User login
Hospitalist Service Change
A growing number of reports indicate that communication failures among physicians at transitions of care are critical to patient safety.16 The practice of physician handoffs at shift and service changes are variable, with no standardized protocol shown to be effective at ensuring complete transmission of information.7 In 2006, the Joint Commission set a National Patient Safety Goal to implement a standardized approach to hand off communications.8 Hospitalists stand to be impacted by this decision due to the frequency of care transitions that are inherent in hospital practice. The Society of Hospital Medicine (SHM) recognizes safe transitions of care as a core competency of hospitalists and is actively exploring standardization of the process.9 While recent attention has focused on improved communication during shift changes, little data exists to guide handoffs among hospitalists at service changes.
Good service change communication is an essential skill of hospital medicine because frequent service handoffs are often unavoidable in hospitalist practices that seek to balance the demand for around‐the‐clock coverage for inpatients and the need to create sustainable schedules to avoid physician burnout.10 But the tradeoff between fewer hours worked and discontinuity of care is well recognized.7 Increasingly fragmented care without corresponding improvements in handoff communication may exacerbate the problem. This study aims to characterize communication practices among hospitalists during service changes and to describe adverse and near miss events that may occur as a result of poor handoffs during these vulnerable care transitions.
Methods
Setting
This study was conducted with Institutional Review Board (IRB) exemption at a single, academic tertiary care institution. The Section of Hospital Medicine at the University of Chicago is comprised of 17 physicians and 5 mid‐level practitioners (Nurse Practitioner and Physician Assistant), and staffs a nonteaching multispecialty service of patients with solid‐organ transplants (excluding heart) or preexisting oncological diagnoses. While hospitalists are the attendings of record, the care of these complex patients often requires the input of subspecialty consultants.
The nonteaching hospitalist service consists of 2 teams, each staffed by 1 hospitalist, and 1 or 2 mid‐level practitioners supporting the hospitalist on weekdays. Hospitalists rotate on the service for 1 or 2 weeks at a time. Mid‐level practitioners work a nonuniform 3 to 4 days per week. The patient census ranges from 2 to 12 patients per team while 3 to 6 new admissions are received every other day. A dedicated nocturnist or moonlighter manages existing patients and new admissions overnight.
At the time of service change, either the incoming or the outgoing physician initiates the communication by pager, telephone, e‐mail, or by face‐to‐face solicitation. A computerized census form on a Microsoft Word template with each patient's identifying information and a summary of the hospital course is updated by the outgoing hospitalist and is accessible to the incoming hospitalist. Mid‐level practitioners, typically, do not participate in service change handoffs because they are not always on duty at the time of service change. Other than through the universal use of the computerized census form, there was no standardized protocol or education on how to perform service changes.
Data Collection
All 17 hospitalists rotating through the nonteaching inpatient service at the University of Chicago Medical Center (UCMC) were recruited to participate. Between May and December 2007, one of the investigators (K.H.) hand‐delivered surveys to the study subjects who usually completed the survey immediately. Those who could not complete the survey on the spot were approached by the investigator a second time a few hours later. The participants were hospitalists who started their duty on the nonteaching service 48 hours earlier. A total of 60 service changes during the study period were the units of analysis in this study.
Eighteen items of the anonymous, paper‐based, self‐administered survey (see Appendix 1) were created to evaluate the characteristics of service change communications found to be salient in previous studies.11, 12 Hospitalists were asked to estimate the time they spent on the handoff communication, and the time they spent dealing with issues that arose as a result of missing information. Responses included <5 minutes, 6‐15 minutes, 16‐30 minutes, 31‐60 minutes, and >60 minutes.
Completeness of the handoff communication and the respondents' certainty about the care‐plans for the patients on the first day of service were rated using 6‐point Likert‐type scales. For example, the possible responses to an item asking respondents to rate the completeness of information in the handoff communication were grossly incomplete, incomplete, somewhat incomplete, somewhat complete, complete, and excessively complete. Respondents were asked to recall how often they encountered consequences of incomplete handoffs such as instances, within the first 48 hours of service, when they required information that should have been discussed at handoff but was not. Another consequence of incomplete handoffs that the survey asked hospitalists to recall was the frequency of near‐miss and adverse events.
