User login
Hospital Diabetes Care
Persons with diabetes have a greater risk of being hospitalized than do nondiabetic persons,1 and hospitalization was a major contributor to health care utilization and costs of patients with diabetes. In 1997, diabetes was the fourth most common comorbid condition in hospitalized patients nationwide. In 2001 in the United States, 562,000 hospital discharges listed diabetes as a principal diagnosis, and more than 4 million discharges listed diabetes in any diagnostic field.24 Nearly one third of diabetes patients may require 2 or more hospitalizations a year,5 and inpatient stays are the largest expense incurred by persons with this disease.6, 7 A substantial number of hospitalized persons are found to have unrecognized diabetes or to develop hyperglycemia during an inpatient stay.8, 9
The severity of hyperglycemia in the hospital has been linked to numerous adverse outcomes in various clinical situations, and recent studies have demonstrated the potential benefits of achieving good glucose control in the inpatient setting.10, 11 Moreover, specific inpatient‐directed interventions can improve the delivery of diabetes care.1216
Unlike the quality of outpatient diabetes care, which has been extensively profiled,1723 little is actually known about inpatient management. However, earlier reports suggested that hyperglycemia is frequently overlooked by health care personnel.8, 24 To develop intervention and educational programs will require insight into how diabetes is being addressed in the hospital. Thus, we undertook a retrospective chart review of inpatients with a discharge diagnosis of diabetes or hyperglycemia in order to assess whether these conditions were being documented and whether glucose management was being addressed.
METHODS
Setting
Our regional referral, academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented at this hospital, including renal, liver, and pancreas transplantation, a level‐2 trauma center, and an inpatient rehabilitation unit. Inpatient care is provided either by postgraduate trainees (residents) or through a separate faculty service; physician assistants and nurse‐practitioners also deliver care. Residents may be supervised by either hospitalist or nonhospitalist attendings. An electronic medical record links outpatient and inpatient records, radiology studies, and laboratory results.
Patient Selection
The study was approved by the Mayo Clinic Institutional Review Board. Patients discharged from our facility during 2003 with a diagnosis code from the International Classification of Diseases, 9th revision, Clinical Modification (ICD‐9‐CM) either for diabetes (ICD‐9‐CM code 250.0) or for hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic records. Data fields retrieved included patient age at admission, ethnicity/race, length of stay, total charges, and type of hospital service with primary responsibility for the patient's care. Because of the large number of available records, we randomly selected 5% of the total for chart review.20, 25, 26
Data Collection
Using an approach similar to that used by others,8 we reviewed admission notes, daily progress notes, and discharge summaries in order to establish whether the practitioner had recorded diabetes or hyperglycemia in the patient's chart. Subjective, objective, assessment, and plan components of notes were reviewed, and credit was given for having addressed diabetes or hyperglycemia if there was any documentation. For patients admitted for elective inpatient procedures, a preoperative outpatient evaluation conducted within 30 days of the hospitalization was counted as the admission note.
Practitioners typically make therapeutic decisions about hyperglycemia management of inpatients on the basis of daily bedside glucose measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. We determined whether bedside glucose levels were ordered and if so, whether they were then recorded in the daily progress notes. We determined the frequency of blood glucose measurements. Notes were examined to determine whether an assessment of hyperglycemia was made (defined as any comment in the progress note that addressed the severity of hyperglycemia or the adequacy of glucose control), and written orders were reviewed to establish any therapeutic changes. On completion of the chart reviews and entry of abstracted data into an electronic file, a link was made to the laboratory database to obtain information on bedside glucose values. We report data on notes written by the inpatient team with the principal caretaking responsibility for the patient (the primary service).
Data Analysis
Four primary outcome measures were of particular interest. First, we analyzed the percentage of patients who had diabetes or hyperglycemia documented in admission, daily progress, or discharge notes. Second, we determined the proportion of patients for whom bedside glucose measurements were ordered. Third, we calculated the percentage of patients with a written assessment of glycemic control. Finally, we examined the proportion of patients who had a change in therapy for treatment of hyperglycemia. Change in therapy was defined as any increase or decrease in the doses of an oral agent or insulin that occurred between admission day orders and the active orders on the day of discharge.
We determined the proportion of patients who had at least one hypoglycemic (glucose <70, <60, <50, <40 mg/dL) or hyperglycemic (>200, >250, >300, >350, >400 mg/dL) measurement documented by bedside monitoring. We also calculated the frequency of hypoglycemic and hyperglycemic values as the number of events per person per 100 measurements; as suggested by others,27 this approach to assessing glycemic control allows adjustment for different numbers of measurements across individuals and captures information on multiple episodes of hypo‐ or hyperglycemia in a single patient. All available bedside glucose values were averaged to determine the overall level of glucose control for the hospitalization and were divided into 3 intervals using cut points based on tertiles; the differences in the proportion of patients who had changes made in diabetes therapy was determined across tertiles using the 2 test. We determined the odds of changing therapy in the second and third tertiles of average bedside glucose relative to the first tertile. Differences in any continuous variables were evaluated using nonparametric methods (Mann‐Whitney test). Cases from all primary services were analyzed in aggregate.
RESULTS
General Patient Characteristics
Of all the patient hospitalization records for 2003, 1812 had a discharge diagnosis of diabetes or hyperglycemia. A random sample of 5% of these 1812 records yielded 90 records for chart review. The mean patient age was 68 years; 53% were male, and 90% were white.. Average length of stay was 4.8 days (Table 1). No significant differences in age, length of stay, sex, race, or source of admission (all P > .1) were detected between the 90 cases undergoing chart review and those cases that were not selected. On admission day, 63% of the patients were placed on insulin therapy, 17% on combination treatment of oral agents and insulin, and 7% on oral agents; the remaining 13% did not receive pharmacotherapy to treat their hyperglycemia. Thus, 80% were placed on insulin on the day they were admitted. By the day of discharge, 61% of the patients were on insulin therapy, either alone or in combination with oral agents. Of those on insulin therapy during their hospital stay, 35% were on a scheduled program of long‐ plus short‐acting insulin, and 65% were only on a sliding scale program.
| Characteristic | Value* |
|---|---|
| |
| Mean age (years) | 68 |
| Mean length of stay (days) | 4.8 |
| Men | 53 |
| White | 90 |
| Diabetes therapy at admission | |
| Insulin only | 63 |
| Oral agents only | 7 |
| Combination oral agents and insulin | 17 |
| Diet | 13 |
| Source of admission | |
| Physician office or clinic | 46 |
| Emergency room | 46 |
| Transfer | 8 |
| Primary service | |
| General medical | 41 |
| Surgical | 31 |
| Other | 28 |
| Teaching service | 48 |
Most patients were admitted through either an outpatient clinic (46%) or the emergency department (46%), with the remainder coming as transfers from other facilities (Table 1). Most inpatients were cared for by a general medical team (general internal or family medicine, 41%), whereas 31% were managed by one of the surgical specialties, and 28% were under the care of other specialties (eg, cardiology, transplantation, rehabilitation). Once hospitalized, most patients (94%) stayed on the original admitting service throughout their stay; 48% of patients were on a service staffed by a postgraduate trainee (Table 1). Two patients required a brief stay in the intensive care unit, but otherwise the sample was made up of noncritically ill patients.
Fifteen patients had their hemoglobin A1c measured in the hospital, with mean A1c of 7.0% 1.4%, whereas 57 patients had a documented preadmission hemoglobin A1c (average time before admission 29 weeks); their average A1c was 6.9% 1.2% (not shown).
Documentation of Diabetes
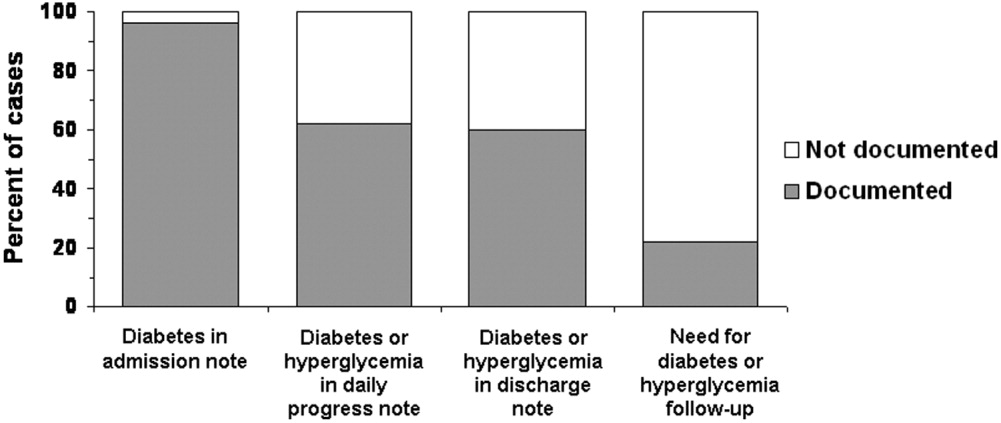
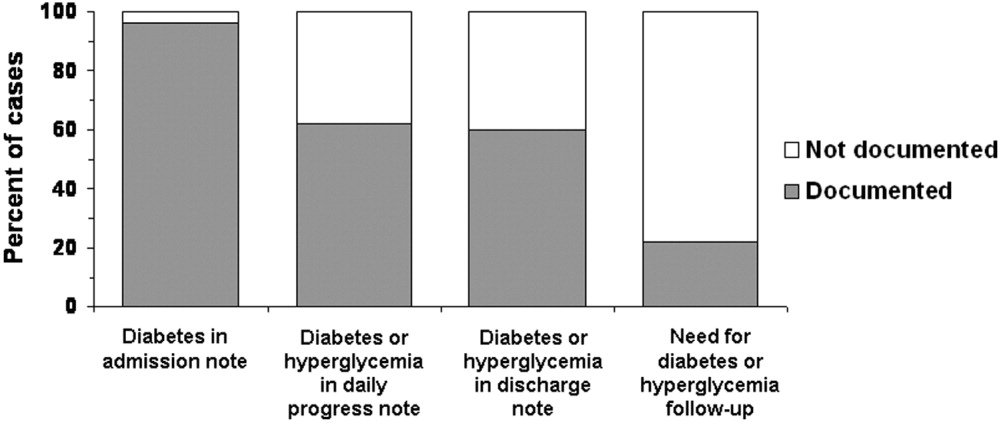
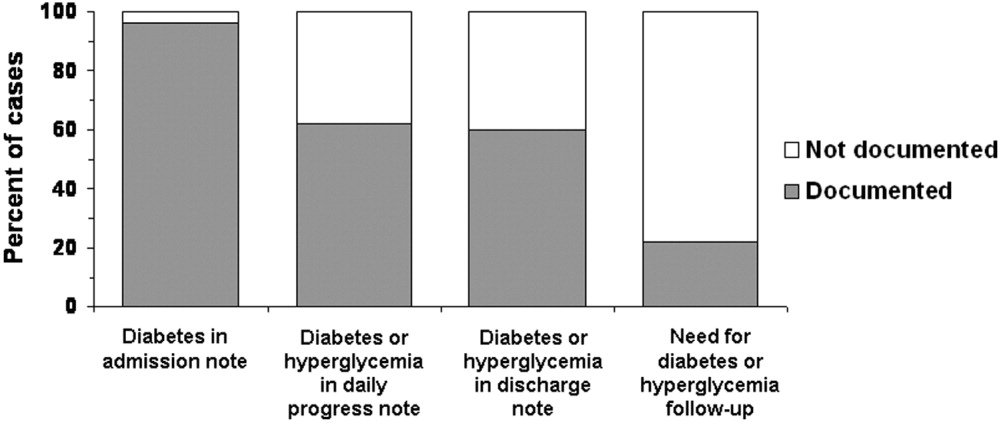
Of the 90 patients whose records were reviewed, 81 had preexisting diabetes, 3 had a diagnosis of metabolic syndrome or abnormal glucose tolerance, and 6 had hyperglycemia that developed during the admission hospitalization. When admission notes of persons with known diabetes or abnormal glucose tolerance were examined (Fig. 1), diabetes was documented in 96%. In the daily progress notes of the primary service, 62% of patients had diabetes documented at least once during their hospitalization, whereas the records of 38% had no mention of diabetes. When only those patients with known diabetes or evidence of inpatient hyperglycemia were considered, documentation of the diabetic condition was made in 60% of discharge summaries, and the need for follow‐up was noted in just 20% (Fig. 1).
