patients are ready for liberation from mechanical ventilation at the time of UE [5,15].
Despite the emergent nature of UE, not all patients experience immediate reintubation. Many instances of UE occur during patient weaning trials or in preparation for planned extubations [5,11], which explains why only 10% to 60% of patients require reintubation [3,5,10,11,15,19,20]. When reintubation is necessary, it results in increased number of ventilator days [10,11], and increased ICU and hospital LOS [1,11]. There is little evidence directly linking reintubation with in-hospital mortality; however, it can cause serious complications such as hypotension, hypertension, arrhythmias, and airway trauma [21]. For hospitals and health care organizations, the need for reintubation results in increased hospital costs, estimated to be $1000 per reintubation event [17,22]. This estimate does not take into account additional costs incurred with increased ICU care, longer periods of mechanical ventilation, and increased LOS. Estimates of these additional costs in pediatric patients are approximately $36,000 [23]. Costs are likely higher in adult patients, due to multiple comorbidities that often accompany the need for mechanical ventilation, as well as increased pharmacy, lab, and diagnostic charges [1].
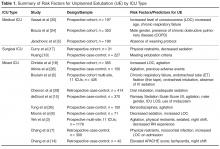
Risk Factors for Unplanned Extubation
Medical ICU Risk Factors
MICUs traditionally have the highest rates of UE [4,8]. Data from a national prevalence study indicated that there were 23.4 episodes of UE in MICUs per 1000 ventilator days [4]. Approximately 9.5% to 15% of all ventilated patients in the MICU experience UE [4,5,8]. Patients in the MICU who require mechanical ventilation often have complex chronic illness with underlying respiratory disease, which can result in prolonged periods of ventilation and increased risk of UE. Specific risk factors investigated in UE research include patient specific factors (age, gender, diagnosis, comorbidities, agitation, level of consciousness, laboratory values), ventilatory factors (ventilator type and setting, type of tracheal tube, method of tube fixation), as well as type of sedation and use of protocols [5,6,24]. Surprisingly, few variables emerge as significant risk factors for UE among MICU patients. Risk factors associated with UE have included male gender [24], presence of chronic obstructive pulmonary disease (COPD) [24], increased level of consciousness [25], and use of weaning protocols [5]. While gender, COPD, and level of consciousness increase risk of UE, the presence of weaning protocols is shown to decrease risk of UE [5]. Although UE are reported most often in MICUs, few risk factors consistently emerge for this specific cohort, making definitive recommendations for prevention of UE difficult.
Surgical ICU Risk Factors
The prevalence of UE for mechanically ventilated patients in the SICU tend to be lower than those for MICU cohorts. Prevalence of UE in the SICU is reported at 1.41 episodes per 100 ventilator days [13], or 6.8 episodes per 1000 ventilator days [4]. Percentages of UE in the SICU range from 2% to 6% [4,8,19]. Similar to MICU patients, critically ill patients in the SICU often have specific risk factors placing them at risk for UE. Causative factors examined in research studies with this population include gender, age, sedation scale scores, need for reintubation, time from intubation to extubation, use of sedatives/analgesics, restraints, ICU nurse experience, location of staff at time of UE, and criteria for extubation [17,19]. Similar to MICU cohorts, few variables are identified as predictors of UE. Significant predictors include use of restraints, decreased sedation [17], and meeting criteria for extubation [19]. Among patients who experienced an UE, 87% were restrained at the time of the UE [17], and most had low levels of sedation (mean Ramsay sedation scale score = 2.42 in the hour preceding the UE). Approximately 64% of patients who experienced UE met criteria for planned extubation and did not require re-intubation [19], suggesting many patients were essentially ready for planned extubation.
Mixed ICU Risk Factors
The majority of research investigating risk factors for UE is conducted within medical-surgical or mixed/general ICUs. The prevalence of UE within this type of unit is reported at 1.59 episodes per 100 patient days [6], or approximately 2% to 10% [4,6,7]. Among this population, potential risk factors are similar to those included in solely MICU or SICU studies. Because of the high number of studies investigating UE in a mixed ICU setting, there are significantly more variables included in as potential risk factors. Variables include patient age, gender, admission diagnosis, injury severity using Acute Physiological and Chronic Health Evaluation (APACHE II), ICU and hospital LOS, patient level of consciousness, agitation, days of mechanical ventilation, ventilator settings, nosocomial infection, sedation, physical restraints, vital signs [7,14,26], laboratory values, medication types, and body mass index [15,26]. One study also included time of UE and ICU nurse level of experience [3]. Among all factors, several were significant predictors of UE: male gender [15], decreased sedation and increased level of consciousness [8], agitation [3,19,26], use of restraints [3,7], sedation practices (particularly use of benzodiazapines) [3,7,15,26,27], lack of strong tube fixation, absence of IV sedation, and orotracheal intubation [6]. UE were more likely to occur on the night shift and among staff that included nurses with fewer years of experience [3]. Many episodes of UE occurred during weaning [10] or among patients who could communicate and were alert [3]. One study reports 57% of patients who intentionally self-extubated explained they simply removed the tube because it was uncomfortable [3].
Strategies for Reducing Adverse Events
Agitation Management
The majority of studies cited agitation, altered level of consciousness, or inadequate sedation as risk factors for UE [3,6–8,15,17,18,25,26,28,29]. These factors directly impact restraint use, another common risk factor for UE [3,7,17]. A key recommendation for agitation management is to identify the source of agitation, which is often caused by delirium onset in the ICU [30–32]. Prevalence of delirium in the ICU ranges from 20% to 80% [33–35]. ICU patients are at high risk for delirium due to sleep deprivation, older age, restraints, abnormal lab values, medications, infection, and respiratory complications [31]. Treatment for delirium centers on prevention, early recognition, interdisciplinary and pharmacologic protocols, increased nursing presence, and use of short-acting sedation when necessary [30–32,36]. While there is no research specifically linking delirium to UE, a quality analysis of risk factors present at the time of UE using bow-tie analysis methods identified delirium as a key factor present in the majority of UE cases [36]. It is possible that agitation reported in other studies investigating risk factors for UE may actually be reflective of underlying delirium. Routine screening using validated tools, such as the Confusion Assessment Method-ICU (CAM-ICU) [37] would aid in early detection and management of delirium, and would provide a standardized method for exploring the relationship of delirium and UE in future trials.
Integration of Weaning Protocols
Protocol-directed weaning is beneficial for decreasing ventilator days, time to wean from mechanical ventilation, and ICU LOS [38]. A systematic review including 7 trials (2434 patients) comparing protocol/non-protocol for weaning from mechanical ventilation reported a 26% decrease in the mean duration of mechanical ventilation for the protocol groups (95% CI 13%–37%, P < 0.001), a 70% reduction in time to wean, (95% CI 27%–88%, P = 0.009), and a decrease in ICU LOS by 11% (95% CI 3%–19%, P = 0.01). Weaning protocols are also an important risk factor for UE [5]. Findings from a prospective cohort study specifically identify the presence of weaning protocols as an important factor for reducing UE; patients who had weaning protocols ordered and followed were least likely to experience UE (P = 0.02) [5]. A separate quality improvement initiative demonstrated an overall decrease in the number of UEs (from 5.2% to 0.9%) after implementing weaning protocols as standard of care [39]. Considering many UEs occur during weaning [10], integration of weaning protocols aids in expediting the process and ensuring timely extubation.
Increased Surveillance
Increasing surveillance and monitoring of ventilated patients is a recommendation based on risk factors presented at the time of UE. Specifically, staffing levels and shifts and the use of physical restraints are variables associated with UE that are amendable to changes in unit processes based on increased surveillance. It is reported that 40% to 76% of UEs occurred during the night shift [14,17,24,40]; many more occur during change of shift or when there is not a nurse present at the bedside [3,17]. Recent trends towards mandatory bedside reporting is a specific intervention that may positively impact UE among patients in the ICU [41]. Meta-analyses of observational studies investigating the effect of nurse staffing on hospital outcomes indicate that increasing the number of RNs is associated with decreased risk of adverse patient outcomes, including UE [42,43]. The addition of 1 additional nurse per patient day can result in a 51% decrease in UE, while a decrease in nursing workload could result in a 45% decrease in UE [42]. Data from a national prevalence study reports ICUs with fewer available resources, including staff, experienced a higher number of UEs [4].
Increasing surveillance by nursing and health care staff may also impact prevalence of physical restraint use. A significant number of patients who experience UE are physically restrained at the time of the incident, ranging from 40% to 90% of intubated patients [5–7,14,17,40]. It is well documented that UE continue to occur despite the use of restraints [5,7,28,29,44] Patients who are physically restrained often experience higher rates of unplanned extubation (42.9% vs. 16.5% , P < 0.001 in Chang et al’s study [7]), and longer ICU LOS (20.3 days vs. 15.8 days, P = 0.009) [7]. Soft wrist restraints are commonly used to prevent pulling of the endotracheal tube; however, research evidence on UE demonstrates this is not always an effective intervention. Increasing surveillance of ventilated patients, treating their agitation and screening for underlying delirium, and integration of weaning protocols are all interventions that may decrease UE and the need for routine use of physical restraints.