Narrative details about missing information from the service change and near misses and adverse events attributable to poor handoffs were solicited using the critical incident technique. This technique is used to elicit open‐ended constructed descriptions of infrequently occurring events through personal observations and experience.13 Respondents were also asked about the frequency and content of any discussions they had with the outgoing hospitalist after the original handoff communication. Finally, suggestions for improving service change handoffs were solicited from each respondent.
Data Analysis
The results of the Likert responses were dichotomized such that incomplete handoffs were defined as response of grossly incomplete, incomplete, or somewhat incomplete. Complete handoffs were defined as response of somewhat complete, complete, or excessively complete. Similarly, certainty about the plan for each patient on the first day of rotation was dichotomized with uncertain defined as response of uncertain, mostly uncertain, or somewhat uncertain, while certain was defined as a response of somewhat certain, mostly certain, or certain. Associations among service change characteristics were compared using chi‐square tests of the dichotomized Likert‐type data.
Narrative responses were analyzed by 3 of the authors (J.F., K.H., V.A.) using the constant comparative method.14 Major categories were created without a priori hypotheses. These categories were compared across surveys to yield integration or refinement into further subcategories. Disagreements were resolved by discussion until 100% agreement was reached.
Results
Service Change Communication
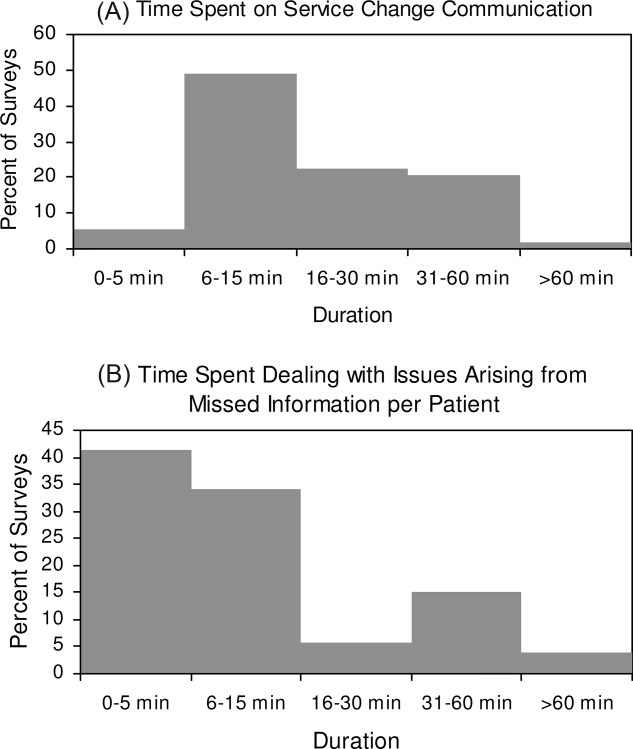
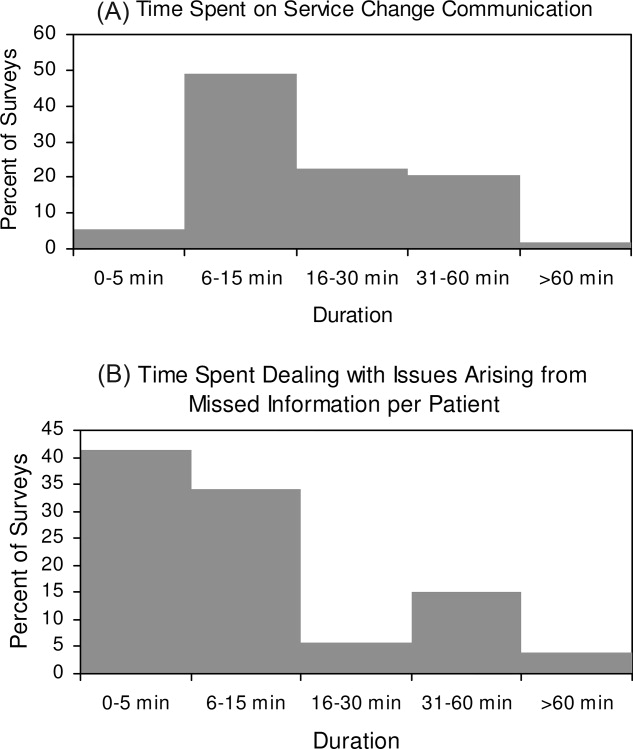
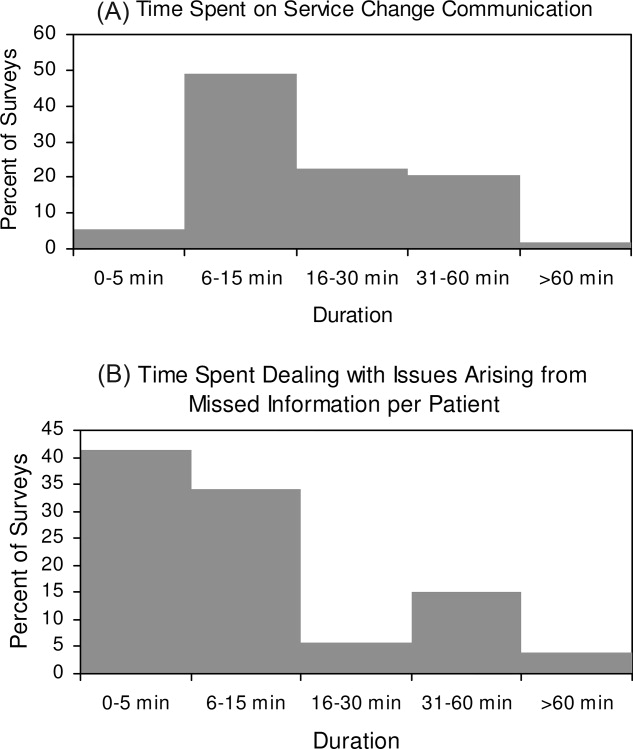
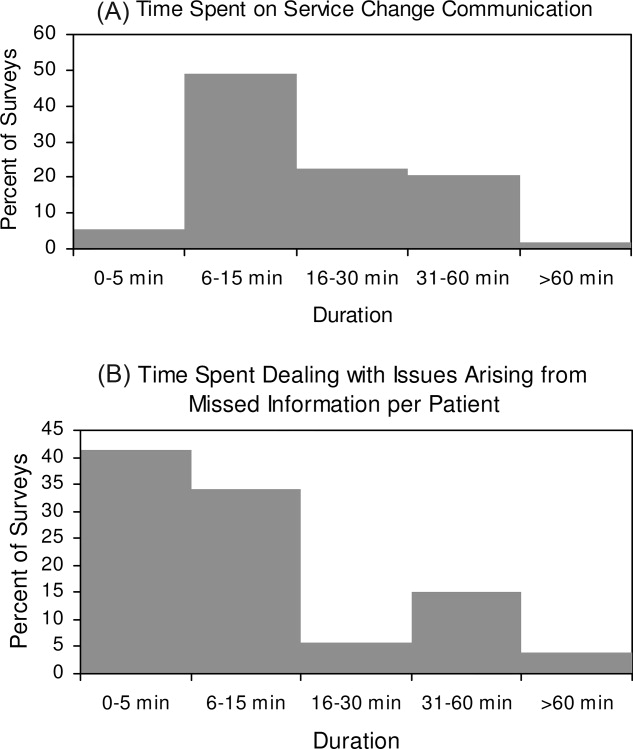
Fifty‐six of 60 (93%) surveys evaluating service changes were completed and returned. All (17) eligible hospitalists participated. All but 1 completed survey indicated that some form of handoff communication took place between the incoming and the outgoing hospitalists. The median time category spent on service change communications was 6 to 15 minutes. Forty‐eight of 55 (87%) respondents who participated in handoff communication reported communicating on the day prior to the transition day, while the remainder communicated 2 or 3 days prior to, or on the transition day. Most communicated verbally, either by telephone (75%) or face to face (16%); 10% of respondents who did not speak with the outgoing physician received e‐mail as the main method of communication. The distribution of time spent on the service change communication is summarized in Figure 1A.
Completeness of Service Changes
Thirteen percent (7/56) of service change communication was described as incomplete. These were associated with consequences of incomplete service changes (see Table 1). Specifically, handoffs characterized as incomplete were more likely to have hospitalists report uncertainty regarding the plan of care (71% incomplete vs. 10% complete, P < 0.01), discover missing information (71% incomplete vs. 24% complete, P = 0.01), and report near‐misses/adverse events (57% incomplete vs. 10% complete, P < 0.01). Completeness was not associated with time spent on the communication (P = 0.77) or with having engaged in verbal communication (88% complete vs. 100% incomplete, P = 0.33). Incomplete handoff communications were also associated with hospitalists spending more than the median time dealing with issues arising from missing or lost information (71% incomplete vs. 22% complete, P < 0.01). The distribution of time spent retrieving missing patient information and resolving issues that arose from it is shown in Figure 1B. The median time category was 6 to 15 minutes per patient.
| Incomplete (n = 7) % | Complete (n = 49) % | P Value | |
|---|---|---|---|
| Uncertainty about the patient care plan (n = 10) | 71 | 10 | <0.01 |
| Discovery of missed information that should have been discussed (n = 17) | 71 | 24 | 0.01 |
| Report of adverse and near miss events (n = 9) | 57 | 10 | <0.01 |
| More than 15 minutes spent dealing with issues arising from missed information (n = 16) | 71 | 22 | <0.01 |
The recovery of missing information involved hospitalists utilizing various sources of information summarized in Table 2. Electronic medical records were used most commonly (86%), followed by the patient chart (82%). 38% of respondents also reported soliciting the outgoing physician to recover information that was missed in the service change. Only 40% reported that patients were aware of the service change and 15% reported that patients' family were aware of the service change. Sixty‐one percent of respondents believe that a more detailed communication at service change can help avoid uncertainty, delays, and adverse events.
| Sources | n (%) |
|---|---|
| |
| Electronic medical records | 48 (86) |
| Patient chart | 46 (82) |
| Consulting physicians | 39 (70) |
| Patients' family | 33 (59) |
| Patients | 32 (57) |
| Outgoing physician (repeat communications) | 21 (38) |
Qualitative Data
Qualitative analyses of omitted information at service change yielded the following major categories: (1) factual patient information; (2) information pertaining to future plan of care; and (3) disagreements about past management (Table 3A). Among the subthemes of the first major category, recommendations by consultants were pointed out as a specific area requiring targeted discussions during the handoff process.