Fifty‐seven percent (n = 51) of the 90 patients whose records were sampled had had some type of consultant involved with their care, but only 13% had had an endocrinology consultation. For 27 patients (30% of all 90 cases), diabetes or hyperglycemia was documented in a consultant's note; thus, there was evidence that the issue of glucose management was being addressed by someone other than a member of the primary team and that someone was not necessarily an endocrinologist. When excluding those patients whose consultant addressed diabetes or hyperglycemia, only 53% had documentation of the problems recorded in the daily progress notes (data not shown).
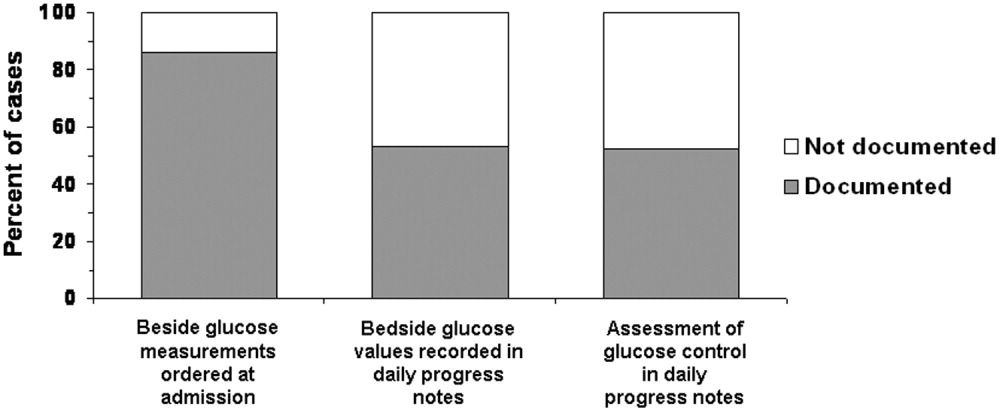
Recording and Assessment of Glucose Values
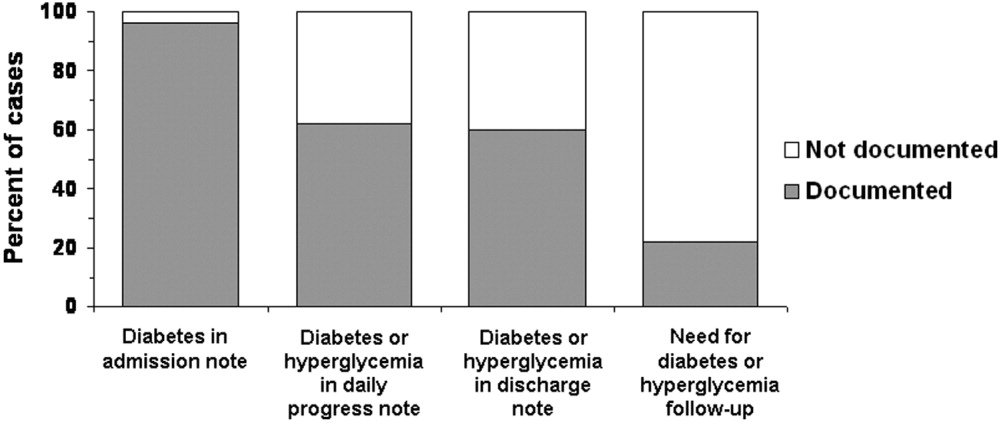
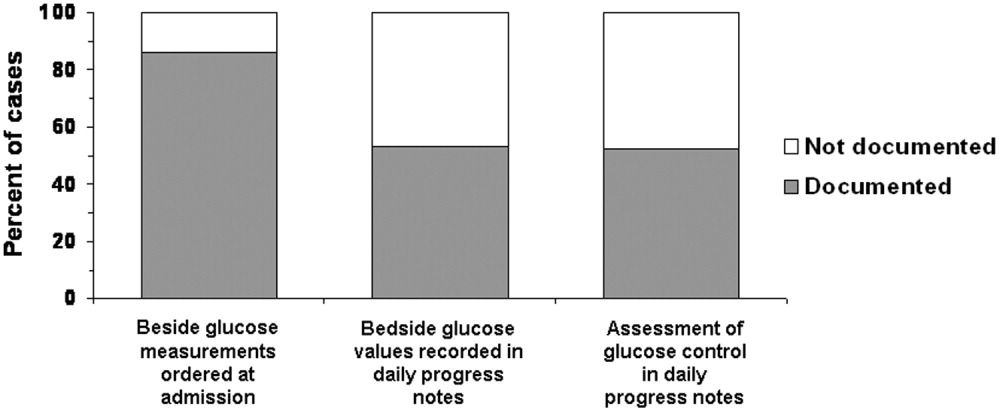
Most of the 90 patients whose records were reviewed (86%; n = 79) had documentation in physician orders for bedside glucose monitoring during their hospital stay (Fig. 2), and 53% had bedside glucose levels recorded in at least one daily progress note, whereas documentation was absent in 47%. A written assessment of glucose control was found in the records of 52% of the hospitalized patients; 48% lacked any evaluation of the severity of their hyperglycemia (Fig. 2). Excluding data listed from consultants, bedside glucose data was recorded for 53% of patients, and an assessment of glycemic control was made for 41%.
Glycemic Control
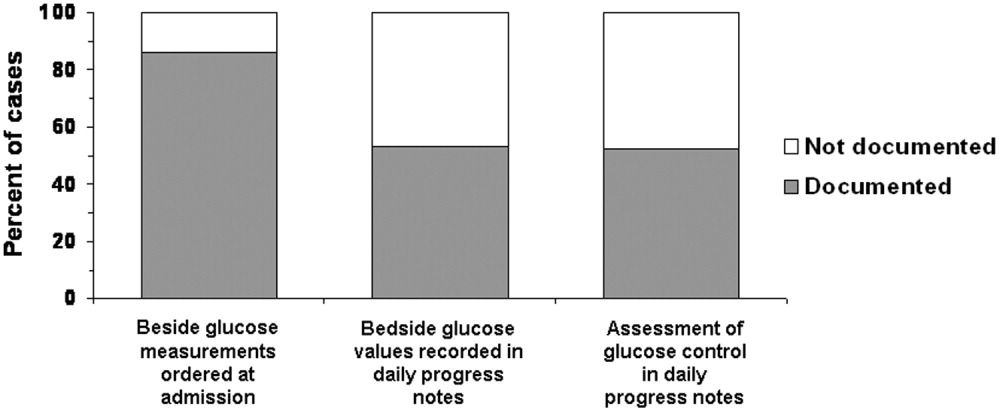
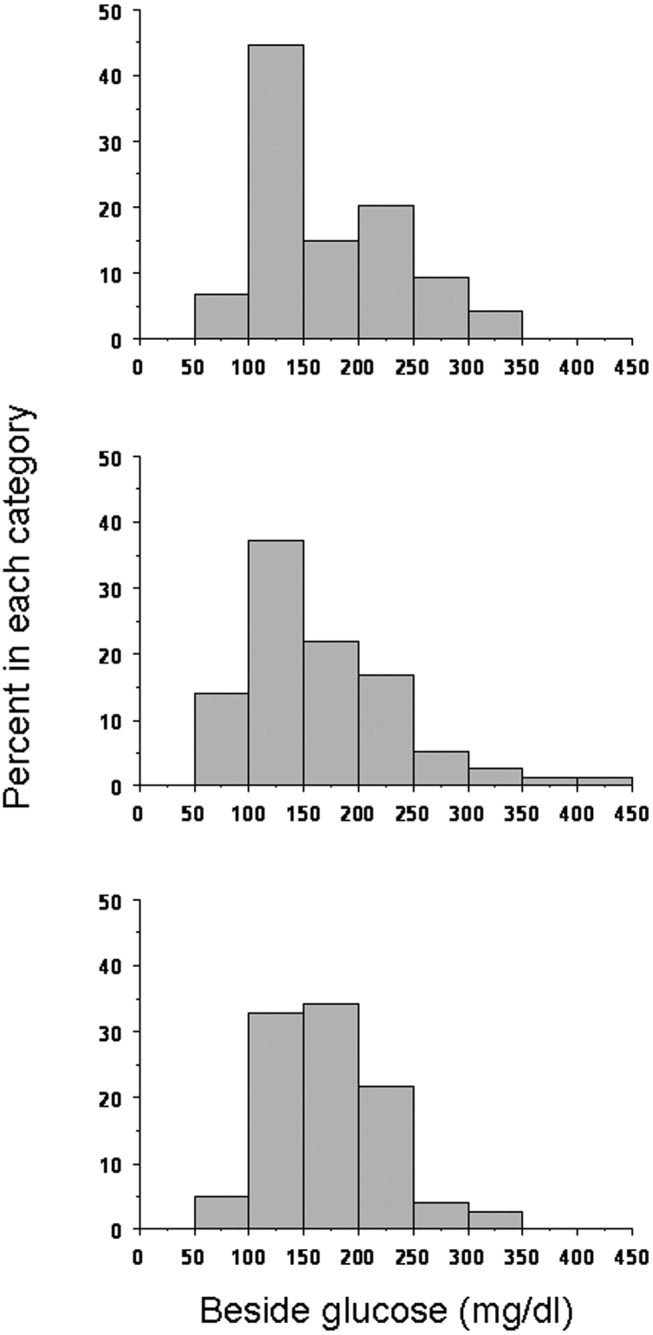
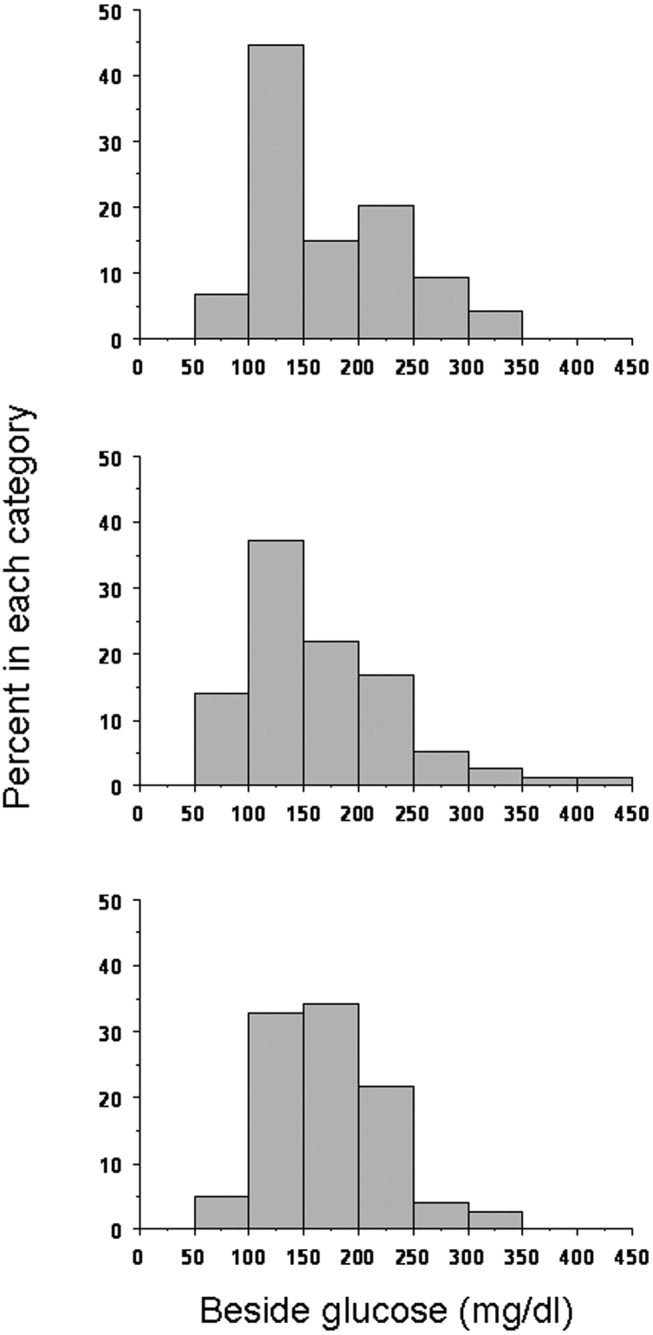
The average daily number of bedside glucose measurements was 4, while the daily frequency of blood glucose tests was only 1; an average of 10 bedside readings were obtained per patient. The mean bedside glucose value (averaged over the length of stay) was 170 mg/dL. At the time of admission, 33% of patients had a bedside glucose value >200 mg/dL (Fig 3, top panel), and 27% had a value >200 mg/dL before discharge (Fig 3, middle panel). Based on the bedside glucose averaged over the length of stay, 29% of patients had persistent hyperglycemia (Fig. 3, bottom panel).