Ongoing Education for Patients and Health Care Staff
Initial and ongoing education about UE, risk factors, and effective interventions is beneficial for patients and health care staff. Although there are no trials investigating effects of educational interventions for patients on UE outcomes, pre-education of surgical patients regarding what to expect while intubated may aid in decreasing delirium risk, agitation, physical restraint use, and possibly UE. Verbal and written educational information during pre-admission testing is a feasible method easily integrated into pre-operative programs.
Because UEs often occur more frequently among less experienced staff, initial education about risk factors for UE is crucial to include in ICU staff orientation programs [3,7]. Educational initiatives should incorporate training on routine delirium screening and avoidance of agitation, use of protocols, and increased surveillance of patients receiving mechanical ventilation [5,15,17,39,45]. Ongoing education of staff regarding ventilatory equipment and risk factors for UE can be particularly effective in decreasing UE [46]. Initial educational efforts should be followed by routine updates for all members of the healthcare team about ongoing quality improvement efforts to monitor UE. Associated factors for UE that may be unit- or process-specific, including methods for endotracheal tube securement and intra-hospital transport, should be communicated with all individuals involved in patient care. Integration of continuous quality improvement programs can decrease UE rates by 22% to 53% [16]. Quality efforts typically focus on standardization of reporting and tracking tools, protocol implementations, and ongoing monitoring, auditing, and recording of UE.
Current Trends and Future Directions
Recent trends in critical care recommendations may mitigate potential risk factors identified in UE research. Integration of lightened sedation and daily wake up periods for intubated patients may decrease prevalence of risk factors for UE, specifically agitation, physical restraint use, and altered level of consciousness [30], while routine weaning protocols may improve ventilatory outcomes, including UE [5,38,40]. Nursing bedside report and purposeful hourly rounding are quickly emerging as mainstays of professional nursing care [41]. Inherent in these 2 initiatives are increased surveillance and vigilance by health care staff, which can result in timely extubation of those who indicate readiness, as well as decreased incidence of adverse events. Delirium remains a key factor that may be a likely cause for UE; recent trends towards early detection and proper management of delirium among ICU staff may result in improved ventilatory outcomes, including weaning, planned extubation, and the prevalence of UE.
Another important trend in critical care is the emergence of a neurocritical care specialty and routine admission of neurocritically ill patients to neuroscience ICUs [47,48]. However, there are no studies investigating prevalence of UE among these patients, who often have higher rates of agitation or restlessness due to cognitive impairment. Among general ICUs, patients with a primary respiratory diagnosis accounted for 23% of all UE in one study, while those with a neurological diagnosis accounted for the second highest percentage (12%) among the study population [15]. A separate study concluded that presence of neurological injury with a concomitant nosocomial infection increased risk of UE among patients in a mixed ICU [7]. A recent systematic review of weaning protocols highlights positive effects on ventilatory outcomes but cites lack of evidence for effectiveness of protocols among those with neurological injury [38]. Areas for future UE research should include factors specific to this patient population, as they may be at higher risk for adverse ventilatory outcomes due to the nature of the neurological injury.
Conclusion
Prevention of UE remains an elusive target, evidenced by little change in reported rates over 2 decades. Research provides data on risk factors that may be patient, unit, or process related. Structuring prevention efforts around modifiable risk factors for UE is a feasible approach amenable to ongoing monitoring for effectiveness. Integration of current trends in health care safety and quality may produce an added benefit of reducing the occurrence of UE in critical care units. Future research evaluating these trends and the prevalence of UE in subspecialty populations is warranted.
Corresponding author: Molly McNett, PhD, RN, CNRN, Attn: NBO, MetroHealth Medical Center, 2500 MetroHealth Drive; Cleveland, OH 44109, mmcnett@metrohealth.org.
Financial disclosures: None.
1. Krinsley JS, Barone JE. The drive to survive: unplanned extubation in the ICU. Chest 2005;128:560–6.
2. Coppolo DP, May JJ. Self-extubations. A 12-month experience. Chest 1990;98:165–9.
3. Yeh SH, Lee LN, Ho TH, et al. Implications of nursing care in the occurrence and consequences of unplanned extubation in adult intensive care units. Int J Nurs Stud 2004;41:255–62.
4. Mion LC, Minnick AF, Leipzig R, et al. Patient-initiated device removal in intensive care units: a national prevalence study. Crit Care Med 2007;35:2714–20.
5. Jarachovic M, Mason M, Kerber K. The role of standardized protocols in unplanned extubations in a medical intensive care unit. Am J Crit Care 2011;20:304–11.
6. Boulain T. Unplanned extubations in the adult intensive care unit: a prospective multicenter study. Association des Reanimateurs du Centre-Ouest. Am J Resp Crit Care Med 1998;157(4 Pt 1):1131–7.
7. Chang LY, Wang KW, Chao YF. Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study. Am J Crit Care 2008;17:408–15.
8. Moons P, Sels K, De Becker W, et al. Development of a risk assessment tool for deliberate self-extubation in intensive care patients. Intensive Care Med 2004;30:1348–55.
9. Chiang AA, Lee KC, Lee JC, Wei CH. Effectiveness of a continuous quality improvement program aiming to reduce unplanned extubation: a prospective study. Intensive Care Med 1996;22:1269–71.
10. Betbese AJ, Perez M, Bak E, et al. A prospective study of unplanned endotracheal extubation in intensive care unit patients. Crit Care Med 1998;26:1180–6.
11. de Lassence A, Alberti C, Azoulay E, et al. Impact of unplanned extubation and reintubation after weaning on nosocomial pneumonia risk in the intensive care unit: a prospective multicenter study. Anesthesiology 2002;97:148–56.
12. Kapadia FN, Tekawade PC, Nath SS, et al. A prolonged observational study of tracheal tube displacements: Benchmarking an incidence <0.5-1% in a medical-surgical adult intensive care unit. Ind J Crit Care Med 2014;18:273–7.
13. Lee JH, Lee HC, Jeon YT, et al. Clinical outcomes after unplanned extubation in a surgical intensive care population. World J Surg 2014;38:203–10.
14. Chang LC, Liu PF, Huang YL, et al. Risk factors associated with unplanned endotracheal self-extubation of hospitalized intubated patients: a 3-year retrospective case-control study. Appl Nurs Res 2011;24:188–92.
15. de Groot RI, Dekkers OM, Herold IH, et al. Risk factors and outcomes after unplanned extubations on the ICU: a case-control study. Crit Care 2011;15:R19.
16. da Silva PS, Fonseca MC. Unplanned endotracheal extubations in the intensive care unit: systematic review, critical appraisal, and evidence-based recommendations. Anesth Analg 2012;114:1003–14.
17. Curry K, Cobb S, Kutash M, Diggs C. Characteristics associated with unplanned extubations in a surgical intensive care unit. Am J Crit Care 2008;17:45–51.
18. Christie JM, Dethlefsen M, Cane RD. Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth 1996;8:289–93.
19. Huang YT. Factors leading to self-extubation of endotracheal tubes in the intensive care unit. Nurs Crit Care 2009;14:68–74.
20. Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet 2008;371:126–34.
21. Mort TC. Unplanned tracheal extubation outside the operating room: a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg 1998;86:1171–6.
22. Jaber S, Chanques G, Altairac C, et al. A prospective study of agitation in a medical-surgical ICU: incidence, risk factors, and outcomes. Chest 2005;128:2749–57.
23. Roddy DJ, Spaeder MC, Pastor W, Stockwell DC, Klugman D. Unplanned extubations in children: impact on hospital cost and length of stay. Ped Crit Care Med 2015.
24. Bouza C, Garcia E, Diaz M, et al. Unplanned extubation in orally intubated medical patients in the intensive care unit: a prospective cohort study. Heart Lung 2007;36:270–6.
25. Vassal T, Anh NG, Gabillet JM, et al. Prospective evaluation of self-extubations in a medical intensive care unit. Intensive Care Med 1993;19:340-342.
26. Tung A, Tadimeti L, Caruana-Montaldo B, et al. The relationship of sedation to deliberate self-extubation. J Clin Anesth 2001;13:24–9.
27. Tanios M, Epstein S, Grzeskowiak M, et al. Influence of sedation strategies on unplanned extubation in a mixed intensive care unit. Am J Crit Care 2014;23:306–14.
28. Atkins PM, Mion LC, Mendelson W, et al. Characteristics and outcomes of patients who self-extubate from ventilatory support: a case-control study. Chest 1997;112:1317–23.