| Major Category | Subtheme | Representative Comment |
|---|---|---|
| ||
| A. Information not discussed at service change that should have been discussed | ||
| Factual patient information | From initial workup | [Was] the preceding MD unaware that the patient had colonic ischemia? |
| Complications during the present hospital course | Would have liked to hear the highlights of previous workup for hyponatremia | |
| Patient family | Would have liked to know how much family members were involved | |
| Consultant recommendation | Consultant recommendations were only partially done and not very well communicated | |
| Future plan of care | Plans to advance hospital course | Plan for dialysis when an existing access catheter was to be removedno explanation of plan |
| Disposition planning | Reasons why home regimen of diuretics were being held and plans to resume or keep holding at discharge | |
| Disagreement about management | Diagnostics | Appropriate surveillance labs not ordered in 12 hours for a patient admitted with a wide anion gap from DKA |
| Therapeutics | No blood transfusion in a patient needing one | |
| B. Adverse and near‐miss events attributable to missed information | ||
| Poor quality of care | Uncoordinated care | Coagulation issue not addressed prior to scheduled procedure leading to delay |
| Deviations from standard care | Patient almost did not receive nephroprotective regimen prior to an angiogram | |
| Stakeholder dissatisfied | Patient dissatisfied | Patient was not placed mainly because of poor communication |
| Consultant dissatisfied | Consultants were unhappy that their [recommendations] were not followed | |
| C. Topics covered in posthandoff communications between physicians | ||
| Clarification of missing information | Medical history | Question regarding patient's baseline mental status |
| Disposition planning | Question about discharge planning and communication with family | |
| Consultant recommendations | Clarification of consult recommendations | |
| Evaluative discussion | Review of medical management | Discussion about antibiotic choice started over the weekend |
| Updates | Preceding physician came and asked me how the patients were doing | |
| D. Suggestions for improving handoff communication | ||
| Techniques to improve the quality of verbal communication | Tension between too much and too little | Maybe it's purely a style issue, but I tend to give a lengthy signout, maybe too detailed but for detail‐oriented person like me a very cursory signout leaves too much uncertainty |
| Focused | The exchange of information should befocused on what are the major vs. minor issues | |
| Systematic | Signout should be more systematictime spent signing out is useless if filled with useless rambling | |
| Techniques to ensure the accurate transmission of information | Read‐back | Read‐back ensures details are correct |
| Transition period | Having the previous hospitalist available to answer questions is enough | |
| Suggested content improvements | Communicate future plan of care | Should focus on the future plan of care and not only on medical problems so that the in‐coming person will have a better idea of what to do on his first day |
| Transmit consultant recommendations | Knowing consult recommendations for patients and plans for procedures | |
| Involving other stakeholders | Inform patients of service change | Preceding MD explained change to all patients and they appreciated it |
| Involve mid‐level practitioners in the communication | Better mid‐level to physician communication would help | |
When asked to describe the nature of near‐miss and adverse events, 2 major categories emerged: (1) poor quality of care; and (2) stakeholder dissatisfaction (Table 3B). Respondents of this study only reported near‐miss events, but included several events that could have resulted in significant patient harm. One respondent wrote, [the] patient almost did not receive nephroprotective regimen prior toangio[gram]. On a service with complicated patients requiring the involvement of multiple subspecialists, the need for coordination through better communication was frequently mentioned.
As previously described, incoming hospitalists who discovered missing information often engaged in discussions with the outgoing hospitalist after the original service change handoff. These repeat communications served to clarify missing information as well as to allow opportunities to review and update information as summarized in Table 3C.
Suggestions for Improving Service Changes
Suggestions for improving service handoff communication yielded four major categories: (1) improve the quality of information relayed; (2) utilization of communication techniques to ensure accurate transmission of data; (3) improve the communication content; and (4) involve other stakeholders (see Table 3D).
The comments around quality of communication highlighted the tension between too much and too little information that may be resolved by organizing the content of the handoff communication without dedicating more time to the process. While some respondents felt that a detailed signout is always helpful, others stressed the need to avoid useless rambling. One respondent, who preferred a minimalist approach, felt that a comprehensive patient summary was difficult to retain and that having the outgoing physician available to answer questions early in the rotation was an effective alternative to a single episodic handoff. Another recommendation included the use of the read‐back technique to ensure accurate transmission of important information.
Discussion
To our knowledge, this is the first study of service changes among hospitalists. The results suggest that hospitalists in an academic medical center face obstacles to effective communication during service changes. A significant number of handoffs were described by hospitalists as incomplete and that missing information were associated with negative outcomes at the patient level. Reports of incomplete handoffs were associated with uncertainty by incoming physicians about the plan of care for patients and with the need to spend more time dealing with issues arising from this uncertainty. Although most of the effects on patients were near‐misses and not adverse events, the details elicited in this study reveal the threats to patient safety that arise from ineffective communication.
Interestingly, verbal communication was not associated with better transmission of information in this study. One reason for this may be the almost universal use of verbal communication in the service change handoffs among hospitalists at the UCMC. The value of verbal communication is supported by other studies that suggest the benefits of verbal exchanges combined with typed information sheets.15
In our study, hospitalists spent a significant amount of time resolving issues that arose from incomplete communication at service change. The need to retrieve missing information from charts and electronic medical records is to be expected, even if the handoffs were complete, but the use of patients and their family as redundant sources of information may lead to delay and stakeholder dissatisfaction. Likewise, consulting physicians were sometimes frustrated by not having their recommendations passed on during hospitalist service changes and of being asked to repeat their recommendations to each new incoming hospitalist. Moreover, many patients and consulting physicians were not informed about upcoming service changes by hospitalists. Informing stakeholders of staffing changes may be an important component of handoffs that requires attention.4, 16
The frequent communication between the outgoing and incoming hospitalists, even after their original handoff communication, points to the possible benefit of an overlap period during which outgoing physicians remain available to fill gaps in information. The willingness of outgoing hospitalists in this study to initiate this interaction reveals an opportunity for an intervention and is contrary to existing concerns that hospitalists, as opposed to primary care physicians, absolve themselves of patient responsibilities when their shift is completed.17, 18
Ensuring that handoff communication is concise and systematic is essential to improving the quality of care provided by hospitalists. An all‐inclusive transmission of unprocessed information, no matter how detailed, does not improve completeness of communication. Instead, we find that the complete transmission of patient information consists of both the discussion of the salient factual information about the case and the outgoing physician's assessment and future plan. A new strategy to improve completeness of service change communication may involve the use of a checklist to ensure a comprehensive review of critical details, as well as the use of narratives to tie together a coherent plan.
Alternative cutpoints for the dichotomized Likert categories for uncertainty about the plan and completeness of the handoff were explored. For example, it is also reasonable to interpret the response somewhat certain, referring to the plan of care on the transition day, as belonging to the dichotomized category uncertain as opposed to certain. A broader definition of uncertain increased the number of responses in that category but the variable's associations with other item responses were not significantly different from the results presented. We chose the symmetrical dichotomization cutpoint to ensure similar number of answers in each category.
There are several limitations with this study. First, the study was limited to self‐reported data without confirmation by direct observation. Additionally, responses to survey questions that ask participants to recollect details of a past handoff communication are subject to recall bias. We tried to minimize this bias effect by adhering to a schedule that surveyed hospitalists almost exactly at 48 hours into their rotation. However, there may still be hindsight bias about the respondents' perceived completeness of the handoffs based on the events of those 48 hours.19 In addition, a service of difficult patients requiring more of the hospitalist's time could influence his or her perception of a poor handoff through reverse causation. The study is not immune to a Hawthorne effect during the 8 months study period.20 This was a single‐center study examining 1 clinical service. The small sample size limits the depth of our analysis, but this is the first work to describe this phenomenon and although the data is not definitive, it may stimulate further work in the area. Although our study focused on completeness as the sole measure of handoff adequacy, additional measures may be explored in future studies. Finally, our findings may not be generalizable because of the unique features of the UCMC's hospitalist program, such as the specialized patient population. An examination of other practice settings is indicated for future studies.
Significant variability exists in the methods used to conduct service changes. Although a previous qualitative study of handoffs at our institution yielded a theme of poor communication around specific individuals,21 consistently poor communicators did not emerge as a theme in this qualitative analysis. We believe that episodes of incomplete communication are not always attributable to individual deficits and suggest that solutions to the communication problem exist at the systems level. The development and implementation of future interventions to improve hospitalist service changes may incorporate some of the elements suggested here.
- ,,.To Err is Human: Building a Safer Health System.Washington, DC:National Academies Press;2000.
- ,.Care transitions for hospitalized patients.Med Clin N Am.2008;92:315–324.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14:401–407.
- ,,.Communicating in the “gray zone”: perceptions about emergency physician‐hospitalist handoffs and patient safety.Acad Emerg Med.2007;14:884–894.
- ,,,.Adequacy of information transferred at resident sign‐out (inhospital handover of care): a prospective survey.Qual Saf Health Care.2008;17:6–10.