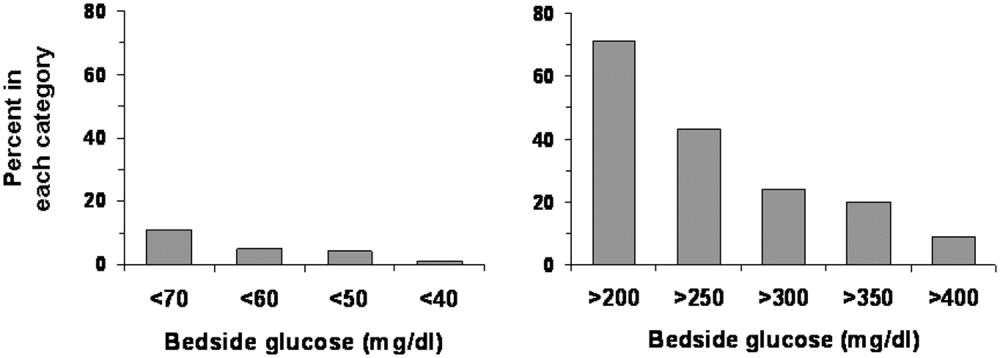
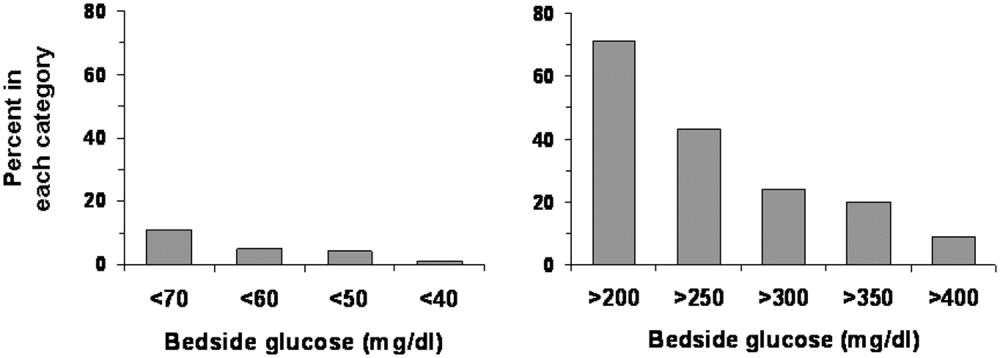
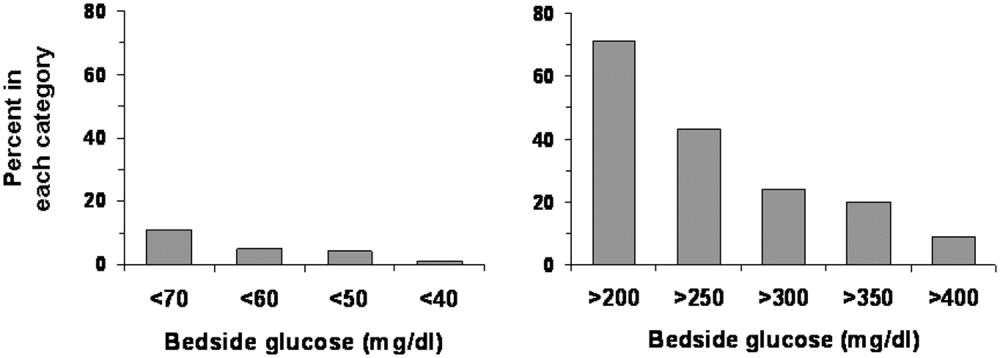
Hypoglycemia was rare. Only 11% of patients had at least one bedside measurement that was <70 mg/dL; 5% a measurement of <60 mg/dL, 4% a measurement of <50 mg/dL, and 1% a measurement of <40 mg/dL (Fig. 4). The frequency of values <70 mg/dL was 1.1 per person per 100 measurements; of values <60 mg/dL, 0.66; of values <50 mg/dL, 0.18; and of values <40 mg/dL, 0.08. In contrast, hyperglycemia was common: 71% of patients had at least one value >200 mg/dL; 43% at least one value >250 mg/dLl 24% at least one value >300 mg/dL; 20% at least one value >350 mg/dL; and 9% at least one value >400 mg/dL (Fig. 4). The frequency of hyperglycemic events was 28.2 per person per 100 measurements for values >200 mg/dL, 11.2 for values >250 mg/dL, 5.3 for values >300 mg/dL, 2.4 for values >350 mg/dL, and 1.1 for values >400 mg/dL.
Changes in Therapy
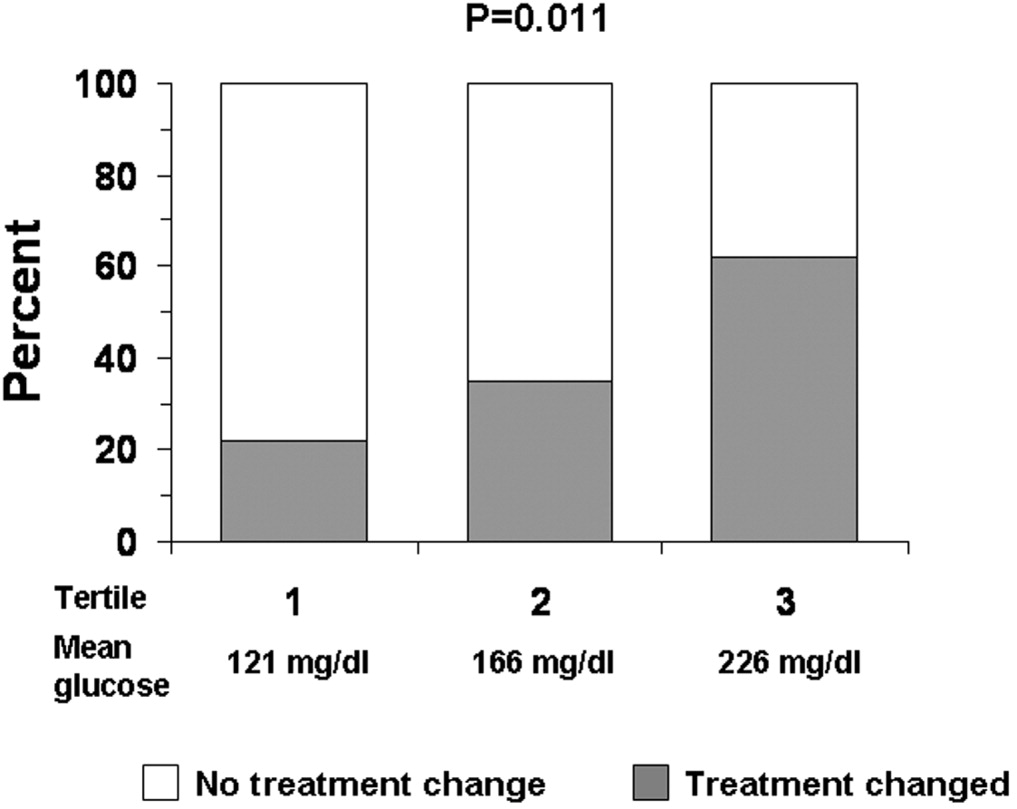
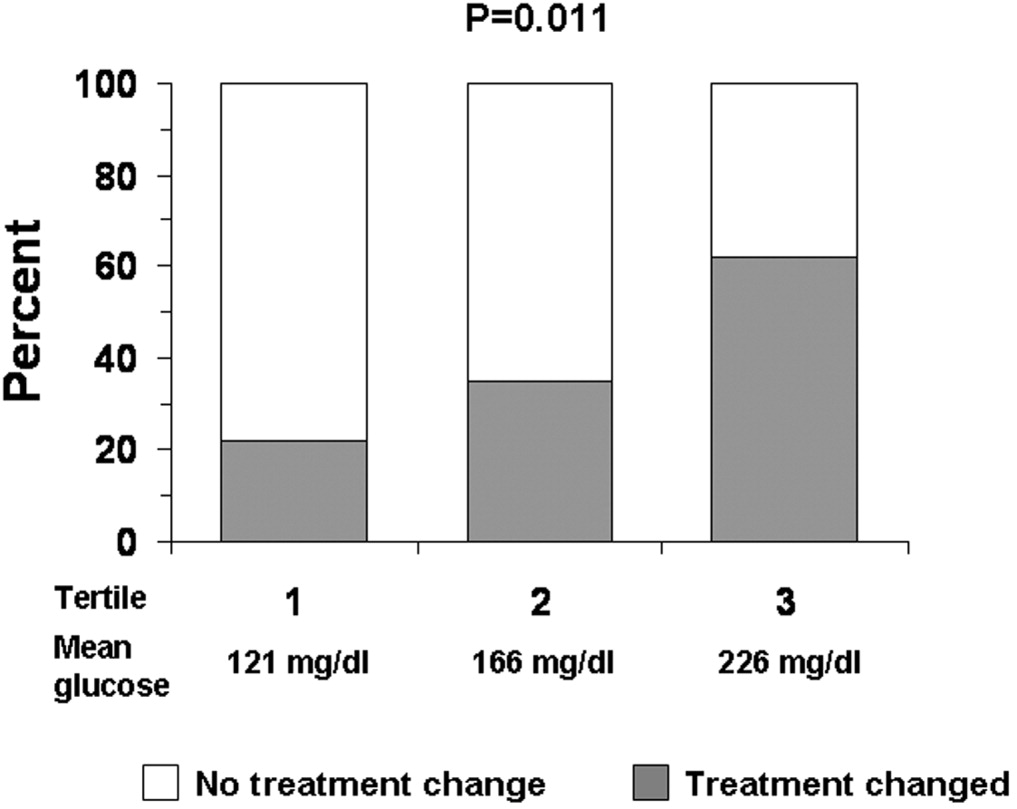
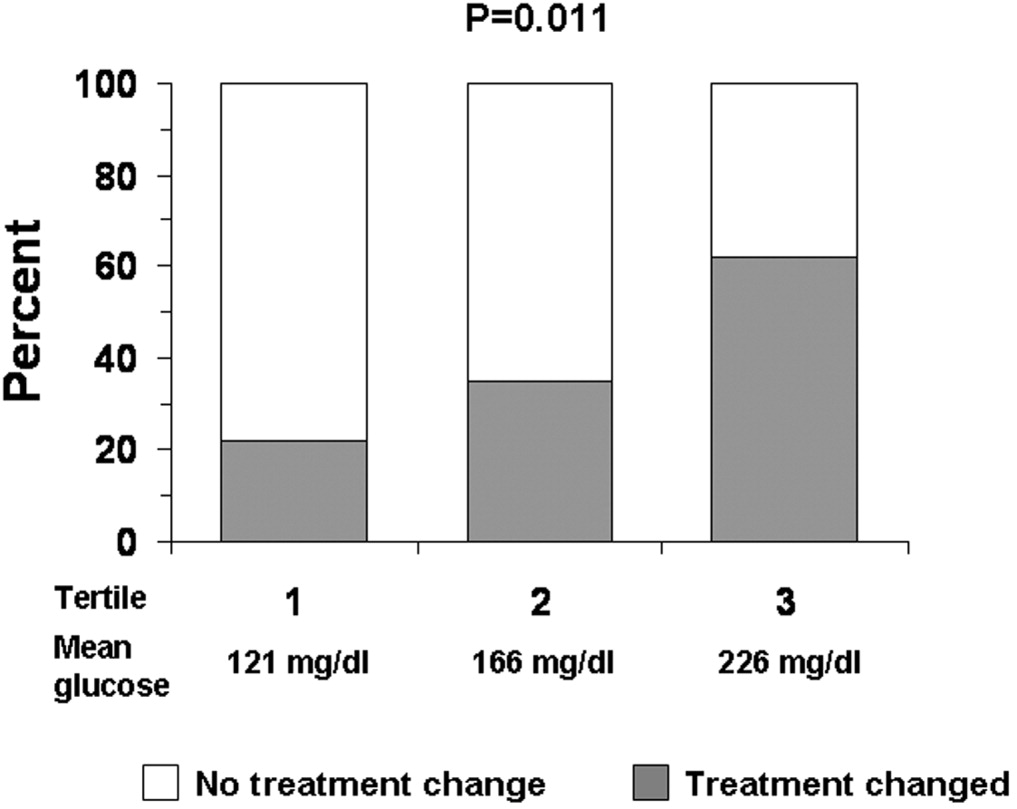
Overall, changes were made in the hyperglycemia therapy of only 34% of patients. Treatment was changed for 50% of patients who had at least one glucose reading >200 mg/dL, and 89% of patients who had at least one glucose reading <70 mg/dL. Figure 5 shows whether changes in treatment occurred by tertiles of average bedside glucose. The percentage of patients with a change in therapy increased with worse hyperglycemia, although 32% in the third tertile still had not had a change in treatment. The odds of those in the second tertile having a change in therapy (compared with those in the first tertile) were 1.9 (95% confidence interval 0.556.25, P = .32), but were 5.6 (95% confidence interval 1.6818.7, P = .005) for patients in the third tertile. The frequency of glucose values <70 mg/dL was 1.8 per person per 100 measurements for patients in the first tertile, 1.1 for patients in the second tertile, but only 0.29 per person per 100 measurements for patients in the third tertile. The average number of glucose measurements >200 mg/dL per person was 2.9 per 100 measurements for patients in the first tertile, 22.7 for patients in the second tertile, and 60.0 for patients in the third tertile (not shown).