29. Chevron V, Menard JF, Richard JC, et al. Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med 1998;26:1049–53.
30. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
31. Morandi A, Jackson JC. Delirium in the intensive care unit: a review. Neurol Clin 2011;29:749–63.
32. Banerjee A, Vasilevskis, EE, Pandharipande, P. Strategies to improve delirium assessment practices in the intensive care unit. J Clin Outcomes Manag 2010;17:459–68.
33. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001;286:2703–10.
34. Ely EW, Stephens RK, Jackson JC, et al. Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: a survey of 912 healthcare professionals. Crit Care Med 2004;32:106–12.
35. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 2003;51:591–8.
36. Kerckhoffs MC, van der Sluijs AF, Binnekade JM, Dongelmans DA. Improving patient safety in the ICU by prospective identification of missing safety barriers using the bow-tie prospective risk analysis model. J Patient Safe 2013;9:154–9.
37. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941–8.
38. Blackwood B, Burns KE, Cardwell CR, O’Halloran P. Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients. Cochrane Database Syst Rev 2014;11:CD006904.
39. Chia PL, Santos DR, Tan TC, et al. Clinical quality improvement: eliminating unplanned extubation in the CCU. Int J Health Care Qual Ass 2013;26:642–52.
40. Balon JA. Common factors of spontaneous self-extubation in a critical care setting. Int J Trauma Nurs 2001;7:93–9.
41. Gregory S, Tan D, Tilrico M, et al. Bedside shift reports: what does the evidence say? J Nurs Admin 2014;44:541–5.
42. Kane RL, Shamliyan TA, Mueller C, et al. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care 2007;45:1195–204.
43. Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Crit Care Med 2010;38:1521–8; quiz 1529.
44. Tindol GA, Jr., DiBenedetto RJ, Kosciuk L. Unplanned extubations. Chest 1994;105:1804–7.
45. Chen CM CK, Fong Y, Hsing SC, et al. Age is an important predictor of failed unplanned extubation. Int J Gerontol 2010;4:120–9.
46. Richmond AL, Jarog DL, Hanson VM. Unplanned extubation in adult critical care. Quality improvement and education payoff. Crit Care Nurs 2004;24:32–7.
47. Kurtz P, Fitts V, Sumer Z, et al. How does care differ for neurological patients admitted to a neurocritical care unit versus a general ICU? Neurocrit Care 2011;15:477–80.
48. McNett MM, Horowitz DA. International multidisciplinary consensus conference on multimodality monitoring: ICU processes of care. Neurocrit Care 2014;21 Suppl 2:S215–28.
49. Gardner A, Hughes, D, Cook R, et al. Best practice in stabilisation of oral endotracheal tubes: a systematic review. Database of abstracts of reivews of effects (DARE): Quality-assessed reviews. 2005. York: Center for Reviews and Dissemination.
50. Hofso K, Coyer FM. Part 1: Chemical and physical restraints in the management of mechanically ventliated patients in the ICU: Contributing factors. Intensive Crit Care Nurs 2007; 23:249–55.
51. Kiekkas P, Diamanto A, Panteli E, et al. Unplanned extubation in critially ill adults: Clinical reviews. Nurs Crit Care 2012;18:123–34.
52. King JN, Elliiot VA. Self/unplanned extubation: Safety, surveillance, and monitoring of the mechanically ventilated patient. Crit Care Nurs Clin North Am 2012;24:469–79.
From the MetroHealth System, Cleveland, OH.
Abstract
- Objective: To describe risk factors for unplanned extubation (UE) among critically ill adults requiring mechanical ventilation and to identify strategies to reduce the occurrence of this adverse event.
- Methods: Review of the literature.
- Results: Inadvertent removal of an endotracheal tube, or a UE, occurs in 7% to 22.5% of mechanically ventilated adult patients and is often due to deliberate patient removal. Despite the multitude of research examining risk factors and predictors of UE, rates have remained unchanged for the past 2 decades. Risk factors can be classified by intensive care unit (ICU) type, including medical ICUs, surgical ICUs, and mixed medical-surgical ICUs. The majority of risk factors for UEs across ICUs may be amenable to changes in unit processes, such as programs for agitation management, use of weaning protocols, increased surveillance of patients, and ongoing education for patients and health care staff.
- Conclusion: Prevention of UE remains an elusive target. Changes in unit processes that target identified risk factors may be an effective method to decrease prevalence of UE.
Unplanned extubation (UE) is the inadvertent removal of an endotracheal tube, either by a patient (deliberate self-extubation), or by a member of the health care team providing routine care such as repositioning, suctioning, or procedures (accidental extubation). Approximately 7% to 22.5% of mechanically ventilated patients in the intensive care unit (ICU) experience UE [1–7]. Estimates are likely higher, as current regulatory and accreditation standards do not include mandatory reporting of this event. Despite numerous studies investigating risk factors associated with UE, it remains a prevalent problem with adverse outcomes for patients and hospitals. The purpose of this review is to provide a summary of the literature on risk factors for UE, review effects on patient and organizational outcomes, and identify evidence-based strategies for reducing occurrence of UE among mechanically ventilated patients.
Prevalence of Unplanned Exubation
There is substantial heterogeneity in how UE is calculated and reported in the research literature. UE is calculated as the number of UE events per 100 or 1000 patient days, or the number of UE per total ventilator days. Rates of UE are also reported as the proportion of patients who experience UE out of all intubated patients over a set time period [8]. Despite efforts aimed at mitigating risk factors for UE, rates have remained static over the past 2 decades. Reported UE rates from 1994–2002 were 2.6% to 14% [3,6,9–11], while rates from 2004–2014 ranged from 1% to 22% [3–5,8,12–15]. Interventions utilizing a multidisciplinary approach have been implemented with the aim of decreasing UE, yet few have proven successful on improving rates nationally.
Unplanned self-extubation by the patient (deliberate self-extubation) is the most common type of UE [3,10,12,16–18]. A multicenter trial of 426 patients from 11 medical centers indicates that 46 patients experienced UE, with 36 of these (78.2%) caused by patient self-extubation [6]. Prospective single-site studies report similar or higher estimates of patient self-extubation, ranging from 75.8% to 91.7% [3,5], while a multisite study of 10,112 patients revealed 32 of 35 UE (91.4%) were due to patient self-extubation [12]. Similarly, a 4-year analysis of 85 UEs reported 82 incidences (96.5%) were a result of deliberate patient removal [13]. Patients either physically pull out the endotracheal tube or use their tongue or coughing/gagging maneuvers to displace or intentionally remove the endotracheal tube [5]. Only 3% to 8% of UEs are caused by inadvertent removal by health care staff [3,5,12,13].
Effects on Patient and Organizational Outcomes
Regardless of the cause of the UE, there are adverse consequences for both patients and hospitals. Some patients who experience UE have higher rates of in-hospital mortality; however, this is often due to contributing factors associated with severity of injury, the need for reintubation, and underlying chronic diseases [13]. Patients who experience accidental UE have higher incidence of nosocomial pneumonia (27.6% vs. 138%, P = 0.002) [11], longer duration of mechanical ventilation, and increased length of stay (LOS) [7,13]. While some studies report UE can result in serious consequences such as respiratory distress, hypoxia [13], and even death [6,12], others report lower mortality and length of stay when UE occurs, likely due to the fact that many patients are ready for liberation from mechanical ventilation at the time of UE [5,15].
Despite the emergent nature of UE, not all patients experience immediate reintubation. Many instances of UE occur during patient weaning trials or in preparation for planned extubations [5,11], which explains why only 10% to 60% of patients require reintubation [3,5,10,11,15,19,20]. When reintubation is necessary, it results in increased number of ventilator days [10,11], and increased ICU and hospital LOS [1,11]. There is little evidence directly linking reintubation with in-hospital mortality; however, it can cause serious complications such as hypotension, hypertension, arrhythmias, and airway trauma [21]. For hospitals and health care organizations, the need for reintubation results in increased hospital costs, estimated to be $1000 per reintubation event [17,22]. This estimate does not take into account additional costs incurred with increased ICU care, longer periods of mechanical ventilation, and increased LOS. Estimates of these additional costs in pediatric patients are approximately $36,000 [23]. Costs are likely higher in adult patients, due to multiple comorbidities that often accompany the need for mechanical ventilation, as well as increased pharmacy, lab, and diagnostic charges [1].
Risk Factors for Unplanned Extubation
Medical ICU Risk Factors
MICUs traditionally have the highest rates of UE [4,8]. Data from a national prevalence study indicated that there were 23.4 episodes of UE in MICUs per 1000 ventilator days [4]. Approximately 9.5% to 15% of all ventilated patients in the MICU experience UE [4,5,8]. Patients in the MICU who require mechanical ventilation often have complex chronic illness with underlying respiratory disease, which can result in prolonged periods of ventilation and increased risk of UE. Specific risk factors investigated in UE research include patient specific factors (age, gender, diagnosis, comorbidities, agitation, level of consciousness, laboratory values), ventilatory factors (ventilator type and setting, type of tracheal tube, method of tube fixation), as well as type of sedation and use of protocols [5,6,24]. Surprisingly, few variables emerge as significant risk factors for UE among MICU patients. Risk factors associated with UE have included male gender [24], presence of chronic obstructive pulmonary disease (COPD) [24], increased level of consciousness [25], and use of weaning protocols [5]. While gender, COPD, and level of consciousness increase risk of UE, the presence of weaning protocols is shown to decrease risk of UE [5]. Although UE are reported most often in MICUs, few risk factors consistently emerge for this specific cohort, making definitive recommendations for prevention of UE difficult.