- ,,,.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- National Patient Safety Goals. Available at: http://www.jcaho.com. Accessed May2009.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- ,,,.Preparing for “diastole”: advanced training opportunities for academic hospitalists.J Hosp Med.2006;1(6):368–377.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: a qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,,.Transfers of patient care between house staff on internal medicine wards: a national survey.Arch Intern Med.2006;166(11):1173–1177.
- .The critical incident technique.Psychol Bull.1954;51:327–358.
- ,.Basics of Qualitative Research.2nd ed.Thousand Oaks, CA:Sage Publications;1998.
- ,,,.Pilot study to show the loss of important data in nursing handover.Br J Nurs.2005;14(20):1090–1093.
- ,,, et al.How do hospitalized patients feel about resident work hours, fatigue, and discontinuity of care.J Gen Intern Med.2008;23(5):623–628.
- ,,.A new doctor in the house: ethical issues in hospitalist systems.JAMA.2000;283(3):336–337.
- ,,,.A theoretical framework and competency‐based approach to improving handoffs.Qual Saf Health Care.2008;17(1):11–14.
- ,.Hindsight bias, outcome knowledge and adaptive learning.Qual Saf Health Care.2003;12(suppl 2):ii46–ii50.
- . Hawthorne and the Western Electric Company.The Social Problems of an Industrial Civilisation.London, UK:Routledge;1949.
- ,.A model for building a standardized hand‐off protocol.Jt Comm J Qual Patient Saf.2006;32(11):646–655.
A growing number of reports indicate that communication failures among physicians at transitions of care are critical to patient safety.16 The practice of physician handoffs at shift and service changes are variable, with no standardized protocol shown to be effective at ensuring complete transmission of information.7 In 2006, the Joint Commission set a National Patient Safety Goal to implement a standardized approach to hand off communications.8 Hospitalists stand to be impacted by this decision due to the frequency of care transitions that are inherent in hospital practice. The Society of Hospital Medicine (SHM) recognizes safe transitions of care as a core competency of hospitalists and is actively exploring standardization of the process.9 While recent attention has focused on improved communication during shift changes, little data exists to guide handoffs among hospitalists at service changes.
Good service change communication is an essential skill of hospital medicine because frequent service handoffs are often unavoidable in hospitalist practices that seek to balance the demand for around‐the‐clock coverage for inpatients and the need to create sustainable schedules to avoid physician burnout.10 But the tradeoff between fewer hours worked and discontinuity of care is well recognized.7 Increasingly fragmented care without corresponding improvements in handoff communication may exacerbate the problem. This study aims to characterize communication practices among hospitalists during service changes and to describe adverse and near miss events that may occur as a result of poor handoffs during these vulnerable care transitions.
Methods
Setting
This study was conducted with Institutional Review Board (IRB) exemption at a single, academic tertiary care institution. The Section of Hospital Medicine at the University of Chicago is comprised of 17 physicians and 5 mid‐level practitioners (Nurse Practitioner and Physician Assistant), and staffs a nonteaching multispecialty service of patients with solid‐organ transplants (excluding heart) or preexisting oncological diagnoses. While hospitalists are the attendings of record, the care of these complex patients often requires the input of subspecialty consultants.
The nonteaching hospitalist service consists of 2 teams, each staffed by 1 hospitalist, and 1 or 2 mid‐level practitioners supporting the hospitalist on weekdays. Hospitalists rotate on the service for 1 or 2 weeks at a time. Mid‐level practitioners work a nonuniform 3 to 4 days per week. The patient census ranges from 2 to 12 patients per team while 3 to 6 new admissions are received every other day. A dedicated nocturnist or moonlighter manages existing patients and new admissions overnight.
At the time of service change, either the incoming or the outgoing physician initiates the communication by pager, telephone, e‐mail, or by face‐to‐face solicitation. A computerized census form on a Microsoft Word template with each patient's identifying information and a summary of the hospital course is updated by the outgoing hospitalist and is accessible to the incoming hospitalist. Mid‐level practitioners, typically, do not participate in service change handoffs because they are not always on duty at the time of service change. Other than through the universal use of the computerized census form, there was no standardized protocol or education on how to perform service changes.
Data Collection
All 17 hospitalists rotating through the nonteaching inpatient service at the University of Chicago Medical Center (UCMC) were recruited to participate. Between May and December 2007, one of the investigators (K.H.) hand‐delivered surveys to the study subjects who usually completed the survey immediately. Those who could not complete the survey on the spot were approached by the investigator a second time a few hours later. The participants were hospitalists who started their duty on the nonteaching service 48 hours earlier. A total of 60 service changes during the study period were the units of analysis in this study.
Eighteen items of the anonymous, paper‐based, self‐administered survey (see Appendix 1) were created to evaluate the characteristics of service change communications found to be salient in previous studies.11, 12 Hospitalists were asked to estimate the time they spent on the handoff communication, and the time they spent dealing with issues that arose as a result of missing information. Responses included <5 minutes, 6‐15 minutes, 16‐30 minutes, 31‐60 minutes, and >60 minutes.
Completeness of the handoff communication and the respondents' certainty about the care‐plans for the patients on the first day of service were rated using 6‐point Likert‐type scales. For example, the possible responses to an item asking respondents to rate the completeness of information in the handoff communication were grossly incomplete, incomplete, somewhat incomplete, somewhat complete, complete, and excessively complete. Respondents were asked to recall how often they encountered consequences of incomplete handoffs such as instances, within the first 48 hours of service, when they required information that should have been discussed at handoff but was not. Another consequence of incomplete handoffs that the survey asked hospitalists to recall was the frequency of near‐miss and adverse events.
Narrative details about missing information from the service change and near misses and adverse events attributable to poor handoffs were solicited using the critical incident technique. This technique is used to elicit open‐ended constructed descriptions of infrequently occurring events through personal observations and experience.13 Respondents were also asked about the frequency and content of any discussions they had with the outgoing hospitalist after the original handoff communication. Finally, suggestions for improving service change handoffs were solicited from each respondent.
Data Analysis
The results of the Likert responses were dichotomized such that incomplete handoffs were defined as response of grossly incomplete, incomplete, or somewhat incomplete. Complete handoffs were defined as response of somewhat complete, complete, or excessively complete. Similarly, certainty about the plan for each patient on the first day of rotation was dichotomized with uncertain defined as response of uncertain, mostly uncertain, or somewhat uncertain, while certain was defined as a response of somewhat certain, mostly certain, or certain. Associations among service change characteristics were compared using chi‐square tests of the dichotomized Likert‐type data.
Narrative responses were analyzed by 3 of the authors (J.F., K.H., V.A.) using the constant comparative method.14 Major categories were created without a priori hypotheses. These categories were compared across surveys to yield integration or refinement into further subcategories. Disagreements were resolved by discussion until 100% agreement was reached.
Results
Service Change Communication
Fifty‐six of 60 (93%) surveys evaluating service changes were completed and returned. All (17) eligible hospitalists participated. All but 1 completed survey indicated that some form of handoff communication took place between the incoming and the outgoing hospitalists. The median time category spent on service change communications was 6 to 15 minutes. Forty‐eight of 55 (87%) respondents who participated in handoff communication reported communicating on the day prior to the transition day, while the remainder communicated 2 or 3 days prior to, or on the transition day. Most communicated verbally, either by telephone (75%) or face to face (16%); 10% of respondents who did not speak with the outgoing physician received e‐mail as the main method of communication. The distribution of time spent on the service change communication is summarized in Figure 1A.