DISCUSSION
Just as clinical trials in the outpatient setting have demonstrated the benefits of good glycemic control,2830 recent studies have also suggested that treatment of hyperglycemia during hospitalization can improve outcomes.10, 11 Consequently, there has been increased attention to the management of glucose in the hospital, with recognition of the need for inpatient‐specific standards for diabetes care.10, 11, 31 Optimization of management and of education about diabetes and hyperglycemia in the hospital requires better understanding of current care practices in order to determine where to direct interventions.
Nearly all the 90 patients whose records we reviewed had preexisting diabetes or a known potential glucose abnormality that was documented either at the time of, or just prior to, hospital admission. The observation that most patients had orders for bedside glucose monitoring also indicated that practitioners were aware of the diagnosis when the patient was admitted. Although clinicians seemed to be aware of the potential problem of glucoseand the majority of clinicians did some trackinga substantial number of hospitalizations (nearly 40%) had no documentation of diabetes or hyperglycemia after admission. If diabetes was not the principal reason for hospitalization, it is possible that the primary team did not focus on managing hyperglycemia. Nonetheless, the hospital encounter does represent an opportunity to address glucose management and perhaps improve care and outcomes, even if the patient was admitted for an unrelated condition.32 Because the average length of stay was almost 5 days, there should have been sufficient time to address diabetes in most patients.
Although most patients had the condition of their diabetes documented in their discharge notes, a substantial proportion of the discharge notes did not mention an outpatient plan to follow up on the diabetes or hyperglycemia. A recent study suggested that direct referral for outpatient diabetes services increased the chances of patient follow‐up.33 Educating practitioners about the need to emphasize to patients the importance of diabetes postdischarge care is a program that could be developed and implemented in the hospital setting.
Although bedside glucose monitoring was appropriately ordered in most instances, the actual recording of values and the assessment of glucose control were documented in the records of only about half the patients during their hospitalizations. Moreover, even among patients who had high bedside glucose levels, changes in therapy often did not occur. Clinician concern about inducing hypoglycemia in hospitalized patients has been cited as a factor limiting the intensification of treatment for diabetes.34 The frequency in our facility of documented low blood glucose values was small, although there may have been unrecognized episodes. However, missed events were probably unusual, given the daily average of 4 bedside glucose measurements per patient, ongoing nursing staff contact with patients, and a formal policy to document and treat hypoglycemia. We found that hyperglycemia was far more common than hypoglycemia and that there were likely many opportunities to control blood glucose more rigorously.
Practitioners appeared to be responding to hypoglycemia, as a large proportion of the patients with a glucose reading of <70 mg/dL had a change in therapy. However, the response to hyperglycemia was delayedthe odds of therapy being changed were significant only for patients whose glucose levels were in the third tertile. Despite evidence of hyperglycemia and the low frequency of hypoglycemia of those whose glucose levels were in the second and third tertiles, a substantial proportion of patients did not have their therapy changed. Combined with the observation that glucose data and diabetes were often not documented, our data suggest that there may be a problem of clinical inertia in the inpatient setting. Clinical inertia has been defined as not initiating or intensifying therapy when doing so is indicated.35, 36 Other reports have also documented clinical inertia in the outpatient environment.23, 3741 Overcoming clinical inertia, at least in regard to diabetes management, can improve glycemic control in patients.35 To improve the management of hyperglycemia in the hospital, educational interventions must be developed to teach health care practitioners effective strategies for glucose reduction. We did not quantify the changes in therapy (eg, how much insulin was changed or in what direction), only whether a change had been made. The observation that the proportion of cases on insulin at discharge was less than on admission day suggests that there may actually have been deintensification of therapy taking placesome of the cases in which therapy was changed, therefore, likely included instances of negative therapeutic momentum despite evidence of hyperglycemia. The control of inpatient hyperglycemia will likely require frequent changes in therapy, as it does in the outpatient setting, and detailed information about treatment strategies actually employed will be necessary to design educational programs.
One limitation of our analysis was that the study was retrospective, which did not allow assessment of the reasons underlying the behavior of the clinicians, such as why they did not document diabetes or change therapy. We selected a 5% sample for our study as per common methods.20, 25, 26 Thus, although the 90 patients making up the sample were randomly selected and were not different demographically from the larger population of patients admitted with diabetes, the number of cases we reviewed was small compared with the actual number of discharged patients with diabetes. Cases were diagnosed by diagnosis codes; therefore, it is likely that some diabetes cases were missed, and other patients with hyperglycemia may not have had the diagnosis even documented.8, 24 Our study design and sample size precluded a comparison of outcomes between cases with in which a consultant was involved with those in which a consultant was not involved or a comparison of cases according to type of consultant involved.1216 Finally, our study focused on noncritically ill patients; thus, our findings cannot be generalized to care provided in the intensive care unit.
There are no definitive guidelines on what method (ie, blood or bedside glucose) should be used to evaluate glycemic control in the hospital. The methods we used here can serve as means to benchmark and track improvement in glycemic control. The observations that most patients had bedside glucose monitoring ordered and that the frequency of these measurements was high compared with the frequency of actual blood glucose assessments support the idea that practitioners favored this method to evaluate the level of glycemic control in the hospital. In practice, it is bedside glucose evaluation that clinicians use to make decisions about day‐to‐day treatment of hyperglycemia. In our facility, the method for bedside glucose monitoring is standardized and is part of a quality assurance program. Moreover, the high average frequency of bedside blood glucose determination increased the chance of detecting hyper‐ and hypoglycemic events.
Current guidelines provide suggestions about target pre‐ and postprandial glucose levels for noncritically ill patients.11 However, these targets are not universally recognized.42 For instance, the Institutes for Healthcare Improvement's Prevent Surgical Site Infections initiative defines a glucose level of <200 mg/dL as its target perioperative glucose control level.43 In practice, it can be difficult to assess glucose control in terms of pre‐ and postprandial categories. Although bedside glucose monitoring in our facility is typically ordered before meals and at bedtime, in many cases prolonged periods of patient fasting, disrupted meal schedules, mismatching insulin with meals, and use of continuous parental and enteral nutritional support all make it difficult to assess pre‐ and postprandial glycemic control retrospectively. Hence, we used as our measures the value of the bedside glucose averaged over the length of the hospital stay and the number of hyper‐ and hypoglycemic events.
In general, our study was hampered by a lack of hospital‐specific process measures to evaluate the quality of inpatient diabetes care. Process measures such as the frequency of hemoglobin A1c monitoring or performance of ophthalmologic examinations,1723 which are commonly used to assess quality of diabetes care in the outpatient arena, may not be optimal variables for evaluating care in the hospital. New methods to guide efforts to improve the quality of inpatient management of diabetes and hyperglycemia are needed.
Despite these limitations, our analysis was helpful in providing direction about how to enhance the care of hospitalized patients with hyperglycemia or known diabetes. Constructing institution‐specific management guidelines for the care of inpatient diabetes and hyperglycemia would provide a yardstick against which to measure the care provided by both the hospital and the individual clinician. Educational programs can be developed to increase awareness among practitioners of the importance of inpatient glucose control and of the need to improve ongoing documentation of the problem. Exploring practitioner barriers to treatment of inpatient hyperglycemia should be an essential component of this educational process. Finally, consensus strategies on when to initiate and change therapy should be designed so that hyperglycemia in the hospital can be managed more effectively. All these areas must be addressed to assure delivery of the highest‐quality inpatient care to patients with diabetes.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America: National Diabetes Data Group.2nd ed.Bethesda (MD):National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;1995:553–563.
- .Hospitalization in the United States, 1997: HCUP fact book no. 1: diagnosis, charges, length of stay, insurance coverage, discharge status, inhospital deaths.Rockville (MD):Agency for Healthcare Research and Quality;2000.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmfirst/table1.htm. Accessed: June 2,2005.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed: June 2,2005.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,,.Excess costs of medical care for patients with diabetes in a managed care population.Diabetes Care.1997;20:1396–1402.
- ,,,American Diabetes Association.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,,American Diabetes Association Diabetes in Hospitals Writing Committee, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591. Erratum in: Diabetes Care. 2004;27:856 and Diabetes Care. 2004;27:1255.
- ,,,,,,American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,,.Effect of physician specialty on outcomes in diabetic ketoacidosis.Diabetes Care.1999;22:1790–1795.
- ,,,.Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes.Am J Med.1995;99:22–28.
- ,,.Effects of an intervention by a diabetes team in hospitalized patients with diabetes.Diabetes Care.1997;20:1553–1555.
- ,.Nursing case management: an innovative model of care for hospitalized patients with diabetes.Diabetes Educ.1993;19:517–521.
- ,,,,.Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial.Diabet Med.2001;18:301–307.
- ,,,,,.Variation in office‐based quality. A claims‐based profile of care provided to Medicare patients with diabetes.JAMA.1995;273:1503–1508.
- ,,,,,, et al.Outpatient management of diabetes mellitus in five Arizona Medicare managed care plans.Am J Med Qual.1996;11:87–93.
- ,,,.Quality of outpatient care provided to diabetic patients: a health maintenance organization experience.Diabetes Care.1996;19:601–6.
- United States General Accounting Office: report to the Chairman, Subcommittee on Health and Environment, Committee on Commerce, House of Representatives.Medicare: most beneficiaries with diabetes do not receive recommended monitoring services. GAO/HEHS‐97–48.1997.
- ,,,,.Care of patients with type II diabetes: a study of family physicians' compliance with clinical practice guidelines.J Fam Pract.1997;44:374–381.
- ,,,,,.A diabetes report card for the United States: quality of care in the 1990s.Ann Intern Med.2002;136:565–574.
- ,,,University HealthSystem Consortium (UHC) Diabetes Benchmarking Project Team.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,,.An audit of the management and outcome of hospital inpatients with diabetes: resource planning implications for the diabetes care team.Diabet Med.1992;9:753–755.
- .Improving outcomes in public health practice: strategy and methods.Gaithersburg (MD):Aspen Publishers;1997:175–213.
- ,,,,,.Outpatient diabetes management of Medicare beneficiaries in four Mississippi fee‐for‐service primary care clinics.J Miss State Med Assoc.1999;40:8–13.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- The Diabetes Control and Complications Trial Research Group.The effect of intensive treatment of diabetes on the development and progression of long‐term complications in insulin‐dependent diabetes mellitus.N Engl J Med.1993;329:977–986.
- UK Prospective Diabetes Study (UKPDS) Group.Intensive blood‐glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33).Lancet.1998;352:837–53. Erratum in: Lancet. 1999;354:602.
- UK Prospective Diabetes Study (UKPDS) Group.Effect of intensive blood‐glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34).Lancet.1998;352:854–65. Erratum in: Lancet. 1998;352:1557.
- ,,.Current standards of care for inpatient glycemic management and metabolic control: is it time for definite standards and targets?Endocr Pract.2004;10(Suppl 2):10–12.
- ,.Windows of opportunity to improve diabetes care when patients with diabetes are hospitalized for other conditions.Diabetes Care.2001;24:1371–1376.
- ,,, et al.Inpatient to outpatient transfer of care in urban patients with diabetes: patterns and determinants of immediate postdischarge follow‐up.Arch Intern Med.2004;164:447–453.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–1500.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- .Management of older hypertensive patients: is there a difference in approach?J Clin Hypertens (Greenwich).2003;5(Suppl 4):11–16.