Surgical ICU Risk Factors
The prevalence of UE for mechanically ventilated patients in the SICU tend to be lower than those for MICU cohorts. Prevalence of UE in the SICU is reported at 1.41 episodes per 100 ventilator days [13], or 6.8 episodes per 1000 ventilator days [4]. Percentages of UE in the SICU range from 2% to 6% [4,8,19]. Similar to MICU patients, critically ill patients in the SICU often have specific risk factors placing them at risk for UE. Causative factors examined in research studies with this population include gender, age, sedation scale scores, need for reintubation, time from intubation to extubation, use of sedatives/analgesics, restraints, ICU nurse experience, location of staff at time of UE, and criteria for extubation [17,19]. Similar to MICU cohorts, few variables are identified as predictors of UE. Significant predictors include use of restraints, decreased sedation [17], and meeting criteria for extubation [19]. Among patients who experienced an UE, 87% were restrained at the time of the UE [17], and most had low levels of sedation (mean Ramsay sedation scale score = 2.42 in the hour preceding the UE). Approximately 64% of patients who experienced UE met criteria for planned extubation and did not require re-intubation [19], suggesting many patients were essentially ready for planned extubation.
Mixed ICU Risk Factors
The majority of research investigating risk factors for UE is conducted within medical-surgical or mixed/general ICUs. The prevalence of UE within this type of unit is reported at 1.59 episodes per 100 patient days [6], or approximately 2% to 10% [4,6,7]. Among this population, potential risk factors are similar to those included in solely MICU or SICU studies. Because of the high number of studies investigating UE in a mixed ICU setting, there are significantly more variables included in as potential risk factors. Variables include patient age, gender, admission diagnosis, injury severity using Acute Physiological and Chronic Health Evaluation (APACHE II), ICU and hospital LOS, patient level of consciousness, agitation, days of mechanical ventilation, ventilator settings, nosocomial infection, sedation, physical restraints, vital signs [7,14,26], laboratory values, medication types, and body mass index [15,26]. One study also included time of UE and ICU nurse level of experience [3]. Among all factors, several were significant predictors of UE: male gender [15], decreased sedation and increased level of consciousness [8], agitation [3,19,26], use of restraints [3,7], sedation practices (particularly use of benzodiazapines) [3,7,15,26,27], lack of strong tube fixation, absence of IV sedation, and orotracheal intubation [6]. UE were more likely to occur on the night shift and among staff that included nurses with fewer years of experience [3]. Many episodes of UE occurred during weaning [10] or among patients who could communicate and were alert [3]. One study reports 57% of patients who intentionally self-extubated explained they simply removed the tube because it was uncomfortable [3].
Strategies for Reducing Adverse Events
Agitation Management
The majority of studies cited agitation, altered level of consciousness, or inadequate sedation as risk factors for UE [3,6–8,15,17,18,25,26,28,29]. These factors directly impact restraint use, another common risk factor for UE [3,7,17]. A key recommendation for agitation management is to identify the source of agitation, which is often caused by delirium onset in the ICU [30–32]. Prevalence of delirium in the ICU ranges from 20% to 80% [33–35]. ICU patients are at high risk for delirium due to sleep deprivation, older age, restraints, abnormal lab values, medications, infection, and respiratory complications [31]. Treatment for delirium centers on prevention, early recognition, interdisciplinary and pharmacologic protocols, increased nursing presence, and use of short-acting sedation when necessary [30–32,36]. While there is no research specifically linking delirium to UE, a quality analysis of risk factors present at the time of UE using bow-tie analysis methods identified delirium as a key factor present in the majority of UE cases [36]. It is possible that agitation reported in other studies investigating risk factors for UE may actually be reflective of underlying delirium. Routine screening using validated tools, such as the Confusion Assessment Method-ICU (CAM-ICU) [37] would aid in early detection and management of delirium, and would provide a standardized method for exploring the relationship of delirium and UE in future trials.
Integration of Weaning Protocols
Protocol-directed weaning is beneficial for decreasing ventilator days, time to wean from mechanical ventilation, and ICU LOS [38]. A systematic review including 7 trials (2434 patients) comparing protocol/non-protocol for weaning from mechanical ventilation reported a 26% decrease in the mean duration of mechanical ventilation for the protocol groups (95% CI 13%–37%, P < 0.001), a 70% reduction in time to wean, (95% CI 27%–88%, P = 0.009), and a decrease in ICU LOS by 11% (95% CI 3%–19%, P = 0.01). Weaning protocols are also an important risk factor for UE [5]. Findings from a prospective cohort study specifically identify the presence of weaning protocols as an important factor for reducing UE; patients who had weaning protocols ordered and followed were least likely to experience UE (P = 0.02) [5]. A separate quality improvement initiative demonstrated an overall decrease in the number of UEs (from 5.2% to 0.9%) after implementing weaning protocols as standard of care [39]. Considering many UEs occur during weaning [10], integration of weaning protocols aids in expediting the process and ensuring timely extubation.
Increased Surveillance
Increasing surveillance and monitoring of ventilated patients is a recommendation based on risk factors presented at the time of UE. Specifically, staffing levels and shifts and the use of physical restraints are variables associated with UE that are amendable to changes in unit processes based on increased surveillance. It is reported that 40% to 76% of UEs occurred during the night shift [14,17,24,40]; many more occur during change of shift or when there is not a nurse present at the bedside [3,17]. Recent trends towards mandatory bedside reporting is a specific intervention that may positively impact UE among patients in the ICU [41]. Meta-analyses of observational studies investigating the effect of nurse staffing on hospital outcomes indicate that increasing the number of RNs is associated with decreased risk of adverse patient outcomes, including UE [42,43]. The addition of 1 additional nurse per patient day can result in a 51% decrease in UE, while a decrease in nursing workload could result in a 45% decrease in UE [42]. Data from a national prevalence study reports ICUs with fewer available resources, including staff, experienced a higher number of UEs [4].
Increasing surveillance by nursing and health care staff may also impact prevalence of physical restraint use. A significant number of patients who experience UE are physically restrained at the time of the incident, ranging from 40% to 90% of intubated patients [5–7,14,17,40]. It is well documented that UE continue to occur despite the use of restraints [5,7,28,29,44] Patients who are physically restrained often experience higher rates of unplanned extubation (42.9% vs. 16.5% , P < 0.001 in Chang et al’s study [7]), and longer ICU LOS (20.3 days vs. 15.8 days, P = 0.009) [7]. Soft wrist restraints are commonly used to prevent pulling of the endotracheal tube; however, research evidence on UE demonstrates this is not always an effective intervention. Increasing surveillance of ventilated patients, treating their agitation and screening for underlying delirium, and integration of weaning protocols are all interventions that may decrease UE and the need for routine use of physical restraints.
Ongoing Education for Patients and Health Care Staff
Initial and ongoing education about UE, risk factors, and effective interventions is beneficial for patients and health care staff. Although there are no trials investigating effects of educational interventions for patients on UE outcomes, pre-education of surgical patients regarding what to expect while intubated may aid in decreasing delirium risk, agitation, physical restraint use, and possibly UE. Verbal and written educational information during pre-admission testing is a feasible method easily integrated into pre-operative programs.
Because UEs often occur more frequently among less experienced staff, initial education about risk factors for UE is crucial to include in ICU staff orientation programs [3,7]. Educational initiatives should incorporate training on routine delirium screening and avoidance of agitation, use of protocols, and increased surveillance of patients receiving mechanical ventilation [5,15,17,39,45]. Ongoing education of staff regarding ventilatory equipment and risk factors for UE can be particularly effective in decreasing UE [46]. Initial educational efforts should be followed by routine updates for all members of the healthcare team about ongoing quality improvement efforts to monitor UE. Associated factors for UE that may be unit- or process-specific, including methods for endotracheal tube securement and intra-hospital transport, should be communicated with all individuals involved in patient care. Integration of continuous quality improvement programs can decrease UE rates by 22% to 53% [16]. Quality efforts typically focus on standardization of reporting and tracking tools, protocol implementations, and ongoing monitoring, auditing, and recording of UE.
