Article
Patient-centric pain management decision aid reduces opioid use posthysterectomy
- Author:
- Kathy Christie, Senior Editor
The average number of opioids prescribed at discharge dropped from 25 to 10, and hydrocodone went from being prescribed in 99...
News
Making a difference: ACOG’s guidance on low-dose aspirin for preventing superimposed preeclampsia
- Author:
- Kathy Christie, Senior Editor
Study results suggest that ACOG’s recommendations for preventing superimposed preeclampsia are having a significant positive impact on outcomes....
Video
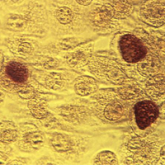
Chlamydia infection: Common, and consequential to women's health
- Author:
- Kathy Christie, Senior Editor
- Tyler Mundhenk, Web and Multimedia Editor
Article
Dispensing hormonal contraceptives in 1-year supplies saves state $43 million and avoids 15,000 unintended pregnancies
- Author:
- Kathy Christie, Senior Editor
News

Educate patients about dense breasts and cancer risk
- Author:
- Kathy Christie, Senior Editor
Approximately one-third of cancers in dense breasts have a delayed diagnosis on mammography, and 70% of cancers occur in dense breasts, emphasizes...