- ,,, et al.Narrowing the gap in hypertension: effectiveness of a complex antihypertensive program in the elderly.Dis Manag.2004;7:235–243.
- ,,, et al.Clinical inertia in the management of Type 2 diabetes metabolic risk factors.Diabet Med.2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med.2003;163:2677–2678.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available from: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed June 2,2005.
Persons with diabetes have a greater risk of being hospitalized than do nondiabetic persons,1 and hospitalization was a major contributor to health care utilization and costs of patients with diabetes. In 1997, diabetes was the fourth most common comorbid condition in hospitalized patients nationwide. In 2001 in the United States, 562,000 hospital discharges listed diabetes as a principal diagnosis, and more than 4 million discharges listed diabetes in any diagnostic field.24 Nearly one third of diabetes patients may require 2 or more hospitalizations a year,5 and inpatient stays are the largest expense incurred by persons with this disease.6, 7 A substantial number of hospitalized persons are found to have unrecognized diabetes or to develop hyperglycemia during an inpatient stay.8, 9
The severity of hyperglycemia in the hospital has been linked to numerous adverse outcomes in various clinical situations, and recent studies have demonstrated the potential benefits of achieving good glucose control in the inpatient setting.10, 11 Moreover, specific inpatient‐directed interventions can improve the delivery of diabetes care.1216
Unlike the quality of outpatient diabetes care, which has been extensively profiled,1723 little is actually known about inpatient management. However, earlier reports suggested that hyperglycemia is frequently overlooked by health care personnel.8, 24 To develop intervention and educational programs will require insight into how diabetes is being addressed in the hospital. Thus, we undertook a retrospective chart review of inpatients with a discharge diagnosis of diabetes or hyperglycemia in order to assess whether these conditions were being documented and whether glucose management was being addressed.
METHODS
Setting
Our regional referral, academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented at this hospital, including renal, liver, and pancreas transplantation, a level‐2 trauma center, and an inpatient rehabilitation unit. Inpatient care is provided either by postgraduate trainees (residents) or through a separate faculty service; physician assistants and nurse‐practitioners also deliver care. Residents may be supervised by either hospitalist or nonhospitalist attendings. An electronic medical record links outpatient and inpatient records, radiology studies, and laboratory results.
Patient Selection
The study was approved by the Mayo Clinic Institutional Review Board. Patients discharged from our facility during 2003 with a diagnosis code from the International Classification of Diseases, 9th revision, Clinical Modification (ICD‐9‐CM) either for diabetes (ICD‐9‐CM code 250.0) or for hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic records. Data fields retrieved included patient age at admission, ethnicity/race, length of stay, total charges, and type of hospital service with primary responsibility for the patient's care. Because of the large number of available records, we randomly selected 5% of the total for chart review.20, 25, 26
Data Collection
Using an approach similar to that used by others,8 we reviewed admission notes, daily progress notes, and discharge summaries in order to establish whether the practitioner had recorded diabetes or hyperglycemia in the patient's chart. Subjective, objective, assessment, and plan components of notes were reviewed, and credit was given for having addressed diabetes or hyperglycemia if there was any documentation. For patients admitted for elective inpatient procedures, a preoperative outpatient evaluation conducted within 30 days of the hospitalization was counted as the admission note.
Practitioners typically make therapeutic decisions about hyperglycemia management of inpatients on the basis of daily bedside glucose measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. We determined whether bedside glucose levels were ordered and if so, whether they were then recorded in the daily progress notes. We determined the frequency of blood glucose measurements. Notes were examined to determine whether an assessment of hyperglycemia was made (defined as any comment in the progress note that addressed the severity of hyperglycemia or the adequacy of glucose control), and written orders were reviewed to establish any therapeutic changes. On completion of the chart reviews and entry of abstracted data into an electronic file, a link was made to the laboratory database to obtain information on bedside glucose values. We report data on notes written by the inpatient team with the principal caretaking responsibility for the patient (the primary service).
Data Analysis
Four primary outcome measures were of particular interest. First, we analyzed the percentage of patients who had diabetes or hyperglycemia documented in admission, daily progress, or discharge notes. Second, we determined the proportion of patients for whom bedside glucose measurements were ordered. Third, we calculated the percentage of patients with a written assessment of glycemic control. Finally, we examined the proportion of patients who had a change in therapy for treatment of hyperglycemia. Change in therapy was defined as any increase or decrease in the doses of an oral agent or insulin that occurred between admission day orders and the active orders on the day of discharge.
We determined the proportion of patients who had at least one hypoglycemic (glucose <70, <60, <50, <40 mg/dL) or hyperglycemic (>200, >250, >300, >350, >400 mg/dL) measurement documented by bedside monitoring. We also calculated the frequency of hypoglycemic and hyperglycemic values as the number of events per person per 100 measurements; as suggested by others,27 this approach to assessing glycemic control allows adjustment for different numbers of measurements across individuals and captures information on multiple episodes of hypo‐ or hyperglycemia in a single patient. All available bedside glucose values were averaged to determine the overall level of glucose control for the hospitalization and were divided into 3 intervals using cut points based on tertiles; the differences in the proportion of patients who had changes made in diabetes therapy was determined across tertiles using the 2 test. We determined the odds of changing therapy in the second and third tertiles of average bedside glucose relative to the first tertile. Differences in any continuous variables were evaluated using nonparametric methods (Mann‐Whitney test). Cases from all primary services were analyzed in aggregate.
RESULTS
General Patient Characteristics
Of all the patient hospitalization records for 2003, 1812 had a discharge diagnosis of diabetes or hyperglycemia. A random sample of 5% of these 1812 records yielded 90 records for chart review. The mean patient age was 68 years; 53% were male, and 90% were white.. Average length of stay was 4.8 days (Table 1). No significant differences in age, length of stay, sex, race, or source of admission (all P > .1) were detected between the 90 cases undergoing chart review and those cases that were not selected. On admission day, 63% of the patients were placed on insulin therapy, 17% on combination treatment of oral agents and insulin, and 7% on oral agents; the remaining 13% did not receive pharmacotherapy to treat their hyperglycemia. Thus, 80% were placed on insulin on the day they were admitted. By the day of discharge, 61% of the patients were on insulin therapy, either alone or in combination with oral agents. Of those on insulin therapy during their hospital stay, 35% were on a scheduled program of long‐ plus short‐acting insulin, and 65% were only on a sliding scale program.
| Characteristic | Value* |
|---|---|
| |
| Mean age (years) | 68 |
| Mean length of stay (days) | 4.8 |
| Men | 53 |
| White | 90 |
| Diabetes therapy at admission | |
| Insulin only | 63 |
| Oral agents only | 7 |
| Combination oral agents and insulin | 17 |
| Diet | 13 |
| Source of admission | |
| Physician office or clinic | 46 |
| Emergency room | 46 |
| Transfer | 8 |
| Primary service | |
| General medical | 41 |
| Surgical | 31 |
| Other | 28 |
| Teaching service | 48 |
Most patients were admitted through either an outpatient clinic (46%) or the emergency department (46%), with the remainder coming as transfers from other facilities (Table 1). Most inpatients were cared for by a general medical team (general internal or family medicine, 41%), whereas 31% were managed by one of the surgical specialties, and 28% were under the care of other specialties (eg, cardiology, transplantation, rehabilitation). Once hospitalized, most patients (94%) stayed on the original admitting service throughout their stay; 48% of patients were on a service staffed by a postgraduate trainee (Table 1). Two patients required a brief stay in the intensive care unit, but otherwise the sample was made up of noncritically ill patients.
Fifteen patients had their hemoglobin A1c measured in the hospital, with mean A1c of 7.0% 1.4%, whereas 57 patients had a documented preadmission hemoglobin A1c (average time before admission 29 weeks); their average A1c was 6.9% 1.2% (not shown).
Documentation of Diabetes
Of the 90 patients whose records were reviewed, 81 had preexisting diabetes, 3 had a diagnosis of metabolic syndrome or abnormal glucose tolerance, and 6 had hyperglycemia that developed during the admission hospitalization. When admission notes of persons with known diabetes or abnormal glucose tolerance were examined (Fig. 1), diabetes was documented in 96%. In the daily progress notes of the primary service, 62% of patients had diabetes documented at least once during their hospitalization, whereas the records of 38% had no mention of diabetes. When only those patients with known diabetes or evidence of inpatient hyperglycemia were considered, documentation of the diabetic condition was made in 60% of discharge summaries, and the need for follow‐up was noted in just 20% (Fig. 1).
Fifty‐seven percent (n = 51) of the 90 patients whose records were sampled had had some type of consultant involved with their care, but only 13% had had an endocrinology consultation. For 27 patients (30% of all 90 cases), diabetes or hyperglycemia was documented in a consultant's note; thus, there was evidence that the issue of glucose management was being addressed by someone other than a member of the primary team and that someone was not necessarily an endocrinologist. When excluding those patients whose consultant addressed diabetes or hyperglycemia, only 53% had documentation of the problems recorded in the daily progress notes (data not shown).
Recording and Assessment of Glucose Values
Most of the 90 patients whose records were reviewed (86%; n = 79) had documentation in physician orders for bedside glucose monitoring during their hospital stay (Fig. 2), and 53% had bedside glucose levels recorded in at least one daily progress note, whereas documentation was absent in 47%. A written assessment of glucose control was found in the records of 52% of the hospitalized patients; 48% lacked any evaluation of the severity of their hyperglycemia (Fig. 2). Excluding data listed from consultants, bedside glucose data was recorded for 53% of patients, and an assessment of glycemic control was made for 41%.
Glycemic Control
The average daily number of bedside glucose measurements was 4, while the daily frequency of blood glucose tests was only 1; an average of 10 bedside readings were obtained per patient. The mean bedside glucose value (averaged over the length of stay) was 170 mg/dL. At the time of admission, 33% of patients had a bedside glucose value >200 mg/dL (Fig 3, top panel), and 27% had a value >200 mg/dL before discharge (Fig 3, middle panel). Based on the bedside glucose averaged over the length of stay, 29% of patients had persistent hyperglycemia (Fig. 3, bottom panel).
Hypoglycemia was rare. Only 11% of patients had at least one bedside measurement that was <70 mg/dL; 5% a measurement of <60 mg/dL, 4% a measurement of <50 mg/dL, and 1% a measurement of <40 mg/dL (Fig. 4). The frequency of values <70 mg/dL was 1.1 per person per 100 measurements; of values <60 mg/dL, 0.66; of values <50 mg/dL, 0.18; and of values <40 mg/dL, 0.08. In contrast, hyperglycemia was common: 71% of patients had at least one value >200 mg/dL; 43% at least one value >250 mg/dLl 24% at least one value >300 mg/dL; 20% at least one value >350 mg/dL; and 9% at least one value >400 mg/dL (Fig. 4). The frequency of hyperglycemic events was 28.2 per person per 100 measurements for values >200 mg/dL, 11.2 for values >250 mg/dL, 5.3 for values >300 mg/dL, 2.4 for values >350 mg/dL, and 1.1 for values >400 mg/dL.
Changes in Therapy
Overall, changes were made in the hyperglycemia therapy of only 34% of patients. Treatment was changed for 50% of patients who had at least one glucose reading >200 mg/dL, and 89% of patients who had at least one glucose reading <70 mg/dL. Figure 5 shows whether changes in treatment occurred by tertiles of average bedside glucose. The percentage of patients with a change in therapy increased with worse hyperglycemia, although 32% in the third tertile still had not had a change in treatment. The odds of those in the second tertile having a change in therapy (compared with those in the first tertile) were 1.9 (95% confidence interval 0.556.25, P = .32), but were 5.6 (95% confidence interval 1.6818.7, P = .005) for patients in the third tertile. The frequency of glucose values <70 mg/dL was 1.8 per person per 100 measurements for patients in the first tertile, 1.1 for patients in the second tertile, but only 0.29 per person per 100 measurements for patients in the third tertile. The average number of glucose measurements >200 mg/dL per person was 2.9 per 100 measurements for patients in the first tertile, 22.7 for patients in the second tertile, and 60.0 for patients in the third tertile (not shown).
DISCUSSION
Just as clinical trials in the outpatient setting have demonstrated the benefits of good glycemic control,2830 recent studies have also suggested that treatment of hyperglycemia during hospitalization can improve outcomes.10, 11 Consequently, there has been increased attention to the management of glucose in the hospital, with recognition of the need for inpatient‐specific standards for diabetes care.10, 11, 31 Optimization of management and of education about diabetes and hyperglycemia in the hospital requires better understanding of current care practices in order to determine where to direct interventions.