Current Trends and Future Directions
Recent trends in critical care recommendations may mitigate potential risk factors identified in UE research. Integration of lightened sedation and daily wake up periods for intubated patients may decrease prevalence of risk factors for UE, specifically agitation, physical restraint use, and altered level of consciousness [30], while routine weaning protocols may improve ventilatory outcomes, including UE [5,38,40]. Nursing bedside report and purposeful hourly rounding are quickly emerging as mainstays of professional nursing care [41]. Inherent in these 2 initiatives are increased surveillance and vigilance by health care staff, which can result in timely extubation of those who indicate readiness, as well as decreased incidence of adverse events. Delirium remains a key factor that may be a likely cause for UE; recent trends towards early detection and proper management of delirium among ICU staff may result in improved ventilatory outcomes, including weaning, planned extubation, and the prevalence of UE.
Another important trend in critical care is the emergence of a neurocritical care specialty and routine admission of neurocritically ill patients to neuroscience ICUs [47,48]. However, there are no studies investigating prevalence of UE among these patients, who often have higher rates of agitation or restlessness due to cognitive impairment. Among general ICUs, patients with a primary respiratory diagnosis accounted for 23% of all UE in one study, while those with a neurological diagnosis accounted for the second highest percentage (12%) among the study population [15]. A separate study concluded that presence of neurological injury with a concomitant nosocomial infection increased risk of UE among patients in a mixed ICU [7]. A recent systematic review of weaning protocols highlights positive effects on ventilatory outcomes but cites lack of evidence for effectiveness of protocols among those with neurological injury [38]. Areas for future UE research should include factors specific to this patient population, as they may be at higher risk for adverse ventilatory outcomes due to the nature of the neurological injury.
Conclusion
Prevention of UE remains an elusive target, evidenced by little change in reported rates over 2 decades. Research provides data on risk factors that may be patient, unit, or process related. Structuring prevention efforts around modifiable risk factors for UE is a feasible approach amenable to ongoing monitoring for effectiveness. Integration of current trends in health care safety and quality may produce an added benefit of reducing the occurrence of UE in critical care units. Future research evaluating these trends and the prevalence of UE in subspecialty populations is warranted.
Corresponding author: Molly McNett, PhD, RN, CNRN, Attn: NBO, MetroHealth Medical Center, 2500 MetroHealth Drive; Cleveland, OH 44109, mmcnett@metrohealth.org.
Financial disclosures: None.
From the MetroHealth System, Cleveland, OH.
Abstract
- Objective: To describe risk factors for unplanned extubation (UE) among critically ill adults requiring mechanical ventilation and to identify strategies to reduce the occurrence of this adverse event.
- Methods: Review of the literature.
- Results: Inadvertent removal of an endotracheal tube, or a UE, occurs in 7% to 22.5% of mechanically ventilated adult patients and is often due to deliberate patient removal. Despite the multitude of research examining risk factors and predictors of UE, rates have remained unchanged for the past 2 decades. Risk factors can be classified by intensive care unit (ICU) type, including medical ICUs, surgical ICUs, and mixed medical-surgical ICUs. The majority of risk factors for UEs across ICUs may be amenable to changes in unit processes, such as programs for agitation management, use of weaning protocols, increased surveillance of patients, and ongoing education for patients and health care staff.
- Conclusion: Prevention of UE remains an elusive target. Changes in unit processes that target identified risk factors may be an effective method to decrease prevalence of UE.
Unplanned extubation (UE) is the inadvertent removal of an endotracheal tube, either by a patient (deliberate self-extubation), or by a member of the health care team providing routine care such as repositioning, suctioning, or procedures (accidental extubation). Approximately 7% to 22.5% of mechanically ventilated patients in the intensive care unit (ICU) experience UE [1–7]. Estimates are likely higher, as current regulatory and accreditation standards do not include mandatory reporting of this event. Despite numerous studies investigating risk factors associated with UE, it remains a prevalent problem with adverse outcomes for patients and hospitals. The purpose of this review is to provide a summary of the literature on risk factors for UE, review effects on patient and organizational outcomes, and identify evidence-based strategies for reducing occurrence of UE among mechanically ventilated patients.
Prevalence of Unplanned Exubation
There is substantial heterogeneity in how UE is calculated and reported in the research literature. UE is calculated as the number of UE events per 100 or 1000 patient days, or the number of UE per total ventilator days. Rates of UE are also reported as the proportion of patients who experience UE out of all intubated patients over a set time period [8]. Despite efforts aimed at mitigating risk factors for UE, rates have remained static over the past 2 decades. Reported UE rates from 1994–2002 were 2.6% to 14% [3,6,9–11], while rates from 2004–2014 ranged from 1% to 22% [3–5,8,12–15]. Interventions utilizing a multidisciplinary approach have been implemented with the aim of decreasing UE, yet few have proven successful on improving rates nationally.
Unplanned self-extubation by the patient (deliberate self-extubation) is the most common type of UE [3,10,12,16–18]. A multicenter trial of 426 patients from 11 medical centers indicates that 46 patients experienced UE, with 36 of these (78.2%) caused by patient self-extubation [6]. Prospective single-site studies report similar or higher estimates of patient self-extubation, ranging from 75.8% to 91.7% [3,5], while a multisite study of 10,112 patients revealed 32 of 35 UE (91.4%) were due to patient self-extubation [12]. Similarly, a 4-year analysis of 85 UEs reported 82 incidences (96.5%) were a result of deliberate patient removal [13]. Patients either physically pull out the endotracheal tube or use their tongue or coughing/gagging maneuvers to displace or intentionally remove the endotracheal tube [5]. Only 3% to 8% of UEs are caused by inadvertent removal by health care staff [3,5,12,13].
Effects on Patient and Organizational Outcomes
Regardless of the cause of the UE, there are adverse consequences for both patients and hospitals. Some patients who experience UE have higher rates of in-hospital mortality; however, this is often due to contributing factors associated with severity of injury, the need for reintubation, and underlying chronic diseases [13]. Patients who experience accidental UE have higher incidence of nosocomial pneumonia (27.6% vs. 138%, P = 0.002) [11], longer duration of mechanical ventilation, and increased length of stay (LOS) [7,13]. While some studies report UE can result in serious consequences such as respiratory distress, hypoxia [13], and even death [6,12], others report lower mortality and length of stay when UE occurs, likely due to the fact that many patients are ready for liberation from mechanical ventilation at the time of UE [5,15].
Despite the emergent nature of UE, not all patients experience immediate reintubation. Many instances of UE occur during patient weaning trials or in preparation for planned extubations [5,11], which explains why only 10% to 60% of patients require reintubation [3,5,10,11,15,19,20]. When reintubation is necessary, it results in increased number of ventilator days [10,11], and increased ICU and hospital LOS [1,11]. There is little evidence directly linking reintubation with in-hospital mortality; however, it can cause serious complications such as hypotension, hypertension, arrhythmias, and airway trauma [21]. For hospitals and health care organizations, the need for reintubation results in increased hospital costs, estimated to be $1000 per reintubation event [17,22]. This estimate does not take into account additional costs incurred with increased ICU care, longer periods of mechanical ventilation, and increased LOS. Estimates of these additional costs in pediatric patients are approximately $36,000 [23]. Costs are likely higher in adult patients, due to multiple comorbidities that often accompany the need for mechanical ventilation, as well as increased pharmacy, lab, and diagnostic charges [1].
Risk Factors for Unplanned Extubation
Medical ICU Risk Factors
MICUs traditionally have the highest rates of UE [4,8]. Data from a national prevalence study indicated that there were 23.4 episodes of UE in MICUs per 1000 ventilator days [4]. Approximately 9.5% to 15% of all ventilated patients in the MICU experience UE [4,5,8]. Patients in the MICU who require mechanical ventilation often have complex chronic illness with underlying respiratory disease, which can result in prolonged periods of ventilation and increased risk of UE. Specific risk factors investigated in UE research include patient specific factors (age, gender, diagnosis, comorbidities, agitation, level of consciousness, laboratory values), ventilatory factors (ventilator type and setting, type of tracheal tube, method of tube fixation), as well as type of sedation and use of protocols [5,6,24]. Surprisingly, few variables emerge as significant risk factors for UE among MICU patients. Risk factors associated with UE have included male gender [24], presence of chronic obstructive pulmonary disease (COPD) [24], increased level of consciousness [25], and use of weaning protocols [5]. While gender, COPD, and level of consciousness increase risk of UE, the presence of weaning protocols is shown to decrease risk of UE [5]. Although UE are reported most often in MICUs, few risk factors consistently emerge for this specific cohort, making definitive recommendations for prevention of UE difficult.
Surgical ICU Risk Factors
The prevalence of UE for mechanically ventilated patients in the SICU tend to be lower than those for MICU cohorts. Prevalence of UE in the SICU is reported at 1.41 episodes per 100 ventilator days [13], or 6.8 episodes per 1000 ventilator days [4]. Percentages of UE in the SICU range from 2% to 6% [4,8,19]. Similar to MICU patients, critically ill patients in the SICU often have specific risk factors placing them at risk for UE. Causative factors examined in research studies with this population include gender, age, sedation scale scores, need for reintubation, time from intubation to extubation, use of sedatives/analgesics, restraints, ICU nurse experience, location of staff at time of UE, and criteria for extubation [17,19]. Similar to MICU cohorts, few variables are identified as predictors of UE. Significant predictors include use of restraints, decreased sedation [17], and meeting criteria for extubation [19]. Among patients who experienced an UE, 87% were restrained at the time of the UE [17], and most had low levels of sedation (mean Ramsay sedation scale score = 2.42 in the hour preceding the UE). Approximately 64% of patients who experienced UE met criteria for planned extubation and did not require re-intubation [19], suggesting many patients were essentially ready for planned extubation.