Completeness of Service Changes
Thirteen percent (7/56) of service change communication was described as incomplete. These were associated with consequences of incomplete service changes (see Table 1). Specifically, handoffs characterized as incomplete were more likely to have hospitalists report uncertainty regarding the plan of care (71% incomplete vs. 10% complete, P < 0.01), discover missing information (71% incomplete vs. 24% complete, P = 0.01), and report near‐misses/adverse events (57% incomplete vs. 10% complete, P < 0.01). Completeness was not associated with time spent on the communication (P = 0.77) or with having engaged in verbal communication (88% complete vs. 100% incomplete, P = 0.33). Incomplete handoff communications were also associated with hospitalists spending more than the median time dealing with issues arising from missing or lost information (71% incomplete vs. 22% complete, P < 0.01). The distribution of time spent retrieving missing patient information and resolving issues that arose from it is shown in Figure 1B. The median time category was 6 to 15 minutes per patient.
| Incomplete (n = 7) % | Complete (n = 49) % | P Value | |
|---|---|---|---|
| Uncertainty about the patient care plan (n = 10) | 71 | 10 | <0.01 |
| Discovery of missed information that should have been discussed (n = 17) | 71 | 24 | 0.01 |
| Report of adverse and near miss events (n = 9) | 57 | 10 | <0.01 |
| More than 15 minutes spent dealing with issues arising from missed information (n = 16) | 71 | 22 | <0.01 |
The recovery of missing information involved hospitalists utilizing various sources of information summarized in Table 2. Electronic medical records were used most commonly (86%), followed by the patient chart (82%). 38% of respondents also reported soliciting the outgoing physician to recover information that was missed in the service change. Only 40% reported that patients were aware of the service change and 15% reported that patients' family were aware of the service change. Sixty‐one percent of respondents believe that a more detailed communication at service change can help avoid uncertainty, delays, and adverse events.
| Sources | n (%) |
|---|---|
| |
| Electronic medical records | 48 (86) |
| Patient chart | 46 (82) |
| Consulting physicians | 39 (70) |
| Patients' family | 33 (59) |
| Patients | 32 (57) |
| Outgoing physician (repeat communications) | 21 (38) |
Qualitative Data
Qualitative analyses of omitted information at service change yielded the following major categories: (1) factual patient information; (2) information pertaining to future plan of care; and (3) disagreements about past management (Table 3A). Among the subthemes of the first major category, recommendations by consultants were pointed out as a specific area requiring targeted discussions during the handoff process.
| Major Category | Subtheme | Representative Comment |
|---|---|---|
| ||
| A. Information not discussed at service change that should have been discussed | ||
| Factual patient information | From initial workup | [Was] the preceding MD unaware that the patient had colonic ischemia? |
| Complications during the present hospital course | Would have liked to hear the highlights of previous workup for hyponatremia | |
| Patient family | Would have liked to know how much family members were involved | |
| Consultant recommendation | Consultant recommendations were only partially done and not very well communicated | |
| Future plan of care | Plans to advance hospital course | Plan for dialysis when an existing access catheter was to be removedno explanation of plan |
| Disposition planning | Reasons why home regimen of diuretics were being held and plans to resume or keep holding at discharge | |
| Disagreement about management | Diagnostics | Appropriate surveillance labs not ordered in 12 hours for a patient admitted with a wide anion gap from DKA |
| Therapeutics | No blood transfusion in a patient needing one | |
| B. Adverse and near‐miss events attributable to missed information | ||
| Poor quality of care | Uncoordinated care | Coagulation issue not addressed prior to scheduled procedure leading to delay |
| Deviations from standard care | Patient almost did not receive nephroprotective regimen prior to an angiogram | |
| Stakeholder dissatisfied | Patient dissatisfied | Patient was not placed mainly because of poor communication |
| Consultant dissatisfied | Consultants were unhappy that their [recommendations] were not followed | |
| C. Topics covered in posthandoff communications between physicians | ||
| Clarification of missing information | Medical history | Question regarding patient's baseline mental status |
| Disposition planning | Question about discharge planning and communication with family | |
| Consultant recommendations | Clarification of consult recommendations | |
| Evaluative discussion | Review of medical management | Discussion about antibiotic choice started over the weekend |
| Updates | Preceding physician came and asked me how the patients were doing | |
| D. Suggestions for improving handoff communication | ||
| Techniques to improve the quality of verbal communication | Tension between too much and too little | Maybe it's purely a style issue, but I tend to give a lengthy signout, maybe too detailed but for detail‐oriented person like me a very cursory signout leaves too much uncertainty |
| Focused | The exchange of information should befocused on what are the major vs. minor issues | |
| Systematic | Signout should be more systematictime spent signing out is useless if filled with useless rambling | |
| Techniques to ensure the accurate transmission of information | Read‐back | Read‐back ensures details are correct |
| Transition period | Having the previous hospitalist available to answer questions is enough | |
| Suggested content improvements | Communicate future plan of care | Should focus on the future plan of care and not only on medical problems so that the in‐coming person will have a better idea of what to do on his first day |
| Transmit consultant recommendations | Knowing consult recommendations for patients and plans for procedures | |
| Involving other stakeholders | Inform patients of service change | Preceding MD explained change to all patients and they appreciated it |
| Involve mid‐level practitioners in the communication | Better mid‐level to physician communication would help | |
When asked to describe the nature of near‐miss and adverse events, 2 major categories emerged: (1) poor quality of care; and (2) stakeholder dissatisfaction (Table 3B). Respondents of this study only reported near‐miss events, but included several events that could have resulted in significant patient harm. One respondent wrote, [the] patient almost did not receive nephroprotective regimen prior toangio[gram]. On a service with complicated patients requiring the involvement of multiple subspecialists, the need for coordination through better communication was frequently mentioned.
As previously described, incoming hospitalists who discovered missing information often engaged in discussions with the outgoing hospitalist after the original service change handoff. These repeat communications served to clarify missing information as well as to allow opportunities to review and update information as summarized in Table 3C.
Suggestions for Improving Service Changes
Suggestions for improving service handoff communication yielded four major categories: (1) improve the quality of information relayed; (2) utilization of communication techniques to ensure accurate transmission of data; (3) improve the communication content; and (4) involve other stakeholders (see Table 3D).
The comments around quality of communication highlighted the tension between too much and too little information that may be resolved by organizing the content of the handoff communication without dedicating more time to the process. While some respondents felt that a detailed signout is always helpful, others stressed the need to avoid useless rambling. One respondent, who preferred a minimalist approach, felt that a comprehensive patient summary was difficult to retain and that having the outgoing physician available to answer questions early in the rotation was an effective alternative to a single episodic handoff. Another recommendation included the use of the read‐back technique to ensure accurate transmission of important information.
Discussion
To our knowledge, this is the first study of service changes among hospitalists. The results suggest that hospitalists in an academic medical center face obstacles to effective communication during service changes. A significant number of handoffs were described by hospitalists as incomplete and that missing information were associated with negative outcomes at the patient level. Reports of incomplete handoffs were associated with uncertainty by incoming physicians about the plan of care for patients and with the need to spend more time dealing with issues arising from this uncertainty. Although most of the effects on patients were near‐misses and not adverse events, the details elicited in this study reveal the threats to patient safety that arise from ineffective communication.
Interestingly, verbal communication was not associated with better transmission of information in this study. One reason for this may be the almost universal use of verbal communication in the service change handoffs among hospitalists at the UCMC. The value of verbal communication is supported by other studies that suggest the benefits of verbal exchanges combined with typed information sheets.15
In our study, hospitalists spent a significant amount of time resolving issues that arose from incomplete communication at service change. The need to retrieve missing information from charts and electronic medical records is to be expected, even if the handoffs were complete, but the use of patients and their family as redundant sources of information may lead to delay and stakeholder dissatisfaction. Likewise, consulting physicians were sometimes frustrated by not having their recommendations passed on during hospitalist service changes and of being asked to repeat their recommendations to each new incoming hospitalist. Moreover, many patients and consulting physicians were not informed about upcoming service changes by hospitalists. Informing stakeholders of staffing changes may be an important component of handoffs that requires attention.4, 16
The frequent communication between the outgoing and incoming hospitalists, even after their original handoff communication, points to the possible benefit of an overlap period during which outgoing physicians remain available to fill gaps in information. The willingness of outgoing hospitalists in this study to initiate this interaction reveals an opportunity for an intervention and is contrary to existing concerns that hospitalists, as opposed to primary care physicians, absolve themselves of patient responsibilities when their shift is completed.17, 18
Ensuring that handoff communication is concise and systematic is essential to improving the quality of care provided by hospitalists. An all‐inclusive transmission of unprocessed information, no matter how detailed, does not improve completeness of communication. Instead, we find that the complete transmission of patient information consists of both the discussion of the salient factual information about the case and the outgoing physician's assessment and future plan. A new strategy to improve completeness of service change communication may involve the use of a checklist to ensure a comprehensive review of critical details, as well as the use of narratives to tie together a coherent plan.