Nearly all the 90 patients whose records we reviewed had preexisting diabetes or a known potential glucose abnormality that was documented either at the time of, or just prior to, hospital admission. The observation that most patients had orders for bedside glucose monitoring also indicated that practitioners were aware of the diagnosis when the patient was admitted. Although clinicians seemed to be aware of the potential problem of glucoseand the majority of clinicians did some trackinga substantial number of hospitalizations (nearly 40%) had no documentation of diabetes or hyperglycemia after admission. If diabetes was not the principal reason for hospitalization, it is possible that the primary team did not focus on managing hyperglycemia. Nonetheless, the hospital encounter does represent an opportunity to address glucose management and perhaps improve care and outcomes, even if the patient was admitted for an unrelated condition.32 Because the average length of stay was almost 5 days, there should have been sufficient time to address diabetes in most patients.
Although most patients had the condition of their diabetes documented in their discharge notes, a substantial proportion of the discharge notes did not mention an outpatient plan to follow up on the diabetes or hyperglycemia. A recent study suggested that direct referral for outpatient diabetes services increased the chances of patient follow‐up.33 Educating practitioners about the need to emphasize to patients the importance of diabetes postdischarge care is a program that could be developed and implemented in the hospital setting.
Although bedside glucose monitoring was appropriately ordered in most instances, the actual recording of values and the assessment of glucose control were documented in the records of only about half the patients during their hospitalizations. Moreover, even among patients who had high bedside glucose levels, changes in therapy often did not occur. Clinician concern about inducing hypoglycemia in hospitalized patients has been cited as a factor limiting the intensification of treatment for diabetes.34 The frequency in our facility of documented low blood glucose values was small, although there may have been unrecognized episodes. However, missed events were probably unusual, given the daily average of 4 bedside glucose measurements per patient, ongoing nursing staff contact with patients, and a formal policy to document and treat hypoglycemia. We found that hyperglycemia was far more common than hypoglycemia and that there were likely many opportunities to control blood glucose more rigorously.
Practitioners appeared to be responding to hypoglycemia, as a large proportion of the patients with a glucose reading of <70 mg/dL had a change in therapy. However, the response to hyperglycemia was delayedthe odds of therapy being changed were significant only for patients whose glucose levels were in the third tertile. Despite evidence of hyperglycemia and the low frequency of hypoglycemia of those whose glucose levels were in the second and third tertiles, a substantial proportion of patients did not have their therapy changed. Combined with the observation that glucose data and diabetes were often not documented, our data suggest that there may be a problem of clinical inertia in the inpatient setting. Clinical inertia has been defined as not initiating or intensifying therapy when doing so is indicated.35, 36 Other reports have also documented clinical inertia in the outpatient environment.23, 3741 Overcoming clinical inertia, at least in regard to diabetes management, can improve glycemic control in patients.35 To improve the management of hyperglycemia in the hospital, educational interventions must be developed to teach health care practitioners effective strategies for glucose reduction. We did not quantify the changes in therapy (eg, how much insulin was changed or in what direction), only whether a change had been made. The observation that the proportion of cases on insulin at discharge was less than on admission day suggests that there may actually have been deintensification of therapy taking placesome of the cases in which therapy was changed, therefore, likely included instances of negative therapeutic momentum despite evidence of hyperglycemia. The control of inpatient hyperglycemia will likely require frequent changes in therapy, as it does in the outpatient setting, and detailed information about treatment strategies actually employed will be necessary to design educational programs.
One limitation of our analysis was that the study was retrospective, which did not allow assessment of the reasons underlying the behavior of the clinicians, such as why they did not document diabetes or change therapy. We selected a 5% sample for our study as per common methods.20, 25, 26 Thus, although the 90 patients making up the sample were randomly selected and were not different demographically from the larger population of patients admitted with diabetes, the number of cases we reviewed was small compared with the actual number of discharged patients with diabetes. Cases were diagnosed by diagnosis codes; therefore, it is likely that some diabetes cases were missed, and other patients with hyperglycemia may not have had the diagnosis even documented.8, 24 Our study design and sample size precluded a comparison of outcomes between cases with in which a consultant was involved with those in which a consultant was not involved or a comparison of cases according to type of consultant involved.1216 Finally, our study focused on noncritically ill patients; thus, our findings cannot be generalized to care provided in the intensive care unit.
There are no definitive guidelines on what method (ie, blood or bedside glucose) should be used to evaluate glycemic control in the hospital. The methods we used here can serve as means to benchmark and track improvement in glycemic control. The observations that most patients had bedside glucose monitoring ordered and that the frequency of these measurements was high compared with the frequency of actual blood glucose assessments support the idea that practitioners favored this method to evaluate the level of glycemic control in the hospital. In practice, it is bedside glucose evaluation that clinicians use to make decisions about day‐to‐day treatment of hyperglycemia. In our facility, the method for bedside glucose monitoring is standardized and is part of a quality assurance program. Moreover, the high average frequency of bedside blood glucose determination increased the chance of detecting hyper‐ and hypoglycemic events.
Current guidelines provide suggestions about target pre‐ and postprandial glucose levels for noncritically ill patients.11 However, these targets are not universally recognized.42 For instance, the Institutes for Healthcare Improvement's Prevent Surgical Site Infections initiative defines a glucose level of <200 mg/dL as its target perioperative glucose control level.43 In practice, it can be difficult to assess glucose control in terms of pre‐ and postprandial categories. Although bedside glucose monitoring in our facility is typically ordered before meals and at bedtime, in many cases prolonged periods of patient fasting, disrupted meal schedules, mismatching insulin with meals, and use of continuous parental and enteral nutritional support all make it difficult to assess pre‐ and postprandial glycemic control retrospectively. Hence, we used as our measures the value of the bedside glucose averaged over the length of the hospital stay and the number of hyper‐ and hypoglycemic events.
In general, our study was hampered by a lack of hospital‐specific process measures to evaluate the quality of inpatient diabetes care. Process measures such as the frequency of hemoglobin A1c monitoring or performance of ophthalmologic examinations,1723 which are commonly used to assess quality of diabetes care in the outpatient arena, may not be optimal variables for evaluating care in the hospital. New methods to guide efforts to improve the quality of inpatient management of diabetes and hyperglycemia are needed.
Despite these limitations, our analysis was helpful in providing direction about how to enhance the care of hospitalized patients with hyperglycemia or known diabetes. Constructing institution‐specific management guidelines for the care of inpatient diabetes and hyperglycemia would provide a yardstick against which to measure the care provided by both the hospital and the individual clinician. Educational programs can be developed to increase awareness among practitioners of the importance of inpatient glucose control and of the need to improve ongoing documentation of the problem. Exploring practitioner barriers to treatment of inpatient hyperglycemia should be an essential component of this educational process. Finally, consensus strategies on when to initiate and change therapy should be designed so that hyperglycemia in the hospital can be managed more effectively. All these areas must be addressed to assure delivery of the highest‐quality inpatient care to patients with diabetes.
Persons with diabetes have a greater risk of being hospitalized than do nondiabetic persons,1 and hospitalization was a major contributor to health care utilization and costs of patients with diabetes. In 1997, diabetes was the fourth most common comorbid condition in hospitalized patients nationwide. In 2001 in the United States, 562,000 hospital discharges listed diabetes as a principal diagnosis, and more than 4 million discharges listed diabetes in any diagnostic field.24 Nearly one third of diabetes patients may require 2 or more hospitalizations a year,5 and inpatient stays are the largest expense incurred by persons with this disease.6, 7 A substantial number of hospitalized persons are found to have unrecognized diabetes or to develop hyperglycemia during an inpatient stay.8, 9
The severity of hyperglycemia in the hospital has been linked to numerous adverse outcomes in various clinical situations, and recent studies have demonstrated the potential benefits of achieving good glucose control in the inpatient setting.10, 11 Moreover, specific inpatient‐directed interventions can improve the delivery of diabetes care.1216
Unlike the quality of outpatient diabetes care, which has been extensively profiled,1723 little is actually known about inpatient management. However, earlier reports suggested that hyperglycemia is frequently overlooked by health care personnel.8, 24 To develop intervention and educational programs will require insight into how diabetes is being addressed in the hospital. Thus, we undertook a retrospective chart review of inpatients with a discharge diagnosis of diabetes or hyperglycemia in order to assess whether these conditions were being documented and whether glucose management was being addressed.
METHODS
Setting
Our regional referral, academic teaching hospital is a 200‐bed facility in metropolitan Phoenix, Arizona. All adult general medical and surgical specialties are represented at this hospital, including renal, liver, and pancreas transplantation, a level‐2 trauma center, and an inpatient rehabilitation unit. Inpatient care is provided either by postgraduate trainees (residents) or through a separate faculty service; physician assistants and nurse‐practitioners also deliver care. Residents may be supervised by either hospitalist or nonhospitalist attendings. An electronic medical record links outpatient and inpatient records, radiology studies, and laboratory results.
Patient Selection
The study was approved by the Mayo Clinic Institutional Review Board. Patients discharged from our facility during 2003 with a diagnosis code from the International Classification of Diseases, 9th revision, Clinical Modification (ICD‐9‐CM) either for diabetes (ICD‐9‐CM code 250.0) or for hyperglycemia (ICD‐9‐CM code 790.6) were identified in a search of the hospital's electronic records. Data fields retrieved included patient age at admission, ethnicity/race, length of stay, total charges, and type of hospital service with primary responsibility for the patient's care. Because of the large number of available records, we randomly selected 5% of the total for chart review.20, 25, 26
Data Collection
Using an approach similar to that used by others,8 we reviewed admission notes, daily progress notes, and discharge summaries in order to establish whether the practitioner had recorded diabetes or hyperglycemia in the patient's chart. Subjective, objective, assessment, and plan components of notes were reviewed, and credit was given for having addressed diabetes or hyperglycemia if there was any documentation. For patients admitted for elective inpatient procedures, a preoperative outpatient evaluation conducted within 30 days of the hospitalization was counted as the admission note.
Practitioners typically make therapeutic decisions about hyperglycemia management of inpatients on the basis of daily bedside glucose measurements. In our institution, bedside glucose monitoring is performed with an instrument that scans and records patient identification, followed by direct downloading to our laboratory database. We determined whether bedside glucose levels were ordered and if so, whether they were then recorded in the daily progress notes. We determined the frequency of blood glucose measurements. Notes were examined to determine whether an assessment of hyperglycemia was made (defined as any comment in the progress note that addressed the severity of hyperglycemia or the adequacy of glucose control), and written orders were reviewed to establish any therapeutic changes. On completion of the chart reviews and entry of abstracted data into an electronic file, a link was made to the laboratory database to obtain information on bedside glucose values. We report data on notes written by the inpatient team with the principal caretaking responsibility for the patient (the primary service).
Data Analysis
Four primary outcome measures were of particular interest. First, we analyzed the percentage of patients who had diabetes or hyperglycemia documented in admission, daily progress, or discharge notes. Second, we determined the proportion of patients for whom bedside glucose measurements were ordered. Third, we calculated the percentage of patients with a written assessment of glycemic control. Finally, we examined the proportion of patients who had a change in therapy for treatment of hyperglycemia. Change in therapy was defined as any increase or decrease in the doses of an oral agent or insulin that occurred between admission day orders and the active orders on the day of discharge.
We determined the proportion of patients who had at least one hypoglycemic (glucose <70, <60, <50, <40 mg/dL) or hyperglycemic (>200, >250, >300, >350, >400 mg/dL) measurement documented by bedside monitoring. We also calculated the frequency of hypoglycemic and hyperglycemic values as the number of events per person per 100 measurements; as suggested by others,27 this approach to assessing glycemic control allows adjustment for different numbers of measurements across individuals and captures information on multiple episodes of hypo‐ or hyperglycemia in a single patient. All available bedside glucose values were averaged to determine the overall level of glucose control for the hospitalization and were divided into 3 intervals using cut points based on tertiles; the differences in the proportion of patients who had changes made in diabetes therapy was determined across tertiles using the 2 test. We determined the odds of changing therapy in the second and third tertiles of average bedside glucose relative to the first tertile. Differences in any continuous variables were evaluated using nonparametric methods (Mann‐Whitney test). Cases from all primary services were analyzed in aggregate.