Mixed ICU Risk Factors
The majority of research investigating risk factors for UE is conducted within medical-surgical or mixed/general ICUs. The prevalence of UE within this type of unit is reported at 1.59 episodes per 100 patient days [6], or approximately 2% to 10% [4,6,7]. Among this population, potential risk factors are similar to those included in solely MICU or SICU studies. Because of the high number of studies investigating UE in a mixed ICU setting, there are significantly more variables included in as potential risk factors. Variables include patient age, gender, admission diagnosis, injury severity using Acute Physiological and Chronic Health Evaluation (APACHE II), ICU and hospital LOS, patient level of consciousness, agitation, days of mechanical ventilation, ventilator settings, nosocomial infection, sedation, physical restraints, vital signs [7,14,26], laboratory values, medication types, and body mass index [15,26]. One study also included time of UE and ICU nurse level of experience [3]. Among all factors, several were significant predictors of UE: male gender [15], decreased sedation and increased level of consciousness [8], agitation [3,19,26], use of restraints [3,7], sedation practices (particularly use of benzodiazapines) [3,7,15,26,27], lack of strong tube fixation, absence of IV sedation, and orotracheal intubation [6]. UE were more likely to occur on the night shift and among staff that included nurses with fewer years of experience [3]. Many episodes of UE occurred during weaning [10] or among patients who could communicate and were alert [3]. One study reports 57% of patients who intentionally self-extubated explained they simply removed the tube because it was uncomfortable [3].
Strategies for Reducing Adverse Events
Agitation Management
The majority of studies cited agitation, altered level of consciousness, or inadequate sedation as risk factors for UE [3,6–8,15,17,18,25,26,28,29]. These factors directly impact restraint use, another common risk factor for UE [3,7,17]. A key recommendation for agitation management is to identify the source of agitation, which is often caused by delirium onset in the ICU [30–32]. Prevalence of delirium in the ICU ranges from 20% to 80% [33–35]. ICU patients are at high risk for delirium due to sleep deprivation, older age, restraints, abnormal lab values, medications, infection, and respiratory complications [31]. Treatment for delirium centers on prevention, early recognition, interdisciplinary and pharmacologic protocols, increased nursing presence, and use of short-acting sedation when necessary [30–32,36]. While there is no research specifically linking delirium to UE, a quality analysis of risk factors present at the time of UE using bow-tie analysis methods identified delirium as a key factor present in the majority of UE cases [36]. It is possible that agitation reported in other studies investigating risk factors for UE may actually be reflective of underlying delirium. Routine screening using validated tools, such as the Confusion Assessment Method-ICU (CAM-ICU) [37] would aid in early detection and management of delirium, and would provide a standardized method for exploring the relationship of delirium and UE in future trials.
Integration of Weaning Protocols
Protocol-directed weaning is beneficial for decreasing ventilator days, time to wean from mechanical ventilation, and ICU LOS [38]. A systematic review including 7 trials (2434 patients) comparing protocol/non-protocol for weaning from mechanical ventilation reported a 26% decrease in the mean duration of mechanical ventilation for the protocol groups (95% CI 13%–37%, P < 0.001), a 70% reduction in time to wean, (95% CI 27%–88%, P = 0.009), and a decrease in ICU LOS by 11% (95% CI 3%–19%, P = 0.01). Weaning protocols are also an important risk factor for UE [5]. Findings from a prospective cohort study specifically identify the presence of weaning protocols as an important factor for reducing UE; patients who had weaning protocols ordered and followed were least likely to experience UE (P = 0.02) [5]. A separate quality improvement initiative demonstrated an overall decrease in the number of UEs (from 5.2% to 0.9%) after implementing weaning protocols as standard of care [39]. Considering many UEs occur during weaning [10], integration of weaning protocols aids in expediting the process and ensuring timely extubation.
Increased Surveillance
Increasing surveillance and monitoring of ventilated patients is a recommendation based on risk factors presented at the time of UE. Specifically, staffing levels and shifts and the use of physical restraints are variables associated with UE that are amendable to changes in unit processes based on increased surveillance. It is reported that 40% to 76% of UEs occurred during the night shift [14,17,24,40]; many more occur during change of shift or when there is not a nurse present at the bedside [3,17]. Recent trends towards mandatory bedside reporting is a specific intervention that may positively impact UE among patients in the ICU [41]. Meta-analyses of observational studies investigating the effect of nurse staffing on hospital outcomes indicate that increasing the number of RNs is associated with decreased risk of adverse patient outcomes, including UE [42,43]. The addition of 1 additional nurse per patient day can result in a 51% decrease in UE, while a decrease in nursing workload could result in a 45% decrease in UE [42]. Data from a national prevalence study reports ICUs with fewer available resources, including staff, experienced a higher number of UEs [4].
Increasing surveillance by nursing and health care staff may also impact prevalence of physical restraint use. A significant number of patients who experience UE are physically restrained at the time of the incident, ranging from 40% to 90% of intubated patients [5–7,14,17,40]. It is well documented that UE continue to occur despite the use of restraints [5,7,28,29,44] Patients who are physically restrained often experience higher rates of unplanned extubation (42.9% vs. 16.5% , P < 0.001 in Chang et al’s study [7]), and longer ICU LOS (20.3 days vs. 15.8 days, P = 0.009) [7]. Soft wrist restraints are commonly used to prevent pulling of the endotracheal tube; however, research evidence on UE demonstrates this is not always an effective intervention. Increasing surveillance of ventilated patients, treating their agitation and screening for underlying delirium, and integration of weaning protocols are all interventions that may decrease UE and the need for routine use of physical restraints.
Ongoing Education for Patients and Health Care Staff
Initial and ongoing education about UE, risk factors, and effective interventions is beneficial for patients and health care staff. Although there are no trials investigating effects of educational interventions for patients on UE outcomes, pre-education of surgical patients regarding what to expect while intubated may aid in decreasing delirium risk, agitation, physical restraint use, and possibly UE. Verbal and written educational information during pre-admission testing is a feasible method easily integrated into pre-operative programs.
Because UEs often occur more frequently among less experienced staff, initial education about risk factors for UE is crucial to include in ICU staff orientation programs [3,7]. Educational initiatives should incorporate training on routine delirium screening and avoidance of agitation, use of protocols, and increased surveillance of patients receiving mechanical ventilation [5,15,17,39,45]. Ongoing education of staff regarding ventilatory equipment and risk factors for UE can be particularly effective in decreasing UE [46]. Initial educational efforts should be followed by routine updates for all members of the healthcare team about ongoing quality improvement efforts to monitor UE. Associated factors for UE that may be unit- or process-specific, including methods for endotracheal tube securement and intra-hospital transport, should be communicated with all individuals involved in patient care. Integration of continuous quality improvement programs can decrease UE rates by 22% to 53% [16]. Quality efforts typically focus on standardization of reporting and tracking tools, protocol implementations, and ongoing monitoring, auditing, and recording of UE.
Current Trends and Future Directions
Recent trends in critical care recommendations may mitigate potential risk factors identified in UE research. Integration of lightened sedation and daily wake up periods for intubated patients may decrease prevalence of risk factors for UE, specifically agitation, physical restraint use, and altered level of consciousness [30], while routine weaning protocols may improve ventilatory outcomes, including UE [5,38,40]. Nursing bedside report and purposeful hourly rounding are quickly emerging as mainstays of professional nursing care [41]. Inherent in these 2 initiatives are increased surveillance and vigilance by health care staff, which can result in timely extubation of those who indicate readiness, as well as decreased incidence of adverse events. Delirium remains a key factor that may be a likely cause for UE; recent trends towards early detection and proper management of delirium among ICU staff may result in improved ventilatory outcomes, including weaning, planned extubation, and the prevalence of UE.
Another important trend in critical care is the emergence of a neurocritical care specialty and routine admission of neurocritically ill patients to neuroscience ICUs [47,48]. However, there are no studies investigating prevalence of UE among these patients, who often have higher rates of agitation or restlessness due to cognitive impairment. Among general ICUs, patients with a primary respiratory diagnosis accounted for 23% of all UE in one study, while those with a neurological diagnosis accounted for the second highest percentage (12%) among the study population [15]. A separate study concluded that presence of neurological injury with a concomitant nosocomial infection increased risk of UE among patients in a mixed ICU [7]. A recent systematic review of weaning protocols highlights positive effects on ventilatory outcomes but cites lack of evidence for effectiveness of protocols among those with neurological injury [38]. Areas for future UE research should include factors specific to this patient population, as they may be at higher risk for adverse ventilatory outcomes due to the nature of the neurological injury.