Alternative cutpoints for the dichotomized Likert categories for uncertainty about the plan and completeness of the handoff were explored. For example, it is also reasonable to interpret the response somewhat certain, referring to the plan of care on the transition day, as belonging to the dichotomized category uncertain as opposed to certain. A broader definition of uncertain increased the number of responses in that category but the variable's associations with other item responses were not significantly different from the results presented. We chose the symmetrical dichotomization cutpoint to ensure similar number of answers in each category.
There are several limitations with this study. First, the study was limited to self‐reported data without confirmation by direct observation. Additionally, responses to survey questions that ask participants to recollect details of a past handoff communication are subject to recall bias. We tried to minimize this bias effect by adhering to a schedule that surveyed hospitalists almost exactly at 48 hours into their rotation. However, there may still be hindsight bias about the respondents' perceived completeness of the handoffs based on the events of those 48 hours.19 In addition, a service of difficult patients requiring more of the hospitalist's time could influence his or her perception of a poor handoff through reverse causation. The study is not immune to a Hawthorne effect during the 8 months study period.20 This was a single‐center study examining 1 clinical service. The small sample size limits the depth of our analysis, but this is the first work to describe this phenomenon and although the data is not definitive, it may stimulate further work in the area. Although our study focused on completeness as the sole measure of handoff adequacy, additional measures may be explored in future studies. Finally, our findings may not be generalizable because of the unique features of the UCMC's hospitalist program, such as the specialized patient population. An examination of other practice settings is indicated for future studies.
Significant variability exists in the methods used to conduct service changes. Although a previous qualitative study of handoffs at our institution yielded a theme of poor communication around specific individuals,21 consistently poor communicators did not emerge as a theme in this qualitative analysis. We believe that episodes of incomplete communication are not always attributable to individual deficits and suggest that solutions to the communication problem exist at the systems level. The development and implementation of future interventions to improve hospitalist service changes may incorporate some of the elements suggested here.
A growing number of reports indicate that communication failures among physicians at transitions of care are critical to patient safety.16 The practice of physician handoffs at shift and service changes are variable, with no standardized protocol shown to be effective at ensuring complete transmission of information.7 In 2006, the Joint Commission set a National Patient Safety Goal to implement a standardized approach to hand off communications.8 Hospitalists stand to be impacted by this decision due to the frequency of care transitions that are inherent in hospital practice. The Society of Hospital Medicine (SHM) recognizes safe transitions of care as a core competency of hospitalists and is actively exploring standardization of the process.9 While recent attention has focused on improved communication during shift changes, little data exists to guide handoffs among hospitalists at service changes.
Good service change communication is an essential skill of hospital medicine because frequent service handoffs are often unavoidable in hospitalist practices that seek to balance the demand for around‐the‐clock coverage for inpatients and the need to create sustainable schedules to avoid physician burnout.10 But the tradeoff between fewer hours worked and discontinuity of care is well recognized.7 Increasingly fragmented care without corresponding improvements in handoff communication may exacerbate the problem. This study aims to characterize communication practices among hospitalists during service changes and to describe adverse and near miss events that may occur as a result of poor handoffs during these vulnerable care transitions.
Methods
Setting
This study was conducted with Institutional Review Board (IRB) exemption at a single, academic tertiary care institution. The Section of Hospital Medicine at the University of Chicago is comprised of 17 physicians and 5 mid‐level practitioners (Nurse Practitioner and Physician Assistant), and staffs a nonteaching multispecialty service of patients with solid‐organ transplants (excluding heart) or preexisting oncological diagnoses. While hospitalists are the attendings of record, the care of these complex patients often requires the input of subspecialty consultants.
The nonteaching hospitalist service consists of 2 teams, each staffed by 1 hospitalist, and 1 or 2 mid‐level practitioners supporting the hospitalist on weekdays. Hospitalists rotate on the service for 1 or 2 weeks at a time. Mid‐level practitioners work a nonuniform 3 to 4 days per week. The patient census ranges from 2 to 12 patients per team while 3 to 6 new admissions are received every other day. A dedicated nocturnist or moonlighter manages existing patients and new admissions overnight.
At the time of service change, either the incoming or the outgoing physician initiates the communication by pager, telephone, e‐mail, or by face‐to‐face solicitation. A computerized census form on a Microsoft Word template with each patient's identifying information and a summary of the hospital course is updated by the outgoing hospitalist and is accessible to the incoming hospitalist. Mid‐level practitioners, typically, do not participate in service change handoffs because they are not always on duty at the time of service change. Other than through the universal use of the computerized census form, there was no standardized protocol or education on how to perform service changes.
Data Collection
All 17 hospitalists rotating through the nonteaching inpatient service at the University of Chicago Medical Center (UCMC) were recruited to participate. Between May and December 2007, one of the investigators (K.H.) hand‐delivered surveys to the study subjects who usually completed the survey immediately. Those who could not complete the survey on the spot were approached by the investigator a second time a few hours later. The participants were hospitalists who started their duty on the nonteaching service 48 hours earlier. A total of 60 service changes during the study period were the units of analysis in this study.
Eighteen items of the anonymous, paper‐based, self‐administered survey (see Appendix 1) were created to evaluate the characteristics of service change communications found to be salient in previous studies.11, 12 Hospitalists were asked to estimate the time they spent on the handoff communication, and the time they spent dealing with issues that arose as a result of missing information. Responses included <5 minutes, 6‐15 minutes, 16‐30 minutes, 31‐60 minutes, and >60 minutes.
Completeness of the handoff communication and the respondents' certainty about the care‐plans for the patients on the first day of service were rated using 6‐point Likert‐type scales. For example, the possible responses to an item asking respondents to rate the completeness of information in the handoff communication were grossly incomplete, incomplete, somewhat incomplete, somewhat complete, complete, and excessively complete. Respondents were asked to recall how often they encountered consequences of incomplete handoffs such as instances, within the first 48 hours of service, when they required information that should have been discussed at handoff but was not. Another consequence of incomplete handoffs that the survey asked hospitalists to recall was the frequency of near‐miss and adverse events.
Narrative details about missing information from the service change and near misses and adverse events attributable to poor handoffs were solicited using the critical incident technique. This technique is used to elicit open‐ended constructed descriptions of infrequently occurring events through personal observations and experience.13 Respondents were also asked about the frequency and content of any discussions they had with the outgoing hospitalist after the original handoff communication. Finally, suggestions for improving service change handoffs were solicited from each respondent.
Data Analysis
The results of the Likert responses were dichotomized such that incomplete handoffs were defined as response of grossly incomplete, incomplete, or somewhat incomplete. Complete handoffs were defined as response of somewhat complete, complete, or excessively complete. Similarly, certainty about the plan for each patient on the first day of rotation was dichotomized with uncertain defined as response of uncertain, mostly uncertain, or somewhat uncertain, while certain was defined as a response of somewhat certain, mostly certain, or certain. Associations among service change characteristics were compared using chi‐square tests of the dichotomized Likert‐type data.
Narrative responses were analyzed by 3 of the authors (J.F., K.H., V.A.) using the constant comparative method.14 Major categories were created without a priori hypotheses. These categories were compared across surveys to yield integration or refinement into further subcategories. Disagreements were resolved by discussion until 100% agreement was reached.