RESULTS
General Patient Characteristics
Of all the patient hospitalization records for 2003, 1812 had a discharge diagnosis of diabetes or hyperglycemia. A random sample of 5% of these 1812 records yielded 90 records for chart review. The mean patient age was 68 years; 53% were male, and 90% were white.. Average length of stay was 4.8 days (Table 1). No significant differences in age, length of stay, sex, race, or source of admission (all P > .1) were detected between the 90 cases undergoing chart review and those cases that were not selected. On admission day, 63% of the patients were placed on insulin therapy, 17% on combination treatment of oral agents and insulin, and 7% on oral agents; the remaining 13% did not receive pharmacotherapy to treat their hyperglycemia. Thus, 80% were placed on insulin on the day they were admitted. By the day of discharge, 61% of the patients were on insulin therapy, either alone or in combination with oral agents. Of those on insulin therapy during their hospital stay, 35% were on a scheduled program of long‐ plus short‐acting insulin, and 65% were only on a sliding scale program.
| Characteristic | Value* |
|---|---|
| |
| Mean age (years) | 68 |
| Mean length of stay (days) | 4.8 |
| Men | 53 |
| White | 90 |
| Diabetes therapy at admission | |
| Insulin only | 63 |
| Oral agents only | 7 |
| Combination oral agents and insulin | 17 |
| Diet | 13 |
| Source of admission | |
| Physician office or clinic | 46 |
| Emergency room | 46 |
| Transfer | 8 |
| Primary service | |
| General medical | 41 |
| Surgical | 31 |
| Other | 28 |
| Teaching service | 48 |
Most patients were admitted through either an outpatient clinic (46%) or the emergency department (46%), with the remainder coming as transfers from other facilities (Table 1). Most inpatients were cared for by a general medical team (general internal or family medicine, 41%), whereas 31% were managed by one of the surgical specialties, and 28% were under the care of other specialties (eg, cardiology, transplantation, rehabilitation). Once hospitalized, most patients (94%) stayed on the original admitting service throughout their stay; 48% of patients were on a service staffed by a postgraduate trainee (Table 1). Two patients required a brief stay in the intensive care unit, but otherwise the sample was made up of noncritically ill patients.
Fifteen patients had their hemoglobin A1c measured in the hospital, with mean A1c of 7.0% 1.4%, whereas 57 patients had a documented preadmission hemoglobin A1c (average time before admission 29 weeks); their average A1c was 6.9% 1.2% (not shown).
Documentation of Diabetes
Of the 90 patients whose records were reviewed, 81 had preexisting diabetes, 3 had a diagnosis of metabolic syndrome or abnormal glucose tolerance, and 6 had hyperglycemia that developed during the admission hospitalization. When admission notes of persons with known diabetes or abnormal glucose tolerance were examined (Fig. 1), diabetes was documented in 96%. In the daily progress notes of the primary service, 62% of patients had diabetes documented at least once during their hospitalization, whereas the records of 38% had no mention of diabetes. When only those patients with known diabetes or evidence of inpatient hyperglycemia were considered, documentation of the diabetic condition was made in 60% of discharge summaries, and the need for follow‐up was noted in just 20% (Fig. 1).
Fifty‐seven percent (n = 51) of the 90 patients whose records were sampled had had some type of consultant involved with their care, but only 13% had had an endocrinology consultation. For 27 patients (30% of all 90 cases), diabetes or hyperglycemia was documented in a consultant's note; thus, there was evidence that the issue of glucose management was being addressed by someone other than a member of the primary team and that someone was not necessarily an endocrinologist. When excluding those patients whose consultant addressed diabetes or hyperglycemia, only 53% had documentation of the problems recorded in the daily progress notes (data not shown).
Recording and Assessment of Glucose Values
Most of the 90 patients whose records were reviewed (86%; n = 79) had documentation in physician orders for bedside glucose monitoring during their hospital stay (Fig. 2), and 53% had bedside glucose levels recorded in at least one daily progress note, whereas documentation was absent in 47%. A written assessment of glucose control was found in the records of 52% of the hospitalized patients; 48% lacked any evaluation of the severity of their hyperglycemia (Fig. 2). Excluding data listed from consultants, bedside glucose data was recorded for 53% of patients, and an assessment of glycemic control was made for 41%.
Glycemic Control
The average daily number of bedside glucose measurements was 4, while the daily frequency of blood glucose tests was only 1; an average of 10 bedside readings were obtained per patient. The mean bedside glucose value (averaged over the length of stay) was 170 mg/dL. At the time of admission, 33% of patients had a bedside glucose value >200 mg/dL (Fig 3, top panel), and 27% had a value >200 mg/dL before discharge (Fig 3, middle panel). Based on the bedside glucose averaged over the length of stay, 29% of patients had persistent hyperglycemia (Fig. 3, bottom panel).
Hypoglycemia was rare. Only 11% of patients had at least one bedside measurement that was <70 mg/dL; 5% a measurement of <60 mg/dL, 4% a measurement of <50 mg/dL, and 1% a measurement of <40 mg/dL (Fig. 4). The frequency of values <70 mg/dL was 1.1 per person per 100 measurements; of values <60 mg/dL, 0.66; of values <50 mg/dL, 0.18; and of values <40 mg/dL, 0.08. In contrast, hyperglycemia was common: 71% of patients had at least one value >200 mg/dL; 43% at least one value >250 mg/dLl 24% at least one value >300 mg/dL; 20% at least one value >350 mg/dL; and 9% at least one value >400 mg/dL (Fig. 4). The frequency of hyperglycemic events was 28.2 per person per 100 measurements for values >200 mg/dL, 11.2 for values >250 mg/dL, 5.3 for values >300 mg/dL, 2.4 for values >350 mg/dL, and 1.1 for values >400 mg/dL.
Changes in Therapy
Overall, changes were made in the hyperglycemia therapy of only 34% of patients. Treatment was changed for 50% of patients who had at least one glucose reading >200 mg/dL, and 89% of patients who had at least one glucose reading <70 mg/dL. Figure 5 shows whether changes in treatment occurred by tertiles of average bedside glucose. The percentage of patients with a change in therapy increased with worse hyperglycemia, although 32% in the third tertile still had not had a change in treatment. The odds of those in the second tertile having a change in therapy (compared with those in the first tertile) were 1.9 (95% confidence interval 0.556.25, P = .32), but were 5.6 (95% confidence interval 1.6818.7, P = .005) for patients in the third tertile. The frequency of glucose values <70 mg/dL was 1.8 per person per 100 measurements for patients in the first tertile, 1.1 for patients in the second tertile, but only 0.29 per person per 100 measurements for patients in the third tertile. The average number of glucose measurements >200 mg/dL per person was 2.9 per 100 measurements for patients in the first tertile, 22.7 for patients in the second tertile, and 60.0 for patients in the third tertile (not shown).
DISCUSSION
Just as clinical trials in the outpatient setting have demonstrated the benefits of good glycemic control,2830 recent studies have also suggested that treatment of hyperglycemia during hospitalization can improve outcomes.10, 11 Consequently, there has been increased attention to the management of glucose in the hospital, with recognition of the need for inpatient‐specific standards for diabetes care.10, 11, 31 Optimization of management and of education about diabetes and hyperglycemia in the hospital requires better understanding of current care practices in order to determine where to direct interventions.
Nearly all the 90 patients whose records we reviewed had preexisting diabetes or a known potential glucose abnormality that was documented either at the time of, or just prior to, hospital admission. The observation that most patients had orders for bedside glucose monitoring also indicated that practitioners were aware of the diagnosis when the patient was admitted. Although clinicians seemed to be aware of the potential problem of glucoseand the majority of clinicians did some trackinga substantial number of hospitalizations (nearly 40%) had no documentation of diabetes or hyperglycemia after admission. If diabetes was not the principal reason for hospitalization, it is possible that the primary team did not focus on managing hyperglycemia. Nonetheless, the hospital encounter does represent an opportunity to address glucose management and perhaps improve care and outcomes, even if the patient was admitted for an unrelated condition.32 Because the average length of stay was almost 5 days, there should have been sufficient time to address diabetes in most patients.
Although most patients had the condition of their diabetes documented in their discharge notes, a substantial proportion of the discharge notes did not mention an outpatient plan to follow up on the diabetes or hyperglycemia. A recent study suggested that direct referral for outpatient diabetes services increased the chances of patient follow‐up.33 Educating practitioners about the need to emphasize to patients the importance of diabetes postdischarge care is a program that could be developed and implemented in the hospital setting.
Although bedside glucose monitoring was appropriately ordered in most instances, the actual recording of values and the assessment of glucose control were documented in the records of only about half the patients during their hospitalizations. Moreover, even among patients who had high bedside glucose levels, changes in therapy often did not occur. Clinician concern about inducing hypoglycemia in hospitalized patients has been cited as a factor limiting the intensification of treatment for diabetes.34 The frequency in our facility of documented low blood glucose values was small, although there may have been unrecognized episodes. However, missed events were probably unusual, given the daily average of 4 bedside glucose measurements per patient, ongoing nursing staff contact with patients, and a formal policy to document and treat hypoglycemia. We found that hyperglycemia was far more common than hypoglycemia and that there were likely many opportunities to control blood glucose more rigorously.
Practitioners appeared to be responding to hypoglycemia, as a large proportion of the patients with a glucose reading of <70 mg/dL had a change in therapy. However, the response to hyperglycemia was delayedthe odds of therapy being changed were significant only for patients whose glucose levels were in the third tertile. Despite evidence of hyperglycemia and the low frequency of hypoglycemia of those whose glucose levels were in the second and third tertiles, a substantial proportion of patients did not have their therapy changed. Combined with the observation that glucose data and diabetes were often not documented, our data suggest that there may be a problem of clinical inertia in the inpatient setting. Clinical inertia has been defined as not initiating or intensifying therapy when doing so is indicated.35, 36 Other reports have also documented clinical inertia in the outpatient environment.23, 3741 Overcoming clinical inertia, at least in regard to diabetes management, can improve glycemic control in patients.35 To improve the management of hyperglycemia in the hospital, educational interventions must be developed to teach health care practitioners effective strategies for glucose reduction. We did not quantify the changes in therapy (eg, how much insulin was changed or in what direction), only whether a change had been made. The observation that the proportion of cases on insulin at discharge was less than on admission day suggests that there may actually have been deintensification of therapy taking placesome of the cases in which therapy was changed, therefore, likely included instances of negative therapeutic momentum despite evidence of hyperglycemia. The control of inpatient hyperglycemia will likely require frequent changes in therapy, as it does in the outpatient setting, and detailed information about treatment strategies actually employed will be necessary to design educational programs.
One limitation of our analysis was that the study was retrospective, which did not allow assessment of the reasons underlying the behavior of the clinicians, such as why they did not document diabetes or change therapy. We selected a 5% sample for our study as per common methods.20, 25, 26 Thus, although the 90 patients making up the sample were randomly selected and were not different demographically from the larger population of patients admitted with diabetes, the number of cases we reviewed was small compared with the actual number of discharged patients with diabetes. Cases were diagnosed by diagnosis codes; therefore, it is likely that some diabetes cases were missed, and other patients with hyperglycemia may not have had the diagnosis even documented.8, 24 Our study design and sample size precluded a comparison of outcomes between cases with in which a consultant was involved with those in which a consultant was not involved or a comparison of cases according to type of consultant involved.1216 Finally, our study focused on noncritically ill patients; thus, our findings cannot be generalized to care provided in the intensive care unit.
There are no definitive guidelines on what method (ie, blood or bedside glucose) should be used to evaluate glycemic control in the hospital. The methods we used here can serve as means to benchmark and track improvement in glycemic control. The observations that most patients had bedside glucose monitoring ordered and that the frequency of these measurements was high compared with the frequency of actual blood glucose assessments support the idea that practitioners favored this method to evaluate the level of glycemic control in the hospital. In practice, it is bedside glucose evaluation that clinicians use to make decisions about day‐to‐day treatment of hyperglycemia. In our facility, the method for bedside glucose monitoring is standardized and is part of a quality assurance program. Moreover, the high average frequency of bedside blood glucose determination increased the chance of detecting hyper‐ and hypoglycemic events.
Current guidelines provide suggestions about target pre‐ and postprandial glucose levels for noncritically ill patients.11 However, these targets are not universally recognized.42 For instance, the Institutes for Healthcare Improvement's Prevent Surgical Site Infections initiative defines a glucose level of <200 mg/dL as its target perioperative glucose control level.43 In practice, it can be difficult to assess glucose control in terms of pre‐ and postprandial categories. Although bedside glucose monitoring in our facility is typically ordered before meals and at bedtime, in many cases prolonged periods of patient fasting, disrupted meal schedules, mismatching insulin with meals, and use of continuous parental and enteral nutritional support all make it difficult to assess pre‐ and postprandial glycemic control retrospectively. Hence, we used as our measures the value of the bedside glucose averaged over the length of the hospital stay and the number of hyper‐ and hypoglycemic events.