Conclusion
Prevention of UE remains an elusive target, evidenced by little change in reported rates over 2 decades. Research provides data on risk factors that may be patient, unit, or process related. Structuring prevention efforts around modifiable risk factors for UE is a feasible approach amenable to ongoing monitoring for effectiveness. Integration of current trends in health care safety and quality may produce an added benefit of reducing the occurrence of UE in critical care units. Future research evaluating these trends and the prevalence of UE in subspecialty populations is warranted.
Corresponding author: Molly McNett, PhD, RN, CNRN, Attn: NBO, MetroHealth Medical Center, 2500 MetroHealth Drive; Cleveland, OH 44109, mmcnett@metrohealth.org.
Financial disclosures: None.
1. Krinsley JS, Barone JE. The drive to survive: unplanned extubation in the ICU. Chest 2005;128:560–6.
2. Coppolo DP, May JJ. Self-extubations. A 12-month experience. Chest 1990;98:165–9.
3. Yeh SH, Lee LN, Ho TH, et al. Implications of nursing care in the occurrence and consequences of unplanned extubation in adult intensive care units. Int J Nurs Stud 2004;41:255–62.
4. Mion LC, Minnick AF, Leipzig R, et al. Patient-initiated device removal in intensive care units: a national prevalence study. Crit Care Med 2007;35:2714–20.
5. Jarachovic M, Mason M, Kerber K. The role of standardized protocols in unplanned extubations in a medical intensive care unit. Am J Crit Care 2011;20:304–11.
6. Boulain T. Unplanned extubations in the adult intensive care unit: a prospective multicenter study. Association des Reanimateurs du Centre-Ouest. Am J Resp Crit Care Med 1998;157(4 Pt 1):1131–7.
7. Chang LY, Wang KW, Chao YF. Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study. Am J Crit Care 2008;17:408–15.
8. Moons P, Sels K, De Becker W, et al. Development of a risk assessment tool for deliberate self-extubation in intensive care patients. Intensive Care Med 2004;30:1348–55.
9. Chiang AA, Lee KC, Lee JC, Wei CH. Effectiveness of a continuous quality improvement program aiming to reduce unplanned extubation: a prospective study. Intensive Care Med 1996;22:1269–71.
10. Betbese AJ, Perez M, Bak E, et al. A prospective study of unplanned endotracheal extubation in intensive care unit patients. Crit Care Med 1998;26:1180–6.
11. de Lassence A, Alberti C, Azoulay E, et al. Impact of unplanned extubation and reintubation after weaning on nosocomial pneumonia risk in the intensive care unit: a prospective multicenter study. Anesthesiology 2002;97:148–56.
12. Kapadia FN, Tekawade PC, Nath SS, et al. A prolonged observational study of tracheal tube displacements: Benchmarking an incidence <0.5-1% in a medical-surgical adult intensive care unit. Ind J Crit Care Med 2014;18:273–7.
13. Lee JH, Lee HC, Jeon YT, et al. Clinical outcomes after unplanned extubation in a surgical intensive care population. World J Surg 2014;38:203–10.
14. Chang LC, Liu PF, Huang YL, et al. Risk factors associated with unplanned endotracheal self-extubation of hospitalized intubated patients: a 3-year retrospective case-control study. Appl Nurs Res 2011;24:188–92.
15. de Groot RI, Dekkers OM, Herold IH, et al. Risk factors and outcomes after unplanned extubations on the ICU: a case-control study. Crit Care 2011;15:R19.
16. da Silva PS, Fonseca MC. Unplanned endotracheal extubations in the intensive care unit: systematic review, critical appraisal, and evidence-based recommendations. Anesth Analg 2012;114:1003–14.
17. Curry K, Cobb S, Kutash M, Diggs C. Characteristics associated with unplanned extubations in a surgical intensive care unit. Am J Crit Care 2008;17:45–51.
18. Christie JM, Dethlefsen M, Cane RD. Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth 1996;8:289–93.
19. Huang YT. Factors leading to self-extubation of endotracheal tubes in the intensive care unit. Nurs Crit Care 2009;14:68–74.
20. Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet 2008;371:126–34.
21. Mort TC. Unplanned tracheal extubation outside the operating room: a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg 1998;86:1171–6.
22. Jaber S, Chanques G, Altairac C, et al. A prospective study of agitation in a medical-surgical ICU: incidence, risk factors, and outcomes. Chest 2005;128:2749–57.
23. Roddy DJ, Spaeder MC, Pastor W, Stockwell DC, Klugman D. Unplanned extubations in children: impact on hospital cost and length of stay. Ped Crit Care Med 2015.
24. Bouza C, Garcia E, Diaz M, et al. Unplanned extubation in orally intubated medical patients in the intensive care unit: a prospective cohort study. Heart Lung 2007;36:270–6.
25. Vassal T, Anh NG, Gabillet JM, et al. Prospective evaluation of self-extubations in a medical intensive care unit. Intensive Care Med 1993;19:340-342.
26. Tung A, Tadimeti L, Caruana-Montaldo B, et al. The relationship of sedation to deliberate self-extubation. J Clin Anesth 2001;13:24–9.
27. Tanios M, Epstein S, Grzeskowiak M, et al. Influence of sedation strategies on unplanned extubation in a mixed intensive care unit. Am J Crit Care 2014;23:306–14.
28. Atkins PM, Mion LC, Mendelson W, et al. Characteristics and outcomes of patients who self-extubate from ventilatory support: a case-control study. Chest 1997;112:1317–23.
29. Chevron V, Menard JF, Richard JC, et al. Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med 1998;26:1049–53.
30. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
31. Morandi A, Jackson JC. Delirium in the intensive care unit: a review. Neurol Clin 2011;29:749–63.
32. Banerjee A, Vasilevskis, EE, Pandharipande, P. Strategies to improve delirium assessment practices in the intensive care unit. J Clin Outcomes Manag 2010;17:459–68.
33. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001;286:2703–10.
34. Ely EW, Stephens RK, Jackson JC, et al. Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: a survey of 912 healthcare professionals. Crit Care Med 2004;32:106–12.
35. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 2003;51:591–8.
36. Kerckhoffs MC, van der Sluijs AF, Binnekade JM, Dongelmans DA. Improving patient safety in the ICU by prospective identification of missing safety barriers using the bow-tie prospective risk analysis model. J Patient Safe 2013;9:154–9.
37. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941–8.
38. Blackwood B, Burns KE, Cardwell CR, O’Halloran P. Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients. Cochrane Database Syst Rev 2014;11:CD006904.
39. Chia PL, Santos DR, Tan TC, et al. Clinical quality improvement: eliminating unplanned extubation in the CCU. Int J Health Care Qual Ass 2013;26:642–52.
40. Balon JA. Common factors of spontaneous self-extubation in a critical care setting. Int J Trauma Nurs 2001;7:93–9.
41. Gregory S, Tan D, Tilrico M, et al. Bedside shift reports: what does the evidence say? J Nurs Admin 2014;44:541–5.
42. Kane RL, Shamliyan TA, Mueller C, et al. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care 2007;45:1195–204.
43. Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Crit Care Med 2010;38:1521–8; quiz 1529.
44. Tindol GA, Jr., DiBenedetto RJ, Kosciuk L. Unplanned extubations. Chest 1994;105:1804–7.
45. Chen CM CK, Fong Y, Hsing SC, et al. Age is an important predictor of failed unplanned extubation. Int J Gerontol 2010;4:120–9.
46. Richmond AL, Jarog DL, Hanson VM. Unplanned extubation in adult critical care. Quality improvement and education payoff. Crit Care Nurs 2004;24:32–7.
47. Kurtz P, Fitts V, Sumer Z, et al. How does care differ for neurological patients admitted to a neurocritical care unit versus a general ICU? Neurocrit Care 2011;15:477–80.
48. McNett MM, Horowitz DA. International multidisciplinary consensus conference on multimodality monitoring: ICU processes of care. Neurocrit Care 2014;21 Suppl 2:S215–28.
49. Gardner A, Hughes, D, Cook R, et al. Best practice in stabilisation of oral endotracheal tubes: a systematic review. Database of abstracts of reivews of effects (DARE): Quality-assessed reviews. 2005. York: Center for Reviews and Dissemination.
50. Hofso K, Coyer FM. Part 1: Chemical and physical restraints in the management of mechanically ventliated patients in the ICU: Contributing factors. Intensive Crit Care Nurs 2007; 23:249–55.
51. Kiekkas P, Diamanto A, Panteli E, et al. Unplanned extubation in critially ill adults: Clinical reviews. Nurs Crit Care 2012;18:123–34.