Results
Service Change Communication
Fifty‐six of 60 (93%) surveys evaluating service changes were completed and returned. All (17) eligible hospitalists participated. All but 1 completed survey indicated that some form of handoff communication took place between the incoming and the outgoing hospitalists. The median time category spent on service change communications was 6 to 15 minutes. Forty‐eight of 55 (87%) respondents who participated in handoff communication reported communicating on the day prior to the transition day, while the remainder communicated 2 or 3 days prior to, or on the transition day. Most communicated verbally, either by telephone (75%) or face to face (16%); 10% of respondents who did not speak with the outgoing physician received e‐mail as the main method of communication. The distribution of time spent on the service change communication is summarized in Figure 1A.
Completeness of Service Changes
Thirteen percent (7/56) of service change communication was described as incomplete. These were associated with consequences of incomplete service changes (see Table 1). Specifically, handoffs characterized as incomplete were more likely to have hospitalists report uncertainty regarding the plan of care (71% incomplete vs. 10% complete, P < 0.01), discover missing information (71% incomplete vs. 24% complete, P = 0.01), and report near‐misses/adverse events (57% incomplete vs. 10% complete, P < 0.01). Completeness was not associated with time spent on the communication (P = 0.77) or with having engaged in verbal communication (88% complete vs. 100% incomplete, P = 0.33). Incomplete handoff communications were also associated with hospitalists spending more than the median time dealing with issues arising from missing or lost information (71% incomplete vs. 22% complete, P < 0.01). The distribution of time spent retrieving missing patient information and resolving issues that arose from it is shown in Figure 1B. The median time category was 6 to 15 minutes per patient.
| Incomplete (n = 7) % | Complete (n = 49) % | P Value | |
|---|---|---|---|
| Uncertainty about the patient care plan (n = 10) | 71 | 10 | <0.01 |
| Discovery of missed information that should have been discussed (n = 17) | 71 | 24 | 0.01 |
| Report of adverse and near miss events (n = 9) | 57 | 10 | <0.01 |
| More than 15 minutes spent dealing with issues arising from missed information (n = 16) | 71 | 22 | <0.01 |
The recovery of missing information involved hospitalists utilizing various sources of information summarized in Table 2. Electronic medical records were used most commonly (86%), followed by the patient chart (82%). 38% of respondents also reported soliciting the outgoing physician to recover information that was missed in the service change. Only 40% reported that patients were aware of the service change and 15% reported that patients' family were aware of the service change. Sixty‐one percent of respondents believe that a more detailed communication at service change can help avoid uncertainty, delays, and adverse events.
| Sources | n (%) |
|---|---|
| |
| Electronic medical records | 48 (86) |
| Patient chart | 46 (82) |
| Consulting physicians | 39 (70) |
| Patients' family | 33 (59) |
| Patients | 32 (57) |
| Outgoing physician (repeat communications) | 21 (38) |
Qualitative Data
Qualitative analyses of omitted information at service change yielded the following major categories: (1) factual patient information; (2) information pertaining to future plan of care; and (3) disagreements about past management (Table 3A). Among the subthemes of the first major category, recommendations by consultants were pointed out as a specific area requiring targeted discussions during the handoff process.
| Major Category | Subtheme | Representative Comment |
|---|---|---|
| ||
| A. Information not discussed at service change that should have been discussed | ||
| Factual patient information | From initial workup | [Was] the preceding MD unaware that the patient had colonic ischemia? |
| Complications during the present hospital course | Would have liked to hear the highlights of previous workup for hyponatremia | |
| Patient family | Would have liked to know how much family members were involved | |
| Consultant recommendation | Consultant recommendations were only partially done and not very well communicated | |
| Future plan of care | Plans to advance hospital course | Plan for dialysis when an existing access catheter was to be removedno explanation of plan |
| Disposition planning | Reasons why home regimen of diuretics were being held and plans to resume or keep holding at discharge | |
| Disagreement about management | Diagnostics | Appropriate surveillance labs not ordered in 12 hours for a patient admitted with a wide anion gap from DKA |
| Therapeutics | No blood transfusion in a patient needing one | |
| B. Adverse and near‐miss events attributable to missed information | ||
| Poor quality of care | Uncoordinated care | Coagulation issue not addressed prior to scheduled procedure leading to delay |
| Deviations from standard care | Patient almost did not receive nephroprotective regimen prior to an angiogram | |
| Stakeholder dissatisfied | Patient dissatisfied | Patient was not placed mainly because of poor communication |
| Consultant dissatisfied | Consultants were unhappy that their [recommendations] were not followed | |
| C. Topics covered in posthandoff communications between physicians | ||
| Clarification of missing information | Medical history | Question regarding patient's baseline mental status |
| Disposition planning | Question about discharge planning and communication with family | |
| Consultant recommendations | Clarification of consult recommendations | |
| Evaluative discussion | Review of medical management | Discussion about antibiotic choice started over the weekend |
| Updates | Preceding physician came and asked me how the patients were doing | |
| D. Suggestions for improving handoff communication | ||
| Techniques to improve the quality of verbal communication | Tension between too much and too little | Maybe it's purely a style issue, but I tend to give a lengthy signout, maybe too detailed but for detail‐oriented person like me a very cursory signout leaves too much uncertainty |
| Focused | The exchange of information should befocused on what are the major vs. minor issues | |
| Systematic | Signout should be more systematictime spent signing out is useless if filled with useless rambling | |
| Techniques to ensure the accurate transmission of information | Read‐back | Read‐back ensures details are correct |
| Transition period | Having the previous hospitalist available to answer questions is enough | |
| Suggested content improvements | Communicate future plan of care | Should focus on the future plan of care and not only on medical problems so that the in‐coming person will have a better idea of what to do on his first day |
| Transmit consultant recommendations | Knowing consult recommendations for patients and plans for procedures | |
| Involving other stakeholders | Inform patients of service change | Preceding MD explained change to all patients and they appreciated it |
| Involve mid‐level practitioners in the communication | Better mid‐level to physician communication would help | |
When asked to describe the nature of near‐miss and adverse events, 2 major categories emerged: (1) poor quality of care; and (2) stakeholder dissatisfaction (Table 3B). Respondents of this study only reported near‐miss events, but included several events that could have resulted in significant patient harm. One respondent wrote, [the] patient almost did not receive nephroprotective regimen prior toangio[gram]. On a service with complicated patients requiring the involvement of multiple subspecialists, the need for coordination through better communication was frequently mentioned.
As previously described, incoming hospitalists who discovered missing information often engaged in discussions with the outgoing hospitalist after the original service change handoff. These repeat communications served to clarify missing information as well as to allow opportunities to review and update information as summarized in Table 3C.
Suggestions for Improving Service Changes
Suggestions for improving service handoff communication yielded four major categories: (1) improve the quality of information relayed; (2) utilization of communication techniques to ensure accurate transmission of data; (3) improve the communication content; and (4) involve other stakeholders (see Table 3D).
The comments around quality of communication highlighted the tension between too much and too little information that may be resolved by organizing the content of the handoff communication without dedicating more time to the process. While some respondents felt that a detailed signout is always helpful, others stressed the need to avoid useless rambling. One respondent, who preferred a minimalist approach, felt that a comprehensive patient summary was difficult to retain and that having the outgoing physician available to answer questions early in the rotation was an effective alternative to a single episodic handoff. Another recommendation included the use of the read‐back technique to ensure accurate transmission of important information.
Discussion
To our knowledge, this is the first study of service changes among hospitalists. The results suggest that hospitalists in an academic medical center face obstacles to effective communication during service changes. A significant number of handoffs were described by hospitalists as incomplete and that missing information were associated with negative outcomes at the patient level. Reports of incomplete handoffs were associated with uncertainty by incoming physicians about the plan of care for patients and with the need to spend more time dealing with issues arising from this uncertainty. Although most of the effects on patients were near‐misses and not adverse events, the details elicited in this study reveal the threats to patient safety that arise from ineffective communication.