In general, our study was hampered by a lack of hospital‐specific process measures to evaluate the quality of inpatient diabetes care. Process measures such as the frequency of hemoglobin A1c monitoring or performance of ophthalmologic examinations,1723 which are commonly used to assess quality of diabetes care in the outpatient arena, may not be optimal variables for evaluating care in the hospital. New methods to guide efforts to improve the quality of inpatient management of diabetes and hyperglycemia are needed.
Despite these limitations, our analysis was helpful in providing direction about how to enhance the care of hospitalized patients with hyperglycemia or known diabetes. Constructing institution‐specific management guidelines for the care of inpatient diabetes and hyperglycemia would provide a yardstick against which to measure the care provided by both the hospital and the individual clinician. Educational programs can be developed to increase awareness among practitioners of the importance of inpatient glucose control and of the need to improve ongoing documentation of the problem. Exploring practitioner barriers to treatment of inpatient hyperglycemia should be an essential component of this educational process. Finally, consensus strategies on when to initiate and change therapy should be designed so that hyperglycemia in the hospital can be managed more effectively. All these areas must be addressed to assure delivery of the highest‐quality inpatient care to patients with diabetes.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America: National Diabetes Data Group.2nd ed.Bethesda (MD):National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;1995:553–563.
- .Hospitalization in the United States, 1997: HCUP fact book no. 1: diagnosis, charges, length of stay, insurance coverage, discharge status, inhospital deaths.Rockville (MD):Agency for Healthcare Research and Quality;2000.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmfirst/table1.htm. Accessed: June 2,2005.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed: June 2,2005.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,,.Excess costs of medical care for patients with diabetes in a managed care population.Diabetes Care.1997;20:1396–1402.
- ,,,American Diabetes Association.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,,American Diabetes Association Diabetes in Hospitals Writing Committee, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591. Erratum in: Diabetes Care. 2004;27:856 and Diabetes Care. 2004;27:1255.
- ,,,,,,American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,,.Effect of physician specialty on outcomes in diabetic ketoacidosis.Diabetes Care.1999;22:1790–1795.
- ,,,.Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes.Am J Med.1995;99:22–28.
- ,,.Effects of an intervention by a diabetes team in hospitalized patients with diabetes.Diabetes Care.1997;20:1553–1555.
- ,.Nursing case management: an innovative model of care for hospitalized patients with diabetes.Diabetes Educ.1993;19:517–521.
- ,,,,.Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial.Diabet Med.2001;18:301–307.
- ,,,,,.Variation in office‐based quality. A claims‐based profile of care provided to Medicare patients with diabetes.JAMA.1995;273:1503–1508.
- ,,,,,, et al.Outpatient management of diabetes mellitus in five Arizona Medicare managed care plans.Am J Med Qual.1996;11:87–93.
- ,,,.Quality of outpatient care provided to diabetic patients: a health maintenance organization experience.Diabetes Care.1996;19:601–6.
- United States General Accounting Office: report to the Chairman, Subcommittee on Health and Environment, Committee on Commerce, House of Representatives.Medicare: most beneficiaries with diabetes do not receive recommended monitoring services. GAO/HEHS‐97–48.1997.
- ,,,,.Care of patients with type II diabetes: a study of family physicians' compliance with clinical practice guidelines.J Fam Pract.1997;44:374–381.
- ,,,,,.A diabetes report card for the United States: quality of care in the 1990s.Ann Intern Med.2002;136:565–574.
- ,,,University HealthSystem Consortium (UHC) Diabetes Benchmarking Project Team.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,,.An audit of the management and outcome of hospital inpatients with diabetes: resource planning implications for the diabetes care team.Diabet Med.1992;9:753–755.
- .Improving outcomes in public health practice: strategy and methods.Gaithersburg (MD):Aspen Publishers;1997:175–213.
- ,,,,,.Outpatient diabetes management of Medicare beneficiaries in four Mississippi fee‐for‐service primary care clinics.J Miss State Med Assoc.1999;40:8–13.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- The Diabetes Control and Complications Trial Research Group.The effect of intensive treatment of diabetes on the development and progression of long‐term complications in insulin‐dependent diabetes mellitus.N Engl J Med.1993;329:977–986.
- UK Prospective Diabetes Study (UKPDS) Group.Intensive blood‐glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33).Lancet.1998;352:837–53. Erratum in: Lancet. 1999;354:602.
- UK Prospective Diabetes Study (UKPDS) Group.Effect of intensive blood‐glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34).Lancet.1998;352:854–65. Erratum in: Lancet. 1998;352:1557.
- ,,.Current standards of care for inpatient glycemic management and metabolic control: is it time for definite standards and targets?Endocr Pract.2004;10(Suppl 2):10–12.
- ,.Windows of opportunity to improve diabetes care when patients with diabetes are hospitalized for other conditions.Diabetes Care.2001;24:1371–1376.
- ,,, et al.Inpatient to outpatient transfer of care in urban patients with diabetes: patterns and determinants of immediate postdischarge follow‐up.Arch Intern Med.2004;164:447–453.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–1500.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- .Management of older hypertensive patients: is there a difference in approach?J Clin Hypertens (Greenwich).2003;5(Suppl 4):11–16.
- ,,, et al.Narrowing the gap in hypertension: effectiveness of a complex antihypertensive program in the elderly.Dis Manag.2004;7:235–243.
- ,,, et al.Clinical inertia in the management of Type 2 diabetes metabolic risk factors.Diabet Med.2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med.2003;163:2677–2678.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available from: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed June 2,2005.
- ,,,,.Diabetes‐related hospitalization and hospital utilization. In:Diabetes in America: National Diabetes Data Group.2nd ed.Bethesda (MD):National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases;1995:553–563.
- .Hospitalization in the United States, 1997: HCUP fact book no. 1: diagnosis, charges, length of stay, insurance coverage, discharge status, inhospital deaths.Rockville (MD):Agency for Healthcare Research and Quality;2000.
- Centers for Disease Control and Prevention. Hospitalization for diabetes as first‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmfirst/table1.htm. Accessed: June 2,2005.
- Centers for Disease Control and Prevention. Hospitalizations for diabetes as any‐listed diagnosis. Available from: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm. Accessed: June 2,2005.
- ,,,.Multiple hospitalizations for patients with diabetes.Diabetes Care.2003;26:1421–1426.
- ,,,.Excess costs of medical care for patients with diabetes in a managed care population.Diabetes Care.1997;20:1396–1402.
- ,,,American Diabetes Association.Economic costs of diabetes in the US in 2002.Diabetes Care.2003;26:917–932.
- ,,,,.Unrecognized diabetes among hospitalized patients.Diabetes Care.1998;21:246–249.
- ,,,,,.Hyperglycemia: an independent marker of in‐hospital mortality in patients with undiagnosed diabetes.J Clin Endocrinol Metab.2002;87:978–982.
- ,,,,,,American Diabetes Association Diabetes in Hospitals Writing Committee, et al.Management of diabetes and hyperglycemia in hospitals.Diabetes Care.2004;27:553–591. Erratum in: Diabetes Care. 2004;27:856 and Diabetes Care. 2004;27:1255.
- ,,,,,,American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control, et al.American College of Endocrinology position statement on inpatient diabetes and metabolic control.Endocr Pract.2004;10:77–82.
- ,,,.Effect of physician specialty on outcomes in diabetic ketoacidosis.Diabetes Care.1999;22:1790–1795.
- ,,,.Impact of endocrine and diabetes team consultation on hospital length of stay for patients with diabetes.Am J Med.1995;99:22–28.
- ,,.Effects of an intervention by a diabetes team in hospitalized patients with diabetes.Diabetes Care.1997;20:1553–1555.
- ,.Nursing case management: an innovative model of care for hospitalized patients with diabetes.Diabetes Educ.1993;19:517–521.
- ,,,,.Evaluation of a hospital diabetes specialist nursing service: a randomized controlled trial.Diabet Med.2001;18:301–307.
- ,,,,,.Variation in office‐based quality. A claims‐based profile of care provided to Medicare patients with diabetes.JAMA.1995;273:1503–1508.
- ,,,,,, et al.Outpatient management of diabetes mellitus in five Arizona Medicare managed care plans.Am J Med Qual.1996;11:87–93.
- ,,,.Quality of outpatient care provided to diabetic patients: a health maintenance organization experience.Diabetes Care.1996;19:601–6.
- United States General Accounting Office: report to the Chairman, Subcommittee on Health and Environment, Committee on Commerce, House of Representatives.Medicare: most beneficiaries with diabetes do not receive recommended monitoring services. GAO/HEHS‐97–48.1997.
- ,,,,.Care of patients with type II diabetes: a study of family physicians' compliance with clinical practice guidelines.J Fam Pract.1997;44:374–381.
- ,,,,,.A diabetes report card for the United States: quality of care in the 1990s.Ann Intern Med.2002;136:565–574.
- ,,,University HealthSystem Consortium (UHC) Diabetes Benchmarking Project Team.Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change.Diabetes Care.2005;28:337–442.
- ,,,.An audit of the management and outcome of hospital inpatients with diabetes: resource planning implications for the diabetes care team.Diabet Med.1992;9:753–755.
- .Improving outcomes in public health practice: strategy and methods.Gaithersburg (MD):Aspen Publishers;1997:175–213.
- ,,,,,.Outpatient diabetes management of Medicare beneficiaries in four Mississippi fee‐for‐service primary care clinics.J Miss State Med Assoc.1999;40:8–13.
- ,,.Glycemic control and sliding scale insulin use in medical inpatients with diabetes mellitus.Arch Intern Med.1997;157:545–552.
- The Diabetes Control and Complications Trial Research Group.The effect of intensive treatment of diabetes on the development and progression of long‐term complications in insulin‐dependent diabetes mellitus.N Engl J Med.1993;329:977–986.
- UK Prospective Diabetes Study (UKPDS) Group.Intensive blood‐glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33).Lancet.1998;352:837–53. Erratum in: Lancet. 1999;354:602.
- UK Prospective Diabetes Study (UKPDS) Group.Effect of intensive blood‐glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34).Lancet.1998;352:854–65. Erratum in: Lancet. 1998;352:1557.
- ,,.Current standards of care for inpatient glycemic management and metabolic control: is it time for definite standards and targets?Endocr Pract.2004;10(Suppl 2):10–12.
- ,.Windows of opportunity to improve diabetes care when patients with diabetes are hospitalized for other conditions.Diabetes Care.2001;24:1371–1376.
- ,,, et al.Inpatient to outpatient transfer of care in urban patients with diabetes: patterns and determinants of immediate postdischarge follow‐up.Arch Intern Med.2004;164:447–453.
- ,,, et al.Hospital hypoglycemia: not only treatment but also prevention.Endocr Pract.2004;10(Suppl 2):89–99.
- ,,, et al.Diabetes in urban African‐Americans. XVI. Overcoming clinical inertia improves glycemic control in patients with type 2 diabetes.Diabetes Care.1999;22:1494–1500.
- ,,, et al.Clinical inertia.Ann Intern Med.2001;135:825–834.
- .Management of older hypertensive patients: is there a difference in approach?J Clin Hypertens (Greenwich).2003;5(Suppl 4):11–16.
- ,,, et al.Narrowing the gap in hypertension: effectiveness of a complex antihypertensive program in the elderly.Dis Manag.2004;7:235–243.
- ,,, et al.Clinical inertia in the management of Type 2 diabetes metabolic risk factors.Diabet Med.2004;21:150–155.
- ,.Clinical inertia: errors of omission in drug therapy.Am J Health Syst Pharm.2004;61:401–404.
- .Overcome clinical inertia to control systolic blood pressure.Arch Intern Med.2003;163:2677–2678.
- ,.Counterpoint: inpatient glucose management: a premature call to arms?Diabetes Care.2005;28:976–979.
- Institute for Healthcare Improvement. Getting started kit: prevent surgical site infections. Available from: www.ihi.org/NR/rdonlyres/00EBAF1F‐A29F‐4822‐ABCE‐829573255AB8/0/SSIHowtoGuideFINAL.pdf. Accessed June 2,2005.
Copyright © 2006 Society of Hospital Medicine