52. King JN, Elliiot VA. Self/unplanned extubation: Safety, surveillance, and monitoring of the mechanically ventilated patient. Crit Care Nurs Clin North Am 2012;24:469–79.
1. Krinsley JS, Barone JE. The drive to survive: unplanned extubation in the ICU. Chest 2005;128:560–6.
2. Coppolo DP, May JJ. Self-extubations. A 12-month experience. Chest 1990;98:165–9.
3. Yeh SH, Lee LN, Ho TH, et al. Implications of nursing care in the occurrence and consequences of unplanned extubation in adult intensive care units. Int J Nurs Stud 2004;41:255–62.
4. Mion LC, Minnick AF, Leipzig R, et al. Patient-initiated device removal in intensive care units: a national prevalence study. Crit Care Med 2007;35:2714–20.
5. Jarachovic M, Mason M, Kerber K. The role of standardized protocols in unplanned extubations in a medical intensive care unit. Am J Crit Care 2011;20:304–11.
6. Boulain T. Unplanned extubations in the adult intensive care unit: a prospective multicenter study. Association des Reanimateurs du Centre-Ouest. Am J Resp Crit Care Med 1998;157(4 Pt 1):1131–7.
7. Chang LY, Wang KW, Chao YF. Influence of physical restraint on unplanned extubation of adult intensive care patients: a case-control study. Am J Crit Care 2008;17:408–15.
8. Moons P, Sels K, De Becker W, et al. Development of a risk assessment tool for deliberate self-extubation in intensive care patients. Intensive Care Med 2004;30:1348–55.
9. Chiang AA, Lee KC, Lee JC, Wei CH. Effectiveness of a continuous quality improvement program aiming to reduce unplanned extubation: a prospective study. Intensive Care Med 1996;22:1269–71.
10. Betbese AJ, Perez M, Bak E, et al. A prospective study of unplanned endotracheal extubation in intensive care unit patients. Crit Care Med 1998;26:1180–6.
11. de Lassence A, Alberti C, Azoulay E, et al. Impact of unplanned extubation and reintubation after weaning on nosocomial pneumonia risk in the intensive care unit: a prospective multicenter study. Anesthesiology 2002;97:148–56.
12. Kapadia FN, Tekawade PC, Nath SS, et al. A prolonged observational study of tracheal tube displacements: Benchmarking an incidence <0.5-1% in a medical-surgical adult intensive care unit. Ind J Crit Care Med 2014;18:273–7.
13. Lee JH, Lee HC, Jeon YT, et al. Clinical outcomes after unplanned extubation in a surgical intensive care population. World J Surg 2014;38:203–10.
14. Chang LC, Liu PF, Huang YL, et al. Risk factors associated with unplanned endotracheal self-extubation of hospitalized intubated patients: a 3-year retrospective case-control study. Appl Nurs Res 2011;24:188–92.
15. de Groot RI, Dekkers OM, Herold IH, et al. Risk factors and outcomes after unplanned extubations on the ICU: a case-control study. Crit Care 2011;15:R19.
16. da Silva PS, Fonseca MC. Unplanned endotracheal extubations in the intensive care unit: systematic review, critical appraisal, and evidence-based recommendations. Anesth Analg 2012;114:1003–14.
17. Curry K, Cobb S, Kutash M, Diggs C. Characteristics associated with unplanned extubations in a surgical intensive care unit. Am J Crit Care 2008;17:45–51.
18. Christie JM, Dethlefsen M, Cane RD. Unplanned endotracheal extubation in the intensive care unit. J Clin Anesth 1996;8:289–93.
19. Huang YT. Factors leading to self-extubation of endotracheal tubes in the intensive care unit. Nurs Crit Care 2009;14:68–74.
20. Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet 2008;371:126–34.
21. Mort TC. Unplanned tracheal extubation outside the operating room: a quality improvement audit of hemodynamic and tracheal airway complications associated with emergency tracheal reintubation. Anesth Analg 1998;86:1171–6.
22. Jaber S, Chanques G, Altairac C, et al. A prospective study of agitation in a medical-surgical ICU: incidence, risk factors, and outcomes. Chest 2005;128:2749–57.
23. Roddy DJ, Spaeder MC, Pastor W, Stockwell DC, Klugman D. Unplanned extubations in children: impact on hospital cost and length of stay. Ped Crit Care Med 2015.
24. Bouza C, Garcia E, Diaz M, et al. Unplanned extubation in orally intubated medical patients in the intensive care unit: a prospective cohort study. Heart Lung 2007;36:270–6.
25. Vassal T, Anh NG, Gabillet JM, et al. Prospective evaluation of self-extubations in a medical intensive care unit. Intensive Care Med 1993;19:340-342.
26. Tung A, Tadimeti L, Caruana-Montaldo B, et al. The relationship of sedation to deliberate self-extubation. J Clin Anesth 2001;13:24–9.
27. Tanios M, Epstein S, Grzeskowiak M, et al. Influence of sedation strategies on unplanned extubation in a mixed intensive care unit. Am J Crit Care 2014;23:306–14.
28. Atkins PM, Mion LC, Mendelson W, et al. Characteristics and outcomes of patients who self-extubate from ventilatory support: a case-control study. Chest 1997;112:1317–23.
29. Chevron V, Menard JF, Richard JC, et al. Unplanned extubation: risk factors of development and predictive criteria for reintubation. Crit Care Med 1998;26:1049–53.
30. Barr J, Fraser GL, Puntillo K, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
31. Morandi A, Jackson JC. Delirium in the intensive care unit: a review. Neurol Clin 2011;29:749–63.
32. Banerjee A, Vasilevskis, EE, Pandharipande, P. Strategies to improve delirium assessment practices in the intensive care unit. J Clin Outcomes Manag 2010;17:459–68.
33. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001;286:2703–10.
34. Ely EW, Stephens RK, Jackson JC, et al. Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: a survey of 912 healthcare professionals. Crit Care Med 2004;32:106–12.
35. McNicoll L, Pisani MA, Zhang Y, et al. Delirium in the intensive care unit: occurrence and clinical course in older patients. J Am Geriatr Soc 2003;51:591–8.
36. Kerckhoffs MC, van der Sluijs AF, Binnekade JM, Dongelmans DA. Improving patient safety in the ICU by prospective identification of missing safety barriers using the bow-tie prospective risk analysis model. J Patient Safe 2013;9:154–9.
37. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941–8.
38. Blackwood B, Burns KE, Cardwell CR, O’Halloran P. Protocolized versus non-protocolized weaning for reducing the duration of mechanical ventilation in critically ill adult patients. Cochrane Database Syst Rev 2014;11:CD006904.
39. Chia PL, Santos DR, Tan TC, et al. Clinical quality improvement: eliminating unplanned extubation in the CCU. Int J Health Care Qual Ass 2013;26:642–52.
40. Balon JA. Common factors of spontaneous self-extubation in a critical care setting. Int J Trauma Nurs 2001;7:93–9.
41. Gregory S, Tan D, Tilrico M, et al. Bedside shift reports: what does the evidence say? J Nurs Admin 2014;44:541–5.
42. Kane RL, Shamliyan TA, Mueller C, et al. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care 2007;45:1195–204.
43. Penoyer DA. Nurse staffing and patient outcomes in critical care: a concise review. Crit Care Med 2010;38:1521–8; quiz 1529.
44. Tindol GA, Jr., DiBenedetto RJ, Kosciuk L. Unplanned extubations. Chest 1994;105:1804–7.
45. Chen CM CK, Fong Y, Hsing SC, et al. Age is an important predictor of failed unplanned extubation. Int J Gerontol 2010;4:120–9.
46. Richmond AL, Jarog DL, Hanson VM. Unplanned extubation in adult critical care. Quality improvement and education payoff. Crit Care Nurs 2004;24:32–7.
47. Kurtz P, Fitts V, Sumer Z, et al. How does care differ for neurological patients admitted to a neurocritical care unit versus a general ICU? Neurocrit Care 2011;15:477–80.
48. McNett MM, Horowitz DA. International multidisciplinary consensus conference on multimodality monitoring: ICU processes of care. Neurocrit Care 2014;21 Suppl 2:S215–28.
49. Gardner A, Hughes, D, Cook R, et al. Best practice in stabilisation of oral endotracheal tubes: a systematic review. Database of abstracts of reivews of effects (DARE): Quality-assessed reviews. 2005. York: Center for Reviews and Dissemination.
50. Hofso K, Coyer FM. Part 1: Chemical and physical restraints in the management of mechanically ventliated patients in the ICU: Contributing factors. Intensive Crit Care Nurs 2007; 23:249–55.
51. Kiekkas P, Diamanto A, Panteli E, et al. Unplanned extubation in critially ill adults: Clinical reviews. Nurs Crit Care 2012;18:123–34.
52. King JN, Elliiot VA. Self/unplanned extubation: Safety, surveillance, and monitoring of the mechanically ventilated patient. Crit Care Nurs Clin North Am 2012;24:469–79.