Interestingly, verbal communication was not associated with better transmission of information in this study. One reason for this may be the almost universal use of verbal communication in the service change handoffs among hospitalists at the UCMC. The value of verbal communication is supported by other studies that suggest the benefits of verbal exchanges combined with typed information sheets.15
In our study, hospitalists spent a significant amount of time resolving issues that arose from incomplete communication at service change. The need to retrieve missing information from charts and electronic medical records is to be expected, even if the handoffs were complete, but the use of patients and their family as redundant sources of information may lead to delay and stakeholder dissatisfaction. Likewise, consulting physicians were sometimes frustrated by not having their recommendations passed on during hospitalist service changes and of being asked to repeat their recommendations to each new incoming hospitalist. Moreover, many patients and consulting physicians were not informed about upcoming service changes by hospitalists. Informing stakeholders of staffing changes may be an important component of handoffs that requires attention.4, 16
The frequent communication between the outgoing and incoming hospitalists, even after their original handoff communication, points to the possible benefit of an overlap period during which outgoing physicians remain available to fill gaps in information. The willingness of outgoing hospitalists in this study to initiate this interaction reveals an opportunity for an intervention and is contrary to existing concerns that hospitalists, as opposed to primary care physicians, absolve themselves of patient responsibilities when their shift is completed.17, 18
Ensuring that handoff communication is concise and systematic is essential to improving the quality of care provided by hospitalists. An all‐inclusive transmission of unprocessed information, no matter how detailed, does not improve completeness of communication. Instead, we find that the complete transmission of patient information consists of both the discussion of the salient factual information about the case and the outgoing physician's assessment and future plan. A new strategy to improve completeness of service change communication may involve the use of a checklist to ensure a comprehensive review of critical details, as well as the use of narratives to tie together a coherent plan.
Alternative cutpoints for the dichotomized Likert categories for uncertainty about the plan and completeness of the handoff were explored. For example, it is also reasonable to interpret the response somewhat certain, referring to the plan of care on the transition day, as belonging to the dichotomized category uncertain as opposed to certain. A broader definition of uncertain increased the number of responses in that category but the variable's associations with other item responses were not significantly different from the results presented. We chose the symmetrical dichotomization cutpoint to ensure similar number of answers in each category.
There are several limitations with this study. First, the study was limited to self‐reported data without confirmation by direct observation. Additionally, responses to survey questions that ask participants to recollect details of a past handoff communication are subject to recall bias. We tried to minimize this bias effect by adhering to a schedule that surveyed hospitalists almost exactly at 48 hours into their rotation. However, there may still be hindsight bias about the respondents' perceived completeness of the handoffs based on the events of those 48 hours.19 In addition, a service of difficult patients requiring more of the hospitalist's time could influence his or her perception of a poor handoff through reverse causation. The study is not immune to a Hawthorne effect during the 8 months study period.20 This was a single‐center study examining 1 clinical service. The small sample size limits the depth of our analysis, but this is the first work to describe this phenomenon and although the data is not definitive, it may stimulate further work in the area. Although our study focused on completeness as the sole measure of handoff adequacy, additional measures may be explored in future studies. Finally, our findings may not be generalizable because of the unique features of the UCMC's hospitalist program, such as the specialized patient population. An examination of other practice settings is indicated for future studies.
Significant variability exists in the methods used to conduct service changes. Although a previous qualitative study of handoffs at our institution yielded a theme of poor communication around specific individuals,21 consistently poor communicators did not emerge as a theme in this qualitative analysis. We believe that episodes of incomplete communication are not always attributable to individual deficits and suggest that solutions to the communication problem exist at the systems level. The development and implementation of future interventions to improve hospitalist service changes may incorporate some of the elements suggested here.
- ,,.To Err is Human: Building a Safer Health System.Washington, DC:National Academies Press;2000.
- ,.Care transitions for hospitalized patients.Med Clin N Am.2008;92:315–324.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14:401–407.
- ,,.Communicating in the “gray zone”: perceptions about emergency physician‐hospitalist handoffs and patient safety.Acad Emerg Med.2007;14:884–894.
- ,,,.Adequacy of information transferred at resident sign‐out (inhospital handover of care): a prospective survey.Qual Saf Health Care.2008;17:6–10.
- ,,,.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- National Patient Safety Goals. Available at: http://www.jcaho.com. Accessed May2009.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- ,,,.Preparing for “diastole”: advanced training opportunities for academic hospitalists.J Hosp Med.2006;1(6):368–377.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: a qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,,.Transfers of patient care between house staff on internal medicine wards: a national survey.Arch Intern Med.2006;166(11):1173–1177.
- .The critical incident technique.Psychol Bull.1954;51:327–358.
- ,.Basics of Qualitative Research.2nd ed.Thousand Oaks, CA:Sage Publications;1998.
- ,,,.Pilot study to show the loss of important data in nursing handover.Br J Nurs.2005;14(20):1090–1093.
- ,,, et al.How do hospitalized patients feel about resident work hours, fatigue, and discontinuity of care.J Gen Intern Med.2008;23(5):623–628.
- ,,.A new doctor in the house: ethical issues in hospitalist systems.JAMA.2000;283(3):336–337.
- ,,,.A theoretical framework and competency‐based approach to improving handoffs.Qual Saf Health Care.2008;17(1):11–14.
- ,.Hindsight bias, outcome knowledge and adaptive learning.Qual Saf Health Care.2003;12(suppl 2):ii46–ii50.
- . Hawthorne and the Western Electric Company.The Social Problems of an Industrial Civilisation.London, UK:Routledge;1949.
- ,.A model for building a standardized hand‐off protocol.Jt Comm J Qual Patient Saf.2006;32(11):646–655.
- ,,.To Err is Human: Building a Safer Health System.Washington, DC:National Academies Press;2000.
- ,.Care transitions for hospitalized patients.Med Clin N Am.2008;92:315–324.
- ,,,,.Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis.Qual Saf Health Care.2005;14:401–407.
- ,,.Communicating in the “gray zone”: perceptions about emergency physician‐hospitalist handoffs and patient safety.Acad Emerg Med.2007;14:884–894.
- ,,,.Adequacy of information transferred at resident sign‐out (inhospital handover of care): a prospective survey.Qual Saf Health Care.2008;17:6–10.
- ,,,.Lost in translation: challenges and opportunities in physician‐to‐physician communication during patient handoffs.Acad Med.2005;80:1094–1099.
- ,,,,.Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign‐out.J Hosp Med.2006;1(4):257–266.
- National Patient Safety Goals. Available at: http://www.jcaho.com. Accessed May2009.
- ,,,,.Core competencies in hospital medicine: development and methodology.J Hosp Med.2006;1(1):48–56.
- ,,,.Preparing for “diastole”: advanced training opportunities for academic hospitalists.J Hosp Med.2006;1(6):368–377.
- ,,,,.Resident uncertainty in clinical decision making and impact on patient care: a qualitative study.Qual Saf Health Care.2008;17:122–126.
- ,,,.Transfers of patient care between house staff on internal medicine wards: a national survey.Arch Intern Med.2006;166(11):1173–1177.
- .The critical incident technique.Psychol Bull.1954;51:327–358.
- ,.Basics of Qualitative Research.2nd ed.Thousand Oaks, CA:Sage Publications;1998.
- ,,,.Pilot study to show the loss of important data in nursing handover.Br J Nurs.2005;14(20):1090–1093.
- ,,, et al.How do hospitalized patients feel about resident work hours, fatigue, and discontinuity of care.J Gen Intern Med.2008;23(5):623–628.
- ,,.A new doctor in the house: ethical issues in hospitalist systems.JAMA.2000;283(3):336–337.
- ,,,.A theoretical framework and competency‐based approach to improving handoffs.Qual Saf Health Care.2008;17(1):11–14.
- ,.Hindsight bias, outcome knowledge and adaptive learning.Qual Saf Health Care.2003;12(suppl 2):ii46–ii50.
- . Hawthorne and the Western Electric Company.The Social Problems of an Industrial Civilisation.London, UK:Routledge;1949.
- ,.A model for building a standardized hand‐off protocol.Jt Comm J Qual Patient Saf.2006;32(11):646–655.
Copyright © 2009 Society of Hospital Medicine